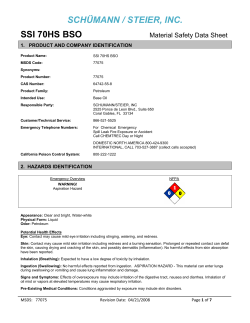
Chapter 18 Should the Ovaries be Removed During a Hysterectomy?
Chapter 18 Should the Ovaries be Removed During a Hysterectomy? Michael S. Broder, MD, MSHS Wendy C. Hsiao, BS Introduction In the US, bilateral salpingo-oophorectomy (BSO) at the time of hysterectomy for benign disease is commonly done to prevent the subsequent development of ovarian cancer. Almost all BSOs (87%) are done at time of hysterectomy [1]. Oophorectomy rates appear to have peaked recently, with 55% of hysterectomies accompanied by the procedure in 1999 compared to 39-45% in more recent years [2, 3, 4]. Recent data show age remains the strongest predictor of elective BSO, with 40% of women 40-44 years old, 78% of women 50-54 years old, and 68% of women 55 years or older having had BSO at hysterectomy [5]. Despite the common practice of “risk-reducing” or prophylactic oophorectomy at the time of hysterectomy for benign disease, an increasing body of evidence suggests removal of normal ovaries has minimal overall benefit for those women who are not at an increased risk of breast or ovarian cancer. Several large cohort studies suggest that while removing normal ovaries reduces the risk of ovarian cancer to almost zero, prophylactic oophorectomy does not appear to increase overall survival. This chapter will address the history of risk-reducing oophorectomy, assess the evidence for the practice, and consider its appropriateness in light of recent studies. History The development of modern abdominal surgery and the search for safe surgical treatments for ovarian tumors are closely intertwined. In 1806, Ephraim McDowell removed an ovarian tumor, and made history when the patient survived. Forty-seven years later, Walter Burnham performed the first successful hysterectomy [6]. The ensuing 100 years saw a substantial increase in oophorectomy resulting from better anesthesia, the introduction of aseptic techniques and effective antibiotics, and the widespread use of exogenous replacements for ovarian hormones. Advances in anesthesia and reductions in infection increased oophorectomy indirectly by contributing to the more widespread use of hysterectomy, while the synthetic estrogens removed a major barrier to incidental BSO: the reluctance to induce surgical menopause and its concomitant risks. . In the second half of the 19th century, the use of ether and chloroform allowed physicians to experiment with surgical procedures that previously could not be attempted. In 1867, Joseph Lister published his treatise “On the Antiseptic Principle of the Practice of Surgery”, and not long after, the “hand-washing fool”, Ignaz Semmelweis, dramatically reduced rates of puerperal sepsis by introducing hand-washing to Vienna General Hospital’s obstetric service. Halsted introduced the sterilized medical glove in 1890, but even with these infection-reducing innovations, the mortality rate for hysterectomy was 30% in the late 19th century [6]. The modern antibiotic era began with mass production of penicillin (driven by the needs of U.S. troops in World War II). By 1950, penicillin was reported to reduce morbidity after vaginal hysterectomy. As the mortality fell, it became more appropriate to consider 1 hysterectomy for non-life threatening conditions, and in 1984 more than a third of women could expect to have a hysterectomy by age 60 [7]. Although hysterectomy rates rose steadily in the late 20th century, rates of BSO remained fairly constant. A multi-center study showed hysterectomy was accompanied by BSO at a rate of between 9 and 12% over the 25 years from 1928 to 1953 [8]. This began to change when, in the 1950s, a series of publications raised concern among gynecologists about ovarian cancer in “residual” ovaries--those not removed at hysterectomy [9, 10]. Case series of women who developed ovarian cancer years after hysterectomy were extrapolated to calculate the number of women who could be “saved” had all such procedures been accompanied by BSO [11, 12]. As a result, by the 1960’s, gynecologists were enthusiastically recommending BSO at hysterectomy after age 40, or younger if childbearing was complete [8]. The primary disadvantage of BSO before natural menopause was considered to be the combination of symptoms caused by lack of ovarian hormones and osteoporosis. In 1941, the newly established FDA approved DES to treat menopausal symptoms, and approval of conjugated equine estrogens followed the year after. Several books published over the next 25 years, most notably Feminine Forever by gynecologist Robert Wilson, depicted menopause as the enemy of youth [13]. As estrogen therapy (ET) began to be seen as the cure for the scourge of menopause, the number of women using it to treat menopausal symptoms rose: from about 2.5 million women in 1966 to over 4.7 million women in 1975. After unopposed estrogen was linked to endometrial cancer, the number dropped to 2.3 million in 1980. The introduction of combination estrogen/progestin therapy (E+P) negated this risk, and by 1995 10 million US women were using exogenous estrogen. A proposed cardiovascular benefit helped drive this up to approximately 15 million by 2001 [14, 15, 16]. Following the publication of data from the Women’s Health Initiative (WHI) in 2002, faith in hormone therapy drastically declined [17]. This large randomized placebo-controlled trial of E+P in postmenopausal women was terminated prematurely when the overall health risks were demonstrated to exceed the benefits [18]. By 2003, fewer than 8.3 million women were taking exogenous estrogen, a level not seen since the mid-1990s [15, 16]. With no reliable tools to screen for or prevent ovarian cancer, oophorectomy has been seen as the best form of prevention, with hormone deprivation its primary downside. Thus, when faith in estrogen was high, the oophorectomy rate climbed; when faith declined, so did the rate of BSO. The figure shows this relationship. In 1965, 25% of hysterectomies in the US were accompanied by BSO. By 1975 the proportion had increased to almost 40% [7, 19]. The percentage of hysterectomies with BSO peaked in1999 at 55%, but by 2006 was estimated at only 36% [2, 3]. (Fig. 18.1). Recent Evidence Two recent large prospective cohort studies have provided new evidence concerning the benefits and risks of BSO. These studies, together involving more than 50,000 US women, estimated the health effects of BSO compared to ovarian conservation at hysterectomy on mortality and a variety of other outcomes. Taken together, they represent the best evidence currently available to estimate the influence of BSO on overall health. The Nurses’ Health Study (NHS) is a large, prospective cohort study of female nurses aged 30-55 in 1976. In 2009, we published a study of 29,380 women enrolled in the NHS who had hysterectomy for benign disease [21]. Of these, 55.6% had BSO and 44.4% had ovarian conservation. The mean age at enrollment was 51 years, and the cohort consisted mostly of white women with relatively uniform 2 education, socioeconomic status, and access to health care. These women were followed for an average of 24 years, from 1976 through 2002, and they reported new diagnoses and health conditions every 2 years by mail-in survey. Survey data were confirmed in interviews and by review of medical records. We stratified the cohort into those < 45, 45-54, and 55 years or older at the time of hysterectomy. The study analyzed the incidence of breast, epithelial ovarian, lung, or colorectal cancer; hip fracture; coronary heart disease (CHD); stroke; pulmonary embolism (PE); cause-specific death for each of these causes; and death due to all causes. The second large cohort study was published in 2011 and followed 25,448 post-menopausal women from the WHI Observational Study who had hysterectomy [22]. The WHI Observational Study is a prospective cohort study of women aged 50-79 years at enrollment who were invited to participate in a randomized controlled trial (RCT) comparing dietary modification to exogenous hormones, but who were ineligible or declined to participate. Study participants were contacted yearly and reported any hospitalizations or events related to outcomes of interest. Survey data were confirmed by medical record review. Mean follow-up time was slightly less than 8 years, compared to 24 years in the NHS analysis. Like the NHS, 56% had BSO and 44% had ovarian conservation. The mean age at enrollment was 63 years, compared to 51 in the NHS, but the cohorts were otherwise similar. Study subjects were stratified into those < 40, 40-49, and 50 years or older at time of hysterectomy. Outcome measures included incident ovarian, breast, lung, or colorectal cancer; hip fracture; cardiovascular events including CHD, stroke, and total CVD events; and all-cause death. The study did not report cause-specific death. Both studies performed separate analyses among women who did not use ET. We summarize the study results by outcome below. Cancer Breast cancer The NHS demonstrated a statistically significantly reduced risk of breast cancer in women who had BSO compared to those who had ovarian conservation (all women, HR 0.75, 95% CI 0.68-0.84; women < 45 years old at hysterectomy, HR 0.62, 95% CI 0.53-0.74). In women who never used ET, BSO reduced the point estimate for breast cancer risk, but the difference was not statistically significant (all women, HR 0.85, 95% CI 0.61-1.20; women < 50 years old at hysterectomy, HR 0.66, 95% CI 0.431.03). There was no difference in the risk of death from breast cancer between BSO and ovarian conservation (all women, HR 0.94, 95% CI 0.70-1.26) [21]. The WHI data showed a statistically significant protective effect of BSO on breast cancer in women < 40 at time of hysterectomy with no history of ET use (HR 0.36, 95% CI 0.14-0.95). The authors did not attempt to estimate the risk of death from breast cancer [22]. Both studies suggest BSO reduces breast cancer risk, particularly in younger women, but it may not reduce risk of death from breast cancer. Power calculations suggest that if the actual reduction in mortality were equal to that observed in the NHS (0.94), an RCT of over 400,000 patients would be required to have 80% power to detect such a difference. (Table 18.2) Ovarian cancer The NHS showed that BSO statistically significantly reduced the risk of ovarian cancer in all women (HR 0.04, 95% CI 0.01-0.09) and reduced the risk of death from ovarian cancer (all women, HR 0.06, 95% CI 0.02-0.21) [21]. In the WHI study, there was a 0.02% incidence of ovarian cancer in women who received both BSO and hysterectomy, compared to 0.33% incidence in women with hysterectomy alone. BSO statistically significantly reduced the risk of ovarian cancer in women who did not use ET (0.04% vs. 0.23%) [22]. There is some evidence from other studies that hysterectomy alone 3 reduces the risk of ovarian cancer, but BSO at hysterectomy clearly reduces both the risk of ovarian cancer and the risk of death from this disease. Lung Cancer BSO was associated with a statistically significantly increased risk of lung cancer (HR 1.26, 95% CI 1.02-1.56) and an increased risk of death from lung cancer in the NHS (HR 1.31, 95% CI 1.02-1.68) in all women. Risk of lung cancer was further increased in women who had never used ET (HR 2.09, 95% CI 1.01-4.33) [21]. There was no association of BSO with lung cancer in the WHI study (all women, HR 0.96, 95% CI 0.72-1.27) [22]. There is no agreed-upon biological explanation of the observations from the NHS, although some theories have been proposed [23, 24]. Total cancer In the NHS, BSO was associated with a statistically significantly reduced risk of total cancer (all women, HR 0.90, 95% CI 0.84-0.96), consistent with the reduction in breast and ovarian cancer. However, the risk of death from all cancers was statistically significantly increased in all women who had BSO (HR 1.17, 95% CI 1.04-1.32) [21]. The WHI study found a similar point estimate for the risk of total cancer, but the result was not statistically significant (all women, HR 0.96, 95% CI 0.87-1.05) [22]. The study did not report cancer-specific mortality. Cardiovascular Disease In the NHS, BSO was associated with a statistically significantly increased risk of CHD (all women, HR 1.17, 95% CI 1.02-1.35). BSO was associated with increased point estimates of risk for stroke among all women, although the results were not statistically significant (HR 1.14, 95% CI 0.981.33). The effect of BSO on cardiovascular disease risk was greater in women who had not used ET: in the group of never users, BSO statistically significantly increased the risk of stroke (HR 1.85, 95% CI 1.09-3.16). Women younger than 50 who did not use ET had increased risk of both CHD (HR 1.98, 95% CI 1.18-3.32) and stroke (HR 2.19, 95% CI 1.16-4.14). BSO was associated with a statistically significantly increased risk of death from CHD (HR 1.28, 95% CI 1.00-1.64) and an increased point estimate of the risk of death from stroke (HR 1.11, 95% CI 0.82-1.51), although this last finding did not reach statistical significance [21]. In contrast, the WHI study found no difference in the risk of cardiovascular disease between women who had BSO compared to those with ovarian conservation (all women, HR 0.99, 95% CI 0.911.09). Among women who did not use ET, the point estimate for risks of CHD (HR 1.24, 95% CI 0.921.68), stroke (HR 1.31, 95% CI 0.92-1.87), and total cardiovascular disease (HR 1.05, 95% CI 0.89-1.25) were increased, but these findings were not statistically significant. The WHI findings are limited by short follow-up (~ 8 years), especially since CHD may take approximately 15 years to develop following oophorectomy [22, 26]. Overall, the evidence suggests that BSO at the time of hysterectomy increases the risk of cardiovascular disease and cardiovascular-disease-related mortality. Lack of ET use further increases risk. Inconsistencies between studies may be due to lower power in the WHI study [22]. Hip Fracture 4 In both the NHS and WHI studies, there was no statistically significant association between BSO and hip fracture (all women, HR 0.89, 95% CI 0.71-1.12 in the NHS; all women, HR 0.83, 95% CI 0.631.10 in the WHI), and these findings were consistent whether or not there was history of ET use [21, 22]. Survival The NHS found that BSO statistically significantly increased all-cause mortality (all women, HR 1.12, 95% CI 1.03-1.21), related in part to the increased risk of death from lung cancer, all cancers, and CHD. Risk of all-cause mortality was statistically significantly increased in women less than 50 at hysterectomy who had never used ET (HR 1.40, 95% CI 1.01-1.96) [21]. The WHI study found no statistically significant difference in mortality among all women (HR 0.98, 95% CI 0.87-1.10). In women less than 40 who had not used ET, the point estimate for mortality was increased, but this was not statistically significant (HR 1.15, 95% CI 0.78-1.70) [22]. Neither study reported a survival benefit for BSO at any age or in any subgroup. (Table 18.3) Other Evidence While these two studies represent the largest and best-controlled studies to examine the impact of oophorectomy compared to conservation of the ovaries at hysterectomy, other studies have addressed various aspects of the question. A recent systematic review of the impact of BSO on CHD found oophorectomy did not increase the risk of CHD overall, but most of the trials were low quality. The review found no benefit of BSO [25]. A large cohort study published in 2011 investigated cardiovascular disease risk in 184,441 hysterectomized women in the Swedish Inpatient Register, showing statistically significantly increased risks of both CHD and stroke in women younger than 50 who had BSO at hysterectomy compared to those who had neither hysterectomy nor BSO [27]. A retrospective cohort study of 2,383 women in Olmsted County, MN found an increase in all-cause mortality in women < 45 who had oophorectomy, but observed no such increase in older women [28]. Using the same cohort, an association between oophorectomy and increased risk of neurologic conditions (Parkinsonism, dementia, and anxiety or depression) was identified, but the findings await confirmation in other populations [29, 30]. Finally, a Markov model estimated that overall mortality was increased in women who had oophorectomy before age 65. At no age was there a survival advantage with oophorectomy [31]. 18. Recommendations Oophorectomy at the time of hysterectomy has become a common operation, primarily as a prophylactic measure to reduce the risk of ovarian cancer. There are several reasons why this traditional practice should be reconsidered for women who do not have a clearly elevated risk of breast or ovarian cancer due to BRCA mutation or family or personal history. First, a major driver of the increase in oophorectomy rates was the availability of exogenous estrogen therapy. As recent studies have shown, however, encouraging long term drug therapy without long term outcome studies is fraught with potential dangers. Fewer women are willing to begin taking estrogen, and among those who do, the continuation rate is low. Even if women could be persuaded to stay on therapy, long term estrogen has not been shown to lengthen life, nor does it completely mitigate the risks of oophorectomy. Second, while oophorectomy does dramatically reduce the risk of ovarian cancer in all women and reduces the risk of breast cancer in younger women, there is no evidence that it prolongs life. In fact, the best available evidence suggests either a net harmful effect or, at best, a neutral effect. Current evidence indicates this lack of overall benefit likely relates to the relatively low incidence of ovarian cancer in contrast to the relatively common nature of CHD, the risk of which is increased with oophorectomy. 5 The data on which these conclusions are based derive from observational studies. However, the data supporting prophylactic oophorectomy were based on even lower quality evidence—namely, theoretical considerations and case series. Considering the weight of the evidence, if “prophylactic oophorectomy” was a new drug or device, regulatory agencies would be unlikely to approve it. Waiting for evidence for RCTs before deciding whether to recommend BSO for a woman having hysterectomy might be reasonable (although given the necessary size of such a trial, analysis of patient outcomes would entail a long wait), but in the meantime, it might be wise to consider the admonition to “first, do no harm.” 6 TABLES Table 18.1 Proportion of hysterectomies accompanied by BSO Annual no. of women using ET (estimated from number of prescription fills [15, 16]) Sources: See Ref. 2 See Ref. 3 * See Ref. 7 ● See Ref. 8 ■ ▲ See Ref. 14 See Ref. 15 See Ref. 19 See Ref. 20 7 Table 18.2. Impact of Oophorectomy on Cancer Outcomesa Hazard Ratio (95% Confidence Interval) Breast cancer Ovarian cancer All cancers Incidence Death Incidence Death Incidence Death 0.62 (0.53-0.74) 0.74 (0.47-1.18) 0.03 (0.01-0.14) 0.06 (0.01-0.43) 0.83 (0.75-0.92) 1.08 (0.91-1.27) 0.72 (0.51-1.02) - - - 0.97 (0.81-1.17) - 0.66 (0.43-1.03) - - - - - 0.36 (0.14-0.95) - - - 0.93 (0.62-1.39) - 1.05 (0.71-1.55) 1.28 (0.46-3.54) 0.07 (0.01-0.60) - 1.01 (0.79-1.29) 1.50 (0.91-2.45) 1.02 (0.74-1.41) - - - 1.08 (0.89-1.32) - 1.88 (0.66-5.32) - - - - - 0.77 (0.41-1.45) - - - 0.92 (0.63-1.33) - 0.75 (0.68-0.84) 0.94 (0.70-1.26) 0.04 (0.01-0.09) 0.06 (0.02-0.21) 0.90 (0.84-0.96) 1.17 (1.04-1.32) 0.96 (0.81-1.13) - - - 0.96 (0.87-1.05) - 0.85 (0.61-1.20) - - - - - 0.72 (0.49-1.05) - - - 0.90 (0.74-1.10) - Younger women < 45 years < 40 yearsb No ET use, < 50 years old No ET use, < 40 years oldb Older women ≥ 55 years old ≥ 50 years oldb No ET use, ≥ 50 years old No ET use, ≥ 50 years oldb All women All ages b All ages No ET use, all ages No ET use, all agesb a b See Ref. 21, unless otherwise noted See Ref. 22 8 Table 18.3. Impact of Oophorectomy on Non-Cancer Health Outcomesa Hazard Ratio (95% Confidence Interval) Incidence Death Incidence Death All-Cause Mortality Death 1.26 (1.04-1.54) 1.14 (0.81-1.61) 1.19 (0.96-1.49) 0.85 (0.54-1.34) 1.06 (0.95-1.18) < 40 years No ET use, < 50 years old No ET use, < 40 years oldb Older women 0.98 (0.72-1.35) - 1.13 (0.81-1.58) - 0.90 (0.72-1.13) 1.98 (1.18-3.32) - 2.19 (1.16-4.14) - 1.40 (1.01-1.96) 1.33 (0.77-2.30) - 1.44 (0.78-2.65) - 1.15 (0.78-1.70) ≥ 55 years old 1.31 (0.73-2.36) 1.51 (0.86-2.64) 2.26 (0.85-5.95) 1.14 (0.85-1.52) ≥ 50 years oldb No ET use, ≥ 50 years old No ET use, ≥ 50 years oldb All women 1.02 (0.74-1.41) 4.10 (0.4141.06) - 0.98 (0.68-1.41) - 1.07 (0.84-1.35) 0.70 (0.34-1.44) - 1.21 (0.48-3.00) - 2.05 (0.87-4.79) 1.00 (0.56-1.78) - 1.37 (0.62-3.00) - 0.97 (0.62-1.52) 1.17 (1.02-1.35) 1.28 (1.00-1.64) 1.14 (0.98-1.33) 1.11 (0.82-1.51) 1.12 (1.03-1.21) 1.00 (0.85-1.18) - 1.04 (0.87-1.24) - 0.98 (0.87-1.10) 1.42 (0.93-2.16) - 1.85 (1.09-3.16) - 1.20 (0.91-1.57) 1.24 (0.92-1.68) - 1.31 (0.92-1.87) - 0.99 (0.80-1.23) CHD Stroke Younger women < 45 years b All ages b All ages No ET use, all ages No ET use, all agesb a b See Ref. 21, unless otherwise noted See Ref. 22 9 REFERENCES 1. Melton LJ 3rd, Bergstralh EJ, Malkasian GD, et al. Bilateral oophorectomy trends in Olmsted County, Minnesota, 1950-1987. Epidemiology. 1991 Mar;2(2):149-52. 2. Keshavarz H, Hillis SD, Kieke BA, Marchbanks PA. Hysterectomy surveillance—United States, 19941999. MMWR Surveill Summ. 2002;51(SS05):1-8. 3. Asante A, Whiteman MK, Kulkarni A, et al. Elective oophorectomy in the United States: trends and in-hospital complications, 1998-2006. Obstet Gynecol. 2010 Nov;116(5):1088-95. 4. Lowder JL, Oliphant SS, Ghetti C, et al. Prophylactic bilateral oophorectomy or removal of remaining ovary at the time of hysterectomy in the United States, 1979-2004. Am J Obstet Gynecol. 2010 Jun;202(6):538.e1-9. 5. Jacoby VL, Vittinghoff E, Nakagawa S, et al. Factors associated with undergoing bilateral salpingo-oophorectomy at the time of hysterectomy for benign conditions. Obstet Gynecol. 2009 Jun;113(6):1259-67. 6. Rock JA. Historical development of pelvic surgery. In: Thompson JD, Rock JA, eds. Te Linde’s Operative Gynecology. 7th ed. Philadelphia, PA: J. B. Lippincott Company; 1992:1. 7. Pokras R, Hufnagel VG. Hysterectomy in the United States, 1965-84. Am J Public Health. 1988 Jul;78(7):852-3. 8. Randall CL, Paloucek FP. The frequency of oophorectomy at the time of hysterectomy: trends in surgical practice, 1928-1953. Am J Obstet Gynecol. 1968 Mar 1;100(5):716-26. 9. Christ JE, Lotze EC. The residual ovary syndrome. Obstet Gynecol. 1975 Nov;46(5):551-6. 10. Speert H. Prophylaxis of Ovarian Cancer. Ann Surg. 1949 Apr;129(4):468-75. 11. Grundsell H, Ekman G, Gullberg B, et al. Some aspects of prophylactic oophorectomy and ovarian carcinoma. Ann Chir Gynaecol. 1981;70(1):36-42. 10 12. Sightler SE, Boike GM, Estape RE, et al. Ovarian cancer in women with prior hysterectomy: a 14-year experience at the University of Miami. Obstet Gynecol. 1991 Oct;78(4):681-4. 13. Stefanick ML. Estrogens and progestins: background and history, trends in use, and guidelines and regimens approved by the US Food and Drug Administration. Am J Med. 2005 Dec 19;118 Suppl 12B:64-73. 14. Kennedy DL, Baum C, Forbes MB. Noncontraceptive estrogens and progestins: use patterns over time. Obstet Gynecol. 1985 Mar;65(3):441-6. 15. Hersh AL, Stefanick ML, Stafford RS. National use of postmenopausal hormone therapy: annual trends and response to recent evidence. JAMA. 2004 Jan 7;291(1):47-53. 16. Wysowski DK, Golden L, Burke L. Use of menopausal estrogens and medroxyprogesterone in the United States, 1982-1992. Obstet Gynecol. 1995 Jan;85(1):6-10. 17. Wegienka G, Havstad S, Kelsey JL. Menopausal hormone therapy in a health maintenance organization before and after women's health initiative hormone trials termination. J Womens Health (Larchmt). 2006 May;15(4):369-78. 18. Writing Group for the Women's Health Initiative Investigators, Rossouw JE, Anderson GL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002 Jul 17;288(3):321-33. 19. Pokras R, Hufnagel VG. Hysterectomies in the United States. Vital Health Stat. 1987;13(92):1-32. 20. Wysowski DK, Governale LA. Use of menopausal hormones in the United States, 1992 through June, 2003. Pharmacoepidemiol Drug Saf. 2005 Mar;14(3):171-6. 21. Parker WH, Broder MS, Chang E, et al. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses' health study. Obstet Gynecol. 2009 May;113(5):102737. 22. 11 Jacoby VL, Grady D, Wactawski-Wende J, et al. Oophorectomy vs ovarian conservation with hysterectomy: cardiovascular disease, hip fracture, and cancer in the Women's Health Initiative Observational Study. Arch Intern Med. 2011 Apr 25;171(8):760-8. 23. Brinton LA, Gierach GL, Andaya A, et al. Reproductive and hormonal factors and lung cancer risk in the NIH-AARP Diet and Health Study cohort. Cancer Epidemiol Biomarkers Prev. 2011 May;20(5):900-11. 24. Liu Y, Inoue M, Sobue T, et al. Reproductive factors, hormone use and the risk of lung cancer among middle-aged never-smoking Japanese women: a large-scale population-based cohort study. Int J Cancer. 2005 Nov 20;117(4):662-6. 25. Jacoby VL, Grady D, Sawaya GF. Oophorectomy as a risk factor for coronary heart disease. Am J Obstet Gynecol. 2009 Feb;200(2):140.e1-9. 26. Parrish HM, Carr CA, Hall DG, et al. Time interval from castration in premenopausal women to development of excessive coronary atherosclerosis. Am J Obstet Gynecol. 1967 Sep 15;99(2):155-62. 27. Ingelsson E, Lundholm C, Johansson AL, et al. Hysterectomy and risk of cardiovascular disease: a population-based cohort study. Eur Heart J. 2011 Mar;32(6):745-50. 28. Rocca WA, Grossardt BR, de Andrade M, et al. Survival patterns after oophorectomy in premenopausal women: a population-based cohort study. Lancet Oncol. 2006 Oct;7(10):821-8. 29. Rocca WA, Bower JH, Maraganore DM, et al. Increased risk of cognitive impairment or dementia in women who underwent oophorectomy before menopause. Neurology. 2007 Sep 11;69(11):1074-83. 30. Rocca WA, Bower JH, Maraganore DM, et al. Increased risk of parkinsonism in women who underwent oophorectomy before menopause. Neurology. 2008 Jan 15;70(3):200-9. 31. Parker WH, Broder MS, Liu Z, et al. Ovarian conservation at the time of hysterectomy for benign disease. Obstet Gynecol. 2005 Aug;106(2):219-26. 12
© Copyright 2026