Alternatives to Vancomycin for the Treatment of Staphylococcus aureus
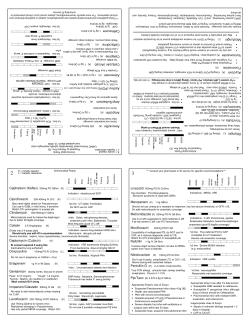
SUPPLEMENT ARTICLE Alternatives to Vancomycin for the Treatment of Methicillin-Resistant Staphylococcus aureus Infections Scott T. Micek Department of Pharmacy, Barnes-Jewish Hospital, St. Louis, Missouri Vancomycin has been considered to be the reference standard for the treatment of invasive methicillin-resistant Staphylococcus aureus (MRSA) infections, as a result of its relatively clean safety profile, its durability against the development of resistance, and, for many years, the lack of other approved alternatives. However, the advent and testing of new compounds with antiMRSA activity, for comparison with vancomycin, have rendered results that call into question the efficacy of vancomycin in the treatment of many serious infections. The reasons for clinical failure of vancomycin are many and have been hypothesized to include poor penetration of the drug to certain tissues [1–3], loss of accessory gene–regulator function in MRSA [4], and potential escalation of vancomycin MICs for MRSA [5]. Additionally, an increasing number of reports of vancomycin-intermediate S. aureus (VISA) and vancomycin-resistant S. aureus (VRSA) have populated the literature dating back to 1999. Many alternatives for the treatment of MRSA infections, including linezolid, daptomycin, tigecycline, and quinupristin/dalfopristin, Reprints or correspondence: Dr. Scott T. Micek, Dept. of Pharmacy, BarnesJewish Hospital, Mailstop 90-52-411, 216 S. Kingshighway Blvd., St. Louis, MO ([email protected]). Clinical Infectious Diseases 2007; 45:S184–90 2007 by the Infectious Diseases Society of America. All rights reserved. 1058-4838/2007/4506S3-0005$15.00 DOI: 10.1086/519471 S184 • CID 2007:45 (Suppl 3) • Micek are currently approved by the US Food and Drug Administration (FDA). Additionally, there are several investigational compounds with demonstrated in vitro activity against MRSA. The chemical structures of these agents are shown in figure 1. LINEZOLID Linezolid is a synthetic oxazolidinone that inhibits the initiation of protein synthesis at the 50S ribosome [6]. It is currently approved by the FDA for the treatment of complicated skin and skin-structure infections (SSSIs) and nosocomial pneumonia caused by susceptible pathogens, including MRSA. Several retrospective analyses of pooled data from randomized trials have compared linezolid with vancomycin in patients with proven MRSA infection. An analysis of 2 double-blind studies of patients with MRSA nosocomial pneumonia found that 75 patients treated with linezolid had survival rates that were significantly higher than those of 85 patients treated with vancomycin (80% vs. 64%; P p .03) [7]. The authors hypothesized that a possible explanation for the finding was vancomycin’s poor penetration of the lung, particularly when the standard dosage is 1 g administered every 12 h. However, aggressive dosing strategies for vancomycin (goal trough concentrations of 115 mg/mL, or 4⫺5⫻ the MIC value) may not offer an advantage over traditional dosing strategies [8, 9]. A follow-up, randomized, double-blind Downloaded from http://cid.oxfordjournals.org/ by guest on September 9, 2014 Vancomycin remains the reference standard for the treatment of systemic infection caused by methicillinresistant Staphylococcus aureus (MRSA). However, as a result of limited tissue distribution, as well as the emergence of isolates with reduced susceptibility and in vitro resistance to vancomycin, the need for alternative therapies that target MRSA has become apparent. New treatment options for invasive MRSA infections include linezolid, daptomycin, tigecycline, and quinupristin/dalfopristin. Additionally, a number of new anti-MRSA compounds are in development, including novel glycopeptides (dalbavancin, telavancin, and oritavancin), ceftobiprole, and iclaprim. The present article will review clinical issues surrounding the newly marketed and investigational agents with activity against MRSA. trial is under way that compares these 2 agents in hospitalized patients with nosocomial pneumonia due to MRSA. Similarly, retrospective evaluations of complicated skin and soft-tissue infections (SSTIs) caused by MRSA have found that, compared with vancomycin, linezolid is associated with significantly higher clinical cure rates and reduced lengths of hospitalization [6, 10]. A retrospective analysis of pooled data from 5 randomized studies did not find linezolid to be superior to vancomycin in patients with secondary MRSA bacteremia [11]. Linezolid should also be considered for necrotizing infections, including skin lesions [12], fasciitis [13], and pneumonia [14] caused by community-associated MRSA, particularly the USA300 strain. The severity of these infections may be associated with allotypes of mobile genetic elements found in USA300 that code for pathogenic toxins, including PantonValentine leukocidin, enterotoxin Q, and enterotoxin K [15]. It has been hypothesized that antibiotics with the ability to inhibit protein synthesis may demonstrate efficacy against susceptible toxin-producing strains. Linezolid, along with clindamycin, has recently been found to reduce production of Panton-Valentine leukocidin, a-hemolysin, and toxic-shock syndrome toxin–1, whereas vancomycin and nafcillin have been found to increase such production in an in vitro model [16]. Despite the apparent advantages of linezolid in the treatment of MRSA infections, concerns about safety often limit its use. Of particular concern is the association of linezolid with serotonin toxicity and thrombocytopenia [17, 18]. Linezolid exhibits weak reversible inhibition of monoamine oxidase and can induce toxicity when used in combination with agents that have serotonergic activity, most commonly selective serotonin reuptake inhibitors. Twenty-nine cases of linezolid-associated serotonin toxicity were recently reported. Postmarketing information submitted to the FDA regarding 29 patients with serotonin toxicity showed that 61% had received concomitant treatment with a selective serotonin reuptake inhibitor [17]. Three patients died, possibly because of serotonin toxicity, and another 13 patients required medical treatment [13]. Linezolid used concomitantly with selective serotonin reuptake inhibitors in hospitalized patients has also been evaluated in a retrospective study [19]. This study found a high probability of serotonin toxicity in association with 2 of 72 concomitant uses. The authors suggest that linezolid Novel Antibiotics for MRSA • CID 2007:45 (Suppl 3) • S185 Downloaded from http://cid.oxfordjournals.org/ by guest on September 9, 2014 Figure 1. Molecular structures of novel antibiotics for methicillin-resistant Staphylococcus aureus infections SSTIs (899 patients [87 patients with MRSA]) Bacteremia and endocarditis (246 patients [89 patients with MRSA]) Fowler et al. [29] SSTIs (546 patients [0 with documented MRSA and 8 with presumed MRSA]) Bacteremia (53 patients with MRSA) b SSTIs (285 patients with MRSA) Nosocomial pneumonia (160 patients with MRSA) Infection treated (no. of patients in study) Arbeit et al. [28] DPT Breedt et al. [25] TIG Shorr et al. [11] Wiegelt et al. [6] Wunderink et al. [7] LZD Drug, authors [reference] Efficacy The rate of adverse events was similar between treatment groups (LZD, 80%; VM, 70%), as c were the rate of serious adverse events (LZD, 47%; VM, 39%) and the rate of treatment discontinuation (LZD, 37%; VM, 39%); all differences were NS Adverse events similar between 2 groups, but there were increased rates of nausea and vomiting in the TIG group and higher rates of rash and increases in LFT results in the VM/ ATN group Clinical cure rate: LZD, 56% (14 of 25 patients); VM, 46% (13 of 28 patients); OR, 1.47 (95% CI, 0.50–4.34) Clinical response rate: TIG, 84%; VM/ATN, 87% (P p NS). Pathogen eradication rate: TIG, 85%; VM/ATN, 93% (P p .02). DPT (6 mg/kg iv q24h); OR VM (1 g d q12h) or PRPs (2 g q4h) plus GM (1 mg/kg iv q8h) Clinical success rate at day 42 of treatment: DPT, Overall incidence of adverse events was similar 44%; comparators, 42%. Clinical success rate between treatment groups. Rate of serious ade (patients with MRSA): DPT, 44%; comparators, verse events: DPT, 52%; comparators, 45%. Increases in creatine kinase levels were more 32%. common in the DPT group (7% vs. 1%) (P p .04). Frequency and distribution of adverse events were similar between treatment groups Drug-related adverse events were reported in similar numbers of patients in both treatment a arms Not reported Safety Clinical cure rate: LZD, 89% (124 of 140 patients); VM, 67% (97 of 145 patients) (P ! .001) DPT (4 mg/kg iv q24h for 7–14 days); Clinical success rate (all evaluable patients): DPT, comparators (results pooled) in83%; comparators, 84%. Clinical success rate d cluded PRPs (4–12 g/day iv) or VM (patients with MRSA): DPT, 75%; comparators, (1 g iv q12h) 68%. TIG (100 mg/day, with an initial 100mg loading dose); VM (1 g q12h) plus ATN (2 g q12h) LZD (600 mg) or VM (1 g each q12h); ATN is added in studies of pneumonia LZD (600 mg iv or po q12h) or VM (1 g q12h) LZD (600 mg q12h) or VM (1 g q12h); Clinical cure rate: LZD, 59% (36 of 61 patients); both plus ATN for 7–12 days VM, 36% (22 of 62 patients) (P ! .01). Survival rate: LZD, 80% (60 of 75 patients); VM, 64% (54 of 85 patients) (P p .03). Regimen Table 1. Overview of novel antimicrobial agents available to treat methicillin-resistant Staphylococcus aureus (MRSA). Downloaded from http://cid.oxfordjournals.org/ by guest on September 9, 2014 S186 TLV (7.5 mg/kg/day iv); standard therapy: VM (1 g q12h), NAF or OX (2 g q6h), and Clox (0.5–1 g q6h) SSTIs due to gram-positive pathogens CTB (500 mg q12h); VM (1 g q12h) (784 patients [125% with MRSA]) f Clinical cure rate: CTB, 93%; VM, 93%. MRSA clinical response rate: CTB, 92%; VM, 90%. Overall test-of-cure rate: TLV, 80%; standard therapy, 77%. MRSA test-of-cure rate: TLV, 82%; standard therapy, 69%. MRSA microbiological eradication rate: TLV, 84%; standard therapy, 74% Overall success rate: DBV, 87%; VM, 73% Clinical efficacy at test-of-cure: DBV, 89%; LZD, 91% There were few serious treatment-related adverse events, the incidences of which were similar between treatment groups Fewer serious adverse events were noted with TLV; the most common adverse events were similar between treatment groups and included nausea, psychiatric disorder, headache, vomiting, and dyspnea Adverse events were generally mild and were comparable in the 2 treatment groups Adverse events involving the GI tract were the most common adverse events in both treatment groups; a higher proportion of patients receiving LZD had adverse events that were judged by investigators to be treatment related f e d c b a Diarrhea, nausea, and thrombocytopenia were most commonly associated with LZD, and anemia, nausea, and pruritus were most commonly associated with VM. Pooled analysis of results from 5 studies. Details regarding the nature of the serious adverse events are not available. Investigators assessed each event as serious or not serious. Clox, flucloxacillin, NAF, and OX. Serious adverse events included infections and infestations, cardiac disorders, respiratory, thoracic, and mediastinal disorders, nervous system disorders, psychiatric disorders, and laboratory abnormalities. Phase 2 study. NOTE. ATN; aztreonam; Clox, cloxacillin; CR-BSIs, catheter-related bloodstream infections; CTB, ceftobiprole; DBV, dalbavancin; DPT, daptomycin; GI, gastrointestinal; GM, gentamicin; iv, intravenously; LFT, liver function test; LZD, linezolid; MRSA, methicillin-resistant Staphylococcus aureus; NAF, nafcillin; NS, not significant; OX, oxacillin; po, by mouth; PRPs, penicillinase-resistant penicillins; q4h, every 4 h; q6h, every 6 h; q8h, every 8 h; q12h, every 12 h; q24h, every 24 h; SSTIs, skin and soft-tissue infections; TIG, tigecycline; TLV, telavancin; VM, vancomycin. Basilea Pharmaceutica [33] CTB Stryjewski et al. [32] SSTIs (167 patients [48 patients with MRSA]) CR-BSIs (75 patients [14 patients with DBV (1000 mg on day 1, followed by MRSA]) 500 mg iv on day 8); VM (1 g q12h for 14 days) Raad et al. [31] TLV SSTIs (660 patients [287 patients with DBV (1000 mg on day 1, followed by MRSA]) 500 mg iv on day 8); LZD (600 mg iv or po q12h for 14 days) Jauregui et al. [30] DBV Downloaded from http://cid.oxfordjournals.org/ by guest on September 9, 2014 S187 may be used concomitantly with selective serotonin reuptake inhibitors, with careful monitoring, and they recommend prompt discontinuation of the serotonergic agent if serotonin syndrome is suspected [19]. The occurrence of thrombocytopenia has proven to be not significantly different than that encountered in patients with nosocomial pneumonia or orthopedic infections. Of note, patients with renal insufficiency may be at higher risk of developing this toxicity [20, 21]. Finally, there have been sporadic reports of peripheral neuropathy, typically in patients with osteomyelitis or other underlying diseases, and lactic acidosis [22, 23]. TIGECYCLINE DAPTOMYCIN Daptomycin is a cyclic lipopeptide that causes depolarization of the bacterial cell membrane. The indicated dose for MRSA- S188 • CID 2007:45 (Suppl 3) • Micek GLYCOPEPTIDES Dalbavancin. Dalbavancin is a semisynthetic lipoglycopeptide that inhibits cell wall synthesis and has in vitro activity against MRSA [34]. The unique feature of this investigational agent is its long half-life (6–10 days), which allows for onceweekly dosing. In a randomized, double-blind trial, dalbavancin (1000 mg given intravenously on day 1 and 500 mg given intravenously on day 8) has been compared with linezolid in the treatment of SSSIs [30]. Overall clinical success rates are presented in table 1. In this trial, 51% of the isolates were found to be MRSA. In a phase 2, open-label study of the treatment of catheter-related bloodstream infections, once-weekly treatment with dalbavancin was compared with treatment with vancomycin [31]. MRSA was identified at baseline in 5 patients who received dalbavancin, and, in the overall intention-to-treat analysis, dalbavancin was found to result in a success rate significantly higher than that noted with vancomycin (87% vs. 50%; P ! .05). The most common adverse events included nausea and diarrhea or constipation; however, dalbavancin may also be associated with hypotension, hypokalemia, and increases in alanine aminotransferase and aspartate aminotransferase levels measured in liver function tests, although, to date, the reports of these adverse events are conflicting [34]. Telavancin. Telavancin is another semisynthetic lipoglycopeptide that has a dual mechanism of action, including inhibition of cell wall synthesis and disruption of membrane barrier function [35]. It has a half-life of 7–9 h, which allows once-daily dosing (7.5–10 mg/kg/day). The disruption of membrane barrier function translates to rapid bactericidal ac- Downloaded from http://cid.oxfordjournals.org/ by guest on September 9, 2014 Tigecycline is the first drug approved in the class of glycylcyclines, a derivative of minocycline. A modified side chain on tigecycline enhances binding to the 30S ribosomal subunit, inhibiting protein synthesis and bacterial growth across a broad spectrum of pathogens, including MRSA [24]. In addition, this structural modification circumvents resistance mechanisms that plague tetracycline and other antibiotics in this class. Tigecycline is approved in the United States for the treatment of complicated SSSIs due to MRSA. The drug is also approved for the treatment of complicated intra-abdominal infections but only for those caused by methicillin-susceptible S. aureus. At this time, the published experience with tigecycline for the treatment of MRSA infections is limited to 2 double-blind comparison studies of vancomycin and aztreonam in patients with complicated SSSIs and case reports [25, 26]. Tigecycline has a large volume of distribution and produces high concentrations in tissues outside of the bloodstream, including bile, the colon, and the lung. Conversely, serum concentrations of tigecycline rapidly decrease after infusion, and the area under the concentration-time curve (AUC) after administration of multiple 50-mg doses every 12 h is ∼3 mg7h/mL [27]. On the basis of studies of the pharmacodynamic properties of tetracycline, the target AUC for tigecycline should be 2–4 times the MIC, in an effort to optimize efficacy in the treatment of MRSA infections. Given a tigecycline MIC90 range of 0.25–0.5 mg/mL for MRSA, caution should be used when using tigecycline for the treatment of patients with suspected or proven bacteremia [27]. The results of further clinical evaluation should be cumulated and assessed to determine whether to accept or refute this potential limitation. The approved dose is a 100-mg intravenous loading dose followed by 50 mg given every 12 h. Nausea and vomiting are the predominant adverse events, and they increase in frequency with dose escalation. associated complicated SSTIs is 4 mg/kg once daily, and that for bloodstream infections, including right-side endocarditis, is 6 mg/kg once daily [28]. Of note, daptomycin should not be used in the treatment of MRSA pneumonia, because the activity of the drug is inhibited by pulmonary surfactant. The results of daptomycin trials in patients with complicated SSTIs and bacteremia/endocarditis are shown in table 1 [28, 29]. In brief, of the patients who had MRSA isolated, 20 (44%) of 45 were successfully treated with daptomycin, and, of the patients in the bacteremia/endocarditis trial, 14 (32%) of 44 patients were successfully treated with vancomycin. The difference between daptomycin and standard therapy in the treatment of MRSA infections was not statistically significant. Significantly, for 6 patients who experienced microbiological failure while receiving daptomycin, it was reported that, during therapy, the MICs for the isolated pathogen increased from 0.25 or 0.5 mg/mL to 2 or 4 mg/mL [29]. The mechanism for resistance development while receiving therapy is, at present, not understood, but it is likely to be a consequence and a concern in patients who require prolonged courses of daptomycin therapy. ylococci are susceptible to ceftaroline [43]. Phase 2 studies of this agent in patients with SSTIs are under way. ICLAPRIM Iclaprim is a diaminopyrimidine that inhibits the enzyme dihydrofolate reductase. Data on iclaprim are limited. However, it has activity against MRSA, and preliminary results from a phase 3 trial in patients with complicated SSTIs showed noninferiority of iclaprim to linezolid at the test of cure [44]. In this study, ∼25% of the infections were due to MRSA. CONCLUSIONS Several antibiotics with anti-MRSA activity, including linezolid, tigecycline, and daptomycin, have been approved by the FDA. Additionally, there are a number of compounds in development that will likely provide a broader armamentarium for clinicians in the management of infections due to MRSA. The emergence of vancomycin-intermediate and vancomycin-resistant strains of S. aureus has also created a need for agents with expanded coverage. The in vitro activity of new and investigational agents against VISA and VRSA has recently been reviewed elsewhere [45]. In brief, linezolid, daptomycin, tigecycline, and quinupristin/dalfopristin, as well as the new investigational compounds dalbavancin, telavancin, oritavancin, ceftobiprole, and iclaprim, have demonstrated in vitro activity against VISA and VRSA. CEFTOBIPROLE AND CEFTAROLINE Ceftobiprole is an investigational cephalosporin engineered to bind tightly to penicillin-binding protein 2a, a peptidoglycan transpeptidase that confers b-lactam resistance in S. aureus isolates harboring the mecA gene [40, 41]. This compound is the first of the b-lactam antibiotics to have activity against MRSA as well as penicillin-resistant streptococci. Importantly, in preclinical, multipassage resistance-selection studies, ceftobiprole demonstrated a low potential to select for resistance; the highest MIC found in the presence of prolonged serial passages with ceftobiprole at subinhibitory concentrations was 8 mg/mL in 1 of 10 strains after 50 passages [42]. Ceftobiprole is administered twice daily by the intravenous route and has been granted fasttrack status by the FDA for the indications of complicated SSSIs and health care–associated pneumonia [41]. Two phase 3 trials for complicated SSSIs have been completed (STRAUSS and STRAUSS II), with preliminary results reportedly demonstrating noninferiority of ceftobiprole to comparators overall and in patients with MRSA [40, 33]. The most common adverse effects were nausea and taste disturbances. Ceftaroline is another broad-spectrum cephalosporin with gram-positive and gram-negative bactericidal activity. Early testing indicates that MRSA and vancomycin-resistant staph- Acknowledgments Supplement sponsorship. This article was published as part of a supplement entitled “Bugging the Bugs: Novel Approaches in the Strategic Management of Resistant Staphylococcus aureus Infections,” jointly sponsored by the Dannemiller Memorial Educational Foundation and Emeritus Educational Sciences and supported by an educational grant from OrthoMcNeil, Inc., administered by Ortho-McNeil Janssen Scientific Affairs, LLC. Potential conflicts of interest. S.T.M. has received research/grant support from Ortho-McNeil. References 1. Albane`se J, Le´one M, Bruguerolle B, Ayem ML, Lacarelle B, Martin C. Cerebrospinal fluid penetration and pharmacokinetics of vancomycin administered by continuous infusion to mechanically ventilated patients in an intensive care unit. Antimicrob Agents Chemother 2000; 44:1356–8. 2. Cruciani M, Gatti G, Lazzarini L, et al. Penetration of vancomycin into human lung tissue. J Antimicrob Chemother 1996; 38:865–9. 3. Lamer C, de Beco V, Soler P, et al. Analysis of vancomycin entry into pulmonary lining fluid by bronchoalveolar lavage in critically ill patients. Antimicrob Agents Chemother 1993; 37:281–6. 4. Sakoulas G, Moellering RC Jr, Eliopoulos GM. Adaptation of methicillin-resistant Staphylococcus aureus in the face of vancomycin therapy. Clin Infect Dis 2006; 42(Suppl 1):S40–50. 5. Robert J, Bismuth R, Jarlier V. Decreased susceptibility to glycopeptides in methicillin-resistant Staphylococcus aureus: a 20 year study in a large French teaching hospital, 1983–2002. J Antimicrob Chemother 2006; 57:506–10. Novel Antibiotics for MRSA • CID 2007:45 (Suppl 3) • S189 Downloaded from http://cid.oxfordjournals.org/ by guest on September 9, 2014 tivity against pathogens, including MRSA. It is currently under investigation for the treatment of SSTIs, nosocomial pneumonia, and uncomplicated bacteremia due to S. aureus [35]. As shown in table 1, the efficacy of telavancin was similar to that of standard therapy in early trials [32, 36]. Preliminary, unpublished phase 3 results indicate that the clinical cure and eradication rates associated with telavancin were higher than those associated with vancomycin, particularly in patients infected with MRSA [37]. Adverse events reported to date include nausea, taste disturbance, and insomnia. Oritavancin. Oritavancin is also a semisynthetic glycopeptide that is in development. The mechanism of action of this drug involves disruption of transmembrane potential, and it has demonstrated activity against vancomycin-resistant strains of staphylococci and enterococci [38]. Oritavancin has a very long half-life of ∼100 h, and dosing once daily or every other day is likely to be recommended. The percentage of time above the MIC of the free drug was found to be the determinant of microbiological and clinical response in bacteremia [39]. Studies of oritavancin are being conducted in patients with complicated SSTIs, catheter-related bloodstream infections, and nosocomial pneumonia [38]. Preliminary results of studies of SSTIs showed noninferiority of oritavancin to vancomycin and cephalexin. Adverse events associated with oritavantin include headache, nausea, and sleep disorders. S190 • CID 2007:45 (Suppl 3) • Micek 26. Sacchidanand S, Penn RL, Embil JM, et al. Efficacy and safety of tigecycline monotherapy compared with vancomycin plus aztreonam in patients with complicated skin and skin structure infections: results from a phase 3, randomized, double-blind trial. Int J Infect Dis 2005;9: 251–61. 27. Rodvold KA, Gotfried MH, Cwik M, Korth-Bradley JM, Dukart G, Ellis-Grosse EJ. Serum, tissue and body fluid concentrations of tigecycline after a single 100 mg dose. J Antimicrob Chemother 2006; 58: 1221–9. 28. Arbeit RD, Maki D, Tally FP, Campanaro E, Eisenstein BI. The safety and efficacy of daptomycin for the treatment of complicated skin and skin-structure infections. Clin Infect Dis 2004; 38:1673–81. 29. Fowler VG Jr, Boucher HW, Corey GR, et al. Daptomycin versus standard therapy for bacteremia and endocarditis caused by Staphylococcus aureus. N Engl J Med 2006; 355:653–65. 30. Jauregui LE, Babazadeh S, Seltzer E, et al. Randomized, double-blind comparison of once-weekly dalbavancin versus twice-daily linezolid therapy for the treatment of complicated skin and skin structure infections. Clin Infect Dis 2005; 41:1407–15. 31. Raad I, Darouiche R, Vazquez J, et al. Efficacy and safety of weekly dalbavancin therapy for catheter-related bloodstream infection caused by gram-positive pathogens. Clin Infect Dis 2005; 40:374–80. 32. Stryjewski ME, O’Riordan WD, Lau WK, et al. Telavancin versus standard therapy for treatment of complicated skin and soft-tissue infections due to gram-positive bacteria. Clin Infect Dis 2005; 40:1601–7. 33. Basilea Pharmaceutica. Basilea reports excellent pivotal data for ceftobipriole, a novel anti-MRSA broad-spectrum investigational antibiotic, at ICAAC. Available at: http://www.basilea.com/template_ loader.php?tplpage_idp34&modepdetails&idp73Accessed.Accessed 2 February 2007. 34. Pope SD, Roecker AM. Dalbavancin: a novel lipoglycopeptide antibacterial. Pharmacotherapy 2006; 26:908–18. 35. Kanafani ZA. Telavancin: a new lipoglycopeptide with multiple mechanisms of action. Expert Rev Anti Infect Ther 2006; 4:743–9. 36. Stryjewski ME, Chu VH, O’Riordan WD, et al. Telavancin versus standard therapy for treatment of complicated skin and skin structure infections caused by gram-positive bacteria: FAST 2 Study. Antimicrob Agents Chemother 2006; 50:862–7. 37. Theravance. Theravance announces positive results in phase 3 telavancin complicated skin and skin structure infection program. Available at: http://ir.theravance.com/ReleaseDetail.cfm?ReleaseIDp208110. Accessed 2 February 2007. 38. Ward KE, Mersfelder TL, LaPlante KL. Oritavancin—an investigational glycopeptide antibiotic. Expert Opin Investig Drugs 2006; 15:417–29. 39. Bhavnani SM, Passarell JA, Owen JS, Loutit JS, Porter SB, Ambrose PG. Pharmacokinetic-pharmacodynamic relationships describing the efficacy of oritavancin in patients with Staphylococcus aureus bacteremia. Antimicrob Agents Chemother 2006; 50:994–1000. 40. Chambers HF. Ceftobiprole: in-vivo profile of a bactericidal cephalosporin. Clin Microbiol Infect 2006; 12(Suppl 2):17–22. 41. Page MG. Anti-MRSA b-lactams in development. Curr Opin Pharmacol 2006; 6:480–5. 42. Bogdanovich T, Ednie LM, Shapiro S, Appelbaum PC. Antistaphylococcal activity of ceftobiprole, a new broad-spectrum cephalosporin. Antimicrob Agents Chemother 2005; 49:4210–9. 43. Cerexa. Ceftaroline acetate. Available at: http://www.cerexa.com/ products.html. Accessed 2 February 2007. 44. Arpida. Intravenous iclaprim. Available at: http://www.arpida.ch/ index.php?MenuIDp13&UserIDp1&ContentIDp65. Accessed 2 February 2007. 45. Drew RH. Emerging options for treatment of invasive, multidrugresistant Staphylococcus aureus infections. Pharmacotherapy 2007; 27: 227–49. Downloaded from http://cid.oxfordjournals.org/ by guest on September 9, 2014 6. Weigelt J, Itani K, Stevens D, et al. Linezolid versus vancomycin in treatment of complicated skin and soft tissue infections. Antimicrob Agents Chemother 2005; 49:2260–6. 7. Wunderink RG, Rello J, Cammarata SK, Croos-Dabrera RV, Kollef MH. Linezolid vs vancomycin: analysis of two double-blind studies of patients with methicillin-resistant Staphylococcus aureus nosocomial pneumonia. Chest 2003; 124:1789–97. 8. Hidayat LK, Hsu DI, Quist R, Shriner KA, Wong-Beringer A. Highdose vancomycin therapy for methicillin-resistant Staphylococcus aureus infections: efficacy and toxicity. Arch Intern Med 2006; 166:2138–44. 9. Jeffres MN, Isakow W, Doherty JA, et al. Predictors of mortality for methicillin-resistant Staphylococcus aureus health-care–associated pneumonia: specific evaluation of vancomycin pharmacokinetic indices. Chest 2006; 130:947–55. 10. Itani KM, Weigelt J, Li JZ, Duttagupta S. Linezolid reduces length of stay and duration of intravenous treatment compared with vancomycin for complicated skin and soft tissue infections due to suspected or proven methicillin-resistant Staphylococcus aureus (MRSA). Int J Antimicrob Agents 2005; 26:442–8. 11. Shorr AF, Kunkel MJ, Kollef M. Linezolid versus vancomycin for Staphylococcus aureus bacteraemia: pooled analysis of randomized studies. J Antimicrob Chemother 2005; 56:923–9. 12. Baggett HC, Hennessy TW, Rudolph K, et al. Community-onset methicillin-resistant Staphylococcus aureus associated with antibiotic use and the cytotoxin Panton-Valentine leukocidin during a furunculosis outbreak in rural Alaska. J Infect Dis 2004; 189:1565–73. 13. Miller LG, Perdreau-Remington F, Rieg G, et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med 2005; 352:1445–53. 14. Micek ST, Dunne M, Kollef MH. Pleuropulmonary complications of Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus: importance of treatment with antimicrobials inhibiting exotoxin production. Chest 2005; 128:2732–8. 15. Diep BA, Gill SR, Chang RF, et al. Complete genome sequence of USA300, an epidemic clone of community-acquired methicillin-resistant Staphylococcus aureus. Lancet 2006; 367:731–9. 16. Stevens DL, Ma Y, Salmi DB, McIndoo E, Wallace RJ, Bryant AE. Impact of antibiotics on expression of virulence-associated exotoxin genes in methicillin-sensitive and methicillin-resistant Staphylococcus aureus. J Infect Dis 2007; 195:202–11. 17. Lawrence KR, Adra M, Gillman PK. Serotonin toxicity associated with the use of linezolid: a review of postmarketing data. Clin Infect Dis 2006; 42:1578–83. 18. Perry CM, Jarvis B. Linezolid: a review of its use in the management of serious gram-positive infections. Drugs 2001; 61:525–51. 19. Taylor JJ, Wilson JW, Estes LL. Linezolid and serotonergic drug interactions: a retrospective survey. Clin Infect Dis 2006; 43:180–7. 20. Lin YH, Wu VC, Tsai IJ, et al. High frequency of linezolid-associated thrombocytopenia among patients with renal insufficiency. Int J Antimicrob Agents 2006; 28:345–51. 21. Wu VC, Wang YT, Wang CY, et al. High frequency of linezolid-associated thrombocytopenia and anemia among patients with end-stage renal disease. Clin Infect Dis 2006; 42:66–72. 22. Senneville E, Legout L, Valette M, et al. Effectiveness and tolerability of prolonged linezolid treatment for chronic osteomyelitis: a retrospective study. Clin Ther 2006; 28:1155–63. 23. Palenzuela L, Hahn NM, Nelson RP Jr, et al. Does linezolid cause lactic acidosis by inhibiting mitochondrial protein synthesis? Clin Infect Dis 2005; 40:e113–6. 24. Rose WE, Rybak MJ. Tigecycline: first of a new class of antimicrobial agents. Pharmacotherapy 2006; 26:1099–110. 25. Breedt J, Teras J, Gardovskis J, et al. Safety and efficacy of tigecycline in treatment of skin and skin structure infections: results of a doubleblind phase 3 comparison study with vancomycin-aztreonam. Antimicrob Agents Chemother 2005; 49:4658–66.
© Copyright 2026