Recent advances in the treatment of scoliosis in children Focus On Genetics
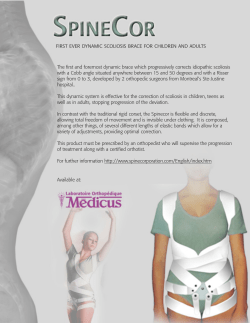
Focus On Recent advances in the treatment of scoliosis in children Genetics Adolescent idiopathic scoliosis (AIS) has been shown in both clinical and genetic studies to have a genetic component to its aetiology,1-8 although the pattern of inheritance still remains elusive; X-linked dominant,3 autosomal dominant or multifactorial patterns1,2,7 have all been suggested. Genealogy work with a cohort of 145 patients with AIS demonstrated a 97% connectedness to other families with AIS, with differences in both expressivity and penetrance, suggesting that there is more than one gene responsible for AIS.9 Work using genome-wide scanning continues to support this hypothesis by identifying specific areas on the human genome which are potentially significant in the aetiology.7 Miller et al,6 in one study of 1198 individuals in 202 families, reported linkage to loci on chromosomes 6p, 6q, 9q, 16q, 17p and 17q. This followed work by Wise et al,10 who identified loci on chromosomes 6p, 10q and 18q in one polygeneration family and Chan et al,11 who reported loci on chromosomes 19p and 2q. Predicting the risk of curve progression has also been the focus of genome studies. Braun et al12 identified 12 DNA markers as having diagnostic utility in AIS. When compared with standard radiological methods, these markers provided a superior assessment of risk of progression. Further development of this work has led to the ‘Scoliscore AIS prognostic test’ becoming available to spine specialists in the US in 2009.13 This salivabased genetic test uses 53 DNA markers which have been linked to the progressive form of scoliosis. Validation work by the development company, Axial Biotech, quotes a 99% negative predictive value (95% confidence interval (CI) 96% to 100%) but independent validation is awaited. Bracing The use of orthotics to treat AIS is a time-honoured tradition in countries around the world.14 Despite bracing being the mainstay of conservative treatment, its efficacy has not been demonstrated definitively in prospective or randomised clinical studies.15 It is possible to find support in the literature on the effectiveness of braces in preventing curve progression.16-20 This support includes the Scoliosis Research Society brace study, which is the only prospective, multicentre controlled study so far reported, that compares bracing with observation and concluded that bracing was more effective than observation alone21,22 but it must be noted that this study “was nonrandomised, non-blinded, the baseline differences between the groups were not statistically adjusted for and the results did not include the surgical rates”.14 A meta-analysis performed in 199715 also supported the use of brace treatment and advocated a 23-hour regimen. This was shown to be significantly more effective than any other form of conservative treatment, including regimens that involved fewer hours per day in the brace. Conversely, there are multiple studies which have concluded that bracing is ineffective in preventing curve progression,23-25 including a review article in 199926 which critically deconstructs the results and conclusions of previous papers which support bracing, while advocating a watchful waiting policy. A more recent systematic review of the relevant clinical studies aimed to identify a pooled estimate of the incidence of surgery in patients who had been treated by observation only (three studies, 139 patients) and for those treated in a brace (15 studies, 1814 patients). The pooled surgical rate was 23% (95% CI 20% to 24%) after bracing and 22% (95% CI 16% to 29%) after observation leading to the conclusion that there was no evidence to recommend bracing rather than observation.27 Compliance with brace use has always been a major problem, with most regimens being intensive in terms of time, social acceptance and limitations in physical activity. By designing a discrete choice experiment28 it was shown that patients with scoliosis would be prepared to undergo brace treatment only if it were to provide a sizeable reduction in the risk of surgery. Effectiveness and discomfort in wearing a brace were the most important determinants of choice. The issue of brace efficacy is thus far from resolved. In an attempt to improve brace comfort and, therefore, compliance, there has been work undertaken on flexible spinal orthoses.29 However, as yet these have not proven to be better than rigid orthoses in either efficacy or patient acceptance.30 It appears that there are many issues in respect of the brace treatment of AIS that have yet to be resolved. In order to help clinicians, patients and parents make a more informed choice about brace treatment, better quality prospective studies are needed. Some key issues may be answered in the Bracing in Adolescent Idiopathic Scoliosis Trial (BrAIST), a 27-centre randomised, controlled trial currently undergoing its second year of recruitment.31 This trial aims to randomise patients at high risk of curve progression into either a group treated with a thoracolumbar spinal orthosis or a group treated by observation alone, and will compare clinical, radiographic and psychosocial outcomes. ©2011 British Editorial Society of Bone and Joint Surgery 1 2 M. STENNING, I. NELSON Instrumentation and fusion The instrumentation technique used to supplement fusion in surgery for AIS is constantly evolving. Harrington's spinal instrumentation system32 gave improved curve correction and allowed early mobilisation in a brace rather than a bulky cast. Luque introduced the principles of segmental instrumentation and correction via translation and derotation by using sublaminar wires.33 With the advent of Cotrel-Dubousset implants34 these concepts have been expanded to include hook, hybrid and most recently, all-screw constructs.35 In the last decade in particular, increased attention has been paid to re-establish normal sagittal balance during the surgical correction of scoliosis. All-screw constructs have become the gold standard instrumentation technique for thoracic AIS. A pedicle screw achieves three-column fixation of the vertebral body35 and displays biomechanical properties that are superior to other forms of construct.36-38 This allows the surgeon to achieve greater correction of the curve in all three planes, including rotation, with relatively simple rod derotation manoeuvres; this was a failing of techniques that used hooks. There is also less canal intrusion and risk of dislodgement or migration into the canal when compared with hook fixation.35 Coronal correction of the curve by up to 70% has been reported with all-screw constructs, hook fixation achieving less than 50%.35,39-42 Better correction of the reduced thoracic kyphosis seen in AIS has also been reported with the use of an all-screw technique,34,42 although some have noted a tendency for all-screw constructs to cause flattening of the thoracic spine during the correction,35,43 which occurred when rods of inadequate thickness were used . Before the introduction of all-screw constructs, the more severe thoracic AIS curves (Cobb angle > 60°) required a combined anterior and posterior fusion in order to improve the coronal correction and fusion rates. The deterioration in pulmonary function with a thoracotomy in these cases is well documented.44,45 A posterior spinal fusion using an all-screw construct has been shown to provide an equivalent degree of curve correction compared with the combined approach in patients with a curve of 70° to 100°, negating the need for thoracotomy in these patients.45 Pedicle screws are not only effective but have also been shown to be safe in all types of curve. This was an initial concern for many surgeons with their use in the thoracic spine. Three recent, large studies have demonstrated the complication rates of using pedicle screws in AIS. Neurological injuries have been reported in 0% to 1.5% of patients, with all deficits being transient.35,46,47 Screw malposition is said to be 1.5% when assessed by plain radiography47 and 6% when assessed by finecut CT scans; however, these patients were asymptomatic and did not require screw revision anyway.46 A pedicle fracture rate of 0.24% was seen, with one patient out of 462 requiring revision surgery; intraoperative screw loosening was noted in 0.76% of patients.47 Peri-operative pulmonary function has also been shown to improve in patients after all-screw constructs when compared with hook systems. This is thought to be because of improved alignment of the chest wall with all-screw constructs.35,41 The use of all-screw constructs has been extended from AIS to adult idiopathic scoliosis. Adult curves are stiffer and have a higher rate of pseudarthrosis when compared with their adolescent counterparts.48,49 Hook-based constructs are less likely to provide adequate curve correction and this can lead to an increased need for combined anterior and posterior surgery. The improved biomechanical profile of all-screw constructs results in improved curve correction while avoiding the morbidity of anterior surgery; in one study this conferred a significantly lower complication rate.50 Re-establishment of normal sagittal balance is particularly important in the adult and may necessitate spinal osteotomies such as the chevron or Ponte, pedicle subtraction osteotomy or vertebral column resection. Surgical treatment of early onset scoliosis Patients with AIS typically present at a stage in their development where the thorax has achieved most of its adult volume and has near-normal vital capacity. Surgical treatment involves definitive spinal fusion and has a negligible effect on thoracic growth or long-term pulmonary outcome. Early-onset scoliosis, irrespective of cause (congenital, neuromuscular, etc.) presents the surgeon with a different set of challenges. Spinal lordosis and curve rotation leaves the thorax with a volumedepletion deformity and growth inhibition ultimately leading to Thoracic Insufficiency Syndrome (TIS). This is defined as “the inability of the thorax to support normal respiration or lung growth”.51 Associated abnormalities of the rib cage can add to the thoracic disability. Standard surgical treatment of scoliosis is often not possible in these cases because of the detrimental effect that spinal fusion might have on spinal and thoracic growth.52 The goal of surgical treatment in early-onset scoliosis is “to stop the progression of the curve whilst allowing maximum growth of the spine, lungs and thoracic cage”.53 In order to achieve this a number of different surgical approaches can be employed. Posterior instrumentation without fusion, using dual growing rods, is used when the primary problem is at the vertebral column.54 The dual rod technique has been shown to give significantly better correction of the scoliosis when compared with single rod techniques.55 Subperiosteal dissection and fusion is performed only at the upper and lower anchor sites of the construct. Each rod is then measured, contoured and cut into an upper and lower portion. A connector, usually placed at the thoracolumbar junction, links the upper and lower rods on either side of the spine.53 The best time between lengthening procedures is about six months, with longer intervals leading to less spinal growth and poorer correction of the scoliosis.56 The results of dual growing rods in 23 patients with minimum of two years' follow-up have been presented by the Growing Spine Study Group (GSSG).57 These patients, with a mean age of 5.4 years at first surgery, required a mean of 6.6 lengthening procedures. The Cobb angle was reduced from a mean of 82° before surgery to 36° at the end of treatment. Meanwhile, the mean spinal growth was 1.21 cm per year, which approaches that associated with normal spinal growth.53 THE JOURNAL OF BONE AND JOINT SURGERY RECENT ADVANCES IN THE TREATMENT OF SCOLIOSIS IN CHILDREN When the primary problem involves the thoracic cage, for example TIS has developed or the patient has rib fusions, reconstruction of the thoracic cage needs to be considered. Expansion thoracoplasty and insertion of a vertical expandable prosthetic titanium rib (VEPTR) has been developed to treat such cases.58 This technique addresses all related components of the thoracic deformity in the growing child, including the spine, rib cage and diaphragm, without compromising thoracic growth.55 Rather than directly correcting the spinal deformity with instrumentation, this technique involves correcting the thoracic deformity with rib osteotomies or intercostal muscle lysis. This enlarges the constricted thorax which is then maintained by insertion of the VEPTR device. As with the growing rods, lengthening is required approximately every six months. Growth of the spine in cases where the VEPTR technique has been used is nearly normal.59,60 Improvement in thoracic constriction and lung function has been difficult to confirm because of the problems in measuring pulmonary function in young children; however, some studies have shown a decreased ventilator dependence and increases in thoracic and lung volumes.58-63 The interpretation of these results must be guarded as all of the studies are non-randomised case series without controls.54 The surgical treatment of progressive, early-onset scoliosis is complex and associated with a high complication rate. A 48% complication rate during treatment was quoted in a GSSG followup of 23 patients who had received dual growing rods; four patients (17%) had required unplanned procedures for infection. Implant problems, such as rod breakage, hook dislodgement and screw pull-out, were all addressed during planned lengthening as were two alignment problems (one crankshaft phenomenon and one junctional kyphosis.57 A further study in 48 patients, also by the GSSG, identified 55 complications in 29 patients, with 23 patients requiring unplanned procedures.64 Again, wound problems were the most common cause of unplanned procedures while most implant problems could be addressed during a planned procedure. This study also noted that younger patients had higher complication rates and the complications changed from wound problems to implant problems as the interval between lengthening procedures increased. The VEPTR devices are less likely to break when compared with growing rods. Meanwhile, spontaneous spinal fusion adjacent to the device is uncommon but infection and soft-tissue scarring are common, while drifting of the rib and spinal anchor points can occur. With repetitive lengthening the expansion portion of the device can be outgrown and requires exchanging, which is a more extensive procedure compared with simple lengthening.54 Mr M Stenning MBBS, MPhil, FRCS (Tr & Orth) Mr I Nelson MBBS, MChOrth, FRCS. Department of Orthopaedic Spine Surgery North Bristol NHS Trust Frenchay Hospital Bristol BS16 1LE Email: [email protected] 3 References 1. Wynne-Davies R. Familial (idiopathic) scoliosis. A family survey. J Bone Joint Surg (Br) 1968;50:24-30. 2. Riseborough EJ, Wynne-Davies R. A genetic survey of idiopathic scoliosis in Boston, Massachusetts. J Bone Joint Surg (Am) 1973;55:974-982. 3. Cowell HR, Hall JN, MacEwen GD. Genetic aspects of idiopathic scoliosis. A Nicholas Andry Award essay, 1970. Clin Orthop Relat Res 1972;86:121-131. 4. Justice CM, Miller NH, Marosy B, et al. Familial idiopathic scoliosis: evidence of an X-linked susceptibility locus. Spine 2003;28:589-594. 5. Lowe TG, Edgar M, Margulies JY, et al. Etiology of idiopathic scoliosis: current trends in research. J Bone Joint Surg (Am) 2000;82:1157-1168. 6. Miller NH, Justice CM, Marosy B, et al. Identification of candidate regions for familial idiopathic scoliosis. Spine 2005;30:1181-1187. 7. Clough M, Justice CM, Marosy B, et al. Males with familial idiopathic scoliosis: a distinct phenotypic subgroup. Spine 2010;35:162-168. 8. Kesling KL, Reinker KA. Scoliosis in twins. A meta-analysis of the literature and report of six cases. Spine 1997;22:2009-2014. 9. Ogilvie JW, Braun J, Argyle V, et al. The search for idiopathic scoliosis genes. Spine 2006;31:679-681. 10. Wise CA, Barnes R, Gillum J, et al. Localisation of susceptibility to familial idiopathic scoliosis. Spine 2000;25:2372-2380. 11. Chan V, Fong GC, Luk KD, et al. A genetic locus for adolescent idiopathic scoliosis linked to chromosome 19p13.3. Am J Hum Genet 2002; 1:401-406. 12. Braun JT, Nelson L,Ogilvie J, Ward K. Twelve DNA markers accurately assess risk of progression in adolescent idiopathic scoliosis. Scoliosis Research Society 42nd Annual Meeting and Course. Sept 2007, Edin. 13. www.scoliscore.com Nov 2010 14. Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis. An evidence-based review. Spine 2007;195:S91-100 15. Rowe DE, Bernstein SM, Riddick MF, et al. A meta-analysis of the efficacy of nonoperative treatments for idiopathic scoliosis. J Bone Joint Surg (Am) 1997; 79: 664-674. 16. Lonstein JE, Winter RB. The Milwaukee brace for the treatment of adolescent idiopathic scoliosis: a review of one thousand and twenty patients. J Bone Joint Surg (Am) 1994; 76: 1207-1221. 17. Fernandez-Feliberti R, Flynn J, Ramirez N, et al. Effectiveness of TLSO bracing in the conservative treatment of idiopathic scoliosis. J Pediatr Orthop 1995; 15: 176-181. 18. Olafsson Y, Saraste H, Soderland V, et al. Boston brace in the treatment of idiopathic scoliosis. J Pediatr Orthop 1995; 15: 524-527. 19. D’Amato CR, Griggs S, McCoy B. Night-time bracing with the Providence brace in adolescent girls with idiopathic scoliosis. Spine 2001; 26: 2006-2012. 20. Gabos PG, Bojescul JA, Bowen JR, et al. Long-term follow-up of female patients with idiopathic scoliosis treated with the Wilmington orthosis. J Bone Joint Surg (Am) 2004; 86:1891-1899. 21. Peterson LE, Nachemson AL. Prediction of progression of the curve in girls who have adolescent idiopathic scoliosis of moderate severity: logistic regression analysis based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Surg (Am) 1995; 77: 823-827. 22. Nachemson AL, Peterson LE. Effectiveness of treatment with a brace in girls who have adolescent idiopathic scoliosis: a prospective, controlled study based on data from the Brace Study of the Scoliosis Research Society. J Bone Joint Sur (Am) 1995; 77: 815822. 23. Noonan KJ, Weinstein SL, Jacobson WC, et al. Use of the Milwaukee brace for progressive idiopathic scoliosis. J Bone Joint Surg (Am) 1996; 78: 557-567. 24. Goldberg CJ, Moore DP, Fogarty EE, et al. Adolescent idiopathic scoliosis: the effect of brace treatment on the incidence of surgery. Spine 2001: 26: 42-47. 25. Karol LA. Effectiveness of bracing in male patients with idiopathic scoliosis. Spine 2001; 26: 2001-2005. 26. Dickson RA, Weinstein SL. Bracing and screening: yes or no? J Bone Joint Surg (Br) 1999; 81: 193-198. 27. Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence based review. Spine 2007; 32: S91-S100. 28. Bunge EM, de Bekker-Grob EW, van Biezen FC, et al. Patients’ preferences for scoliosis brace treatment: a discrete choice experiment. Spine 2009; 35: 57-63. 29. Coillard C, Leroux MA, Zabjek KF, et al. SpineCor- a non-rigid brace for the treatment of idiopathic scoliosis: post-treatment results. Eur Spine J 2003; 12: 141-148. 30. Sang Wong M, Cheng JCY, Lam TP, et al. The effect of rigid versus flexible spinal orthosis on the clinical efficacy and acceptance of the patients with adolescent idiopathic scoliosis. Spine 2008; 33: 1360-1365. 4 M. STENNING, I. NELSON 31. Dolan LA, Weinstein SL. BrAIST: Planning and current status of bracing in adolescent idiopathic scoliosis trial. From 6th international conference on conservative management of spinal deformities. May 2009;Lyon, France. 49. Kim YJ, Bridwell KH, Lenke LG, et al. Pseudarthrosis in adult spinal deformity following multisegmental instrumentation and arthrodesis. J Bone Joint Surg (Am) 2006; 88:721-728. 32. Harrington P. Technical details in relation to the successful use of instrumentation in scoliosis. Orthop Clin North Am 1972; 3: 49-67. 50. Rose PS, Lenke LG, Bridwell KH, et al. Pedicle screw instrumentation for adult idiopathic scoliosis: an improvement over hook/hybrid fixation. Spine 2009;34: 852-857. 33. Luque ER. Segmental spine instrumentation for correction of scoliosis. Clin Orthop 1982;163:192-198. 51. Campbell RM Jr, Smith MD, Mayes TC, et al. The characteristics of thoracic insufficiency syndrome associated with fused ribs and congenital scoliosis. J Bone Joint Surg (Am) 2003; 85: 399-408. 34. Lehman RA, Lenke LG, Keeler KA, et al. operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine 2008; 33: 1598-1604. 35. Liljenqvist U, Hackenberg L, Link T, et al. Pullout strength of pedicle screws versus pedicle and laminar hooks in the thoracic spine. Acta Orthop Belg 2001: 67: 157-163. 36. Lehman RA Jr, Polly DW Jr, Kuklo TR, et al. Straight forward versus anatomic trajectory technique of thoracic pedicle screw fixation: a biomechanical analysis. Spine 2003;28:2058-2065. 37. Lehman RA Jr, Kuklo TR. Use of the anatomic trajectory for thoracic pedicle screw salvage after failure/violation using the straight forward technique: a biomechanical analysis. Spine 2003;28:2072-2077. 38. Suk SI, Lee CK, Kim WJ, et al. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine 1995; 20:1399-1405. 39. Liljenqvist U, Lepsien U, Hackenberg L, et al. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J 2002;11:336-343. 40. Kim YJ, Lenke LG, Kim J, et al. Comparative analysis of pedicle screw versus hybrid instrumentation in posterior spinal fusion of adolescent idiopathic scoliosis. Spine 2006; 31:291-298. 41. Suk SI, Lee SM, Chung ER, et al. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year followup. Spine 2005;30:1602-1609. 42. Suk SI, Kim WJ, Kim JH, et al. Restoration of thoracic kyphosis in the hypokyphotic spine: A comparison between multiple hook and segmental pedicle screw fixation in adolescent idiopathic scoliosis. J Spinal Disord 1999;12: 489-495. 43. Lowenstein JE, Matsumoto H, Vitale MG, et al. Coronal and sagittal plane correction in adolescent idiopathic scoliosis: a comparison between all pedicle screw versus hybrid thoracic hook lumbar screw constructs. Spine 2007;32:448-452. 44. Vendantam R, Lenke LD, Bridwell KH, et al. A prospective evaluation of pulmonary function in patients with adolescent idiopathic scoliosis relative to the surgical approach used for spinal arthrodesis. Spine 2000;25:82-90. 45. Luhmann SJ, Lenke LG, Kim YJ, et al. Thoracic adolescent idiopathic scoliosis curves between 70 and 100 degrees: is anterior release necessary? Spine 2005;30: 2061-2067. 46. Kim YJ, Lenke LG, Bridwell KH, et al. Free hand pedicle screw placement in the thoracic spine: is it safe? Spine 2004;29:333-342. 47. Suk SI, Kim WJ, Lee SM, et al. Thoracic pedicle screw fixation in spinal deformities: are they really safe? Spine 2001;26:2049-2057. 48. Takahashi S, Delecrin J, Passuti, N. Surgical treatment of idiopathic scoliosis in adults: an age-related analysis of outcome. Spine 2002;27:1742-1748. 52. Campbell RM Jr, Smith MD. Thoracic insufficiency syndrome and exotic scoliosis. J Bone Joint Surg (Am) 2007; 89:108-122. 53. Behrooz AA. Management themes in early onset scoliosis. J Bone Joint Surg (Am) 2007;89:42-54. 54. Yazici M, Emans J. Fusionless instrumentation systems for congenital scoliosis: expandable spinal rods and vertical expandable prosthetic titanium rib in the management of congenital spine deformities in the growing child. Spine 2009;34 1800-1807. 55. Thompson GH, Akbarnia BA, Kostial P, et al. Comparison of single and dual growing rod techniques followed through definitive surgery: A preliminary study. Spine 2005;30:2039-2044. 56. Breakwell LM, Akbarnia BA, Marks DS, et al. End results of dual growing rod technique followed until final fusion. The effect of frequency of lengthening. Read at the Annual Meeting of the Scoliosis Research Society; 2005 Oct 29; Miami, FL. 57. Akbarnia BA, Marks DS, Boachie-Adjei O, et al. Dual growing rod technique for the treatment of progressive early-onset scoliosis: a multicentre study. Spine 2005; 30(17 Suppl): S46-57. 58. Campbell RM Jr, Smith MD, Hell-Vocke AK. Expansion thoracoplasty: The surgical technique of opening-wedge thoracostomy. Surgical technique. J Bone Joint Surg (Am). 2004; 86-A (suppl 1): 51-64. 59. Campbell RM Jr, Hell-Vocke AK. Growth of the thoracic spine in congenital scoliosis after expansion thoracoplasty. J Bone Joint Surg (Am) 2003; 85-A: 409-20. 60. Emans JB, Caubet JF, Ordonez CL, et al. The treatment of spine and chest wall deformities with fused ribs by expansion thoracostomy and insertion of vertical expandable prosthetic titanium rib: growth of thoracic spine and improvement of lung volumes. Spine 2005; 30: S58-68. 61. Motoyama EK, Deeney VF, Fine GF, et al. Effects on lung function of multiple expansion thoracoplasty in children with thoracic insufficiency syndrome: a longitudinal study. Spine 2006;31:284-290. 62. Gollogly S, Smith JT, Campbell RM Jr. determining lung volume with three dimensional reconstructions of CT scan data: a pilot study to evaluate the effects of expansion thoracoplasty on children with severe spinal deformities. J Pediatr Orthop 2004;24:323328. 63. Latalski M, Fatyga M, Gregosiewicz. The vertical expandable prosthetic titanium rib (VEPTR) in the treatment of scoliosis and thoracic deformities. Preliminary report. Ortop Traumatol Rehabil 2007;9:459-466. 64. Akbarnia BA, Asher MA, Bagheri R, et al. Complications of dual growing rod technique in early onset scoliosis: can we identify risk factors? Read at the Annual Meeting of the Scoliosis Research Society: 2006 Sep 15; Monterey, CA. THE JOURNAL OF BONE AND JOINT SURGERY
© Copyright 2026