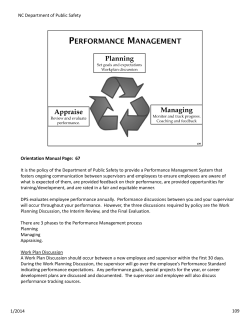
Orientation Manual Interns and Residents 2013 / 2014
Orientation Manual Interns and Residents 2013 / 2014 1 Welcome to the PAH Emergency Department Your role in the emergency department team is vital. Orientation To function effectively in your role you must read / watch the following prior to commencing your first shift: PAH ED General Information Intern and Resident Orientation Manual PAH ED Clinical Practice Manual PAH ED Orientation Videos These manuals can be found on the PAH ED Intranet site or the emergpa website, www.emergpa.net . The Emergency Department has developed an orientation package that is available online via the internet. The orientation package is available via the online learning platform: 'iLearn@Qhealth' http://ilearn.health.qld.gov.au/course/view.php?id=275&edit=0&sesskey=pkerWtJp5p This website has the advantage of being accessible from home (unlike QHEPS), as well as allowing you to track your progress as you work through the resources available. It can be accessed at any time of day and at your convenience. We do require that you work through the learning material prior to starting in the unit. Your Ilearn@QHealth login will be your surname followed by your first initial. Your password is currently set as the generic 'changeme'. When you first login to the site please change your password and please keep this safe. For example: Name : John Smith Login: smithj Password: changeme If you forget your login or password you can request a reminder on the login page that will be sent to your Groupwise email account. It is vital you undertake the above as there is only a brief orientation to the ED held upon commencing your first shift. The expectation is that you will have been orientated by undertaking the above reading. In addition, at some time during your first shift you will need to make contact with Jillian Vernon (ED Office Manager), or one of her support staff, to ensure we have your correct contact details etc. Learning Objectives Your term in Emergency Medicine is likely to be the only time during your pre-vocational training where you have the opportunity to be the first doctor to see patients with undifferentiated medical problems. The primary objective of your term is to learn how to safely approach the patient with undifferentiated illness. To obtain this primary objective, you will be expected to achieve the following goals: Be a member of a resuscitation team, under direction Understand that management of critical conditions may precede full assessment Be able to take an accurate, focussed history 2 Be able to perform a competent, focussed physical examination Be able to create a problem list for each patient Be able to formulate basic management plans Be able to carry out management plans, with assistance Be competent at communicating with families, nursing staff, allied health staff and medical staff Be a reliable team member These learning objectives are attainable primarily through seeing patients on the floor. Your time in formal teaching will be complementary to your experience with patient management. Dress Code Junior medical officers are to dress to the standard they would for other terms within the hospital. For men, ties are not required. Communication The majority of communication will occur via email so ensure you check your GroupWise account regularly. Passwords You need the following passwords to work in the ED: Novell Login EDIS password (will be emailed to you) Auslab password (Pathology) PACS password (Radiology) If you do not have any of these please see the ED Office Manager prior to commencing. Term Content Casemix and Workload PAH ED has a relatively high acuity workload with complex medical cases and multi-system trauma being a feature. An expansive knowledge and skill set is required with particular emphasis on acute resuscitative skills. PAH ED sees approximately 55 000 presentations per year, with a 30% admission rate. A high proportion arrives by QAS (50%) which underlines the high acuity of the presentations the ED manages. Being one of the 3 major trauma centres for QLD, PAH ED attends to a high number of trauma cases. With access to interventional cardiologists and a catheter lab, acute cardiology patients are also a feature of PAH ED. Mental health patients (8% of PAH ED’s presentations) are catered for by a dedicated ED Mental Health Service which operates 24/7. PAH ED has its own 14 bed Short Stay Ward for ED patients and access to Hospital in the Home and Nursing Home programs. Expected Level of Involvement Your role in the team is vital. How to function effectively in your role is outlined in the PAH ED Clinical Practice Manual. 3 Managing your Workload/ Debriefing The ED can be a busy and stressful environment. Some adapt more readily than others to this. To assist in managing your workloads during the term consider the following: Take your breaks throughout the shift (patients are always arriving and always waiting to be seen). Allow 30 minutes for lunch and tea. Try to take your lunch break if you are on a day shift after 13:00 when the evening team commence. Smaller breaks (5-10 minutes) may also be useful to ‘recharge your batteries’ during your shift. Try to finish your shift on time. Though it is often busy and you may be requested to stay back – when possible, aim to leave on time. Thus, avoid picking up potentially complicated patients within the last hour of your shift – let your registrar know and they will allocate you an appropriate patient. Enjoy your days off. Debriefing is an important part of our support to you. If you feel at all concerned about anything that happens to you in the Emergency Department please talk to the ED consultant or registrar or the RN in charge at the time, who will assist you with your concerns. Otherwise see Dr Tina Bazianas or Dr Jonathon Isoardi, who are the contacts for resident support issues. Don’t be afraid to ask. Scope of Practice Please refer to APPENDIX A, titled “Scope of Practice for Interns Working at the PA Hospital & Secondment Hospitals” for the Hospital policy on Scope of Practice. The Emergency Department is a highly supervised environment. All invasive procedures, apart from (most) peripheral IV cannulation, will be supervised directly by a Registrar or Consultant. Expectations of practice are well described in the PAH ED Clinical Practice Manual (CPM). If, at any stage, you are unsure about any aspect of patient care, please ask your supervisor for help. Educational Opportunities The consultants and registrars within the ED place a high priority on resident medical education. The education provided takes a number of forms. ‘Coalface’ teaching – every patient a resident sees within the ED will be discussed with senior ED medical staff. This allows for one on one interaction and education with a consultant or registrar many times throughout a shift. These informal interactions form the majority of the teaching within the ED. Discussing theory in the practical setting of seeing a patient is commonly the most productive means of learning and retaining new information. MoLIE program (More Learning for Interns in Emergency) – Interns (only) will be involved in dedicated MoLIE teaching sessions. More detail is provided in APPENDIX B. Morning teaching sessions – House Officers (only) - At 08:00 Monday – Friday (except Thursdays) there are 30 minute multidisciplinary teaching sessions run by a consultant or registrar for the resident and nursing staff on duty. If you are coming on duty for your shift, delay picking up patients until after the tutorial. Occasionally, due to excessive activity in the department the tutorial may have to be cancelled. The education syllabus is based around a weekly educational theme, with daily topics addressing the week’s theme. 4 Weekly syllabus Orientation Week Acute Cardiology in the ED Shortness of breath in the ED Infection in the ED Shock in the ED Trauma Acute Orthopaedics Acute Neurology Toxicology and Toxinology Review Week Facility Education Program for Interns – The Medical Education Unit in the Hospital coordinates Intern Training on Tuesdays and Fridays from 12:00 to 13:00. If you are not rostered to work during this time, you are welcome to attend these sessions. The MoLIE program will thoroughly cover interns’ educational needs during their term in Emergency Medicine. EMERGENCY MEDICINE TRAINING – Finally if at any stage before, during or after your ED term you would like more information about undertaking a career in emergency medicine please contact Dr Darren Powrie or Dr Jonathon Isoardi (Co-Directors of Emergency Medicine Training). Rostering The roster is a 10 week rotating roster with 4 shifts per week. Day shifts start at 08:00 and end at 18:30. Evening shifts start at 13:00 and end at 23:30. Night shifts start at 22:00 and end at 08:30. MoLIE shifts start at 08:30 and end at 17:00. Night shifts are split into Monday – Thursday and Friday – Sunday. Each day there is one person from the ‘day shift’ assigned to remote call after their finishing time (1830). They are on-call until 08:00 the following morning and may be called in to assist with excessive department activity. Week-ends also have an assigned remote-call person to cover for potential sick leave. Hence, interns will be rostered for 76 hours per fortnight, except during Line A of the roster (when it will be 78). House officers will be rostered for 80 hours per fortnight. Any changes to the roster (e.g. swaps, leave etc) must be approved by the Office Manager, Jillian Vernon. Essentially, swaps in the roster can only occur with people at the same level (i.e. intern with intern; SHO with SHO) and should only occur within the same fortnightly pay period. Any changes to the roster (e.g. shift swaps, sick leave) are to be written on the Roster Adjustment Form which is located in a folder within the medical write-up area. An example of the intern roster is attached (APPENDIX C). Please note, this is an example only. The roster may change from term to term, and even week to week depending on staff flux. Please use the most recent version of the roster, which will be distributed by Jillian Vernon, the ED Office Manager. The House Officer Roster is more complicated and changes frequently for many reasons. As such, it is not included in the Orientation Manual, but can be obtained from Jillian Vernon. Handover Handover is a crucial part of patient safety in the Emergency Department. It also acts as a good opportunity for learning. This topic is covered in the PAH ED CPM under “Finishing your shift”. 5 Other general points PAY SHEETS Time sheets are generated for the Pay Office automatically as per your roster. Any changes to these hours that occur during the pay period need to be documented on a Roster Adjustment Form (RAF) at the end of each shift (i.e. document un-rostered overtime, sick leave, shift swaps etc). The Roster Adjustment Form is located in a folder within the medical write-up area. SICK LEAVE You must notify the Consultant (or registrar) on the floor (3176 7215) and the Office Manager (Jillian Vernon 3176 7513 or 0421871368 24/7) as early as possible if you are unable to attend for your shift due to illness. This allows the remote call doctor to be called in to cover your shift. WARD CALL There is no ward call associated with rotations to ED. Supervision The Educational Supervisor responsible for co-ordinating intern and house officer assessments is Dr Tina Bazianas. The MoLIE, and House Officer teaching co-ordinator is Dr Jonathon Isoardi. You can approach any of the consultants or registrars for advice or help. As previously stated, the Emergency Department is a highly supervised environment. During your shift, there will always be at least two supervising registrars on the floor. All the registrars in this department are Advanced Trainees in Emergency Medicine. You will be allocated a specific registrar to whom you will report, at the start of each shift. From the hours of 0800 to 2200, there will be at least one consultant on the floor. From 2200 – 0800 overnight, there will be a consultant on call from home. See ATTACHMENT: PAH INTERN SUPERVISION POLICY for the Hospital’s supervision policy. Term Assessment You will have assessments at mid-term (week 5) and end of term (week 10). All consultants and registrars provide input to your assessment which is conducted with one of the consultant staff. An assessment form is completed and will be discussed with you. A timetable for the assessments will be posted around the ED by the Office Manager at the appropriate time. See ATTACHMENT: PAH INTERN ASSESSMENT POLICY If an assessment at mid term identifies some problems / issues resulting in sub-standard performance, an IPAP (Improving Performance Action Plan) will be formulated during a meeting between the junior doctor, the Educational Supervisor and a member of the Medical Education Unit. The goal here is to work together to improve the junior doctor’s performance towards satisfactory completion of the term. See ATTACHMENTS: RESIDENT MEDICAL OFFICER ASSESSMENT FORM PAH POLICY – INFORMING INTERN OF SERIOUS CONCERNS 6 APPENDIX A Scope of Practice for Interns Working at the PA Hospital & Secondment Hospitals Scope of Practice – What the Intern is NOT able to do Initiate patient treatment/management or change patient treatment/management without discussion and approval from clinical supervisor. Obtain consent for surgical operations/procedures with which the Intern is not familiar (PAH Hospital Wide Policies and Procedures: 01542/v5/02/2008) Scope of Practice – What the Intern is able to do when rostered to work 1. Interns must be familiar and act appropriately in accordance with the Queensland Health Intern Induction and Orientation Program Framework (Integrated Resource Manual 3.7-12) 2. Must comply with PAH guidelines/protocols (PAH Hospital Wide Policies and Procedures 01516/v6/05/2009) for communicating with staff involved in patient care including informing nursing, allied health and other relevant staff regarding instructions from the clinical supervisor/s regarding patient treatment and management. 3. Must complete documentation regarding patient treatment/management as per the PAH Hospital Wide Policies and Procedures (60059/v1/09/2007) 4. Contact directly the Consultant and/or Registrar/PHO re any change in the status of their allocated patients. 5. Attend rostered duties in ward, theatre and clinics as appropriate and punctually. 6. Order tests/investigations as agreed by the Consultant and/or Registrar/PHO. 7. Access results of patients, review these tests and communicate unexpected findings to Consultant and or Registrar/PHO. 8. Prescribe medications as directed by the Consultant and/or Registrar/PHO and notify if any problems occur as a result. 9. Complete patient discharge summaries. 10. Carry pagers whilst on duty (other than in ED or off site) and check pager is working as required. 11. Participate in Rapid Response Team as per roster. 12. Participate in rostered after hours ward call shifts. 7 APPENDIX B MoLIE (More Learning for Interns in Emergency) Also known as BARRIE (Better Arrangements, Resources and Role-Modelling for Interns in Emergency) Welcome to the PA and QE2 Emergency Department BARRIE program. BARRIE has been developed to promote better learning opportunities for interns during their term in the PA or QE2 Emergency Department. The program is co-ordinated by: Dr Jonathon Isoardi Angela O’Connor Catherine Weldon FACEM Medical Education Officer Administration Officer If you have any problems during your Emergency term, please approach one of us so that we can work together to resolve the issue. We will not be involved in assessing your performance during the term. Your week will comprise of three clinical shifts and one BARRIE day. During this BARRIE day, you will participate in two interactive teaching sessions. The sessions will go from 08:30 – 12:30, and 13:00-17:00. There will be a different facilitator for each session. For PA interns, you will not be expected to attend BARRIE during your run of nights from Monday to Thursday (line A of the roster). Otherwise, attendance is part of your job and hence compulsory. As for your clinical shifts, punctuality is required for BARRIE. There are 20 modules that will run during your term. They are listed below, and will run in the listed order. BARRIE MODULES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. General approach to the ED patient The patient with chest pain The breathless patient Abdominal pain in the ED Altered level of consciousness The poisoned patient The patient with PV bleeding Collapse and syncope The multiply injured patient Minor injuries ENT and eye complaints The febrile patient Resuscitation Communication in the ED Paediatrics Environmental injuries The patient with headache The patient with GIT bleeding The patient with weakness Case presentations You will only need to bring yourself and a pen to the sessions. BARRIE will be run in on eof the Education / Conference Rooms within the ED Administration Area.. No formal assessment will be made of your performance during the teaching sessions. Please enjoy yourself and the company of your peers. The educational value of BARRIE is dependent on intern participation, so come prepared to contribute to discussion. You will be asked to evaluate the BARRIE program and your feedback is greatly appreciated. 8 APPENDIX C INTERN ROSTER A B C D E F G H I J K L MondayTuesda WednesThursd Friday SaturdaSundayHours N N N N OFF OFF OFF 40 OFF M E E E OFF OFF 38 OFF M E E E OFF OFF 38 D® M OFF OFF OFF D D 38 D M E E OFF OFF OFF 38 D® E OFF M D OFF OFF 38 OFF E M OFF OFF E E 38 D® 38 E OFF M OFF OFF D E OFF M OFF OFF E E 38 OFF OFF M OFF N N N 38 OFF OFF M OFF D E E 38 LSA OFF M D D OFF OFF 38 D 0800-1830 D® 0800-1830 + ON CALL TO 0800 0830-1700 M E 1300-2330 LSA 1300-2330 subacute N 2200-0830 9 PRINCESS ALEXANDRA HOSPITAL PROCEDURE MANUAL Section: Support Procedure No. 52046/v2/06/2013 Procedure Title: Intern Supervision – Medical Education Unit Review Officer: Medical Education Unit nd Review Summary: 2 Version Applicable To: Princess Alexandra Hospital Intern and training Program Interns and Supervisors Last Review Date: 06 2013 Purpose: To ensure that all Interns are supervised by appropriately qualified medical practitioners so as to ensure a safe clinical environment for patients and an effective and safe learning environment for Interns as they acquire appropriate skills and attitudes in their professional development. Next Review Date: 06 2015 Authority: Director of Clinical Training ……………………………………… Signature of Authorising Officer Authorised to Undertake the Procedure: Definitions Supervisors • Clinical supervisors at the Princess Alexandra Hospital are Replaces: 52046v1 senior doctors, employed at the level of Principal House Key Words: Intern, Supervision Officer/Registrar or above. • Shift supervisors are senior doctors, employed at the level of Accreditation Reference: Principal House Officer/Registrar or above, available in the junior PMCQ Accreditation Standard and doctor’s immediate work area during all shifts in which the junior Guidelines – Function 1 Standard 1, Function 1 Standard 6, Function 2 doctor is working. Standard 8. • Unit educational supervisors are senior doctors responsible for deciding on whether performance is satisfactory or not satisfactory. This person may or may not be a clinical supervisor. • Ward call supervisors may be on-site shift supervisors and/or senior doctors who are also on call in cases of emergency. Levels of Intern Supervision • Level 1 Supervision – The supervisor is physically present with the intern during the performance of the intern’s duties • Level 2 Supervision – The supervisor is not physically present, but is immediately available on site if required by the intern without impediment to access. Risks and Precautions: Non compliance with this policy will result in risk rating of EXTREME – immediate action required. Procedure: • • Interns employed by Princess Alexandra Hospital must be supervised at all times, regardless of which shift they are working, or the location of their workplace. The responsibility for ensuring the appropriate level of supervision is provided to the interns lies with the Executive Director of Medical Services of the facility to which the Intern is allocated. In Practice 1. Each junior doctor’s clinical and/or educational supervisor will be clearly identified at the beginning of each term. 2. Supervisors provide overall supervision of the junior doctor’s work performance and training. In this respect, they are responsible for implementing the Unit’s education programs, and have mentoring, teaching, appraisal and assessment roles. 3. Supervisors must ensure that supervision of Interns: Printed version is an uncontrolled copy 1 - Is adequate at all times, to ensure safe patient care; and - Provides a safe and valuable learning environment for the Intern; and - Meets the criterion as per the definition of Level 1 or Level 2 supervision. In considering this, clinical and educational supervisors should be aware of the skills and experience and workloads of all clinicians who may be providing supervision at any time during an allocated term. 4. Each junior doctor’s shift supervisor will be clearly identified at the beginning of each shift. 5. Shift supervisors provide direct supervision of the junior doctor’s work. They provide mentoring, teaching and appraisal, and provide appraisal information to the educational supervisor who completes the junior doctor’s term assessment. 6. Junior doctors on ward call will be supervised by the shift supervisor in the work area to which they have been rostered. The assessment of performance on ward call is included in the full assessment process. 7. At all times, junior doctors and shift supervisors are able to contact more senior doctors who may or may not be on site but will be contactable by telephone. 8. Supervisors “on call” must be within thirty (30) minutes from the hospital. 9. Where the Director of Clinical Teaching or Executive Director Medical Services is notified of concerns regarding the adequacy of supervision of an intern, an investigation is undertaken with a degree of urgency to: a) Obtain relevant background detail, e.g. failure to advise of name of delegated supervisor during a period of absence of term supervisor or failure to advise change of roster in event of notification of inadequacy of supervision on ward call. b) Ensure that steps are put in place to provide adequate supervision. Delegation of Responsibility for Supervision • If the Interns unit educational supervisor is absent or unavailable then the second educational supervisor in the unit will supervise the Intern. The unit educational supervisor is always a consultant. • If the shift supervisor who is a registrar or principal house officer is absent or unavailable, then the consultant rostered on for the team will supervise. • If the ward call supervisor who is a registrar or principal house officer is absent or unavailable, then the consultant on call or consultant for the patient must be contacted for supervision. • The Medical Superintendent on call must be contacted by an Intern if no other supervisors are available. Evaluation Method: General Clinical Education Committee will evaluate this procedure against feedback provided by Interns each term. Recommendations will be forwarded to individual Term Supervisors and Medical Services Directors Committee. HYPERLINK TO: Medical Education Unit Procedures Printed version is an uncontrolled copy 2 PRINCESS ALEXANDRA HOSPITAL PROCEDURE MANUAL Section: Support Procedure No. 52044/v2/06/2013 Procedure Title: Intern Assessment – Medical Education Unit Review Officer: Medical Education Unit nd Review Summary: 2 Version Applicable To: Interns, Intern Supervisors, MEU Staff Last Review Date: 06 2013 Next Review Date: 06 2015 Purpose: To ensure that appraisal (formative assessment) and assessment (summative assessment) at Princess Alexandra Hospital provide ongoing constructive feedback to Interns, so that each Intern’s training and professional development objectives are met and that the requirements of the Medical Board of Australia are satisfied when considering an application for removal of probationary conditions. Authority: Director of Clinical Training ……………………………………… Signature of Authorising Officer Replaces: 52044v1 Key Words: Assessment Accreditation Reference: PMCQ Accreditation Standards and Guidelines – Function 1 Standard 3, Function 2 Standard 9. Definitions: Intern Education and Training Program (IETP) The Intern Education and Training Program is the organisation’s medical education and training program for Interns, which should comprise a formal alignment or rotation of Terms and the Facility Education Program (FEP). Assessments of the intern in the rotation of Terms are collated to provide evidence to the Medical Board that an intern is suitable to be fully registered in Queensland. Assessment Assessment is a crucial component of the Intern Education and Training Program (IETP) and essential for Intern learning and development. The Princess Alexandra Hospital and affiliated Metro South Hospitals are responsible for ensuring that the Postgraduate Medical Council of Queensland (PMCQ) state-wide assessment process is implemented and has a process for distributing the assessment tool to supervisors and Interns and for return of these forms to the Director Clinical Training (DCT) for review. The process of review of these assessment forms should also be clearly identified including remediation processes should problems be identified. Assessors The designated educational supervisors gather information on an intern’s performance during their term allocated to a specific unit. Performance is assessed by direct observation, and from reports provided by other supervisors (as listed below) and from nursing and allied health staff. Educational supervisors are senior doctors, employed at the level of Principal House Officer/Registrar or above, in Hospitals within the Metro South Health Service District and elsewhere. If an Intern is allocated to a primary care setting off campus in a non compulsory term supervision is provided by a vocationally trained General Practitioner. Shift supervisors are the senior doctors available in the junior doctor’s immediate work area during any rostered shifts. They provide information to the educational supervisor about the intern’s performance. Ward call supervisors may be on-site shift supervisors and/or senior doctors who are also on call in cases of emergency and who are responsible for assessment of the intern while on ward call. Feedback Interns receive appraisal on their performance from their supervisor/s at mid term and an assessment of performance in a formal interview process at end of term. The midterm feedback process is necessary to provide a learning opportunity for Interns, enabling them to review and adjust their performance, and provides the Intern with an opportunity to strengthen skills before the end of term summative assessment. Risks and Precautions: Non compliance with this procedure will compromise accreditation status of the Facility and/or unit and compromise the Intern’s full registration with the Medical Board of Australia. Printed version is an uncontrolled copy 1 Procedure: Assessment refers to the process of describing monitoring, reviewing and reporting on the performance of interns employed within the Metro South District. Assessment comprises an appraisal of performance at mid term and a summative assessment at the end of a term. The Postgraduate Medical Council of Queensland (PMCQ) state-wide assessment form is utilised for the purpose of documentation. The Princess Alexandra Hospital utilises an electronic database called PROSE (Princess Alexandra Hospital Resident Medical Officer Online System of Assessment and Evaluation) for this purpose. Some hard copy assessment forms are submitted. The completed assessment form must be viewed by the Intern and the Intern be given an opportunity to provide written comment. Where Princess Alexandra Hospital Interns are allocated to terms off campus, there will be a Memorandum of Understanding which outlines specific obligations of the Facility in terms of supporting Interns with supervision, assessment and feedback and a description of how this information is given to the Interns and provided to the Primary Allocation Hospital. Where Princess Alexandra Hospital Interns are rostered to ward call they are assessed using a Ward Call Assessment Form which is completed by the clinical supervisor for the shift. Intern performance is assessed as satisfactory, unsatisfactory or unable to be assessed. The level of contact upon which the assessment is based is also noted by the clinical supervisor. The Intern also has an opportunity to evaluate the level of support received on the shift and if perceived as unsatisfactory, comments can be made by the Intern. When an assessment indicates that an Intern’s performance requires assistance through the development of an Improving Performance Action Plan (as per Postgraduate Medical Council of Queensland Guidelines), the process should involve the Intern, Medical Education Officer, Director of Clinical Teaching and Executive Director Medical Services if necessary. All summative assessment forms must be returned to the Medical Education Unit in a timely fashion to enable completion of the annual Intern Reports for the Medical Board of Australia. In Practice 1. At the beginning of the intern year, the Assessment procedure and the process of assessing interns both within the Facility and within affiliated South Metro facilities where the intern may be seconded, is to be outlined. 2. The Orientation Assessment package is to contain copies of: - The end of term assessment form, - The Assessment procedure document and process for assessing interns, - The process for assessing clinical skills, - The Supervision Procedure, - The Grievance Procedure, - A list of possible advocates for interns. 3. At Term orientation Interns receive: - An outline of the assessment processes of that particular Term, - A date of mid-term Assessment (if longer than five weeks), - Identification of the educational Supervisor, - Identification of ward call supervisors and shift supervisors, - A copy of the ward call assessment form and process, - A list of the personnel responsible for giving feedback and appraisals, and how this information will be collated, e.g. direct observation, reports from supervisors, and information from co-workers such as nursing and allied health staff. 4. Feedback sessions should be incorporated within a shift where possible as part of debriefing and should include feedback by others (e.g. nursing and allied health staff) observing the doctor’s performance. 5. Where ward call is allocated ensure that the assessment process addresses the following: - The clinical supervisor for ward call is included in the full assessment process. - The Intern is aware of any change in assessment procedures. - The educational supervisor for the compulsory term liaises with both shift and ward call supervisors. Printed version is an uncontrolled copy 2 6. The process for instigating the Improving Performance Action Plan (IPAP): - A junior doctor who has been rated on any two of the criteria on the assessment form as “Requires further development” (RFD) or any one “Requires substantial assistance” (RSA), is to be informed of the need for the development of an Improving Performance Action Plan. The Director of Clinical Training or the Medical Education Officer in the Medical Education Unit is to be involved in this process. - An Improving Performance Action Plan (IPAP) identifies problems/issues and includes strategies to assist the Intern and the supervising clinician to improve the Intern’s performance. The Intern must agree to the Improving Performance Action Plan before signing the Improving Performance Action Plan Form. - The objective of the Improving Performance Action Plan is to improve the likelihood that an “unsatisfactory progress” at mid term may become a “satisfactory progress” at the end of term. - If at the end of a term, a junior doctor receives an “unsatisfactory progress”, an Improving Performance Action Plan is to be completed and discussed with the Clinical Supervisor in the next rotation. - An “unsatisfactory progress” at the end of a term may delay general registration for an Intern. - All “unsatisfactory progress” reports for junior doctors will be notified to the Executive Director of Medical Services by Medical Education Unit (MEU) staff. - Where the Intern has an Improving Performance Action Plan and is allocated to a term off campus this information will be shared with the Director of Clinical Training (DCT) at the secondment facility. 7. Confidentiality of intern assessment data must be safeguarded. The Medical Education Unit will retain a copy of the form for registration, reference and ongoing performance management purposes. The assessment forms will be stored as confidential documents in a locked location. 8. The Medical Education Unit at the Princess Alexandra Hospital provides notice of impending end of term or mid term assessment via email. Assessments returns are recorded in an electronic data base and reports generated from this are presented at the General Clinical Education Committee. Evidence 1. End of term/mid term assessment form. 2. Assessment Process. 3. Assessment form returns report. 4. Copy of policy for informing Intern of serious concerns. 5. Copy of process for assessing clinical skills and records kept. Evaluation Method: The General Clinical Education Committee will evaluate this procedure against feedback provided by General Clinical Education Committee Members. Printed version is an uncontrolled copy 3 RESIDENT MEDICAL OFFICER ASSESSMENT FORM Postgraduate Medical Education Council of Queensland (Queensland) Medical Board of Queensland The information on this form contributes to decisions on registration for interns (PGY1) and International Medical Graduates on conditional registration. It also provides RMOs with feedback each term on their performance and professional development. The criteria listed on the form can be used as the basis for discussing goals and objectives at the start of term. It is suggested the criteria listed on the form be used as the basis for providing a formative assessment at mid term. Preferably the form should be completed at that time and signed by both the supervisor and RMO. At the END OF TERM ASSESSMENT, this form must be completed by the clinical supervisor, with input from other members of the team where appropriate. The form must be signed by both supervisor and RMO. • • • Clinical Supervisor/s to tick (√) appropriate boxes in columns Ticks in the shaded areas require comments by the clinical supervisor on page 2 One criterion assessed as “requires substantial assistance” (RSA), or two assessed as “requires further development” (RFD) must trigger development of an Improving Performance Action Plan (IPAP) (page 3) RMO Name ……………………………………………… Term Unit……………………………………………………… Hospital /Facility ..................................................... Term Dates……………………………………………………. Please tick the relevant boxes below. Position PGY1 (Intern) Start of term unit orientation PGY2 (JHO) YES PGY3 + (SHO/PHO) NO Expectations of RMO discussed Assessment process & learning objectives discussed End Term Assessment Mid Term Appraisal CRITERIA AMC Candidate Requires substantial assistance Requires further development Consistent with level of appointment Performance better than expected Performanc e exceptional N/A Not observed CLINICAL Knowledge base. Demonstrates adequate knowledge of basic and clinical sciences. Clinical skills. Elicits and records accurate, complete history and clinical examination findings. Clinical judgement/decision making skills. Applies knowledge base and clinical findings in organising, synthetising and acting on information. Emergency skills. Acts effectively, and when appropriate acknowledges own limitations and seeks help. Procedural skills. Performs procedures competently. COMMUNICATION Patient and Family. Interacts effectively and sensitively with patients and families/care givers. Medical Records/Clinical Documentation. Provides clear, comprehensive and accurate records. PERSONAL AND PROFESSIONAL Professional Responsibility. Demonstrates, appropriate attitudes and behaviours, including punctuality, reliability, honesty and self-care. Teaching. Demonstrates commitment to learning, reflective thinking, and teaching others. Time management skills. Organises and prioritises tasks to be undertaken. Teamwork and colleagues. Works and communicates effectively within a team. PMCQ RMO Assessment Form updated 12 Mar 07 1 Supervisors are required to comment on the following: Describe strengths: ..................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... List areas for improvement/advancement ....................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... If ticked ‘Requiring substantial assistance’ and/or ‘Further development’, give specific examples, and complete Improving Performance Action Plan on attached page, in consultation with DCT and Medical Educator(s). .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... Please tick (√) appropriate box Satisfactory progress for this term Unsatisfactory* progress for this term * If assessment includes “requires substantial assistance” x 1 (or more) or “requires further development” x 2 (or more) Has the RMO had a formal feedback session about this assessment? Yes No Comments by Resident Medical Officer .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... .......................................................................................................................................................................................................................................................................................................................................................................................... RMO ............................................…………. Name (please print) Clinical Supervisor….. .............................................. Name & Position (please print) ................................................. ………………….. Signature Date ……………………………………. …………………. Signature Date Director of Clinical Training ....................................... Name (please print) ........................……………….. Signature ………………… Date Director of Medical Services ...................................... Name (please print) ........................………………. Signature ………………… Date PMCQ is the authorised accrediting body of the Medical Board of Queensland PMCQ RMO Assessment Form updated 12 Mar 07 2 Improving Performance Action Plan (IPAP) to Address Identified Issues (Please refer to IPAP Guidelines) To be completed by the Clinical Supervisor, in consultation with Medical Education Staff and the RMO. The Director of Clinical Training has responsibility for ongoing implementation of Action Plans. Name of Resident Medical Officer: ……………………………………………………. Unit: ……………………………… Term: ………………………………………………… Issues related to criteria Term Dates: ……………………………………………. Actions/Tasks Timeframe Review Date Dates and Notes/Comments by DCT at Interview/s with Resident Medical Officer Signatures: Clinical Supervisor ………………………………………………………………. Date ……../……../…….. Director of Clinical Training…………………………………………………….. Date ……../……../…….. RMO …………………………………………………………………………………. Date ……../……../…….. Endorsed by PMCQ, the authorised accrediting body of the Medical Board of Queensland. PMCQ RMO Assessment Form updated 12 Mar 07 3 PRINCESS ALEXANDRA HOSPITAL PROCEDURE MANUAL Section: Support Procedure No. 52041/v2/06/2013 Procedure Title: Informing Intern of Serious Concerns – Medical Education Unit (MEU) Review Officer: Medical Education Unit nd Review Summary: 2 Version Applicable To: Princess Alexandra hospital Intern Education and Training Program Interns and Supervisors Purpose: To ensure that Interns are informed of serious concerns in a systematic, transparent and documented manner to ensure a safe learning environment for Interns as they acquire appropriate skills and attitudes in their professional development. Last Review Date: 06 2013 Next Review Date: 06 2015 Risks and Precautions: Authority: Director of Clinical Training Non compliance with this procedure will result in risk rating of EXTREME – immediate action required. ……………………………………… Signature of Authorising Officer Replaces: 52041v1 Authorised to Undertake the Procedure: Definitions: Supervisors Accreditation Reference: • Clinical Supervisors at the Princess Alexandra Hospital are PMCQ Accreditation Standards and senior doctors, employed at the level of Principal House Guidelines – Function 2 Standard 9. Officer/registrar or above. • Shift supervisors are senior doctors, employed at the level of Principal House Officer/Registrar or above, available in the junior doctor’s immediate work area during all shifts in which the junior doctor is working. Term Supervisors are senior clinicians responsible for deciding on whether performance of a junior doctor is satisfactory or not satisfactory. This person may or may not be a clinical supervisor. Ward call supervisors are on-site shift supervisors. PRIME is the Queensland Health Clinical Incident management system. It is an on-line system for reporting and managing clinical incidents involving all Queensland Health staff. Identifying that an incident has occurred, deciding on its significance and reporting the circumstances around it provide the organisation with a process and opportunity to effectively manage outcomes in a timely and effective way. Collected data is used to assist the organisation and individual patients through identifying and analysing systems and processes needing change to prevent or minimise the reoccurrence of the incident type. IPAP – The Improving Performance Action Plan – The Australian Health Practitioner Regulation Agency (AHPRA) endorsed process for managing substandard performance of junior doctors. The process is triggered by a team supervisor’s assessment of the Junior Doctor as unsatisfactory. This allocation of responsibilities for implementation of the remediation plan and timeframe for review. The process should involve the Intern, Medical Education Officer (MEO), Director of Clinical Training (DCT) and if necessary the Executive Director Medical Services (EDMS). DCT – Director of Clinical Training – Are medical practitioners appointed in each facility to support the training of junior doctors. MEO – Medical Education Officer – An experienced educationalist employed to assist the DCT in developing educational processes and procedures supportive of the Intern Education and Training Program (IETP). Key Words: Intern, Serious Concerns • • • • • • Procedure: Statement: In the context of the process of an Intern’s performance assessment by the term supervisor: • The assessment form to be completed by the term supervisor is the form endorsed by Australian Health Practitioner Regulation Agency (AHPRA) and the Post Graduate Medical Education Council of Queensland. Printed version is an uncontrolled copy 1 • • • • • • • • • An intern rated: - On any two of the criteria on the assessment form as “requires further development” (RFD); or - On any one of the criteria as “requires substantial assistance” (RSA) is to be advised that such an assessment is considered unsatisfactory, and must trigger the development of an “Improving Performance Action Plan” (IPAP). The supervisor is to provide the Intern with details as to the reasons for the ratings in a formal feedback session. The Intern is given an opportunity to make comment on the assessment (utilising the section on the assessment form). The Director of Clinical teaching (DCT) or Deputy (DDCT) and/or the Medical Education Officer (MEO) in the Medical Education Unit (MEU) is to be informed of the outcome of the assessment in a timely manner. An Improving Performance Action Plan (IPAP) is to be developed in consultation with the intern, the supervisor and the Director of Clinical Teaching (DCT) or Medical Education Officer (MEO). An IPAP generated at mid term of a full ten or twelve week term is to be utilised for the purpose of providing support for the intern. Such support should be aimed at maximising the opportunity for the intern to achieve the level of “satisfactory progress” for the term by the end of the term. The DCT is to be responsible for ensuring the action plans related to the issues identified on the IPAP are implemented. An Intern rated as not achieving a satisfactory level of progress at the end of an allocated term must be provided with this information in a formal feedback interview. An IPAP is to be developed utilising the process mentioned above. Details regarding prior term performance may be provided to the supervisor of the following allocated term. From the commencement of the following term, issues identified in the IPAP are to be addressed utilising an agreed action plan and, as previously, the process is to be overseen by the DCT. An intern who has not achieved a “satisfactory performance” by the completion of a term is to be informed of the possibility of a need to extend the period of internship and hence the potential need to defer a request to the Australian Health Practitioner Regulation Agency (AHPRA) to consider the lifting of probationary conditions. A term assessment rated as unsatisfactory may also trigger a change in allocations to ensure the intern is allocated to a Unit in the primary allocation facility for the subsequent term. The Executive Director of Medical Services is to be provided with timely reports on interns who are not achieving a satisfactory level of performance. The EDMS is to ensure that an intern working within the dictates of an IPAP is to be provided with appropriate support and mentoring throughout the period and beyond as long as is deemed necessary by the DCT. In the context of the global assessment of performance of an intern: • The DCT is to be provided with any report where concerns about the professional behaviour or clinical practice of an intern has led to its generation. • A report may initially have been forwarded to Patient Safety via the PRIME system. In other instances concerns regarding an intern may have been brought to the attention of the DCT in an informal manner. • Dependant on the content of the report, the intern is to be contacted and interviewed by the DCT or Deputy and/or the MEO. Notes of the interview are to be filed and the Intern is to be advised that records are kept by the DCT. The Intern is advised that an advocate or support person may be with the Intern at the interview. • Where an intern is the subject of multiple reports as upon investigation there is cause for significant concern, the intern is advised of the need for remediation. • An appropriate programme is to be developed with a mutually agreed timeframe for completion and evaluation. An IPAP for may be utilised for this process. • The intern is to be advised of the necessity to involve the term supervisor. • The DCT is to ensure the EDMS remains apprised of all relevant detail in a timely manner. • Where it is suspected that substandard performance or inappropriate behaviour is the result of substance abuse or mental health problems, the Intern is not to be managed by an IPAP but referred directly to the EDMS. Evaluation Method: • General Clinical Education Committee will evaluate this procedure against feedback by interns each term. Recommendations will be forwarded to individual Term Supervisors and Medical services Directors Committee. HYPERLINK TO: Medical Board of Australia Post Graduate Medical Education Council of Queensland (PMCQ) Printed version is an uncontrolled copy 2
© Copyright 2026