Notice of Medicare Non-Coverage (NOMNC) checklist for Skilled Nursing Facilities (SNF)
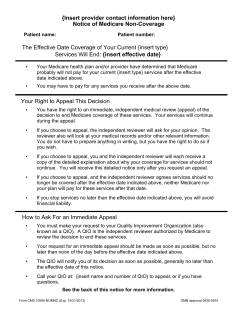
Notice of Medicare Non-Coverage (NOMNC) checklist for Skilled Nursing Facilities (SNF) Use this checklist to ensure you thoroughly and accurately complete the NOMNC form. A NOMNC must be issued a minimum of 2 days prior to the last day the patient is anticipated to be at SNF level of care. NOMNCs can be issued earlier to accommodate a weekend or to provide a longer transition period. With respect to weekends, although Quality Improvement Organizations (QIO) are open, Regence is closed. Providers should try to deliver the Regence NOMNC form early enough in the week to minimize the possibility of extended liability for weekend services. Completing the NOMNC form The last day of covered SNF level care is identified and discussed with the patient and family or authorized representative. SNF selects the Regence SNF NOMNC form. Be sure to select the correct version of the form. Versions vary by service area. Verify that the form includes the following elements: The type of service to be terminated (Skilled Nursing Services, Home Health Services or Comprehensive Outpatient Rehabilitation Services) is listed in the two fields referring to termination of services, in the first and second sections of the form. (These fields are identified by the instruction “Insert Type.”) Accurate Regence contact information Correct QIO information for the service area The delivering provider’s name, address and telephone number is entered above the title of the form. The patient name and the Regence member number are entered in the top section of the form. If the Regence member number is not available, the facility medical record number can be used. Do not use the patient’s Medicare number. The last covered day is entered on the form. The signature date must be two days prior to last covered day The patient or authorized representative signs the NOMNC form on page 2. If the patient is unable to sign, and the SNF is working with an authorized representative who is unable to be present at the facility that day, the SNF may issue the NOMNC by telephone. For a telephonic notice to be valid, the documentation on the NOMNC must include all of the following: The name of the staff person initiating the contact The name of the representative contacted by phone The date and time of the telephone contact The telephone number called A notation that full appeal rights were given to the representative The date of the properly documented telephone conversation is the date of the receipt of the notice. The facility must confirm the telephone contact by sending written notice to the authorized representative on that same date. Copies of the completed NOMNC are: 1. Given to the patient or the authorized representative who signed the NOMNC 2. Placed in the patient’s medical record at the SNF 3. Faxed to Regence at 1 (855) 240-6498 as soon as possible after the form is signed Contact your provider relations representative or Regence MedAdvantage Provider Customer Service if you have additional questions. Regence NOMNC instructions Revised October 2012 Discharge and appeals The patient may choose to discharge sooner than the designated day. In this case, the NOMNC must still be signed, and a note should be added detailing the circumstances of the early discharge. If the patient chooses to appeal, he or she must contact the QIO to request a review no later than noon on the day before services are to end. The QIO appeal decision will generally be completed within 48 hours of the patient's request for a review. If the patient appeals, the SNF should be prepared to provide documentation to Regence quickly to assist the review process. Skilled Nursing Facility sample scenario: On May 25th, Jane Doe is admitted to a SNF after surgery. On June 2nd, Regence MedAdvantage contacts the SNF to deliver a Regence NOMNC form to Ms. Doe indicating her last approved day will be June 4th, with discharge to a lower level of care on June 5th. Date Member agrees with discharge Jane Doe is admitted to SNF NOMNC Distribution Date Jane Doe receives advance notice that June 4th will be the last SNF day paid by Regence MedAdvantage Member disagrees with discharge Jane Doe is admitted to SNF NOMNC Distribution Date Jane Doe receives advance notice that June 4th will be the last SNF day paid by Regence MedAdvantage June 3rd Jane continues to receive SNF-level services Jane files an appeal with the QIO by noon and continues to receive SNF-level services June 4th Last Authorized Day Jane continues to receive SNF-level services June 5th Jane discharges to lower level of care as planned Last Authorized Day Jane continues to receive SNF-level services and should receive QIO decision by end of day If QIO upholds NOMNC, member is liable for cost of care starting today. If QIO overturns NOMNC or determines a new discharge date, Regence is liable for cost of care today. May 25th June 2nd Steps SNF delivers Regence NOMNC form Member or authorized representative signs Copies to member, medical record and Regence (by fax) QIO notifies Regence to provide medical information and detailed notice to the QIO by end of day. SNF may be asked to provide copy of the signed NOMNC and medical records. QIO can overturn, uphold or determine a new discharge date and will notify the member of its decision by end of day. QIO informs Regence of its decision. Regence contacts SNF to extend the authorization if NOMNC is overturned or new discharge date was determined. Regence NOMNC instructions Revised October 2012 < Provider Name> Insert provider name and address <Provider Address> <Pro Insert telephone number vider Phone Number> Notice of Medicare Non-Coverage patientName> name Patient Name: Insert <Member Patient Number: Insert <Subscriber RegenceID> member number Insert type of services ending The Effective Date Coverage of Your Current Comprehensive Outpatient Physical Services Will End: Last covered day _____________________________ Your Medicare provider and/or health plan have determined that Medicare Insert type of services ending probably will not pay for your current Current Comprehensive Outpatient Physical services after the effective date indicated above. You may have the pay for any services you receive after the above date. Your Right to Appeal This Decision You have the right to an immediate, independent medical review (appeal) of the decision to end Medicare coverage of these services. Your services will continue during the appeal. If you choose to appeal, the independent reviewer will ask for your opinion. The reviewer also will look at your medical records and/or other relevant information. You do not have to prepare anything in writing, but you have the right to do so if you wish. If you choose to appeal, you and the independent reviewer will each receive a copy of the detailed explanation about why your coverage for services should not continue. You will receive this detailed notice only after you request an appeal. If you choose to appeal, and the independent reviewer agrees services should no longer be covered after the effective date indicated above: o Neither Medicare nor your plan will pay for these services after that date. If you stop services no later than the effective date indicated above, you will avoid financial liability. How to Ask For an Immediate Appeal You must make your request to your Quality Improvement Organization (also known as a QIO). A QIO is the independent reviewer authorized by Medicare to review the decision to end these services. Your request for an immediate appeal should be made as soon as possible, but no later than noon of the day before the effective date indicated above. The QIO will notify you of its decision as soon as possible, generally no later than two days after the effective date of this notice if you are on Original Medicare. If you are in a Medicare health plan, the QIO generally will notify you of its decision by the effective date of this notice. Call your QIO at: Qualis Health, 1 (877) 290-4346 (TTY: 711) to appeal, or if you have questions. Form CMS 10123-NOMNC (Approved 12/31/2011) OMB approval 0938-0953 See page 2 if this notice for more information If You Miss The Deadline to Request An Immediate Appeal, You Might Have Other Appeal Rights: If you have Original Medicare: Call the QIO listed on Page 1. If you belong to a Medicare health plan: Call your plan at the number given below. Plan contact information: Regence MedAdvantage PO Box 12625 Salem, OR 97309 1 (866) 749-0355 (TTY: 711) Additional Information (Optional): Please sign below to indicate you received and understood this notice. I have been notified that coverage of my services will end on the effective date indicated on this notice and that I may appeal this decision by contacting my QIO. ____________________________________ Signature of Patient or Representative Form CMS 10123-NOMNC (Approved 12/31/2011) ___________________ Date OMB approval 0938-0953
© Copyright 2026