Contents Identification of Developmental Coordination Disorder
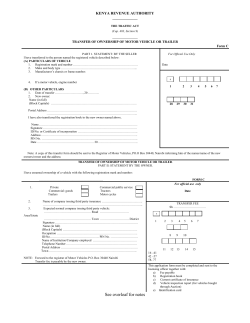
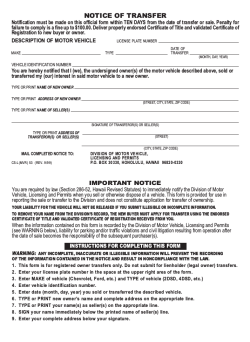
Contents Identification of Developmental Coordination Disorder 10/21/2010 | 2 1. Movement ABC-2 2. Early signs of DCD 3. Identification of DCD at school age 4. Relationship between different measuring Marina Schoemaker University Medical Centre Groningen Centre for Human Movement Sciences Groningen instruments 5. Conclusion Movement Assessment Battery for children 10/21/2010 | 4 Revision of the Movement Assessment Battery for children Marina Schoemaker University Medical Centre Groningen Centre of Human Movement Sciences Groningen Necessity for MABC-2 revision Norm data 15 years old (US data) Ambiguity in instructions Expansion of age range 4-12+ -> 3-16 years Reduction of Age bands 4 -> 3 More comparable tasks per section task specificity Scores that can be used for research standard scores Hygiene plastic instead of wood MABC-1 (1992) Henderson & Sugden MABC-2 (2007) Henderson, Sugden & Barnett What is new? Extension of age range 2nd edition of the Test of Movement ABC also includes 3-year-old-children ! 3 and 4 year old children have norms per 6 months (not per year) What is new? Reduction of age bands Primary uses of MovementABC2 10/21/2010 | 8 Identification Age band 1 4,5,6 years Age band 2 7,8 years Age band 3 9,10 years Age band 4 11,12 years Clinical exploration and intervention planning Treatment evaluation Research (select participants for experimental studies) Age band 1 3,4,5,6 years Age band 2 7,8,9,10 years Age band 3 11-16 years Standardization sample 10/21/2010 | 9 Changes in scoring system (1) MABC-1: Per item: raw scores converted in score between 1 and 5. Total score: Summation of 8 item scores (0-40) Percentile ranks for different total scores Changes in scoring system (2) Raw score Converted to Standard score (mean 10, sd 3) Total test score(TTS) Sum of standard ScoresÆ converted to Standard scores Percentiles Standardscores Changes in scoring system 10/21/2010 | 13 10/21/2010 | 14 Traffic light system: Age Band 1 3-6 years Age Band 2 7-10 years Age Band 3 11-16 years Manual Dexterity1 Posting coins Placing Pegs Turning pegs Manual Dexterity 2 Threading beads Threading Lace Triangle with nuts and bolts Manual Dexterity 3 A&C: Catching Bicycle Trail I Bicycle Trail II | 15 Bicycle Trail III Catching bean Two-hand bag catch One-hand catch A&C: Aiming Throwing bean bag into box Throwing bean bag into mat Throwing at wall target Static Balance One-leg balance One-board balance Two-board balance Dynamic Balance 1 Jumping in squares Hopping in squares Zig-zag hopping Dynamic Balance 2 Walking heels raised Heel-to-toe walking Walking backwards Bicycle trails: age bands 1 and 2 10/21/2010 | 17 What is new? Age band 1 1. 2. 3. 4. 5. 6. 7. 8. Material instructions different Tasks different posting coins in a bank box (each hand), threading beads; drawing a line into a trail; different trail catching a bean bag throwing bean bag onto mat standing on one leg ; walking heels raised on a line jumping on mats. What is new? 1. 2. 3. 4. 5. 6. 7. 8. Material instructions different Tasks different posting coins in a bank box (each hand), threading beads; drawing a line into a trail; different trail catching a bean bag throwing bean bag onto mat standing on one leg ; walking heels raised on a line jumping on mats. Throwing bean bag 10/21/2010 | 19 What is new? 1. 2. 3. 4. 5. 6. 7. 8. Material instructions different Tasks different posting coins in a bank box (each hand), threading beads; drawing a line into a trail; different trail catching a bean bag throwing bean bag onto mat standing on one leg ; walking heels raised on a line jumping on mats. What is new? Age band 2 What is new? Age band 3 Bicycle trail • • Throwing bean bag onto mat What is new? Age band 3 • • • • • • • • Turning pegs Triangle with nuts and bolts Bicycle Trail III One-hand catch Throwing at wall target Two-board balance Zig-zag hopping Walking backwards • • • • • • Turning pegs Triangle with nuts and bolts Bicycle Trail III One-hand catch Throwing at wall target Two-board balance Zig-zag hopping Walking backwards What is new? Age band 3 • • • • • • • • Turning pegs Triangle with nuts and bolts Bicycle Trail III One-hand catch Throwing at wall target Two-board balance Zig-zag hopping Walking backwards What is new? Age band 3 • • • • • • • • Norms Turning pegs Triangle with nuts and bolts Bicycle Trail III One-hand catch Throwing at wall target Two-board balance Zig-zag hopping Walking backwards 2010: Dutch standardization of MABC-2 Dutch norms deviate from UK norms!! Æ standardization in Norway is recommended. Why is early identification important? 1. Early recognition of DCD 10/21/2010 | 27 10/21/2010 | 28 DCD is often not diagnosed until the age Decreased Physical fitness of 5 or 6. Less social ParticipationÆ Decreased self-esteem At risk for co-morbidity Reason: before that age, motor development can be rather variable. Little is known about possible risk factors! Early recognition of DCD is important Early Intervention Variability in motor development 102 typically developing children at 23 months Also measured at 9,11, 13,16 and 21 months Gross motor signs of DCD in the pre-school child:‘red flags’ 10/21/2010 | 30 Frequency of scores below the 16th percentile Gross motor skills Fine motor skills 1x 2x 3x 4x 5x 16 8 7 2 3 21 11 7 1 0 Darrah et al., (2003) Early Human Development, 72(2), 97-110 › › › › › › Delayed motor mile stones Falls often Difficulty jumping or skipping Dislikes climbing (anxious) Late riding tricycle; Cannot ride bicycle Fatigues easily Fine motor signs of DCD in the pre-school child 10/21/2010 | 31 Instruments for 3-5 year old children 10/21/2010 | 32 Early Years Movement Skill (3-5 years) › Little interest in construction play › Difficulty manipulating small objects (LEGO, puzzles) › Difficulty using utensil (pencil, scissors) › Difficulty with bimanual activities › (doing up buttons, cutting) Recently developed questionnaire: 23 items Limited information about reliability and validity MABC2 (2007): ageband 1: 3-5 years 10/21/2010 | 33 Little DCD-Q 3-5 years of age 15 items To be filled out by parents Proposed motor function assessment: prenatal period to age 5 years1 Phase I: Screening for motor function difficulties in the preschool years Failure to meet motor milestonesÆ Ages and Stages Questionnaire Additional questions: Cross cultural study (Canada, Israel, Brasil, Belgium, England, Germany, The Netherlands) Reliability and validity Proposed motor function assessment: prenatal period to age 5 years (2) Phase II: Proposed ‘‘second-order’’ assessment of children who fail a screening phase (administration of a motor test) Phase III: Protocol for specialist (clinical) assessment to detect the onset/offset of specific developmental motor disorders (dimensional measure(s) of motor difficulty) Diagnosis (CP, DCD, Muscular dystrophy etc.) ‘‘Is there anything your baby/child is doing with their arms, legs or body movements that concerns you?’’ ‘‘Is there anything your baby/child is not doing with their arms, legs and body movements that concerns you?’’ ‘‘Is there anything that you have tried to teach your infant/child to do involving their hands or whole body movementthat has taken longer to learn than you think it should?’’ 1Rosenbaum et al. (2009) Conclusion early identification of DCD 10/21/2010 | 36 Difficult before the age of 5 Before the age of 5: DCD should not ne diagnosed before the age of 5!! Variability of motor development before this age Gross motor development is essentially well established by about the age of 5 years (postural control skills and locomotor skills) Children with ‘red flags’ need to be followed, as they may be at risk for DCD. 2. Identification of DCD at school age 10/21/2010 | 37 Diagnostic Criteria for Developmental Coordination Disorder (DSM-IV) Criterion A. “Performance in daily activities that require motor coordination is substantially below that expected given the person’s chronological age and measured intelligence”. Criterion B. “The disturbance in criterion A significantly interferes with academic achievement or activities of daily living.” “Tests don’t diagnose, people do!” Criterion C. “The disturbance is not due to a general medical condition (e.g., cerebral palsy, hemiplegia or muscular dystrophy) and does not meet criteria for a Pervasive Developmental Disorder.” Criterion D. “If mental retardation is present, the motor difficulties are in excess of those usually associated with it.” DSM Criterion A 10/21/2010 | 39 “Performance in daily activities that require motor coordination is substantially below that expected given the person’s chronological age and measured intelligence. This may be manifested by marked delays in achieving motor milestones (e.g., walking, crawling, sitting), dropping things, “clumsiness”, poor performance in sports, or poor handwriting. ” (DSM-IV-TR, 2000 p. 58). Leeds Criterion A. Diagnosis 10/21/2010 | 40 Developmental coordination disorder (DCD) is evident when there is a marked impairment in the performance of motor skills. Core aspects of the disorder include difficulties with gross and/or fine motor skills, which may be apparent in locomotion, agility, manual dexterity, complex skills (e.g. ball games) and /or balance. Individually administered and culturally appropriate, How do we measure criterion A? What is meant with ‘substantially below’? norm-referenced test of general motor competence. The cut off point at or below the 5th percentile. Checklists may be used as an initial screening tool. Children that score below the 15th should be monitored Norm referenced motor tests Available tests BGMA Basic Gross Motor Assessment Advantages: Objective standardized BOT-2 Bruininks-Oseretsky Test 2nd ed. M-ABC Movement Assessment Battery for Children Disadvantages: Snapshot Æ Influence of performance variables (fatigue, anxiety) Time consuming Qualified tester is necessary MAND McCarron Assessment of Neuromuscular Development PDMS-2 Peabody Developmental Motor Scale 2nd ed. TGMD-2 Test of Gross Motor Development ZNA Zurich Neuromotor Assessment 10/21/2010 | 41 10/21/2010 | 42 Best rated tests1 10/21/2010 | 43 M-ABC 2001: used in 67% of the studies published until then Most popular test for DCD at the moment Reliable and valid TGMD-2 Not often used in DCD population Validity and reliability only demonstrated for TD group DSM Criterion B 10/21/2010 | 44 “The disturbance in criterion A significantly interferes with academic achievement or activities of daily living.” (DSM-IV-TR, 2000 p. 58). academic achievement: writing and physical education activities of daily living: drawing/writing, dressing, locomotion, speech and use of tools/objects Bruininks- Oseretsky Test Used in 6% of the studies published until 2001 Reliability and validity have been critized Mainly used in USA 1 Slater et al. (2010). Pediatric Physical Therapy Leeds Criterion B. Diagnosis 10/21/2010 | 45 The specific skill of handwriting is usually affected, and is known to adversely affect academic achievement and should therefore be assessed. Tests for measuring ADL? MABC(2) – test for motor skills, but not for ADL PEDI Assessment should reflect culturally relevant developmental norms relating to activities of daily living tasks and should include consideration of self-care, play, leisure and schoolwork (including handwriting, PE and tool use). – is not discriminative enough for use in children with DCD (School)-AMPS (Assessment of Motor and Process Skills) – limited to functional skills at school How to measure criterion B? How to measure criterion B? 10/21/2010 | 47 10/21/2010 | 48 At present no test of ADL has been developed. Questionnaires are used to assess functioning in ADL tasks Advantage: Performance across a larger time scale is taken into account Fast and easy to administer Disadvantage: Subjective, raters may lack sufficient knowledge to rate motor behavior (knowlegde of motor development) Parent-questionnaire Teacher-questionnaires DCD-Q Checklist-Movement ABC Motor Observation Questionnaire for Teachers (MOQ-T, previously called GMO) TEAF Child-questionnaire Children’s self-perception of adequacy in and predilection for physical activity (CSAPPA) Checklist Movement-ABC2 10/21/2010 | 49 Aim: assessment of motor performance of children in the school environment • Age: children from 4 to 12 years of age • To be filled out by teachers • 30 questions, divided over 2 sections Section 1 The child is stationary and the environment stable Stand on one leg in a stable position. Section 3 The child is stationary and the environment is changing Intercept and stop a moving object as it approaches. Checklist MM-ABC: reliable and valid (Schoemaker et al., submitted)) 3 Sections 10/21/2010 | 51 2 Motor section (A and B) Section 2 The child is moving and the environment stable Skip or gallop a distance of 4.5 meter. Section A Section 4 The child is moving and the environment is changing Run to catch an Approaching ball. Section B MOQ-T Motor Observation Questionnaire for Teachers 10/21/2010 | 52 Aim: screening of movement problems at school by 1 Non-motor section (section C: teachers impulsiveness, distractibility, passiveness, upset by failure etc.) Scoring: Total Test Score (summed score for sections A and B) Interpretation: Traffic Light system age: 5 - 12 yrs filled in by: teacher; requested time 5 minutes 18 items, measuring 2 factors: General motor functioning handwriting Separate norms for age and gender MOQMOQ-T (previously: GMO): reliable and valid (see Schoemaker et al, 2008) DCD-Q Developmental Coordination Disorder-Questionnaire 10/21/2010 | 53 Aim: screening of problems with gross and fine motor coordination . age: 8 to 14;6 yrs filled in by: parent(s); approximately 5 minutes 15 items; 3 factors: Motor control Fine motor skills / handwriting General coordination DCDDCD-Q : reliable and valid (see Wilson et al., 2000; Schoemaker et al., 2006)) New instrument for ADL To develop an instrument to assess ADL in children with DCD Goals: Representative set of ADL Objective and systematic 30 Minutes Development of a new measuring instrument for ADL skills 10/21/2010 | 55 To be used in addition to the M-ABC Literature study and expert interviews To compose a list of ADL skills that might be difficult for children with DCD The DCDDaily (Van der Linde, Van Netten, Schoemaker) 10/21/2010 | 56 DCDDaily: Motor assessment Reflect ‘A normal day’ Self-maintenance (home) Productivity (school) Play 21 items Expert meeting Scoring: performance and speed (good, moderate, poor) DCDDaily-Questionnaire (child and parent) (Occupational model, Dunford et al., 2005; DCDDaily: items Reed and Sanderson, 1992) Movie 1 10/21/2010 | 57 ‘Home’ Cutting gingerbread Box and Bag Walk to school ‘School’ Tinkering: folding, coloring, cutting Constructional play: Lego Handwriting ‘Break’ Pooring a drink Walking with drink to table ‘Shopping’ Dressing: socks, polo-shirt, trousers, body warmer ‘Outdoor play activities’ Playing with marbles Hopping Discriminative ability 10/21/2010 | 60 23 DCD and 72 TD (6-8 years) Discriminative ability How to use the DCD-Daily? (nDCD = 17; nTD = 69) To assist in assising criterion B To get an impression of problems with 3 functional skills at home or at school To evaluate treatment Item scores 2,5 DCD TD 2 Treatment: shift from process-oriented to more functional task-oriented approaches. 1,5 1 13* 10* 20* 8* 9* 5 7* 2* 6* 15* 17* 12* 18* 14* 4* 1* 11* 19* 21* 3 16* Items Usefulness of questionnaires for identification of children with DCD? Conclusion 10/21/2010 | 64 Present situation: Only questionnaires are available to assess ADL performance and to decide whether the performance of a child meets Criterion B. Important aspects of a screening instrument: Two samples: Random sample (children from mainstream schools) Referred sample (50% children referred to child rehabilitation; 50% control children) 10/21/2010 | 65 Sensitivity Specificity Can only be reliably determined if there is an accepted gold standard. 10/21/2010 | 66 Sensitivity: The percentage of children who fail the M-ABC who are correctly identified by a screenings-instrument. In Table: a / (a+c) Gold standard: a diagnostic test that is regarded as definitive A hypothetical ideal gold standard test has a : sensitivity, of 100% (it identifies all individuals with a disease; it does not have any false-negative results) specificity of 100% (it does not falsely identify someone with a condition that does not have the condition; it does not have any false-positive results). DCD: gold standard: ???? Æ does not exist! But: M-ABC is often used as a gold standard Questionnaire DCD (< 15th %) No DCD > 15th % DCD a c M-ABC No DCD b d Sensitivity of the questionnaires (M-ABC is gold standard (15th % cut-off criterion)) 10/21/2010 | 67 Sensitivity Specificity: The percentage of children who pass the M-ABC who are correctly identified by a screenings-instrument. In Table: d / (b+d) Questionnaire DCD (< 15th %) No DCD > 15th % DCD a M-ABC No DCD b c False positives Referred sample Checklist M-ABC 2 44% ?? DCD-Q 29% 82% MOQ-T 39% 81% d Specificity of the questionnaires (M-ABC is gold standard (15th % cut-off criterion)) Specificity Random sample Random sample Conclusion 10/21/2010 | 70 Sensitivity of questionnaires: is good in referred sample, but too low for population screening (random sample) Referred sample Checklist MABC2 91% ?? DCD-Q 89% 89% MOQ-T 89% 62% Specificity of questionnaires: Is good for population screening, Is good for DCD-Q in referred sample but slightly too low for MOQ-T in referred sample Why should we be careful to use the M-ABC as a gold standard? 10/21/2010 | 71 1. DCD is a heterogeneous disorder 2. M-ABC does not cover the full range of motor abilities that might be implicated. 10/21/2010 | 72 Motor Abilities Prospective study 1 2 M-ABC VMI BHK (handwriting) IQ-test (WISC-R) Child Behavior Check List Teacher Report Form 3 4 Motor performance 5 6 7 8 Outcome Prospective study (N=107, all referred) Features of “Non-DCD group” DCD M-ABC < 15th percentile Non-DCD (M-ABC > 15th percentile M-ABC 86 (80%) 21 (20%) Medical problem 0 2 IQ < 70 0 1 Co-morbidity according to CBCLscores 58% 52% 13 out of 19 non-DCD children had fine motor problems : Handwriting (BHK) Visuo-motor problems (VMI) Conclusion: When only the M-ABC is used for criterion A, children with fine motor disorders may be missed. 3. What is the agreement between different measures designed to identify children with DCD? Participants: 10/21/2010 | 77 Teachers Parents MOQ-T DCD-Q Children M-ABC 10/21/2010 | 78 Random sample: • 233 children (126 boys / 107 girls) • Age range 5-11 years old • Mean age: 8 years 1 months • All attending meanstream schools Referred sample: • 76 children (68 boys / 8 girls) • Age range 5-11 years old • Mean age: 7 years 3 months • Referred to rehabilitation clinic for coordination problems. Random sample M-ABC 15th percentile Population sample (N=233) 10/21/2010 | 80 DCD-Q 6% Instruments identify partly MOQ-T 3.8% 1.7% 6.4% 5% 4% 4.7% 9.8% N=21 M-ABC the same partly different children If 15th centile is used, only 4% of the children (n=10) are identified by all measures (1.7 % (n=4) if the 5th centile is used) M-ABC does not identify children with primarily fine motor problems (n=9) Using failure on the MABC as the only criterion for DCD might lead to over-identification (21/233). DCD-Q < 15th % or MOQ-T < 15th % 24% 56/233 M-ABC < 15th % M-ABC < 5th % 9% 21/233 4% 9/233 Referred sample (N=76) Referred sample 10/21/2010 | 82 DCD-Q 1% MOQ-T 13% 4% 54% 9% 7% 5% M-ABC Overlap between measures is relatively large. 6.4% 13% of the children are not identified by the MABC because of fine motor problems Not all children referred to a rehabilitation clinic can be diagnosed as DCD (other developmental, school or educational problems) Conclusions DCD-Q < 15th % or MOQ-T < 15th % 88% 67/76 M-ABC < 15th % 70% 53/76 M-ABC < 5th % 51% 39/76 Conclusion 10/21/2010 | 83 1. Some children fail on the MABC but do not have problems according to either parents or teachers. 2. Children with fine motor problems might be missed when only the M-ABC is used as an instrument to identify children with DCD. 3. Multiple measures are recommended to be used to identify children with DCD 10/21/2010 | 84 Identification of children with DCD: not as easy as it seems to be! Multiple measures are needed to identify children with DCD in a reliable way, according to the diagnostic criteria for DCD The development of new measuring instruments might be helpful in the identification process.
© Copyright 2026