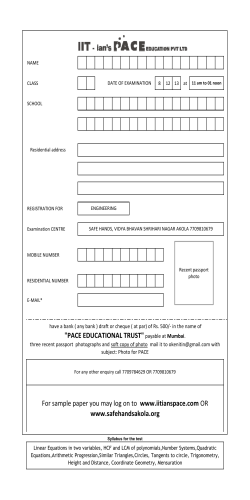
PACE 2014 PROVIDER OFFICE MANUAL 1
PACE 2014 PROVIDER OFFICE MANUAL 1 TABLE OF CONTENTS INTRODUCTION..............................................................................................................5 PARTICIPANT BILL OF RIGHTS ................................................................................8 PARTICIPANT IDENTIFICATION CARD ................................................................12 REFERRALS & PRIOR AUTHORIZATIONS ...........................................................13 URGENT & EMERGENCY CARE ..............................................................................14 CREDENTIALING & RECREDENTIALING ............................................................15 • • • • • • • • • • • Physician & Healthcare Providers .................................................................................... 15 Facility .............................................................................................................................. 15 Skilled Nursing Facility .................................................................................................... 15 Delegated credentialing .................................................................................................... 16 Medical Record Review .................................................................................................... 16 Provider Information......................................................................................................... 17 Adverse Credentialing Determination ............................................................................. 17 Request for Additional Information .................................................................................. 17 Appeals ............................................................................................................................. 18 Provider Termination ........................................................................................................ 19 Private Contract “Opt Out” ............................................................................................... 20 ADVERSE REIMBURSEMENT CHANGE.................................................................21 SANCTIONS ....................................................................................................................21 REINSTATEMENT ........................................................................................................21 RESOLUTION OF DISPUTES ......................................................................................22 ARBITRATION ...............................................................................................................22 BILLING/CLAIMS SUBMISSION ...............................................................................23 • Payment/Participant Held Harmless ......................................................................23 • General Billing .......................................................................................................24 • NPI (National Provider Identifier) .........................................................................24 • Paper Claims Submission ......................................................................................24 • Present on Admission ............................................................................................26 2 • • • • • • Facility claims ........................................................................................................26 Late Claims ............................................................................................................27 Reconsiderations ....................................................................................................28 Explanation of Payment .........................................................................................28 Claims Inquiries .....................................................................................................29 Notice of Overpayment ..........................................................................................31 MEDICAL RECORD KEEPING ..................................................................................33 • Access to Medical Records ....................................................................................33 • Record Retention ...................................................................................................33 • Access and Audit of Records .................................................................................34 • HITECH Act ..........................................................................................................36 FRAUD WASTE & ABUSE ...........................................................................................37 HIPAA COMPLIANCE & RELEASE OF INFORMAITON.....................................38 QUALITY ASSURANCE & PERFORMANCE IMPROVEMENT ...................................... 38 PARTICIPANT APPEALS & GRIEVANCE ...............................................................40 Grievance Procedure ..........................................................................................................40 Appeals Procedure .............................................................................................................41 Expedited Appeals Process ................................................................................................41 Additional Appeal Rights under Medicare & Medicaid ....................................................41 Provider Demographic Change Form............................................................................42 DEFINITIONS .................................................................................................................43 3 How to Contact ArchCare Senior Life/ PACE Administrative Office/Plan Address 33 Irving Place 11th Floor New York, NY 10003 Customer Service (866) 263-9083: 24 hour answering service available after business hours and weekends TTY/TDD (Teletype) should dial 711 Provider Services: Telephone Fax Inquiries 1-866-263-9083 1-646-417-7157 Provider Services can provide Authorizations, Credentialing information, Contract Status, Provider Information Changes, Training and Orientations. Compliance Hotline Telephone (Fraud and Abuse Prevention) 1-800-443-0463 Claims: Telephone 1-866-263-9083 All services must be prior authorized and billed through ArchCare Senior Life. Services may be provided by network providers ONLY and must be pre-authorized. Failures to contact ArchCare Senior Life prior to the provision of non-emergency services will forfeiture of billing rights for all unauthorized services. In an Emergency, Prior Authorization is not required. If the patient is presenting in an emergency room, please contact ArchCare Senior Life immediately at (866) 263-9083. Claims Submission Address TriState Benefit Solutions C/o ArchCare Senior Life / PACE 619 Oak Street Cincinnati, OH 45206 Electronic Claims (Payer ID 31144) TriState Benefits Solution Claims Inquiry Telephone 4 1-513-569-5049 Introduction To ArchCare Senior Life (PACE) Provider Manual 5 Introduction Welcome to ArchCare Senior Life. ArchCare Senior Life is a community based model of care for nursing home eligible participants sponsored by ArchCare, the continuing care community of the Archdiocese of New York. As a provider of services, you have a special place in our program. Through effective use of services that focus on enhancing our participants’ quality of life and functional capacity, we can achieve our program goal of managing the frail elderly in their homes and community as long as it is socially, medically, and economically feasible. ArchCare Senior Life is a PACE Model of Care The PACE program is based on a successful long-term care model developed in San Francisco known as On Lok. Nationally known as PACE (Program of All-Inclusive Care for the Elderly), it was developed as a special health plan for senior citizens that helps them stay as independent as possible for as long as possible. The PACE is a unique model of managed care service delivery for a small number of very frail community-dwelling elderly, most of whom were dually eligible for Medicare and Medicaid coverage and all of whom were assessed as being eligible for nursing home placement according to the standards established by the State. The model of care includes as core services the provision of adult day health care and multidisciplinary team case management, through which access to and allocation of all health services was controlled. Physician, therapeutic, ancillary and social support services are furnished in the participant’s residence or on-site at the adult day health center, unless those locations were not feasible. Hospital, nursing home, home health, and other specialized services are furnished under contract. Financing of this model is accomplished through prospective capitation of both Medicare and Medicaid payments. 6 Eligibility To be eligible to enroll as an ArchCare Senior Life participant, an individual must be: 1. 55 years of age or older 2. A resident of New York (Manhattan), Bronx or Richmond counties 3. Eligible for nursing home level of care based on an established criterion for New York State 4. Eligible for Medicare and/or Medicaid and/or willing to pay privately 5. Able to live safely in the community with the services of the plan 6. Expected to need the long term care services of the plan for at least 120 days The ArchCare Senior Life Intake Enrollment department assesses all potential participants prior to enrollment and verifies that all persons meet nursing home eligibility requirements. When the participant is enrolled, their care is planned and directed by ArchCare Senior Life’s interdisciplinary team. Care is focused on preventive services and maintenance or improvement of functional status as well as ongoing medical care. Periodic assessment by the interdisciplinary team keeps the care plan and service delivery on track. ArchCare Senior Life offers a full range of services, including primary medical care and rehabilitative therapy services at our PACE center, home care, inpatient services; both acute care through local hospitals and nursing home care through affiliated providers, drugs, and durable medical equipment and supplies. When a participant is enrolled in ArchCare Senior Life, we become the sole provider and payer of services. This ensures a coordinated, comprehensive approach to our participants’ care. Services are available 24 hours a day, 7 days a week, and 365 days a year. Most of these services will be provided in ArchCare Senior Life’s PACE center. Those services that cannot be provided at the center will be provided in the home, or by our network of contracted providers, such as you, in consultation with our interdisciplinary team. This Provider manual is meant to assist you in working with our participant’s within the framework of ArchCare Senior Life’s policies and procedures. Familiarizing yourself with and adhering to the procedures outlined in this Manual will help to ensure a mutually beneficial, productive relationship in caring for our enrolled participants. 7 Participant Rights Participant’s Rights in the Program of All-inclusive Care for the Elderly (PACE) The Program of All-inclusive Care for the Elderly, (PACE) is a Special program that combines medical and long-term care services in a community setting. When enrolled in a PACE program participants have certain rights and protections. The PACE program must fully explain the rights to all participants or someone acting on their behalf in a way that they can understand at the time they join. As a provider, you have the responsibility to respect every participant’s rights. The PACE Participant Bill of Rights follows: 1. They have the right to be treated with dignity and respect at all times and to have all of their care kept private, and to get compassionate, considerate care. 2. They have the right: • To get all of their health care in a safe, clean environment. • To be free from harm. This includes physical or mental abuse, neglect, physical punishment, being placed by themselves against their will, and any physical or chemical restraint that is used on them for discipline or convenience of staff and that they do not need to treat their medical symptoms or to prevent injury. • To be encouraged to use their rights in the PACE program. • To get help, if they need it, to use the Medicare and Medicaid complaint and appeal processes, and their civil and other legal rights. • To be encouraged and helped in talking to PACE staff about changes in policy and services they think should be made. • To use a telephone while at the PACE Center. • To not have to do work or services for the PACE program. 8 3. You have a right to protection against discrimination. Discrimination is against the law. Every company or agency that works with Medicare and Medicaid must obey the law. They cannot be discriminated against because of their: • Race /Ethnicity and National Origin • Religion • Age • Sex • Mental or physical ability • Sexual Orientation • Source of payment for your health care (For example, Medicare or Medicaid) If they think you have been discriminated against for any of these reasons, contact a staff member at the PACE program to help them resolve your problem. If they have any questions, they can call the Office for Civil Rights at 1-800-368-1019. TTY users should call 1-800-537-7697. 4. They have a right to information and assistance. They have the right to get accurate, easy-to-understand information and to have someone help you make informed health care decisions. They have the right: • To have someone help them if they have a language or communication barrier so they can understand all information given to them. • To have the PACE program interpret the information into their preferred language in a culturally competent manner, if their first language is not English and they can’t speak English well enough to understand the information being given to them. • To get marketing materials and PACE rights in English and in any other frequently used language in their community. They can also get these materials in Braille, if necessary. • To get a written copy of their rights from the PACE program. The PACE program must also post these rights in a public place in the PACE center where it is easy to see them. • To be fully informed, in writing, of the services offered by the PACE program. This includes telling you which services are provided by contractors instead of the PACE staff. You must be given this information before you join, at the time you join, and when you need to make a choice about what services to receive. • To look at, or get help to look at, the results of the most recent review of their PACE program. Federal and State agencies review all PACE programs. They also have a right to review how the PACE program plans to correct any problems that are found at inspection. 5. They have a right to a choice of providers. They have the right to choose a health care provider within the PACE program’s network and to get quality health care. Women have the right to get services from a qualified women’s health care specialist for routine or preventive women’s health care services. 6. They have a right to access emergency services. 9 They have the right to get emergency services when and where they need them without the PACE program’s approval. A medical emergency is when they think their health is in serious danger—when every second counts. They may have a bad injury, sudden illness or an illness quickly getting much worse. They can get emergency care anywhere in the United States. 7. They have a right to participate in treatment decisions. They have the right to fully participate in all decisions related to their health care. If they cannot fully participate in their treatment decisions or they want to have someone they trust help them, they have the right to choose that person to act on their behalf. They have the right: • • • • 8. To have all treatment options explained to them in a language they understand, to be fully informed of their health status and how well they are doing, and to make health care decisions. This includes the right not to get treatment or take medications. If they choose not to get treatment, they must be told how this will affect their health. To have the PACE program, help them create an advance directive. An advance directive is a written document that says how they want medical decisions to be made in case they cannot speak for themselves. They should give it to the person who will carry out their instructions and make health care decisions for them. To participate in making and carrying out their plan of care. They can ask for their plan of care to be reviewed at any time. To be given advance notice, in writing, of any plan to move them to another treatment setting and the reason they are being moved. They have a right to have your health information kept private. They have the right to talk with health care providers in private and to have their personal health care information kept private as protected under State and Federal laws. They have the right to look at and receive copies of their medical records. They can also be assured that: • All of the information in their health record, including information contained in an automated data bank is treated in a confidential manner at all times. • Their written consent will be required and obtained before any information is released to any person not otherwise authorized under law to receive it. • They have the right to provide written consent that limits the degree of information and the persons to whom information may be given. 10 There is a patient privacy rule that gives them more access to their own medical records and more control over how their personal health information is used. If they have any questions about this privacy rule, please call the Office for Civil Rights at 1-800-368-1019. TTY users should call 1-800-537-7697. They also have the right to confidentiality in the treatment, payment, and health care operations, provided that such use or disclosure is consistent with other applicable requirements of the HIPPA Privacy Rule. 9. They have a right to file a complaint. They have a right to complain about the services they receive or that they need and don’t receive, the quality of their care, or any other concerns or problems they have with their PACE program. They have the right to a fair and timely process for resolving concerns with their PACE program. They have the right: • • • 10. 11 To a full explanation of the complaint process. To be encouraged and helped to freely explain their complaints to PACE staff and outside representatives of their choice. They must not be harmed in any way for telling someone their concerns. This includes being punished, threatened, or discriminated against. To appeal any treatment decision by the PACE program, staff, or contractors. They have a right to leave the program. If, for any reason, they do not feel that the PACE program is what they want, they have the right to leave the program at any time. Participant ID Card Every ArchCare Senior Life participant will receive an identification card that will detail the participant’s name and identification number. This card, which identifies them as an ArchCare Senior Life participant should be presented to physicians and other providers when seeking health care services. If the participant does not have an identification card, but they represent that they are an ArchCare Senior Life participant, please contact customer service at 1-866-2639083 for member eligibility. Medicare and Medicaid will not be responsible for claims for the participant while they are enrolled as a participant of ArchCare Senior Life. All claims for services provided to ArchCare Senior Life participants need to be submitted to ArchCare Senior Life at the address listed on the “How to Reach Us” page. Below is a sample of the ArchCare Senior Life participant identification card: THIS CARD IS NOT CURRENT. JANET TO SHOW NAZIA FOR INSERTING Front of the card: 12 Back of the card: Referrals and Prior Authorization When ArchCare Senior Life participants need services that cannot be provided at our center, our interdisciplinary team will make all of the arrangements, including calling for the appointment and arranging transportation. As a provider, you will receive a “Service Authorization” form via fax or email with instructions regarding where to send the report of services rendered. This process ensures our participants receive all of the care they need and that all care is coordinated within our network. Providers must only provide services as authorized by the ArchCare Senior Life interdisciplinary team, on the “Service Authorization” form. Any services that may be necessary need to be authorized by ArchCare Senior Life’s Medical Director/ interdisciplinary team. Services not authorized or arranged for by the ArchCare Senior Life Interdisciplinary team will not be paid for unless it is an emergency. Authorizations for urgently needed care or post stabilization services should be obtained by calling 866-263-9083. ArchCare Senior Life will respond to an authorization request as quickly as possible and not to exceed three days. The interdisciplinary team may conduct a re-assessment as the members condition requires. All services must be prior authorized and billed through ArchCare Senior Life. Services may be provided by network providers ONLY and must be pre-authorized. Failures to contact ArchCare Senior Life prior to the provision of non-emergency services will forfeiture of billing rights for all unauthorized services. In an Emergency, Prior Authorization is not required. If the patient is presenting in an emergency room, please contact ArchCare Senior Life immediately at (866) 2639083. 13 Urgent and Emergency Care ArchCare Senior Life provides coverage for the treatment of an emergency medical condition, which is defined by CMS as a condition that manifests itself by acute symptoms of sufficient severity (including severe pain) such that a prudent layperson, who possesses an average knowledge of health and medicine, could reasonably expect the absence of immediate medical attention to result in: • Placing the health of the individual in serious jeopardy • Serious impairment to bodily functions, or • Serious dysfunction of any bodily organ or part Inpatient and outpatient emergency health services are covered both inside and outside the ArchCare Senior Life service area. In the event of an emergency, the participant should seek immediate care, or call 911 for assistance. Prior authorization is not required for emergency care, and ArchCare Senior Life may not deny payment if an ArchCare Senior Life contracted health care provider instructs a participant to seek emergency services. Enrollment in ArchCare Senior Life includes coverage for post-stabilization care, defined as nonemergency services needed to ensure that the participant remains stabilized after an emergency. Providers must only provide services as authorized by ArchCare Senior Life Interdisciplinary Team. Any additional services needed must be discussed with the ArchCare Senior Life Interdisciplinary Team. Unauthorized services will not be paid by ArchCare Senior Life unless it is an emergency or ArchCare Senior Life fails to respond to an authorization request within one hour of being contacted for urgently needed or post-stabilization services. Urgently needed services are defined as those conditions which require immediate medical attention due to unexpected illness or injury. Fevers, abdominal pain, nausea and vomiting and difficulty urinating are some examples of situations requiring urgently needed services. Urgent care services are covered for participants when they are temporarily outside of the ArchCare Senior Life service area. Providers must notify ArchCare Senior Life within 24 hours or the next business day of providing emergency or urgent services to an ArchCare Senior Life participant, or if the participant is admitted to a hospital. Participants are encouraged to carry their ArchCare Senior Life identification card at all times and to notify their care manager or provider should they need urgent or emergency care. 14 Credentialing/Recredentialing All physician and health care providers providing health services to ArchCare Senior Life participants must be credentialed in accordance with ArchCare Senior Life policies and procedures. Under CMS regulation, the credentialing process and approval must be completed by any network provider administering care to an ArchCare Senior Life participant. Recredentialing will occur every three years thereafter for all contracted physicians, other health care providers, facilities, and hospitals. The following items are required along with the provider credentialing applications in order to complete the credentialing process: • • • • • • • • • • • • • • • • • • • • • 15 Physician and Health Care Providers Current Curriculum Vitae Work history past five years Current valid State license to practice Valid DEA & CDS (controlled dangerous substances) certificates Education and Training Copy of Insurance Certificate Board Certification status Hospital admitting privileges Disclosure Statement and Signed Attestation Verification of “Opt Out” or Private Contract from Medicare participation History of professional liability claims that resulted in settlements or judgments paid by the or on behalf of practitioner Facility Credentialing Medicare and/or Medicaid license Copy of New York State Operating License Copy of Insurance Certificate Copy of any accreditations and/or surveys A copy of any notice of disciplinary actions taken within the past five years by the New York State Department of Health or other government agency that regulates the services by the provider; A copy of any notice of sanctions imposed upon the provider within the past five years by the Medicare or Medicaid program; Skilled Nursing Facility Credentialing Medicare, Medicaid or JCAHO accreditation Copy of License Copy of Insurance Certificate Copy of last 3 years of federal and state surveys including any sanctions • • A copy of any notice of disciplinary actions taken within the past five years by the New York State Department of Health or other government agency that regulates the services by the provider; A copy of any notice of sanctions imposed upon the provider within the past five years by the Medicare or Medicaid program; The credentialing process is considered complete when the credentialing committee approves the credentialing application. Once the credentialing process has been completed, and an executed contract is received and countersigned, the physician or health care provider will be considered participating. The physician or health care provider will use their NPI (National Provider Identification) number as their “provider number”. Delegated Credentialing ArchCare Senior Life offers delegated credentialing for large groups of health care providers. ArchCare Senior Life delegates the credentialing function to groups that meet ArchCare Senior Life and National Committee for Quality Assurance (NCQA) standards and state and federal law. The decision by ArchCare Senior Life to delegate the credentialing function results from a review of the group’s credentialing policies and procedures and an on-site audit of the group’s credentialing files. The ArchCare Senior Life Credentialing Committee reviews the resulting delegation report and makes a determination to approve, defer or grant provisional delegated status for the group. If provisional status is granted, this is followed by a reassessment within a specified period of time and a final decision to approve or defer. Groups granted “delegated status” are required to sign a delegated credentialing agreement with ArchCare Senior Life. Medical Record • As part of the re-credentialing process ArchCare Senior Life will review on a quarterly basis medical quality and utilization management data on an aggregate basis. This tracking and reporting of data supports analysis of trends and outliers across sites and within specific service areas. Pharmaceutical management and utilization practices is tracked and discussed quarterly by the Medical Director. ArchCare Senior Life newly hired PCP’s and mid-level practitioners receive competency and orientation checklist which is reviewed and signed off by the Medical Director. The ASL PACE Medical Director administers and completes the competency evaluation initially and is on-going. Prior to the physician date for recredentialing, a provider relations representative will contact the Medical Director of PACE to determine current performance evaluations and job competencies meet standards for re-credentialing. 16 Provider Information Providers are responsible for contacting ArchCare Senior Life to report any changes in their practice. It is essential that ArchCare Senior Life maintain an accurate provider database in order to ensure proper payment of claims and capitation, to comply with provider information reporting requirements mandated by governmental and regulatory authorities, and to provide the most up-to-date information on provider choices to our participants. Any changes to the following list of items must be reported to ArchCare Senior Life within 30 (thirty) days of the change, using our Provider Change Request Form attached in the appendix of this manual: • Provider’s name and Tax ID number(s) • Provider’s address, zip code, telephone or fax • Provider’s billing address • Languages spoken in the provider’s office • Wheelchair accessibility • Provider’s NY license (e.g., revocation, suspension) • National Provider Identification Number (if applicable) • Provider’s board eligibility/board certification status • Hospital affiliation status Please use the “Provider Addition/Change Request” form found on page 39. Adverse Credentialing Determination Appeals As a network provider, you have the right to: • Review information submitted to your credentialing application. • Correct erroneous information collected during the credentialing process. • Be informed of the status of your credentialing or re-credentialing application. • Be notified of these rights. Requests for Additional Information If ArchCare Senior Life receives information from an outside source that differs substantially from information you have provided us, we will contact you directly as soon as the discrepancy is noted and request your clarification in writing within 10 business days. Requests should be made in writing to: ArchCare Senior Life Attention: Credentialing Department 33 Irving Place, 11th Floor New York, NY 10003 17 Appeals Process for Providers Terminated or Rejected from the ArchCare Senior Life Provider Network A provider has the right to appeal a Peer Review and Credentialing Sub-Committee decision that has negatively impacted the provider. ArchCare Senior Life complies with all state and federal mandates with respect to appeals for providers terminated or rejected from the ArchCare Senior Life Provider Network. ArchCare Senior Life notifies the provider in writing of the reason for the denial, suspension and termination. Terminated or rejected providers may submit a request for an appeal as outlined in the letter of rejection/termination sent by ArchCare Senior Life. In addition, the request for appeal must be received by ArchCare Senior Life within ten (10) days of the date of the rejection/termination letter. Upon receipt of the letter by ArchCare Senior Life, the appeal is forwarded to the ArchCare Senior Life Peer Review Committee for review and further processing ArchCare Senior Life will ensure that the majority of the hearing panel members are peers of the affected physician. Provider Monitoring & Evaluation ArchCare Senior Life, DOH, CMS and their designees shall each have the right, during provider's normal operating hours, and at any other time a contractor function or activity is being conducted, to monitor and evaluate, through inspection or other means, provider's performance, including, but not limited to, the quality, appropriateness, access to service and timeliness of services provided under the provider contract. All providers are required to cooperate with and provide reasonable assistance to ArchCare Senior Life, DOH, CMS and their designee in the monitoring and evaluation of the services provided under the provider contract. 18 Physician or Health Care Provider Termination ArchCare Senior Life or its participating providers may decide to terminate or elect not to renew a provider agreement. Termination procedures are subject to the provisions of the provider agreement. If there are conflicts between the provisions in this Provider Manual and any provider agreement, the terms of the provider agreement will apply. All providers who wish to terminate their contractual relationship with ArchCare Senior Life are bound by the applicable provisions of the individual or group provider agreement or hospital agreement that may govern the termination of an ArchCare Senior Life provider. All providers voluntarily terminating their participation with ArchCare Senior Life must give ninety (90) days prior written notice of the termination. ArchCare Senior Life will not accept any verbal notification as sufficient to initiate the termination process. Provider shall complete any course of treatment to any individual Member, in accordance with the terms of his/her agreement, for whom treatment was ongoing on the date of termination, unless ArchCare Senior Life makes reasonable and medically appropriate provision for the assumption of such services by another participating provider. For those members confined to an inpatient facility, provider shall also complete any course of treatment in progress until a medically appropriate discharge or transfer is made, or completion of the course of treatment is made, whichever first occurs, provided that the confinement or course of treatment was commenced during the paid premium period. For information, regarding contracted physicians or health care providers including facilities termination; please refer to your provider agreement. Requests should be made in writing to: ArchCare Senior Life Attention: Credentialing Department 33 Irving Place, 11th Floor New York, NY 10003 You may also contact Provider Relations at 1-800-373-3177 or fax 646-417-7157. 19 Private Contract “Opt Out” ArchCare Senior Life will not pay, directly or indirectly, on any basis, for services (other than post stabilization, emergency or urgently needed services) furnished to a Medicare enrollee by a physician or other health care provider who has filed an affidavit with the Medicare carrier agreeing to furnish Medicare covered services to Medicare beneficiaries only through private contracts with the beneficiaries. ArchCare Senior Life verifies, with the local Medicare intermediary, the Opt Out or Private Contract list during credentialing and re-credentialing to ensure that our contracted providers are not included on the list. Upon written notification from the carrier of a physician’s or other health care provider’s decision to “opt out” of the Medicare program, Provider Relations will send a letter to the physician or other health care provider stating that the physician or provider will be removed from the list of ArchCare Senior Life contracted physicians and providers. No payments will be made to the physician or provider for two years after the effective date of the affidavit. In addition, ArchCare Senior Life will send a letter to each ArchCare Senior Life participant assigned to the physician or provider notifying the enrollee that the physician or provider is no longer contracted and advising the enrollee to select a new Primary Care Physician, if appropriate. Participants with claims pending for services from a physician or provider who has “opted out” of Medicare, or participants submitting claims from physicians or providers who have “opted out” of Medicare will receive a letter containing the following information: • The participant is accessing a physician or provider who has “opted out” of Medicare. • Payments by ArchCare Senior Life are prohibited. • The services are not covered, the current claim(s) will not be paid by ArchCare Senior Life and the physician or provider must have entered into a private contract with the participant in order to receive payment from the participant. • Payments will not be made for items or services rendered after the date of the physician “opt out.” Physicians and health care provider are responsible for notifying ArchCare Senior Life when their affidavit has expired if they desire to apply for reinstatement. 20 Adverse Reimbursement Change ArchCare Senior Life will provide ninety (90) days’ notice to providers of an adverse reimbursement change. Providers have the opportunity to terminate their contract by providing ArchCare Senior Life with written notice within 30 days of receipt of the notice of the change. This provision is not applicable to reimbursement/rates changes mandated by New York State or the federal government. This provision is not applicable to hospitals, diagnostic and treatment centers, home care agencies, or other institutions. Sanctions Upon written notification from CMS – by letter or the lists published by the Office of Inspector General (OIG) and Government Accountability Office (GAO) – of a physician’s or other health care provider’s exclusion from original Medicare, ArchCare Senior Life will send a letter to the physician or provider stating the physician or provider will be removed from the ArchCare Senior Life list of contracted physicians and providers. Except for post stabilization, emergency and urgently needed care; no payments will be made to the physician or provider after the exclusion effective date. Members are notified that the physician or other health care provider is no longer contracted and are advised to select a new Primary Care Physician or health care provider, if appropriate. Members with claims pending for items or services from an excluded physician or provider, or member’s submitting claims for items or services from an excluded physician or provider for the first time, will receive a letter notifying the enrollee of the following: • • • The enrollee is accessing a sanctioned physician or provider. Payments to a Medicare-excluded physician or provider are prohibited. Payments will not be made for items or services rendered after the date of exclusion or after notification to the enrollee (whichever date is later). Participating physicians and other healthcare providers are also prohibited from employing or contracting with an individual who is excluded from participation in Medicare, or with an entity that employs or contracts with such an individual, for the provision of health care, utilization review, medical social work or administrative services. Reinstatement Upon reinstatement by CMS, the physician or provider is responsible for notifying ArchCare Senior Life and apply for reinstatement. 21 Resolution of Disputes Contract concern or complaint The services you provide are essential to our ability to serve our participants. If you have a concern or complaint about any aspect of our relationship with you, please let us know about it. You can send a letter outlining the details of your complaint to ArchCare Senior Life Provider Relations Department or call our toll free number (866) 263-9083. The Provider Relations staff will seek to address and resolve your concerns as quickly as possible. • Acknowledge your complaint within 5 business days of receipt. • Investigate your complaint and arrive at a mutually satisfactory resolution within 30 days. If there is no resolution to the complaint after following the above procedures, arbitration proceeding may be filed as described below and in our provider services agreement. Arbitration ArchCare Senior Life will conduct arbitration proceedings under your agreement under the auspices of the American Arbitration Association, as further described in our provider services agreement. For more information on the American Association guidelines, visit their website at www.adr.org. 22 Billing Procedures All participant ArchCare Senior Life providers are required to submit claims/encounters for services reimbursed fee-for-service and for services provided under a capitation model of care. Agreement. Encounter data is essential for claims processing and utilization reporting as well as for complying with the reporting requirements of CMS, New York State and other governmental and regulatory agencies. It is essential that this information be submitted in a timely and accurate manner. Payment for services rendered is subject to verification that the participant was enrolled in ArchCare Senior Life at the time the service was provided and the provider’s compliance with ArchCare Senior Life medical management and prior authorization policies at the time of service. • • Providers should verify participant eligibility at the time of service to ensure that the participant is enrolled in ArchCare Senior Life. Failure to do so may affect claims payment. Note, however, that participant’s may retroactively lose their eligibility with ArchCare Senior Life after the date of service. Therefore, verification of eligibility is not a guarantee of payment by ArchCare Senior Life. Claims submitted for services rendered without proper authorization (as appropriate) will be denied for ‘failure to obtain authorization’. No payment will be made. Payment is made directly to the participating hospital for all employed providers who are covered by the hospital’s participation agreement with ArchCare Senior Life and who practice in hospital outpatient departments and hospital owned community-based sites. For all other providers, payment is made directly to the provider or to the designated payee. In certain cases, a managed care plan participant may change health plans during the course of a hospital stay. When this occurs, provider should bill the health plan to which the participant belonged at the time of admission to the hospital. ArchCare Senior Life Payment in Full / Participant Held Harmless Pursuant to the provider contract, participating providers are prohibited from seeking payment, billing or accepting payment from any participant for fees that are the legal obligation of ArchCare Senior Life, including in the event that ArchCare Senior Life becomes insolvent or denies payment on a claim, regardless of the reason. Participating providers must refund all amounts incorrectly collected from ArchCare Senior Life participants or from others on behalf of the participant. ArchCare Senior Life is not financially responsible for reimbursing non-covered services provided to participants. 23 General Billing Requirements: Submitting Claims Electronically For all electronic claims, ArchCare utilizes the Emdeon clearinghouse and MD On-line, a free online service for non-facility providers who do not have claims submission software. Claims submitted electronically receive a status report indicating the claims are accepted, rejected and/or pending. Claims submitted electronically must include: 1. The ArchCare Payer ID Number 31144 on each claim. 2. A complete ArchCare Senior Life Participant ID Number. 3. A National Provider Identifier (NPI). To sign up for electronic billing with Emdeon, providers must contact their software vendor and request that their ArchCare claims be submitted through Emdeon. Providers can also direct their current clearinghouse to forward claims to Emdeon. To sign up for electronic billing with Emdeon or for more information visit www.emdeon.com or call 1-866-924-4634, #4. To enroll your office for Online Claim submission with MD On-line, visit www.tbsmdol.com to register on line or call 1-888-499-5465 (A representative is available to assist you between the hours of 8:30AM to 6PM / EST.) Submitting Claims on Paper All paper claims should be submitted to: ArchCare Senior Life C/o TriState Benefit Solutions 619 Oak Street Cincinnati, OH 45206 All paper claims should include the National Provider Identifier (NPI) as well as the ArchCare Provider ID Number (the latter is not required for electronic claims). The ArchCare Provider ID is a unique provider number. Note for group practices and facilities: When submitting claims, please ensure separate billing NPI and provider NPI numbers are entered in the appropriate fields. Office visit claims submitted for the group practice, with the group practice NPI number instead of the individual NPI number for the servicing provider, cannot be processed. 24 Required Data elements and Claim Forms Prior to being adjudicated, all claims are reviewed within the ArchCare Claims Department for completeness and correctness of the data elements required for processing payments, reporting and data entry into the ArchCare Senior Life claims processing system. If the following information is missing from the claim, the claim is not ‘clean’ and will be rejected: Data Element CMS 1500 UB-04 Patient Name X X Patient Date of Birth X X Patient Address X X Patient Gender X X ArchCare Senior Life Participant ID Number X X Coordination of Benefits (COB / other insured’s medical insurance coverage information.) X X Date(s) of Service X X ICD – 9 Diagnosis Code(s) including 4 and 5 digit, when required X X CPT- 4 Procedure Code(s) X X HCPCS Code(s) X X Service Code Modifier(s), when required X X Place of Service X Service Units X X Charges per Service and total charges X X Provider Name X X Provider Address / Phone Number X X National Provider Identifier - NPI X X Tax ID Number X X ArchCare Senior Life Provider Number – for Paper Claims Only X X ArchCare Senior Life Payer ID Number 31144 – for EDI Claims Only X X th th Hospital / Facility Name and Address X Type of Bill X Admission Date and Type X Patient Discharge Status Code X Condition Code(s) X 25 Data Element CMS 1500 UB-04 Occurrence Codes and Dates X Value Code(s) X Revenue Code(s) and corresponding CPT / HCPCS Code(s) X Health Insurance Prospective Payment System (HIPPS) Rate Code(s), when required X Principal, Admitting, and Other ICD – 9 Diagnosis Codes including 4th and 5th digit, when required X Present on Admission (POA) indicator, as applicable X Present on Admission (POA) The POA indicator applies to diagnosis codes for certain health care claims. POA indicator reporting is mandatory for claims involving inpatient admissions to general acute care hospitals or other facilities. It clarifies whether a diagnosis was present at the time of admission. ArchCare requires POA indicators for all primary and secondary diagnosis codes as well as the external cause of injury codes, regardless of the manner in which claims are submitted (i.e., paper or electronic). Please refer to the instructions provided by CMS regarding identification of the POA for all diagnosis codes for inpatient claims submitted on the UB-04 and ASCX12N 837 Institutional (837I) forms. Requirements for Billing by Facilities Facilities, including hospitals, must submit inpatient and outpatient facility claims on the UB04 or on electronic media: • Report the name, NPI and ArchCare Senior Life provider ID number of the attending provider in Field 76 (ArchCare Senior Life’s provider ID number is not required on electronic transactions) Professional services that are not part of the facility claim should be billed on a CMS 1500 form. 26 Time Frames for Claim Submission, Adjudication and Payment Timely Claim Submission Providers should submit all claims within thirty (30) days of the date of service for prompt adjudication and payment. When claims are submitted later than the time period set forth in the provider’s agreement with ArchCare Senior Life, the claim will not be paid except under certain circumstances. In no event will ArchCare Senior Life pay claims submitted more than one hundred eighty (180) calendar days from the date of service. Late Claim Submission In certain circumstances, ArchCare Senior Life will process claims submitted after the time period required under the provider’s agreement with ArchCare Senior Life. Please note that ‘unclean’ claims that are returned to the provider for necessary information are adjudicated according to the original date of service. They do not fall into the category of exceptions to the time period required. The following situations allow for special handling of claims. Claims must be submitted with a written explanation and appropriate documentation showing the date the claim came within the provider’s control: Reason for Delay Litigation involving payment of the claim Within ninety (90) calendar days from the time the Medicare or other third party processing delays affecting the claim Within ninety (90) calendar days from the time the Delay in member eligibility determination Within ninety (90) calendar days from the time of notification of eligibility (submit with documentation substantiating the delay) Member’s Enrollment with ArchCare Advantage was not known on the date of service Within ninety (90) days from the time the member’s enrollment is verified. Providers must make diligent attempts to determine the member’s coverage with the Plan. submission came within the provider’s control submission came within the provider’s control Coordination of Benefits (COB) Coordination of Benefits (COB) ensures that the proper payers are held responsible for the cost of healthcare services and is one (1) of the factors that can help hold down co-payments. ArchCare Senior Life follows all standard guidelines for COB. Participants are asked to provide information about other medical health insurance plans under which they are covered. 27 ArchCare Senior Life is Always the secondary Payer in the Following Circumstances • Workers compensation • Automobile medical • No-fault or liability auto insurance ArchCare Senior Life Does Not Pay for Services Provided Under the Following Circumstances When There is COB • The Department of Veterans Affairs (VA) or other VA facilities (except for certain emergency hospital services) • When VA-authorized services are provided at a non-VA hospital or by a non-VA provider ArchCare Senior Life will use the same guidelines as Medicare for the determination of primary and secondary payer. As a result, ArchCare Advantage is the secondary payer for all of the cases listed above as well as for the following: • Most Employer Group Health Plans (EGHP) • Most EGHPs for disabled members • All benefits payable under an EGHP in the case of individuals who are entitled to benefits solely or partly on the basis of end stage renal disease (ESRD) during a period of thirty (30) months. (This applies to all services, not just ESRD. If the individual entitlement changes from ESRD to over sixty-five [65] or disability, the coordination period will continue.) Explanation of Payment (EOP) The EOP describes how claims for services rendered to ArchCare Senior Life Participants were reviewed. It details the adjudication of claims, describing the amounts paid or denied and indicating the determinations made on each claim. The EOP includes the following elements (see Appendix A for a sample of the EOP): • Payer’s Name • Vendor Name and Identification (ID) Number • Provider Name and Identification (ID) Number • Patient’s Name • Member’s Identification (ID) Number • Claim Date of Service • Service • Total Billed Charges • Allowed Amount 28 • Explanation for Denied Charges • Amount Applied to Deductible • Co-payment/Co-insurance Amount • Total Payment Made and to Whom The EOP is arranged by vendor by provider. Each claim represented on an EOP may be comprised of multiple rows of text. The line number indicated to the left of the date of service identifies the beginning and end of a particular claim. Key fields that indicate payment amounts and denials are as follows: • Paid Claim Lines: If the Paid Amount field reads greater than zero (0), the claim line was paid in the amount indicated. • Denied Claim Lines: If the Not Covered field is greater than zero (0) and equal to the charged amount, the service was denied. • Claim Processed as a Capitated Service: If the Paid Amount field is zero (0), but the EOP Explanation Codes is ‘171’ – Capitated Covered Services, the service was processed as a Capitated Service. • End of Claim: Each claim is summarized by a claim total. If there are multiple claims for a single member, the EOP also summarizes the total amount paid for that member. Claim Inquiries, claim Reconsideration and Appeal Process Claim Inquiries Providers may call Provider Services at 1-800-373-3177 to request claim status. Requests for Review and Reconsideration of a Claim Please note that the process described here does not apply to utilization management determinations concerning medical necessity. See appropriate section (page XX) for information on medical management appeals. A provider may be dissatisfied with a decision made by ArchCare Senior Life regarding a claim determination. Some of the common reasons include, but are not limited to: • Claim was incorrectly processed • Denial of a service / claim • Denial for the untimely submission of claim(s) • Failure to obtain prior authorization 29 Providers who are dissatisfied with a claim determination made by ArchCare Senior Life must submit a written request for review and reconsideration with all supporting documentation within sixty (60) business days from ArchCare Senior Life’s initial date of action that led to the dispute, to the following address: ArchCare Senior Life 33 Irving Place, 11th Floor New York, NY 10003 Attention: Provider Disputes Provide a clear explanation of the basis upon which you believe the initial determination/action is incorrect along with all supporting documentation and a copy of the Explanation of Payment (EOP) or include: • • • • • • • The provider’s full name The provider’s identification number The provider’s contact information The Participant’s name and ArchCare Senior Life’s Participant identification number Date(s) of service The ArchCare Senior Life claim(s) number A copy of the original claim or corrected claim, if applicable ArchCare Senior Life will investigate all written requests for review and reconsideration and issue a written explanation stating that the claim has been either reprocessed or the initial denial has been upheld within 45 calendar days from the date of receipt of the provider’s request for review and reconsideration. ArchCare Senior Life will not review or reconsider claim determinations which are not appealed according to the procedures set forth above. If a provider submits a request for review and reconsideration after the 60 business day time frame, the request is deemed ineligible and will be dismissed. Providers will not be paid for any services irrespective of the merits of the underlying dispute if the request for review and reconsideration is not timely filed. In such cases providers may not bill members for services rendered. All questions concerning request for review and reconsideration should be directed to the ArchCare Senior Life Provider Relations Department at 1-800-373-3177. 30 Corrected Claim Submission If you need to correct and re-submit a claim and reduce the risk that your corrected claim is rejected by ArchCare Senior Life as a ‘duplicate’ of the first claim, submit the CMS-1500 or UB04 and written clearly ‘Corrected Claim Re-submission’ in bold at the top of the claim form and specify the ArchCare Senior Life claim number to the right of the re-submission statement on the CMS-1500 or UB-04, as appropriate. Over payments ArchCare Senior Life periodically reviews payments made to providers to ensure the accuracy of claim payment pursuant to the terms of the provider contract or as part of its continuing utilization review and fraud control programs. In doing so, ArchCare Senior Life may identify instances when we have overpaid a provider for certain services. When this happens, ArchCare Senior Life provides notice to the provider and recoups the overpayment consistent with Section 3224-b of the New York Sate Insurance Law. ArchCare Senior Life will not pursue overpayment recovery efforts for claims older than twentyfour (24) months after the date of the original payment to a provider unless the overpayment is: • • • Based upon a reasonable belief of fraud, intentional misconduct or abusive billing; Required or initiated by the request of a self-insured plan or, Required by a state or federal government program. In addition, if a provider asserts that ArchCare Senior Life has underpaid any claim(s) to a provider, ArchCare Senior Life may offset any underpayments that may be owed against past overpayments made by ArchCare Senior Life dating as far back as the claim underpayment. Notice of Overpayments Before Seeking Recovery If ArchCare Senior Life has determined that an overpayment has occurred, ArchCare Senior Life will provide thirty (30) days written notice to the provider of the overpayment and request repayment. This notice will include the Participant’s name, service date(s), payment amount(s), proposed adjustment and a reasonably specific explanation of the reason for the overpayment and the adjustment. In response to this notice, the provider may dispute the finding or remit payment as outlined below. 31 If you Agree That We Have Overpaid You Upon receipt of a request for repayment, providers may voluntarily submit a refund check made payable to ArchCare Senior Life within 30 calendar days from the date the overpayment notice was mailed by ArchCare Senior Life. Providers should further include a statement in writing regarding the purpose of the refund check to ensure the proper recording and timely processing of the refund. Refund check should be mailed to: ArchCare Senior Life 33 Irving Place, 11th Floor New York, NY 10003 Attention: Provider Disputes If You Disagree that We Overpaid You If a provider disagrees with ArchCare Senior Life’s determination concerning the overpayment, the provider must submit a written request for an appeal within 30 calendar days from the date the overpayment notice was mailed by ArchCare Senior Life and include all supporting documentation in accordance with the provider appeal procedure. If upon reviewing all supporting documentation submitted by a provider, ArchCare Senior Life determines that the overpayment determination should be upheld, providers may initiate arbitration pursuant to their provider agreement. ArchCare Senior Life will proceed to offset the amount of the overpayment prior to any final determination made pursuant to binding arbitration. If You Fail to Respond to Our Notice of Overpayment If a provider fails to dispute a request for repayment concerning an overpayment determination made by ArchCare Senior Life within 30 calendar days from the date the overpayment notice was mailed by ArchCare Senior Life, the provider will have acknowledged and accepted the amount requested by ArchCare Senior Life. ArchCare Senior Life will offset the amount outstanding against current and future claim remittance(s) until the full amount is recovered by ArchCare Senior Life. 32 Medical Records 1. Access to Medical Records a. Provider shall maintain adequate medical records for all participants treated by Provider. Subject to all applicable statutory and legal privacy and confidentiality requirements, such medical records shall remain available to each physician and other health professionals treating the Participant, and upon request to any ArchCare Senior Life committee for review to determine whether the medical record and quality of services provided are acceptable, as well as for peer review and incident and grievance review and investigation. b. During normal business hours, ArchCare Senior Life, New York State Department of Health, CMS, or the Comptroller of the State of New York or the authorized representatives have the right, upon request, to inspect the accounting, administrative, and medical records maintained by Providers pertaining to ArchCare Senior Life, the participant, and to the Provider's participation hereunder during the term of this agreement and for ten (10) years thereafter. Provider shall comply with all applicable state and federal law regarding access to books and records. 2. Record Retention a. Provider shall keep and maintain all records relating to ArchCare Senior Life in compliance with applicable requirements of DOH and CMS. These records include but are not limited to: 1) Records related to services provided to Participants, including separate Medical Record for each Participant; 2) all financial records and statistical data that DOH and any other state or federal agency may require including books, accounts, journals, ledgers, and all financial records relating to capitation payments, third party health insurance recovery, and other revenue received and expenses incurred under this Agreement; 3) appropriate financial records to document fiscal activities and expenditures, including records relating to the sources and application of funds and to the capacity of Provider or its subcontracts, if relevant, to bear the risk of potential financial losses; and 4) Personnel records. b. ArchCare Senior Life shall maintain all financial records and statistical data according to generally accepted accounting principles. 33 c. Provider agrees to preserve records related to their contract with ArchCare Senior Life for the term the agreement is in effect and for ten (10) years thereafter, with disposal by Provider of any records during said period permitted only upon prior written approval by ArchCare Senior Life and DOH. Records involving matters in litigation shall be kept for a period permitted only upon prior written approval by ArchCare Senior Life and DOH. Records involving matters in litigation shall be kept for a period of not less than three (3) years following the termination of the litigation, in addition to the previously specified ten years, Microfilm or Electronic copies of records may be substituted for the originals with the prior written approval of ArchCare Senior Life and DOH, provided that the microfilming procedures are accepted by ArchCare Senior Life and DOH as reliable and are supported by an adequate retrieval system. d. All provisions of this Agreement relating to maintaining and retaining records shall survive the termination of your Agreement with ArchCare Senior Life and shall bind Provider until the expiration of the records retention period. 3. Access and Audit of Records a. At all times during the period that our ArchCare Senior Life is in force and for a period of ten (10) years thereafter, Provider shall provide ArchCare Senior Life and all authorized representatives of the state and federal governments with full access to its records which pertain to services performed, and determination of amounts payable under this agreement, including access to appropriate individuals with knowledge of financial records (including providers independent public auditors) and full access to any additional records they may process which pertain to services performed and determination of amounts payable under this Agreement, permitting such representatives to examine, audit and copy such records at the site at which they are located. Such access shall include both announced and unannounced inspections and on-site audits. b. All records and information obtained by ArchCare Senior Life pursuant to the provision of their agreement with providers, whether by audit or otherwise, shall be usable by ArchCare Senior Life in any manner, in its sole discretion, it deems appropriate and provider shall have no right of confidentiality or proprietary interest in such records or information. c. Notwithstanding the preceding sentence, ArchCare Senior Life agrees, in those instances in which it has discretion, not to disclose outside of its agency the following data: • • • • 34 any resume or other description of qualification which includes the name of an individual; any individual’s actual salary; provider’s indirect rates including labor, overhead, G&A and fee; and, the methodology for calculating those indirect rates including the allocation base. d. ArchCare Senior Life will use or disclose Medicaid recipient identifiable information obtained only as authorized under applicable provisions of federal and state law. • Provider shall promptly notify ArchCare Senior Life of any request for access to any records maintained pursuant to their contract with ArchCare Senior Life. • All provisions of your Agreement with ArchCare Senior Life relating to access and audit of records shall survive the termination of the Agreement and shall bind provider until the expiration of the record retention period. HITECH Act The Health Information Technology for Economic and Clinical Health (HITECH) Act was passed as part of the American Recovery and Reinvestment Act of 2009 to promote the adoption and meaningful use of health information technology. Subtitle D of the HITECH Act addresses the privacy and security concerns associated with the electronic transmission of health information, in part, through several provisions that strengthen the civil and criminal enforcement of the HIPAA rules. Enacted in part to assist healthcare providers who are, or will be, utilizing electronic health records (EHR) systems, the HITECH Act addresses consumer access to their EHR, increases application of HIPAA privacy standards to business associates of covered entities, and implements a tiered system of civil monetary penalties for HIPAA violations. Under the HITECH Act, business associates are now responsible for complying with the provisions and regulations of HIPAA and are directly answerable to the government for HIPAA breaches. Business associates are now also directly liable for civil and criminal penalties. This increased statutory liability for business associates under HIPAA will likely result in the necessity of updating business associate and vendor lists as well as renegotiating business associate agreements. In addition, business associates will most likely incur costs associated with bringing themselves into direct HIPAA compliance. The Secretary of the Department of Health and Human Services (HHS) will ultimately issue guidance regarding these safeguards. The HITECH Act also expands the notification requirements due to breaches of an individual’s PHI. Both covered entities and business associates are now obligated to notify individuals of breaches of their PHI. In cases where more than 500 “residents of a State or jurisdiction” have had their PHI breached, “prominent media outlets” serving that area must also be notified. Individuals should be notified in writing or e-mail if that is their preferred method of contact, and be provided with basic information about the breach, such as: • when the breach happened, when the event was discovered, and a brief statement about what happened; • what type of PHI was breached; • things that the individual can do in order “to protect themselves from potential harm resulting from the breach”; 35 • what corrective actions and investigation the covered entity is doing to prevent future breaches and mitigate losses; and contact information for the individual to use in case of any questions. In addition to disclosure accounting, the individual is also entitled to receive a copy of his or her electronic health record, if they request; this information may be sent to the individual, or another person designated by individual. For more information about the HITECH Act, please visit the CMS website at www.cms.gov. 36 Fraud Waste & Abuse ArchCare Senior Life operates a comprehensive compliance program that actively investigates allegations of fraud, abuse and waste on the part of providers and participants. Fraud and abuse are broadly defined as intentional deception or misrepresentation that results in an unauthorized benefit, payment or inappropriate care. The following are some examples of fraudulent, abusive, and unacceptable practices that are prohibited by ArchCare Senior Life: • • • • • • • Submission of false information for the purpose of obtaining greater compensation than that to which the provider is legally entitled (i.e. up coding or unbundling of charges). Billing for services not rendered or billing in advance of care. Knowingly demanding or collecting any compensation in addition to claims submitted for covered services (except where permitted by law). Ordering or furnishing inappropriate, improper, unnecessary or excessive care services or supplies. Failing to maintain or furnish, for audit and investigative purposes, sufficient documentation on the extent of care and services rendered to participants. Offering or accepting inducements to influence participants to join the plan or to use or avoid using a particular service. Submitting bills or accepting payment for care, services or supplies rendered by a provider who has been disqualified from participation in the Medicare or Medicaid programs. Providers must comply with federal laws and regulations designed to prevent fraud, waste and abuse, but not limited to, applicable provisions of federal criminal law, the False Claims Act, the anti-kickback statute, and the Health Insurance Portability and Accountability Act administrative simplification rules, applicable state and federal law, including, but not limited to, Title VI of The Civil Rights Act of 1964, the Rehabilitation Act of 1973, the Age Discrimination Act of 1975, the Americans with Disabilities Act and all other laws applicable to recipients of federal funds from which payments to providers under this Agreement are made in whole or in part, and all applicable Medicare laws, regulations, reporting requirements, and CMS instructions. Confirmed cases of fraud and abuse are reported to the appropriate state agency. Providers who suspect fraud, waste and abuse on the part of another provider or a participant should contact the ArchCare Compliance Hotline at 1-800-4430463. Remember, you may report anonymously as ArchCare Senior Life abides by a zero-tolerance against non-compliance. 37 HIPAA and Releasing Information ArchCare Senior Life is concerned with protecting participant privacy and is committed to complying with the Health Insurance and Portability Act (HIPAA) privacy regulations. Generally, covered health plans and covered providers are not required to obtain individual participant consent or authorization for use and disclosure of Protected Health Information (PHI) for treatment, payment and health care operations. Activities such as: care coordination, reviewing the competence of health care professionals, billing/claims management, and quality improvement fall into this category. If you have further concerns, please contact Customer Service at 1-866263-9083. QUALITY ASSESSMENT AND PERFORMANCE IMPROVEMENT (QAPI) A. ArchCare Senior Life's Quality Management Committee performs a critical element of quality assessment performance improvement through audits of authorized services, review of incidents, investigation of service delivery failures, and participant satisfaction surveys. The process of service delivery in the PACE model requires the team to identify participant problems, determine appropriate treatment goals, select interventions, and evaluate efficiencies of care on an individual basis. This activity is the foundation for all subsequent QAPI and utilization review activities. B. ArchCare Senior Life maintains a written QAPI Plan provides a system of ongoing assessment, implementation, evaluation, and revision of activities related to overall program administration and services. The QAPI plan identifies specific and measurable activities to be undertaken. The QAPI plan includes, at the minimum, the following essential elements: • • • 38 Standards that are performance benchmarks, established in conjunction with the Provider, and are incorporated into the Provider Manual as appropriate. Such performance benchmarks may include measures of access and availability of service including response time to referrals, timelines of treatment/ implementation of plan of care Performance goals provide a framework for QAPI activities, evaluation, and corrective action. Performance Improvement indicators need to be single outcome measurable variables related to the required services provided by ArchCare Senior Life. The methodology should assure that all care settings (e.g., ArchCare Senior Life’s contracted Providers, PACE Center, and home health care settings) are included in the scope of services being measured and monitored. Quality performance indicators should be selected for review on the basis of high volume, high risk, diagnoses or clinical procedures, adverse outcomes, functional outcomes, or other problem related to the health and welfare of the participants. • • • • • • • • Process to review the effectiveness of ArchCare Senior Life’s interdisciplinary team in its ability to assess participant’s care needs, identify the participant’s treatment goals, assess the effectiveness of interventions, evaluate adequacy and appropriateness of service utilization and reorganize a plan of care as necessary. Process for aggregating data for purposes of conducting overall program utilization analysis and provider performance analysis. Contracted Providers are asked to complete and communicate feedback via the Contract Providers Survey and provide written summaries of participant care and service delivery. Policies and procedures related to establishing quality committees that: Evaluate data collected pertaining to quality indicators; include contracted service provider MDS reports, NYS DOH survey results and quarterly care conference per contract request. address the process and outcomes of the QAPI plan; and provide input related to ethical decision making including end-of-life issues and implementation of the Patient Self-Determination Act. Participant, contracted service providers and caregiver involvement in the QAPI plan and evaluation of Participant satisfaction with services. 39 Participant Grievances and Appeals ArchCare Senior Life promotes open communication with its participants, and is committed to addressing any complaints, either written or verbal regarding dissatisfaction with service delivery, quality of care, and non-coverage or nonpayment of services being provided by ArchCare Senior Life. A participant or designated representative may make a complaint at any time, or an appeal when there has been a denial, reduction or termination of services. It is policy that ArchCare Senior Life continues to provide care to the participant during the grievance or appeal process without fear of any reprisal. A grievance or appeal will be kept confidential and in no way will the grievance or appeal adversely affect a person's care or services. ArchCare Senior Life investigates grievances and appeals, and informs participants of their complaint and appeal rights at each juncture of the process. We hope that grievances and appeals are addressed to one's satisfaction in a prompt and courteous manner. The right to file a grievance or appeal is made known to the participant in writing upon enrollment, and annually thereafter. For persons who do not speak English, a bilingual staff member, or translation service are available to help with the grievance and appeal processes. GRIEVANCE PROCEDURES: Definition: A grievance is a complaint, either written or verbal, expressing dissatisfaction with service delivery or quality of care. Each time there is an expression of dissatisfaction with service delivery or quality of care a participant has a grievance. The participant will be provided with, and will have an opportunity to discuss, a written explanation of the specific steps that will be taken or already have been taken to resolve the grievance. Participants are encouraged to give complete information regarding their grievance so that appropriate staff can resolve grievances in a timely manner. Participants may designate a representative to file a grievance on their behalf. Contractors receiving complaints from participants must report them to the ArchCare Senior Life Director of Quality Management or the Executive Director. When a participant files a grievance you may contact ArchCare Senior Life staff in person or call (866) 263-9083. Our 24 hour answering service is available after business hours and on the weekends. If a solution is immediately found regarding a grievance and agreed to by the participant (or designated representative), the grievance is considered resolved. ArchCare Senior Life staff seeks to address and resolve grievances as quickly as possible to ensure satisfaction. A participant may request reconsideration of a grievance decision if they are dissatisfied with the outcome of the grievance process. To do so, they may contact the ArchCare Senior Life Quality Management Department or Executive Director within thirty (30) days of the team’s written decision. 40 APPEAL PROCEDURES: Definition: An appeal is a participant’s action taken with respect to noncoverage of or nonpayment for a service including denials, reduction or termination of services. A participant has up to 45 days to request an appeal from the date of notification of noncoverage. Participants or designated representatives may make an appeal with any staff member. Participants are encouraged to give complete information so following up on an appeal can be completed in a timely manner. Participants may designate a representative to file an appeal on their behalf. Contractors receiving complaints must report them to ArchCare Senior Life. The Director of Clinical Services coordinates appeals. Clinical aspects of appeals are reviewed by qualified clinical personnel not involved in the decision. During the appeals process, ArchCare Senior Life may not reduce or terminate disputed services while an appeal is pending if the participant has requested continuation of the services. If the decision is not in the participant’s favor, the participant may be held liable for the cost of services. EXPEDITED APPEALS PROCESS: An expedited appeal may be requested should a participant believe that his or her life, health, or ability to regain or maintain maximum function could be seriously jeopardized absent the provision of a service. ArchCare Senior Life will respond in writing to confirm receipt of appeal within 24 hours of receipt. An expedited appeal must be resolved within 72 hours. Notification of the resolution will be shared with the participant (or designated representative) verbally and in writing immediately upon resolution. Care will continue until notification of this resolution. ADDITIONAL APPEAL RIGHTS UNDER MEDICARE AND MEDICAID: The appeal processes are reviewed with participants upon enrollment and annually thereafter by the social worker. The social worker is responsible for informing participants or designated representatives of their additional appeal rights under Medicare or Medicaid managed care, or both, and a right to having a Fair Hearing. The social worker may assist the participant in choosing which to pursue if both are applicable. In the event that Medicaid is applicable, ArchCare Senior Life's social worker can offer a Fair Hearing notice to the participant to exercise an external appeal to the New York State Office of Hearing and Appeals. When Medicare is involved, an external appeal, if elected, will be forwarded to the Medicare Designated Review Agent. State and Federal Complaint Options: A participant or designated representative may file a complaint at any time. To pursue complaints with the New York State Department of Health Managed Long Term Care hotline call 1-866-712-7197. 41 APPENDIX – A ArchCare Senior Life Provider Addition/Change Request Form INSTRUCTIONS: Type or print your information on this form. If a question does not apply, write "N/A" in the field. A separate form will be needed for each Provider. Check the appropriate box: o Change of Information* o Credentialing Request Date of Request Practice Name Provider Name Specialty Board Certification o Yes oNo Tax ID NPI Primary Office Location Secondary Office Location Provider Signature *Requests for change of demographic information will be reflected in ArchCare Senior Life within 48 hours. representative will contact you within that time frame to advise when the change has taken effect. A In receiving this form from the physician or entity, ArchCare Senior Life relies on the truth of all the following statements: � � � 42 All information entered is accurate and complete, and that if any of that information changes, Provider will notify ArchCare Senior Life of any such change within 30 days. By submitting this form, Provider agrees to abide by all Medicare statutes, rules, and policies. Please submit request form to: ArchCare Senior Life / PACE Attention: Credentialing Department 33 Irving Place, 11th Floor New York, NY 10003 Fax: 646-417-7157 Definitions I. Enrollment Agreement is defined as the Enrollment Agreement issued by ArchCare Senior Life that describes its obligations to arrange for the delivery of medical care to ArchCare Senior Life participants who are eligible for such services pursuant to the terms of Plan's contract with the New York State Department of Health and Department of Health and Human Services (DHHS), Centers for Medicare and Medicaid Services. II. Covered Service is defined as those services which are medically indicated and which Participants are entitled to receive under the terms of the Enrollment Agreement. III. DOH is defined as the New York State Department of Health. IV. An Emergency medical condition is defined as a condition manifesting itself by acute symptoms of sufficient severity (including severe pain) such that a prudent lay person, with an average knowledge of health and medicine, could reasonably expect the absence of immediate attention to result in: a. Serious jeopardy to the health of the individual; b. Serious impairment to bodily functions; or c. Serious dysfunction of any organ or part. V. CMS is defined as the Centers for Medicare and Medicaid Services. VI. Medically Indicated Services is defined as those health care services or items defined by the Plan's medical director and a) provide for the diagnosis, prevention, or direct care of a medical condition; b) are appropriate and necessary, for the diagnosis, prevention, or treatment of a medical condition and could not be omitted without adversely affecting the Participant’s condition; c) are within standards of good medical practice recognized within the organized medical community; d) are appropriate to and consistent with the Participant’s diagnosis and, (except for Emergency Services or Urgent Services) their plan of care; e) would be likely to materially improve or to help in maintaining the Participant’s physical condition; or f) would be likely to materially improve or to help in maintaining the Participant’s ability to engage in essential activities of daily living g) are not primarily for the convenience of the Participant or his/ her family, his/ her physician, or another care provider; and h) are the most appropriate and economical level and source of care or supply that can be provided safely. The foregoing provisions shall be determined by the Plan's medical director or designee. 43 VII. Participant is defined as any person who is eligible to receive Covered Services under the eligibility criteria set by DOH and is enrolled in ArchCare Senior Life. VIII. Interdisciplinary Team is defined as a group of health professionals or care givers composed of the primary care physician, registered nurse, social worker, physical therapist, occupational therapist, recreational therapist, activity coordinator, dietitian, PACE Center manager, home health care coordinator, home health aides/ personal care attendants, and drivers. IX. PACE is defined as the Program of All-Inclusive Care for the Elderly. It offers a benefit plan to frail seniors who are nursing home eligible who live at home with the support of PACE services. PACE is an integrated comprehensive program that combines the services of an adult day center, home health care, medical outpatient clinic on-site, and network of specialty care providers including inpatient hospital and nursing home care when needed. Funding combines both Medicare and Medicaid capitated payments in paying for the services. X. Participating Agency is defined as an agency or health care provider that has signed an ArchCare Senior Life Service Agreement. XI. Primary Physician is defined as any physician, professional service corporation or partnership who or which has agreed to provide specific primary health services to Participants and to coordinate the overall health care of Participants as their primary care physician. XII. A Provider is defined as those individual providers of individual services who are contracted vendors. The Provider must meet applicable New York state licensure, certification, or registration requirements in which they practice, and meet ArchCare Senior Life’s credentialing criteria. XIII. Quality Assurance Performance Improvement (QAPI): ArchCare Senior Life has a quality assurance performance improvement committee consisting of its program director, director of participant services, medical director and other clinical and non-clinical professional staff as deemed appropriate. All Contracted Service Providers are encouraged to participate in Quality Assessment. CENTERS FOR MEDICARE & MEDICAID SERVICES 44 Quick Facts about Programs of All-inclusive Care for the Elderly (PACE) What are Programs of All-inclusive Care for the Elderly (PACE)? PACE is a Medicare program for older adults and people over age 55 living with disabilities. This program provides community-based care and services to people who otherwise need nursing home level of care. PACE was created as a way to provide you, your family, caregivers, and professional health care provider’s flexibility to meet your health care needs and to help you continue living in the community. An interdisciplinary team of professionals will give you the coordinated care you need. These professionals are also experts in working with older people. They will work together with you and your family (if appropriate) to develop your most effective plan of care. PACE provides all the care and services covered by Medicare and Medicaid, as authorized by the interdisciplinary team, as well as additional medically-necessary care and services not covered by Medicare and Medicaid. PACE provides coverage for prescription drugs, doctor care, transportation, home care, check ups, hospital visits, and even nursing home stays whenever necessary. With PACE, your ability to pay will never keep you from getting the care you need. Who can join a PACE Plan? You can join PACE if you meet the following conditions: • You are 55 years old or older. • You live in the service area of a PACE organization. • You are certified by the state in which you live as meeting the need for the nursing • home level of care. You are able to live safely in the community when you join with the help of PACE services. - Note: You can leave a PACE program at any time. 45 PACE services include but aren’t limited to the following: � Primary Care (including doctor and nursing services) � Adult Day Care � Hospital Care � Recreational Therapy � Medical Specialty Services � Meals � Prescription Drugs � Dentistry � Nursing Home Care � Nutritional Counseling � Emergency Services � Social Services � Home Care � Laboratory / X-Ray Services � Physical Therapy � Social Work Counseling � Occupational Therapy � Transportation PACE also includes all other services determined necessary by your team of health care professionals to improve and maintain your overall health. You should know this about PACE: PACE Provides Comprehensive Care PACE uses Medicare and Medicaid funds to cover all of your medically-necessary care and services. You can have either Medicare or Medicaid or both to join PACE. The Focus is on You You have a team of health care professionals to help you make health care decisions. Your team is experienced in caring for people like you. They usually care for a small number of people. That way, they get to know you, what kind of living situation you are in, and what your preferences are. You and your family participate as the team develops and updates your plan of care and your goals in the program. PACE Covers Prescription Drugs PACE organizations offer Medicare Part D prescription drug coverage. If you join a PACE program, you’ll get your Part D-covered drugs and all other necessary medication from the PACE program. Note: If you are in a PACE program, you don’t need to join a separate Medicare drug plan. If you do, you will lose your PACE health and prescription drug benefits. 46 You should know this about PACE: (continued) PACE Supports Family Caregivers PACE organizations support your family members and other caregivers with caregiving training, support groups, and respite care to help families keep their loved ones in the community. PACE Provides Services in the Community PACE organizations provide care and services in the home, the community, and the PACE center. They have contracts with many specialists and other providers in the community to make sure that you get the care you need. Many PACE participants get most of their care from staff employed by the PACE organization in the PACE center. PACE centers meet state and Federal safety requirements and include adult day programs, medical clinics, activities, and occupational and physical therapy facilities. PACE is Sponsored by the Health Care Professionals Who Treat You PACE programs are provider sponsored health plans. This means your PACE doctor and other care providers are also the people who work with you to make decisions about your care. No higher authorities will overrule what you, your doctor, and other care providers agree is best for you. If you disagree with the interdisciplinary team about your care plan, you have the right to file an appeal. Preventive Care is Covered and Encouraged The focus of every PACE organization is to help you live in the community for as long as possible. To meet this goal, PACE organizations focus on preventive care. Although all people enrolled in PACE are eligible for nursing home care, only 7% live in nursing homes. PACE Provides Medical Transportation PACE organizations provide all medically-necessary transportation to the PACE center for activities or medical appointments. You can also get transportation to appointments in the community. What You Pay for PACE Depends on Your Financial Situation If you qualify for Medicare, all Medicare-covered services are paid for by Medicare. If you also qualify for your State’s Medicaid program, you will either have a small monthly payment or pay nothing for the long-term care portion of the PACE benefit. If you don’t qualify for Medicaid you will be charged a monthly premium to cover the long-term care portion the PACE benefit and a premium for Medicare Part D drugs. However, in PACE there is never a deductible or copayment for any drug, service, or care approved by the PACE team. 47 For more information about PACE do the following: • Visit www.npaonline.org on the web. This website is sponsored by the National PACE Association. • Visit www.medicare.gov/Nursing/Alternatives/PACE.asp on the web. • Call 1-800-MEDICARE (1-800-633-4227). TTY users should call 1-877-4862048. CMS Publication No. 11341 January 2008 48
© Copyright 2026