Marathon run: cardiovascular adaptation and
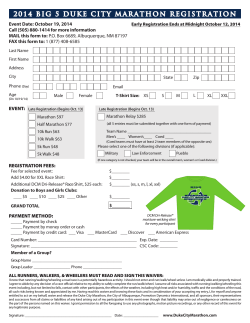
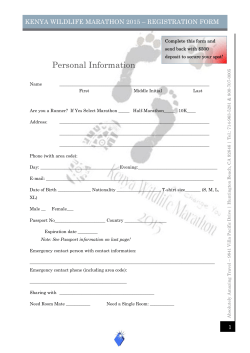
REVIEW European Heart Journal (2014) 35, 3091–3096 doi:10.1093/eurheartj/eht502 Clinical update Marathon run: cardiovascular adaptation and cardiovascular risk Hans-Georg Predel* Institute of Cardiovascular Research and Sports Medicine, German Sport University Cologne, Am Sportpark Mu¨ngersdorf 6, Cologne 50933, Germany Received 21 November 2012; revised 24 October 2013; accepted 20 November 2013; online publish-ahead-of-print 9 January 2014 ----------------------------------------------------------------------------------------------------------------------------------------------------------Keywords Marathon run † Endurance exercise † Middle-aged athletes † Cardiovascular adaptation Introduction Inspired by the ancient run from Marathon to Athens 490 BC, the idea to revive this long-distance run was born in the context of the first modern Olympic Games in 1896 taking place in Athens, Greece. While this first marathon run of modern times had a distance of 40 km today’s official distance of 42.195 km was established with the marathon run of the Olympic Games in London 19081 (Table 1). In recent decades, participation in a ‘marathon run’ has become increasingly attractive for millions of non-professional endurance athletes worldwide each year. Regarding the cohort of athletes participating in city-marathon events, there are only a small number of high-performance professional athletes aged between 18 and 35 years. These athletes are generally healthy, continuously medically supervised, and supported by experienced trainers. In contrast, the number of non-elite recreational marathon runners, including individuals of all age groups, is continuously rising. Indeed, the athletic and demographical characteristics of marathon runners are rapidly changing. According to a demographical analysis of these amateur athletes, the majority are middle-aged male amateur runners competing at amazing performance levels.2 For example, the winning time of the marathon run of the Olympic Games in 1936 was matched by the running time of the best M55 amateur runner of the 2012 Berlin marathon.3 These aspects are of special importance since several studies revealed that middle-aged amateur runners frequently exhibit a cardiovascular risk profile, which is typical for their age group.2,4,5 Meanwhile, it is well known and widely accepted that regular and moderate physical activity (PA) has beneficial effects on nearly all biological structures and functions of the human body, including the cardiopulmonary system (Table 2). With respect to the ideal dose of endurance PA, the Harvard Alumni Study demonstrated an optimal cardiovascular health effect by an additional energy consumption of 2000– 3000 kcal/week or 300–400 kcal/day.6,7 Even moderate * Corresponding author. Tel: +49 221 49825270, Fax: +49 221 4912906, Email: [email protected] Published on behalf of the European Society of Cardiology. All rights reserved. & The Author 2013. For permissions please email: [email protected] Downloaded from by guest on December 3, 2014 The first marathon run as an athletic event took place in the context of the Olympic Games in 1896 in Athens, Greece. Today, participation in a ‘marathon run’ has become a global phenomenon attracting young professional athletes as well as millions of mainly middle-aged amateur athletes worldwide each year. One of the main motives for these amateur marathon runners is the expectation that endurance exercise (EE) delivers profound beneficial health effects. However, with respect to the cardiovascular system, a controversial debate has emerged whether the marathon run itself is healthy or potentially harmful to the cardiovascular system, especially in middle-aged non-elite male amateur runners. In this cohort, exercise-induced increases in cardiac biomarkers—troponin and brain natriuretic peptide—and acute functional cardiac alterations have been observed and interpreted as potential cardiac damage. Furthermore, in the cohort of 40- to 65-year-old males engaged in intensive EE, a significant risk for the development of atrial fibrillation has been identified. Fortunately, recent studies demonstrated a normalization of the cardiac biomarkers and the functional alterations within a short time frame. Therefore, these alterations may be perceived as physiological myocardial reactions to the strenuous exercise and the term ‘cardiac fatigue’ has been coined. This interpretation is supported by a recent analysis of 10.9 million marathon runners demonstrating that there was no significantly increased overall risk of cardiac arrest during long-distance running races. In conclusion, intensive and long-lasting EE, e.g. running a full-distance Marathon, results in high cardiovascular strain whose clinical relevance especially for middle-aged and older athletes is unclear and remains a matter of controversy. Furthermore, there is a need for evidence-based recommendations with respect to medical screening and training strategies especially in male amateur runners over the age of 35 years engaged in regular and intensive EE. 3092 Table 1 H.-G. Predel History of the ‘Marathon’ run 490 BC First ‘Marathon’ (Marathon—Athens 40 km) Pheidippides: 3 –4 h 1896 First modern Olympics Marathon Athens, Greece [40.0 km (24.85 miles)] Spyridon Louis: 2:58:50 h 1908 Olympic Games London Great Britain: new distance: 42.195 km (26.22 miles) Johnny Hayes: 2:55:18 h 1921 International Amateur Athletic Federation (IAAF) setting 42.195 km (26.22 miles) as the standard distance 2013 Current World record for women: Paula Radcliffe: 2:15:25 h (London 2003) 2013 Current World record for men: Patrick Makau: 2:03:38 h (Berlin 2011) Table 2 training Cardiovascular benefits of regular endurance Endothelial function Coronary flow reserve Tolerance of myocardial ischaemia Figure 1 Potential association between dose of endurance sports and cardiovascular events (modified from La Gerche et al.38). emerged whether preparation for and participation in a marathon run is beneficial or harmful to the human health. Thus, the following review will critically analyse the available information on the acute and chronic effects of marathon running on the cardiovascular system focussing on middle-aged amateur marathon runners. Ventricular fibrillation thresholds Arterial blood pressure Arterial stiffness amounts of regular PA (15 min per day) are associated with significant preventive effects towards a variety of diseases, e.g. diabetes, cancer, and cardiovascular events,8 but also prolonging life expectancy.9,10 However, concerning beneficial health effects, it is difficult to define the optimal individual amount of endurance exercise (EE) as well as the upper ‘dose-limit’ on the basis of currently available studies. Nevertheless, regarding certain cardiovascular diseases, such as atrial fibrillation (AF), there are indications about potential ‘overdoses’ of EE. 11 In this context, in a case –control study, Elosua et al.12 identified a threshold of more than 1500 lifetime hours of exercising. Furthermore, Mo¨hlenkamp et al.5 observed a relatively high coronary artery calcification (CAC) burden in presumably healthy male athletes (.55 years old) who had performed at least five marathon runs during the previous 3 years. Taking these considerations into account, regular EE at moderate doses and intensities is recommended for the prevention of cardiovascular diseases by international guidelines (Figure 1).13 – 16 Acute and chronic adaptations of the cardiovascular system to marathon running Regarding these aspects and based on a series of studies in middle-aged amateur marathon runners, a controversial debate has Myocardial adaptations to endurance exercise Intensive and long-lasting EE is characterized by a significant increase in skeletal muscle oxygen demand met by a marked elevation of pulmonary oxygen uptake and transport of the oxygen-enriched blood to the working skeletal muscles. Under physiological conditions, the acute cardiopulmonary adaptation to EE encompasses increases in pulmonary ventilation, heart rate, stroke volume, and cardiac output accompanied by a moderate increase in systolic blood pressure, peripheral vasoconstriction, and vasodilatation.17 On the aerobic exercise level, these acute cardiac adaptation processes can be maintained over several hours by the endurance-trained heart. In high-performance endurance athletes, these adaptations may lead to the development of the so-called athlete’s heart, which is morphologically characterized by harmonically increased left ventricular (LV) and right ventricular (RV) volumes, increased LV wall thickness, and myocardial mass and functionally by a five- to sixfold increased cardiac output and reduced resting heart rate.17 – 19 It must be stressed, however, that the development of an athlete’s heart requires intensive endurance training.20 Whether the development of the athlete’s heart in middle-aged and older amateur endurance athletes follows the same patterns than in young endurance athletes is not entirely clear and needs further investigations.17 Potential functional and structural myocardial abnormalities in marathon runners The adaptation processes leading to the athlete’s heart must be strongly differentiated from pathological structural myocardial adaptations occurring in the context of hypertensive heart disease or Downloaded from by guest on December 3, 2014 Myocardial capillary density 3093 Cardiovascular adaptation and cardiovascular risk after the Hawaii Ironman Triathlon. Neilan et al.31 described diastolic myocardial dysfunction in predominantly middle-aged male marathon runners directly after finishing the Boston Marathon. In contrast to these acute reactions, the chronic effects are characterized by a significantly improved diastolic function in endurance trained athletes (see below). Furthermore, Neilan et al.31 observed increased troponin levels related to training volumes and interpreted these findings as myocardial injury. This interpretation sparked an intensive debate about the potential negative heath consequences of marathon running especially for the cohort of inadequately trained middle-age male runners. Recent advances in echocardiographic and magnetic resonance tomography (MRT) imaging, tissue Doppler imaging, and strain rate imaging, including tools for the quantitative assessment of segmental ventricular function, have enabled investigators to collect more detailed information concerning the functional and structural status of the marathon runners heart. With respect to LV systolic function, the findings are quite controversial. A recent meta-analyses based on 294 individuals performing EE (60–1440 min) revealed a small but significant transient reduction of LV systolic function with signs of LV strain and twist.19,32 – 34 The evaluation of diastolic functional parameters related to EE provided more consistent findings. In general, EE leads to an increased early diastolic LV filling, suggesting that diastolic function is superior in highly trained endurance athletes when compared with untrained controls. The findings of suppressed diastolic function directly after the marathon run especially in untrained non-elite amateur runners was opposed by further echocardiographic studies demonstrating a complete normalization of these functional alterations generally within 24 h after the marathon run.35,36 Therefore, such a transient exercise-induced reduction in ventricular systolic and/or diastolic function is often interpreted as physiological ‘cardiac fatigue’.30,37 Focus on the right heart Figure 2 Myocardial adaptation to intensive endurance exercise in middle-aged athletes—physiological vs. Pathological. The introduction of innovative imaging techniques allowing to investigate the right ventricle revealed signs of potential structural and functional abnormalities affecting the right ventricle occurring in young professional as well as in middle-aged amateur athletes engaged in intensive EE. In most studies, these abnormalities returned to normal within a short time frame. Especially, long-term intensive EE may cause dilation of the right atrium and ventricle also showing signs of potential myocardial scarring and/or myocardial fibrosis in prone individuals.38 – 41 However, the available data are inconsistent and at present many issues related to the effects of endurance training on the right heart remain unclear. The long-term clinical significance of these alterations requires further investigations. In summary, based on our current knowledge, the alterations of systolic and diastolic myocardial function associated with marathon running may be interpreted as a phenomenon within the physiological range at least in the majority of endurance athletes. A small subgroup of prone runners may develop functional and/or structural abnormalities with clinical significance. Further studies, using modern imaging techniques such as MRT are necessary to further clarify the effect of marathon running on myocardial structure and function and to identify athletes at risk for maladaptation. Downloaded from by guest on December 3, 2014 hypertrophic cardiomyopathy.21 Nevertheless, ever since its first description by Henschen in 1899,22 the athlete’s heart has provoked controversial discussions with respect to its health-related consequences. Although professional young athletes may also experience serious cardiovascular maladaptations and/or complications,23 – 25 the available data do not suggest that these adverse cardiovascular events are generally related to the functional and structural adaptations associated with the development of an athlete’s heart. In accordance with this view, long-term studies in professional endurance athletes26,27 do not point towards an increased cardiovascular event rate in this cohort. A recently published study on Tour de France participants even revealed a significantly lower cardiovascular event rate and a prolonged life expectancy when compared with agematched ‘ordinary’ French men.28 The situation may be different in middle-aged amateur marathon runners frequently performing on a level that was previously reserved to professional and young athletes. In this cohort, high training volumes and intensities as well as exercising during the marathon run are requiring cardiac outputs of 20– 25 L/min over periods of several hours. It is evident that this workload imposes a high degree of stress to all myocardial structures including the coronary vessels and the electrical conduction system which may potentially lead to functional and structural maladaptations and/or myocardial injury and fibrosis at least in a subgroup of prone middle-aged individuals (Figure 2).5,29 With the development of advanced and mobile Doppler echocardiography, it became possible to perform detailed non-invasive functional and structural measurements of the heart of highly endurance-trained athletes under resting and exercising conditions. Many working groups have utilized 2D and Doppler techniques before and after marathon runs in order to evaluate the morphological and functional myocardial status. Already in 1987, Douglas et al.30 described abnormalities in LV systolic and diastolic function 3094 Marathon and myocardial injury Numerous studies have reported clinically significant increases in serological markers potentially indicating myocardial damage during and/or directly after a marathon run.31,42 – 46 Recent findings, however, demonstrated that the elevated cardiac biomarkers regressed to normal values within a period of 24 –48 h and, therefore, may be the result of transient and reversible alterations of the cardiac myocytes without negative clinical consequences.35,47,48 This interpretation is supported by a recent study of Hanssen et al.49 who combined measurements of cardiac biomarkers with cardiac magnetic resonance, including late gadolinium enhancement, demonstrating an absence of detectable myocardial necrosis despite a transient increase in cardiac biomarkers. Nevertheless, taking into account the complexity of myocardial troponin and brain natriuretic peptide release, further experimental studies are warranted to elucidate the biochemical mechanisms and the clinical dignity of the increases in these cardiac biomarkers. Marathon and the vascular system platelet hyperreactivity, and increased activity of several coagulation factors. In contrast, regularly endurance trained subjects reveal a significant increase in the fibrinolysis activity. These potentially adaptive changes might offer protection against the risks of thrombotic events.58,59 The precise clinical relevance of these findings is unclear, however. In summary, functional and structural responses of the arterial vasculature and the blood clotting system to acute and chronic intensive EE are very complex and await further investigation. Coronary arteries and marathon running In recent years, evidence has accumulated that regular PA is protective with respect to coronary artery disease (CAD). A large number of studies have shown that regular PA over longer time periods is associated with a marked reduction in CAD and all-cause mortality. These protective effects were especially observed in subjects exercising in mild and moderate exercise intensities when compared with sedentary individuals. These beneficial effects are mainly mediated through improvements of risk factors for CAD, positive effects on endothelial function, autonomic balance, and the blood coagulation system.16,60,61 In contrast to these beneficial findings, Mo¨hlenkamp et al.5 found CAC scores in 108 middle-aged male marathon runners who have completed five marathon runs during previous 3 years exceeding the CAC scores of controls matched for age and Framingham risk score. The authors offered several potential explanations for these somewhat unexpected findings: a rise in vascular oxidative stress due to exercise-induced high blood flow,62 inflammatory cytokines induced by intensive EE such as marathon running.63 Potential proarrhythmic effects of marathon running There is a general consensus that elite endurance athletes commonly present several electrophysiological alterations frequently in combination with atrial and ventricular ectopy (VE), which have been perceived as functional adaptations not predisposing to serious arrhythmogenic events or sudden cardiac death (SCD).64 – 66 However, at least in a subgroup of middle-aged male endurance athletes, a significant, five-fold, increase in the prevalence of AF has been observed.67 – 69 Although clear evidence about the underlying causes and the pathophysiological mechanisms is lacking, the following hypothesis among others are being discussed: alterations in the autonomic system, fluid shifts, and electrolyte abnormalities potential chronic systemic inflammation, fibrosis of myocardial structures, and even the potential intake of illicit drugs (Figure 3). Clinically, AF associated with EE occurs usually paroxysmal and frequently at night in the beginning, often progressing to persistent AF. Despite the high prevalence, AF in athletes is perceived as abnormal and clinical relevant and requires intensive diagnostic procedures by cardiovascular and sports-medical experts including a thorough sport anamnesis.11,70 The natural course and long-term prognosis of lone AF has not been intensively documented in endurance athletes. In a Downloaded from by guest on December 3, 2014 There is sufficient evidence that long-term EE induces beneficial functional and structural adaptations of the vascular system, including positive effects on arterial vascular stiffness.50,51 In a recent meta-analysis relating to high-performance endurance athletes, Green et al.52 came to the conclusion that endurance athletes possess enlarged arteries with a decrease in arterial wall thickness. With respect to peripheral resistance arteries, middle-aged endurance trained athletes exhibited improved acetylcholine-mediated vasodilatation suggesting—according to the authors—that athletic training may retard the effects of ageing on the vasculature. On the other hand, there is limited evidence for improved arterial responsiveness to exercise-induced stimulation in athletes. In conclusion, the majority of the available data suggests that there is an improved function of peripheral resistance vessels in high-performance athletes.52 The effects of acute and chronic EE on blood pressure and heart rate are well documented, demonstrating a significant decrease in peripheral blood pressure, peripheral arterial resistance, and heart rate, which is especially pronounced in hypertensive patients.53 However, no sufficient data are available on the effects of EE on central blood pressure.54,55 In contrast, in strength-trained athletes, an increase in arterial stiffness was observed.55,56 In a recent study in 49 regularly trained middle-aged marathon runners, a slight increase of blood pressure and pulse wave velocity was observed when compared with age-matched controls. Directly after the marathon run, a significant fall in wave reflections in the presence of an unchanged pulse wave velocity was detected. The authors hypothesized that long lasting extremely vigorous and competitive exercise like marathon running may result in an inverted U-shaped relation with arterial stiffness.57 Again, further studies are warranted to clarify this issue. A further interesting field of research is the status of the blood clotting system during and after prolonged EE. Acute and intensive exercise results in a transient hypercoagulability state, especially pronounced in untrained individuals mostly due to increased thrombin generation, H.-G. Predel 3094a Cardiovascular adaptation and cardiovascular risk Figure 3 Potential mechanisms for atrial fibrillation induced by high-intensity-endurance sports. Complex ventricular ectopy and sudden cardiac death associated with endurance exercise Complex VE, including ventricular tachycardia, is also well documented in endurance-trained athletes; they typically originate from a mildly dysfunctional RV and/or the interventricular septum.42,45,74,75 The severity and clinical significance of the VEs are very variable and subject of controversial discussions. Serious VEs leading to cardiac arrest mainly result from underlying heart disease, such as cardiomyopathies or coronary abnormalities as well as inflammatory and fibrosing processes.37,74 – 76 Fortunately, SCD among marathon runners is very rare.42,44,77 In this context, Kim et al.45 investigated the incidence and outcome of cardiac arrests during marathon and half-marathon races in the USA and Canada during the period from 2000 to 2010. In the 10.9 million runners examined, 59 cases of cardiac arrests occurred in association with a marathon run. Men were significantly more likely to experience cardiac arrest and SCD than women. These findings are consistent with other reports.78,79 The event rates were significantly correlated with the age of the runners and significantly more frequent in ‘full’ marathon runs (42.195 km) than in ‘half’ marathon runs.45 Indeed, the final mile (1.6 km), representing ,5% of the whole marathon distance, accounts for almost 50% of the SCDs.42,45,80 Risk stratification in endurance athletes There is general acceptance for the need of regular medical screenings of endurance athletes. The European Society of Cardiology (ESC) has published recommendations for an athlete’s screening.76 However, there is a controversy about the detailed diagnostic procedures in order to effectively detect potential pathologic conditions predisposing to exercise-related cardiovascular events. This refers especially to the value of the electrocardiography (ECG) as a diagnostic tool. For instance, in high-performance athlete’s screening, the European guidelines differ from the US recommendations. While the European guidelines suggest a routine ECG, the US recommendations are principally limited to physical examination and anamnesis.76,81 Currently, the controversy regarding the role of a routine ECG screening remains unsettled. Considering the serious consequences of exercise-induced cardiovascular events on one side and the large number of athletes to be screened on the other side, it is strongly necessary to evaluate the diagnostic sensitivity of all components of the proposed screening procedures, including the ECG, and to develop effective diagnostic strategies that are highly sensitive in detecting athletes at increased risk for such events. In addition, the clinical value of further diagnostic tools, such as cardiac biomarkers, echocardiography, and/or advanced imaging techniques remains to be clarified. Referring to the cohort of middle-aged and older endurance athletes, the appraisal concerning the role of the ECG is different. There is general consensus that in this cohort, an exercise ECG especially in the presence of CV risk factors is recommendable.82 The European Association of Cardiovascular Prevention and Rehabilitation has recently published a comprehensive position stand for the cardiovascular evaluation of middle-aged/ senior individuals engaged in leisuretime sport activities.60 The authors state that these recommendations ‘rely on existing scientific evidence, and in the absence of such, on expert consensus’. For the screening of this very large cohort, selfassessment of the habitual PA level and of the cardiovascular risk profile based on systematic coronary risk evaluation (SCORE) are recommended.83 In individuals at increased risk and those who intend to exercise at moderate and high intensity, the medical Downloaded from by guest on December 3, 2014 prospective study with 9-year follow-up in 30 male endurance athletes with paroxysmal AF, Hoogsteen et al.71 observed that paroxysmal AF remained stable in 50% and the progression to permanent AF occurred only in 17% of the athletes. Treatment of AF in endurance-trained athletes as well as estimating the prognosis is difficult because large-scale prospective, randomized clinical trials and guidelines focussing directly on the endurance-trained athletes are lacking. Nevertheless, the current guidelines for the management of AF may be helpful and also apply to middle-aged and older endurance athletes. The therapeutic options include restriction of dose and intensity of EE, direct-current cardioversion, and ablation strategies. The value and indication of pharmacotherapy is controversial especially with respect to thromboembolic prophylaxis.72,73 3094b screening should include anamnesis including family history, physical examination, and a 12-lead resting ECG. Because the sensitivity of the resting ECG with respect to CAD is rather low, in middle-aged/older individuals, an additional exercise test with ECG is recommended in order to detect potential CAD by ST-segment depression and also to evaluate the functional capacity. Despite the absence of strong evidence for these recommendations, we strongly suggest applying these recommendations in middle aged and older endurance athletes, especially in those with increased global risk score. H.-G. Predel 5. 6. 7. 8. Conclusion 9. Acknowledgement The author would like to thank Mrs Nora Zoth, PhD for her excellent assistance in the preparation of the manuscript. Conflict of interest: none declared. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. References 1. Wilcock B. The 1908 Olympic Marathon. J Olympic Hist 2008;16:31 –47. 2. Leyk D, Erley O, Gorges W, Ridder D, Ru¨ther T, Wunderlich M, Sievert A, Essfeld D, Piekarski C, Erren T. Performance, training and lifestyle parameters of marathon runners aged 20 –80 years: results of the PACE-study. Int J Sports Med 2009;30: 360 –365. 3. www.bmw-berlin-marathon.com (6 September 2013). 4. Mo¨hlenkamp S, Schmermund A, Kro¨ger K, Kerkhoff G, Bro¨cker-Preuss M, Adams V, Hensel M, Kiefer D, Lehmann N, Moebus S, Leineweber K, Elsenbruch S, 25. 26. Downloaded from by guest on December 3, 2014 Running a full-distance Marathon is a great challenge for the entire human organism. Though there is evidence that EE delivers beneficial health effects and a significant increase in life expectancy, the strain imposed on the cardiopulmonary system is extremely high. Longterm excessive EE may cause adverse functional and morphological cardiac adaptations, especially in the continuously growing cohort of middle-aged amateur runners. These athletes who exercise at extremely high doses and intensities should, therefore, be aware that there is a potentially increased risk for cardiovascular complications. However, further investigations to identify the optimal individual dose and intensity of long-term EE are warranted. Presently, regarding the large number of middle-aged male amateur marathon runners, the recommendations of the current ESC guidelines for Physical Activity and Public Health should be observed. Thorough medical screening—including ECG—of the cardiovascular system in association with professional analysis and planning of the training is essential to avoid acute and long-term cardiovascular complications in young elite as well as in middle-aged and older endurance athletes. For the detection of CAD in the cohort of the middle-aged and older endurance athletes, an additional exercise test with ECG should be performed. Further studies are warranted to profoundly understand the acute and long-term effects of intensive EE, such as marathon running, on the cardiovascular system in order to identify individuals at risk and to develop individualized training recommendations. Finally, it seems to be prudent to advise the middle-aged or older endurance athlete to content himself with a ‘half-marathon’ performed with ‘full pleasure’. Such an approach will offer the best perspective for experiencing the fascination of marathon running and simultaneously delivering positive health effects to the cardiovascular system and the entire human body. Barkhausen J, Halle M, Hambrecht R, Siegrist J, Mann K, Budde T, Jo¨ckel KH, Erbel R. Coronary atherosclerosis and cardiovascular risk in masters male marathon runners. Rationale and design of the ‘marathon study’. Herz 2006;31:575 –585. Mo¨hlenkamp S, Lehmann N, Breuckmann F, Bro¨cker-Preuss M, Nassenstein K, Halle M, Budde T, Mann K, Barkhausen J, Heusch G, Jo¨ckel KH, Erbel R, Marathon Study Investigators, Heinz Nixdorf Recall Study Investigators. Running: the risk of coronary events: prevalence and prognostic relevance of coronary atherosclerosis in marathon runners. Eur Heart J 2008;29:1903 – 1910. Paffenbarger RS, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med 1993;328:538 –545. Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni 1978. Am J Epidemiol 1995;142:889–903. Wen CP, Wai JP, Tsai MK, Yang YC, Cheng TY, Lee MC, Chan HT, Tsao CK, Tsai SP, Wu X. Minimum amount of physical activity for reduced mortality and extended life expectancy: a prospective cohort study. Lancet 2011;378:1244 –1253. Teramoto M, Bungum TJ. Mortality and longevity of elite athletes. J Sci Med Sport 2010;13:410 –416. Chakravarty EF, Hubert HB, Lingala VB, Fries JF. Reduced disability and mortality among aging runners: a 21-year longitudinal study. Arch Intern Med 2008;168: 1638 –1646. Mont L, Elosua R, Brugada J. Endurance sport practice as a risk factor for atrial fibrillation and atrial flutter. Europace 2009;11:11–17. Elosua R, Arquer A, Mont L, Sambola A, Molina L, Garcia-Moran E, Brugada J, Marruqat J. Sport practice and the risk of lone atrial fibrillation: a case-control study. Int J Cardiol 2006;108:332 –337. Garber CE, Blissmer B, Deschenes Mr, Franklin BA, Lamonte MJ, Lee IM, Nieman DC, Swain DP. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 2011;43:1334 –1359. Graham I, Atar D, Borch-Johnsen K, Boysen G et al. European guidelines on cardiovascular disease prevention in clinical practice: full text. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur J Cardiovasc Prev Rehabil 2007;14(Suppl. 2):S1 –S113. Vanhees L, De Sutter J, Geladas N, Doyle F, Prescott E, Cornelissen V, Kouidi E, Dugmore D, Vanuzzo D, Bo¨rjesson M, Doherty P (on behalf of the writing group of the EACPR). Importance of characteristics and modalities of physical activity and exercise in defining the benefits to cardiovascular health within the general population: Recommendations from the EACPR (Part I). Eur J Prev Cardiol 2012;19: 670 –686. Vanhees L, Geladas N, Hansen D, Kouidi E, Niebauer J, Reiner Z, Cornelissen V, Adamopoulos S, Prescott E, Bo¨rjesson M, (on behalf of the writing group). Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular health in individuals with cardiovascular risk factors: recommendations from the EACPR (Part II). Eur J Prev Cardiol 2012;19:1005 – 1033. George K, Spence A, Naylor LH, Whyte GP, Green DJ. Cardiac adaptation to acute and chronic participation in endurance sports. Heart 2011;97:1999 –2004. Pelliccia A, Culasso F, Di Paolo FM, Maron BJ. Physiologic left ventricular dilatation in elite athletes. Ann Intern Med 1999;130:23 –31. Weiner RB, Baggish AL. Exercise-induced cardiac remodelling. Prog Cardiovasc Dis 2012;54:380 –386. Urhausen A, Kindermann W. Nichtinvasive Differentialdiagnostik vergro¨ßerter Herzen bei Sporttreibenden. Dtsch Z Sportmed 1987;38:290–296. Maron BJ, Maron MS. Hypertrophic cardiopmyopathy. Lancet 2013;381:242 –255. Henschen S. Skilauf und Skiwettlauf. Eine medizinische Sportstudie. Mitt Med Klin Upsala 1899:2. Chandra N, Bastiaenen R, Papadakis M, Sharma S. Sudden cardiac death in young athletes: practical challenges and diagnostic dilemmas. J Am Coll Cardiol 2013;61: 1027 –1040. Baldesberger S, Bauersfeld U, Candinas R, Seifert B, Zuber M, Ritter M, Jenni R, Oechslin E, Luthi P, Scharf C, Marti B, Attenhofer Jost CH. Sinus node disease and arrhythmias in the long-term follow-up of former professional cyclists. Eur Heart J 2008;29:71– 78. Heidbu¨chel H, Hoogsteen J, Fagard R, Vanhees L, Ector H, Willems R, Van Lierde J. High prevalence of right ventricular involvement in endurance athletes with ventricular arrhythmias. Role of an electrophysiologic study in risk stratification. Eur Heart J 2003;24:1473 –1480. Pelliccia A, Kinoshita N, Pisicchio C, Quattrini F, Di Paolo FM, Ciardo R, Di Giacinto B, Guerra E, De Blasiis E, Casasco M, Culasso F, Maron BJ. Long-term clinical consequences of intense, uninterrupted endurance training in Olympic athletes. J Am Coll Cardiol 2010;55:1619 –1625. 3097 Cardiovascular adaptation and cardiovascular risk 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. 63. 64. 65. 66. 67. 68. 69. 70. 71. 72. 73. 74. 75. resonance imaging of myocardial injury and ventricular torsion after marathon running. Clin Sci 2011;120:143 – 152. Whyte JJ, Laughlin MH. The effects of acute and chronic exercise on the vasculature. Acta Physiol 2010;199:441 –450. Schmidt-Trucksa¨ss A, Weisser B. Vascular aging, arterial hypertension and physical activity. Dtsch Med Wochenschr 2011;136:2367 –2371. Green DJ, Spence A, Rowley N, Thijssen DH, Naylor LH. Vascular adaptation in athletes: is there an ‘athlete’s artery’? Exp Physiol 2012;97:295 – 304. Cornelissen VA, Goetschalckx K, Verheyden B, Aubert AE, Arnout J, Persu A, Rademakers F, Fagard RH. Effect of endurance training on blood pressure regualtion, biomarkers and the heart in subjects at a higher age. Scand J Med Sci Sports 2011;21: 526 –534. Sharman JE, McEniery CM, Campbell RI, Coombes JS, Wilkinson IB, Cockcroft JR. The effect of exercise on large artery haemodynamics in healthy young men. Eur J Clin Invest 2005;35:738 – 744. Otsuki T, Maeda S, Iemitsu M, Saito Y, Tanimura Y, Ajisaka R, Miyauchi T. Relationship between arterial stiffness and athletic training programs in young adult men. Am J Hypertens 2007;20:967–973. Collier SR, Kanaley JA, Carhart R Jr, Frechette V, Tobin MM, Hall AK, Luckenbaugh AN, Fernhall B. Effect of 4 weeks of aerobic or resistance exercise training on arterial stiffness, blood flow and blood pressure in pre- and stage-1 hypertensives. J Hum Hypertens 2008;22:678 –686. Vlacholoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness: a systematic review and meta-analysis. J Am Coll Cardiol 2010;55:1318 –1327. Sucker C, Zotz RB, Senft B, Scharf RE, Kro¨ger K, Erbel R, Mo¨hlenkamp S. Exercise-induced haemostatic alterations are detectable by rotation thrombelastography (ROTEM): a marathon study. Clin Appl Thromb Hemost 2010;16:543 – 548. Lippi G, Maffulli N. Biological influence of physical exercise on hemostasis. Semin Thromb Hemost 2009;35:269 –276. Borjesson M, Urhausen A, Kouidi E, Dugmore D, Sharma S, Halle M, Heidbu¨chel H, Bjo¨rnstadt HH, Gielen S, Mezzani A, Corrado D, Pelliccia A, Vanhees L. Cardiovascular evaluation of middle-aged/senior individuals engaged in leisure-time sport activities: position stand from the section of exercise physiology and sports cardiology of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil 2011;18:446 –458. Lo¨llgen H, Bo¨ckenhoff A, Knapp G. Physical activity and all-cause mortality: an updated meta-analysis with different intensity categories. Int J Sports Med 2009;30: 213 –224. Kojda G, Hambrecht R. Molecular mechanisms of vascular adaptations to exercise. Physical activity as an effective antioxidant therapy? Cardiovasc Res 2005;67: 187 –197. Suzuki K, Nakaji S, Yamada M, Liu Q, Kurakake S, Okamura N, Kumae T, Umeda T, Sugawara K. Impact of a competitive marathon race on systemic cytokine and neutrophil responses. Med Sci Sports Exerc 2003;35:348 –355. Maron BJ. Hypertrophic cardiomyopathy and other causes of sudden cardiac death in young competitive athletes, with consideration for preparticipation screening and criteria for disqualification. Cardiol Clin 2007;25:399–414. Nassenstein K, Breuckmann F, Lehmann N, Schmermund A, Hunold P, Broecker-Preuss M, Sandner TA, Halle M, Mann K, Jo¨ckel KH, Heusch G, Budde T, Erbel R, Barkhausen J, Mo¨hlenkamp S. Left ventricular volumes and mass in marathon runners and their association with cardiovascular risk factors. Int J Cardiovasc Imaging 2009;25:71 –79. Goel R, Majeed F, Vogel R, Corretti MC, Weir M, Mangano C, White C, Plotnick GD, Miller M. Exercise-induced hypertension, endothelial dysfunction, and coronary artery diseases in a marathon runner. Am J Cardiol 2007;99:743 –744. Mont L. Arrhythmias and sport practice. Heart 2010;96:398 –405. Bisbal F, Mont L. Arrhythmias in the athlete. Herzschrittmacherther Elektrophysiol 2012;23:76 –81. Abdulla J, Nielsen JR. Is the risk of atrial fibrillation higher in athletes than in the general population? A systematic review and meta-analysis. Europace 2009;11: 1156 –1159. Furlanello F, Bentivegna S, Cappato R, De Ambroggi L. Arrhythmogenic effects of illicit drugs in athletes. Ital Heart J 2003;4:829 –837. Hoogsteen J, Schep G, Van Hemel NM, Van Der Wall EE. Paroxysmal atrial fibrillation in male endurance athletes. A 9-year follow up. Europace 2004;6:222 –228. Wasmer K. Mangement of atrial fibrillation around the world: a comparison of current ACCF/AHA/HRS, CCS, and ESC guidelines. Europace 2011;13:1368 –1374. Turagam MK, Velagapudi P, Kocheril AG. Atrial fibrillation in athletes. Am J Cardiol 2012;109:296 –302. Biffi A, Pelliccia A, Verdile L, Fernando F, Spataro A, Caselli S, Santini M, Maron BJ. Long-term clinical significance of frequent and complex ventricular tachyarrhythmias in trained athletes. J Am Coll Cardiol 2002;40:446 – 452. Ector J, Ganame J, Van der Merwe N, Adriaenssens B, Pison L, Willems R, Gewellig M, Heidbu¨chel H. reduced right ventricular ejection fraction in endurance athletes Downloaded from by guest on December 3, 2014 27. Clarke PM, Walter SJ, Hayen A, Mallon WJ, Heijmans J, Studdert DM. Survival of the fittest: retrospective cohort study of the longevity of Olympic medallists in the modern era. BMJ 2012;345:e8308. 28. Marijon E, Tafflet M, Antero-Jacquemin J, El Helou N, Berthelot G, Celermajer DS, Bougouin W, Combes N, Hermine O, Empana JP, Rey G, Toussaint JF, Jouven X. Mortality of French participants in the Tour de France (1947 –2012). Eur Heart J 2013. 29. Pelliccia A, Maron MS, Maron BJ. Assessment of left ventricular hypertrophy in a trained athlete: differential diagnosis of physiologic athlete’s heart from pathologic hypertrophy. Prog Cardiovasc Dis 2012;54:387 –396. ´ Toole ML, Hiller WD, Hackney K, Reichek N. Cardiac fatigue after 30. Douglas PS, O prolonged exercise. Circulation 1987;76:1206 –1213. 31. Neilan TG, Yoerger DM, Douglas PS, Marshall JE, Halpern EF, Lawlor D, Picard MH, Wood MJ. Persistent and reversible cardiac dysfunction among amateur marathon runners. Eur Heart J 2006;27:1079 –1084. 32. Middleton N, Shave R, George K, Whyte G, Hart E, Atkinson G. Left ventricular function immediately following prolonged exercise: a meta-analysis. Med Sci Sports Exerc 2006a;38:681–687. 33. Richand V, Lafitte S, Reant P, Serri K, Lafitte M, Brette S, Kerouani A, Chalabi H, Dos Santos P, Douard H, Roudaut R. An ultrasound speckle tracking (two-dimensional strain) analysis of myocardial deformation in professional soccer players compared with healthy subjects and hypertrophic cardiomyopathy. Am J Cardiol 2007;100: 128 –132. 34. Baggish AL, Yared K, Wang F, Weiner RB, Hutter AM Jr, Picard MH, Wood MJ. The impact of endurance exercise training on left ventricular systolic mechanics. Am J Physiol Heart Circ Physiol 2008;295:H1109 –H1116. 35. Knebel F, Schimke I, Scheoeckh S, Peters H, Eddicks S, Schattke S, Brechtel L, Lock J, Wernecke KD, Dreger H. Myocardial function in older male amateur marathon runners: assessment by tissue Doppler echocardiography, speckle tracking and cardiac biomarkers. J Am Soc Echocardiogr 2009;22:803 –809. 36. Scharhag J, Herrmann M, Urhausen A, Haschke M, Herrmann W, Kindermann W. Independent elevations of N-terminal pro-brain natriuretic peptide and cardiac troponins in endurance athletes after prolonged strenuous exercise. Am Heart J 2005; 150:1128 –1134. 37. Oxborough D, Birch K, Shave R, George K. ‘Exercise-induced cardiac fatigue’—a review of the echocardiographic literature. Echocardiography 2010;27:1130 – 1140. 38. La Gerche A, Burns T, Mooney DJ, Inder WJ, Taylor AJ, Bogaert J, Macisaac AI, Heidbu¨chel H, Prior DL. Exercise-induced right ventricular dysfunction and structural remodelling in endurance athletes. Eur Heart J 2012;33:998 – 1006. 39. Karlstedt E, Chelvanathan A, Da Silva M, Cleverley K, Kumar K, Bhullar N, Lytwyn M, Bohonis S, Oomah S, Nepomuceno R, Du X, Melnyk S, Zeglinski M, Ducas R, Sefidgar M, Mackenzie S, Sharma S, Kirkpatrick ID, Jassal DS. The impact of repeated marathon running on cardiovascular function in the aging population. J Cardiovasc Magn Reson 2012;14:58–64. 40. Spence AL, Carter HH, Murray CP, Oxborough D, Naylor LH, George KP, Green DJ. Magnetic resonance imaging-derived right ventricular adaptations to endurance versus resistance training. Med Sci Sports Exerc 2013;45:534 –541. 41. Scharhag J, Schneider G, Urhausen A, Rochette V, Kramann B, Kindermann W. Athlete’s heart: right and left ventricular mass and function in male endurance athletes and untrained individuals determined by magnetic resonance imaging. J Am Coll Cardiol 2002;40:1856 –1863. 42. Redelmeier DA, Greenwald JA. Competing risks of mortality with marathons: retrospective analysis. BMJ 2007;335:1275 –1277. 43. Whyte G, Stephens N, Senior R, Goerge K, Shave R, Wilson M, Sharma S. Treat the patient not the blood test: the implications of an increase in cardiac troponin after prolonged endurance exercise. Br J Sports Med 2007;41:613–615. 44. Scharhag J, George K, Shave R, Urhausen A, Kindermann W. Exercise-associated increases in cardiac biomarkers. Med Sci Sports Exerc 2008;40:1408 – 1415. 45. Kim JH, Malhotra R, Chiampas G, d´Hemecourt P, Troyanos C, Cianca J, Smith RN, Wang TJ, Roberts WO, Thompson PD, Baggish AL, Race Associated Cardiac Arrest Event Registry (RACER) Study Group. Cardiac arrest during long-distance running races. N Engl J Med 2012;366:130 –140. 46. Sheppard MN. The fittest person in the morgue? Histopathology 2012;60:381–396. 47. Scharhag J, Urhausen A, Schneider G, Herrmann M, Schumacher K, Haschke M, Krieg A, Meyer T, Herrmann W, Kindermann W. Reproducibility and clinical significance of exercise-induced increase in cardiac troponins and N-terminal pro brain natriuretic peptide (NT-proBNP) in endurance athletes. Eur J Cardiovasc Prev Rehabil 2006;13:388–397. ´ Hanlon R, Prasad S, Oxborough D, Godfrey R, Alpendurada F, Smith G, 48. Wilson M, O Wong J, Basavarajalah S, Sharma S, Nevill A, Gaze D, Whyte G. Biological markers of cardiac damage are not related to measure of cardiac systolic and diastolic function using cardiovascular magnetic resonance and echocardiography after acute bout of prolonged endurance exercise. Br J Sports Med 2011;45:780–784. 49. Hanssen H, Keithahn A, Hertel G, Drexel V, Stern H, Schuster T, Lorang D, Beer AJ, Schmidt-Trucksa¨ss A, Nickel T, Weis M, Botnar R, Schwaiger M, Halle M. Magnetic 3098 76. 77. 78. 79. 80. 81. presenting with ventricular arrhythmias: a quantitative angiographic assessment. Eur Heart J 2007;28:345 –353. Corrado D, Pelliccia A, Bjornstad HH, Vanhees L, Biffi A, Borjesson M, Panhuyzen-Goedkoop N, Deligiannis A, Solberg E, Dugmore D, Mellwig KP, Assanelli D, Delise P, van-Buren F, Anastasakis A, Heidbuchel H, Hoffmann E, Fagard R, Priori SG, Basso C, Arbustini E, Blomstrom-Lundquist C, Mc Kenna WJ, Thiene G. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: proposal for a common European protocol. Eur Heart J 2005;26:516 –524. Lee J, Patte R, Lavie CJ, Blair SN. Running and all-cause mortality risk is more better? Med Sci Sports Exerc 2012;44:990–994. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden death in young competitive athletes: analysis of 1866 deaths in the United States, 1980–2006. Circulation 2009;119:1085 – 1092. Albert CM, Mittelman MA, Chae CU, Lee IM, Hennekens CH, Manson JE. Triggering of sudden death from cardiac causes by vigorous exertion. N Engl J Med 2000;343: 1355 –1361. Jaworski CA. Medical concerns of marathons. Curr Sports Med Rep 2005;4:137 –143. Maron BJ, Thompson PD, Ackerman MJ, Balady G, Berger S, Cohen D, Dimeff R, Douglas PS, Glover DW, Hutter AM Jr, Krauss MD, Maron MS, Mitten MJ, H.-G. Predel Roberts WO, Puffer JC, American Heart Association Council on Nutrition, Physical Activity and Metabolism. Recommendations and considerations related to preparticipation screening for cardiovascular abnormalities in competitive athletes: 2007 update: a scientific statement from the American Heart Association Council on Nutrition, Physical Activity, and Metabolism: endorsed by the American College of Cardiology Foundation. Circulation 2007;115:1643 – 1645. 82. Maron BJ, Araujo CG, Thompson PD, Fletcher GF, de Luna AB, Fleg JL, Pelliccia A, Balady GJ, Furlanello F, Van Camp SP, Elosua R, Chaitman BR, Bazzarre TL, World Heart Federation; International Federation of Sports Medicine; American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention. Recommendations for preparticipation screening and the assessment of cardiovascular disease in masters athletes: an advisory for healthcare professionals from the working groups of the World Heart Federation, the International Federation of Sports Medicine, and the American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation 2001;103:327–334. 83. Conroy RM, Pyo¨ra¨la¨ K, Fitzgerlad AP, Sans S, Menotti A, De Backer G, De Bacquer D, Ducimetie`re P, Jousilahti P, Keil U, Njolstad I, Oganov RG, Thomsen T, Tunstall-Pedoe H, Tverdal A, Wedel H, Whincup P, Wilhelmsen L, Graham IM, on behalf of the SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003;24:987–1003. Downloaded from by guest on December 3, 2014
© Copyright 2026