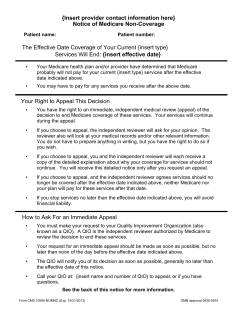
N C OTICE OF MEDICARE
OMB Approval No. 0938-0910
NOTICE OF MEDICARE NON-COVERAGE
Patient Name:
Patient ID Number:
THE EFFECTIVE DATE COVERAGE OF YOUR CURRENT SKILLED
NURSING FACILITY SERVICES WILL END: {insert effective date}
•
•
Your Medicare Advantage (MA) plan and/or provider have determined that Medicare
probably will not pay for your current SKILLED NURSING FACILITY services after
the effective date indicated above.
You may have to pay for any SKILLLED NURSING FACILITY services you receive
after the above date.
YOUR RIGHT TO APPEAL THIS DECISION
•
You have the right to an immediate, independent medical review (appeal), while your
services continue, of the decision to end Medicare coverage of these services.
•
If you choose to appeal, the independent reviewer will ask for your opinion. The
reviewer will also look at your medical records and/or other relevant information.
You do not have to prepare anything in writing, but you have the right to do so
if you wish.
•
If you choose to appeal, you and the independent reviewer will each receive a copy
of the detailed explanation about why your coverage for services should not
continue. You will receive this detailed notice only after you request an appeal.
•
If you choose to appeal, and the independent reviewer agrees that services should
no longer be covered after the effective date indicated above, neither Medicare nor
your MA plan will pay for these services after that date.
•
If you stop services no later than the effective date indicated above, you will avoid
financial liability.
HOW TO ASK FOR AN IMMEDIATE APPEAL
•
•
You must make your request to your Quality Improvement Organization (also known
as a QIO). A QIO is the independent reviewer authorized by Medicare to review the
decision to end these services.
Your request for an immediate appeal should be made as soon as possible, but no
later than noon of the day before the effective date indicated above.
See the next page for more information
•
•
The QIO will notify you of its decision as soon as possible, generally by no later than
the effective date of this notice.
Call your QIO at:
Quality Insights of Pennsylvania
2601 Market Place Street, Suite 320
Harrisburg, PA 17110
1-800-322-1914
to appeal, or if you have questions.
OTHER APPEAL RIGHTS:
•
If you miss the deadline for requesting an immediate appeal with the QIO, you still
may request an expedited appeal from your MA plan. If your request does not meet
the criteria for an expedited review, your MA plan will review the decision under its
rules for standard appeals. Please see your Evidence of Coverage for more
information.
•
Contact your MA plan or 1-800-MEDICARE (1-800-633-4227), or TTY/TDD: 1-877486-2048 for more information about the MA appeals process.
ADDITIONAL INFORMATION (OPTIONAL)
Contact your health plan at
Highmark Blue Shield/FreedomBlue
Medicare Advantage Healthcare Management Services Appeal Department
P.O. Box 535073
Pittsburgh, PA 15253-5073
FAX: Medicare Advantage Appeal Department
1-800-485-9610
Fax# 1-800-894-7947
TTY/TDD# 1-888-422-1226
If you have any questions you can contact your health plan at 1-866-306-1061 Monday through
Friday, 8:00am-4:30pm. If you have a hearing or speech impairment, please call us at
TTY/ TDD 1-800-988-0668 Monday through Friday, 8:00am-4:30pm.
Please sign below to indicate that you have received this notice.
I have been notified that coverage of my services will end on the effective date indicated on
this notice and that I may appeal this decision by contacting my QIO.
__________________________________________
Signature of Patient or Authorized Representative
_____________
Date
Form No. CMS-10095
Exp. Date 03/31/2007
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a
valid OMB control number. The valid OMB control number for this information collection is 0938-0910. The time required to prepare and
distribute this collection is 15 minutes per notice, including the time to select the preprinted form, complete it and deliver it to the enrollee.
If you have comments concerning the accuracy of the time estimates or suggestions for improving this form, please write to CMS, PRA
Clearance Officer, 7500 Security Boulevard, Baltimore, Maryland 21244-1850.
OMB Approval No. 0938-0910
NOTICE OF MEDICARE NON-COVERAGE
Patient Name:
Patient ID Number:
THE EFFECTIVE DATE COVERAGE OF YOUR CURRENT HOME HEALTH
AGENCY SERVICES WILL END: {insert effective date}
•
•
Your Medicare Advantage (MA) plan and/or provider have determined that Medicare
probably will not pay for your current HOME HEALTH AGENCY services after the
effective date indicated above.
You may have to pay for any HOME HEALTH AGENCY services you receive after
the above date.
YOUR RIGHT TO APPEAL THIS DECISION
•
You have the right to an immediate, independent medical review (appeal), while your
services continue, of the decision to end Medicare coverage of these services.
•
If you choose to appeal, the independent reviewer will ask for your opinion. The
reviewer will also look at your medical records and/or other relevant information.
You do not have to prepare anything in writing, but you have the right to do so
if you wish.
•
If you choose to appeal, you and the independent reviewer will each receive a copy
of the detailed explanation about why your coverage for services should not
continue. You will receive this detailed notice only after you request an appeal.
•
If you choose to appeal, and the independent reviewer agrees that services should
no longer be covered after the effective date indicated above, neither Medicare nor
your MA plan will pay for these services after that date.
•
If you stop services no later than the effective date indicated above, you will avoid
financial liability.
HOW TO ASK FOR AN IMMEDIATE APPEAL
•
•
You must make your request to your Quality Improvement Organization (also known
as a QIO). A QIO is the independent reviewer authorized by Medicare to review the
decision to end these services.
Your request for an immediate appeal should be made as soon as possible, but no
later than noon of the day before the effective date indicated above.
See the next page for more information
•
•
The QIO will notify you of its decision as soon as possible, generally by no later than
the effective date of this notice.
Call your QIO at:
Quality Insights of Pennsylvania
2601 Market Place Street, Suite 320
Harrisburg, PA 17110
1-800-322-1914
to appeal, or if you have questions.
OTHER APPEAL RIGHTS:
•
If you miss the deadline for requesting an immediate appeal with the QIO, you still
may request an expedited appeal from your MA plan. If your request does not meet
the criteria for an expedited review, your MA plan will review the decision under its
rules for standard appeals. Please see your Evidence of Coverage for more
information.
•
Contact your MA plan or 1-800-MEDICARE (1-800-633-4227), or TTY/TDD: 1-877486-2048 for more information about the MA appeals process.
ADDITIONAL INFORMATION (OPTIONAL)
Contact your health plan at
Highmark Blue Shield/FreedomBlue
Medicare Advantage Healthcare Management Services Appeal Department
P.O. Box 535073
Pittsburgh, PA 15253-5073
FAX: Medicare Advantage Appeal Department
1-800-485-9610
Fax# 1-800-894-7947
TTY/TDD# 1-888-422-1226
If you have any questions you can contact your health plan at 1-866-306-1061 Monday through
Friday, 8:00am-4:30pm. If you have a hearing or speech impairment, please call us at
TTY/ TDD 1-800-988-0668 Monday through Friday, 8:00am-4:30pm.
Please sign below to indicate that you have received this notice.
I have been notified that coverage of my services will end on the effective date indicated on
this notice and that I may appeal this decision by contacting my QIO.
__________________________________________
Signature of Patient or Authorized Representative
_____________
Date
Form No. CMS-10095
Exp. Date 03/31/2007
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a
valid OMB control number. The valid OMB control number for this information collection is 0938-0910. The time required to prepare and
distribute this collection is 15 minutes per notice, including the time to select the preprinted form, complete it and deliver it to the enrollee.
If you have comments concerning the accuracy of the time estimates or suggestions for improving this form, please write to CMS, PRA
Clearance Officer, 7500 Security Boulevard, Baltimore, Maryland 21244-1850.
Form Instructions
Notice of Medicare Non-Coverage (NOMNC)
“The Advance Notice”
CMS-10095-A
A MedicareAdvantage (MA) provider must deliver an advance, completed copy of this
notice to enrollees receiving skilled nursing, home health or comprehensive outpatient
rehabilitation facility services not later than 2 days before the termination of services. This
notice fulfills the requirement at 42 CFR § 422.624(b)(2).
This is a standard notice. MA providers may not deviate from the content of the form
except where indicated. (You may modify the form for mass printing to indicate the kind
of service being terminated if only one type of service is provided, i.e., skilled nursing,
home health, or comprehensive outpatient rehabilitation.) In situations where the
termination decision is not delegated to the provider, the MA plan must provide the
termination of services date to the provider not later than 2 days before the termination of
services for timely delivery to occur.
The NOMNC should not be used when MA plans determine that an enrollee’s services
should end based on the exhaustion of Medicare benefits (such as the 100-day SNF limit).
Instead, MA plans must issue the Notice of Denial of Medical Coverage.
MA plans and providers will note that the notice must be validly delivered. Valid delivery
means that the enrollee must be able to understand the purpose and contents of the notice in
order to sign for receipt of it. The enrollee must be able to understand that he or she may
appeal the termination decision. If the enrollee is not able to comprehend the contents of
the notice, it must be delivered to and signed by an authorized representative of the
enrollee. Valid delivery does not preclude the use of assistive devices, witnesses, or
interpreters for notice delivery. Thus, if an enrollee is able to comprehend the notice, but
either is physically unable to sign it, or needs the assistance of an interpreter to translate it
or an assistive device to read or sign it, valid delivery may be achieved by documenting the
use of such assistance. Furthermore, if the enrollee refuses to sign the notice, the notice is
still valid as long as the provider documents that the notice was given, but the enrollee
refused to sign.
Notice Delivery to Authorized Representatives
CMS requires that notification of changes in coverage for an enrollee who is not competent
be made to an authorized representative acting on behalf of the enrollee. Notification to the
authorized representative may be problematic because he or she may not be available in
person to acknowledge receipt of the required notification. MA plans and providers are
required to develop procedures to use when the enrollee is incompetent or incapable of
receiving the notice, and the provider cannot obtain the signature of the enrollee’s
representative through direct personal contact.
• If the provider is unable to personally deliver a notice of noncoverage to a person
legally acting on behalf of an enrollee, then the provider should telephone the
representative to advise him or her when the enrollee’s services are no longer covered.
•
The enrollee’s appeal rights must be explained to the representative, and the name and
telephone number of the appropriate quality improvement organization (QIO) should
be provided.
• The date of the conversation is the date of the receipt of the notice. Confirm the
telephone contact by written notice mailed on that same date.
• Place a dated copy of the notice in the enrollee’s medical file and document the
telephone contact to include: name of person initiating the contact, name of the
representative contacted, date and time of the contact and the telephone
number called.
• When direct phone contact cannot be made, send the notice to the representative by
certified mail, return receipt requested.
• The date that someone at the representative’s address signs (or refuses to sign) the
receipt is the date of receipt.
• Place a copy of the notice in the enrollee’s medical file and document the attempted
telephone contact to include: the name of person initiating the contact, the name of
the representative you attempted to contact, the date and time of the attempted contact
and the telephone number called.
• When notices are returned by the post office, with no indication of a refusal date, then
the enrollee’s liability starts on the second working day after the provider’s
mailing date.
These procedures also may be used where an enrollee has authorized an individual to act on
his or her behalf, and the provider cannot obtain the signature of the enrollee’s
representative through direct personal contact.
INSTRUCTIONS FOR CMS-10095-A PAGE 1:
Heading: MA plans and/or providers must be identified in this space. Logos may be used
if they include the name of the organization, address and telephone number of the
organization responsible for the termination decision above the title of the notice.
Patient Name: Insert the patient’s full name.
Patient ID Number: Insert a unique patient identifier such as the HIC number or Medical
Record number, if applicable.
THE EFFECTIVE DATE COVERAGE OF YOUR CURRENT {insert type}
SERVICES WILL END: {insert effective date}: Fill in the type of services ending,
{home health, skilled nursing, or comprehensive outpatient rehabilitation services}
and the actual date the covered service will end. The date should be in no less than 12point type. Note that if the effective date for the service termination changes after delivery
of the notice, the provider may contact the patient or authorized representative by phone to
inform him or her of the new service termination date. Confirm the telephone contact by
written notice mailed on that same date.
YOUR RIGHT TO APPEAL THIS DECISION
Bullet # 1
Bullet # 2
N/A
N/A
2
Bullet # 3
Bullet # 4
Bullet # 5
N/A
N/A
N/A
HOW TO ASK FOR AN IMMEDIATE APPEAL
Bullet # 1
Bullet # 2
Bullet # 3
Bullet # 4
N/A
N/A
N/A
Insert the name and telephone numbers (including TTY/TDD) of the
applicable QIO in no less than12-point type.
INSTRUCTIONS FOR CMS-10095-A PAGE 2 - Signature page:
OTHER APPEAL RIGHTS
Bullet # 1
Bullet #2
N/A
N/A
ADDITIONAL INFORMATION (OPTIONAL)
This space is available, at the option of the plan or relevant provider, to furnish additional
relevant information to the enrollee, such as further details about the reason for the service
termination, or the timing of any additional liability risk. The use of this space does not
replace the requirement to provide the Detailed Notice of Non-Coverage (DENC) to either
the enrollee or the QIO when an appeal is filed.
Signature line: The enrollee or the authorized representative must sign this line.
Date: The enrollee or the authorized representative must fill in the date that he or she signs
the document.
According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless
it displays a valid OMB control number. The valid OMB control number for this information collection is 0938-0910. The
time required to prepare and distribute this collection is 15 minutes per notice, including the time to select the preprinted
form, complete it and deliver it to the enrollee. If you have comments concerning the accuracy of the time estimates or
suggestions for improving this form, please write to CMS, PRA Clearance Officer, 7500 Security Boulevard, Baltimore,
Maryland 21244-1850.
3
© Copyright 2026