Orthopnea and Tidal Expiratory Flow Limitation in Chronic Heart Failure*
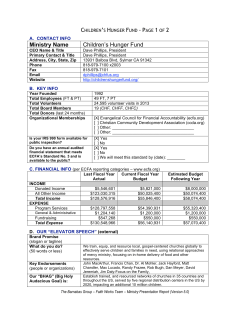
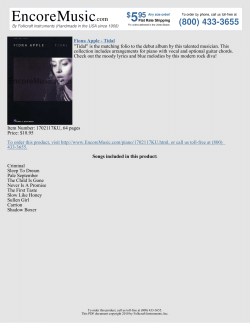
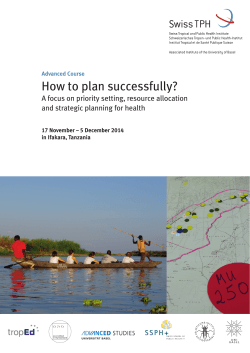
CHEST Original Research HEART FAILURE Orthopnea and Tidal Expiratory Flow Limitation in Chronic Heart Failure* Roberto Torchio, MD; Carlo Gulotta, MD; Pietro Greco-Lucchina, MD; Alberto Perboni, MD; Luigina Avonto, MD; Heberto Ghezzo, MD; and Joseph Milic-Emili, MD Background: Tidal expiratory flow limitation (FL) is common in patients with acute left heart failure and contributes significantly to orthopnea. Whether tidal FL exists in patients with chronic heart failure (CHF) remains to be determined. Purpose: To measure tidal FL and respiratory function in CHF patients and their relationships to orthopnea. Methods: In 20 CHF patients (mean [ⴞ SD] ejection fraction, 23 ⴞ 8%; mean systolic pulmonary artery pressure [sPAP], 46 ⴞ 18 mm Hg; mean age, 59 ⴞ 11 years) and 20 control subjects who were matched for age and gender, we assessed FL, Borg score, spirometry, maximal inspiratory pressure (PImax), mouth occlusion pressure 100 ms after the onset of inspiratory effort (P0.1), and breathing pattern in both the sitting and supine positions. The Medical Research Council score and orthopnea score were also determined. Results: In the sitting position, tidal FL was absent in all patients and healthy subjects. In CHF patients, PImax was reduced, and ventilation and P0.1/PImax ratio was increased relative to those of control subjects. In the supine position, 12 CHF patients had FL and 18 CHF patients claimed orthopnea with a mean Borg score increasing from 0.5 ⴞ 0.7 in the sitting position to 2.7 ⴞ 1.5 in the supine position in CHF patients. In contrast, orthopnea was absent in all control subjects. The FL patients were older than the non-FL patients (mean age, 63 ⴞ 8 vs 53 ⴞ 12 years, respectively; p < 0.03). In shifting from the seated to the supine position, the P0.1/PImax ratio and the effective inspiratory impedance increased more in CHF patients than in control subjects. The best predictors of orthopnea in CHF patients were sPAP, supine PImax, and the percentage change in inspiratory capacity (IC) from the seated to the supine position (r2 ⴝ 0.64; p < 0.001). Conclusions: In sitting CHF patients, tidal FL is absent but is common supine. Supine FL, together with increased respiratory impedance and decreased inspiratory muscle force, can elicit orthopnea, whom independent indicators are sPAP, supine PImax and change in IC percentage. (CHEST 2006; 130:472– 479) Key words: chronic heart failure; expiratory tidal flow limitation; orthopnea Abbreviations: AHF ⫽ acute heart failure; CHF ⫽ chronic heart failure; Dlco ⫽ diffusing capacity of the lung for carbon monoxide; ERV ⫽ expiratory reserve volume; FEF75 ⫽ forced expiratory flow when 75% of FVC has been exhaled; FL ⫽ flow limitation; FRC ⫽ functional residual capacity; IC ⫽ inspiratory capacity; MRC ⫽ Medical Research Council; NEP ⫽ negative expiratory pressure; P(A-a)O2 ⫽ alveolar-arterial oxygen pressure difference; PCWP ⫽ pulmonary capillary wedge pressure; PEEPi ⫽ intrinsic positive end-expiratory pressure; Pimax ⫽ maximal inspiratory pressure; Pimus ⫽ pressure generated from inspiratory muscles; P0.1 ⫽ mouth occlusion pressure 100 ms after onset of inspiratory effort; Prs ⫽ relaxation pressure; Raw ⫽ airway resistance; RV ⫽ residual volume; sPAP ⫽ systolic pulmonary artery pressure; TLC ⫽ total lung capacity; V˙o2max ⫽ maximal oxygen uptake; Vr ⫽ relaxation volume; Vt ⫽ tidal volume rthopnea is a major complaint of patients with acute O heart failure (AHF). Although its nature is multifactorial, recent studies1,2 have shown that tidal expiratory flow limitation (FL) is common in supine patients with acute AHF in whom, by imposing an inspiratory threshold 472 Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 load due to dynamic hyperinflation and intrinsic positive end-expiratory pressure (PEEPi), contributes significantly to orthopnea. While in the sitting patients with chronic heart failure (CHF) tidal FL is absent,3 its prevalence in patient in the supine position has not as yet been assessed. Original Research Accordingly, in seated and supine CHF patients and in age-matched and sex-matched control subjects we have assessed the following: the prevalence of tidal FL and its association to dyspnea and orthopnea. In addition, we have measured the maximal inspiratory pressure (Pimax), blood gas levels at rest, and the control of breathing. Materials and Methods Patients The study was carried out on 20 stable ambulatory patients (18 men) with congestive heart failure due to cardiomyopathy (6 postischemic patients) without pleural effusions. No patients had been hospitalized within the 20 days preceding the study. No patients were current smokers, but nine patients were exsmokers. All patients received therapy with diuretics. Within a month prior to our study, the Weber class was determined by cardiopulmonary exercise testing as follows4: Weber class B, 7 patients (maximal oxygen uptake [V˙o2max], between 16.0 and 19.8 mL/kg/min); Weber class C, 10 patients (V˙o2max, between 11.7 and 15.5 mL/kg/min); and Weber class D, 3 patients (V˙o2max, between 7.1 and 9.8 mL/kg/min). Heart failure was defined as symptomatic left ventricular dysfunction, with a left ejection fraction of ⬍ 0.45 documented by bidimensional echocardiography. Patients were excluded from the study if they had primary pulmonary, neurologic, or myopathic disease. Echocardiographic ejection fraction, systolic pulmonary artery pressure (sPAP), and heart diameters were measured within the 2 weeks preceding our study. Twenty healthy subjects (ie, control subjects) matched for sex and age were also studied. All control subjects were nonsmokers, but nine patients were ex-smokers (Table 1). The study was approved by the local ethics committee, and informed consent was obtained from each subject. In the subjects in the present study, the closing capacity and gas exchange were assessed in the sitting position, as previously described.3 Chronic dyspnea was scored using the modified Medical Research Council (MRC) scale based on six increasing grades (0 to 5).5 Seated and supine dyspnea were measured by a modified Borg scale, ranking the magnitude from 0 (none) to 10 (maximal).6 Twenty minutes of positioning in the decubitus position was required before assessing the supine Borg score. Orthopnea was defined as a worsening of the Borg score with the patient in the supine position.7 Twelve months after this study, it was possible to retrieve the clinical data of 13 of the 20 patients. Three patients had died, and 10 patients were still alive. *From Fisiopatologia Respiratoria (Drs. Torchio, Gulotta, and Perboni) and Cardiology (Drs. Greco-Lucchina and Avonto), Ospedale San Luigi Gonzaga, Orbassano, Turin, Italy; and Meakins-Christies Laboratories (Drs. Ghezzo and Milic-Emili), McGill University, Montreal, QC, Canada. The authors have reported to the ACCP that no significant conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article. Manuscript received December 23, 2005; revision accepted February 13, 2006. Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml). Correspondence to: Roberto Torchio, MD, Fisiopatologia Respiratoria, Ospedale S Luigi Gonzaga, I-10043 Orbassano, Torino, Italy; e-mail: [email protected] DOI: 10.1378/chest.130.2.472 www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 Table 1—Anthropometric Characteristics and Baseline Respiratory Data for Control Subjects and CHF Patients Measured in the Seated Position* Variables Sex, No. Male Female Age, yr BMI, kg/m2 Nonsmokers, No. Ex-smokers, No. Ejection fraction, % sPAP, mm Hg LVTDV, mL FEV1, % predicted FVC, % predicted FEV1/FVC, % predicted FEF75, % predicted TLC, % predicted FRC, % predicted IC, % predicted ERV, % predicted RV, % predicted Dlco, % predicted P(A-a)O2, kPa MRC score Borg score Control Subjects CHF Patients (n ⫽ 20) (n ⫽ 20) 18 2 59 ⫾ 11 23 ⫾ 8 11 9 105 ⫾ 11 103 ⫾ 11 105 ⫾ 7 78 ⫾ 23 97 ⫾ 7 93 ⫾ 13 103 ⫾ 13 103 ⫾ 13 93 ⫾ 11 94 ⫾ 11 2.7 ⫾ 0.5 0 0 18 2 59 ⫾ 11 26 ⫾ 3 11 9 23 ⫾ 8 46 ⫾ 18 313 ⫾ 61 82 ⫾ 19 82 ⫾ 18 102 ⫾ 7 51 ⫾ 24 81 ⫾ 15 78 ⫾ 12 84 ⫾ 20 56 ⫾ 23 88 ⫾ 17 69 ⫾ 21 4.3 ⫾ 1.2 2.2 ⫾ 1 0.5 ⫾ 0.7 p Value NS NS ⬍ 0.001 ⬍ 0.001 NS ⬍ 0.001 ⬍ 0.001 ⬍ 0.001 ⬍ 0.001 ⬍ 0.001 NS ⬍ 0.001 ⬍ 0.001 *Values are given as the mean ⫾ SD, unless otherwise indicated. BMI ⫽ body mass index; LVTDV ⫽ left ventricular telediastolic volume; NS ⫽ not significant. Each patient underwent a spirometric, plethysmographic, and diffusing capacity of the lung for carbon monoxide (Dlco) study that was performed in the sitting position. Using a plethysmograph (Autobox 2800; SensorMedics; Yorba Linda, CA), airway resistance (Raw) was measured at a panting frequency of ⬍ 1 Hz. Spirometric and plethysmographic volumes were assessed according to European Respiratory Society (ERS).8 Dlco was measured with a water-sealed spirometer (Biomedin; Padua, Italy) using helium for alveolar volume measurement.8 Predicted values for Raw were from Peslin et al,9 and those for Dlco from the ERS.8 Breathing pattern, mouth occlusion pressure 100 ms after the onset of inspiratory effort (P0.1), and Pimax were measured (VMAX 229; SensorMedics) as previously described.10 The Pimax was measured at residual volume (RV) according to American Thoracic Society/ERS11 with predicted values from Black and Hyatt.12 Tidal FL was assessed with the negative expiratory pressure (NEP) technique.13 A NEP of ⫺5 cm H2O was applied (Direc/ NEP System 200A; Raytech Instruments; Vancouver, BC, Canada) 0.2 s after the onset of expiration. Flow-volume curves obtained without and with NEP were superimposed as follows: patients in whom the expiratory flow with NEP was the same as the reference flow during part of the whole expiration were considered to have FL.13 Pao2 and Paco2 were also measured with a blood gas analyzer (ABL 735; Radiometer; Copenhagen, Denmark); the PAo2 that was used to compute the alveolar-arterial oxygen pressure difference (P[A-a]O2) was estimated with the following equation: PAo2 ⫽ [(PB ⫺ 47) ⫻ Fio2)] ⫺ Paco2/R CHEST / 130 / 2 / AUGUST, 2006 473 where PB is barometric pressure, Fio2 is the fraction of inspired O2, and R is the respiratory quotient, which was assumed to be 0.8. Statistical Analysis The data are presented as the mean ⫾ SD. Correlation coefficients were obtained with the Spearman ( value) nonparametric test for MRC score and the Pearson test (r value) for all other parameters. Where appropriate, paired and unpaired Student t tests were used. Statistical analysis was performed using a statistical software package (SPSS; SPSS Inc; Chicago, IL). Results Seated Table 1 shows the anthropometric characteristics and baseline respiratory data of CHF patients and control subjects. In control subjects, all respiratory data were within normal limits, the MRC and resting Borg scores were zero, and tidal FL was absent. In the CHF patients, the total lung capacity and its subdivisions were reduced relative to control subjects, while the FEV1/FVC ratio was within normal limits. In CHF patients, the functional residual capacity (FRC) percent predicted correlated negatively with the telediastolic volume of the left ventricle (r ⫽ ⫺0.52; p ⬍ 0.02) [Fig 1]. None of the CHF patient experienced FL in the seated position. In the CHF patients, the mean MRC score amounted to 2.2 ⫾ 1.0 (moderate breathlessness) and the mean Borg score was 0.5 ⫾ 0.7, with the two scores being weakly correlated (p ⬍ 0.05). In CHF patients, resting ventilation and P0.1 were Figure 1. Relationship between left ventricular telediastolic volume and FRC. % pred ⫽ percent predicted. 474 Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 high with respect to control subjects (Table 2). Since Pimax was reduced in CHF patients, the mean P0.1/Pimax ratio was very high relative to that in control subjects (5.3 ⫾ 4.2% vs 2.5 ⫾ 0.9%, respectively; p ⬍ 0.01). The Pao2 and Paco2 were lower in CHF patients than in control subjects, while the P(A-a)o2 was higher (Table 1). The MRC score was significantly higher in the CHF patients than in control subjects. This score was correlated with P0.1/Pimax ratio and respiratory rate. The mean MRC score and P0.1/Pimax ratio were the only significantly different parameters among CHF patients who died within 12 months and survivors (1.7 ⫾ 0.8 vs 3.3 ⫾ 1.2 [p ⬍ 0.02]; and 4 ⫾ 2 vs 11 ⫾ 8, respectively [p ⬍ 0.02]). Supine None of the control subjects experienced FL while in the supine position. In contrast, 12 CHF patients experienced FL while in the supine position, reflecting the decrease in supine expiratory reserve volume (ERV) with consequent decrease in expiratory flow reserve. None of the variables studied varied significantly among the 12 CHF patients who experienced FL while in the supine position and in the other 8 patients who did not experience FL while in the supine position. In contrast, there was a significant difference in mean age between these two groups (63 ⫾ 8 years vs 53 ⫾ 12 years, respectively; p ⬍ 0.03) but not in Weber class. The percentage of the tidal volume that entailed FL also correlated with age (r ⫽ 0.527; p ⬍ 0.02). It should be noted, however, that among the 12 FL patients 58% were ex-smokers, whereas in the non-FL group only 2 of 8 patients (25%) were ex-smokers. In the supine position, the Borg score increased markedly in CHF patients (ie, orthopnea7), while in the control subjects it remained zero (Table 2). This was associated with increased P0.1 and especially increased P0.1/Pimax ratio, with the latter reflecting in part the concurrent decrease in Pimax. The mean effective inspiratory impedance14 also increased from 5.3 ⫾ 1.8 to 7.6 ⫾ 2.7 cm H2O/L/s (p ⬍ 0.001), whereas the slight increase observed in control subjects was not significant. Supine Pimax was significantly reduced in both CHF patients (p ⬍ 0.001) and control subjects (p ⬍ 0.05). Moreover, in CHF patients with FL the mean Pimax reduction was highly significant (70 ⫾ 30 to 55 ⫾ 27 cm H2O; p ⬍ 0.001). The supine Borg score correlated with the change in inspiratory capacity (⌬IC) [r ⫽ ⫺0.59; p ⬍ 0.01] (Fig 2), supine Pimax (r ⫽ ⫺0.58; p ⬍ 0.01), sPAP (r ⫽ 0.53; p ⬍ 0.02) [ Fig 3], P0.1/Pimax ratio Original Research Table 2—Cardiac and Respiratory Data for 20 Control Subjects and 20 CHF Patients Measured in the Seated and Supine Positions* Control Subjects (n ⫽ 20) CHF Patients (n ⫽ 20) Variables Seated Supine Seated Supine IC, L ERV, L FVC, L FEV1, L FEV1/FVC ratio, % FEF75, L/s V˙e, L/min Vt, L Respiratory rate, breaths/min Pimax, % predicted P0.1/ Pimax, % P0.1/(Vt/tI), cm H2O/L/s MRC score FL/NFL ⌬Borg score 3.07 ⫾ 0.79 1.06 ⫾ 0.46 4.06 ⫾ 1.1 3.29 ⫾ 0.9 80 ⫾ 5 1.36 ⫾ 0.38 10.2 ⫾ 2.7 0.72 ⫾ 0.18 14.2 ⫾ 4.0 87 ⫾ 23 2.5 ⫾ 0.9 5.5 ⫾ 2.0 0 0/20 0 3.49 ⫾ 0.74† 0.74 ⫾ 0.32† 4.01 ⫾ 1.1 3.19 ⫾ 0.82 80 ⫾ 9 1.33 ⫾ 0.39 10.4 ⫾ 3.5 0.82 ⫾ 0.17¶ 13.2 ⫾ 4.0¶ 75 ⫾ 29¶ 3.6 ⫾ 1.5† 6.2 ⫾ 1.7 2.50 ⫾ 0.68‡ 0.62 ⫾ 0.28㛳 3.16 ⫾ 0.85㛳 2.49 ⫾ 0.64㛳 78 ⫾ 5 0.84 ⫾ 0.32㛳 12.9 ⫾ 5.0‡ 0.72 ⫾ 0.23 17.9 ⫾ 5.1‡ 69 ⫾ 30‡ 5.3 ⫾ 4.2㛳 5.3 ⫾ 1.8 2.2 ⫾ 1.0 0/20 0.5 ⫾ 0.8 2.73 ⫾ 0.82§ 0.28 ⫾ 0.19† 3.00 ⫾ 0.80¶ 2.30 ⫾ 0.62† 75 ⫾ 6§ 0.73 ⫾ 0.27¶ 11.8 ⫾ 3.0¶ 0.68 ⫾ 0.13 17.6 ⫾ 5.8 58 ⫾ 28† 8.2 ⫾ 5.9† 7.6 ⫾ 2.7† 0/20 0 12/8 2.7 ⫾ 1.1 *Values are given as the mean ⫾ SD, unless otherwise indicated. P0.1/(VT/tI) ⫽ pulmonary impedance. V˙e ⫽ minute ventilation; NFL ⫽ negative flow limitation. †p ⬍ 0.001 (sitting vs supine position; paired t test). ‡p ⬍ 0.05 (CHF patients vs control subjects; unpaired t test). §p ⬍ 0.005 (sitting vs supine position; paired t test). 㛳p ⬍ 0.005 (CHF patients vs control subjects; unpaired t test). ¶p ⬍ 0.05 (sitting vs supine position; paired t test). Borg score ⫽ 2.61 ⫹ 0.033 sPAP (r ⫽ ⫺0.48; p ⬍ 0.003), inspiratory time/total breath cycle time ratio (r ⫽ ⫺0.50; p ⬍ 0.024), and supine ERV (r ⫽ ⫺0.461; p ⬍ 0.04). Stepwise multivariate regression analysis selected all of the above parameters as significant independent contributors to Borg score, reflecting its multifactorial nature. However, the best predictors were supine Pimax (cm H2O), sPAP (mm Hg), and ⌬IC, as follows: where r ⫽ 0.80, r2 ⫽ 0.64, and p ⬍ 0.001. In FL patients, the supine Borg score was correlated with the ⌬IC (r ⫽ ⫺0.67; p ⬍ 0.017), whereas in non-FL patients this was not the case. Figure 2. Relationship between supine Borg score and ⌬IC from the seated to the supine position. Figure 3. Relationship between supine Borg score and sPAP. www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 (1) ⫺ 0.019 Pimax ⫺ 0.042 ⌬IC CHEST / 130 / 2 / AUGUST, 2006 475 Discussion The new findings of this study are as follows: (1) in CHF patients, tidal FL is absent while sitting but is common while in the supine position; (2) the patients who experienced FL in the supine position were significantly older than those who did not; (3) in the supine position, almost all patients (18 of 20 patients) exhibited orthopnea, the nature of which appears to be multifactorial; but its best predictors, selected by multiple regression analysis, were sPAP, supine Pimax, and ⌬IC from the seated to the supine position. Sitting In line with most previous reports,3,15,16 our CHF patients exhibited a reduction of total lung capacity, FRC, and RV but had a normal FEV1/FVC ratio. The FRC reduction was correlated with cardiomegaly, since there was a significant correlation of left end-diastolic volume to FRC (Fig 1). This finding could partially explain the difference between our data and those of Yap et al17 and Hart et al,18 who found no reduction of FRC in their CHF patients. Eight of 10 patients in the study by Yap et al17 and 5 of 10 patients in the study by Hart et al18 had CHF due to coronary artery disease or hypertension, whereas most of our patients had idiopathic cardiomyopathy. As previously reported,3,16,19 –21 Pimax was also reduced. The nature of the inspiratory muscle weakness is multifactorial, including the reduction of respiratory muscle blood flow, hypoxia, oxidative stress, disuse, medication, systemic inflammation, and nutritional depletion. The enlarged chest wall due to cardiomegaly and increased intrathoracic blood volume should also contribute to reduced Pimax because the pressure generated from inspiratory muscles (Pimus) should decrease due to length tension and geometric factors.22 This uncoupling of the lung and chest wall with a concurrent decrease in the relaxation volume (Vr) of the respiratory system, as reflected by the decreased FRC, should also decrease the Pimax measured at RV because of the decreased contribution of the relaxation pressure (Prs) of the respiratory system to Pimax. In fact, as in the following equation: Pimax ⫽ Pimus ⫺ Prs (2) it follows that at RV Pimax decreases as a result of both decreased Pimus and Prs. Altered diaphragmatic position can also modify its length-tension relationships and contribute to reduced Pimax.23 Ventilation and Neuromuscular Inspiratory Drive: Resting ventilation in CHF patients was high relative 476 Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 to control subjects, resulting in reduced mean Paco2 (4.9 ⫾ 0.4 mm Hg vs 5.2 ⫾ 0.3 mm Hg, respectively; p ⬍ 0.03). In patients with reduced Pimax, P0.1 underestimates the inspiratory neural drive. Accordingly, the P0.1/Pimax ratio is used instead as an index of neuromuscular inspiratory drive normalized for muscle strength. In agreement with most previous studies,3,16,19,20 but not all,21 we found an increase in P0.1/Pimax ratio in CHF patients relative to control subjects (5.3 ⫾ 4.2 vs 2.5 ⫾ 0.9, respectively; p ⬍ 0.01). Bruschi et al24 found increased P0.1/Pimax ratio in CHF patients who are at risk for nocturnal Cheynes-Stokes respiration and showed that this parameter, together with respiratory frequency, is a useful predictor of Cheynes-Stokes respiration. Reduced levels of Paco2 and increased pH were previously found in patients with high pulmonary capillary wedge pressure (PCWP) because the stimulation of pulmonary receptors, as a result of raised PCWP, heightens the central neural drive.25 However, we found no significant correlation of sPAP to P0.1 or P0.1/Pimax ratio. This may be due to the fact that most of our patients had elevated levels of sPAP, which may mask any correlation between sPAP and other variables. Recently, Meyer et al26 found respiratory muscle weakness in patients with idiopathic pulmonary hypertension and found P0.1 to be significantly higher than in those patients than in control subjects. In their patients, the P0.1/Pimax ratio showed significant correlation with the total ventilation-carbon dioxide slope during exercise. This observation confirms that increased ventilation and increased respiratory drive are hallmarks of heart failure. Hyperventilation during exercise, whether or not it was associated with periodic breathing, is now considered to be an independent risk factor for mortality and morbidity in CHF patients.27 Supine Tidal Flow Limitation: In the study by Duguet et al,1 9 of 12 patients with acute left ventricular failure exhibited tidal expiratory FL when in the supine position, and all of these 9 patients claimed to have orthopnea. By contrast, only one of the three subjects who denied having orthopnea exhibited tidal FL while in the supine position. Recently, Boni et al2 showed that in patients with both AHF and CHF supine FL is relatively common and that it can be reversed by therapy with diuretics. Age is a major factor promoting FL, because with increasing age the maximal expiratory flows at low lung volume decrease progressively due to gas trapping.28 De Bischopp et al29 recently studied apparently healthy subjects aged from 66 to 88 years and found that Original Research ⬎ 30% had FL even in the seated position. The patients studied by Duguet et al1 and Boni et al2 were quite old (mean age, 78 ⫾ 15 years and 77 ⫹ 7 years, respectively). A reduction in expiratory flow reserve plays a pivotal role in determining tidal flow limitation. Similarly, a reduction of the ERV plays an important role. In fact, when a subject breathes tidally at low volumes (ie, with a low ERV), the tidal volume changes occur over a portion of the maximal flowvolume curve with low maximal flows. Since the ERV is normally reduced while in the supine position,22 the prevalence of tidal FL in the supine position is generally higher than that in the sitting position.1,2 Orthopnea: Tidal FL in the supine position is associated with orthopnea in COPD patients,7 obese patients,30 and goiter patients.31 Almost all of our CHF patients (18 of 20 patients) claimed to have orthopnea,7 the critical trigger for which is commonly attributed to increased pulmonary venous return while in the supine position. This is supported by the significant correlation between PCWP and orthopnea.32 We found a significant correlation between supine Borg score and sPAP (r ⫽ 0.53; p ⬍ 0.02) [Fig 3]. Furthermore, the two CHF patients who denied orthopnea were younger (48 and 57 years) and had relatively low values of sPAP (25 mm Hg and 35 mm Hg). The several following mechanisms25,33,34 have been suggested to link the increase in central blood volume in CHF patients to orthopnea: (1) stimulation of the juxtacapillary receptors and increased vagal afferentation due to congestion and edema; (2) increased inspiratory loading; and (3) impaired Pimax. Increased vagal afferentation may lead to hyperventilation and cause breathlessness. Minute ventilation was higher than that in control subjects, both in the sitting and supine position, and the P0.1/Pimax ratio increased significantly in the supine position in both CHF patients and control subjects (p ⬍ 0.001), but in CHF patients the mean increase was much more pronounced (62 ⫾ 50% vs 44 ⫾ 28%, respectively). The postural increase in respiratory impedance (45 ⫾ 33% vs 20 ⫾ 35%, respectively; p ⬍ 0.03) was also higher in CHF patients. This implies increased inspiratory loading and could be due in part to the increased Raw and respiratory system elastance caused by the reduction in FRC. In our 12 patients who had FL while in the supine position, the FEV1/FVC ratio (p ⬍ 0.001), forced expiratory flow when 75% of FVC has been exhaled (FEF75) [p ⬍ 0.05], and Pimax (p ⬍ 0.001) decreased significantly when shifting from the sitting to www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 the supine position, while such changes were not significant in the 8 non-FL patients. The increase in mean Borg score with posture was higher in these subjects with respect to non-FL patients (from 0.5 ⫾ 0.7 to 3.0 ⫾ 1.4 vs 0.5 ⫾ 0.8 to 2.1 ⫾ 1.5, respectively), and the supine Borg score was negatively correlated with the ⌬IC, as previously described.2 In our study, ⌬IC also correlated with left ventricular telediastolic volume (r ⫽ ⫺0.457; p ⬍ 0.05). In adopting the supine position, there is normally little or no change in vital capacity, while ERV is substantially reduced with a concurrent increase of IC.22 The latter is caused by a reduction of Vr due to gravity.22 In our CHF patients, the supine ERV was very small (ie, close to RV), probably due to cardiomegaly and increased intrathoracic liquid volume.31 In our patients, the supine Borg score correlated with supine ERV (r ⫽ ⫺0.46; p ⬍ 0.04). Such an association is also found in patients with morbid obesity,30 and it has been suggested that, in these patients, the supine Vr is located below RV. This implies the presence of PEEPi at RV. This phenomenon was probably also present in our FL subjects and may explain the paradoxical reduction of Pimax observed in these patients (see below). Tidal FL seems to be a factor contributing to orthopnea in CHF patients, but the finding that supine Borg score correlated also with sPAP and supine Pimax suggest a multifactorial origin for this symptom. In a previous work,3 sPAP was correlated to P(A-a)O2 and to the closing volume/vital capacity ratio. In most of the patients (13 of 20 patients), CC exceeded FRC (ie, during tidal breathing there was a cyclic opening and closing of peripheral airways with a concurrent maldistribution of ventilation, with decreased Pao2 and increased P[A-a]O2). Supine positioning that reduces FRC could enhance this phenomenon, contributing to the worsening of orthopnea. Inspiratory Load and Muscular Force: The overall increase in inspiratory load is reflected by the significant mean increase in effective inspiratory impedance with change in posture in CHF patients compared to that in control subjects (7.6 ⫾ 2.7 vs 6.2 ⫾ 1.7, respectively; p ⫽ 0.05) indicating that P0.1 was sufficient not only to overcome the increased breathing load but also to induce hyperventilation. The decrease in Pimax in the supine position contributed to the disproportionate increase in P0.1/ Pimax ratio, reflecting increased effort in the face of weakened muscles with a concurrent increase in Borg score (Table 2). In fact, Pimax in the supine position together with sPAP and ⌬IC were the most significant independent contributors to Borg score CHEST / 130 / 2 / AUGUST, 2006 477 (equation 1). In FL patients, the decreases in Pimax and the increases in Borg score with change in posture were greater than in non-FL subjects. In stable CHF patients, Nava et al35 found a strong correlation between orthopnea and increased diaphragmatic effort in the supine position. The reduction of diaphragmatic effort through assisted noninvasive ventilation correlated significantly with the reduction in orthopnea. Tidal FL was not assessed, but dynamic PEEPi was increased in the supine position with a concurrent increase in resistance and transdiaphragmatic pressure. The effect of posture on Pimax in healthy subjects is controversial. In two previous studies,22,36 no differences between Pimax measured in the upright and supine position were found, while in another study37 Pimax was significantly lower in the supine position. There is no study comparing Pimax in the upright and supine positions in CHF patients. We found a slight reduction in Pimax in control subjects and in CHF patients. The percentage change in posture was similar in the two groups. The reduction in mean Pimax was significantly higher in the 12 FL subjects compare to non-FL subjects (⫺24 ⫹ 16 vs ⫺6 ⫹ 18%, respectively). This was probably due to the fact that in the supine patient Vr was below RV, and hence PEEPi was present at RV. Since PEEPi corresponds to positive Prs (equation 2), Pimax should be less than Pimus in the supine position. In contrast, Prs is normally negative at RV, and hence Pimax is higher than Pimus. It should be noted that altered diaphragmatic position23 and chest wall geometry22 may also contribute to changes in Pimax with posture. In conclusion, the present data show that, as a result of a marked decrease in ERV in the supine position, most CHF patients also exhibit tidal FL when supine with concurrent inspiratory threshold loading. This, together with increased respiratory resistance and elastance, and decreased inspiratory muscle force, elicits orthopnea. References 1 Duguet A, Tantucci C, Lozinguez O, et al. Expiratory flow limitation as a determinant of orthopnea in acute left heart failure. J Am Coll Cardiol 2000; 35:690 –700 2 Boni E, Bezzi M, Carminati M, et al. Expiratory flow limitation is associated with orthopnea and reversed by vasodilators and diuretics in left heart failure. Chest 2005; 128:1050 –1057 3 Torchio R, Gulotta C, Greco-Lucchina P, et al. Closing capacity and gas exchange in chronic heart failure. Chest 129; 5:1330 –1336 4 Weber KT, Kinasewitz GT, Janicki JS. Oxygen utilization and ventilation during exercise in patients with chronic cardiac failure. Circulation 1982; 65:1213–1223 5 Bestall JC, Paul EA, Garrod R, et al. Usefulness of the medical research council (MRC) dyspnea scale as a measure 478 Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 of disability in patients with chronic obstructive lung disease. Thorax 1999; 54:581–586 Borg G. Psychophysical basis of perceived exertion. Med Sci Sports Exerc 1982; 14:377–381 Eltayara L, Ghezzo H, Milic-Emili J. Orthopnea and tidal expiratory flow limitation in patients with stable COPD. Chest 2001; 119:99 –104 Quanjer PhH, Tammeling JE, Cotes OF, et al. Lung volumes and forced ventilatory flows: Report Working Party Standardization of Lung Function Tests; European Coal and Steel Community. Eur Respir J 1993; 16:5– 40 Peslin R. Resistance. In: Milic-Emili J, Lucangelo U, Pesenti A, et al, eds. Basics of respiratory mechanics and artificial ventilation. Milano, Italy: Springer-Verlag, 1999; 37–57 Whitelaw WA, Derenne JP, Milic-Emili J. Occlusion pressure as a measure of respiratory center output in conscious man. Respir Physiol 1975; 23:181–199 American Thoracic Society/European Respiratory Society. ATS/ERS statement on respiratory muscle testing. Am J Respir Crit Care Med 2002; 166:518 – 624 Black LF, Hyatt RE. Maximal respiratory pressures: normal values and relationship to age and sex. Am Rev Respir Dis 1969; 99:696 –702 Koulouris NG, Valta P, Lavoie A, et al. A simple method to detect expiratory flow limitation during spontaneous breathing. Eur Respir J 1995; 8:306 –313 Hussain SNA, Pardy RL, Dempsey JA. Mechanical impedance as determinant of inspiratory neural drive during exercise in humans. J Appl Physiol 1985; 59:365–375 Collins JV, Clark TJK, Brown J. Airway function in healthy subjects and patients with left heart disease. Clin Sci Mol Med 1975; 49:217–228 Ambrosino, Opasich C, Crotti P, et al. Breathing pattern, ventilatory drive and respiratory muscle strength in patients with chronic heart failure. Eur Respir J 1994; 7:17–22 Yap JCH, Moore DM, Cleland JGF, et al. Effect of supine posture on respiratory mechanics in chronic left ventricular failure. Am J Respir Crit Care Med 2000; 162:1285–1291 Hart N, Kearney MT, Pride NB, et al. Inspiratory muscle load and capacity in chronic heart failure. Thorax 2004; 59:477– 482 Meyer FJ, Borst MM, Zugck C, et al. Respiratory muscle dysfunction in congestive heart failure: clinical correlation and prognostic significance. Circulation 2001; 103:2153–2158 McParland C, Krishnan B, Wang Y, et al. Inspiratory muscle weakness and dyspnoea in chronic heart failure. Am Rev Respir Dis 1992; 148:467– 472 Witt C, Borges AC, Haake H, et al. Respiratory muscle weakness and normal ventilatory drive in dilatative cardiomyopathy. Eur Heart J 1997; 18:1322–1328 Agostoni E, Hyatt RE. Static behavior of the respiratory system. In: Handbook of physiology: the respiratory system; mechanics of breathing. Bethesda MD: American Physiological Society, 1986; 113–130 Caruana L, Petrie MC, McMurray JJ, et al. Altered diaphragm position and function in patients with chronic heart failure. Eur J Heart Fail 2000; 3:183–187 Bruschi C, Fanfulla F, Traversi E, et al. Identification of chronic heart failure patients at risk of Cheyne-Stokes respiration. Monaldi Arch Chest Dis 1999; 54:319 –324 Lorenzi-Filho G, Azevedo ER, Parker JD, et al. Relationship of carbon dioxide tension in arterial blood to pulmonary wedge pressure in heart failure. Eur Respir J 2002; 19:37– 40 Meyer FJ, Lossnitzer D, Kristen AV, et al. Respiratory muscle dysfunction in idiopathic pulmonary arterial hypertension. Eur Respir J 2005; 25:125–130 Original Research 27 Bradley TD, Floras JS. Sleep apnea and heart failure: part II. Central sleep apnea. Circulation 2003; 107:1822–1826 28 Knudson RJ. Physiology of the aging lung. In: Crystal RG, West JB, Weibel FR, et al, eds. The lung: scientific foundations. New York, NY: Raven Press Ltd, 1991; 1749 29 De Bisschop C, Marty ML, Tessier JF, et al. Expiratory flow limitation and obstruction in the elderly. Eur Respir J 2005; 26:594 – 601 30 Ferretti A, Giampiccolo P, Cavalli A, et al. Expiratory flow limitation and orthopnea in massively obese subjects. Chest 2001; 119:1401–1408 31 Torchio R, Gulotta C, Perboni A, et al. Orthopnea and tidal expiratory flow limitation in patients with euthyroid goiter. Chest 2003; 124:133–140 32 Mancini DM, La Manca J, Donchez L, et al. The sensation of dyspnea during exercise is not determined by the work of www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 10/28/2014 33 34 35 36 37 breathing in patients with heart failure. J Am Coll Cardiol 1996; 28:391–395 Paintal A. Mechanism of stimulation of type J pulmonary receptors. J Physiol 1969; 203:511–532 Bradley TD, Holloway RM, McLaughlin PR, et al. Cardiac output response to continuous positive airway pressure in congestive heart failure. Am Rev Respir Dis 1992; 145:377–382 Nava S, Larovere MT, Fanfulla F, et al. Orthopnea and inspiratory effort in chronic heart failure patients. Respir Med 2003; 97:647– 653 Yap YCH, Watson RA, Gilbey S, et al. Effects of posture on respiratory mechanics in obesity. J Appl Physiol 1995; 79: 1199 –1205 Koulouris N, Mulvey DA, Laroche CM, et al. The effect of posture and abdominal binding on respiratory pressures. Eur Respir J 1989; 2:961–965 CHEST / 130 / 2 / AUGUST, 2006 479
© Copyright 2026