PI-19668 (02/06) ACE INA PRIVACY STATEMENT The ACE INA
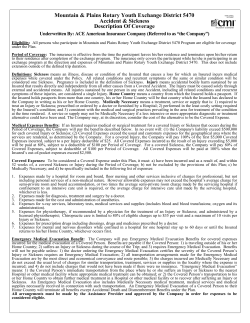
ACE INA PRIVACY STATEMENT The ACE INA group of companies strongly believes in maintaining the privacy of information we collect about individuals. We want you to understand how and why we use and disclose the collected information. The following provides details of our practices and procedures for protecting the security of nonpublic personal information that we have collected about individuals. This privacy statement applies to policies underwritten by ACE American Insurance Company. INFORMATION WE COLLECT The information we collect will vary depending on the type of product or service individuals seek or purchase, and may include: • • • Information we receive from individuals, such as their name, address, age, phone number, social security number, assets, income, or beneficiaries; Information about individuals’ transactions with us, with our affiliates, or with others, such as policy coverage, premium, payment history, motor vehicle records; and Information we receive from a consumer reporting agency, such as a credit history. INFORMATION WE DISCLOSE We do not disclose any personal information to anyone except as is necessary in order to provide our products or services to a person, or otherwise as we are required or permitted by law. We may disclose any of the information that we collect to companies that perform marketing services on our behalf or to other financial institutions with whom we have joint marketing agreements. THE RIGHT TO VERIFY THE ACCURACY OF INFORMATION WE COLLECT Keeping information accurate and up to date is important to us. Individuals may see and correct their personal information that we collect except for information relating to a claim or a criminal or civil proceeding. CONFIDENTIALITY AND SECURITY We restrict access to personal information to our employees, our affiliates' employees, or others who need to know that information to service the account or in the course of conducting our normal business operations. We maintain physical, electronic, and procedural safeguards to protect personal information. CONTACTING US If you have any questions about this privacy statement or would like to learn more about how we protect privacy, please write to us at ACE INA Customer Services, P.O. Box 1000, 436 Walnut Street, WA04F, Philadelphia, PA 19106. Please include the policy number on any correspondence with us. ACE American Insurance Company PI-19668 (02/06) DISTRICT OF COLUMBIA LIFE AND HEALTH INSURANCE GUARANTY ASSOCIATION NOTICE SUMMARY OF GENERAL PURPOSES AND CURRENT LIMITATIONS OF COVERAGE Residents of the District of Columbia who purchase health insurance, life insurance and annuities should know that the insurance companies licensed in the District of Columbia to write these types of insurance are members of the District of Columbia Life and Health Insurance Guaranty Association (“Guaranty Association”). The purpose of the Guaranty Association is to assure that policyholders will be protected, within limits, in the unlikely event that a member insurer becomes financially unable to meet its obligations. If this should happen, the Guaranty Association will assess its other member insurance companies for the money to pay the claims of insured persons who live in the District of Columbia and, in some cases, to keep coverage in force. The valuable extra protection provided by insurers through the Guaranty Association is limited, however, as noted on the other side of this page. District of Columbia Life and Health Insurance Guaranty Association Disclaimer The District of Columbia Life and Health Insurance Guaranty Association provides coverage of claims under some types of policies if the insurer becomes impaired or insolvent. COVERAGE MAY NOT BE AVAILABLE FOR YOUR POLICY. Even if coverage is provided, there are significant limitations and exclusions. Coverage is generally conditioned on residence in the District of Columbia. Other conditions may also preclude coverage. The District of Columbia Life and Health Insurance Guaranty Association or the District of Columbia Insurance Commissioner will respond to any questions you may have which are not answered by this document. Your insurer and agents are prohibited by law from using the existence of the Association or its coverage to sell you an insurance policy. You should not rely on availability of coverage under the Life and Health Insurance Guaranty Association Act of 1992 when selecting an insurer. Policyholders with additional questions may contact: Mr. Robert M. Willis Executive Director District of Columbia Life and Health Insurance Guaranty Association 1200 G Street, N.W. Washington, DC 20005 (202) 434-8771 Fax: (202) 347-2990 Ms. Gennet Purcell Commissioner District of Columbia Department of Insurance, Securities and Banking 810 First Street, N.E., Suite 701 Washington, DC 20002 (202) 727-8000 The District of Columbia law that provides for this safety-net coverage is called the Life and Health Insurance Guaranty Association Act of 1992. The other side of this page contains a brief summary of this law's coverages, exclusions and limits. This summary does not cover all provisions of the law; nor does it in any way change anyone's rights or obligations under the Act or the rights or obligations of the Guaranty Association. If you have obtained this document from an agent in connection with the purchase of a policy, you should be aware that its delivery to you does not guarantee that your policy is covered by the Guaranty Association. Revised 01152010 COVERAGE Generally, individuals will be protected by the District of Columbia Life and Health Insurance Guaranty Association if they live in the District of Columbia and are insured under a health insurance, life insurance, or annuity contract issued by a member insurer, or if they are insured under a group insurance contract, issued by a member insurer. The beneficiaries, payees or assignees of insured persons are protected as well, even if they live in another state. EXCLUSIONS FROM COVERAGE However, persons holding such policies are not protected by the Guaranty Association if: • they are eligible for protection under the laws of another state. This may occur when the insolvent insurer was incorporated in another state whose guaranty association protects insureds who live outside of that state of incorporation; • their insurer was not authorized to do business in the District of Columbia; or • their policy was issued by a charitable organization, a fraternal benefit society, a mandatory state pooling plan, a mutual assessment company, an insurance exchange, a non-profit hospital or medical service organization, a health maintenance organization, or a risk retention group. The Guaranty Association also does not provide coverage for: • any policy or portion of a policy which is not guaranteed by the insurer or for which the individual has assumed the risk; • any policy of reinsurance unless an assumption certificate was issued; • any plan or program of an employer or association that provides life, health, or annuity benefits to its employees or members to the extent the plan is self-funded or uninsured; • interest rate guarantees that exceed certain statutory limitations; • dividends, experience rating credits, or fees for services in connection with a policy; • credits given in connection with the administration of a policy by a group contract holder; or • unallocated annuity contracts. LIMITS ON AMOUNT OF COVERAGE The Act also limits the amount the Guaranty Association is obligated to pay. The benefits for which the Guaranty Association may become liable shall be limited to the lesser of: • the contractual obligations for which the insurer is liable or for which the insurer would have been liable if it were not an impaired or insolvent insurer, or, • with respect to any one life, regardless of the number of policies, contracts, or certificates: o $300,000 in life insurance death benefits but not more than $100,000 in net cash surrender or net cash withdrawal values for life insurance; or o $100,000 in health insurance benefits, including net cash surrender or net cash withdrawal values; or o $300,000 in the present value of annuity benefits, including net cash surrender or net cash withdrawal values. Finally, in no event is the Guaranty Association liable for more than $300,000 with respect to any one individual. Revised 01152010 ACE American Insurance Company (A Stock Company) Philadelphia, PA 19106 Blanket Accident and Sickness Policy POLICYHOLDER: Trustee of the ACE USA Accident & Health Insurance Trust POLICY NUMBER: GLM N04947988R POLICY EFFECTIVE DATE: October 1, 2011 POLICY TERM: October 1, 2011 to October 1, 2012 STATE OF DELIVERY: District of Columbia This Policy takes effect at 12:00 a.m. (midnight) at the Policyholder’s address on the Policy Effective Date shown above. It will remain in effect for the duration of the Policy Term shown above if the premium is paid according to the agreed terms. This Policy terminates at 12:00 a.m. (midnight) at the Policyholder’s address, on the last day of the Policy Term unless the Policyholder and We agree to continue coverage under this Policy for an additional Policy Term. If coverage is continued for an additional Policy Term and the required premiums are paid on or before the Premium Due Date, We will issue an amendment to identify the new Policy Term. This Policy is governed by the laws of the state in which it is delivered. Signed for ACE AMERICAN INSURANCE COMPANY at Philadelphia, Pennsylvania THIS IS A BLANKET LIMITED MEDICAL INSURANCE POLICY. IT PAYS OUT-OF-COUNTRY MEDICAL EXPENSE BENEFITS ONLY. PLEASE READ THE POLICY CAREFULLY. AH-15090 ACE American Insurance Company 1 TABLE OF CONTENTS SECTION PAGE SCHEDULE OF BENEFITS.......................................................................................................... 3 DEFINITIONS ............................................................................................................................... 8 ELIGIBILITY FOR INSURANCE ................................................................................................. 11 EFFECTIVE DATE OF INSURANCE ......................................................................................... 11 TERM OF COVERAGE .............................................................................................................. 11 TERMINATION DATE OF INSURANCE .................................................................................... 11 SCOPE OF COVERAGE ....................................................................................................................12 DESCRIPTION OF BENEFITS................................................................................................... 12 EXCLUSIONS............................................................................................................................. 18 CLAIM PROVISIONS.................................................................................................................. 21 ADMINISTRATIVE PROVISIONS .............................................................................................. 22 GENERAL PROVISIONS ........................................................................................................... 23 AH-15090 ACE American Insurance Company 2 SCHEDULE OF BENEFITS PREMIUM DUE DATE: Monthly in arrears, on or before the 15th of each month. CLASSES OF ELIGIBLE PERSONS: A person may be insured only under one Class of Eligible Persons even though he or she may be eligible under more than one class. Also, a person may not be insured as a Dependent and an Insured at the same time. Class 1 Citizens or Permanent residents of the U.S. and Pratt Institute international students that have a current passport and are temporarily residing outside the U.S. and registered in a U.S. academic institution or in a recognized study abroad program. Dependents of Class 1 Insureds are eligible for coverage under this Policy. *For purposes of this insurance, if the Eligible Person’s Home Country (passport country) is different from the Eligible Person’s country of permanent residence (location in which the Eligible Person permanently resides), the Eligible Person will not be covered in either location. Permanent residents are not eligible for coverage under this Policy. COVERED ACTIVITIES: We will pay the benefits described in this Policy only if a Covered Person suffers a loss or incurs a Covered Expense as the direct result of a Covered Accident or Sickness while traveling: 1. outside of his or her Home Country; 2. up to the Maximum Period of Coverage shown in the Schedule of Benefits; and 3. engaging in educational or research activities. BENEFITS MEDICAL EXPENSE BENEFITS Maximum Lifetime Benefit: $500,000 Maximum Benefit for: Covered Accident or Sickness that occurs while participating in an amateur, club, intramural, interscholastic, or intercollegiate sport: $5,000 All other Covered Accident or Sickness: $250,000 Covered Inpatient Expenses For Hospital Room & Board: Maximum Benefit: Maximum Benefit Period per Occurrence: AH-15090 ACE American Insurance Company $1,000 per day 30 days 3 For Intensive Care Unit: Additional $600 per day for up to 8 days Maximum for Ancillary Hospital Expenses: $500 per day Maximum for Doctor’s Non-Surgical Expenses Initial Visit: Each Medically Necessary Follow-up Visit: Consultant Visit: Pre-Admission Tests within 7 days before Hospital admission: $60 $60 per visit for 1 visit per day for up to a maximum of 30 visits $400 $900 Doctor’s Surgical Expense Maximum Benefit per Occurrence: $,000 Maximum for Anesthetics and their administration: 25% of Surgical Allowance Maximum for Assistant Surgeon: 25% of Surgical Allowance Covered Outpatient Expenses Doctor’s Surgical Expense Maximum Benefit per Occurrence: $50,000 Maximum Anesthetics and their administration: 25% of Surgical Allowance Maximum Assistant Surgeon: 25% of Surgical Allowance Maximum for Doctor’s Non-Surgical Expenses: $60 per visit for 1 visit per day for up to a maximum of 30 visits Maximum for Outpatient Diagnostic X-Rays and Lab Services for: CAT Scan, PET Scan or MRI: All Other Procedures: Maximum for Medical Emergency Expenses: For Prescription Drugs* Benefit Maximum per Policy Term: AH-15090 ACE American Insurance Company $250 $400 75% of the Usual & Customary up to a maximum of $10,000 $1,000 4 Other Covered Expenses Maximum for Ambulance Services: $400 Maximum for Initial Orthopedic Prosthesis or brace: $1,000 Maximum for Rehabilitative Braces or appliances: $1,000 Maximum for Emergency Replacement of Eyeglasses, Contact lenses and Hearing Aids: $300 Maximum for Physiotherapy/Physical Medicine: (includes Chiropractic and Acupuncture expenses) $75 per visit for 1 visit per day for up to a maximum of 12 visits Maximum for Chemotherapy and/or Radiation Therapy: $1,000 For Mental and Nervous Expenses (Psychotherapy) Benefit Maximum per Policy Term: Maximum Number of Days: Maximum for Pregnancy: paid as any other covered Sickness 40 days $7,500 Additional section Maximum for Newborn Nursery Care: $500 Maximum for Therapeutic Termination of Pregnancy: $500 Maximum for Dental Treatment (Injury Only): $1,000 $2,500 for Deductible: $0 Co-insurance Rate: 100% of the Usual Customary Charges Maximum Benefit Period: Pregnancy: Covered Accidents and all other Covered Sickness: Incurral Period: Pregnancy: Covered Accidents and all other Covered Sickness: Maximum Period of Coverage: AH-15090 ACE American Insurance Company C- and 300 days 90 days from the date of a Covered Accident or Sickness conception must occur while coverage is in force 180 days from the date of a Covered Accident or Sickness 19 months 5 Emergency Medical Benefits Benefit Maximum: up to $10,000 Emergency Medical Evacuation Benefit Benefit Maximum: 100% of the Covered Expenses Emergency Reunion Benefit Benefit Maximum: $2,500 Daily Benefit Maximum: $100 Maximum Number of Days: 7 days Lost Baggage Benefit Deductible per Trip: $0 Benefit Maximum per Trip: $500 Benefit Maximum per Item or Set of Items: $250 subject to a Maximum of 2 bags Repatriation of Remains Benefit Benefit Maximum: 100% of the Covered Expenses Trip Interruption Benefit Benefit Maximum: $2,500 AGGREGATE LIMIT: Benefit Maximum: $250,000 We will not pay more than the Benefit Maximum for all losses per Covered Accident. If, in the absence of this provision, We would pay more than Benefit Maximum for all losses from one Covered Accident, then the benefits payable to each person with a valid claim will be reduced proportionately, so the total amount We will pay is the Benefit Maximum. Accidental Death & Dismemberment Benefits Principal Sum: $25,000 Time Period for Loss: 365 days from the date of a Covered Accident Coma Benefit Benefit Amount: AH-15090 Benefits are payable initially as 1% of the Principal Sum per Month up to 11 months and thereafter in a lump sum of 100% of the Principal Sum ACE American Insurance Company 6 INITIAL PREMIUM RATES: Covered Person Class 1 Insured: Age 25 and under: Age 26-29: Age 30-65: Dependents: AH-15090 Monthly Premium $ 31.00 $ 50.00 $126.00 $165.00 ACE American Insurance Company 7 DEFINITIONS Please note, certain words used in this document have specific meanings. These terms will be capitalized throughout the document. The definition of any word, if not defined in the text where it is used, may be found either in this Definitions section or in the Schedule of Benefits. “Covered Accident” means an accident that occurs while coverage is in force for a Covered Person and results directly and independently of all other causes in a loss or Injury covered by the Policy for which benefits are payable. “Covered Activity ” means any activity that the Policyholder requires the Covered Person to attend, or that is under its supervision and control listed in the Schedule of Benefits and insured under the Policy. “Covered Expenses” means expenses actually incurred by or on behalf of a Covered Person for treatment, services and supplies covered by the Policy. Coverage under the Policyholder’s Policy must remain continuously in force from the date of the Covered Accident or Sickness until the date treatment, services or supplies are received for them to be a Covered Expense. A Covered Expense is deemed to be incurred on the date such treatment, service or supply, that gave rise to the expense or the charge, was rendered or obtained. “Covered Loss” or “Covered Losses” means an accidental death, dismemberment or other Injury covered under the Policy. “Covered Person” means any Insured and Dependent who enrolls for coverage and for whom the required premium is paid. “Deductible” means the dollar amount of Covered Expenses that must be incurred as an outof-pocket expense by each Covered Person per Covered Accident or Sickness basis before Medical Expense Benefits and/or other Additional Benefits paid on an expense incurred basis are payable under the Policy. “Dependent” means an Insured’s lawful spouse under age 66; or an Insured’s unmarried child, from the moment of birth to age 19, 26 if a full-time student, who is chiefly dependent on the Insured for support. A child, for eligibility purposes, includes an Insured’s natural child; adopted child, beginning with any waiting period pending finalization of the child’s adoption; or a stepchild who resides with the Insured or depends chiefly on the Insured for financial support. A Dependent may also include any person related to the Insured by blood or marriage and for whom the Insured is allowed a deduction under the Internal Revenue Code. Insurance will continue for any Dependent child who reaches the age limit and continues to meet the following conditions: 1) the child is handicapped, 2) is not capable of self-support and 3) depends chiefly on the Insured for support and maintenance. The Insured must send Us satisfactory proof that the child meets these conditions, when requested. We will not ask for proof more than once a year. If the Insured has elected coverage for a Dependent child, any newly born child of the Insured will be covered from the moment of birth for 31 days. Coverage may be continued beyond this time period if the Insured notifies Us within 31 days of the child’s birth and pays any required premium. AH-15090 ACE American Insurance Company 8 “Doctor” means a licensed health care provider acting within the scope of his or her license and rendering care or treatment to a Covered Person that is appropriate for the conditions and locality. It will not include a Covered Person or a member of the Covered Person’s Immediate Family or household. “Home Country ” means a country from which the Covered Person holds a passport. If the Covered Person holds passports from more than one country, his or her Home Country will be that country which the Covered Person has declared to Us in writing as his or her Home Country. “Hospital” means an institution that: 1) operates as a Hospital pursuant to law for the care, treatment, and providing of in-patient services for sick or injured persons; 2) provides 24-hour nursing service by Registered Nurses on duty or call; 3) has a staff of one or more licensed Doctors available at all times; 4) provides organized facilities for diagnosis, treatment and surgery, either: (i) on its premises; or (ii) in facilities available to it, on a pre-arranged basis; 5) is not primarily a nursing care facility, rest home, convalescent home, or similar establishment, or any separate ward, wing or section of a Hospital used as such; and 6) is not a place solely for drug addicts, alcoholics, or the aged or any separate ward of the Hospital. “Immediate Famil y Me mber” means a person who is related to the Covered Person in any of following ways: spouse; parent (includes stepparent); child age 18 or older (includes legally adopted and step child); brother or sister (includes stepbrother or stepsister); parent-in-law; son- or daughter–in–law; and brother- or sister-in-law. “Injury” means accidental bodily harm sustained by a Covered Person that results directly and independently from all other causes from a Covered Accident. The Injury must be caused solely through external, violent and accidental means. All injuries sustained by one person in any one Covered Accident, including all related conditions and recurrent symptoms of these injuries, are considered a single Injury. “Insured” means a person in a Class of Eligible Persons who enrolls for coverage and for whom the required premium is paid making insurance in effect for that person. An Insured is not a Dependent covered under the Policy. “Medical Emergency” means a condition caused by an Injury or Sickness that manifests itself by symptoms of sufficient severity that a prudent lay person possessing an average knowledge of health and medicine would reasonably expect that failure to receive immediate medical attention would place the health of the person in serious jeopardy. “Medically Necessary ” means a treatment, service, or supply that is: 1) required to treat an Injury or Sickness; 2) prescribed or ordered by a Doctor or furnished by a Hospital; 3) performed in the least costly setting required by the Covered Person’s condition; and 4) consistent with the medical and surgical practices prevailing in the area for treatment of the condition at the time rendered. Purchasing or renting 1) air conditioners; 2) air purifiers; 3) motorized transportation equipment; 4) escalators or elevators in private homes; 5) eyeglass frames or lenses; 6) hearing aids; 7) swimming pools or supplies for them; and 8) general exercise equipment are not Medically Necessary. A service or supply may not be Medically Necessary if a less intensive or more appropriate diagnostic or treatment alternative could have been used. We may consider the cost of the alternative to be the Covered Expense. AH-15090 ACE American Insurance Company 9 “Sickness” means an illness, disease or condition of the Covered Person that causes a loss for which a Covered Person incurs medical expenses while covered under the Policy. All related conditions and recurrent symptoms of the same or similar condition will be considered one Sickness. Pregnancy is included in the definition of Sickness. “Trip” means Policyholder sponsored travel by air, land, or sea from the Covered Person’s Home Country. “Usual and Customary Cha rge” means the average amount charged by most providers for treatment, service or supplies in the geographic area where the treatment, service or supply is provided. “We”, “ Our”, “Us” means the insurance company underwriting this insurance or its authorized agent. AH-15090 ACE American Insurance Company 10 ELIGIBILITY FOR INSURANCE Each person in one of the Classes of Eligible Persons shown in the Schedule of Benefits is eligible to be insured on the Policy Effective Date, or the day after he or she becomes eligible, if later. We maintain the right to investigate eligibility status and attendance records to verify eligibility requirements are met. If We discover the eligibility requirements are not met, Our only obligation is to refund any premium paid for that person. An Insured’s Dependent is eligible on the date: 1. the Insured is eligible, if the Insured has Dependents on that date; or 2. the date the person becomes a Dependent, if later. In no event will a Dependent be eligible if the Insured is not eligible. EFFECTIVE DATE OF INSURANCE Insurance for an Eligible Person who is required to contribute to the cost of this insurance or insurance for an Insured’s Dependent who enrolls during the enrollment period is effective on the latest of the following dates: 1. the Policy Effective Date; 2. the date We receive the completed enrollment form, if any; 3. the date the required premium is paid; 4. the date of the scheduled Trip departure date; or 5. the date of his or her departure from his or her Home Country. A Dependent’s insurance will not be in effect prior to the date an Eligible Person is insured. TERM OF COVERAGE This coverage will start on the actual start of the Trip. It does not matter whether the Trip starts at the Covered Person’s home, place of work, or other place. It will end on the first of the following dates to occur: 1. The date the Covered Person returns to his or her Home Country 2. The date the Covered Person makes a Personal Deviation. “Personal Deviation” means: 1. An activity that is not reasonably related to Covered Activity; and 2. Not incidental to the purpose of the Trip. TERMINATION DATE OF INSURANCE An Insured’s coverage will end on the earlier of the date: 1. the policy terminates; 2. the Insured is no longer eligible; 3. the date the Insured reaches age 66; 4. the period ends for which premium is paid; 5. the scheduled Trip return date; 6. the Insured returns to his or her Home Country; AH-15090 ACE American Insurance Company 11 7. 8. the date the Policyholder’s participation under the Policy ends; or the Trip exceeds the Maximum Period of Coverage. A Dependent’s coverage will end on the earliest of the date: 1. he or she is no longer a Dependent; 2. the Insured’s coverage ends; 3. the period ends for which premium is paid; 4. the scheduled Trip return date; 5. the Dependent returns to his or her Home Country; 6. the date the Policyholder’s participation under the Policy ends; or 7. the Trip exceeds the Maximum Period of Coverage. SCOPE OF COVERAGE Full Excess Benefits We pay Covered Expenses: 1. after the Covered Person satisfies any Deductible; and 2. only when they are in excess of amounts paid by any other Health Care Plan. We pay benefits without regard to any Coordination of Benefits provisions in any other Health Care Plan. “Health Care Plan” means a policy or other benefit or service arrangement for medical or dental care or treatment under: 1) group or blanket coverage, whether on an insured or self-funded basis; 2) hospital or medical service organizations on a group basis; 3) Health Maintenance Organizations on a group basis; 4) group labor-management plans; 5) employee benefit organization plans; 6) association plans on a group or franchise basis; or 7) any other group employee welfare benefit plan as defined in the Employee Retirement Income Security Act of 1974, as amended. DESCRIPTION OF BENEFITS The following Provisions explain the benefits available under the Policy. Schedule of Benefits for the applicability of these benefits on a class level. Please see the MEDICAL EXPENSE BENEFITS We will pay Medical Expense Benefits for Covered Expenses that result directly, and from no other cause, from a Covered Accident or Sickness. These benefits are subject to the Deductibles, Coinsurance Rates, Maximum Benefit Period, Benefit Maximums and other terms or limits shown in the Schedule of Benefits. Medical Expense Benefits are only payable: 1. for Usual and Customary Charges incurred after the Deductible, if any, has been met; 2. for those Medically Necessary Covered Expenses that the Covered Person incurs; 3. for charges incurred for services rendered to the Covered Person while traveling outside of his or her Home Country; and AH-15090 ACE American Insurance Company 12 4. provided the first charge is incurred within the Incurral Period shown in the Schedule of Benefits. Covered Medical Expenses 1. Hospital Room and Board Expenses: the daily room rate when a Covered Person is Hospital Confined and general nursing care is provided and charged for by the Hospital. In computing the number of days payable under this benefit, the date of admission will be counted but not the date of discharge. 2. Ancillary Hospital Expenses: services and supplies including operating room, laboratory tests, anesthesia and medicines (excluding take home drugs) when Hospital Confined. This does not include personal services of a non-medical nature. 3. Daily Intensive Care Unit Expenses: the daily room rate when a Covered Person is Hospital Confined in a bed in the Intensive Care Unit and nursing services other than private duty nursing services. 4. Medical Emergency Care (room and supplies) Expenses: incurred within 72 hours of a Covered Accident or onset of a covered Sickness and including the attending Doctor's charges, X-rays, laboratory procedures, use of the emergency room and supplies. 5. Newborn Nursery Care Expenses. 6. Outpatient Surgical Room and Supplies Expenses for use of the surgical facility. 7. Outpatient diagnostic X-rays, laboratory procedures and tests. 8. Doctor Non-Surgical Treatment/Examination Expenses (excluding medicines) including the Doctor's initial visit, each Medically Necessary follow-up visit and consultation visits when referred by the attending Doctor. 9. Doctor's Surgical Expenses. 10. Assistant Surgeon Expenses when Medically Necessary. 11. Anesthesiologist Expenses for pre-operative screening and administration of anesthesia during a surgical procedure whether on an inpatient or outpatient basis. 12. Outpatient Laboratory Test Expenses. 13. Physiotherapy/Physical Medicine/Chiropractic/Acupuncture Expenses on an inpatient or outpatient basis limited to one visit per day (as shown in the Schedule of Benefits). Expenses include treatment and office visits connected with such treatment when prescribed by a Doctor, including diathermy, ultrasonic, whirlpool, or heat treatments, adjustments, manipulation, massage or any form of physical therapy. 14. X-ray Expenses (including reading charges) but not for dental X-rays. 15. Dental Expenses including dental x-rays for the repair or treatment of each injured tooth that is whole, sound and a natural tooth at the time of the accident, and emergency AH-15090 ACE American Insurance Company 13 alleviation of dental pain. 16. Dental Expenses for impacted wisdom tooth. 17. Outpatient Registered Nurse Services if ordered by a Doctor. 18. Ambulance Expenses for transportation from the emergency site to the Hospital. 19. Rehabilitative braces or appliances prescribed by a Doctor. They must be durable medical equipment that 1) are primarily and customarily used to serve a medical purpose; 2) can withstand repeated use; and 3) generally are not useful to a person in the absence of Injury. No benefits will be paid for rental charges in excess of the purchase price. 20. Prescription Drug Expenses including dressings, drugs and medicines prescribed by a Doctor and administered on an outpatient basis. 21. Medical Equipment Rental Expenses for a wheelchair or other medical equipment that has therapeutic value for a Covered Person. We will not cover computers, motor vehicles or modifications to a motor vehicle, ramps and installation costs, eyeglasses and hearing aids. 22. Medical Services and Supplies: expenses for blood and blood transfusions; oxygen and its administration. 23. Eyeglasses, contact lenses and hearing aids when damage occurs in a Covered Accident that requires medical treatment. 24. Mental and Nervous Disorders: expenses for treatment of a disorder that results, directly and from no other cause, from a Covered Accident or Sickness, while Hospital Confined or on an outpatient basis. Benefits are limited to one treatment per day. "Mental and Nervous Disorders" means neurosis, psychoneurosis, psychopathy, psychosis, or mental or emotional disease or disorder of any kind. 25. Expenses due to an aggravation or re-injury of a Pre-existing Condition. 26. Therapeutic termination of pregnancy. Emergency Medical Benefits We will pay Emergency Medical Benefits as shown in the Schedule of Benefits for Covered Expenses incurred for emergency medical services to treat a Covered Person. Benefits are payable up to the Maximum Benefit shown in the Schedule of Benefits if the Covered Person: 1. suffers a Medical Emergency during the course of the Trip; and 2. is traveling outside of his or her Home Country. Covered Expenses: 1. Medical Expense Guarantee: expenses for guarantee of payment to a medical provider. 2. Hospital Admission Guarantee: expenses for guarantee of payment to a Hospital or treatment facility. AH-15090 ACE American Insurance Company 14 Benefits for these Covered Expenses will not be payable unless: 1. the charges incurred are Medically Necessary and do not exceed the charges for similar treatment, services, or supplies in the locality where the expense is incurred; and 2. do not include charges that would not have been made if there were no insurance. Benefits will not be payable unless We (or Our authorized assistance provider) authorize in writing, or by an authorized electronic or telephonic means, all expenses in advance, and services are rendered by Our assistance provider. Emergency Medical Evacuation Benefit We will pay Emergency Medical Evacuation Benefits as shown in the Schedule of Benefits for Covered Expenses incurred for the medical evacuation of a Covered Person. Benefits are payable up to the Benefit Maximum shown in the Schedule of Benefits, if the Covered Person: 1. suffers a Medical Emergency during the course of the Trip; 2. requires Emergency Medical Evacuation; and 3. is traveling outside of his or her Home Country. Covered Expenses: 1. Medical Transport: expenses for transportation under medical supervision to a different hospital, treatment facility or to the Covered Person’s place of residence for Medically Necessary treatment in the event of the Covered Person’s Medical Emergency and upon the request of the Doctor designated by Our assistance provider in consultation with the local attending Doctor. 2. Dispatch of a Doctor or Specialist: the Doctor’s or specialist’s travel expenses and the medical services provided on location, if, based on the information available, a Covered Person’s condition cannot be adequately assessed to evaluate the need for transport or evacuation and a doctor or specialist is dispatched by Our service provider to the Covered Person’s location to make the assessment. 3. Return of Dependent Child(ren): expenses to return each Dependent child who is under age 18 to his or her principal residence if a) the Covered Person is age 18 or older; and b) the Covered Person is the only person traveling with the minor Dependent child(ren); and c) the Covered Person suffers a Medical Emergency and must be confined in a Hospital. 4. Escort Services: expenses for an Immediate Family Member or companion who is traveling with the Covered Person to join the Covered Person during the Covered Person’s emergency medical evacuation to a different hospital, treatment facility, or the Covered Person’s place of residence. “Immediate Family Member” means a Covered Person’s spouse, child, brother, sister, parent, grandparent, or in-laws. Benefits for these Covered Expenses will not be payable unless: 1. the Doctor ordering the Emergency Medical Evacuation certifies the severity of the Covered Person’s Medical Emergency requires an Emergency Medical Evacuation; 2. all transportation arrangements made for the Emergency Medical Evacuation are by the most direct and economical conveyance and route possible; 3. the charges incurred are Medically Necessary and do not exceed the charges for similar transportation, treatment, services, or supplies in the locality where the expense is incurred; and 4. do not include charges that would not have been made if there were no insurance. AH-15090 ACE American Insurance Company 15 Benefits will not be payable unless We (or Our authorized assistance provider) authorize in writing, or by an authorized electronic or telephonic means, all expenses in advance, and services are rendered by Our assistance provider. In the event the Covered Person refuses to be medically evacuated, we will not be liable for any medical expenses incurred after the date medical evacuation is recommended. Emergency Reunion Benefit We will pay up to the Benefit Maximum as shown in the Schedule of Benefits for expenses incurred to have a Covered Person’s Family Member accompany him or her to the Covered Person’s Home Country or the Hospital where the Covered Person is confined if the Covered Person is: 1) confined in a Hospital for at least 3 days due to a covered Injury or Sickness and the attending Doctor believes it would be beneficial for the Covered Person to have an Family Member at his or her side; or 2) the victim of a Felonious Assault. The Family Member’s travel must take place within 3 days of the date the Covered Person is confined in the Hospital, or the date of the occurrence of the Felonious Assault. “Felonious Assault” means a violent or criminal act reported to the local authorities which was directed at the Covered Person during the course of, or an attempt of, a physical assault resulting in serious injury, kidnapping, or rape. Covered expenses include an economy airline ticket and other travel related expenses not to exceed the Daily Benefit Maximum and the Maximum Number of Days shown in the Schedule of Benefits. All transportation and lodging arrangements must be made by the most direct and economical route and conveyance possible and may not exceed the usual level of charges for similar transportation or lodging in the locality where the expense is incurred. Benefits will not be payable unless We (or Our authorized assistance provider) authorize in writing, or by an authorized electronic or telephonic means, all expenses in advance, and services are rendered by Our assistance provider. “Family Member” means a Covered Person’s parent, sister, brother, husband, wife, child, grandparent, or immediate in-law. Repatriation of Remains Benefit We will pay Repatriation Benefits as shown in the Schedule of Benefits for preparation and return of a Covered Person’s body to his or her home if he or she dies as a result of a Medical Emergency while traveling outside of his or her Home Country. Covered expenses include: 1. expenses for embalming or cremation; 2. the least costly coffin or receptacle adequate for transporting the remains; 3. transporting the remains; 4. Escort Services: expenses for an Immediate Family Member or companion who is traveling with the Covered Person to join the Covered Person’s body during the repatriation to the Covered Person’s place of residence. All transportation arrangements must be made by the most direct and economical route and conveyance possible and may not exceed the Usual and Customary Charges for similar transportation in the locality where the expense is incurred. Benefits will not be payable unless AH-15090 ACE American Insurance Company 16 We (or Our authorized assistance provider) authorize in writing, or by an authorized electronic or telephonic means, all expenses in advance, and services are rendered by Our assistance provider. Lost Baggage Benefit We will reimburse the Covered Person’s replacement costs of clothes and personal hygiene items, up to the Benefit Maximum shown in the Schedule of Benefits, if the Covered Person’s luggage is checked onto a common carrier, and is then lost, stolen, or damaged beyond his or her use. Replacement costs are calculated on the basis of the depreciated standard for the specific personal item claimed and its average usable period. The Covered Person must file a formal claim with the transportation provider and provide Us with copies of all claim forms and proof that the transportation provider has paid the Covered Person its normal reimbursement for the lost, stolen, or damaged luggage. Trip Interruption Benefit We will reimburse the cost of a round-trip economy air and/or ground transportation ticket for a Covered Person’s Trip, up to the Benefit Maximum shown in the Schedule of Benefits, if his or her Trip is interrupted as the result of: 1. the death of a Family Member; or 2. the unforeseen Injury or Sickness of the Covered Person or a Family Member. The Injury or Sickness must be so disabling as to reasonably cause a Trip to be interrupted; or 3. a Medically Necessary covered Emergency Medical Evacuation to return the Covered Person to his or her Home Country or to the area from which he or she was initially evacuated for continued treatment, recuperation and recovery of an Injury or Sickness; or 4. substantial destruction of the Covered Person’s principal residence by fire or weather related activity. “Family Member” means a Covered Person’s parent, sister, brother, spouse, child, grandparent, or in-law. Accidental Death & Dismemberment Benefits If Injury to the Covered Person results, within the Time Period for Loss shown in the Schedule of Benefits, in any one of the losses shown below, We will pay the Benefit Amount shown below for that loss. The Principal Sum is shown in the Schedule of Benefits. If multiple losses occur, only one Benefit Amount, the largest, will be paid for all losses due to the same Covered Accident. Covered Loss Schedule of Covered Losses Benefit Amount Life ........................................................................................................100% of the Principal Sum Two or more Members..........................................................................100% of the Principal Sum Quadriplegia..........................................................................................100% of the Principal Sum One Member ...........................................................................................50% of the Principal Sum Hemiplegia ..............................................................................................50% of the Principal Sum Paraplegia...............................................................................................75% of the Principal Sum Thumb and Index Finger of the Same Hand...........................................25% of the Principal Sum Uniplegia .................................................................................................25% of the Principal Sum AH-15090 ACE American Insurance Company 17 “Quadriplegia” means total Paralysis of both upper and lower limbs. “Hemiplegia” means total Paralysis of the upper and lower limbs on one side of the body. “Uniplegia” means total Paralysis of one lower limb or one upper limb. “Paraplegia” means total Paralysis of both lower limbs or both upper limbs. “Paralysis” means total loss of use. A Doctor must determine the loss of use to be complete and not reversible at the time the claim is submitted. “Member” means Loss of Hand or Foot, Loss of Sight, Loss of Speech and Loss of Hearing. “Loss of Hand or Foot” means complete Severance through or above the wrist or ankle joint. “Loss of Sight” means the total, permanent Loss of Sight of one eye. “Loss of Speech” means total and permanent loss of audible communication that is irrecoverable by natural, surgical or artificial means. “Loss of Hearing” means total and permanent Loss of Hearing in both ears that is irrecoverable and cannot be corrected by any means. “Loss of a Thumb and Index Finger of the Same Hand” means complete Severance through or above the metacarpophalangeal joints of the same hand (the joints between the fingers and the hand). “Severance” means the complete separation and dismemberment of the part from the body. Coma Benefit We will pay the Coma Benefit in a lump sum as shown in the Schedule of Benefits, if a Covered Person becomes Comatose within 31 days of a Covered Accident and remains in a Coma for at least 31 days. We reserve the right, at the end of the first 31 days of Coma, to require proof that the Covered Person remains Comatose. This proof may include, but is not limited to, requiring an independent medical examination at Our expense. A person is deemed to be “Comatose” or in a “Coma”, if he or she is in a profound stupor or state of complete and total unconsciousness, as the result of a Covered Accident. EXCLUSIONS We will not pay benefits for any loss or Injury that is caused by, or result from: 1. intentionally self-inflicted Injury. 2. suicide or attempted suicide. 3. war or any act of war, whether declared or not. 4. piloting or serving as a crewmember or riding in any aircraft except as a fare-paying passenger on a regularly scheduled or charter airline. 5. commission of, or attempt to commit, a felony, an assault or other illegal activity. 6. commission of or active participation in a riot or insurrection. 7. flight in, boarding or alighting from an aircraft or any craft designed to fly above the Earth's surface, except as: a. a fare-paying passenger on a regularly scheduled commercial or charter airline; b. a passenger in a non-scheduled, private aircraft used for pleasure purposes with no commercial intent during the flight; c. a passenger in a military aircraft flown by the Air Mobility Command or its foreign equivalent. 8. travel in or on any on-road and off-road motorized vehicle not requiring licensing as a motor vehicle. 9. an accident if the Covered Person is the operator of a motor vehicle and does not AH-15090 ACE American Insurance Company 18 10. 11. 12. possess a valid motor vehicle operator's license, except while participating in a Driver's Education Program. alcoholism, drug addiction or the use of any drug or narcotic except as prescribed by a Doctor. an accident that occurs while on active duty service in the military, naval or air force of any country or international organization. Upon Our receipt of proof of service, We will refund any premium paid for this time. Reserve or National Guard active duty training is not excluded unless it extends beyond 31 days. for specific named hazards: motorcycling, scuba diving, jet, snow or water skiing, mountain climbing (where ropes or guides are used), sky diving, amateur racing, piloting an aircraft, bungee jumping, spelunking, whitewater rafting, surfing, and parasailing. In addition to the exclusions above, We will not pay Medical Expense Benefits for any loss, treatment or services resulting from: 1. treatment by persons employed or retained by a Policyholder, or by any Immediate Family Member or member of the Covered Person's household. 2. treatment of Osgood-Schlatter's Disease, osteochondritis, osteomyelitis, cardiac disease or conditions, pathological fractures, congenital weakness, detached retina unless caused by an Injury, or mental disorder or psychological or psychiatric care or treatment (except as provided in the Policy), whether or not caused by a Covered Accident or Sickness. 3. damage to or loss of dentures or bridges, or damage to existing orthodontic equipment. 4. expense incurred for treatment of temporomandibular or craniomandibular joint dysfunction and associated myofacial pain. 5. blood, blood plasma, or blood storage, except expenses by a Hospital for processing or administration of blood. 6. cosmetic surgery, except for reconstructive surgery needed as the result of an Injury or Sickness. 7. any elective treatment, surgery, health treatment, or examination, including any service, treatment or supplies that: (a) are deemed by Us to be experimental; and (b) are not recognized and generally accepted medical practices in the United States. 8. eyeglasses, contact lenses, hearing aids, wheelchairs, braces, appliances, examinations or prescriptions for them, or repair or replacement of existing artificial limbs, orthopedic braces, or orthopedic devices, except as provided in the Policy. 9. expenses payable by any automobile insurance policy without regard to fault. (This exclusion does not apply in any state where prohibited.) 10. treatment or service provided by a private duty nurse. 11. eye refractions or eye examinations for the purpose of prescribing corrective lenses or for the fitting thereof, unless caused by an Injury incurred while covered under the Policy. 12. covered medical expenses for which the Covered Person would not be responsible for in the absence of the Policy. 13. conditions that are not caused by a Covered Accident or Sickness. 14. participation in any activity or hazard not specifically covered by the Policy. 15. any treatment, service or supply not specifically covered by the Policy. 16. any treatment, services or supplies received by the Covered Person that are incurred or received while he or she is in his or her Home Country. 17. personal comfort or convenience items. These include but are not limited to: Hospital telephone charges; television rental; or guest meals. 18. routine nursery care. 19. routine physicals. AH-15090 ACE American Insurance Company 19 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. birth defects and congenital anomalies; or complications which arise from such conditions. routine dental care and treatment. rest cures or custodial care. any condition for which the Covered Person is entitled to benefits under any Workers' Compensation Act or similar law. organ or tissue transplants and related services. Injury sustained while participating in professional or semi-professional sports. confinement of institutional care. services, supplies, or treatment including any period of Hospital confinement which were not recommended, approved and certified as necessary and reasonable by a Doctor; or expenses which are non-medical in nature. expenses incurred for services related to the diagnostic treatment of infertility or other problems related to the inability to conceive a child, unless such infertility is a result of a covered Injury or Sickness. expenses Incurred for birth control including surgical procedures and devices. nasal or sinus surgery, except surgery made necessary as the result of a covered Injury, or a deviated nasal septum including sub mucous resection and surgical correction thereof. expenses incurred in connection with weak, strained or flat feet, corns, calluses or toenails. treatment of acne. In addition to the Policy Exclusions, We will not pay Lost Baggage Benefit for: 1. Loss or damage due to: a. Moth, vermin, insects, or other animals; wear and tear; atmospheric or climatic conditions; or gradual deterioration or defective materials or craftsmanship; b. Mechanical or electrical failure; c. Any process of cleaning, restoring, repairing, or alteration; 2. More than a reasonable proportion of the total value of the set where the loss or damaged article is part of a set or pair; 3. Devaluation of currency or shortages due to errors or omissions during monetary transactions; 4. Any loss not reported to either the police or transport carrier within 24 hours of discovery; 5. Any loss due to confiscation or detention by customs or any other authority; 6. Electronic equipment or devices including, but not limited to: cellular telephones; citizen band radios; tape players; radar detectors; radios and other sound reproducing or receiving equipment; PDAs; BlackBerrys; laptop computers; and handheld computers. This insurance does not apply to the extent that trade or economic sanctions or regulations prohibit Us from providing insurance, including, but not limited to, the payment of claims. CLAIM PROVISIONS Notice Of Claim: A claimant must give Us or Our authorized representative written (or authorized electronic or telephonic) notice of claim within 90 days after any loss covered by the Policy occurs. If notice cannot be given within that time, it must be given as soon as reasonably possible. This notice should identify the Covered Person and the Policy Number. AH-15090 ACE American Insurance Company 20 Claim Forms: Upon receiving written notice of claim, We will send claim forms to the claimant within 15 days. If We do not furnish such claim forms, the claimant will satisfy the requirements of written proof of loss by sending the written (or authorized electronic or telephonic) proof as shown below. The proof must describe the occurrence, extent and nature of the loss. Proof Of Loss: Written (or authorized electronic or telephonic) proof of loss must be sent to the agent authorized to receive it. Written (or authorized electronic or telephonic) proof must be given within 90 days after the date of loss. If it cannot be provided within that time, it should be sent as soon as reasonably possible. In no event, except in the absence of legal capacity, will proof of loss be accepted if it is sent later than one year from the time proof is otherwise required. Claimant Cooperation Provision: Failure of a claimant to cooperate with the Us in the administration of a claim may result in the termination of a claim. Such cooperation includes, but is not limited to, providing any information or documents needed to determine whether benefits are payable or the actual benefit amount due. Time Pa yment Of Claims: Any benefits due will be paid when We receive written (or authorized electronic or telephonic) proof of loss. Payment Of Claims: If the Covered Person dies, any death benefits or other benefits unpaid at the time of the Covered Person’s death will be paid to the beneficiary our records indicate the Covered Person designated for these plan benefits. If there is no named beneficiary or surviving beneficiary on record with us or Our authorized agent, We pay benefits in equal shares to the first surviving class of the following: 1) Spouse; 2) Children; 3) Parents; 4) Brothers and sisters. If there are no survivors in any of these classes, We will pay the Covered Person’s estate. All other benefits will be paid to the Covered Person. If the Covered Person is: (1) a minor; or (2) in Our opinion unable to give a valid release because of incompetence, We may pay any amount due to a parent, guardian, or other person actually supporting him or her. Any payment made in good faith will end Our liability to the extent of the payment. Beneficiary: The Covered Person may designate a beneficiary. The Covered Person has the right to change the beneficiary at any time by written (or electronic and telephonic) notice. If the Covered Person is a minor, his or her parent or guardian may exercise this right for him or her. The change will be effective when We or Our authorized agent receive it. When received, the effective date is the date the notice was signed. We are not liable for any payments made before the change was received. We cannot attest to the validity of a change. The Insured is the beneficiary for any covered Dependent. Assignment: At the request of the Covered Person or his or her parent or guardian, if the Covered Person is a minor, medical benefits may be paid to the provider of service. Any payment made in good faith will end our liability to the extent of the payment. Physical Examinations And Autops y: We have the right to have a Doctor of Our choice examine the Covered Person as often as is reasonably necessary. This section applies when a claim is pending or while benefits are being paid. We also have the right to request an autopsy AH-15090 ACE American Insurance Company 21 in the case of death, unless the law forbids it. We will pay the cost of the examination or autopsy. Legal Actions: No lawsuit or action in equity can be brought to recover on the Policy: (1) before 60 days following the date proof of loss was given to Us; or (2) after 3 years following the date proof of loss is required. Recovery of Overpayment: If benefits are overpaid or paid in error, We have the right to recover the amount overpaid or paid in error, by any or all of the following methods. 1. A request for lump sum payment of the amount overpaid or paid in error. 2. Reduction of any proceeds payable under the Policy by the amount overpaid or paid in error. 3. Taking any other action available to Us. Subrogation: We may recover any benefits paid under the Policy to the extent a Covered Person is paid for the same Injury or Sickness by a third party, another insurer, or the Covered Person’s uninsured motorists insurance. We may only be reimbursed to the amount of the Covered Person’s recovery. Further, We have the right to offset future benefits payable to the Covered Person under the Policy against such recovery. We may file a lien in a Covered Person’s action against the third party and have a lien on any recovery that the Covered Person receives whether by settlement, judgment, or otherwise, and regardless of how such funds are designated. We shall have a right to recovery of the full amount of benefits paid under the Policy for the Injury or Sickness, and that amount shall be deducted first from any recovery made by the Covered Person. We will not be responsible for the Covered Person’s attorney’s fees or other costs. Upon request the Covered Person must complete the required forms and return them to Us or Our authorized agent. The Covered Person must cooperate fully with Us or Our representative in asserting its right to recover. The Covered Person will be personally liable for reimbursement to Us to the extent of any recovery obtained by the Covered Person from any third party. If it is necessary for Us to institute legal action against the Covered Person for failure to repay Us, the Covered Person will be personally liable for all costs of collection, including reasonable attorneys’ fees. ADMINISTRATIVE PROVISIONS Premiums: The premiums for the Policy will be based on the rates currently in force, the plan and amount of insurance in effect. Changes In Premium Rates: We may change the premium rates from time to time with at least 31 days advanced written, or authorized electronic or telephonic notice. No change in rates will be made until 12 months after the Policy Effective Date. An increase in rates will not be made more often than once in a 12 month period. However, We reserve the right to change rates at any time if any of the following events take place: 1. The terms of the Policy change. 2. A division, subsidiary, affiliated organization or eligible class is added or deleted from the Policy. 3. There is a change in the market or factors bearing on the risk assumed. 4. There is a misrepresentation in the information We relied on in establishing the rate. AH-15090 ACE American Insurance Company 22 5. Any federal or state law or regulation is amended to the extent it affects Our benefit obligation. If an increase or decrease in rates takes place on a date that is not a Premium Due Date, a pro rata adjustment will apply from the date of the change to the next Premium Due Date. Payment of Premium: The first premium is due on the Policy Effective Date. If any premium is not paid when due, the Policy will be canceled as of the Premium Due Date, except as provided in the Policy Grace Period section. Policy Grace Period: A Policy Grace Period of 31 days will be granted for the payment of the required premiums. The Policy will remain in force during the Grace Period. If the required premiums are not paid during the Policy Grace Period, insurance will end on the last Premium Due Date on which required premiums were paid. The Policyholder will be liable to Us for any unpaid premium for the time the Policy was in force. GENERAL PROVISIONS Entire Con tract; Chan ges: The Policy (including any endorsements or amendments), the signed application of the Policyholder and any individual applications of Covered Persons, are the entire contract. Any statements made by the Policyholder or Covered Persons will be treated as representations and not warranties. No such statement shall void the insurance, reduce the benefits, or be used in defense of a claim for loss incurred unless it is contained in a written application. To be valid, any change or waiver must be in writing (or authorized electronic or telephonic communications). It must be signed by our President or Secretary and be attached to the Policy. No agent has authority to change or waive any part of the Policy. Policy Effective Date And Termination Date: The Policy begins on the Policy Effective Date shown on page 1 of the Policy. We may terminate this Policy by giving 31 days advance notice in writing (or authorized electronic or telephonic means) to the Policyholder. The Policyholder may terminate this Policy on any Premium Due Date by giving 31 days advance written (or authorized electronic or telephonic) notice to Us. This Policy terminates automatically on the earlier of: 1) the last day of the Policy Term; or 2) the Premium Due Date if Premiums are not paid when due. Termination takes effect at 12:00 a.m. (midnight) at the Policyholder's address on the date of termination. Clerical Error: If a clerical error is made, it will not affect the insurance of any Covered Person. No error will continue the insurance of a Covered Person beyond the date it should end under the Policy terms. Reporting Requireme nts: The Policyholder or its authorized agent must report all of the following to Us by the premium due date: 1. the names of all persons insured on the Policy Effective Date; 2. the names of all persons who are insured after the Policy Effective Date; 3. the names of those persons whose insurance has terminated; 4. any additional information required by Us. AH-15090 ACE American Insurance Company 23 Examination Of Reco rds And Audit: We shall be permitted to examine and audit the Policyholder’s books and records at any time during the term of the Policy and within 2 years after the termination of the Policy as they relate to the premiums or subject matter of this insurance. Certificates Of Insurance: Where it is required by law, or upon the request of the Policyholder, We will make available certificates outlining the insurance coverage and to whom benefits are payable under the Policy. Conformity With State La ws: On the effective date of the Policy, any provision that is in conflict with the laws in the state where it is issued is amended to conform to the minimum requirements of such laws. Not In Lieu Of Workers’ Compensation: The Policy is not a Workers’ Compensation policy. It does not provide Workers’ Compensation benefits. AH-15090 ACE American Insurance Company 24 ACE American Insurance Company (A Stock Company) Philadelphia, PA 19106 IMPORTANT NOTICE Insurance policies providing certain health insurance coverage issued or renewed on or after September 23, 2010 are required to comply with all applicable requirements of the Patient Protection and Affordable Care Act (“PPACA”). However, there are a number of insurance coverages that are specifically exempt from the requirements of PPACA (See §2791 of the Public Health Services Act). ACE maintains this insurance is short-term, limited duration insurance and is not subject to PPACA. ACE continues to monitor healthcare reform laws and regulations to determine any impact on its products. In the event these laws and regulations change, your plan and rates will be modified accordingly. Please understand that this is not intended as legal advice. For legal advice on PPACA, please consult with your own legal counsel or tax advisor directly. Important Notice (Student Health Policy)
© Copyright 2026