A randomized, double-blind, placebo-controlled, cross
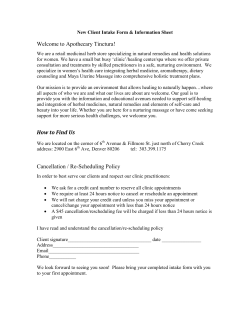
ARTICLE IN PRESS Phytomedicine 17 (2010) 389–396 Contents lists available at ScienceDirect Phytomedicine journal homepage: www.elsevier.de/phymed A randomized, double-blind, placebo-controlled, cross-over pilot study on the use of a standardized hop extract to alleviate menopausal discomforts R. Erkkola a, S. Vervarcke b, S. Vansteelandt c, P. Rompotti d, D. De Keukeleire e, A. Heyerick e,n a Department of Obstetrics and Gynecology, Turku University Central Hospital, 20521 Turku, Finland Metagenics Belgium, 8400 Ostend, Belgium c Department of Applied Mathematics and Computer Science, Ghent University-UGent, 9000 Ghent, Belgium d MaxMedica Oy, 24910 Halikko, Finland e Laboratory of Pharmacognosy and Phytochemistry, Department of Pharmaceutics, Ghent University-UGent, Harelbekestraat 72, 9000 Ghent, Belgium b a r t i c l e in fo Keywords: Menopause Phytoestrogens Hop (Humulus lupulus L.) Kupperman index Visual analogue scale Menopause rating scale abstract Objectives: To examine the efficacy of a hop extract (standardized at 100 mg 8-prenylnaringenin per day) for relief of menopausal discomforts. Methods: A 16-week randomized, double-blind, placebo-controlled, cross-over study was conducted with 36 menopausal women. The participants were randomly allocated to either placebo or active treatment (hop extract) for a period of eight weeks after which treatments were switched for another eight weeks. The Kupperman Index (KI), the Menopause Rating Scale (MRS) and a multifactorial Visual Analogue Scale (VAS) were assessed at baseline, and after eight and sixteen weeks. Results: After 8 weeks, both active treatment and placebo significantly improved all outcome measures when compared to baseline with somewhat higher average reductions for placebo than for the active treatment. After 16 weeks only the active treatment after placebo further reduced all outcome measures, whereas placebo after active treatment resulted in an increase for all outcome measures. Although, the overall estimates of treatment efficacy (active treatment-placebo) based on linear mixed models do not show a significant effect, time-specific estimates of treatment efficacy indicate significant reductions for KI (P = 0.02) and VAS (P = 0.03) and a marginally significant reduction (P = 0.06) for MRS after 16 weeks. Conclusions: Whereas the first treatment period resulted in similar reductions in menopausal discomforts in both treatment groups, results from the second treatment period suggest superiority of the standardized hop extract over placebo. Thus, phytoestrogen preparations containing this standardized hop extract may provide an interesting alternative to women seeking relief of mild vasomotor symptoms. & 2010 Elsevier GmbH. All rights reserved. Introduction The interest in the use of phytoestrogens for the management of menopausal complaints has increased considerably since the widely publicized and discussed results of the Women’s Health Initiative and the One Million Women Study. Phytoestrogens are mostly non-steroidal polyphenolic plant-derived compounds that functionally mimic the activity of the human estrogen, 17b-estradiol and typical sources include soy and red clover (isoflavones), flaxseed (lignans) and hops (prenylflavonoids) (Cos et al., 2003). A large body of scientific evidence from both epidemiological and experimental studies suggests that the n Corresponding author. Tel.: + 32 9 264 8058; fax: +32 9 264 8192. E-mail address: [email protected] (A. Heyerick). 0944-7113/$ - see front matter & 2010 Elsevier GmbH. All rights reserved. doi:10.1016/j.phymed.2010.01.007 consumption of phytoestrogen-rich diets may have protective effects on estrogen-related conditions, such as menopausal symptoms (Huntley and Ernst, 2004), and estrogen-related diseases, such as prostate and breast cancers (Holzbeierlein et al., 2005; Wu et al., 2008), osteoporosis (Messina et al., 2004; Ye et al., 2006), and cardiovascular diseases (Clerici et al., 2007). On the other hand, systematic reviews of randomized, controlled trials (RCTs) show contradictory results and meta-analyses failed to demonstrate a statistically significant reduction of vasomotor symptoms for phytoestrogens (Krebs et al., 2004; Kronenberg and Fugh-Berman, 2002; Lethaby et al., 2007). In more selected patient populations, however, such as in women in early natural menopause with mild to moderate vasomotor symptoms, a systematic review found a significant reduction of hot flashes in five out of five RCTs (Tempfer et al., 2007). It should be noticed that intervention studies with phytoestrogens suffer from large ARTICLE IN PRESS 390 R. Erkkola et al. / Phytomedicine 17 (2010) 389–396 variabilities in outcome measures and very limited reproducibility between studies. A major factor that could significantly contribute to the highly variable clinical results is the large interindividual variability in bioavailability with a critical role for the gut microbiota in the bioactivation of phytoestrogens (Nielsen and Williamson, 2007; Possemiers et al., 2007). As there is a scientific rationale for the efficacy of phytoestrogens and as no serious side effects have been associated with short term use, the position statement of the North American Menopause Society (NAMS) for the treatment of menopause-associated vasomotor symptoms suggests that changes in lifestyle, either alone or combined with the use of phytoestrogen preparations should be considered for the relief of mild vasomotor symptoms (Santoro et al., 2004). A complete vasomotor symptom treatment algorithm was recently proposed by Panay (Panay, 2007). Although hops have been known to be estrogenic from both traditional medicine and anecdotal reports, phytoestrogen preparations based on hops (Humulus lupulus L.) are relatively new, as the estrogenic principle, 8-prenylnaringenin (8-PN), was only identified in 1999 (Milligan et al., 1999). In contrast, most commercially available hop-derived preparations (often in combination with other plants, such as Valeriana officinalis L. and Melissa officinalis L.) are focused on the tranquilizing (sedative) effect of the plant and lack estrogenic acitivity. Comparisons with well-known phytoestrogens such as coumestrol (from clover or alfalfa), genistein and daidzein (from soy) shows that 8-PN is one of the most potent phytoestrogens currently known (Milligan et al., 1999). In addition, it was recently discovered that isoxanthohumol, another hop-derived prenylflavonoid that is usually present in much larger quantities, can act as proestrogen as it can be metabolized into 8-PN by the intestinal microbiota (Possemiers et al., 2006, 2005). Animal studies have reported a variety of beneficial effects related to menopausal complaints and diseases, including the reduction in tail-skin-temperature as a model for hot flashes (Bowe et al., 2006), the reduction in serum LH and FSH and in gonadotropin-releasing hormone (GnRH) receptor transcripts (Christoffel et al., 2006), and the protection of ovariectomy induced bone loss with a minimal trophic effect on ¨ the uterus (Humpel et al., 2005). Until now, only one RCT on the use of a standardized hop extract to alleviate menopausal discomforts has been carried out (Heyerick et al., 2006). This randomized, double-blind, placebocontrolled study over 12 weeks with 67 menopausal women showed a significant reduction in menopausal discomforts and complaints as assessed by the Kupperman index (KI) and by a simplified patients’ questionnaire in both the placebo and treatment groups. However, the effect of the hop extract standardized at 100 mg 8-PN per day was only significantly superior to placebo after 6 weeks (P = 0.023), but not after 12 weeks (P = 0.086). Furthermore, no dose-response relationship could be established, as the higher dose (250 mg 8-PN per day) appeared less active than the lower dose both after 6 weeks and after 12 weeks. Both the relatively small sample scale and factors affecting the bioavailability may have contributed to the absence of a clear dose-response relationship, as large interindividual differences in metabolic activation of the proestrogen IX to 8-PN exist in a typical menopausal population (Bolca et al., 2007). Still, a trend for a more rapid decrease of the KI was noticed for both active groups as compared to placebo, while most interestingly, especially the hot flash score (as an isolated item of the KI) was significantly reduced in both treatment groups after 6 weeks (P o 0.01). The current study aimed to further investigate the effect of the daily intake of a hop phytoestrogen containing dietary supplement standardized on 8-PN on menopausal discomforts using a randomized, double-blind, placebo-controlled, cross-over design. Menopausal discomforts were scored by the medical professional using the KI (Kupperman et al., 1953), while the Menopause Rating Scale (MRS) (Schneider et al., 2000) and a multifactorial Visual Analogue Scale (VAS) were used as a self-reporting tool for the participants. Materials and methods Participants Healthy postmenopausal volunteers were recruited from the Turku area (Finland) mainly via an announcement in the local newspaper. In total, fourty women aged between 45 and 60 years were considered for inclusion in the study. All subjects were healthy postmenopausal Caucasian females. Subjects were eligible for inclusion in the study if they had an intact uterus and had not experienced menses for at least 12 months and were willing to sign informed consent forms after being informed about the study in detail. Exclusion criteria were history of breast cancer, endometrial cancer or other hormone-dependent cancers, use of hormone therapy during the last 3 months before the trial and the use of a dietary supplement containing phytoestrogens during the last month before the trial. Subjects were assessed for eligibility by a gynecologist (RE). Four women did not comply with the inclusion-exclusion criteria, so finally 36 women were enrolled and assigned to the treatments according to the study protocol. Study protocol A randomized, double-blind, placebo-controlled, cross-over study was designed to compare the effects of either placebo or daily doses of a standardized hop extract on menopausal complaints as assessed by the KI, the MRS and a multifactorial VAS. The study was designed for a total of 50 participants and randomization was carried out by distributing random numerical codes to the two treatment regimens, ie. 25 test-placebo and 25 placebo-test items, respectively (based on an on-line randomizer, available at: http://www.random.org/sform.html, last accessed on September 20, 2009). After randomization, the codes were arranged in a list according to increasing numbers and blinded to both the gynecologist and the participant. The treatments were assigned chronologically to the eligible participants, who received a box containing 60 capsules of either placebo (12 participants) or standardized hop extract (24 participants) for the first treatment period, as shown in Fig. 1. At the next visit after 8 weeks the participants were asked to return the container and the other box containing the opposite treatment was then distributed. At the last visit after 16 weeks after baseline examination. The containers were again returned. At week 8 and week 16, the returned capsules were counted in order to check for compliance. The compositions of the capsules are given in Table 1. Placebo capsules contained maltodextrin (Lab 2509, La Roquette, Lille, France) instead of the hop extract. The hop extract in the active treatment capsules was identical to that contained in the food supplement MenoHops (PL 162/447, Biodynamics, Ostend, Belgium, Lifenols-extract (Naturex, Avignon, France)). It is derived from hydroalcoholic extraction of spent hops, the material remaining after extraction of hops with liquid or supercritical carbon dioxide. The dark-green opaque gelatin capsules size 3 (Capsugel, Bornem, Belgium) additionally contained dicalcium phosphate (Rhodia, Chicago Heights Illinois, USA), silicium dioxide (Degussa, Rheinfelden, Germany), and magnesium stearate (Undesa Union Derivan, Barcelona, Spain). ARTICLE IN PRESS R. Erkkola et al. / Phytomedicine 17 (2010) 389–396 391 Fig. 1. The participant’s flow diagram. Table 1 Composition (mg) of the capsules. Hop extract Maltodextrin Dicalcium phosphate Silicium dioxide Magnesium stearate Total Placebo Active treatment 0.0 75.1 124.9 1.0 1.0 202 75.1 (100 mg 8-PN) 0.0 124.9 1.0 1.0 202 (Hop extract: 8-prenylnaringenin: 0.13%, xanthohumol: 2.72%, isoxantohumol: 1.60%, 6-prenylnaringenin: 0.12%). Capsules were prepared in a semi-automatic capsulation machine (Ultra 8 II, Capsugel-Divison of Warner Lambert, Greenwood, South Carolina, USA) and the hop extract capsules were controlled for content of 8-prenylnaringenin (8-PN or ( 7)-2,3-dihydro5,7-dihydroxy-2-(4-hydroxyphenyl)-8- (3-methylbut-2-enyl)-4Hbenzopyran-4-one) by applying HPLC-MS (in analogy to Rong et al., 2000). In short, the powder obtained from the capsules was extracted with methanol under sonication for 15 min at room temperature and, after filtration, an aliquot of 20 ml was injected onto an XTerras MS reversed-phase C18 column (250 x 4.6 mm, 5 mm) (Waters, Milford, MA, USA). A linear gradient at a flow rate of 1 ml.min-1 comprised of 250 ppm formic acid in water (solvent A) and 250 ppm formic acid in acetonitrile (solvent B) ranging from 40% B in A to 95% B in A over 40 min was applied. All analyses were carried out using an Agilent 1200 Series LC/MSD SL system (Agilent Technologies, Santa Clara, CA, USA). External calibration was carried out using pure standards obtained via chemical synthesis (8-PN and 6-prenylnaringenin) or preparative HPLC of hop cone extracts (isoxanthohumol and xanthohumol). The capsules were found to contain a total of 3.4470.10 mg of prenylflavonoids per capsule, composed of 1.2070.04 mg of isoxanthohumol, 0.11 70.01 mg of 8-PN, 0.0970.01 mg of 6-prenylnaringenin, and 2.0470.06 mg of xanthohumol. Participants in this study were evaluated by three different tools. The KI was scored by the gynecologist (RE), while both the MRS and a multifactorial VAS were used as self-assessment questionnaires. For the KI each item is scored from 0 (not present or not disturbing) to 3 (very severe) depending on the intensity (Kupperman et al., 1953). Each score is multiplied by a given factor depending on the contribution to the index. The maximal score for the KI is 51. The MRS is a scale based on 11 items divided into three domains: somatic, psychological, and urogenital (Schneider et al., 2000). Scoring is based on a five-point Likert scale ranging from no symptoms to mild, moderate, marked or severe complaints. The maximal score for the MRS is 44. A multifactorial VAS presenting three items, respectively hot flashes, night sweats and sleep disturbances, was scored by the women themselves. These items were chosen because hot flashes and night sweats are the primary menopausal complaints. Sleep disturbances were added to this VAS because hop extracts have traditionally been used as sleeping aids. Participants were asked to rate the intensity of the symptoms for each item by placing a vertical mark a on a 0-100 mm scale (0 =no complaints,100 mm= very severe complaints). The scores of the individual items were combined and the maximal combined score for the VAS is thus 300. The participants filled in the MRS and VAS before the gynecologist scored the KI. Statistical analysis Comparison of baseline characteristics was based on means and standard deviations for continuous outcome measures, provided these were approximately normally distributed according to QQ-plots. If not, they were based on medians and interquartile range (IQR) otherwise. Raw estimates of treatment efficacy at each measurement occasion were based on the intention-to-treat principle, using a Welch Two-sample t-test to allow for different measurement variance in different treatment groups. Normality of the outcomes at each time in each treatment arm was assessed and found satisfactory according to QQ-plots. In order to obtain more powerful treatment comparisons, the primary analysis of the data was based on a linear mixed effects’ model for the outcome measurements at the different occasions jointly, including the baseline outcome (Verbeke and Molenberghs, 2000). We allowed for a nonlinear time evolution under placebo and for treatment-by-period interaction (different treatment effects allowed in different periods). Detailed model checking revealed substantial evidence for the presence of random intercepts (there was substantial evidence that the overall level of ARTICLE IN PRESS 392 R. Erkkola et al. / Phytomedicine 17 (2010) 389–396 postmenopausal symptoms varies between patients) and a residual autoregressive correlation structure (informally, there was substantial evidence that measurements taken more closely in time are more strongly correlated than measurements taken further apart), both of which were accounted for in all analyses. All reported results are based on models which fit the observed data well according to scaled residual plots (Fitzmaurice et al., 2004). Reported p-values for treatment efficacy are based on Wald tests. Paired Student’s t-tests (2-tailed) were used to make comparisons between different time points for all outcome measures within a treatment group. Analyses were conducted in SAS Version 9.1 and SPSS 15.0. Ethics approval for the study The protocol is consistent with the principles of the Declaration of Helsinki and the Joint Ethical Committee of the University of Turku and University Central Hospital of Turku approved the study protocol. An oral and written informed consent was received from all participants. Results Although the study was designed for 50 participants, only 40 participants, of which 36 were found eligible, could be recruited within a reasonable time frame. Three volunteers were excluded because of the use of HT and one because of the use of a dietary supplement containing phytoestrogens. As the randomization list was set up without block-randomization for an estimated 50 participants, the random allocation to the two treatment groups coincidentally resulted in considerable differences with 24 participants receiving first the active treatment followed by placebo (test-placebo), while only 12 participants received placebo first followed by the active treatment (placebo-test). No adverse events were reported and there were no drop-outs. The baseline characteristics of the women in each treatment arm were similar (Table 2). As no substantial differences with respect to these characteristics were found, no adjustments were made in the primary analysis of treatment effectiveness. Fig. 2 shows the box-and-whisker diagrams for the 3 outcome measures at baseline, after 8 weeks and after 16 weeks, separately for both patient groups. Table 3 shows the mean outcome measures ( 7 standard deviations) for both treatment groups after 8 weeks and after 16 weeks. After 8 weeks, both active treatment and placebo significantly improved all outcome measures compared to baseline with somewhat higher average reductions for placebo than for the active treatment. On the other hand, more pronounced and opposite effects can be observed for all outcome measures at Table 2 Characteristics of the patients at baseline (mean 7 SD; time since menopause measured in median 7 IQR). Characteristic Active-Placebo (n= 24) Placebo-Active (n = 12) Age, yr Time since menopause, yr Height, cm Weight, kg BMI, kg/m2 Baseline KI Baseline MRS Baseline VAS 52.8 7 3.5 4.3 7 3.8 164.3 7 4.7 67.2 7 9.1 24.8 7 3.2 24.2 7 7.2 23.0 7 4.0 173.1 7 61.5 54.3 7 3.7 4.75 7 4.3 163.9 7 3.8 67.7 7 6.3 25.2 7 2.4 23.3 7 9.8 21.3 7 4.9 163.4 7 78.6 SD, standard deviation; IQR, interquartile range; BMI, body mass index; MRS, menopause rating scale; KI, Kupperman index; VAS, visual analogue scale. week 16, as the active treatment after placebo further reduced all outcome measures, whereas placebo after the active treatment resulted in a slight increase for all outcome measures. Additionally, it can be observed that the measurement variability stays more or less constant over time. Table 4 shows the raw estimates of treatment efficacy (active treatment – placebo) at each time and for each outcome. After 8 weeks, placebo shows somewhat higher efficiency on all outcome measures in comparison with active treatment. After 16 weeks, the effects are opposite and more pronounced. The results after 16 weeks with p-values of 0.05, 0.06 and 0.07, for VAS, MRS and KI, respectively, indicate marginal evidence of a treatment effect of the active treatment over placebo. In order to enhance power, a joint analysis of the repeated measurements at each time was performed using linear mixed models. Although the treatment effects were opposite at months 2 and 4, there was insufficient evidence in the observed data to distinguish whether this is systematic or just the result of sampling error. Specifically, only marginal evidence of treatment-by-period interaction (P = 0.08 for KI, P = 0.09 for MRS, and P = 0.11 for VAS) was found and, henceforth, it was chosen to base inference on the overall treatment effect (i.e. averaged over the 2 occasions). Table 5 summarizes the results showing no significant effect of active treatment over placebo. Specifically, it was found that the experimental treatment yields non-significant reductions (as compared to placebo and over a 2 month period) in KI with 2.3 (P = 0.10, 95% CI: -5.1; 0.5) on average, in MRS with 0.6 (P = 0.40, 95% CI: -1.9; 0.8) on average, and in VAS with 15.3 (P = 0.28, 95% CI: -43.2; -12.7) on average. To correct for possible baseline imbalances and to reduce outcome variation, a further secondary analysis was performed and adjustment for baseline covariates was carried out. This did not affect the treatment effect estimates on MRS and KI because none of the baseline covariates were significantly associated with the outcomes. Treatment effect estimates on VAS changed slightly from -15.3 to -16.0 with a corresponding p-value of 0.25 instead of 0.28. Given the fact that opposite treatment effects were observed at the 2 follow-up measurement occasions, we subsequently estimated treatment effects at the 2 time points separately. Table 6 summarizes the results and reveals significant treatment effects on the average KI (P = 0.02) and the average VAS at week 16 (P = 0.03), whereas the treatment effect on the average MRS was only marginally significant (P = 0.06). The active treatment lowered the KI by 5.9 (95% CI: -10.8; -1.1), on average, at week 16 as compared to placebo. Likewise, the active treatment lowered the VAS with 45.4 (95% CI -86.0; - 4.7) on average at week 16 as compared to placebo. Finally, all outcome measures within each group were compared at each time point using paired Student’s t-tests (2-tailed) (for P-values see Fig. 2). Although both the active treatment and the placebo show significant reductions in all outcome measures after 8 weeks when compared to baseline (P o 0.05), only the active treatment after placebo retains significance for all outcome measures after 16 weeks when compared to baseline, whereas placebo after active treatment loses significance for both KI and MRS when compared to baseline. Discussion Although the overall estimates of treatment efficacy in this randomized, double-blind, placebo-controlled, cross-over study do not indicate any significant effect of the treatment in comparison to placebo, more detailed analysis uncovers interesting indications of the superiority of the active treatment over ARTICLE IN PRESS R. Erkkola et al. / Phytomedicine 17 (2010) 389–396 393 Active Placebo Placebo Active 60 60 P = 0.244 50 P = 0.017 P = 0.066 30 40 KI KI 40 20 10 10 0 0 After 8 weeks After 16 weeks Time Baseline 40 P = 0.021 After 8 weeks After 16 weeks Time P = 0.277 25 30 20 15 15 10 10 After 8 weeks After 16 weeks Time Baseline P = 0.030 300 P = 0.007 300 P = 0.306 VAS 200 100 0 0 After 8 weeks After 16 weeks Time P = 0.786 After 8 weeks After 16 weeks Time P = 0.008 P = 0.038 P = 0.448 200 100 Baseline P = 0.002 25 20 Baseline P = 0.019 35 MRS 30 MRS P = 0.408 40 P = 0.143 35 VAS P = 0.008 30 20 Baseline P = 0.008 50 Baseline After 8 weeks Time After 16 weeks Fig. 2. Box-and-whisker diagrams for both treatment groups at each time and for each outcome (Kuppermann index (KI), Menopause Rating Scale (MRS), Visual analogue Scale VAS) with P-values for paired t-test comparisons between different time points within the treatment group (n = outlier). Table 3 Mean outcome measures (7 SD) for both treatments groups. Outcome measure KI MRS VAS Active-Placebo Placebo-Active 8 weeks 8 weeks 16 weeks 16 weeks 19.9 7 10.1 22.4 7 7.5 18.2 7 8.5 15.9 7 10.3 20.6 7 4.6 21.4 7 4.9 18.3 7 4.3 17.9 7 4.9 135.1 7 87.4 146.6 7 76.0 115.8 7 77.7 95.2 7 68.9 SD, standard deviation; KI, Kupperman index; MRS, menopause rating scale; VAS, visual analogue scale. placebo. Cross-over trials have some inherent issues. For example, the order of the treatment may have a considerable effect on the overall outcome, especially when a placebo effect is likely. When such a set-up is being used in studies on menopausal complaints, it should be taken into account that menopausal complaints are typically sensitive to a large and persistent placebo effect, especially over shorter time periods (Lethaby et al., 2007). In addition, menopausal complaints also naturally decrease over longer time periods. As expected, also in this study, placebo results in a significant reduction in menopausal complaints over the first eight weeks (20%-35% depending on the specific outcome). The reduction in menopausal complaints for placebo is even more pronounced than for the active treatment after eight weeks. In sharp contrast, switching from active treatment to placebo after eight weeks resulted in a slight increase in menopausal complaints after sixteen weeks, whereas switching from placebo to active treatment further reduced the menopausal complaints. ARTICLE IN PRESS 394 R. Erkkola et al. / Phytomedicine 17 (2010) 389–396 Table 4 Raw estimates of treatment efficacy (active treatment - placebo) at each time and for each outcome. Outcome Week Effect 95% CI P KI 8 16 8 16 8 16 1.7 -6.5 2.3 -3.5 19.4 -51.5 -4.9 ; 8.3 -13.6 ; 0.6 -0.9 ; 5.5 -7.1 ; 0.1 -39.7 ; 78.5 -103.5 ; 0.6 0.60 0.07 0.15 0.06 0.50 0.05 MRS VAS CI, confidence interval; KI, Kupperman index; MRS, menopause rating scale; VAS, visual analogue scale. Table 5 Overall estimates of treatment efficacy (active treatment - placebo) for each outcome, based on linear mixed model analysis. Outcome Effect 95% CI P KI MRS VAS -2.3 -0.6 -15.3 -5.1 ; 0.5 -1.9 ; 0.8 -43.2 ; 12.7 0.10 0.40 0.28 CI, confidence interval; KI, Kupperman index; MRS, menopause rating scale; VAS, visual analogue scale. Table 6 Time-specific estimates of treatment efficacy (active treatment - placebo) for each outcome, based on linear mixed model analysis. Outcome Week Effect 95% CI P KI 8 16 8 16 8 16 1.1 -5.9 1.3 -2.8 13.3 -45.4 -3.1 ; 5.3 -10.8 ; -1.1 -0.9 ; 3.5 -5.6 ; 0.1 -30.1 ; 56.7 -86.0 ; - 4.7 0.60 0.02 0.24 0.06 0.61 0.03 MRS VAS CI, confidence interval; KI, Kupperman index; MRS, menopause rating scale; VAS, visual analogue scale. This observation is confirmed by the secondary analyses taking into account the time-specific estimates of treatment efficacy, showing significant effects of active treatment in comparison to placebo for both KI and VAS and a marginally significant effect for MRS, suggesting that the standardized hop extract is superior to placebo with respect to the potency to reduce menopausal complaints. The results of this study should be interpreted with caution as this study is subject to a number of limitations. Although the number of participants seems low in comparison with the previous study, it should be noticed that the cross-over design resulted in a total of 72 interventions divided evenly between placebo and active treatment, whereas in the previous study only 67 interventions were carried out, including 26 placebo, 20 normal dosage treatments and 21 higher dosage treatments (Heyerick et al., 2006). Unfortunately, the populations in the two different treatment regimens were imbalanced (12 vs 24) as block randomization was not used during the preparation of this study. The significant effects observed in the second treatment period are, therefore, mostly based on the results of the smaller group and may thus be more prone to statistical error. Furthermore, the active treatment regimen was only given for 8 weeks, whereas it is customary to use a 12 week study time for vasomotor studies (Lethaby et al., 2007). In addition, no wash out phase between the cross-over strategy has been used. However, based on circumstantial evidence and results of the first study it was anticipated that the standardized hop extract would exert its activity within a short period after treatment, while pharmacokinetic data also indicate wash-out of the active ingredients within a relatively short time (Rad et al., 2006). As it is known that menopausal symptoms are self-limiting with time, it could be argued that the study population was not ideally suited to study the effect on menopausal complaints as the mean time since menopause was more than 4 years on average. Women indeed typically experience hot flashes for 6 months up to 2 years, but some women experience hot flashes for 10 years or longer (Santoro et al., 2004). In a Swedish population, it was found that the maximal prevalence of hot flashes was about 60% at 52 to 54 years of age, declining to 30% at 60 and 9% at 72 years (Rodstrom et al., 2002) and more recently, in a 13 year follow-up study it was found that the mean duration of vasomotor symptoms was 5.2 7 3.8 years (Col et al., 2009). Given the mean age of the population under study and the mean time since menopause, it can be concluded that this population is still relevant with respect to the study carried out. This is corroborated by the fact that the mean baseline parameters for menopausal symptoms (Menopause Rating Scale and Kupperman Index) were indicative of significant menopausal symptoms, in line with the baseline parameters of many other studies investigating the effect of a treatment on menopausal symptoms (e.g. raloxifene+ estradiol: (Valiati et al., 2009), soy phytoestrogens: (Nahas et al., 2007), physical exercise: (Moriyama et al., 2008)). The scales used to measure menopausal discomforts (KI, MRS and VAS) are not direct measures of vasomotor symptoms, but rather summaries of quality-of-life in relation to overall menopausal complaints. More direct results on vasomotor symptoms could be derived from the use of a hot flash diary with daily scoring of frequency and intensity of hot flashes and night sweats. With respect to the VAS scores, it should be noticed that both the vasomotor symptoms and sleep disturbances contributed equally to the reduction of the VAS parameter, indicating that the standardized hop extract could also exert improved sleep quality, which is in correspondence with its traditional use as mild sedative most often in combination with valerian (Koetter et al., 2007). Although further studies are required to confirm the observations made in this and the previous study (Heyerick et al., 2006), phytoestrogen preparations containing this standardized hop extract may provide an interesting alternative to women seeking relief of mild vasomotor symptoms, as suggested in the NAMS position statement (Santoro et al., 2004). Herbal treatments for menopausal complaints have been studied extensively over the last decade. Although epidemiological studies suggest a relationship between the intake of soyderived phytoestrogens (isoflavones) and reduced menopausal complaints, randomized intervention trials with either increased soy intake or isolated soy-derived phytoestrogens have reported inconsistent results (Lethaby et al., 2007). Analogously, also intervention studies with red clover or black cohosh extracts failed to produce consistent results (Booth et al., 2006; Borrelli and Ernst, 2008). In most studies, a large heterogeneity in individual responses has been observed, with some participants responding only weakly to the treatment or even in the opposite direction, while others respond strongly to the treatment. In addition to the highly variable response to the placebo effect, it is also quite likely that interindividual differences in exposure to the active ingredients (eg. soy isoflavones) after oral intake may co-determine the individual response to the treatment. Apart from interindividual differences in absorption, distribution, metabolism en excretion, it is now recognized that also the gut microflora may have a significant impact on the final exposure to both the type and the concentration of the active ingredients ARTICLE IN PRESS R. Erkkola et al. / Phytomedicine 17 (2010) 389–396 (Atkinson et al., 2005; Nielsen and Williamson, 2007; Tamura, 2006). In both the previous (Heyerick et al., 2006) and this present study, similar large differences in individual responses were observed. Differences in metabolism may in part account for these differences. More specifically, isoxanthohumol can be converted into 8-PN by the intestinal microbiota (Possemiers et al., 2005). This transformation is subject to a high interindividual variability, as in a small population of menopausal women only 35% were categorized as high or moderate 8-PN producers, whereas 65% was categorized as weak or non-producers (Bolca et al., 2007; Possemiers et al., 2006). As isoxanthohumol is present in the standardized hop extract at a level that is ten times higher than 8-PN, the final exposure to 8-PN may be subject to a high interindividual variability. Therefore, it can be speculated that specific phytoestrogen preparations may have beneficial properties only in selected patient groups. As a consequence, it would be advisable that future intervention studies estimating the effect of phytoestrogens on menopausal complaints incorporate the analysis of a marker for the individual exposure to the active ingredients (eg. steady-state concentration in serum or the daily excretion in urine) in order to correlate the effective exposure with the observed effects. In this study, no adverse effects have been recorded, while the hop extract has shown a good tolerability as there were no dropouts. Hop-derived extracts have traditionally been used with a high safety profile. The safety of phytoestrogen preparations in general, given their estrogenic potency, form the focus of recent investigations. Intervention studies with phytoestrogen preparations including soy isoflavones and black cohosh did not show any adverse effects on the endometrium (Palacios et al., 2007; Reed et al., 2008). Although animal experiments have shown possibly negative effect of 8-PN on the uterus (Overk et al., 2008), the endometrial safety of the standardized hop extract was investigated in a recently finished study with good results (results to be published). In conclusion, the results obtained in this randomized, double blind, placebo-controlled, cross-over study showed that administration of a hop extract standardized on 8-PN (100 mg per daily dose) to post-menopausal women during 8 weeks can reduce discomforts and complaints associated to the menopause as measured by the KI, MRS and a multifactorial VAS. Although both placebo and active treatment similarly reduced the menopausal complaints after the first eight weeks, only the active treatment could further reduce the menopausal complaints after switching the treatments, whereas for placebo an increase of menopausal complaints was observed. Significant reductions in menopausal complaints for the active treatment in comparison with placebo were observed after 16 weeks, suggesting that the standardized hop extract is superior to placebo with respect to its potency to reduce menopausal complaints. Although the observed effects still need to be confirmed in further studies, phytoestrogen preparations containing this standardized hop extract may provide an interesting alternative to women seeking relief of mild vasomotor symptoms. Source of funding and conflict of interest This study was financed by MaxMedica, Finland and Metagenics Belgium, Ostend, Belgium, with the principal aim of evaluating their food supplement MenoHops. The study and the analysis of the results, however, were done independently of MaxMedica and Metagenics Belgium, apart from occasional advice on matters of protocol. The supporting source had no influence on the decision to submit the results of the study for publication. 395 Acknowledgements The participating women are thanked for their kind co-operation. The logistics support of Metagenics Belgium, Ostend, Belgium, is kindly acknowledged. References Atkinson, C., Frankenfeld, C.L., Lampe, J.W., 2005. Gut bacterial metabolism of the soy isoflavone daidzein: exploring the relevance to human health. Exp. Biol. Med. 230, 155–170. Bolca, S., Possemiers, S., Maervoet, V., Huybrechts, I., Heyerick, A., Vervarcke, S., Depypere, H., De Keukeleire, D., Bracke, M., De Henauw, S., Verstraete, W., Van de Wiele, T., 2007. Microbial and dietary factors associated with the 8-prenylnaringenin producer phenotype: a dietary intervention trial with fifty healthy post-menopausal Caucasian women. Br. J. Nutr. 98, 950–959. Booth, N.L., Piersen, C.E., Banuvar, S., Geller, S.E., Shulman, L.P., Farnsworth, N.R., 2006. Clinical studies of red clover (Trifolium pratense) dietary supplements in menopause: a literature review. Menopause 13, 251–264. Borrelli, F., Ernst, E., 2008. Black cohosh (Cimicifuga racemosa) for menopausal symptoms: a systematic review of its efficacy. Pharmacol. Res. 58, 8–14. Bowe, J., Li, X.F., Kinsey-Jones, J., Heyerick, A., Brain, S., Milligan, S., O’Byrne, K., 2006. The hop phytoestrogen, 8-prenylnaringenin, reverses the ovariectomyinduced rise in skin temperature in an animal model of menopausal hot flushes. J. Endocrinol. 191, 399–405. Christoffel, J., Rimoldi, G., Wuttke, W., 2006. Effects of 8-prenylnaringenin on the hypothalamo-pituitary-uterine axis in rats after 3-month treatment. J. Endocrinol. 188, 397–405. Clerici, C., Setchell, K.D.R., Battezzati, P.M., Pirro, M., Giuliano, V., Asciutti, S., Castellani, D., Nardi, E., Sabatin, G., Orlandi, S., Baldoni, M., Morelli, O., Mannarino, E., Morelli, A., 2007. Pasta naturally enriched with isoflavone aglycons from soy germ reduces serum lipids and improves markers of cardiovascular risk. J. Nutr. 137, 2270–2278. Col, N.F., Guthrie, J.R., Politi, M., Dennerstein, L., 2009. Duration of vasomotor symptoms in middle-aged women: a longitudinal study. Menopause 16, 453–457. Cos, P., De Bruyne, T., Apers, S., Berghe, D.V., Pieters, L., Vlietinck, A.J., 2003. Phytoestrogens: recent developments. Planta Med. 69, 589–599. Fitzmaurice, G., Laird, N., Ware, J., 2004. Applied Longitudinal Analysis. Wiley. Heyerick, A., Vervarcke, S., Depypere, H., Bracke, M., De Keukeleire, D., 2006. A first prospective, randomized, double-blind, placebo-controlled study on the use of a standardized hop extract to alleviate menopausal discomforts. Maturitas 54, 164–175. Holzbeierlein, J.M., McIntosh, J., Thrasher, J.B., 2005. The role of soy phytoestrogens in prostate cancer. Curr. Opin. Urol. 15, 17–22. ¨ Humpel, M., Isaksson, P., Schaefer, O., Kaufmann, U., Ciana, P., Maggi, A., Schleuning, W.D., 2005. Tissue specificity of 8-prenylnaringenin: protection from ovariectomy induced bone loss with minimal trophic effects on the uterus. J. Steroid Biochem. Mol. Biol. Huntley, A.L., Ernst, E., 2004. Soy for the treatment of perimenopausal symptoms – a systematic review. Maturitas 47, 1–9. Koetter, U., Schrader, E., Kaufeler, R., Brattstrom, A., 2007. A randomized, double blind, placebo – Controlled, prospective clinical study to demonstrate clinical efficacy of a fixed valerian hops extract combination (Ze 91019) in patients suffering from non-organic sleep disorder. Phytother. Res. 21, 847–851. Krebs, E.E., Ensrud, K.E., MacDonald, R., Wilt, T.J., 2004. Phytoestrogens for treatment of menopausal symptoms: a systematic review. Obstet. Gynecol. 104, 824–836. Kronenberg, F., Fugh-Berman, A., 2002. Complementary and alternative medicine for menopausal symptoms: a review of randomized, controlled trials. Ann. Intern. Med. 137, 805–813. Kupperman, H.S., Blatt, M.H.G., Wiesbader, H., Filler, W., 1953. Comparative evaluation of estrogenic preparations by the menopausal and amenorrheal indices. J. Clin. Endocrinol. Metab. 13, 688–703. Lethaby, A.E., Brown, J., Marjoribanks, J., Kronenberg, F., Roberts, H., Eden, J., 2007. Phytoestrogens for vasomotor menopausal symptoms. Cochrane Database Syst. Rev. Messina, M., Ho, S., Alekel, D.L., 2004. Skeletal benefits of soy isoflavones: a review of the clinical trial and epiderniologic data. Curr. Opin. Clin. Nutr. Metab. Care 7, 649–658. Milligan, S.R., Kalita, J.C., Heyerick, A., Rong, H., De Cooman, L., De Keukeleire, D., 1999. Identification of a potent phytoestrogen in hops (Humulus lupulus L.) and beer. J. Clin. Endocrinol. Metab. 84, 2249–2252. Moriyama, C.K., Oneda, B., Bernardo, F.R., Cardoso, C.G., Forjaz, C.L.M., Abrahao, S.B., Mion, D., Fonseca, A.M., Tinucci, T., 2008. A randomized, placebocontrolled trial of the effects of physical exercises and estrogen therapy on health-related quality of life in postmenopausal women. Menopause 15, 613–618. Nahas, E.A.P., Nahas-Neto, J., Orsatti, F.L., Carvalho, E.P., Oliveira, M., Dias, R., 2007. Efficacy and safety of a soy isoflavone extract in postmenopausal women: A randomized, double-blind, and placebo-controlled study. Maturitas 58, 249–258. ARTICLE IN PRESS 396 R. Erkkola et al. / Phytomedicine 17 (2010) 389–396 Nielsen, I.L.F., Williamson, G., 2007. Review of the factors affecting bioavailability of soy isoflavones in humans. Nutr. Cancer 57, 1–10. Overk, C.R., Guo, J., Chadwick, L.R., Lantvit, D.D., Minassi, A., Appendino, G., Chen, S.N., Lankin, D.C., Farnsworth, N.R., Pauli, G.F., van Breemen, R.B., Bolton, J.L., 2008. In vivo estrogenic comparisons of Trifolium pratense (red clover) Humulus lupulus (hops), and the pure compounds isoxanthohumol and 8-prenylnaringenin. Chem. Biol. Interact. 176, 30–39. Palacios, S., Pornel, B., Bergeron, C., Chantre, P., Nogales, F., Aubert, L., Vazquez, F., Eden, J., Mares, P., 2007. Endometrial safety assessment of a specific and standardized soy extract according to international guidelines. Menopause 14, 1006–1011. Panay, N., 2007. Integrating phytoestrogens with prescription medicines – A conservative clinical approach to vasomotor symptom management. Maturitas 57, 90–94. Possemiers, S., Bolca, S., Eeckhaut, E., Depypere, H., Verstraete, W., 2007. Metabolism of isoflavones, lignans and prenylflavonoids by intestinal bacteria: producer phenotyping and relation with intestinal community. FEMS Microbiol. Ecol. 61, 372–383. Possemiers, S., Bolca, S., Grootaert, C., Heyerick, A., Decroos, K., Dhooge, W., De Keukeleire, D., Rabot, S., Verstraete, W., Van de Wiele, T., 2006. The prenylflavonoid isoxanthohumol from hops (Humulus lupulus L.) is activated into the potent phytoestrogen 8-prenylnaringenin in vitro and in the human intestine. J. Nutr. 136, 1862–1867. Possemiers, S., Heyerick, A., Robbens, V., De Keukeleire, D., Verstraete, W., 2005. Activation of proestrogens from hops (Humulus lupulus L.) by intestinal microbiota; Conversion of isoxanthohumol into 8-prenylnaringenin. J. Agric. Food Chem. 53, 6281–6288. Rad, M., Humpel, M., Schaefer, O., Schoemaker, R.C., Schleuning, W.D., Cohen, A.F., Burggraaf, J., 2006. Pharmacokinetics and systemic endocrine effects of the phyto-oestrogen 8-prenylnaringenin after single oral doses to postmenopausal women. Br. J. Clin. Pharmacol. 62, 288–296. Reed, S.D., Newton, K.M., LaCroix, A.Z., Grothaus, L.C., Grieco, V.S., Ehrlich, K., 2008. Vaginal, endometrial, and reproductive hormone findings: randomized, placebo-controlled trial of black cohosh, multibotanical herbs, and dietary soy for vasomotor symptoms: the Herbal Alternatives for Menopause (HALT) Study. Menopause 15, 51–58. Rodstrom, K., Bengtsson, C., Lissner, L., Milsom, I., Sundh, V., Bjorkelund, C., 2002. A longitudinal study of the treatment of hot flushes: the population study of women in Gothenburg during a quarter of a century. Menopause 9, 156–161. Rong, H., Zhao, Y., Lazou, K., De Keukeleire, D., Milligan, S.R., Sandra, P., 2000. Quantitation of 8-prenylnaringenin, a novel phytoestrogen in hops (Humulus lupulus L.), hop products, and beers, by benchtop HPLC-MS using electrospray ionization. Chromatographia 51, 545–552. Santoro, N.F., Clarkson, T.B., Freedman, R.R., Fugh-Berman, A.J., Loprinzi, C.L., Reame, N.K., Board Trustees, N.A.M.S., 2004. Treatment of menopauseassociated vasomotor symptoms: position statement of The North American Menopause Society. Menopause 11, 11–33. Schneider, H.P.G., Rosemeier, H.P., Schnitker, J., Gerbsch, S., Turck, R., 2000. Application and factor analysis of the menopause rating scale [MRS] in a postmarketing surveillance study of Climen (R). Maturitas 37, 113–124. Tamura, M., 2006. Effects of intestinal flora on the metabolism and absorption of isoflavones. Japan Agri. Res. Quart. 40, 45–50. Tempfer, C.B., Bentz, E.K., Leodolter, S., Tscherne, G., Reuss, F., Cross, H.S., Huber, J.C., 2007. Phytoestrogens in clinical practice: a review of the literature. Fertil. Steril. 87, 1243–1249. Valiati, B., Capp, E., Edelweiss, M.I., de Freitas, F.M., Wender, M.C.O., 2009. Effect of raloxifene and low-dose percutaneous 17 beta-estradiol on menopause symptoms and endometrium – A randomized controlled trial. Maturitas 62, 81–84. Verbeke, G., Molenberghs, G., 2000. Linear Mixed Models for Longitudinal Data. Springer-Verlag. Wu, A.H., Yu, M.C., Tseng, C.C., Pike, M.C., 2008. Epidemiology of soy exposures and breast cancer risk. Br. J. Cancer 98, 9–14. Ye, Y.B., Tang, X.Y., Verbruggen, M.A., Su, Y.X., 2006. Soy isoflavones attenuate bone loss in early postmenopausal Chinese women – A single-blind randomized, placebo-controlled trial. Eur. J. Nutr. 45, 327–334.
© Copyright 2026