Open Reduction and Internal Fixation of Pediatric T
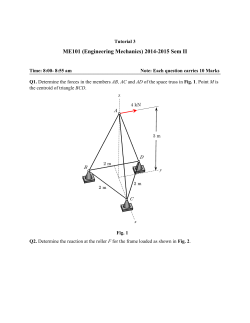
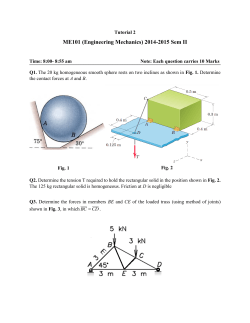
Open Reduction and Internal Fixation of Pediatric T-Condylar Fractures Keith D. Baldwin and John M. Flynn DEFINITION ■■ ■■ ■■ T-condylar fractures of the distal humerus in children and adolescents are relatively rare occurrences. They are thought to represent 2% of all pediatric elbow fractures.5 The proposed mechanism is similar to that of pediatric supracondylar fractures but with a higher energy mechanism of injury.6 A C ■■ ■■ 8 CHAPTER The olecranon acts as a wedge during hyperextension and creates a Y- or T-shaped fracture with the center in the olecranon fossa. These fractures are less likely to be comminuted than in adults. In younger children, an acceptable result can often be obtained with closed reduction and pinning, although this is generally not as straightforward as in a standard supracondylar humerus fracture (FIG 1). B D FIG 1 l A,B. An 8-year-old boy with T-condylar distal humerus E F fracture. C,D. Fixed with mini-open reduction with intercondylar screw compression and K-wire fixation of the distal humerus to the shaft. E,F. After hardware removal, the patient had 0 to 140 degrees range of motion with no pain. 1 2 Pa r t 4 Pediatric A B C FIG 2 l A,B. A 15-year-old boy with type IIIA open distal humerus comminuted T-condylar humerus fracture. C,D. Three months following open reduction and internal fixation with olecranon osteotomy. Range of motion 0 to 140 degrees with no pain. D ■■ ■■ ■■ Older children and young adolescents will often require an open approach. Comminution in the fossa may necessitate an olecranon osteotomy (FIG 2). Generally, pediatric fractures are less comminuted than adult fractures and may not require a full osteotomy. ■■ A Morrey slide approach is used in such a case where the triceps and ulnar periosteum are elevated off the ulna medially to expose the distal humerus without performing an osteotomy.3 ■■ It was originally described to avoid olecranon osteotomies in cases where total elbow replacement would be a salvage operation. ■■ It can be useful in adolescents because the fractures are not as comminuted, but excellent visualization of the joint A is desirable to provide anatomic reduction and restoration of elbow function. ANATOMY ■■ ■■ ■■ ■■ The distal humerus is a complex articulation. The ulnohumeral articulation is the articulation which needs to be reconstructed in this type of fracture. Occasionally, the radiocapitellar joint is also damaged with capitellar comminution (FIG 3A). The remainder of the limb should be carefully examined. Coexisting wrist fractures can increase the risk of compartment syndrome and other soft tissue complications (FIG 3B). Conceptually, the distal humerus is a hinge which contains a medial and a lateral column connected by a middle hinge. B FIG 3 l A. A 13-year-old boy with a T-condylar humerus fracture with coronal split of the capitellum. B. Fracture blisters result from severe soft tissue injury. C h a p t e r 8 Open Reduction and Internal Fixation of Pediatric T-Condylar Fractures Medial column 3 Lateral column Olecranon fossa FIG 4 l Triangle of stability concept. The me- Medial epicondyle chanical properties of the distal humerus are based on a triangle of stability, comprising the medial and lateral columns and the articular surface. (Adapted from Bonczar MR, Rikli D, Ring D. Distal humerus 13-C1 open reduction; perpendicular [biplanar] plating. AO Foundation Web site. Available at: http://bit.ly/1wEegQS. Published June 21, 2007. Accessed November 1, 2013.) Articular surface Olecranon ■■ ■■ ■■ ■■ ■■ This creates a “triangle of stability,” which must be recreated in order for fixation to be successful in T-condylar humerus fractures.2 Regardless of the fixation strategy, this concept must be followed (FIG 4). Posteromedially, the ulnar nerve travels through a groove in the distal humerus called the cubital tunnel. The nerve must be exposed along the medial border of the triceps down to the first motor branch, which pierces the flexor carpi ulnaris. The triceps covers the distal humerus and attaches to the proximal ulna at the olecranon process. The olecranon obscures the view of the distal humerus articular surface, with the elbow in extension. To visualize the fracture line with the Morrey slide, the elbow must be flexed past 90 degrees. Also important, the distal fracture fragments typically rotate with the apex anteriorly, which is important to remember when reducing the joint surface. PATHOGENESIS ■■ ■■ The mechanism of injury is a direct impact of the semilunar notch or coronoid process of the olecranon. Either of these structures can wedge into the trochlea, causing a split in the condyles. This most frequently occurs with a fall of the flexed elbow. ■■ IMAGING AND OTHER DIAGNOSTIC STUDIES ■■ ■■ ■■ ■■ The natural history of this fracture without anatomic restoration is characterized by stiffness, varus malunion, and chronic elbow dysfunction. PATIENT HISTORY AND PHYSICAL FINDINGS ■■ ■■ Mechanism of injury is important to obtain, higher energy injuries suggest an increased risk for compartment syndrome A careful neurovascular examination should be performed, with particular attention to the median, ulnar, and radial nerves. Quality anteroposterior (AP) internal and external oblique views can be useful if the diagnosis is in question. Traction views can often be useful in fractures where shortening is present, although children and adolescents will often tolerate these poorly. Computed tomography (CT) can be useful, but the coronal and sagittal reconstructions must be rendered in the plane of the joint or perpendicular to it (normal AP and lateral planes); otherwise, the information obtained will be difficult to interpret. Coronal fragments may be missed if high-quality imaging is not obtained (see FIG 3A). DIFFERENTIAL DIAGNOSIS ■■ ■■ ■■ NATURAL HISTORY ■■ The limb should be inspected for open wounds. High-energy T-condylar fractures are often open injuries. T-condylar fractures must be differentiated from other fractures of the distal humerus in children and adolescents because the treatment will differ. High-quality radiographs are generally sufficient to make this diagnosis. A CT or traction views can be helpful if the diagnosis is in question or if a coronal shear fragment is suspected on plain radiographs. NONOPERATIVE MANAGEMENT ■■ ■■ ■■ Initial management includes a well-padded splint following adequate physical examination. If the injury is open, an intravenous (IV) first-generation cephalosporin should be administered as soon as the injury is identified. If there is excessive contamination, comminution, or soft tissue injury, IV gentamicin is also recommended. There is limited value in nonsurgical management with the exception of patients with nonfunctional upper limbs at baseline. 4 Pa r t 4 Pediatric SURGICAL MANAGEMENT ■■ ■■ ■■ ■■ ■■ ■■ Open injuries should be addressed surgically within 24 hours; closed injuries may be addressed semielectively. Attention is given to the distal radius; “floating elbows,” in which both the distal humerus and distal radius and/or ulna are affected, are not uncommon. These injuries should be identified early, as they are at increased risk for compartment syndrome. The soft tissue envelope is an important consideration. Fracture blisters (see FIG 3B) can be present, which can compromise the sterility and the closure of the procedure. The vast majority of T-condylar humerus fractures require operative treatment. In younger children, a percutaneous or mini-open approach may be possible. In older children and adolescents, an open posterior approach offers direct visualization and anatomic reduction and fixation of fracture fragments. Preoperative Planning ■■ ■■ ■■ ■■ High-quality AP and lateral radiographs are mandatory prior to surgery. Internal and external oblique views may be useful in identifying columnar comminution. CT scan can be useful in identifying coronal shear fragments. Method of fixation should be chosen by patient age, degree of displacement, and amount of comminution. ■■ Specialized distal humeral plating systems are available from several different manufacturers to allow either bicolumn or “90:90” plating. Positioning ■■ ■■ ■■ TECHNIQUES ■■ A B FIG 5 l A,B. Patient positioning for distal humerus fractures. (Courtesy of Samir Mehta, MD.) ■■ ■■ ■■ ■■ We prefer positioning in a lateral position. The patient is intubated supine and then flipped to a lateral position over a beanbag. The bony prominences of the lateral malleolus and fibular head are carefully padded. A pillow is placed between the legs. The beanbag is inflated holding the patient in lateral decubitus, and an axillary roll is placed. ■■ ■■ ■■ Approach ■■ ■■ Exposure ■■ In highly comminuted fractures, an olecranon osteotomy is recommended for full joint visualization and reduction of comminuted pieces. ■■ Morrey ■■ ■■ The contralateral arm is flexed at the shoulder and elbow to 90 degrees and placed on an arm board that is rotated so it is flush with the bed. This arm is then secured to the arm board. The operative arm is laid over a radiolucent arm board or paint roller so that the elbow is flexed 90 degrees (FIG 5). C-arm is brought in to assure that AP and lateral x-rays are adequate. The arm is then prepped and draped sterilely. A sterile tourniquet is used if one is desired. A “brain bag” is placed under the arm to be used to catch any blood or irrigant that comes from the field. The Bovie and suction are also placed in this bag for use. As described in the following text. A posterior incision is used. ■■ ■■ Slide The fascia is then divided and the ulnar nerve identified proximally in the perineural fat adjacent to the medial head of the triceps. The ulnar nerve is then dissected free of the cubital tunnel and traced back distally to its first motor branch. After identification of the ulnar nerve, the superficial fascia of the forearm is incised to the distal extent of the incision. ■■ ■■ A long posterior midline incision is used, the skin incision curves medially around the olecranon and then proceeds along the posterior border of the ulna. The incision is around 7 cm distal to the olecranon and 9 cm proximal as originally described. Then the dissection is carried deeply until the fascia is identified. The periosteum of the medial ulna is incised 6 cm below the tip of the olecranon (TECH FIG 1A). The periosteum and fascia are preserved together as a unit and reflected in a subperiosteal fashion off the bone (TECH FIG 1B). At the insertion of the triceps, Sharpey fibers connect the triceps to the olecranon (TECH FIG 1C). A modification of the Morrey technique exists in which a small wafer of bone is detached with C h a p t e r 8 Open Reduction and Internal Fixation of Pediatric T-Condylar Fractures ■■ Following release of the triceps, the remainder of the periosteum/fascial sleeve is slid laterally. This allows for visualization of the elbow joint. If access to the radial head is desired for capitellar comminution, the anconeus can be elevated off of the lateral ulna. The tip of the olecranon can also be excised if joint exposure is insufficient (TECH FIG 1E). Forearm fascia Forearm fascia Olecranon ■■ Superior ulnar collateral a. Olecranon Ulnar n. Triceps Medial epicondyle Ulnar n. Triceps Superior ulnar collateral a. B A Flexor carpi ulnaris Bone sliver Olecranon Joint capsule Joint capsule Triceps C D TECH FIG 1 l A. Superficial exposure. B. Elevation of the triceps off of the ulna. C. Medial periosteal flap being created. D. Morrey slide technique with bone wafer modification. (continued) TECHNIQUES ■■ the periosteal sleeve at this point in order to have bone-to-bone healing and not to risk disconnecting the tendon altogether (TECH FIG 1D). If the bone wafer technique is not employed, the arm should be extended to 20 to 30 degrees to relieve tension and allow safe release of the entire triceps mechanism with the periosteal sleeve. 5 6 TECHNIQUES Pa r t 4 Pediatric Anconeus m. Radial head Cut olecranon tip Olecranon fossa Triceps E TECH FIG 1 l (continued) E. The tip of the olecranon can be resected if more joint visualization is required. Additionally, the anconeus can be subperiosteally reflected if access to the radial head is necessary in the case of a coronal capitellar split. (Adapted from Bryan RS, Morrey BF. Extensive posterior exposure of the elbow: a triceps-sparing approach. Clin Orthop Relat Res 1982;[166]:188–192.) ■■ Reduction ■■ ■■ ■■ ■■ ■■ and Fixation Articular reduction must be accomplished first. In adolescent T-condylar fractures, there tend to be three large fragments, the medial condyle, the lateral condyle, and the shaft. Occasionally, coronal splits or comminution exist. These will occasionally necessitate an olecranon osteotomy approach. The condyles tend to be rotated toward each other in the axial plane toward the midline (TECH FIG 2A). A large reduction clamp can be placed on each epicondyle and used to reduce and compress the condyles. The condyles are then provisionally fixed with Kirschner wires. If comminution exists, generally the joint is provisionally reconstructed in an anterior to posterior direction.4 The shaft is then reduced to the now intact and provisionally fixed joint. The joint is generally flexed and anteriorly translated with respect to the shaft. The distal arm is translated posteriorly and the elbow flexed and extended until an anatomic reduction is obtained. A 5/64 or 7/32 Kirschner wires are then placed in a cross-pin configuration in such a way that they are out of the way of the final fixation (usually dual plates in adolescents). When the ■■ ■■ ■■ ■■ ■■ ■■ ■■ ■■ provisional fixation is in place, a medial and lateral plate are selected that are most appropriate for the patient’s bone. Of note, 2.7-mm precontoured plates are now available from various vendors that allow for the smaller sizes needed in pediatric-sized elbows. The plates are provisionally fixed on the bone in one of the distal screw holes (traditionally hole 2 from distal to proximal). A proximal screw is then placed in the slotted hole of the more proximal portion of the plate but not fully tightened (TECH FIG 2B). Fluoroscopic shots are obtained at this point to assure that the provisional reduction is adequate. A large bone clamp is then used to compress the bone between the plates (ie, placed from the medial to the lateral plate). Two distal screws (one medial and one lateral) are then placed using the locking towers. These screws should engage the opposite column of bone.4 Following this, the proximal screws are placed with the condyles in compression with a large clamp (TECH FIG 2C,D). The remaining distal locking screws are then placed. Final intraoperative image intensifier shots are then obtained after provisional fixation is removed. C h a p t e r 8 Open Reduction and Internal Fixation of Pediatric T-Condylar Fractures Rotated anteriorly toward midline A Lateral plate Medial plate Plate screw B TECH FIG 2 l A. Fragments tend to be rotated anteriorly toward the midline. B. Plates are provisionally held on with Kirschner wires and shaft screws. (continued) TECHNIQUES Kirschner wire 7 TECHNIQUES 8 Pa r t 4 Pediatric Lateral subcondylar compression C Medial subcondylar compression D TECH FIG 2 l (continued) Supracondylar compression is accomplished first laterally (C) then medially (D). (Adapted from O’Driscoll SW. Green’s Operative Hand Surgery, ed 4. New York: Churchill Livingstone, 1999:339.) C h a p t e r 8 Open Reduction and Internal Fixation of Pediatric T-Condylar Fractures ■■ ■■ ■■ ■■ The surgical field is carefully irrigated with 3 L of normal saline solution. If the bone wafer technique is used, the wafer is replaced anatomically using heavy, transosseous nonabsorbable suture. If the elevation is used, the triceps is repaired to the bone through transosseous sutures (TECH FIG 3). The ulnar nerve is not routinely transposed unless there appears to be pressure on the nerve from the plate. ■■ ■■ ■■ The fascia/periosteum layer is carefully repaired to itself using heavy Vicryl suture. A 10F Jackson-Pratt drain is routinely placed. A subcutaneous loose closure of 2-0 Vicryl is then used. Last, the skin is closed with simple nylon stitches if the closure appears to be complex or if it is simple and loose, absorbable monofilament simple stitches may be placed, although the patient should be advised that they take several months to reabsorb and fall off. Transosseous sutures Superficial fascia Medial epicondyle Anconeus m. Cut olecranon Ulnar n. Triceps TECH FIG 3 l Transosseous sutures are used to repair the triceps to the olecranon. The defect in the fascia/periosteum unit is then repaired. (Adapted from Bryan RS, Morrey BF. Extensive posterior exposure of the elbow: a triceps-sparing approach. Clin Orthop Relat Res 1982;[166]:188–192.) P EAR LS AND P I T FA L LS Visualizing the fracture ■■ The C-arm should be brought in prior to draping to assure that adequate imaging can be obtained intraoperatively. A radiolucent arm board is quite helpful in this regard. Preoperative planning ■■ A CT scan or traction x-rays can be helpful preoperatively to assess the degree of comminution or presence of coronal split fracture lines which could impede reduction at the time of surgery. Obtaining the reduction ■■ The articular block should be reconstructed first; in adolescents, there is generally less comminution than in adults, so this block can generally be reconstructed into one large fragment. After this fragment is reduced, the articular block can be reduced to the shaft segment. Preventing stiffness ■■ The goal of surgery is to provide a stable enough construct that immediate motion or, at the very least, motion within 3 weeks is possible. Often, adolescents are nonadherent to self-therapy regimens, and frequent follow-up is necessary to prevent elbow stiffness or need for arthrolysis. Consider a continuous passive motion (CPM) postoperatively. Patients should be advised that usually 10 degrees of extension loss can be expected. Closure ■■ Closure with staples or nylon stitches is advised; remove every other day at 10–14 days. These will allow for wound care with early motion. Follow-up ■■ Follow-up once a week for 4–6 weeks for motion checks. Multiple x-rays are unnecessary, but monitoring the early motion is essential. TECHNIQUES ■■ Closure 9 10 Pa r t 4 Pediatric POSTOPERATIVE CARE ■■ ■■ ■■ ■■ ■■ ■■ ■■ A well-padded posterior splint in about 70 degrees of flexion is placed, and a sling applied. The patient is kept in house for 24 to 48 hours; the drain is pulled when less than 20 mL of drainage per shift is recorded. In open fractures, antibiotics are given for 48 hours. In closed fractures, antibiotics are stopped after 24 hours. Patients are sent home in a posterior splint which is removed five times a day for active and active-assisted range of motion (30 repetitions each session). They may also shower at this point. The patient is seen back in 2 weeks for a wound check. At 6 weeks, all immobilization is removed, and the patient is started on home low load prolonged stretching exercises and formal physical therapy. No gym or sports are allowed for 3 months or until the maximum range of motion (or full range of motion) has occurred and physical therapy has cleared the patient for activity. OUTCOMES ■■ ■■ Re et al6 reported a series of T-condylar humerus fractures in children and adolescents and reported that the Bernard Morrey approach resulted in significantly better motion than the more traditional triceps-splitting approach. This group also reported that early motion resulted in better final flexion and earlier functional range of motion than when range of motion was delayed. Beck et al1 reported on 26 children and adolescents who had T-condylar fractures who were operatively treated. Approximately, one-third had elbow stiffness at final followup. Early range of motion resulted in earlier return to motion. COMPLICATIONS ■■ ■■ ■■ ■■ Stiffness is quite common in T-condylar humerus fractures; preventing stiffness can be achieved by adequate stabilization to allow early motion. Symptomatic hardware is common; in adolescents, we do not routinely remove hardware unless the patient complains of it. Infection is more common in open injuries but still quite rare. Nerve injuries are generally neurapraxias and resolve spontaneously in 3 to 6 months. REFERENCES 1. 2. 3. 4. 5. 6. Beck NA, Ganley TJ, McKay S, et al. T-condylar fractures of the distal humerus in children: does early motion affect final range of motion? J Child Orthop 2014;8:161–165. Bonczar MR, Rikli D, Ring D. Distal humerus 13-C1 Open reduction; perpendicular (biplanar) plating. AO Foundation Web site. Available at: http://bit.ly/1wEegQS. Published June 21, 2007. Accessed November 11, 2013. Bryan RS, Morrey BF. Extensive posterior exposure of the elbow. A triceps-sparing approach. Clin Orthop Relat Res 1982;(166):188–192. Green DP, Hotchkiss RN, Pederson WC; Dr. D. Sergeant Pepper Memorial Fund. Green’s Operative Hand Surgery, ed 4. New York: Churchill Livingstone, 1999. Maylahn DJ, Fahey JJ. Fractures of the elbow in children: review of three hundred consecutive cases. J Am Med Assoc 1958;166:220–228. Re PR, Waters PM, Hresko T. T-condylar fractures of the distal humerus in children and adolescents. J Pediatr Orthop 1999;19:313–318.
© Copyright 2026