Insulin-like growth factor-II delays myocardial infarction in experimental coronary artery occlusion ´
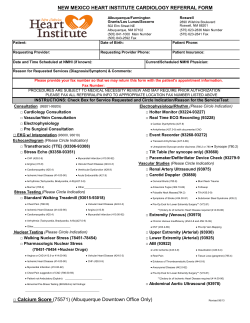
Cardiovascular Research 33 Ž1997. 469–477 Insulin-like growth factor-II delays myocardial infarction in experimental coronary artery occlusion Achim M. Vogt, Patrik Htun, Angelika Kluge, Rene´ Zimmermann, Wolfgang Schaper ) Max Planck Institute for Physiological and Clinical Research, (W.G. Kerckhoff Institute), Department of Experimental Cardiology, Benekestrasse 2, D-61231 Bad Nauheim, Germany Received 24 June 1996; accepted 26 September 1996 Objective: We have previously shown that short pulses of myocardial ischemia cause increased mRNA expression of the insulin-like growth factor II ŽIGF-II. gene. The expression of IGF-II precedes the expression of its binding protein 5 ŽIGFBP-5.. The cardioprotective actions of the IGF-II peptide and of its binding protein 5 as well as the underlying mechanisms were investigated in this study. Methods and results: Human recombinant IGF-II Ž0.25 mgrml. was applied by means of direct intramyocardial infusion ŽIM. for 60 min prior to a 60 min LAD occlusion and 120 min reperfusion. Myocardial infarction, compared to the region at risk, was significantly decreased by IGF-II treatment, whereas infusion of Krebs-Henseleit buffer did not show any protective effect ŽIGF-II, 78.75 " 1.51%; control, 100%; P - 0.005.. A comparable degree of cardioprotection was observed after infusion of an equipotent concentration of recombinant human insulin Ž0.02 IUrml; 88.25 " 1.45%; P - 0.05.. Lavendustin A Ž100 mM., an inhibitor of protein tyrosine kinases, prevented the observed cardioprotection. The protective effect of IGF-II was lost when IGFBP-5 was simultaneously infused. Conclusion: IGF-II, a peptide that binds to the insulin receptor and whose mRNA is rapidly transcribed by cardiac myocytes following ischemic stress, is cardioprotective and mimics ischemic preconditioning. Its observed actions are probably based on its metabolic effects and are mediated by the insulin or the IGF-I receptor. IGFBP-5, whose expression follows IGF-II’s expression with a short delay, inhibits the cardioprotection afforded by IGF-II and may thus account for the limited temporal duration of ischemic preconditioning. Keywords: Insulin-like growth factor II; Insulin; Myocardial protection; Preconditioning; Myocardial infarction 1. Introduction Repetitive coronary occlusions of short duration render the heart resistant against a subsequent long period of ischemia. This experimental intervention, termed ‘ischemic preconditioning’ w1x, is the most powerful protection against myocardial infarction for the in situ beating heart. Previous work from our laboratory had demonstrated significant changes in myocardial gene expression in myocardium subjected to ischemic preconditioning w2x. Amongst other genes, insulin-like growth factor II ŽIGF-II. and insulin-like growth factor binding protein 5 ŽIGFBP-5. w3x were upregulated by ischemiarreperfusion but also by surgical stress. The insulin-rinsulin-like growth factor system is an endocrinerparacrine physiologic system controlling metabolism, growth, differentiation, and the response to stress ŽFig. 1. w4,5x. Recent observations in neuronal models suggest trophic and protective actions of the IGFs in the setting of ischemia and reperfusion w1,6–9x. Like adult myocytes, neurons are terminally differentiated cells that exhibit pathways of endogenous protection similar to ischemic preconditioning in the heart w10–14x. In skeletal muscle, it was demonstrated that the IGFs stimulate glucose uptake by their insulin-like activity w15,16x. It is therefore tempting to speculate that in times of metabolic stress, as in ischemia, the heart expresses ‘its own insulin’ by making use of the metabolic properties of IGF-II. Since the expression of IGF-II is followed by the expression of one of its binding proteins which terminates its action, we hypothesize that ischemic preconditioning can, at least in part, be explained on the basis of changes of the IGF tissue concentration. ) Corresponding author. Tel. q49 6032 705-402; Fax q49 6032 705-419. Time for primary review 21 days. 0008-6363r97r$17.00 Copyright q 1997 Elsevier Science B.V. All rights reserved. PII S 0 0 0 8 - 6 3 6 3 Ž 9 6 . 0 0 2 1 2 - X Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 Abstract 470 A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 2. Methods The experimental protocol described in this study was approved by the Bioethical Committee of the District of Darmstadt, Germany. Furthermore, all animals in this study were handled in accordance with the guiding principles in care and use of animals as approved by the American Physiological Society and the investigation conformed with the Guide for Care and Use of Laboratory Animals published by the US National Institutes of Health. 2.1. Animal preparation Sixteen castrated male German landrace-type domestic pigs with body weights between 27.5 and 35.5 kg Ž32.6 " 0.22 kg. were premedicated with 2 mg P kgy1 BW i.m. azaperone ŽStresnil, Janssen Pharmaceutica, Neuss, Germany. and 2 mg P kgy1 BW s.c. piritramid ŽDipidolor, Janssen Pharmaceutica, Neuss, Germany. 30 min prior to the initiation of the anesthesia with 10 mg P kgy1 BW metomidate ŽHypnodil, Janssen Pharmaceutica, Neuss, Germany.. After either oral or endotracheal intubation, a bolus of 25 mg P kgy1 BW of a-chloralose ŽSigma, Deisenhofen, Germany. was given intravenously. Anesthe- sia was maintained by a continuous intravenous infusion of 25 mg P kgy1 BW P hy1 a-chloralose. The animals were ventilated artificially with a pressure-controlled respirator ŽStephan Respirator ABV, F. Stephan GmbH, Quickborn, Germany. with room air enriched with 2 l P miny1 oxygen. Arterial blood gases were analyzed frequently to guide adjustment of the respirator settings. Additional doses of piritramid Ž10 mg. were given i.v. every 60 min. Both internal jugular veins were cannulated with polyethylene tubes for administration of saline, piritramid and a-chloralose. Arterial sheath catheters Ž7F. were inserted into both common carotid arteries. To measure aortic blood pressure, the left sheath was advanced into the aortic arch and connected with a Statham transducer ŽP23XL, Statham, Puerto Rico.. A 5F high-fidelity catheter-tipped manometer ŽMillar Instruments, Houston, TX, USA. was inserted via the right common carotid artery into the left ventricle to measure left ventricular pressure and to calculate its first derivative ŽLV dPrdt.. The chest was opened by a midsternal thoracotomy and the heart was suspended in a pericardial cradle. A loose silk ligature was placed halfway around the left anterior descending coronary artery ŽLAD., and was subsequently tightened to occlude the vessel. After preparation, a stabilization period of 20 min was allowed and the different experimental protocols were started. Index ischemia was a 60 min LAD occlusion followed by 120 min reperfusion. If ventricular fibrillation occurred, a defibrillator with paddles placed onto the external chest wall was used for conversion. Data from DC-amplifiers including surface ECG ŽHeinemann, FrankfurtrMain, Germany. were digitized by an analog-digital converter ŽMacLabr8, AD Instruments Pty Ltd., Castle Hill, Australia. and continuously recorded onto the hard disc of a personal computer ŽPower Book 180, Apple Computer Inc., Cupertino, CA, USA.. Body temperature was maintained within the physiological range by thermal isolation of the animals. Of the 16 animals investigated, 5 experienced ventricular fibrillation during LAD occlusion and were successfully defibrillated. To avoid the side-effects of systemic injections of either IGF-II or insulin on systemic glucose metabolism w22x we treated the myocardium of interest only locally by intramyocardial infusion as described in detail previously w23,24x. Eight 26-gauge needles with a free length of 5 mm that were connected by tubing with a peristaltic pump ŽMinipuls, Gilson, Germany. were placed in pairs into the subsequently ischemic myocardium perpendicular to the epicardial surface. The substances were infused at 20 mlrminrneedle, amounts far below those causing distension of the myocardium. 2.2. Experimental groups The experimental design is demonstrated in Fig. 2. Five groups of animals were studied Žin a sixth group of animals a different design and methodology was used.. Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 Since the appearance of protein may follow the increased mRNA content with only a short delay w17x, the aim of the present study was to investigate whether the increased expressions of IGF-II and its binding protein 5 may be operative in increasing myocardial resistance against infarction. To test its cardioprotective actions, human recombinant IGF-II was directly infused into porcine myocardium prior to coronary occlusion and reperfusion normally causing myocardial infarction. To further elucidate the underlying mechanism, an equipotent dose concerning IGF-II’s metabolic effects of recombinant human insulin was tested in a second group. The receptors involved were further characterized by simultaneous infusion of lavendustin A to block the protein tyrosine kinase domain of either the IGF-I or the insulin receptor w18,19x. There is very little knowledge available yet about the physiologic functions of the IGF-binding proteins. Recent investigations have demonstrated that the physiologic actions of the IGFs Ži.e., cellular glucose uptake. can be inhibited by their binding proteins w16,20x. In our porcine model of repeated short coronary occlusions, the expression of IGFBP-5 follows the expression of IGF-II with a short delay w1,3x. Due to the good correlations of the time courses of the appearance of IGFBP-5 mRNA and the vanishing protection of ischemic preconditioning w21x we hypothesized that the increased content of IGFBP-5 with prolonged reperfusion periods will inhibit IGF-II’s cardioprotective actions. Possible interference of the expression of IGFBP-5 was investigated by a simultaneous infusion of IGFBP-5 with IGF-II prior to ischemia and reperfusion. A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 471 Fig. 2. Experimental groups. Six experimental groups were investigated. After stabilization Ž20 min., groups 1 to 3 consisted of animals receiving microinfusions of Krebs-Henseleit buffer, IGF-II, or insulin respectively. The animals of groups 4 and 5 were treated with simultaneous infusions of IGF-IIrinsulin and lavendustin A. Group 6 was subjected to microinfusions of IGF-II and IGFBP-5. In all animals, index ischemia causing myocardial infarction was 1 h LAD occlusion followed by 2 h of reperfusion. Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 Fig. 1. Signal transduction pathway of the insulinrIGF system. Insulin, IGF-I and IGF-II bind to their own receptors with high Žbold arrows. and to the other receptors with lower Žthin arrows. affinity. Insulin does not bind to the IGF-II receptor. The insulin and the IGF-I receptor are homodimers consisting of extracellular Ž a ., transmembrane and intracellular domains Žb .. The intracellular domains have protein tyrosine kinase activity that can be blocked with lavendustin A. In general, the insulin receptor mediates metabolic effects whereas anabolic and proliferative effects are transmitted by the IGF-I receptor. The IGF-II receptor that was not detectable in cardiac tissue by Northern blot analysis w3x is a G-protein-coupled receptor. Its exact function remains to be elucidated. 472 A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 2.3. Exclusion criteria Perfusion sites were excluded from evaluation if systolic-diastolic cardiac movements caused dislocation of microinfusion needles or if protected areas were not totally surrounded by pNBT-negative, necrotic tissue. Successful DC countershock treatment of ventricular fibrillation was not a criterion for exclusion. Since intramyocardial infusion was finished before the onset of index ischemia, a possible dislocation of the microinfusion needles at this time point could not interfere with the result and was hence not an exclusion criterion. 2.4. Measurement of infarct size At the end of the experimental protocol, the left anterior descending coronary artery was occluded again and 1 g fluorescein-sodium ŽFluka, Neu-Ulm, Germany, dissolved in 10 ml saline. was injected as a bolus intravenously. After the overall distribution of the dye the animals were sacrificed with an intravenous bolus of 20% potassium chloride Ž30 ml. to achieve cardiac arrest. The heart was excised and both atria and the right ventricle were removed. The left ventricle was cut into slices along the pairwise inserted microinfusion needles perpendicular to the LAD. After weighing the slices, the ischemic area was identified as the non-fluorescent area by blacklight examination. The infarcted area was demarcated using p-nitroblue-tetrazolium ŽpNBT. staining. The results of the stainings were documented on transparency film for further planimetric evaluation. Due to the onset of rigor mortis the heart slices sometimes shrink between drawing of the fluorescein outlines and the tetrazolium incubation, which makes it sometimes difficult to match the outlines of the risk region with that of the infarct. Since the fluorescein leaks out during incubation, it is impossible to determine the risk region and the infarct size after the tetrazolium bath. We have therefore replaced in some animals the fluorescein method with fluorescent microspheres that do not leak out during incubation. The color transparencies of the risk region and of the infarcts were scanned into an Apple Quadra computer and a composite image was created using ‘Photoshop’ graphics software. 2.5. Planimetry and quantification of myocardial protection Since only a fraction of the ischemic myocardium was reached by the infused substances, quantification of myocardial protection was done as follows: Myocardial infarcts in the pig after 60 min coronary occlusion and 120 min reperfusion are homogenous and transmural. Fig. 3 demonstrates that the substances were infused into a region that, according to our experience, becomes necrotic afterwards. Intramyocardial infusions of fluorescein sodium Ždone in several animals. helped us to identify the perfused myocardial areas, as determined by blacklight examination. PNBT-positive Žviable. myocardial areas in the tissue close to the needles Ž3b., totally surrounded by pNBT-negative Žnecrotic. tissue, were regarded as myocardial areas protected by intramyocardial infusion. Description and statistical evaluation of myocardial protection was done in two ways as follows. Using a nominal scale, evaluation was done by differentiating between the infusion sites showing ‘protection’ and ‘no protection’. These results are shown in Table 1. The other method consisted of comparing the infarcted areas by planimetry: The border zones between ischemic and nonischemic myocardium were not reached by our microinfusion technique, as determined by dye infusions Ž3a.. Thus, we made sure that the outline of the infarct remained unaffected by the active compounds. In this way, every myocardial slice planimetred served as its own control: Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 In all animals index ischemia was a 60 min LAD occlusion followed by 120 min reperfusion. The control group Ž1. consisted of animals receiving intramyocardial infusions of Krebs-Henseleit buffer for 60 min prior to index ischemia. In group 2, recombinant human IGF-II Ž250 ngrml, Biomol, Hamburg, Germany. was infused for 60 min. The animals of group 3 received infusions of recombinant human insulin Ž0.02 IUrml, H-insulin Hoechst w , Hoechst AG, Frankfurt, Germany. in an equipotent concentration with regard to IGF-II’s metabolic effects. In groups 4 and 5, either IGF-II or insulin were co-infused with lavendustin A Ž100 mM., a potent and selective inhibitor of protein tyrosine kinases w25x. To make sure that protein tyrosine kinases were inhibited at the onset of IGF-IIrinsulin infusion, lavendustin A was infused alone 30 min before adding the other substances. To test the expected inhibitory action of IGFBP-5, the animals of group 6 received co-infusions of IGF-II and recombinant human IGFBP-5 ŽAustral Biologicals, San Ramon, CA, USA. in equimolar concentrations. The concentrations used were determined in previous pilot experiments. Concerning IGF-II’s cardioprotective actions, a dose–response testing indicated no protection at the concentrations of 2.5 and 25 ngrml. At 50 ngrml, a small, inconstant effect was observed whereas 250 ngrml showed reproducible, marked protective effects. IGF-II stimulates metabolic insulin effects with a potency of about 25% of the action of insulin itself w15,26x. For this reason we have chosen the insulin concentration as described above Ži.e., 25% of IGF-II’s molar concentration.. IGFBP-5, a protein showing two bands at 31 and 32 kD in SDS-PAGE w27x, was tested in concentrations of 50, 100 and 200% relative to IGF-II’s molar concentration. The cardioprotective effect of IGF-II was inhibited at equimolar concentrations and when IGFBP-5 was co-infused. Since IGFBP-5 shows no affinity to insulin w28x, this experimental situation was not tested. A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 473 previously described w3,29,30x. Quantification and referencing of the Northern signal were carried out by PhosphorImager as previously described w3,29,30x. 2.7. Statistical analysis All data are given as mean values with standard error of mean. Statistical comparisons between groups were done by ANOVA ŽScheffe´ test. unless mentioned otherwise. A P-value smaller than 0.05 was considered statistically significant. 3. Results 3.1. Hemodynamic data Fig. 4 shows the hemodynamic data recorded throughout the experiments. Compared to baseline values Ž t s 0 min., intramyocardial microinfusion for 60 min did not affect systemic hemodynamics. The time course of hemodynamics during ischemia and reperfusion follows the First, we determined the infarcted area that would have occurred without protection Ži.e., the total area of the transmural infarction.. This area was set as 100%. In the second step, we determined the infarcted area Žtransmural area minus protected myocardial area. and related this value to the area obtained in step one. Per animal and substance, one mean ratio Žin percent risk region. was determined and subjected to further statistical evaluation. 2.6. RNA isolation and Northern hybridization Six additional animals were anesthetized, intubated and artificially ventilated as described. In 3 animals a PTCA catheter was advanced into the left anterior descending coronary artery that was occluded by balloon inflation for 10 min. Catheter inflation was performed at pressures that occluded but did not stretch the arteries. Occlusion was checked by fluoroscopy and contrast medium injection. The catheter was thereafter deflated and withdrawn for 30 min and again advanced under fluoroscopic guidance into the LAD for another round of 10 min occlusion and 30 min of reperfusion. Thereafter the animal was sacrificed by an overdose of the anesthetic plus a bolus of concentrated KCl. The heart was removed and quickly dissected into the ischemic-reperfused LAD region and the normal left ventricle. In 3 other pigs only the arterial cutdown was performed and the hearts were removed after 80 min of anesthesia, an identical amount of contrast medium injection and after sacrifice with nembutal and KCl. These hearts served as controls; they were dissected in an identical way to that of the PTCA hearts. RNA extraction, electrophoresis and cDNA probe fashioning were done according to standard protocols and as Fig. 4. Hemodynamic data. Systemic hemodynmic data from all experiments shown as mean"standard error of mean. Minutes y30 to 60: intramyocardial microinfusion. Minutes 61 to 120: LAD occlusion. Minutes 121 to 240: reperfusion. LVP s left ventricular pressure; AOP s aortic pressure; dPrdt s first derivative of left ventricular pressure; s s systolic; d s diastolic; HR s heart rate. Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 Fig. 3. Intramyocardial microinfusion. The microinfusion needles were placed in pairs into the LAD territory that will become ischemic afterwards Ž3a.. Tissue distribution Žas determined by dye infusions. indicated by dark areas. After pNBT staining to detect myocardial infarction Žlower row., myocardial protection was seen by pNBT-positive, viable tissue surrounding the needles Žstriped areas in 3b. which did not occur if the infused substances were without protective effect. Myocardial protection was expressed by relating the actual infarcted area Žwhite area in 3b, left. to the infarcted area that would have become necrotic assuming transmural infarction Žwhite area in 3b, right.. 474 A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 Fig. 5. Areas at risk. Bar graph showing constant areas at risk Žischemic areas. in the different experimental groups. 3.2. Myocardial protection Table 1 demonstrates myocardial protection achieved in the different experimental groups. Statistical analysis of the data by contingency table analysis shows that the P-value would be ) 0.001 in the case of one dropout Ži.e., a change in the wrong direction.. Since we had no dropouts, the P-value would be even smaller. IGF-II as well as insulin displayed cardioprotection at every infusion site investigated Ž n s 16. in 4 animals. These effects were inhibited by the simultaneous infusion of lavendustin A, an inhibitor of protein tyrosine kinases, blocking the signal transduction of IGF-II and insulin at the receptor level. Likewise, simultaneous infusion of IGFBP-5 in all experiments prevented protection by IGF-II. Fig. 6. Infarct size. Infarct size expressed as percentage of control, transmural infarction. Open symbols represent single experiments; mean values with standard errors of mean are given by filled symbols. C s control; IGF s IGF-II microinfusions; INS s insulin; LAV A s lavendustin A; BP 5 s IGFBP-5. Significances between the experimental groups are given by the symbols $, %, and a ŽANOVA.. Fig. 7. Infarct imaging. Representative experiment showing the salvaging influence of intramyocardial infusion. The non-ischemic region is in red with light dots from the microsphere injection with the LAD re-closed at the end of the experiment. Infarcted tissue is yellow green and ischemic tissue surrounding the 2 infusion needles is dark blue–magenta. Fig. 8. IGF-II mRNA expression in closed-chest pigs. Northern hybridization of blotted RNA obtained from normal and ischemic preconditioned regions Žocclusions by balloon catheter. that were probed with an IGF-II cDNA probe. Two experiments are shown with strong expression of the 2.8 and 6 kb bands typical of ischemia. The induction was 3.5-fold and 5-fold above control. Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 pattern as previously described w31x and is not shown here in detail. A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 Table 1 Myocardial protection in the different experimental groups using a nominal scale Group Protection Yes No Control IGF INS IGFqLAV INSqLAV IGFqBP5 0 16r4 16r4 0 0 0 16r4 0 0 16r4 16r4 16r4 The first number indicates the slices evaluated, the second number the animals investigated. For further explanation, see text. 3.3. IGF-II expression IGF-II mRNA is 4-fold overexpressed following coronary occlusion by balloon inflation in two animals Žsee Fig. 8.. The third balloon-occluded animal died of ventricular fibrillation. The data of 2 control animals are not shown because no increased IGF mRNA expression was noted. In 1 control animal the RNA was degraded. No statistical analysis was attempted because of the small number of animals and the large differences in mRNA expression between balloon-occluded and control tissue. 4. Discussion In a previous paper w3x we described increased and very fast IGF-II mRNA expression following repeated brief ischemia under open-chest conditions in the pig. Since the expression of the IGF binding protein 5, which interferes with the action of IGF-II, was also upregulated, albeit with a phase lag of about 30 min, we hypothesized that the protection caused by ischemic preconditioning can also be explained by the action of the IGF system where protection is initiated by IGF-II and terminated by IGFBP-5. Since this hypothesis cannot be proven by mRNA data alone and since available antibodies directed at human recombinant IGF-II do not cross-react with the porcine homolog, we tested this idea by direct intramyocardial infusion of the peptides involved. Our results show that indeed IGF-II delays the progression of an experimental infarct just like ischemic preconditioning and IGFBP-5 neutralizes this effect. We show further that the protective effect is mediated via the insulin receptor which belongs to the tyrosine kinase class of receptors and that the effect can be neutralized by the tyrosine kinase inhibitor lavendustin. IGF-II binds either to the IGF-I receptor, the IGF-IIrmannose 6-phosphate or to the insulin receptor and has hence either a mitogenic or a metabolic effect. Our results suggest that the cardioprotection is based on the metabolic effects of IGF-II because: Ø insulin itself produced a similar degree of protection, Ø insulin does not bind to the IGF-II and only weakly to the IGF-I receptor, Ø neither the IGF-I nor the IGF-II receptor produces a metabolic effect w5,32x and Ø the IGF-II receptor is not expressed under the experimental conditions that we have created w33x, which is compatible with the low number of IGF-II receptors reported for the adult heart w1,34x. The mRNAs of the insulin and the IGF-I receptor, on the other hand, are abundantly expressed in porcine heart. To the best of our knowledge, this is the first report describing cardioprotection by one of the insulin-like growth factors. In contrast to the heart, the role of the IGF’s is better investigated in neuronal models. Recent investigations reported a beneficial role for the IGF’s in brain ischemia w6,9x, and the effect was also produced by its metabolic effects w6,7x. In the heart, influencing glucose metabolism has been shown to be beneficial in ischemiarreperfusion settings w35–37x and our preliminary experiments with positron emission tomography Žtogether with Schwaiger, unpublished. showed increased focal glucose uptake after intramyocardial IGF-II infusion, from which we conclude that this was one of the underlying mechanisms responsible for the increased ischemia resistance of the myocardium w15,16x. Interestingly, increased myocardial glucose uptake is a characteristic feature also of ‘hibernating myocardium’ w1,38x to protect itself from sustained ischemic stress w39x. Thus, the increased mRNA content for IGF-II may be interpreted to take place as a self-defense mechanism of myocardium subjected to repeated episodes of ischemia. Thereby the heart circumvents its inability to synthesize insulin itself. Instead, it increases its production of insulin-like growth factor II, ‘the heart’s own insulin’, to increase its tolerance against subsequent ischemic episodes. Since IGF-II mRNA is markedly overexpressed in preconditioned porcine myocardium and IGF-II peptide was demonstrated to be protective in the setting of cardiac ischemia and reperfusion, an involvement of IGF-II in preconditioning’s cardioprotection appears likely since the translation of small-peptide hormones may happen quickly, even in ischemia w17x. The delay that is necessary for ischemic preconditioning to become manifest may correspond to the time necessary to translate IGF-II mRNA. Although recent reports in the rabbit suggest ischemic preconditioning to be independent of de noÕo protein synthesis w40x, the conclusion rested on the assumption that the dose of cycloheximide was sufficient to inhibit global protein synthesis. This may not apply to small peptides like the IGFs. The 30 min delay with which IGFBP-5 mRNA expression follows the expression of IGF-II w3x could explain why the memory effect of ischemic precon- Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 Fig. 5 demonstrates that the data for areas at risk did not differ significantly in the groups investigated. The conventional way of expressing infarct size is shown in Fig. 6. An example of infarct imaging is given in Fig. 7. 475 476 A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 inhibits the cardioprotection afforded by IGF-II and thereby possibly accounts for the limited protective time frame of ischemic preconditioning. IGF-II and adenosine cooperate by increasing the glucose uptake in ischemic-reperfused myocardium and they may act via translocation of the glucose transporter. 4.1. Limitations of the study The method of direct infusion of tool drugs into the myocardium was developed for the study of focal arrhythmias w46x. We show here and in a previous paper w24x that it is also useful for the application of hormones that act mainly locally and that cannot be applied systemically in large animals due to cost and to serious side-effects. The disadvantage of the method is that the concentration of the hormone at some distance from the infusion needle is not known. With continuous infusion the gradients of concentration will decrease, but the final space of distribution remains unknown. Experiments with dyes showed that at a rate of infusion of 20 mlrmin a volume of approximately 1 cm3 is reached within 10 min. Longer infusion times increase the volume of distribution, but we do not at present know where the saturation point is. References w1x Murry CE, Jennings RB, Reimer KA. Preconditioning with ischemia: a delay of lethal cell injury in ischemic myocardium. Circulation 1986;74:1124–1136. w2x Schaper W, Zimmermann R, Kluge A, et al. Patterns of myocardial gene expression after cycles of brief coronary occlusion and reperfusion. Ann NY Acad Sci 1994;723:284–291. w3x Kluge A, Zimmermann R, Munkel B, Verdouw P, Schaper J, ¨ Schaper W. Insulin-like growth factor II is an experimental stress inducible gene in a porcine model of brief coronary occlusions. Cardiovasc Res 1995;29:708–716. w4x Cochik WS, Clemmons DR. The insulin-like growth factors. Annu Rev Physiol 1993;55:131–153. w5x Sara VR, Hall K. Insulin-like growth factors and their binding proteins. Physiol Rev 1990;70:591–614. w6x Zhu CZ, Auer RN. Intraventricular administration of insulin and IGF-1 in transient forebrain ischemia. J Cereb Blood Flow Metab 1994;14:237–242. w7x Zhu CZ, Auer RN. Centrally administered insulin and IGF-1 in transient forebrain ischemia in fasted rats. Neurol Res 1994;16:116– 120. w8x Strong AJ, Fairfield JE, Monteiro E, et al. Insulin protects cognitive function in experimental stroke. J Neurol Neurosurg Psychiatry 1990;53:847–53. w9x Hamilton MG, Tranmer BI, Auer RN. Insulin reduction of cerebral infarction due to transient focal ischemia. J Neurosurg 1995;82:262– 268. w10x Aoki M, Abe K, Kawagoe J, Nakamura S, Kogure K. The preconditioned hippocampus accelerated HSP70 heat shock gene expression following transient ischemia in the gerbil. Neurosci Lett 1993;155:7–10. w11x Aoki M, Abe K, Kawagoe J, Nakamura S, Kogure K. Acceleration of HSP70 and HSC70 heat shock gene expression following transient ischemia in the preconditioned gerbil hippocampus. J Cereb Blood Flow Metab 1993;13:781–788. Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 ditioning Ži.e., the fact that it ‘remembers’ short occlusions. is ‘forgotten’ after less than 1 hour following the last conditioning short occlusion and that cardioprotection is no longer present after that time w21x. By extending the time period after the repetitive coronary occlusions the increase in IGFBP-5 content will terminate preconditioning’s cardioprotection: i.e., the protection observed is the resultant of the myocardial content of IGF-II Žprotective. and IGFBP-5 Žinhibitory.. This proposed mechanism explains the observation that in our porcine model ischemic preconditioning is not yet optimal when shorter protocols of repetitive coronary occlusions w41x are used Ž2 occlusions of 10 min or 4 occlusions of 5 min are needed for protection, but only the first produced significant amounts of adenosine. in contrast to other species w24,42x. This would suggest that the adenosine hypothesis in the porcine heart can only partially explain the protective effect of short occlusions and that an additional factor has to be assumed. This is most likely the IGF system: the multiple occlusions needed for protection in our model produce the necessary amounts of IGF-II. The functional synergism between adenosine and insulin with regard to glucose uptake that is stimulated by both agents is indeed very helpful for cytoprotection w43,44x. Although it was shown that neither insulin nor adenosine increase glucose uptake during prolonged ischemia, the reperfusion periods in between brief occlusions may stimulate glucose uptake. Other properties of IGF-II-like inhibition of protein breakdown and preservation of translation may add to the cytoprotective profile of the hormone w45x. One argument encountered during the review of our previous paper was that the upregulation of IGF-II mRNA expression may not be specific for ischemia but may also have been caused by the surgical stress of the open-chest situation, because a statistically non-significant trend seemed to indicate that. Furthermore, there was no difference in IGF-mRNA between ischemic-reperfused and adjacent non-ischemic myocardium. This argument can now be placed into proper perspective with our new data that show upregulation of IGF-II mRNA expression in a closed-chest model only with ischemia and in the ischemic region Žsee Fig. 8.. We conclude from these and from the previous findings that both surgical stress and ischemia proper are able to upregulate IGF-II mRNA. On the basis of mRNA data alone it cannot be inferred that IGF-II may have a protective effect because it could have been an epiphenomenon related to stress. However, our direct infusion studies show clearly the protective potency of the hormone. In summary, our data describe a cardioprotective effect of IGF-II, a tissue hormone with insulin-like actions whose mRNA is 4- to 5-fold overexpressed in preconditioned myocardium. The cardioprotection caused by IGF-II is mediated via the insulin receptor. IGFBP-5, whose expression follows the expression of IGF with a short delay, A.M. Vogt et al.r CardioÕascular Research 33 (1997) 469–477 w29x Kluge A, Zimmermann R, Munkel B, et al. Insulin-Like Growth ¨ Factor II ŽIGF-II. ist ein Stress-Gen und ein trophischer Faktor im Herzmuskel des Schweines. Z Kardiol 1993;82ŽSuppl 1.:521ŽAbstract.. w30x Kluge A, Zimmermann R, Munkel B, Verdouw PD, Schaper J, ¨ Schaper W. Localization of insulin-like growth factor II ŽIGF-II., a stress-response gene, in ischemic porcine heart. J Mol Cell Cardiol 1993;25Žsuppl I.:III-P-4ŽAbstract.. w31x Schott RJ, Rohmann S, Braun ER, Schaper W. Ischemic preconditioning reduces infarct size in swine myocardium. Circ Res 1990;66:1133-1142. w32x Kornfeld S. Structure and function of the mannose 6-phosphaterinsulin like growth factor II receptors. Annu Rev Biochem 1992;61:307–330. w33x Kluge A, Zimmermann R, Weihrauch D, et al. Coordinate expression of the insulin-like growth factor system after microembolisation in porcine heart. Cardiovasc Res 1996;in press. w34x Roth RA, Kiess W. Insulin-like growth factor: recent developments and new methodologies. Growth Regul 1994;1:31–38. w35x Apstein C, Gravino F, Haudenschild C. Determinants of a protective effect of glucose and insulin on the ischemic myocardium. Circ Res 1983;52:515–526. w36x Opie L, Bruyneel K, Owen P. Effects of glucose, insulin and potassium infusion on tissue metabolic changes within first hour of myocardial infarction in baboon. Circulation 1975;52:49–57. w37x Maroko PR, Kjekshus JK, Sobel BE, et al. Factors influencing infarct size following experimental coronary artery occlusion. Circulation 1971;43:67–82. w38x Rahimtoola SH. Chronic myocardial hibernation. Circulation 1994;89:1907. w39x Camici P, Ferranini E, Opie LH. Myocardial metabolism in ischemic heart disease: basic principles and application to imaging by positron emission tomography. Prog Cardiovasc Dis 1989;32:217–238. w40x Thornton J, Striplin S, Liu GS, et al. Inhibition of protein synthesis does not block myocardial protection afforded by preconditioning. Am J Physiol 1990;259:H1822–H1825. w41x Strasser R, Arras M, Elsasser A, et al. Preconditioning of porcine ¨ myocardium: How much ischemia is required for induction? What is its duration? Is a renewal effect possible? Circulation 1994;90Žpart 2.:579ŽAbstract.. w42x Lawson CS, Downey JM. Preconditioning: state of the art myocardial protection. Cardiovasc Res 1993;27:542–550. w43x Law WR, McLane MP. Adenosine enhances myocardial glucose uptake only in the presence of insulin. Metabolism 1991;40:947–952. w44x Law W, McLane M, Raymond R. Adenosine is required for myocardial insulin responsiveness in vivo. Diabetes 1988;37:842–845. w45x Dale WE, Hale CC, Kim HD, Rovetto MJ. Myocardial glucose utilization: failure of adenosine to alter it and inhibiton by the adenosine analogue N 6 -ŽL-2-phenylisoprophyl. adenosine. Circ Res 1991;69:791–799. w46x Podzuweit T. Catecholamine-cyclic AMP-Ca2q-induced ventricular tachycardia in the intact pig heart. Basic Res Cardiol 1980;75:772– 779. Downloaded from http://cardiovascres.oxfordjournals.org/ by guest on June 9, 2014 w12x Liu Y, Kato H, Nakata N, Kogure K. Temporal profile of heat shock protein-70 synthesis in ischemic tolerance induced by preconditioning ischemia in rat hippocampus. Neuroscience 1993;56:921–927. w13x Gidday JM, Fitzgibbons JC, Shah AR, Park TS. Neuroprotection from ischemic brain injury by hypoxic preconditioning in the neonatal rat. Neurosci Lett 1994;168:221–224. w14x Kato H, Liu Y, Kogure K, Kato K. Induction of 27-kDa beat shock protein following cerebral ischemia in a rat model of ischemic tolerance. Brain Res 1994;634:235–244. w15x Burguera B, Elton CW, Tapscott EB, Pories WJ, Dimarchi R, Sakano K. Stimulation of glucose uptake by insulin-like growth factor IIrmannose 6-phosphate receptor. Biochem J 1994;300:781– 785. w16x Bevan SJ, Parry-Billings M, Opara E, Liu CT, Dunger DB, Newsholme EA. The effect of insulin-like growth factor II on glucose uptake and metabolism in the rat skeletal muscle in vitro. Biochem J 1992;286:561–565. w17x Tonnessen T, Giaid A, Saleh D, Neass PA, Yanagisawa M, Christensen G. Increased in vivo expression and production of endothelin-1 by porcine cardiomyocytes subjected to ischemia. Circ Res 1995;76:767–772. w18x Draznin B, Chang L, Leitner JW, Takata Y, Olefsky JM. Insulin activates p21Ras and guanine nucleotide releasing factor in cells expressing wild type and mutant insulin receptors. J Biol Chem 1993;268:19998–20001. w19x O’Dell TJ, Kandel ER, Grant SG. Long-term potentiation in the hippocampus is blocked by tyrosine kinase inhibitors. Nature 1991;353:558–560. w20x Hellenius M, Brismar K, Gerglund B, De Faire U. Effects on glucose tolerance insulin secretion, insulin-like growth factor 1 and its binding protein, IGFBP-1, in a randomized controlled diet and exercise study in healthy, middle aged men. J Intern Med 1995;238:121–130. w21x Sack S, Mohri M, Arras M, Schwarz ER, Schaper W. Ischaemic preconditioning—time course of renewal in the pig. Cardiovasc Res 1993;27:551–555. w22x Lewitt MS. Role of the insulin-like growth factors in the endocrine control of glucose homeostasis. Diabetes Res Clin Pract 1994;23:3– 15. w23x Vogt A, Barancik M, Weihrauch D, Arras M, Podzuweit T, Schaper W. Protein kinase C inhibitors reduce infarct size in pig hearts in vivo. Circulation 1994;90:3486ŽAbstract.. w24x Vogt AM, Htun P, Arras M, Elsasser A, Podzuweit T, Schaper W. ¨ Intramyocardial infusion of tool drugs for the study of molecular mechanisms in ischemic preconditioning. Basic Res Cardiol 1996;91:389–400. w25x Burke TJ. Protein-tyrosine kinases: potential targets for anticancer drug development. Stem Cells Dayt 1994;12:1–6. w26x Froesch ER, Schmid C, Schwander J, Zapf J. Actions of insulin-like growth factors. Annu Rev Physiol 1985;47:443–467. w27x Cohik W, Clemmons D. The insulin-like growth factors. Annu Rev Physiol 1985;55:131–153. w28x Herington AC. Insulin-like growth factors: biochemistry and physiology. Baillieres Clin Endocrinol Metab 1991;5:531–551. 477
© Copyright 2026