Validity and reliability of the Movement Assessment Battery for
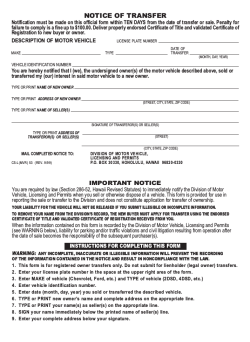
DEVELOPMENTAL MEDICINE & CHILD NEUROLOGY ORIGINAL ARTICLE Validity and reliability of the Movement Assessment Battery for Children-2 Checklist for children with and without motor impairments MARINA M SCHOEMAKER 1 | ANUSCHKA S NIEMEIJER 2 | BOUDIEN C T FLAPPER 3 , 4 | BOUWIEN C M SMITS-ENGELSMAN 5 , 6 1 Centre for Human Movement Sciences, University Medical Center Groningen, University of Groningen, Groningen, the Netherlands. 2 Sint Maartenskliniek, Research Development and Education, Nijmegen, the Netherlands. 3 Department of Paediatrics, Effatha Guyot Centre, Groningen, the Netherlands. 4 University Medical Center Groningen, Groningen, the Netherlands. 5 Avans+, University for Professionals, Breda, the Netherlands. 6 Faculty of Kinesiology and Rehabilitation Sciences, KU Leuven, Belgium. Correspondence to Dr Marina M Schoemaker, University Medical Center Groningen, Sector F, Center for Human Movement Sciences, PO Box 196, 9700 AD Groningen, the Netherlands. E-mail: [email protected] PUBLICATION DATA AIM The aim of this study was to investigate the validity and reliability of the Movement Accepted for publication 4th October 2011. Published online 9th February 2012. METHOD Teachers completed the Checklist for 383 children (age range 5–8y; mean age 6y 9mo; ABBREVIATIONS DCD DCDQ'07 MABC-2 TMS TTS Developmental coordination disorder Developmental Disorder Coordination Questionnaire 2007 Movement Assessment Battery for Children-2 Total motor score Total test score Assessment Battery for Children-2 Checklist (MABC-2). 190 males; 193 females) and the parents of 130 of these children completed the Developmental Disorder Coordination Questionnaire 2007 (DCDQ’07). All children were assessed with the MABC2 Test. The internal consistency of the 30 items of the Checklist was determined to measure reliability. Construct validity was investigated using factor analysis and discriminative validity was assessed by comparing the scores of children with and without movement difficulties. Concurrent validity was measured by calculating correlations between the Checklist, Test, and the DCDQ’07. Incremental validity was assessed to determine whether the Checklist was a better predictor of motor impairment than the DCDQ’07. Sensitivity and specificity were investigated using the MABC-2 Test as reference standard (cut-off 15th centile). RESULTS The Checklist items measure the same construct. Six factors were obtained after factor analysis. This implies that a broad range of functional activities can be assessed with the Checklist, which renders the Checklist useful for assessing criterion B of the diagnostic criteria for DCD. The mean Checklist scores for children with and without motor impairments significantly differed (p<0.001). The scores for the Checklist ⁄ Test and DCDQ’07 were significantly correlated (rS=)0.38 and p<0.001, and rS=)0.36 and p<0.001, respectively). The Checklist better predicted motor impairment than the DCDQ’07. Overall, the sensitivity was low (41%) and the specificity was acceptable (88%). INTERPRETATION The Checklist meets standards for validity and reliability. According to the diagnostic criteria in the DSM-IV-TR,1 children with developmental coordination disorder (DCD) have a marked impairment in motor coordination which hampers the performance of academic and daily-life motor skills, without evidence of a medical disorder or intellectual impairment.1 Early identification of the condition is recommended,2–4 but correct identification is impeded by the lack of a universally accepted criterion standard for DCD.5,6 To solve this problem, a multiple assessment approach has been advocated to assess whether the inclusion criteria for DCD have been met.7–9 Motor questionnaires can be used to investigate whether the performance of daily-life motor skills at home or at school is affected (criterion B). A motor test can also be administered to assess the extent and severity of the movement difficulties (criterion A). Several questionnaires have been developed to gather information about functional motor performance from parents (Developmental Disorder Coordination Questionnaire 2007 [DCDQ’07];10 Children Activity Scales for Parents11), teachers (Teacher Estimation of Activity Form;12 Motor Observation Questionnaire for Teachers;13 Children Activity Scales for Teachers;11 Movement Assessment Battery for Children Checklist [MABC Checklist]14,15), or from the children themselves (Children’s Self-perceptions of Adequacy in and Predilection for Physical Activity16). Few motor tests are available to assess objectively the severity and extent of children’s movement difficulties (e.g. MABC-215 and the Bruininks–Oseretsky Test of Motor Proficiency); the MABC is most commonly used in research.17 Despite the popularity of the MABC Test, its counterpart, the MABC Checklist, has been used far less often in clinical studies. One of the reasons for this is probably its length (48 items), which has rendered it too laborious to administer. Recently, both the Test and the Checklist of the MABC have been revised.15 The length of the Checklist has been reduced to 30 items, and the content of some of the items has 368 DOI: 10.1111/j.1469-8749.2012.04226.x ª The Authors. Developmental Medicine & Child Neurology ª 2012 Mac Keith Press been changed. Although the reliability and validity of the original version of the Checklist have been investigated,7,8,18 a limitation of the revised version is the lack of research on its reliability and validity.19 Therefore, the aim of the present study was to investigate these psychometric properties. The internal consistency of the items of the Checklist was investigated as a measure of reliability. Concurrent validity was examined in two ways: first, by conducting correlations between the Checklist, the Test, and the DCDQ’07 as a parental questionnaire and, second, by investigating whether children with scores in the clinical range on the MABC-2 Checklist also fail on the Test. In order to diagnose a child with DCD, both criteria A and B of the diagnostic criteria for DCD have to be met. According to the manual,15 one of the functions of the Checklist is to assist in diagnosing DCD as it provides a view of how a child performs everyday movement tasks at home or at school (criterion B). The MABC-2 Test is often used to ascertain whether criterion A has been met (i.e. there is a marked impairment in motor coordination). Consequently, the classification agreement between Test and Checklist is interesting from both a clinical and a psychometric point of view. Lastly, the extent to which the Checklist has any added value with respect to existing questionnaires was addressed by investigating whether the Checklist increased detection of motor impairment compared with the DCDQ’07,10 a popular parental questionnaire used to identify children with DCD. METHOD Participants The Dutch standardization study of the MABC-2 includes a Dutch and a Flemish (Dutch-speaking part of Belgium) sample. The Dutch sample is representative of the Dutch population regarding sociodemographic status (ethnicity, parental educational level, distribution of geographic region; see the manual of the Dutch MABC-220). For the standardization study, teachers were asked to randomly select five Dutch children aged between 3 and 16 years from their school class, which gave a total of 825 students. Of these students, all 500 students aged 5 to 8 years were selected for the present study. The teachers of these students were asked to fill out the Checklist. The participating teachers had on average 12 years’ teaching experience (range 1–40y). Of the 447 Checklists that were returned, 64 had to be excluded because more than three items in one section were missing, giving a final sample of 383 children (86%). Five items were difficult to fill out for teachers; presumably those skills are not regularly observed in a school situation: (A1.5, ‘Pours liquid from one container to another’; B22, ‘Hits a moving ball with a bat’; B25, ‘Participates in a team game’; B31, ‘Rides a bicycle without stabilizers’; B3,3 ‘Maintains balance in water’). All 383 children were assessed with the MABC-2 Test, which has eight items, and gives a total test score ranging from 8 to 152. About one-third of the parents of the 383 participating children (randomly selected) were asked to fill out the DCDQ’07 (n=130). Either the father or the mother could fill out the questionnaire. The educational level of the father was measured on a 5-point scale What this paper adds • This is the first study to investigate the reliability and validity of the MABC-2 Checklist. • The Checklist can discriminate between children with and without motor impairment. • The Checklist is useful for assessing criterion B of the diagnostic criteria for developmental disorder coordination. as a predictor of socio-economic status (1=only primary school education; 5=university education). The median educational level of the father (3.0) was representative of the educational level in the Dutch population. Informed consent was obtained from parents of the children. The study was approved by the local medical ethics committee. Procedure Sixteen therapists (mean age 25y) with at least 4 years’ experience in the administration of MABC-1 were trained to administer the revised version of the MABC-2 Test. The MABC-2 Test (age bands 1 and 2) was administered in a quiet room at each child’s school. Instruments MABC-2 Checklist The Dutch translation of the Checklist with accompanying Dutch norms was used in this study. A forward–back translation procedure was adopted to translate the Checklist into Dutch. The Checklist is designed to identify children with motor difficulties in the age range 5 to 11 years. It has a motor and a non-motor part. The motor part contains 30 items divided into two sections. Section A measures movement in a static and ⁄ or predictable environment and section B measures movement in a dynamic and ⁄ or unpredictable environment. The non-motor part was outside the scope of the present study. Each section is subdivided into three parts, each containing five items. Section A measures self-care skills, classroom skills, and physical education ⁄ recreational skills; section B measures self-care ⁄ recreational skills, ball skills, and physical education ⁄ recreational skills. For each item, teachers have to rate the motor competence of a child on a 4-point scale (0=very well; 3=not close). The total motor score (TMS) is the sum of the 30-item scores; the higher the TMS, the poorer the performance. According to the manual of the MABC-2,15 children with scores at or above the 95th centile are highly likely to have a motor impairment in daily-life, children with scores between the 85th and 94th centile are ‘at risk’ of having a motor impairment, and children with scores up to the 85th centile have no detectable motor impairment. Movement ABC-2 Test The aim of the Test is to classify children of 3 to 16 years 11 months of age according to degree of motor impairment. There are three age-related item sets, each consisting of eight items measuring manual dexterity (three items), aiming and catching (two items), and balance (three items). Following the procedure described in the MABC-2 manual,15 item scores can be transformed into standard scores (mean=10; Validity of the MABC-2 Checklist Marina M Schoemaker et al. 369 SD=3).15 The total test score (TTS) is the sum of the eightitem standard scores (range 8–152). Standard scores are also provided in the manual for the TTS (mean=10; SD=3).15 Test–retest reliability of the TTS is good (0.80).15,20,21 The previous version of this Test had acceptable validity, but so far information about the validity of the revised version is limited.19 Dutch norms of the Test and Checklist were used in this study.20 DCDQ'07 The DCDQ’07 is a parent questionnaire developed to identify motor problems in children aged from 5 to 15 years.10 The questionnaire contains 15 items regarding motor coordination. For each item, parents have to compare the degree of coordination of their child with other children of the same age, and rate this on a 5-point scale. By adding the scores for each item, a total DCDQ score can be calculated. The higher the score, the better the motor performance level. The internal consistency of the questionnaire is high (Cronbach’s alpha=0.89). Data analysis When fewer than four questions on the Checklist contained missing values, missing values were replaced as instructed in the manual of the MABC-2.15 If an item was missing from any of the subsections within either section A or B, then the remaining four items in that section were reviewed. If the child’s scores were 0 or 1, than a score of ‘1’ was assigned for the missing item, if the scores were 2 or 3, than a score of ‘2’ was assigned for the missing item. In cases where scores were mixed, a score of ‘1’ was assigned.15 Reliability Cronbach’s alpha was calculated to determine the degree of consistency among the 30 motor items of the Checklist. Construct validity In order to explore which items of the Checklist cluster together in a meaningful way, a factor analysis (principal components analysis with varimax rotation) was carried out on the raw item scores. Varimax rotation was used to maximize the loading of each item onto one of the extracted factors whilst minimizing the loading on all other factors. This simplifies the interpretation as it results in a small number of items loading highly onto each factor.22 The factor structure is achieved by looking for items that correlate highly with other items (loading >0.40) but do not correlate with other items outside that group. A two-way analysis of variance was carried out to investigate the effects of age (4) and sex (2) on the TMS of the Checklist. As the assumption of homogeneity of variance was violated, the analysis was performed on the logarithmic transformation of the TMS scores. Discriminant validity In the present study, the sample was split into two groups, a group with standard scores up to 7 on the MABC-2 Test (including children with significant motor impairment and 370 Developmental Medicine & Child Neurology 2012, 54: 368–375 those at risk for motor impairment; henceforth called the group with motor impairments) and a typically developing group with total standard scores above 7 on the MABC-2 Test. A total standard score of 7 is associated as closely as possible with the 15th centile cut-off. The 15th centile was chosen as the cut-off point as it is recommended in the European guidelines for assessment and intervention for DCD as the cut-off point for motor impairment when using a motor test. A logistic regression analysis was performed in order to predict the classification of children with and without motor impairments, with TMS scores as the predictor variable. A receiver operating characteristic curve was composed in order to provide a graphical picture of the ability of the Checklist to discriminate between children with and without motor impairment based upon their MABC-2 test scores. In addition, the mean TMS of the group with motor impairments was compared with the mean TMS of the typically developing group (analysis of variance). The number of items per age group for which significant differences were obtained (t-test) between the groups was also calculated in order to investigate the discriminative ability of the Checklist across age groups. Concurrent validity The degree of concurrent validity between the Test and the Checklist and between the DCDQ’07 and the Checklist was examined using Spearman’s rank order correlation on MABC2 TSS, DCDQ’07 total scores, and the Checklist’s TMS. The concurrent validity was also investigated by calculating the percentage of agreement between the Checklist and the Test in classifying children as those with motor impairment (impaired and at-risk groups) and those without motor impairment, and by calculating the sensitivity and specificity of the Checklist. Sensitivity refers to the percentage of children with problems according to the Test that is correctly detected by the Checklist (80% is preferable).23 Specificity refers to the percentage of children without problems who are correctly identified (90% is preferable). Cohen’s kappa was calculated to evaluate the proportion of agreements that is actually observed between the Checklist and the Test in classifying children as those with and those without motor impairment after adjusting for the proportion of agreements that take place by chance.24 Incremental validity Logistic regression analysis was conducted to determine whether TMS scores of the Checklist or DCDQ’07 total scores were better able to predict the presence or absence of motor impairment on the MABC-2 Test. Logistic regression was chosen as the outcome was a categorical variable (children with motor impairments [standard scores £7 on MABC-2 Test] vs typically developing children [standard scores >7]). In step 1, the DCDQ’07 total scores were entered as predictor variables with age and sex as possible confounders. In step 2, the Checklist’s TMS were added. The assumptions for regression analysis (i.e. no multicollinearity) were checked beforehand. Alpha was set at 0.05. Table I: Mean (SD) total motor scores for the Movement Assessment Battery for Children-2 (MABC-2) Checklist and mean (SD) total standard scores for the MABC-2 Test for age and sex separately Age (y) n 5 97 6 94 7 84 8 108 Total 383 Sex (n) Checklist total motor score MABC-2 total standard score Males (47) Females (50) Males (51) Females (43) Males (48) Females (36) Males (44) Females (64) Males (190) Females (193) 11.9 (11.2) 11.8 (10.6) 11.5 (10.6) 7.3 (6.8) 10.6 (11.6) 3.2 (4.6) 4.8 (6.3) 2.2 (3.2) 9.7 (11.2) 6.0 (7.8) 9.2 (3.4) 9.3 (3.2) 9.0 (3.2) 10.5 (3.1) 8.7 (3.5) 11.5 (3.4) 9.2 (3.4) 11.1 (3.2) 9.0 (3.4) 10.6 (3.4) RESULTS Table I provides an overview of the number of children across age and sex, and the mean and SD of scores on the Checklist and Test. Twenty-five per cent of the Checklists had one, two, or three items missing, which in the majority of cases included the item ‘Maintains balance in water among other children (B3.3)’, as teachers in the Netherlands generally do not observe children in water. Construct validity Cronbach’s alpha was 0.94 for all 30 items together, suggesting that all items measure the same construct. Factor structure of the motor items of the Checklist Six factors were extracted with an eigenvalue of less than 1, which together explain 69% of the variance (see Table II for an overview of the six factors, their content, and factor loading). The first factor explained most of the variance (20%) and was formed by items requiring gross motor coordination during self-care or classroom activities. Factor 2 was formed by items involving ball skills, factor 3 by items measuring recreational skills, factor 4 by items measuring fine motor skills, factor 5 by items that measure the ability to keep rhythm, and factor 6 by items that involve dynamic balance. Three items did not load on any factor: A1.5, ‘Pours liquid from one container to another’; A3.3, ‘Throws a beanbag or ball so that another stationary child can catch it’; and B3.1, ‘Rides a bicycle without stabilisers’. Teachers noted that two of these items (A1.5 and B3.1) were difficult to fill out as they can generally not be observed in a school setting (missing data: 19% for both items). A significant effect of age (F3,375=21.329; p<0.001) and sex (F1,375=14.056; p<0.001) was obtained for the TMS, as well as a significant interaction between them (F3,375=2.651; p=0.049). As the effect of age was significant, post-hoc analyses were carried out for age using the Bonferroni procedure. The results revealed that the mean TMS of 8-year-old children differed significantly from the mean TMS of all other age groups. The mean TMS of the 6- and 7-year-old children did not differ significantly from each other, but did differ significantly from those of the 5- and 8-year-old children. The TMS were equal for males and females at 5 years of age, but after that age the mean TMSs of males declined less than those of females. Discriminant validity The TMS was a significant predictor of motor impairment ⁄ non-motor impairment (B [standard error, SE]=)0.082 [0.015]; p<0.001 [odds ratio 0.92; CI 0.90–0.95]). Figure 1 shows the ability of the Checklist to discriminate between children with and without motor impairment based upon their MABC-2 Test scores. The results of the analysis of variance revealed that, for each age group, the mean TMSs of children in the group with motor impairments significantly differed from those of children in the typically developing group (see Table III). The number of items discriminating significantly between the group with motor impairments and the typically developing group for 5-, 6-, 7-, and 8-year-old children was respectively 21, 16, 22, and 11 out of 30 items. Concurrent validity A significant correlation (Spearman’s rho) was obtained between the TMS and the TTS (rS=)0.38; p<0.001; n=383), and between the total scores of the DCDQ’07 and the TMS (rS=)0.36; p<0.001; n=130). The groups used for calculating the correlation between the TMS and the TTS, on the one hand, and the TMS and the DCDQ’07, on the other hand, did not differ significantly in age (6y 9mo and 6y 8mo, respectively; p=0.12). The correlation between the TMS and the TTS for the smaller group (n=130) was comparable to that of the whole group (rS=)0.35; p<0.001). The percentage agreement between the Checklist and Test was 80% (307 ⁄ 383) (see Table IV). A kappa value of 0.28 was obtained, which is considered to be fair. Sensitivity was 41% (26 ⁄ 64) and specificity 88% (281 ⁄ 319) across all age groups if the 15th centile was used as a cut-off for the Test and the Checklist. Overall, 16.7% (n=64) of the children performed below the 15th centile on both instruments, and 6.8% and 5.7% performed below the 5th centile on the Test and the Checklist, respectively. Incremental validity In step 1 of the logistic regression analysis, DCDQ’07 total scores significantly predicted the outcome on the MABC-2 Test (R2=4.6%). When the Checklist TMSs were entered into the analysis in step 2, they significantly predicted the outcome on the MABC-2 Test (R2=7.3%), whereas the DCDQ’07 total scores no longer significantly added to the predicted outcome (see Table V).25 DISCUSSION The aim of this study was to investigate the psychometric properties of the motor part of the MABC-2 Checklist in a sample of children almost twice as large as the sample of 203 5- to 8-year-old children described in the MABC-2 manual.15 To start with, the internal consistency of the items of the Checklist was very good, which implies that each question addressed an aspect of functional motor performance. Validity of the MABC-2 Checklist Marina M Schoemaker et al. 371 Table II: Factor loadings of the six factors found after factor analysis on the 30 items of the motor part of the Movement Assessment Battery for Children-2 Checklist Item Maintains balance while standing to pull on clothing (A1.1) Puts on clothing over the head (A1.2) Washes and dries hands (A1.4) Walks around classroom avoiding objects and persons (A2.4) Transports objects without dropping them (A2.5) Crosses the playground avoiding collision with objects ⁄ persons (A3.5) Maintains balance when frequent adjustments are required (B1.1) Moves around a busy classroom collecting objects (B1.2) Carries a tray around a room avoiding moving persons (B1.3) Crosses the playground avoiding collision with moving persons (B3.5) Catches a ball with two hands (B2.1) Hits a moving ball with a bat (B2.2) Throws a ball on the move to another child (B2.3) Continually bounces a large ball (B2.4) Participates in a team game using skills of throwing and catching (B2.5) Uses stationary playground equipment (A3.4) Participates in chasing games (B3.2) Maintains balance in water among other children (B3.3) Uses non-stationary playground equipment (B3.4) Fastens buttons (A1.3) Manipulates small objects (A2.1) Forms letters using a pen (A2.2) Uses scissors to cut paper (A2.3) Keeps time to a musical beat by clapping hands (B1.4) Moves body in time with music (B1.5) Jumps keeping two feet together on take off and landing (A3.1) Hops on either foot (A3.2) Eigenvalue Amount of variance explained (%) Factor 1, gross motor coordination skills Factor 2, ball skills Factor 3, recreational skills Factor 4, fine motor skills 0.57a 0.57 0.51 0.79 0.18 0.09 )0.03 0.08 0.28 0.42 0.47 )0.05 0.24 0.22 0.04 0.22 0.30 0.24 0.32 0.08 0.23 )0.16 )0.09 0.15 0.82 0.79 0.10 0.14 0.05 0.09 0.11 0.10 0.14 0.02 0.14 0.25 0.63 0.07 0.26 0.16 0.26 0.26 0.71 0.64 0.14 0.32 0.32 0.11 0.16 0.19 0.22 0.34 0.15 )0.06 0.77 0.15 0.28 0.15 )0.03 0.24 0.18 0.06 0.18 0.18 0.12 0.53 0.87 0.85 0.80 0.78 0.23 0.13 0.03 0.12 0.15 0.35 0.07 0.09 0.18 )0.01 0.20 0.07 0.13 0.17 0.09 0.34 0.11 0.13 0.17 )0.03 0.21 0.04 0.16 0.23 0.33 0.29 0.19 0.27 0.30 0.25 0.33 0.04 0.22 0.30 0.07 0.20 0.01 0.15 0.03 0.28 0.28 0.20 0.69 0.76 0.56 0.79 0.32 )0.04 )0.01 0.09 0.16 0.14 0.33 )0.01 0.10 0.16 0.05 0.60 0.53 0.77 0.70 0.19 0.18 0.11 0.13 0.01 )0.06 0.14 )0.09 0.47 0.18 0.25 0.75 0.76 0.09 0.23 )0.03 0.26 0.11 )0.16 0.22 0.18 0.23 0.10 0.13 0.65 0.39 6.059 20 0.24 4.075 16 0.08 3.336 11 0.26 2.659 8 Factor 5, rhythmic skills 0.17 2.327 8 Factor 6, dynamic balance 0.58 1.815 6 a Factor loadings above 0.50 are printed in bold. Exploration of the factor structure of the Checklist revealed a six-factor solution, implying that the Checklist measures a broad range of functional motor abilities. This is important for an instrument designed to assess functional motor impairment in children at risk for DCD considering the heterogeneous nature of the disorder. In comparable questionnaires, such as the Motor Observation Questionnaire for Teachers and the DCDQ’07, gross motor skills were found to explain most of the variance. The factor solution of the Checklist is in line with these findings, as the three factors explaining most of the variance all consist of items requiring gross motor coordination. The finding that gross motor skills are covered by three factors instead of one is probably due to the larger number of items in the Checklist that cover a particular aspect of gross motor performance, such as ball skills or recreational skills, which cluster together. In addition, similar to the Motor Observation Questionnaire for Teachers and the DCDQ’07, 372 Developmental Medicine & Child Neurology 2012, 54: 368–375 a factor covering fine motor skills was found. Factor analysis on the Checklist also revealed two additional factors (rhythmic skills and dynamic balance skills) which did not appear as separate factors in the DCDQ’07 or Motor Observation Questionnaire for Teachers, either because none of the items referred to these skills or because they were covered by only one item. Significant but moderate correlations were obtained between the Checklist and the Test scores ()0.38), and between the Checklist and the DCDQ’07 ()0.36), which implies that these instruments assess both overlapping but also slightly distinct motor skills. The obtained correlation between the Checklist and the Test is lower than that found in the UK standardization sample for 5- to 12-year-old children ()0.55) (Barnett A, personal communication 2010) and also lower than the correlations reported in previous populationbased studies between the original MABC Test and Checklist, which varied between 0.44 and 0.51.8,18 1.0 ROC Curve Sensitivity 0.8 0.6 0.4 AUC=0.673 0.2 0.0 0.0 0.2 0.4 0.6 1 - Specificity 0.8 1.0 Figure 1: Receiver operating characteristic (ROC) curve for the Movement Assessment Battery for Children-2 (MABC-2) Checklist in relation to MABC-2 Test performance. AUC, area under the curve. The results regarding incremental validity imply that scores on the Checklist are a better predictor of outcome on the MABC (performance above or below 15th centile) than scores on the DCDQ’07. However, the fact that the DCDQ’07 was no longer a significant predictor of motor impairment when the Checklist was added as a predictor in the regression analysis actually indicates that the questionnaires are highly correlated. Consequently, it is too premature to conclude that teachers are better able to rate motor performance than parents. In addition, the content of the questions in both questionnaires might also be responsible for the results regarding incremental validity. A study in which both questionnaires are filled out by parents and teachers might shed more light on this issue. The Checklist was found to be able to discriminate between the group with motor impairments and the typically developing group across all ages. As expected, a developmental trend was found. Older children in both groups were able to master more functional skills than younger children according to their teachers, which was reflected in a decrease in the number of items discriminating between the two groups (age 5y: 21 out of 30 items; age 8y: 11 out of 30 items). Males obtained poorer scores on the Checklist than females. An important question is whether children with functional impairments as measured with the Checklist (Criterion B) also have motor impairments as measured with the Test (Criterion A). Overall, the classification agreement between the Checklist and the Test was 80%, which is comparable to the agreement found for the UK standardization sample (78%; Barnett A, personal communication 2010). Also, sensitivity and specificity rates were comparable in the Dutch and UK samples (sensitivity Dutch sample, 41% vs 50% in the UK sample; specificity Dutch sample, 88% vs 84% in the UK sample). This implies that only 41% of the children with motor impairments on the Test have functional motor impairments at school as measured with the Checklist. Low rates for either sensitivity or specificity are a common finding in population-based samples, irrespective of which questionnaire measuring functional motor impairment is used and irrespective of whether parents or teachers are asked to rate motor performance.3,12,18 A practical implication of these findings is that the Checklist cannot be recommended for use for population-based screening owing to its low sensitivity, which is in agreement with the advice in the manual of the MABC-2 and with the recommendations of the European Academy of Childhood Disability (EACD) for assessment and intervention for children with DCD regarding DCD questionnaires in general.15,26 Several explanations can be given for the findings regarding sensitivity and specificity. First, in the present study, a random sample of mainstream school children was included. As a consequence, the number of children with motor impairment was rather small. In addition, performance on the MABC-2 Test was only used as a criterion measure. For future studies, it might be informative to include a clinical sample of children who meet all four diagnostic criteria for DCD, as the sensitivity and specificity of an instrument can be more reliably determined in a sample in which 50% of included children have DCD.27 Second, school teachers are generally not formally trained to observe and rate motor development, which may have affected the results. Finally, the assessment of motor dysfunction is complicated by the multifactorial nature of motor capacity. To provide a reliable picture of a child’s motor skills, measurement of a large number of skills is required, especially in a heterogeneous condition such as DCD.28 However, so Table III: Mean (SD) total motor scores of the Movement Assessment Battery for Children-2 Checklist across age for the group with motor impairment ⁄ at risk for motor impairment and the typically developing group Age (y) Motor impairment ⁄ at risk for motor impairment, n (TTS £15th%) Typically developing group, n (TTS >15th%) 95% CI on difference between group means p-value 5 6 7 8 17, 22.3 (15.0) 13, 18.0 (12.3) 15, 15.3 (15.3) 19, 6.3 (7.3) 80, 9.6 (8.3) 81, 8.2 (10.0) 69, 5.3 (7.1) 89, 2.6 (3.9) 8.00–17.10 3.75–15.85 4.95–15.05 1.39–6.01 <0.001 0.002 <0.001 0.002 TTS, total test score; CI, confidence intervals. Validity of the MABC-2 Checklist Marina M Schoemaker et al. 373 Table IV: Agreement between Movement Assessment Battery for Table V: Results of logistic regression analysis with Developmental Disor- Children-2 (MABC-2) Test and Checklist in classifying a child as motor der Coordination Questionnaire 2007 (DCDQ'07) total scores and Move- impaired or not motor impaired ment Assessment Battery for Children-2 (MABC-2) Checklist scores as predictor variables and motor impairment ⁄ no motor impairment as criteMABC-2 Checklist MABC-2 Test Motor impairment No motor impairment Total rion variable Motor impairment No motor impairment Total 26 38 64 42 277 319 68 315 383 Probability that both instruments rate child as motor impaired: (68 ⁄ 383)·(64 ⁄ 383)=3%. Probability that both instruments rate child as not motor impaired: (319 ⁄ 383)·(315 ⁄ 383)=68%. Kappa=(PA)PC) ⁄ (1)PC)=(79.1)71) ⁄ (1)71)=28%. PA, observed per cent agreement=(26+277) ⁄ 383=79%. PC, per cent agreement expected from chance=71% (68%+3%). far, an empirically determined ‘criterion standard’ is lacking for the identification of DCD.27 In the absence of a true criterion standard, conclusions regarding the sensitivity and specificity of the Checklist need to be treated with caution. LIMITATIONS OF THE STUDY Only the internal consistency of the motor items could be studied as an aspect of reliability. No data regarding test–retest reliability were available. It would be worthwhile including those aspects of reliability in future studies. In addition, the psychometric properties of the Checklist were assessed in a mainstream school sample in which the number of children with movement difficulties was small. This may have influenced our findings. 95% CI for odds ratio B (SE) p-value Lower Odds ratio Upper Step 1 Age Sex DCDQ’07 )0.16 (0.22) 0.57 (0.48) 0.05 (0.02) 0.46 0.24 0.009 0.56 0.69 1.01 0.85 1.76 1.05 1.30 4.53 1.09 Step 2 Age Sex DCDQ’07 MABC-2 Checklist )0.38 (0.24) 0.33 (0.51) 0.03 (0.02) )0.07 (0.03) 0.12 0.52 0.19 0.01 0.43 0.52 0.99 0.88 0.69 1.39 1.03 0.93 1.10 3.75 1.07 0.98 R2=0.046 (Hosmer and Lemeshow)29, 0.052 (Cox and Snell)30 for step 1, R2=0.073 (Hosmer and Lemeshow), 0.081 (Cox and Snell) for step 2 (p=0.01). CLINICAL IMPLICATIONS The Checklist is a valid instrument that provides information about the performance of a child in a broad range of activities of daily living. Therefore, it is a useful tool for assessing Criterion B of the diagnostic criteria for DCD. ACKNOWLEDGEMENTS The authors would like to thank Dr Anna Barnett for her valuable comments on the manuscript. REFERENCES 1. American Psychiatric Association. DSM-IV-TR. Diagnostic and Statistical Manual of Mental Disorders, 4th edn, text revision. Washington, DC: American Psychiatric Association, 2000. 2. Jongmans MJ. Early identification of children with Developmental Coordination Disorder. In: Sugden DA, Chambers ME, editors. Children with Developmental Coordination Disorder. London: Whurr Publishers, 2005, 155–67. 3. Schoemaker MM, Flapper B, Verheij NP, Wilson BN, Rein- disorder in Singapore. Dev Med Child Neurol 1996; 38: 1099–105. 14. Henderson SE, Sugden DA. The Movement Assessment Bat- Psychometric properties of the movement ABC checklist as a tery for Children. San Antonio, TX: The Psychological Cor- screening instrument for children with Developmental Coordination Disorder. Br J Educ Psychol 2003; 73: 425–41. 9. Sugden DA. Leeds Consensus Statement: Economic Science Research Council Seminar Series. Cardiff: Dyscovery Trust, 2006. 10. Wilson BN, Crawford SG, Green D, Roberts G, Aylott A, mental Coordination Disorder Questionnaire as a screening Kaplan BJ. Psychometric properties of the revised Develop- instrument. Dev Med Child Neurol 2006; 48: 668–73. mental Motor Coordination Questionnaire. Phys Occup Ther Pediatr 2009; 29: 182–202. BE, Hay JA. Evaluating the CSAPPA sub-scales as potential 11. Rosenblum S. The development and standardization of the screening for developmental coordination disorder. Arch Dis Children Activity Scales (ChAS-P ⁄ T) for the early identifica- Child 2007; 92: 987–91. tion of children with developmental coordination disorders. 5. Henderson SE, Barnett AL. The classification of specific motor coordination disorders in children: some problems to be solved. Hum Mov Sci 1998; 17: 449–69. 6. Larkin D, Rose E. Assessment of developmental coordination disorder. In: Sugden DA, Chambers ME, editors. Children with Developmental Coordination Disorder. London: Whurr Publishers, 2005: 135–54. 7. Wright HC, Sugden DA. A two-step procedure for the iden- 27: 190–9. 8. Schoemaker MM, Smits-Engelsman BCM, Jongmans MJ. ders-Messelink HA, De Kloet A. Evaluation of the Develop- 4. Cairney J, Veldhuizen S, Kurdyak P, Missiuna C, Faught developmental coordination disorder. Hum Mov Sci 2008; Child Care Health Dev 2006; 32: 619–32. 12. Faught BE, Cairney J, Hay J, Veldhuizen S, Missiuna C, Spi- poration, 1992. 15. Henderson SE, Sugden DA, Barnett AL. Movement Assessment Battery for Children – 2 Examiner’s Manual. London: Harcourt Assessment, 2007. 16. Hay JA, Hawes R, Faught BE. Evaluation of a screening instrument for developmental coordination disorder. J Adolesc Health 2004; 34: 308–13. 17. Geuze RH, Jongmans MJ, Schoemaker MM, Smits-Engelsman BCM. Clinical and research diagnostic criteria for developmental coordination disorder: a review and discussion. Hum Mov Sci 2001; 20: 7–47. 18. Junaid K, Harris SR, Carswell A. Teacher’s use of the MABC Checklist to identify children with motor difficulties. Pediatr Phys Ther 2000; 12: 158–63. ronello CA. Screening for motor coordination challenges in 19. Brown T, Lalor A. The Movement Assessment Battery for children using teacher ratings of physical ability and activity. Children-Second Edition (MABC-2): a review and a critique. Hum Mov Sci 2008; 27: 177–89. Phys Occup Ther Pediatr 2009; 29: 86–103. 13. Schoemaker MM, Flapper BCT, Reinders-Messelink HA, 20. Smits-Engelsman BCM. Movement Assessment Battery for De Kloet A. Validity of the motor observation questionnaire Children-2. Dutch Standardization. Pearson Education: for teachers as a screening instrument for children at risk for Amsterdam, 2010. tification of children with developmental co-ordination 374 Developmental Medicine & Child Neurology 2012, 54: 368–375 21. Smits-Engelsman BC, Niemeijer AS, van Waelvelde H. Is 25. Hunsley J, Meyer GJ. The incremental validity of psycholog- the Movement Assessment Battery for Children-2nd edition ical testing and assessment: conceptual, methodological, and a reliable instrument to measure motor performance in statistical issues. Psychol Assessment 2003; 15: 446–55. 3 year old children? Res Dev Disabil 2011; 32: 1370–7. 22. Field A. Discovering Statistics using SPSS. London: Sage Publications, 2005. 23. American Psychological Association. Standards for Educational and Psychological Tests. Washington, DC: American Psychological Association, 1985. 24. Cohen J. A coefficient of agreement for nominal scales. Educ with Developmental Coordination Disorder? Br J Occup Ther 2005; 68: 2–10. 28. Cools W, De Martelaer K, Samaey C, Andries C. Movement 26. Blank R, Smits-Engelsman B, Polatajko H, Wilson P. Euro- skill assessment of typically developing preschool children: a pean Academy for Childhood Disability (EACD): recom- review of seven movement skill assessment tools. J Sports mendations on the definition, diagnosis and intervention of developmental coordination disorder (long version). Dev Med Child Neurol 2012; 54: 54–93. Sci Med 2008; 8: 154–68. 29. Hosmer DW, Lemeshow S. Applied Logistic Regression. New York: Wiley, 1989. 27. Green D, Bishop T, Wilson BN, et al. Is questionnaire-based screening part of the solution to waiting lists for children 30. Cox DR, Snell DJ. The Analysis of Binary Data, 2nd edn. London: Chapman & Hall, 1989. Psychol Meas 1960; 20: 37–47. Validity of the MABC-2 Checklist Marina M Schoemaker et al. 375
© Copyright 2026