Working with Managed Care
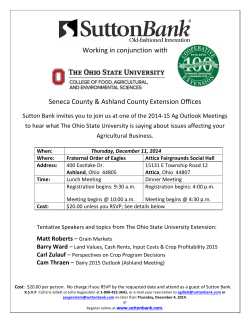
Working with Managed Care OACCA Conference April 28, 2014 Timia DelPrete-Brown, Ph.D, LPCC-S Director, High Risk Care Management and Jonas Thom, MA,PCC-S VP of Behavioral Health OACCA Conference Agenda • • • • • • • What is Managed Care? Who is CareSource CareSource Clinical Programs High Risk Case Management BH Programs and Covered Services Opportunities for Collaboration Q&A 2 Mission: The CareSource Heartbeat Making a difference in the lives of underserved people by improving their health care Vision CareSource Management Group will be an innovative leader in the management of quality public sector health care programs 3 What is Managed Care? • Ohio Department of Medicaid (ODM) ‒ A health plan that attempts to control the costs and quality of care ‒ Operates throughout the state of Ohio • “Hands-on health insurance" ‒ Combines the responsibility for paying for a defined set of health services with an active program to control the costs associated while at the same time attempting to control the quality of and access to those services. 4 What is Managed Care? • CareSource ‒ Founded on quality and service ‒ Delivered with compassion ‒ Understands Medicaid, Medicare, and the associated regulatory environments ‒ Process efficiencies and value-added benefits ‒ HEDIS initiatives 5 What is Managed Care? 6 What is Managed Care? BH Services • Ohio Medicaid BH Services • OMHAS Services • FFS/Managed Care Services 7 Who is CareSource? • The largest non-profit Medicaid managed health care plan in Ohio • 2nd largest Medicaid managed health care plan in the country • Established in 1989 – Then known as Dayton Area Health Plan, CareSource pioneered the state's first mandatory Medicaid managed care program in the Dayton area. • URAC & NCQA accredited • Headquarters Based in Dayton, Ohio with offices in Cleveland, Columbus, and Kentucky • Recent partnership/alliance with Humana 8 Who is CareSource? • CareSource serves 950,000+ Ohio citizens • CareSource contracts with 24,000+ Ohio providers • CareSource employs 1,500+ individuals 9 Care Source Health Services Division Quality Improvement Care Management Pharmacy • CareSource 24 • Disease Management • Care Transitions/Bridge to Home • High Risk Case Management Health and Wellness Behavioral Health Medical Management 10 CareSource Programs Quality programs • HEDIS • Support quality care • Medical Management • Identify services/resources • Prior authorization management • Quality Improvement • Entry point for member voice and continuous quality improvement 11 CareSource Programs • Disease Management ‒ Self Management ‒High risk Asthma ‒Diabetes ‒ Different levels of DM ‒ Proactive calls ‒ Minimum contacts ‒ Smoking Cessation ‒Informal connection 12 CareSource Programs Triage/CareSource24 • Assess the severity of the member's symptoms and guide the caller to the appropriate level of care • Assists members in navigating the healthcare system while educating and empowering the member. • 24 hours a day, 7 days a week 13 The Care Transitions Program • Bridge To Home: • Contact each member having a hospital or skilled nursing facility confinement within 14 days of discharge – Adherence to scheduled primary/specialty care follow up care – Medication reconciliation and education – Identification of potential member gaps in understanding discharge instructions or changes in the member’s medication regime post discharge – Assessment and identification of member educational needs with a focus on member self-management and knowledge of the member’s individual triggers and individualized care treatment plan 14 CareSource Programs • Population Specific ‒ Coordinated Services/Care4U ‒ Opiate RX abuse ‒ 12+ active RX, 4 docs/pharmacies ‒ Care management and coordination ‒ Prenatal/NICU ‒ Manage high risk pregnancies ‒ Child is in the NICU ‒ ABD Children 15 Who are the ABD Children? • There are approximately 37,000 Ohio children who are eligible for Medicaid due to a disability • On July 1, 2013, ABD children were enrolled in a one of Ohio’s Medicaid Managed Care Plans • Exclusions included those eligible for Medicaid on waivers, children who reside in institutional settings, or children who received both Medicare and Medicaid benefits 16 Top Complex Medical Conditions for Children: Developmental disorder Epilepsy PDD & Mood Disorders Bipolar disorder Deaf Anoxic Brain Damage Cardiac Septal Defects Traumatic brain injury Spina Bifida Substance Dependence Psychotic disorders Sickle Cell Blind Transplant Status Quadriplegia and paraplegia Cancer diagnosis 17 ABD Children's Advisory Council • Developed in March 2012 • Charged with providing CareSource staff and stakeholders with key recommendations for ensuring children with special health care needs are successfully transitioned to the health plan • Recommendations led in developing strategies for attaining the best possible health outcomes for these newly eligible children Family Voices Parent Advocate Ohio Council of Behavioral Health & Nationwide Children's Family Services Providers Easter Seals Children’s Defense Fund BCMH Voices for Ohio’s Children Ohio Association of University Centers for Excellence in Children Services DD Ability Center of Greater Dayton Children’s Hospital Toledo Respite Coalition 18 ABD Children's Top Chronic Conditions 19 Who Are High Risk Members? • ODM compiled utilization data regionally and nationally (“Hot Spotters” article published in New Yorker magazine) • ODM determined that a very small percentage of members are driving Medicaid (ABD & CFC) costs. Those individuals are known as “hot spotters” • ODM mandated that all managed care companies operating in the State of Ohio revise their case management model to focus on the top 1% of “hot spotters” 20 What Are the Program’s Requirements? • ODM’s Requirements: • Need-based guidelines • High Risk, top 1% • Mobile and community based workers • Face-to-face & telephonic interactions with members • 1:25 staff/member ratio • Reimbursed for improved health outcomes (HEDIS) 21 High Risk Care Management: Community Based Model Multidisciplinary team approach • Members/Caregivers • Case Managers • LPN’s • Social Workers • Patient Navigators • Care Management Support Specialists • PCPs and Specialists • Community Partners Integrates professional Standards of Practice Coordination of member’s health care needs across care continuum Focus on quality outcomes, regulatory and accreditation requirements 22 What is CareSource’s High Risk Case Management Model? • Incorporates the Case Management Society of America and the American Association of Managed Care Nursing Standards of Practice – Commitment to the CM Process: identification, assessment, planning, facilitation, monitoring, evaluation, & advocacy • Integrates the Harold P. Freeman Patient Navigation model • Integrates behavioral and physical health intervention strategies • Utilizes a multidisciplinary team approach 23 High Risk Case Management Components Identification • Predictive modeling • Health risk assessments • Provider and community referrals Engagement • Face-to-face meetings at least quarterly with ongoing regular telephonic contact • Assessment of member’s needs • Planning, facilitation, intervention, and advocacy to meet identified needs • Ongoing monitoring and evaluation of the case management plan Outcomes • • • • Clinical Financial Satisfaction Quality of Life 24 Who Are High Risk Members? •Identification Mechanisms: 1. Referrals from CareSource’s Medical Management Department 2. Referrals from CareSource’s data department based on electronic Predictive Risk Modeling – John Hopkins University ACG software combines medical, behavioral health, and pharmacy claims, creating clinically relevant categories as well as risk scores for our members 3. Referrals from provider & community partners who work with members in crisis on a daily basis, in real-time 25 High Risk Care Management Demographic Cost Predictive Modeling Utilization Diagnosis 26 High Risk Criteria Greater than four chronic co-morbidities (such as: DM, CAD, HTN, CKD, COPD, Asthma, SCD, HIV) Behavioral health diagnosis including Schizophrenia, Major Depression, Bipolar Disorder A sudden disability (e.g., stroke, head injury, spinal cord injury, paraplegia) Hospital re-admit within 90 days Multiple avoidable ER visits in the past 6 months Greater than 12 prescriptions or high cost drugs High Risk pregnancy Unable to access PCP/unable to keep or get to preventive visits Limited or no caregiver resource NICU admission > 7 days 27 Focus of High Risk Case Management Member-driven case management process Help members regain optimum health and function Promote adherence with prescribed treatment plan Self-management education, preventive care support Improving health outcomes and health care costs Partnership with providers to maximizes benefits of primary care and medical home 28 What Services Does CareSource’s High Risk Case Management Program Provide? • • • • • Care Coordination Health Promotion Advocacy & Access Outreach Linkage for Basic Needs • Collaboration 29 Care Coordination The Primary Service of High Risk Case Management. Facilitate care across health, social and enabling services through: • Comprehensive health assessments: bio, psycho, social, spiritual • Individualized care plans based on Member’s strength, needs, and preferences • Identification and inclusion of all providers • Provision of clinical and service summaries, such as the Provider Portal • Proactive communication with all providers, members and families 30 Health Promotion Skill & asset building to help members mange their illness and maximize wellness through: • Developing understanding about their conditions and importance of treatment/medication adherence • Utilizing available treatments and pathways to health • Building skills and resources for self-management and wellness 31 Advocacy and Access Ensuring members have the services and resources they need across: • Healthcare providers • Social service systems • Enabling services, such as transportation and peer support 32 Outreach Community based work, to engage members in healthcare, including: • Serving members “where they are,” based on their preferences • Assertive engagement, including home and provider visits • Identifying health and support resources 33 Linkage for Basic Needs Linking members and families to resources that are prerequisites to healthcare: • Food • Clothing • Shelter 34 Collaboration CareSource Members + Family CareSource RN Case Manager, Social Worker, Behavior Health, Patient Navigator, Disease Management, Pharmacy, Care Transitions Primary Care Physician Community Services Community Behavior Health YMCA 35 Collaboration (cont.) CareSource’s Provider Portal: • • • • • Confirm member’s eligibility Review coordination of benefit information Submit prior authorizations Review care plans Make referrals for care or disease management • Review individual member or practice HEDIS measures • Review the Clinical Practice Registry • Review the Member Profile 36 HRCM Program Evaluation • Quality • HEDIS • Condition Specific • Satisfaction • Survey • Grievances • Cost • Overall Medicaid costs • ED utilization rates • Inpatient rate 37 BH Strategy: Enhance our clinical programs • Embed BH Specialist into all CM teams • BH Coordinator role for BH Specialist staff • Ongoing training and learning for all clinical staff • Deploy “BH Pathways” for all member facing staff • Ensure CM, MM, & Care Transitions collaboration • Provide member self-management tools 38 BH Strategy: Web Based Tools • Provider Portal • Health Home Portal • Snapshots 39 BH Strategy: Improve provider services Access • Availability of BH in primary care • Telehealth • Fill gaps in CMHC care Care Coordination Resources for BH Providers • • • • Integrate staff BH Provider data sharing solutions Medication interventions Provider and stakeholder education 40 BH Strategy: Advocacy Lead local, state and federal advocacy • Initiatives • Regulatory alignment • Plan Alignment 41 We want to collaborate with you! • CareSource Programs • Tools and Resources • Specific Partnerships 42 We want to collaborate with you! CareSource Programs • Participate with our shared members in our programs • Work with our community based care management! 43 Collaborations Tools and Resources • Member Profile • Clinical Practice Registry • Care coordination • Inpatient notification system for BH 44 Collaboration CareSource Provider Portal (right) Clinical Practice Registry (below) Case Management Referral 45 We want to collaborate with you! Specific Partnerships We want to work with you to help members… Do you … • Know your Member’s payers? • Understand OH Medicaid programs’ coverage? 46 Summary • CareSource thrives on partnerships ‒ Open to creating new ways to partner • More Behavioral Health services not less ‒ BH is essential to overall health wellness and community tenure • Contact Jonas Thom, M.A., PCC-S Vice President of Community Programs ‒ [email protected] ‒ 937-531-2137 47 Questions? Contact Information: Timia DelPrete-Brown [email protected] (216) 896-8205 Jonas Thom [email protected] (937) 531-2137 Terry Jones, Director of Behavioral Health [email protected] (937) 531-2401 48 Mission: The CareSource Heartbeat Making a difference in the lives of underserved people by improving their health care Vision CareSource Management Group will be an innovative leader in the management of quality public sector health care programs 49
© Copyright 2026