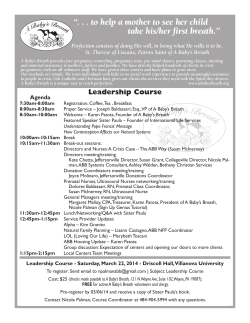
Pregnancy Guide Henderson&Walton Women's Center Congratulations
Pregnancy Guide Henderson&Walton Women's Center Congratulations We are pleased that you have chosen us to be a part of this very special time in your life. Through this booklet, we want to provide you with some helpful information about your prenatal care and your baby. Our top priority is to give our patients the highest quality obstetrical care by competent, compassionate, and caring physicians. The information in this booklet is intended for patient education purposes only. Based upon your individual needs, the attending physician may change, add, or delete any procedures listed in this booklet. We hope this pregnancy guide will aid in your understanding and enjoyment of your prenatal care. We look forward to spending the next few months with you! INDEX SECTION 1 First Trimester * Conception through week 12 SECTION 2 Second Trimester * Weeks 13 through 27 SECTION 3 Third Trimester * Weeks 28 through 40 SECTION 4 Postpartum SECTION 5 Your Baby SECTION 6 Common Questions SECTION 7 Special Test Information SECTION 8 Glossary FIRST TRIMESTER Conception through week 12 YOUR DOCTOR & WHAT WILL BE DONE By now, you have discovered that you are pregnant and have had your first visit with the doctor. During the first trimester, you will probably make two visits to the doctor. Remember, your care will depend on your needs and the needs of your baby. Therefore, don’t be surprised if your physician does not perform every procedure mentioned here or requests something that is not included. The list below highlights what probably occurred during your first visit. INITIAL VISIT WILL INCLUDE • • • • • • • • • • • • Interview with a member of our clinical staff to update medical history Weight check Complete physical by the doctor, including Pap smear Blood work Urinalysis Prescription of prenatal vitamins and iron supplements We encourage you to meet with each MD throughout your pregnancy It was recommended that you contact your hospital or certified childbirth instructor to schedule prenatal classes. You were instructed on how to schedule future appointments. You were given hospital preadmission forms. Discuss any exercise habits or exercise plans with your doctor Tests for cystic fibrosis can be done if you request it. 10-14 weeks Visit PHYSICAL EXAMINATION & TESTING • • • • • Interview with clinical staff Weight check Blood Pressure check Urinalysis Possible iron level check (if level was low on previous visit) • • • Fetal heartbeat check (It is not always heard in the beginning weeks) Assessment of the accuracy of the baby’s due date Just a reminder: be sure to take your prescribed prenatal vitamins and/or iron supplements SECOND VISIT WILL INCLUDE: • • • • The doctor will discuss your prenatal lab work including rubella, blood type, and Rhogam. If necessary, the nurse will schedule your amniocentesis and genetic counseling. See chapter 7 If you elect to have the AFP-Triple Screen test performed, it should be scheduled now for your visit at 16 weeks. (See pg. 39). The receptionist will assist you in scheduling your future visits. You will need to schedule a visit once every four weeks, unless advised differently by your doctor. YOUR BABY: 4-6 Weeks Your baby is now a small, almost tadpole-like, embryo. In the next few weeks, vital organs will begin to develop, which will include the spine, heart, digestive tract, and arm and leg buds. 6-10 Weeks Your baby will weigh approximately one third ounce and grow to about one and one fourth inches. The heart will be beating and the arms and legs will grow and begin developing fingers and toes. 8-12 Weeks By the end of this month, your baby will be about two and a half to three inches long and weigh about a half an ounce. Amniotic fluid cushions the fetus allowing the baby to move easily. Your baby is able to open and shut its mouth and turn its head, as well as make a fist and kick. More organs are beginning to develop, including the reproductive organs, however, it is difficult to distinguish the gender at this point. YOUR BODY: You will begin to see many changes in your body during your pregnancy, as well as changes in your mood. Your breasts may become very tender and full, you may need to urinate frequently, you may experience nausea, heartburn and indigestion, and you will more than likely be fatigued much of the time. These symptoms are all part of the changes your body is undergoing to manufacture your baby’s life-support system. It is important that you pay attention to your body and eat right, get plenty of rest, and don’t feel guilty about being tired! Here are some specific symptoms you may be experiencing and tips for handling them: MORNING SICKNESS: Many women experience nausea and/or vomiting during the first trimester of their pregnancy – and morning sickness doesn’t always confine itself to the morning. There really isn’t a cure for it, but here are several ways to minimize the effects: • • • Ask your doctor about B-6 to reduce nausea If you are experiencing vomiting with nausea it is important to drink plenty of fluids to replace the fluids you lose through vomiting. You might find fluids are easier to get down than solids, and they can provide vital nutrients . Try to eat several small meals or snacks throughout the day before you get hungry. This will keep your system from triggering nausea because of an empty stomach. • • • Take your time getting out of bed in the morning. Have a high carbohydrate snack in bed before you get up such as crackers, toast, or a bagel. Also, try to get plenty of sleep and relaxation – fatigue can increase your morning sickness. Save your liquids until you’re finished eating to help with nausea Try not to be around foods that make you queasy. Don’t go to a fast food restaurant if the smell of greasy food makes you feel bad. Eat right! A diet that is high in protein and complex carbohydrates will help fight nausea. Ask your physician about over-the-counter medications like Emetrol and Emechek CONSTIPATION CONCERNS: Constipation can sometimes pose a problem during pregnancy, which makes it difficult for bowel movements to occur on a regular basis; however, it can be prevented and corrected by using the following guidelines: • • • • • Drink at least eight eight-ounce glasses of water each day (24-hour period). Include liberal amounts of whole-grain breads in your diet. Also, include a daily serving of cereal that contains four or more grams of fiber per serving. Eat several servings of raw vegetables and fruits daily (including dried fruits). Establish a regular bowel habit at about the same time each day. Don’t strain or try to sit for long periods of time on the toilet. Include a regular exercise program such as walking or swimming, but always consult your physician first. NUTRITION: During pregnancy, it is important to eat a balanced diet. Nutritional support for you and your baby is best achieved by selecting foods from the food guide pyramid. Snack foods should also come from these groups, rather than from the “empty calories” found in high-fat or high-sugar foods such as candy, desserts, chips, juices and sweetened beverages. The following sample daily food plan illustrates a balanced approach to eating. You should choose from each food group for every meal so that the total number of servings per day is as indicated on the following page. IMPORTANT POINTS TO REMEMBER • • • • • Eat a variety of foods from each food group. Eat whole-grain breads and cereals. Eat raw vegetables and fruits daily. Drink at least six to eight glasses of waterdaily. Instead of coffee, tea, and carbonated beverages, drink milk, juice, and water to decrease your caffeine intake. FOOD GUIDE PYRAMID Adapted for Pregnant and Breastfeeding Women Sample Diet for Pregnant Women Option 1 Option 2 Breakfast Egg Toast, 2 slices or cereal Fruit or juice 2% Milk Breakfast Bran cereal Toast, 2 slices Fruit or juice 2% Milk Snack Low-fat crackers and cheese Lunch Lunch Low-fat meat and cheese sandwich (with Lettuce and tomato or a side salad) Fresh fruit 2% Milk Salad (with low-fat cheese, meat, and egg on a bed of vegetables with low-fat dressing) Fresh fruit Crackers Snack Cottage cheese with fruit Dinner Dinner Lean meat, fish, or poultry Starchy vegetable (fat-free) Green vegetable (fat-free) Bread Fresh or canned fruit 2% Milk Homemade soup or stew Bread or crackers Fresh fruit 2% Milk Snack 2% Milk with cereal or graham Remember: • • • • Check fat on packaged snacks Use correct serving sizes Drink at least 2-3 quarts per day for adequate hydration (and milk production for the breastfeeding woman). Emphasize water. Limit added fat to 1 serving per meal. (Check the Nutrition Facts label to determine the serving size.) • DO NOT omit fat in your diet. Your body cannot produce essential fatty acids. You must eat at least 1 serving of fat at each meal to provide these nutrients GAINING WEIGHT DURING PREGNANCY: You should expect to gain between 22 and 30 pounds while you’re pregnant. It should be gained gradually, about two to four pounds during the first 12 weeks and about two to three pounds per month thereafter with the majority gained during the last six months. Even if you are overweight, the extra weight you will gain is necessary to nourish the baby. This is not a time to lose weight. The baby will account for about one-fourth of your total weight gain. For example, if you gain 25 pounds, this is how the weight will be distributed. Baby…………. 7 ½ lbs Placenta…………. 1 ½ lbs Uterus (womb)….. 2 lbs Amniotic fluid…….. 2 lbs Breasts…………… 1 lb Blood volume……… 3 lbs Tissue and fluid…. 3 lbs Maternal reserves….. 5 lbs Total………………25 lbs WORKING MOTHERS-TO-BE: If you decide to work throughout your pregnancy, be sure to take breaks often. Try not to stand or sit for long periods of time. And when you get home, lie down for an hour or so before you begin cooking or cleaning. Try to share chores with your partner, and above all, get plenty of rest. TRAVELING: When traveling by vehicle, be sure to make frequent stops so you can stretch and walk around. There may be some airlines that will not allow you to fly after your seventh or eighth month without a letter or permission from your doctor. Consult with your doctor before traveling more than one hour away from the hospital after 34 weeks. BUCKLE UP. IT’S THE LAW! You are not only looking after your own safety, but also after the safety of your unborn child. Wear both the lap belt and shoulder harness no matter how uncomfortable they can be, and secure the lap belt below your abdomen. Wearing your seatbelt is not only required by the law, it greatly reduces the chances of injury to you and your baby if you are in an accident. Be sure to call your doctor if you are involved in a motor vehicle accident, no matter how minor. WARNING SIGNS (Call us if any of the following signs occur!) • • • • • • • • Any type of vaginal bleeding. A headache that does not go away and is accompanied by stomach pain or blurred vision. Abdominal pain that lasts more than 4 hours. Continuing intermittent abdominal tightening (contractions or cramping). Leaking or gushing fluid from the vagina. Sudden puffiness or swelling of the hands, feet, or face. Pain or burning sensation when urinating. Fever over 100 ºF (38 ºC). PREGNANCY HAZARDS • DON’T SMOKE! Women who smoke during pregnancy often have premature and low-birthweight babies and have twice the risk of placental abruption (miscarriage). Children who live in smoke-filled households have four times the number of colds as children in non-smoking households. There is also an increased risk of sudden infant death syndrome (SIDS) in smoking households. • HAVE YOUR PARTNER CHANGE THE CAT LITTER: Toxoplasmosis is an infection humans can acquire from cat feces. There are no visible symptoms, but it can cause eye and brain defects in the unborn baby. Have your partner change the litter. But, petting and holding your pet is acceptable. Also, remember to wear gloves while gardening because of possible soil contamination from cat feces. • DON’T DO DRUGS! Even in small amounts, street drugs are very dangerous. Marijuana use can result in complications during labor and cause low birth weight. Cocaine or crack can cause miscarriages, premature births, placental abruption, and brain damage to the baby. The baby can be born addicted to these drugs and have to go through a withdrawal process that could be fatal. • MOTHERS CAN PASS AIDS TO THEIR BABIES! Women most frequently acquire AIDS from an infected partner or by sharing needles during intravenous drug use. About half of the babies whose mothers have the AIDS virus will become infected. If treated during pregnancy, the risk of infecting the baby can be reduced significantly. SECOND TRIMESTER Weeks 13 through 27 14-16 WEEKS Visit PHYSICAL EXAMINATION AND TESTING • • • • • • • • Interview with clinical staff Weight and blood pressure check Urinalysis Fetal heartbeat Possible iron level check Possible alpha-fetoprotein (AFP) performed (Chapter 7). Amniocentesis and genetic counseling, if previously scheduled Keep in mind that a physician’s exam or ultrasound may result in a change of this date. Your baby’s birth will be considered “on time” if it arrives within two weeks before this date or two weeks after. The management of labor outside this time frame will be made on an individual basis. THIRD VISIT WILL INCLUDE The doctor will advise you to schedule an ultrasound between the 18 th and 22 nd week. This is a good time to speak with your doctor about symptoms you’ve been experiencing, especially unusual ones. 17-22 WEEKS Visit PHYSICAL EXAMINATION & TESTING • • • • • • Interview with clinical staff Weight and blood pressure check Urinalysis Fetal heartbeat Ultrasound Possible iron level check FOURTH VISIT WILL INCLUDE: • • • • The doctor will finalize your approximate due date and discuss ultrasound results, if applicable. The ultrasound is not a more accurate due date unless it varies by more than ten days from your LMP (last menstrual period) due date. The doctor will discuss your alpha-fetoprotein (AFP) results, if applicable. The doctor will discuss your amniocentesis results, if applicable. Most hospital preadmission forms should be completed and mailed by this visit. 23-27 WEEKS VISIT PHYSICAL EXAMINATION & TESTING • • • • • Interview with clinical staff Weight and blood pressure check Urinalysis Fetal heartbeat Possible iron level check FIFTH VISIT WILL INCLUDE: • • The doctor will ask you to schedule a glucose screening. If you have RH negative blood, you will have an antibody screen and you will get a Rhogam injection in the 28 th week of pregnancy. YOUR BABY: 16-20 WEEKS The baby now weighs between four and six ounces and is four to five inches long with the head making up about one-third of its length. Your baby will grow very rapidly during this month, and the gender can probably be determined by this point. The eyelashes and fingernails have begun to grow, but the toenails have not. And, even though the vocal cords have formed, the baby is unable to cry yet. The baby’s nourishment is provided by the placenta. The baby has begun swallowing amniotic fluid and is now urinating and forming meconium, the stool, in its intestines. The tongue is also working, so the baby can begin gentle sucking. 20-24 WEEKS Your baby now weighs between eight ounces and a pound and is eight to 12 inches long – still small enough to hold in the palm of your hand. The head, trunk, and limbs are now properly proportioned in size. Toenails, eyebrows, and hair are beginning to grow, and teeth are forming under the gums. There is fine, soft hair now covering the body called lanugo, and a creamy, white covering over the skin called vernix. During this month, you will begin feeling the baby move, but you could mistake it for gas bubbles. Your baby is able to kick and turn over by now, and your everyday activity gently rocks the baby in the amniotic sac. 24-28 WEEKS By now your baby weighs about one and one half pounds and is between 12 and 14 inches long. There is a little body fat, and the skin is still thin, but the baby could survive with intensive care if born near the end of this month. The eyelids are beginning to part, and your baby can open its eyes. Because it is swallowing some amniotic fluid, you could feel rhythmic jerks or jolts when it hiccups. Your baby’s unique fingers and toes are now visible. You may begin to recognize your baby’s pattern of activity and rest during the sixth month. It is different for every baby, but most will kick or turn at least 10 times in a 12hour period. YOUR BODY: As you and your baby continue to grow, your uterus will expand and your abdomen will stretch. You may start to notice reddish streaks on your abdomen, breasts, buttocks and thighs, which will fade to fine silvery lines after birth. Oils, creams, and lotions may relieve the itchy, dry feelings as your skin stretches, but they will not make these lines disappear. Also, because of increased hormones, a dark line may form from your pubic bone to your navel called the linea nigra. This is more likely to occur in women with dark hair and skin. It will become lighter after birth. Some women experience another result of increased hormones, which are brown patches appearing on the nose, forehead, neck and cheeks. This is a natural change during pregnancy. They will begin to lighten and may disappear after birth. You may begin experiencing a yellowish fluid leaking from your nipples. This is colostrum or “the first breast milk.” It is high in protein and low in fat, which is exactly what the baby will need. It will continue to ooze throughout your pregnancy, but do not squeeze it from your nipples. Because you will have an increased amount of blood in your body, you might notice that you have unusually red palms or tiny red spots on your face, neck, upper chest or arms. These are tiny groups of blood vessels on the surface of the skin. ROUND LIGAMENT PAIN: As early as 18-20 weeks, you might experience some pain in your lower abdomen or groin. This is because of stretching of the round ligaments, which are tissues attached to the uterus that hold it in place. They stretch as the uterus expands. After long periods of sitting, you may experience discomfort upon standing. Some relief measures you can take are: • • • • • • Stand up slowly to allow the ligaments to stretch gradually. Soak in a warm bath. Lie on the painful side with your hips turned and place a pillow between your knees. Do the pelvic tilt exercise (see pg.16). Tylenol may be taken to relive pain Heating pad on a low setting BRAXTON HICKS CONTRACTIONS: Throughout your pregnancy, you may experience uterine contractions or “false labor.” They do not mean the baby is coming. The contractions simply help circulate blood throughout the uterus and prepare the uterine muscles for labor. While the pain is mild, it can still be very annoying. The pain might ease if you increase or decrease your activity. Also, a warm bath, Tylenol, rest, and drinking plenty of fluids often makes them stop, but, if you have six or more in an hour that do not go away, call your doctor. RESTING OR SLEEPING: You may find the best position for rest is on your left side. This allows for the best flow of blood to you and your baby. When you lie on your back, the uterus presses on the large abdominal vein and this can lower your blood pressure and cause you to become light-headed. WAYS TO REDUCE SWELLING (EDEMA): Swelling is common in pregnancy, especially in the hands and feet. Usually a good night’s rest, while lying on your left side, will help reduce the swelling. Other recommendations to avoid swelling: • • • • • • • Restrict the amount of salty food in your diet, but do not eliminate your salt intake entirely. You need some salt to keep a normal fluid balance. Whenever possible, elevate your feet for periods of 20 to 30 minutes, several times a day. Avoid standing for long periods of time. Try sleeping with your feet slightly higher than your heart. Raise the foot of your bed on two to three inch blocks. Wear support stockings. Remove your rings before they get too tight. Lie on your left side when you sleep or rest. This allows for maximum flow of blood and nutrients to the fetus and more efficient kidney function for you, providing a better means for the elimination of fluids, thus reducing swelling. • Walking helps the muscles in your legs move the fluid out of your legs. NAGGING BACKACHES: To help ease nagging backaches: • • • • • • • • Squat, rather than bend, to lift objects. Wear low-heeled, support shoes. Try sitting cross-legged. Always roll to your side before sitting up from a lying position. Apply either heat or cold to your back. Ask your partner or a friend to give you a back rub. Place a board under your mattress to create a firmer sleeping surface that will support your back. Wear an obstetric girdle, also called a maternity belt. You can find them in department stores and maternity shops. DIET AND EXERCISE AID IN DIGESTION: During pregnancy, both the baby and the uterus press on your intestines slowing the movement of food and causing gas. Hormones during pregnancy cause the digestive tract to relax and work more slowly causing constipation. Here are some tips to help you ease this uncomfortable situation: • • • • • • Set up regular times for both bowel movements and exercise. Chew your food slowly to avoid swallowing air, and thus prevent gas from forming in the intestines. Avoid gas-forming foods such as cabbage, beans, and fried foods. Drink more water and juice. Drink decaffeinated tea or hot lemon water first thing in the morning to ease constipation. Avoid the use of straws. They cause constipation and gas to form in the intestines . HEARTBURN RELIEF: Many women get heartburn throughout their pregnancy. Here are a few tips on how to avoid it: • • • • • • • • • • Avoid eating too much at one time. Try six small meals instead of three large meals. Avoid fried and spicy foods. Do not drink as much liquid as you normally do during a meal. Avoid bending over and lying down with a full stomach. Take walks. Chew sugarless gum after eating. Avoid eating just before bed time. Prop yourself up with pillows when sleeping. Take an antacid (do not use baking soda, it contains too much sodium). See Section 6 Eat plenty of whole grains, fresh and dried fruits, and raw vegetables. EXERCISE GUIDELINES FOR MOMS-TO-BE: Before you begin exercising, check with your doctor to make sure the activities you’ve chosen are safe. Exercising for 20-30 minutes three times a week is usually recommended, although more frequent exercise is preferred. Follow these simple guidelines: • • • • • • • • Avoid any jerking or bouncing movements, instead, use smooth flowing movements. Low impact aerobics are acceptable (walking, treadmill, etc.). Ask your doctor about continuing any aerobic workouts. Don’t strain. Stop and rest when necessary and resume the activity when rested. Do not lie flat on your back after the fourth month. Avoid exercising in hot, humid weather. Try to stay cool. Exercise on a firm surface. Do not hold your breath. Breathe completely and avoid becoming winded. Always drink water before, during, and after exercising. Listen to the signals your body gives you. Stop if you get dizzy, feel pain or cramps, lose muscle control, or can’t catch your breath. • • • • • Do not participate in any activity or exercise that would cause you to lose your balance (i.e. switch from your road bike to a stationary bicycle, do your step class without the step, etc.). Wear clothing that is comfortable and allows you to move freely. After your baby arrives, resume your regularly pre-pregnancy routine gradually. Listen to your body, it’s just been through a lot! Pregnancy requires an additional 300 calories. If you exercise regularly, you will need even more calories to keep your body going. When exercising, be sure not to lock your knees while standing. Keep knees slightly bent, and do not stand motionless for long periods of time. If you keep moving and keep your joints slightly bent, you will keep the blood flowing and help prevent dizzy spells. COMMON EXERCISES DURING PREGNANCY: LIGHT AEROBIC EXERCISE/LOW IMPACT: Aerobic exercise stimulates your heart and lungs, improves your blood flow, and expedites the use of oxygen. We recommend walking, swimming, and riding a stationary bike to help you increase your strength. To resist fatigue, always keep a comfortable pace. CONDITIONING EXERCISES: Conditioning exercises tone your abdominal wall and pelvic muscles preparing you for childbirth. Performing these exercises will make your recovery quicker. These are described below: • KEGEL EXERCISE: Tighten your pelvic floor muscles, as you do to stop urinating, and hold for three seconds. Repeat groups of 10 to 12 several times a day. • STRETCHING EXERCISES: Stretching exercises not only make you more flexible, they also help relieve some of the aches and pains of pregnancy. • TAILOR SITTING: While sitting on the floor, bend your knees and hold the soles of your feet together in front of you. Slowly lean forward until you feel the stretch in your inner thighs. When you feel the stretch, hold and gently push, do not force, your knees towards the floor, you will feel stretching in your inner thigh and pelvic floor. Hold this position for 30 to 60 seconds. • HAMSTRING STRETCH: Securely support yourself by holding onto the back of a chair with both hands. While standing with your knees slightly bent, extend your right leg, heel down, toes up. Keeping your heel firmly planted in front of you, slowly begin bending your left leg. Bend at the waist and push your hips back without arching your back! You should feel the stretch in your hamstring, located on the back of your right thigh. Hold this position for 30 to 60 seconds, then repeat on the left side. • PELVIC TILT: Get on your hands and knees keeping your back flat and straight, not arched, and your knees comfortably apart. Tighten your pelvic and abdominal muscles to arch your lower back. Hold for a count of five, relax, and return to starting position. Repeat 10 to 12 times. Do not sag your stomach. This exercise is excellent for lower back pain. • CALF STRETCH: Stand facing a wall. With your hands on the wall, place one foot about 12 inches in front of the other. While slowly leaning forward, bend your front knee, keeping both heels on the floor, and hold your back leg straight. Make sure your knee is directly aligned over your heel. You will feel stretching in your back leg. Try to hold this position for 30 to 60 seconds. Switch legs and repeat. Many women experience muscle spasms in their calves, especially at night. Performing this exercise before going to bed can help relieve these cramps. • CALF HAMSTRING STRETCH: While sitting with your legs spread apart in front of you, reach slowly toward your left foot until you feel a stretch in the back of your thigh, and hold for 30 to 60 seconds. Then do the same toward the right foot. THIRD TRIMSTER WEEKS 28 through 40 26-30 WEEKS VISIT PHYSICAL EXAMINATION & TESTING • • • • • • • • Interview with clinical staff Weight check Blood pressure check Urinalysis Fetal heartbeat Glucose screening Possible iron level check If necessary, a Rhogam injection will be given between 28 and 32 weeks, following your antibody screening SIXTH VISIT WILL INCLUDE • Your doctor will talk to you about selecting a pediatrician. CONTINUING VISITS (30 weeks – Delivery) PHYSICAL EXAMINATION & TESTING Your doctor may want to schedule more frequent examinations at this point. You will need to schedule your next appointment based on your doctor’s orders. • • • • Interview with clinical staff Weight check Blood pressure check Urinalysis • • • Fetal heartbeat Possible iron level check Regular pelvic exams will probably begin at 38 weeks. (Depending on your situation, you may be having them already.) QUESTIONS & ANSWERS • • • • • • • You should attend a breast-feeding class. (If you are undecided about whether or not to breast-feed, this class can help you with your decision.) The doctor will discuss anesthesia, labor, and delivery expectations with you, if this has not yet been done. The nurse will give you an information sheet on symptoms of labor which was also provided in folder given at initial visit. You will be reminded that you will need to see the doctor four to six weeks following your delivery. Please remember to schedule this appointment as soon as possible after you deliver. You should select a pediatrician that best suits your needs. Disability forms regarding your maternity leave should be brought to the office and left with the delivery physician’s office personnel. Please allow 5-7 days for completion and return. If your company requires earlier completion, please turn them in on an earlier visit. We encourage you to work until delivery as disability is usually given for obstetric or medical complications only! Your hospital stay will vary according to the type of delivery that you have - vaginal or Caesarean section. For a vaginal delivery, you should plan on at least a 24-hour stay; the average is a 48-hour stay. (You should also check with your insurance company to determine whether you have an approved maximum length of stay). YOUR BABY: 28-32 Weeks During your last trimester, your baby will grow significantly. In fact, it will more than double its weight. At this point, however, your soon-to-be newborn only weighs two to three pounds and is 14-17 inches long. Lanugo, fine downy hair, begins to disappear, first from the face, although vernix, a thick white creamy substance, still covers the body and protects the skin. Your baby’s vision has developed and his/her ears are now capable of picking up sound. If you shine a light directly on your abdomen, your baby will react to it. Your baby can also hear your heartbeat, as well as food moving through your body and blood flowing through your uterus. You may also be surprised that your baby knows your voice and enjoys certain kinds of music, but be aware that loud music or sudden movements will cause your baby to jerk. This movement is known as the startle reflex. You will become very familiar with it once your baby is born. In fact, by this point in your pregnancy, your baby’s movement probably has become more intense. This is because he/she has grown larger and may squirm and kick instead of roll. If your baby seems inactive for any extended period of time, lie down and relax for a few minutes, then count the number of movements the baby makes during an hour. More than 10 movements per hour is fine. Repeat this during the day, and, if the number of times the baby moves seems low, contact your doctor. 32-36 Weeks By this month, your baby weighs approximately five pounds and is from 16 to 18 inches long. This is a time of tremendous growth, especially of the brain. Most of the baby’s systems are well developed by this point, except the lungs, which could still be underdeveloped. Calcium, protein and iron are very important in these last few weeks for your baby’s growth. Your baby is developing new skills that will allow it to eat, and taste buds are now present on his/her tongue. 36-40 Weeks Your baby is now plump with pink, smooth skin and can weigh from six to nine pounds. Since your baby is much larger and is possibly engaged in the pelvis, it may seem less active. The bones in the head are firm, but still soft enough to allow the head to pass through the birth canal without injury. YOUR BODY Your prenatal visits will now be weekly, or as specified by the physician. These visits will include a pelvic exam (38 weeks) in addition to the usual weight check and lab work. It is possible to experience painless spotting immediately after or within 48 hours of the pelvic exam. You may also notice an increase in a mucous-like discharge after the pelvic exam. You may experience low backaches, abdominal pressure, and leg pains. Vaginal discharge will likely increase. These symptoms are normal, indicating that the baby has assumed the birth position. LIGHTENING (36-40 Weeks) If you are a first-time mother, you may notice your baby’s head moving down into the pelvis two to four weeks before birth. This is known as lightening. If you have had other children, this lightening may not occur until labor begins. When lightening takes place, the shape of your abdomen may change. This will make it easier for you to breathe because your lungs will now have more room to expand and your stomach will be less confined. You may also find indigestion and constipation are no longer problems. After lightening occurs, your baby’s head now presses on your bladder causing frequent urination. Your baby’s new position may cause more leg cramps, thigh pains, and aches in your pelvis. At the same time, your cervix will become softer and thinner, which will help prepare your uterus for delivery. The term for this softening and thinning of the cervix is “effacement.” THE ONSET OF LABOR When labor begins, some or all of the following symptoms will occur: • Regular contractions: For first-time pregnancies, the contractions should be eight to 10 minutes apart for one to two hours. For succeeding pregnancies, they should be 10 minutes apart for one hour. Use a watch with a second hand to time from the beginning of one contraction to the beginning of the next one. • • • Rupture of membranes (water breaking): There will be a sudden gush or trickle of clear, watery liquid from the vagina that may or may not be accompanied by contractions. If this occurs, notify your physician immediately. Spotting: Spotting may occur and/or blood-streaked mucous may be present. Should you experience heavy bright-red vaginal bleeding, notify your physician immediately. You may experience a loss of your mucus plug. The onset of labor may follow in days or weeks following the loss of the mucus plug. This is your body’s way of preparing for labor. If you go into labor during office hours: Monday – Friday, 8:00 a.m. – 5:00 p.m. and Saturday 8:00am – 12:00pm , notify your physician through his/her clinical staff by calling the office. You may be instructed to come into the office for an examination, or you may be told to go directly to Labor & Delivery depending on your condition. If you go into labor during non-office hours: Call the office at (205) 930-1800 . If you are in labor, you will be instructed to go to Labor & Delivery. After you are settled in a room in Labor & Delivery, a family member should go to the Admissions desk of the hospital and present your patient insurance information. LABOR INDUCTION: WHEN IS IT DONE? Inducing labor may be done for you if it is appropriate. Inductions are either medically indicated or elective. Those that are medically indicated are those that your physician believes will be safer from a complication for you and/or your baby by delivering you early. Examples of medical indications for induction would be growth problems with the baby, maternal blood pressure problems, or post-dates (42 weeks gestational age). Elective inductions are those that are not medically indicated. These inductions may by appropriate for some, but not for all patients. Your physician can help you determine if you are a candidate for induction. Part of the process is to determine if your cervix is favorable or “ripe”, otherwise the induction could be a long process that may not be successful and even result in a C-Section for you. Generally, labor that you do on your own may be better that an induction . CHECKLIST FOR HOSPITAL STAY: EN ROUTE: • • • Cash for parking, if necessary Watch or clock with second hand for timing contractions Paper and pen for recording contractions FOR LABOR (DELIVERY AND RECOVERY ROOM (LDR) • • • • • • • • • • • • Lotion for massages A baby name book (if needed) Sugarless candy to keep your mouth moist Books, magazines, playing cards Warm socks and slippers Address book or list of family and friends to be called Robe and two or three nightgowns Perfume, deodorant, powder, cosmetics, toothbrush, toothpaste Hair brush, hair dryer, curling iron Soap, shampoo, conditioner Glasses or contact lenses (with necessary paraphernalia) Cameras, film, tapes, and fresh batteries GOING HOME ITEMS FOR BABY: • • • • • • Infant car seat (mandatory state regulation) One undershirt, socks or booties Going home outfit One receiving blanket Sweater and cap, in cool weather Heavy blanket, in cold weather GOING HOME ITEMS FOR MOM: • • • • • • Bra (nursing bra, if breast-feeding) A roomy outfit Panties and slip Shoes, hosiery, or socks Coat or sweater (if necessary) Shopping bag to bring home gifts POSTPARTUM YOUR DOCTOR • • • • • • You should have a postpartum check-up four weeks after a Cesarean section or six weeks after vaginal delivery. If you are not immune or rubella (German measles), you will receive a rubella vaccine during your postpartum check-up if it was not given while you were in the hospital. You should continue your postpartum exercises. You should discuss birth control options with your physician at your postpartum visit. Questions regarding breast-feeding can be directed to the hospital’s Lactation Consultant. Your annual Pap smear will be performed at your postpartum visit. YOUR BODY POSTPARTUM Once you deliver the placenta or “afterbirth,” your body begins to recover. It usually takes six to eight weeks for muscles and skin to regain their normal tone. Because of hormonal changes, you should expect mood swings. After delivery, the uterus, which is located at/or below the level of the navel, is approximately the size of a grapefruit and feels firm. The uterus shrinks onehalf inch each day. Massaging the uterus and breast-feeding will help continue this process. By the 10 th day after delivery, the uterus will have returned to normal position in the pelvis. It is common to experience swelling in the lower leg and feet soon after delivery. Elevate your legs above the hips, decreased activity, and increase your water intake. If you experience headaches, shortness of breath, dizziness, and/or nausea with swelling, contact our office. EPISIOTOMY Stitches from the episiotomy will dissolve in about two weeks. The episiotomy site may itch as it heals. Discomfort from this procedure usually goes away in two or three weeks. Follow these tips to promote healing and prevent infection of the episiotomy site: • • • Keep the episiotomy site clean and dry. After urinating, wipe front to back and use a squirt bottle of warm water to rinse the episiotomy site. Pat area dry. Take a shower instead of bath during the first few weeks. In some cases, your doctor may recommend taking a sitz bath. To relieve episiotomy soreness: • • • • Apply ice packs to soothe and reduce swelling. Take a sitz bath by sitting in three to four inches of very warm water for 20 minutes, two or three times a day as needed for 10-14 days postpartum. Apply anesthetic spray or Tucks pads (cotton pads soaked in Witch Hazel). Lie on your side with your knees up to relieve pressure and pain. The Kegel exercise will help the vagina recover, (see page 15). Unlike some types of exercises, you can begin doing the Kegel exercise immediately after you deliver. This exercise contracts the vaginal muscles, helping to strengthen the vagina, which takes about six weeks to regain its muscle tone and shape. If you do 20 sets of 10 repetitions a day, your vagina should return to its normal tone much quicker. BODY SECRETIONS A day or so after birth, your body will begin to rid itself of extra fluid by increased urination. You also may perspire heavily, especially at night. The vaginal discharge you will notice for several weeks after birth is known as “lochia.” It is blood and tissue left over from delivery. The amount and appearance will vary from day to day. For the first few days, lochia is heavy and bright red. Your flow may be heavier when you change positions or nurse your baby. Gradually, the amount of lochia will lessen. The color will change from bright red to dark red in color, and then brown to yellow to white to clear. During this time, do not use tampons, and continue to avoid douches and vaginal sprays. You can, however, use mini pads. A sudden increase in the amount of lochia, or a return to a bright red color, signals the need for more rest. Occasionally, heavy bleeding may occur for one to two hours two weeks after delivery. This is usually due to the shedding of placenta scarring. SHOULD YOU EXPERIENCE ANY OF THE FOLLOWING SIGNS, CALL YOUR PHYSICIAN: • • • • • • • • Heavy bleeding requiring more than one full-sized sanitary pad per hour Unusual pain or pain that does not go away Fever greater than 100º Pain or burning when you urinate Cracked or bleeding nipples Reddened, tender areas in the breasts Tender red streaks in your legs Depression for more than two weeks AFTERBIRTH PAINS Contractions of your uterus that are similar to menstrual cramps are called “after pains.” They can be painful, especially if you have had more than one child. After pains often occur during breast-feeding and should disappear after the first week. To relieve after pains, use prescribed pain medication as needed. HEMORRHOIDS AND CONSTIPATION You will probably have difficult bowel movements for a few more weeks. To help ease them, drink plenty of liquids. Be sure to exercise your abdominal muscles by walking regularly. Continue eating fresh fruits and raw vegetables, and increase your intake of bran and whole grains. An over-the-counter stool softener like Metamucil, Senokot, or Colace may be used. SEXUAL ACTIVITY Normal sexual relations may be resumed four to six weeks after your baby is born. You may experience some discomfort during intercourse, and you should inform your partner immediately if you do. If you are breast-feeding, you may experience some vaginal dryness. Use of a water-soluble lubricant is recommended. It is not surprising that some women do not feel very “sexy” after delivery, especially considering the lack of sleep and other demands of motherhood. It is best to communicate these feelings with your partner and work together to achieve your optimum sexual relationship. PREGNANCY IS POSSIBLE If you are bottle-feeding, you may begin to menstruate again six to eight weeks after birth; however, your period may not start for several months if you are breast-feeding. Ovulation often occurs before your periods resume, therefore, the use of contraception is recommended. Whether bottle or breast-feeding, remember that pregnancy can occur even in the absence of a period. POSTPARTUM BLUES/DEPRESSION Approximately half of all new mothers experience postpartum blues, commonly known as the “baby blues.” Unhappiness, anxiety, mood swings, and weepiness are just some of the common symptoms that occur during the first six weeks after delivery and periodically reoccur. The major cause of postpartum blues is the wide fluctuation in hormone levels. Other contributing factors include the physical and psychological adjustments that must be made, especially by a new mother. Such stress factors may include fatigue, guilt, change in status, lower self-esteem, and negative body image, as well as the pressures of caring for other children, housekeeping, and job concerns. Try not to place too many expectations on yourself or your baby. Be determined to do something nice for yourself. You should eat correctly, exercise, and nap\sleep when you can. Most of all, do not be afraid to ask for help from those around you. Depression that continues for two weeks or more that leads to a feeling of despondency, and an inability to cope with the demands of daily life, is known as postpartum depression. The majority of new mothers experience some feelings of depression, but postpartum depression lasts longer and is more serious; however, it occurs in only 10 percent of new mothers. Should you experience a severe continual feeling of depression, we recommend that you contact your physician. Remember, adjusting to parenthood is as demanding as it is rewarding. Check the list of references below for further reading material on how to cope. REFERENCES The following is a list of excellent references to utilize during and after pregnancy. 1. What to Expect While You are Expecting, Eisenberg, Murkoff, and Hathaway. Workman Publishing: New York , New York , 1989. 2. What to Expect the First Year, Eisenberg, Murkoff, and Hathaway. Workman Publishing: New York , New York , 1989. 3. www.aap.org/family/brstguid.htm 4. AAP – A Woman’s Guide to Breastfeeding YOUR BABY IT IS IMPORTANT TO NOTE THAT THE BEST SOURCE OF INFORMATION REGARDING THE HEALTH OF YOUR BABY AND ITS’ HABITS IS FROM YOUR PEDIATRICIAN. EATING PATTERNS For the first few months, it is better to feed your baby on demand. Over several months, a feeding schedule will develop. Make every effort for this time to be enjoyable for both of you. RULE OF THUMB FOR BREAST-FEEDING: Every one and a half to three hours for 20-30 minutes. RULE OF THUMB FOR BOTTLE-FEEDING: In the first few days, expect the baby to drink between one and three ounces per feeding. The amount of time between feedings is equivalent to the number of ounces he/she drinks (i.e. one ounce equals one hour). Regardless of whether you breast or bottle-feed, do not be anxious about counting ounces or minutes, but never go longer than four hours between feedings. All is normal if your baby wets five or six diapers per day and has regular bowel movements. Be aware that babies go through growth spurts at three and six weeks and three and six months. They may want to feed more frequently. CALL YOUR PEDIATRICIAN IF YOUR BABY HAS ANY OF THESE CONDITIONS: • • • Skin around the cord or circumcision is red, warm, and/or has a foulsmelling discharge. Axillary (under arm) temperature measures less than 96º or greater than 99º, or rectal temperature is less than 98º or greater than 101º. Baby struggles to breathe, grunts, has nostrils flaring with inspiration, or takes more than 50 breaths per minute. • • • • • • • • • Baby shows no interest in feeding or sucking for more than a six-hour period. Baby has no wet diapers for more than a six-hour period after the third day. Skin is bluish around the mouth or over the whole body. (Blue hands and feet mean baby is chilled). Baby is shaking and very irritable. Baby vomits forcefully, more than once, not the usual spitting up or dribbling with burps. Soft spot bulges. There is a constant yellow discharge from the eyes. Whites of eyes or whole body turns yellow. Your instincts and observations tell you something is wrong. HOW TO BUY A SAFE CAR SEAT Today, it is required by law that all babies ride in a car seat until the age of five. There are several types of car seats, and they fall into two basic categories. You can use an “infant-only” car seat until the baby weighs 20 pounds. At that time, you must begin using a toddler-sized seat. All infant car seats face the rear of the car and are light enough to double as a carrier outside the car. Be sure to support the infant’s head and shoulders with a rolled blanket or similar padding. Once you change to the toddler seat, install it facing forward. If you have two cars, consider buying two seats, since the baby must be in a car seat at all times. Household infant seats, carriers, and travel beds are unsafe in the car, and it is even more dangerous to allow the baby to ride in someone’s arms. There is now a seat that can be used as both an infant and a toddler car seat called the “convertible car seat.” It usually stays buckled in the car. It is heavier and costs more, but is more cost-effective in the long run since you’re not buying two. There are many places you can buy car seats, such as children’s stores, drug stores, and discount outlets. Or you could ask your hospital about renting or buying one. We suggest you buy a car seat before your baby arrives so you can learn how it works and how to install it in your car. When choosing a seat, ask yourself these questions: Is it easy to use? Will it fit easily into my car? Is it easy to fasten and unfasten? How difficult will it be to remove? How difficult will it be to put my child in the seat? All car seats are held in place by a seatbelt. Some also have a tether, which is a strap on the back of the seat that gives extra security. This tether must be permanently bolted to the body of the car. If it doesn’t have a tether, you can move it between the front or back seats, although the back seat is safer. If your car has a passenger side air bag, you must place the car seat in the back seat.* *It is a state law that your baby be discharged from the hospital in an approved car seat. COMMON QUESTIONS The following are some common questions asked during pregnancy. These answers have been decided upon collectively by our physicians, although answers may vary slightly, depending on the physician and the situation. Is it normal to have bloody spotting? No, but it is occasionally seen (i.e., following sexual intercourse, strenuous exercise, or a Pap smear). This does not necessarily mean you will have a miscarriage. Is it normal to have a nosebleed during pregnancy? Nosebleeds are normal and are usually caused by the increase in blood volume and the thinning of the vessels in the lining of the sinuses during pregnancy. If nosebleeds increase in frequency, please contact your physician. Are backaches sometimes related to pregnancy? Yes, a great deal of stress is placed on the lower back because the abdominal muscles are relaxing, the center of gravity is changing, and the round ligaments, which are attached to the uterus, are stretching as the uterus enlarges. What is the sharp, pulling pain I occasionally feel in my side? It is round-ligament pain, which is caused by the stretching of these ligaments due to weight gain and uterine growth. May I travel long distances? Yes, but only until you reach 34 weeks of pregnancy. After 34 weeks, you should go no further than one hour away from the hospital without your doctor’s permission. You should stop every one to two hours and walk for about 10 minutes to increase circulation and prevent leg and feet swelling. May I ride in a boat? Riding in a boat is acceptable, as long as the ride is smooth and does not cause a jarring motion. May I water ski? No, because of the possibility of abdominal injury. May I participate on the rides at the amusement parks? Yes, as long as the signs do not mention restrictions. Do not go on the rides that swing or jerk. May I go swimming? Yes, provided you have not experienced a rupture of your membranes (water breaking). May I go to the dentist while I’m pregnant? Yes, we encourage you to do so. Your dentist should use only local anesthesia and must cover the abdominal area during all X-rays. No nitrous oxide may be used. May I go horseback riding? No, because of the jarring motion and the possibility of being thrown from the horse. May I get a hair permanent? Yes, after the first trimester (13 weeks). Remember, because of the changes in your body related to pregnancy, the permanent may not take. May I have my hair dyed? Yes, after the first trimester (13 weeks). What may I take for gas or indigestion? Over-the-counter antacids – NO ROLAIDS. May I use vapor rub or nose spray? The use of vapor rub externally and saline nose spray is permissible. If dryness and nosebleeds are a problem, you may want to consider a cool-mist humidifier for your bedroom. May I use a salt substitute? No, because it contains potassium salts that could cause problems. Are diet drinks okay? Yes, after the first trimester (13 weeks), but try not to drink more than one a day. If given a choice, use products with Aspartame or Sucralose. May I drink coffee, tea, or drinks with caffeine? In moderation. (No more than the equivalent of two cups of coffee per 24-hour period.) Water is most important. May I paint, use bug spray, or clean my oven? Yes, in a well-vented room. Do not allow them to touch your skin. If you start feeling faint, nauseated, or get a headache, leave the area immediately. May I travel by plane? Yes, with authorization of your attending physician. Some airlines require a written letter from the physician authorizing travel by air. Remember, if you go out of town, take a copy of your prenatal records with you. Must I stop smoking during pregnancy? Yes, It is harmful to both you and your baby. (Please see the warning against cigarette smoking on page 36.) When will I feel the baby move for the first time? You may feel the baby move around 18 to 22 weeks. If this is not your first pregnancy, you may feel movement earlier. If I do not drink milk, how should I get the recommended amount of calcium? It is especially important that you have four servings per day from dairy foods such as cheese, yogurt, and cottage cheese. If you feel you are not getting the proper amount of calcium, please talk to your doctor about a calcium supplement. May I douche during pregnancy? No, because of the possibility of infection. May I have intercourse throughout my pregnancy? Yes. There are no restrictions as long as there are no complications (i.e., vaginal bleeding or premature labor). If in doubt, consult your physician. Intercourse is not allowed once your water has broken. May I exercise during my pregnancy? Yes, but only in moderation as directed by your physician. Low impact or prenatal aerobic exercise classes, as well as walking and swimming, are recommended. Remember, do not lie flat on your back during any exercise. May I use acne medication during pregnancy? Yes, consult your physician for the permissible medications. May I sit in a Jacuzzi or hot tub? No, because your body temperature could become too high. This could be harmful to both you and your baby. May I use a tanning bed? No, because the ultraviolet rays increases your body temperature. May I use an electric blanket or heating pad? It is permissible, as long as it does not raise your body temperature. Is alcohol safe? Since no safe level of alcohol consumption has been documented at any point, our general recommendation is to avoid all alcohol intake throughout the entire pregnancy. If you have any further questions, please consult your physician. MEDICATION USE DURING PREGNANCY Any medications taken during pregnancy could have an effect on the developing baby; therefore, the best rule to remember during pregnancy is that no drug may be assumed to be harmless. Unless prescribed by our physicians, it is wise to avoid taking any medication during your pregnancy, even laxatives, eye drops, nasal sprays, nasal drops, mild pain relievers, and external ointments. If you have a condition that requires you to take medication regularly, please discuss this with your physician. Should a special need for medication arise, your physician will choose the safest drug available for you and your baby. For more common conditions, the following list of drugs are the only types of medication that our physicians have approved for you to use. Please remember that these should only be used in moderation if you feel you must take something. RECOMMENDED MEDICATIONS: COLD, COUGH, OR SORE THROAT • • • • • Tylenol or Extra Strength Tylenol: Take one or two every four hours Tylenol Cold Formula, Actifed, Sudafed, Claritin, Claritin –D, Chlortrimeton Chloraseptic throat spray, Cepacol lozenges or gargle every two hours with one cup of warm water containing 1 teaspoon of salt. Nasal sprays or saline drops use as directed (Afrin twice daily) Robitussin DM, Delsym, or Hall’s cough drops use as directed. HEADACHE OR FEVER • Tylenol (Acetaminophen) Regular or extra strength take 1-2 every four hours INDIGESTION/REFLUX SYMPTOMS • • • Elevate the head of your bed on a brick or thick board Use Maalox, Mylanta, Gaviscon, Riopan Plus, or Tums Use Pepcid AC, Zantac, or Prilosec OTC (these can be taken daily if needed) NAUSEA AND/OR VOMITING • • • • Use Emetrol or Emecheck as directed on the label Vitamin B-6 may also be taken Non-drowsy Dramamine as directed on the label If nausea or vomiting affects your fluid or food intake for more than 1 day, contact our office CONSTIPATION • • • • • Use Metamucil, Citracel or Fibercon as a fiber bulking agent Use Colace (stool softeners) 100mg at bedtime or twice daily Fruits, prunes, and all types of whole bran cereal are also helpful in the prevention of constipation For acute constipation try Milk of Magnesia, Senokot, Dulcolax tablets or suppositories, or glycerin rectal suppositories If the above recommendations are unsuccessful, a Fleet enema may be used as needed DIARRHEA • • Kaopectate (use only for 1 day, as directed) Imodium AD use as directed HEMORRHOIDS • • Preparation H Cream or suppositories, Anusol cream or suppositories or Tuck pads Warm sitz baths with Epsom Salts YEAST INFECTIONS • Monistat 3 (or generic brand) or GyneLotrimin (after the first trimester, be careful inserting the applicator) FOR ANY QUESTIONS REGARDING MEDICATION USE DURING PREGNANCY PLEASE CALL THE OFFICE DURING REGULAR BUSINESS HOURS BETWEEN 8:00 AM AND 5:00PM MONDAY THROUGH FRIDAY AND 8:00-12:00 ON SATURDAY. CALLS MADE TO THE ANSWERING SERVICE AFTER HOURS SHOULD BE LIMITED TO EMERGENCY SITUTATIONS ONLY. OTHER CONCERNS During your pregnancy, you should be aware of certain substances that can affect the health of you and your baby. We urge you to adhere to the following guidelines. LEAD Because lead can be dangerous to the developing fetus, the Food and Drug Administration has issued a warning to pregnant women concerning its use. When a container made with lead is used for coffee, tea, or other acidic beverages, especially when they are heated, the lead in the container can pass into the liquid. This warning also applies to the housing of acidic foods such as tomato sauce and fruit juices in containers made with lead. Ceramic mugs, lead crystal (including lead crystal baby bottles), pewter, and sliver-plated hollowware are some common lead containers that should be avoided. For daily use, pregnant women are encouraged to use regular glassware and plastic. CONTAMINATED FISH Although PCB’s or polychlorinated biphenyls (industrial residues) were banned in 1979, they continue to linger in our nation’s waters. As a result, they are often found in the tissues of salmon, swordfish, and lake whitefish. If ingested in large enough doses by pregnant women, or women who may become pregnant, they can harm the developing fetus. Mercury, which is released into our waters by the burning of fuels and industrial waste, accumulates in larger fish that live for many years, such as tuna, shark and swordfish. Consumer Report says that the most prudent approach for women who are pregnant, or who may become pregnant, is to avoid eating these fish altogether. On the other hand, many experts believe it is safe for women to include these fish in their diets as long as they avoid excessive amounts of any particular kind. Tuna presents the biggest concern since other fish such as swordfish, salmon, lake whitefish and shark, are rarely consumed in large quantities in our culture. Experts also suggest that pregnant women who do not give up fish should limit their intake to once or twice per week. ARTIFICIAL SWEETENERS Aspartame and Sucralose (Splenda ), artificial sweeteners that occurs naturally in all complete-protein foods, has been determined to be safe for consumption. However, our physicians recommend that you choose Aspartame or Sucralose rather that saccharine. However, we also recommend that you limit your intake of artificial sweeteners as well as caffeine. Talk with your doctor is you have any questions. ALCOHOL No safe limit of alcohol has been found for pregnancy. We recommend that you omit alcohol entirely. CIGARETTE SMOKING Cigarette smoking during pregnancy exposes you and your baby to approximately 1,000 different chemicals. A pregnant woman who smokes one package of cigarettes a day will inhale smoke approximately 11,000 times during an average pregnancy and may spend 10 percent of her waking day smoking. Scientific evidence indicates smoking during pregnancy increases the risk of death to an unborn infant, damage to the fetus while in the uterus, and complications for the mother during pregnancy. Tobacco smoke contains many harmful components, such as nicotine, carbon monoxide, hydrogen cyanide, tars, resins, and potential carcinogens. The diverse nature of tobacco smoke makes it difficult to tell exactly which chemical is responsible for the side effects. A scientific study originally published in 1957 reported a lower birth weight for those infants born to mothers who were smokers. There have been over 45 studies involving 500,000 deliveries that have confirmed this original scientific study. Children of mothers who smoked during pregnancy have been observed to have significantly lower IQ scores and a higher incidence of reading disorders than offspring of non-smokers. A higher incidence of minimal brain dysfunction syndrome (hyperactivity) is also reported in the children of mothers who smoke. Cigarette smoking during pregnancy also increases the risk of spontaneous miscarriage, fetal and neonatal death. Smoking not only increases the risk of fetal damage, but also increases the incidence of serious complications in the mother. The possibility of damage to the placenta (the organ through which the baby receives oxygen and nutrients) and incidence of placenta previa (abnormal location of the placenta) are both increased in smoking mothers. Smoking during pregnancy creates an extremely high-risk condition for both baby and mother. It is our position that if you are pregnant, you should stop smoking entirely and permanently at this time. It is also our position that if you continue to smoke while pregnant, you assume responsibility for the risks. The American Lung Association offers an eight week class for those who are interested in a group setting for instruction and support while “kicking the habit.” Please call your local chapter and ask about the Freedom From Smoking class in your area. SPECIAL TEST INFORMATION AFP-TRIPLE SCREEN TEST The alpha-fetoprotein (AFP) test helps identify a small number of women whose unborn babies may have certain defects such as Down’s Syndrome or an open neural tube defect. This test is available to women who are between weeks 15 and 19 of their pregnancies. A small amount of blood is drawn from a vein in the arm of the pregnant woman and is then tested for a variety of factors. Through this screening test, an open neural tube defect can usually be identified. It can detect approximately 50% of cases of Down’s Syndrome. The downside of the test is that it has a 90% false positive rate. Women who have a positive blood test will need amniocentesis for further evaluation. We will be glad to answer any questions you have concerning this matter. GLUCOSE SCREENING During pregnancy, the metabolic system experiences added stress. In some women, this additional stress results in a temporary rise in the blood sugar level. For this reason, your blood sugar level will be tested between 24 and 30 weeks. You will be notified as to when you should schedule your glucose screening. You will be given some Trutol, which is a sweet drink containing a measured dosage of glucose. An hour later, a blood sample will be drawn. You will be notified if your glucose level is elevated. If it is, you should begin following the special diet you will be given and schedule a follow-up blood sugar test. Please remember that an elevation in your glucose level does not mean anything is wrong with you or your baby. It does mean, however, that you will need to make some changes in your diet, and we will have to do some additional testing. NON-STRESS TEST (NST) In the last trimester, you may need a non-stress test (NST). During an NST, two monitor straps are placed around your abdomen to check the baby’s heartbeat and any contractions you might be having. (This is the same type of monitoring you will have in the labor room at the hospital.) This test lasts approximately 20 minutes. You will be monitored while lying in a recliner. If you need this type of test, it may be performed on a weekly basis. You will see the doctor with each scheduled NST appointment. GROUP B STREP INFORMATION Group B Strep is normally found in the vagina of 15% to 40% of all healthy adult women. Group B Strep should not be confused with Group A Strep which causes strep throat. GBS does not cause problems for the adult female. Most women carry it and don’t know it. GBS can cause illness in babies born to women with GBS. Therefore, your HWWC physician will check for GBS between 35-37 weeks. If the test is positive, you will be notified as well Labor & Delivery. You will be treated with antibiotics while you are in labor & delivery. Treatment is not recommended before labor & delivery because the transmission of the bacteria usually would occur during labor and/or delivery. CYSTIC FYBROSIS TESTING INFORMATION Cystic Fibrosis is a genetic disease that causes breathing problems, lung infections and digestive problems. These problems can require daily medication and respiratory (lung) therapy. Cystic Fibrosis does not cause a person to have learning problems or to look different. Most people that have a child with cystic fibrosis DO NOT have a family history of cystic fibrosis. Gene carriers have one altered copy of the CF gene and one normal copy. They do not have any symptoms of CF. Individuals with VF have two altered copies of the CF gene. If both parents are CF carriers they have a 1 in 4 chance (25%) to have a child with CF. Couples with the greatest chance to be a CF carrier that are planning a pregnancy or seeking prenatal care should consider CF Carrier Testing. You should also consider testing if you or your partner has a family member with CF. Testing should be considered if you are partners with an individual with CF or CF carrier. If you are interested in getting tested you should discuss this with your doctor or genetic counselor. The test will require a blood sample taken from the arm. For more information about Cystic Fibrosis please contact the following organizations: Cystic Fibrosis Foundation 6931 Arlington Road Bethesda, MD 20814 1-800-FIGHT CF www.ccf.org March of Dimes 1275 Mamaroneck Avenue White Plains, NY 10605 1-800-MODIMES www.marchofdimes.com UAB Department of Genetics Hugh Kaul Genetics Building 720 20 th Street South Suite 241 Birmingham, AL 35294-0024 (205) 934-4983 CHORIONIC VILLI SAMPLING This test is used to test for chromosomal abnormalities and genetic birth defects. Women who are over the age of 35 should consider CVS because of the increased risk of Down Syndrome and other chromosomal conditions. Women who have had a previous child with a genetic birth defect (including chromosomal), a family history of a genetic disorder, or an abnormal first trimester screening should also consider CVS. The ideal time to have the test done is 10-12 weeks of pregnancy. Using an ultrasound as a guide, the health care provider inserts a thin tube through the vagina and cervix to take a tiny tissue sample from outside the sac where the baby develops. The risks associated with CVS are a small risk of miscarriage (1 in 100 or less). Some women have cramping or spotting after the procedure. Studies suggest that the procedure may pose a very small risk (about 1 in 3000) of birth defects involving missing or shortened fingers or toes. This test is only available at Vanderbilt University in Nashville, TN. ULTRASOUND We recommend that all obstetrical patients have an ultrasound between the 17 th and 22 nd weeks of pregnancy. An ultrasound (or sonogram) is a test that uses sound waves to project an image on a screen, thus allowing your doctor to check your baby’s growth. There are no known side-effects to the baby from an occasional ultrasound examination. This test requires no special preparation. (You will not need to have a full bladder.) During the exam, you will lie on your back and a gel will be spread over your bare abdomen. This gel improves the conduction of sound as the transducer is moved over your abdomen. The echoes produced as the sound waves bounce off parts of the baby are recorded. Depending on the position of the fetus, you may be able to see the head, arms and legs, and even the beating heart. If you are in the early stages of pregnancy (before 16 weeks), we may use a device called a transvaginal probe, which is inserted into your vagina just like a tampon and enables us to see early pregnancy with great accuracy. The exam will not hurt you or your baby. By providing this service in our office, we are able to offer convenience, as well as lower medical costs for our patients; however, some insurance companies do not provide coverage for these charges. After your ultrasound appointment, you will see the doctor for a routine visit. We also offer ultrasounds for the purpose of sex determination. There is an additional fee for this particular procedure, and it will not be filed with your insurance company. You may be required to pay at the time of the procedure. Sex determination can usually be detected after 24 weeks (six months) of pregnancy. ON THE DAY OF YOUR ULTRASOUND Our ultrasounds are performed by registered sonographers. These qualified technicians are delighted to be a part of your birthing experience. To make this experience the best it can be, please allow the sonographer to complete the diagnostic test before asking questions. During this time, the technician’s full attention will be on you and your baby. Measurements will be made to calculate your due date and your baby’s weight. Your baby’s head, abdomen and extremities will be evaluated for abnormalities. When the test has been completed, the sonographer will gladly show you your baby. Family members are welcome to view the ultrasound. In order to have your ultrasound performed in a timely manner, please follow these suggestions: • • • • Children and other family members are always welcome, but please remind them to watch quietly. Space is limited. Please keep children off the scan table for their own protection. It is best to save questions until the ultrasound is completed. The sonographer will be glad to answer any questions at this point, or refer you to your doctor for further explanation. Because of the number of pre-scheduled ultrasounds performed every day, your patience is greatly appreciated if an emergency test has to be worked into the schedule; however, if you have not been notified of a delay and have been waiting over 20 minutes, please see the receptionist. PLEASE NOTE: In the course of performing a basic screening ultrasound, abnormalities or congenital anomalies of the fetus may be detected; however, it is not intended to detect all fetal abnormalities. You should be aware that a normal result on a basic screening ultrasound is not a guarantee that your baby will be born without birth defects. AMNIOCENTESIS An amniocentesis may be performed during pregnancy to help determine an inherited, genetic abnormality that the fetus may have. This procedure involves the careful passage of a thin needle through the abdomen of the mother and into the sac of the amniotic fluid surrounding the fetus. (This is done under ultrasound-guidance.) A small amount of the fluid is then withdrawn for analysis. • WHO SHOULD CONSIDER IT? The principle reasons for genetic amniocentesis are: maternal age of 35 years of older (at time of anticipated delivery), and a previous child with a proven chromosomal abnormality. Other reasons, which rarely occur, include testing for unusual enzyme deficiencies, neural tube (brain and spine) defects, sickle cell disease, and so forth. These often require additional counseling with a geneticist. • WHAT IS GENETIC AMNIOCENTESIS: Genetic amniocentesis is usually performed on an outpatient basis. This test is able to detect fetal sex and almost all chromosomal abnormalities. It is also able to detect 85 to 90 percent of neural tube defects by taking a sample of amniotic fluid and testing the level of alpha-fetoprotein. • WHAT ARE ITS LIMITATIONS? o o o o It cannot detect non-chromosomal congenital abnormalities such as cleft palate, intestinal or cardiac abnormalities, etc., which occur in approximately three percent of pregnancies. Its accuracy exceeds 99.9 percent, but cannot be totally guaranteed. There is a very remote possibility of error (one in 10,000 cases) in the interpretation of fetal cells grown from amniotic fluid. Fluid cannot be obtained on rare occasions because of technical difficulties or decreased amounts of fluid. The attempt must be postponed if this occurs. A second amniocentesis (seven to 14 days later) is needed on rare occasions because cells in the initial sample may not have grown enough to permit valid interpretation. • WHAT ARE THE RISKS? The principle risk of amniocentesis is spontaneous abortion (miscarriage), which occurs very rarely. Additional risks include, but are not limited to, death, possible fetal or maternal injury, infection or bleeding. Because there is a risk involved, it is important to note that this test is only recommended when there is a specific reason to believe that a detectable genetic disease may be present. The occurrence of these complications in our practice is unusual for several reasons. Most importantly, the physicians who perform this procedure are very experienced practitioners. Secondly, ultrasound is utilized to help determine the gestational age of the fetus, the position of the placenta, and the best area for the proper and safe placement of the amniocentesis needle. • WHAT IS THE COST? Essentially, there are two categories of charges: the charge for the procedure, and the charge for the laboratory analysis. If you do not have insurance, you will need to pay for the procedure prior to having it performed. If you do have insurance, it will be filed, and you will be billed for the amount not covered by your insurance. GLOSSARY The list of terms pertains to pregnancy, labor, and delivery. Most of these terms are found in this booklet. Others may come up in further reading or discussions with your doctor. Afterbirth: Placenta and membranes that are expelled after the birth of the child. Afterbirth Pains: Uterine cramps due to contraction of the uterus, occurring during the first few days after childbirth. Usually the pain is more severe during nursing, but rarely lasts longer than 48 hours after your baby is delivered. Alpha-fetoprotein (AFP): A protein produced by a growing fetus; it is present in amniotic fluid and, in small amounts, in the mother’s blood. Amniocentesis: A procedure in which a small amount of amniotic fluid is taken from the sac surrounding the fetus and tested to detect genetic disorders or maternal-fetal blood incompatibility. Amniotic Fluid: The liquid contained in the amnion. This fluid is transparent and almost colorless. The liquid protects the fetus from injury, and helps maintain an even temperature. Amniotic Sac: Known as the amnion; a thin transparent sac that holds the fetus suspended in amniotic fluid. Antibody: A protein produced in the blood as reaction to foreign substances in the blood. Apgar Score: A system of scoring infant’s physical condition one minute and five minutes after birth. The heart rate, respiration, muscle tone, response to stimuli, and color are rated 0, 1 or 2. The maximum score is 10. Areola: Circular dark area surrounding the nipple. Arterioles: Small arteries that can become larger and smaller, lowering and increasing the blood pressure. Axillary Temperature: Body temperature checked by using a thermometer under the armpit. Blood Pressure: The force of the blood against the wall of the arteries. Braxton Hicks Contractions: Uterine contractions which occur at various times during pregnancy. They are random, usually are not painful, do not increase in frequency, and do not dilate the cervix. They are not true labor contractions. Breech Presentation (Position): A situation in which a fetus is positioned to be born buttocks or feet first. Caesarean Birth (C-Section): Delivery of a baby through an incision made in the mother’s abdomen and uterus. Cervix: The opening to the uterus. Chorionic Villus Sampling (CVS): A procedure to test for genetic fetal defects. CVS can be done earlier than amniocentesis - usually between 9 and 11 weeks of pregnancy. Circumcision: Surgical removal of the end of the foreskin of the penis. Circumcision is usually performed at the request of the parents. There are very few medical indications for this procedure. Cleft Palate: An abnormality resulting from failure of facial processes of the embryo to fuse, which results in the roof of the mouth forming an opening between the mouth and nasal cavities. Colostrum: A thin white fluid discharged from the breasts at the beginning of milk production, usually noticeable during the last few weeks of pregnancy. Contraction: A shortening or tightening of uterine muscles where the sensation is felt in the abdomen, back, or both. Contraction Stress Test: Used to test the condition of the fetus. Mild contractions of the mother’s uterus are induced and the fetal heart rate is recorded in response to the contractions. Doppler: A form of ultrasound that reflects motion such as the fetal heartbeat in audible signals. Down’s Syndrome: A genetic disorder causing moderate to severe mental retardation and physical abnormalities. Women at high risk of giving birth to a child with Down’s Syndrome are those over 35, or those who have had a previous child with the syndrome. Eclampsia: Another name for seizures during pregnancy that occur because of high blood pressure. Ectopic pregnancy: Pregnancy that occurs outside the uterus, most often in the fallopian tubes. Edema: Swelling. Effacement: During the normal process of delivery, the dilation of the cervix, enlarging the cross-section area of the canal to permit passage of the fetus. (Softening of the pelvis). Electronic Fetal Monitoring: A method in which electronic instruments are used to record the heartbeat of the fetus and contractions of the mother’s uterus. Embryo: Stage in prenatal development between the ovum and the fetus. Between the 2 nd and 8 th week. Endometriosis: A condition in which tissue that looks and acts like the tissue lining the uterus grows outside the uterus. Epidural: A form of anesthesia used during labor. It is given via a narrow catheter threaded through a needle inserted into the space immediately around the spinal cord. Episiotomy: An incision between the vagina and rectum made during childbirth to widen the vaginal opening. Estradiol Level Test: A test used in infertility treatment to determine estrogen levels in the blood. This can help determine when ovulation occurs. External Version: A technique performed late in pregnancy in which the doctor manually attempts to move a breech baby into the normal, head down position. False Labor: During the final weeks or days of pregnancy, many women experience the contractions of false labor. These contractions are considered false labor because they do not become more frequent and they are not accompanied by dilation of the cervix or descent of the fetus. Fetal Distress: Problems with the baby which occur before birth that endanger the baby and require immediate delivery. Fetoscope: An optical device, usually flexible and made of fiberoptic materials, used to view the fetus in the uterus. Fetus: The child in utero from the third month to birth. Prior to that time it is called an embryo. Forceps: Special instruments placed around the baby’s head to help guide it out of the birth canal during delivery. Fontanelle: A soft spot lying between the cranial bones of the skull of a fetus. Gestational Diabetes: A disorder occurring only during pregnancy resulting from inadequate production or utilization of insulin. It can be controlled by diet and/or may require insulin injections. It is estimated to occur in about 3% of pregnancies and usually disappears after delivery. Glucose: A sugar. In medicine, the word is used to indicate the sugar dextrose. Glucose is the most important carbohydrate in body metabolism. Glucose Screening: A blood test given, ideally between the 24 th and 28 th week of pregnancy, identifying persons who should have a 3-hour glucose tolerance test to rule out gestational diabetes. Hemophilia: A hereditary blood disease in which the blood fails to clot and abnormal bleeding occurs. High-Risk Pregnancy: A pregnancy with complications that need special medical attention. Examples include: previous C-section, advanced maternal age, history of miscarriages, uterine abnormalities, and smoking during pregnancy. Your doctor will determine if you have any of these risk factors. Induced Labor: Labor that is started or speeded up through the intervention of a doctor, usually by using a drug. Kegel: An exercise for strengthening the pubococcygeal and levator ani muscles. Strengthening these muscles aids in childbirth, controlling urinary incontinence, and may enhance the pleasure derived from sexual intercourse. Lactation: The function of secreting milk. Lanugo (Down): Fine soft hair covering the skin of the newborn. Laparoscopy: An operation in which the organs inside the lower abdomen can be viewed through a lighted telescope. Lightening: Descent of the presenting part of the fetus into the pelvis. This often occurs two to three weeks prior to the beginning of the first stage of labor. Linea Nigra: Dark line from the pubic bone to the navel. Lochia: Vaginal discharge after delivery. Maternal Serum Alpha-fetoprotein (MASAFP Screening): Test of the amniotic fluid level used to evaluate fetal development. Membrane: A thin, soft, pliable layer of tissue that lines a tube or cavity, covers an organ or structure, or separates one part from another. Midline Incision: A vertical incision made from the navel to the pubic bone for Caesarean birth. Miscarriage: Spontaneous loss of a pregnancy before the fetus can survive outside the uterus. Natural Childbirth: Childbirth where breathing, relaxation, and massage techniques are used in place of medication. Neural Tube Defects: Fetal birth defects that result from improper development of the brain or spinal cord. Non-Stress Test (NST): A test in which fetal movements felt by the mother or noted by the doctor are recorded, along with changes in fetal heart rate. Obstetrician: A physician who treats women during pregnancy, labor, and delivers the infant. Ovulation: The monthly release of an egg from one of the ovaries. Perineum: The area between the vagina and the rectum. Placenta (afterbirth): Tissue connecting mother and fetus that brings nourishment and takes away waste. Pediatrician: A physician who specializes in pediatrics; the care of infants and children and the treatment of their diseases. Placenta Previa: A condition in which the placenta lies very low in the uterus, so that the opening of the uterus is partially or completely covered. Preeclampsia: A condition of pregnancy in which there is high blood pressure, swelling due to fluid retention, and abnormal kidney function. Premature: A baby born before 37 weeks. Prenatal: Existing or taking place after birth. Prenatal Care: Program of care for a pregnant woman before the birth of her baby. Postpartum: Occurring in the period shortly after childbirth. Rh Immune Globulin (RhIG): A drug that suppresses an Rh negative person’s antibody response to Rh positive blood cells. Rhogam Injection: RhoGAM is a trade name for Rho (D) immune globulin. Round Ligament: Two round cord-like structures passing from the front of the body of the uterus into the anterior wall of the broad ligament, below the fallopian tubes, outward through the inguinal canals to the soft tissues of the labia majora. Rubella: An acute infectious disease resembling both scarlet fever and measles (German Measles.) Show: Blood-tinged mucous-like discharge. Sickle Cell Disease: A hereditary chronic form of anemia in which abnormal sickle or crescent-shape blood cells are present. This is mostly found in the African-American population. Sonographer: A technologist trained in the application of ultrasound for diagnostic and therapeutic purposes. Tay Sachs disease: An inherited disease transmitted as an autosomal recessive trait mostly found in the Ashkenazi-Jewish population of Eastern Europe . Toxoplasmosis: A disease caused by an organism found in raw and rare meat, garden soil, and cat feces. The disease, which is generally not harmful to adults, can cause injury to the fetus and the placenta. Transverse Position: When the fetus is positioned crosswise in the uterus. Trimester: Each three-month period of pregnancy. Pregnancy is divided into three trimesters of equal length. Tubal Occlusion: Blockage of the fallopian tubes. Ultrasound: A test in which sound waves are used to examine the fetus or view the internal organs. Varicose veins: Enlarged twisted superficial veins. May occur in almost any part of the body, but are mostly commonly observed in the legs. Vacuum Extraction: The use of a special instrument that attaches to the baby’s head and helps guide it out of the birth canal during delivery. Vernix: Creamy white covering over the skin of the baby. Vertex Presentation: A position normally assumed by a fetus before labor and delivery in which the head is positioned down, at the top of the birth canal, ready to be delivered first. Urinalysis: A specimen of urine used for testing purposes. Uterus: An organ of the female reproductive system for containing and nourishing the embryo and fetus from the time the fertilized egg is implanted to the time for birth of the fetus. //
© Copyright 2026