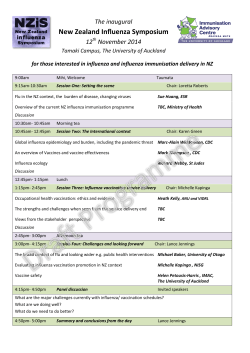
Influenza Virus Infects Bone Marrow Mesenchymal
Cell Transplantation, Vol. 22, pp. 461–468, 2013 Printed in the USA. All rights reserved. Copyright 2013 Cognizant Comm. Corp. 0963-6897/13 $90.00 + .00 DOI: http://dx.doi.org/10.3727/096368912X656063 E-ISSN 1555-3892 www.cognizantcommunication.com Influenza Virus Infects Bone Marrow Mesenchymal Stromal Cells In Vitro: Implications for Bone Marrow Transplantation Mahesh Khatri and Yehia M. Saif Food Animal Health Research Program, Ohio Agricultural Research and Development Center, The Ohio State University, Wooster, OH, USA Mesenchymal stromal cells (MSCs) have differentiation, immunomodulatory, and self-renewal properties and are, therefore, an attractive tool for regenerative medicine and autoimmune diseases. MSCs may be of great value to treat graft-versus-host disease. Influenza virus causes highly contagious seasonal infection and occasional pandemics. The infection is severe in children, elderly, and immunocompromised hosts including hematopoietic stem cell transplant patients. The objective of this study was to determine if MSCs are permissive to influenza virus replication. We isolated MSCs from the bone marrow of 4- to 6-week-old germ-free pigs. Swine and human influenza virus strains were used to infect MSCs in vitro. MSCs expressed known influenza virus a-2,3 and a-2,6 sialic acid receptors and supported replication of swine and human influenza viruses. Viral infection of MSCs resulted in cell lysis and proinflammatory cytokine production. These findings demonstrate that bone marrow-derived MSCs are susceptible to influenza virus. The data also suggest that transplantation of bone marrow MSCs from influenza virus-infected donors may transmit infection to recipients. Also, MSCs may get infected if infused into a patient with an ongoing influenza virus infection. Key words: Mesenchymal stromal cells (MSCs); Influenza virus; Cell therapy INTRODUCTION Mesenchymal stromal cells (MSCs) were first identi fied by Friendstein in bone marrow as precursors for fibroblasts or stromal cells. MSCs have the potential to differentiate into cells of mesenchymal, mesodermal, neuroectodermal, or endodermal lineage (16). MSCs constitute a small population (approximately 0.001–0.01% nucleated cells) of adult human bone marrow cells. MSCs support and regulate hematopoiesis via the secretion of cytokines and growth factors (14,29). Several studies using a variety of animal models have shown the beneficial effects of MSCs in conditions such as infarcted myocardium, lung injury, damaged bone, tendon, and cartilage (1,31,33,36). Bone marrow-derived and tissue resident MSCs isolated from humans as well as from other mammalian species are strongly immunosuppressive and inhibit inflammation and immunological responses both in vitro and in vivo (15). The mechanisms of MSC-mediated immunosuppression are not completely understood; however, MSCs have been shown to secrete several immunosuppressive mediators including interleukin-10 (IL-10), transforming growth factor-b (TGF-b), prostaglandin E2, nitric oxide (NO), indoleamine 2,3-dioxygenase (IDO), and hepatocyte growth factor (HGF) and promote generation of regulatory T-cells (37). MSCs improve the outcome of allogeneic transplantation by promoting hematopoietic engraftment (22) and also reduce graft-versus-host disease (25,26) autoimmunity and other immune disorders (37). Due to their differentiation and immunoregulatory properties, pluripotent stem cells are an attractive tool for tissue engineering and regenerative medicine. Influenza viruses cause a highly contagious respiratory infection in humans and animals. These viruses cause seasonal epidemics and infrequent pandemics in humans with young children, elderly, and immunocompromised individuals at high risk. In hematopoietic stem cell transplantation recipients, influenza virus caused persistent infection and severe respiratory failure (2,5,9,11). During the last century, influenza viruses caused three human pandemics. The 2009 human pandemic was caused by a novel H1N1 virus of swine origin (13). Influenza virus mainly replicates in the respiratory tract; however, virus replication has been detected in nonpulmonary tissues including the bone marrow (43,49). Moreover, highly pathogenic avian influenza (HPAI) H5N1 virus, which has Received October 17, 2011; final acceptance April 7, 2012. Online prepub date: September 21, 2012. Address correspondence to Dr. Mahesh Khatri, Food Animal Health Research Program, Ohio Agricultural Research and Development Center, The Ohio State University, 1680 Madison Avenue, Wooster, OH 44691, USA. Tel: +1-330-263-3751; Fax: +1-330-263-3677; E-mail: [email protected] 461 462 crossed the species barrier and can infect humans without prior adaptation, replicates extensively in the lungs and extra-pulmonary tissues leading to acute respiratory distress syndrome, multiple-organ dysfunction, lympho penia, and hemophagocytosis (6,40,47). In the bone marrow, influenza virus caused the apoptosis of primitive B-cells by inducing the production of proinflammatory cytokines, mainly tumor necrosis factor-a (TNF-a) (39). However, the phenotype of cell(s) permissive to influenza virus and the cellular source of cytotoxic cytokines in virus-infected bone marrow are not known. Swine is an excellent animal model to study the pathogenesis of influenza virus because the clinical manifestations and pathogenesis of influenza in pigs closely resemble that observed in humans (23). In the present study, we investigated whether MSCs are susceptible to influenza virus infection. Here we show, for the first time, that swine bone marrow MSCs are permissive to replication of swine and human influenza viruses. Transplanta tion of virus-infected MSCs may transmit infection to the host and viral infection of MSCs may affect the outcome of the transplantation. Virus-infected MSCs produce pro inflammatory cytokines and, therefore, may play an impor tant role in the pathogenesis of influenza infection. MATERIALS AND METHODS Chemicals are from Sigma, USA, unless otherwise stated. Isolation and Culture of MSCs Near term pregnant Landrace-Yorkshire white-Duroc crossbred sows [Swine herd, The Ohio State University (OSU), Columbus, OH, USA] were delivered by hysterectomy and piglets were maintained in sterile gnotobiotic isolator units as described previously (46). The piglets of either sex were maintained and euthanized in accordance with the standards of the Institutional Laboratory Animal Care and Use Committee, The Ohio State University. Femur bones were obtained from 4- to-6-week-old germfree pigs (n = 4). MSCs were isolated by previously described methods (19,35). Briefly, the tip of each bone was removed and the marrow was harvested by inserting a syringe needle into one end of the bone and flushing with Dulbecco’s modified Eagle’s medium (DMEM; Gibco, USA). The bone marrow cells were filtered through a 70-μm nylon mesh filter (BD Falcon, USA), and mononuclear cells were obtained by density gradient centrifugation over Ficoll-Hypaque (GE Healthcare, USA). Cells (1–5 ´ 105/cm2) were plated in 25-cm2 cell culture flasks in DMEM containing 10% fetal bovine serum (FBS, Gibco), 2 mm l-glutamine (Gibco), 1% antibiotic solution (Gibco). Cultures were incubated at 37°C in a humidified atmosphere containing 95% air and 5% CO2. The nonadherent cells were removed after 72 h of Khatri and Saif culture. When primary cultures became nearly confluent, the cells were detached with 0.025% trypsin containing 0.02% EDTA (Life Technologies, Invitrogen, USA) and used for future experiments. Expression of Stem Cell Markers and Phenotyping of MSCs Porcine MSCs cultured on coverslips were fixed in methanol/acetone (1:1) for 3 min and then blocked with 3% bovine serum albumin (BSA) for 30 min. Cells were incubated at 4°C with the following primary antibodies: rabbit anti-human octamer binding transcription factor (Oct3/4) (Santa Cruz Biotechnology, USA) and mouse anti-human stage-specific embryonic antigen-1 (SSEA-1) (Millipore, USA). After overnight incubation, cells were washed and incubated for 1 h at room temperature with the following respective fluorescein isothiocyanate (FITC)-labeled secondary antibodies: goat anti-rabbit IgG and goat anti-mouse IgG. Cell nuclei were then counterstained with 4¢,6-diamidino-2-phenylindole (DAPI; Life Technologies). Phenotypic analysis of MSCs was performed by flow cytometry analysis (17). MSCs were detached by treatment with 0.25% trypsin-EDTA, and single cell suspension was stained with following primary antibodies: mouse anti-pig CD29, mouse anti-human CD90 (BD Biosciences, Pharmingen, USA), mouse anti-pig CD44 and CD45 (VMRD, USA) for 20 min at 4°C in the dark. After washing, cells were incubated with secondary antibodies conjugated with allophycocyanin (APC) or spectral red (BD Biosciences, Pharmingen, USA) for 30 min. Relevant isotype and secondary antibodies were used as controls for nonspecific binding. The cells were acquired by C6 flow cytometer (BD Accuri Cytometers, USA) and analyzed using CFlow® plus Software (Accuri). Anti-human Oct3/4, SSEA-1, and CD90 antibodies are cross-reactive with pig Oct3/4, SSEA-1 and CD90 antigens, respectively (3,21). MSC Differentiation MSCs were examined for differentiation into adipocytes and osteocytes (19,35). Differentiation of MSCs into adipocytes was induced by culturing confluent MSC cultures in DMEM supplemented with 10% FBS, 1 μM dexamethasone, 10 μg/ml insulin, and 0.2 mM indomethacin for 21 days. The medium was replaced every 3–4 days. Adipogenesis was assessed by Oil Red O staining. Osteogenic differentiation was induced by culturing the cells in DMEM supplemented with 10% FBS, 100 nM dexamethasone, 10 mM b-glycerophosphate, 0.05 mM l-ascorbic acid-2-phosphate. The medium was refreshed every 3–4 days, and cells were maintained in these conditions for 21 days. Calcium deposition indicative of osteogenesis was detected by Von Kossa staining. INFLUENZA VIRUS INFECTION OF MESENCHYMAL STROMAL CELLS Detection of Influenza Virus Receptors on MSCs Influenza viruses infect cells by binding to sialic acid receptors. Sialic acid receptors on MSCs were detected by immunocytochemical staining (48). MSCs were grown on coverslips to confluency and were fixed with 3.7% formaldehyde in PBS for 30 min. After blocking the cells with 2% BSA in PBS for 30 min, the cells were incubated with FITC-labeled Maackia amurensis lectin II (MAA) or Sambucus niagra agglutinin (SNA) (EY Laborato ries, USA) for 30 min in dark. Cell nuclei were stained with DAPI. Infection of MSCs With Influenza Virus Swine (Sw/OH/24366/07; H1N1) and human (Hu/ OH/K1130/06; H1N1) influenza viruses (in house); referred to as SwH1N1 and HuH1N1, (respectively, in the text) were propagated in 10-day-old embryonated chicken eggs (Charles River Laboratories, USA)(18). MSCs were infected with SwH1N1 and HuH1N1 at a multiplicity of infection (MOI) of 1. Following washing with PBS, the cells were incubated with viruses diluted in DMEM supplemented with 0.02 μg/ml TPCK (tolylsulfonyl phenylalanyl chloromethyl ketone)-treated trypsin and 0.2% BSA. After adsorption for 1 h, the cells were washed and fresh medium was added to the cells. At indicated intervals, the 463 supernatants containing viruses were titrated in Madin Darby Canine Kidney (MDCK) cells (in house). Influenza Virus-Infected MSCs Produce TNF-a and IL-6 The production of TNF-a and IL-6 in cultures of mock-, SwH1N1-, and HuH1N1-infected MSCs was quantified at 24 and 48 h after infection by ELISA (Thermoscientific, USA, and R&D Systems, USA, respectively) as described earlier (17). RESULTS Characteristics of Porcine Bone Marrow MSCs MSCs isolated from pig bone marrow showed a fibroblast-like morphology (Fig. 1A). MSCs expressed stem cell markers: Oct4 and SSEA-1 (Fig. 1B). Oct4 has been shown to regulate the pluripotency and self-renewal of embryonic and adult stem cells of human and animal origin (24). Phenotypically, these cells expressed CD29, CD44, and CD90 (Thy-1) but not CD45, indicating that these cells were of the mesenchymal lineage (Fig. 1C). Upon culturing in appropriate induction media, swine bone marrow-derived MSCs readily differentiated into adipocytes and osteocytes. MSCs incubated for 21 days in adipogenic medium showed differentiation into adipocytes. In adipogenic cultures, intracellular accumulation Figure 1. Characteristics of porcine bone marrow-derived MSCs. Bone marrow mesenchymal stromal cells (MSCs) were isolated from the femur bones of germ-free pigs. (A) Morphology of MSCs. (B) MSCs express stem cell markers octamer binding transcription factor 4 (Oct4) and stage-specific embryonic antigen-1 (SSEA-1). (C) Phenotype of porcine MSCs. Phenotype of MSCs was analyzed by flow cytometry. MSCs were positive for mesenchymal markers CD29, CD44, and CD90 and negative for hematopoietic marker CD45. Black line, isotype control; red line, specific antibody. (D) Oil Red O staining for lipid-filled vesicles (red) in cultures of MSCs in adipogenic differentiation media. (E) von Kossa staining for calcified mineral nodules (black) in cultures of MSCs in osteogenic differentiation media. 464 Khatri and Saif of lipid droplets were stained with Oil Red O, indicating adipogenesis (Fig. 1D). In osteogenic cultures mineralized nodule-like structures showing calcium deposition were observed, which stained black with Von Kossa staining (Fig. 1E). with SwH1N1 or HuH1N1. Cells were incubated with viruses at a MOI of 1 for 1 h. As shown in Figure 2, both SwH1N1 and HuH1N1 replicated in MSCs and produced cytopathic changes (Fig. 2B); however, SwH1N1 replicated to higher titers as compared to HuH1N1 (Fig. 2C). MSCs Express Receptors for Influenza Virus Influenza virus infects cells through binding to cell surface sialic acid receptors. To examine the susceptibility of MSCs to influenza virus, we first evaluated by immunocytochemistry these cells for the presence of sialic acid receptors. The a-2,3- and a-2,6-linked sialic acid receptors were detected on the surface of MSCs by MAA and SNA staining, respectively. Expression of both a-2,3- and a-2,6-linked sialic acid receptors was detected on a majority of the MSCs, suggesting that viruses of avian and mammalian lineages may be able to replicate in these cells (Fig. 2A). Influenza Virus Induces the Production of TNF-a and IL-6 in MSCs Influenza virus infection in humans and animal species is associated with the production of proinflammatory cytokines (4,41,42). To determine whether influenza virus-infected MSCs produce proinflammatory cyto kines, MSCs were infected with SwH1N1 or HuH1N1 influenza viruses. After 24 and 48 h, culture super natants were harvested and examined for the production of TNF-a and IL-6 by ELISA. The levels of TNF-a and IL-6 were substantially greater in virus-infected MSCs than in uninfected control at both time points tested (Fig. 3). The levels of TNF-a were higher at 24 h whereas IL-6 production was higher at 48 h after infection. There was no significant difference in TNF-a and IL-6 production between influenza viral strains at both time points (Fig. 3). Influenza Virus Replicates in MSCs After confirming the stemness and expression of influenza virus receptors in MSCs, we assessed the susceptibility of MSCs to influenza virus. MSCs were infected Figure 2. Replication of influenza virus in swine bone marrow-derived MSCs. (A) MSCs express a-2,3- and a-2,6-linked sialic acid receptors. MSCs were stained with fluorescein isothiocyanate (FITC)-labeled Maackia amurensis lectin II (MAA) specific for a-2,3linked sialic acid receptors (avian influenza virus) and Sambucus niagra agglutinin (SNA), specific for a-2,6-linked sialic acid receptors (mammalian influenza virus). (B) MSCs were infected with swine (SwH1N1; SwIV) or human (HuH1N1; HuIV) influenza virus at a multiplicity of infection (MOI) of 1. Virus-induced cytopathic changes in MSCs at 24 h after infection. (C) Virus production in infected culture supernatants as measured by titration in Madin Darby Canine Kidney (MDCK) cells. TCID50 = median tissue culture infective dose. INFLUENZA VIRUS INFECTION OF MESENCHYMAL STROMAL CELLS Figure 3. Influenza virus infection induces inflammatory cyto kines in MSCs. MSCs were infected with SwH1N1 or HuH1N1. After indicated times, supernatants from MSC cultures were examined for (A) tumor necrosis factor (TNF)-a and (B) interleukin (IL)-6 by ELISA. The data are expressed as mean ± SEM of two separate experiments. DISCUSSION In this study, for the first time, we have shown that influenza virus productively infects the primary swine bone marrow MSCs in vitro. Swine MSCs expressed receptors for influenza viruses and virus-infected MSCs produced proinflammatory cytokines: TNF-a and IL-6. In this study, we first examined MSCs for the expression of receptors for influenza virus. Immunofluorescence staining showed that MSCs express a-2,3 and a-2,6 sialic acid receptors utilized by avian and mammalian influenza viruses, respectively. Based on our results on the presence of virus receptors in MSCs, these cells were expected to support influenza virus replication. Indeed, we were able to detect productive infection of MSCs by swine and human influenza viruses. Previously, we and others have demonstrated the susceptibility of bone marrow derived MSCs to a variety of viruses (20,32,38). The susceptibility of MSCs to influenza virus expands the population of host target cells the virus can use for replication. Virus-infected MSCs could potentially contribute to the virus induced pathology by directly or indirectly affecting other known targets of the virus, including progenitor epithelial and other immune cells. In bone marrow compartments, virus-infected MSCs may transmit 465 virus to other stem and precursor cells in the bone marrow. As reported in this study, virus infection may cause the lysis of bone marrow MSCs, thus significantly reducing their potential for renewal and ability to differentiate into specialized cells and tissues. MSCs are known to regulate hematopoiesis via secretion of growth factors. We detected the production of IL-6 and TNF-a in influenza virus-infected MSCs. Virus infection of MSCs and factors secreted by infected cells could affect hematopoiesis and may alter the characteristics of immune progenitor cells. Production of IL-6 and TNF-a was also detected in human MSCs stimulated with polyinosinic–polycytidylic acid (poly (I:C)) (27,44). IL-6 regulates inflammatory responses and hematopoiesis (34), and its overproduction interferes with differentiation of monocytes into dendritic cells, thereby decreasing their stimulation ability on T-cells (8). IL-6 also enhances the pathology of autoimmune diseases and tissue remodeling. TNF-a is present in the inflammatory milieu (12). The production of IL-6 and TNF-a thus suggests that infection of MSCs with influenza virus might affect their differentiation potential and potentiate the virus-induced inflammatory response as observed in humans and animal species following infection with influenza virus (4,41,42). MSCs have been shown to possess immunoregulatory properties and inhibit both innate and adaptive immune cells. Infection and lysis of MSCs by influenza virus as observed in this study may result in immune dysregulation allowing hyperactivation and proliferation of inflammatory cells and excessive production of proinflammatory cytokines. Studies are underway to examine the effect of virus infection of MSCs on their differentiation potential and their ability to support hematopoiesis. A previous report (39) showed that influenza virus caused depletion of pre-B and immature B-cells in bone marrow of infected mice which was mediated by release of TNF-a produced locally in the bone marrow. However, the precise identity of the cellular source of TNF-a was not determined. Although we have not examined the direct effect of MSCs and secreted TNF-a on bone marrow immune cells, our results provide evidence that TNF-a produced by virus-infected bone marrow MSCs may mediate the apoptosis of pre-B and immature B-cells as previously observed (39). The depletion of B-cells may suppress humoral immune response against influenza virus and/or other coinfecting pathogens. In light of our data demonstrating that MSCs are susceptible to influenza virus infection in vitro, it is likely that they may be viral transmitters. MSCs derived from a donor with ongoing influenza virus infection could therefore carry virus to the recipient. Based on MSCs transplantation studies in animal models, MSCs are known to first home in the lungs after transplantation (10). Similar to humans, the respiratory tract is the primary site of 466 Khatri and Saif influenza virus replication in swine also. Therefore, transplantation of influenza virus-infected MSCs could infect susceptible cell populations in the lung and induce fatal interstitial pneumonitis after infusion. Infusion of cytomegalovirus (CMV)-infected MSCs caused widespread CMV infection in different tissues and organs in recipients (7). Taken together, these data indicate that bone marrow cells need to be tested for influenza virus before transplantation to prevent virus transmission to recipients. MSCs have been shown to possess potent immunosuppressive properties and are being evaluated in clinical settings to reduce graft-versus-host disease and transplantation rejection. In immunocompromised hosts such as hematopoietic stem cell transplant (HSCT) patients, MSC-induced immunosuppression may suppress the immune responses to infections. Several studies have reported the higher incidence and prolonged persistence of respiratory viral agents in HSCT patients (28,30,45). Our results clearly demonstrate that MSCs are susceptible to infection with influenza virus; therefore, ongoing virus infection in the recipient may infect transplanted MSCs and alter their immunomodulatory and differentiation abilities. Further studies are needed to confirm the infection of infused MSCs in influenza virus-infected pigs/animal models. In summary, we provide evidence that the bone marrow-derived MSCs are permissive to productive influ enza virus infection. Future study of influenza virus infection of MSCs in vivo and effects of virus infection on MSCs self-renewal, differentiation, and immunoregulatory functions will help to understand the critical role of MSCs in the pathogenesis of influenza virus. ACKNOWLEDGMENTS: We acknowledge the salaries and research support provided by state and federal funds appropriated to the Ohio Agriculture Research and Development Center, The Ohio State University. We are indebted to Dr. Linda Saif’s laboratory for providing the femur bones from germ-free pigs. We are grateful to Dr. Kuldeep S. Chattha for valuable assistance with the flow cytometry and cytokines ELISA. We also thank Kelly Scheuer for critically reviewing the manuscript. The authors have no financial conflict of interest. REFERENCES 1. Awad, H. A.; Boivin, G. P.; Dressler, M. R.; Smith, F. N.; Young, R. G.; Butler, D. L. Repair of patellar tendon injuries using a cell-collagen composite. J. Orthop. Res. 21:420–431; 2003. 2. Bastos, D. A.; Rodrigues, C. A.; Patah, P.; Kallas, E. G.; Rocha, V.; Novis, Y. Pandemic influenza A H1N1/09 virus infection in hematopoietic SCT recipient. Bone Marrow Transplant. 46:467–468; 2011. 3. Bosch, P.; Pratt, S. L.; Stice, S. L. Isolation, characterization, gene modification, and nuclear reprogramming of porcine mesenchymal stem cells. Biol. Reprod. 74:46–57; 2006. 4. Cheung, C. Y.; Poon, L. L.; Lau, A. S.; Luk, W.; Lau, Y. L.; Shortridge, K. F.; Gordon, S.; Guan, Y.; Peiris, J. S. Induction of proinflammatory cytokines in human macrophages by influenza A (H5N1) viruses: A mechanism for the unusual severity of human disease? Lancet 360:1831– 1837; 2002. 5. Choi, S. M.; Boudreault, A. A.; Xie, H.; Englund, J. A.; Corey, L.; Boeckh, M. Differences in clinical outcomes after 2009 influenza A/H1N1 and seasonal influenza among hematopoietic cell transplant recipients. Blood 117:5050– 5056; 2011. 6. Claas, E. C.; Osterhaus, A. D.; van Beek, R.; De Jong, J. C.; Rimmelzwaan, G. F.; Senne, D. A.; Krauss, S.; Shortridge, K. F.; Webster, R. G. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet 351:472–477; 1998. 7. Crapnell, K. B.; Almeida-Porada, G.; Khaiboullina, S.; St. Jeor, S. C.; Zanjani, E. D. Human haematopoietic stem cells that mediate long-term in vivo engraftment are not susceptible to infection by human cytomegalovirus. Br. J. Haematol. 124:676–684; 2004. 8. Djouad, F.; Charbonnier, L. M.; Bouffi, C.; Louis-Plence, P.; Bony, C.; Apparailly, F.; Cantos, C.; Jorgensen, C.; Noel, D. Mesenchymal stem cells inhibit the differentiation of dendritic cells through an interleukin-6-dependent mechanism. Stem Cells 25:2025–2032; 2007. 9. Espinosa-Aguilar, L.; Green, J. S.; Forrest, G. N.; Ball, E. D.; Maziarz, R. T.; Strasfeld, L.; Taplitz, R. A. Novel H1N1 influenza in hematopoietic stem cell transplantation recipients: Two centers’ experiences. Biol. Blood Marrow Transplant. 17:566–573; 2011. 10. Gao, J.; Dennis, J. E.; Muzic, R. F.; Lundberg, M.; Caplan, A. I. The dynamic in vivo distribution of bone marrowderived mesenchymal stem cells after infusion. Cells Tissues Organs 169:12–20; 2001. 11. George, B.; Ferguson, P.; Kerridge, I.; Gilroy, N.; Gottlieb, D.; Hertzberg, M. The clinical impact of infection with swine flu (H1N109) strain of influenza virus in hematopoietic stem cell transplant recipients. Biol. Blood Marrow Transplant. 17:147–153; 2011. 12. Go, Y. M.; Kang, S. M.; Roede, J. R.; Orr, M.; Jones, D. P. Increased inflammatory signaling and lethality of influenza H1N1 by nuclear thioredoxin-1. PLoS One 6:e18918; 2011. 13. Guan, Y.; Vijaykrishna, D.; Bahl, J.; Zhu, H.; Wang, J.; Smith, G. J. The emergence of pandemic influenza viruses. Protein Cell 1:9–13; 2010 14. Haynesworth, S. E.; Baber, M. A.; Caplan, A. I. Cytokine expression by human marrow-derived mesenchymal progenitor cells in vitro: Effects of dexamethasone and IL-1a. J. Cell. Physiol. 166:585–592; 1996. 15. Iyer, S. S.; Rojas, M. Anti-inflammatory effects of mesenchymal stem cells: Novel concept for future therapies. Expert Opin. Biol. Ther. 8:569–581; 2008. 16. Jiang, Y.; Jahagirdar, B. N.; Reinhardt, R. L.; Schwartz, R. E.; Keene, C. D.; Ortiz-Gonzalez, X. R.; Reyes, M.; Lenvik, T.; Lund, T.; Blackstad, M.; Du, J.; Aldrich, S.; Lisberg, A.; Low, W. C.; Largaespada, D. A.; Verfaillie, C. M. Pluripotency of mesenchymal stem cells derived from adult marrow. Nature 418:41–49; 2002. 17. Khatri, M.; Dwivedi, V.; Krakowka, S.; Manickam, C.; Ali, A.; Wang, L.; Qin, Z.; Renukaradhya, G. J.; Lee, C. W. Swine influenza H1N1 virus induces acute inflammatory INFLUENZA VIRUS INFECTION OF MESENCHYMAL STROMAL CELLS immune responses in pig lungs: A potential animal model for human H1N1 influenza virus. J. Virol. 84:11210– 11218; 2010. 18. Khatri, M.; O’Brien, T. D.; Goyal, S. M.; Sharma, J. M. Isolation and characterization of chicken lung mesenchymal stromal cells and their susceptibility to avian influenza virus. Dev. Comp. Immunol. 34:474–479; 2010. 19. Khatri, M.; O’Brien, T. D.; Sharma, J. M. Isolation and differentiation of chicken mesenchymal stem cells from bone marrow. Stem Cells Dev. 18:1485–1492; 2009. 20. Khatri, M.; Sharma, J. M. Susceptibility of chicken mesenchymal stem cells to infectious bursal disease virus. J. Virol. Methods 160:197–199; 2009. 21. Kim, S.; Kim, J. H.; Lee, E.; Jeong, Y. W.; Hossein, M. S.; Park, S. M.; Park, S. W.; Lee, J. Y.; Jeong, Y. I.; Kim, H. S.; Kim, Y. W.; Hyun, S. H.; Hwang, W. S. Establishment and characterization of embryonic stem-like cells from porcine somatic cell nuclear transfer blastocysts. Zygote 18:93– 101; 2010. 22. Koc, O. N.; Gerson, S. L.; Cooper, B. W.; Dyhouse, S. M.; Haynesworth, S. E.; Caplan, A. I.; Lazarus, H. M. Rapid hematopoietic recovery after coinfusion of autologousblood stem cells and culture-expanded marrow mesenchymal stem cells in advanced breast cancer patients receiving high-dose chemotherapy. J. Clin. Oncol. 18:307–316; 2000. 23. Kuiken, T.; Taubenberger, J. K. Pathology of human influenza revisited. Vaccine 26 Suppl 4:D59–66; 2008. 24. Lavial, F.; Acloque, H.; Bertocchini, F.; Macleod, D. J.; Boast, S.; Bachelard, E.; Montillet, G.; Thenot, S.; Sang, H. M.; Stern, C. D.; Samarut, J.; Pain, B. The Oct4 homologue PouV and Nanog regulate pluripotency in chicken embryonic stem cells. Development 134:3549– 3563; 2007. 25. Le Blanc, K.; Rasmusson, I.; Sundberg, B.; Gotherstrom, C.; Hassan, M.; Uzunel, M.; Ringden, O. Treatment of severe acute graft-versus-host disease with third party haploidentical mesenchymal stem cells. Lancet 363:1439– 1441; 2004. 26. Le Blanc, K.; Ringden, O. Mesenchymal stem cells: Properties and role in clinical bone marrow transplantation. Curr. Opin. Immunol. 18:586–591; 2006. 27. Liotta, F.; Angeli, R.; Cosmi, L.; Fili, L.; Manuelli, C.; Frosali, F.; Mazzinghi, B.; Maggi, L.; Pasini, A.; Lisi, V.; Santarlasci, V.; Consoloni, L.; Angelotti, M. L.; Romagnani, P.; Parronchi, P.; Krampera, M.; Maggi, E.; Romagnani, S.; Annunziato, F. Toll-like receptors 3 and 4 are expressed by human bone marrow-derived mesenchymal stem cells and can inhibit their T-cell modulatory activity by impairing Notch signaling. Stem Cells 26:279– 289; 2008. 28. Ljungman, P.; Ward, K. N.; Crooks, B. N.; Parker, A.; Martino, R.; Shaw, P. J.; Brinch, L.; Brune, M.; De La Camara, R.; Dekker, A.; Pauksen, K.; Russell, N.; Schwarer, A. P.; Cordonnier, C. Respiratory virus infections after stem cell transplantation: A prospective study from the Infectious Diseases Working Party of the European Group for Blood and Marrow Transplantation. Bone Marrow Transplant. 28:479–484; 2001. 29. Majumdar, M. K.; Thiede, M. A.; Mosca, J. D.; Moorman, M.; Gerson, S. L. Phenotypic and functional comparison of cultures of marrow-derived mesenchymal stem cells (MSCs) and stromal cells. J. Cell. Physiol. 176:57–66; 1998. 467 30. Nichols, W. G.; Guthrie, K. A.; Corey, L.; Boeckh, M. Influenza infections after hematopoietic stem cell transplantation: Risk factors, mortality, and the effect of antiviral therapy. Clin. Infect. Dis. 39:1300–1306; 2004. 31. Noel, D.; Djouad, F.; Jorgense, C. Regenerative medicine through mesenchymal stem cells for bone and cartilage repair. Curr. Opin. Investig. Drugs 3:1000–1004; 2002. 32. Parsons, C. H.; Szomju, B.; Kedes, D. H. Susceptibility of human fetal mesenchymal stem cells to Kaposi sarcomaassociated herpesvirus. Blood 104:2736–2738; 2004. 33. Pelttari, K.; Steck, E.; Richter, W. The use of mesenchymal stem cells for chondrogenesis. Injury 39 Suppl 1:S58– S65; 2008. 34. Pevsner-Fischer, M.; Morad, V.; Cohen-Sfady, M.; RoussoNoori, L.; Zanin-Zhorov, A.; Cohen, S.; Cohen, I. R.; Zipori, D. Toll-like receptors and their ligands control mesenchymal stem cell functions. Blood 109:1422–1432; 2007. 35. Pittenger, M. F.; Mackay, A. M.; Beck, S. C.; Jaiswal, R. K.; Douglas, R.; Mosca, J. D.; Moorman, M. A.; Simonetti, D. W.; Craig, S.; Marshak, D. R. Multilineage potential of adult human mesenchymal stem cells. Science 284:143– 147; 1999. 36. Pittenger, M. F.; Martin, B. J. Mesenchymal stem cells and their potential as cardiac therapeutics. Circ. Res. 95:9–20; 2004. 37. Ren, G.; Su, J.; Zhang, L.; Zhao, X.; Ling, W.; L’Huillie, A.; Zhang, J.; Lu, Y.; Roberts, A. I.; Ji, W.; Zhang, H.; Rabson, A. B.; Shi, Y. Species variation in the mechanisms of mesenchymal stem cell-mediated immunosuppression. Stem Cells 27:1954–1962; 2009. 38. Rollin, R.; Alvarez-Lafuente, R.; Marco, F.; Jover, J. A.; Hernandez-Garcia, C.; Rodriguez-Navas, C.; Lopez-Duran, L.; Fernandez-Gutierrez, B. Human parvovirus B19, varicella zoster virus, and human herpesvirus-6 in mesenchymal stem cells of patients with osteoarthritis: Analysis with quantitative real-time polymerase chain reaction. Osteoarthritis Cartilage 15:475–478; 2007. 39. Sedger, L. M.; Hou, S.; Osvath, S. R.; Glaccum, M. B.; Peschon, J. J.; van Rooijen, N.; Hyland, L. Bone marrow B cell apoptosis during in vivo influenza virus infection requires TNF-a and lymphotoxin-a. J. Immunol. 169:6193– 6201; 2002. 40. Subbarao, K.; Klimov, A.; Katz, J.; Regnery, H.; Lim, W.; Hall, H.; Perdue, M.; Swayne, D.; Bender, C.; Huang, J.; Hemphill, M.; Rowe, T.; Shaw, M.; Xu, X.; Fukuda, K.; Cox, N. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science 279:393–396; 1998. 41. Suzuki, K.; Okada, H.; Itoh, T.; Tada, T.; Mase, M.; Nakamura, K.; Kubo, M.; Tsukamoto, K. Association of increased pathogenicity of Asian H5N1 highly pathogenic avian influenza viruses in chickens with highly efficient viral replication accompanied by early destruction of innate immune responses. J. Virol. 83:7475–7486; 2009. 42. Szretter, K. J.; Gangappa, S.; Lu, X.; Smith, C.; Shieh, W. J.; Zaki, S. R.; Sambhara, S.; Tumpey, T. M.; Katz, J. M. Role of host cytokine responses in the pathogenesis of avian H5N1 influenza viruses in mice. J. Virol. 81:2736– 2744; 2007. 43. To, K. F.; Chan, P. K.; Chan, K. F.; Lee, W. K.; Lam, W. Y.; Wong, K. F.; Tang, N. L.; Tsang, D. N.; Sung, R. Y.; Buckley, T. A.; Tam, J. S.; Cheng, A. F. Pathology of fatal human infection associated with avian influenza A H5N1 virus. J. Med. Virol. 63:242–246; 2001. 468 44. Tomchuck, S. L.; Zwezdaryk, K. J.; Coffelt, S. B.; Waterman, R. S.; Danka, E. S.; Scandurro, A. B. Toll-like receptors on human mesenchymal stem cells drive their migration and immunomodulating responses. Stem Cells 26:99–107; 2008. 45. Whimbey, E.; Elting, L. S.; Couch, R. B.; Lo, W.; Williams, L.; Champlin, R. E.; Bodey, G. P. Influenza A virus infections among hospitalized adult bone marrow transplant recipients. Bone Marrow Transplant. 13:437–440; 1994. 46. Yuan, L.; Ward, L. A.; Rosen, B. I.; To, T. L.; Saif, L. J. Systematic and intestinal antibody-secreting cell responses and correlates of protective immunity to human rotavirus in a gnotobiotic pig model of disease. J. Virol. 70:3075– 3083; 1996. Khatri and Saif 47. Yuen, K. Y.; Chan, P. K.; Peiris, M.; Tsang, D. N.; Que, T. L.; Shortridge, K. F.; Cheung, P. T.; To, W. K.; Ho, E. T.; Sung, R.; Cheng, A. F. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 351:467–471; 1998. 48. Zeng, H.; Goldsmith, C.; Thawatsupha, P.; Chittaganpitch, M.; Waicharoen, S.; Zaki, S.; Tumpey, T. M.; Katz, J. M. Highly pathogenic avian influenza H5N1 viruses elicit an attenuated type i interferon response in polarized human bronchial epithelial cells. J. Virol. 81:12439–12449; 2007. 49. Zhang, Z.; Zhang, J.; Huang, K.; Li, K. S.; Yuen, K. Y.; Guan, Y.; Chen, H.; Ng, W. F. Systemic infection of avian influenza A virus H5N1 subtype in humans. Hum. Pathol. 40:735–739; 2009.
© Copyright 2026