Angiogenic signal triggered by ischemic stress induces myocardial
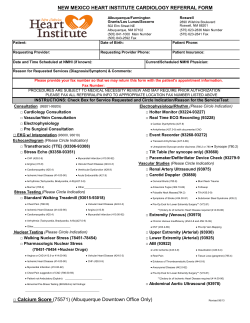
Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 www.elsevier.com/locate/yjmcc Original Article Angiogenic signal triggered by ischemic stress induces myocardial repair in rat during chronic infarction Shoji Fukuda a, Shigeaki Kaga a, Hiroaki Sasaki a, Lijun Zhan a, Li Zhu a, Hajime Otani b, Reni Kalfin c, Dipak K Das, Nilanjana Maulik a,* b a Molecular Cardiology Laboratory, University of Connecticut Medical School, Farmington, Connecticut, USA Department of Thoracic and Cardiovascular Surgery, Kansai Medical University, School of Medicine, Osaka, Japan c Bulgarian Academy of Sciences, Institute of Physiology, Sofia, Bulgaria Received 5 November 2003; received in revised form 23 January 2004; accepted 4 February 2004 Abstract In the present study, we examined a novel method of stimulating myocardial angiogenesis through ischemic preconditioning (IP) in the form of in vivo four repetitive cycles of coronary artery occlusion each followed by reperfusion. Rats divided into 4 groups: Control+Sham surgery (CS), Control+ Left anterior descending coronary artery (LAD) occlusion (CMI), IP+ Sham surgery (IPS) and IP+LAD occlusion (IPMI). For cardiac function, rats were subjected to stress testing with dobutamine after 2, 4, 7, 14 and 21 operative days. Capillary density (CD) and arteriolar density (AD) were evaluated by immunohistochemistry. Western blot was performed to examine the expression pattern for VEGF and anti-death candidates, Bcl-2 and survivin. Blood flow and the extent of endothelial and cardiomyocyte cell death were examined. The protein/DNA array was performed to determine the status of various transcription factor related to stress signal. Left ventricular functional reserve was better preserved in IPMI compared to the CMI group. The infarct size and apoptotic cell death were reduced in IPMI group significantly. Left ventricular regional blood flow, perfused capillary density and AD increased significantly in the IPMI group. VEGF, Bcl-2 and survivin expression were increased in IPMI compared to CMI. VEGF mediated vascular permeability was controlled in the IPMI due to suppression of c-Src in the infarcted myocardium. Our study documented first time the ability of IP to induce angiogenesis in the infarcted myocardium along with the activation of several transcription factors such as Stat3, Pax-5, NFjB, TFIID, SP1 and reduction of VEGF mediated vascular permeability by inhibition of c-Src in IPMI group thereby reducing ischemic injury in rat MI model. © 2004 Elsevier Ltd. All rights reserved. Keywords: Angiogenesis; Ischemic Stress; Myocardial Infarction; Edema; VEGF 1. Introduction Angiogenic therapy for the human heart is currently being vigorously pursued. In the past ten years, alternative revascularization/angiogenesis strategies have progressed from bench to bedside, focusing on the capillary sprouting and/or growth of new vessels to replace the old. However, most of the strategies involve the delivery of growth factors. Very little success with these strategies has been demonstrated so far for various reasons. Our approach to IP mediated angiogenesis and growth factors/receptors * Correspondence: Nilanjana Maulik, Ph. D. Molecular Cardiology Laboratory, Cardiovascular Division, Department of Surgery University of Connecticut School of Medicine, Farmington, CT 06030-1110, USA Tel: (860) 679-2857 Fax: (860) 679-2825. E-mail address: [email protected] (N. Maulik). © 2004 Elsevier Ltd. All rights reserved. doi:10.1016/j.yjmcc.2004.02.002 stimulation for cardioprotection is a very novel and potentially very exciting strategy for myocardial protection. Preconditioning of heart by repeated ischemia and reperfusion was found to delay the onset of subsequent irreversible ischemic injury [1]. It is well known that preconditioning provides cardioprotection by reducing subsequent postischemic ventricular dysfunction, decreasing incidence of arrhythmias, and infarct size. Such myocardial preservation by repeated short-term reversible ischemia leads to the development of the concept of stress adaptation [2]. After myocardial infarction (MI), left ventricular (LV) enlargement is a frequent development and this process is known as postinfarction ventricular remodeling. Capillary density becomes lower in the border zone than in the remote areas of the infarcted ventricle [3]. The development of coronary collateral circulation in the infarcted myocardium is the heart’s own bypass mechanism (adaptation) by which it retains the 548 S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 blood supply to the myocardium at risk [4]. Thus, it is extremely important to develop body’s natural angiogenic process in order to create increased circulation in areas where blocked coronary arteries deprive the heart muscle of sufficient blood flow, e.g., in the settings of myocardial ischemia [5]. Ischemia or coronary artery occlusion has been shown to induce vascular endothelial growth factor (VEGF) mRNA in rat hearts [6]. VEGF is a well known endothelial cell-specific angiogenic factor and also a critical regulator of angiogenesis that stimulates proliferation, migration, and proteolytic activity of endothelial cells [7]. Additional reports suggested VEGF induced expression of Bcl-2 which eventually functions to enhance the survival of endothelial cells in the toxic, oxygen-deficient environment [8]. This report points out that enhanced level of VEGF may have some role in the inhibition of cardiomyocyte and endothelial cell apoptosis. In addition to the most popular Bcl-2 family which plays a significant role in all aspects of cell death and survival, another group of proteins/molecules (inhibitor of apoptosis, IAP) were also found to play a prominent role in the inhibition of apoptosis [9–11]. The most prominent member of this family is survivin, which has been characterized as mammalian IAP. It is a bifunctional protein and is involved in suppression of apoptosis and cell division. The importance of the expression of this anti-apoptotic protein survivin, during myocardial adaptation, was never studied so far. In the present study we showed for the first time significant upregulation of the expression of this anti-death molecule survivin along with the expression of Bcl-2 in the ischemic preconditioned myocardium subjected to myocardial infarction. Several important transcription factors such as Pax-5, TFIID, SP1, Stat3, NFjB, were also found to be activated and involved in IP mediated myocardial angiogenesis. This report also demonstrates for the first time that IP reduced VEGF-mediated vascular permeability by downregulation of c-Src protein expression and reduction of edema formation leading to cardioprotection. Therefore, this study was undertaken to investigate the possibility of long-term cardioprotective effects of IP in the post-MI in vivo rat model involving permanent coronary occlusion. The aim of this study was to demonstrate the extent to which IP is capable of exerting long-term cardioprotection through preserving cardiac function after MI and possibly retard the development of overt heart failure. We also sought to investigate whether augmentation of the myocardial angiogenic response in the form of increased activation of angiogenic (VEGF) and anti-apoptotic proteins (Bcl-2 and survivin) and transcription factors (Stat3, Pax-5, NFjB, SP1) could stimulate angiogenesis in the form of increased capillary and/or arteriolar density and ultimately contribute towards cardioprotection. Moreover, this study also determined cardioprotection by c-Src inhibition by IP compared to control because suppression of Src decreases vascular permeability that minimizes heart injury. 2. Materials and methods 2.1. Animals All animals used in this study received human care in compliance with the principles of laboratory animal care formulated by the National Society for Medical Research and Guide for the Care and use of Laboratory Animals published by NIH. 2.2. Surgical procedure Male Sprague Dawley rats weighing between 250 and 300g was anesthetized with ketamine HCl (100 mg/kg i.p.) and xylazine (10 mg/kg i.p.). Cefazolin (25 mg/kg i.p.) was administered as preoperative antibiotic cover. After tracheotomy and initiation of ventilation (room air, Harvard Apparatus Rodent Ventilator:Model 683), the heart was exposed through a left lateral thoracotomy (4th intercostal space). A 6-0 polypropylene suture was passed with tapered needle under the left anterior descending coronary artery (LAD) just below the tip of the left auricle, and a non-traumatic occluder was applied on the artery. The myocardium was preconditioned by carrying out a short duration of temporary regional ischemia (5 min) followed by a period of reperfusion (10 min) repeated four times (4 × PC). Myocardial infarction was produced by permanent LAD occlusion. In the non-PC group, the rats underwent the LAD ligation after opening the chest for 60 min without the PC procedure. The rats in the sham group underwent the same procedure except for the LAD ligation. After completion of all surgical protocols, the chest wall was re-closed. After application of buprenorphine (0.1 mg/kg s.c.), and weaning from the respirator, the rats were placed on a heating pad while recovering from anesthesia. 2.3. Hemodynamics After surgical procedures (2, 4, 7, 14 and 21 days), the rats were anesthetized and ventilated as described above. The arterial catheter was advanced into the left ventricle through the right carotid artery. Hemodynamics were measured using PowerLab equipment with Chart v5 software (ADInstruments, Castle Hill, Australia) at a sampling rate of 1000/s, and averaged over three consecutive cycles. For the assessment of contractile reserve in infarcted myocardium, dobutamine stress test was performed. After resting left ventricular functional study, dobutamine was administered intravenously at a dose of 5 µg/kg body weight /minute for 3 min. 2.4. Measurement of perfused capillary and arteriolar density To measure the perfused capillary density, animals were perfused just before sacrifice in vivo with FITC conjugated S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 BS1-lectin staining to identify perfused vascular endothelium (Vector Laboratories) 2, 4, 7, 14 and 21 days after permanent LAD occlusion. For determination of arteriolar density, cross sections of paraffin-embedded specimens were stained with FITC conjugated mouse monoclonal anti-a smooth muscle actin antibody. For the quantitative purpose, the number of perfused capillary and arteriolar density were counted on area at risk from the endocardium through the epicardium of the mid portion of the left ventricular free wall. Four sections from each heart were examined. 2.5. Measurement of infarct size 2, 4, 7, 14 and 21 days after infarction (n = 5), infarct size and area at risk were measured as previously described [12]. The infarct size was measured in the 8 horizontal sections between the point of ligation and the apex. The area at risk was recognized as the area demarcated with 5% Evans blue dye, whereas the non-infarcted and infracted areas were demarcated after incubation with 1% triphenyltetrazolium chloride (TTC) phosphate buffered solution (pH 7.4) at 37°C for 15 min and fixed in 10% formalin to increase the contrast of the Evans blue and TTC staining. With the use of NIH imaging, the volumes of infarcted myocardium were calculated. Infarct size was reported as a percent of the area at risk. 2.6. Myocardial blood flow 2, 4, 7, 14 and 21 days after permanent LAD occlusion, myocardial blood flow in the area at risk was measured with stable gold labeled microspheres (BioPAL, Worcester, MA). Approximately 1,000,000 microspheres were injected into the LV. Simultaneously, a reference blood sample was withdrawn from an arterial catheter (0.5 ml/min). At the end of the experiments the animals were killed by 2 mEq KCl intravenously. The microscopically visible left ventricular tissue within 1.5 mm distance from edge of scar tissue were carefully dissected and weighed. All tissue and blood samples were sent to Bio PAL and microspheres concentration of each sample were estimate during spectrophotometric analysis. Myocardial blood flow was calculated as ml/min/g tissue [13,14]. 2.7. Determination of cardiomyocyte and endothelial cell apoptosis The formaldehyde-fixed left ventricle (1, 2, 4 and 7 days after MI) was embedded in paraffin, cut into transverse sections (4 µm thick) and deparaffinized with a graded series of xylene and ethanol solutions. Immunohistochemical detection of apoptotic cells was carried out using TUNEL in which residues of digoxigenin-labelled dUTP are catalytically incorporated into the DNA by terminal deoxynucleotidyl transferase, an enzyme which catalyzes a template-independent addition of nucleotide triphosphate to the 3′-OH ends of double- or single-stranded DNA [15]. The incorporated 549 nucleotide was incubated with a sheep polyclonal antidigoxigenin antibody followed by a FITC-conjugated rabbit anti-sheep IgG as a secondary antibody as described by the manufacturer (Apop Tag Plus, Oncor Inc., Gaithersburg, MD). The sections (n = 5) were washed in PBS three times, blocked with normal rabbit serum and incubated with mouse monoclonal antibody recognizing-a-sarcomeric actin (Sigma Japan, Tokyo, Japan) followed by staining with TRIRC-conjugated rabbit anti-mouse IgG (200:1 dilution, Dako Japan, Tokyo, Japan) [16]. For detection of apoptosis in endothelial cells the sections were first stained with TUNEL (FITC staining). The sections were then incubated with rabbit polyclonal anti-von Willebrand factor (Dako) as a primary antibody followed by incubation with tetrarhodamine isothiocyanate-conjugated goat anti-rabbit IgG as a secondary antibody. The fluorescence staining was viewed with confocal laser microscopy (Fluoview, Olympas, Tokyo, Japan). For the quantitative purpose, the number of TUNELpositive cardiomyocytes and endothelial cells were counted on 100 high power fields (HPF, magnification × 600) from the endocardium through the epicardium of the mid portion of the left ventricular free wall in five sections from each heart [12,17]. Representative confocal images show von Willebrand factor-positive endothelial cells (strong red staining in their cytosol) which are negative for TUNEL staining (absence of green staining in the nucleus) as well as those positive for TUNEL staining (magnification ×1200). 2.8. Protein/DNA array Nuclear extracts from the left ventricular tissue 2 days after MI were prepared with the commercially available kit (Panomics Nuclear Extraction Kit). Each nuclear extract sample (3–5 µg/µl, 5 µl) were mixed with TranSignal Probe Mix (10 µl, from Panomics) and dH2O, 5 µl, this mixture was incubated at 15°C for 30 minutes. 2% agarose gel was prepared in 0.5 × TBE, sample was loaded and were run for 15 min at 120 V. The gel area was excised that contains protein/DNA complex and were transferred to 1.5 ml tube. One ml of Extraction buffer (supplied by the company, Panomics, Redwood city, CA) A was added and incubated at 55–60°C. 6 µl of gel extraction beads were added and incubated at room temperature for 10 min. The mixture was centrifuged at 10,000 rpm for 30 sec to pellet out the beads. The beads were washed and resuspended the pellet in 150 µl of extraction buffer B (supplied) and centrifuged at 10,000 rpm for 30 sec. Pellets were dried (air) for 10 min. Bound probe was eluted by resuspending the pellet in 50 µl of dH2O with a pipet and incubate at room temperature for 10 min. After centrifugation at 10,000 rpm for 1 min, supernatant was transferred to a fresh 0.2 tube. Eluted probe was stored on ice until proceeding to hybridization. This labeled probe was hybridized to the array membrane (Panomics, Catalog No. MA1010, Redwood City, CA). After hybridization and washing the membrane were treated with Enhanced Chemi-Luminescence (ECL from Amersham) reagent and 550 S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 the transcription factors were detected by autoradiography for variable lengths of time with Kodak X-Omat film. 2.9. Gel-Shift analysis To determine SP1, AP-1, NFjB, STAT3, TFIID and Pax-5 binding activity, nuclear proteins were isolated from the heart of sham, CMI and IPMI groups. Sp1 (5′ GAT-CCT-TCTGGG-AAT-TCC-TAG-ATC 3′), AP-1 (5′ CGC-TTG-ATGAGT-CAG-CCG-GAA-3), NFjB(5′ AGT-TGA-GGG-GACTTT-CCC-AGG-C-3′), STAT3 (5′GAT-CCT-TCT-GGG-AATTCC-TAG-ATC 3′), TFIID (5′GCA-GAG-CAT-ATA-AGGTGA-GGT-AGG-AGG-A 3′) and Pax-5(5′GAA-TGG-GGCACT-GAG-GCG-TGA-CCA-CCG-3′) oligonucleotides were labeled using T4 polynucleotide kinase as described [18]. 2.10. Western blot analysis for VEGF, Bcl-2, Survivin and c-Src To quantify the abundance of the angiogenic factor VEGF and anti-apoptotic factors Bcl-2, survivin and cytoplasmic tyrosine kinase, c-Src (we included 1day data only for c-Src study) 2, 4, 7, 14 and 21 days after MI, we performed standard Western blot using specific antibodies (Santa Cruz Biotech, Santa Cruz, CA) as previously described [19]. 2.11. Src inhibitor The Src-inhibitor PP1 (BIOMOL, Plymouth Meeting, Pennsylvania) was used for our experimental purposes. PP1 or vehicle in control was injected (IP) at 1.5 mg/kg [20] immediately after permanent LAD occlusion. 2.12. Measurement of % water content Myocardial water content of left ventricle was measured after 2, 4 and 7 days following MI as previously described [21]. Left ventricular water content was calculated as percentage difference between initial wet and dry weights after 48 hours incubation at 60°C. 2.13. Statistical analysis Results are expressed as mean± standard error of the mean (±SEM). Differences between groups were tested for statistical significance by two-way analysis of variance (ANOVA) and Student’s t-test (p < 0.05). 3. Result 3.1. Effect of ischemic preconditioning on cardiac function Pharmacological cardiac stress testing with dobutamine infusion at 0 and 5 µg/kg/min for 3 min revealed differences in the extent of cardiac contractile reserve between CMI and IPMI as shown in Fig. 1A. This was evident from differences in the extent of change in LVdP/dtmax values displayed by CMI and IPMI groups during the course of such stress testing 2, 4, 7, 14 and 21 days after surgical intervention. The differences remained statistically significant after 2, 4, 7, 14 and even after 21 days. The IPMI group displayed significantly elevated contractile reserve at “0”dose point of evaluation compared to the CMI group after 7, 14 and 21 days after MI. However, this enhanced preservation of contractile reserve in the IPMI group was apparent at 5 µg/kg/min after 2, 4, 7, 14 and 21 days (3128 ± 253 mmHg/s in IPMI group vs. 1808 ± 336mm Hg/s in CMI group at 21 days after MI). There was no difference in heart rate between the groups even after 3 weeks of MI (data not shown). Both in CMI and IPMI left ventricular end-diastolic pressure (LVEDP) was increased significantly compared to the sham operated groups, however, in IPMI group the LVEDP at 21 days after MI was found to be reduced significantly at 5µg/kg/min of dobutamine (21.2 ± 2.52 vs. 32.4 ± 1.98 mmHg in CMI group) (data not shown). 3.2. Measurement of infarct size Heart sections, which were obtained 2, 4, 7, 14 and 21 days after permanent LAD occlusion and stained for the extent of infarction demonstrated significantly lowered infarct size in the IPMI group (36 ± 2.2% at 2 days post-op) when compared to the CMI group (53.8 ± 3.7% at 2 days post-op) (Fig. 1B). This lowered infarction size was well maintained even after 21 days of post-operation in the IPMI group. We found PP1 (1.5 mg/kg/i.p) injection (i.p) just after LAD ligation in the control MI group can reduce infarct size significantly when compared to the non-PP1 control group of hearts (Fig. 9C) following 2 days after MI. 3.3. Effect of ischemic preconditioning on microvascular Density 3.3.1. (a) Measurement of perfused capillary density At 400× magnification, 8 non-overlapping random fields, each selected from non-infarcted, risk area of 4 different left ventricular sections per sample were examined under fluorescence microscope to determine FITC conjugated BS1lectin labeled capillaries. The IPMI group showed significant increase in perfused capillary density compared to the control MI group (Fig. 2A). The IPMI group showed significant difference in perfused capillary density after 2 days post MI. IPMI group demonstrated increased capillary density (1880 ± 210 counts/mm2) compared to the CMI group (1660 ± 296 counts/mm2). The increased level of capillary density in the IPMI group was also maintained significantly even after 14 days (2650 ± 120 counts/mm2) and 21 days (2760 ± 252 counts/mm2) compared to the CMI group (1940 ± 73 counts/mm2 at 14 days and 2030 ± 185 counts/mm2 at 21 days, respectively). S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 551 A LVdP/dtmax (mmHg/s) 5000 4000 ** ** ** 3000 * * 2000 * * * 1000 0 DOB (µg/kg/min) 0 5 0 4 days 5 7 days 0 0 5 14days 5 21days 80 %Infarct/Area at risk B 0 5 2 days 60 40 * * * * 2 days 4 days 7 days 14 days * 20 0 21 days Fig. 1. (A) Measurement of LV dP/dt max during dobutamine (5ug/kg/min) stress test for 3min. Changes in LV dP/dt max 2, 4, 7, 14 and 21 days after MI were recorded with and without dobutamine. Differences were considered significant at p < 0.05. Where * p < 0.05, ** p < 0.01 compared to CMI. [● ] CS, [ C ] IPS, ["] CMI, [◆] IPMI. (B) Infarct size of the hearts, expressed as a percentage of the area at risk 2, 4, 7, 14 and 21 days after LAD occlusion. Results are expressed as means ± S.E.M of 6 hearts/group. * p < 0.05 compared to CMI. [ ] CMI and [ ] IPMI. 3.3.2. (b) Measurement of arteriolar density We evaluated the arteriolar density in the non-infarcted risk area 2, 4, 7, 14 and 21 days after the surgical intervention (MI). We examined the arteriolar density in the 8 non-overlapping fields in the 4 horizontal sections from middle portion of left ventricle at 400× magnification. The ischemic preconditioned myocardium showed no change in arteriolar density even after 4 days after MI however a marked increase in arteriolar density was observed after 7, 14 and 21 days after MI when compared to the non-preconditioned myocardium. Arteriolar density remained almost the same in the CMI group after 7 (2.2 ± 0.8 counts/mm2), 14 (2.2 ± 0.2 counts/mm2) and 21 days (2.3 ± 0.6 counts/mm2) of infarction. In contrast, in the IPMI group, the arteriolar density increased markedly after 7 (2.7 ± 1.0 counts/mm2), 14 (2.9 ± 0.4 counts/mm2) and 21 days (3.1 ± 0.8 counts/mm2) compared to the CMI group (Fig. 2B). 3.4. Measurement of blood flow In the ischemic preconditioned myocardium, significant increase in regional blood flow was observed with neutron activation technique just after IP which was maintained even after 2 days post operation. Four days later the flow in IPMI group was significantly higher (1.48 ± 0.7 ml/kg/gm) compared to the CMI group (0.89 ± 0.4 ml/kg/gm). This in- creased flow persisted significantly even after 21 days (1.68 ± 0.2 vs. 1.22 ± 0.7 ml/kg/gm) as shown in Fig. 2C. We also determined significant increase in blood flow when PP1 (1.5 µg/kg/i.p) was injected to CMI group compared to non-PP1 control following 2 days after MI. 3.5. Extent of apoptotic cell death (cardiomyocyte and endothelial) Total number of myocytes in 100 high power fields, which cover almost 2/3 of mid portion of left ventricular free wall, was examined for detecting apoptotic cells. In this regional ischemia model, apoptotic cells are exclusively distributed to the border area of infarction. Thus, in a border area, apoptotic cells may exceed 30% at one day after MI, while in other areas remote from the infarct zone percent apoptotic cells is virtually zero. Therefore, the data were expressed in counts/100 high power field and not percent apoptotic cells, because it is valid only in a global ischemia model. The number of endothelial and cardiomyocyte apoptotic cells was significantly high at 1 and 2 days after MI in both groups (CMI and IPMI), however, in IPMI group the number of apoptotic cells was significantly lower than that in the CMI group at each time point. The differences even 4 and 7 days after MI was significant (Fig. 3A and 3B). 552 S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 2800 2600 2400 2200 2000 1800 1600 1400 permanent LAD occlusion 3000 4PC Perfused Capillary Density 2 ( counts/mm ) A Before IP B ** ** * 2 days 4 days 7 days 4PC Arteriolar Density 2 ( counts/mm ) 2.5 2.0 1.5 1.0 0.5 0 C permanent LAD occlusion 3.5 3.0 Before IP * 2 days 4 days permanent LAD occlusi on Blood Flow (ml/min/g) 2.0 1.5 1.0 0.5 ** ** 14days 21days * * 7 days 14days ** ** 7 days 14days 21days ** ** * 0 Before IP 2 days 4 days 21days Fig. 2. Measurement of Left ventricular perfused capillary (A) and arteriolar density (B) and Regional Blood flow (C) in risk area. 8 non-overlapping random fields of the tissue sections after in vivo FITC conjugated BS1-lectin perfusion and anti-a smooth muscle actin staining were selected from risk area of four different left ventricular sections of each hearts (32 fields per heart, 128 fields per group, magnification of 400 × were used, n = 4). Images were captured and stored in digital tiff file format for image analysis. Counts of capillary density and arteriolar density per mm2 were obtained after superimposing a calibrated morphometric grid on each digital image using Adobe Photoshop Software. Where * p < 0.05, ** p < 0.01 compared to CMI. ["] CMI and [◆] IPMI. (C) Regional blood flow in risk area was measured with gold label neutron activation technique. Blood flow was estimated before IP, after IP, 30min, 2 , 4, 7, 14 and 21 days after permanent LAD occlusion. Differences were considered significant at p < 0.05. Where * p < 0.05, ** p < 0.01 compared to CMI. [ ] CMI and [ ] IPMI. 3.6. Evaluation of protein/DNA array and gel-shift analysis Protein/DNA array analysis revealed significant increase in the DNA binding activity of Sp1 (2.4 fold), NFjB (1.2 fold), Stat3 (1.7 fold), TFIID (1.65 fold), Pax-5 (1.2 fold) compared to the CMI group. The pro-apoptotic transcription factor AP-1 was significantly (1 fold) reduced in the IPMI group (Fig. 4) compared to the corresponding CMI. This result was again validated by the gel-shift analysis as shown in Figure 5. 3.7. Expression of VEGF after MI IP induced VEGF protein expression in IPMI group significantly when compared to the CMI group 7, 14 and 21 days after MI. The protein band density of VEGF in IPMI group increased with each time compared to the CMI group even 21 days after operation as shown in Figure 6. S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 553 Fig. 3. TUNEL assay for apoptotic cardiomyocyte (A) and endothelial cells (B). a through d, double immunofluorescence staining for a-sarcomeric actin (specific for cardiomyocyte; red fluorescence) and TUNEL-positive (green fluorescence). e through h, double immunofluorescence staining for von Willebrand factor (specific for endothelial cells; red fluorescence) and TUNEL-positive (green fluorescence). a and e, control heart 1 day of post MI; b and f, IPMI heart 1 day of post MI; c and g, control heart 7 days of post MI; d and h, IPMI heart 7 days of post MI. Data was expressed in counts/100 high power field. Bar graph shows the extent of particular cell death by apoptosis after 1, 2, 4 and 7 days of post MI. Where * p < 0.01 compared to CMI group. [ ] CMI and [ ] IPMI. 3.8. Expression of anti-apoptotic protein Bcl-2 and survivin The induction of Bcl-2 was observed in both the groups (CMI and IPMI) as shown in Figure 7 when compared to the corresponding sham operated group. However, IP upregulated anti-apoptotic protein Bcl-2 in the infarcted myocardium significantly compared to the CMI group and remained significantly stimulated even 21 days after LAD occlusion. The figure clearly demonstrated robust expression of Bcl-2 in the ischemic preconditioned myocardium 2, 4, 7, 14 and 21 days after myocardial infarction when compared to the baseline, Non-IP sham and IP sham groups. Two days after MI, in the preconditioned myocardium we found significant induction of anti-apoptotic protein survivin and the increased level was maintained up to 7 days after MI as shown in Figure 8 compared to the CMI group. However, after 7 days of post operation in the preconditioned group we found that the level of survivin was almost at the baseline (sham) level. These results suggest earlier anti-apoptotic function of survivin in the infarcted myocardium. Whereas increased Bcl-2 protein expression was maintained from day-2 till day-21 in the IPMI group compared to CMI. 3.9. Expression of c-Src after MI Western blot analysis revealed significant induction of c-Src expression (60 kDa) in CMI group right after 1day of LAD occlusion when compared to sham as well as IPMI (1day) group. The significant expression of c-Src was maintained in CMI group even after 21 days. However in IPMI group the expression of c-Src was maintained at baseline or sham control level throughout the experiment (Fig. 9A). 3.10. Myocardial water content Src-mediated vascular permeability influences the level of water content (edema) after MI. We demonstrated that suppression of c-Src by ischemic preconditioning (IPMI) as well as PP1 decreases the water content of the infarcted myocardium and thus the edema formation significantly as shown in Figure 9D compared to CMI after 24 hrs of post myocardial infarction. 4. Discussion The results of our study documented that ischemic preconditioning can possess angiogenic potential and can improve myocardial blood flow and cardiac function followed by severe ischemic myocardial injury. Therefore, myocardial adaptation to intermittent ischemia appears to be a highly promising approach to induce angiogenesis in a rat model of myocardial infarction as evidenced by increased capillary and arteriolar density. This increased micro vascular growth was found to be associated with a reduced infarct size and 554 S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 Fig. 4. Representative Protein/DNA array analysis demonstrates the activation of several transcription factors after two days of post LAD occlusion. Significant activation of Stat3, Sp1, AP-1, TFIID, Pax-5, NFjB were observed in IPMI group. Where Sham: Control+Sham; CMI: non-preconditioned followed by LAD occlusion; IPMI: ischemic precondition followed by LAD occlusion. Fig. 5. Representative gel-shift analysis demonstrates and validates Protein/DNA array result in sham, CMI and IPMI groups. Significant activation of Stat3, Sp1, TFIID, Pax-5 and NFjB transcription factors were observed in IPMI group compared to CS and CMI groups. However pro-apoptotic transcription factor AP-1 was found to be significantly reduced in IPMI group compared to CMI group. S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 555 Fig. 6. Representative Western Blots showing the effects of ischemic preconditioning followed by LAD occlusion on the expression of VEGF in rat myocardium in vivo after sham surgery, 2, 4, 7, 14, 21 days after LAD occlusion. VEGF protein was expressed as 40 kDa. Similar results were obtained in six independent experiments performed in triplicate. Densitometric scanning from Western blots was expressed as percentage mean value of the baseline control (sham). Where * p < 0.01 compared to B, † p < 0.01 compared to CMI. Fig. 7. Representative Western blots showing the effects of ischemic preconditioning followed by LAD occlusion on the expression of Bcl-2 in rat myocardium in vivo after sham surgery and after 2, 4, 7, 14 and 21 dyas of post MI. Bcl-2 was expressed as 28 kDa. Similar results were obtained in six independent experiments performed in triplicate. Densitometric scanning from Western blots was expressed as percentage mean value of the baseline control (sham). Where * p < 0.01 compared to BL, † p < 0.01 compared to CMI. 556 S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 Fig. 8. Representative Western blot showing the effect of ischemic preconditioning followed by LAD occlusion on the expression of survivin in rat myocardium in vivo after sham surgery and after 2, 4, 7, 14 and 21 days of post MI. Survivin was expressed as 16.5 kDa. Similar results were obtained in 4 independent experiments performed in triplicate. Densitometric scanning from Western blots was expressed as percentage mean value of the baseline control (sham). Where * p < 0.01 compared to BL, † p < 0.05 compared to CMI. significant preservation of contractile functional reserve. Pharmacological cardiac stress testing with dobutamine revealed differences in the extent of cardiac contractile reserve between IPMI and CMI. The ischemic preconditioned group displayed significantly elevated contractile reserve compared to CMI group. LV contractile reserve measured with dobutamine is a sensitive means of detecting differences in the extent of infarction. Dobutamine stress test is often utilized to detect the presence of hibernating myocardium in clinical chronic myocardial ischemia. Angiogenic effects of ischemic preconditioning in the functional improvements and the decreased infarct size are very general. In hibernating myocardium, the myocytes are viable, but can not contract normally because of the lack of sufficient blood supply. The presence of hibernating myocardium indicates that such a myocardial region is absent from blood supply through the major coronary arteries but is rich in collateral blood vessels as a result of enhanced angiogenesis. In our experiment, the dobutamine stress test appears to suggest the presence of larger areas of hibernating myocardium in the ischemic preconditioned heart than in non-preconditioned heart. In the present study ischemic preconditioning also triggered significant expression of VEGF and increased perfused capillary density along with increased blood flow. Based on these results, it is also reasonable to find smaller infarction in the IP heart because the presence of collateral arteries allows more myocytes to be alive after the cessation of blood supply by LAD occlusion. However, we can not ascribe all infarct sizelimiting effects of IP to angiogenesis, because direct protec- tive effects on myocytes of IP can not be eliminated. Such a direct effect may be observed early after LAD occlusion, direct effects of IP on myocytes rather than enhanced angiogenesis is a more likely mechanism for early salvage of myocardium. This may in turn improve contractile function as assessed by LV dP/dt max. Therefore, infarct size-limiting effect of IP via direct salvage of myocytes early after LAD occlusion only negligibly affected contractile performance in a chronic stage. However, when compared after dobutamine stress test, IP heart showed greater increase in LV dP/dt max than non-IP MI hearts, indicative of the presence of larger number of viable but hibernating myocytes being supplied blood flow presumably through newly developed collateral blood vessels in IP heart. The blood flow data also determined increased blood supply in the IPMI group after 2 days post-op compared to CMI group in this study, which persisted even after 21 days post-op. To explore the mechanism of this beneficial effect of intermittent ischemic preconditioning in rat myocardium in the setting of myocardial infarction we tried to explore the signal transduction pathway by studying various transcription factors and their involvement with several anti- death factors in relation to cell death. We know that various transcription factors such as AP-1 [21], SP1 [22] and NFjB [23] are known to be regulated and found to be important regulator of angiogenesis. Several studies have shown that AP-1 and NFjB are differentially activated by oxygen tension [24]. Several potential binding sites for the transcription factors AP-1, AP-2, and SP1 are localized in the VEGF gene S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 557 Fig. 9. (A) Representative Western blot analysis showing the effect of ischemic preconditioning (IP) on the expression of c-Src in rat myocardium in vivo at 1, 2, 4, 7, 14 and 21 day(s) after MI. c-Src was expressed as 60 kDa protein. (B) Effect of Src inhibition on blood flow in control with PP1. Where * p < 0.01 compared to control. (C) Effect of Src inhibition on infarct size in control with PP1. Where * p < 0.01 compared to control. (D) Effect of Src inhibition on infarct size in control with PP1. Where * p <0.01 compared to control. [ ] CMI and [ ] CMI+PP1. promoter and amongst eight glioma cell lines, cellular mRNA levels of transcription factors SP1 and AP-1 were found to be closely correlated with those of VEGF [25]. Besides redox regulated transcription factors Stat3, Pax-5 and TFIID were also found to be significantly activated (except AP-1) by Protein/DNA array analysis (Fig. 4) and latter validated by gel-shift analysis (Fig. 5) in the IPMI group after 2 days of LAD occlusion compare to control MI group. In the ischemic preconditioned group the proapoptotic transcription factor AP-1 was rightly manipulated and therefore reduced compared to CMI group. Where as activation of Stat3, in this model demonstrates significant beneficial effect of ischemic preconditioning mediated cardioprotection in the infarcted heart through the induction of anti-apoptotic gene Bcl-2 and survivin. However, significant activation of Pax-5, which is a key regulator of lineagespecific gene expression and TFIID in the setting of MI is yet to explore. Now, Angiogenesis induced by the most promising protein, VEGF has been found to be associated with enhanced cell survival in human umbilical vein endothelial cells in vitro [26,27]. It is well established that adjunctive local injection of VEGF demonstrated great promise for many patients who would not be candidates for any form of revascularization. Currently it is undergoing clinical trial both as gene therapy and direct administration of protein. In rabbits, myocardial angiogenesis has been demonstrated with both intra-arterial [28] and intra-muscular [29] injection of 558 S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 recombinant VEGF. Controlled formation of new vessels attenuating or abrogating ischemia or infarction by the administration of VEGF is supposed to be known as therapeutic angiogenesis. This constitutes a novel treatment option for the patients who are not suitable for interventions similar as PTCA or CABG. The temporal pattern of VEGF, Bcl-2 and survivin expression documented in this study at the protein level by Western blot analysis correspond to the histological evidence of angiogenesis in the rat myocardial infarction model. Our findings suggest that VEGF and Bcl-2 upregulated in response to ischemic preconditioning after 2 days of myocardial infarction and the expression of both the proteins stayed high enough significantly at the latter stage of MI (studied up to 21 days) and functioned endogenously to promote myocardial angiogenesis. Recently Kawata et al [30] have also suggested that IP elevated VEGF gene expression and angiogenesis through nuclear translocation of PKC e in the infracted myocardium. These results complement previous studies in which supplemental VEGF and Bcl-2 in vitro and in vivo have been shown to induce angiogenesis in various tissues and in cell cultures [17]. Whereas survivin another anti-apoptotic protein downstream of Bcl-2 plays a significant role in the earlier phase than the latter phase of anti-apoptotic pathways. The expression of survivin was found to be significant after 2 days of MI in the preconditioned group which increased further compared to the corresponding CMI group and slowly went down and became normal after 7 days. This result force us to speculate its role in the earlier phase to protect the myocardium rather than its role in the latter phase of myocardial infarction. It is suggested that myocardial infarction leads to persistent post-ischemic vasogenic edema which develops as a result of increased vascular permeability (VP). This promotes fluid extravasation and interstitial edema, increased interstitial pressure, collapsing of small vessels and the loss of perfusion. Hence reducing VP following MI prevent myocardial damage. Vascular leak caused by a variety of myocardial injuries including myocardial ischemia results in myocardial edema, which represents one of major complications associated with myocardial ischemia. VEGF in response to ischemic injury promotes vascular permeability (VP). Previous studies demonstrated that Src kinase regulates VEGF mediated VP in the brain following injury [20]. In our present study we have determined significant down regulation of c-Src protein expression in the IPMI heart following MI compared to CMI. Src kinase activity is known to be increased during the acute phase of preconditioning as a result of oxidative stress [29]. We presented blocked of Src by PP1 attenuated myocardial edema following MI, leading to reduced infarction and increased blood flow. Therefore, inhibition of c-Src activity in conjunction with VEGF overexpression enhances the benefit of this angiogenic growth factor while obviating its potential detrimental effect on myocardial survival and function through an increase in vascular permeability. In the other hand, VEGF stimulates angiogenesis and play an important role in prevention of apoptosis of endothelial cells through upregulation of the most recently described anti-apoptotic protein, survivin which demonstrated significant expression in the myocardium within 4 days after MI in the ischemic preconditioned group of animals. This also documents that this particular protein plays an important role in the earlier stage due to ischemic preconditioned mediated trigger of survival pathway. We found that survivin is upregulated within 4 days but it doesn’t stay upregulated for longer time period. It was almost at baseline level after 1 week of MI in the preconditioned group of animals. The most important anti-death candidate Bcl-2 expression also increased within 4 days of MI in the preconditioned group and maintained this level even after 3 weeks of MI. This observed phenomenon we think is extremely important for clinical purposes. Survivin perhaps plays a significant role in the initial phase of angiogenesis by reducing both endothelial and cardiomyocyte cell death. Whereas Bcl-2 expression by ischemic preconditioning might be extremely important throughout MI to protect from ischemic injury. Furthermore, we found that capillary as well as arteriolar densities were also significantly increased in the border zone of the ischemic myocardium. The capillary density was increased significantly and was maintained even after 3 weeks of MI compare to CMI. Whereas arteriolar density was found to be increased after a week of MI and persisted for 21 days. The extent of myocardial infarction after coronary occlusion was reduced after 2, 4,7,14 and 21 days after MI significantly and the amount of viable myocardium was found to be more abundant in IPMI group compared to the CMI as observed by cardiomyocyte and endothelial cell survival. Possible mechanisms to salvage infarcted myocardium in the IPMI group compared to CMI may be due to increased VEGF expression which increases coronary flow, opening of latent collateral vessels by its vasodilating effect, induction of vascular growth and direct cellular protection. In summary, we observed significant improvements in regional myocardial function along with increased capillary and arteriolar density following induction of survival factors VEGF, Bcl-2 and survivin (first time) in the setting of fully established chronic rat myocardial infarction model subjected to ischemic preconditioning. Again, transient suppression of Src activity within several days following MI might reduce ischemia induced heart injury and prevent long term myocardial damage without disrupting VEGF-mediated revascularization. Thus, co-administration of or sequential gene therapy with VEGF, Bcl-2 and survivin might prove beneficial to enhance myocardial collateral blood vessel function and may represent a new approach to the treatment of cardiovascular disease. Acknowledgements This study was supported by National Institutes of Health Grant HL 56803 to NM, HL69910 to NM, HL 33889 to DKD and NATO LST.CLG.979224 to NM and RK. S. Fukuda et al. / Journal of Molecular and Cellular Cardiology 36 (2004) 547–559 References [1] [2] [3] [4] [5] [6] [7] [8] [9] [10] [11] [12] [13] [14] [15] [16] Murry N, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation 1986; 74:1124–36. Das DK, Moraru II, Maulik N, Engelman RM. Gene expression during myocardial adaptation to ischemia and reperfusion. Ann NY Acad Sci 1994;723:292–307. Epstein S, Williams DO, Amsterdam EA, Miller RR. Functional significance of coronary collateral vessels in patients with acute myocardial infarction: Relation to pump performance, cardiogenic shock and survival. Am J Cardiol 1988;61:345–51. Cohen MV, Yang X-M, Neumann T, Heusch G, Downey JM. Favorable remodeling enhances recovery of regional myocardial function in the weeks after infarction in ischemically preconditioned hearts. Circulation 2000;102:579–83. Rivard A, Isner JM. Angiogenesis and vasculogenesis in treatment of cardiovascular disease. Mol Med 1998;4:429–40. Hashimoto E, Ogita T, Nakaoka T, Matsuoka R, Takao A, Kira Y. Rapid induction of vascular endothelial growth factor expression by transient ischemia in rat heart. Am J Physiol 1994;267:H1948–54. Maruyama K, Mori Y, Murasawa S, Masaki H, Takahashi N, Tsutusmi Y, Moriguchi Y, Shibazaki Y, Tanaka Y, Shibuya M, Inada M, Matsubara H, Iwasaka T. Interleukin-1 beta upregulates cardiac expression of vascular endothelial growth factor and its receptors KDA/FLK-1 via activation of protein tyrosine kinases. J Mol Cell Cardiol 1999;31:607–17. Nor JE, Christensen J, Mooney DJ, Polverini PJ. Vascular endothelial growth factor (VEGF)-mediated angiogenesis is associated with enhanced endothelial cell survival and induction of Bcl-2 expression. Am J Pathol 1999;154:375–84. Altieri DC, Marchisio C. Survivin Apoptosis :An interloper between cell death and cell proliferation in cancer. Lab Invest 1999;79:1327– 32. Reed JC. The survivin saga goes in vivo. J Clin Invest 2002;108: 965–9. Zhu L, Fukuda S, Gerald C, Das DK, Maulik N. Anti-apoptotic protein survivin plays a significant role in tubular morphogenesis of human coronary arteriolar endothelial cells by hypoxic preconditioning. FEBS Lett 2001;508:369–74. Sasaki H, Ray PS, Zhu L, Otani H, Asahara T, Maulik N. Hypoxia/Reoxygenation promotes myocardial angiogenesis via an NFjB–dependent mechanism in a rat model of chronic myocardial infarction. J Mol Cell Cardiol 2001;33:283–94. Reffelmann T, Dow JS, Dai W, Hale SL, Simkhovich BZ, Kloner RA. Transplantation of neonatal cardiomyocytes after permanent coronary artery occlusion increase regional blood flow of infracted myocardium. J Mol Cell Cardiol 2003;35:607–13. Reinhardt CP, Dalhberg S, Tries MA, Marcel R, Leppo JA. Stable labeled microspheres to measure perfusion: validation of a neutron activation assay technique. Am J Physiol 2001;280:H108–16. Kajstura J, Cheng W, Reiss K, Clark WA, Sonnenblick EH, Krajewski S, Reed JC, Olivett G, Anversa P. Apoptotic and necrotic myocyte cell deaths are independent contributing variables of infarct size in rats. Lab Invest 1996;74:86–107. Maulik N, Yoshida T, Zu Y-L, Sato M, Banerjee A, Das DK. Ischemic preconditioning triggers tyrosine kinase signaling: a potential role for MAPKAP kinase 2. Am J Physiol 1998;275:H1857–64. 559 [17] Gerber HP, McMurtrey A, Kowalski J, Yan M, Keyt BA, Dixit V, Ferrara N. Vascular endothelial growth factor regulates cell survival through the phosphatidylinositol 3′-Kinase/Akt signal transduction pathway. J Biol Chem 1998;273(46):33036–43. [18] Maulik N, Sato M, Price BD, Das DK. An essential role of NFjB in tyrosine kinase signaling of p38 MAP kinase regulation of myocardial adaptation to ischemia. FEBS Lett 1998;429:365–9. [19] Sasaki H, Fukuda S, Otani H, Zhu L, Yamaura G, Engelman RM, Das DK, Maulik N. Hypoxic preconditioning triggers myocardial angiogenesis: a novel approach to enhance contractile functional reserve in rat with myocardial infarction. J Mol Cell Cardiol 2002;34: 335–48. [20] Paul R, Zhang ZG, Eliceiri BP, Jiang Q, Boccia AD, Zhang RL, Chopp M, Cheresh DA. Src deficiency or blockade of Src activity in mice provides cerebral protection following stroke. Nature Med 2001; 7(2):222–7. [21] Starr JP, Jia CX, Armirhamzeh MM, Rabkin DG, Hart JP, Hsu DT, Fisher PE, Szabolcs M, Spotnitz HM. Coronary perfusate composition influences diastolic properties, myocardial water content, and histologic characteristics of the rat left ventricle. Ann Thorac Surg 1999;68(3):925–30. [22] Bandyopadhyay RS, Phelan M, Faller DV. Hypoxia induces AP-1 regulated genes and AP-1 transcription factor binding in human endothelial and other cell types. Biochem Biophys 1995;1264:72–8. [23] Yao KS, Xanthoudakis S, Curran T, O’Dwyer PJ. Involvement of NFjB in the induction of NAD(P)H quinone oxidoreductase by hypoxia, oltipraz and mitomycin C. Biochem Pharmacol 1995;49: 275–82. [24] Maulik N, Sasaki H, Addya S, das DK. Regulation of cardiomyocyte apoptosis by redox-sensitive transcription factors. FEBS Letters 2000;485:7–12. [25] Ryuto M, Ono M, Izumi H, Yoshida S, Weich HA, Kohno K, Kuwano M. Induction of vascular endothelial growth factor by tumor necrosis factor in human glioma cells. J Biol Chem 1996;271: 28220–8; Shweiki D, Itin A, Soffer D, Keshet E. Vascular endothelial growth factor induced by hypoxia may mediate hypoxia-initiated angiogenesis. Nature 1992;359:843–5. [26] Alon T, Hemo I, Itin A, Pe’er J, Stone J, Keshet E. Vascular endothelial growth factor acts as a survival factor for newly formed retinal vessels and has implications for retinopathy of prematuarity. Nat Med 1995; 1:1024–8. [27] Bauters C, Asahara T, Zheng LP, Takeshita S, Bunting S, Ferrara N, Symes JF, Isner JM. Site specific therapeutic angiogenesis after systemic administration of vascular endothelial growth factor. J Vasc Surg 1995;21:314–25. [28] Takeshita S, Pu LQ, Stein LA, Sniderman AD, Bunting S, Ferrara N, Isner JM, Symes JF. Intramuscular administration of vascular endothelial growth factor dose dependent collateral artery augmentation in a rat model of chronic limb ischemia. Circulation 1994;90:228–34. [29] Nakashima I, Kato M, Akhand AA, Suzuki H, Takeda K, Hossain K, Kawamoto Y. Redox-linked signal transduction pathways for protein tyrosine kinase activation. Antioxid Redox Signal 2002(3):517–31. [30] Kawata H, Yoshida K-I, Kawamoto A, Kurioka H, Takase E, Sasaki Y, Hatanaka K, Kobayashi M, Ueyama T, Hashimoto T, Dohi K. Ischemic preconditioning upregulates vascular endothelial growth factor mRNA expression and neovascularization via nuclear traslocation of protein kinase C e in the rat ischemic myocardium. Circ Res 2001;88:696–704.
© Copyright 2026