File - Bristol Regional Medical Center Kings Mountain
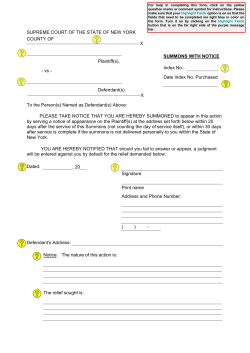
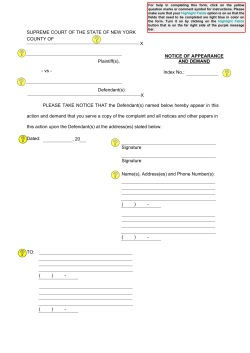
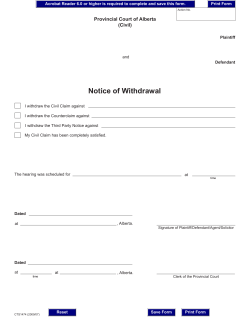
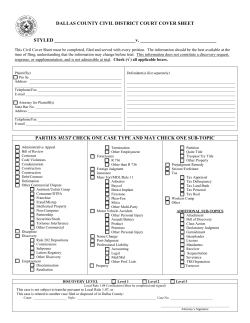
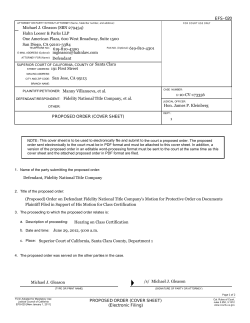
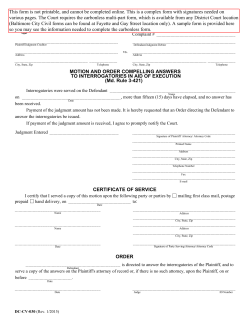
Legal Considerations for Respiratory Therapists King’s Mountain Symposium Wellmont Bristol Regional Medical Monarch Auditorium October 23, 2014 Jimmie C. Miller Hunter, Smith & Davis, LLP 1212 North Eastman Road Kingsport, Tennessee 37664 [email protected] 423-378-8852 Objectives • Discuss General Legal Concepts and Terms • Discuss Cases in Med-Mal Litigation as Related to RT • Discuss Med-Mal Litigation Time Frames • Discuss Areas of Potential Liability Exposure for RT • Discuss actions of RT to minimize legal risk • Discuss Documentation Issues Legal Terms and Concepts • Plaintiff – patient or family members who bring a lawsuit • Defendant – physician, nurse, RT, hospital, or other entity that is being sued • Complaint – the document that is filed in court and begins the lawsuit process • Negligence – a breach by the defendant(s) of the applicable standard of care that causes injuries to the plaintiff/patient Legal Terms - continued • Standard of care – what a reasonable RT would do under same or similar circumstances in the medical community or a similar medical community • Causation – evidence that establishes that the injury to the plaintiff was caused by the breach of the standard of care, i.e. the injuries would not occurred but for the breach by the RT Legal Terms • Health Care Liability Action – new terminology used in Tennessee law instead of medical malpractice • Statute of Limitations – length of time a plaintiff has to sue a defendant for med-mal – In Tennessee – In Virginia 1 year + 120 days 2 years Legal Concepts • Notice of Intent – – Law requires plaintiff provide written notice to defendant at least 60 days before suit is filed and provide a HIPAA compliant authorization – Frequently provides good procedural defense because statute requirements are often not met Expert Testimony • Law requires plaintiff prove her/his case by expert testimony. • Expert witness must generally be licensed in field of defendant/ RT expert if RT is defendant; MD expert if MD is defendant • Expert must be licensed in Tennessee or a contiguous state • Expert must be familiar with Standard of care in our community or a community similar to our community Damages • Economic Medical expenses, past and future, Life Care Planners Death cases evaluated less than cases where plaintiff requires extensive future medical treatment Lost Earnings • Non-economic Pain and suffering, loss of consortium Tennessee has cap of $750,000 or $1 million. Larger cap applies if amputation of two limbs, spinal cord injury involving paraplegia or quadriplegia, or third degree burns of forty (40) percent of body or face, or death of parent with minor children. BUT cap is not applicable if medical records are falsified, destroyed or concealed with purpose of evading liability in the case. - Documentation Cases – Newborn Death • 2001, Seattle, Washington • Delivery, nurse documented “alert & responsive” • Vital signs not taken “at specified time” then newborn not breathing • Breathing tube was placed. • Allegation that RT used wrong adaptor and O2 was going into baby with no way out Newborn case - continued • Lungs hyper-inflated • Baby had cerebral palsy and suffered brain damage • Settlement with hospital $7.8 million • Confidential then court ordered release of documents Monitoring of Vent Pt During CT • Mercer v. Vanderbilt University, Inc. and nurse and RT, • 1998 event/final decision 2004, $7,366,000 jury verdict in favor of plaintiff against hospital • Pt in MVA/blood alcohol .13, place on ventilator and had severe agitation presumable from alcohol withdrawal • Four days after admission, needed CT for facial injuries CT Monitoring case - continued • RN and RT accompanied Pt to CT, with portable cardiac monitor and portable ventilator attached to 1 of 3 oxygen tanks, 1 full and 2 half-full • RT did not record ventilator settings and alarm parameters prior to leaving neuro ICU • 1030 am pt given paralytic, scans at 1047 and 1056 • Pt retracted from CT scanner table, pink and breathing CT Monitoring case - continued • • • • • Pt moved to his bed 1105 Code called and team resuscitated pt. Severe and permanent brain damage sustained At trial pt living in NHC Healthcare in Dickson, TN Plaintiff claimed RT attached ventilator to an oxygen tank only half-full and tank ran out during CT • Defense was pt suffered a catastrophic event, seizure or a malignant heart arrhythmia caused by alcohol withdrawal Case – Unsuccessful intubation • Kott v. St. Joseph’s Hospital, Syracuse, NY • 2011 • Pt. admitted for SOB and dx pulmonary hypertension • Patient fell in bathroom while being attended by nurse • Nurse called CART Team, but no MDA responded Unsuccessful intubation -continued • RT attempted to intubate but unable to do so because blood obstructed airway • Pt intubated after sixteen minutes without oxygen • Death • Lawsuit based upon information contained in the report of the investigation by the Department of Health • Finding: “inaccuracies in documentation“ Case – Transport/Lack of Training • 6/28/13, Hughes v. Cataret General Hospital, NC • Pt, age 13, hit head riding a skateboard • CT at local hospital normal, but decision to transfer to tertiary center because of concern of skull fx, pt. was intubated • Ambulance staffed with 2 EMTs, 1 RN, 1RT • RT licensed less than one year Transport case -continued • Pt awoke, pulled out intubation tube • Ambulance pulled over, parents in car behind ambulance • Crew worked to sedate and re-intubate, RT primarily responsible for intubation • Pt given paralytics and sedatives • Pt intubated in esophagus, no confirmation testing, i.e. colorimetric testing or capnography Transport - continued • HR 30, no pulse, CPR initiated, epinephrine • Defibrillator utilized • Called ED MD to obtain permission for use of Amiodarone, MD advised to check tube placement and suction, alleged no testing performed • Ambulance diverted to another closer hospital • RT in ED extubated and re-intubated at Carolina East Hospital Transport – continued • Pt transferred to tertiary hospital, Vidant Medical Center • No brain activity, life support withdrawn • Father employed at hospital • Suit filed, allegations against hospital were that RT failed to keep patient sedated and was not trained in transport Case – Repositioning of ET tube • 2008, San Diego area • Pt, Florida resident at California weight loss spa • Pt admitted to hospital for tonsil abscess • Surgery performed, taken to PACU • Radiologist called RN in PACU to advise that endotracheal tube needed to be repositioned • RT at RN’s instruction repositioned tube Repositioning of ET tube – continued • Pt died • Autopsy – complications from tonsillar abscess • Allegations of “cover up” by hospital Negligent Intubation • Tennessee case • Pt. admitted for repair of brain aneurysm • Tracheostomy performed, stay suture placed to help reinsert the trach if became dislodged • Trach dislodged while pt being turned • Several unsuccessful intubation attempts Negligent intubation - continued • Surgeon who performed trach pulled suture line which opened airway and allowed intubation • Prolonged oxygen deprivation, patient had brain injury and required life time care • Settled for confidential amount Negligent Ventilator Setup • Tennessee case • Same plaintiff’s lawyer, John Day in Nashville • Minor child born prematurely, d/c home on ventilator • Periods where child could breathe without the assistance of the ventilator. • Mother detected an irregularity with ventilator Negligent Ventilator Setup • RT set up a backup ventilator and allegedly improperly set the control settings. • Mother awakened by irregular breath sounds from ventilator • Trach tube attached to ventilator had come out of child’s neck. • Due to improper settings, the ventilator alarm did not sound. • Child suffered permanent injuries • Case settled during mediation Timeline for Med Mal Speedy Justice is a Myth • • • • • • • February 7, 2010 Feb. 20, 2010 February 19, 2011 June 18, 2011 December, 2011 December, 2012 March 2013 Pt. admitted to hospital Pt. expires Notice of Intent letter Lawsuit filed Discovery begins First Trial date New trial date Exposure Areas for RT • • • • • Airway management Medications (Atrovent/glaucoma) Vents/alarms and other equipment failures Infection Failure Patient falls Protection • If an employee of a hospital or nursing home or other entity, then should be an insured under your employer’s professional liability (med-mal) insurance policy • If you work as an “independent contractor” for an entity, or if you do work for an agency part-time or PRN, then you may or may not be covered. Confirm in writing if you are covered by med mal insurance. Documentation • Central Focus in every medical malpractice case • Best friend v. worse enemy • Shield or sword Documentation Myth • If it’s not documented, it wasn’t done. – If not documented, it’s not documented. – Impossible to document every action. – Patient care priority not documentation. Medical Record – Legal Aspects • • • • Internal Peer Review Investigations by Department of Health Disciplinary Investigations by Licensing Boards Medical Malpractice Lawsuits Documentation – All Relevant • Physicians’ orders, progress notes, operative notes, H & P, Discharge, etc • Nurses’ notes • Dietary • Imaging • Labs • Pathology • Physical Therapy • Respiratory Therapy Common Charting Errors • • • • • • Omissions Vagueness Inconsistency Alterations or additions Subjective versus Objective Descriptions Unapproved Abbreviations Electronic Health Record Legal Implications • New in legal cases – Initial Impressions • Confusion can lead to suspicion that information is missing or being withheld. – What clinician views on screen may not exist. – Systems built for care not court. • Not Fit for Print – What prints is usually not the format that provider is used to viewing. – Nearly impossible to reproduce exactly what provider saw – Views differ between provider, i.e. MD sees different screen than RT or nurse EHR – legal implications • Conflicting terms – varying definitions, e.g. “Accept” • Could mean a record was pending, filed, shared, or officially accepted by a physician. • Paper record, pending would be equivalent of MD writing note on a piece of paper, helpful at the time, but not intended for the medical record, like sticky note EHR – legal implications • Time Stamps • Even time stamps, which would seem to be irrefutable, may need explaining, e.g. RT takes pulse ox at 9 am. But does not close the entry for another 30 minutes, reading may post to the record with a time stamp of 930. • Or RT testifies she was in ED at 1000, but HER indicates she accessed records on another floor at the same moment. The time stamp may have been recorded when a coworker completed and filed the record—after RT raced to the ED. • Both instances require explanation in court. EHR - Legal Implications • Audit Trails – Now regularly requested in med mal cases – In most cases more than one witness is needed to explain how the system works – Issues relate to record creation, storage, and metadata – One case required hospital to bring vendor’s trainer to explain system Audit Trails • Used to contradict knowledge of provider, e.g. • Patient returned to ED, MD testified that she was unaware of patient’s return to ED, audit trail revealed that MD was aware • Not relevant to SOC issues, but now MD’s credibility at worse, memory at best, is in dispute. Concerning Aspects of EHR • Every assessment is identical, day after day, page after page, and problem created is whether provider made a new assessment or simply pressed a key to restate prior assessment. E.g. case where neuro assessment is identical, down to same typographical errors. • Critical clinical documentation looks exactly the same as someone’s dietary assessment. Other issues • EHR information more legible • Pop-up alerts, reminders for follow-up • See in pharmacy cases with drug interactions • Copy and Paste Function can perpetuate mistakes • Error as easy as click of mouse Questions?
© Copyright 2026