CHEST Original Research
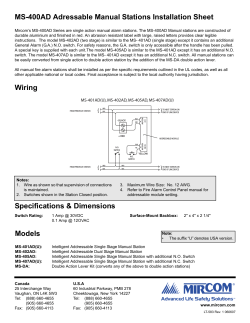
CHEST Original Research INTERVENTIONAL PULMONOLOGY Real-time Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration in Mediastinal Staging of Non-Small Cell Lung Cancer* How Many Aspirations Per Target Lymph Node Station? Hee Seok Lee, MD†; Geon Kook Lee, MD, PhD†; Hyun-Sung Lee, MD, PhD; Moon Soo Kim, MD; Jong Mog Lee, MD; Hyae Young Kim, MD, PhD; Byung-Ho Nam, PhD; Jae Ill Zo, MD, PhD; and Bin Hwangbo, MD Objective: The goal of this study was to determine the optimal number of aspirations per lymph node (LN) station during endobronchial ultrasound (EBUS)-guided transbronchial needle aspiration (TBNA) for maximum diagnostic yield in mediastinal staging of non-small cell lung cancer (NSCLC) in the absence of rapid on-site cytopathologic examination. Methods: EBUS-TBNA was performed in potentially operable NSCLC patients with mediastinal LNs accessible by EBUS-TBNA (5 to 20 mm). Every target LN station was punctured four times. Results: We performed EBUS-TBNA in 163 mediastinal LN stations in 102 NSCLC patients. EBUS-TBNA confirmed malignancy in 41 LN stations in 30 patients. Two malignant LN stations were missed in two patients. The sensitivity, specificity, positive predictive value, negative predictive value (NPV), and accuracy of EBUS-TBNA in predicting mediastinal metastasis were 93.8%, 100%, 100%, 96.9%, and 97.9%, respectively. Sample adequacy was 90.1% for one aspiration, and it reached 100% for three aspirations. The sensitivity for differentiating malignant from benign LN stations was 69.8%, 83.7%, 95.3%, and 95.3% for one, two, three, and four aspirations, respectively. The NPV was 86.5%, 92.2%, 97.6%, and 97.6% for one, two, three, and four aspirations, respectively. Maximum diagnostic values were achieved in three aspirations. When at least one tissue core was obtained by the first or second aspiration, the sensitivity and NPV of the first two aspirations were 91.9% and 96.0%, respectively. Conclusions: Optimal results can be obtained in three aspirations per LN station in EBUS-TBNA for mediastinal staging of potentially operable NSCLC. When at least one tissue core specimen is obtained by the first or second aspiration, two aspirations per LN station can be acceptable. (CHEST 2008; 134:368 –374) Key words: endobronchial ultrasound; lung cancer; staging Abbreviations: EBUS ⫽ endobronchial ultrasound; LN ⫽ lymph node; NPV ⫽ negative predictive value; NSCLC ⫽ nonsmall cell lung cancer; PET ⫽ positron emission tomography; PPV ⫽ positive predictive value; ROSE ⫽ rapid on-site cytopathologic examination; TBNA ⫽ transbronchial needle aspiration ndobronchial ultrasound (EBUS)-guided transE bronchial needle aspiration (TBNA) is a new bronchoscopic method that enables real-time aspiration of peribronchial or peritracheal lesions. Evidence of the usefulness of EBUS-TBNA in the diagnosis of mediastinal lymph nodes (LNs) is increasing.1–9 EBUS-TBNA has a high sensitivity and a 368 Downloaded From: http://journal.publications.chestnet.org/ on 11/24/2014 high negative predictive value (NPV) in the mediastinal staging of lung cancer.3,8 EBUS-TBNA is a recently introduced technique. Details of EBUS-TBNA methodology, such as the number of aspirations per target needed and the need for on-site cytopathologic support, have not been determined. According to Japanese reports2,3,8 Original Research about EBUS-TBNA, aspirates were evaluated by an on-site cytopathologist, and the median number of needle passes was two for each site. In some studies1,4,5 not using rapid on-site cytopathologic examination (ROSE), one to three aspirates were obtained from the target lesion; judgment concerning the number of aspirates required was made according to the macroscopic appearance of the aspirate or arbitrarily by a bronchoscopist. In other studies6,7 not using ROSE, two needle passes were made at every site. Some authors10 suggest that three to four needle passes are associated with 90% sensitivity. The goal of this study was to determine the optimal number of aspirations per LN station required during EBUS-TBNA for maximum diagnostic yield in the mediastinal staging of non-small cell lung cancer (NSCLC) when ROSE is not available. Materials and Methods Patients This study was conducted between July 2006 and April 2007 at the Center for Lung Cancer, National Cancer Center, South Korea. Patients with strongly suspected or histologically confirmed potentially operable NSCLC were enrolled. To be included in the study, patients were required to have a mediastinal LN accessible by EBUS-TBNA with a short diameter of 5 to 20 mm on axial chest CT. LN status was classified according to the international staging system reported by Mountain and Dressler.11 Tumor resectability was evaluated after an imagebased staging workup for NSCLC, including CT of the chest and upper abdomen, brain MRI, whole-body positron emission tomography (PET)-CT, and/or bone scan. We excluded patients with M1 disease, inoperable T4 disease, evident N3 disease with spread to supraclavicular LNs, bulky mediastinal LN (short diameter ⬎ 2 cm on axial image of chest CT), or extranodal invasion of the mediastinal LN visible on chest CT. Patients with unresectable tumors diagnosed by white light bronchoscopy or patients with a Pancoast tumor were also excluded. Medical operability was assessed, and patients who were not physically suitable for surgery were excluded. The ethical committee of our institute approved this study. Informed consent was obtained from all patients included in this study. *From the Center for Lung Cancer (Drs. H. S. Lee, G. K. Lee, H-S Lee, M. S. Kim, J. M. Lee, H. Y. Kim, Zo, and Hwangbo), Research Institute and Hospital; and Cancer Biostatistics Branch (Dr. Nam), Research Institute for National Cancer Control and Evaluation, National Cancer Center, Gyeonggi, Korea. †These authors contributed equally to this work. This work was supported by the National Cancer Center grant 710620. The authors have no conflicts of interest to disclose. Manuscript received August 20, 2007; revision accepted January 12, 2008. Reproduction of this article is prohibited without written permission from the American College of Chest Physicians (www.chestjournal. org/misc/reprints.shtml). Correspondence to: Bin Hwangbo, MD, Center for Lung Cancer, National Cancer Center, 809 Madu-dong, Ilsan-gu, Goyang, Gyeonggi, 411–764, Korea; e-mail: [email protected] DOI: 10.1378/chest.07-2105 www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 11/24/2014 EBUS-TBNA EBUS-TBNA was performed with a flexible ultrasonic puncture bronchoscope with a linear scanning transducer (CP-EBUS, XBF-UC260F-OL8; Olympus; Tokyo, Japan). All EBUS-TBNA procedures were performed by the same bronchoscopist (B.H.). Local anesthesia (lidocaine) was applied. The procedure was performed under conscious sedation (midazolam). After full inspection of the mediastinal LNs accessible by EBUS-TBNA, target nodal stations considered to be necessary in mediastinal staging were selected by the judgment of a bronchoscopist. In selecting, we considered the likelihood of metastasis of the target nodal stations based on imaging studies and the potential pathway of lymphatic metastasis. We also considered the impact of metastasis of the target nodal station in deciding on treatment. Each target nodal station was aspirated four times with a dedicated 22-gauge needle (NA-201SX-4022; Olympus). We tried to target different areas of each nodal station for each aspiration to cover large parts of a nodal station (Fig 1). Different needles were used for different nodal stations to avoid contamination. N3 nodes were sampled first, and then N2 nodes were punctured. Procedure time was calculated from the insertion of the bronchoscope through mouth to the retrieval of the bronchoscope after the procedure. The aspirate was expelled onto glass slides, smeared, and immediately fixed with 95% alcohol. We made three pairs of smear slides for each aspiration, if possible. Tissue cores (the solid substances in the aspiration needle obtained by EBUS-TBNA) were put into a solution of 10% neutral-buffered formalin. All specimens were numbered with respect to the order of aspiration. The remnants of each aspirate from the same nodal station were collected in one bottle filled with 95% alcohol for cell block. Smeared cytology slides were stained with hematoxylin-eosin and Papanicolaou. Tissue cores and cell blocks were stained with hematoxylin-eosin. Cytopathologic specimens were categorized as positive (presence of tumor cells), negative (lymphocytes or lymphoid tissue only), or inadequate (no cellular component, blood only, or cartilage or bronchial epithelial cells only). A pathologist (G.K. Lee), blinded to the details of the patients performed the cytopathologic examinations. Treatment Based on the EBUS-TBNA results, we recommended surgery for patients without mediastinal metastasis (open thoracotomy or video-assisted thoracic surgery including systematic LN dissection). Mediastinoscopy was not performed. We recommended chemotherapy (with or without radiotherapy) for patients with mediastinal metastasis with curative or neoadjuvant intent. Statistical Analysis The sensitivity, specificity, positive predictive value (PPV), NPV, and diagnostic accuracy of EBUS-TBNA were determined. The diagnostic consistency according to the number of aspirations was analyzed using the McNemar test. Differences in diagnostic values with respect to the presence of tissue core samples were examined with 2 or Fisher exact test; p values ⬍ 0.05 were considered statistically significant. All statistical analyses were performed using statistical software (STATA9, Stata Statistical Software Release 9; StataCorp; College Station, TX). Results Characteristics of Patients and LNs We enrolled 105 patients in the study (Fig 2). Small cell lung cancer was diagnosed in three paCHEST / 134 / 2 / AUGUST, 2008 369 Figure 1. Each LN station was aspirated four times. A representative 4R LN station is shown. SVC ⫽ superior vena cava. tients. We evaluated 102 NSCLC patients (Table 1). In 102 patients, we encountered 234 mediastinal nodal stations accessible by EBUS-TBNA that contained at least one LN ⱖ 5 mm on axial chest CT. We obtained cytopathologic samples from 163 nodal stations according to the judgment of a bronchoscopist. We successfully aspirated each of the 162 nodal stations four times. In a 74-year-old man with COPD (FEV1, 1.29 L; 61% of expected), EBUS-TBNA was stopped after two aspirations of the 4R station due to hypoxemia during the procedure. He recovered from hypoxemia after EBUS-TBNA. Otherwise, there were no procedure-related complications. Diagnostic Values of EBUS-TBNA for the Diagnosis of Mediastinal Metastasis Among the 102 NSCLC patients studied, mediastinal metastasis was confirmed by EBUS-TBNA in 41 nodal stations in 30 patients (N2, n ⫽ 25; N3, n ⫽ 5). A positive EBUS-TBNA result was considered a true positive because the chance of contamination is rare.8 Seventy-two patients were found to have benign mediastinal LNs based on EBUSTBNA. Five patients chose not to have surgery in our hospital. Moreover, we found unexpected pleural EBUS-TBNA N=105 NSCLC N=102 (163 LNS*) SC L C N=3 N2/N3 negative N=72 N2/N3 positive N=30 (41LNS) Refused surgery N=5 Surgery N=67 N2 positive N= 2 (2LNS) N2/N3 negative N=63 No LN dissection# N=2 Figure 2. The clinical course of 105 patients who enrolled in this study. *Mediastinal LN stations (LNS). #Due to pleural metastasis. SCLC ⫽ small cell lung cancer. 370 Downloaded From: http://journal.publications.chestnet.org/ on 11/24/2014 metastasis in two patients; thus, LN dissection was not performed for those patients. Of 65 patients who underwent surgery and mediastinal LN dissection (open thoracotomy, n ⫽ 43; VATS, n ⫽ 22), we surgically confirmed two metastatic N2 nodal stations that were benign by EBUS-TBNA in 2 patients (Fig 2). One patient had a 5-mm metastasis in the subcarinal station of which the long axis was 39 mm on coronal chest CT. The other patient had two metastatic foci (7 mm and 6 mm) in the subcarinal station; the long axis of the nodal station was 51 Table 1—Characteristics of Patients and LNs* Characteristics Data Patients, No. Male/female gender, No. Median age (range), yr Histologic type of lung cancer Adenocarcinoma Squamous cell carcinoma Large cell carcinoma Sarcomatoid carcinoma Adenocarcinoma/squamous cell carcinoma, double primary LN stations per patient† One LN station Two LN stations Three LN stations Location of LN station 2R 2L 4R 4L 7 Median LN size on CT image (range), mm‡ Short axis Long axis Mean time of EBUS-TBNA (range), min§ One LN station Two LN stations Three LN stations 102 82/20 64.3 (35.0–81.1) 46 (45.1) 45 (44.1) 9 (8.8) 1 (1.0) 1 (1.0) 49 (48.0) 45 (44.2) 8 (7.8) 163 7 (4.3) 1 (0.6) 59 (36.2) 31 (19.0) 65 (39.9) 8.6 (5.1–19.3) 15.2 (7.2–39.9) 33.4 (12–70) 21.6 (12–50) 41.2 (27–70) 60.3 (53–70) *Data are presented as No. (%) unless otherwise indicated. †Data are presented as No. of patients (%). ‡Size of biggest LN in each LN station. §One patient who underwent two aspirations for the 4R station was excluded in this calculation. Original Research Cytologic samples Tissue-core samples Overall 52 (8.0%) 99 (15.2%) 158 (24.3%) 117 (18.0%) 434 (66.8%) No sample 130 (20.0%) 468 (72.0%) 359 (55.2%) 31(4.8%) 102 (15.7%) Inadequate Positive Negative Figure 3. Cytopathologic results of 650 aspirates from 163 mediastinal LN stations. mm on coronal chest CT. Among LN stations not sampled by EBUS-TBNA, LN dissection did not reveal any metastatic nodes. Considering surgicalpathologic staging as the “gold standard,” the sensitivity, specificity, PPV, NPV, and accuracy of EBUSTBNA in the prediction of mediastinal LN metastasis were 93.8% (30 of 32 patients), 100% (63 of 63 patients), 100% (30 of 30 patients), 96.9% (63 of 65 patients), and 97.9% (93 of 95 patients), respectively. stations, cell block specimens were obtained from 13 stations. Eight specimens contained malignant cells. Cell blocks from the two LN stations for which diagnosis of malignancy was missed were inadequate or negative. Diagnostic Values of EBUS-TBNA According to the Number of Aspiration The cumulative sensitivity, specificity, PPV, NPV, and diagnostic accuracy of EBUS-TBNA according to the number of aspirations used are presented in Table 2. Diagnostic values were calculated based on 126 LN stations from 91 patients. We excluded one benign nodal station that was not aspirated four times and 36 benign nodal stations that were not surgically dissected (in 9 LN stations due to refusing surgery in our hospital; in 3 LN stations due to pleural metastasis found by thorocotomy; in 8 LN stations due to confirmed N2 or N3 disease by EBUS-TBNA; and in 16 LN stations due to contralateral locations of the LN stations by the surgical site). The sensitivity for differentiating malignant and benign nodal station increased to 95.3% when three aspirations were performed. NPV increased to 97.6% when three aspirations were performed. Likewise, the cumulative diagnostic accuracy increased to 98.4% with three aspirations. The fourth aspiration did not confer an additional diagnostic yield. There was a significant difference in the EBUS-TBNA Characteristics of Aspirates by EBUS-TBNA We obtained 650 aspirates from 163 mediastinal nodal stations (Fig 3). On average, 5.9 smear slides (range, 3 to 6 smear slides) were made for each aspiration. We obtained tissue cores in 75.7% of aspirates. However, 6.3% (n ⫽ 31) of tissue core samples were inadequate for evaluation (cartilage only, n ⫽ 4; blood clot only, n ⫽ 27). Considering the cytologic and histologic results combined, 92.0% of aspirates were adequate for evaluation. We evaluated cumulative sample adequacy in 101 patients (162 LN stations) who had four successful aspirations per site. Sample adequacy was 90.1% (146 of 162 LN stations) for one aspiration, 98.1% (159 of 162 LN stations) for two aspirations, and reached 100% (162 of 162 LN stations) in three aspirations. We could make only 55 cell block specimens (33.7% of 163 LN stations) due to the poor cellularity of the collected remnants. Of 43 malignant nodal Table 2—Cumulative Diagnostic Values of EBUS-TBNA Shown by the Number of Aspirations* Aspirations, No. Variables 1 2 3 4 Sensitivity Specificity PPV NPV Accuracy 69.8 (30/43) 100 (83/83) 100 (30/30) 86.5 (83/96) 89.7 (113/126) 83.7 (36/43) 100 (83/83) 100 (36/36) 92.2 (83/90) 94.4 (119/126) 95.3 (41/43) 100 (83/83) 100 (41/41) 97.6 (83/85) 98.4 (124/126) 95.3 (41/43) 100 (83/83) 100 (41/41) 97.6 (83/85) 98.4 (124/126) *Data are presented as % (No./total). We considered inadequate samples as negative results. www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 11/24/2014 CHEST / 134 / 2 / AUGUST, 2008 371 Table 3—Diagnostic Values of EBUS-TBNA According to the Presence of a Tissue Core Sample and the Number of Aspirations* Aspirations, No. 1 2 3 4 Variables Tissue Core No Tissue Core Tissue Core No Tissue Core Tissue Core No Tissue Core Tissue Core No Tissue Core Sensitivity NPV Accuracy 75.9 (22/29) 89.9 (62/69) 92.3 (84/91) 57.1 (8/14) 77.8 (21/27) 82.9 (29/35) 91.9 (34/37) 96.0 (72/75) 97.2 (106/109) 33.3 (2/6) 73.3 (11/15) 76.5 (13/17) 95.1 (39/41) 97.5 (79/81) 98.3 (118/120) 100 (2/2) 100 (4/4) 100 (6/6) 95.2 (40/42) 97.6 (81/83) 98.4 (121/123) 100 (1/1) 100 (2/2) 100 (3/3) *Data are presented as % (No./total). We considered inadequate samples as negative results. diagnostic results after one vs two aspirations (p ⫽ 0.031, McNemar test). There was a borderline difference in diagnostic results after two vs three aspirations (p ⫽ 0.063, McNemar test). Analysis of Diagnostic Values According to the Presence of Tissue Core Sample Of 650 aspirates, aspirates with tissue cores were more likely to be adequate for evaluation than aspirates without tissue cores: 96.1% (473 of 492 aspirates) vs 78.5% (124 of 158 aspirates) [p ⬍ 0.001, 2 test]. We evaluated diagnostic values with respect to the presence of tissue core samples and the number of aspirations (Table 3). The 126 nodal stations mentioned above were analyzed. When at least one tissue core was obtained by the first or second aspiration, the sensitivity of the first two aspirations was significantly higher compared to the two aspirations without tissue core samples (91.9%, vs 33.3%, p ⫽ 0.004; Fisher exact test). Significant differences in NPV (96.0%, vs 73.3%, p ⫽ 0.014, Fisher exact test) and diagnostic accuracy (97.2%, vs 76.5%, p ⫽ 0.006, Fisher exact test) were also found to be dependent on the presence of the tissue core in the first or second aspiration. Discussion EBUS-TBNA has been reported to be an accurate and safe diagnostic method for the mediastinal staging of lung cancer.3,8 In this study, we performed EBUS-TBNA safely under local anesthesia, with only one COPD patient experiencing hypoxemia, which led us to discontinue the EBUS-TBNA procedure. Overall, our diagnostic accuracy was consistent with previous studies.3,8 In this study, maximal diagnostic values of EBUSTBNA were obtained in three aspirations. Sample adequacy reached 100% in three aspirations. We missed two metastatic mediastinal LN stations that contained tumor cells in small parts of the node 372 Downloaded From: http://journal.publications.chestnet.org/ on 11/24/2014 station, even though we aspirated four times per site. Practically, it is not easy to aspirate more than four times per site due to the duration of the procedure. In our study, median procedure time was 1 h when three nodal stations were punctured. Our results suggest that a fourth aspiration is not necessary in EBUS-TBNA for the mediastinal staging of NSCLC. The sensitivity of the first aspiration was 68.9%. The sensitivity increased to 83.7% after two aspirations and to 95.3% after three aspirations. This suggests that one needle pass per nodal station is insufficient for staging of NSCLC, while three aspirations is optimal. However, the macroscopic appearance of aspirates may influence the decision to perform further aspirations. Aspirates that contained a tissue core were more likely to be adequate in this study compared to aspirates lacking tissue core. Even though 6.3% of tissue core samples that we obtained were inadequate for evaluation, the sensitivity (91.7%), NPV (96.0%), and accuracy (97.2%) were high when a tissue core sample was obtained in the first two aspirations. These data suggest that two aspirations per LN station can be acceptable when at least one tissue core specimen is obtained by the first two aspirations. As well as the macroscopic appearance of aspirated samples, the adequacy of targeting can also affect the number of aspirations performed during EBUS-TBNA. If a bronchoscopist thinks that the targeting is inadequate or insufficient, an additional aspiration would be performed. It is common for an LN station to contain many LNs. Some nodes may be too large to be sufficiently sampled with only one or two aspirations. Therefore, bronchoscopists should select LNs or areas even in a single nodal station. The size of the LN, the appearance of the LN on chest CT, result of PET or PET-CT, sonographic features of the LN, and proximity of the LN to the tumor in the potential pathway of lymphatic metastasis would influence the decision of a bronchoscopist in the selection of LNs. Larger LNs are more likely to be malignant, but this is not always the Original Research case.12,13 PET is more accurate than CT in mediastinal staging14 and PET can guide invasive mediastinal staging.15,16 The common path of LN metastasis of lung cancer is known.17 Some echo features of LNs are associated with metastasis in endoscopic ultrasound18,19 and remain to be evaluated by EBUS. Depending on the subjective decision of a bronchoscopist considering the factors mentioned above, we performed EBUS-TBNA by first attempting to target the most promising area in each nodal station. However, the targeting was not always successful. Adequate targeting can reduce the number of aspirations needed. Targeting issues were not evaluated in this study. The number of aspirations needed in conventional TBNA has also been studied, and the maximum diagnostic yield was obtained in five to seven needle passes.20,21 Conventional TBNA is a technique that does not employ direct visualization. It is guided by endobronchial landmarks and a mental reconstruction of CT images. There are greater limitations in the size and location of accessible LNs that can be aspirated using TBNA vs EBUS-TBNA. In a metaanalysis,22 the pooled sensitivity of conventional TBNA in the mediastinal staging of NSCLC was reported to be 39 to 78%. The benefit of ROSE was evaluated in conventional TBNA.23–25 ROSE was cost-effective and improved diagnostic yield.23,24 ROSE also improved the diagnostic yield of in endoscopic ultrasound-guided fine needle aspiration.26 If ROSE were available in our institution, our cytologic results suggest that we could have stopped EBUS-TBNA in 68.3% of malignant nodal stations after the first aspiration and after the second aspiration in an additional 14.6% of stations. In one study8 using ROSE, the mean examination time of EBUS-TBNA was approximately 15 min. In our study, the mean procedure time was 33.4 min when we punctured four times per nodal station (average, 1.6 stations per patient). The procedure time would be shorter if two to three aspirations per site were performed. The benefits of ROSE with respect to procedure time, cost-effectiveness, and diagnostic yield remain to be studied in EBUS-TBNA. This study has several limitations. We selected the target LN stations considered to be necessary in mediastinal staging. Another limitation is that all negative LN stations by EBUS-TBNA were not surgically confirmed. We could not surgically confirm the negative LN stations sampled in patients with mediastinal metastasis proved by EBUS-TBNA. We also could not get surgical samples from 16 contralateral nodal stations from 15 surgical patients with surgical stage I or II disease because LN dissection of the contralateral side was considered not to be beneficial for those patients. The selection of LNs and the www.chestjournal.org Downloaded From: http://journal.publications.chestnet.org/ on 11/24/2014 limitations of surgical confirmation would have affected the diagnostic values, especially NPV. In our study, we collected the remnants of all aspirates from each nodal station for a cell block, rather than making a cell block for each aspiration. After three pairs of slides were made, the cellularity of the remnants was often scant. The cytologic results of cell blocks did not influence the overall diagnostic values of EBUS-TBNA. We think it is unlikely that collecting the remnants would influence the interpretation of our data. In conclusion, our results suggest that optimal diagnostic results of EBUS-TBNA can be obtained with three aspirations per LN station in the mediastinal staging of potentially operable NSCLC. When at least one tissue core specimen is obtained by the first or second aspiration, two aspirations per LN station can be acceptable. ACKNOWLEDGMENT: The authors thank Dr. K. Yasufuku and Dr. T. Fujisawa (Chiba University, Japan) for their instruction and advice concerning EBUS-TBNA. References 1 Krasnik M, Vilmann P, Larsen SS, et al. Preliminary experience with a new method of endoscopic transbronchial real time ultrasound guided biopsy for diagnosis of mediastinal and hilar lesions. Thorax 2003; 58:1083–1086 2 Yasufuku K, Chiyo M, Sekine Y, et al. Real-time endobronchial ultrasound-guided transbronchial needle aspiration of mediastinal and hilar lymph nodes. Chest 2004; 126:122–128 3 Yasufuku K, Chiyo M, Koh E, et al. Endobronchial ultrasound guided transbronchial needle aspiration for staging of lung cancer. Lung Cancer 2005; 50:347–354 4 Rintoul RC, Skwarski KM, Murchison JT, et al. Endobronchial and endoscopic ultrasound-guided real-time fine-needle aspiration for mediastinal staging. Eur Respir J 2005; 25:416 – 421 5 Vilmann P, Krasnik M, Larsen SS, et al. Transesophageal endoscopic ultrasound-guided fine-needle aspiration (EUSFNA) and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) biopsy: a combined approach in the evaluation of mediastinal lesions. Endoscopy 2005; 37:833– 839 6 Herth FJ, Ernst A, Eberhardt R, et al. Endobronchial ultrasound-guided transbronchial needle aspiration of lymph nodes in the radiologically normal mediastinum. Eur Respir J 2006; 28:910 –914 7 Herth FJ, Eberhardt R, Vilmann P, et al. Real-time endobronchial ultrasound guided transbronchial needle aspiration for sampling mediastinal lymph nodes. Thorax 2006; 61:795– 798 8 Yasufuku K, Nakajima T, Motoori K, et al. Comparison of endobronchial ultrasound, positron emission tomography, and CT for lymph node staging of lung cancer. Chest 2006; 130:710 –718 9 Wong M, Yasufuku K, Nakajima T, et al. Endobronchial ultrasound: new insight for the diagnosis of sarcoidosis. Eur Respir J 2007; 29:1182–1186 10 Lennon AM, Rintoul RC, Penman ID. Competition for eus (a) ebus-tbna (b) video assisted thoracoscopy. Endoscopy 2006; 38(suppl 1):S80 –S83 CHEST / 134 / 2 / AUGUST, 2008 373 11 Mountain CF, Dressler CM. Regional lymph node classification for lung cancer staging. Chest 1997; 111:1718 –1723 12 McLoud TC, Bourgouin PM, Greenberg RW, et al. Bronchogenic carcinoma: analysis of staging in the mediastinum with CT by correlative lymph node mapping and sampling. Radiology 1992; 182:319 –323 13 Prenzel KL, Monig SP, Sinning JM, et al. Lymph node size and metastatic infiltration in non-small cell lung cancer. Chest 2003; 123:463– 467 14 Toloza EM, Harpole L, McCrory DC. Noninvasive staging of non-small cell lung cancer: a review of the current evidence. Chest 2003; 123(suppl 1):137S–146S 15 De Leyn P, Lardinois D, Van Schil PE, et al. ESTS guidelines for preoperative lymph node staging for non-small cell lung cancer. Eur J Cardiothorac Surg 2007; 32:1– 8 16 Bernasconi M, Chhajed PN, Gambazzi F, et al. Combined transbronchial needle aspiration and positron emission tomography for mediastinal staging of NSCLC. Eur Respir J 2006; 27:889 – 894 17 Sharma A, Fidias P, Hayman LA, et al. Patterns of lymphadenopathy in thoracic malignancies. Radiographics 2004; 24: 419 – 434 18 Bhutani MS, Hawes RH, Hoffman BJ. A comparison of the accuracy of echo features during endoscopic ultrasound (EUS) and EUS-guided fine-needle aspiration for diagnosis of malignant lymph node invasion. Gastrointest Endosc 1997; 45:474 – 479 374 Downloaded From: http://journal.publications.chestnet.org/ on 11/24/2014 19 Catalano MF, Sivak MV, Rice T, et al. Endosonographic features predictive of lymph node metastasis. Gastrointest Endosc 1994; 40:442– 446 20 Chin R Jr, McCain TW, Lucia MA, et al. Transbronchial needle aspiration in diagnosing and staging lung cancer: how many aspirates are needed? Am J Respir Crit Care Med 2002; 166:377–381 21 Diacon AH, Schuurmans MM, Theron J, et al. Transbronchial needle aspirates: how many passes per target site? Eur Respir J 2007; 29:112–116 22 Holty JE, Kuschner WG, Gould MK. Accuracy of transbronchial needle aspiration for mediastinal staging of non-small cell lung cancer: a meta-analysis. Thorax 2005; 60:949 –955 23 Diacon AH, Schuurmans MM, Theron J, et al. Utility of rapid on-site evaluation of transbronchial needle aspirates. Respiration 2005; 72:182–188 24 Davenport RD. Rapid on-site evaluation of transbronchial aspirates. Chest 1990; 98:59 – 61 25 Baram D, Garcia RB, Richman PS. Impact of rapid on-site cytologic evaluation during transbronchial needle aspiration. Chest 2005; 128:869 – 875 26 Klapman JB, Logrono R, Dye CE, et al. Clinical impact of on-site cytopathology interpretation on endoscopic ultrasoundguided fine needle aspiration. Am J Gastroenterol 2003; 98: 1289 –1294 Original Research
© Copyright 2026