How Can I Exclusively Breastfeed My Baby
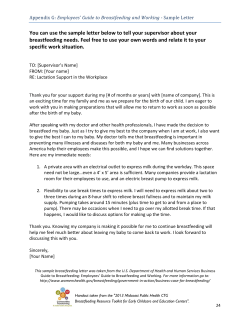
African Population and Health Research Center Breastfeeding Briefing #1 | October 2013 How Can I Exclusively Breastfeed My Baby In Kenya, according to the Kenya Demographic and Health Survey (KDHS) 2008-2009, What’s so Great about Exclusive Breastfeeding? Breastfeeding is the most natural way to feed newborn babies, yet millions of babies are not breastfed adequately. UNICEF and WHO recommendations for infant feeding during the first two years of life include (WHO 2003): only 32% of children ⁍⁍ under the age of six ⁍⁍ months are exclusively ⁍⁍ breastfed. Immediate initiation of breastfeeding after birth Exclusive breastfeeding for first six months Sustained breastfeeding for two years or beyond with appropriate complementary feeding from six months This breastfeeding practice is critical for child growth, development and survival. It reduces infections and mortality in children, improves mental and motor development, and protects against obesity and metabolic diseases and premature deaths later in the life course (Black et al 2013, Lanigan and Singal 2009, Black et al. 2008, Victora et al. 2008, Grantham-McGregor et al 2007). ...In urban slums in Nairobi, Kenya, only 2% of infants are breastfed exclusively for the first six months according to research by APHRC (Kimani-Murage 2011). But how does Breastfeeding Provide all these Benefits? Human breast milk uniquely benefits the baby. It contains various components including bioactive proteins that are lacking or are in lower quantities in other milk substitutes such as cow milk. These components offer various benefits to the baby including enzyme activities, antimicrobial effects, enhanced nutrient absorption and growth stimulation. It also contains milk fat globule membranes Practical Concerns In Realizing The WHO Recommendations For Breastfeeding In Urban Poor Settings In Nairobi (MFGM), which may explain the difference in infection levels and cognitive development between breastfed and formula fed children. While some studies have found no consistent difference in adiposity between formula-fed and breastfed infants in the first six months of life, others have found that breastfed infants may gain more fat in the first six months of life but gain more fat-free mass after six months, which reduces the risk of obesity later in life (Ziegler 2006, Lonnerdal 2010). The Global Nutrition Target The 65th Session of the World Health Assembly (WHA), Geneva, May 21-26, 2012 endorsed six nutrition targets, including increasing exclusive breastfeeding rates in the first six months up to at least 50% by 2025. This is an ambitious target, given the current situation globally of sub-optimal breastfeeding practices, where only 39% of children are exclusively breastfed for the first six months (UNICEF global databases 2012 - www.childinfo.org/ breastfeeding_status.html). In Kenya, according to the Kenya Demographic and Health Survey (KDHS) 2008-2009, only 32% of children under the age of six months are exclusively breastfed. Even fewer children in the urban slums, where majority of urban residents in Kenya live, are adequately breastfed. Only 2% of children are exclusively breastfed for the first six months, and 15% of children stop breastfeeding by the end of one year (Kimani-Murage 2011). 1 To improve breastfeeding practices, and achieve the WHA target of a 50% increase in exclusive breastfeeding for six months by 2025, context-specific interventions are needed. Breastfeeding in Kenyan Slum Settings In April 2013, the African Population and Health Research Center (APHRC) carried out a study to establish the factors that influence breastfeeding practices among the urban poor in Nairobi, Kenya. The study found that though the urban poor highly esteem the WHO guidelines for breastfeeding, these recommendations are impractical in the urban slum settings due to several factors affecting breastfeeding in these settings. In this briefing paper, we outline the root causes of poor breastfeeding practices among the urban poor. Five socio-economic and structural barriers to exclusive breastfeeding in slum settings 1 Due to limited livelihood opportunities in the slums, most people work for a daily wage. Most working women are casual laborers in neighboring factories or domestic workers in nearby middle income estates, and these work environments are not conducive for breastfeeding. They are therefore said to be hustlers, struggling to make ends meet. With no option for maternity leave, most resume work weeks, sometimes even days, after delivery. Sometimes it is because of the many problems they encounter. For example, a mother cannot sit, caring for the young baby when she has 5 children to take care of. The other children will suffer. She has to go out and hustle for what they will eat. In most cases she will stop to breastfeed since she cannot carry the baby to work (FGD, Village Elders) 2 Food insecurity due to chronic poverty is a major deterrent to optimal breastfeeding, as lack of food means inadequate breast milk for the baby. … if you ask her she will ask you how she will breastfeed and she hasn’t eaten. And if you look at the breasts, they have flattened and are sagging to the side and she is a girl, she hasn’t eaten… So even if you tell her to breastfeed, first of all that milk is not there because there is no food in that house Here in Korogocho, there are many girls who get children out of wedlock so after delivery they start the baby on bottle feeding because their parents tell them not to breastfeed so that they go back to school”. (FGD: Mothers) (FGD, Village Elders) 5 Poor professional and social support was considered an important factor. Many mothers give birth at home so no professional counseling, many have no domestic help so resume household chores immediately, while for married women, husbands were also hustlers and often drunkards, offering little support. Now you’ll find the problem which is here, is that the child is born and after one month it is given these adults’ foods. That is one problem and it is as if the mother doesn’t know… Most children are born just here at home ... The mother didn’t even go to the clinic, she was not taught about to take care of the child, she doesn’t know if she is (HIV) positive or negative”. (FGD, Village Elders) Recommendation: Recommendation: There is need for social protection measures such as cash transfers for vulnerable breastfeeding mothers in urban poor settings and baby friendly income generating activities and work environments. Additionally, counseling of mothers on birth planning should encourage saving to cater for the first six months after birth. Further, maternal, Infant and Young Child Nutrition (MIYCN) interventions must be carried out hand in hand with reproductive health provisions addressing the number of and spacing of children. though the urban poor highly esteem the WHO guidelines for breastfeeding, these recommendations are impractical in the urban slum settings due to several factors affecting breastfeeding in these settings. 2 3 Teenage pregnancy and single motherhood are key factors because many mothers are young and single. They have concerns of body image (aging and breasts sagging), they are still in school and they are still busy with their lives, often working as commercial sex workers to make ends meet, not conducive for breastfeeding Adolescent reproductive health interventions including sex education in schools are required in these settings 4 HIV in an area with high prevalence, twice the national level is also considered a key factor. There is mixed understanding regarding breastfeeding for HIV positive women, which affects practice for HIV victims and other uninfected women. Some people believe those who breastfeed (exclusively) for six months are HIV positive. (FGD, mothers) Recommendation: There is need to ensure correct and consistent messaging on breastfeeding for HIV positive women. Additionally, there is need for creation of awareness at the community level on the importance of exclusive breastfeeding amongst all mothers and not just for HIV-positive ones to reduce HIV-related stigma associated with exclusive breastfeeding. Recommendation: There is need for creation of awareness on the need for support for breastfeeding mothers including on the need for spousal support. Additionally, baby friendly community initiatives such as providing breastfeeding counselling and support at the community level may make a change. Conclusion To improve breastfeeding practices, and achieve the WHA target of a 50% increase in exclusive breastfeeding for six months by 2025, context-specific interventions are needed. For example in the urban slum settings, approaches aimed at improving breastfeeding practices must consider the wider ecological setting in order to be successful. Interventions should also target empowerment such as with income generating activities that offer conducive environment for breastfeeding and social protection measures such as cash transfers for the first few months after delivery. 3 ...A mother cannot sit, caring for the young baby when she has 5 children to take care of. The other children will suffer. She has to go out and hustle for what they will eat... Because Urban Poor Mothers Are Hustlers! APHRC carried out a study to establish the factors that influence breastfeeding practices among the urban poor in Nairobi, Kenya. Research Methods ⁍⁍ ⁍⁍ Data collection period: April 2012 Qualitative interviews – IDIs, KIIs & FGDs (n=40) with mothers; health care workers, community leaders and traditional birth attendants Study Context ⁍⁍ ⁍⁍ ⁍⁍ ⁍⁍ ⁍⁍ ⁍⁍ ⁍⁍ ⁍⁍ ⁍⁍ ⁍⁍ Two slums of Nairobi: Korogocho & Viwandani Densely populated areas 63,318 and 52,583 inhabitants/km2 Fourth largest informal settlement in Nairobi Located 12km northeast of Nairobi’s Central Business District Inhabited by stable long-term residents In existence since 1972 Total area: 0.97 sq. kilometers Population density: 46, 961 Poor housing, livelihood opportunities (low average monthly wage of approx. USD 70), water and sanitation Poor health conditions: high level of early sexual debut (10% of adolescents <15 years sexually active); high levels of under five malnutrition at 40%; high HIV prevalence at 12%; high prevalence of severe food insecurity (50% of households) Contributors Kimani-Murage, E ., Wekesah F., Kyobutungi, C ., Wanjohi M1., Muriuki P1., Ezeh A1., Musoke R2., Norris S3., Madise, N4., Griffiths P5., 1 1 African Population and Health Research Center (APHRC); P.O. 10787, 00100, Nairobi Kenya; [email protected]; University of Nairobi, Kenya; 3 University of the Witwatersrand, Johannesburg, South Africa, 4 University of Southampton, UK; 5 Loughborough University, UK; 1 2 Sources Black, R.E., et al., Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet, 2013. 382(9890): p. 427-51. Black, R.E., et al., Maternal and child undernutrition: global and regional exposures and health consequences. Lancet, 2008. 371(9608): p. 243-60. Kenya National Bureau of Statistics (KNBS) and ICF Macro, Kenya Demographic and Health Survey 2008-09. 2009: Calverton, Maryland: KNBS and ICF Macro. Kimani-Murage, E., et al., Patterns and determinants of breastfeeding and complementary feeding practices in urban informal settlements, Nairobi Kenya. BMC Public Health, 2011. 11(396). Lonnerdal, B., Bioactive proteins in human milk: mechanisms of action. J Pediatr, 2010. 156(2 Suppl): p. S26-30. Victora, C.G., et al., Maternal and child undernutrition: consequences for adult health and human capital. Lancet, 2008. 371(9609): p. 340-357. WHO, Global strategy for infant and young child feeding. 2003, WHO Geneva. Ziegler, E.E., Growth of breast-fed and formula-fed infants. Nestle Nutr Workshop Ser Pediatr Program, 2006. 58: p. 51-9; discussion 59-63 *IDIs=Indepth interviews | KII=Key Informant Interview | TBA=Traditional Birth Attendant | FGD=Focus Group Discussion | CHWs=Community Health Workers African Population and Health Research Center, APHRC Campus | 2nd Floor, Manga Close, Off Kirawa Road | P.O. Box 10787-00100, Nairobi, Kenya | [email protected] | www.aphrc.org
© Copyright 2026