The role of enoyl-CoA hydratase short chain 1 and
FEBS Letters 584 (2010) 3185–3192 journal homepage: www.FEBSLetters.org The role of enoyl-CoA hydratase short chain 1 and peroxiredoxin 3 in PP2-induced apoptosis in human breast cancer MCF-7 cells Xiang Liu, Renqing Feng *, Liying Du College of Life Sciences, Peking University, Beijing 100871, PR China a r t i c l e i n f o Article history: Received 12 April 2010 Revised 25 May 2010 Accepted 2 June 2010 Available online 10 June 2010 Edited by Quan Chen Keywords: Breast cancer Apoptosis 4-Amino-5-(4-chlorophenyl)-7-(tbutyl)pyrazolo[3,4-d]pyrimidine Enoyl-CoA hydratase short chain 1 Peroxiredoxin 3 a b s t r a c t We show that 4-amino-5-(4-chlorophenyl)-7-(t-butyl)pyrazolo[3,4-d]pyrimidine (PP2) induces apoptosis and down-regulates the expression of enoyl-CoA hydratase short chain 1 (ECHS1) and peroxiredoxin 3 (PRDX3) in human breast cancer MCF-7 cells. The decrease of ECHS1 and PRDX3 was validated by Western blot and quantitative real-time reverse transcription-PCR in MCF-7 and other carcinoma cells. Knockdown and over-expression of ECHS1 and/or PRDX3 further supported the key role of ECHS1 and PRDX3 in regulation of PP2-induced apoptosis. These results suggest a possible apoptotic pathway whereby down-regulation of ECHS1 and PRDX3 potentiates PP2-induced apoptosis in MCF-7 cells. Ó 2010 Federation of European Biochemical Societies. Published by Elsevier B.V. All rights reserved. 1. Introduction Breast cancer is now the most prevalent cancer in women worldwide [1]. Although endocrine therapy brings improvement to breast cancer, it inevitably results in recurrence with uncontrolled growth and metastasis [2,3]. c-Src, a non-receptor tyrosine kinase, plays key roles in mediating many functions during the progression of cancer. c-Src itself is weakly oncogenic [4], but phosphorylation of c-Src activates downstream targets, and therefore it can regulate many cellular processes. Because of its pivotal roles in many signal pathways that regulate cell growth, adhesion, migration and survival, c-Src may be characterized as a therapeutic target for cancers [5–7]. Recent interest in c-Src as a therapeutic target for cancer has led to the development of small molecule inhibitors [8,9]. Among these inhibitors, PP2 (4-amino-5-(4-chlorophenyl)-7-(t-butyl) pyrazolo[3,4-d]pyrimidine) was first identified as a pyrazolo- Abbreviations: PP2, 4-amino-5-(4-chlorophenyl)-7-(t-butyl)pyrazolo[3,4d]pyrimidine; ECHS1, enoyl-CoA hydratase short chain 1; PRDX3, peroxiredoxin 3; MMP, mitochondrial membrane potential * Corresponding author. Address: Department of Biochemistry and Molecular Biology, College of Life Sciences, Peking University, Beijing 100871, PR China. Fax: +86 10 62751526. E-mail address: [email protected] (R. Feng). pyrimidine compound that fits into the ATP binding site of cSrc and therefore is a potent and selective inhibitor of the cSrc family kinases [10]. PP2 has been reported to induce apoptosis in murine B cell leukemia [11]. PP2 has also been reported to potentiate the apoptosis in human neuroblastoma cells [12]. Although many characters of PP2-induced apoptosis have been described, the molecular mechanism remains unknown. In addition, PP2 has not been studied for its effect on mitochondrial protein expression in breast cancer cells. In the present study, we observed that PP2 induced apoptosis in MCF-7 cells with a concomitant decrease of mitochondrial membrane potential (MMP) and an alteration of Bcl-2 family proteins, suggesting the possible mitochondria-mediated apoptotic pathway. Using two-dimensional electrophoresis and mass spectrometry, we identified two significantly down-regulated mitochondrial proteins, enoyl-CoA hydratase short chain 1 (ECHS1) and peroxiredoxin 3 (PRDX3) after c-Src suppression by PP2. RT-PCR and Western blot analysis demonstrated the down-regulation of ECHS1 and PRDX3 at the transcription and protein levels in MCF-7 and other carcinoma cells. In addition, we provide evidence that ECHS1 and PRDX3 may play a key role in PP2-induced apoptosis by using knockdown and over-expression strategy. These findings provide important insights into c-Src suppression by PP2. Thus, for the first time ECHS1 and PRDX3 are shown to be down-regulated after c-Src suppression. 0014-5793/$36.00 Ó 2010 Federation of European Biochemical Societies. Published by Elsevier B.V. All rights reserved. doi:10.1016/j.febslet.2010.06.002 3186 X. Liu et al. / FEBS Letters 584 (2010) 3185–3192 2. Materials and methods 2.1. Cell culture All cell lines used in this work were obtained from American Type Culture Collection (Manassas, VA). Cells were seeded at an initial concentration of 105 cells/ml in DMEM (Invitrogen, Carlsbad, CA) supplemented with 10% fetal bovine serum (FBS, Hyclone, Pittsburgh, PA), 3.75 g/L sodium bicarbonate, 100 U/mL penicillin and 100 lg/mL streptomycin. Cells were cultured at 37 °C in a humidified incubator containing 5% CO2. 2.2. Cell growth assay MCF-7 cells were seeded in 96-well plates (Costar, Corning, NY) with complete culture medium (DMEM containing 10% FBS) and grown for 24 h. Cells were then cultured with different concentrations of PP2 (Merck, Whitehouse Station, NJ) or without PP2 for 48 h. At the end of the treatment period, 20 lL 3-(4,5)-dimethylthiahiazo (zy1)-3,5-di-phenytetrazoliumromide (MTT, Amresco, Solon, OH) was added to each well and cells were incubated at 37 °C for 3 h. The reacting product formazan crystals were dissolved in 200 lL DMSO (Sigma, St. Louis, MO) after removing the supernatant. After shaking plates for 15 min, the optical density of the wells was measured at the wavelength of 570 nm with Microplate Reader (Bio-Rad, Hercules, CA). Each concentration of PP2 was performed in three wells and cell growth assay was repeated for three times. at an accelerating voltage of 20 kV using CHCA as the matrix. The spectra were internally calibrated using trypsin autolysis products. All PMFs obtained were used to search the NCBI database using the MASCOT search engine (http://www.matrixscience.com/) with a tolerance of ±100 ppm and one missed cleavage site. 2.5. Western blot analysis Twenty micrograms of cell lysates of each sample was separated by 12.5% SDS–PAGE. Proteins were transferred onto PVDF membrane (Millipore) and incubated with primary antibodies at optimal dilution at 4 °C overnight, followed by incubating with secondary antibody (HRP-conjugated goat anti-mouse IgG was used, Jackson ImmunoResearch, West Grove, PA) at 37 °C for 1 h. The immunoblot was visualized with Enhanced Western Luminescent Detection Kit (Vigorous, Beijing, China). All Western blots were performed at least three times for each experiment. The relative amount of immunoblot band was measured by densitometry using Imagemaster 2D Software. Monoclonal antibodies to peroxiredoxin 3, Bcl-2 and Bax were obtained from Santa Cruz Biotechnology (Santa Cruz, CA). Monoclonal antibody to glyceraldehyde-3-phosphate dehydrogenase (GAPDH) was obtained from Proteintech Group (Chicago, IL). Monoclonal antibody to enoyl-CoA hydratase short chain 1 was a generous gift from Dr. Jian’en Gao (Beijing Proteome Research Center, China). 2.6. Quantitative real-time reverse transcription-PCR (qRT-PCR) analysis 2.3. Protein extraction for two-dimensional gel electrophoresis (2-DE) MCF-7 cells were cultured for 30 h in DMEM containing 0.2% FBS for the synchronization of cell cycle, which was also evaluated by FACS analysis. Cells were collected before PP2 treatment or after 10 lM PP2 treatment for 12 h, 24 h and 30 h. Cells were washed three times with washing buffer (0.25 M sorbitol, 0.01 M Tris, pH 7.5) and centrifuged at 500g for 10 min at 4 °C. The cell pellet was resuspended in lysis buffer (8 M urea, 2 M thiourea, 4% CHAPS, 40 mM DTT, containing protease inhibitor cocktail, Roche, Mannheim, Germany). Total cell lysates were centrifuged at 16 000g for 1 h at 4 °C. The supernatant was collected and purified with 2-D Clean-Up Kit (Amersham Pharmacia Biotech, Piscataway, NJ). Protein concentration was determined by 2-D Quant Kit (Amersham Pharmacia Biotech). 2.4. 2-DE and mass spectrometry analysis 2-DE was carried out according to the protocol described before [13,14]. Briefly, protein samples (70 lg for analytical gel, 1 mg for preparative gel) were loaded on 24 cm Immobiline 4–7 linear DryStrips (Amersham Pharmacia Biotech) and IEF was run at 30 V for 8 h, 50 V for 4 h, 100 V for 1 h, 300 V for 1 h, 500 V for 1 h, 1000 V for 1 h, and 8000 V for 12 h. Then second dimensional SDS–PAGE was carried out in the Ettan Dalt Six Elect Unit 230 (Amersham Pharmacia Biotech) at 2 W/gel for 45 min and then 15 W/gel until the dye front reached the bottom of the gel. The analytical gels for quantification were silver stained and the preparative gels were stained with PhastGel Blue R (CBB R350, Amersham Pharmacia Biotech). Spot detection, quantification and analysis were performed using Imagemaster 2D Software (version 4.01, Amersham Pharmacia Biotech). The ‘‘Total Spot Volume Normalization” method was used in order to correct the differences in sample loading or stain intensity among gels. Spots of interest were excised from 2-D gels that were stained with CBB R350 and followed by in gel digestion. All mass spectra from MALDI-TOF MS were obtained on an Ultraflex TOF/TOF (Bruker Daltonics, Bremen, Germany) in positive ion mode Total RNA was extracted by TRIzol reagent (Invitrogen) according to the suggested protocol. RNA (5 lg) was used to synthesize the first-strand cDNA with the Superscript first-strand synthesis system (Invitrogen) for RT-PCR according to the manufacturer’s recommendation. Gene-specific primers for RT- and qRT-PCR analyses were synthesized commercially at AuGCT Biotechnology (Beijing, China) as follows, ECHS1: 50 -CGCTGCTGTCAATGGCTATG-30 (forward) and 50 -CTTGGCGTCCTGGGCTGAGA-30 (reverse); PRDX3: 50 -GCCGTTGTCAATGGAGAGTTC-30 (forward) and 50 - GCAAGATGGCTAAAGTGGGAA-30 (reverse). Human GAPDH gene was used as internal control (forward primer, 50 -GGGAGCCAAAAGGGTCATCATC-30 ; reverse primer, 50 -CCATGCCAGTGAGCTTCCCGTTC-30 ). The qRT-PCR was performed using the SYBR Green qPCR Kits (NEB, Ipswich, MA) and a DNA Engine Opticon continuous fluorescence detection system (Bio-Rad) according to the manufacturer’s instruction. All results were obtained from at least three independent experiments using different RNA samples. 2.7. Analysis of apoptosis by flow cytometry After different treatment, apoptotic cells were detected by staining with FITC-conjugated Annexin V and propidium iodide (PI) using a commercially available apoptosis detection kit (Biosea, Beijing, China). Briefly, 2 105 cells were collected, washed three times with PBS and resuspended in binding buffer. After incubation for 15 min with FITC-conjugated Annexin V and PI according to the manufacturer’s instructions, apoptotic cells were analyzed by FACS Calibur flow cytometer. The Summit software (version 4.0, DakoCytomation, CO) was used to determine the number of apoptotic cells. 2.8. Measurement of mitochondrial membrane potential (MMP) Mitochondrial membrane potential was measured using fluorescent probe tetramethylrhodamine, methyl ester, perchlorate (TMRM, Invitrogen). After different treatment, 20 nM TMRM was X. Liu et al. / FEBS Letters 584 (2010) 3185–3192 added to the external solution and cells were incubated for 20 min in darkness at 37 °C. Fluorescent signals were detected by a confocal microscopy at the wavelength of Ex540 nm/Em595 nm. The fluorescent intensity was determined using a FACSCalibur flow cytometer. Totally, 10 000 cells per sample were analyzed in the gate region used for calculation. 2.9. Small interfering RNA (siRNA) Small interfering RNAs were synthesized by Genepharma Company (Shanghai, China). The target sequences for ECHS1 siRNAs were: 50 -AACCATGATGTGTGATATCAT-30 (508–528 bp, clone #2) and 50 -AAGAAGTAAGTTGGAGAAGAA-30 (835–855 bp, clone #3) and for PRDX3 siRNAs were: 50 -AAGGTTCTGGTCTTGCACTAA-30 (521–541 bp, clone #2) and 50 -AAGGCGTTCCAGTATGTAGAA-30 (649–669 bp, clone #3). Scramble siRNA duplexes were used as a negative control (NC). Cells were transfected with 100 nM target siRNAs or control siRNA using Lipofectamine 2000 Reagent (Invitrogen) according to the instructions of the manufacturers, and transfection was carried out for 5 h. After that, culture medium was replaced with complete DMEM supplemented with 10% FBS. Cells were collected after transfection for 48 h and silencing effects were evaluated by Western blot analysis. 3187 2.10. Plasmid constructs and transfection cDNAs of human PRDX3 and ECHS1 were obtained using RT-PCR with RNA extraction from MCF-7 cells (for PRDX3, Forward primer: 50 -CGGGATCCCGATGGCGGCTGCTGTAGGA-30 , Reverse primer: 50 CCGAATTCCTACTGATTTACCTTCTGAAAGTAC-30 ; for ECHS1, Forward primer: 50 -CGGGATCCCGATGGCCGCCCTGCGTGTC-30 , Reverse primer: 50 -CCGAATTCTCACTGGTCTTTGAAGTTGGC-30 ). Full length of ECHS1 or PRDX3 was cloned into pcDNA3.1/myc-His A mammalian expression vector (Invitrogen) using BamHI and EcoRI sites. Correct integrity of both genes was confirmed by restriction digests and sequencing. MCF-7 cells were transfected by 2 lg pcDNA3.1PRDX3 vector, pcDNA3.1-ECHS1 vector or with empty vector using Lipofectamine 2000 Reagent (Invitrogen), and transfection was carried out for 5 h. After that, culture medium was replaced with complete DMEM supplemented with 10% FBS. Cells were collected after transfection for 48 h and over-expression of both proteins was evaluated by Western blot analysis. 2.11. Statistical analysis Statistic significance of differences in each condition was estimated using One Way ANOVA with SigmaStat software (Version Fig. 1. PP2 inhibited cell proliferation, induced apoptosis with a decrease of mitochondrial membrane potential and an alteration of Bcl-2 family proteins in MCF-7 cells. (A) PP2 caused a dose-dependent inhibition on the proliferation of MCF-7 cells. Cells were treated with different concentrations of PP2 for 48 h. Relative cell number (y-axis) was shown as percentage of control (with the same concentration of DMSO) after treatment with indicated concentrations of PP2. (B) PP2 caused a time-dependent inhibition on proliferation of MCF-7 cells. Cells were treated with 10 lM PP2 for indicated times. (C) The apoptosis was observed after 10 lM PP2 treatment for 12 h, 24 h and 30 h. Cells were stained with Annexin V-FITC/PI and the apoptosis was analyzed by flow cytometry. (D) The percentage of apoptotic cells was determined by counting the number of cells only with Annexin V-FITC-positive and normalizing to the number of total cells. (E) Mitochondrial membrane potential of MCF-7 cells after 10 lM PP2 treatment was measured by TMRM staining. Fluorescent signal was detected by confocal microscopy (left lane). The fluorescent intensity was measured by flow cytometric analysis and the numbers gated in each phase areas are the mean of three independent experiments (right lane). Bar scale, 30 lm. (F) PP2 induced the decrease of Bcl-2 and increase of Bax in MCF-7 cells. Cells were collected before PP2 treatment or after 10 lM PP2 treatment for 12 h, 24 h and 30 h. Total protein lysates (20 lg) were separated by SDS–PAGE followed by Western blot analysis using antibodies specific to Bcl-2, Bax and GAPDH (as internal control). 3188 X. Liu et al. / FEBS Letters 584 (2010) 3185–3192 3.5, Germany). Differences were considered to be significant when P < 0.05. In all experiments, * indicates P < 0.05. 3. Results 3.1. PP2 inhibited cell proliferation in MCF-7 cells We first examined the c-Src inhibitor PP2 for its effect on cell growth to determine the suitable concentration of PP2. As shown in Fig. 1A, PP2 caused a dose-dependent inhibition on the proliferation of MCF-7 cells. As the PP2 concentration increased from 1 lM to 50 lM, the number of living cells decreased dramatically according to cell growth assay (Fig. 1A). In general, 25.8 lM PP2 induced about 50% growth inhibition of MCF-7 cells, which was in accordance with a previous study [15]. Thus, MCF-7 cells were cultured in DMEM with 10 lM PP2 in the subsequent experiments. Fig. 1B shows 10 lM PP2 inhibited cell proliferation in a timedependent manner. The phosphorylation of c-Src was greatly inhibited by 10 lM PP2 while the total level of c-Src was not changed (our unpublished data). 3.2. PP2 induced apoptosis with a decrease of MMP and alteration of Bcl-2 family proteins in MCF-7 cells As shown in Fig. 1C and D, PP2 treatment for 30 h induced about 30% apoptosis in MCF-7 cells. We then conducted experiments to Fig. 1 (continued) X. Liu et al. / FEBS Letters 584 (2010) 3185–3192 measure MMP in MCF-7 cells treated with PP2. Using TMRM as the marker of mitochondrial membrane integrity, confocal microscopy images revealed evident depolarization of mitochondrial membrane due to the decrease in fluorescent intensity and the blurring of mitochondrial morphology (Fig. 1E). FACS quantification showed a 21% decrease in fluorescent intensity after PP2 treatment for 30 h. Because the mitochondria-mediated apoptotic pathway is regulated by Bcl-2 family proteins [16,17], we next examine the expression of Bcl-2 (anti-apoptotic protein) and Bax (pro-apoptotic protein) after PP2 treatment. Western blot analysis showed that Bcl-2 was suppressed rapidly after PP2 treatment for 12 h, whereas Bax was up-regulated (Fig. 1F). 3.3. PP2 down-regulated ECHS1 and PRDX3 at the protein and transcription levels in MCF-7 and other carcinoma cells To investigate changes of protein expression in the entire cell cycle, MCF-7 cells were cultured in the presence of 10 lM PP2 3189 for 12 h, 24 h and 30 h. Total proteins were extracted at each time point and separated by IEF followed by SDS–PAGE. Of the identified proteins that expressed differentially after PP2 treatment, ECHS1 and PRDX3 are considered interesting because they play important roles in fatty acid metabolism and redox balance of mitochondria (Fig. 2A). Because both 2-DE (Fig. 2A) and Western blot (Fig. 2B) validated the decrease of ECHS1 and PRDX3, we next examined the effect of PP2 on the transcription of these two genes. The qRT-PCR results indicated that ECHS1 mRNA decreased to 58.2% while PRDX3 mRNA decreased to 38.6% (Fig. 2C) after PP2 treatment for 30 h compared to the control sample (100%). The decreased protein and transcription levels of ECHS1 and PRDX3 were also validated in other carcinoma cells (Supplementary Fig. 1). 3.4. Knockdown of ECHS1 and PRDX3 by RNAi increased apoptosis induced by PP2 in MCF-7 cells To confirm the role of ECHS1 and/or PRDX3 in PP2-induced apoptosis, we used the siRNA strategy to deplete ECHS1 and/or PRDX3. Western blot analysis demonstrated that ECHS1 and PRDX3 were significantly suppressed in two siRNA clones and in a double knockdown clone (Fig. 3A). But there was no difference between parental cells and mock cells transfected with scramble siRNA. Depletion of ECHS1 and/or PRDX3 with concomitant PP2 treatment led to significant increase in the number of apoptotic cells. Treatment of MCF-7 cells with 10 lM PP2 for 12 h increased the number of apoptotic cells from 15.57 ± 1.31% in negative control Fig. 2. PP2 induced Down-regulation of ECHS1 and PRDX3 in MCF-7 cells. (A) Decreased protein expression of ECHS1 and PRDX3 on 2D gels. The gel images of protein spot were displayed on top of the graph as representative of three independent experiments. Relative protein abundance (y-axis) was determined by ImageMaster 2D software using the ‘‘Total Spot Volume Normalization” method to correct the differences in sample loading or stain intensity among gels. Column, the mean of three independent experiments; bars, S.D. *P < 0.05. (B) Western blot analysis of ECHS1 and PRDX3 after 10 lM PP2 treatment for the indicated times. MCF-7 cells were collected before PP2 treatment or after 10 lM PP2 treatment for indicated times. Total protein lysates (20 lg) were separated by SDS–PAGE followed by Western blot analysis using antibodies specific to ECHS1, PRDX3 and GAPDH (as internal control). The relative amounts of ECHS1 and PRDX3 were measured by densitometry. Data were calculated as the mean optical density of treated samples as a percent of untreated cells normalized against GAPDH. (C) qRTPCR analysis of ECHS1 and PRDX3 after 10 lM PP2 treatment for the indicated times. Relative transcription level (y-axis) was determined according to the manufacturer’s instruction with control as calibrator (1-fold). Column, the mean of three independent experiments; bars, S.D. *P < 0.05. Fig. 3. Knockdown of ECHS1 and PRDX3 potentiated PP2-induced apoptosis. (A) Depletion of ECHS1 and PRDX3 in MCF-7 cells. Western blot analysis indicated that ECHS1 and PRDX3 were suppressed in two separated siRNA clones and a double knockdown clones compared to that of parental cells (no treatment) or mock cells (negative control siRNA, NC). (B) Knockdown of ECHS1 and PRDX3 increased PP2induced apoptosis. After 36 h transfection with 100 nM siRNAs or scramble siRNAs (NC, negative control), MCF-7 cells were treated with 10 lM PP2 for additional 12 h. Apoptosis was measured by flow cytometry after staining with Annexin V-FITC/PI. Data represent the percentage of apoptotic cells relative to the total cells. (C) Knockdown of ECHS1 and PRDX3 induced the decrease of mitochondrial membrane potential compared to the NC in MCF-7 cells when exposure to 10 lM PP2 for 12 h. (D) Knockdown of ECHS1 and PRDX3 induced the alteration of Bcl-2 and Bax in MCF-7 cells in the presence of PP2. 3190 X. Liu et al. / FEBS Letters 584 (2010) 3185–3192 cells to about 23.75 ± 2.21% in cells with depletion of ECHS1 and/or PRDX3 (Fig. 3B and Supplementary Fig. 2). The addition of PP2 further increased the dissipation of MMP in siRNA-ECHS1 and/or siRNA-PRDX3-transfected cells compared to cells transfected with scramble siRNAs (Fig. 3C). Knockdown of ECHS1 and/or PRDX3 induced the decrease of Bcl-2 after PP2 treatment. But knockdown of ECHS1 and/or PRDX3 had less effect on Bax expression in MCF-7 cells when exposure to PP2 (Fig. 3D). 3.5. Over-expression of PRDX3 inhibited PP2-induced apoptosis in MCF-7 cells Next, we transiently transfected MCF-7 cells with expression vectors pcDNA3.1-ECHS1 or pcDNA3.1-PRDX3. Western blot analysis demonstrated the over-expression of ECHS1 and/or PRDX3 (Fig. 4A). Over-expression of PRDX3 induced less reduction in the number of apoptotic cells compared to cells transfected with empty vector in the presence of PP2. The reduction in apoptotic levels was more evident in the cells over-expressing both PRDX3 and ECHS1, whereas no significant difference in cells over-expressing ECHS1 (Fig. 4B and Supplementary Fig. 3). Furthermore, less reduction of MMP was observed after over-expression of PRDX3 compared to cells transfected with empty vector when exposure to PP2 (Fig. 4C). Over-expression of ECHS1 and/or PRDX3 induced the decrease of Bax in the presence of PP2. Over-expression of ECHS1 had less effect on Bcl-2 expression, whereas PRDX3 overexpression induced the increase of Bcl-2 after PP2 treatment Fig. 4. Over-expression of PRDX3 attenuated PP2-induced apoptosis in MCF-7 cells. (A) Over-expression of ECHS1 and/or PRDX3 in MCF-7 cells. Western blot analysis demonstrated the over-expression of ECHS1 and/or PRDX3 compared to cells transfected with empty vector (OX: over-expression). (B) Over-expression of PRDX3 attenuated PP2-induced apoptosis. After 36 h transfection, MCF-7 cells were treated with 10 lM PP2 for additional 12 h. Apoptosis was measured by flow cytometry after staining with Annexin V-FITC/PI. Data represent the percentage of apoptotic cells relative to the total cells. (C) Over-expression of PRDX3 in MCF-7 cells led to less reduction of MMP compared to cells transfected with empty vector when exposure to 10 lM PP2 for 12 h. (D) Over-expression of ECHS1 and/or PRDX3 induced alteration of Bcl-2 family proteins in MCF-7 cells in the presence of PP2. (Fig. 4D). These results suggest that PRDX3 over-expression may alleviate PP2-induced apoptosis, whereas over-expression of ECHS1 itself has no such effect. 4. Discussion In this study, we have investigated PP2-induced apoptosis in human breast cancer MCF-7 cells. The decrease of MMP and alteration of Bcl-2 family proteins suggest the possible mitochondriamediated apoptotic pathway after PP2 treatment. Using a proteomic approach, we identified thirteen differentially expressed proteins (Supplementary Fig. 4 and Supplementary Table 1). The small number of differences is likely due to the low sensitivity of the method in which differential 2-D gel spots are identified by mass spectrometry. Because of their low expression level or low molecular weight, five protein spots were not identified. We then focused on two mitochondrial proteins that are involved in fatty acid metabolism and redox balance. Protein spot 1 with a decrease of 2.07-fold after PP2 treatment for 30 h was identified as ECHS1 (Fig. 2A). ECHS1 is a key enzyme that catalyzes the second step in the physiologically important boxidation pathway of fatty acid metabolism. This enzyme is located in the matrix of mitochondria and catalyzes the hydration of a,b-unsaturated enoyl-CoA thioesters to the corresponding bhydroxybutyryl-CoA thioesters [18,19]. It is reported that ECHS1 is expressed 1.89 times higher in breast cancer tissue than in normal tissue [20]. The decrease of ECHS1 may cause a reduction of boxidation of fatty acid. Protein spot 11 with a decrease of 2.73-fold after PP2 treatment for 30 h was identified as PRDX3 (Fig. 2A). There are six known isoforms of PRDX family in mammalian cells, and all of them play important roles in the removal of harmful reactive oxygen species (ROS) [21]. PRDX3 is located in the matrix of mitochondria and is therefore a mitochondria-specific ROS-scavenging protein. PRDX3 is found to be over-expressed in some human cancers, which might protect growing tumor cells against apoptosis [22,23]. It is reported that PRDX3 is expressed 15.86 times higher in breast cancer tissue than in normal tissue [20]. The decrease of PRDX3 may weaken the capability of mitochondria to neutralize the production of harmful ROS derived from physiological reaction. Because the continuous accumulation of oxidative stress and depolarization of mitochondrial membrane is a part of the mitochondria-mediated apoptotic pathway [24], the downregulation of ECHS1 and PRDX3 may functionally impair the integrity of the mitochondria and subsequently activate and initiate apoptosis. Depletion of ECHS1 and/or PRDX3 by siRNAs in MCF-7 cells potentiated the early apoptosis when exposure to PP2 for 12 h. The over-expression of PRDX3 alleviated the responsiveness of MCF-7 cells to PP2 treatment, which confirmed the involvement of PRDX3 during PP2-induced apoptosis. It was reported that over-expression of PRDX3 in mouse thymoma cells protected cells against H2O2-induced apoptosis [21]. On the other hand, PP2-induced apoptosis was not significantly inhibited in cells overexpressing ECHS1 in our experiments. The Bcl-2 family proteins have been reported to play key roles in determining whether cells will undergo apoptosis [25]. It has been reported that the ratio of Bax and Bcl-2, rather than Bcl-2 alone, is important for the survival of drug-induced apoptosis in cancer cells [26]. Moreover, Bax translocation into mitochondria may target the mitochondrial intermembrane contact sites and release cytochrome c, resulting in the sequence of apoptotic processes [27,28]. It has been shown that Akt inhibits a conformational change in Bax protein and prevents its translocation into mitochondria, thus inhibiting the disruption of mitochondrial inner membrane potential and apoptosis [29,30]. The inactivation of Akt will facilitate the translocation of Bax from X. Liu et al. / FEBS Letters 584 (2010) 3185–3192 cytosol to mitochondria [30]. c-Src has been shown to be involved in the activation of Akt [5]. It is reported that Akt activity is inhibited by PP2 in preadipocytes and lung cancer cells [31,32]. Besides, the intracellular ROS may also induce Bax conformational change and its subsequent translocation to mitochondria [33,34]. In the present study, depletion of PRDX3 with concomitant PP2 treatment led to significant increase in the intracellular ROS levels. Treatment of MCF-7 cells with 10 lM PP2 for 12 h increased the ROS levels from 56.88 ± 4.61% in negative control cells to about 72.12 ± 4.57% in cells with depletion of PRDX3 (Supplementary Fig. 5A and B). Furthermore, the decrease in ROS levels was observed after over-expression of PRDX3 compared to cells transfected with empty vector when exposure to PP2 (Supplementary Fig. 5C and D). Cell fractionation results indicated that Bax was decreased in the cytosolic fractions and increased in the mitochondrial fractions after PRDX3 silencing by siRNA (Supplementary Fig. 6). These results suggest that intracellular ROS levels may be upstream factor for Bax activation. Further study may be required to investigate the details of how ROS regulate Bax activation. Down-regulation of ECHS1 and PRDX3 after PP2 treatment was confirmed in MCF-7 cells by Western blot and qRT-PCR. The discrepancy between 2-DE and Western blot analysis (especially between samples with PP2 treatment for 12 h) may be due to the application of different experimental methods. Western blot may be more sensitive and reliable because of the specificity of antibody. 2-DE may be a useful tool for preliminary separation and identification for differentially expressed proteins. But 2-DE is influenced by many factors, such as loading efficiency of protein sample, sensitivity of silver staining. Despite the existing discrepancy, both ECHS1 and PRDX3 were significantly decreased after PP2 treatment for 30 h in 2-DE and Western blot analysis. There could be several reasons for the discrepancy between RNA and protein levels. One possibility is that translation and transcription of ECHS1 or PRDX3 may be differently regulated after c-Src suppression by PP2. The discrepancy may also be associated with posttranscriptional regulation or half-life period. But RNA and protein levels of ECHS1 or PRDX3 were consistently decreased after PP2 treatment for 30 h. Further study may be required to investigate the details of regulational mechanism that lead to the down-regulation of ECHS1 and PRDX3 after PP2 treatment. However, we have found that ECHS1 and PRDX3 were not only down-regulated in MCF-7 cells but also in other carcinoma cells, such as MDA-MB231 (breast adenocarcinoma cell line), T-47D (breast ductal carcinoma cell line), HepG2 (hepatocellular carcinoma cell line), DU 145 (prostate carcinoma cell line), HCT-8 (colon adenocarcinoma cell line) and SKOV-3 (ovarian adenocarcinoma cell line). Therefore, down-regulation of ECHS1 and PRDX3 may be a common response to PP2 treatment in different carcinoma cells. In conclusion, our study demonstrated that PP2 induced apoptosis through the mitochondria-mediated pathway and down-regulated the expression of ECHS1 and PRDX3. Change of ECHS1 and PRDX3 may be a direct response for carcinoma cells when face to PP2 or other pro-apoptotic stimuli. Acknowledgments We thank Professor Jeang Kuan-Teh (NIH/NIAID) for revision of our manuscript. We thank Professor Yuxian Zhu and Zhenquan Guo (College of Life Sciences, Peking University) for guidance in accomplishing this work. We thank Dr. Jian’en Gao (Beijing Proteome Research Center, China) for the generous gift of anti-enoylCoA hydratase short chain 1 monoclonal antibody. This work was supported by the National Natural Science Foundation of China (No. 30571711) and Beijing Natural Science Foundation (No. 5092012) to Renqing Feng. 3191 Appendix A. Supplementary data Supplementary data associated with this article can be found, in the online version, at doi:10.1016/j.febslet.2010.06.002. References [1] Parkin, D.M., Bray, F., Ferlay, J. and Pisani, P. (2005) Global cancer statistics, 2002. CA Cancer J. Clin. 55, 74–108. [2] Clarke, R., Skaar, T.C., Bouker, K.B., Davis, N., Lee, Y.R., Welch, J.N. and Leonessa, F. (2001) Molecular and pharmacological aspects of antiestrogen resistance. J. Steroid Biochem. Mol. Biol. 76, 71–84. [3] Clarke, R. et al. (2003) Antiestrogen resistance in breast cancer and the role of estrogen receptor signaling. Oncogene 22, 7316–7339. [4] Alvarez, R.H., Kantarjian, H.M. and Cortes, J.E. (2006) The role of Src in solid and hematologic malignancies: development of new-generation Src inhibitors. Cancer 107, 1918–1929. [5] Summy, J.M. and Gallick, G.E. (2006) Treatment for advanced tumors: SRC reclaims center stage. Clin. Cancer Res. 12, 1398–1401. [6] Giaccone, G. and Zucali, P.A. (2008) Src as a potential therapeutic target in non-small-cell lung cancer. Ann. Oncol. 19, 1219–1223. [7] Rucci, N., Susa, M. and Teti, A. (2008) Inhibition of protein kinase c-Src as a therapeutic approach for cancer and bone metastases. Anticancer Agents Med. Chem. 8, 342–349. [8] Golas, J.M. et al. (2003) SKI-606, a 4-anilino-3-quinolinecarbonitrile dual inhibitor of Src and Abl kinases, is a potent antiproliferative agent against chronic myelogenous leukemia cells in culture and causes regression of K562 xenografts in nude mice. Cancer Res. 63, 375–381. [9] Lee, D. and Gautschi, O. (2006) Clinical development of SRC tyrosine kinase inhibitors in lung cancer. Clin. Lung Cancer 7, 381–384. [10] Hanke, J.H., Gardner, J.P., Dow, R.L., Changelian, P.S., Brissette, W.H., Weringer, E.J., Pollok, B.A. and Connelly, P.A. (1996) Discovery of a novel, potent, and Src family-selective tyrosine kinase inhibitor. Study of Lck- and FynT-dependent T cell activation. J. Biol. Chem. 271, 695–701. [11] Lee, M., Kim, J.Y. and Koh, W.S. (2004) Apoptotic effect of PP2 a Src tyrosine kinase inhibitor, in murine B cell leukemia. J. Cell. Biochem. 93, 629–638. [12] Beierle, E.A., Ma, X., Trujillo, A., Kurenova, E.V., Cance, W.G. and Golubovskaya, V.M. (2000) Inhibition of focal adhesion kinase and src increases detachment and apoptosis in human neuroblastoma cell lines. Mol. Carcinog. 49, 224–234. [13] Wang, B.C., Wang, H.X., Feng, J.X., Meng, D.Z., Qu, L.J. and Zhu, Y.X. (2006) Posttranslational modifications, but not transcriptional regulation, of major chloroplast RNA-binding proteins are related to Arabidopsis seedling development. Proteomics 6, 2555–2563. [14] Shevchenko, A., Wilm, M., Vorm, O. and Mann, M. (1996) Mass spectrometric sequencing of proteins silver-stained polyacrylamide gels. Anal. Chem. 68, 850–858. [15] Nam, J.S., Ino, Y., Sakamoto, M. and Hirohashi, S. (2002) Src family kinase inhibitor PP2 restores the E-cadherin/catenin cell adhesion system in human cancer cells and reduces cancer metastasis. Clin. Cancer Res. 8, 2430–2436. [16] Wang, Y., He, Q.Y., Sun, R.W., Che, C.M. and Chiu, J.F. (2005) GoldIII porphyrin 1a induced apoptosis by mitochondrial death pathways related to reactive oxygen species. Cancer Res. 65, 11553–11564. [17] Zhou, J., Zhang, S., Ong, C.N. and Shen, H.M. (2006) Critical role of proapoptotic Bcl-2 family members in andrographolide-induced apoptosis in human cancer cells. Biochem. Pharmacol. 72, 132–144. [18] Jackson, S., Schaefer, J., Middleton, B. and Turnbull, D.M. (1995) Characterisation of a novel enzyme of human fatty acid beta-oxidation: a matrix-associated, mitochondrial 2-enoyl-CoA hydratase. Biochem. Biophys. Res. Commun. 214, 247–253. [19] Agnihotri, G. and Liu, H.W. (2003) Enoyl-CoA hydratase. Reaction, mechanism, and inhibition. Bioorg. Med. Chem. 11, 9–20. [20] Huang, T.C., Chang, H.Y., Hsu, C.H., Kuo, W.H., Chang, K.J. and Juan, H.F. (2008) Targeting therapy for breast carcinoma by ATP synthase inhibitor aurovertin B. J. Proteome Res. 7, 1433–1444. [21] Nonn, L., Berggren, M. and Powis, G. (2003) Increased expression of mitochondrial peroxiredoxin-3 (thioredoxin peroxidase-2) protects cancer cells against hypoxia and drug-induced hydrogen peroxide-dependent apoptosis. Mol. Cancer Res. 1, 682–689. [22] Noh, D.Y., Ahn, S.J., Lee, R.A., Kim, S.W., Park, I.A. and Chae, H.Z. (2001) Overexpression of peroxiredoxin in human breast cancer. Anticancer Res. 21, 2085–2090. [23] Kinnula, V.L., Lehtonen, S., Sormunen, R., Kaarteenaho-Wiik, R., Kang, S.W., Rhee, S.G. and Soini, Y. (2002) Overexpression of peroxiredoxins I, II, III, V, and VI in malignant mesothelioma. J. Pathol. 196, 316–323. [24] Kim, R., Emi, M. and Tanabe, K. (2005) Caspase-dependent and -independent cell death pathways after DNA damage (Review). Oncol. Rep. 14, 595–599. [25] Gross, A., McDonnell, J.M. and Korsmeyer, S.J. (1999) BCL-2 family members and the mitochondria in apoptosis. Genes Dev. 13, 1899–1911. [26] Raisova, M. et al. (2001) The Bax/Bcl-2 ratio determines the susceptibility of human melanoma cells to CD95/Fas-mediated apoptosis. J. Invest. Dermatol. 117, 333–340. [27] Gao, C.F., Ren, S., Zhang, L., Nakajima, T., Ichinose, S., Hara, T., Koike, K. and Tsuchida, N. (2001) Caspase-dependent cytosolic release of cytochrome c and 3192 [28] [29] [30] [31] X. Liu et al. / FEBS Letters 584 (2010) 3185–3192 membrane translocation of Bax in p53-induced apoptosis. Exp. Cell Res. 265, 145–151. De Giorgi, F. et al. (2002) The permeability transition pore signals apoptosis by directing Bax translocation and multimerization. FASEB J. 16, 607–609. Tsuruta, F., Masuyama, N. and Gotoh, Y. (2002) The phosphatidylinositol 3kinase (PI3K)-Akt pathway suppresses Bax translocation to mitochondria. J. Biol. Chem. 277, 14040–14047. Yamaguchi, H. and Wang, H.G. (2001) The protein kinase PKB/Akt regulates cell survival and apoptosis by inhibiting Bax conformational change. Oncogene 20, 7779–7786. Yang, S.-J., Chang, S.-C., Wen, H.-C., Chen, C.-Y., Liao, J.-F. and Chang, C.-H. (2010) Plumbagin activates ERK1/2 and Akt via superoxide, Src and PI3-kinase in 3T3-L1 Cells. Eur. J. Pharmacol. 638, 21–28. [32] Meng, X.N. et al. (2009) Characterisation of fibronectin-mediated FAK signalling pathways in lung cancer cell migration and invasion. Br. J. Cancer 101, 327–334. [33] Zheng, Y., Yamaguchi, H., Tian, C., Lee, M.W., Tang, H., Wang, H.G. and Chen, Q. (2005) Arsenic trioxide (As(2)O(3)) induces apoptosis through activation of Bax in hematopoietic cells. Oncogene 24, 3339–3347. [34] Chen, Q., Chai, Y.C., Mazumder, S., Jiang, C., Macklis, R.M., Chisolm, G.M. and Almasan, A. (2003) The late increase in intracellular free radical oxygen species during apoptosis is associated with cytochrome c release, caspase activation, and mitochondrial dysfunction. Cell Death Differ. 10, 323–334.
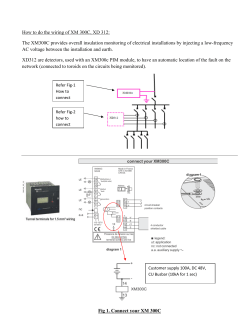
© Copyright 2026