View it here! - College of Licensed Practical Nurses of Manitoba
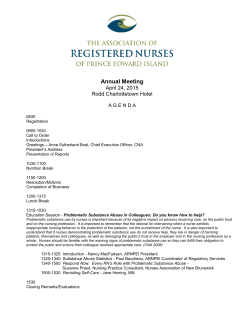
April 2015 practical nursing committed to excellence Donagh Peters, LPN took part in the Continuing Competence Program (CCP) Audit; to learn more, please see page 24. To become a CCP Auditor, please see page 9. 2 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba President Christy Froese LPN Board of Directors District I – Elisa Wiebe LPN District II – Cheryl Geisel LPN District III – Rodney Hintz LPN District IV – Lindsay Maryniuk LPN District V – Jodi La France LPN District VI – Yvonne Maguet LPN Public Members – Darlene Barbe – Tricia Conroy – Judy Harapiak – Diwa Marcelino – Susan Swan Executive Director Jennifer Breton LPN, RN, BN Executive Office Vicky Bering Executive Assistant Barbara Palz, HB Com, CGA Business Manager Renata Neufeld, BA (Hons), MPA Consultant, Policy, Process and Communications Registration Department Kathy Halligan, BA (Hons), CTESL, CACE Consultant, Credential Assessment Carrie Funk, LPN Consultant, Registration Professional Conduct Department Nikki Brett, LPN Consultant, Conduct Alyssa Harder Administrative Assistant, Conduct table of contents President’s Message 3 Meet the New Vice President of the CLPNM 5 Nursing Competencies for Licensed Practical Nurses in Manitoba 7 Ask a Practice Consultant 8 Wanted: Ccp Auditors 9 2015 Annual General Meeting & Awards and Recognition Dinner June 1, 2015 11-13 Legal Issues in Nursing: Communication Patient Safety – Everyone’s Responsibility! 14 Did You Know? 15 15-17 Getting Ready for the RHPA The Centre on Aging: Spring Research Symposium Self-Regulation Rules of Order and Procedure 22 Annual General Meeting Agenda 23 Meet Donagh Peters LPN, CCP Auditor 24-25 Notice to Registrants: By-law Amendments by the CLPNM Board of Directors 2015 Office Closure Dates May 18, 2015 July 1, 2015 October 12, 2015 Education and Program Evaluation Department Michael Roach, BScN Consultant, Education Programs Evaluation June 1, 2015 August 3, 2015 November 11, 2015 Advertising To advertise in the Practical Nursing Journal, please contact: McCrone Publications Inc. Email: [email protected] Toll Free: 1-800-727-0782 Fax: 1-866-413-9328 18 20-21 Professional Nursing Practice Department Tracy Olson, LPN Consultant, Practice Reception Dina Bering Receptionist 10 25 September 7, 2015 Fragrance-Free Notice In response to health concerns, CLPNM has a Fragrance-Free Policy and is a scent-free environment. Please do not use scented products while on the CLPNM premises for work, education, appointments, or other business. College of Licensed Practical Nurses of Manitoba 463 St. Anne’s Road Winnipeg, MB R2M 3C9 Telephone: (204) 663-1212 Toll Free: 1-877-663-1212 Fax: (204) 663-1207 Email: [email protected] Publications Agreement #40013238 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 3 President’s Message I was recently reading through old journal articles from various nursing regulatory colleges looking for inspiration for the last article that I will write for the College of Licensed Practical Nurses of Manitoba’s (CLPNM’s) Practical Nursing Journal. I stumbled upon Lynn Marks’ (former President of the CLPNM) last journal article. Here is an excerpt from it: As the College of Licensed Practical Nurses of Manitoba (CLPNM) moves towards the Regulated Health Professions Act (RHPA), all stakeholders, including licensed practical nurses (LPNs), have the responsibility to stay informed regarding the subject of professional self-regulation. Do you as a registrant know the role of your regulatory college? What is the difference between a professional association, a union, and a regulatory college? Do you know your obligations as a member of a self-regulated profession? Over the years, I have often heard questions such as “What does the College do for me?” or “What does the College do with my fees?” It is important for all registrants to understand that the CLPNM is not an association, and as per legislation, we do not advocate on the registrants’ behalf. The CLPNM is a regulatory body with a mandate of protecting the public through fair, consistent nursing regulation. The role of CLPNM is defined in legislation. Unfortunately, little has changed since Lynn’s retirement in 2012. The CLPNM still faces the same challenges and is still being asked the same questions. As an LPN it is our responsibility to understand what it means to be a member of a self-regulated profession. If you are struggling to answer any of the above questions, I challenge you to participate in a Jurisprudence Education Session offered, free of charge, at the CLPNM. Participating in the CLPNM’s Annual General Meeting (AGM) would also give you a greater understanding of the role of the CLPNM. I would like to take this opportunity to invite you to our AGM on June 1st at the Viscount Gort in Winnipeg. Come and hear about the activities of the CLPNM over the past year and about some of the proposed bylaw changes! I would like to thank the CLPNM’s Board of Directors, Jennifer Breton, Executive Director, committee members, staff members, the practical nursing (PN) schools, other regulators and the Manitoba Nurses Union (MNU) for their friendships and collaborative spirit over the past three years. I am so grateful for the relationships that were established and for all I have learned. All the best to Yvonne Maguet in her new role! -Christy Froese LPN 4 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 5 Meet the New President of the CLPNM how much joy and fulfillment her work gave her being able to help others in need. At the age or twenty-seven the opportunity came around that enabled me to go to school. It was the first and only thing I felt was worth the time it would take away from my family. To this day, I feel it was one of the best decisions I have ever made. How long have you been nursing? I have been nursing for twelve years; I graduated in June 2003. Where do you work and in which area of nursing? I am currently working for the Winnipeg Regional Health Authority as a home visiting nurse. Yvonne Maguet On April 13, 2015, the CLPNM Board of Directors elected Yvonne Maguet as the new President. Yvonne’s term begins June 1, 2015. Christy Froese, current President of the CLPNM, had the opportunity to ask her a few questions about herself and her nursing career. Can you tell me a little bit about yourself? I have been married to my husband for twenty years, and we have two great teenage boys; my husband and my sons are the three most important people in my life. Together we enjoy spending our down time in the kitchen cooking great food from the heart and drinking coffee. When the weather permits, we like to spend time together in the great outdoors. Camping, cooking over an open fire, hiking trails and roasting marshmallows to make s’mores are some of our favourite outdoor activities, which we enjoy with family and friends. What made you decide to go into nursing? My mom is a nurse and she is an amazing lady who I wanted to emulate. When I was young, I saw When did you join the Board of Directors and why? I joined the CLPNM Board of Directors in 2013 because I wanted to do more to help our profession grow. I thought it was fate when the email came out in the spring of 2013 asking for nominations to fill the seat, so I put my name forward. Being chosen as the successful candidate has been a great fortune for the past 2 years. Being a member of the Board has been a great experience and I look forward to the new ones I will have as CLPNM’s new President. 6 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 7 Nursing Competencies for Licensed Practical Nurses in Manitoba The College of Licensed Practical Nurses of Manitoba (CLPNM) is in the process of developing a new competency profile for the Licensed Practical Nurse (LPN) in Manitoba. The new competency profile has gone through an extensive review, which includes a number of revisions and updates to better articulate LPN practice in Manitoba. The competency profile is designed to represent the individual competencies within the profession’s scope of practice. The practical nursing scope of practice comprises the knowledge, skills and judgement that an LPN is legally authorized to perform. Scope of practice is determined through legislation and includes all activities in which practical nurses have been educated in their entry level programs, their individual experience, ongoing professional development and both formal and informal post-basic education. All registrants of the CLPNM are expected to practice within the legislated scope of practice of the profession. Today’s health care and practice settings continue to change rapidly, offering new opportunities and challenges for the LPN. The LPN’s practice requires them to possess the theoretical and practical knowledge required to adapt to these changes in a variety of roles, responsibilities and settings. The LPN’s entry level education is designed to provide the foundation for all of the competencies in the profile, so that knowledge and skills that go beyond entry level knowledge and practice can be achieved through further training and experience. The competency profile for LPNs in Manitoba is designed to outline the outer boundaries of the theoretical knowledge and practical skills of the LPN that fall within the nurse’s scope of practice. As each LPN has individual competencies, work experience and their professional development differs, the competencies that each individual LPN possesses will be unique to them. As this document represents all of the possible competencies an LPN can perform, it is not expected that any one LPN would have all the competencies outlined in the document. What are the Next Steps? The competency profile is in the final stages of review at the CLPNM. Very shortly, the document will be posted on the CLPNM’s website for review by our members and the public. This will be your opportunity to view the draft version of the document and provide feedback to the CLPNM. Once the draft document goes live on the website, you will be sent an email outlining the next steps. 8 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba ASK A PRACTICE CONSULTANT Question: I have accepted a job on a post-partum unit where I will be required to give immunizations. Does this fall within the scope of a licensed practical nurse (LPN) in Manitoba? Answer: Yes, LPNs in Manitoba immunize clients throughout the lifespan. The Manitoba Competency Profile for LPNs (v. May 2007) outlines LPN competencies and specifically covers immunizations in the following major competencies: • Clinic Based Nursing (S) o S-3-1 Demonstrate knowledge and ability to perform a variety of clinic procedures such as (...) immunizations (item #9) • Occupational Health and Safety (T), o T-1-4 Demonstrate ability to achieve competence and/or certification in areas such as ... immunization (item #3) o T-2-2 Demonstrate ability to perform specific health screening and assessment tests such as (...) providing immunizations (item #2) • Medication Administration (U) o U-8-8 Demonstrate ability to administer injections such as: • Subcutaneous * • Intradermal * • Intramuscular * • Intravenous *i.e. routes indicated for immunizations It is the College of Licensed Practical Nurses of Manitoba’s (CLPNM’s) expectation that every LPN in Manitoba will practice within the profession’s scope of practice, their own level of competence, and in accordance with the CLPNM’s Standards of Practice and Code of Ethics. If a nurse feels that they do not have the knowledge, skills or ability to perform immunizations safely and competently, the nurse must ensure that they receive the appropriate and necessary training before administering immunizations independently. Although LPNs in Manitoba receive formal education for this skill set during their entry level program, it is the LPN’s responsibility to ensure employer policy authorizes LPNs to perform immunizations. As per the CLPNM’s Standards of Practice, the LPN is expected to adhere to policies in the employment setting. Before administering an immunization to a client, the LPN must consider: • if informed consent has been obtained; • if a prescription or a medical directive is in place; • if she or he is competent to administer and manage the vaccine including knowledge of the: o normal expected outcomes of the vaccine, o pathophysiology of the vaccine, o risks associated with the delivery of the vaccine, o assessments required with vaccine administration, o nursing interventions pre and post vaccine administration, o if an emergency protocol is in place for anaphylactic reactions, and o documentation requirements associated with the immunization/ facility policy. Should a nurse feel that he/she requires further education or review before administering immunizations, the following resources may be of assistance: • Immunization Competence Education Program (ICEP) for Health Care Professionals (http://www.gov.mb.ca/health/ publichealth/cdc/div/icep.html) • Immunization Competencies for Health Care Professionals (per Public Health Agency of Canada, (http://www.phac-aspc.gc.ca/im/pdf/ ichp-cips-eng.pdf) • WRHA Regional Immunization Manual (http://www.wrha.mb.ca/ professionals/immunization/ 01-01.php) All LPNs are responsible and accountable for their own professional practice and are expected to collaborate with the employer to ensure they have the competencies required to fulfill their role. The CLPNM practice department provides consultation to registrants, employers and other stakeholders regarding LPN practice. The practice department can be reached by phone at (204) 663-1212 or by email at [email protected]. Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba WANTED: CCP AUDITORS Would you like to become more involved with the College of Licensed Practical Nurses of Manitoba (CLPNM)? A great way to start is to become a Continuing Competence Program (CCP) auditor. Auditors are active practicing licensed practical nurses (LPNs) who are responsible for auditing submitted CCP materials. The CLPNM is asking our registrants for assistance in the peer auditing process. The CCP audit occurs in three phases every year from January to April. Auditors spend 1 to 3 days auditing during each phase. CCP auditors are compensated for time spent auditing. If you are interested in serving as a CCP auditor, please submit your resume to: The College of Licensed Practical Nurses of Manitoba 463 St. Anne’s Road Winnipeg, MB R2M 3C9 or by email at [email protected] For further information, please contact the CLPNM at (204) 663-1212. CCP Auditor CCP Auditors 9 10 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 2015 Annual General Meeting & Awards AND Recognition Dinner jUNE 1, 2015 2015 Annual General Meeting RSVP & Awards Recognition Dinner Registration Form Attendee Information: Name:____________________________________________________________ Registration Number (if applicable):__________________________________ Address: __________________________________________________________ City: ____________________ Province:________ Postal Code: _____________ The AGM and Awards and Recognition Dinner will take place at the Viscount Gort Hotel located at 1670 Portage Ave, Winnipeg, Manitoba. The AGM is called to order at 2:30pm * Registration opens at 2:00pm Phone #:_____________ Email:_______________________________________ I am attending: Annual General Meeting (no cost) Awards and Recognition Dinner ($40) Annual Report: Mail me a copy of the Annual Report (no cost) I will access the Annual Report online at www.clpnm.ca. Awards Recognition Dinner Payment Information: Awards and Recognition Dinner Please join us as we honour some exceptional individuals that have made significant contributions to the LPN profession. Dinner will be served at 6:30pm *Cash bar opens at 6:00pm Paid by debit/credit card at the CLPNM office Please charge my (Visa/MasterCard) $____________________________ Card Number:_____________________________________________________ Expiry Date:_______________________________________________________ Signature of Card Holder:___________________________________________ Please complete this form and submit by: • Email to [email protected]; • Fax to (204) 663-1207; or • Mail to: CLPNM 463 St. Anne’s Road Winnipeg MB R2M 3C9 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 11 Legal Issues in Nursing: Communication This article was originally published in CARE Magazine, Fall 2014 issue, by the College of Licensed Practical Nurses of Alberta (www.clpna.com). Reprinted with permission. Article written by: Chris Rokosh, RN, PNC(C), Legal Nurse Consultant and president of CanLNC Incorporated; he is a popular speaker on legal issues in nursing across Canada and in the US. When medical errors cause lasting injury, the patient can sue both the doctor and the nurse. This can result in a medical malpractice lawsuit. Nurses who have been through this experience describe it as extremely difficult - as difficult as other catastrophic life events such as death, divorce and job loss. The experience of being sued affected their work life, personal life, health and well-being. Emotions such as shock, shame, anger, depression and fear were common. Many nurses felt so isolated by their peers that they left their jobs. You do not want this to happen to you. The outcomes of malpractice lawsuits affect patients, healthcare professionals, public funding and the institutions that provide healthcare, but a workplace culture of denial and shame can keep us from talking about the errors that lead to lawsuits, or using them to learn and improve. So let us start a conversation about the most common nursing issues that result in malpractice lawsuits, with a goal of gaining knowledge, avoiding errors and improving patient safety. Because really, isn’t that why we are all here? This article will focus on the source of more medical malpractice lawsuits than any other: communication. Communication issues are so common that research shows that as many as 70% of medical errors involve some form of communication breakdown between the doctor and the nurse. The courts view communication as a critical part of any nurses’ job. The nurse is seen as ‘the eyes and ears’ of the often-absent doctor, and it is accepted that doctors rightly depend heavily on nurses to keep them fully informed of the patient’s condition. The nursing and medical experts who review malpractice cases say that nurses are required to relay important information to the doctor according to hospital policy and the standards of care, and then to document that they have done so. Professional associations direct nurses to communicate appropriate information to appropriate members of the healthcare team through designated channels. Throughout my career as a Legal Nurse Consultant, I have reviewed more than 1000 medical malpractice lawsuits, many of which focused, in part, on what the nurse did or did not tell the doctor. The most common scenario involves a change in a patient’s condition, and either no communication with the doctor or a phone call followed by documentation that simply states ‘doctor aware.’ The nursing notes do not say what doctor is aware, what they were told or what their response was. If the patient later develops an injury and launches a lawsuit, the doctor will often say, “Yes, the nurse phoned me, but she did not tell me how serious the situation was. 12 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba If she had, I would have attended to the patient immediately.” Without supportive documentation in the medical record this can result in a showdown of the nurses’ word against the doctors’. It will be up to the judge to decide who said what and whether or not the nurse met the standard of care. Let us learn more about this from a medical malpractice case involving a lack of communication between a doctor and a nurse. CASE STUDY One summer evening at 7:38 p.m., 17-year-old Will Johnston was struck by a car as he crossed the street on his skateboard. The force of the impact fractured his right tibia, threw him onto the hood of the car and smashed the windshield. He was taken to the E.R. by ambulance where it was noted that his right leg had an obvious deformity and his right calf was very swollen. The toes on his right foot were cyanosed. His foot had normal sensation but limited movement and decreased pulses. Will was in a lot of pain and had multiple doses of IV morphine. At 10:45 p.m., Will was transferred to the O.R. for Intramedullary Nailing of the right tibia. Following surgery, the incision was covered with Sofratulle and gauze, and his leg was stabilized with a back ‘slab cast’ and wrapped with a tensor bandage. Will was transferred to the recovery room ‘in good condition.’ Shortly before 1:00 a.m., he was transferred to the nursing unit where he was cared for by LPN Donna. At 1:45 a.m., Nurse Donna documented that Will was awake, swearing and complaining of ‘excessive pain.’ His right toes were described as ‘pink and warm’ with normal movement. Nurse Donna noted that Will only had ‘fair relief’ from the multiple doses of IV morphine he had been given postoperatively. At 2:00 a.m., Nurse Donna documented that Will was awake and oriented. The colour, sensation and movement to his right foot were described as ‘good’ with a capillary refill time of less than 3 seconds. Will was noted to have ‘severe weakness’ and tingling in his right leg. Overnight, Nurse Donna documented information regarding Will’s medications, intake and output, but there was no further assessment of the colour, warmth, sensation and movement of Will’s foot for the remainder of her shift. At 8:00 a.m., day shift LPN Lucinda started her shift. She described Will as confused. He was not able to correctly identify the month or where he was. He only opened his eyes when he was spoken to. His right leg was again noted to have ‘severe weakness’ and he refused assistance with bathing, stating ‘Leave me alone!’ Serosanguinous drainage was noted on pillow underneath Will’s leg. Nurse Lucinda did not document colour, warmth, sensation or movement. At 9:20 a.m., Will was noted to be ‘yelling and complaining of pain’. Nurse Lucinda documented that she reassured Will’s parents that the amount of pain and drainage were ‘normal for the surgery.’ At 12:00 noon, Nurse Lucinda documented, ‘Right leg remains in slab cast, small amount of sanguinous drainage on upper side. Foot cool, toes swollen and dark, patient states is not able to wiggle toes because it hurts. Has tingling sensation. Will monitor.’ At 1:00 p.m., physiotherapist Steve arrived to teach Will how to walk with crutches. He described Will as ‘anxious ++, yelling out when moved.’ He refused to get out of bed. At 1:25 p.m., orthopedic resident Dr. Smithson arrived on the unit. He noticed that Will had decreased sensation in his right foot and was unable to point or flex his toes. Dr. Smithson removed the cast, measured the pressures in the calf muscles, and diagnosed posttraumatic compartment syndrome. Will was taken back to the OR for fasciotomies to relieve the pressure. Following surgery, he developed multiple complications. The leg became infected and necrotic in spite of surgical intervention and arterial grafting. Fourteen days later, it was amputated below the knee. Will remained in hospital for several weeks. Eighteen months after his discharge, his family filed a multimillion dollar lawsuit against Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 13 LEGAL ISSUES IN NURSING (Continued) the doctor and the hospital, claiming, among other things, that nurse Donna and nurse Lucinda failed to communicate important information to the doctor or the charge nurse. They claimed that the standard of care required them to tell someone about Will’s pain, weakness, sensory loss and colour change. They also indicated that if the doctor had been called earlier, Will would not have lost his leg. Do you think the nurses met the standard of care? Compartment syndrome is a potentially life-threatening condition caused by high pressure in a closed fascial space. The most common site of compartment syndrome is the lower leg (Abramowitz and Schepsis 1994) and young men with traumatic soft tissue injury are known to be at particular risk (Mc- Queen et al 2000). It is a potentially devastating complication of tibial fractures and requires prompt recognition and intervention, as early intervention is critical to avoid permanent damage to the muscles and the nerves. Symptoms of compartment syndrome may include pain that is disproportionate to the injury, pallor of the affected limb, altered sensation (numbness, tingling), tension of the affected muscles, pulselessness below the level of the swelling and, as a late sign, paralysis. Postoperative narcotic administration may mask the pain, which is often the first symptom of compartment syndrome; therefore, it requires careful monitoring for the other symptoms. The nursing plan of care for a patient with a traumatic fracture of the tibia must include, among other things, knowledge and awareness of the possible development of compartment syndrome along with careful and frequent monitoring of the affected limb for colour, warmth, sensation, movement and pulse strength. Monitoring may be required as frequently as every hour, but certainly every 4 hours in the early postoperative period. Monitoring guidelines are often established by hospital policy or care plans or may be provided by doctors’ orders. Signs and symptoms of compartment syndrome must be reported immediately to the charge nurse and/ or responsible physician. The nursing standard of care would be to notify the physician immediately, requesting a ‘hands on’ assessment of the patient. The nurse must provide an accurate clinical picture of patient status and raise the level of concern. If the physician does not respond promptly to the nursing request for assessment, the nurse must act in the best interest of the patient and persist in finding appropriate medical attention. This may require repeated pages/phone calls to the physician, refusing to take doctors’ orders over the phone, notifying the nursing supervisor or accessing the appropriate ‘Chain of Command.’ The lawyer representing Will in this malpractice lawsuit asked other nurses to review the medical record to determine whether or not nurse Donna and nurse Lucinda had met the standard of care. Their opinion was that Donna and Lucinda had not met the standards in two important areas: by not assessing Will’s leg as thoroughly and frequently as required by hospital policy, and by not reporting his pain, weakness, colour change and sensory loss to the charge nurse or the doctor. Their opinion was that nurse Donna should have reported these changes no later than 2:00 a.m. when she documented that Will had severe weakness and tingling in his right leg. Since this did not happen, their opinion was that nurse Lucinda should have performed a full assessment of the leg at 8:00 a.m. and asked the doctor to see Will right away. The reviewing nurses said that these failures represented a lack of nursing knowledge and critical thinking as well as a failure to meet the standard of care. They also said that the lack of communication contributed to a delay in treating Will’s compartment syndrome, which ultimately led to the loss of his leg. Based on this information, the case settled out of court for an undisclosed amount of money. The doctor in this case was also sued, but ‘let out’ of the lawsuit when it was discovered that he did not know that anything was wrong with Will’s leg because the nurses had not communicated with him. By the time the resident examined Will on rounds, the compartment syndrome had already caused irreversible damage. Use this case study to spark a conversation on communication with your colleagues. How would you rate the level of communication in your workplace? Have you ever witnessed, or been part of a situation where communication caused a problem? Did the patient suffer as a result? What are the designated channels of communication in your workplace? Do they work? If not, what actions have you taken to fix or improve the situation? What will you do better now that you know what you know? 14 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba Patient Safety – everyone’s responsibility! Most of the time, people’s experiences as patients, family members, and healthcare providers in the healthcare system are positive. However, at times things do not go as planned. Patient safety involves the complex interaction among institutions, technologies, and individuals, including patients themselves. In other words, patient safety is everyone’s responsibility. 5.What are key interpersonal and communication skills required for effectively working with patients and families, and within multidisciplinary healthcare teams? In Canada and the world, there are significant numbers of people who are harmed or who die as a result of their care and not the treatment process or risks involved. In a 2004 study1, using data from 2000, there was an adverse event rate of 7.5% in acute care hospital admissions in Canada. By extrapolation, it was estimated that: Healthcare providers try to do the right thing, but because they work in a complex, imperfect system with many variables, at times patient safety incidents reach the patient. Some incidents do not cause harm, but others do affect patients - the people health providers are committed to helping. 6.What are the major concepts related to recognizing and managing risks to patients in healthcare environments? The tradition and culture of healthcare provision has been one that suggests that error is unacceptable, and acknowledgement of mistakes is an admission of lack of skill. It has become evident from our successes, and from patients who have been harmed during the healthcare delivery process, that this approach has deterred the development of a culture that supports learning and improvement. Patient safety – make it YOUR responsibility! • 185,000 of 2.5 million similar admissions to acute care hospitals in Canada were associated with an adverse event; • close to 70,000 of the adverse events were potentially preventable, and • between 9,000 and 24,000 Canadians died from adverse events that could have been prevented. Since the 2004 study, studies in pediatric healthcare and home care have been conducted. The Canadian Pediatric Adverse Event Study2 involved 22 hospitals in 7 provinces. The study determined that 9.2% of children hospitalized in Canada experience an adverse event. “Safety at Home – A PanCanadian Home Care Study” found the rate of adverse events in Canadian home care clients was 10 -13 per cent over a period of one year3. Extrapolating to the over one million home care recipients per year in Canada suggests that up to 130,000 Canadians receiving home care experience an adverse event, with half being considered to be preventable. Acknowledging that patient incidents do happen is important to taking personal and organizational steps to improvement. A key strategy to support your learning is to reflect on basic concepts of patient safety, and how you can apply these concepts in your daily practice. In upcoming issues of the Practical Nursing Journal, key patient safety topics will be highlighted along with questions to stimulate self-reflection about your own practice. Topics to be covered will be aimed at providing answers to the following questions: 1.How do key human and environmental factors contribute to patient safety? 2.What is a culture of patient safety? 3.What are the key elements of effective patient and family centred care? 4.What are key factors that promote effective teamwork in multidisciplinary healthcare teams? 7.What are the key elements required in responding to and disclosing harmful incidents? For more information on patient safety, go to the Manitoba Institute for Patient Safety website at www.mips.ca. 1 Baker, GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian Adverse Events Study: The incidence of adverse events among hospital patients in Canada. Canadian Medical Association Journal. 25 May 2004; 170 (11): 1678 – 1686. 2 Matlow AG, Baker GR, Flintoft G, Cochrane D, Coffey C, Cohen E, et al. Adverse events among children in Canadian hospitals. The Canadian Paediatric Adverse Events Study. Canadian Medial Association Journal. 18 September 2012; 194 (13): E709 – E718. 2 The Canadian Patient Safety Institute. Safety at Home – A Pan Canadian Home Care Safety Study. 2013. Available at http://www.patientsafetyinstitute.ca/ English/research/commissionedResearch/ SafetyatHome/Documents/Safety%20 At%20Home%20Care.pdf Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba Did you know? 15 Getting Ready for the RHPA The College of Licensed Practical Nurses of Manitoba (CLPNM) continues to work on the transition to the Regulated Health Professions Act (RHPA). In recent editions of the Practical Nursing Journal, we have introduced you to the RHPA, outlined some of the changes you can expect, and invited your input to help inform the transition. As this work continues, we will keep you updated in each edition of this Journal. The College of Licensed Practical Nurses of Manitoba (CLPNM) is a member of the Manitoba Alliance of Health Regulatory Colleges (MAHRC). Together, the members of the MAHRC regulate over twenty health professions. We ensure health care is delivered by providers who are appropriately educated and who follow standards of conduct and codes of ethics. Our goal is safe, quality health care. Read more about the MAHRC and health regulation in Manitoba at mahrc.net. What is the RHPA? For those who missed our previous articles on this topic, the RHPA is a law that will eventually govern the practice of 22 regulated health professions in Manitoba. It is being rolled out incrementally. It will modernize and standardize how Manitoba’s health professions are authorized and regulated. The goals of the RHPA are to: • continue to support self-regulation by Manitoba’s health professions; • continue to protect patients and the public interest; • remove barriers to interprofessional practice; • foster greater confidence in the provincial health care system, and • better regulate certain high-risk health care activities. The RHPA does not yet apply to LPNs, but it soon will. Practical nursing in Manitoba will continue to be governed by the Licensed Practical Nurses Act and its Regulations until they are replaced by the RHPA. As part of the transition to the RHPA, the CLPNM has published a new Code of Ethics and is in the process of finalizing an updated Competency Profile. The new Code of Ethics is available on the CLPNM website at www.clpnm.ca. The CLPNM will also post a draft of the revised Competency Profile for review and comment this spring. We have also begun a review of the profession’s scope of practice statement, and have continued validating the reserved acts that Manitoba LPNs have the competence and skill to perform. 16 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba Scope of Practice A profession’s scope of practice refers to the outer range of activities that its members are educated and legally authorized to perform. This scope of practice is described in a scope of practice statement. Scope of practice statements typically form part of the legislation that regulates the profession. They are intended as concise, but comprehensive, descriptions of the limits within which a member of a profession can practice. With the transition to the RHPA, we are presented with a rare opportunity to review the scope of practice statement that defines the profession of practical nursing in Manitoba. The current scope of practice statement in Section 2 of the Licensed Practical Nurses Act is: “the provision of nursing services for the purpose of assessing and treating health conditions, promoting health, preventing illness, and assisting individuals, families and groups to achieve an optimal state of health.” Does this capture the profession? Do you see your practice in this statement? Tell us what you think at: clpnm.ca/rhpa! A scope of practice statement describes a profession as a whole. Each member of that profession also has his or her own individual scope of practice, informed by professional standards, any conditions on his or her license, employer policies and the individual’s unique competencies. If you want to learn more, please visit : www.clpnm.ca/standardsguidelines/scope-of-practice/ The CLPNM has begun working on this review collaboratively with representatives from Manitoba Health, Healthy Living and Seniors. The goal is to ensure that the scope of practice statement, eventually set out in the RHPA’s Regulations, appropriately captures the profession of practical nursing in Manitoba today. As part of this review, we have conducted an environmental scan of other Canadian jurisdictions. We have also reviewed information about current LPN practice in Manitoba to identify areas that may not be well-reflected in the existing scope of practice statement. It is important to note that revisions to the scope of practice statement are not intended to change the actual practice of Manitoba’s LPNs. Rather, revisions are intended to ensure that the statement correctly reflects today’s practice. It is also important to note that, in keeping with the goals of encouraging interprofessional practice and improving access to health care, it is possible that different health professions will have overlapping scopes of practice. We will continue to work on this review with Manitoba Health, Healthy Living and Seniors and keep our members updated through the Journal. Reserved Acts While we are reviewing the scope of practice, we are continuing to validate the reserved acts that Manitoba’s LPNs have the competence and skill to perform. The reserved acts are a list of health care activities that could pose significant risk or possible harm to the public if performed by someone without the necessary training. There are 21 reserved acts listed in the RHPA. A few examples are: • performing a procedure below the dermis • inserting or removing an instrument, device, hand or finger into an opening of the body • administering a substance by injection, inhalation, mechanical ventilation, irrigation or by enteral or parenteral instillation • prescribing, compounding, dispensing, selling or administering a drug or a vaccine For a complete list of the reserved acts, please visit www.clpnm.ca/rhpa. As each regulated health profession transitions to the RHPA, the Manitoba Government will develop Regulations that identify which reserved acts each profession can perform. The CLPNM’s role, as a regulatory body, is to propose which activities Manitoba’s practical nurses can perform safely and effectively. To ensure this proposal captures the full extent of current LPN practice, we are consulting with LPNs, educators, employers, LPN regulators, and other stakeholders. Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 17 Are you an LPN who works in an Emergency Department or Mental Health Care setting? Manitoba, please review the Competency Profile at www.clpnm.ca. The CLPNM needs to hear more about your role and about the reserved acts you perform in these environments. We will be holding the following consultation sessions: What’s Next? May 5 May 6 May 7 May 8 1700 – 1830 Mental Health 1430 – 1600 Emergency Department 1700 – 1830 Emergency Department 1430 – 1600 Mental Health All sessions will take place in person at 463 St. Anne’s Road in Winnipeg and by teleconference. Please register in advance by calling 204-663-1212 or 1-877-663-1212 (toll free), or online at www.clpnm.ca. Sessions with low registration may be cancelled. To date, these consultations have included 12 group sessions with practising LPNs from across the province, and two online member surveys. One survey provided us with information on unique LPN roles in Manitoba. The other gathered information on the reserved acts that LPNs perform in Manitoba today. These surveys were open to our members between July and December 2014, and resulted in hundreds of responses from LPNs across the province, working in practice settings including community, primary care, emergency, medicine, surgery, geriatrics, pediatrics, operating rooms, mental health, labour and delivery, post-partum, dialysis, home care, long-term care, palliative care, corrections, and foot care, among others, and in roles ranging from staff nurse to educator, charge nurse and administrator. These responses will help to ensure that CLPNM’s proposal to Government reflects the range within the LPN profession and is supported with specific examples from current practice. We are now reviewing and analyzing the data, and in the coming months we will be contacting some survey respondents with follow-up questions on topics that require more detailed information. If you are one of the respondents, please keep your eyes on your inbox. During the course of our consultations, we heard many questions about the reserved acts and some concerns about how they might impact practice. You can review these questions and our responses in our Frequently Asked Questions available at www.clpnm.ca/rhpa. How do Scope of Practice and Reserve Acts Relate? When a reserved act is authorized for a profession, it will serve as confirmation that the activity falls within that profession’s scope of practice. The reserved acts will help to fill in the picture. However, the reserved acts will only represent a portion of any profession’s scope. They will only fill in part of the picture. This is because the list of reserved acts is limited only to certain health care activities that pose particular risk to the public. It is not a comprehensive list of all health care activities. To view a more detailed description of the competencies that fall within the profession of practical nursing in In the coming months, work on the RHPA transition will also include: • determining which reserved acts LPNs should be authorized to delegate to others, including unregulated health care providers • revisions to the profession’s Standards of Practice • development of the processes CLPNM will need to effectively regulate corporations that carry on the practice of practical nursing, referred to as “health profession corporations” in the RHPA More information on these topics will appear in future Practical Nursing Journal articles. The transition to the RHPA will result in a lot of change. Ongoing communication with and input from our members and stakeholders will be critical throughout the process. If you are interested in providing information about your current practice, participating in a discussion to help inform the RHPA transition, or have questions related to the RHPA, please contact: Renata Neufeld, Consultant Policy, Process and Communications College of Licensed Practical Nurses of Manitoba 204-663-1212 1-877-663-1212 toll free [email protected] If you would like to read more about the RHPA, please visit www.clpnm.ca/rhpa. 18 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba The Centre on Aging: Spring Research Symposium The Centre on Aging, University of Manitoba, is a university-wide research unit reporting to the Vice President (Research & International). Established on July 1, 1982, the Centre developed and established a national and international reputation for research excellence in aging. The Centre’s vision is “To be a recognized leader in research in aging; to improve the lives of older adults, their caregivers and families, and to enhance communities within and outside of Manitoba.” The Centre on Aging conducts, stimulates and promotes research on aging, provides an interdisciplinary focus for the research activities in aging at the universities in Manitoba, and supports the teaching of students in aging. The Centre serves as the focal point for the integration and dissemination of research on aging in Manitoba. The Centre on Aging holds an annual Spring Research Symposium to promote a dialogue between university researchers and the community-at-large. Researchers present findings from their research, and community representatives discuss the impact of the research on policy, practice and quality of life for older adults. Topics vary from year to year. In the past, over 400 individuals registered for the event. These included faculty members, graduate students, and staff from various faculties, federal government representatives, provincial government representatives, program representatives from regional health authorities, hospital staff, representatives from personal care homes/long-term care facilities/ supportive housing from other social agencies and the public. The Symposium promises to be an exciting and educational day. There is no charge for the symposium. All are welcome to attend. For information, please contact the Centre at (204) 474-8754. Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 19 32nd Annual Spring Research Symposium May 4–5, 2015 727 McDermot Ave | Bannatyne Campus, University of Manitoba Registration forms are available at: http://www.umanitoba.ca/centres/aging/events/384.htm Monday, May 4, 2015 8:45 a.m.–4:00 p.m. | Brodie Centre 8:00 a.m. Registration desk is open in Brodie Centre 8:45–9:15 a.m. Welcome and greetings Presentation of research fellowships and student awards 9:15–10:30 a.m. OPENING PLENARY The Canadian Longitudinal Study on Aging: What’s in it for me? Parminder Raina, Ph.D., Director of the Evidence-based Practice Center; Professor, Department of Clinical Epidemiology & Biostatistics, McMaster University; Lead Principal Investigator of the Canadian Longitudinal Study on Aging (CLSA); Verena Menec, Ph.D., Professor, Department of Community Health Sciences, College of Medicine, University of Manitoba; Canada Research Chair in Healthy Aging; Manitoba Site CoPrincipal Investigators for CLSA The Canadian Longitudinal Study on Aging (CLSA) is a large, national, long-term study that will follow approximately 50,000 men and women between the ages of 45 and 85 for at least 20 years. The ultimate aim of the CLSA is to find ways to improve the health of Canadians by better understanding the aging process and the factors that shape the way we age. Information about the changing biological, medical, psychological, social, lifestyle and economic aspects of people’s lives is being collected and analyzed. By January 2015 the first 45,000 participants were recruited. Dr. Raina and Dr. Menec will describe how CLSA data may be used to help improve the lives of people in Canada and around the world over the next 20 years. 10:30–11:00 a.m. Morning break, Brodie Centre 20 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba Self-regulation The practical nursing profession is one of several self-regulating health professions in Manitoba. Do you know what self-regulation means? Do you know how it affects your profession and practice? Self-regulation is a privilege and responsibility granted by the Government of Manitoba to the members of the practical nursing profession. It recognizes your specialized expertise. By granting self-regulation, the government has acknowledged that practical nurses are in the best position to hold one another accountable for providing safe and effective care that meets the standards of the profession and serves the interests of the public. Effective self-regulation contributes to confidence in the profession overall. When members of the profession hold one another accountable, the public can trust that it will receive safe, competent and ethical care. When you contribute to self-regulation, you help to maintain and strengthen this trust. You also help to maintain the privilege of self-regulation itself. The profession’s authority to self-regulate is delegated by government, which means that, if not done effectively, the authority could be limited or even taken away. Self-regulation differs from the role of a professional nursing association or union. While each have nurses as their membership base, the goal of self-regulation is to protect the public interest. This does not mean that the interests of nurses and their clients are in conflict. For example, nurses and clients share an interest in quality care and good clinical outcomes; however, when the interests of a nurse and the public do not align, it is the duty of the selfregulating profession to uphold and protect the public interest above all else. Self-regulation is carried out in part through the College of Licensed Practical Nurses of Manitoba (CLPNM). The Board of Directors, committees and staff of the CLPNM all include LPNs who use their nursing expertise daily when reviewing education programs, making licensure decisions, supporting practice, informing the public and employers about the profession, and overseeing professional conduct. However, all practical nurses in Manitoba share the responsibility of self-regulation, including you. There are a number of ways that your LPN peers are participating in self-regulation by contributing to the work, programs, and governance of the CLPNM. Each year, the continuing competence program (CCP) reviews are carried out by your peers. CCP auditors are active practising LPNs. They review your learning plans and provide you with feedback to help you grow as a competent nurse. In the rare circumstances where practice audits or investigations are needed, these are also carried out by active practising LPNs. This past year, many LPNs offered their time and experience by participating in consultation sessions and surveys on LPN practice. These were held to inform how the profession will be supported and regulated under the Regulated Health Professions Act (RHPA). Initial consultations focused on confirming the health care activities that LPNs have the skills to perform. Additional Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba consultations will be carried out this coming year. This ongoing input from CLPNM members will help to inform how the profession is defined, enabled and regulated in the future. In addition to participating on the Board and committees of the CLPNM, LPNs contribute to the governance of the profession by attending the Annual General Meeting (AGM). Each year at the AGM, LPNs have an opportunity to learn more about the activities of the CLPNM, speak their opinion and vote on issues that impact the profession. LPNs also have an opportunity to contribute to the governance of the profession by nominating and electing peers to the CLPNM Board. Engaging in the work, programs and governance of the CLPNM are some of the ways that LPNs help to support and regulate the profession. Self-regulation happens at many levels though. As practical nurses, we contribute to self-regulation each day when we take personal accountability for ensuring we have the knowledge, skills and judgement to provide safe, competent and ethical care, and by ensuring that our peers do as well. You are contributing to self-regulation when you… Know Your Standards Review, understand and apply the professional expectations in your Standards of Practice, Code of Ethics and Regulatory Bulletins. ` Ask Questions Acknowledge if you do not understand a professional obligation. Seek guidance by consulting a peer or mentor in your workplace, calling a CLPNM Practice Consultant or attending a CLPNM jurisprudence session. Build Your Knowledge Demonstrate your commitment to lifelong learning. Stay current on best practices in nursing. Assess your knowledge, identify gaps and follow through with a learning plan. Help Others Grow Provide feedback to your peers. Act as a resource to new nurses. Support others to practice to the full scope of their competence. Hold Others Accountable Hold your peers accountable to the standards of the profession. Advocate for your clients; take action when you see unsafe practice, and if necessary, exercise your duty to report. For more information on self-regulation and how you can become more involved, contact the CLPNM by email at [email protected] or by telephone at 204-663-1212 or 1-877-663-1212 toll free, or visit us at www.clpnm.ca. We contribute to selfregulation each day when we take personal accountability for ensuring we have the knowledge, skills and judgement to provide safe, competent and ethical care. 21 22 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba RULES OF ORDER AND PROCEDURE 1. 2. 3. 4. 5. 6. The current edition of Robert’s Rules of Order Newly Revised shall be the parliamentary authority on any procedural matter. Every member who is a practicing licensed practical nurse in good standing with the College is entitled to voice and vote. Every graduate and student practical nurse is entitled to voice at Annual or Special meetings of the College. Every Associate member [non-practicing, senior] is entitled to voice at Annual or Special meetings of the College. Public representatives are entitled to voice at the annual or special meeting of the College. Members will be required to present at the meeting, current photo identification as evidence of entitlement to vote. 7. Voting members shall be issued a voting card, in a colour designated by the President. A majority of registrants present and eligible to vote at the meeting shall be needed for adoption of any business, unless otherwise stated in the bylaws. 8. 9. The eligible voting members present at the meeting shall determine the manner of voting. A vote may be taken by ballot or by show of hands. The meeting Chair shall appoint three [3] Scrutineers, who shall tabulate the vote for and against in the show of hands, or in the event of a ballot vote shall distribute, collect and count the ballots and report the results in writing to the chair. 10.In the event of a tie vote, either by show of hands or ballot vote, the Chair of the meeting shall cast the deciding vote. 11.A quorum for any annual general meeting or special general meeting of the College shall be the number of members on the register of practicing licensed practical nurses who attend the meeting. 12.At any time if a member exits the meeting room for the day, the member must turn their voting card over to one of the Scrutineers designated by the Chair. Members shall not enter or exit the meeting room when there is a motion on the floor. 13.Any member or Board member wishing to speak shall go to a microphone, address the Chair, give their name and district, and shall indicate whether they are speaking in the affirmative or negative on the motion. 14.All motions and amendments shall be in writing on motion paper, signed by the maker and seconded, and shall be sent to the Chair after they have placed it before the membership. 15.Only voting members have the right to make a motion and shall have the right to speak to the motion first. 16.Members and Board members shall speak only once to any given question until all members wishing to speak have done so. 17.Debate is limited to two [2] minutes for each member and ten [10] minutes for each question. The Chair shall alternate between microphones. 18.A timekeeper shall be designated for each microphone and shall signal with a yellow card when two minutes has passed, and shall signal with a red card when allotted time for debate on the question has expired. 19.Time for debate may be extended by a two-thirds [2/3] vote of the members. 20.A call to close debate [move the previous question] requires a two-thirds [2/3] vote of the members. Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 23 Annual General Meeting Agenda Date: Monday June 1, 2015 Time: 1430hrs Location: Viscount Gort Hotel Winnipeg, MB Registration (begins at 1400hrs) Announcements Call to Order (1430hrs) Credentials Report Approval of Agenda Introductions President’s Welcome Appointment of Scrutineers Annual Report & Current College Activities Adoption of Proposed By-law Changes Election Results – Presentation of Board of Directors Open Forum Adjournment 24 Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba Meet Donagh Peters LPN, CCP Auditor Every year for the annual Continuing Competence Program (CCP) audit, an audit party consisting of active practicing licensed practical nurses (LPNs) assesses submitted CCP materials to determine if they comply with the expected standards. The auditors, the CLPNM, and the registrants all work together to ensure that LPNs are aware of their expectations with the CCP. The CLPNM offers registrants guidance on how to complete their CCP by way of regularly scheduled informative sessions offered in-house at the CLPNM or via teleconference. In addition, a CCP instruction guide and various fact sheets are made available for registrants in order to provide further direction and support with regard to their expectations surrounding the CCP. To register to attend a free-of-charge CCP information session and to find the instruction guide, please go to the CLPNM website at www.clpnm.ca. Licensed practical nurses understand that competence is continually acquired and maintained through professional self-reflection and lifelong learning that is integrated into nursing practice. Understanding and complying with the CCP contributes to continued competence of LPNs, which ultimately contributes to the CLPNM’s mandate to protect the public. Meet Donagh Peters, LPN and a 2014 CCP auditor. Donagh graduated from the practical nursing program at Assiniboine Community College (ACC) in May 2012. She began her career in the Short Stay Unit at the Grace General Hospital. In August 2013, Donagh took a position at the Misericordia Health Centre where she continues to work today in the Interim Care Unit. In April 2014, Donagh completed the CLPNM-approved nursing foot care course at ACC. In addition to her casual position at Misericordia Health Centre, Donagh is now co-owner of PediHealth Services where she practices nursing foot care as an independent practitioner. In the three years Donagh has been a nurse, she has contributed to the self regulation of her profession by assisting the CLPNM in its public protection work. Since 2013, Donagh has been a member of the CLPNM’s Education Approval Committee (EAC), whose responsibility it is to review and monitor practical nursing education in Manitoba. In 2014, the Board of Directors appointed Donagh as a practice auditor and an investigator for the CLPNM. In addition, she has participated as a CCP auditor in 2014 and 2015. Recently, the CLPNM had an opportunity to sit down with Donagh to learn more about her and to have her share her experience participating as a CCP auditor. 1. How would you describe your role as a CCP auditor? This was my second year as an auditor for the Continuing Competence Program. My role as an auditor requires me to seek out evidence of nurses’ continued learning and growth. Along with the other members of the auditing team, I am assessing for the inclusion of evidence of learning interventions, evidence of knowledge gained and evidence of knowledge applied into practice. It is a large and important task that I enjoy but take very seriously. As a member of a self-regulating profession, I recognize the importance in assuring that all of us are meeting our practice standards and registration requirements. 2. How has the role of CCP auditor impacted you? Taking the time to fully understand the CCP then having the opportunity to work alongside such a great group of LPNs during the audit has taught me so much about this profession. The experience has been a great opportunity to see all the different areas in which LPNs are practicing, and it has allowed me to share in their wealth of knowledge. Completing my nursing foot care education and entering into independent practice has been an overwhelming but rewarding challenge. By participating as an auditor, I have gained a better understanding of my responsibilities in policy development and implementation. I fully believe continuing our education as nurses is so important to ensure continued best practice and compliance with our practice standards. I have really enjoyed being a part of this process. Practical Nursing | April 2015 | College of Licensed Practical Nurses of Manitoba 3. Why do you think it is important to be involved with your regulatory body? Being involved with the CLPNM was something I knew I wanted to do since graduating from the practical nursing program. I recognize the importance and privilege of being a member of a self-regulating profession. I understand that selfregulation allows for the profession itself to monitor our members to ensure they are delivering safe, competent and ethical nursing care. Keeping my clients safe is very important to me. Being actively involved with the CLPNM is another way that I can contribute to their safety and it is a way that I can make a difference in my profession. Also being a member of the Education Approval Committee allows me to contribute to practical nursing education in the province—to make a difference in the development of future members of the profession. 25 If you are interested in serving as a CCP auditor, please submit your resume to: The College of Licensed Practical Nurses of Manitoba 463 St. Anne’s Road Winnipeg, MB R2M 3C9 Or by email at [email protected] For further information, please contact the CLPNM at (204) 663-1212. Notice to Registrants: By-law Amendments by the CLPNM Board of Directors The CLPNM Board of Directors has amended the By-laws. The amendments will be presented for approval at the 2015 Annual General Meeting (AGM). Please contact Christy Froese LPN, President, if you have any questions or comments by phone at (204) 663-1212, or by email at [email protected]. Current By-law Wording Proposed Changes: Rationale 2.7 Associate Members The current 2.7 would be deleted and replaced with: The category of non-practicing associate members will be phased out. Previously, this membership category entitled individuals to receive information and documents from the CLPNM. These are now issued electronically and publicly, making the membership category and the fees associated with it unnecessary. Associate members shall include the following categories; nonpracticing and honorary members, as defined by registration policies. 2.7 Honorary Members The Board may confer honorary memberships upon any individual, in accordance with Board policies. The Board would retain the ability to grant honorary memberships. Honorary memberships, like awards, are a means of recognizing an important contribution to the profession. They do not authorize the individual to practice the profession.
© Copyright 2026