Original PCE Study Guide
PNE Written Component Prepared by PABC Members: Jason Shane ([email protected], www.facebook.com/shanephysiotherapy and Amanda Mrsic ([email protected]), for the FREE distribution to whomever may benefit from its use. Our way of paying it forward. Hopefully the time (let’s be honest, a ridiculous amount of time) we spent making this will help you studying for the national exam. As we used to say “you’re going to rock it!” (p.s. go to the end of the document...we have a goodbye note...and a page count, yikes!) SAMPLE LIST OF AREAS OF PRACTICE EVALUATED BY THE PCE 01.01. Neuromusculoskeletal (50%±5%) (This list is not necessarily exhaustive.) 01.01.01 Muscle contusions/strains/tears/weakness Mm Strains: majority occur in bi-articular mm at the mm-tendon jx, most occur during eccentric loading; Rx: - Acute Phase: PRICE, crutches if in LE; - Repair Phase: modalities, DTF’s, strength, stretching; - Remodeling phase: strength (incr loading and velocity), stretching (static and dynamic) 01.01.02 Pelvic floor dysfunction Can be assessed via: digital, EMG, manometric, dynamometer, RTUS real time ultra sound, MRI & biofeedback. Rx: isolate PFM during exercise, avoid accessory mm use, eg. Glutes, abs; overload the mm by holding longer with shorter rest periods; weakness or laxity of PFM can occur during pregnancy or childbirth, further loss of elasticity and mm tone later in life (or even after pregnancy) can lead to: - cystocele=herniation of bladder into vagina, - rectocele= rectum into vagina, - uterine prolapse = uterus into vagina; Sy’s of pelvic pain: pain down post thigh Add in more info from patho lecture - female reproductive pathology Jason Shane and Amanda Mrsic Apr 2015 01.01.03 Ligament sprains/tears Grade 2 syndesmotic ankle sprain (high ankle sprains): Rx: - Phase 1 (protection phase 2wks) Goal to protect and decr inflam, PRICE, NWB with crutches, modalities to decr edema, light ROM; - Phase 2 (management phase 2-4weeks) goal is normal mobility, incr strength and fx ambulate (PWB w/o P), bilateral stance training, joint mobs, strength training; - Phase 3 (management) goal to incr function and unilateral balance and strength; - Phase 4 Return to sport 01.01.04 Tendonopathy, tendon ruptures/tears, tendonosis Achilles tendonopathy, Rx-eccentric heel drop program, footwear/orthoses, stretching/mobs De Quervain’s Tenosynovitis = a tendinosis of the sheath or tunnel that surrounds the tendons of EPB (O: lower post 1/3rd of radius, I: base of prox. Phalynx of thumb) & APL (O:ulna, radius, interos. Memb, I: base of 1st metacarpal) (mm which radially deviate the thumb). To test for it: tuck thumb in fist and ulnarly deviate wrist, look for P along area of distal radius APL, EPB, fray of sheath, scar tissue forms (inflamm, repair) Lateral Elbow P = 90% involve ECRB (O:lateral epi, I: post base of 3rd metacarpal, Fx:extends and abducts hand at the wrist), other 10% are b/w common extensor tendon and origin (tenoperiosteal Jx) and origin of ECRL (O: lateral supracondylar ridge, I: dorsal surface of base of 2nd metacarpal on radial side, Fx: extensor at the wrist joint, abducts the hand at the wrist; usually symptomatic with activities involving wrist and/or finger extension and/or gripping); Test for it: P w/ resisted extension of D3; Rx: Acute-control P and inflame, rest, ice, US, tennis strap, TENS, Pt ed, maintain mm length and mobility, AROM for elbow, wrist, and hand; Repair-gently stress collagen via DTFM and eccentric strength training, cont with stretches 01.01.05 Fasciitis, fascial tearing, myofascial restriction P59 O’Sullivan Fascia - found in ligaments, tendons, bone and muscle Rx: soft tissue work, needling, exercises 01.01.06 Joint derangements/dysfunction (e.g., loose bodies, hypermobility, hypomobility) Loose body: free floating piece of bone or cartilage; often result of OA or chip fracture; typical symptom is locking or catching Hypermobility: spondylosis (OA of joints in spine and narrowing of foramina), listhesis (fracture and slip of cranial vert anteriorly), lysis (fracture of pars) Jason Shane and Amanda Mrsic Apr 2015 Hypomobility: capsular patterns, O’sullivan pg 4 01.01.07 Fractures, dislocations, subluxations Fractures: K&C (Kisner and Colby) pg 321-325 Comminuted fracture = fracture with more than 2 fragments Subluxations: - AC joint, K&C pg 494; clavicle post and sup on acromion, - Shoulder (GH joint) dislocation: Rx-scapular stabilization/posture, rotator cuff strengthening/functional rehab SLAP lesion = Superior Labral tear Anterior to Posterior Bankart lesion = injury to ant/inf portion of glenoid labrum 01.01.08 Osteoporosis/osteopenia Depleted BMD Women 10X more than Men esp post. menopause Fracture of: Tsp, Lsp, Femoral neck, Prox humerus, prox tibia, pelvis, distal radius NORMAL = WITHIN -1 SD FOR BMD OSTEOPENIA = -1 TO -2.5 SD BMD OSTEOPOROSIS = -2.5 SD AND BELOW 01.01.09 Tumour/pathological fractures Primary malignant tumors of soft tissues and bone are rare but may occur in youth Osteosarcoma = occur at either end of long bones, produce jt pain, Agg: activity, X-ray: moth eaten appearance, Rx = surgery (Terry Fox had this) Primary malignant tumors are rare in bone, usually are secondary Synovial sarcoma = usually in larger joints, P (often at night or w/ activity), swelling and instability, Rx: Sx +/- chemo/rad Malignant tumors=may metastasize to bone Mets from breast, lung, prostate, kidney, thyroid cancers Osteoid osteoma = benign bone tumor, exercise related bone P and tenderness (often mistaken for bone #), characterized by presence of night P and abolition of Sy’s with aspirin, CT scan shows a central focus point, Rx: ablation, ethanol, laser 01.01.10 Degenerative joint disease Mechanical change, jt disease and jt trauma Degeneration of articular cartilage: hypertrophy of subchondral bone and ht capsule Jason Shane and Amanda Mrsic Apr 2015 (wt bearing jts) Meds: corticosteroids and NSAIDS OA: decreased jt space, dec cartilage height, osteophytes PT goals: jt protection, improve jt mechanics, aquatics 01.01.11 Mechanical spinal abnormalities (e.g., low back pain, scoliosis, postural dysfunction) REMEMBER THIS PICTURE, it can be useful!!! Posture: RSPT 518 Oct 8th Posture and LBP: RSPT 544 Oct 13 (May Nolan lecture) 01.01.12 Inflammatory/infectious conditions of the neuromusculoskeletal system (e.g., osteomyelitis) Osteomyelitis = Inflamm response in bone caused by infection; O’Sullivan pg 37, usually a staph aureus infection Goals: maintain joint function, cast care More common in kids and immune supressed, M>F, antibiotics to treat: Sx if in the jt Tendonitis = Inflammation due to micro trauma Tendinosos = Chronic tendon dysfunction: common sites supraspinatus, common extensor tendon of elbow, patella Jason Shane and Amanda Mrsic Apr 2015 Bursitis -caused by overuse, trauma, gout, infection; S and S is pain with rest, active and PROM are limited; Rx-flexibility, mobs, thermal agents 01.01.13 Amputations Causes: diabetes mellitus, PVD, trauma, congenital/correction of deformity, tumors, infected TKR Sites of amputation (the tricky ones): toe (ray resection), ankle (symes) Effects of: 1)Toe amputation - decreased power for push off, decrease balance d/t decreased proprioception and BOS 2)Partial foot - lose forefoot lever, decrd balance, risk for tissue breakdown secondary to incrd pressure on remaining WB surface - prosthesis: shoe filler, carbon fiber afo, complete prosthesis 3)Ankle (Symes): goes through the jt, distal end of tip and fib intact - long lever, bulbous end, better than transtibial - high risk of skin breakdown - prosthesis: similar to trans-tib, trap door to fit over malleoli, can have partial patellar WB 4) Transtibial - can’t WB through the end, some ppl can achieve a normal gait pattern - Prosthetic sockets: total surface bearing, patellar tendon bearing - Pressure sensitive: anterior/distal end of tib, fibula - head and end, bottom of stump - pressure tolerant: post mm mass, patellar tendon, medial/lateral flares - suspension: supracondylar, suprapatellar cuff, sleeve (req lots of hand strength), locking pin, suction (1 way valve) gait deviations: stance: foot flat or foot slap, knee hyperextension or buckling, early heel rise, swing: inc/dec stride length, toe drag, lat/med whip, vaulting 5) knee disarticulation - thigh mm preserved, potential to WB through the stump, prosthetic: trap door for condyles 6) transfemoral - no WB on end, takes 60% more energy to ambulate with prosthesis compared to able body walking, may require a gait aid, often asymmetrical gait, WB through Ischial Tuberosities and hydrostatic loading, pressure sensitive areas= end of residual limb, adductor tendon - Knee prosthesis: manual lock, mechanical/friction, hydraulic/pneumatic/microprocessor gait deviations: Jason Shane and Amanda Mrsic Apr 2015 stance: ABduction, lat trunk shift, excessive trunk lordosis, hip flex, dec stance time, swing: medial or lateral whips, circumduction, hip hike, vaulting with good leg 7) hip disarticulation - probs require gait aid, asymm gait pattern 210% energy expenditure 8) hemipelvectomy PT education: - contracture prevention, knee or hip flex contracture >20% will prevent prosthetic use, pain management, edema control, shaping, fall prevention, foot care of remaining limb, falls prevention (risk @ night) - NO PILLOWS under legs in supine or between legs for transfemoral - Socket-supports body wt - Liner-interface b/w socket and limb - Suspension-system used to keep prosthesis on the residual limb - Socks-ensure proper fit - Shank/pylon-connects socket to foot, provides ht 01.01.14 Congenital malformations (e.g., talipes equinovarus, hip dysplasia) Duchennes Muscular Dystrophy: X-linked recessive mm weakness proximal to distal, die as late adolescents, +ve gowers Talipies Equinovarus = CLUB FOOT-plantar flexed (talocrural), adducted, inverted (subtalar, talocalcaneal, talonavicular, calcaneo-cuboid), supination at midtarsal joints 2 types: 1) Talipes Equinovarus - abnormal equinovarus - abnormal development of head and neck of talus - hereditary or neuromuscular disorders; 2) Postural - feet squished in utero; Rx: casting and splinting or Sx Equinus = PF foot; Etiology = congenital bone deformity, CP, contracture of calf mm 01.01.15 Nerve compression (e.g., Carpal Tunnel Syndrome, radiculopathy, spinal stenosis) Radiculopathy = Si’s & Sy’s depend on degree of compression and may include: P, tingling, numbness, loss of N conduction, mm weakness, decrd skin sensation, and loss of reflex Spinal Stenosis = hypertrophy of spinal lamina, ligamentum flavum, facets; vascular or neural compromise; (also see May Nolan L-Spine lecture pg 15) Rx: joint mobs, flexion bias exercises, avoid extension, traction Thoracic Outlet- subclavian artery vein, brachial plexus, vagus/phrenic N, sympathetic trunk compress at: sup thoracic outlet, scalene triangle, clavicle and rib 1, pec minor and Jason Shane and Amanda Mrsic Apr 2015 thoracic wall Rx: restore mm imbalance, Sx NERVE ENTRAPMENT1) ulnar nerve-normally occurs in cubital tunnel, could be d/t trauma, compression, thickened retinaculum in FCU, Sy’s medial elbow pain, +ve tinnel sign 2) median nerve-occurs in pronator teres, and under FDS, occurs with repetitive gripping activities; aching pain, forearm pain 3) radial nerve-entrapment of distal branches (post interosseous nerve) occurs in radial tunnel Carpal Tunnel: can do Phalen’s test, long term compression of median nerve can cause atrophy of thenar mm 01.01.16 Peripheral nerve injuries Wallerian Degeneration - transection results in degen or axon and sheath distal to site of injury Segmental Demyelination -axons are preserved but are demyelinated; remyelination restores fx, ex GBS Axonal Degeneration- axonal degeneration of axon cylinder and myelin, distal to proximal, “dying back of nerves,”, ex-peripheral neuropathy NEUROPATHY: any disease of nerves characterized by deteriorating neural function TRAUMATIC: Expect to see motor, sensory, and potentially autonomic changes (ex), and pain; an MRI or nerve conduction test is used to confirm a peripheral nn injury Neuropraxia= just a compression of the nerve, causes a transient disruption, good recovery w/good prognosis which could take minutes to weeks Axonotemesis= disruption of axon but myelin sheath is still intact, may cause paralysis of the motor, sensory, and autonomic. Mainly seen in crush injury. Longer recovery with fair prognosis which can take months Neurotemesis=completely severed axon and sheath; recovery is only possible with surgery with variable success; i.e. it may never recover Charcot Marie Tooth Disease =a hereditary motor and sensory neuropathology causing extensive demyelination of motor and sensory nerves of the foot Presentation: slow progression of symmetric mm weakness, atrophy of foot intrinsics, diminished deep tendon reflexes, pes cavus/hammer toes, weak dorsiflexors and pronators PT Rx: contracture management (stretching mm), management/education on foot care Bell’s Palsy=d/t latent herpes virus, days before onset Pt reports pain around Jason Shane and Amanda Mrsic Apr 2015 mastoid; virus causes inflam response over facial N Facial N innervates-mm of facial expression, stapedius mm of inner ear, sensory and autonomic fibers for taste (ant aspect of tongue), tears, salivation Clinical manifestations-unilateral facial paralysis Rx: corticosteroids, estim?, protect eye Thoracic Outlet Syndrome=an entrapment syndrome caused by pressure on brachial plexus Risks for getting it-posture, growth, trauma, body comp Pathology-chronic compression of N roots results in edema and ischemia of N roots→ neuropraxia and wallerian degen can occur presentation-paraesthesia, weakness and pain in arm, neck pain may radiate into face, scapula, ant chest; coldness, edema, raynaud’s, fatigue in hand, distension of veins Rx: correct posture, surgical mngmt if vasculature gets compromised Diabetic neuropathy=peripheral nn disorder in diabetes that occurs w/o any other cause for neuropathy Pathology-chronic metabolic disturbance affects nn and schwann cells-->loss of both myelinated and unmyelinated axons Presentation-symmetric, distal pattern of sensory loss, painless paraesthesia with minimal motor weakness Rx:control hyperglycemia, skin care, amputation 01.01.17 Neural tissue dysfunction/neuro-dynamic dysfunction Dural Tension Double Crush - compression of N along several sites proximal and distal SLR, PKB, ULTT, SLUMP etc. 01.01.18 Scars Keloid scar: thick scar that goes beyond the margins of the original wound Hypertrophic: thick scars that do not extend beyond the boundary of the original wound but has an excess amount of tissue in relation to what is needed to replace the damaged dermis 01.02 Neurological (20%±5%) (This list is not necessarily exhaustive.) 01.02.01 Cerebral Vascular Accident/transient ischemic attack Jason Shane and Amanda Mrsic Apr 2015 Stroke: Ischemic (80%) or Hemorrhagic (20%) TIA: brief blockage of circulation 01.02.02 Acquired brain injury TRAUMATIC =change in brain fx d/t external force; forces can include blunt (MVA, fall, accel/decel), contusion, shearing, bruising, axonal tearing, rotational forces, penetrating, blast Hematomas: Epidural-outside the dura, 90% assocd with skull fractures, most often in temporal or temproparietal region, arterial bleed Sub-dural-brain collects between brain and dura, often requires surgical intervention (burr holes or craniotomy), venousl bleed Intracranial-most common, blood within the brain Diffuse axonal injury=shearing of the brain’s long connecting nerve fibers; usually causes a coma, can’t see on MRI; can affect grey/white matter interfaces Secondary brain injuries=cerebral blood flow is 50% less than normal post injury, bruising, inflammation, incrd ICP Intracranial pressure: normal is 0-10mm Hg, >20mm Hg is BAAAD Physio problem list: Resp complications (decrd tidal volumes, small airway, atelectasis), ICP, abnormal posture, mobility, contractures, confusion/agitation, fatigue Decerebrate posturing=indicates brain stem damage (lesions or compression in midbrain) and lesions in cerebellem Decorticate posturing= arms flexed, legs extended, damage to areas including cerebral hemisphere, thalamus, cord, corticospinal tract Rx: Initial medical management=prevent hypoxia, maintain adequate BP, adequate fluids to maintain Mean Arterial Pressure, HOB 30 degrees Nutrition: hypermetabolism, energy expenditure may be doubled for up to 4 weeks Other complications: 40% get post traumatic epilepsy; DVTs, and PE’s Basal skull fracture=signs are blood or CSF out of nose or ears, raccoon eyes, bruising over mastoid (battle sign) Coma=altered state of consciousness so that no amount of stimulus or only pain will cause Pt to respond Frontal lobe injury=disinhibition, memory impairment, anosmia (can’t smell), seizures, expressive aphasia) Temporal lobe= receptive aphasia, dyslexia, dysgraphia, amnesic syndromes, Jason Shane and Amanda Mrsic Apr 2015 epilepsy AND NON TRAUMATIC BRAIN INJURY STROKE ischaemic = 80% of strokes; could be d/t a thrombus (slower sy’s to evolve) or embolism (occurs rapidly w/o warning); risk factors are atherosclerosis, HTN, cardiac disease, diabetes, TIA=sudden onset, last 24hrs, warning sign of stroke; majority have full stroke w/in 1 year hemorrhagic = 20%, aneurysms and AV malformations, HTN, head trauma, illicit drugs, bleeding disorders S’s and Sy’s = confusion, headache, trouble speaking, understanding speech, numbness or weakness on one side, can’t see, trouble walking, dizziness, loss of balance or coordination, sudden severe headache Rx: thrombolytic agents, Tissue Plasminogen Activator (TPA)=activates plasminogen to digest fibrin which breaks down the clot, TPA can salvage penumbral tissue if given within 3 hours; mechanically widening an artery White matter is NOT plastic, grey matter is Lacunar strokes (infarcts)-subgroup of ischemic strokes, small but deep in the brain; assocd with HTN and diabetes, correlation with decreased cognition What causes a stroke: Arterial factors - artherosclerotic plaques, aneurysms, pressure on artery walls Venous factors - tendency for person’s blood to clot quickly, irritation or inflammation of lining of vein, DVT’s Penumbra = an area of the brain at risk for dying; is located between an area of perfusion and necrosis Progression of and Risk for a Stroke: ABCD Score; Age, Blood pressure, Clinical features (hemi-weakness, speech problems), Duration Brain Stem stroke = not very common v. disabling b/c it can take out ALL the ascending and descending tracts Prevention of recurrent of stroke: anticoagulants (aspirin), lipid lowering agents, lifestyle changes cortex=grey matter and capable of neuroplasticity Cortico-spinal tract-made up of white matter, is not plastic CONCUSSION = a complex pathological process affecting the brain, induced by traumatic biomechanical forces. Jason Shane and Amanda Mrsic Apr 2015 -mild form of brain injury (most common TBI) -loss of consciousness may or may not be present -diagnose with signs, behavioral change, cognitive impairment, sleep disturbance -baseline cognitive Ax: SCAT 2 -second impact syndrome- rare/fatal uncontrolled swelling of brain, minor 2nd blow before initial symptoms are resolved -post concussion syndrome: persistent symptoms: headache, dizzy, irritable, memory, vision, concentration - 3+ concussions = 5X greater risk Alzheimer's, 3x memory deficits - coup, contre-coup - grade 1: does not lose consciousness, dazed - grade 2: no LOC, period of confusion, does NOT recall event - grade 3: loss of consciousness for short time, No memory of event, requires eval asap risk: contact sports, anti-coagulants, prior events S&S: dizzy, headache, vomit, sudden weakness, nystagmus, change in pupil size, emotional lability, memory loss, drowsy, confused TBI ***head down positioning is CONTRAINDICATED! for those with traumatic brain injury****** positioning: limit neck flex and rotation suctioning: pre/post oxygenation at 100%O2 resting splints 6-8hrs to prevent contractures aspiration risks: turn feed tube off 20mins prior to Rx 01.02.03 Spinal cord injury We recommend you look over this section.... Jason Shane and Amanda Mrsic Apr 2015 Causes of SCI: Traumatic; 40% are cervical incomplete Types of traumatic injuries: Hyperflexion, hyperextension, axial load, rotation, penetrating injury Non-traumatic: cancer, infection and inflammation, motor neuron disorders, vascular diseases (spinal cord infarcts); most are paraplegic Reasons for Sx: unstable # or soft tissue injury, neuro sy’s getting worse Benefits of Sx: realignment, stabilization, early mobilization, early rehab, less medical complications, decrd hospital stay Myelopathy = refers to pathology of the spinal cord. When due to trauma, it is known as spinal cord injury Lumbar laminectomy=helps to decompress the cauda equine/roots Cauda equina syndrome: Jason Shane and Amanda Mrsic Apr 2015 -affects more than one nerve root, surgical emergency -Usually presents with: bilateral leg pain/numbness, sacral root problems, urinary retention, stool incontinence, absent reflexes Mobility orders from doctor: “Spine stable” = column is assumed unstable, +/- neuro deficits, at risk for additional injury; Pt must: 1)maintain neutral spine at all times, 2) bedrest, 3) HOB at zero degrees; 2-3 person turns at all times “Spine stable” - requires protection = confirmed spinal column, +/- neuro deficits, Pt must maintain neutral spine at all times, Pt can turn independ with neutral alignment, mob and rehab begins “Spine stable-no restrictions ”= injury decided stable by surgeon, patient may do all mvmts of spine w/I comfort limits; Pt may be taught to log roll with neutral spine Important to classify SCI b/c: to define level and extent of injury, gives a baseline, used for prognosis and outcome measure ASIA: Sensory exam: light touch and pin prick tested; - Grade 0: Pts does not reliably report being touched, - Grade 1: Pt correctly reports being touched and differentiating b/w sharp and dull BUT describes feeling of sharpness as different, - Grade 2: Pt normal Hyperpathia=everything feels sharp Deep Anal Pressure (DAP): if present, Pt has a sensory incomplete injury ASIA B Voluntary Anal Contraction=if present indicates motor incomplete (AIS C) Motor exam: 10 bilateral myotomes C5 ABD/elbow flexors, C6 wrist extensors, C7 elbow ext, C8 thumb ext/ ulnar dev, long finger flexors, T1 finger abductors Level of lesion = defined as the most caudal segment of the spinal cord with normal sensory and motor Fx on BOTH sides of the body - Sensory level-most caudal segment w/bilateral score of 2 for BOTH light touch and pin prick - Motor level-most caudal segment with a grade greater than or equal to 3 provided ALL segments above are grade 5 Clinical syndromes: Complete injury = no sensory or motor Fx is preserved in the sacral segments S4-S5; there may be dermatomes below the sensory level and myotomes below the motor Jason Shane and Amanda Mrsic Apr 2015 level that remain partially innervated…KNOWN as Zone of Partial Preservation, the most caudal segment with some sensory defines extent of ZPP Anterior Cord Syndrome=loss of motor Fx, P and temp below injury level; dorsal column is spared (i.e. kinesthesia, proprioception, vibration) Central Cord Syndrome=upper motor and sensory Fx more impaired than LE; often associated with spinal canal stenosis Brown Secard= one side of cord more damaged than the other; IPSILATERAL loss of motor Fx and dorsal column Fx (reason is they cross in medulla); CONTRALATERAL loss of P and temp sensation a few levels below the lesion Conus and Cauda Equina=spinal cord terminates at L1-L2; injuries at conus can affect both conus and root resulting in a varied neuro picture; i.e. mixture of UM and LMNL Prognosis for neuro injuries: pinprick preservation (LE and sacral) w/i 72hrs is good prognosticator of motor function to return and ability to walk SCI Effects on Resp Fx: ● C4 is normally the level Pt’s need to breathe independently ● T11 and below, normal vital capacity ● Cough Fx: C1-C3 absent, C4-T1 non functional, T2-T4 poor, T5-T10 weak, T11 and below is normal ● C2-C7 innervate accessory mm of breathing ● T1-T11 innervate intercostals ● T6-L1 innervate abdominals Levels of injury: C1-C4: Patterns of weakness - paralysis of trunk and UE, probably diaphragm Possible mvmts: neck mvmts, slight sh retraction and add Role of PT: ROM, spasticity management, neck strengthening, chest physio, prevent contractures Major mm innervated: FULL: C1-C3 SCM, neck extensors, neck flexors C2-C4 traps PARTIAL: C3-C5 Lev scap, diaphragm, supraspinatus, infraspinatus C4-C5 rhomboids C5: Patterns of weakness - sig imbalance around sh girdle, absence of elbow ext, wrist pronation, ext, flex or any hand/finger movement Possible mvmt - sh abd, flex, ext, elbow flexion and supination, scapular add and abd Jason Shane and Amanda Mrsic Apr 2015 FULL: all of the C4 mm plus diaphragm, rhomboids (C4-5 dorsal scapular), levator scapula (C3-4 and dorsal scapular) PARTIAL: Deltoid, biceps, brachioradialis, teres minor (C5-6) Hand Fx-use wrist splints and universal cuffs C6: Patterns of weakness - no wrist flexion, elbow ext, hand movt Possible mvmt - radial wrist ext, some horiz adduction, can extend elbow in some positions using ER of shoulder; have tenodesis grip which permits a weak grasp w/o any hand mm Slide board transfer possible, manual W/C possible, FIRST LEVEL OF SCI to have potential to live in community w/o care PT role: maximize strength for transfer to functional tasks, teach “trick” mvmt strategies, ROM and stretching, prescribe equipment C7-C8: Patterns of weakness - limited grasp and release dexterity d/t lack of intrinsic mm of hand Mvmt possible - elbow ext (C7), wrist ext, DIP/PIP flex, MP flex (C8) Triceps allow independent transfers, manual W/C, indep with most/all ADL’s Hand function - C8 gives finger and thumb flexors (which are weak) and no lumbricals Thoracic paraplegia - intact UE Fx, mainly use W/C Lumbar paraplegia-more motor sparing more efficient gait, possible to have functional gait, if conus or cauda equina may have flaccid bowel and bladder 2 tests for spasticity: Modified Ashworth, Tardieu Lat spinothalamic - P and temp Ant spinothalamic - crude touch and pressure Dorsal columns – fine touch, stereognosis, vibration Lateral corticospinal - the 90% that cross in the pyramid motor Anterior corticospinal - the 10% cross at the level of innervations motor Autonomic effects of SCI on Heart and Lungs: Sympathetic NS - Chain T1-L1, fight or flight, increases HR and BP and blood flow to skeletal mm, RELAXES bronchial mm (one would think it would contract them BUT if a bear was chasing you, you would want the mm to relax to incr O2 supply) Parasympathetic NS-craniosacral, primary interest in Vagus nerve; decreases HR and contractility, decr blood flow to smooth mm, contracts bronchial mm Jason Shane and Amanda Mrsic Apr 2015 With Level of injury T6 and above: (in general) - Sympathetic influence is dependent on level of injury (b/c it goes from T1-L1) - Parasympathetic influence remains intact and UNOPPOSED via the vagus nerve in injuries T6 and higher - Limits cardiac output and shunting of blood from inactive to active ones - Blunting of heart rate often to only110-120bpm - Heart response is d/t vagal withdrawal rather than sympathetic drive (normally sympathetic would drive up HR but it is no longer intact there must rely on removing parasymp) Spinal Shock = temporary suppression of all reflex activity below the level of injury (24-48 hrs) Neurogenic shock (T6 and above) = body’s response to sudden loss of symp. control, therefore parasymp dominance, loss of vasomotor control; 3 clinical signs are: 1) bradycardia, 2) hypotension, 3) Hypothermia Rx for hypotension: volume resuscitation (saline), vasopressors (to counter loss of sympathetic tone) Health risks with SCI: DVT, pulmonary embolus, HO (2 main contraindication for Rx are forced PROM and serial casting), osteoporosis AND Post traumatic syringomyelia=a formation of an abnormal tubular cavity in the spinal cord; the dura tethers/scars to the arachnoid blocking CSF flow, CSF is forced into the spinal cord progressively enlarging the cyst which compresses the cord and its vascular supply Spastic bladder = injuries above the conus, messages will continue to travel b/w bladder and spinal cord since reflex arc is still intact, may be triggered by “tapping”, bladder can be trained to empty on its own, bladder mngmt is either intermittent catheters or condom/foley drainage Flaccid bladder = in conus and cauda equina injuries, messages don’t travel b/w spinal cord and bladder since the reflex centre is damaged, bladder loses ability to empty reflexively, bladder will continue to fill AND must be catheterized Misc info: - CVD is major cause of death in people surviving 30 years+ - L ventricular myocardial atrophy seen in SCI - 100x higher rate of bladder cancer in people with SCI - Spasticity, common clinical characteristics: incrd mm tone or firmness, incrd stretch reflex, uncontrolled mvmts 01.02.04 Tumour (Can you believe it, they put tumors on the blueprint twice! Bah!) tumor = neoplasm, benign or malignant, soft tissue or bone, develop from or within tissue in a localized area - later they can spread (mets) Jason Shane and Amanda Mrsic Apr 2015 - epithelial = carcinoma mesenchymal (type of undifferentiated loose connective tissue from the mesoderm)= sarcoma glial = glioma - most common site of tumors in the brain lymphoid = lymphoma hematopoietic = leukemia melanocytic = melanoma LUNG carcinoma = squamous metaplasia, squamous diplasia, carcinoma in situ, invasive carcinoma COLON cancer = 2nd cause of death BREAST = hormonal and genetic risk factors, axillary node disection PROSTATE = in men over 50 usually, Tx: surgery, external beam radiation, brachytherapy, androgen deprivation therapy etiology = viruses, chemical agents, physical agents (radiation, asbestos), drugs, hormones, alcohol Rx: surgery, radiation, chemotherapy (usually in kids), biotherapy, antiangiogenic therapy, hormonal therapy kids: acute lymphocytic leukemia, non-hodgkins, hodgkins, brain, small round blue cell, sarcoma (bone based - osteosarcoma, ewing’s sarcoma) Skin Cancer: - Basal Cell Carcinoma (BCC) = most common form of skin cancer, low risk of spreading, translucent and red in color - Squamous Cell Carcinoma (SCC)=solid skin tumor, often volcano shaped, high risk for mets - Malignant melanoma = most dangerous form of skin cancer; high potential for mets - ABCD rule for melanoma- Asymmetry, Border, Color, Diameter 01.02.05 Degenerative neurological/neuromuscular disorders (e.g., muscular dystrophies, amyotrophic lateral sclerosis, Parkinson disease) ALS - amyotrophic lateral sclerosis (Lou Gerigs) = a motor neurone disease and gradual deterioration of BOTH UMN and LMN (may have both flaccid and spastic paresis), characterized by rapidly progressive weakness, muscle atrophy and fasciculations, muscle spasticity, difficulty speaking (dysarthria), difficulty swallowing (dysphagia), and decline in breathing ability. Amyotrophy - mm fiber atrophy Jason Shane and Amanda Mrsic Apr 2015 Lateral- lateral column atrophy Sclerosis-sclerosis (harden/thickening) of those axons Starts peripherally, moves central, mm groups are affected asymmetrically sensory system, cognition, bowel and bladder are spared Rx: resp difficulties, complications of immobility, sy relief Parkinson disease = chronic neurodegenerative disease, reduction in dopamine produced by substantia nigra Possible causes: infectious/post encephalitis (irritation and swelling (inflammation) of the brain, most often due to infections), drug induced Dopamine normally inhibits Ach, without dopamine there is excessive excitatory output Motor disturbances: resting tremor, rigidity, akinesia/bradykinesia, postural instability, impairments of voice, dexterity, balance, gait Non-motor disturbances: pain, visual/spatial, proprioceptive, postural hypotension,sleep disturbance, depression, anxiety, fatigue, dementia Limiting factors and contraindications to exercise: cardiac or resp condition, MSK problems, postural hypotension, severe dyskinesia DMD = issue with mm CT, fat infiltration, hypertrophy (esp in calves) and weakness, dystrophyn affected (protein), Gower’s sign (difficulty standing up, uses on hand on leg to get up) - mutation in single gene on X chromosome - fail to produce dystrophin protein - dystrophin links sarcolemma to actin - mm cells replaced by fat and CT - progessive symmetric mm wasting - CK levels high (necrotic mm) - normally diagnoses by 5, dead by ~20 - gowers and calf pseudohypertrophy -prox mm weakness, waddling gait, toe walking, lordosis, freq falls, difficulty standing up and climbing stairs, lower IQ -pelvic girlde then shoulder, scoliosis PT: work on strength, independence, advocate 01.02.06 Demyelinating disorders (e.g., multiple sclerosis) Multiple Sclerosis = an inflammatory disease in which the fatty myelin sheaths around the axons of the brain and spinal cord are damaged, leading to demyelination and scarring - typical onset 20-40yo - Sy’s: fatigue, mm weakness, paraesthesia, optic neuritis or diplopia, vertigo, Jason Shane and Amanda Mrsic Apr 2015 bowel and bladder, impaired cognition/memory, pain, depression Types: Relapsing remitting – new symptoms or old symptoms may resurface or worse and it can be full or partial recovery relapses can be days weeks or months recovery can be slow or instantaneous Primary progressive there is a gradual worsening of symptoms overtime may stabilize but no remission Secondary progressive – starts off as relapsing remitting then steadily worsens Progressive relapsing --there is a steady progression with attacks PT Rx: treat vestibular dysfunction, posture, proprioception, core, stretches Contraindications and precautions to exercise: heat, fatigue, pregnancy 01.02.07 Inflammatory/infectious conditions of nervous system (e.g., meningitis, Lyme disease) Lyme disease: from a bacteria, Borrelia burgdorferi, through ticks may occur in stages, stage 1) localized presentation, erythema, flu like stage 2) neuro (headache and neck stiffness) MSK and cardiac (tachy, brady, arrythmia, myocarditis) , may have Bells palsy 3) final stage: long term neuro, with arthritis(1/3) and cognitive deficits Info: mimics other diseases like MS, fibromyalgia, chronic fatigue syndrome, guillan barre Rx: antibiotics to treat PT management: relieve pain, prep deconditioned patients for home ex, ed re FITT w/out exacerbating symptoms, improve strength meningitis: infectious disease that causes inflammation of meninges (all 3: pia, arachnoid, dura) Info: increased risk of infarctions, cortical veins may develop thomboses, may be block of CSF secondary to scar tissue (can cause hydrocephaly - excess amount of fluid in the brain) which causes headache (the CARDINAL SIGN!) Presentation: can present as acute (hrs-days); sub acute (2wks plus); chronic (1mo plus) Types: 1) aseptic (fungus, virus, parasite, can also get with: herpes simplex 2, epstein barr, lupus) 2) tuberculosis: abscess or edema 3) bacterial: in child or infant is considered a medical emergency Physical test for meningitis: patient supine, passively flex neck, Brudzinski’s sign: Jason Shane and Amanda Mrsic Apr 2015 knees and hips will flex Creutzfeldt Jakob disease = caused by prions; is bovine spongiform encephalopathy in cows (mad cow disease); occurs in young adults, is a movement disorder/dementia; it is rapidly progressive and fatal Pathology - contracted by ingestion or via the nose; incubates 5-8yrs 01.02.08 Post-polio syndrome (from Wikipedia) - Poliovirus attacks neuron in brainstem + ant horn cells of spinal cord - Motor neurons controlling skeletal mm die - sprouting may occur = some recovery of movement = motor neuron enlargement - mm weakness and paralysis after years of metabolic stress on neuron - ongoing denervation and reinnervation, with overall loss of motor units 01.02.09 Cerebellar disorders -MS - hereditary ataxia, Friedreich’s ataxia -neoplastic, metastatic tumors -infection -vascular: stroke -developmental: ataxic cerebral palsy, arnold chiari syndrome -trauma: TBI -drugs: heavy metals -chronic alcoholism; acute alcohol poisoning, effects GABA receptors 1) archicerbellum lesions: central vestib system, gait and trunk ataxia 2) paleocerebellum lesions: hypotonia, trunk ataxia, ataxic gait 3) neocerebellum: intention tremor, dysdiadochokinesia, dysmetria, dyssynergia, errors in timing additional impairments: asthenia (generalized weakness), hypotonia, motor learning impairments, cog deficits, emotional dysregulation 01.02.10 Vestibular disorders cause of dizziness: cardiovascular, neurological, visual, psychogenic, cervicogenic, meds, vestibular 3 functions of vestibular: 1) gaze stabilization - objects in visual field stay clear with head movement; 2) postural stabilization - maintain balance and equilibrium; 3)resolution of sensory motor mismatch (proprioception, vestibular and visual)= sea sickness/motion intolerance anatomy: Jason Shane and Amanda Mrsic Apr 2015 semicircular canals x3; horizontal, anterior, posterior= GAZE/ angular displacement of the head otolith: utricle- detects horizontal plane motion, saccule- detects sagittal plane motion; together detect acceleration and deceleration= POSTURAL vertigo = the subjective experience of nystagmus (room spinning around you) - get it with BPPV dizziness = discrepancy between R and L side, patient can’t work out where they are in space oscillopsia = blurred vision antibiotic → GENTOMYCIN = affects vestibular system UVL-unilateral vestibular loss= peripheral dysfunction: cause- infection (vestib neuritis, labyrinthitis, disease (Menieres- too much endolymph squishes structures in the ear S&S: low freq hearing loss, tinnitis), trauma, BPPV) presentation: dizziness, oscillopsia, imbalance BPPV(UVL) = benign paroxysmal positional vertigo - displaced otoconia go to the posterior canal presentation: brief transient vertigo when looking up/down, rolling to that side in bed, sitting to supine -Dix Hallpike maneuver to test - head 45 deg to test ear, 30 deg ext, lower from sit to supine and keep for 30 sec +ve test nystagmus- delayed onset, brief and rotary CI’s arthritis, vertebral art insufficiency, 5D’s Rx: modified Epley maneuver BVL: causes: toxicity, bilat infection, vestibular neuropathy, otosclerosis BVL presentation: very poor balance, NO DIZZINESS vestibular occular reflex= maintain stable vision during movement; deficient with unilateral and bilateral vestibular loss Central vestibular disorders= TIA, Stroke, head injury, brain tumor, MS, Ax: direction changing nystagmus recovery dependent on cortical reorganization motion sensitivity: 1) sensitivity to movement of the head - position change, repetitive movement, car train or boat travel 2) sensitivity to moving visual field - visual vertigo, ocular dizziness, reading Jason Shane and Amanda Mrsic Apr 2015 01.02.11 Neuropathies (e.g., peripheral neuropathies, complex regional pain syndrome) peripheral neuropathy = injury to peripheral N that may be due to injury or illness -mononeuropathy, mononeuritis, polyneuropathy, autonomic neuropathy, neuritis most common cause is from diabetes. can also be due to injury or other diseases like : lyme, HIV, shingles, Gullian-Barre Complex Regional Pain Syndrome (formerly known as Reflex Sympathetic Dystrophy)= a chronic pain condition believed to be the result of dysfx in central or peripheral NS Typical features: changes in the color and temp of the skin over the affected limb or body part, with intense burning pain, skin sensitivity, sweating, swelling, stiffness Stage 1 (0-3 mo) puffy swelling, redness, warmth, stiffness, allodynia, pos bone scan Stage 2 (3-6 mo) incrd P and stiffness, firm edema, cyanosis, atrophy, osteopenia on xray Stage 3 (6mo plus) tight, smooth, glossy, cool, pale skin; stiffness and contractures, nail and hair changes; severe osteopenia PT Rx: prevention and early detection → early ROM and use, P and edema mngmt (desensitization, contrast baths, modalities), education 01.02.12 Developmental/birth injuries (e.g., cerebral palsy, myelomeningocele, Erb’s palsy) Cerebral Palsy: CP: non progressive lesion of the brain that occurs before the age of 2, hearing and speech problems, hydroencephalus, microencephaly, scoliosis, hip dislocation, mental retardation - anoxia, haemorrhage (intraventricular, periventricular leukomalacia - most common ishcemic brain injury in premature babies) or brain damage risk factors: of mom is older, low birth wt, IVF (invitro fertilization) mono, di, tri, quad, hemi spastic: mm stiffness, dec ROM, movements limited to synergies - primitive movement patterns- trouble start/stop movement athetoid: slow twisting wide amplitude movements, changing of mouth positions ataxic: abnormal rate, range, force, duration of movements; difficulty with rapid move, gait, fine motor, balance dystonic: long sustained involuntary movements and postures hypotonic: lack of tone, weakness hip subluxation, spasticity of adductor longus and iliopsoas, dislocate posteriorly Rx: seating, botox to adductors, surgery, baclofen pump, tendon release, Jason Shane and Amanda Mrsic Apr 2015 PT: manage atypical mm, habituation, not rehab, positioning, orthotics, maintain ROM Sitting modifications-put pummel between legs Spina bifida: neural tube defect resulting in vertebral and/or spinal cord malformation 1) spina bifida occulta - no spinal cord involvement, may be indicated by hair tuft 2) spina bifida cystica - visible or open lesion a)meningocele - cyst includes cerebrospinal fluid cord intact b) myelomeningocele - cyst includes CSF and herniated cord tissue -link between maternal decreased maternal decreased folic acid, infection, exposure to teratogens (alcohol) -hydrocephalus - meningitis -foot deformities -talipes equinovarus (club foot) esp with L4, L5 level -latex allergy Erb’s palsy (waiters tip) - C5, C6, injury in infants, usually come out of birth canal - can affect: rhomboids, levator scapulae, serratus anterior, delts, supraspinatus, infraspinatus, biceps, brachioradialis, brachialis, supinator, long extensors of wrist, fingers, thumb Rx: immobilization initially, gentle ROM, play exercises Klumke (claw hand) -C8,T1 effect: intrinsic mm of hand, flexors and extensors of wrist and fingers Median N palsy (ape hand) - C6-8, T1 median N - impairment of thenar mm -can’t ABduct and oppose thumb 01.02.13 Dementia, affective and cognitive disorders Dementia: Impairment in: memory, language, visual spatial skills, cognition, personality – Most pts die of pneumonia -Mini Mental State Exam (MMSI) is most used outcome measure PT concerns: prevent falls, retain motor activities, reduce restlessness improve sleeping support for caregivers 01.02.14 Altered level of consciousness (e.g., coma, seizures) Coma = lowest level of consciousness - use GCS to assess; will not obey commands, open eyes, or interpret words Jason Shane and Amanda Mrsic Apr 2015 ● Epilepsy/ seizures - disturbances in CNS S&S: altered consciousness, motor activity (convulsions), sensory phenomena, autonomic, cognitive 1) primary generalized seizures - bilateral and symmetrical w/out local onset ● a) tonic-clonic (grand mal) - dramatic, whole body - 2-5 mins ● b) absence seizures (petit mal) - brief, almost imperceptible LOC, come back to full conciousness, no change in posture, can be up to 100/day 2) partial seizures ● a) simple - usually one part of the body - focal motor = clonic activity on specific area of body - focal motor with march (Jacksonian) - orderly spread or march of clonic movements; can progress to whole side - temporal lobe seizure - episodic change in behavior, complex hallucinations, ● b) complex partial seizures - simple partial seizures followed by impairment of consciousness NEUROANATOMY (Admit it, this reminds you of coloring class, who doesn’t like colored pens and pencils) ASCENDING TRACTS: Lat Spinothalamic - tests pain, hot/cold of limbs and trunk; receptors are free nerve endings sharp P is A delta fibers, slow/dull are type C fibers; ascends in lateral white column of spinal cord, crosses w/i 1-2 segments; finishes in parietal lobe (this lobe integrates sensory information from different modalities); IF HALF THE CORD has lesion, at the level there is ipsilateral loss, and contralateral loss below the lesion Ant (ventral) Spinothalamic- crude touch and pressure; receptors are Merckel discs and Ruffini corpuscles and free nerve endings; A delta and A beta; ascends in ant white column; crosses w/i 1-2 segments; finishes in parietal lobe as well; IF HALF THE CORD has lesion, at the level there ipsilateral loss, and contralateral loss below the lesion Dorsal columns (medial lemniscus)- 2-pt discrimination, fine touch, stereognosis, vibration; receptors are pacinian corpuscles (vibration), merckels’s disc, meissners (light touch); a beta; fibers cross in the brain stem; lesion below medulla=ipsilateral loss; lesion above medulla=contralateral loss; finishes in parietal lobe Jason Shane and Amanda Mrsic Apr 2015 DESCENDING TRACTS: Lateral corticospinal = primary motor tract; 90% cross in pyramids (part of the brain stem); synapses in ant horn cell in grey matter of spinal cord, goes out on an alpha motor neuron, terminates at the neuromuscular junction; LESION above level of medulla where they cross→ loss of vol mvmt contralateral to the lesion below level of medulla Anterior corticospinal = primary motor; 10% that cross at level of innervation; target lower motor neurons; start in frontal lobe; don’t cross in the pyramids; travel in ventral white column; IF LESION is on one side of the cord→ loss of 10% voluntary mvmt contralateral to the lesion CEREBRAL ARTERIES: Internal carotid artery= collateral supply is possible thru ant. and middle cerebral arteries; deficit=contralat. hemiplegia and hemisensory disturbance, global aphasia (if dominant side), mentally slow, contralateral homonymous hemianopia, partial Horner’s syndrome, gaze palsy (eyes to opp side); is the main supply for ant cerebral a., post CA, middle cerebral a. Anterior cerebral artery=weakness and sensory loss of contralat limbs, self care problems, emotional lability Middle cerebral artery= contralat hemiplegia, hemisensory loss, hemianopia, contralat neglect, aphasia(impaired language ability) if on dominant side, apraxia (disorder of motor planning, can’t carry out purposeful movements), impaired hearing, difficulty dressing, may also produce motor speech dysfunction (Broca’s area) Vertebral artery= two join to form basilar artery; imp branches to watch for strokes PICA (largest branch of vertebral a.), AICA, PCA Post cerebral artery (PCA)= supplies occipital lobes; vision problems, CN III palsy, contralateral hemiplegia, chorea (abnormal invol. mvmts, looks like dancing), hemiballismas (involuntary flinging mvmts of extremities), hemisensory impairment, contralat homonymous hemianopia, difficulty with naming and colors Superior cerebellar artery= supplies cerebellum, limb ataxia, Horner’s syndrome (droopy eyelid, red face), contralateral sensory loss Ant inf cerebellar= supplies cerebellum, ipsilateral limp ataxia, ipsilateral horner’s, sensory loss, facial weakness, paralysis of lateral gaze, and contralateral sensory loss of limbs and trunk PICA=supplies cerebellum, disarthria (poor articulation while speaking d/t motor issues), ipsilateral limb ataxia, vertigo, nystagmus, ipsilateral horners, sensory loss (p and temp) of face, Jason Shane and Amanda Mrsic Apr 2015 pharyngeal and laryngeal paralysis, contralateral sensory loss (p and temp) of trunk, visual sy’s (paralysis of vertical eye mvmts and decrd pupillary light reflex) Broca’s(receptive) aphasia= Broca’s area is located in the left frontal lobe Wernicke’s(expressive) aphasia= Wernicke’s area is located in the left temporal lobe Primary somatosensory= located in both parietal lobes, resp for all sensation Primary visual=located in both occipital lobes Primary auditory=located in both temporal lobes Olfactory area=located in both temporal lobes LEFT CVA mean most muscles on R side of body are affected. Also aphasias, used more reasoning, numerical and scientific skills, spoken and written language, sign language. RIGHT CVA means decreased musical and artistic awareness, spatial and pattern perception, recognition of faces, emotional content of language (speak in montotnous voice), discriminating smells, damage to right brodmann’s area have difficulty differentiating smells CRANIAL NERVES: 1) Olfactory - does smell; damage to can cause anosomia (inability to detect smells, seen with frontal lobe lesions) 2) Optic - does vision; damage to can cause homonymous hemianopsia (hemianopic visual field loss on the same side of both eyes. Hemianopias occur because the right half of the brain has visual pathways for the left hemifield of both eyes, and the left half of the brain has visual pathways for the right hemifield of both eyes) 3) Occulomotor - does pupillary reflexes; damage to can cause absence of pupillary constriction or Horner’s syndrome (combination of drooping of the eyelid (ptosis) and constriction of the pupil (miosis), sometimes accompanied by decreased sweating of the face on the same side; redness of the conjunctiva of the eye is often also present) 4) Trochlear - turns adducted eye downwards 5) Trigeminal - V1 sensory on face, V2 opthalmic branch (touch with cotton), V3 motor mm of mastication 6) Abducens - turns eye out 7) Facial - facial expression; damage to presents as inability to close eye, droopy corner of mouth, difficulty speaking; innervates ant aspect of tongue 8) Vestibular - balance, gaze stability, auditory; damage to can cause vertigo, nystagmus, deafness 9) Glossopharyngeal - phonation (voice quality), swallowing; damage to can cause dysphonia (hoarse or nasal voice); innervates the back of the tongue 10) Vagus - elevates the soft palate and controls position of uvula, gag reflex 11) Accessory (spinal) - innervates traps and SCM; damage to will cause inability to shrug ipsilateral shoulder (traps) or inability to turn head to opp side (SCM) 12) Hypoglossal - tongue movement; damage to can cause dysarthria or deviation of tongue to the weak side Jason Shane and Amanda Mrsic Apr 2015 SAMPLE LIST OF AREAS OF PRACTICE EVALUATED BY THE PCE (continued) 01.03 Cardiopulmonary-vascular (15%±5%) (This list is not necessarily exhaustive.) 01.03.01 Heart disease/malformation/injury (e.g., arteriosclerosis, blunt trauma, tamponade, aortic aneurysm) valvular heart disease: valves break; failure of valved to open completely thereby impede forward flow (stenosis), regurgitations(insufficiency): fail valve to close-reverse blood flow dilated cardiomyopathy: heart with increased mass, heart has trouble pumping; risks: third trimester, alcohol hypertrophic cardiomyopathy: hypertrophied heart, abnormalities in filling ; young athletes at risk of dying; S&S chest pain, SOB, sudden cardiac tamponade: compression of the heart due to blood or fluid buildup in the pericardial sac, may occasionally be the result of puncture wound through the heart during a procedure Sy’s-jugular distension, hypotension, muffled heart sounds arteriosclerosis = stiffening of the arteries; thickening and loss of elasticity hardening of arteries atherosclerosis: plaques into lumen and weakened underlying artery; heart attack, stroke, aortic aneurism; atheromas (plaques, cholesterol or lipids) form within the intima of artery aortic stenosis = calcification due to age or lipid accumulation; consequences: heart murmur, hypertrophy, angina, syncope aneurism = localized abnormal dilation of the wall of a blood vessel, all aneurisms may rupture causes; atherosclerosis, trauma, congenital defects most common site: abdominal aortic aneurism aortic dissection: chest pain, dissecting aneurism Blunt trauma to the heart: Flail Chest=multiple rib fractures, free floating rib section; Inspiration-flail segment sucks in→ lung, heart, mediastinum shift away, reducing air entry into the unaffected lung; expiration - flail segments pushes outward→ lung, heart, mediastinum are pushed toward flail segment Jason Shane and Amanda Mrsic Apr 2015 Rx-pain control, intubation/ventilation if necessary, O2, airway clearance, occasionally Sx pneumothorax= collapse of the lung due to air in pleural space; can be due to puncture of chest wall or lung spont bursts; hyperresonant percussion; aspirate or chest tube 1) open - stabbed- air into pleural space; 2) tension - v.serious! - open wound becomes sealed on expiration, air goes from affected lung into pleural space - on inspiration air will stay in pleural space, increase pressure on heart that can stop beating :( spontaneous pneumothorax- spont rupture of air containing space of lungs hemothorax- collapse of lung due to blood in pleural space ; less breath sounds 01.03.02 Myocardial ischaemia and infarction (including surgical interventions) Terrible Triad: (3 I’s) 1) Ischaemia= Inverted T waves, poor blood supply and hypoxia, occurs w/i seconds of onset and is REVERSIBLE 2) Injury= Elevated ST segment, myocardial tissue injured during MI occurs in 20-40mins, IS REVERSIBLE Depressed ST segment: inj to myocardial tissue, can occur during angina 3) Infarction= abnormal Q waves and QS complexes, can also be tall R waves NOT REVERSIBLE, occurs 2hrs after onset BRADYcardia <60bpm TACHYcardia >100bpm Ventricular fibrillation= incompatible with life = requires defib (shock!) - 1st degree AVblock= caused by prolonged conduction in AV node; P-wave normal Jason Shane and Amanda Mrsic Apr 2015 - 2nd degree AV block (2 types, mobitz 1 and 2) =block occurs at occurs at AV node and is transient; PR lengthens until totally blocked then NO QRS follows a P causing a missed beat (MOBITZ type 1) MOBITZ type 2: block occurs at bundle branches/bundle of His; abrupt drop of QRS, but PR interval normal - 3rd degree AV block: block at AV node, bundle of His OR bundle branches; complete disassociation between atria and ventricles, this produces independent atrial and ventricIular rate (atrial faster) - bundle branch block: in bundle branches and QRS is longer 01.03.03 Heart failure, CHF: congestive heart failure - heart is unable to pump blood at a rate required by tissues of the body, or it does so at elevated filling pressures - marked by breathlessness and abnormal retention of sodium and water resulting in edema with congestion of lungs or peripheral circ or BOTH - two types: systolic; deterioration of contractile function diastolic: can’t accommodate ventricular blood volume Right sided heart failure: common cause: L sided heart failure; damming of blood in periphery, congestion of the portal system: liver damage and enlarged spleen, dec flow in periphery, kidney and brain issues, pitting edema Left sided heart failure: due to: damming of blood in pulmonary circulation; SOB when lying, nocturnal gasp of breath when sleeping, kidney and brain dec perfusion cor pulmonale: failure of the R side of heart; due to chronic severe pulm HTN: emphysema and chronic bronchitis (COPD) ischemic heart disease: caused by myocardial ischemia; S&S angina, MI, sudden cardiac death 90% due to atherosclerosis angina pectoris: paroxysmal (short and frequent) recurrent episodes of chest discomfort caused by transient myocardial ischemia: stable, unstable, prinzmetal(variant) occurs at rest MI: release troponin and creatine kinase 01.03.04 Tumour (oh, sorry, tumors are on the blueprint THREE times!!!) Jason Shane and Amanda Mrsic Apr 2015 LUNG CANCER: 2 types: 1)small cell: 20-25%: develops in bronchial cell mucosa, spread rapidly, and metastasize early 2) non-small cell: - 1) squamous cell - spread slow, arise in central portion near hilum, mets late - 2) adenocarcinoma- 35-40%- slow to mod spread, early mets throughout lungs brain and other organs - 3) large cell - rapid spread, wide spread mets, kidney, liver, adrenals, poor prognosis risk: SMOKING OF COURSE! PT management: manage fatigue Brain tumours = 2nd to stroke, is #1 cause of death (in the brain) 50% chance of survival, kills more ppl than MS and lymphoma, sig cause of death in kids (intra-tentorial) 1) intracerebral primary = tumors neurons don’t proliferate (other cells around proliferate) 2) intracerebral metastatic = come from lung, breast, prostate - compensate by dec brain tissue vol, CSF vol and blood flow vol 3) Intra-spinal- signs: N root pain, worse at night, pain with cough, radicular pain Rx: surgery or radiation low grade astrocytoma - benign, good survival if treated early anaplastic astryocytoma - aggressive medulloblastomas - freq metastasize to other spots in brain and spine neuronomas: a) schwannoma - cranial N 8 (vestibular) S&S headache and seizure, nausea, vomit, cognition and behavior 01.03.05 Pneumonia (primary or post-operative/preventive) inflammation of parenchyma of lungs (lung tissue); could be caused by: 1) bacterial, viral or fungal, 2) inhalation of toxic chemicals (smoke, dust, gas), 3) aspiration; normally airborne pathogens most are preceded by an upper respiratory infection followed by sudden and sharp chest pain, coughs up green sputum, can also have dyspnea, tachypnea Rx: antibacterials/antibiotics, airway clearance techniques, antifungals (if fungal infection), oxygen support, positioning - Hospital acquired pneumonia has a higher mortality rate than community typical (sudden onset of symptoms - bacterial often, fever, sputum, physical sign of consolidation) and; atypical (walking- no symptoms, little sputum, min chest signs) aspiration: impaired consciousness- alc abuse, after surgery, neuro disease Jason Shane and Amanda Mrsic Apr 2015 01.03.06 Atelectasis (primary or post-operative/preventive) Atelecatsis = collapse of normally expanded and aerated lung tissue at any structural level involving all or part of the lung; can be patchy, segmental or lobar distribution can be due to: 1) blockage of bronchus/bronchiole, lung is prevented from expanding due to: paralysis, diaphragmatic disorders, mucous or airway obstruction, hypoventilation; 2) compression due to pneumothorax, pleural effusion, space-occupying lesion (tumor) which prevents alveoli from expanding; 3) postanesthetic - effects of anaesthesia and prolonged recumbency Presentation: x-ray=shifting of lung structures toward collapse, if involves entire lobe may show a shadow; quiet breath sounds, possibly dyspnea, tachypnea, cyanosis Rx: identify underlying cause, suctioning if d/t secretions, chest tube if d/t pneumo/hemo thorax or extensive pleural effusion 01.03.07 Adult/infant respiratory distress syndrome (e.g., acute lung injury) ARDS: acute respiratory failure with severe hypoxemia as a result of pulmonary or systemic problem; lung injury characterized by increased permeability on alveolar capillary membrane; leakage of fluid and blood into lung interstitium and alveoli INFLAMMatory reaction; alveolar edema and collapse causes: severe trauma; aspiration; embolism; indirect- happen after viral infection or pneumonia key feature on x-ray = WHITE OUT Rx: PEEP to keep airways open, tackle underlying cause, PRONE position SARS: severe acute respiratory syndrome = viral resp illness; unlike the flu, will get pneumonia if you have SARS abscess: infection leading to necrosis of lung tissue and cavity formation IRDS: occurs in infants whose lungs have not fully developed; lack surfactant (helps lungs inflate with air and keeps the sacs from collapsing) risks: prematurity, c-section, multiple preggers, blue baby, stop breathing, grunts Rx: deliver artificial surfactant hypoxemic resp failure (gas exchange failure): arterial hypoxemia - low blood O2, no inc in CO2, due to: pneumonia, ARDS, obstructive lung disease, pulmonary embolism hypercapnic resp failure: too much CO2 in the blood, leads to dec O2 in the blood, due to dec ventilation (depress of resp ctr by drugs), acute upper/lower Jason Shane and Amanda Mrsic Apr 2015 airway obstruction, weak/impaired resp mm, SCI 01.03.08 Asthma chronic inflamm of the lungs characterized by variable airflow limitation and hyperresponsiveness; chronic inflamm disorder of airways - airway hyper-responsiveness: recurrent episode; wheezing, breathlessness, chest tightness, coughing (often reversible unlike COPD), smooth mm contraction gas exchange normal, hyperinflated during attack, normal elastic recoil, exercise capacity reduced, allergic exposure- child or adults 2 categories: 1) extrinsic - allergic or atopic - normally due to allergen; mast cells release mediators which cause bronchospasm and hypersecretion - KIDS more 2) intrinsic - non allergic- hypersensitivity to bacteria, virus, drugs, cold air, stress - ADULTS more Rx: prevent triggers, pharmacological - inhaled corticosteroids exercise induced: smooth mm constrict - upright, lean forward and pursed lip breathing 01.03.09 Chronic obstructive pulmonary disease (e.g., emphysema, bronchitis, bronchiectasis) COPD= chronic resp condition characterized by progressive airway obstruction that is not fully reversible, gas exchange is normal, always hyperinflated, decreased elastic recoil, age of onset middle aged to older adults Rx: pharmacological 2 focuses, 1) smooth mm relaxation, 2) reduce airway inflammation O2 therapy, BUT NOT FOR Pts with pulmonary HTN, CHF Bronchiectasis: irreversible destruction(necrosis) and dilation of the airways with chronic bacterial infection; excess mucus, can be caused by CF, TB, and endobronchial tumors; eventually alveoli replaced with scar tissue due to chronic inflamm Rx: bronchodilators, antibiotics, secretion clearance Bronchitis: excess mucus production Emphysema = pathological diagnosis, destruction of air spaces distal to the terminal bronchiole with destruction of alveolar septa which causes merging of alveoli into larger air spaces→ this reduces the surface area for gas exchange; loss of airways and capillaries as well; Impact: hyperventilation put the diaphragm at mechanical disadvantage (it’s flattened) Jason Shane and Amanda Mrsic Apr 2015 01.03.10 Restrictive pulmonary disease (e.g., fibrosis) interstitial lung disease: stiff, less compliant lungs (not airway obstruction) S&S dyspnea, severe O2 desaturation, finger clubbing, scarring on CT Rx: O2 therapy, lung transplant, pulmonary rehab pulmonary fibrosis: ⅔ no known cause; ⅓ TB, inhaling harmful particles, radiation therapy, meds idiopathic pulmonary fibrosis: scarring and fibrotic tissue asbestosis: caused by inhaling harmful particles pneumoconiosis (coal workers lung): 01.03.11 Tuberculosis (mycobacterium tuberculosis) - infectious, inflamm systemic disease that affects lungs and may disseminate to involve kidneys, growth plates, meninges, avascular necrosis of hip jt, lymph nodes and other organ - airbourne particles S&S: productive cough 3+wks, wt loss, fever, night sweats, fatigue, bronchial breath sounds TB skin test: inject in forearm: determine of body’s immune response has been activated by TB before medical management: 10 drugs PT: thorough history and self protection (masks etc) 01.03.12 Pleural effusion accumulation of fluid in the pleural space due to disease - this can impair breathing by limiting expansion of the lungs transudate: commonly due to heart fail - low protein, clear exudate: formation of fluid by inflammation or disease, caused by infection or Jason Shane and Amanda Mrsic Apr 2015 cancer of the pleura - opaque symptoms: SOB, chest pain, percussion - dull, decreased or ABSENT breath sounds, may hear a pleural rub may cause mediastinal shift 01.03.13 Pulmonary edema increased fluid in extravascular spaces of the lungs; may be increased hydrostatic pressure due to heart or kidney failure - pushes fluid out of vessels, or increased alveolar permeability (drug induced, ARDS, inhalation of noxious gas) presents as stiffer lungs - incrd work of breathing, and dyspnea classic symptom: cough that produces a frothy pink tinged sputum on auscultation: FINE CRACKLES Pulmonary embolus = bloody sputum, dyspnea, incrd RR, SOB, cyanotic, 01.03.14 Cystic fibrosis - inherited autosomal disorder that affects all exocrine glands results in defective Cl- excretion and Na+ absorption = THICK MUCUS - can get: recurrent chest infections, consolidation, atelectasis and thickened bronchial walls - diagnose with fam history, sweat test - chloride content of sweat, 2 copies of abnormal gene - respiratory symptoms most common; also get: finger clubbing, breathlessness, delayed puberty and skeletal maturity, infertility in males, symptomatic steatorrhea, diabetes mellitus, liver disease, osteoporosis Rx: airway clearance techniques, bronchodilators, aggressive antibiotics 01.03.15 Peripheral arterial disease account for 95% of arterial occlusive disease; atherosclerosis is the underlying cause S&S -occur distal to site of narrowing or obstruction; intermittent claudication, acute ischemia (pallor, pain paralysis, pulseless), ulceration and gangrene, skin (shiny, thin, hairless); often occurs in feet Outcome-decreased mobility d/t pain and loss of function or limb PERIPHERAL VASCULAR DISEASE: (same as peripheral artery disease) - artherosclerotic obstruction of iliac, femoral, and politieal arteries in the legs - feel pain during physical activity, most often in the calf - pathologic conditions of blood vessels that supply extremities and major abdominal organs underlying cause: atherosclerosis S&S: intermittent claudication, dec pulses, ulcers, cool skin, limit mobility, pain or loss of function of limb Jason Shane and Amanda Mrsic Apr 2015 01.03.16 Venous disorders THROMBOPHLEBITIS - partial or complete occlusion of a vein by a thrombus with secondary inflammation - superficial or deep DVT - can become pulm emboli S&S: tender calf (d/t thrombus in calf vein), fever, test with Homan’s; risk is it may become a PE CHRONIC VENOUS INSUFFICIENCY - inadequate venous return over a prolonged period - cause: DVT trauma, obstruction by tumor, - damaged or destroyed valves lead to venous stasis, can get edema, thickening brown skin and ulcers Varicose veins = faulty valves cause abnormal dilation of veins leading to twisting and turning of the vessel; at risk for thrombosis (Don’t even know how many times we’ve learned this diagram over the years) Jason Shane and Amanda Mrsic Apr 2015 Volumes TIDAL VOLUME (TV): Volume inspired or expired with each normal breath. (500mL) INSPIRATORY RESERVE VOLUME (IRV): Maximum volume that can be inspired over the inspiration of a tidal volume/normal breath. Used during exercise/exertion. (2-3L) EXPIRATORY RESERVE VOLUME (ERV): Maximal volume that can be expired after the expiration of a tidal volume/normal breath.(1L) RESIDUAL VOLUME (RV): Volume that remains in the lungs after a maximal expiration. CANNOT be measured by spirometry(1L) Capacities: INSPIRATORY CAPACITY ( IC): Volume of maximal inspiration: IRV + TV (2.5L-4L) FUNCTIONAL RESIDUAL CAPACITY (FRC): Volume of gas remaining in lung after normal expiration, cannot be measured by spirometry because it includes residual volume: ERV + RV(2L) VITAL CAPACITY (VC): Volume of maximal inspiration and expiration: IRV + TV + ERV = IC + ERV (3-4.5L) TOTAL LUNG CAPACITY (TLC): The volume of the lung after maximal inspiration. The sum of all four lung volumes, cannot be measured by spirometry because it includes residual volume: IRV + TV + ERV + RV = IC + FRC (4-6L) DEAD SPACE: Volume of the respiratory apparatus that does not participate in gas exchange, approximately 300 ml in normal lungs. --ANATOMIC DEAD SPACE: Volume of the conducting airways, approximately 150 ml --PHYSIOLOGIC DEAD SPACE: The volume of the lung that does not participate in gas exchange. In normal lungs, is equal to the anatomic dead space (150 ml). May be greater in lung disease. FORCED EXPIRATORY VOLUME in 1 SECOND (FEV1): The volume of air that can be expired in 1 second after a maximal inspiration. Is normally 80% of the forced vital capacity, expressed as FEV1/FVC. In restrictive lung disease both FEV1 and FVC decrease , thus the ratio remains greater than or equal to 0.8. In obstructive lung disease, FEV1 is reduced more than the FVC, thus the FEV1/FVC ratio is less than 0.8. CARDIAC REHAB 3 goals: - 1) restore optimal function - 2) prevent progression of underlying processes - 3) reduce the risk of sudden death and re-infarction S&S of cardiopulmonary disease: pain in chest, neck, jaw, arms; SOB at rest or mild exertion; dizzy or syncope; orthopnea (SOB while lying flat) or nocturnal dyspnea, ankle edema, palpitations or tachycardia, intermittent claudication, known heart murmur, unusual fatigue exercises to avoid: NO VALSALVA!; extensive upper body activity; isometric/ Jason Shane and Amanda Mrsic Apr 2015 static exercises; PHASES: phase 1: inpatient phase 2: outpatient 12 week program phase 3: in the community cardiothoracic index = size of heart in relation to thorax 01.04 Multisystem (15%±5%) (This list is not necessarily exhaustive.) 01.04.01 Episodic disease (e.g., oncology, HIV/AIDS, autoimmune disorders, rheumatic diseases, haemophilia) Oncology: (the Alliance is being sneaky this time, they’re calling it “oncology” instead of tumors) Staging cancer: - TNM: Tumor (extent/spread), Nodes (lymph), Mets (distant ones) PT relevant Rx: PT’s can teach Pt’s to stretch mm when radiation therapy begins to mitigate occurrence of contractures Physical activity: - During Rx - improves QOL, physical Fx, fatigue; Precautions-severe anemia, immune compromised, severe fatigue - Following Rx - goals are to have appropriate weight, be physically active, healthy diet - ACSM guidelines - prescription must be individualized according to cancer survivors pre-Rx aerobic fitness, medical comorbidities, response to Rx, and the neg side effects of Rx Clinical presentation of cancer survivors: fatigue, myalgia, arthralgia, bone health, peripheral neuropathy (impact on balance), deconditioning Palliative Care: Goals are to provide comfort, support, maximize independence; PT’s can help with respiratory, stress reduction, education AIDS: acquired immunodeficiency syndrome - caused by hiv1 or 2; loss of immune system function; can get pneumonia, Tb, malignancy, encephalitis, meningitis, dementia, herpes zoster - reduction of CD4+ helper T cells - transmission through contact with infected body fluids: blood, saliva, semen CSF, breast milk, vaginal/cervical secretions NOT: urine, sweat, vomit diagnosed with clinical findings and systemic evidence - AIDS - related complex (precursor to full blown AIDS) - lab evidence: HIV -1 antibody test, CD4 cell count 200-500/ml (normal = 800-1200/ml Jason Shane and Amanda Mrsic Apr 2015 - no cure med interventions = 1) multidrug antiviral therapy 2) symptomatic treatment: maintain nutrition, maintain functional mobility, education, - PT goals: use precautions when working, exercises- mod aerobic, strength, avoid exhaustive, acute = reduce to mild levels, activity pacing, energy conservation, stress management Autoimmune disorders: Guillan Barre Syndrome = antibody mediated demyelination of schwann cells; see a generalized inflammatory response Presentation: initially see a “socks and gloves” pattern of areas that initially go numb; is perfectly symmetrical; maximal weakness occurs in 2-3 weeks and takes months to recover; absent deep tendon reflexes Rx: plasmapheresis, Iv administration of immunoglobulin (decreases the immune response) PT Rx: early on - prevent ulcers (posning), early PROM; later - mm strength Connective tissue disorders that may involve skin as well as organs: Lupus erythematosus - can involve kidney, CNS, cardiac, pulmonary; on skin may find BUTTERFLY rash, localized erythema and edema, alopecia (loss of hair), photosensitivity, mucosal ulcers, Raynaud’s (fingers are cold sensitive), effusion in joints; associated with positive serum “antinuclear antibodies” (ANA) Sclerodema-autoimmunity provokes massive fibrotic tissue response which may lead to joint contractures, pulmonary fibrosis, GI dysmotility (esp esophagus) Dermatomyositis and polymyositis=inflam connective tissue disorders characterized by proximal limb girdle weakness, often w/o P. Dermatomyositis- affects both skin and mm; is also assocd. w/ a photosensitive skin rash, purplish erythematous eruption over face (esp upper eyelids), hands, forearms Polymyositis- mm only Haemophilia: Type A - is the most common of hereditary clotting factor deficiencies X-linked recessive (Males have the condition, and the gene that causes it is carried by women) - If the mother carries the haemophilia gene and the father does not have haemophilia: A male child will have a 50:50 chance of having haemophilia. A female child will have a 50:50 chance that she will carry the haemophilia gene. - If the father is affected by haemophilia and the mother is not a carrier: A female child will be a carrier (she is known as an obligate carrier). A male child will not be affected by the haemophilia gene and cannot pass Jason Shane and Amanda Mrsic Apr 2015 haemophilia onto his future children. Presentation: profuse post circumcision bleeding, joint and soft tissue bleeding, excessive bleeding, operative and post-traumatic hemorrhage Signs and Symptoms: ● Big bruises; ● Bleeding into muscles and joints, especially the knees, elbows, and ankles; ● Prolonged bleeding after a cut, tooth removal, surgery, or an accident. ● Serious internal bleeding into vital organs, most commonly after a serious trauma Bleeding in the joints is the most common problem. The symptoms of a joint bleed are as follows: ● Tightness in the joint with no real pain. ● Tightness and pain before any bleeding ● Swollen and hot to touch, hard to move ● All movement lost, severe pain ● Bleeding slows after several days when the joint is full of blood There can be disabling arthritis if this is not treated. Rx: recombinant factor VIII infusion; note, before VIII available many Pts received blood products in the 80’s and died of AIDS and many got Hep C Desmopressin (or DDAVP) can be used for sufferers of mild haemophilia - Rheumatic diseases: Rheumatoid arthritis: synovitis is the main feature; synovium becomes swollen and cells proliferate→ a dense cellular membrane (pannus) spreads over articular cartilage and erodes the underlying cartilage and bone; over time the pannus may extend to the opposite articular surface creating: 1) fibrous scar tissue, 2) adhesions, 3) bony ankylosing; immobility and consolidation (bones form a single unit) of a joint; bones can become osteopenic and ligaments and tendons become damaged or ruptured; surrounding mm deteriorate leaving joint unstable and prone to deformity symmetrical pattern Criteria for RA: - morning stiffness >1hr (6 weeks), arthritis of >/= 3 joints (6 weeks), arthritis of hand joints, symmetric arthritis (6 weeks), rheumatoid nodules, serum rheumatoid factor, radiographic changes Have an abnormal antibody HLA-DR4 in 80% of people with RA Increased risk: after mother gives birth, cigarette smoking, pollution Clinical features: pain, fatigue, stiffness (decreased ROM), swelling, joint deformity, mm atrophy Management: Meds (DMARDs, NSAIDs, tylenol, cortisone) Jason Shane and Amanda Mrsic Apr 2015 Rehab: Acute phase- energy conservation, ice, splints, gentle ROM, NO STRETCHING as it may stretch the synovial membrane and cause irreversible damage Chronic phase- relieve pain, i.e. modalities, splints, exercise (gentle ROM), relaxation/rest; Reduce stiffness-gentle ROM, aquatic ex, heat; functional ex’s, prevent deformity Inflam conditions: - pain worse in morning, morning stiffness greater than 1hr Non-Inflam condition: - yes, after used, morning stiffness less than 30min Joint count assessment = an indicator of the disease activity of RA 1) Joint effusion 2) joint line tenderness 3) stress pain Commonly affected joint in RA: 1) atlanto-axial joint (esp transverse lig) ● S&S of atlanto axial subluxation - clunking in repositioning in Sharp Purser test, dysphagia, dizziness, blurred vision 2) TMJ - end stage may result in fusion of open bite 3) Shoulder - humeral head moves superiorly 4) AC joint 5) elbow - loss of extension, i.e. flexion deformity; superior radioulnar joint commonly involved→ erosion of radial head 6) hip (groin P, flexion deformity) 7) knee - baker’s cyst, flexion deformity, valgus deformity, quad wasting RHEUMATIC Con’t: Hallux valgus - 1st MTP synovitis, big toe is lateral, lig laxity and erosion, sublux→ dislocation, prox phalanx drifts lat, causes pronation of midfoot MTP subluxation - synovitis, displacement of the flexors, unopposed extensors pull the prox phalanx into hyperext, metatarsal head prolapses and get dislocation and lat drift of toes: Sign = callouses Claw toe - MTP synovitis, MTP ext, PIP+DIP flex, often all toes except big toe Hammer toe - MTP and PIP synovitis, usually involves 2nd toe, flex of PIP and hyperext of DIP (similar to boutonniere) Mallet toe - flex of DIP, affects longest toe Swan neck - (rheumatoid) flex of MCP(not always), hyperext of PIP, flex DIP Boutonniere - zig zag deformity - MCP hyperext (not always), flex of PIP, hyperext of DIP Jason Shane and Amanda Mrsic Apr 2015 Gout = Genetic disorder of purine metabolism, incrd serum uric acid (hyperuricemia). ● Acid ▲ to crystals and deposits into jts, ● most= knee and great toe of foot ● Meds: NSAIDS, cox2-inhibitors, corticosteroids, ACTH ● PT goals: injury prevention ed, fast intervention Osteoarthritis=release of enzymes and abnormal biomechanical forces cause fibrillation and damage of articular cartilage leading to cartilage loss; increase in bone turnover→ osteophytes 7 risk factors: 1) age, 2) sex (more women), 3) genetic, 4) obesity, 5) physical inactivity, 6) injury, 7) joint stress(occupation) Dx by x-ray finding: 4 main features 1) joint space narrowing, 2) osteophytes, 3) subchondral cysts, 4) subchondral sclerosis Sources of pain in OA: - bone, soft tissue, inflammation, mm spasm 4 questions to diagnose OA: 1) pain most days in last month, 2) pain over the last year, 3) worse with activity, 4) relieved with rest 3 tests indicative of OA of the knee: 1) flexion contracture, 2) abnormal gait, 3) swipe test or patellar tap Main joints it affects: ● Spine - osteophytes in facet jts of l-spine can cause stenosis ● Shoulder and Elbow - uncommon ● Wrist - uncommon unless scaphoid fracture or avascular necrosis ● Hand - PIP is Bouchard node, DIP is Hebernen’s node; CMC joints (esp thumb) ● Knee - most common jt affected by OA, varus, flexion contracture, crepitus ● Hip - walk with trendelenburg, groin pain, osteophytes, flexion deformities Types of FAI (femoral acetabular impingement): Cam - decrease or absent waist of the jx of femoral neck and head; during hip flexion the abnormal femoral head drives into acetabulum, most common in young men Pincer - d/t abnormal acetabulum that provides excessive cover of the femoral head, retroverted or deep acetabulum; impingement occurs when femoral neck pushes against overarching acetabulum; more common in women age 30-40 years ● Ankle - uncommon Jason Shane and Amanda Mrsic Apr 2015 ● Foot - first metatarsal joint; osteophytes can form at this jt causing hallux valgus and rigidus, may have bunions Rx: First line-exercise, weight loss, acetaminophen Spondyloarthritis: don’t have a rheumatoid factor, common in the spine Common features - inflammation in the spine (spondylitis and sacroiliitis), synovitis (affecting peripheral joints) typically unilateral, inflammatory of the eye (iritis/uveitis and conjunctivitis), no rheumatoid factor (seronegative), can be hereditary HLA-B27 Spondyloarthritis Rx: Meds - DMARDs, NSAIDs, corticosteroids, biologics Physical Management - control/decrease inflammation, P management, reduce stiffness/increase ROM, posture correction, increase mm strength and endurance, increase cardio Psoriatic Arthritis: Pt has psoriasis, M=F, can begin with kids, Chronic, erosive, inflamm most common = digit jts and axial skeleton Dactylitis = sausage like fingers d/t swelling; Enthesitis = usually in heels and back Meds: acetaminophen, NSAIDs, DMARDs, corticosteroids, biological response modifiers PT goals: jt protections strategies, maintain jt mechanics, endurance Enteropathic Spondylitis - assocd with ulcerative colitis (affects just the lower half of the bowels) and Crohn’s disease (affects the whole digestive system, it’s worse), may affect spine and SI joint Reactive arthritis - triggered by infection (possibly STI) in bowel or GI tract, hot swollen joints, may go away and come back Ankylosing spondylitis - stiffness/fusing of the spine by inflammation, disease of young adults; associated with genetic marker HLA B27 - Features: - MSK: sacroiliitis, enthesitis, synovitis; other signs-eyes, bowels, lungs, heart - The hallmark sign is sacroiliitis; may also feel deep, dull pain in buttuck area d/t inflammation of SI joint; fusion can occur over time Jason Shane and Amanda Mrsic Apr 2015 Enthesitis - inflammation of entheses leading to bony erosion and overgrowth; common sites are spine, hip, peripheral regions; syndesmophytes (bony spurs on 2 sides of a joint) can also cause bony fusion and rigidity (entheses = where tendons, ligs, and joint capsule attach to bone) Synovitis - usually affects peripheral jts, commonly shoulders, hips, knees, ankles Clinical criteria of AS = LBP and stiffness for more than 3 months that improves with ex but is not relieved with rest, limitation of motion of L-spine (d/t pain, tissue contractures, mm guarding, fusing), limitation of chest expansion (diaphragmatic breathing pattern), decreased strength d/t disuse, joint effusion, and pain, flexion posture, fatigue d/t disease process, cardiac involvement, decrd vital capacity Quick overview: onset before 40, low back pain, sacroiliitis, kyphotic deformity Csp, Tsp, dec lumbar lordosis, M>F Meds: NSAIDS, corticosteroids, cytotoxic, tumor necrosis factor Diagnosis – HLA-B27 PT goals: trunk flexibility, endurance, increase resp function (relaxation) Physical Ax - posture (tragus to wall), lateral trunk flexion, trunk flexion (modified schober's), trunk extension (smythe test), trunk rotation, chest expansion, cervical mobility Juvenile Idiopathic arthritis - signs and Sy’s must be present for 6 weeks to make diagnosis, avoid resisted ex’s with active disease, P does not indicate joint damage; improved strength (non-active period of the disease) reduces P and increases stability - complete remission in 75% of kids if occurs before age 16 - Sy’s-joint pain, stiffness, warm swollen joints, eye issue (uveitis), HLA-B27, fatigue, Erythrocyte sedimentation rate, rheumatoid factor Inflamm back pain - usually prolonged, >60min, max P and stiffness in early AM, chronic, age of onset 12-40 years, radiographs show sacroiliitis, syndesmophytes, and spinal ankylosis Mechanical back pain - minor <40min, max P and stiffness late in the day, activity worsens Sy’s, acute/chronic, 20-65 yrs, radiographs show osteophytes, disc space narrowing, misalignment 01.04.02 Metabolic disorders/conditions (e.g., diabetes) Jason Shane and Amanda Mrsic Apr 2015 DIABETES Hypoglycemia=dizzy, nausea, weak, sweating profusely (this rules out orthostatic hypotension) Hyperglycemia=blurred vision, fatigue, thirst, frequent urination 01.04.03 Chronic pain/fibromyalgia Chronic pain = pain that persists past the normal time of healing Chronic fatigue syndrome=may be viral ● Dx: by exclusion; persistent or relapsing fatigue for at least 6 months, not resolved with bed rest, reduces daily activity by at least 50% ● Rx: Analgesics, anti-inflamm, NSAIDS, nutrition, psych support ● PT Rx: check ex tolerance Fibromyalgia = chronic pain syndrome affecting mm and soft tissue (nonarticular rheumatism) ● Etiology: unknown ● Sy’s - headaches, sensitivity to stimuli, fatigue, myalgia (mm pain), generalized aching, sleep disturbances ● Anxiety and depression are common; more common in women ● 11 of 18 points: 1) Occiput (suboccipital insertions), 2) low cervical (ant aspects of intertransverse spaces at C5-C7), 3) Traps (mid-pt of upper border), 4) Supraspinatus (at origin), 5) Second rib (lateral to 2nd costochondral junction),6) lateral epicondyle, 7) gluteal, 8) greater Jason Shane and Amanda Mrsic Apr 2015 ● ● trochanter, 9) knee (at medial fat pad proximal to joint line) Rx: anti-inflamm, mm relaxants, pain meds, psychological support, nutrition PT Rx: energy conservation, aquatic therapy 01.04.04 Lymphedema = lymph accumulating in tissues 2 types: ● Primary - rare, inherited condition caused by problems with the dvlpmt of lymph vessels ● Secondary - d/t identifiable damage to or obstruction of normally functioning lymph vessels and notes;ex-Sx, radiation, parasitic infections Fx of lymph system: - removal from body tissues of fluid, proteins, bacteria, viruses - smooth mm in walls contract to move lymph Risk factors: radiation, age, axillary node dissection, arm infection/injury, obesity, weight gain since operation Prevention: skin care (avoid trauma/injury to reduce infection), activity (and maintain body wt), avoid limb constriction, avoid extreme temperatures Role of PT’s: exercise (weight loss), education on what to avoid (BP cuffs), educating on signs and symptoms Rx: compression garments, manual lymph drainage, manage risk factors [Cording = tight fibrous bands that go from axilla to elbow or wrist and restrict ROM] 01.04.05 Sepsis - body has severe response to bacteria or other germs; whole body inflammatory state; have SIRS and a proven infection - SIRS = systemic inflammatory response syndrome; whole body inflammatory state diagnose with body temp, HR, RR, WBC count 01.04.06 Obesity Excess body fat; BMI=weight (kg)/height (m)^2 - overweight BMI= 25-29.9 - OBESITY= BMI > or = to 30 - morbidly obese > or = to 40 skin caliper test fat greater than 1 inch is excess ● health risks associated with obesity: HTN, hyperlipidemia, type 2 diabetes, cardiovascular disease, glucose intolerance, gallbladder disease, menstrual irreg, infertility, cancer ● abdominal obesity = independent predictor of morbidity and mortality ● causes of obesity: excess calorie intake, psych/enviro factors, genetic factors, endocrine and metabolic disorders Jason Shane and Amanda Mrsic Apr 2015 Rx: lifestyle modifications, behavior therapy, pharmacology, surgery; exercise=moderate intensity 40-60% progress to 50-70% HRR, 5-7d/wk, 4560mins, circuits or aquatics 01.04.07 Pregnancy and post-partum conditions ● NORMAL = gain 20-30lbs ● postural changes = kyphosis, forward lean in Csp, lumbar lordosis, balance change, lig laxity (hypermobile SI - teach jt protections PT can teach: relaxation and breathing ex, provide ed, teach exercises to maintain abdominal and pelvic floor mm Diastasis recti abdominis = lateral separation or split of rectus abdominus; separation from midline >2cm sig; ab wall decrd support; get back pain pelvic floor disorders = due to stretching; can lead to partial or total organ prolapse - cystocele : herniation of bladder into vagina - rectocele: herniation of rectum into vagina - uterine prolapse: bulge of uterus into vagina - pelvic pain, urinary incontinence, pain with sexual intercourse PT Rx: pelvic floor mm ex, postural re-ed, low back and pelvic pain - PT Rx: teach body mechanics, balance activity and rest, massage, modalities for Pain SI dysfunction - post pelvic pain, buttock pain, may radiate to leg, pain with sit, walk, stand - PT Rx: external stabilization, ed on no single leg WB varicose veins - PT Rx: elevate extremities, elastic stockings preeclampsia = preg induced, acute HTN after 24wks gestation - PT evaluate for S&S: HTN, edema, headache, visual disturb, hyper-reflex C- section - PT Rx: TENS for incision pain, breathing ex, gentle ab ex, pelvic floor ex, postural ex, ambulation, prevent incisional adhesions (scar massage) 01.04.08 Burns Superficial Jason Shane and Amanda Mrsic Apr 2015 Partial Thickness Full thickness Zones: Zone of coagulation = point of maximum damage, irreversible tissue loss Zone of stasis = decrd tissue perfusion, potentially salvageable Zone of hyperemia = increased perfusion, will recover unless sepsis occurs Effects of burns: ● CV: Increased capillary permeability->interstitial edema; peripheral vasoconstriction; hypovolemia; myocardial depression->hypotension and decreased organ perfusion ● Resp: bronchoconstriction, ARDS ● Metabolism: increased 3x ● Immune system: compromised ● Renal: b/c of loss of fluids, vasoconstriction, decrd GFR, incrd myoglobin gets processed by kidneys and can block tubules Signs of inhalation injury: singed eyebrows/nasal hairs/burnt face, black oral/nasal discharge, swollen lips, hoarse voice, abnormal oxygenation, Hx of being enclosed in closed room - Inhalation injury process: w/i 24hrs upper airway obstruction/pul edema; 2448 just pulmonary edema; 48 hrs plus bronchiolitis, alveolitis, pneumonia, ARDS - Mngmt of inhalation injury: early mobilization, breathing ex’s, post drainage Rx of burns: first 2-3 weeks AROM and PROM to maintain range, positioning, edema management, encourage ambulation, scar management BECAUSE as early as 1-4 days can get a scar tissue contracture Contraindications to exercise: exposed joint, fresh skin graft, DVT, compartment syndrome Sx: Split Thickness Skin Graft = uses skin graft, stitched, glued or sutured in place; immobile for 5 days Full Thickness Skin Graft=skin transplant Skin graft Rx: scar massage, sun protection, ROM, pressure garments, strengthening can begin in 3-4 weeks Scar from burns: 3 stages 1) 0-4 weeks Fibroblastic/proliferative, Jason Shane and Amanda Mrsic Apr 2015 2) 4-12 weeks early remodeling, 3) 12-40 weeks late remodeling/maturation Factors influencing scar: age, smoking, type of tissue, nutrition Therapeutic mngmt of scar: pressure garments, massage, moisture 01.04.09 Wounds/ulcers Ulcers Causes: Pressure (round sore), shearing (abrasion/scrape), friction (blisters can be a sign), deep tissue damage from banging or bumping (purple or bruising) 4 Stages of wounds: 1) reddened (non blanchable), 2) skin is broken, small crater, 3) deep crater,might be infected, may be black, dead tissue 4) deep through mm to the bone or joint 01.04.10 Skin conditions (e.g., dermatitis, psoriasis) Psoriasis = an autoimmune disease that affects the skin. - occurs when the immune system mistakes the skin cells as a pathogen, and sends out faulty signals that speed up the growth cycle of skin cells; i.e profound cutaneous inflammation and epidermal hyperproliferation - Plaques frequently occur on the skin of the elbows and knees, but can affect any area, including the scalp, palms of hands and soles of feet, and genitals. In contrast to eczema, psoriasis is more likely to be found on the outer side of the joint. - Fingernails and toenails are frequently affected (psoriatic nail dystrophy) and can be seen as an isolated sign. Psoriasis can also cause inflammation of the joints, which is known as psoriatic arthritis. Between 10—30% of all people with psoriasis also have psoriatic arthritis 5 Cardinal morphologic features: 1) placque (raised lesions), 2) well circumscribed margins, 3) bright salmon red color, 4) silvery micaceous (shiny) scales, 5) symmetric distribution - Complications: pruritus (desire to scratch), severe psoriasis is associated with increased risk of CVD and shortened lifespan - Rx: Topical creams containing glucocorticoids, tars, vitamin D or A; phototherapy with UV light; systemic therapy with immunosuppressive drugs such as methotrexate or cyclosporine; systemic prednisone usually not used Eczema (means “boiling over) = is a form of dermatitis, or inflammation of the epidermis (the outer layer of the skin); is an itchy, red, scaly disorder Two types: 1) Atopic dermatitis (“endogenous” eczema) - is an intensely itchy inflammatory skin disorder associated with “atopy” (predisposition toward developing certain allergic hypersensitivity reactions): asthma, hayfever, and Jason Shane and Amanda Mrsic Apr 2015 allergic conjunctivitis Presentation: itchiness is the most outstanding feature; can also be erythema, lichenification (thickening skin lines), excoriations (scratching or picking at skin) 3 Phases: 1) Infantile (2mo-2 years) - facial and extensor distribution 2) Childhood - dry skin, flexural distribution (popliteal and cuboid fossa) 3) Adult - atopic dermatitis generally improves with age, less flexural distribution, primarily affect the hands Rx: avoid irritating factors, moisturizers, topical glucocorticoids, oral antihistamines, UV 2) Contact dermatitis (“exogenous” eczema) a) allergic contact dermatitis-immune hypersensitivity to an allergen in contact with the skin (e.g. nickel, poison ivy) b) irritant contact dermatitis-contact of skin with something that primarily causes direct local irritation (harsh detergents, chemicals) Seborrheic dermatitis (dandruff)=occurs in areas of higher sebaceous gland activity (oily areas) such as scalp, face, central chest and back; is probably due to an excessive immune response to a yeast; Rx: antifungals Associated disorders: seen frequently in PD patients and Pt’s with neurologic disorders that decrease their mobility (eg stroke, TBI, SCI), as well as HIV infection 01.04.11 Tumours (covered elsewhere) 01.04.12 Competing diagnoses (management of 1° diagnosis is changed by 2° diagnosis) Graves disease = hyperthyroidism, autoantibodies stimulate the thyroid (TSH receptor), T3 and T4 (these inhibit the secretion of TSH) will be high, affects men>women Sy’s: fever, wt loss, exercise intolerance, goiters, bulging eyes (exophthalmos), tachycardia, decrd fertility Rx: betablockers for HR, anti-thyroid drug therapy, radioactive Iodine, Sx removal of thyroid Hashimoto thyroiditis= hypothyroid, autoimmune destruction of thyroid gland, T3 and T4 are low, TSH is high; affects men>women Sy’s: wt gain, cold intolerance, round puffy face, bradycardia, constipation, depression Rx: thyroid hormone replacement Jason Shane and Amanda Mrsic Apr 2015 Addison’s=autoimmune process against the adrenal cortex, fatal if not treated, great prognosis if treated Sy’s: weakness, fatigue, anorexia, hyponatremia, hypoglycemia, hyperpigmentation Rx: replace missing adrenal hormone with aldosterone and cortisol Cushing’s disease=chronic glucocorticoid (cortisol) excess (usually iatrogenic in Pts taking them for immunosuppression, can also get from cancer of adrenal gland Sy’s: moon face, central obesity, abdominal striations Rx: surgical if caused by tumor (tumor in pituitary or adrenal gland) PAEDS: Slipped capital femoral epiphysis = growth plate slips off the head of the femur Developmental milestones O’Sullivan pg 247 Infant reflexes diminished/gone 2-6 mo PRACTICAL COMPONENT LIST OF FUNCTIONS EVALUATED BY THE PCE (This list is not necessarily exhaustive.) 02.01 ASSESSMENT AND EVALUATION (35%±5%) Data Collection Obtain the following client information and interpret implications for intervention: Jason Shane and Amanda Mrsic Apr 2015 02.01.01.01 Past and current history (e.g., medical, surgical, developmental, psychosocial, current status/symptoms, concurrent and past treatments) 02.01.01.02 Results of tests and diagnostic procedures (e.g., imaging, laboratory tests, functional capacity evaluation, pulmonary function tests) 02.01.01.03 Medications (past and current) 02.01.01.04 Home/work/leisure/play environments, family and community support systems and resources 02.01.01.05 Client expectations and goals Tests/Measurements 02.01.02.01 Select and justify evaluation/assessment procedures based on client needs and expectations, responses, and best available evidence 02.01.02.02 Perform selected physiotherapy evaluations/assessments in a safe and accurate manner including handling all monitoring devices, equipment, or lines attached to or around client 02.01.02.03 Examine and evaluate neuromusculoskeletal, neurological, cardiopulmonary-vascular, integumentary and other systems using appropriate tests and measures 02.01.02.04 Examine and evaluate mental status (e.g., cognition, memory), hearing, and visual acuity as they relate to client’s participation in physiotherapy programs and attainment of goals 02.01.02.05 Screen for contraindications and precautions for treatment planning (e.g., medical issues; psychosocial issues; safety issues; language comprehension; educational needs; risk factors and mediators) 02.01.02.06 Observe client’s response to the physiotherapy evaluation/assessment and respond accordingly 02.01.02.07 Assess client need for assistive, adaptive, and protective devices (e.g., positional supports, mobility aids, orthotic or prosthetic devices) LIST OF FUNCTIONS EVALUATED BY THE PCE (continued) (This list is not necessarily exhaustive.) 02.02 INTERPRETATION, PLANNING, INTERVENTION, AND RE-EVALUATION (50%±5%) Data Interpretation 02.02.01.01 Develop a list of physiotherapy differential diagnoses and determine the most probably cause of client’s problem 02.02.01.02 Identify indications, barriers, precautions, and contraindications to treatment, using the best available evidence 02.02.01.03 Determine need for physiotherapy treatment, collaboration, consultation, or referral Prognosis Jason Shane and Amanda Mrsic Apr 2015 02.02.02.01 Determine the potential for recovery or decline with or without physiotherapy intervention Goal Setting and Care Planning In consultation/collaboration with the client and family: 02.02.03.01 Establish short-and long-term goals that are client-centred; and specific, measurable, attainable, relevant and time-based (SMART) 02.02.03.02 Identify which aspects of intervention involve consultation, collaboration, delegation, and/or referral 02.02.03.03 Prioritize client’s problems and associated treatments within the context of available resources 02.02.03.04 Select and justify treatments and procedures, using the best available evidence and considering environmental factors, safety factors, family/cultural factors, and client’s impairments, activities and participation levels 02.02.03.05 Identify appropriate outcome measures for use in determining efficacy of intervention 02.02.03.06 Identify aspects of treatment that can be performed by client independently or with caregiver/family assistance 02.02.03.07 Schedule treatments to optimize client’s response (e.g., time of day, medication timing) 02.02.03.08 Facilitate procurement of client equipment and aids 02.02.03.09 Participate in interprofessional continuum of care planning and follow-up care with client, family and other care givers Implementation Use the following interventions in a safe, effective, and ethical manner with individuals or groups: 02.02.04.01.01 Exercise with or without equipment (e.g., passive, active assisted, active, resisted, neuromuscular, vestibular, muscle patterning, PNF) - NORMAL ROM - Vestibular exercises PNF patterns: (Yes, they may still ask you about this what year is it again, 1980?) UPPER EXTREMITY D1 Flexion UE flexion, (horiz) adduction, external rotation Close your hand, turn & lift up and across your face "Grab your seat belt", verbal cue for D1 Flexion UE D1 Extension UE extension, (horiz) abduction, internal rotation Open your hand, turn & push down and out "Fasten your seat belt" verbal cue for D1 Extension UE Jason Shane and Amanda Mrsic Apr 2015 D2 Flexion UE flexion, (horiz) abduction, external rotation Open your hand, turn & lift up and out "Pizza man" verbal cue for D2 Flexion UE D2 Extension UE extension, (horiz) adduction, internal rotation Close your hand, turn & push down and across "sword in the side" verbal cue for D2 Extension UE LOWER EXTREMITY D1 Flexion LE flexion, adduction, external rotation Foot up, turn & lift up and across "cross leg on opp knee foot bottom up" “kick soccer ball” verbal cue for D1 Flexion LE D1 Extension LE extension, abduction, internal rotation Foot down, turn & push down and out verbal cue for D1 Extension LE D2 Flexion LE flexion, abduction, internal rotation Foot up, turn & lift up and out "going over a hurdle" verbal cue for D2 Flexion LE D2 Extension LE extension, adduction, external rotation Foot down, turn & push down and across "cross feet with toes pointed at ankles" verbal cue for D2 Extension LE Capsular patterns: ROM loss O’sullivan pg 4 02.02.04.01.02 Joint mobilization go through doc made by classmates open and closed pack positions ● CI’s - cancer, acute arthritis, fracture, dislocation, bone disease, inflammation, empty/bony end feel, anticoagulant/steroid use, sign of ze BUTT, vertebral artery insufficiency, CV lig instability Jason Shane and Amanda Mrsic Apr 2015 02.02.04.01.03 Joint manipulation ● CI’s - fracture, jt instability, inflammation, inflamm jt disease, bone disease, open wound, poor circulation, sensory deficit in area, spasm or incrd pain with a test pull (pre manip hold), unsure gen health/diagnosis, anti-coag, hemophiliacs, can’t relax 02.02.04.01.04 Soft tissue techniques (e.g., massage, friction, stretching) Friction - CI: ossification, infection, skin breakdown, inflam skin/jt disease Stretching - CI: acute inflam/infection, unhealed fracture, jt effusion, recent corticosteroid injection to the involved tissue, in the direction of hypermobility, specific to certain surgeries ex-hip replacement PNF Stretching = the use of inhibition techniques to assist mm elongation; when the stretch reflex is activated in a mm being recruited, the mm on the opp side is inhibited massage: ● CI’s - autoimmune diseases during flare ups, fever, haemorrhage, flu, migraine headache, serious psych diagnosis, recent surgery, acute RA, sickle cell disease ● relative CI’s (DOC Clearance) - cancer, stroke, bleed disorders, CHF, HTN, kidney stones 02.02.04.01.05 Fitness/conditioning/endurance exercise programs 02.02.04.01.06 Functional activity training 02.02.04.01.07 Posture training 02.02.04.01.08 Positioning 02.02.04.01.09 Gait/mobility education and training with or without equipment Jason Shane and Amanda Mrsic Apr 2015 - Cane - widen base of support, help balance, Quad cane - not that good for stairs Crutches - help with lateral stability and improve balance Forearm crutches - allows for use of hands, but need more arm strength to use NORMAL GAIT: stance 60%, swing 40% 4 POINT GAIT - 3 points of support on ground at all times; 1 aid advanced, then opposite LE advanced, can be done with CRUTCHES OR CANES, slow stable gait 2 POINT GAIT similar to 4 point only 2 points of contact maintained at all times, less stable, req better balance CRUTCHES OR CANES - one leg and contralateral aid advance at same time (ex R cane and L leg together, then L cane and R leg together 3 POINT GAIT - 3 points of support on floor, NWB, PWB (<80% can’t use CANE), FeWB on affected LE - pt1) affected LE advanced, pt2) wt transferred to floor through aid (both crutches at the same time or walker), pt3) unaffected leg advanced, and wt returned to unaffected leg STEP TO, or STEP THROUGH, can be done with CRUTCHES OR WALKER 02.02.04.01.10 Neurodynamic techniques (e.g., nerve gliding/flossing exercises) Jason Shane and Amanda Mrsic Apr 2015 ● ● ● nerve gliding/flossing - do not Ax or treat in presence of CNS signs: myotomes, dermatomes, reflexes peripheral N conduction signs: Ax but don’t treat don’t treat if worsening or undiagnosed symptoms KEEP READING, THERE’S GOOD STUFF BELOW, COLLEGE GUIDELINES... LIST OF FUNCTIONS EVALUATED BY THE PCE (continued) (This list is not necessarily exhaustive.) 02.02.04.01.11 Balance training/proprioceptive training Balance = ability to maintain COG over base of support; 3 things necessary for balance are visual, vestibular, proprioception Proprioception = sensations of jt mvmt (kinesthesia), and joint position 02.02.04.01.12 Sensory training (e.g., desensitization, protective education, sensory integration) 02.02.04.01.13 Techniques to optimize oxygen transport and facilitate airway clearance (e.g., positioning, suctioning, secretion clearance, forced expiratory techniques) ● Auscultation - know 6 points antrly and 10 points postrly 02.02.04.01.14 Mechanical agents (e.g., traction, continuous passive movement, compression garment and devices, vasopneumatic devices) ● Traction - incrd IVF diameter, pain inhibition, decreased mm spasm, mm stretching; Indications-nerve root compression, disc pathology, degeneration, jt dsfx, hypomobility, pain; ● CI-fracture, infection/inflam, pain with manual traction, signif trauma w/o xrays, SCI signs and Sy’s 02.02.04.01.15 Conductive thermal agents (e.g., contrast baths, whirlpools, paraffin wax, hot packs, ice/cold) 02.02.04.01.16 Electrical agents (e.g., EMG biofeedback, iontophoresis, transcutaneous electrical nerve stimulation [TENS], neuromuscular electrical nerve stimulation [NMES], interferential current [IFC], high voltage pulsed current [HVPC]) 02.02.04.01.17 Electromagnetic energy agents (e.g., shortwave diathermy, LASER, ultraviolet) 02.02.04.01.18 Acoustic agents (e.g., ultrasound) 02.02.04.01.19 Protective, adaptive, or assistive devices (e.g., tape, splints, orthotics, prostheses) 02.02.04.02 Recognize and respond to the adverse effects of intervention (e.g., pain, deterioration in client status) and/or non-adherence Jason Shane and Amanda Mrsic Apr 2015 Education/Communication/Advocacy 02.02.05.01 Communicate the purpose and results of physiotherapy evaluation/assessment, proposed treatment procedures, expected outcomes and progress to client, family, and healthcare and other service providers and verify their understanding of same 02.02.05.02 Use teaching and communication strategies with clients and family members that respect culture, learning, communication, language style, and abilities 02.02.05.03 Educate client, family, and healthcare and other service providers in safe and effective physiotherapy techniques and use and care of equipment as appropriate 02.02.05.04 Educate the client, family/significant others about the condition, selfmanagement, coping and prevention strategies 02.02.05.05 Educate client regarding credibility of external educational materials/resources 02.02.05.06 Assist, and where necessary advocate on behalf of, client in obtaining access to necessary services, funding, equipment, and treatment within the continuum of care 02.02.05.07 Educate client, family, and healthcare and other service providers about transitions (e.g., change in level of care, care provider or care funder), other services, and discharge plans Intervention Progression 02.02.06.01 Assess client satisfaction and response to treatment with appropriate outcome measures and benchmarks 02.02.06.02 Perform re-evaluations/re-assessments at appropriate intervals or based on changes in client status as appropriate 02.02.06.03 Adjust, revise, or discontinue treatment plan when goals are achieved, client’s status changes, or treatment is no longer effective LIST OF FUNCTIONS EVALUATED BY THE PCE (continued) (This list is not necessarily exhaustive.) 02.03 PROFESSIONAL RESPONSIBILITIES (15%±5%) Professional Accountability 02.03.01.01 Respect the knowledge, rights, confidentiality, and dignity of client and family 02.03.01.02 Adhere to professional and regulatory codes of ethics/conduct and standards of practice 02.03.01.03 Participate in processes that evaluate and improve quality and outcomes of services Jason Shane and Amanda Mrsic Apr 2015 Communication and Collaboration 02.03.02.01 Secure informed consent for evaluation/assessment and treatment 02.03.02.02 Participate in collaborative health care service delivery (e.g., rounds, specialty care clinics or meetings) 02.03.02.03 Consult and collaborate with healthcare and other service providers to ensure services to clients are coordinated and client’s needs are met Professional Judgment and Reasoning 02.03.03.01 Recognize and practice within the scope and limitations of self and profession 02.03.03.02 Demonstrate continuing competence (e.g., reflective practice, selfdirected learning) Practice Management 02.03.04.01 Document all relevant aspects of care including client evaluation/assessment, treatment plan, progress notes and discharge plan 02.03.04.02 Adhere to federal and provincial laws regarding storage, protection, disclosure of information, business practices, etc. 02.03.04.03 Assign tasks, guide, and supervise activities of support personnel as needed Yah, we went there, we actually went the the College’s website to find this!!!! CPTBC Practice Standard No 3. Assignment of Task to a Physical Therapist Support ASSIGNMENT OF TASK TO A PHYSICAL THERAPIST SUPPORT WORKER Assignment of Task: Transfer of a component of a physical therapy treatment plan to a physical therapist support worker (PTSW). Physical Therapist Support Worker: an individual who works under the direction and supervision of a physical therapist. Supervision: the means by which the physical therapist monitors the performance of the PTSW. An individual who does not work under the direction and supervision of a physical therapist is not considered a PTSW. 1. The physical therapist must obtain informed consent from each patient for the involvement of a PTSW in the delivery of their physical therapy treatment plan. PTSW must be made aware that patient consent can be revoked at any time. 2. The physical therapist must explain to each patient the relationship between the physical therapist and the PTSW for the purpose of clarifying the difference in roles and responsibilities as they relate to patient assessment and treatment. 3. The physical therapist must ensure the PTSW is competent (has the knowledge, skills and abilities) to carry out the assigned tasks. 4. The physical therapist is responsible for the physical therapy task(s) assigned to the PTSW. 5. The assigned task must be recorded in the clinical record in accordance with the Practice Standard on Clinical Records. 6. To determine the appropriate level of supervision the physical therapist must exercise clinical judgment. The following factors should be considered: Jason Shane and Amanda Mrsic Apr 2015 • Patient preference, practice setting, complexity of the assigned task and environment, competencies of the PTSW, acuity of the patient’s condition, degree of judgment and decision making required to carry out the task, level of risk associated with the task, and patient’s cognitive status. 7. Assigned tasks must be within the physical therapist’s level of competence and be within the physical therapy scope of practice. 8. The physical therapist must ensure that the PTSW has been instructed in standard infection control measures CPTBC Practice Standard No 3. Assignment of Task to a Physical Therapist Support Worker 9. The physical therapist must ensure that the PTSW is aware of patient confidentiality standards and College Bylaws 10. The physical therapist must be available for consultation. If unavailable, the physical therapist must arrange for transfer of supervision to another physical therapist. 11. The physical therapist must instruct the PTSW to recognize any adverse treatment reactions, cease treatment and immediately report to the supervising physical therapist. 12. The physical therapist must reassess the patient at timely intervals. 13. The physical therapist must make any changes to the treatment plan and record the changes in the clinical record. 14. Physical therapists must NOT assign any physical therapy task which has an evaluation component that immediately influences the treatment program. A physical therapist must not assign the following tasks to PTSW: • Interpretation of referrals, diagnosis, or prognosis • Performance of assessment/evaluative procedures • Interpretation of assessment findings • Discussion of physical therapy diagnosis or treatment rationale with anyone other than the physical therapist • Planning or initiating physical therapy treatment goals or programs • Tasks requiring a physical therapist’s clinical judgment • Modification of treatment beyond established limits • Completion of documentation that is the physical therapist’s responsibility • Electro-physical agents (except neuromuscular stimulation or TENS) • Teaching of the assigned task to another person • Discharge planning 02.03.04.04 Procure and maintain safe and effective equipment 02.03.04.05 Ensure client safety in all aspects of assessment/evaluation and intervention 02.03.04.06 Use routine precautions for infection control in all aspects of client interaction 02.03.04.07 Manage and administer physiotherapy practice using ethical business Jason Shane and Amanda Mrsic Apr 2015 practices 02.03.04.08 Establish and manage a transparent prioritization process when demand exceeds ability to deliver services EXTRAS: Sign of the Buttock: - RONFISS; Rheumatic fever, Osteomyelitis, Neoplasm, Fracture, Ischiorectal abscess, Septic bursitis, Septic arthritis Synovium = Oct 18th - lines inner surfaces of joints, prod synovial fluid, lines tendons and form sheaths, forms bursae - injury = contusion or compression, friction or stress Intervertebral disc - annulus fibrosus = outer layer vascular and nerves ; nucleus pulposus = inside jelly - degen disc disease P due to facet jt compress, pain on N root, injury to annulus and to end plates Cartilage: - hyaline: between joints ; - elastic: resp system and ear; - fibrocartilage: meniscus (even force distribution) - insertion cartilage: tendons and ligaments - heal by repair of adj cells from synovium and labrum Imaging: X-rays: penetrates soft tissue, doesn’t penetrate bone X-ray arthrogram: dye injected into jt to see it Fluoroscopy: live action x-ray CT: 2D x rays made into 3D by the computer MRI: magnets used to align and alter the H nuclei in water: detects change in magnetic field Bone scan: detect BMD, and check for mets, fractures, infections Ultrasound: soft tissues – LIKE THE BABIES!!!!!! Floroquinolones: broad spec antibiotics for COPD, pneumonia, GU infections: inc risk of tendon ruptures (and corticosteroids) Osteomyleitis: infection of bone: get it with sepsis, open trauma, infected surgical implant; children at highest risk Effects of Aging: Jason Shane and Amanda Mrsic Apr 2015 Sarcopenia: reduction and mm mass and function Tendons: less metabolic active, more wear and tear, more cross linking, less of strength at enthesis; Achilles and supraspinatus most prone to injury with age IMMOBILIZATION: Effects of bed rest on mm: dec mito, dec red blood supply, fat infiltration, dec strength, atrophy and contractures Bones: osteopenia Ten and lig: disorganization of parallel arrays and less strong Cartilage: loss of thickness; synovium: adhesions form between synovium and cartilage; Synovium: inflamed, fatty infiltration; less jt fluid production Patellar dislocation: due to tight lat retinaculum, weak VMO, direct blow Ganglion: pocket of synovial fluid Contracture: shortening of soft tissue: ex dupuytren's Adhesion: abnormal adherence of collagen fibers Reflex mm guarding: myofascial trigger points, Pain mm guard around it Intrinsic mm spasm: prolonged contraction of mm in resp to circulatory and metabolic changes and it is contracted Myofacial compartment syndrome: fascia too small to accommodate for mm growth, can cause mm necrosis Rhabdomyolosis: mm compressed and starts breaking down, myoglobin accumulates and backs up in the kidneys, can get kidney failure Protein balance for mm: contact and stretch release MGF mm growth factor, take steroids; GH, testosterone, IGF-1; cortisol = breaks down mm, Mm training: increased cross sectional area, dec fat, inc angle of pennation, resistance training: dec number of mitochondria (mito used or endurance energyt prod), more caps, more type 2 mm fibres Satellite cell: mm stem cell; on the periphery, activated by exercise and trauma, and can completely regenerate mm myofibres Tenocytes: get more collagen – align into rays, progenitor cells: repair of tendon Pacinian corpuscles: strength, tension, in jt capsule and free N endings EIMD: how long, magnitude and vel of strain affect EIMD; age, gender affect it too; ECCENTRIC DOMS: peak 48hrs after, not correlated with markers of mm damage Repeated bout effect: adaptation of mm after eccentric EIMD, after 2nd bout indirect markers of Jason Shane and Amanda Mrsic Apr 2015 mm damage are reduced MO: bone formation in the mm; same as HO (neuro) Deformation curve, toe, linear, elastic, deformation Types of Collagen: Collagen type 1 = tendon, end scar strongest Collagen type 2 = hyaline cartilage Collagen type 3 = granulation tissue, scar Achilles rupture; 35, 70, risks: age BMI, sport, male Jumper’s knee: patellar tendon tendinopathy, lots in kids Tennis elbow: lat epicondylitis, ECRB Golfer’s elbow: med epicondylitis Tib post tendinopathy: compressed under med mal, if hyperpronate can irritate BONES: TYPES: flat, tubular, irregular (vertebral bones), sesamoid bones (develop in tendons), supernumerary (centre of talus – os trigonum) Osteomalacia – defect in mineralization of collagen matrix – Vit d deficiency (rickets - kids) Paget’s disease: 2nd most common bone disease., excessive osteoclast, abnormal regeneration Ostopetrosis: v rare, inherited, deficiency of carbonic anhydrase, body inability to resorb bone Osteochondrosis: disorders of epiphyseal growth plates Kohlers disease: avascular necrosis of navicular Osgood schlatter's: irritation to tibial tuberosity, or pull bone off Legg-Calve-Perth: necrosis of femoral head – put in adduction Osteochondritis dissecans: subchondral necrosis of bone followed by recalcification, bone and cartilage can pull away Salter Harris fracture: fracture of the growth plate Congenital hip dysplasia: malformation of the hip present at birth; hip dislocation, asymm leg positions Marfans: lack of fibrillin , long hands, genetic Larsen syndrome: prominent forehead and wide spaced eyes, genetic disorder, multiple jt dislocations Osteogenesis imperfecta: brittle bone disease Achondroplasia: dwarfism, impaired cartilage formation and effects growth factor for bones growing. Multiple epiphyseal dysplasia: cluster of disorders affect epiphyseal growth plates, short stature and limbs Acromegaly: overactive pituitary gland Fibrillation: loss of normal smooth surface, rough edges into tiny fibrils SCOLIOSIS: Jason Shane and Amanda Mrsic Apr 2015 3 kinds: 1) Idiopathic, 2) Congenital, 3) Neuromuscular; can be structural or functional Rx: Education, bracing, stretching, strengthening, postur Scoliosis Kisner Colby...page 396/7... Scoliosis usually involves the thoracic and lumbar regions. Typically, in right-handed individuals, there is a mild right thoracic, left lumbar S-curve, or a mild left thoracolumbar C-curve. There may be asymmetry in the hips, pelvis, and lower extremities. Structural scoliosis involves an irreversible lateral curvature with fixed rotation of the vertebrae (Fig. 14.13A). Rotation of the vertebral bodies is toward the convexity of the curve. In the thoracic spine, the ribs rotate with the vertebrae so there is prominence of the ribs posteriorly on the side of the spinal convexity and prominence anteriorly on the side of the concavity. ECG’s, what is the issue with three PVC’s in a row=>Ventricular tachycardia=>which can b/co ventricular fibrillation, VERY BAD! Prob that the atria are not contracting because no wave Cyanosis = bluish discoloration of skin and nailbeds of fingers and toes alont with cold and moist palms; caused by excess deoxygenated hemoglobin in the blood Apraxia = disorder of the brain and nervous system that is a person is unable to perform tasks and movements when asked ● Verbal apraxia-inability to produce motor patterns resulting in speech; in the absence of ● ● ● impaired understanding , mm paralysis/ weakness or intellect Ideational apraxia: Cannot carry out learned complex tasks in the proper order, such as putting on socks before putting on shoes due to mis-identification motor apraxia= disorder of voluntary movement notwithstanding the in absence of paralysis or mm weakness constructional apraxia - unable to draw objects in absence of paralysis Astereognosis (tactile agnosia) = inability to identify held objects in the absence of language or sensory loss Right brain is dominant for body awareness Anosognosia = a lack of awareness or a denial of a neurologic defect or illness in general, especially paralysis, on one side of the body (like a limb). It may be attributable to a lesion in the right parietal lobe. Somatognosia= Inability to correctly identify or orient the parts of one's body or the body of another. Expressive aphasia=Broca’s Receptive aphasia=Wernicke’s CEREBELLAR: cerebellar ataxia - jerky inaccurate, uncoordinated movement, w/ normal strength and no hypertonia Jason Shane and Amanda Mrsic Apr 2015 dysmetria = overshoot the intended goal dysarthria - trouble with speaking, slurred due to lack of motor coordination intention tremor - tremor when initiate movement dysdiadochokinesia - inability to perform rapid alternating movements NON CEREBELLAR: athetosis - slow continuous involuntary movements chorrea - rapid repeated jerky coarse movements dystonia - frequent maintained contraction of hypertonic mm hemiballismus - sudden stabbing movements of one side of the body fasciculation - twitching of mm fibers in single motor neuron unit (often visible on surface, occur with LMNL) fibrillation - abnormal contraction of a single mm, only visible with EMG, and seen with dying neurons Huntington’s chorea = genetic disorder with writhing (choreoform) movements including limbs, speech (sound drunk) due to loss of neurotransmitters and GABA Korsokoff’s syndrome = genetic metabolic injury due to malnutrition or alcoholism, can’t make new memories, characterized by confabulation spastic hypertonia (spasticity) - velocity dependent increase in resistance to passive movement rigid hypertonia - velocity INDEPENDENT increase resistance to passive movement Metabolic syndrome = pre cursor to Type 2 diabetes, abdominal obesity, high triglycerides, low HDL’s, HTN, high fasting plasma glucose Glaucoma =loss of peripheral vision first, followed by central blindness Cataracts =a clouding of the lens, gradual loss of vision, central vision is lost first, then peripheral Resistance exercise is CONTRAINDICATED in Pts with signif: Bony mets, osteoporosis, low platelet count (<20,000) *********************** CARDIORESP Types of breathing: ● breath stacking: stacking little breaths on top of one another when a deep breath is too painful ● active cycle of breathing: diaphragmatic breaths with a hold at the top, then to normal Jason Shane and Amanda Mrsic Apr 2015 ● ● ● ● ● breathing, repeat cycle then 3 huffs autogenic drainage: use breathing to clear secretions flutter: breath out thru device, vibrations from device will loosen secretions diaphragmatic breathing: post op, obstructive or restrictive segmental breathing: improved vent to hypo-ventilated lung areas pursed lip breathing: help blow off CO2, inc tidal vol, red resp rate, red dyspnea; for COPD BREATH SOUNDS: p20 reid and cheung ● bronchial breath sounds: hollow, high pitched, harsh: consolidated pneumonia or lobar collapse ● normal: soft and low pitched ● decreased or absent: pleural effusion, hemothorax, pneumothorax, emphysema, obese or elderly ● crackles: fine: atelectasis, interstitial pulmonary fibrosis; coarse: retained secretions ● wheezes: asthma, COPD will have inc FRC: vol of air remaining in lungs at end of ordinary expir with age p38 R&C ABG’s p178 O’ Sullivan normal range pH7.35-7.45 - lower: resp or metabolic acidosis; high: metabolic or resp alkalosis PaCO2 35-45mmHG high = resp acidosis (from hypoventilation - COPD, flail chest, neuromuscular disorders, sleep apnea): help with secretion clearance - low = resp alkalosis (hyperventilation, pain or anxiety or breathlessness); mechanical vent PaO2 80-100mmHG HCO3 22-28 - decreased: metabolic acidosis; - increased: metabolic alkalosis ● ● ● ● resp compensation mins to hours renal compensation is 1-5 days metabolic acidosis: renal failure, lactic acidosis, ketoacidosis metabolic alkalosis: sodium base overload, potassium depletion, vomiting HAEMODYNAMICS: WBC low: lethargic, bruise easy Hb 85-110: put on iron; below 85 = transfusion - low: fatigue, dizzy, headache, lack of concentration Jason Shane and Amanda Mrsic Apr 2015 platelets: low = thrombocytopenia, get lots of bruising, and get small bleeds; Normal platelet count is 150-450,000/uL of blood IRN: looks at coagulation and clotting time of blood low levels: will have restricted activity or bed rest potassium: reg mm tissue, digestion and metabolism low: hypokalemia- weak, fatigue, vomit, nausea; high: hyperkalemia - min symptoms sodium: reg blood vol, blood pressure, osmotic equlib, pH - low; hyponatremia: headaches, confusion, mm spasm, seizures - high; hypernatremia: S&S of dehydration magnesium: - high: hypermagnesemia- nausea, vom, mm weakness - low: mag deficiency - mm cramps, hyperactive reflexes, tremors and overall weakness calcium: - low: hypocalcemia, prolonged QTwave - high - kidney stones, groans, bones (risk of #) thrones: diarrhea, psyc overtones ***************** LINES: PICC - peripherally inserted central catheter: treatments such as chemo or antibiotics, samples of blood, no freq needles; have to wait to mobilize until PICC insertion cleared by x-ray, close off before shower or hydrotherapy Central venous line: sits at vena cava: monitors R atrial pressure, venous tone and circ blood vol., central venous pressure normal = 5-12 gtube = facial trauma - tube for feeding, turn feed off before PT treatment arterial line: measure BP, blood sampling for ABG’s, admin meds pulmonary arterial line: vena cava into R atrium, pulm art or pulm cap: measure pulm art pressure, pulmonary capillary wedge pressure (L art pressure), right atrial pressure, CO MORE DEFINITIONS: TPN: total parenteral nutrition, amino acids and lipids lumbar drain: drains CSF continuous bladder irrigation: continuous flow of fluid, prevents obstruction and cleaning, bag higher than bladder hemodialysis: removes wastes and extra fluid in blood and returns clean blood to patient: renal insufficiency and get rid of antibodies in plasma intracranial pressure ICP: 10-15mmHg infarction: necrosis develops distal to occlusion of an artery embolism: passage of any material capable of getting lodged in a blood blood vessel pulmonary infarctions: death of lung tissue S&S: SOB, chest pain, edema: presence of excess fluid in interstitial space; anasarca: total body edema effusion: excess fluid in body cavities transudate: low in proteins exudate: high in protein Jason Shane and Amanda Mrsic Apr 2015 *********** OUTCOME MEASURES: - Kurtzke Expanded Disability Scale: for MS - Expanded Disability Status Scale (EDSS): MS - Oswestry Disability Index: lower back pain - Hoehn and Yahr Classification of Disability: Parkinson’s - Unified Parkinson’s Disease Rating Scale (UPDRS): Parkinson’s - Disability Rating Scale (DRS): Traumatic Brain Injury - - - Fugl-Meyer Motor strength test: stroke Stroke Impact Scale (SIS): evaluates how stroke has impacted health and life from Pt’s perspective; a questionnaire Rivermead mobility index: functional mobility following stroke The Community Balance and Mobility Scale: detect “high” level balance and mobility deficits The Dynamic Gait Index: Assesses individual’s ability to modify balance while walking in the presence of external demands The Functional Independence Measure: measures the level of a patient's disability and indicates how much assistance is required for the individual to carry out activities of daily living. Barthel scale or Barthel ADL index is an ordinal scale used to measure performance in activities of daily living (ADL) Knee injury and OA Outcome Scale (KOOS): evaluates s/t and l/t Pt relevant outcomes of knee injury that can result from post-traumatic OA (ACL injury, meniscus injury) McMaster Toronto Arthritis Patient Preference Disability Questionnaire (MACTAR): assesses disability in Pts with RA ********************************* PCE Electro Review Interferential Current: - Low voltage, medium intensity - 2 sinusoidal waves – alternating current - Each wave = slightly different frequencies and interfere with one another in tissues creating new wave (linear super-position) - Series of wave packets (beats) - Balanced, symmetrical, biphasic, amplitude modulated - Can output 50-90mA (other machines = much lower) – NO THORACIC APPLICATION OVER 50mA - Used for pain, edema, increases blood flow, muscle stimulation - Motor = 1-10Hz; Sensory (pain) = 80-150Hz Jason Shane and Amanda Mrsic Apr 2015 - 20-40mins TENS - Low voltage, low intensity - Gate control theory or extrasegmental Conventional: o High frequency (80-150Hz), low pulse duration (60microsec.) o Comfortable tingle o Acute – analgesic effect only while machine on o Electrodes bracket pain Acupuncture-like: o Low frequency (5-10Hz), high pulse duration (200microsec) o Motor twitch o Chronic pain – 4-6 hours analgesia o Electrodes on motor point (want twitch) LASER 3 features of a laser: 1) Monochromaticity (all photons have a single wavelength), 2) coherence (all photons travel in same phase and direction), 3) collimation (minimal divergence over distance) - Used to increase tissue healing, decrease pain, decrease inflammation (wound management) - Choose laser head based on depth of lesion (red-near infrared = 1-5mm; near-mid infrared = 5-10mm) Dose: acute = 2J/per point; chronic = 4 J/per point (look at WALT) - Frequency: acute = <1000kHz; chronic = >1000kHz - Continuous or pulsed (laser lasts longer) - Contact or noncontact (scanning/grid) - Wear eyewear Heat: - 2 fibers for perception of thermal sensation (warmth and heat (>45deg. C) - Major source of heat gain = metabolism (also absorption of radiation from environment, etc.) - Heat loss major source = radiation (also exhalation, evap. of sweat, urine) - Thermoregulation is controlled by the hypothalamus - As you get hotter, metabolism increases – Van Hoft (in body temperature >45C = protein damage) - Therapeutic effects of superficial tissue heating: tissue healing, pain relief, reduction of muscle spasm, sedative effect, increased joint ROM, facilitates fine movements - Paraffin wax baths – 6-8layers, 15minutes (contraindications – skin infections or acute inflammation of underlying joints should not receive wax; dermatitis can get worse Contrast bath (hot then cold then hot) – produces blood flow to tissues – good sensory Jason Shane and Amanda Mrsic Apr 2015 - stimulation (no evidence of reduction of local edema) – treatment starts and ends with immersion in hot water – hot = 3-4mins, cold = 1min (repeat 3-4X) Whirlpool – gating effect – stimulation of moving water – may gently debride wounds (may sometimes increase edema – dependent position?) Superficial heat precautions – local burns, altered thermal sensation, ischemic disease restricting local circulation, DM, PVD, altered heat loss mechanism (ex: obesity), fungus, exacerbation of dermatitis or eczema, malignancies, open wounds) COLD - Cooling reduces metabolic rate – enhances survival of vulnerable cells that have survived the initial injury – reduces edema (allows vulnerable cells to remain closer to O2 supply), reduces sharp pain (blocks nerve conduction) – little value for chronic pain (doesn’t affect those fibers) - Mild cooling can increase isometric strength, but greater cooling can reduce this strength, cooling reduces tremor, can reverse conduction block associated with demyelination of peripheral nerves (heating exacerbates it) – ex: MS - Therapeutic uses: recent injuries, pain, muscle spasm, spasticity, muscle strengthening, chronic inflammatory conditions, chronic edema - Check for allergic reaction to cold after 1 minute and after 5 minutes - Dangers/contraindications: ice burn, peripheral nerve damage, frostbite, reduced peripheral blood supply (can further damage tissue), cold sensitivity (Raynaud's, cold urticaria) UV - Contraindications = photosensitivity, skin cancer, and CT disorder (be aware of drugs causing photosensitivity) Used to treat: psoriasis, eczema, vitiligo, pruritus (secondary to liver/kidney disease), acne, photodermatoses, wound healing, atopic dermatitis On eyes can cause conjunctivitis or photokeratitis (inflammation of cornea) – cataracts are caused by chronic exposure to UV HVPC - High voltage, high peak intensity, low average intensity - Monophasic (can build up a bigger net charge) - Frequency = 1-200Hz, pulse width fixed (5-65microsec.), peak current is high (higher risk of burning), but long interpulse interval so charge has a chance to dissipate allowing safer application (total current is very low) - Mainly used for: decreased pain, decreased edema, increased wound healing, muscle stim. (enhances oxygenation, blood flow and tissue formation) - High voltage = more comfortable and large punch = better at punching away or bringing in molecules - Wound healing = 50-100Hz (submotor), edema reduction = 5-20Hz (want twitch), muscle stim = 35-65Hz, pain = same parameters as TENS - Galvanotaxis – can repel molecules or attract desired cells based on polarity Jason Shane and Amanda Mrsic Apr 2015 - Don’t use for inflammation (don’t want to add energy to injury) For acute edema – active red on edema and set it as negative to push away positive proteins OR put it on muscle twitch on motor point and nerve trunk (chronic) Wound healing – one electrode in wound and one 10-20cm away Phonophoresis and Iontophoresis Phonophoresis (don’t need to know) - using US to enhance delivery of topically applied drugs – avoid risks of IV, reduce risk of OD, local Rx, easy method to terminate and bypass liver ● Primary uses: decrease tissue inflammation, reduce pain ● 3 common meds – local anesthetics, anti-inflammatories, counter-irritants Iontophoresis – method of Rx using current flow between two electrodes to push ions through the skin barrier ● Current is direct current ● Positively charged drug can be made to cross the skin away from positive electrode ● Under the anode may get an acidic reaction (hardening of skin over time (sclerotic) and under cathode may get alkaline reaction (softening and burning of skin) – but most electrodes have buffering agents to prevent this ● Keep the cathode larger (current density is therefore lower and skin is less likely to burn) ● Used for: hyperhidrosis, MSK inflammatory disorders, plantar fasciitis, TMJ disorders, ischemic skin ulcer, fungal infections, bursitis and tendonitis ● Contraindications include over damaged skin or open lesions, allergy to therapeutic ions, impaired sensation, over electric implants Short Wave Diathermy ● Therapeutically heat body tissues at any depth ● 2 types of electromagnetic fields producing the heat (electrostatic and electromagnetic) – thermal and non-thermal effects ● Physiological effects of pulsed SWD: increased tissue healing, enhance nerve regeneration, pressure ulcers, chronic low back pain, soft tissue injuries (some evidence it can be used for pain, muscle spasm, chronic inflammation, delayed wound healing, chronic infection) ● 2 main indications for application = OA and ankle sprain ● Main contraindications = metallic implants and pacemakers (implanted devices) ● Can get burns (unequal spacing, perspiration, etc.) – patient should just feel mild, comfortable warmth EMG Biofeedback: ● Nerve conduction testing – estimates velocity of depolarization along an alpha motor neuron ● In skeletal muscle, normally silent at rest (short burst of electrical activity during needle insertion) ● reduced insertional activity seen in fibrotic or severely atrophied muscle (when put needle in), -increased activity when a muscle is irritable Jason Shane and Amanda Mrsic Apr 2015 ● ● ● ● Abnormal electrical activity at rest suggests neuropathy or myopathy and is indicated by fibrillation potentials (rapid, irregular contractions of muscles), positive sharp waves, or fasciculation potentials Surface EMG – provides information about muscle activity (in order to uptrain or downtrain activity) Used to: improve control over defective muscles or improve control over stressed muscles (ex: hemiplegia, SCI, spasticity, dystonia, recovering peripheral nerve injuries) Used as a tool not a treatment NMES: ● The use of electrical stimulation to generate an action potential in a nerve leading to contraction of skeletal muscle - Pulsed and biphasic ● Used for: pain modulation, edema management, decrease spasticity, muscle strengthening ● Parameters: pain = same as TENS – intensity can be turned up to sensory or motor threshold, edema = same as HVPC – intensity to muscle twitch, muscle stim and spasticity = 35-65Hz – intensity to tetany ● On:off time set based on muscle grade of strength – grade 5 muscle strength = 1:1 and grade 1 = 1:5 ● Electrode placement – anode = nerve trunk (or muscle belly), cathode = motor point (or muscle belly) – can surf cathode to get the right spot (1/3 proximal, 2/3 distal for motor point) ● Side effects: rhabdomyelosis, ischemic colitis, inappropriate ICD discharge ● 12-15 contractions per session Ultrasound: ● Sound waves ● Maintain contact and keep head moving and perpendicular to tissue ● Parameters: frequency 1MHz (deep) and 3MHz (superficial); intensity (0.5 acute and 2 = high for chronic while 1-1.2 = moderate for chronic), pulsed (acute) and continuous (chronic); acute = 5-10mins, chronic = 20 minutes ● Apply to area not larger than 2-2.5xERA (ERA = area producing 5% or more of max. power output – higher = better) ● Used for – thermal effects: decreased pain, decreased joint stiffness, improved blood flow, promote healing (decreases inflammation) and non-thermal effects: wound healing, inflammation and soft tissue healing ● Contraindications: implantable devices, malignancy, bleeding disorder, infection, DVT, don’t use on Medtronic stimulation system Functional Electrical Stimulation ● Used for: treatment of disuse atrophy, increasing ROM, re-educating muscle, managing spasticity, gait orthoses, improving motor recruitment, increasing muscle endurance, re-educating gait ● Individuals with CNS condition benefit from this – stroke, MS, SCI, CP, PD, TBI and Jason Shane and Amanda Mrsic Apr 2015 ● ● orthopedic conditions or conditions resulting from deconditioning Individuals who cannot benefit – LMNL, peripheral nerve lesions, motor neuron disease, GBS, polio and post-polio syndrome, fixed contractures Especially used for drop-foot stimulation (reduce fall risk) and improving subluxation of GH joint ESTIM CONTRAINDICATIONS - Areas where it could affect electrical devices (ex: pacemaker) - Low back/abdomen/acupuncture points of pregnant women - Areas of malignancy - Acute hemorrhage - DVT or thrombophlebitis - CVA or TIA - TB - Osteomyelitis - Chest if cardiac issues - Neck/head region in people with seizures - Damaged/at risk skin areas - Infection - Recently radiated areas - Impaired sensory awareness - Acute inflammation - Trans-thoracically or trans-cerebrally - Cognition impairments - NMES contraindicated to chest, intercostals, and lower abdomen **** NERVES Common Peroneal branches: Common peroneal in popliteal fossa: - Sensory: Superficial peroneal - Motor: Peroneus brevis, Peroneus longus, Cutaneous sensory: - Lower leg: Anterolateral - Foot: Dorsum of foot and big toe - Medial & Intermediate dorsal cutaneous nerves of foot Deep peroneal - Motor branches in leg: Tibialis anterior, Extensor hallucis & Extensor digitorum longus, Peroneus tertius Lateral terminal branch in foot: Extensor digitorum brevis Jason Shane and Amanda Mrsic Apr 2015 Tibial nerve: ● branch of the sciatic nerve, passes through the popliteal fossa to pass below the arch of soleus. ● In the popliteal fossa the nerve gives off branches to: ○ motor = gastrocnemius, popliteus, soleus and plantaris muscles ○ cutaneous = becomes the sural nerve (distal branch of the tibial nerve and supplies the back of the leg and lateral side of the foot and little toe) - Below the soleus muscle the nerve lies close to the tibia and supplies the: ● motor = tibialis posterior, the flexor digitorum longus and the flexor hallucis longus. - In the foot it divides into the: 1) Medial plantar (calcaneal) nerve ● cutaneous: supplies the heel and medial sole of the foot ● motor: abductor hallucis, the flexor digitorum brevis, the flexor hallucis brevis 2) Lateral plantar nerve ● cutaneous: to the lateral sole and lateral one and one half toes (like the ulnar nerve). ● motor: quadratus plantae, flexor digiti minimi, adductor hallucis, the interossei, three lumbricals. and abductor digiti minimi. LUMBAR PLEXUS - draw out If I Get Laid F*** Off Sex (Hey, kids may be reading this ;) Jason Shane and Amanda Mrsic Apr 2015 Nerve Segment Innervated muscles Cutaneous branches Iliohypogastric T12-L1 • Transversus abdominis • Abdominal internal oblique • Anterior cutaneous ramus • Lateral cutaneous ramus Ilioinguinal L1 Genitofemoral L1, L2 Lateral femoral cutaneous L2, L3 Obturator L2-L4 • Obturator externus (ADduct thigh, LAT rotate) • Adductor longus • Adductor brevis • Gracilis • Pectineus • Adductor magnus • Cutaneous ramus Femoral L2-L4 • Iliopsoas • Pectineus • Sartorius • Anterior cutaneous branches • Anterior scrotal nerves in males • Anterior labial nerves in females • Cremaster in males • Femoral ramus • Genital ramus • Lateral femoral cutaneous Jason Shane and Amanda Mrsic Apr 2015 • Quadriceps femoris Short, direct muscular branches • Saphenous • Psoas major • Quadratus lumborum • Iliacus • Lumbar intertransverse T12-L4 PES ANSERINE: (medial side of knee) Sartorius....................Femoral Gracilis........................Obturator Bursae = pes anserine burase semiTendinosus............Tibial SGT FOT LUMBO-SACRAL PLEXUS Nerve Segment Innervated muscles Superior gluteal L4-S1 Gluteus medius Gluteus minimus Tensor fasciae latae Jason Shane and Amanda Mrsic Apr 2015 Cutaneous branches Inferior gluteal L5-S2 Posterior cutaneous femoral S1-S3 Gluteus maximus Posterior cutaneous femoral • Inferior cluneal nerves • Perineal branches Direct branches from plexus • Piriformis S1-2 Piriformis • Obturator internus L5-S1 Obturator internus • Quadratus femoris L5-S1 Quadratus femoris L4-S3 Semitendinosus (Tib) Semimembranosus (Tib) Biceps femoris • Long head (Tib) • Short head (Fib common peroneal) Adductor magnus (medial part, Tib) Sciatic Sciatic Tibial L4S3 Common fibular (peroneal) Fibular L4-S2 Lateral sural cutaneous Communicating fibular • Superficial fibular L5-S2 lateral compartment Peroneus longus (runs post to lat malleolus) Peroneus brevis Medial dorsal cutaneous Intermediate dorsal cutaneous • Deep fibular (peroneal) L4-S2 anterior compartment and dorsum of foot Tibialis anterior Extensor digitorum longus Extensor digitorum brevis Extensor hallucis longus Extensor hallucis brevis Peroneus tertius Lateral cutaneous nerve of big toe Intermediate dorsal cutaneous Tibial nerve L4-S3 DEEP Posterior compartment Triceps surae Plantaris Popliteus Tibialis posterior Flexor digitorum longus Flexor hallucis longus Medial sural cutaneous Lateral calcaneal Medial calcaneal Lateral dorsal cutaneous SUPERFICIAL post compartment Gastrocnemius and soleus Jason Shane and Amanda Mrsic Apr 2015 (S1-2) • Medial plantar (from tibial nerve) Abductor hallucis Flexor digitorum brevis Flexor hallucis brevis (medial head) Lumbrical (first and second) Cutaneous to medial plantar aspect of foot • Lateral plantar (from tibial nerve) Flexor hallucis brevis (lateral head) Quadratus plantae Abductor digiti minimi Flexor digiti minimi Lumbrical (third and fourth) Plantar interossei (first to third) Dorsal interossei (first to fifth) Adductor hallucis Cutaneous to lateral plantar aspect of foot Pudendal and coccygeal Pudendal (Pudendal plexus) S2-S4 Muscles of the pelvic floor: Levator ani Superficial transverse perineal Deep transverse perineal Bulbospongiosus Ischiocavernosus Sphincter anus externus Urethral sphincter Coccygeal (Coccygeal plexus) S5-Co1 Coccygeus Jason Shane and Amanda Mrsic Apr 2015 Inferior rectal Perineal • Posterior scrotal/labial • Dorsal penis/clitoris Anococcygeal Dorsal branches sural nerve: formed by the junction of the medial sural cutaneous (from tibial nerve) with the peroneal anastomotic branch of the lateral sural cutaneous nerve (from common fibular nerve) Jason Shane and Amanda Mrsic Apr 2015 BRACHIAL PLEXUS From Nerve Roots[2] Muscles Cutaneous roots dorsal scapular nerve C5 rhomboid muscles and levator scapulae - Jason Shane and Amanda Mrsic Apr 2015 roots long thoracic nerve C5, C6,C7 serratus anterior - upper trunk nerve to the subclavius "C5",C6 subclavius muscle - upper trunk suprascapular nerve C5, C6 supraspinatus and infraspinatus - lateral cord lateral pectoral nerve C5, C6, C7 pectoralis major (by communicating with the medial pectoral nerve) - lateral cord (terminal N) musculocutan eous nerve C5, C6, C7 coracobrachialis, brachialis and biceps brachii becomes the lateral cutaneous nerve of the forearm lateral cord lateral root of the median nerve C6, C7 fibres to the median nerve - posterior cord superior/uppe r subscapular nerve C5, C6 subscapularis (upper part) - posterior cord thoracodorsal nerve(middle subscapular nerve) C6, C7, C8 latissimus dorsi - posterior cord lower / inferior subscapular nerve C5, C6 subscapularis (lower part ) and teres major - posterior cord axillary nerve C5, C6 anterior branch: deltoid and a small area of overlying skin posterior branch: teres minor and deltoid muscles posterior branch becomes upper lateral cutaneous nerve of the arm posterior cord (terminal N) radial nerve C5, C6, C7, C8, T1 triceps brachii, supinator, anconeus, the extensor muscles of the forearm, and brachioradialis skin of the posterior arm as the posterior cutaneous nerve of the arm medial cord medial pectoral nerve C8, T1 pectoralis major and pectoralis minor - medial cord medial root of the median nerve C8, T1 fibres to the median nerve all flexors of forearm except FCU, part of portions of hand not served by ulnar or radial Jason Shane and Amanda Mrsic Apr 2015 FDP, medial cord medial cutaneous nerve of the arm C8, T1 - front and medial skin of the arm medial cord medial cutaneous nerve of the forearm C8, T1 - medial skin of the forearm medial cord (terminal N) ulnar nerve C8, T1 flexor carpi ulnaris, the medial two bellies of flexor digitorum profundus, the intrinsic hand muscles except the thenar muscles and the two most lateral lumbricals the skin of the medial side of the hand and medial one and a half fingers on the palmar side and medial two and a half fingers on the dorsal side The main portion of the MEDIAN NERVE supplies the following muscles: Superficial group: ● Pronator teres ● Flexor carpi radialis ● Palmaris longus Intermediate group: ● Flexor digitorum superficialis muscle The anterior interosseous branch of the median nerve supplies the following muscles: Deep group: ● Flexor digitorum profundus (only the lateral half) ● Flexor pollicis longus ● Pronator quadratus Hand - median nerve supplies:1st and 2nd lumbrical muscles, muscles of the thenar eminence by a recurrent thenar branch. The rest of the intrinsic muscles of the hand are supplied by the ulnar nerve. The median nerve innervates the skin of the palmar side of the thumb, the index and middle finger, half the ring finger, and the nail bed of these fingers. The lateral part of the palm is supplied by the palmar cutaneous branch of the median nerve, which leaves the nerve proximal to the wrist creases. This palmar cutaneous branch travels in a separate fascial groove adjacent to the flexor carpi radialis and then superficial to the flexor retinaculum. It is therefore spared in carpal tunnel syndrome. Jason Shane and Amanda Mrsic Apr 2015 - The muscles of the hand supplied by the median nerve can be remembered using the mnemonic, "LOAF" for Lumbricals 1 & 2, Opponens pollicis, Abductor pollicis brevis and Flexor pollicis brevis. (NB: OAF are the thenar eminence) Jason Shane and Amanda Mrsic Apr 2015 Layers of the Anterior Forearm All median nerve except FCU and medial half of FDP 1. Superficial - pronator teres - flexor carpi radialis - palmaris longus - flexor carpi ulnaris (ulnar nerve) 2. Intermediate - flexor digitorum superficialis (ulnar nerve is medial half) 3. Deep -innervated by ant. interosseous nerve which is branch of median nerve - pronator quadratus - flexor digitorum profundus - flexor pollicis longus All innervated by RADIAL nerve: ● triceps, ● brachoradialis All mm listed below are innervated by post interosseous nerve which is a branch of the radial nerve - supinator 1. Extend hand (carpi) - extensor carpi radialis brevis - extensor carpi radialis longus - extensor carpi ulnaris 2. Extend medial 4 digits (fingers) - extensor digitorum Jason Shane and Amanda Mrsic Apr 2015 - extensor indicis - extensor digiti minimi 3. Extends thumb (pollex) (snuff box) - abductor pollicis longus - extensor pollicis brevis - extensor pollicis longus Muscles of Anterior Compartment: INNERVATED by MEDIAN Nerve except FCU 1. Superficial - pronator teres - flexor carpi radialis - palmaris longus - flexor carpi ulnaris (INNERVATED BY ULNAR NERVE) 2. Intermediate - flexor digitorum superficialis 3. Deep - pronator quadratus - flexor digitorum profundus 1 and 2 - flexor pollicis longus thenar eminence (OAF): opponens pollicis, ABD pollicis, flex pollicis brevis 1st 2 lumbrical; LOAF ULNAR NERVE innervates: - Hypothenar eminence (OAF)- opponens DM, ABductor DM, Flexor DM brevis - Interossei- Pad, and Dab - ADDuctor pollicis - 3rd and 4th lumbricals - FCU - medial ½ of FDP - FCU ************** NEURO: RANCHOS LOS AMIGOS: - does not predict improvement over long term, helps understand behaviour and progression of brain injury over time, useful for therapist, PT, and family; Jason Shane and Amanda Mrsic Apr 2015 1=no response, 5=confused, 10=normal OUTCOME I NO RESPONSE: Does not respond to voices, sounds, light, or touch; appears in a deep sleep. II GENERALIZED RESPONSE: Limited, inconsistent, non-purposeful responses; first reaction may be to deep pain; may open eyes but will not seem to focus on anything in particular III LOCALIZED RESPONSE: Inconsistent responses but purposeful in that reacts in a more specific manner to stimulus; may focus on a presented object; may follow simple commands. IV CONFUSED, AGITATED: Heightened state of activity; confusion; unable to do self-care; unaware of present events. Reacts to own inner confusion, fear, disorientation; excitable behavior may be abusive or aggressive. V CONFUSED, INAPPROPRIATE, NON-AGITATED: Appears alert; responds to commands; follows tasks for 2-3 minutes but easily distracted by environment; frustrated; verbally inappropriate; does not learn new information. VI CONFUSED APPROPRIATE: Follows simple directions consistently; needs cueing; can relearn old skills; serious memory problems but improving; attention improving; self-care tasks performed without help; some awareness of self and others. VII AUTOMATIC APPROPRIATE: If physically able, can carry out routine activities but may have robot-like behavior, minimal confusion, shallow recall; poor insight into condition; initiates tasks but needs structure; poor judgement, problem-solving and planning skills; overall appears normal. VIII PURPOSEFUL APPROPRIATE: Jason Shane and Amanda Mrsic Apr 2015 Alert, oriented; recalls and integrates past events; learns new activities and can continue without supervision; independent in home and living skills; capable of driving; defects in stress tolerance, judgment; abstract reasoning persist; many function at reduced levels in society. Glasgow coma scale: eye opening, verbal response, motor response; from 0-15, less than 8 is severe head injury LANDMARKS: Jason Shane and Amanda Mrsic Apr 2015 second rib = superior angle of scapula Well, that’s it. If you actually made it to the end of this document, congrats! We feel pretty confident you’ll not only pass, but kill the written exam. By the way, not sure if you counted, but this doc is 88 pages long. Whoa, can you say OCD! Happy studying :) Jason + Amanda Jason Shane and Amanda Mrsic Apr 2015
© Copyright 2026
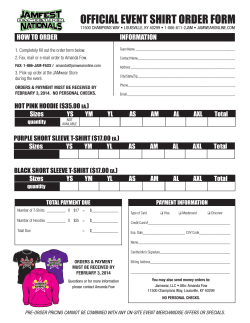



![[Providing secretariat support] FCJ Alliance FCJ INDUSTRY LEADERS](http://cdn1.abcdocz.com/store/data/000912031_1-08458a87461599b827279855750bd754-250x500.png)