Chapter 5 - Dissertations
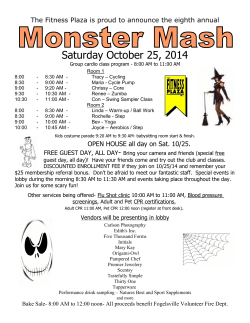
Chapter 5 PET Imaging in thyroid carcinoma Hans H.G. Verbeek, Ha T.H. Phan, Adrienne H. Brouwers Klaas P. Koopmans, Thera P. Links Methods of Cancer Diagnosis, Therapy and Prognosis. Vol. 7. Editor: M.A. Hayat. Springer Sience + Business Media BV 2010. Chapter 5 Introduction Thyroid cancer is the most common endocrine malignancy. It is divided in several types with papillary, folliculary, and Hürthecell cancer (also called differentiated thyroid cancer) originating from the follicular epithelial cells as the most common types (>90%). Other types are medullary thyroid carcinoma (a neuroendocrine tumour originating from the calcitonin producing C-cells) (3%-10%) and anaplastic carcinoma (often a dedifferentiated form of the other types) (2%-10%).1 There is a different treatment for each of these types of thyroid cancer. In differentiated thyroid cancer the initial therapy is total thyroidectomy with or without lymph node dissection, followed by adjuvant radioactive iodine therapy. Radioactive iodine therapy with 131 I can be used successfully due to the active uptake of iodine in tumour cells of thyroid origin. However, this property can be lost during dedifferentiation, which limits the use of this therapy in anaplastic carcinoma. Medullary thyroid tumour cells show no iodine uptake at all and curative options are therefore mainly limited to surgical resection of primary tumour and metastases.2 The prognosis for differentiated thyroid cancer is good, with an average 10-years survival between 80% and 95%. However, these tumours can dedifferentiate, which results in limited therapeutic options, leading to a much poorer prognosis with a 5-years survival of 30%. Medullary thyroid carcinoma has a 10-years survival of 20%-70%, and for anaplastic thyroid carcinoma the median survival is 2-6 months.3-5 Imaging is especially important in determining the right therapeutic approach for patients with differentiated and medullary thyroid carcinoma. Different imaging techniques are available such as computed tomography (CT), magnetic resonance imaging (MRI), conventional nuclear scintigraphy, positron emission tomography (PET), etc.. While MRI and CT are imaging techniques which show morphologic structures, PET imaging depicts pathophysiological processes and is described as functional imaging. The value of PET imaging is emerging mainly in the follow-up of thyroid cancer. Several PET imaging techniques are available for different types of thyroid cancer and these techniques and their applications are discussed in this chapter. 74 PET imaging in thyroid carcinoma Positron Emission Tomography Positron emission tomography imaging is a technique used in nuclear medicine which is based on the use of positron emitting isotopes in specific molecules which are relevant for specific metabolic pathways. The PET technique yields a high resolution and the capability to quantify the amount of radioactivity measured in a specific region. Positrons, emitted by an unstable atom nucleus, are the antiparticles of electrons and have the same mass, but an opposite charge. Positrons are not detected by a PET camera, but photons, which are formed when a positron fuses with an electron, are detected. This means that the positron binds with an electron to form a positronium which annihilates. In this annihilation process all the mass is converted into energy by which two photons are formed. These photons, always carrying an energy of 511 keV, are emitted in opposite directions under an angle of 180º and are detected by the PET camera.6 Radioisotopes used in PET imaging usually have a short half live, such as carbon-11(11C; half-life (T½) 20 min), nitrogen-13 (13N; T½ 10 min), oxygen-15(15O; T½ 2 min) and fluorin18(18F; T½ 110 min). Positron emitting radionuclides are in most cases produced by bombarding the target material with highly accelerated particles (deuterons or protons) using a cyclotron and inducing a nuclear reaction. Centres which use isotopes with a very short halflife, such as 15O, 13N, and 11C, need to have an on-site cyclotron. Other longer living isotopes can be made elsewhere and then transported to the PET imaging facility.7 A cyclotron is a type of particle accelerator which accelerates charged particles using a high-frequency, alternating voltage. A perpendicular magnetic field causes the particles to assume a circular orbit so that they reencounter the accelerating voltage many times. When the particles are accelerated fast enough they are bombarded on to specific atoms and radionuclides are formed. These radionuclides are trapped and transported to the laboratory where they can be processed for clinical use. The resulting end-products are called radiotracers. The most commonly used tracers are precursors for metabolic pathways, although many other tracer types exist. After preparation and careful quality monitoring, tracers can be injected. The imaging device used is the PET camera. Most PET cameras consist of a ring of special detectors which are well suited for the detection of 511 keV gamma rays. Software registers only simultaneously entering photonpairs on different detectors. This is called coincidence detection. Coincidence detection removes the need for a lead collimator such that the 75 Chapter 5 sensitivity of the PET imaging system is much higher than for the conventional Anger camera that is used in planar nuclear imaging or single photon emission computed tomography (SPECT). Both the specific block detector structure and the absence of a collimator contribute to a higher resolution as compared with SPECT. Another advantage of PET is that the amount of radioactivity injected in the body can be quantitatively determined. PET is a non-invasive, sensitive imaging tool for depicting of molecular and biochemical processes without changing its physical properties.6 In contrast to radiologic imaging which shows the morphologic structures, nuclear medicine techniques depict pathophysiological processes and are also described as functional imaging methods. The imaging with PET is considered to be an useful diagnostic tool for the detection of cancer, brain diseases, and coronary artery diseases. Combined PET/CT The combination of PET and CT scanning is a new promising imaging technique. The integrated PET/CT scanner allows acquisition of CT and PET images in one session. The combination of morphologic and functional imaging leads to more precise anatomical localization of tumour lesions. The localization of tumour foci is important for initiating the appropriate treatment such as surgery. Especially in patients with a negative radioiodine scan where surgery is the only therapeutic option, the integrated PET/CT scan can be helpful in guiding therapeutic management. 18 Fluorine-fluorodeoxyglucose (18F-FDG) PET Mechanism Fluorodeoxyglucose (FDG) is a glucose analogue and is used as a precursor for glucose metabolism. In both benign and malignant tissue it enters the cell by the same glucose transporters. However, the need for glucose in malignant cells is strongly increased because these cells have a considerably less efficient energy metabolism.8 For example, the energy production per molecule of glucose in malignant cells is decreased because anaerobic glycolysis is strongly increased instead of the much more efficient energy production from the citric acid cycle. This inefficient use of glucose is the basis for the preferential uptake of glucose or an offered glucose analogue as FDG in malignant cells. 76 PET imaging in thyroid carcinoma In the cell FDG is phosphorylated by a hexokinase enzyme into FDG-6 phosphate which, in contrast to glucose-6-phospate, cannot be further metabolized. Therefore, the FDG-6phosphate does not leave the cell and becomes trapped intracellulary. The final quantity of FDG-6-phosphate is proportional to the glycolytic rate of the cell. Besides the increased glycolysis, it has been demonstrated that in malignant cells levels of transmembrane glucose transporters (e.g., the GLUT-1 transporter) and possibly some hexokinase isoenzymes are also increased, also resulting in increased FDG uptake.9 However, in all metabolically active tissues, such as brain cells, active muscles, and activated macrophages, increased glucose metabolism leads to an increased FDG uptake. 18FFDG PET is, therefore, a marker for glucose metabolism in general. In most normal tissues (e.g., liver, kidney, intestine, muscle and some tumour cells) the level of phosphate activity is variable; nevertheless, FDG-6-phospate accumulation is lower than in malignant tissues. In addition, some benign tissues require more glucose.10,11 So, the uptake mechanism of FDG with irreversible trapping in malignant tissue is ideal for PET imaging and has been applied widely in oncology. However, it is important to make a correct interpretation of these PET images, for non-malignant tissue also has FDG uptake. Scan method Uptake of 18 F-FDG occurs rapidly after administration and the amount taken up increases with time. The most applied imaging moment is 60-90 min after tracer administration. The reason is that the excretion of 18F-FDG via the kidneys reduces 18F-FDG in the blood, which causes clearance of ‘background’ uptake and the decay of fluorin-18 (T½ 110 min). Generally the patient preparation consists of an 18 F-FDG injection in a fasting condition and after oral prehydration. The injected dose varies between 2-8 MBq/kg. Clinical application Thyroid nodules The value of 18F-FDG PET in the distinction between malignant and benign thyroid nodules before surgery is unclear. Several studies reported that 18 F-FDG PET is useful in the preoperative evaluation of cytologicaly inconclusive nodules with a high negative predictive value.12-14 De Geus-Oei et al. observed that the probability for thyroid cancer increased from 14% (pre-PET) to 32% (post-PET) in case the nodule was positive on 18F-FDG PET.12 In this study 18F-FDG PET could reduce the number of futile hemithyroidectomies by 66%. 77 Chapter 5 A. 18F-FDG PET B. CT-lung C. 18F-FDG PET/CT Figure 1 These are the images of a 68-year old male known with follicular thyroid cancer. This patient showed 131 increased serum Tg level (14 ng/ml) suspected for recurrent or metastatic disease. Blind treatment with I 18 was given followed by a post-treatment whole body scan (WBS) after 10 days which was negative. F-FDG PET (A) showed a focal lesion in the lower lobe of the left lung (arrow), confirmed by CT (B, arrow). Picture C 18 showed the fusion image of F-FDG PET and CT for the lesion in the left lung (arrow). However, recent studies by Kim et al. and Bogsrud et al., demonstrated that 18F-FDG PET is not helpful in differentiating between malignant and benign nodules, and therefore has only limited value in preoperative evaluation of indeterminate thyroid nodules.15,16 So, conflicting results are reported on the usefulness of 18 F-FDG PET in the prediction of malignancy in thyroid nodules in case of inconclusive cytology, and therefore further research is needed. Meanwhile histopathological examination remains the gold standard. Differentiated thyroid cancer (DTC): follow-up More information is available regarding the value of 18F-FDG PET in the follow-up of thyroid cancer such as the detection of recurrences or metastases, especially in patients with a negative radioiodine scan or in patients who has lost the ability to accumulate iodine. A 78 PET imaging in thyroid carcinoma complementary uptake of 18 F-FDG and radioiodine can be present, which is known as the ‘flip-flop’ phenomenon and was first described by Joensuu and Ahonen.17 This phenomenon might be explained by the degree of tissue differentiation. Well differentiated thyroid tissue has the capability to take up iodine but is metabolically inactive while less differentiated thyroid cancer tissue loses its capability to trap iodine and becomes metabolically more active. This makes 18 F-FDG PET scanning the method of choice for the detection of 131 I negative metastases of differentiated thyroid carcinoma.18 Performance of 18F-FDG PET during thyrotropin (TSH) stimulation improves the results in comparison to the scanning during the euthyroid state (during thyroxin treatment) as was shown by van Tol et al..19 In vitro studies have shown a stimulating effect of TSH on Glut 1 expression and glucose transport.20,21 This increase in glucose carriers results in a higher uptake of glucose and also 18F-FDG in thyroid cancer cells, which improves the result of the PET-scan. Stimulation with exogenous TSH (recombinant human(rh) TSH) also increases 18 F-FDG uptake by differentiated thyroid cancer, and therefore more lesions can be detected and tumour/background contrast is enhanced.22,23 The influence of rhTSH on the background is not well-known, but there is evidence that rhTSH increases 18F-FDG uptake in the tumour lesion itself. Several studies have been performed to assess the value of 18 F-FDG PET imaging in the follow up of thyroid cancer. Hooft et al. performed a meta-analysis of studies that investigated the role of 18 F-FDG PET in patients with thyroid cancer after negative radioiodine scintigraphy and elevated serum thyroglobulin.24 The diagnostic accuracy of these studies was assessed. Observed sensitivity and specificity in these studies were ranging from 70%-95% and 77%-100%, respectively. Furthermore, they observed that there are methodological problems in these studies such as small sample size, validity of reference tests, and short follow-up. Nonetheless, 18 F-FDG PET is now considered a valuable diagnostic imaging tool in the follow-up of 131I-negative patients for the detection of recurrences or metastases. However, it is not known whether PET is superior to bone scintigraphy in the detection of bone metastases in thyroid cancer. Comparative studies of bone scans and lacking. In a retrospective study, 24 patients had undergone both 18 18 F-FDG PET are F-FDG PET and bone scans within six months because of suspected bone metastases.25 This study shows that bone scintigraphy is still valuable in differentiated thyroid cancer, as it was found that 38% of bone metastases could be missed on 18F-FDG PET. Further prospective studies in a higher number of patients are required to define the exact role of bone scan and 18 F-FDG PET in the detection of bone metastases in patients with differentiated thyroid cancer (DTC). 79 Chapter 5 Combined or integrated 18F-FDG PET/CT in patients with negative 131I scans and elevated thyroglobulin (Tg) showed that the diagnostic accuracy can be improved compared to 18 F- FDG PET or CT alone. The combination of these imaging techniques has also led to a change in patient management and therapy, e.g., extension of surgery by providing precise anatomical localization of the recurrent or metastatic disease.26 Medullary thyroid cancer (MTC) The detection of recurrence or metastases in MTC is difficult and there is no single method sensitive enough to reveal all MTC recurrences or metastases. In comparison with the calcitonin tumour marker nearly all imaging modalities (Ultrasonography, CT, MRI, and scintigraphy) have limited sensitivities. The clinical role of 18F-FDG PET in the diagnosis and staging of recurrent and metastatic MTC seems promising.27 The sensitivity and specificity of 18F-FDG PET ranges between 73%-88% and 76%-80%, respectively. In a study by de Groot et al., 18 F-FDG PET was performed in patients with elevated serum tumour markers after total thyroidectomy.28 Compared with imaging(lesion based sensitivity: morphological imaging (87%), 18 41%), 99m Tc(V)DMSA 111 scintigraphy In-octreotide (57%) and F-FDG PET (96%) was superior. However, morphological imaging will always be needed because 18 F-FDG PET only yields functional data and no morphological information, which is necessary to assess resectability. The combination of 18F-FDG PET/CT can have a useful role in medullary thyroid cancer. Because surgery only can cure the disease, precise anatomical localization and the extent of the recurrent or metastatic disease is mandatory. However, little data and case reports have shown an increased diagnostic accuracy so further studies are needed.27 18 Fluorine-dihydroxyphenylalanine (18F-DOPA) Mechanism The mechanism responsible for uptake of 18 Fluorine-dihydroxyphenylalanine (18F-DOPA) in medullary thyroid carcinoma is probably the strongly upregulated transmembrane transport of amino acids via the large amino acid transporters in medullary thyroid carcinoma cells. It is not yet clear whether the increased uptake of 18F-DOPA PET is the result of the increased transporter capabilities or the increased metabolic activity of the catecholamine pathway. 80 PET imaging in thyroid carcinoma After transmembrane transport, 18 F-DOPA is intracytoplasmatically converted into dopamine by the enzyme aromatic acid decarboxylase (AADC). The formed 18F-dopamine is transported into secretory vesicles via the vesicular mono aminoacid transporters (VMAT) in which it can be further metabolized to 18F-noradrenalin and 18F-adrenalin.29 Although the 18F atom influences the metabolism of 18F-DOPA there is no or little effect on the transport into the intracellular environment. In the kidneys, 18F-DOPA is rapidly converted into 18F-dopamine which is than excreted actively in urine. This conversion can be inhibited by oral administration of carbidopa prior to tracer administration.30 Carbidopa also lowers the physiological uptake of 18F-DOPA in the pancreas, but it is yet unknown which mechanism is responsible for this decrease in pancreatic uptake. The reduction in renal and urinary activity leads to a better image quality in the surroundings of the urinary system. Also, the reduced uptake in the pancreas makes the identification of lesions in the pancreatic region easier. It can be speculated that by reducing the excretion of 18 F-DOPA, more 18 F-DOPA is available for neuroendocrine tumour lesions; thereby, increasing the tumour to background ratio, leading to a better discrimination of neuroendocrine lesions. Scan method In most centres, patients are prepared with oral administration of carbidopa, either in a fixed dose or in a dose calibrated to body weight. Patients are scanned in a fasting condition for 4-6 h. In most centres a whole body study will be performed ranging from the skull to the upper femora. The average injected dose is 200 MBq, the radiation burden ~ 4 mSv.30 Attenuation correction is applied, either by using a CT in a PET-CT machine or by using camera-specific attenuation protocols. Clinical application Medullary thyroid cancer Although 18 F-DOPA PET is not yet in widespread use, it is a promising new functional imaging procedure for imaging neuroendocrine tumours. More and more centres gain access to this tracer either via on-site production or production elsewhere. Hoegerle et al. were the first to describe the use of 18 F-DOPA PET in medullary thyroid cancer.31 In this study DOPA PET was compared with 18 F-FDG PET, SRS, and CT/MRI. A high precision of 18 F- 18 F- DOPA PET was observed in the diagnosis of lymph node metastases (sensitivity 88%), while 81 Chapter 5 organ metastases were better detected with conventional imaging (sensitivity 13%). In the recently published study by Koopmans et al. diagnostic accuracy was assessed for 18F-DOPA PET in patients with carcinoid tumours which are, like medullary thyroid carcinoma, neuroendocrine tumors.32 Compared to conventional somotostatine receptor scintigraphy (SRS) they showed improved sensitivity of 18F-DOPA PET in staging and identify carcinoid tumours. A. 18F-FDG PET B. 18F-DOPA PET Figure 2 These are the images of a patient known with medullary thyroid cancer. In this patient 18F-FDG PET 18 18 (A) and F-DOPA PET (B) were performed. The F-DOPA PET (B) showed multiple lesions in the liver and 18 several lesions in the spinal column(arrows) while the F-FDG PET showed hardly any lesions. The value of 18 F-DOPA PET for the detection of recurrent or residual disease in 21 patients with postsurgically elevated calcitonin or CEA was assessed by Koopmans et al..33 They compared 18F-DOPA PET with 18F-FDG PET, 99mT(V)DMSA, and CT/MRI. 18F-DOPA PET was superior to conventional imaging for the detection of MTC on patient (sensitivity 87%) and regional (89%) level. On lesional level 18 F-DOPA PET (sensitivity 71%) was equal to morphological imaging (64%) but superior to 18F-FDG PET (30%) and 99mT(V)DMSA (19%). In the recent study by Beuthien-Baumann et al., specific than 18 18 18 F-DOPA-PET also seems to be more F-FDG PET for the detection of metastases of MTC.34 Thus, compared with F-FDG PET and conventional imaging techniques, 18F-DOPA PET provides better results in the imaging of medullary thyroid cancer. However, it is still unclear if this improved imaging results in different therapeutic approaches, and so further research is needed. 82 PET imaging in thyroid carcinoma 11 C-Methionine (MET) PET Mechanism Proteins play an important role in virtually all biological processes. Proteins are built from a set of 20 amino acids. Amino acid transport across the cell membranes into the cells occurs primarily via carrier-mediated processes. Amino acid transport is generally increased in malignant transformation.35-37 This increased protein metabolism in cancer cells is important for metabolic tumour imaging, for which radiolabeled amino acids can be applied. These amino acid tracers could help in imaging areas where 18 F-FDG is limited such as the interference of high (physiologic) 18F-FDG uptake in the brain. Another reason is that amino acid imaging is less influenced by inflammatory disease. The most frequently used radiolabeled amino acid is L-[methyl-11C]-methionine. Normal biodistribution of radiolabeled methionine occurs in the pancreas, liver, spleen, kidney, and salivary glands. Scan method 11 C-MET PET scanning can be performed 10 to 20 min after intravenous injection of a fixed dose or a dose calibrated on body weight (suggested range is 70 MBq to 1100 MBq), in a fasting condition for 2-6 h. Images are corrected, either by using a CT in a PET/CT machine or by using camera-specific attenuation protocols. Clinical application Differentiated thyroid cancer The need for new tracers and improvement of diagnostic tools in thyroid cancer is growing. So far, no data on the application of methionine (MET) PET in thyroid cancer are available. The general feasibility of amino acid imaging in many tumour types has been sufficiently shown.37 It is imaginable that thyroid cancer could sufficiently concentrate amino acids due to its metabolically inert nature and high protein synthesis (e.g., thyroglobulin). In a feasibility study by Phan et al., 11C-MET PET has been compared with 18F-FDG PET in the detection of recurrent or metastatic disease in 20 patients with negative 131I scans and elevated Tg.38 Six of the 20 patients showed uptake on both PET scans, but the abnormalities were more 18F-FDGavid and more extensive on the 18F-FDG PET in 3 patients. In four of the 20 patients uptake 83 Chapter 5 was only observed on the 11 C-MET PET; however, no anatomical localization could be confirmed. Presently, the significance of the MET uptake in these four patients is unclear, so the clinical value of 11 C-MET PET in the detection of recurrent DTC disease still has to be proven in the (long-term) follow-up. A. 11C-MET PET B. 18F-FDG PET Figure 3 These are the images of a 68-y old female known with papillary thyroid cancer. This patient had unreliable Tg due to the presence of Tg antibodies (which were increasing in the course of the follow-up). The 131 post-treatment I whole body scan (WBS) was negative. Due to suspicion of dedifferentiated, metastatic 11 18 11 disease C-MET PET (A) and F-FDG PET (B) were performed. C-MET PET (A) showed lesions in the 11 18 mediastinum with slightly to moderate C-MET uptake. F-FDG PET (B) also showed multiple lesions in the 18 mediastinum, but the lesions showed clearly higher F-FDG uptake and the abnormalities were more extensive. 124 Iodine-PET Mechanism Iodine-124 is a positron emitting isotope, which is suitable for PET imaging, with a half-life of 4.2 days.39 This isotope has been used for dosimetric purposes or thyroid volume measurements.40 While the radioisotopes 123 I and especially diagnosis and treatment of many thyroid disorders, 124 131 I are used on a wide scale in I has received little attention. Chemically identical to nonradioactive iodine, this radioisotope allows thyroid cancer imaging with the high resolution PET technique.39,40 84 PET imaging in thyroid carcinoma Scan method The 124I -PET scan can be obtained 24 h to 6 days after administration of 74-100 MBq of 124I. A whole body PET scan (from the upper thigh up until the top of the skull) can be performed in 2D or 3D mode, using standard energy window setting of 350-650 keV (or energy window setting 425-650 keV or 460-562 keV in case of the presence of high amounts of 131I.41 Clinical application Differentiated thyroid cancer Accumulation of iodine is a highly specific characteristic for differentiated thyroid cancer (DTC) cells. In patients with increasing or recurrent detectable Tg a blind treatment (meaning after a negative diagnostic 131I scan) with high dose 131I followed by a post-treatment 131I scan is used as a diagnostic tool. However, this strategy with (unnecessary) high radiation exposure must be taken into account in patients without 131I uptake in their metastases. Besides the high radiation exposure, there is a high TSH level which potentially stimulates thyroid cancer cell growth. Based on the higher spatial resolution, 124 I-PET is potentially able to detect recurrent 131 disease in DTC with a higher sensitivity than (diagnostic) sensitivity and the possibility to combine the 124 I scans. With this higher I-PET scan with morphologic imaging, such as CT data, an appropriate therapeutic decision in terms of surgery and/or additional high dose 131 I can be made. 124 I-PET imaging might, therefore, become the diagnostic tool of choice in the follow-up of DTC. In the study by Freudenberg et al., compared with the high dose 131 respectively. So, these I-PET (/CT) modalities were I-WBS in 12 patients with DTC.42 They showed an overall lesion detectability of 87 %, 83%, and 100% for 124 124 124 I, 131 I-WBS and combined 124 I-PET/CT I-PET (/CT) modalities are promising diagnostic tools and are suitable alternative to the high dose 131I-WBS in the follow-up of DTC patients. In a prospective, feasibility study by Phan et al., 20 patients with advanced DTC (T4, extranodal tumour growth, distant metastasis) underwent a low-dose diagnostic 124 I PET scan, and a high-dose (posttreatment) the 124 I-PET images. diagnostic 131 124 131 I scan.43 The 131 131 I scan, a I images were compared to I-PET proved to be a superior diagnostic tool as compared to low dose I scans, and showed comparable findings with the post-treatment 131 I-WBS which was in agreement with the study by Freudenberg et al. and Abdul Fatah et al..42,44 Therefore, 124 I-PET could be used as a diagnostic tool in the follow-up of patients with DTC for the favourable radiation exposure burden compared to the high dose diagnostic 131 I-WBS 85 Chapter 5 and the superior diagnostic accuracy compared to low dose diagnostic 131 I-WBS and the fusion possibility with CT which improves clinical decision making. A. Post-treatment 131I-WBS B. 124I-PET C. 18F-FDG PET Figure 4 These are the images of a 68-year old male known with follicular thyroid cancer. This patient showed 131 increased serum Tg level (14 ng/ml) suspected for recurrent or metastatic disease. Blind treatment with I 124 was given followed by a post-treatment whole body scan (WBS) after 10 days (A), which was negative. The IPET (B) was also negative, besides physiological uptake in the salivary glands, oesophagus, gastro-intestinal 18 tract, kidney and bladder. F-FDG PET (C) showed a focal lesion in the lower lobe of the left lung (arrow), 18 confirmed by CT. This complementary uptake of radioiodine and F-FDG is known as the flip-flop phenomenon. Conclusion This chapter on PET imaging in thyroid cancer gives an overview of the different PET techniques available in thyroid cancer. PET imaging is based on two principles: the ability of unstable atom nucleus to emit positrons and the labelling of organic molecules, which are used in specific metabolic pathways. 86 PET imaging in thyroid carcinoma For differentiated thyroid cancer the most frequently used PET technique is 18F-FDG PET imaging, which is based on the use of a glucose analogue. Although its application in the preoperative assessment of thyroid nodules is still unclear, it is considered an useful tool in the follow up of differentiated thyroid cancer. The use of PET/CT scanning which combines functional imaging with morphological imaging is promising, providing more accurate localization of tumour sites, which is important for further treatment. Other PET radiotracers have been developed: the clinical value of amino acid tumour imaging with 11 C-MET PET is unclear and still has to be proven in the follow-up of differentiated thyroid cancer. Another relative new PET imaging technique is the iodine isotope 124 I. Compared with the high dose diagnostic 131 I whole body scan, 124 I-PET showed similar findings and can therefore be used as a diagnostic tool in the follow-up of differentiated thyroid cancer. For the follow-up of medullary thyroid cancer imaging technique. However, 18 18 F-FDG PET is also the most employed F-DOPA PET, which is based on a precursor of dopamine, seems to be superior compared to 18F-FDG PET in the follow up of medullary thyroid cancer. A potential new tracer is 11 C-5-HTP, which is based on a precursor of serotonin and already has been applied in neuroendocrine tumours. The value of this technique has to be further assessed in medullary thyroid cancer. The need for new tracers and advanced PET imaging to improve the diagnostic sensitivities and accuracy in detection, staging, and follow-up of thyroid cancer patients is growing. Knowledge of the pathogenesis, the molecular characteristics and the behaviour of the tumour cell is crucial for developing of specific tracers and techniques, e.g., radiolabeled Tg, (rh) TSH. Although new tracers are developed and applied in patients, little data are available on the changes in therapeutic management these new PET-techniques give. While PET-imaging is still in development, more research is needed to assess the effects on therapy of these new developments. In conclusion, PET imaging is a useful diagnostic tool in thyroid cancer and new promising techniques are developed which could further improve the diagnostic accuracy and therapeutic approaches. 87 Chapter 5 References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 88 Schlumberger M, Pacini F. Epidemiology. In: Anonymous Thyroid Tumours. Paris: Editions nucleon; 2003. p 51-60. Sherman SI, Angelos P, Ball DW, et al. Thyroid carcinoma. J Natl Compr Canc Netw 2005;3:404-457. Modigliani E, Cohen R, Campos JM, et al. Prognostic factors for survival and for biochemical cure in medullary thyroid carcinoma: results in 899 patients. The GETC Study Group. Groupe d'etude des tumeurs a calcitonine. Clin Endocrinol (Oxf) 1998;48:265-273. Tubiana M, Haddad E, Schlumberger M, Hill C, Rougier P, Sarrazin D. External radiotherapy in thyroid cancers. Cancer 1985;55:2062-2071. Venkatesh YS, Ordonez NG, Schultz PN, Hickey RC, Goepfert H, Samaan NA. Anaplastic carcinoma of the thyroid. A clinicopathologic study of 121 cases. Cancer 1990;66:321-330. Bailey DL, Karp JS, Surti S. Physics and instrumentation in PET. In: PE Valk, DL Bailey, DW Townsend, MN Maisey, editors. Positron Emission Tomography; Basic Sience and Clinical Practice. London: Springer; 2003. Mason NS, Mathis CA. Radiohalogens for PET imaging. In: PE Valk, DL Bailey, DW Townsend, MN Maisey, editors. Positron emission tomography basic science and clinical practice. London: Springer; 2003. Warburg OH, Dickens F, Kaiser Wilhelm If. The Metabolism of Tumours: Investigations from the Kaiser Wilhelm Institute for Biology, Berlin-Dahlem. : Richard R. Smith; 1931. Brown RS, Goodman TM, Zasadny KR, Greenson JK, Wahl RL. Expression of hexokinase II and Glut-1 in untreated human breast cancer. Nucl Med Biol 2002;29:443-453. Kubota R, Yamada S, Kubota K, Ishiwata K, Tamahashi N, Ido T. Intratumoral distribution of fluorine18-fluorodeoxyglucose in vivo: high accumulation in macrophages and granulation tissues studied by microautoradiography. J Nucl Med 1992;33:1972-1980. Strauss LG. Fluorine-18 deoxyglucose and false-positive results: a major problem in the diagnostics of oncological patients. Eur J Nucl Med 1996;23:1409-1415. de Geus-Oei LF, Pieters GF, Bonenkamp JJ, et al. 18F-FDG PET reduces unnecessary hemithyroidectomies for thyroid nodules with inconclusive cytologic results. J Nucl Med 2006;47:770775. Mitchell JC, Grant F, Evenson AR, Parker JA, Hasselgren PO, Parangi S. Preoperative evaluation of thyroid nodules with 18FDG-PET/CT. Surgery 2005;138:1166-74; discussion 1174-5. Kresnik E, Gallowitsch HJ, Mikosch P, et al. Fluorine-18-fluorodeoxyglucose positron emission tomography in the preoperative assessment of thyroid nodules in an endemic goiter area. Surgery 2003;133:294-299. Kim JM, Ryu JS, Kim TY, et al. 18F-fluorodeoxyglucose positron emission tomography does not predict malignancy in thyroid nodules cytologically diagnosed as follicular neoplasm. J Clin Endocrinol Metab 2007;92:1630-1634. Bogsrud TV, Karantanis D, Nathan MA, et al. The value of quantifying 18F-FDG uptake in thyroid nodules found incidentally on whole-body PET-CT. Nucl Med Commun 2007;28:373-381. Joensuu H, Ahonen A. Imaging of metastases of thyroid carcinoma with fluorine-18 fluorodeoxyglucose. J Nucl Med 1987;28:910-914. Schluter B, Bohuslavizki KH, Beyer W, Plotkin M, Buchert R, Clausen M. Impact of FDG PET on patients with differentiated thyroid cancer who present with elevated thyroglobulin and negative 131I scan. J Nucl Med 2001;42:71-76. van Tol KM, Jager PL, Piers DA, et al. Better yield of (18)fluorodeoxyglucose-positron emission tomography in patients with metastatic differentiated thyroid carcinoma during thyrotropin stimulation. Thyroid 2002;12:381-387. Filetti S, Damante G, Foti D. Thyrotropin stimulates glucose transport in cultured rat thyroid cells. Endocrinology 1987;120:2576-2581. Hosaka Y, Tawata M, Kurihara A, Ohtaka M, Endo T, Onaya T. The regulation of two distinct glucose transporter (GLUT1 and GLUT4) gene expressions in cultured rat thyroid cells by thyrotropin. Endocrinology 1992;131:159-165. Petrich T, Borner AR, Otto D, Hofmann M, Knapp WH. Influence of rhTSH on [(18)F]fluorodeoxyglucose uptake by differentiated thyroid carcinoma. Eur J Nucl Med Mol Imaging 2002;29:641-647. PET imaging in thyroid carcinoma 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. Chin BB, Patel P, Cohade C, Ewertz M, Wahl R, Ladenson P. Recombinant human thyrotropin stimulation of fluoro-D-glucose positron emission tomography uptake in well-differentiated thyroid carcinoma. J Clin Endocrinol Metab 2004;89:91-95. Hooft L, Hoekstra OS, Deville W, et al. Diagnostic accuracy of 18F-fluorodeoxyglucose positron emission tomography in the follow-up of papillary or follicular thyroid cancer. J Clin Endocrinol Metab 2001;86:3779-3786. Phan HT, Jager PL, Plukker JT, Wolffenbuttel BH, Dierckx RA, Links TP. Detection of bone metastases in thyroid cancer patients: bone scintigraphy or 18F-FDG PET? Nucl Med Commun 2007;28:597-602. Shammas A, Degirmenci B, Mountz JM, et al. 18F-FDG PET/CT in patients with suspected recurrent or metastatic well-differentiated thyroid cancer. J Nucl Med 2007;48:221-226. Nanni C, Rubello D, Fanti S, et al. Role of 18F-FDG-PET and PET/CT imaging in thyroid cancer. Biomed Pharmacother 2006;60:409-413. de Groot JW, Links TP, Jager PL, Kahraman T, Plukker JT. Impact of 18F-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) in patients with biochemical evidence of recurrent or residual medullary thyroid cancer. Ann Surg Oncol 2004;11:786-794. Pearse AG. The APUD cell concept and its implications in pathology. Pathol Annu 1974;9:27-41. Brown WD, Oakes TR, DeJesus OT, et al. Fluorine-18-fluoro-L-DOPA dosimetry with carbidopa pretreatment. J Nucl Med 1998;39:1884-1891. Hoegerle S, Altehoefer C, Ghanem N, Brink I, Moser E, Nitzsche E. 18F-DOPA positron emission tomography for tumour detection in patients with medullary thyroid carcinoma and elevated calcitonin levels. Eur J Nucl Med 2001;28:64-71. Koopmans KP, de Vries EG, Kema IP, et al. Staging of carcinoid tumours with 18F-DOPA PET: a prospective, diagnostic accuracy study. Lancet Oncol 2006;7:728-734. Koopmans KP, de Groot JW, Plukker JT, et al. 18F-dihydroxyphenylalanine PET in patients with biochemical evidence of medullary thyroid cancer: relation to tumor differentiation. J Nucl Med 2008;49:524-531. Beuthien-Baumann B, Strumpf A, Zessin J, Bredow J, Kotzerke J. Diagnostic impact of PET with 18FFDG, 18F-DOPA and 3-O-methyl-6-[18F]fluoro-DOPA in recurrent or metastatic medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging 2007;34:1604-1609. BUSCH H, DAVIS JR, HONIG GR, ANDERSON DC, NAIR PV, NYHAN WL. The uptake of a variety of amino acids into nuclear proteins of tumors and other tissues. Cancer Res 1959;19:1030-1039. Isselbacher KJ. Sugar and amino acid transport by cells in culture--differences between normal and malignant cells. N Engl J Med 1972;286:929-933. Jager PL, Vaalburg W, Pruim J, de Vries EG, Langen KJ, Piers DA. Radiolabeled amino acids: basic aspects and clinical applications in oncology. J Nucl Med 2001;42:432-445. Phan HT, Jager PL, Plukker JT, Wolffenbuttel BH, Dierckx RA, Links TP. Comparison of 11C-methionine PET and 18F-fluorodeoxyglucose PET in differentiated thyroid cancer. Nucl Med Commun 2008;29:711-716. Pentlow KS, Graham MC, Lambrecht RM, et al. Quantitative imaging of iodine-124 with PET. J Nucl Med 1996;37:1557-1562. Eschmann SM, Reischl G, Bilger K, et al. Evaluation of dosimetry of radioiodine therapy in benign and malignant thyroid disorders by means of iodine-124 and PET. Eur J Nucl Med Mol Imaging 2002;29:760-767. Lubberink M, van Schie A, de Jong HW, van Dongen GA, Teule GJ. Acquisition settings for PET of 124I administered simultaneously with therapeutic amounts of 131I. J Nucl Med 2006;47:1375-1381. Freudenberg LS, Antoch G, Jentzen W, et al. Value of (124)I-PET/CT in staging of patients with differentiated thyroid cancer. Eur Radiol 2004;14:2092-2098. Phan HT, Jager PL, Paans AM, et al. The diagnostic value of 124I-PET in patients with differentiated thyroid cancer. Eur J Nucl Med Mol Imaging 2008;35:958-965. Abdul Fatah S, Brans B, Huijberts M, Sels J, Nieuwenhuijzen Kruseman A, Teule G. Impact of I-124 PETCT in the loco-regional staging of differentiated thyroid carcinoma. J NUCL MED MEETING ABSTRACTS 2007;48:127P-c. 89 90
© Copyright 2026