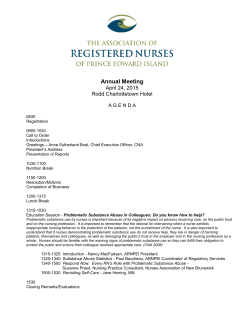
Program Book - College of Nursing
NURSING RESEARCH CONFERENCE 2015 April 24, 2015 (7:30AM – 4:30PM) Diversity and Collaboration in Research and Practice University of Arkansas for Medical Sciences I. Dodd Wilson Education Building 4301 West Markham Street Little Rock, Arkansas 72205 College of Nursing, University of Arkansas for Medical Sciences Central Arkansas Veterans Healthcare System Nursing Service Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) Nursing Workforce Diversity Grant# D19HP26966 Sigma Theta Tau International Gamma XI Chapter Arkansas Hartford Center of Geriatric Nursing Excellence University of Arkansas for Medical Sciences Medical Center CHI St. Vincent Infirmary 1 Welcome to Nursing Research Conference 2015 This annual nursing conference has grown over the past few years and broadened its scope to include evidence-based practice, advanced nursing practice, nursing education, and staff development in a variety of nursing practice settings and academic nursing research. Here are some tips for a more productive day: Please take time to review the activities scheduled for the day. Note that times and room numbers are listed on the detailed schedule of activities. There are four points in the day in which attendees have multiple concurrent options from which to choose. Review the titles listed on the detailed schedule and the abstracts (available online) to plan which you will attend. Breakout Session I: A or B or C Breakout Session II: D or E or F Poster Session I (multiple rooms) Poster Session II (multiple rooms) Rooms will present posters with common topics. Visit the exhibits to learn about career opportunities Network with others who have similar interests in nursing, nursing science, and evidence for practice. Consider noting contact information and/or abstract numbers for later use. Restrooms and the elevator are along the west side of the building. Stairs are in the middle of the building. Lunch will be served on the first level of the building for everyone’s convenience. Name badges are coded for the type of lunch requested. Contact Hour certificates will be awarded upon submission of completed evaluation forms and hours are based on hours of actual participation in the day’s activities. Those who cannot stay the whole day are welcome to request hours for the sessions attended. CONTINUING NURSING EDUCATION CONTACT HOURS At the completion of this conference, the participant will be able to: Describe techniques, methods, and strategies used in evidence-based practice. Discuss the utilization of nursing research based on current findings. Describe educational and clinical practice innovations and resources. All program planners and presenters have signed Conflict of Interest forms, indicating that they have no financial relationships with commercial entities which produce or disseminate pharmaceutical or other patientcare products or devices, that they will not discuss off-label use of such products or devices, and will not endorse products of these entities. Any support from commercial entities will be provided in the form of unrestricted educational grants which will not influence the educational program. If provided, such commercial support will be announced during the opening session, and published in the program book. By attending the entire program, nurses will earn 6.25 Continuing Nursing Education contact hours. In order to earn these hours, nurses must submit the completed evaluation form, which will be exchanged for a certificate of completion. Less contact hours may be earned by those who attend only part of the program. Central Arkansas Veterans Healthcare System is an approved provider of continuing nursing education by Arkansas Nurses Association, an accredited approver by the American Nurses Credentialing Center’s COA. 2 Nursing Research Conference 2015 SPONSORS Osmonetta Beard College of Nursing University of Arkansas Medical Sciences 4301 West Markham Street, Slot 529 Little Rock, AR 72205 2015: SPONSORS Office: 501.296.1040 Fax: 501.686.7591 Email: [email protected] The Growing Our Own in the Delta (GOOD) program is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under the Nursing Workforce Diversity grant (Grant# D19HP26966). Central Arkansas Veterans Healthcare System Nurse Recruitment (118/LR) 4300 West 7th Street Little Rock, Arkansas 72205 (501) 257-6153 Email: [email protected] [email protected] [email protected] Sigma Theta Tau International Honor Society of Nursing Gamma Xi Chapter http://nursing.uams.edu/gammaxi Mitch Highfill, Nurse Recruiter Arkansas Children’s Hospital Children’s Way, Slot 607 Little Rock, AR 72202 Office: 501.364.1398 E-mail: [email protected] CHI St. Vincent Infirmary Amy Funderburk, MSN, RN, NE-BC Executive Director of Nursing Jack Stephens Heart Institute Phone: 501-552-3772 Fax: 501-552-4216 Email: [email protected] 3 Susan Erickson, RN, MNSc, BC-NA, CHCR Nurse Recruiter & Recruitment/Retention officer University of Arkansas Medical Sciences 4301 West Markham Street, Slot 526 Little Rock, AR 72205 Office: 501.686.7144 Fax: 501.686.5698 E-mail: [email protected] Claudia J. Beverly PhD, RN, FAAN Director, Arkansas John A. Hartford Center for Geriatric Nursing Excellence College of Nursing University of Arkansas for Medical Sciences 501-686-5979 Email: [email protected] ARKANSAS ACTION COALITION Debra Jeffs, PhD, RN Co-Director Director, Academic Nursing Education Arkansas Children’s Hospital 4 Nursing Research Conference 2015 PLANNING COMMITTEE Affiliation University of Arkansas for Medical Sciences, College of Nursing Roles Conference Program Planning and Coordination Abstract Review Event Staffing Registration Processes Evaluation Analysis Door Prize, Donations, Exhibitors Committee Member Ayasha Thomason, MNSc, APN, WHNP-BC Becky Patterson, PhD, RN, CPNP Beth Ann West, Administrative Analyst Bill Buron, PhD, RN, FNP/GNP-BC Cathrin Carithers, DNP, RN Ednarene Rodgers, Administrative Assistant II Lee Blackwood, Department Business Manager Mark Tanner, MNSc, BSN, RN; Karen Davis, MSN, RN Melodee Harris, PhD, RN Sara Jones, PhD, APRN, PMHNP-BC Seongkum Heo, PhD, RN, Research Day Chair Stacy Hoyle, MHSA, Assistant Dean for Administration Tamisha Henderson, MSN, MHA, RN, CCM; Tina Pettey, PhD, RN, FNP-BC, APRN Trisha Wright, PhD, MPH, RN UAMS CON Development Office Central Arkansas Veterans Healthcare System Nursing Service Continuing Nursing Education (CNE) Provider CNE evaluation forms and certificates Conference Program Planning; Abstract Review Charlotte Brunner, MNSc, RN, CCRN Michael Farruggia, PhD,RN Sheila Sullivan, PhD, RN Taryn Bailey, MSN, RN-BC University of Arkansas for Medical Sciences, Medical Center Conference Program Planning Abstract Review Event Staffing Financial Support Tammy Jones, PhD, RNC Amy Hester, BSN, RN, BC Arkansas Children’s Hospital Conference Program Planning Abstract Review Conference Program Planning Angela Green, PhD, APRN, RN, NNP-BC Amy C. Huett, PhD(c), RN Debra Jeffs, PhD, RN Conference Program Planning Amy Funderburk, MSN, RN, NE-BC Debbie Campbell, RN Penny Sikes, BSN, RNP, OCN, RN Peggy Diaz, RN Hartford Center for Geriatric Nursing Excellence St. Vincent hospital Robin Mcatee, PhD, RN 5 Sigma Theta Tau International— Gamma Xi Chapter Financial Support Networking Student Poster Awards Tammy Webb, MS, RN, NE-BC, President Tamisha Gatewood-Henderson, MSN, MHA, CCM, Awards Chair Leanne Lefler, PhD, ACNS, APRN, FAHA, Research Chair 6 Nursing Research Conference 2015 ABSTRACT REVIEWERS Name and Credentials Name and Credentials Anita Mitchell, PhD, RN, APRN, FNP-BC Laura Evans, PhD, RN Ashley Jensen, PhD, RN Leanne Lefler, PhD, RN, APRN, ACNS-BC Becky Parnell MNSc, RN, APRN, ACNC-BC Leonie DeClerk, DNP, RN, APRN, FNP-BC Becky Patterson, PhD, PPCNP-BC Marilyn Hughes, MNSc, RN Becky Webb, MNSc, RN Mark Tanner, MNSc, RN Beverly English, MNSc, RN Natalie Capps, MNSc, RN Bill Buron, PhD, RN, APRN, GNP/FNP-BC Neena Grissom, MSN, RN, CNE Cathrin Carithers, DNP, RN, APRN, FNP-C Nicole Ward, MNSc, RN, APRN, WHNP-BC Cheryl Schmidt, PhD, RN, CNE, ANEF, FAAN Pao-Feng Tsai , PhD, RN Christina Pettey, PhD, RN, APRN, FNP-BC Patricia Kittle, RN, BSN, MN Deborah Krueger, MSN, RN, NE-BC, CHTP Patricia Schafer, RN, PhD Dona Dorman, MNSc, RN, RNP Sandra R. Brown, MNSc, APRN, WHNP-BC Donna Gullette, PhD, RN, APRN, AGACNP Sara Jones, PhD, RN, APRN, PMHNP-BC Elizabeth Riley, MNSc, RNC-NIC Seongkum Heo, PhD, RN Heba Sadaka, MSN, RN, CNE Tamisha Henderson, MSN, RN, CCM, MHA Janet Smith, MNSc, RN Tammy Webb, MSN, RN, NE-BC Karen Davis, DNP, RN, CNE Teresa Whited, MS, RN, APRN, CPNP-PC Kelly Betts, Ed.D, RN Trish, Wright, PhD, RN, MPH Keneshia Bryant, PhD, RN, APRN, FNP-BC Veneine Cuningkin, DNP, RN Lana Brown, PhD, RN, NEA-BC 7 Nursing Research Conference 2015 MODERATORS Name Name Alexa Bessette Laura Mayfield Amy Funderburk Leonie DeClerk Ann Cato Marlene Walden Ayasha Thomason Melodee Harris Cheryl Schmidt Neena Grissom Claudia Beverly Shelia Sullivan Debra Jeffs Sherri Graves Fermin Renteria Teresa Whited Heba Sadaka Tina Pettey Karen Davis Veneine Cunningkin Keneshia Bryant 8 Nursing Research Conference 2015 VOLUNTEERS Name Name Heather Alverson Laila Litonjua Becca Austin Sherry Oldner Alexa Bessette Marie Patterson Gina Boshears Edna Rogers Erin Bush Cassandra Ruddy Latisha Davis Anita Sanders Paisley Dixon Rebekah Thacker Natalie Dumont Medea Thomas Lisa Ferris Sheila Thomas Heather Heister Cheryl Washington Amy Hester Beth Ann West Deborah Johnson Betsy Wieland Latasha Johnson 9 KEYNOTE SPEAKER Impact of Diversity in Research Norma Martínez Rogers, PhD, RN, FAAN Professor, University of Texas Health Science Center, San Antonio, TX Dr. Martínez Rogers spent the early years of her life in public housing, Dr. Norma Martinez Rogers has spent her life in service to the community, first as a teacher in the Edgewood Independent School District and a Caseworker for San Antonio’s Catholic Family and Children services, before embarking on a career in nursing education. She has served the needs of the San Antonio population as a nurse, a nurse educator, an advocate for the underserved population, and an advocate for health policy changes in regards to healthcare. She has a PHD in “Cultural Foundations” from the University of Texas at Austin and subsequently earned two postdoctoral fellowships at the Indiana University School of Nursing. In 1996 she joined the graduate faculty of the UT Health Science Center’s School of Nursing, where she currently serves as a Professor. Dr. Martinez Rogers co-founded a non- profit organization, Martinez Street Women’s Center whose primary purpose is to provide support and educational services to women and female adolescents. At the University of Texas Health Science Center she founded “Juntos Podemos”, a mentorship program for students who are at risk to not be successful academically. This program began with a $5,000 stipend has been funded by Health Resources Service Administration for the past 14 years. Dr. Martinez Rogers partnered with the US Western District Court Probation Office to provide a female specific program for women convicted of a federal felon and under community supervision. She began this program to prevent relapse/recidivism. It was the only female group in the Western District Court. In November, 2006 she was selected to be a Fellow in the American Academy of Nursing (FAAN) which is the highest honor one can achieve in nursing. You have to be nominated by two members of the Academy and then selected by the board of the American Academy of Nursing. Dr. Martinez Rogers is one of a few Hispanic nurses who are fellows in the Academy and there are approximately 1500 FAAN’s out of 2.9 million nurses in the US. She is past President of the National Association of Hispanic Nurses (NAHN). After a rigorous selection process she was appointed by the U.S. Government Accountability Office to be a member of the Medicaid and CHIP Payment and Access Commission (MACPAC) which will examine how Medicaid physician pay affects access to care by Medicaid patients and those in the Children's Health Insurance Program, among other issues. She recently founded the International Association Latino Nurse Faculty. 10 KEYNOTE SPEAKER Interprofessional Education Lee Wilbur, MD, FAAEM Professor and Vice Chair, Department of Emergency Medicine, Director, Interprofessional Education UAMS College of Medicine Dr. Lee Wilbur (Lee) is the Vice Chair for the Department of Emergency Medicine and as the Director of Interprofessional Education within the UAMS Office of Academic Affairs. Lee and his wife are originally from Kansas where they both attended Kansas State University. Lee received his medical degree from the University of Kansas School of Medicine in 2000, completed a surgical internship at St. Joseph’s Hospital in Denver (2001), and finished his residency as a chief resident at Denver Health Medical Center in 2004. Following residency, he joined the faculty at Indiana University as an Assistant Professor of Clinical Emergency Medicine. His scholarship interests began with a passion for medical education and service based initiatives to serve vulnerable populations. He served as the Assistant/ Associate Program Director for the IU Emergency Medicine residency until 2013. During his tenure as APD, he created innovative curricula, obtained extramural funding, and produced consistent scholarship across a broad range of topics to include: Interpersonal Violence, Sexual Assault, HIV testing, Geriatric Emergency Medicine, and High Fidelity Simulation. In 2010, Lee was promoted to the rank of Associate Professor of Clinical Emergency Medicine. Following this promotion, he was recruited to lead various undergraduate health professions efforts which included the Interprofessional Education (IPE) Curricular Reform Initiative at IU. He has consistently collaborated throughout his career on the local, regional, National, and International level to further develop an expertise in IPE and collaborative practice. As the Director of Interprofessional Education at UAMS, Lee works closely with the Executive leadership, clinical faculty, and students of all the health related schools at UAMS to improve the care, improve the health, and decrease the cost of healthcare for the patients we serve through the UAMS system. The vision for IPE at UAMS is to be recognized as a National model for innovation, creativity, and expertise. While it may seem that Lee may work too much…he actually avoids work as much as possible! His true passions are his faith and family. He works hard to spend time with what he truly loves…his wife, daughter, and son. As a family, the Wilbur’s like to travel, explore the outdoors, and cheer on their KSU Wildcats. He is very proud to call Little Rock home and is open to talk to anyone and everybody that may be interested in UAMS to let them know the exceptional level of care and education we provide daily. 11 Nursing Research Conference 2015 Friday, April 24, 2015 TIME 7:30 – 8:15AM 8:15 – 8:30AM 8:30 – 9:30AM 9:30 – 9:45AM 9:45 – 11:00AM Breakout Session I: Room IDW 104 Tobacco Cessation in Older Adults: The Patient Perspective Lana Brown, PhD, RN, NEA-B Moderator: Keneshia Bryant E-cigarettes and Pregnancy Nicole Ward, MSN, APRN, FNP-BC Moderator: Fermin Renteria 11:00 – 11:30AM 11:30 – 12:30PM TOPIC Registration and Continental Breakfast Welcome/Introductions/Building Orientation Keynote Address: Impact of Diversity in Research Keynote Speaker: Norma Martínez Rogers, PhD, RN, FAAN Moderator: Tina Pettey Break BREAKOUT SESSIONS I Breakout Session II: Room IDW 114 Breakout Session III: Room IDW 115 Breakout Session IV: Room IDW 126 Breakout Session V: Room IDW 226 Increasing Hepatitis C Screening Rates by Screening CDC Recommended Birth Cohorts Prior to Endoscopy Lynn Frazier, MSNc, APRN, CNP-BC, ACNP Application of Diffusion of Innovation Theory to Increase APRN Adoption of Arkansas’ Prescription Monitoring Program Elizabeth Jarvis, MSN, CNS-C The Association of Sleep Disturbance, Depression, and Prodromal Symptoms of Coronary Heart Disease in Women Christina Pettey, PhD, APRN Incorporating the Electronic Medical Record into Nursing Curriculum Carolyn Morrisey, DNP, RN, CCRN Moderator: Ann Cato Moderator: Marlene Walden Moderator: Cheryl Schmidt Moderator: Claudia Beverly Systematic Review of the Impact of Glucose Control on Infections Following Cardiac Surgery Cassidy Estes, MSN, APRN, FNP-BC Inclusion of APRNs as Part of an Interprofessional Rapid Response Team: A Business Case Analysis Mark Tanner, MNSc, RN Feasibility & Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology & Psychosocial Support in Patients with Heart Failure: A pilot study Seongkum Heo , PhD, RN Knowledge & Training During the Medication Administration Process Kelly Betts, Ed.D, RN Nursing Students’ Moderator: Laura Mayfield Moderator: Sherri Graves Moderator: Leonie DeClerk Moderator: Ayasha Thomason nd Poster Session I: Rooms IDW 105 & 106; Student Posters - 2 floor Moderators: 1st floor-Melodee Harris 2nd floor- Teresa Whited Lunch (provided for all pre-registrants. Refer to color on name badge.) 12 12:30 – 1:00PM 1:00 – 1:15PM 1:15 – 2:15PM 2:15 – 2:30PM 2:30 – 3:45PM Breakout Session I: Room IDW 104 Perceived Need for HIV Testing among Rural & Urban African American Cocaine Users Trish Wright, PhD, MPH, RN Moderator: Neena Grissom Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions Pamela Williams, PhD, JD, RN Poster Session II: Rooms IDW 105 & 106; Student Posters- 2nd floor Moderators: 1st floor- Karen Davis 2nd floor- Amy Funderburk Break Keynote Address: Interprofessional Education Keynote speaker: Lee Wilbur, MD, FAAEM Moderator: Tina Pettey Break BREAKOUT SESSIONS II Breakout Session II: Room IDW 114 The Impact of School Based Health Centers on Absenteeism in Rural Middle School Students Gianna M. Grant, MNSC, APRN, GNP-C, FNP-C Breakout Session III: Room IDW 115 Secondhand Smoke & Allelic Variances on Codon 98 as Risk Factors for Cervical Cancer Ayasha Thomason, MNSc, APRN, WHNP-BC, PhD(c) & Natalie Capps, MNSc, RN Moderator: Debra Jeffs Moderator: Alexa Bessette Nurses Educating to Help Save Lives: A Red Cross Program to Increase Blood Donations Cheryl K. Schmidt, PhD, RN, CNE, ANEF, FAAN Eye Drops & Adverse Events after Eye Examinations for Retinopathy of Prematurity Anita Mitchell, PhD, APRN & Howard Hendrickson, PhD Breakout Session IV: Room IDW 126 Breakout Session V: Room IDW 226 The Effects of Shared Medical Appointments on Managing Hypertension in the Veteran Population Telischa Lewis, APRN, FNP-C A Decade of Change: Nurse Practitioners in the Southern United States Thomas Kippenbrock, EdD, RN Moderator: Marlene Walden Moderator: Heba Sadaka Improving Adherence to ADA/APA Guideline Recommendations for Metabolic Monitoring: An Outpatient Quality Improvement Initiative Michele Reynolds, MNSc, APRN-BC, PMHNP-BC Adherence to Prostate Cancer Screening Recommendations after a Community/Internet- based Educational Program Jody A Purifoy, APRN, CNP Moderator: Shelia Sullivan Moderator: Sherri Graves 3:45 – 4:30PM Awards, Submit Evaluations, Pick Up Contact Hours Certificates, Door Prizes! Moderator: Ann Cato 13 Moderator: Veneine Cuningkin Moderator: Heba Sadaka Poster Session I (11:00AM-11:30AM) 14 POSTER SESSION I (11:00AM-11:30AM) ROOM 105 ( I. Dodd Wilson Education Building, First Floor) Affiliation Abstract # Title 003 Relationship between nurse demographics, employee separation and unit assignment in an acute psychiatric hospital. 004 Preventing Central-Line Associated Bloodstream Infections in the Pennington, Tina NICU: Are We Up to Date? UAMS 007 Registered nurse and unlicensed assistive personnel perceptions Sisoukrath, Kaylee on barriers to communication and teamwork: A pilot study UAMS 008 Preventing Needle Stick Injuries with new generation safety device technology: Can your device be safer? Arkansas Children's Hospital 009 Perspectives About Cyclic Vomiting Syndrome: Adult Explanatory Jensen, Ashley Models 012 Primary Author Aromatherapy for Stress Reduction: A Strategy for Self-Care *Leave posters in place until 2:15pm 15 Cuningkin, Veneine Allen, Amy Stroman, Sheila UAMS UAMS UAMS POSTER SESSION I (11:00AM-11:30AM) ROOM 106 ( I. Dodd Wilson Education Building, First Floor) Title Abstract # 013 015 017 018 021 022 Affiliation Primary Author Effects of a 12 Week Maternal CPR Practice Program on Nursing Student Performance Recall Haley, Brandy Predictors of Substance Use Recidivism in Arkansas Nurses Powers, Cynthia Symptom Onset to Arterial Reperfusion (SOAR) Research Study Meiklejohn, Deborah Tracing Zeroes for Our Heroes Hill, Edward Lee Delirium in Acutely Ill Elders: The Role of Nurses Bryant, Jody A Sweet Lesson in Research Cockerham, Jennifer *Leave posters in place until 2:15pm 16 UAMS Union University Jackson, TN St. Vincent Hospital Central Arkansas Veterans Healthcare System Central Arkansas Veterans Healthcare System POSTER SESSION I (11:00AM-11:30AM) 2nd Floor: Poster Area 1 ( I. Dodd Wilson Education Building, Second Floor) Title 044 Perceived Health Status and Self-Efficacy of Adult Survivors of Pediatric Orthotopic Heart Transplant: Pilot Study Hays, Laura UAMS, CON 045 Improving Infection Control Practices in a Long Term Care Facility through a Quality Improvement Project Lingo, Joshuah UAMS, CON 046 A Qualitative Pilot Study: Nursing Workplace Environment and Nurses’ Perspectives on Patient Outcomes Davidson, Elizabeth Sloan UAMS, CON 047 Identifying Gaps between Resources and Parents with Children Diagnosed with Autism-A Pilot Study Richardson, Leah UAMS, CON 048 Content Validity Methods Applied to New Psychosocial Scale for Dumont, Natalie Social Burden in Rare Genetic Conditions UAMS, CON 049 Older Adults Who Exercise Display Lower Temporal Discounting Tate, Linda Rates Than Non- Exercisers UAMS, CON 050 Adverse Events and Retinopathy of Prematurity Eye Exams Orahood, Jennifer UAMS, CON 051 Development of a fall injury prediction model Hester, Amy UAMS, CON Family Coping after a Child's Traumatic Brain Injury Huett, Amy UAMS, CON 053 Psychological Differences in Adolescents Who Sexually Offend with a History of Childhood Sexual Abuse Bean, Sarah UAMS, CON 054 Benzodiazepines as an effective first-line treatment for insomnia in older adults Robinson, Sundra Henderson State University 055 How Nurse’s Instructions Affect Patient Understand of NPO Worsham, Alexis Henderson State University 052 Primary Author Affiliation Abstract # 17 056 Fibromyalgia Syndrome and Hydrotherapy Howell, Amy UAMS, CON 057 Factors Related to Early Breastfeeding Cessation Taylor, Shannon University of Arkansas at Monticello 058 Strategies to Prevent Medication Errors Lawson, Allisa University of Arkansas at Monticello *Leave posters in place until 2:15pm 18 POSTER SESSION I (11:00AM-11:30AM) 2nd Floor: Poster Area 2 ( I. Dodd Wilson Education Building, Second Floor) Title Abstract # Primary Author Affiliation 059 How Various Sexual Education Programs Influence Adolescents’ Risky Sexual Behavior Morris, Leanna University of Arkansas at Monticello 060 Effects of Chlorhexidine Gluconate Bathing on MRSA Colonization and Infection Rates in Inpatient Populations Burton, Haley UAMS, CON 061 Effects of E-Cigarettes in Smoking Cessation Onecic, Mara UAMS, CON 062 Effects of Interventions on Depression in Caregivers Who Take Care of Alzheimer’s or Dementia Patients Allard, Julie UAMS, CON 063 It’s a Small World: Providing Culturally Competent Care Funderburk, Amy UAMS, CON 064 Electronic Cigarettes- Awareness, Perception, and Education Willard, Mary J. UAMS, CHI St. Vincent Infirmary 065 Washington County Arkansas’ progress toward accomplishing Healthy Jones, James People 2020 objective MHMD-8 UAMS, CON 066 The Effect of Oral Care on the Incidence of Ventilator-Associated Pneumonia Jones, Katlin UAMS, CON Wilson, Katrena UAMS, CON McDowell, Karen UAMS, CON 067 068 The Use of Dexmedetomidine in Post-Operative Heart Surgery Patients for Decreasing Length of Stay and Post-Operative Complications Bloodstream Infection Reduction: Utilizing Alcohol-Impregnated Caps in Patients with Central-Lines 069 Assistive devices and rehabilitation in the older adult with visual impairment: Literature review Childs, Casey Southern Arkansas University 070 Falls in the Older Adult Hensley, Adam Southern Arkansas University 071 Caring for the Caregiver Vann, Abigail Southern Arkansas University 072 Elder Mistreatment Assessment Davis, Dana Southern Arkansas University 073 The Causes and Challenges Associated with Elderly Homelessness Clinton, Laura Southern Arkansas University 19 Poster Session II (12:30PM-1:00PM) 20 POSTER SESSION 2 (12:30PM-1:00PM) ROOM 105 ( I. Dodd Wilson Education Building, First Floor) Title Abstract # Affiliation Primary Author 023 Reducing Heart Failure Readmissions Huff, Jennifer St Vincent Infirmary Medical Center 024 One Stick Too Many: Reducing PIV Sticks and Infiltrates in Pediatric Patients Janisko, Jennifer St Vincent Infirmary Medical Center 028 Don't Leave It To Chance… give breast milk a second glance! Shelton, Kristina Arkansas Children's Hospital 029 Fall Prevention: A Concept Analysis Urban, Kelly UAMS 037 Decreasing Length of Stay in Veterans undergoing a Primary Total Joint Procedure with the Total Joint Academy PreOperative Educational Class Effrein, Rebecca Central Arkansas Veterans Healthcare System 038 Diversional Activities to Decrease Harmful Behavior in Patients with Dementia Lyle, Rebecca Central Arkansas Veterans Healthcare System *Leave posters in place until 2:15pm 21 POSTER SESSION 2 (12:30PM-1:00PM) ROOM 106 ( I. Dodd Wilson Education Building, First Floor) Title Abstract # 039 040 Affiliation Primary Author Safe Flow Rate Nipple Selection for NICU Infants, Post Discharge Use PHASE II Camp, Carol A. UAMS Early Prone Positioning: Why Wait for ARDS? Shelby, Race Central Arkansas Veterans Healthcare System 041 Evaluation of Implementation of an Influenza Cocooning Practice Smith, Rebecca in the NICU for Infant Household Caregivers 042 World Peace and the Standardization of Arterial Lines in a Pediatric Hospital in Arkansas Barron, Sharon Arkansas Children's Hospital 043 Utilization of an interdisciplinary (ID) team to expand programming within an inpatient dual diagnosis program- quality improvement project. Burnett, Stephanie Central Arkansas Veterans Healthcare System *Leave posters in place until 2:15pm 22 POSTER SESSION II (12:30PM-1:00PM) 2nd Floor: Poster Area 1 ( I. Dodd Wilson Education Building, Second Floor) Title Abstract # Primary Author Affiliation Southern Arkansas University 074 Elderly and the Use of Telemedicine Hill, William 075 Sleep Quality of the Older Adult using the Pittsburg Sleep Quality Index and Epworth Raney, Kari 076 Fatigue and the Elderly: Expected versus Unexpected Prakriti, K. C. 077 Prevention of Rehospitalizations in Older Adults LaBorde, Samantha 078 Visitor effects on intracranial pressure of traumatic brain activity of traumatic brain injury patients Decker, Sadie Henderson State University 079 Exercise in the Elderly Alfaro, Berenice Southern Arkansas University 080 Using the Beers Criteria for Potentially Inappropriate Medication use in the elderly Moore, Rebecca Southern Arkansas University 081 Controversial Aging Theories Price, Ashley Southern Arkansas University 082 Older Adult Suicide Prevention Driggers, Laura Southern Arkansas University 083 Receipt of Immunizations in the Older Adult Terry, Lauren Southern Arkansas University 084 Importance of Assessing and Managing Delirium Patients Andrews, Lacey Southern Arkansas University 085 The Effect of Baby Boomers on the Healthcare System Geesing, Courtney Southern Arkansas University 23 Southern Arkansas University Southern Arkansas University Southern Arkansas University 086 Functional Decline in Older Adults: Assessment tools Saulsbury, Morgan 087 Muscle Wasting in Elderly Women Coleman, Shelley 088 Effects of Advanced Directives on Patient Care Curtis, Jessica *Leave posters in place until 2:15pm 24 Southern Arkansas University Southern Arkansas University Southern Arkansas University POSTER SESSION II (12:30PM-1:00PM) 2nd Floor: Poster Area 1 ( I. Dodd Wilson Education Building, Second Floor) Title Abstract # Primary Author Affiliation 089 Effects of Education and Attitudes Parents have Regarding Immunizing their Children Grubbs, Gary Henderson State University 090 Loneliness and the Older Adult-Effective Strategies of Intervention Martin, Antonia Southern Arkansas University 091 Housing the Elderly Sinclair, Morgan 092 Telemedicine and the Older Adult Litton, Brandy Southern Arkansas UniversityArkansas Southern 093 Identifying Intensive Care Unit Patients at Risk for Chronic Posttraumatic Stress Disorder Hines, Briana UAMS, CON Pay for Performance Policy Effect on Primary Care Hypertension Management Effective Interventions to Decrease Childhood Obesity: Parental Role Kitch, Stephanie UAMS, CON Bailey, Jennifer University of Arkansas at Monticello Evidence-Based Nursing Interventions for the Prevention of Ventilator-Associated Pneumonia for Patients in the ICU Romero, Marcos University of Arkansas at Monticello 097 Evidence of the Effectiveness of Assessment tools for Palliative Care in Dementia Gill, Laura University of Arkansas at Monticello 098 Establishing a Motivational Interviewing (MI) Learning Community Brown, Sandra R. Vanderbilt University School of Nursing 099 Perinatal Mortality Rates Compared in Home and Hospital Births Davis, Anna Henderson State University 100 Is the Mini Nutritional Assessment (MNA) Essential for Geriatric Patients as a Preventive Tool? Gulley, Sonya L. Southern Arkansas University 094 095 096 University 25 102 Effective Rehabilitations for Patients with Brain Disorders Sanders, Shelby Southern Arkansas University 103 Restraint Use: The ability to do without Walker, Angela Southern Arkansas University 104 Cultural Adaptation of an Evidence-Based Depression Intervention Loyd, Caroline for the African *Leave posters in place until 2:15pm American Faith Based Based Communities In the Rural Arkansas Delta 26 UAMS, CON Abstract # 001 Title: Systematic Review of the Impact of Glucose Control on Infections Following Cardiac Surgery Authors & Affiliations: Cassidy Estes, MSN, APRN, FNP-BC, Cathrin Carithers, DNP, APRN, FNP-C, Susan Steelman, MLIS, Christina Pettey, PhD, APRN, FNP-BC; University of Arkansas for Medical Sciences Significance: Significance: The Center for Disease Control and Prevention National Vital Statistics Report (2013), identified coronary artery disease (CAD) as the leading cause of death in the United States (US) in 2010. This statistic accounted for 24% of all deaths reported in the US for 2010 (Murphy, 2013). Diabetes Mellitus is a known risk factor for CAD as well as a significant contributor to postsurgical complications in cardiac surgery. Purpose (or Problem): Purpose: A systematic review was conducted using primary source research to identify the optimal blood glucose levels to reduce the incidence of infection in adult patients who have undergone cardiac surgery. PICO Question: PICOT: What is the ideal post-operative blood glucose range to reduce the incidence of post-operative infections in cardiac surgery patients? Search Strategy & Screening: Search Strategy & Screening: An extensive literature review was conducted using OVID to search: The Cochrane Library, MEDLINE, MEDLINE In-process, and IPA. EBSCO was utilized to search CINAHLPlus and Health Source Nursing and Academics. Grey literature sources included The New York Academy of Medicine and Clinicaltrials.gov. Web of Science and the UAMS library catalogue were also searched. The following MeSH terms were used in the search: “cardiac”, “cardiac surgery”, “coronary artery bypass”, “endocarditis”, cardiovascular surgical procedures”, “surgical wound”, “infection”, “diabetes mellitus”, “hyperglycemia”, “insulin”, and “post-operative complications”. The search included all data from 2004, to current to cover a 10 year search history. The articles were screened for relevance and those that were not adult cardiac surgery were excluded. Included were all RCTs, quasi-experimental, and comparative trials that met the inclusion and exclusion criteria. Evidence: Six articles were selected for inclusion in the review; three RCTs, one quasi- experimental, and two comparison studies. Only one study that compared intravenous (IV) insulin to subcutaneous (SC) sliding scale insulin (SSI) post-operatively identified a significant difference in infection rates. Synthesis of Evidence: .Researchers reported the IV insulin was superior to the SSI in reducing infections rates. The remaining five articles reported that glucose levels maintained ≤200mg/dl reduced the incidence of post-operative adult cardiac surgery infections. Conclusions: Maintaining blood glucose levels ≤200mg/dl can reduce the incidence of post- operative infections in adult cardiac surgery patients. There is insufficient data to recommend more aggressive control at levels ≤ 200mg/dl. Establishing a standardized glucose range to be used in research studies will allow for comparison of data across studies to determine if there is benefit to more aggressive glucose control. Implications for Nursing Practice: Implications for Nursing Practice: Management of optimal blood glucose levels by APRNs in persons who have undergone cardiac surgery can reduce the risk of infection leading to a reduction in length of stay, overall hospital cost and improved patient/family outcomes. 27 Abstract #002 Title: A Decade of Change: Nurse Practitioners in the Southern United States Authors & Affiliations: Wne-Juo Lo, PhD, University of Arkansas; Ellen Odell, DNP, RN, John Brown University; Bill Buron, PhD, APRN, FNP/GNP-BC, UAMS Background & Significance: Collectively, the U.S. Southern states are some of the poorest, most rural, and socioeconomically deprived regions in the county. Related to these conditions are the poor healthcare outcomes such as higher morbidities, shorter life spans, and higher death rates. The South is home of many rural citizens and medically underserved areas. Despite national databases affiliated with the Bureau of Labor Statistics and the Health Resources and Services Administration (HRSA), knowledge is limited regarding the nurse practitioner (NP) workforce in rural and medically underserved areas of the country. Purpose: The aim of this research is to gain a better understanding of the characteristics of NPs working in the Southern U. S. More specifically, the objectives are to examine and compare the demographic and descriptive characteristics (gender, race, income, practice specialty, and employer type) of NPs working in (a) health professional shortage areas (HPSA) versus non HPSA; and (b) rural versus urban areas during the past decade. Methods: A non-experimental quantitative methodology employing three data collection sources was used in the study. Over 1,500 NPs were surveyed both in 2000 and 2010 for demographics and descriptive information such as education, income, practice, employer, and workload. Other data sources included Health Resources and Services Administration that identified HPSAs and the U.S. Census Bureau used to distinguish urban and rural employment settings. Results: The most dramatic shifts in NPs were older, more educated, and earned higher incomes; however, gender and race remained the same over the past decade. Hospital employment was the largest increase and the greatest decline was private practice settings. Family practice as a specialty increased slightly while no shift occurred in other specialties. More NPs worked in HPSAs; however, rural located employment declined. Conclusions: Despite three decades of attempting to diversify nursing student enrollment and increase the graduates of NP educational programs; racial diversity was almost non-existent within the NP population over the past decade. The small minority of NP participants in this study is far below the number of Blacks and Hispanics living in the region as reported by the U.S. Census Bureau (Humos, Jones, & Ramirez, 2011; Rastogi, Johnson, Hoeffel, & Drewery, 2011; Ennis, RiosVargus, & Albert, 2011). There is evidence that provider-patient race concordance improves not only patient satisfaction but improves healthcare utilization and outcomes as well (Gornick, Eggers, Reilly, Mentnech, Fitterman, Kucken, Vladeck, 1996; Laviest & Nuru-Jeter, 2002, Laviest, Nuru-Jeter, & Jones, 2003). This evidence supports the need for continued efforts to increase the number of minority NP providers. Implications for Nursing Practice: The U. S. continues to face a serious shortage of primary care clinicians at a time when demands for health care services are expected to rise, particularly in rural and underserved areas. NPs as primary care providers, if allowed to practice to the full extent of their licensure, could impact health care outcomes for Southern citizens. The National Center for Workforce Analysis (2013) projected a national primary care provider shortage of 6,400 FTE in 2020. Compared to the length and cost of physician education, the mobilization of a new NPs can occur more quickly at a relatively lower cost. In addition, NP education and practice typically builds on the expertise and experiences of seasoned registered nurses, who often represent a wide array of ethnic and cultural backgrounds. A renewed emphasis on educating more NPs to meet growing primary care demands would likely improve the diversity of healthcare providers. Furthermore, greater support for NP residencies (as encouraged in the IOM [2010] report) focused on rural and underserved areas may actually lead to improved care at a lower cost among these highly underserved and vulnerable populations. 28 Abstract #003 Title: Relationship between nurse demographics, employee separation and unit assignment in an acute psychiatric hospital. Authors & Affiliations: Veneine Cuningkin, DNP, RN, Denise Thornton-Orr, DNSc, RN, NEA- BC, Faculty Advisor Background & Significance: A state run psychiatric facility experiencing 41% turnover for Registered Nurses(RN) and 68% turnover among Licensed Practical Nurses (LPN). Nursing turnover is a global issue. In healthcare, managing turnover is critical to delivering high quality patient care (Bae, Mark, & Fried, 2010). One of the foundational principles in mental health nursing is building therapeutic relationship; this relationship will not exist without securing and maintaining highly qualified nursing staff. This therapeutic relationship is threatened in a milieu where the instability of staff is prominent. A high nursing turnover is incompatible with creating a safe and therapeutic milieu. Purpose: The purpose of this study is to examine nursing personnel demographics and explore unit specific factors attributing to nursing turnover in state run psychiatric care facilities to assist in the development of future retention strategies. Methods: Descriptive statistics were computed from the demographic data (age, length of employment, prior psychiatric experience, involuntary or voluntary separation, unit assignment, gender, employment status and educational level) over a two year period. A retrospective correlational study design was utilized to examine and /or predict relationships among demographic variables. Results: The statistical significance results determined prior psychiatric experience fostered longer employment than those nurses who had no prior psychiatric experience. Additional significance insisted full time employees tended to stay employed longer (41 months, on average) than part-time employees (11 months, on average). Conclusions: Measures need to be explored to minimize the effects of nursing turnover. The overall length of employment was 32 1/3 months of the 115 licensed employees who separated in a two year time frame. Ninety percent of nursing staff voluntarily separated the psychiatric facility. The average age was 43 years old, 82% female (stayed longer) and 18% male.Unit assignment and educational level demonstrated no statistical significance. Implications for Nursing Practice: Further deliberations should be given to the development of strategies to enhance recruitment and retention of nursing personnel. Improved patient outcomes, financial benefits, and the construction of a therapeutic environment can be established secondary to a reduction in nursing turnover. 29 Abstract #004 Title: Preventing Central-Line Associated Bloodstream Infections in the NICU: Are We Up to Date? Authors & Affiliations: Tina Pennington, BSN, RNC-NIC Significance: Central venous catheters (CVC) are an integral part of the medical management of the hospitalized neonate, but as such, put the neonate at risk for a central-line bloodstream infection (CLABSI). CLABSI’s have not only detrimental mortality/morbidity issues for the neonate but also an economic impact on the family and the healthcare system. Purpose (or Problem): The objective of this literature review is to determine if the NICU at the University of Arkansas for Medical Sciences is doing all that it can do to prevent Central-line bloodstream infections in neonates. PICO Question: Are the central venous catheter insertion and maintenance procedures (I) in the NICU at the University of Arkansas for Medical Sciences (P) in line with the current recommendations for best practice standards (C) in preventing central-line bloodstream inf Search Strategy & Screening: Utilizing the General Systems Theory we formulated a framework for identifying entrance opportunities for the infection (inputs), assess and compare current practice to recommended preventative measures, or changes in our practice (throughputs) needed to prevent any further incidences (outputs), and data collection (feedback) to monitor our compliance. Evidence: The Joint Commission and the Centers for Disease Control has issued guidelines for reducing/eliminating CLABSIs. They recommend strict hand hygiene, barriers, a dedicated group of trained professionals to place and maintain the lines, longer fluid expiration times, and the bundling of steps when accessing ports or changing fluids. Synthesis of Evidence: Review of the literature evidenced current recommended best practices for the prevention of CLABSI. The application of systems thinking to the UAMS PICC practice revealed compliance with most CDC and IHI recommendations for CLABSI prevention in our NICU. We currently have different time frames for fluid changes than recommended and non-standardized use of barriers for other persons in the room besides the person placing the PICC. Conclusions: Review of the literature is a critical step in identifying current evidence based practices. Using findings from our review provided a foundation for evaluation and gap analysis of current practice using General Systems Theory. This approach has led to evidence based practice changes in the NICU that bring us into compliance with current standards Implications for Nursing Practice: Nurses are directly responsible for most placements, and for all maintenance and care of PICCs in our unit, and as such understanding the importance of adherence to our evidencebased practice is paramount in preventing CLABSI outbreaks. Revisiting the literature to evaluate changes in evidence and recommendations for care is an essential process for ensuring our care is congruent with current standards. 30 Abstract #005 Title: The Effects of Shared Medical Appointments on Managing Hypertension in the Veteran Population Authors & Affiliations: Telischa D. Lewis, MSN, APRN, FNP-C; Cathrin Carithers, DNP, APRN, FNP-C Problem & Purpose: Uncontrolled hypertension (HTN) can lead to heart disease, stroke and kidney failure; yet, only about half of those diagnosed are in good control. HTN cost our nation $47.5 billion annually in direct cost (CDC, 2011, p.1). With the increasing number of patients with chronic illnesses such as HTN, and a shortage of healthcare providers, other strategies to deliver effective care require exploration. The purpose of this evidence-based quality improvement project was to test the effectiveness of shared medical appointments (SMAs) for veterans with uncontrolled HTN for the development of the requisite knowledge and skills for optimal HTN management. PICO Question: Are shared medical appointments an effective method for the development of the knowledge and skills for managing hypertension in the Veteran population? Evidence-based practice models & process: The conceptual model used for this project was the Wagner’s Chronic Care Model Relevant Literature: Current provider-patient structured medical visits are ineffective in the management of patients with chronic disease such as HTN. Time limitations imposed on provider appointments encumbers the amount of patient and family education able to be provided to facilitate recommended behavior changes that lead to improved blood pressure control. Evidence supports the effectiveness of SMAs in the improvement of clinical disease- specific outcomes, while seeing more patients at one visit (Loney-Hutchinson et al., 2009) and can improve provider productivity, reduce hospitalizations and improve health behavior (Loney- Hutchinson et al., 2009; Edelman et al., 2012; Clancy, 2007; Housden, Wong, & Martin, 2013). Methods: This project was conducted at a VA clinic in Arkansas and employed a pretest- posttest interventional approach. Two groups made up of a convenience sample of veterans with uncontrolled HTN and a commitment of participation to monthly SMAs for three consecutive months were recruited. To evaluate the effectiveness of SMAs on Veteran participants’ HTN knowledge and management, the HTN of lifestyle and management (HELM) scale were used. Blood pressure readings were also measured at each visit. The SMA healthcare team consisted of an APRN, RN, LPN, dietitian and pharmacist. Outcomes: Out of 23 participants, 14 (60%) completed all three SMAs. The first group had 13 participants with a completion of 10 and the second group started with 10 participants with a completion of four. The Wilcoxon Signed Rank Test revealed a statistically significant improvement in pretest-posttest HTN evaluation of lifestyle and management (HELM) scores following participation in the SMA. The mean score of the HELM improved from pretest mean score 66.5 (SD = 15) to posttest 74.5 (SD = 10.1). There were statistically significant improvements in systolic blood pressure readings among veterans with SMA intervention, however changes in diastolic blood pressure readings were not statistically significant. At SMA three, the mean systolic blood pressure improved to 135.50 mmHg (SD = 11.36) p <.005 with the diastolic mean of 75.57 mmHg (10.54) p<.100. Conclusions: Participation in SMAs in this Veteran population revealed significant improvement in systolic blood pressure readings and enhanced knowledge and skills regarding HTN. VAs should incorporate SMAs that focus on HTN management. Further studies with a larger sample size are needed to verify significance and enhance generalizability. Implications for Nursing Practice: Nurses and APRNs can play an integral role in helping to facilitate recommended behavior change, improve care delivery and patient outcomes by leading an interprofessional team in the incorporation of SMAs into their practice. 31 Abstract #006 Title: Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study Authors & Affiliations: Seongkum Heo, PhD, RN, Assistant Professor, UAMS, College of Nursing; Jean McSweeney, PhD, RN, Professor and Associate Dean for Research, UAMS, CON; Elaine T. Prewitt, DrPh, Associate Professor, UAMS, College of Public Health; Jeannette Y. Lee, PhD, Professor, UAMS, College of Public Health; Debra K. Moser, DNSc, RN, Professor and Gill Chair of Nursing, University of Kentucky, College of Nursing; Allison Shaw-Devine, MD, Assistant Professor, UAMS, College of Medicine; Audrey Fier, RN, UAMS Background & Significance: Patients with heart failure (HF) have poor dietary sodium adherence, and this is an important factor in worsening of HF symptoms, which, in turn, is associated with poor health-related quality of life (HRQOL). Purpose: This pilot study examined the feasibility and acceptability of a tailored dietary sodium intervention combined with technology (MyFitnessPal) and psychosocial support, and examined intervention effects on HF symptoms, HRQOL, and factors affecting dietary sodium adherence. Methods: A 6 session tailored dietary intervention based on baseline sodium intake (24-hour urine) and eating habits (MyFitnessPal) and on factors affecting dietary adherence was delivered to 11 patients with HF (mean age 53 ± 14 years, 82% female). Data on dietary sodium intake (24-hour urine), HF symptoms, HRQOL, and factors affecting dietary sodium adherence (knowledge, skills, experience, confidence, perceived benefits and barriers, social support, and depressive symptoms) were collected at baseline and 3 month followup. Paired t-tests and McNemar test were used to analyze the data. Results: The 11 patients completed 65 of 66 intervention sessions. The mean satisfactory (acceptability) scores for Sessions ranged from 98% to 100%. Sodium intake (24-hour urine) was reduced (3.9 to 2.6 g per day, p = .034), and HF symptoms (46.5 to 26.7, p = .001) and QOL (68.0 to 40.0, p = .001) were improved. Factors affecting dietary adherence, including skills (p < .001), experience (p < .001), confidence (p = .001), perceived benefits and barriers (p = .027), social support (p = .033), and depressive symptoms (p = .004) were also improved. Conclusions: A tailored dietary intervention combined with technology and psychosocial support was feasible and acceptable and showed promising results in reducing dietary sodium intake and improving factors affecting dietary sodium intake, physical and depressive symptoms, HRQOL. Implications for Nursing Practice: Clinicians who take care of patients with heart failure can provide and test this intervention to patients with HF to improve dietary sodium adherence, and, in turn, HF symptoms and HRQOL. 32 Abstract #007 Title: Registered nurse and unlicensed assistive personnel perceptions on barriers to communication and teamwork: A pilot study Authors & Affiliations: Sarah France, BSN, RN and Kaylee Sisoukrath, BSN, RN; University of Arkansas for Medical Sciences Background & Significance: Patient care is dependent on the coordinated effort of registered nurses (RNs) and unlicensed assistive personnel (UAP) participating in teamwork and effective communication. Failure to communicate effectively and work as team could potentially have negative effects on task completion, job performance, and patient care. Purpose: The purpose of this study was to describe and understand both RN and UAP perceptions of teamwork and communication, to identify existing barriers, and to investigate possible interventions for improvement. Methods: Two surveys were designed to assess perceptions of teamwork and communication among RNs and UAP. These were submitted to the RNs and UAP of a 30 bed trauma/med surg unit. 22 RNs and 10 UAP participated. Consent was verified with participation. Surveys were RN and UAP role specific containing lickert scale questions which addressed effectiveness and value of teamwork and communication, workload, stress/busyness, roles/responsibilities, approachability of team members, how often communication should occur between RNs/UAP and whether race/sex affected communication. Additionally, three open ended questions provided participants the opportunity to express their definition of teamwork, what they believe the others’ responsibilities are, and what they would like the other to understand about their job. Results were compiled and analyzed for trends and insight. Results: RNs and UAP found RN/UAP communication to be “somewhat effective.” RNs expressed that stress/busyness does hinder communication, that their education “somewhat prepared” them for delegation, that their workload was heavier than UAP, that UAP are “somewhat approachable”, and that UAP/RN communication should occur a mininimum of 3-4 times regarding a specific patient during an 8 hour shift. UAP expressed that their workload was heavier than RNs, that RNs are “approachable”, and that communication regarding a specific patient should occur 6 or more times in an 8 hour shift. RNs and UAP agreed that race/sex did not hinder communication, and that teamwork is valuable in providing effective patient care. In the open ended portions, UAP definitions of teamwork included themes of communication, collaboration, and assisting with tasks. RN definitions of teamwork focused on patient care needs/outcomes by working together. UAPs wanted RNs to understand that they felt stretched thin and tasks should be shared. RNs wanted UAP to understand that there is great responsibility/difficulty with their job, that when they are “sitting” they are still working (charting or communicating with physicians), and they are ultimately liable for both UAP and RN tasks. Conclusions: Both RNs and UAP value the importance of teamwork and communication, but feel misunderstood and that they have a heavier workload than the other. This study provides a solid foundation for further exploration into bridging the RN/UAP communication gap and building better teamwork for the sake of excellent patient care. Implications for Nursing Practice: As leaders, RNs can take initiative in creating atmospheres of including, understanding, and valuing UAP, can model frequent and open communication, can educate on roles/responsibilities, and ultimately RNs should continue to investigate and address the barriers to ineffective communication and teamwork. 33 Abstract #008 Title: Preventing Needle Stick Injuries with new generation safety device technology: Can your device be safer? Authors & Affiliations: Amy Allen, BSN, RN, NE-BC, Tammy Webb, MS, RN, NE-BC; Arkansas Children's Hospital Problem & Purpose: The purpose of this evidence based practice project was to reduce needle stick injuries (NSI) in a pediatric hospital setting. Even with needle safety programs in place to protect nurses, significant and preventable needle stick injuries still occurred. PICO Question: Will conversion to a retractable safety needle device reduce the incidence of NSI in nurses in a pediatric hospital setting? Evidence-based practice models & process: Melnyk Fineout-Overholt provided the framework for the evidence based practice model and the process was based on improvement science methodology. Relevant Literature: The project team comprised of an interprofessional hospital committee focused on employee injury prevention reviewed the most current research and evidence based practice (including randomized controlled trials, systematic reviews, and the American Nurses Association needle stick prevention guidelines) to determine the most current technology for safety needle devices. The literature provided information supporting the transition from manual device to retractable or passive to reduce needle stick injuries. The conclusion of the review provided the team with evidence to support the decision making for selection of the new retractable safety needle device. Methods: The project team conducted an analysis of needle stick incidences including the type of device, the clinical area, and the circumstances of the event. It was determined that one of the leading causes for nurse needle stick injuries involved the winged steel needle safety device. Based on the literature review, the team searched the market and discovered a retractable winged steel needle safety device. A one month pilot was conducted in inpatient areas with positive results and feedback from nurses. Upon education, the newly adopted device was implemented in July of 2014. Through ongoing employee injury surveillance, a dramatic reduction was seen in NSI after implementation. Outcomes: Data analysis of needle stick injuries post the conversion to the new safety technology revealed a reduction from 15 (Jan 2013 to June 2014) to 0 (Jul to Dec 2014). Based on this reduction in nurse needle stick injuries, there was a financial cost savings of @ $7500.00 based on an average of $500 per employee needle stick. Conclusions: In order to reduce needle stick injuries, the ultimate goal is to remove the needle from the environment as early as possible to avoid the risk of injury. The project team continues to analyze needle stick data for trends in device associated injury and to research new generation technologies to ensure a safer work environment. Implications for Nursing Practice: Even though hospitals have transitioned to safety needle devices, there are needle stick injuries still occurring. Hospitals must continually evaluate current evidence on needle stick injury prevention and newly available safety device technology to ensure the safest work environment. In addition, the hospital should create a structure to evaluate employee needle stick injury data, newly available safety device products and nurse accountability to properly utilize available safety devices. 34 Abstract #009 Title: Perspectives About Cyclic Vomiting Syndrome: Adult Explanatory Models Authors & Affiliations: Ashley D. Jensen, PhD, RN, University of Arkansas for Medical Sciences Background & Significance: Cyclic vomiting syndrome is a chronic gastrointestinal tract disorder affecting 3% to 14% of patients experiencing unexplained nausea and vomiting who were referred to health centers in the United States. Patients experience frequent cycles of severe nausea, vomiting, and abdominal pain placing them at risk for lifethreatening health complications. These incapacitating episodes impact social, emotional, and physical health, however minimal research has focused on descriptions of illness perception, life impact, and response to treatment. Purpose: This study explored (a) CVS-related health experiences, (b) impact on relationships, employment, education, and leisure time as well as (c) responses to CVS-related treatments. Methods: Purposive sampling was used in this phenomenological study to recruit 16 adults, 21 years or older with a diagnosis of CVS for more than one year. Data were collected electronically via Survey Monkey®. Type-written data was analyzed using content analysis and constant comparison techniques. Demographic data, also collected electronically, was described using Excel. Results: All 16 participants were Caucasian. Eleven were female and five were male. Participants ranged in age from 22 to 59 years at the time of the study. Six participants were classified as having pediatric-onset CVS and 10 were classified as having adult-onset CVS. Seven global themes emerged from the data: (a) perceived causes of cyclic vomiting syndrome, (b) triggers for CVS episodes, (c) onset of illness and symptoms of CVS, (d) understanding the chronic course of CVS, (e) impact on day-to-day life, (f) lack of health care provider knowledge, and (g) responses to CVS-related treatments. Participants discussed limited understanding of illness etiology. However, they revealed understanding CVS as a chronic and cyclic illness. Emphasis was placed on triggers for CVS, life impact, lack of health care provider knowledge leading to diagnostic delay, avoidance of care, and inappropriate treatment. Prophylactic, abortive, and self-management was discussed. Discussions of emotional impact highlight the need for multidisciplinary care to insure that physical as well as mental health issues are considered and addressed. Findings present the need for increased CVS awareness and education to improve health care, access, and quality of care. Conclusions: Using the internet to recruit and collect data allowed the author to learn about adult perceptions, impact and response to CVS-related treatments. The knowledge gained from participants’ points of view provided insight about how adults are managing and coping with CVS as a chronic illness, challenges in life while attempting to access appropriate care, and responses to recommended treatments. Future research should focus on health care provider education and family/caregiver perspectives as well as investigation into strategies designed to meet the unique needs of CVS patients during each phase. Implications for Nursing Practice: By incorporating inquiry related to patient beliefs into the evaluation, practitioners will begin to understand the reality of the lived experience and patients will be more likely to accept and follow treatment recommendations. Health care providers can use the information learned from this study to educate peers and to individualize current treatment plans enhancing timely and proper treatment upon entry to the health care facility which will improve health care access. Findings related to feelings of depression, fear, guilt, and embarrassment present the need for multidisciplinary care to insure physical and mental health issues are addressed. 35 Abstract #010 Title: Eye Drops and Adverse Events after Eye Examinations for Retinopathy of Prematurity Authors & Affiliations: Anita Mitchell PhD, APRN; College of Nursing, UAMS; Howard Hendrickson, PhD, Pharmaceutical Sciences, UAMS; Stephen Erickson PhD, Biostatistics, UAMS; Charlotte Yates PhD, PT, University of Central Arkansas; Richard Whit Hall M.D., UAMS College of Medicine, Neonatology Background & Significance: One common complication of preterm birth is Retinopathy of Prematurity (ROP), a disease of the blood vessels on the retina that can lead to blindness. All preterm infants born at less than 32 weeks gestational age or weighing less than 1500 grams undergo screening exams for ROP, but some experience adverse cardiorespiratory events or feeding intolerance after ROP eye exams. One possible cause for adverse events is systemic absorption of cyclopentolate, a drug found in the Cyclomydril eye drops used to dilate pupils before the exam. Cyclopentolate is an anticholinergic drug that can reduce peristalsis and affect respiratory status and heart rate. Purpose: The purpose of the study was to analyze associations between blood levels of cyclopentolate and adverse events after ROP eye exams in preterm infants. Methods: Phase 1: Researchers developed a method to measure cyclopentolate levels one hour after administration of Cyclomydril using only two drops of blood and analyzing with liquid chromatography and tandem mass spectrometry (LC-MS/MS). Blood was collected during routine lab work after parental consent. Phase 2: Researchers carried out a retrospective chart review of 18 infants involved in the study and used correlation and multivariable logistic regression to analyze relationships among infant characteristics, cyclopentolate levels and adverse events. Results: Detectable blood levels of cyclopentolate were found in 15 out of 18 infants Although all infants had received the same dosage of cyclopentolate, levels of this drug were significantly higher in infants who had respiratory distress and were on oxygen (p=0.014). Although 5 infants required additional oxygen after the exam, there were no statistically significant associations between cyclopentolate levels and cardiorespiratory events. However, there was a significant association between cyclopentolate and increased gastric residuals after tube feedings in infants who were not on oxygen (p=0.012). Conclusions: It is possible that infants with chronic lung disease or genetic risk factors may absorb cyclopentolate differently from other infants.There is a need to continue research to confirm findings of adverse events after ROP eye exams and to predict which infants are at risk for higher blood levels of cyclopentolate and adverse events. Implications for Nursing Practice: Lower doses of mydriatic drugs or techniques such as nasolacrimal occlusion to prevent systemic absorption of cyclopentolate may be required for infants at risk. Nurses must carefully monitor preterm infants after ROP eye exams and be prepared to intervene in the event of feeding intolerance or respiratory distress. Parental education is essential when infants are discharged immediately after eye exams. 36 Abstract #011 Title: Secondhand Smoke and Allelic Variances on Codon 98 as Risk Factors for Cervical Cancer Authors & Affiliations: Ayasha Thomason, MNSc, APRN, WHNP-BC, Natalie Capps, MNSc, RN, University of Arkansas for Medical Sciences College of Nursing Background & Significance: Many variables lead to cervical cancer including environmental hazards, tumorigenic growth, dysfunction and immunology of genes, and allelic variances. Codon 98, on FHIT tumor suppressor gene has particular susceptibility to tobacco carcinogens and might explain how cigarette smoke acts genetically. Ninety-six billion health care dollars are spent each year related to smoking and second hand smoke exposure (SHSE). SHSE plays a role in cervical cancer and associated with a 1.8-fold increase in the development of cervical atypia (CA) than non-exposed nonsmokers. Smoking plays a role in human papillomavirus (HPV) proliferation, a cervical cancer risk factor. Purpose: The purpose of this pilot study is to determine a) relationship between alleles on codon 98 and progressive cervical pathology b) examine nucleotide pairings among smokers and SHSE patients compared to non-smokers c) relationship between smoke exposure and cervical pathology. Methods: 70 women with CA (which included those with cervical intraepithelial neoplasia, high grade intraepithelial lesion, low grade intraepithelial lesion, and atypical cells of undetermined significance) were recruited for this prospective cohort study in a colposcopy clinic. Demographic and self-report smoke exposure history was recorded. Pap smear specimen was taken by use of Thin Prep method for extraction of genomic DNA to determine heterozygous or homozygous allele patterns, and pathology. Electronic medical records were used to extract pathology information. Results: Of 70 participants, 68 had heterozygous allele patterns. Logistic regression modeling was done to examine the relationship between smoke exposure and pap results. A 2.25 increased odds of having CA in women SHSE compared to non-smokers (p=0.307). A 1.5 fold increased odds of CA in women who actively smoke compared to non-smokers (p=.619). There was a 3-fold increase in previous CA in women who cohabitated with a partner and were SHSE than those who lived alone and were SHSE (p=0.12), compared to 1.7 fold increase in women who smoke under the same circumstances (p=.087). Conclusions: There was no link between allele patterns and smoking status. Heterozygosity of participants may be indicative of disease process and not smoke exposure due to convenience sample. Those SHSE, who cohabitate with smokers, are more likely to have CA than those SHSE that do not live with a smoker. This may indicate possible dosedependent relationship, and raises question whether women were engaged in unprotected sex with smokers and have seminal fluid that may be heavily concentrated with carcinogens deposited directly on cervix. Further studies with larger sample sizes, sexual information, and HPV status should be done. Implications for Nursing Practice: This was the first study to extract human DNA from a Thin Prep pap smear method. Although the genetic link was not present, the implications are significant since consideration of secondhand smoke from environmental exposure is already known to be hazardous. However, if in fact replication studies prove that seminal fluid is heavily concentrated with carcinogens that directly impact the cervical cells, then condom use and barrier protection methods will become part of the education initiatives regarding protection from secondhand smoke exposure, especially for women in gynecologic settings. Primary care and women's health practitioners need to be aware of additional harms of secondhand smoke exposure. 37 Abstract #012 Title: Aromatherapy for Stress Reduction: A Strategy for Self-Care Authors & Affiliations: Sheila Stroman, University of Central Arkansas Significance: The effects of stress are known to adversely affect physical, psychological, behavioral, and overall well-being. Workplace-related stress leads to decreased productivity, lower morale, reduced job satisfaction, and impaired immunity among practicing nurses. Aromatherapy is recognized as a simple, readily available, and noninvasive therapy that affects mind, body, and spirit. Purpose (or Problem): The purpose of this review was to examine evidence from literature, historical practices, and clinical expereince in the use of aromatherapy for stress management. PICO Question: Among practicing nurses, does the use of aromatherapy assist in management of stress reduction in personal and professional settings? Search Strategy & Screening: A search of common research data bases (OVID, Medline, Google Scholar, EBSCO), along with classic textbook recommendations, and limited case studies were included. Historical use and anecdotal data round out the evidence foundation for examination of the efficacy of aromatherapy in stress reduction. Evidence: Several studies provide evidence that inhalation exposure to selected essential oils (lavender, peppermint, basil, rosemary, and clary sage specifically) may be associated with reduced anxiety, enhanced mental functioning, and improved mood. Recent studies in psychoneuroimmunology (PNI) provide modern support to the relationship of aromas, emotion, and physical changes.Historical use and considerable clinical and patient experiences strengthen the evidence base. Synthesis of Evidence: The use of essential oils shows promise as a cost-effective self-care strategy or adjunct therapy for stress management with fewer side effects that those produced by many pharmaceuticals currently in use. There is a large body of scientific research published in languages other than English, particularly in Chinese, Korean, and Japanese. Conclusions: While the evidence examined supports the efficacy of aromatherapy researchers face several challenges in conducting randomized controlled trials. These include creation of a control exposure to odors, different essential oil chemical variations, use of synthetic aromas, the synergistic effects of multiple oils, and separation of oil effects from the effects of massage. A fertile area for research in English exists in order to test the efficacy of essential oils already in common use in many clinical settings. Future studies should examine inhalation of standardized essential oil formulations and use of a control odor. Implications for Nursing Practice: There is current interest in promoting self-care among nurses. Aromatherapy is a complementary therapy with considerable promise for assisting with stress management in both personal and professional settings. As a complementary therapy, it is a simple, readily available, and cost-effective empowering self-care strategy. 38 Abstract #013 Title: Effects of a 12 Week Maternal CPR Practice Program on Nursing Student Performance Recall Authors & Affiliations: Brandy Haley, MSN, RN Assistant Professor in Nursing, University of Arkansas at Monticello; PhD in Nursing student, UAMS Background & Significance: The prevalence of maternal cardiopulmonary arrest is 17.8 out of 100,000 reported in 2011, up from 8.3 out of 100,000 reported in 1998. Maternal cardiopulmonary arrest is life threatening for the mother and fetus. For higher chances of maternal and fetal survival, a number of unique cardiopulmonary resuscitation (CPR) modifications must be done during resuscitation efforts. Due to the needed CPR modifications for maternal codes and its rarity, how to respond to maternal cardiopulmonary arrest cases is challenging for many health care providers, especially in nursing students. For this reason, healthcare educators are looking for more effective methods to teach maintenance of maternal CPR skills with hopes to improve maternal and neonatal outcomes. Research suggests that practice is needed every two weeks to maintain pediatric CPR competence and every four weeks to maintain adult CPR competence. However, it is unknown exactly how much practice is needed to maintain proficient performance in maternal CPR. Purpose: To test the feasibility of a 12-week maternal CPR practice program with 3 arms in undergraduate nursing students and to gather preliminary data on the effect of practice sessions on maternal CPR performance. Research question: “Is a randomized controlled trial (RCT) study design feasible to conduct measuring maternal CPR performance in undergraduate nursing students?” It was hypothesized that the two intervention groups compared with the control group would show better maternal CPR performance recall after the intervention sessions, but there would be no significant difference between the intervention groups. Methods: This study used a three arm RCT cluster design conducted over a 12 week period at the site of the University of Arkansas at Monticello School of Nursing Simulation lab. The sample included 24 undergraduate senior nursing students (83% females, mean age 22 years, 71% White). Upon enrollment, students were taught maternal CPR through lecture and student demonstration followed by a pre-evaluation performance. Students were then randomized into one of three groups: Intervention Group One (practice maternal CPR every 2 weeks), Intervention Group Two (practice maternal CPR every 4 weeks), or Control Group (no practice sessions). At the end of the 12 weeks from enrollment, a post-evaluation performance was obtained. Demographic data was reported using descriptive frequencies and means. One way ANOVA was used to evaluate the study data. Results: Results showed that 87.5% of students in Group 1 and 75% in Group 2 attended all their practice sessions. Overall attrition rate was 8% (2/24). Post evaluation was completed by 92% (22/24) of the participants. There was a significant difference in the performance recall scores between the intervention groups and the control group at followup (2 week practice group mean 96.25; 4 week practice group mean 90; no practice group mean 61.43; p = .001). There was no statistical significance in performance recall scores between the two intervention groups at follow-up (p = 1.00). Conclusions: Using a RCT study design was feasible. Findings suggest that practicing maternal CPR modifications at least every 4 weeks will increase performance recall. Implications for Nursing Practice: This is the first feasibility study to examine the effects of a CPR training program on retention of maternal CPR performance recall and to examine the dose of practicing on performance recall. Duplication of this study may demonstrate that regular maternal CPR practice programs increase performance retention thereby encouraging nursing education programs to implement the training program into their obstetrical curriculum. In addition, results from a duplicate study could lead to the development of a maternal CPR training program for licensed healthcare providers in the actual clinical environment. Further studies are needed to duplicate this study with larger samples considering other variables affecting maternal CPR practice recall. 39 Abstract #014 Title: The Association of Sleep Disturbance, Depression, and Prodromal Symptoms of Coronary Heart Disease in Women Authors & Affiliations: Christina M. Pettey, PhD, APRN, FNP-BC; Jean McSweeney, PhD, RN, FAHA, FAAN; Mario A. Cleves, PhD, University of Arkansas for Medical Sciences, College of Nursing Background & Significance: Over 240,000 women die from coronary heart disease (CHD) yearly. Sleep disturbance and depression have been implicated in the development of CHD in women. The Nurses study, (n = 71,617) found an age-adjusted relative risk of 1.82 (95% CI: 1.34-2.41) for women sleeping <5 hours per night. Depression is also associated with an increased risk of CHD and is commonly comorbid with it. Few studies have collected longitudinal data to examine the correlation of sleep disturbance and depression with prodromal symptoms of CHD in women. This is important because the identification of risk factors and prodromal symptoms may assist clinicians in diagnosing CHD earlier in women. Purpose: To estimate the association between sleep disturbance and depression with prodromal symptoms of CHD in women. Methods: Data for this multi-site, longitudinal study were collected from women without CHD from cardiology practices in two southern states. They were queried every three months for two years regarding sleep disturbance, depression, and prodromal symptoms of CHD, measured as a positive report of sleep disturbance, score of 16 or greater on the Center for Epidemiologic Studies Depression Scale, and the McSweeney Acute and Prodromal Myocardial Infarction Symptom Survey (MAPMISS) prodromal score. Generalized estimating equations were used adjusting for repeated surveys. Results: 1074 subjects (mean age at baseline 53.8 + 13.9 years; 933 [87%] white;141 [13%] black) with 8593 surveys were analyzed. Depression, Sleep Disturbance and their interaction were significantly associated with increased MAPMISS prodromal score adjusting for age and race. Subjects with Sleep Disturbance without Depression had an increase of 21.5 points in MAPMISS (P < 0.001), while those with Depression and no Sleep Disturbance had an increase of 19.3 points (P < 0.001). In the presence of both Depression and Sleep Disturbance, MAPMISS increased 53.2 points (P<0.001). Conclusions: Sleep Disturbance and Depression were strongly associated with CHD PS in this sample. Women should be educated regarding the possible association between sleep, depression, and PS of CHD so they will seek care when these symptoms develop. Implications for Nursing Practice: The assessment of sleep disturbance, depression, and PS may help clinicians diagnose CHD earlier so interventions can be implemented to delay the progression of CHD in women. 40 Abstract #015 Title: Predictors of Substance Use Recidivism in Arkansas Nurses Authors & Affiliations: Karen Davis, DNP, RN, CNE; Cynthia Powers, BSHA, DNP, RN-BC, CNN, NEA-BC; Union University Jackson, TN; Jasna Vuk, MD, PhD, UAMS; Robert Kennedy, PhD, UAMS Background & Significance: Substance use recidivism endangers the health of nurses and the safety of patients. The Arkansas nurse practice act (NPA) states that one function of the Arkansas State Board of Nursing is to decide on disciplinary actions for inappropriate use or misuse of alcohol or habit-forming drugs (Arkansas State Board of Nursing [ASBN], 2011). Because the Board of Nursing (BON) is under the regulation of the Arkansas state legislature, the public requires evidence regarding the BON’s effectiveness in regulating practice and promoting patient safety, including evidence of the ability to make appropriate decisions regarding disciplinary actions of the state’s nurses. The goal of this study was to provide data to be used as a basis for making decisions regarding the length of probation for substance use violations. Purpose: This retrospective study was designed to explore whether a relationship exists between lengths of probation for nurses with substance use violations and recidivism Methods: Data collected from computer files at the Arkansas State Board of Nursing were allocated to two groups (n = 76/group): registered nurses (RNs) with one substance use disciplinary probation and RNs with more than one substance use disciplinary probation. Variables were length of probation for substance use, age, race, gender, educational level, felony substance conviction, and nature of the violation (habit-forming drugs, alcohol, or both). Results: Results indicated no statistically significant difference in rates of recidivism based on length of probation (p = .05). Odds of recidivism for nurses with a felony substance conviction were 4.6 times higher than for nurses without a felony substance conviction. Odds of recidivism were 5.9 times higher for nurses addicted to both alcohol and habit-forming drugs. Because substance use poses a threat to patient safety and impacts employers and coworkers, further research is needed to identify solutions to this growing problem. Conclusions: Substance use is a growing problem in nursing and BONs are seeing an increase in substance use recidivism. Though this study did not yield data to support decision making regarding the length of probation, substance use felony convictions and addiction to both habit-forming drugs and alcohol were identified as possible predictors of recidivism among RNs in Arkansas. Further research is needed to replicate this study or to focus on other variables, such as the nature of the probationary period and treatment tailored for the substance use trajectory of the individual nurse. Such studies may help reduce the rate of recidivism and identify solutions to this growing problem. Implications for Nursing Practice: The problem of impaired nursing practice and the risk to patient safety is the same in every state. There have been many studies on disciplinary violations and the disciplinary action determined by BONs (Hester et al., 2011; Hudson & Droppers, 2011; Zhong, Kenward, Sheets, Doherty, & Gross, 2009). A number of studies focused on different variables related to the types of violations as well as the type of discipline ordered, such as probation, license restriction, and completion of a drug treatment program (Bettinardi-Angres, Pickett, & Patrick, 2012; Waneka, Spetz, & Keane, 2011; West, 2003; Zhong & Kenward, 2009). 41 Abstract #016 Title: Nurses Educating to Help Save Lives: A Red Cross Program to Increase Blood Donations Authors & Affiliations: Cheryl K. Schmidt, PhD, RN, CNE, ANEF, FAAN, UAMS College of Nursing; Vivian Littlefield, Emerita, University of Wisconsin-Madison; Background & Significance: More than 41,000 blood donations are needed every day, and recent changes in understanding antibody formation during blood transfusions have led to the need to increase donations from different ethnic and racial populations. In human blood, there are more than 600 known antigens besides A and B, and certain blood types are unique to specific racial and ethnic groups. It is essential that the donor diversity match the patient diversity. When blood is phenotypically matched (i.e., close blood type match), patients are at a lower risk of developing complications from transfusion therapy. For this reason, it is extremely important to increase the number of available blood donors from all ethnic/racial groups. Purpose: The purpose of this study was to pilot test an innovative American Red Cross Biomedical program called “Nurses Educating to Help Save Lives” to determine its effectiveness in engaging nurses and nursing students in educating communities about the importance of donating blood. Methods: The American Red Cross Blood Services staff developed a course titled “Nurses Educating to Help Save Lives,” which provides ready-made materials to be used in presenting this important information to community groups. The program is led by the American Red Cross National Nursing Network through the State and Regional Nurse Leaders. Nursing program faculty and students were recruited to present the program in order to decrease the potential fear and anxiety related to donating blood. A Toolkit which was provided contained a PowerPoint presentation called “Blood 101”, an evaluation form, instructor checklist, and supplemental fact sheets about donating blood. Students collaborated with faculty to practice their presentation, arrange sites to talk to community members, and taught the course as part of clinical experience or for service credit. Close collaboration with the American Red Cross Blood Region was required to make the program successful. Results: During pilot testing of this program, over 300 individuals attended the multiple presentations; 72% of them said they would donate blood in the future. At the University of Wisconsin-Madison campus, where the pilot was conducted, several nursing students presented the program to different audiences, and were given course credit for it. The students indicated that they would become Red Cross Nurse volunteers, and donate blood themselves. Attendees reported that the students were professional, and that they benefited from the presentation. Conclusions: This program was successful in populations where there is a need to increase blood donations, such as in African-American communities. The pilot phase of the “Nurses Educating to Help Save Lives” program was conducted in the Madison, Wisconsin, area, leading to adoption of the course in other regions of the United States. Red Cross Blood Regions will track the anticipated increase in blood donations from all populations, particularly those in ethnic and minority groups. Implications for Nursing Practice: Improved matching of antibodies in donated blood products will lead to a decrease in transfusion reactions, especially in patients with conditions that may require more frequent transfusions (e.g., sickle cell disease, hemophilia). Since nurses have been rated as the “most trusted profession” for the past several years, they are an ideal group to promote blood donations throughout the country. The program provides standardized teaching materials and organizational tools (e.g., introduction letters, checklists, thank you letters, etc). The only remaining ingredient for success is a group of enthusiastic nurses or nursing students to present the program. 42 Abstract #017 Title: Symptom Onset to Arterial Reperfusion (SOAR) Research Study Authors & Affiliations: Deborah Meiklejohn, MNSc, RN, St Vincent Infirmary Medical Center, Aravind N. Rao, MD, Heart Clinic Arkansas Background & Significance: A phrase associated with myocardial infarction “Time is Muscle” is well-known, but is not yet guiding the public to seek rapid treatment at the onset of symptoms. A faster response time to reperfusion time can increase myocardial salvage and decrease mortality rate. Two-thirds of the total time from symptom onset to reperfusion occurs from symptom onset to presentation to the ED. The American College of Cardiology (ACC)/American Heart Association (AHA) recommend timely access to primary percutaneous intervention (PCI) to achieve door to balloon (D2B) time of <90 minutes and symptom onset to balloon (S2B) time of <120 minutes. Purpose: The purpose of this study was to analyze existing data on non-transfer patients who experienced a STEMI and received a primary PCI. The study monitored patient response times, the number of patients with D2B times <90 minutes, and S2B < 120 minutes. The study compared patients who arrived in the ER via EMS vs. walk-ins and the impact on D2B times when the cardiac catheterization lab (CCL) was activated from the field based on an electrocardiogram (ECG) faxed from EMS. Methods: The preliminary work for this program of research included identifying and testing our data sources in preparation for the retrospective review of available data. The sample population consisted of patients who experienced a STEMI and received primary PCI at St. Vincent Infirmary Medical Center from 2012-2013. All patients who had a discharge code for (DRG 410.0-410.9 Acute Myocardial Infarction) STEMI and received a primary PCI during the designated time frame were included. Sampling excluded patients with any of the following criteria: The patient was transferred from a non-PCI facility, onset of chest pain was > 2days prior to arrival in the ER and/or lack of a primary PCI for STEMI. Results: For 2012-2013, 20% of the patients received arterial reperfusion in less than 120 minutes from symptom onset which remained consistent for each year. In 2013 compared to 2012, the D2B time within 90 minutes improved for EMS patients from 91.6% to 100% and improved for walk-in patients from 76.9% to 94.4%. SOAR Median times decreased from 2012- 2013 by 26.9% for EMS patients and 45.8% for walk-in patients. The mean age of the largest population of patients in the study was 60 years old. Conclusions: Continuing education should be provided to the ER staff and EMS personnel on policies and procedures for STEMI patients and ways to help decrease D2B times. The positive outcome from pre hospital transmission of an ECG and early activation of the CCL warrants consideration in all PCI-capable facilities. Process improvements that were developed helped to ensure that in-the-field data received by fax from EMS was evaluated promptly by a physician and early activation of the Code STEMI call team. Implications for Nursing Practice: Emergency room nurses and cardiac care specialty nurses are ideally situated to lead in the development of necessary policies and procedures as well as training for emergency room and hospital department staff whose roles will be involved in the process. Multidisciplinary Mock STEMI drills led by the Nurse Educator/Specialty Nurse both in the ER and in-house will help streamline response time and identify needs for improvement. 43 Abstract #018 Title: Tracing Zeroes for Our Heroes Authors & Affiliations: Edward Lee Hill, MNSc, RN, Perry D. MacLaird, BSN, RN, Jody A. Bryant, MSN, RN; Central Arkansas Veterans Healthcare System Problem & Purpose: The purpose of this evidence-based practice (EBP) project was to develop a tool and process for including front-line staff members in assessing continued compliance of survey finding corrections. PICO Question: Will including and empowering front-line staff in performing tracers regarding compliance with survey finding corrections enhance sustainment of the corrections and lead to process change in completing appropriate actions proactively rather than corrections reactively, when compared to previous activities? Evidence-based practice models & process: A basic PDSA (Plan-Do-Study-Act) model for evidence based performance improvement process was used as the framework for this process. Relevant Literature: Tracer methodology was developed and implemented by The Joint Commission in 2004. It has improved focus on the patient care process at the point of care. It allows review across the continuum and offers validation on consistency, safety, and uniform performance of care, treatment, and services. Tracers provide evidence of the communication process of resident care, from admission to discharge and beyond. Use of adult learning principles with front-line staff members facilitated their inclusion in assessing, correcting, and monitoring processes for correction of survey findings and maintaining a priority on high quality, resident focused care. Empowering front-line staff leads to their embracing the process. Methods: The project involved a small work group developing and finalizing the tracer tool. Pre- scheduled and just-intime training/education was provided when implementing this tool and process. Initial responses indicated some misunderstandings of question intent. Front-line staff members were involved in rewording questions for better understanding. Three tracers per week per resident unit were completed. Weekly entry of data allowed timely review of compliance issues and implementing an action plan for any noted continuation of deficiencies or new issues. Minimal acceptable compliance levels were set at 90% with a goal of 100%. Outcomes: Data analysis of compliance on this process was compared to the compliance from the previous survey correction process. Sustainment of changes implemented by the action plans with this process continued versus corrections that returned to the pre-survey level of non- compliance when Performance Improvement and Quality Management performed the tracers previously. Continued compliance increases led to a compliance level of ≥95% in each CMS F- tag. The tracers provided documented evidence that appropriate actions were performed upon admission, rather than after an error was found later during the hospital stay, which led to continued acceptable compliance regardless of the point in the continuum of care time-frame when the tracer was completed. Compliance and sustainment of changes was validated by zero findings for the Community Living Center during the triennial Joint Commission survey. Conclusions: Incorporating the front-line staff in the process from the very beginning is imperative. Staff nurses performing the tracers led to increased recognition of deficient areas, correction of deficiencies, realization of the need to ‘do it right the first time’ to prevent future findings, and sustainment of corrections. Implications for Nursing Practice: Additional use and reviews of this tracer process, following future surveys, could provide further evidence of a successful front-line staff tracer completion. 44 Abstract #019 Title: Application of Diffusion of Innovation Theory to Increase APRN Adoption of Arkansas’ Prescription Monitoring Program Authors & Affiliations: Elizabeth Jarvis, MSN, APRN, CNS-C, Cathrin Carithers, DNP, APRN, FNP-C; University of Arkansas for Medical Sciences Problem & Purpose: Problem and Purpose: The number of opioid prescriptions per 100 persons increased by 35.2% during the period 2000-2009 (Daren, Mack & Auozzle, 2012). This increase in opioid prescriptions can lead to drug abuse and misuse as reported by the Drug Enforcement Agency. The purpose of this evidence-based quality improvement project is to increase awareness of the Prescription Monitoring Program (PMP) for APRN’s in Arkansas. The PMP is a tool to enhance patient care by providing prescription monitoring information that will help to ensure legitimate use of controlled substances in Arkansas. PICO Question: PICO Format Question: What is the awareness of APRN’s in Arkansas in the use of the Prescription Drug Monitoring Program to assist in the reduction of drug abuse and misuse? Evidence-based practice models & process: EPB Model/Process: Roger’s Diffusion of the Innovation Theory is used to facilitate APRN adoption of the use of the PMP tool prior to writing prescriptions for controlled substances. Relevant Literature: Relevant Literature: There is little published literature regarding use of the PMP. Reisman, Schenoy, Atherly, and Flowers (2009) reported that states with a Prescription Monitoring Program (PMP) had lower rates of inpatient drug abuse rehabilitation than those states without a PMP. A survey of U.S. toxicologists revealed that 87% of respondents had some knowledge of the PMP; however, more than one- fourth reported not accessing their state’s PMP. Reasons cited included a lack of knowledge regarding the availability of the PMP or they had not registered to use their state’s PMP. Methods: Method: This project employed a descriptive study design. A convenience sample of 128 APRN’s with prescriptive authority across the State of Arkansas was invited via e-mail to complete an online survey evaluating their knowledge and use of the state’s PMP. Two weeks after the initial survey was e-mailed to participants, an e-mail reminder was sent out again in an attempt to solicit a greater response. Outcomes: Outcomes: Thirty percent (n=38) of the 128 APRN’s responded to the survey. Eighty two percent of respondents reported finding discrepancies in filled prescriptions as a result of checking the PMP. The APRN’s who checked the PMP prior to writing prescriptions reported finding discrepancies on the patients requesting controlled substances. The study revealed three barriers to using PMP is lack of time, hard to use, and/or lack of knowledge of PMP. Conclusions: Conclusions and Recommendations: The majority of APRN’s who participated in the survey are aware of the PMP tool, however, due to time constraints, they do not utilize it to the full potential. A “quick reference guide” that provides instructions regarding how to access the PMP could increase the use of the PMP by APRNs in Arkansas. Implications for Nursing Practice: Implications for Nursing Practice: The use of the PMP by APRN prescribers can positively impact patient care by monitoring patients’ controlled substance histories. This can decrease drug abuse and misuse by identifying multiple prescribers or pharmacies. 45 Abstract #020 Title: The Impact of School Based Health Centers on Absenteeism in Rural Middle School Students Authors & Affiliations: Gianna M. Grant, MNSC, APRN, GNP-C, FNP-C & Cathrin Carithers, DNP, APRN, FNP-C; University of Arkansas for Medical Sciences, College of Nursing Problem & Purpose: High rates of absenteeism in middle school increase the risk of high school dropout (Balfanz & Byrnes, 2012). This project evaluated the effect of a newly established School Based Health Center (SBHC) in a rural middle school on the rate of student absenteeism. PICO Question: Does the availability of a School Based Health Center for rural, middle school students reduce absenteeism over a 4 month period? Evidence-based practice models & process: Utilizing the principles of Risk, Protection, and Resilience in Childhood (Richman &Fraser, 2003), the Washington Middle School (WMS) SBHC sought to modify health risks for children who lacked access to dental and health care, thus improving resilience in learning outcomes. Relevant Literature: The paucity of information regarding SBHC’s and their effect on absenteeism supports this project. Webber et al. (2003); Walker, Kerns, Lyon, Bruns, & Cosgrove (2010); and Van Cura (2010) were homogenous in their findings of improved rates of absenteeism for SBHC users compared to non-users. Geirstanger, Amaral, Mansour, and Walters (2004), however, concluded that insufficient research exists to support a direct correlation between SBHC's and academic performance. Methods: This project used a pre-post intervention design. De-identified aggregate student absenteeism data was obtained from a non-probability consecutive sample of students (n=59) from WMS who were enrolled in the SBHC from September 2014-December 2014. Outcomes: Anticipated outcomes will reflect a decrease in aggregate student absenteeism in the implementation months compared to commensurate months before the inception of the SBHC. Conclusions: These will be made after final data analysis occurs. It is postulated that continued efforts should be made to foster higher inclusion rates of students as users of SBHC’s. In addition, SBHC’s should continue documenting their impact on indicators of academic performance, such as absenteeism. Implications for Nursing Practice: SBHC’s are a burgeoning way to access children and impact their health and development. Interprofessionalism is crucial to the success of SBHC’s. Involvement in SBHC’s development and sustainability places nurses, nurse practitioners, and nurse researchers in an axial position to change the trajectory of lives for children at risk. 46 Abstract #021 Title: Delirium in Acutely Ill Elders: The Role of Nurses Authors & Affiliations: Jody Bryant, MSN RN, Central Arkansas Veterans Healthcare System; Tanya Taylor, BSN RN,and Sheila Cox Sullivan, PhD RN, Veterans Integrated Service Network (VISN) 16 Geriatric Research, Education and Clinical Center Significance: Delirium is a change in mental activity, which results in compromised reasoning and a lack of environmental awareness. Delirium constitutes a medical emergency. Delirium occurs in up to 56% of hospitalized elderly and up to 87% of critically ill patients. Acute delirium is correlated with increased length of stay, increased risk of hospital-acquired infections, and loss of functional ability following hospital discharge. Nurses have many evidencebased options they can implement independently to prevent and treat this potentially fatal brain dysfunction. Purpose (or Problem): The purpose of this literature review was to explore evidence from literature and practice guidelines to summarize independent nursing actions to prevent or treat delirium. PICO Question: In elderly patients with delirium, can increased recognition and implementation of independent nursing interventions decrease the incidence and severity of delirium? Search Strategy & Screening: Our team searched PubMed, CINAHL, PsychInfo, and Medline using the search terms “Delirium”, “Acute Care” and “Elders” in addition to AHRQ’s National Guideline Clearinghouse. We also reviewed references from the obtained documents for additional references. Evidence: The initial literature search produced a total of ¬18 unique articles. Ultimately, we used 22 articles focusing on independent nursing actions for prevention and/or treatment of new onset delirium in hospitalized elders. Synthesis of Evidence: Many facilities do not routinely screen for delirium as a part of nursing assessment. This results in a missed diagnosis of delirium up to 80% of the time. Even when policy dictates that nurses monitor for delirium, only 47% of nurses report completing an assessment. There are simple, well-validated tools available for nurses to use as screening tools, such as the Confusion Assessment Method (CAM). Nurses can also use such interventions focusing on six domains: Cognitive Impairment, which may be addressed with a systematic means of reorientation and therapeutic activities; Sleep deprivation, using care coordination, sleep enhancement strategies, and avoidance of pharmacologic sleep enhancers; Immobility, by using systematic, planned mobilization programs for eligible patients; Visual impairment, ensuring the presence of glasses and adaptive equipment; Hearing impairment, ensuring the presence and adequacy of hearing aids; and Dehydration, systematic means of encouraging the intake of oral fluids, and education aimed at improving rapid recognition of signs and symptoms of dehydration. Conclusions: The articles and guidelines in our literature search reveal that nurses have a prominent role in the prevention and treatment of delirium. Evidence from literature indicates that nurses have a critical role in first line recognition of delirium. Implications for Nursing Practice: Currently, nurses frequently do not routinely assess for delirium in their practice, but providing education to nurses about this common problem, risk factors and interventions could greatly increase positive outcomes such as shorter length of stay, less hospital acquired infections, and a decrease in functional decline, institutionalization and death. 47 Abstract #022 Title: A Sweet Lesson in Research Authors & Affiliations: Jennifer Cockerham, MBA, Paul Easley, MHSA, RRT-NPS, Joyce Grundy, BSN, RN,CCM, Ellen Mallard, BSN, RN, RNC-NIC, Keisha Oglesby-Brown, BSN, RN, Karen Pritchett, BSN, RN, Lorie Beth Proffitt, RN, CCM, Barbara Schmid, CCRP, CRS, Liz Walker, APN, BSN, CCRP, CRS, Mary Kathryn Nelson, BSN, RN Background & Significance: The Institute of Medicine’s (IOM) report, Crossing the Quality Chasm: A New Health System for the 21st Century (2001) posed Evidence-based Practice and Research as a solution for improving the quality and safety of healthcare. In 2003, the IOM re- affirmed the view and further recognized Evidence-Based Practice and Research as key competencies for healthcare professionals (2003). According to the literature, one common barrier to research identified is anxiety regarding the research process (Deck, 2010; Weitzel & Robinson, 2011). Purpose: The purpose of this course was to address the barriers clinicians have regarding research. Participants received education and applied the principals of conducting research to a mock cookie experiment. Methods: A group of seven, multi-disciplinary direct and indirect care staff participated in the Introduction to Research course, which utilized lectures, discussion and hands-on learning experiences. Each step of the research process was then applied to a simple mock experiment, which included conducting scholarly literature reviews, determining the level of evidence, designing a study, writing a mock protocol, submitting to the IRB, conducting an experiment, collecting data, analyzing data, record-keeping, and writing an abstract. Results: Pre and post course participant evaluations indicated an increased comfort and knowledge level with conducting research. When polled about knowledge of conducting a research project, participant responses increased from 1.57 pre to 2.86 post. When polled on comfort level with identifying and overcoming barriers to conducting research, data revealed a large effect size of -0.9006. Conclusions: Class participants found the course to be helpful; not only in learning about the research process and the necessary steps required to conduct a study, but also through learning about available resources. Through application in the experiment, the instructors helped reinforce what was discussed and made the process tangible, which will help with knowledge retention. Having a fundamental understanding of the research process, participants are more likely to apply these research skills in practice. In addition, course participants will present outcomes of the mock cookie taste experiment and educational experiences gleaned. Implications for Nursing Practice: Safety is a core value of Arkansas Children’s Hospital and research has been shown to improve the safety of health care (IOM, 2001). According to Robinson, 2008, this new found comfort and understanding with the research process will ultimately result in better patient outcomes. Participating in this research class, has improved the comfort level with the research process, which ultimately provides safer care for patients. 48 Abstract #023 Title: Reducing Heart Failure Readmissions Authors & Affiliations: Jennifer Huff, RN, BSN, CCRN; St Vincent Infirmary Medical Center Significance: Heart failure is a major and increasing public health problem that affects patients, families, and communities. Approximately 5.7 million Americans have heart failure, with 10 per 1,000 new cases being reported each year after age 65. Over the past 25 years, the annual number of hospitalizations has increased from 800,000 to over 1 million for heart failure as a primary diagnosis and from 2.4 to 3.6 million for heart failure as a primary or secondary diagnosis. Purpose (or Problem): Despite advances in medical care, frequent readmission is of particular concern when treating these patients. Approximately 50% of heart failure patients are readmitted within 6 months of discharge, and 70% of the readmissions are related to the worsening of previously diagnosed heart failure. The direct costs of heart failure readmissions are estimated to have been $39.2 billion in 2014. PICO Question: Among adult in-patients with congestive heart failure, how would using intensive teaching programs, physician order sets, and outpatient focused support reduce hospital readmission rates? Search Strategy & Screening: The literature search used Google Scholar, Cumulative Index to Nursing and Allied Health Literature, professional practice organization websites and manual searches based on guideline reference lists. Search terms used to locate guidelines and research studies: Congestive heart failure readmission rates, heart failure readmissions, CHF, decreasing readmissions, and hospital readmissions. Evidence: The evidence consisted of professional practice guidelines, and experimental observational studies of patients having interventions as in-patients and follow up as outpatients with a diagnosis of heart failure. Synthesis of Evidence: Heart failure readmissions are multi-factorial and involve a variety of issues to address—lack of patient compliance/self-care, inadequate discharge preparation and education, poor communication between acute care and post-acute care providers, and delayed discharge follow-up. A robust, actionable, and evidence-based implementation plan to reduce hospital readmission rates for heart failure patients remains underdeveloped. Conclusions: The lack of comparable conclusions regarding the efficacy of disease management for heart failure patients also hampers executing effective programs. Therefore it is crucial to find proper and feasible strategies from the best evidence in each health care system to reduce readmission rates for heart failure patients. Implications for Nursing Practice: Translation of evidence into practice is a major challenge for health care providers. Despite the best available evidence that supports the effectiveness of health care interventions, gaps exist between evidence, policy, and practice in the real world. Some features of effective programs in outpatient setting include a comprehensive approach that includes in-person contact with clinicians (either physicians or APRNs), close telephone follow-up, and intense self-care education and support. Programs limited to remote data gathering, such as telemonitoring, are less likely to be successful. For inpatient and transitional settings, comprehensive discharge education and support that include immediate follow-up with health care provider and smooth transition to home are key points. Implementing comprehensive and feasible outpatient, inpatient, or transitional strategies to reduce readmission in patients with heart failure is vital in the current health care system. 49 Abstract #024 Title: One Stick Too Many: Reducing PIV Sticks and Infiltrates in Pediatric Patients Authors & Affiliations: Jennifer Janisko, MSN, RN; Terri McMillian, RN; Pam Reed, BSN, RN; Angela Scott, MNSc, APRN, PCNS-BC; Sharon Tunstall, RN Problem & Purpose: Current practice was unable to capture the number of IV sticks patients incurred with a PIV placement. The purpose of this evidence-based practice (EBP) project was to develop a standardized process for vascular access placement and management in pediatric patients. PICO Question: In pediatrics, does the use of a standardized process for PIV placement and management decrease the number of PIV placement attempts, infiltrations and increase staff satisfaction? Evidence-based practice models & process: The Melnyk and Fineout-Overholt Model of Evidence-Based Practice provided the framework for this project. Relevant Literature: The interprofessional team comprised of clinical nurses, IV team nurses, Child Life specialists, Clinical Nurse Specialists and Clinical Educators conducted a thorough review of the literature. The team also gathered evidence from collaboration with other pediatric hospitals and professional practice guidelines. The evidence indicated that the use of scoring tools that defined which clinicians were the most effective in obtaining vascular access based on a patient’s clinical picture, decreased number of IV attempts and increased patient/family and nurse satisfaction (MacPhee, 2002). MacPhee, M. (2002). Using evidence-based practice to create a venous access team. Journal of Pediatric Nursing, 17(6), 450-454. Methods: Through staff surveys deficits were highlighted in the overall process of PIV placement and management taking into consideration factors such as available access sites, age of patient and skill of RN attempting PIV placement. Using the survey data the team collaborated with peer hospitals to identify other evidence-based tools used for proper and effective PIV placement and management. Outcomes: The team developed a multifaceted intervention for PIV placement and management which included a vascular access scoring tool, house wide staff education, medical record documentation, reassessment of infiltrates and development of a comprehensive PIV management policy. As a result of this process change we are now able to capture and monitor data about PIV attempts. Since the implementation of the PIV management policy we have had a 50% reduction in grade III and IV infiltrates in comparison to the same time frame from 2013. A follow up staff survey resulted in an increase in staff satisfaction regarding the PIV placement process. Conclusions: Implementation of a standardized process based on best practices can be successful with proper education and the use of evidence-based tools. Implications for Nursing Practice: Continued monitoring and analysis of the comprehensive PIV management interventions will further increase staff awareness of utilizing the most competent staff for first time successful PIV placement and result in a decline in PIV infiltrates 50 Abstract #025 Title: Incorporating the Electronic Medical Record into Nursing Curriculum Authors & Affiliations: Carolyn Morrisey, DNP, RN, University of Alabama- Birmingham Jacqueline Moss, PhD, RN, FAAN, University of Alabama -Birmingham Background & Significance: Background: The National League of Nursing (NLN) and the American Colleges of Nurses (AACN) suggest incorporation of informatics into nursing curriculum (Gardner & Jones, 2012). Brooks and Erickson (2012) suggest incorporating the use of the EMR into nursing curriculum to increase student familiarity with electronic documentation Purpose: Purpose: This study examined competency in the use of an electronic medical record (EMR) following training in the simulation laboratory using clinical scenarios and high fidelity manikins compared to trained in a traditional computer laboratory. Methods: Methods: The research project combined EMR training with the use of high fidelity simulation manikins with documentation of clinical experiences. After Institutional Review Board approval from the University of Alabama Birmingham, students were assigned to traditional classroom method or to simulation laboratory group for instruction on the EMR. The simulation group participated in a scenario which involved collecting data and charting in EMR. Both groups completed post tests and satisfaction survey. T-Test analysis was performed. Student demographic data was examined. Results: Results: 71 students (22 to 44 years of age, with five males, 65 females) completed the study. Mean scores on the competency assessment were not statistically significant; students trained using simulation did as well as those trained using the traditional method, the students in the simulation group reported greater satisfaction with the learning process than the students in the traditional classroom instruction group. Conclusions: Conclusions: This research utilized knowledge developed regarding experiential learning within nursing curriculum by using the simulation lab coupled with an EMR in which to document activities and assessments. While tests of competency failed to show statistical difference in scores, the students reported increased satisfaction with simulation as a method of learning Implications for Nursing Practice: Implication: Further studies should examine student performance in the practice setting after EMR training in simulation lab.. The results of the study support the adoption of case based applications of EMR training across the curriculum. 51 Abstract #026 Title: Adherence to Prostate Cancer Screening Recommendations after a Community/Internet- based Educational Program Authors & Affiliations: Purifoy, Jody A., APRN, CNP; Cathrin Carithers, DNP, APRN, FNP-C, UAMS CON Faculty; Barbara Pate, PhD., RN; Claudia Beverly, PhD., UAMS CON Faculty; Kristie Hadden, PhD., UAMS COPH Faculty; Rodney Davis, M.D., Chairman of Urology, UAMS Problem & Purpose: Prostate cancer (PCA) is the second most common cancer in American men, however its survivability is good. As a result of two large randomized controlled trials (Pinskey, 2012; Schroder, 2012) on mortality in PCA, United States prostate cancer screening guidelines (PCSG) have changed. These changes promote shared and informed decision- making and have resulted in a prolonged visit with a health care provider in an already strained health care system. The use of decisional aids (DA) for prostate cancer screening (PCS) have been shown to improve knowledge while decreasing decisional conflict (DC). The purpose of this project was to provide a community-based live DA of PCSG education with reinforcement through a validated and reliable website to improve PCS knowledge and decrease DC for men considering PCS. PICO Question: In adult men aged 40-75 years in Arkansas does a community based live DA with reinforcement through a validated website improve men’s knowledge of prostate cancer screening and decrease their decisional conflict? Evidence-based practice models & process: James Bettman’s interpretation of the Consumer Information Processing (CIP) Theory (1997) was used to guide this project. The CIP has two major assumptions: first, individuals are limited on how much information they can process at one time and second, in order to increase usability of information the information should be divided into “chunks” with decision rules to help make choices more easily. The website was created for consumers to access as desired to facilitate informed decision-making regarding PCS Relevant Literature: Three randomized controlled trials evaluated the use of a web based or printed DA compared to usual care (UC). The use of a DA compared to usual care (UC) or no DA resulted in statistically significant increased prostate cancer knowledge, and decreased decisional conflict scores (Allen et al., 2009; Taylor et al., 2013; Williams et al., 2013). Methods: A pre-test, post-test comparative non-experimental design was used to evaluate participant’s decisional conflict and PCS knowledge. Individual one-way between-groups analysis of covariance will be conducted to analyze decisional conflict and PCA knowledge using the decisional conflict scale (DCS) and PROQUEST (PCA knowledge score). Outcomes: Preliminary data evaluating 30 men in the pilot program are expected to show an increase in PROQUEST scores and a decrease in DCS scores. Conclusions: A community based DA educational intervention with access to a website for reinforcement of key concepts provides a cost-efficient approach to improving informed decision making and decreasing decisional conflict in men appropriate for PCS. Implications for Nursing Practice: Advanced Practice Nurse Practitioners and Nurses can provide a community educational program to men in Arkansas in the community to enhance the men’s ability to make an informed decision regarding their personal health and screening choices. 52 Abstract #027 Title: Nursing Students’ Knowledge and Training During the Medication Administration Process Authors & Affiliations: Kelly J. Betts, Ed.D, RN, University of Arkansas for Medical Sciences College of Nursing Problem & Purpose: The purpose of this qualitative study was on students’ perceptions of their knowledge, skill proficiency, and safety during medication administration in the simulation lab and in the patient care setting. PICO Question: During the medication administration process how do nursing students perceive their knowledge and training during the first year of the nursing program? Evidence-based practice models & process: This study used Patricia Benner's from Novice to Expert domains of nursing practice to capture skill competence and knowledge of students during the medication administration process Relevant Literature: The review of the current literature focused on four major areas of concern as it relates to students’ perceptions of the medication administration process. The four areas of focus for the literature review were self knowledge of the medication administration process, clinical stress, medication administration and error reporting, and perceived faculty/preceptor support during the medication administration process in the clinical area. Methods: The methodology of this study was a qualitative case study. Students were interviewed face to face using a semi-structured interview technique. A interview guide was used to ask open-ended questions to participants. Thematic analysis was used to determine study themes and determine educational gaps in student knowledge and training. Outcomes: Ten students participated in the study. Data was collected, transcribed, and analyzed using thematic analysis. Themes that emerged from the data included application of pharmacology knowledge to practice, complexity of patients and multiple medications to administer, fear of making a medication error. Conclusions: The participants in this study identified a need to be better prepared before going into the clinical area to give medications. It took many hours to learn the medications that they were to give to their patient the next day, and the students had to apply pharmacology knowledge to practice and anticipate any adverse events that might occur with the patient related to administration of medications. Participants noted the complexity of the process of administering medications, such as verification of physician orders, completing the tasks of the computer dispensing system, and all the steps required in the process of giving medications. Participants voiced concerns about fear of making a mistake in the process and adverse outcomes that would occur with the patient. The complexity of patients’ medical conditions was also overwhelming to participants. They felt that not only did the patients have complex medical conditions, but the number of medications administered to these patients was very large, adding to the chances of making a medication error. In terms of instructor presence, the participants voiced concerns about performing the skill in front of their instructor or preceptor nurse. This added to their stress level; however, overall the students felt that the instructors were very competent in their teaching and they knew each instructor’s expectations for each clinical day. Implications for Nursing Practice: The area of concern and knowledge identified by participants point to the need to improve student outcomes with medication administration. Based on the findings of concern about study knowledge, proficiency, and safety, there may need to be an additional medication administration course in the curriculum, geared specifically to the knowledge gaps identified in this study. 53 Abstract #028 Title: Don’t Leave It To Chance… give breast milk a second glance! Authors & Affiliations: Kristina Shelton, BSN, RN-NIC; Alice Summitt, RN; Arkansas Children's Hospital Background & Significance: From December 1, 2013-July 29, 2014 there were 74 Expressed Breast Milk (EBM) errors (wrong patient, wrong milk, wrong volume, expired) that were entered into Safety Tracker. Audits were conducted during the month of October and revealed that <5% of the RNs were following policy. Expressed Breast Milk is a bodily fluid that can transmit many communicable diseases. Any inadvertent EBM exposures put the patient at risk for transmission of HIV or Hepatitis B or C. Inadvertent milk exposures also subject the mother who provided the EBM and the exposed infant to having labs drawn (extra lab cost, painful procedure, blood loss) not to mention the anxiety that the exposed infants parents have to endure. Purpose: The Purpose of our study was to decrease the number of errors related to Expressed Breast Milk, by 50%, by June 2015 in the NICU Methods: We recruited frontline staff in the NICU to perform audits for one month. We measured the percentage of RN’s that were adhering to our current policy. At the time of our data collection, current policy required two staff members to verify Expressed Breast Milk at patient bedside for correct patient, correct additives, correct volume and correct date. We also reviewed Safety Tracker for the number of Expressed Breast Milk occurrences for the previous six months. Results: After all of our pre data collection, we found that current policy decreased workflow for the RN, since it required two RN’s to come to the patient’s bedside and verify that the syringe of milk was for the correct patient, had the correct additives, contained the correct volume and was not past expiration. This policy was not being followed in its entirety due to the complexity of the process. After consulting with our hospitals IT department we were able to barcode our Expressed Breast Milk labels and add EBM verification to our electronic work list. This process allowed the RN to scan the patients armband and then scan the barcode on the Breast milk label. This process allowed the second verifier to become the scanning of the barcoded EBM label and the patient armband by the assigned patient RN. The RN is still required to do an independent check to ensure the patient is receiving the correct additives and that milk is not passed expiration date. Conclusions: Patients receiving Expressed Breast Milk are at risk for inadvertent milk exposures. Our current policy was not being followed according to our audits conducted. We were able to change our “Breastmilk Storage & Handling” policy to increase staff workflow and provide a safety net for breast milk verification. We are continuing to follow data through Safety Tracker and since our go live date of December 9th 2014 we have only had two Expressed Breast Milk occurrences to date. Both occurrences involved milk administered at wrong rate and milk administered through wrong route Implications for Nursing Practice: Expressed Breast Milk is a bodily fluid that can transmit many communicable diseases. Any inadvertent EBM exposures put the patient at risk for transmission of HIV or Hepatitis B or C. Inadvertent milk exposures also subject the mother who provided the EBM and the exposed infant to having labs drawn (extra lab cost, painful procedure, blood loss) not to mention the anxiety that the exposed infants parents have to endure. 54 Abstract #029 Title: Fall Prevention: A Concept Analysis Authors & Affiliations: Kelly L. Urban, UAMS, College of Nursing Significance: Fall prevention is a topic of interest because as the age of the population increases so does the incidence of falls. The estimated cost of falls is more than 13 billion dollars annually primarily due to complications. Even though home and community settings are the most common places that falls occur, there is lack of clarification of concept fall prevention in these settings. Purpose (or Problem): The purpose of this poster is to perform a concept analysis by examining the defining characteristics of fall prevention in community dwelling adults and providing clarification. PICO Question: Search Strategy & Screening: The Rodgers’ method was used to analyze the concept of fall prevention. PubMed and CINAHL were utilized to search the terms “fall” and “prevention” for documents with information about research and reviews on fall prevention in the community and home settings. The inclusion criteria were English language, full text, and publication year < 10 years. All abstracts were read to determine the relevance to fall prevention only in home and community settings, and 18 articles were used for this study. Evidence: The antecedents of fall prevention were personal factors (e.g., experiencing fall and any clinical condition that causes loss of balance) and environmental factors (e.g., building structure). The attributes of fall prevention were a goal-oriented action, risk assessment, and multifaceted strategies. The consequences of fall prevention were the lack of or no falls. Synthesis of Evidence: The antecedents of fall prevention were personal factors (e.g., experiencing fall and any clinical condition that causes loss of balance) and environmental factors (e.g., building structure). The attributes of fall prevention were a goal-oriented action, risk assessment, and multifaceted strategies. The consequences of fall prevention were the lack of or no falls. Conclusions: To be successful, fall prevention interventions should be developed based on assessment of both personal and environmental risk factors. To deal with both personal and environmental factors at the same time, comprehensive intervention strategies are needed. Further studies are needed to develop and test more effective fall prevention in home and community settings. Implications for Nursing Practice: To be successful, fall prevention interventions should be developed based on assessment of both personal and environmental risk factors. To deal with both personal and environmental factors at the same time, comprehensive intervention strategies are needed. Further studies are needed to develop and test more effective fall prevention in home and community settings. 55 Abstract #030 Title: Increasing Hepatitis C Screening Rates by Screening CDC Recommended Birth Cohorts Prior to Endoscopy Authors & Affiliations: Lynn M. Frazier, MSNc, APRN, CNP-BC, ACNP, Cathrin Carithers, DNP, APRN, FNP-C Problem & Purpose: Hepatitis C is a silent killer. Only 50% of the projected 5.4 million people in the US are diagnosed with HCV. It is expected that screening based on age will locate the nearly three million Americans with HCV that are undiagnosed. The purpose of this quality improvement project is to determine if the implementation of an HCV screening protocol based on the CDC’s Birth Cohort recommendations prior to endoscopy procedures will increase screening rates at the Kanis Endoscopy Center (KEC). PICO Question: In patients presenting for endoscopy procedures at KEC, does implementing a HCV screening protocol based on CDC and USPTF recommendations increase screening rates compared to screening based only on risk factors during a three month period? Evidence-based practice models & process: This project applied tenets of the Health Belief Model, a behavioral change theoretical framework as a stimulus for promoting screening rates in the recommended birth cohort Relevant Literature: The CDC and USPTF reviewed the NHANES data from 1945 until 1989 which evaluated HCV positive and negative results from participants’ age six and older. The results concluded that patients born from 1945 to 1965 were five times more likely to have HCV than any other age group. Based on the results, the USPTF graded screening as ”B” and the CDC as “strong with a moderate quality of evidence”. Methods: This before-after nonexperimental study compares KEC HCV screening rates prior to implementations of the HCV screening protocol to rates post protocol implementation. During a three month period, from September 2014 to December 2014, patients born from 1945 to 1965 scheduled for outpatient colonoscopy or upper endoscopy without prior diagnosis of viral hepatitis were invited to participate in the project. Patients were responsible for cost associated with HCV screening either insurance or self-pay Outcomes: Of the 224 participants screened at KEC, ten patients exhibited positive HCV AB results. Each of the ten patients was referred to a specialty clinic for further workup and possible treatment Conclusions: Once data analysis is completed, it is projected that implementation of this HCV screening protocol in KEC significantly increased screening rates of adults born from 1945 to 1965 to identify HCV status in adults who may not have known. Early identification of positive HCV AB status will lead to earlier intervention and reduce the likelihood of devastating consequences. Recommendations were made to permanently adopt this screening protocol by KEC providers. Implications for Nursing Practice: Increasing early identification and effective treatment of patients with HCV can assist with the reduction of burden to patients, family, community, and society 56 Abstract #031 Title: Tobacco Cessation in Older Adults: The Patient Perspective Authors & Affiliations: Lana Brown, PhD, RN, NEA-BC, Central Arkansas Veterans Healthcare System Background & Significance: Tobacco use is the single largest preventable cause of premature death and disease in the world and in the United States and is associated with diseases of nearly every organ system. Tobacco cessation is considered the single most important factor to improve the health of older adults who use tobacco. However, minimal research has focused on the process of tobacco cessation or factors influencing this process. Purpose: This qualitative study aimed to identify motivators, facilitators, and barriers to tobacco cessation and prolonged cessation in older adults aged 50 years and older. Methods: This qualitative research study explored tobacco cessation in community dwelling older adults after receiving Institutional Review Board approval. The Transtheoretical Model of Behavior Change was the conceptual framework used to guide this study. Snowball sampling was used to recruit 20 older adults who had ceased using tobacco products for one year or more and remained tobacco free. Semi-structured audio-recorded interviews were conducted in each participant’s home. Data were analyzed using content analysis and constant comparison techniques. Demographic data were described using descriptive statistics. Results: Participants were from three southern states and included 11 males and nine females with 18 Caucasian and two African American. The average age of participants at the time of the interview was 71.5 years, and the average quitting age was 60.5 years. Four global themes related to tobacco cessation in older adults emerged from the analysis: (a) motivators, (b) facilitators, (c) barriers, and (d) life after tobacco. These older adults attribute their successful tobacco cessation to self-motivation, accountability to self and others, and finding replacements for tobacco. Barriers to tobacco cessation included tobacco triggers/temptations and addiction/withdrawal symptoms. Participants described themselves as proud, strong, and independent after quitting. Conclusions: Information gained from older adults who have ceased using tobacco products can be used to develop tobacco cessation interventions that health care providers can use to assist older patients who desire to quit. Implications for Nursing Practice: For health care providers (HCPs), the results of this study indicate that some older adult tobacco users do want to quit and can successfully quit after long- term tobacco use. The tobacco cessation process described by these 20 participants correlated with the gold standard for tobacco cessation clinical practice guidelines in the U.S. Public Health Service's Treating Tobacco Use and Dependence: 2008 Update (USDHHS, 2008). The participants were motivated to quit, set a quit date, prepared for that quit date, and changed their daily routine as well as finding nicotine replacements. Tobacco cessation needs did vary by tobacco dependence level, which supports tailored approaches to quitting. HCPs should assess and assist in developing this tobacco cessation plan and follow up. 57 Abstract #032 Title: Improving Adherence to ADA/APA Guideline Recommendations for Metabolic Monitoring: An Outpatient Quality Improvement Initiative Authors & Affiliations: Michele Reynolds, MNSc, APRN, PMHNP-BC, Cathrin Carithers, DNP, APRN, FNP-BC, UAMS College of Nursing Problem & Purpose: The prevalence of diabetes, dyslipidemia, hypertension, and obesity in persons with serious mental illness (SMI) is approximately 1.5 to 2 times greater than the general population. Cardiovascular disease is the leading cause of premature mortality. Atypical antipsychotic medications are the mainstay of treatment for SMI, but these medications have been associated with weight gain which often results in development of hyperglycemia and hyperlipidemia. Such metabolic abnormalities increase the risk of cardiovascular-related morbidity and mortality if not promptly diagnosed and treated. The purpose of this quality improvement (QI) project was to increase the incidence of orders for blood glucose and lipid levels and documentation of weight (WT)/BMI, waist circumference (WC), and blood pressure (BP) in adult patients prescribed atypical antipsychotic medications to facilitate early detection of abnormalities and prompt treatment intervention. PICO Question: For adults with SMI prescribed atypical antipsychotic medications, does flagging charts with the ADA/APA Consensus Guideline Recommendations for Metabolic Monitoring increase provider adherence to the guidelines to facilitate early diagnosis and treatment of metabolic abnormalities? Evidence-based practice models & process: The FOCUS-Plan-Do-Check-Act framework guided development and implementation of a before and after design quality improvement project. Relevant Literature: Despite the FDA Black Box warning for development of metabolic abnormalities in persons prescribed atypical antipsychotics and published monitoring guideline recommendations from the American Diabetes Association, American Psychiatric Association and other prominent organizations in 2004, guideline adherence by healthcare providers remains low. It has been estimated that less than 1/3 of patients who are prescribed atypical antipsychotic medications have undergone testing for blood glucose and lipid levels. Methods: During the nine week intervention period, charts of adults 18 years of age and older prescribed atypical antipsychotics were flagged with an intervention form that contained the ADA/APA guidelines, as a prompt to increase incidence in orders for blood glucose and lipid levels and documentation of WT/BMI, BP, and WC at recommended intervals. Charts were audited weekly to assess guideline adherence. Logistic regression was performed to assess the impact flagging charts with the guidelines had on the presence of orders for blood glucose/lipid levels and documentation of WT/BMI, WC and BP. Outcomes: Improvement in guideline adherence was associated with the intervention, as evidenced by orders for blood glucose and lipid levels present (OR 67.9) and documentation of WT/BMI (OR 6.1), BP (OR 6.4), and WC (OR 67.8) among flagged charts (N = 239). Conclusions: Flagging charts for persons prescribed atypical antipsychotics significantly improved provider adherence to the monitoring guidelines for metabolic abnormalities. Implications for Nursing Practice: Greater guideline adherence facilitates early detection of abnormalities and prompt treatment intervention. Nurse practitioners have the opportunity to be change agents and to play a leading role in diminishing this healthcare disparity. 58 Abstract #033 Title: Inclusion of APRNs as Part of an Interprofessional Rapid Response Team: A Business Case Analysis Authors & Affiliations: Mark Tanner, MNSc, RN; University of Arkansas for Medical Sciences College of Nursing Problem & Purpose: The purpose of this quality improvement (QI) project is to evaluate the advantages to adding APRNs to the RRT at UAMS. PICO Question: Is it strategically advantageous to add APRNs to the RRT at UAMS compared to the current RRT structure? Evidence-based practice models & process: Rogers’ Diffusion of Innovations theory provides the underpinning for this project. This project employs the five phases of this theory (knowledge, persuasion, decision, implementation, and confirmation) to move toward project implementation. Relevant Literature: Five institutions reported lower unplanned ICU admission, in-patient cardiac arrest, and in-patient mortality rates with the addition of APRNs to their RRT (Benson, Mitchel, Link, Carlson, & Fisher, 2008; Kapu, Wheeler, & Lee, 2014; Morse, Warshawsky, Moore, & Pecora, 2007; Scherr, Wilson, Wagner, & Haughian, 2012; Sonday, Grecsek, & Del Casino, 2010) Methods: Unplanned ICU admission, in-patient cardiac arrest, and in-patient mortality rates were calculated for UAMS for the last four years. The average length of stay (LOS) and average cost for ICU admission data were also obtained. ICU admission, in-patient cardiac arrest, and in-patient mortality rates from the literature were averaged and used as a benchmark for UAMS. In addition, a self-report RRT survey was sent to current members of the RRT at UAMS to evaluate perceptions of the RRT by the current RRT members and their willingness to work with APRNs if added to the RRT. Outcomes: Financial savings for UAMS based on a 1.0 APRN FTE added to the MICU team as a pilot were estimated at $127,779 for one year. Results of the RRT survey demonstrated an overall favorable attitude of the current RRT members toward the current RRT state (Chronbach’s alpha 0.756) and a willingness to accept APRNs as part of the RRT (Chronbach’s alpha 0.852). Conclusions: The current RRT members have a favorable view of the RRT in its current state and are supportive of including APRNs as part of the RRT. Including APRNs as part of the RRT has the potential to save money resultant from a reduction in unplanned ICU admissions as well as improve in-patient cardiac arrest and in-patient mortality rates. Implications for Nursing Practice: If fully implemented UAMS could potentially save up to $776,269 by having APRNs available for 24/7 coverage and improve in-patient cardiac arrest and mortality rates. This improvement in patient outcomes will help UAMS as it strategically places itself for the future. 59 Abstract #034 Title: E-cigarettes and pregancy Authors & Affiliations: Nicole Ward, MNSc, APRN, WHNP-BC, UAMS College of Nursing Significance: Electronic cigarettes are an increasingly popular alternative to tobacco cigarettes. However, they are unregulated and their health effects are unclear. They are marketed in a way that makes them appear to be a safe alternative to smoking, which may increase their appeal among pregnant women. There is no research demonstrating their effects on a fetus, and there are no protocols to care for women who use e-cigarettes. Purpose (or Problem): The purpose of this review was to examine the evidence for and against recommending ecigarettes to pregnant women. PICO Question: In pregnant women, do e-cigarettes compared to tobacco cigarettes cause adverse fetal outcomes? Search Strategy & Screening: Literature searches were conducted using PubMed and CINAHL databases. The keywords "electronic cigarette" and "vaping" were combined using “or”. Articles were reviewed and selected based on their relevance to public perception of e- cigarettes, relevance to obstetrics, and relevance to health consequences that potentially effect pregnancy. A secondary search of PubMed using the keywords "nicotine replacement" and "pregnancy" resulted in 176 articles. These results were limited to randomized controlled trials and resulted in eleven articles that were reviewed for this paper. Evidence: Two separate research studies showed that the perception of e-cigarettes is more favorable than cigarettes. Studies of e-cigarettes also show variation in the amount of nicotine consumed among devices, and there is risk of exposure to unknown ingredients. A systematic review showed there was no difference in adverse outcome between smoking and nicotine replacement, but concluded there is not sufficient evidence to recommend nicotine replacement therapy during pregnancy. There are no research studies showing the effects of e-cigarettes on pregnancy health, but one study found that many healthcare providers do not screen and many feel they are safer than tobacco products. Synthesis of Evidence: E-cigarettes may be more appealing to pregnant women who seek an alternative to smoking during pregnancy. There is no research showing the effects of e- cigarettes on pregnancy outcomes, and no protocol for prenatal care in women who use them. Because this is a new phenomenon, healthcare providers may not be screening for use and may not understand how to advise patients on e-cigarette use. Conclusions: There is no research regarding the safety of e-cigarette use in pregnant women. Additionally, the exposure to nicotine is variable between e-cigarette devices, and there is risk of exposure to unknown substances that are potentially harmful. Implications for Nursing Practice: E-cigarettes are a new phenomenon in healthcare, and are marketed in a way that the public perceives them as safer than tobacco cigarettes. Healthcare providers should screen each patient for e-cigarette use and avoid recommending e-cigarettes until their health effects are clear. Patients should be educated regarding the potential risks of e- cigarette use, and offered methods of tobacco cessation that are safe and effective. 60 Abstract #035 Title: Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions Authors & Affiliations: Pamela Holtzclaw Williams, JD, PhD, RN; Charlie Strange, MD; Natalie Dumont BS; Sara Wienke MS, CGC; Susan Flavin MSN, RN; Deirdre Walker, Lucinda Shore MS; Jim Quill, Marvin Sineath, Barbara Warner Background & Significance: Persons living with rare genetic conditions experience social impact related to the conditions’ genetic etiology and rarity. Social impact is poorly understood, characterized, and quantified. A previous conceptual framework describes impact of genetic conditions as “emotional effect” (McAllister, 2007). This report describes thematic domains that we operationally define as “social burden,” identified through systematic qualitative analysis of self-report by persons living with a rare genetic condition known as alpha-1 antitrypsin deficiency disorder (AATD). This disorder is associated with susceptibility to progressive lung and liver disease across the lifespan. Purpose: The aim of this report is to identify and describe thematic domains of social impact experienced by persons living with a rare genetic condition (AATD) and their implications for clinical care, conceptual frameworks and psychometric scale development to quantify social impact of rare genetic conditions. Methods: A community based participatory research (CBPR) partnership of patients, community leaders, clinicians and scientists designed and conducted focus groups and interviews of patients, families and caregivers within the AATD community. A team of four of the partners conducted a systematic qualitative analysis using NVIVO 10 software to facilitate coding, audits, and creating an analysis trail. Results: An inductive approach to coding, abstraction of meaning, categories, and definitions resulted final set of 5 subdomains of impact attributed to the condition’s rarity and 5 sub- domains of impact attributed to the condition’s genetic etiology. The 10 sub-domains of impact and their abstracted definitions support the reference to them collectively as social burden. Conclusions: The social impact of living with AATD can be thematically categorized around the genetic etiology and rarity of the condition. These thematic categories can now support item generation for future scale and psychometric development to quantify levels of burden carried by individuals and communities. Implications for Nursing Practice: Clinical Practice-genetic counselors, nurses, and physicians must consider how their respective practices can improve support of patients with rare genetic conditions such as AATD. Understanding the impact of rarity and genetic information is critical to intervention development and design. The conclusions are now useable to generate items for a future scale to measure social burden in AATD, and efforts to make the items generalizable to other rare genetic conditions. 61 Abstract #036 Title: Perceived Need for HIV Testing among Rural and Urban African American Cocaine Users Authors & Affiliations: Patricia B. Wright, PhD, MPH, RN, UAMS, College of Nursing; Tyrone F. Borders, University of Kentucky, College of Public Health; Brenda M. Booth, UAMS, Psychiatric Research Institute; Xiaotong Han, University of North Carolina Background & Significance: Incidence rates of HIV continue to be disproportionately high among African Americans compared to other races, especially in the South. Although we have some information about testing among African Americans, most surveys do not include homeless, impoverished, or other disenfranchised and therefore hard-to-reach groups, many of whom may be particularly high-risk for HIV infection, and few studies have compared HIV testing among rural and urban African Americans. There is documented high risk for HIV among non-injecting drug users, particularly sexual risk. Purpose: The purpose of this study, therefore, is to address this gap by systematically examining perceived need for HIV testing among rural as compared to urban, non-injecting African American cocaine users. Methods: This is a cross-sectional, community-based study of 400 not-in-treatment African American cocaine users residing in selected rural and urban areas of Arkansas. We used respondent driven sampling methods to fill our sample. Face-to-face computer assisted interviews were conducted in study offices lasting 1 ½ – 2 hours. A logistic regression model was used to examine the association between perceived need for HIV testing and rural/urban residence while controlling for demographic and clinical characteristics. Covariates in the model included: demographics (age, gender, education, health insurance), clinical characteristics (lifetime drug abuse treatment, lifetime mental health treatment, routine health care visit past year, general health status, ever being tested for Hepatitis C or gonorrhea, number of times tested for HIV), access factors (ease of access to HV testing, availability of HIV testing, skepticism towards medical care, stigma for HIV testing) and behavioral risk factors (perceived risk of acquiring HIV, number of sex partners, inconsistent condom use, ever trading sex for foods or drugs). Results: We did not find significant differences among rural and urban African American cocaine users’ perceived need for HIV testing. Female gender, perceived risk for acquiring HIV, stigma, and receipt of testing for other sexually transmitted diseases were each positively and significantly related to perceived need to be tested for HIV in multivariate regression analysis in which all other variables were held constant. Receipt of routine medical care the past year, being tested for HIV from 3 - 5 times, and skepticism towards medical care were negatively and significantly related to perceived need for HIV testing. Behavioral risk factors or general health status were not significantly associated with perceived need for HIV testing. Access to testing was not perceived as a significant barrier to testing. Conclusions: All participants were not-in-treatment, non-injecting drug users, and most reported engaging in risky sex behaviors; however, risky behavior was not associated with perceived need to be tested for HIV. This research underscores the need to reframe HIV prevention programs targeting African American substance users to separate the importance of testing from risky behaviors and to frame testing as taking care of oneself and one’s health. This research underscores the need to reframe HIV prevention programs targeting African American substance users to separate the importance of testing from risky behaviors and to frame testing as taking care of oneself and one’s health. Implications for Nursing Practice: Wellness, promoting health and preventing illness, is one of the four key themes to guide future research identified in the Strategic Plan of the National Institute of Nursing Research. This study provides important preliminary data that will be used to guide development of interventions to prevent HIV disease and promote health and wellness among this vulnerable, high-risk group. 62 Abstract #037 Title: Decreasing Length of Stay in Veterans undergoing a Primary Total Joint Procedure with the Total Joint Academy Pre-Operative Educational Class Authors & Affiliations: Rebecca Effrein RN, MNSC, APRN, AG-ACNPC; Central Arkansas Veterans Health Care System Problem & Purpose: The purpose of this study is to evaluate the newly implemented Total Joint Academy which is a pre-operative educational program for veterans undergoing a primary total joint procedure (hip and knees only) in reducing length of stay. This program was initiated in March 2014 and is strongly encourage for every veteran and their caregiver to attend. PICO Question: Does having the Total Joint Academy decrease length of stay in the veteran population undergoing a primary total joint procedure? Evidence-based practice models & process: The Evidence Based Practice Model provided the framework for this project. Relevant Literature: A CINHAL and Google Scholar search was performed using key words “total joint academy,” “decreased length of stay in total joint patients, “pre-operative education and reducing length of stay.” Two relevant articles were found in regards to decreasing length of stay in total joint patients. One published by the Annals Royal of the College of Surgeons in England found that the mean length of stay in total knee arthroplasties was significantly reduced in the educational group versus the conventional group. The second article published by the Archives of Physical Medicine and Rehabilitation reviewed decreasing length of staff and the effect it had on rehabilitation units. Methods: First, a retrospective review of patients that had their total joint procedure prior to the initiation of the Total Joint Academy December 2013- February 2014 was completed to evaluate their length of stay. Every patient that underwent a primary total knee (n=24) and total hip arthroplasty (n=20) were included. Next, we implemented a multidisciplinary pre-operative educational class for every patient undergoing a primary total joint procedure. This class is not mandatory, however it is strongly encouraged. The academy includes pre- operative preparation, hospital expectations, post-operative pain management, and physical therapy goals for discharge and physical therapy home program expectations. The first academy class took place on March 13, 2014. A retrospective chart review was completed on all patients that had a primary total joint procedure from March 2014- June 2014. The patients were placed in two different groups, being those that completed the academy course (total knee arthroplasty n= 14 and total hip arthroplasty n=7) and those that had not (total knee arthroplasty n =9 and total hip arthroplasty n=6). Outcomes: Prior the Total Joint Academy the length of stay for primary joints was, 2.95 days for total knee and 5.1 days for total hips. During the period of March 2014- June 2014 23 veterans underwent a primary total knee replacement, of that number 9 did not attend the Total Joint Academy and their length of stay was 4.3 days. On the other hand 14 veterans attended the total joint academy and their length of stay was 3.07 days. During that same period, 13 veterans underwent a primary total hip arthroplasty, of that 6 did not attend the total joint academy and their length of stay averaged 4.3 days. However, for the 7 that did attend the total joint academy their length of stay averaged 1.57 days. Conclusions: The results show that having veterans attend the Total Joint Academy prior to the primary joint procedure decreases the length of stay in both total knee and total hip arthroplasty patients. Implications for Nursing Practice: For future research, it would be best to do a retrospective chart review including an entire year since the inception of the academy. At that point not only review length of stay but post-operative goals met, hospital readmission rates, transfers to rehab and complications after surgery. Veterans who chose not to attend the Total Joint Academy should be surveyed to determine their rationale for not attending. This information may be used to improve attendance rates. 63 Abstract #038 Title: Diversional Activities to Decrease Harmful Behavior in Patients with Dementia Authors & Affiliations: Rebecca Lyle, BSN, RN; Rachael Powers, BSN, RN; Roselyn Whitmore, BSN, RN; Central Arkansas Veterans Healthcare Systems Significance: ElderlyVeterans with dementia frequently display harmful behaviors while hospitalized. Staff members providing care are experiencing role strain without adequate resources. Purpose (or Problem): This review was conducted to determine the effectiveness of diversional activities for Veterans with dementia in order to decrease -harmful behaviors. PICO Question: Does implementing diversional activities for geriatric Veterans with dementia decrease -harmful behaviors? Search Strategy & Screening: The literature search was conducted through CINAHL and EBSCO. Search terms included dementia, self-harm behaviors, diversional activities, non- pharmacological therapies, disruptive behaviors, recreational activities, and dementia-related behavior using the Boolean operator AND. Screening addressed description of disease process, use of diversional activities in various settings, and similar populations. Evidence: Initial results produced over 1,000 articles. Articles from outside the United States, as well as articles unrelated to the PICO question were omitted. A total of 18 review articles were included within this Evidence-Based Literature Review. Synthesis of Evidence: Team members cared for a Veteran with dementia under 1:1 constant observation who demonstrated harmful behaviors. The Veteran was given an imitation tool box to engage in a meaningful activity as he was known to like to “fix things”.” This activity gave the Veteran purpose and meaning. Over time the Veterans behavior settled to the point where close observation was discontinued & the Veteran was discharged home. It has been observed that many Veterans in our care benefit from different diversional activities. Conclusions: “Strategies, such as redirecting, activities, or limiting external stimuli, can be implemented to maintain patient safety” (Taft, 2013. p. 2). Implications for Nursing Practice: Based on evidence, “…effective management of disruptive behaviors has the potential to improve quality of life; decreased caregiver burden, burnout, and turnover; and decrease the use of restraints, and institutionalization of psychiatric hospitalization. As a result, it would likely decrease cost of care over time.” (Curyto, Trevino, Ogland-Hand, & Lichtenberg, 2012. p. 200) 64 Abstract #039 Title: Safe Flow Rate Nipple Selection for NICU Infants, Post Discharge Use PHASE II Authors & Affiliations: Carol A. Camp, MS, CCC-SLP; Jackie Davis, MS, CCC-SLP; Rebecca P Sartini, MSN, RNC-NIC; UAMS Rehabilitation Department & NICU Problem & Purpose: The problem remains that disposable hospital slow flow nipples used in the NICU are not available in commercial stores, making them not available to NICU families after discharge. Commercial slow flow nipples are variable by brand in flow rates, making it difficult to recommend nipples in acute care and after discharge, potentially increasing the risk for aspiration. There is a lack of evidence regarding the varying flow rates of commercial nipples versus disposable nipples with both breast milk and formula. The Phase I study ascertained the average flow rate of a variety of readily available slow flow nipples to assist clinicians in determining the most appropriate nipple in order to provide guidance to parents after discharge. The purpose of Phase II is to prove reliability to the findings in Phase I, thus supporting the validity of the Nipple Flow Rate Continuum. PICO Question: In the NICU population, does the use of a nipple with an appropriate flow rate, as opposed to randomly recommending commercial slow flow nipples, improve consistency in recommendations for safe feeding practice during the NICU stay and for post discharge use. Evidence-based practice models & process: UAMS EBP model Relevant Literature: Current literature supports that flow rate has an effect on safety and efficiency with oral feeds. Literature also supports that higher flow rates can increase aspiration potential in infants with an already compromised suck-swallow-breathe pattern. It is widely documented that flow rate is a factor in safe feeding; however, there is limited research on the variability of nipples labeled slow flow. The current literature reveals that cue based feeding supports oral feeding development and safe swallow function while maintaining and meeting their nutritional needs. Methods: Commonly used commercial nipples were chosen for investigation, as well as the hospital slow flow product. Each nipple type will be tested using a Medela Symphony Breast Pump 2.0 set at the suction rate of 150mm Hg to simulate the sucking action of an infant. The infant nutritionals to be tested include: 20 kcal donor breast milk, 20 kcal formula, 22 kcal formula, and 24 kcal formula at room temperature. The exact amount of liquid transferred from the nipple to the collection bottle from this consistent pumping method will be recorded after 1 minute duration. All nipples will be tested for 5 pumping sessions and data gleaned from the average of the total amount will be documented for comparison. T-Test will be performed on both Phase I and Phase II results as independent groups to support the reliability of the Nipple Flow Rate Continuum developed in Phase I. Outcomes: Pending Conclusions: Promoting safer feeding practices decreases the risk for aspiration leading to improved infant feeding outcomes. These outcomes include: reducing length of stay, assist in the prevention of future oral aversion, feeding dysfunction, persistent respiratory illness, and decrease risk for hospital readmission rates. Typical nipple recommendations are based on the clinician’s clinical experience with different types of nipples, which can be subjective. With the use of the validated Slow Flow Nipple Rate Continuum, recommendations will move from being subjective to objective, based on the appropriate flow rate, which has been proven to promote safe feeding practices and optimal feeding outcomes. Having objective Speech Language Pathologist slow-flow nipple recommendations can promote more consistent nursing and family compliance, improving multidisciplinary feeding practices. Implications for Nursing Practice: Implications for nursing practice include enhancing autonomy for nursing through an evidence based approach to safe feeding of high-risk infants, feeding progression, ultimately optimal feeding outcomes. With appropriate multidisciplinary feeding recommendations, nursing can provide and support optimal feeding practices leading to improved parental education promoting continuity of care after discharge. 65 Abstract #040 Title: Early Prone Positioning: Why Wait for ARDS? Authors & Affiliations: Race Shelby, BSN RN; Central Arkansas Veterans Healthcare System Significance: As a vital role in the interdisciplinary healthcare team, nurses use autonomy, nursing judgment, and nursing interventions every day to improve patient outcomes. They are responsible for being the first line assessors, thus preventing worsening of illness. By acting quickly and independently, nurses can improve results, decrease hospital stay, and decrease costs associated with pneumonia and ARDS. Evidence shows that placing a patient with ARDS in prone position increases oxygenation, but a lack of evidence in pneumonia patients indicates the need for more research in this population. There is currently no specific protocol or training at CAVHS for placing patients in prone position who have pneumonia and early signs of respiratory distress. This lack of training and knowledge decreases consistency of care among nursing staff. Purpose (or Problem): The purpose of this literature review is to show the need for a clinical case and pilot study. PICO Question: In patients with pneumonia, does prone position with chest physiotherapy increase oxygenation and prevent condition from progressing to acute respiratory distress syndrome? Search Strategy & Screening: The literature search process used Cinhal and Google Scholar. Search terms used to locate the appropriate literature were pneumonia, prone position, and lung injury. Evidence: The literature search produced an initial total of 453 studies. Studies were eliminated if they involved children, animals, or used some adjunctive other than prone positioning. A total of 5 studies were reviewed to implement this study. According to the American Lung Association (2016), ARDS is sudden respiratory failure after an initial injury, pneumonia listed as one of the top lung injuries. Prone positioning is used in ARDS patients to improve oxygenation and prevent lung injury from mechanical ventilation (Guérin et. al. (2013). Guérin (2013), indicates the improvement caused by prone positioning comes from reducing intrapulmonary shunting and bettering V/Q mismatch. Pascal Beuret (2001) showed a progressive worsening of oxygenation in supine patients verses prone patients. This was thought to be due to alveolar collapse in the dorsal lung region, the region of the lungs with higher alveolar surface area. Synthesis of Evidence: By taking the results from ARDS research and transposing it to pneumonia patients, nurses can possibly better the outcomes in the pneumonia patient population and prevent further lung injury. Conclusions: After the review of literature, a pilot study using evidence-based research should be developed to show the benefits of prone positioning in pneumonia patients. The pilot study would be used to develop a protocol and bundle to standardize nursing care in these patients. Implications for Nursing Practice: The evidence suggests that prone positioning increases oxygenation in patients who have problems keeping blood oxygen saturations at appropriate levels when the primary cause is in the pulmonary system. A pilot study, in combination with published literature, would standardize nursing care in this patient population. 66 Abstract #041 Title: Evaluation of Implementation of an Influenza Cocooning Practice in the NICU for Infant Household Caregivers Authors & Affiliations: Rebecca K. Smith BSN, RNC-NIC, Sharon V. Wilhelm BSN, RNC-NIC, Rebecca P. Sartini MSN, RNC-NIC Problem & Purpose: Influenza poses an increased risk for hospitalization and mortality among infants less than six months of age. Since these infants are not licensed for administration of influenza vaccine their mothers and other household members are asked to be vaccinated against the influenza virus to provide a cocooning effect from the virus. As NICU infants are at increased risk, cocooning is especially applicable to prevention of viral transference from family members. The purpose of this project is to evaluate participation rates of a five year influenza cocooning program that provided the NICU infants’ mothers and household members the influenza vaccine. PICO Question: In NICU mothers and family members, does a household caregiver participant seeking administration of the influenza vaccine, as opposed to professionals actively seeking participants in the program, promote a larger population of cocooning participants. Evidence-based practice models & process: The UAMS EBP Model provided the framework for this evidence-based practice project. Relevant Literature: The project team included staff RNs who performed a literature review (which included national professional practice recommendations, institutional examples and quantitative meta- analysis) that revealed evidence for influenza vaccine administration to families/caregivers in neonatal intensive care units . The American Academy of Pediatrics and the Center for Disease control recommend that caregivers/family member obtain the influenza vaccine in order to increase the potentiation effect of cocooning in all infants less than six months of age. Methods: Over 5 years, during influenza season, the NICU at UAMS offered free influenza vaccines to all mothers and family members in their households. This program was advertised with signage placed throughout the unit and family areas, encouraged by physicians and nurses during rounds with families, and the importance of this cocooning during parent teaching at the bedside. The first two years, a group of select nurses was assembled, and performed room to room rounds with families to consent and then provide the vaccination. The subsequent three with the same advertisement format was followed, however, when parent or family member requested, nurse volunteers consented, performed the vaccinations, and completed all the necessary paper work in collaboration with the infection control nurse for the hospital. Outcomes: For the following timeframes the results of consented vaccinations to mothers and household family members are: Fall 2009 through Spring 2010(185), Fall 2010 through Spring 2011(200), Fall 2011through Spring 2012(121), Fall 2012 through Spring 2013 (147), and Fall 2013 through Spring 2014 (192). It was evident that the process of active solicitation of participants room to room with a vaccination cart was more effective than the passive provision of influenza vaccination as requested by mothers and household family members. Conclusions: The five year cocooning program at UAMS has gleaned data to support that the active solicitation room to room has been more successful in producing a larger number of participants to support cocooning for the NICU infant after discharge. This was evident in the plummet in participation rates at year 3 and 4, recovering close to baseline at year 5. Implications for Nursing Practice: As the literature supports, to take infant protection from influenza one step further through the provision of vaccinations to mothers and household members has been proven effective. It is vital that the UAMS NICU play a major role in the education of family members regarding disease prevention. Since infants less than 6 months of age cannot be immunized nurses and physicians play a vital role in encouraging families to provide this cocooning affect to one of the most vulnerable at risk populations. Continued research data should be gathered to confirm the theory that active solicitation of NICU household members is a more effective approach. 67 Abstract #042 Title: World Peace and the Standardization of Arterial Lines in a Pediatric Hospital in Arkansas Authors & Affiliations: Sharon Barron, BSN, RN, Jerril Green MD; Arkansas Children's Hospital (ACH) Problem & Purpose: In an effort to support the EBP of standardization, ICU Group Council in collaboration with ICU Committee united to create a standard arterial line monitoring system that would be compatible for patients in all acute care settings at ACH, promoting safety through decreased infections, increasing overall cost effectiveness, and advocating family Centered Care by customizing the 7 current systems into one. PICO Question: Does standardization of arterial lines for patients in an acute care setting decrease blood stream infections compared to current arterial line policies and practices? Evidence-based practice models & process: The Iowa Model of Research use provided the framework for this Evidence Based Practice project. Relevant Literature: The Project team comprised of Acute Care professionals reviewed literature (including randomized controlled trials, systemic reviews, and National professional practice guidelines) and found evidence that supported standardization of practices with closed monitoring systems. Furthermore, literature showed that the use of pressurized valves had increased infection rates, and split septum sampling sites had lower infection rates. (Jarvis et all, 2009) Methods: Through careful review of literature, ACH’s Policies and Procedures, and collaborative meetings with Medical Directors of the acute care settings, a standard model of practice and product for arterial line management and monitoring was developed for trials. The standard product was developed from 7 different monitoring systems at ACH. The first objectives set for trialing in the PICU included a closed monitoring system that allowed for conservative blood sampling and the universal delivery of volume, based on weight via the smart pumps. Outcomes: After a 6 month trial in PICU, the test of change influenced the creation of a 2 bag monitoring system with split septum sampling sites that met all of the objectives set forth. A meeting with vendors created custom dueling kits that were trialed in PICU and CVICU. Evidence collected and feedback secured a final schematic from one vendor which was opened up for trials to ALL the ICU’s, CVOR, and the OR over the next 3 years. In 2011, 2012, and 2013 bloodstream infection data from ACH does suggest a possible link between the standardizations and decreased infection rates however, further data collection and survey are needed to support the link. Conclusions: Throughout the trials and revisions of practice, a closed monitoring system was developed that adapted to every patient population in acute care settings at ACH and became the standard for ALL transduced lines. As a result, standardization and the education of one practice increased patient safety through decreased infections, increased cost effectiveness with one custom kit for all transduced lines, and advocated family centered care. Implications for Nursing Practice: Vendors across the nation have closed arterial monitoring systems for neonatal, pediatric, and adult populations but ACH is the gold standard for one custom kit throughout the hospital for all populations in the acute care settings. 68 Abstract #043 Title: Utilization of an interdisciplinary (ID) team to expand programming within an inpatient dual diagnosis programquality improvement project. Authors & Affiliations: Stephanie Burnett, BSN, RN; Connie Jordan, MSN, MHA, RN, CPAN; Central Arkansas Veterans Healthcare System Problem & Purpose: Current treatment programming within the dual diagnosis unit has proven successful; however, evidence suggests that improved outcomes may also be achieved with the addition of evidence based material/treatments. The purpose of this EBP was to examine the process of implementing new material and piloting new classes within the programming of a dual diagnosis unit using an interdisciplinary group. PICO Question: For improvement in dual diagnosis programs, does ID involvement with program revisions (versus single discipline involvement), promote greater generation of ideas to improve program? Evidence-based practice models & process: The framework provided for this EBP included the Iowa Model of Evidence-Based Practice. Relevant Literature: This project’s ID team included a psychiatrist, psychologist, chaplain, social worker, and 3H nursing staff (RN/LPN). The team reviewed the literature including national professional practice guidelines and recommendations, qualitative studies, and quantitative studies. Evidence suggests that an ID team is better able to generate effective, sustainable programs in healthcare. The ID approach is more conducive to the discovery of multiple problems of the patient, as well as provide more interventions than a single field of discipline (Slack et. al. 1999). Wood et. al. 2013 states, the impact of reaching for quality improvement itself increases positive patient outcomes. The Joint Commission recommends the ID team be involved in process of changes. Methods: All staff on the unit were educated and encouraged to participate in the ID group. The team evaluated previous patient satisfaction surveys to understand where improvements should be made. The group meets monthly to review changes, discuss pilot programs and progress of additional classes implemented, and present new ideas. Material used in all current classes was revised including additional of material based on recommendations from SAMSHA and one new class, gardening, was added. The changes and additions have helped the program become more patient-centered and the patients are better able to tailor the program to their own needs based on personal objectives and goals. Outcomes: The program is more patient-recovery-oriented with more individualized education. When surveyed, the piloted class received a score of 100% in helpfulness. Patients stated they recognize the value of and felt encouraged to continue participation in leisure activities in their daily lives due to success in gardening classes. Classes with revised educational material scored 88.89%-100% in helpfulness. Conclusions: Although the ongoing results of this project may not be generalizable to populations other than the dually diagnosed patient receiving inpatient programming, involving an ID team may be beneficial when generating sustainable new ideas for programming. Implications for Nursing Practice: Additional research with implementation of new classes with input from the ID team should continue to be evaluated. 69 Abstract #044 Title: Perceived Health Status and Self-Efficacy of Adult Survivors of Pediatric Orthotopic Heart Transplant: Pilot Study Authors & Affiliations: Laura Hays, Jean McSweeney, RN, PhD, FAHA, FAAN; University of Arkansas for Medical Sciences College of Nursing Background & Significance: Advanced surgical procedures in the past 30 years have resulted in a new chronic conditions population in adults with congenital heart disease (ACHD). The survival rate to adulthood for ACHD patients has increased from 25% to more than 95%. This population lacks mentorship or tested interventions for increased selfmanagement abilities. Purpose: The purpose of this pilot study was to evaluate recruitment strategies and data collection instruments for the measurement of perceived health status and self-efficacy in adult patients who received orthotopic heart transplant as pediatric patients. Methods: This descriptive, cross-sectional pilot study used a 28 item questionnaire to examine self-rated health, health care utilization, health distress, illness intrusiveness, and exercise behaviors in patients 18 years or older who received orthotopic heart transplant under the age of 18 and at least one year ago. IRB approval was obtained from the University of Arkansas for Medical Sciences. Patients were excluded from the study if they had a comorbidity or neurological injury, either related to the transplant or not, which prevented the patient from understanding or completing the questionnaire, or they had received more than one orthotopic heart transplant. Questions and related psychometric data were obtained through the Stanford Patient Education Research Center. Purposive sampling was used to identify 15 patients meeting the specific inclusion and exclusion criteria, with recruitment at the Arkansas Children’s Hospital transplant clinic on days that orthotopic heart transplant patients were seen for follow- up. Results: Data were collected from a total of 15 individuals with ages ranging from 18 to 37. Transplants occurred between 6 and 21 years ago with age at transplant from 1 month to 17 years old. Descriptive frequency scores showed that most participants reported little or no health distress. Ninety-three percent of participants rated their general health as good, very good, or excellent, and none reported requiring home health services; however, despite little illness intrusiveness, most participants were not currently employed (86.7%) and/or lived with parents (73.3%). Conclusions: This small pilot study identified a lack of successful transitioning to adult self- management in adult participants who received orthotopic heart transplants as children. Self- management skills are important components of self-care in the ACHD population. Because of this, interventions are needed to increase these skills beginning in adolescence and focusing on disease education, communication skills, and increased self-efficacy. Planned future studies will examine 1) self-efficacy in an ACHD sample with an array of congenital heart defect diagnoses and 2) overall ACHD transition from pediatric to adult care status in the United States. Implications for Nursing Practice: An informed and educated patient will have more success in the development and utilization of the skills necessary for effective self-management of physical, emotional, and psychosocial aspects of his/her chronic disease process. Successful transition to adult care for these patients should begin 5 to 7 years before actual transfer to ACHD care with adult providers to allow both parent and patient preparation for the patients’ assumption of care responsibility. 70 Abstract #045 Title: Improving Infection Control Practices in a Long Term Care Facility through a Quality Improvement Project Authors & Affiliations: Joshuah Lingo, Claudia Beverly, PhD Carol Compas, BSN RN, CPHQ ; University of Arkansas for Medical Sciences Background & Significance: Residents of long-term care facilities (LTCFs) are a high-risk population for acquiring health care-associated infections. Current research reveals between one to three million health care associated infections occur annually in this population, contributing to nearly 400,000 deaths each year, and increasing rates of re-hospitalizations. Healthcare providers in LTCFs can help to greatly reduce the spread of multi drug-resistant organisms, C. difficile, and catheter-associated urinary tract infections when properly trained. The development of staff education programs is crucial to reinforce the use of standard precautions to help prevent the spread of infection. Purpose: The purpose of this quality improvement project was to create a culture of safety for residents in a LTCF by improving infection control knowledge. Methods: The setting for this project was a 116-bed licensed LTCF with a staff of 110. The population of interest was a random sampling of licensed and unlicensed nursing staff, dietary personnel, and environmental service staff. General observation methods were initially used to formulate a knowledge survey and design an infection control (IC) education program tailored to the needs of this project facility. Observations were performed on two occasions to visually assess hand hygiene (HH) and IC practices throughout the facility. Random staff members were interviewed during observation rounds to determine current level of knowledge about HH/IC policies and procedures. A knowledge assessment was developed for a pre- and post-test study design along with a 20-minute IC in-service. The knowledge assessment included 5 questions with multiple-choice answers. The in-service included evidence based practice (EBP) for IC limited to HH, proper use of personal protective equipment, and general spread of infectious disease. Seven in-services were conducted for day, evening, and weekend personnel. Approximately 30% of the nursing facilities staff was used as sample for this study. Results: Results: 32 staff members attended one of the seven scheduled in-services. Overall scores and individual questions were evaluated for each participant. The overall average scores 37.5% (range 6.3-59.4%) and 85.6% (range 68.8-96.9%) for pre- and post-test, respectively. Employees were observed using alcohol hand gel properly after the in-service and were much more engaged in the idea quality improvement through EBP best practices. Staff comments acknowledged improved knowledge and a need for frequent reinforcement. Conclusions: A quality improvement study tailored to the needs of target participants can improve both knowledge and practice. Long-term care providers need continuous and on-going education on current evidence based practices regardless of their licensure, certification, or position to create an overall culture of safety. Implications for Nursing Practice: The data shows that reinforcement in-services can help improve knowledge deficits among staff and that dissemination of current EBP is not wide- spread throughout LTCFs. This study reveals that education programs tailored around the needs of the individual facility can ensure survey compliance with IC regulations, improve quality of care for LTCF residents, and potentially reduce morbidity and mortality related to healthcare-associated infections. 71 Abstract #046 Title: A Qualitative Pilot Study: Nursing Workplace Environment and Nurses’ Perspectives on Patient Outcomes Authors & Affiliations: Elizabeth Sloan Davidson MSN, RN, CNE, Patricia Wright, PhD, MPH, RN; University of Arkansas for Medical Sciences Background & Significance: The success of the nursing care is measured by patient care outcomes. The literature regarding hostile nursing work environments suggests a problem that may have direct impact on patients. The majority of studies focus on new nurses or on bullying behaviors portrayed by those in power positions, such as physicians and nurse administrators. The purpose of this qualitative pilot study is to interview acute care staff nurses with at least three years experience in nursing and at least one year in the current job to gain information on their perspectives of how the work environment directly impacts patient care outcomes. Purpose: The purpose of this qualitative pilot study is to interview acute care staff nurses with at least three years experience in nursing and at least one year in the current job to gain information on their perspectives of how the work environment directly impacts patient care outcomes. Methods: Purposive sampling was used for this phenomenological inquiry. Participants for this pilot study were recruited from one large metropolitan hospital via internal email. An interview guide was utilized to conduct a semi-structured individual interview in the participant’s choice of private venue. Interviews were recorded, transcribed verbatim, and entered into Ethnograph 6.0 software. Using constant comparison and content analysis, a codebook was constructed. General themes were identified, and then further broken down into categories for analysis. Results: The sample for this pilot study included three participants. All participants worked in an acute care, inpatient setting. Five themes and fourteen categories were identified: 1. The Good (staff nurses have good ideas and positive nurse leaders), 2. The Bad and the Ugly (nurse bullies, nurse victims, nurse bystanders, tried it, other issues, physicians), 3. Patient Care (what it should be and sometimes is and what it should not be and sometimes is), 4. Are You on the Team or not (teamwork and there’s no “I” in team) and 5. It’s the Little Things that Count (provision of basic care and sentinel events: important yes, but basic care is often neglected). Conclusions: There are multiple issues that affect the ability of the nurse to perform at optimal level for the best patient outcomes. Bullying behaviors lead to a breakdown in the vital function of teamwork and collaboration in today’s high acuity, high tech healthcare world. Implications for Nursing Practice: There are multiple issues that affect the ability of the nurse to perform at optimal level for the best patient outcomes. Bullying behaviors lead to a breakdown in the vital function of teamwork and collaboration in today’s high acuity, high tech healthcare world. More research must be conducted with experienced nurses to navigate the feasibility of potential interventions aimed and breaking the bullying cycle in nursing. 72 Abstract #047 Title: Identifying Gaps between Resources and Parents with Children Diagnosed with Autism-A Pilot Study Authors & Affiliations: Leah Richardson, Dr. Patricia Wright; University of Arkansas for Medical Sciences Background & Significance: Autism spectrum disorder is among the chronic conditions of early childhood that is suspected to be of genetic in etiology and results in developmental disabilities. Autism affects one in 68 children and occurs in all racial, ethnic, and socioeconomic groups. Boys are at of up to 5 times rate higher of being diagnosed with autism than girls. As a result, parents are faced with decisions about their child’s care in regards to getting the right diagnosis and treatment, and seeking information to assist in coping with the autism diagnosis. Purpose: The purpose of this study was to understand parents' use or lack of use of available resources to help them cope with having a child diagnosed with autism Methods: Five individual parents, English speaking were recruited (ages 18 years and older), who had at least one child diagnosed with autism, were recruited for an IRB-approved descriptive study. Perceptions of their child’s diagnosis, resources and obstacles parents faced were measured by one-on-one interviews (qualitative design). Following informed consent, audio recording began and consent was verified. Participants completed the interview within 30 minutes. Results: Major themes that emerged were: 1) Denial-delaying diagnosis or denial, resulting in a delay of receiving resources after the diagnosis is made by parents, family, and physicians; 2) Information that helped or hindered after the diagnosis of autism was made. Internet and resources from physician were mentioned to be both barriers and facilitators; and 3) Consequences, the parents faced, from having a child with autism, that affects resource availability. Isolation and anger/grief emerged from consequences as perceived by the parents interviewed. Conclusions: Parents with children diagnosed with autism have multiple barriers, both internal and external, to receiving resources they need to assist in coping after a child’s diagnosis of autism. The impact of the diagnosis is felt throughout the family and community. Parents need direct instructions on ‘what is next’ and ‘who is out there to help’. Implications for Nursing Practice: Parents, who have children with autism, do not face challenges just at the time of diagnosis. The challenges can extend to all developmental milestones missed or fear the parent has in regards to the challenges their child will face in the future. Tailored instructions to new parents of a child with autism are needed to assist the child in receiving early intervention services, and to assist the parents in coping with the challenges of having a special needs child. 73 Abstract #048 Title: Content Validity Methods Applied to New Psychosocial Scale for Social Burden in Rare Genetic Conditions Authors & Affiliations: Natalie Dumont, BS, Pamela Holtzclaw Williams, JD, PhD, RN; University of Arkansas for Medical Sciences College of Nursing Background & Significance: A community based participatory research partnership, Alpha-1 Community Research Partnership, used focus group, interview and Photovoice data to develop social burden domains in adults with Alpha-1 Antitrypsin Deficiency (AATD). The operational definition for social burden during qualitative methods was “hardships, challenges, frustrations and duties related to interactions within social settings related to their condition.” From qualitative thematic analysis, two social burden domains emerged: rarity and genetic etiology, each with respective subdomains. The partnership generated items to elicit responses that measure levels of burden perceived around rare disease experimental domains. Items were then ready for content validity evaluation; rating how item content represented domain(s) being measured within a scale. Purpose: Evaluate Burden Scale item content validity (I-CVI) and determine scale content validity (S-CVI) Methods: Alpha-1 Community Research Partnership (A1CRP) nominated 9 professionals in expert rater round one. The nominees included 6 Alpha-1 community leaders, 3 professionals in pulmonology, genetics and psychosocial issues. Expert raters received the scale, domain table and scale questionnaire for rating item relevance to its proposed domain. A1CRP nominated four different professionals for the expert raters round two. Nominees included a genetic counselor, advanced practice registered nurse with genetic expertise, medical doctor specializing in rare lung disease and a psychosocial investigator. Nine expert raters evaluated 71 items in the first round of content validity calculation. 33 of the 71 items fell below an item CVI (I-CVI) of 0.78. Mean item content validity for the scale was 0.831, the scale CVI (S-CVI) 0.5149; mean expert proportion (S-CVI/Ave) 0.8310, and I-CVI range 0.44-1.0. A1CRP revised scale items using expert rater feedback. A second round of professional expert raters (n=4) rated 104 items. 3 out of 4 experts agreed on 95 of the 104 items. A small set of items needed special attention due to outlier response. Results: 95 total items were rated valid with an I-CVI > 0.78. Content validity of the scale (S- CVI) is 0.9784. All calculations and data analysis conducted in Microsoft Excel. Conclusions: Two rounds of expert rating and item revisions yielded acceptable content validity index. The scale underwent field testing in the Alpha-1 Antitrypsin Deficiency Disorder (AATD) community via the AATD research registry. Implications for Nursing Practice: Validated Burden Scale will be disseminated across other rare disease communities to measure social burden levels. 74 Abstract #049 Title: Older Adults Who Exercise Display Lower Temporal Discounting Rates Than Non- Exercisers Authors & Affiliations: Linda Tate, Paofeng Tsai, PhD, RN; University of Arkansas for Medical Sciences School of Nursing Background & Significance: As our nation’s population ages, the rates of chronic illness and disability are expected to increase significantly. Despite the knowledge that exercise may prevent chronic disease and promote health among elders, many still are inactive. Factors related to exercise behaviors have been explored in recent years. However, temporal discounting is a motivational concept that has not been explored in regards to exercise in elders. Temporal discounting is a decision making process by which an individual chooses a smaller more immediate reward over a larger delayed reward. Purpose: The purpose of this study is to determine if temporal discounting rates vary between exercising and nonexercising elders. Methods: Design. This study used a non-experimental correlational design. Sample. After completion of screening for eligibility with 151 potential participants, 137 cognitively intact older adults completed the study. Inclusion criteria were 1) community dwelling, and 2) adults 60 years of age and older. Exclusion criteria were 1) cognitive impairment, based on the 6-item Memory Screen and 2) the inability to exercise because of physical impairment, based on the Exercise and Screening for You (EASY) tools. Demographic form. Due to its validity and reliability, the Behavioral Risk Surveillance System (BRFSS) was used to gather data regarding age, race, gender, marital status, education and income status. Yale Physical Activity Survey (YPAS). This study only used the vigorous activity index (VAI) in part two. For participants to be considered an exerciser, they had to score a minimum of 20 with at least a 3 for the frequency section, meaning they exercised 3-4 times per week. Kirby Delay-discounting Monetary Choice Questionnaire (MCQ). The MCQ is a 27-item questionnaire that was shown by Kirby (2009) to valid and reliable in measuring discounting rates. No monetary rewards were issued to the participants making the MCQ purely hypothetical to the participants. Statistical analysis. Univariate analysis was performed to describe the sample. To compare discounting rate between elderly exercisers and non-exercisers, data were analyzed but tests for normality were not met. Therefore, the Mann-Whitney test was used. Results: Participants’ mean age was 65.26 (SD 4.51). Female (60.6%) and Caucasian (77%) are the majority. Eighty-nine percent of participants completed high school education. The results of the study revealed that exercising older adults display lower temporal discounting rates than non-exercising older adults with (W = 1679, p = 0.00406,) indicating older adults who participated in exercise chose a delayed larger reward as opposed to a smaller immediate reward. Conclusions: Exercisers tend to view that long term healthy rewards are more important than short term pleasures, such as watching TV or other sedentary activities. Non-exercisers tend to choose more immediate rewards or pleasures such as watching TV over the long term health benefits of exercise. Implications for Nursing Practice: These findings are significant as several chronic health conditions relate to lack of exercise especially in older adults. If we can promote exercise by offering discounting individuals some type of immediate reward such as money or gift cards then we can improve exercise behaviors in many elders. If we can find the right immediate rewards to provide to discounting elders, we can create programs that will get and keep them involved in exercise, which potentially will improve their health. 75 Abstract #050 Title: Adverse Events and Retinopathy of Prematurity Eye Exams Authors & Affiliations: Jennifer Orahood, Dr. Anita Mitchell, PhD, APRN Stephen Erickson, PhD, Howard Hendrickson, PhD; University of Arkansas for Medical Sciences Background & Significance: To screen for retinopathy of prematurity (ROP), eye examinations are performed on infants who weigh less than 1500 g at birth, are born at gestational age of 30 weeks or less, or have a history of instability. The ROP exam is first performed when infants are 4-6 weeks old. The importance of ROP is based on early detection of retinal detachment in preventing blindness. The eye drops used in ROP exams, Cyclomydril, have two active ingredients: cyclopentolate 0.2% (similar to atropine) and phenylephrine 1% (an adrenergic). A preliminary study found elevated blood cyclopentolate levels in 18 preterm infants indicating that the drug is absorbed systemically. Purpose: The purpose of this study was to determine the association between cyclopentolate levels in preterm infants and the incidence of adverse events (bradycardias, oxygen desaturations, gastric residuals, other gastrointestinal (GI) complications, apnea, and neurological events). Methods: A retrospective chart review was performed to count frequency of adverse events the day before and the day of the eye exam. Chart reviewers were blinded to the infants’ cyclopentolate levels. Two researchers reviewed the charts for 100% inter-rater reliability. For chart review purposes, bradycardia was defined as heart rate less than 80 beats per minute. Oxygen desaturation was defined as pulse oximetry reading less than 80%. Staff nurses recorded gastric residual levels before each tube feeding. Results: After the ROP exam, 72% of infants experienced an adverse event. Cyclopentolate levels were higher in infants on oxygen (p=0.014). There was no statistically significant association between cyclopentolate levels and cardiorespiratory events. There was an association between cyclopentolate levels and gastric residuals in infants after controlling for patient-on-oxygen (p=0.012). Other adverse events recorded include vomiting, apnea, and abnormal sleepiness. Conclusions: Cyclopentolate levels vary in infants following ROP exams. Adverse events are common and include bradycardias, oxygen desaturations, increased gastric residuals, other GI complications such as vomiting, apnea, and neurological events such as abnormal sleepiness. Implications for Nursing Practice: Nurses need to be aware that adverse events are common following ROP exams and pay close attention to infants on the day of their ROP exam. Infants need careful monitoring following their ROP exam whether the exam occurs in the hospital or in the outpatient setting. 76 Abstract #051 Title: DEVELOPMENT OF A FALL INJURY PREDICTION MODEL Authors & Affiliations: Amy Hester, BSN, RN, BC, Pao-Feng Tsai, PhD, RN; University of Arkansas for Medical Sciences College of Nursing Background & Significance: Although there has been significant progress of evidence based practice in the last decade, falls remain the most commonly reported adverse events in hospitalized adults. A majority of research has focused on fall prevention and fall prediction with far fewer studies focusing on injurious falls specifically. While previous research has resulted in validated tools used to predict falls, no tools that specifically predict the risk for injurious falls have been scientifically developed. Purpose: The aims of this study were to examine the association of patient factors and injurious falls and determine if any of these factors are predictors for falls resulting in injury. Ten potential predictor variables were examined in this study including (a) age, (b) gender, (c) fall history, (d) use of diuretics, (e) use of central nervous system (CNS) medications, (f) cognitive impairment (CI), (g) primary discharge diagnoses, (h) abnormal laboratory values, (i) impaired mobility, and (j) body mass index (BMI). Methods: Secondary Data Analysis using t tests and Chi Square analysis to measure associations between identified patient factors and injurious falls; logistic regreaaion to measure which patient factors were predictors of injurious falls. Results: Of the 1,369 falls examined in this study, 381 (27.8%) resulted in some form of injury. A total of 622 females (45.4%) and 747 males (54.6%) comprised the study sample. The mean age for all subjects was 55.1 years. Patients with a primary discharge diagnosis of symptoms, signs and ill-defined conditions had significantly higher odds of experiencing an injurious fall (OR=1.74; 95%CI=1.03-2.94; p=0.037). This association remained significant while adjusting for other predictors in the logistic regression model. Conclusions: Findings here also suggest that clinical decisions on which patients need injury prevention interventions should not focus solely on the aged, females or those with a previous history of falling. In addition, patients receiving CNS medications, those with abnormal laboratory values with bleeding times and those who are underweight warrant close observation for protection against fall related injury as considerable percentages of these patients suffered injury. These findings also lay the foundation for future research aimed at developing a model to predict injurious falls. Implications for Nursing Practice: Results of this study suggest clinicians should pay particular attention to patients with a primary diagnosis of symptoms, signs and ill-defined conditions as these patients may benefit from injury prevention interventions. Diagnoses classified in this category are symptoms that either point to more than one disease or system or are signs and symptoms with an unexplained etiology. Patients having a primary discharge diagnosis of “symptoms, signs and ill-defined conditions” are admitted specifically because their symptom is the reason for the hospitalization and either a more precise diagnosis could not be made or they were admitted for the sole purpose of treating the symptom without treatment or further evaluation of the underlying disease (AHA, 2008). Symptoms, signs and ill-defined conditions include conditions such as nausea and vomiting, malaise and fatigue, sleep disturbances, lack of coordination, paresthesia, abnormal weight loss, urinary incontinence, alterations in consciousness, convulsions, dizziness, and abnormal blood chemistries (Buck, 2013). 77 Abstract #052 Title: Family Coping after a Child's Traumatic Brain Injury Authors & Affiliations: Amy Huett, PhD(c), RN, Angela Green, PhD, APRN; University of Arkansas for Medical Sciences Background & Significance: Pediatric traumatic brain injury (TBI) is a potentially devastating occurrence impacting not only the life of the injured child, but also the family. The CDC estimates 1.365 million emergency department visits related to TBI with over half a million in children 0-14 years of age. While most TBI’s are not life-threatening and often have no lasting sequelae, those that are more severe or repetitive have lasting consequences, for both the child and the family. Purpose: The purpose of this study was to explore the experiences of families after pediatric TBI and their perceptions of what helped them cope and adapt. Specific aims were to explore: 1) the demands placed on a family after pediatric TBI; and 2) the resources, both internal and external, the family uses to cope with life after pediatric TBI; and 3) describe how the family adapts to life after their child’s TBI. Methods: This focused, ethnographic study used purposive sampling to recruit families at the trauma clinic in a large, freestanding pediatric hospital. The family was chosen as often they are responsible for the majority of the child’s ongoing care after discharge from the hospital and also bear the emotional, financial, and social burden that may be associated with that child’s care. Inclusion and exclusion criteria consisted of families with: 1) a child admitted to PICU with accidental TBI; 2) injury occurred at least 6 months prior to interview; and 3) the child had no pre-injury neurological condition. Families completed a brief demographic form and participated in a semi-structured interview. Data were analyzed using thematic analysis. Additional information gleaned from participant observation and transcribed field notes assisted in data analysis. Results: To date, 9 interviews with 11 participants have been conducted. Themes emerging from the data include: protecting myself, managing, reconciling, and forever changing. Conclusions: Families described a cyclical pattern to coping after a child's TBI. As a child's developmental milestone approaches, for example, driving a car, the pattern of stress, coping, and adaptation begin again. Families rely heavily on their faith and their significant other, if present. Some families were proactive in seeking resources for their child and the family, while others felt lost and described a perceived lack of resources. The results from this study will serve as the foundation for a long term program of research to develop interventions tailored to the unique coping styles of the family after pediatric TBI. The impact of the child’s age at injury also warrants further study. Implications for Nursing Practice: Clinicians should be aware of the lasting effects of TBI to help support families after discharge. It is essential that healthcare providers recognize the importance of balancing hope with reality as we strive to educate families and increase both understanding and awareness of the long-term effects of TBI within the family unit. Since support outside of the family is also of extreme importance, it is suggested that community education be provided. 78 Abstract #053 Title: Psychological Differences in Adolescents Who Sexually Offend with a History of Childhood Sexual Abuse Authors & Affiliations: Sarah Bean, Sara Jones, PhD, APRN, PMHNP-BC; University of Arkansas for Medical Sciences Background & Significance: Adolescents who sexually offend (ASOs) account for 30 % of childhood sexual abuse (CSA) cases in the United States, and up to one third of these ASOs will sexually reoffend. While various studies have reported rates of childhood sexual victimization from 10% to over 90% in ASOs, a meta-analysis of 31 studies found that CSA occurred in 46% of ASOs. Compared to non-victimized ASOs, ASOs with a history of CSA are more likely to have witnessed violence, have more experiences of other childhood victimization and higher rates of post-traumatic Stress (PTSD) and conduct disordered behavior. They are also at higher risk for developing major depressive disorder and suicidality. Purpose: The purpose of this pilot study was to evaluate the differences in psychological functioning and traumatic experiences between adolescents who had sexually offended with and without a history of childhood sexual abuse. Methods: : Male ASOs (aged 12-20) were recruited from treatment facilities across the state. Participants were interviewed using the MINI Kid (Mini International Neuropsychiatric Interview for children and adolescents) and the National Survey of Adolescents (NSA), Trauma Assessment. The MINI Kid is a structured diagnostic tool that assesses psychiatric disorders in adolescents, including depression, oppositional defiant disorder, and conduct disorder. The NSA assesses information related to traumatic events in the adolescent’s past, including physical assault and abuse, sexual abuse, and exposure to domestic violence. The participants also completed self-report questionnaires, including the Short Mood and Feelings questionnaire (SMF) and the UCLA PTSD Index for DSM-IV, Adolescent Version. The SMF is an 11-item questionnaire that assesses symptoms related to depression in the past two weeks. The UCLA PTSD Index is a 22-item questionnaire to assess for symptoms of PTSD. Differences between groups were estimated using Wilcoxon-Mann-Whitney rank test for continuous and count variables, and Fisher’s exact test for categorical variables. Results: Participants included 21 non-victimized ASOs and 15 victimized ASOs. Compared to non-victimized ASOs, victimized ASOs had greater histories of suicidality (p=0.01) and experienced significantly more physical abuse (p=0.02) and exposure to domestic violence (p=0.01). The UCLA PTSD Index showed higher median scores on symptoms of PTSD (p<0.001). Results of the MINI showed no significant differences in conduct disorder and oppositional defiant disorder between groups. Further, the MINI and SMF showed no difference in depression between groups. Conclusions: Similar to previous findings, this study found that victimized ASOs experience more childhood traumas, including physical abuse and exposure to domestic violence. Results also concluded that victimized ASOs more symptoms indicative of PTSD. However, unlike previous studies, results show no significant differences in rates of depression, although previous suicidalities were higher, conduct disorder, or oppositional defiant disorder between groups. Implications for Nursing Practice: Treatment of ASOs with history of CSA should provide interventions that focus on treating symptoms related to previous traumas. Trauma informed cognitive behavioral therapy has shown to be effective and should be considered for this population. 79 Abstract #054 Title: Benzodiazepines as an effective first-line treatment for insomnia in older adults Authors & Affiliations: Sundra Robinson, Barbara Landrum, PhD, RN, CNE Henderson State University Nursing Department Chair & Associate Professor Trenton Curry, Austin Wagner; Henderson State University Problem & Purpose: Insomnia is common in older adults. Benzodiazepines are prescribed for the treatment of this condition but research suggests a need for a more effective treatment. PICO Question: For older adults, are benzodiazepines an effective first-line treatment for insomnia? Evidence-based practice models & process: The databases searched are CINHAL Complete and EBSCOhost. Key terms used are: benzodiazepines, insomnia, treatment, and older adults. Restrictions used are: 55years and older, 65 years and older and full text articles. From these searches three studies that adequately answered the PICO question were used in the systematic review. Relevant Literature: Using a combination of the key terms listed above in the before mentioned databases the search yielded a total of 3,122 in EBSCOhost and 370 in CINHAL Complete. Of these, three studies were chosen: (1) “Characteristics associated with benzodiazepine usage in elderly outpatients in Taiwan,” (2) “Effects of chronic insomnia and use of benzodiazepines on daytime performance in older adults” and (3) “Benzodiazepine use and quality of sleep in the community-dwelling elderly population.” Study (1) is a random sample, observational study concluding that participants with insomnia are more likely to receive higher mean dosages of benzodiazepines and longer treatment (Cheng, Huang, Lin & Shih, 2007). Study (2) is a random samplly, descriptive research study. Results show that chronic benzodiazepine use has no effect on daytime performance of insomnia participants (Vignola, Lanoureux, Bastien & Morin, 2000). Study (3) is a random sample, qualitative study which found that users tended to report poorer quality of sleep than non-users of benzodiazepines (Beland, Preville, Dubois, Lorrain, Grenier, Voyer, Perodeau & Moride, 2010). Methods: The studies were systematically reviewed to ensure the PICO question was addressed. Each study provides significant findings regarding the effectiveness of benzodiazepine usage for insomnia in older adults. Outcomes: Each study addressed the PICO question by providing significant findings regarding the effectiveness of benzodiazepine usage for insomnia. The likely effect is not too small because benzodiazepines are more likely to be prescribed for treatment of insomnia (Cheng et al., 2007). The cost of applying the evidence, which would be prescribing other pharmacological interventions, would vary depending on the medication or intervention used. The usual care of benzodiazepines would not be preferred for the first-line treatment of insomnia in older adults because they proved to be ineffective Conclusions: After reviewing these studies, benzodiazepines are not an effective first-line treatment for insomnia in older adults because users reported poorer quality of sleep then non users despite higher mean dosage and long term use. Implications for Nursing Practice: Possible recommendations are doing more studies on the topic. Not using benzodiazepines as a treatment for insomnia would be useful to nurses in the gerontological field because there would be a decrease in occurrences of insomnia. 80 Abstract #055 Title: How Nurse’s Instructions Affect Patient Understand of NPO Authors & Affiliations: Alexis Worsham, Barbara Landrum, PhD, RN, CNE Rachel McNabb, Taneya Taggart; Henderson State University Problem & Purpose: To research evidence based implications that could determine if a nurse’s lack of knowledge has any effect on patients’ perceptions towards NPO status, as well as how long the patients should remain NPO PICO Question: “In pre-operative patients, does the nurse’s ability to give clear instructions affect the patient’s understanding and adherence to the NPO status?” Evidence-based practice models & process: The examined articles indicate that nurses lack the knowledge needed to correctly implement NPO. Nurses felt the research on NPO is difficult to understand, so it is not applied to practice. Patients are being fasted longer that the quoted hours. If a standard NPO policy takes affect and is mandatory, this will result in a better outcome for patients. Relevant Literature: The examined articles indicate that nurses lack the knowledge needed to correctly implement NPO. Nurses felt the research on NPO is difficult to understand, so it is not applied to practice. Patients are being fasted longer that the quoted hours. If a standard NPO policy takes affect and is mandatory, this will result in a better outcome for patients. Methods: The literature search process used CINAHL complete. Search terms used to locate appropriate literature were “Pre-operative fasting,” “NPO,” “Preoperative Fasting,” “fasting, NPO.” Search years were limited: 2000-2013 and article types were limited to research reports. There were no repeated references, and no excluded references. Next we limited options to full text, and excluded reports that didn’t contain full text articles. Our studies were “Pre-Operative fasting for elective surgical patients,” “Pre-operative Fasting: a clinical audit,” “Patient perceptions of the importance of maintaining pre-operative NPO status.” Outcomes: The studies researched determined that nurses lacked knowledge and skills regarding NPO practice changes. Due to this lack of knowledge, patients showed misunderstanding and confusion of how long they should fast. A recommendation would be to have each facility have an in-service, to ensure that the nurses are in complete understanding to the NPO policy. Conclusions: The studies researched determined that nurses lacked knowledge and skills regarding NPO practice changes. Due to this lack of knowledge, patients showed misunderstanding and confusion of how long they should fast. A recommendation would be to have each facility have an in-service, to ensure that the nurses are in complete understanding to the NPO policy. Implications for Nursing Practice: When nurses become more knowledgeable about NPO, patients will be less likely to aspirate during surgery. Patients that are told clearer instructions will feel less concerned about what they are being asked to do. Facilities that address nurses and patients misunderstandings will be incorporated into NPO policies 81 Abstract #056 Title: Fibromyalgia Syndrome and Hydrotherapy Authors & Affiliations: Amy Howell, Carol Enderlin, PhD, RN Jennifer Orahood, Caroline Loyd, Krystal Qualls, Mauri Rogers, Jeffrey Archer, Amber Cockmon, Misty Ervin, Channing Hall, Danelle Heaggans, Jameka Jackson, Brynna Lynch, & Morgan Morrow;University of Arkansas for Medical Sciences College of Nursing Significance: Fibromyalgia Syndrome is a chronic pain disorder characterized by widespread pain and diffuse tenderness. An estimated five million American adults in the United States are diagnosed with Fibromyalgia Syndrome (FS). The overall goal in people with FS is to reduce pain and tender points compared to standard care. Purpose: The purpose of this project is to compare hydrotherapy treatment to standard care for the outcome of pain in clients with FS. PICO Question: How does hydrotherapy treatment compare to standard care for the management of pain in clients with FS? Search Strategy & Screening: The literature search process used PubMed. Search terms used to locate appropriate literature were fibromyalgia, water therapy, bath therapy, spa therapy, hydrotherapy, and balneotherapy. The literature search produced a total of 18 articles. Six articles were reviewed. Four articles were selected for this project based on inclusion of fibromyalgia and a single hydrotherapy intervention, randomized controlled trial design, availability, and year of publication. Evidence: Balneotherapy treatment significantly reduced pain (p < 0.005) and tender points (p < 0.001) compared to standard care. Spa therapy treatment significantly reduced pain (p < 0.161) and tender points (p < 0.411) compared to standard care. Stanger bath treatment significantly reduced pain (p < 0.01) and tender points (p < 0.001) compared to standard care. Mud-bath treatment significantly reduced pain (p < 0.001) and tender points (p < 0.0001) compared to standard care. Synthesis of Evidence: Four out of four studies show significantly improved pain and tender points compared to standard care alone for clients with FS. Conclusions: Hydrotherapy appears to result in improved outcomes when combined with standard care. We recommend hydrotherapy be used as an adjunct therapy with standard care for patients with FS. Implications for Nursing Practice: Adjunct therapy with hydrotherapy may reduce the use of nonsteroidal anti-inflammatory drugs and related adverse outcomes such as gastrointestinal bleeds and renal failure. Less medication use may also decrease adverse outcomes related to polypharmacy. However, hydrotherapy costs may not be covered by insurance. There also may be limited access to facilities that offer hydrotherapy. 82 Abstract #057 Title: Factors Related to Early Breastfeeding Cessation Authors & Affiliations: Shannon Taylor, Dr. Laura K. Evans, Lauren Nix, Morgan Searcy, and Cajun Johnson University of Arkansas at Monticello Significance: According to WHO, breast-feeding is a priority for infants at least up to six months. However, at most, 75 percent of mothers initiate breast-feeding, but many discontinue before their infant is six months old. Interventions that support and/or educate mothers can increase the continuance of breast-feeding to provide infants with nutritional and health benefits. Purpose: The purpose of this evidence-based (EBP) project was to analyze the factors that are associated with early cessation of breast-feeding among postpartum mothers and to determine effective interventions to prevent early cessation of breast-feeding. PICO Question: What factors are associated with early cessation of breast-feeding? What interventions are effective to encourage women to continue breast-feeding for at least 6 months? Search Strategy & Screening: We searched the Cumulative Index for Nursing and Allied Health (CINAHL) database with the keywords: breastfeeding, early cessation, education, factors, and nurse’s role, separately and combined. Limiters included publication between 2009 and 2015, research, full text, and any author is a nurse. Evidence: The search resulted in 74 articles. After review of titles and abstracts for relevance we narrowed the articles down to 13 articles. After quality critique using the John Hopkins Nursing Evidence Based Practice Research Evidence Appraisal Tool the result was 12 articles. Synthesis of Evidence: The results from the 12 articles revealed many factors that contributed to early discontinuation of breastfeeding. Some of these were poor education, lack of support, physical problems with breast feeding, need to return to work, supplementation with formula, and breast milk supply issues. Seven out of twelve articles asked the general question of what factors are associated with early cessation of breast feeding. One study examined BMI as a factor mothers with higher BMI breastfed on average of 15 weeks compared to lower BMI mothers who breastfed for 18 weeks. Four out of the twelve studies had limitations that included a small sample size, therefore, they were not able to compare it to a larger population and were not generalizable. Seven out of the 12 articles focused their concepts and variables at the mother and her sociodemographic information. Three studies stated that supplementation with breast milk substitutes during the first week of life was linked to cessation during the first 3 months. The majority of the articles also focused on the mother’s support system. Support played a big role in early cessation of breastfeeding. Nine out of twelve studies suggested that providing support for the mothers would maybe increase the duration of breastfeeding. The studies wanted to know if there were any support systems, did they know of anyone who would support them, and was there support from the paternal side. The greatest sample size of a study was 29,621 mothers out of Norway. Most of the studies found that mothers who had a lower educational level or were a minority participated in early discontinuation of feeding. Conclusions: Assuring appropriate nutrition and enhancing immunity is important for newborn infants. Breastfeeding for at least six months helps in meeting these goals. Understanding the factors associated with early discontinuation of breastfeeding is important in this vulnerable population. Implications for Nursing Practice: Education and support is imperative for increasing duration of breastfeeding. The first week postpartum is a critical time period. Interventions to achieve this goal would be to address breastfeeding immediately after birth. Assess the mothers’ education level and previous experiences with breast-feeding to obtain information about the patient’s knowledge of breast-feeding. Provide mothers with lower education levels and negative previous experiences with easily accessible and appropriate information about breast-feeding. Assess the mother’s technique and teach proper technique allowing the patient to demonstrate afterwards, educate new mothers on the risks of supplementation with formula while breast- feeding, follow-up care, and setting the mothers up with a support group. 83 Abstract #058 Title: Strategies to Prevent Medication Errors Authors & Affiliations: Allisa Lawson, Dr. Laura K. Evans PhD, RN Aubrey Evans, Hannah Tadlock;University of Arkansas at Monticello Significance: 44,000-98,000 deaths occur each year from preventable medication errors, those numbers do not include the unreported medication errors that occur. Many more patients are seriously harmed due to the same type of errors. Decreasing medication errors not only provides safety for the patient but also decreases costs. Purpose: The purpose of this project was to perform a limited review of literature on interventions that may decrease medication administration errors. PICO Question: What strategies can be implemented by nurses to reduce medication errors in the hospital? Search Strategy & Screening: The literature search process used the Cumulative Index of Nursing and Allied Health (CINAHL) database. Search terms used to locate appropriate literature were medication, prevention, error, hospital, and nurse. Search years were limited to 2010 through 2015, authors were limited to include at least one nurse, and all studies had to come from an academic journal. Quality was critiqued using the Johns Hopkins Nursing Evidence Based Practice instrument. Evidence: The search produced a total of 126 studies, of which twelve studies were selected as relevant for appraisal. Of the twelve studies, two did not meet the critique guidelines. Synthesis of Evidence: Upon analyses of all the articles, eight reported a decrease of medication administration errors using drug round tabards, no interruption zones, bar-code administration system, education of the personnel, decreasing work hours, and having adequate nurse staffing. Findings from two of the ten articles did not report a decrease of medication errors using the proposed interventions. One of the ineffective interventions was donning a sash while on medication administration rounds and the other was the placement of a medication cabinet in the patient room. Conclusions: Due to the potential for patient injury and increased associated costs, it is vitally important to decrease medication errors. Implications for Nursing Practice: Nurses play a vital role in prevention of medication errors. Limitation of disruptions during medication preparation and delivery may decrease the number of medication errors. Adoption of drug round tabards, signs that indicate nurses are preparing or administering medications, signs that indicate no interruptions, using bar-codes, educating staff, and decreasing work hours as well as ensuring adequate staffing are ways that nurses may decrease medication errors. 84 Abstract #059 Title: How Various Sexual Education Programs Influence Adolescents’ Risky Sexual Behavior Authors & Affiliations: Leanna Morris, Laura Evans, PhD, RN Brandon Odom, Teri Poirrier, Shea Wallace;University of Arkansas at Monticello Significance: Approximately 780,000 total pregnancies occur per year among girls aged 10 to 19. Teens also account for over 50% of new sexually transmitted disease diagnoses every year. This early sexual activity has been shown to have a negative effect on education and health in the future. Various sex education programs are in place throughout the United States, but it is still unclear which approach to this specific education is most effective in altering teenage perception of the risks associated with early sexual activity. It is important to discover which programs are most effective in preventing these negative outcomes among teens in order to more widely implement the most appropriate sexual education program in schools. Purpose: The purpose of this evidence-based project was to examine how various types of sexual education influence risky sexual attitudes and behaviors of adolescent females. PICO Question: Among adolescent females in the United States ages 10-19, how do various types of sexual education influence risky sexual attitudes and behaviors? Search Strategy & Screening: To discover the effectiveness of comprehensive sexual education programs, the project team used the Cumulative Index of Nursing and Allied Health (CINAHL), Academic Search, Consumer Health Complete, Health Source-Consumer, Health Source-Nursing, Medline, and PsycInfo databases and searched the terms sex, adolescents, sex education, and prevention using the Boolean operator AND. The terms pregnancy and school nurse were also searched using the OR. Limiters applied included: research article, academic journals, full text, English, geography USA only, and publication date between 2009 and 2014. Evidence: The search produced an initial total of 5, 553,124 articles, but that number was reduced to 50, 233 by applying limiters listed. Adding the additional search terms pregnancy and school nurse reduced the total to 184. After reviewing titles for relevance, 27 articles were selected for quality critiques. The final selection included 12 articles. Synthesis of Evidence: Findings from six studies reported positive effects after the implementation of comprehensive sex education programs including information regarding contraception, parental responsibilities, and risks associated with early sexual activity. Findings from the other six studies reported negative effects after sex education intervention. One report, however, found comprehensive sex education to be ineffective in changing teen behaviors and perceptions. Two studies reported a decreased risk for early sexual activity for those teens actively involved in family and church. One study provided information from the viewpoint of educators and reported strong opinions that comprehensive accurate sex education should be provided in schools. One study demonstrated the lack of knowledge of teens regarding resources for sexual education. Lastly, one study showed that teens are highly influenced to engage in early sexual intercourse by their peers, the media, and personal feelings regardless on sexual education. Conclusions: Teens' perception of risky sexual behaviors can be influenced by a variety of education methods including comprehensive sex education programs, religious education, and family and peer education. Implications for Nursing Practice: Comprehensive sex education combined with simulations and accurate discussion of all options and risks may be reliable in altering teen perceptions of risks associated with early sexual intercourse. 85 Abstract #060 Title: Effects of Chlorhexidine Gluconate Bathing on MRSA Colonization and Infection Rates in Inpatient Populations Authors & Affiliations: Haley Burton, Dr. Seongkum Heo, PhD, RN Sarah McAlister; University of Arkansas for Medical Sciences Significance: Hospital-acquired methicillin-resistant Staphylococcus aureus (MRSA) has been a problem since the 1960s. The Centers for Disease Control and Prevention reported more than 3,000 cases of healthcare-related MRSA infections per 100,000 people in 2012. Patients infected with MRSA have higher mortality rates, longer hospital stays, and higher healthcare costs. Furthermore, beginning October 2008, the Centers for Medicare and Medicaid Services enacted regulations that would cease hospital reimbursement for healthcarerelated MRSA. Chlorhexidine gluconate (CHG) has been shown to reduce intravascular catheter-related infections, and CHG has been commonly used for preoperative skin preparation and ventilator- associated pneumonia prophylaxis. However, it is unclear whether CHG bathing is effective in reducing MRSA colonization or infection. Purpose: The purpose of this study was to examine the effects of CHG bathing on MRSA colonization and infection rates in inpatient populations. PICO Question: In inpatient populations, does CHG bathing compared with regular soap and water bathing or no CHG bathing lead to reduction of MRSA colonization and infection rates? Search Strategy & Screening: Authors searched PubMed, CINAHL, and OVID. Keywords were methicillin resistant (MRSA) and chlorhexidine gluconate (or CHG), resulitng in 484 articles. Inclusion criteria were: English, humans, publication in the last 5 years, and full text. The study designs included: systematic literature reviews/meta-analyses, randomized controlled trials, and quasiexperimental studies. Applying the inclusion criteria, 107 articles remained. We reviewed the abstracts and/or full-text to determine relevance of these articles to the purpose of this study. We excluded 99 articles and 8 remained. We also reviewed articles from the reference list of these 8 articles and added 2 more articles. Therefore, 10 articles were included. Evidence: In one literature review including 6 studies, 3 studies showed reduction in MRSA colonization, and 1 study showed reduction in MRSA infection; while 2 studies did not show reduction in MRSA infection, and 2 studies did not provide clear information about the significance of CHG bathing on MRSA infection rates (2 studies examined both outcomes). In another literature review, 2 studies showed reduction in MRSA colonization, and 1 study showed reduction in MRSA infection, while 4 studies did not show reduction in MRSA infection, and 2 studies did not provide clear information about the significance of CHG bathing on MRSA infection rates. In this literature review, metaanalysis using 2 studies showed that CHG reduced MRSA colonization rates, but meta-analysis using 4 studies did not reduce MRSA infection rates. In another meta-analysis including 10 articles, CHG bathing reduced MRSA colonization and infection rates. Among 7 individual studies, 4 showed reduction in MRSA colonization or infection. Among the 4 studies, 2 showed reduction in MRSA colonization, 1 in MRSA infection, and 1 in both. In 3 individual studies, 2 studies did not reduce MRSA infection, and 1 study did not reduce MRSA colonization or infection. There were no consistent differences in the settings or concentration of CHG between those studies showing significant MRSA reduction and those studies that did not. Synthesis of Evidence: Findings from this literature review consistently showed the effect of CHG on reducing MRSA colonization rates, but were inconsistent in the effect of CHG on MRSA infection rates. More studies showed no reduction in MRSA infection rates, and meta-analyses showed contradicting findings. Conclusions: CHG was effective in reducing MRSA colonization rates, but the effect of CHG in reducing MRSA infection rates was inconclusive. Implications for Nursing Practice: CHG bathing can be implemented to reduce MRSA colonization rates, but additional factors along with CHG bathing should be considered to reduce MRSA infection rates. 86 Abstract #061 Title: Effects of E-Ciggarettes in Smoking Cessation Authors & Affiliations: Mara Onecic, Cheryl Schmidt, PhD, RN, CNE, ANE, FAAN Asfour, S., Brackett, C., Burton, H., Colclasure, M., Connors, A., Hines, B., Poole, L., Mayhue, C., McNeely, L., Peters, J., Stark, C., Owens, C., Yancy, L.; University of Arkansas for Medical Sciences Significance: Health care providers have explored a variety of nicotine replacement therapies in their efforts to decrease or eliminate the dependency on tobacco among patients. Electronic cigarettes (E-cigs) are the latest attempt to create an alternative to using tobacco. Healthcare providers should base their recommendations on evidence rather than advertisement. Purpose: The purpose of this critical appraisal project was to compare the effects of electronic cigarettes to nicotine replacement therapy in cessation of smoking, by critiquing randomized studies. PICO Question: Among nicotine users, are electronic cigarettes an effective alternative compared to traditional nicotine replacement therapies, in smoking reduction and cessation? Search Strategy & Screening: The literature search process used was PubMed and Google Scholar with the following search terms: E-Cigarettes, Smoking Cessation, Nicotine- Replacement Therapies, and Cigarette Substitute. We limited our search to medical journals with full text, published within the last 5 years, human species, English language, and studies trialed in foreign countries. Evidence: The search for E-cigarettes produced an initial total of 1083 studies. By limiting results to full text, publication within the last 5 years and human species, a total of 488 studies were found. Further limiting the results to “e-cigarette smoking cessation” produced 240 studies for appraisal. The four articles used in this project were chosen because of the limited amount of research conducted on electronic cigarettes. Synthesis of Evidence: Although two out of four studies had sufficient sample sizes to conclude that alternative therapies may be useful in smoking cessation, all authors recommended further research. Conclusions: The studies by Bullen et al. (2013) and Caponnetto et al. (2013) supported that the use of electronic devices could help with smoking cessation. The studies by Bullen et al. (2009) and Polosa et al. (2011) had insufficient sample sizes to support the effectiveness of electronic cigarettes in smoking cessation. In conclusion, all authors recommended further studies with larger sample sizes. Healthcare providers should monitor future studies to determine the safest and most effective strategies to use with their patients desiring smoking cessation. Implications for Nursing Practice: Four studies on the effects of alternative therapy on smoking cessation provide examples that there is insufficient evidence of the benefit of the intervention. Further randomized controlled trials to address the uncertainty about the effects of alternative therapy on smoking cessation would need to include larger sample sizes. 87 Abstract #062 Title: Effects of Interventions on Depression in Caregivers Who Take Care of Alzheimer’s or Dementia Patients Authors & Affiliations: Julie Allard, Seongkum Heo, PhD, RN; University of Arkansas for Medical Sciences Significance: Alzheimer’s and dementia are on the rise in the older population worldwide. There are nearly 11 million caregivers taking care of these patients in the United States. Caregivers must manage the patient’s emotional, financial, and behavioral issues, as well as physical limitations. This can increase caregivers’ psychological distress, such as depression. Almost 30% of these caregivers are clinically depressed. Caregivers’ depression can reduce their quality of life and lead to inappropriate care of their patients. Various interventions have been provided to reduce caregivers’ depression. However, it is unclear which intervention is effective in reducing depression in this population. Purpose: The purpose of this study was to examine the effects of interventions on depression in caregivers of Alzheimer’s or dementia patients. PICO Question: In caregivers of Alzheimer’s or dementia patients, which interventions are effective in reducing depression? Search Strategy & Screening: PubMed and OVID were searched using the key words of depression or depressive symptoms, intervention or trial, dementia or demented, and caregiver or carer. When we combined the searches of the keywords, we found 326 articles. The inclusion criteria were full text, humans, English, and published in the last 10 years. In addition, the study designs included in this review were systematic literature reviews/meta-analyses and randomized controlled trials. The remaining 190 articles were reviewed to determine the relevance to the purpose of this study. We excluded 175 articles and 15 remained. Evidence: Among the 15 studies, 2 were systematic literature reviews/meta-analyses, and 13 were RCTs. In one literature review including 26 RCTs, meta-analysis showed that none of psychosocial, telephone-based, and case management interventions were significant in reducing depression. In another literature review, meta-analysis showed that group coping skills interventions alone and with behavioral activation reduced depression (p < .001). In this literature review, 2 studies used web-viewable or home videos improved depression; while 6 studies used group coping skills with behavioral activation, group coping skills, dyadic counseling, cognitive stimulation therapy, or individual behavioral management did not. Among 6 individual RCTs, 5 psychosocial interventions with or without technology, and 1 case management study did not reduce depression. Among 3 individual RCTs, 2 psychosocial interventions and 1 behavioral activation study showed partial effects on depression. The other 4 individual RCTs used psychosocial interventions with or without technology reduced depression. Three of these 4 studies focused on dealing with emotional issues and well-being. All interventions in the 4 studies were delivered by specialized or certified interventionists in psychosocial areas or these types of interventions. Synthesis of Evidence: The findings of the literature reviews/meta-analyses and RCTs showed inconsistent results in reducing depression using a variety of interventions in this population. However, studies that utilized specialized interventionists and/or dealing with emotional issues or well-being more actively showed reductions in depression. Conclusions: There were no specific types of interventions that effectively reduced depression in caregivers of Alzheimer’s or dementia patients. However, psychosocial interventions with specialized interventionists and/or focusing on emotional issues and well-being may be effective in reducing depression. Implications for Nursing Practice: It may be more effective in reducing depression if nurses with enough experience in psychosocial interventions deliver intervention sessions and focus on emotional issues and well-being as well as core components of psychosocial interventions. Further studies are necessary to determine more effective interventions in reducing depression in this population. 88 Abstract #063 Title: It’s a Small World: Providing Culturally Competent Care Authors & Affiliations: Amy Funderburk, MSN, RN, NE-BC, Dr. Cathrin Carithers; University of Arkansas for Medical Sciences Significance: Per the 2010 census, America has become more diverse. Currently, 12.9 % of our population is foreign born and 33.1 % speak another language at home. The nursing workforce does not reflect this diversity. We must find ways to increase the competence of staff caring for a diverse population. Purpose: The diversity of the country and the lack of reflection by healthcare workers creates barriers to care and disparities in treatments. Heath care literacy is also dramatically impacted. Through training these disparities can be minimized and healthcare literacy improved resulting in improved outcomes for patients. PICO Question: Do nurses who attend diversity training have increased cultural competence? Search Strategy & Screening: The initial search utilizing the Boolean phrase “diversity training and healthcare workers” training” resulted in zero results. The search was modified to read “cultural training and nurses” which resulted in eight records, however, many were greater than five years old. MeSH terms “cultural competence and nurses” were employed which yielded 806 records. The following filters were added: limit to five years; full text, academic journals, written or translated into English and research articles resulting in 48 articles for review. Eleven articles were included based upon inclusion and exclusion criteria. Search databases included: CINAHL, PubMed, and OVID. Evidence: Several studies utilized a pre and post assessment of effectiveness, however, program types ranged from courses lasting several hours, one day, and courses spanning several weeks or integrated into a series of semesters. All studies were limited to adult participants, however, the nursing experience ranged from nursing students to non-specific “nursing” populations in the workforce. All articles applied Madeline Leininger and Josepha Campinha-Bacote’s theoretical frameworks. Leininger’s “Cultural Care Theory” states that “an awareness of the patient’s cultural perceptions enables a nurse to provide competent and culturally appropriate care”. Campinha-Bacote’s theoretical framework separates the model into five constructs: cultural awareness, cultural knowledge, cultural skills, cultural encounters and cultural desire. Through training—the type seems not to matter—participants achieved cultural awareness and knowledge through skills, encounters and desire. Achievements were personally driven based on locale, situation and desire. Synthesis of Evidence: Training does increase cultural awareness and knowledge related to diversity and cultural needs. Cultural “sensitivity” seems to improve though more research is needed. Immersion is required to fully achieve “competence”. However, for a majority of situations awareness, knowledge and the willingness to utilize resources to address individualized patient needs improves patient outcomes and staff satisfaction. Conclusions: Providing training and reference resources to nurses improves the care for the patient and may be adapted to multiple settings. Implications for Nursing Practice: Organizations should include training specific to the populations served and provide resources for addressing patient needs. 89 Abstract #064 Title: Electronic Cigarettes- Awareness, Perception, and Education. Authors & Affiliations: Mary Jane Willard, BSN, MBA, MA, RNP, CCRN, CNRN, Susan Ball, PhD, APRN, GNPBC, CNE University of Arkansas for Medical Sciences, CHI St. Vincent Infirmary; University of Arkansas for Medical Sciences College of Nursing Significance: Over 480,000 Americans die each year from smoking related diseases. Approximately 52.9 million Americans smoke cigarettes. Tobacco cessation can reduce the risk of coronary artery disease and lung cancer. This literature review will focus on awareness, perception, and education on vaping {electronic cigarettes, electronic nicotine delivery systems (ENDS), e-cigarettes}. This emergence of e-cigarettes has caused many healthcare providers concern related to the awareness, perception, and education on vaping. E-cigarettes have been promoted as a healthy alternative to tobacco cessation. There are very limited research studies on e-cigarettes. E-cigarettes have been banned in Australia, Brazil, Canada, and Norway; however, they can be purchased on the internet. Wells Fargo has predicted that ecigarettes will surpass regular cigarettes in sales margins by 2017. The FDA does not regulate e-cigarettes or allow manufacturers to market e-cigarettes as a therapeutic approach to smoking cessation. Purpose: To review the literature on perceptions of e-cigarettes among the public. PICO Question: What are the perceptions of e-cigarettes among the public? Search Strategy & Screening: The literature search process used CINAHL with full text, Google Scholar, and EBSCO. The following terms were used to search the literature: smoking, tobacco, e-cigarette, electronic cigarette, and perceptions. Evidence: The initial literature search produced 42 articles, and 10 articles were reviewed for this report. Electronic cigarettes were developed in the 1960’s but did not become popular until the last few years. There are several reasons that people choose to use e-cigarettes. 1) There is a perception that e-cigarettes can be used for tobacco cessation. Smokers who use e- cigarettes as an aid for smoking cessation may not be aware that they are substituting proven strategies to quit smoking for products that have not been proven effective or safe. 2) E- cigarettes can be smoked in restricted smoking areas. 3) The public perceives that e-cigarettes reduce cost associated with tobacco dependence. 4) There is a public perception that e- cigarettes are safer and healthier. Synthesis of Evidence: The studies and AHA guidelines in the literature search demonstrate that the short term and long term safety of electronic cigarettes is unknown at this time. Additional research in this topic should be explored. There is a misconception by the public on the safety of e-cigarettes and there is little knowledge about the potential dangers of e- cigarettes. Conclusions: A few conclusions based on current evidence include the following: 1) Nurses need to be actively involved in educational programs to inform the public of the potential dangers of e-cigarettes. 2) The short-term and long-term risks have not been established. 3) There is no regulatory oversight in the e-cigarette industry. 4) E-cigarettes have not been effective for tobacco cessation. Implications for Nursing Practice: Healthcare providers need to be knowledgeable about the risks of electronic cigarettes. The American Heart Association (AHA) suggests that healthcare providers should not recommend e-cigarettes as primary tobacco cessation aids. The combination of e-cigarettes and conventional tobacco is concerning. Since the AHA and the FDA do not recommend e-cigarettes as a tobacco cessation method, healthcare providers should not recommend this strategy to the public. 90 Abstract #065 Title: Washington County Arkansas’ progress toward accomplishing Healthy People 2020 objective MHMD-8 Authors & Affiliations: James Jones, RN, Sara Jones, PhD, APRN, PMHNP-BC; University of Arkansas for Medical Sciences College of Nursing Significance: The Healthy People 2020 objective MHMD-8 aims to increase the proportion of persons with serious mental illness (SMI) who are employed. In 2012 in Arkansas, 21.2% of adults that received public mental health services were employed. Currently in Washington County, only one community mental health center offers employment assistance or supported employment for persons with SMI seeking employment. Purpose: The purpose of this literature review was to present evidence-based employment interventions for persons with SMI and identify the needs of Washington County, Arkansas, to achieve Healthy People 2020 objective MHMD-8. PICO Question: For persons with SMI residing in Washington County how do interventions offered by the community mental health center compare to current evidence-based interventions in adequacy and effectiveness to improve employment rates? Search Strategy & Screening: A literature search was conducted using PubMed and EBSCO. Search terms included employment and serious mental illness. The search resulted in an initial 206 articles. The search was limited to articles within a 10 year time frame and with full text, leaving 5 articles relevant to employment, interventions, and SMI. Evidence: Usual employment interventions for persons with SMI vary widely and focus primarily on pre-employment training that has proven less effective in assisting this population obtain and continue employment. Interventions such as transitional employment are only for a limited period of time. The Ticket to Work program has demonstrated limited effectiveness as less than 2% of eligible beneficiaries have accessed the program and the program lacks long term services that benefit persons with SMI. Models of supported employment such as Individual Placement & Support (IPS), Assertive Community Treatment (ACT), and Clubhouses have demonstrated more effectiveness than usual employment interventions in achieving positive vocational outcomes by integrating and coordinating vocational and clinical services for persons with SMI. IPS provides an employment specialist that works with other treatment team members to integrate vocational services with psychiatric treatment and assists in identifying client job interests, vocational assessment, job search, and support. ACT programs ensure continuous integration of supported employment with clinical care. Clubhouses effectively provide supported employment along with other rehabilitation services. Crain et al. (2009) presented the successful application of IPS in a Canadian community mental health team through the case study of a competitively employed 42 year old man with schizophrenia. The integration of IPS with clinical services allowed difficult issues he encountered to be dealt with collaboratively. His experience with IPS allowed him to maintain employment longer that he had in the past, increased his self-confidence and social skills, and reduced his need for frequent clinical appointments. Synthesis of Evidence: The community mental health center in Washington County offers transitional employment support, an ACT program, and “clubhouse” services to assist adults with SMI gain meaningful employment. According to the evidence, integrating supported employment and combining vocational rehabilitation with clinical services and other support, such as IPS, ACT, and Clubhouses, would assist Washington County in achieving Healthy People 2020 objective MHMD-8. Conclusions: Arkansas is making progress toward achieving Healthy People 2020 objective MHMD-8. Washington County residents can assist in achieving this objective by contacting their state legislatures to encourage funding for employment services for persons with SMI. Implications for Nursing Practice: Funding can be used to implement and expand evidence- based employment assistance programs for persons with SMI to all community mental health centers in the state and improve their quality of life. 91 Abstract #066 Title: The Effect of Oral Care on the Incidence of Ventilator-Associated Pneumonia Authors & Affiliations: Katlin Jones, James Mark Tanner, Clinical Instructor, MSN Caroline Loyd, Jon Peters, & Mauri Rogers; University of Arkansas for Medical Sciences Significance: Ventilator-associated pneumonia (VAP) is the most common nosocomial infection in mechanically ventilated patients. VAP not only increases morbidity and mortality of patients, but also costs an additional $29,000-$40,000 per patient. Related to recent changes in the medical industry, these costs are now placed on the hospital. Reducing these infections and subsequently reducing costs can improve patient outcomes and hospital financial stability. Purpose: The purpose of this literature review is to discern the best oral practices to reduce the incidence of VAP in ventilated patients. PICO Question: Do mechanically ventilated patients who receive standard protocol oral care compared to patients who received either no oral care or only oral rinsing have a reduced incidence of VAP? Search Strategy & Screening: The literature search process used Google Scholar and CINAHL. Search terms used to locate appropriate literature were ventilator-associated pneumonia, oral care, evidenced-based practice, and nursing interventions. Full text articles with RN or BSN as primary author were examined. Evidence: One study referenced implemented tooth brushing three times a day to reduce VAP. A separate study implemented a combination of tooth brushing three times a day and 0.12% Chlorhexidine rinse. Multiple other studies evaluated used a combination of the practices above or no intervention at all. Synthesis of Evidence: When compared to other nursing interventions used individually, such as oral rinsing with water/mouthwash or Chlorhexidine “swabs”, the results indicate that tooth- brushing techniques are superior for reducing dental plaque colonization and should be completed every eight hours. The combination of standardized tooth brushing and Chlorhexidine rinse further reduced bacterial colonization. Conclusions: Tooth brushing has shown to be more effective then other forms of oral care in reducing VAP in the hospital setting. By providing a standardized form of this care, at least three times a day, a patient’s chance of contacting VAP can be greatly reduced. To implement a oral care protocol hospital-wide staff education will be necessary to ensure this care is completed correctly, and patient/family education will be sufficient as to the reason behind this intervention. Implications for Nursing Practice: Nurses need to be trained in proper oral care techniques including using a toothbrush to prevent dental plaques. Properly brushing the teeth of a mechanically ventilated patient should reduce the incidence of pneumonia in mechanically ventilated patients. 92 Abstract #067 Title: The Use of Dexmedetomidine in Post-Operative Heart Surgery Patients for Decreasing Length of Stay and Post-Operative Complications Authors & Affiliations: Katrena Wilson BSN, RN, Claudia P. Barone, EdD, RN, APRN, LNC, CPC Shannon Hoey; University of Arkansas for Medical Sciences, College of Nursing Significance: The use of sedation in the Intensive Care Unit (ICU) after heart surgery can lead to post-operative complications such as prolonged intubation and increased length of ICU stay. When managing the care of post-operative heart surgery patients, it is imperative that healthcare professionals choose a drug that will provide optimal sedation. A sedative that does not impair cognitive function while decreasing the risk of dangerous adverse events should be taken into consideration. Purpose: The purpose of this literature search was to acquire evidence comparing dexmedetomidine to propofol and morphine in post-operative CABG patients in ICU. PICO Question: In the post-operative care of adult heart surgery patients in the ICU setting, how does the use of dexmedetomidine compare to the standard use of propofol and morphine for the outcomes of early extubation time and decrease length of ICU stay? Search Strategy & Screening: PubMed and Google Scholar Advanced Search databases were searched for evidence and documented for the project. Search terms were dexmedetomidine, propofol, morphine, cardiac surgery, fast-track, and early extubation. Search years were limited to 2000 through 2013, and after reviewing the abstracts, article were limited to systematic reviews and research studies for design and quality screening. Adult patients 18 or older requiring cardiopulmonary bypass and/or minimally invasive valve surgeries were inclusive criteria. Evidence: The PubMed database returned 328 articles and 384 articles were returned from Google Scholar. Limiting the search to ICU adult patients, having any surgery other than heart surgery, measuring extubation times and length of ICU stay as outcomes, resulted in two systematic reviews, two random control trials, and two nationally published professional practice guidelines used in this course project. Synthesis of Evidence: Three of the four articles reviewed for this project imply that dexmedetomidine may provide advantages over propofol by decreasing length of ICU stay. Two articles suggest that dexmedetomidine can facilitate early extubation. One article utilized both propofol and dexmedetomidine in the treatment groups therefore the outcomes are not clear. Professional practice guidelines from the American Heart Association (AHA) and American College of Cardiology Foundation (ACCF) Task Force of 2011 encourages anesthetic management of early post-operative extubation as it can decrease length of stay in the ICU. The American College of Critical Care Medicine guideline from 2002 recommends the use of sedation protocols. Conclusions: The evidence discovered through a focused literature review supports the use of a sedation protocol utilizing dexmedetomidine to obtain early extubation and decrease length of ICU stay. Implications for Nursing Practice: When caring for post-operative heart surgery patients, the use of dexmedetomidine should be considered. Evidence from the literature supports protocols that include a variety of sedatives based on patient specific populations. Delving into sedation policies that will incorporate sedatives other than the standard propofol may facilitate early weaning of mechanical ventilation and thus reducing the amount of time the patient spends in ICU. 93 Abstract #068 Title: Bloodstream Infection Reduction: Utilizing Alcohol-Impregnated Caps in Patients with Central-Lines Authors & Affiliations: Karen McDowell, Tamisha Henderson BSN, RN, MSN Archer, J., Lewis, D., Shellabarger, C.; University of Arkansas for Medical Sciences Significance: The majority of patients in the acute care critical areas have central venous catheters (CVC), which has resulted in an increase in hospital-acquired infections (HAI) from the point of entry. Central line-associated bloodstream infections (CLABSI) can be life threatening with a morality rate of 12% to 25% according to the Center for Disease Control (CDC). The Joint Commission designated CLABSI as a nursing sensitive indicator and developed prevention guidelines. The use of alcohol wipes was one source of prevention on the access port. Another source for prevention is the use of alcohol-impregnated caps. Even though there has been a decline in the number of infections, it is estimated that 200,000 to 400,000 incidents of CLABSI occur yearly in US hospitals (Merrill, Sumner, Linford, Taylor, & Macintosh, 2014, p. 1274). Purpose: The purpose of this literature review was to gather evidence comparing the effectiveness of alcohol-impregnated caps versus alcohol wipes concerning the occurrence of CLABSI. PICO Question: For patients with central-line access, does the use of alcohol-impregnated caps compared with the use of alcohol wipes to disinfect access ports reduce the occurrence of CLABSI? Search Strategy & Screening: The literature search utilized CINAHL, PubMed, Ovid and Google Scholar with the following search terms: CLABSI, infection, infection control, disinfection, reduction, central-line, alcohol, alcohol wipes, blood stream, and HAI. Search years were limited to within five years. We limited the search to full text, human subjects, English language, nursing authors, and nursing and infection journals. Evidence: The search initially revealed approximately 4890 articles, however limiting the results to full text; and English nursing journals, significantly decreased the number of results to 207. Eliminating studies that were not directed related to the subject of CLABSI’s and prevention of HAI’s produced 4 studies for appraisal. Synthesis of Evidence: The examined articles indicate that patients have benefited from the use of alcohol-impregnated caps on central lines in preventing central line associated bloodstream infections. Three out of the four examined articles showed statistically significant results after implementing the disinfectant caps. However, all four articles indicate a reduction in CLABSI when disinfectant caps were used as opposed to scrubbing the hubs with alcohol wipes. Two articles indicated that using such a device significantly reduced contamination and if it did occur involved fewer organisms. In one study the CLABSI rate decreased from 1.9/1000 catheter days to 0.5/1000 catheter days and a 73% compliance rate using the alcohol- impregnated cap by nursing staff. In a second study there was a 12.7 % vs. 5.5% reduction in infections. In a third study there was a 68% overall decrease in CLABSI. In the fourth one the rate of infections decreased by greater than 40%. Conclusions: By utilizing alcohol-impregnated caps on all ports of central lines hospital costs can be reduced, length of stay reduced, and most importantly, reduced the mortality risk of their patients. The evidence from the reviewed articles supports the use of the alcohol-impregnated caps. Along with increased cost and mortality risk, central line associated bloodstream infections increase length of stay in the ICU setting. It is estimated that the cost to treat each CLABSI is roughly $20,000. Continuing education on the reasons for the use of these devices. Implications for Nursing Practice: Acute care nurses can have a significant impact on the CLABSI nursing sensitive indicator. If such devices are not in use in their clinical area, they can use evidence-based practice to promote the use of the caps at their facilities. Nursing compliance with the use of the alcohol-impregnated caps is essential. The ICU nurses access central lines multiple times daily. ICU nurses can use their knowledge of infection prevention to include the alcohol-impregnated caps. 94 Abstract #069 Title: Assistive devices and rehabilitation in the older adult with visual impairment: Literature review Authors & Affiliations: Casey Childs, Pam DeGravelles, PhD (c), RN; Southern Arkansas University Significance: Age related macular degeneration (ARMD) is a disease that affects the population of elder people. Since this disease can cause a decline in eyesight, it is difficult for the older adult to maintain autonomy and perform activities of daily living. ARMD is a concern in all patients of any age, but it is particularly important in older adults because of the safety hazards and decrease in quality of life that can occur due to low vision. These include falls, medication error, social isolation and depression. Purpose: The purpose of this review was to compare the effectiveness of assistive devices, rehabilitation and the combination of both in older adult patients with age related macular degeneration. PICO Question: In older adults (65+), does the combination of rehabilitation and assistive devices increase autonomy and quality of life more than these used separately? Search Strategy & Screening: Gale and Ebscohost were used ito search the literature. The terms that gained useful results were older adults, age-related macular degeneration, low vision aids, assistive technology, reading speed, rehabilitation and visual diseases. Evidence: The 5 articles were published in the last 10 years and were all quantitative. Evaluation of the therapies indicated the most significant therapy. Assistive technology, rehabilitation and the combination of both were assessed. This literature provides evidence that with the assistance of low visual aids along with a short amount of training or information about the aids, the ARMD patient can achieve a faster reading speed which will in turn contribute more effective sight concerning reading. Follow up training was necessary to maintain constancy in the reading speed from rehabilitation. With the combination of both therapies, the ARMD patient would have an increased quality of life and safety. Synthesis of Evidence: For combination therapy, which would be perceived as the most successful, Markowitz, Kent, Schuchard and Fletcher implemented a study about the ability to read medication labels with a low vision rehabilitation program that uses assistive devices. Assessments were made on 57 patients before low vision aids and interventions were prescribed. An assessment was also made on how well the patient could read medication bottles before and after intervention. There were rehabilitation sessions used for dispensing the aids, education about maintenance of the aids and training with an occupational therapist. The ability to read medication labels was tested again at this point using a scale (0-2, 1=able to access partially but not with confidence, 2=able to read the printed directions accurately and reliably. Conclusions: From my study, I would say the most successful would be the combination. The research was there to back it up with additional studies to prove the point. I believe the rehabilitation research is interesting, and it needs to be continued because that would be the preference if the assistive devices were not necessary. The combination therapy would be the most successful I would think because fixation can be averted around the scotoma. With the visual device assistance with that, it would increase magnification while providing education about central scotomas. Implications for Nursing Practice: In the research for combination therapy, the conclusion is it would be the most beneficial. Even though this study seemed weak because of not enough details, sample size, tools for statistical interpretation and test. The article still conveyed a good idea that with the combination of both therapies, the ARMD patient would have an increased quality of life and safety (Markowitz, Kent, Schuchard & Fletcher, 2008). Although there are technology and therapies available for the population with ARMD, it is important for the nurse to advocate and get the resources for their client. It requires the nurse to be knowledgable about the resources and to educate and determine what would best assist the patient. 95 Abstract #070 Title: Falls in the Older Adult Authors & Affiliations: Adam Hensley, Pam DeGravelles, PhD; Southern Arkansas University Significance: Many preventative factors are contributed to many falls in the older adult population. Falls have shown to be detrimental to the health of gerontological patients, some even fatal. The clinical significance of this review was to represent different fall risk assessment tools and scales that identify the causes of falls in older adults. This population’s health is already naturally declining and being able to create safer conditions to decrease their risk of falling can prevent something worse from happening. Purpose: The purpose of this study is to determine the effectiveness of fall risk assessment scales and identifying modifiable and non-modifiable risk factors to determine further appropriate interventions. PICO Question: In older adult populations over the age of 60, how do fall-risk assessment scales prove to show a reduction in the occurrence or reoccurrence of preventative falls? Search Strategy & Screening: The literary search process used EBSCOhost, ScienceDirect, and JSTOR. Terms that were searched during the process were falls, fall-risks, older adults, assessments, and fall-risk scales.The results from each article lead me to believe that based on the assessment scales or tools used in the studies, interventions and programs were able to be identified and applied in order to create a safer environment for patients in order to reduce or prevent older adults from falling. Evidence: Data was taken over the span of 12 months over 2 separates sites in Australia. Any patient over the age of 65 that had fallen was used for this study. The Falls Risk Management Tool and Falls Risk Assessment Tool showed us that the majority of the falls occurred near the bedside from a standing position while the patient was disoriented and confused. Synthesis of Evidence: With the articles that were used and the knowledge that was taught from nursing school, the fall risk assessment tools have been proven to be effective in identifying patients who are at a higher risk of falls than others along with the factors most commonly associated with the cause of the fall. Conclusions: It was difficult for me to determine the exact effectiveness of one-specific fall-risk assessment tool. These different articles chose used different scales to collaborate and identify the factors most associated with falls ad fallrelated injuries. As for implications of nursing practice, these scales should be used more often in clinics and community homes because it has shown to reduce the possibility of a fall occurring in the future. Implications for Nursing Practice: It was difficult for me to determine the exact effectiveness of one-specific fall-risk assessment tool. These different articles chose used different scales to collaborate and identify the factors most associated with falls ad fall-related injuries. As for implications of nursing practice, these scales should be used more often in clinics and community homes because it has shown to reduce the possibility of a fall occurring in the future. 96 Abstract #071 Title: Caring for the Caregiver Authors & Affiliations: Abigail Vann, Pam De Gravelles PhD; Southern Arkansas University Significance: Caregivers may be susceptible to depression, grief, fatigue, and changes in social relationships, along with these one may also experience alterations in physical health. Purpose: The purpose of this paper is to better understand the impact family caregiving has on the caregiver’s social, emotional, physical wellbeing. PICO Question: Does being a full-time caregiver have a negative impact on someone’s life? Search Strategy & Screening: A literature review was undertaken by searching the databases of health and medicine and social and behavioral journals. Included were all journals under these titles in EbscoHost. Articles gathered range in date from 20022013. Five articles were selected to be included in the literature review. Evidence: Three overlapping topics emerged from this literature review, which will be explored further, caregiver burden, role strain theory, and caregiver preparedness. It is often the caregiver’s responsibility to provide physical and emotional care to the care receiver, which can restrict their ability to participate in scheduled activities and events of their own (Bastawrous, 2013). Employed caregivers compared to unemployed caregivers tended to have a higher level of caregiver burden, leading to more negative effects such as decline in health characterized by tiredness, back pain, and anxiety (Wang et al., 2010). According to Schumacher, et al, (2008), “preparedness was associated with lower levels of caregiver strain following hospitalization (Archbold et al., 1990).” Synthesis of Evidence: The review of the literature has found caregivers are more likely to have depression, grief, fatigue, and changes in social relationships, which increase caregiver burden and caregiver role strain. Identifying those families in the healthcare setting prior to going home, has shown to prepare them for the task of caring for a loved one. Conclusions: Evidence has shown caregivers experience many stressors which can lead to burden and role strain. There are factors that lead to burden and role strain, which can possibly be prevented. When the family caregiver is prepared they are more likely to have less emotional and physical stress. It is important for healthcare providers to catch signs of overload and strain early and intervene for the well-being of both the caregiver and care receiver. Implications for Nursing Practice: Evidence has shown caregivers experience many stressors which can lead to burden and role strain. There are factors that lead to burden and role strain, which can possibly be prevented. When the family caregiver is prepared they are more likely to have less emotional and physical stress. It is important for healthcare providers to catch signs of overload and strain early and intervene for the well-being of both the caregiver and care receiver. 97 Abstract #072 Title: Elder Mistreatment Assessment Authors & Affiliations: Dana Davis, Dr. DeGravelles; Southern Arkansas University Significance: Elder mistreatment is defined by intentional actions of physical abuse, sexual abuse, mental abuse, financial exploitation, general neglect or not reporting self-neglect. Mistreatment is common in older adults suffering from cognitive decline, decrease in ability to perform ADLs, social isolation, sharing living quarters with family, women, and those living with individuals with personality disorders or who abuse alcohol or substances. Purpose: The purpose of this review of the literature is to determine if elder mistreatment assessments available correctly identify actual and potential cases of abuse. PICO Question: Are there adequate assessment tools available for nursing personnel to use in effectively diagnosing elder mistreatment, and are said tools accurate? Search Strategy & Screening: EBSCOHost, JSTOR, and NIH (PMC) resources were used. Search terms included elder mistreatment, elder abuse, elder assessment, and abuse assessment. Evidence: The data gathered from the review of the literature findings has not yet been tested in my personal nursing experience. Synthesis of Evidence: No synthesis is available, as the findings have not yet been clinically tested personally. Conclusions: Overall, there are adequate tools for assessing elder mistreatment. Throughout each study, populations known to be vulnerable were used (i.e. elders with disease processes). As a result, these findings should be applied to every older adult we encounter as healthcare professionals and use compassion and trustworthiness when dealing with patients suspected of elder mistreatment to intervene on their behalf in an appropriate manner. Implications for Nursing Practice: This study will guide clinical personnel in more accurate assessments of elder mistreatment cases and aid in improved outcomes for a targeted population of clients. 98 Abstract #073 Title: The Causes and Challenges Associated with Elderly Homelessness Authors & Affiliations: Laura Clinton, Pamela Degravelles; Southern Arkansas University Significance: Homelessness among the elderly contributes to the stress of chronic conditions along with acute conditions while also inhibiting their access to healthcare. People who suffer from homelessness generally have more medical, psychological, and social problems than those who don’t. These problems. along with advanced age and limited access to healthcare, have created a vulnerable, at risk elderly community. Purpose: The purpose of the literature review is to determine the risk factors associated with elderly homelessness, and the challenges faced by this population. PICO Question: What cause the elderly population to become homeless, what triggers it, and what effects can this condition have on their overall health. Search Strategy & Screening: A literature review was conducted using the EBSCOhost database. Articles gathered range in date from 2005-2013. Seven articles were selected to be included in the literature review, and all are quantitative studies. Evidence: The purpose of the literature review is to determine the risk factors associated with elderly homelessness, and the challenges faced by this population. The initial search resulted in numerous articles about homelessness and the effects it has on a person’s health, but very few related to the homeless elderly population. Homelessness is defined as (a) sleeping on the streets or in temporary accommodations; (b) lacking accommodation following eviction or discharge from prison or hospitals; (c) living temporarily with relatives or friends because the person had no accommodations, but only if the stay does not exceed six months, and the person did not pay rent and was required to leave. Adult homelessness has become a significant public health problem, with the elderly homeless making up eight percent of the homeless population, or nine out of every 10,000 elderly being homeless. Synthesis of Evidence: The combined evidence from the literature outlines how at risk this elderly homeless population really is; this in turn shows how important it is for the nurses in the community to help. Conclusions: This review of the literature found that homelessness is associated with earlier mortality rates, significant morbidity and a substantial cost to families and society with worse health problems associated with the length of the time spent homeless. Implications for Nursing Practice: Theoretically healthcare professionals and especially nurses could use this information to enhance the lives of the elderly homeless. They could help identify triggers and even keep some people from becoming homeless by identifying them early on. Nurses could also begin to use mobile health clinics to help reach this vulnerable population. The community nurses could start mobile health programs to take healthcare to this population or set up reward incentives when they do come for regular care and check-ups. They could educate to the population on the importance of seeking medical attention and when they should seek it. 99 Abstract #074 Title: Elderly and the Use of Telemedicine Authors & Affiliations: William Hill, Pam de Gravelles, PhD, RN; Southern Arkansas University Significance: Clinical Significance: With many improvements, in technology; communication has become so important. Telemedicine is a part of the advancing technological world and covers a wide variety of subjects that can be beneficial to the elderly population. Most of the time, the elderly population lacks the resources to commute to medical appointments; thus making telemedicine a feasible option. The goal would be to make healthcare more convenient for the elderly Purpose: Statement of the Problem (or Purpose): The purpose of this review of literature, is to determine the effectiveness of telemedicine within the elderly population. PICO Question: Is telemedicine beneficial to the healthcare of the elderly population? Search Strategy & Screening: Articles were obtained from EBSCO Host, and the Hartford Institute for Geriatric Nursing. The articles ranged from 2005-2012, with all being from credible sources. Search terms used to locate the appropriate literature were elderly and telemedicine. Evidence: The literature search produced an initial total of 5 studies. The articles used appropriate terms and were all clinically related to Telemedicine and the elderly. In a study done by Gambetta et al.,( 2007) elderly heart failure patients were given telemedicine technology and their hospital visits were reduced, which supports the notion that telemedicine can be effective if made available. Based on a study by Chun & Patterson (2012) future direction of health care will be based off of telemedicine systems. Results of Chang et al., (2009) suggest that caregivers and family members favor the implementation of telemedicine in health care for the elderly, which would improve communication between the health care providers and the patient support cast. Synthesis of Evidence: According to this research, telemedicine will benefit the elderly and is being embraced by their caregivers and family members. It improves their care and communication between the elder, their healthcare provider and family members/caregivers. It is the way of the future. Conclusions: In conclusion telemedicine is a rising technology that can be beneficial in the long run for the elderly populations. According to research done in these articles, telemedicine can have a positive outcome going forward if made available. This research is relavent to the nursing profession because of the implications it could have in the future. Implementation of these type programs can reduce the load of nurses and maybe cut out frequent healthcare visits. This study provides relevant information related to the geriatric population and Telemedicine. Research related to this can be used to make resources more available to our elderly population. These results can be used by various health care professionals, further solidifying the need for research related to this field. Implications for Nursing Practice: In conclusion telemedicine is a rising technology that can be beneficial in the long run for the elderly populations. According to research done in these articles, telemedicine can have a positive outcome going forward if made available. This research is relavent to the nursing profession because of the implications it could have in the future. Implementation of these type programs can reduce the load of nurses and maybe cut out frequent healthcare visits. This study provides relevant information related to the geriatric population and Telemedicine. Research related to this can be used to make resources more available to our elderly population. These results can be used by various health care professionals, further solidifying the need for research related to this field. 100 Abstract #075 Title: Sleep Quality of the Older Adult using the Pittsburg Sleep Quality Index and Epworth Sleepiness Scale Authors & Affiliations: Kari Raney, Pam de Gravelles, PhD, RN; Southern Arkansas University Significance: To test the reliability and validity of established assessment tools such as the Pittsburg Sleep Quality Index (PSQI) and the Epworth Sleepiness Scale (ESS) and their effectiveness to evaluate the older adult so that reliable and consistent care can be delivered. By doing so, a proven standard of care would be established for assessment of sleep disturbances in this population as well as information for effective sleep interventions. Purpose: The purpose of this review is to explore the sleep quality of the older adult by the use of the Pittsburgh Sleep Quality Index and Epworth Sleepiness Scale and the use of interventions to promote a better quality of sleep and reduce day time sleepiness. PICO Question: Are the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale reliable and valid tools to utilize in the assessment of the older adult? Search Strategy & Screening: A search of the databases EBSCO and Science Direct was performed, using the keywords “sleep quality”, “PSQI”, “ESS”, and “older adult” to obtain information for the literature review. The articles referenced ranged in date from 2006 – 2011. A total of five quantitative articles are used to provide support to the literature review. Evidence: Two articles tested and reported the reliability and validity of the PSQI and ESS assessment tools for their effectiveness of use in the older adult. The study conducted by Beaudreau, Spira, Stewart, Kezirian, Lui, Ensrud, Redline, Ancoli-Israel, and Stone, (2011) was conducted on community-dwelling older adult black and white females 65 years and older who experience sleep disturbances. The information collected was related to age, ethnicity, and education. The study resulted in establishing reliability and validity in the PSQI and the ESS as standard, self-measurement tools. The results provided internal consistency in the test population; this study is providing nursing care with valid assessment tools in the PSQI and ESS for our older adult patients. The research article by Grandner, Kripke, Yoon, and Youngstedt (2006), the test population was the older adult category ages 59-75 based on age and ethnicity. This study made use of the PSQI, actigraphy, sleep diaries, and the CESD depression scale to further correlate the incidence and reasons for sleep disturbances in the older adult as well as to help establish validity. While the PSQI is valid when standing alone as an assessment tool, once combined with the depression scale it may “partially reflect the negative cognitive viewpoint and pessimistic thinking characteristic of depression”. (Grandner, 2006) Synthesis of Evidence: The articles regarding assessment tools expressed the strengths and weaknesses of the PSQI and the ESS, either used in their entirety or partially. The PSQI and the ESS were used consistently throughout the articles reviewed and established as valid tools for assessment in the older adult population. Conclusions: The review of results proved internal consistency in the test population, providing nursing care with valid assessment tools for Sleep quality in the PSQI and ESS for our older adult patients. By establishing validity and reliability of these assessment tools for the older adult we can put them into nursing practice, thus providing us with the information that is necessary to implement sleep interventions and provide a standard of care to patients. Implications for Nursing Practice: Once validity of these tools have been verified, it allows the nurse to implement them into practice to assess the sleep quality factors such as; subjective sleep efficiency, sleep latency, sleep duration, sleep quality, sleep disturbances, sleep medication use, and daytime dysfunction due to sleepiness. Identification of the patient’s deficit in sleep quality allows the nurse to implement therapeutic interventions such as music, aerobic exercise and reduced day-time napping. The combined effect of nurses’ implementing the use of these assessment tools and providing education of therapeutic interventions helps to promote a better quality of sleep, as well as a healthier lifestyle for the older adult population. 101 Abstract #076 Title: Fatigue and the Elderly: Expected versus Unexpected Authors & Affiliations: KC Prakriti, Pamela DeGravelles, Director BSN/AASN Programs Prakriti KC, BSN, Southern Arkansas University; Southern Arkansas University Significance: Some elderly experience more fatigue than the others. Moreover, there are some who have a mindset that fatigue is normal part of aging process. Purpose: The purpose of this work was to explore and compare different peer reviewed literature to evaluate the expected and unexpected fatigue levels in elderly population. PICO Question: Do balance-impaired elderly, elderly with sedentary lifestyles and elderly in long term care facilities experience more fatigue than healthy elderly or young adults? Search Strategy & Screening: The literature search process used Science Direct and EBSCOhost. Search terms used to locate the appropriate literature were fatigue, elderly, mobility, sedentary, aging and balance. Evidence: The literature search produced 121 peer reviewed articles. Six studies were chosen for review. Five of the articles focused on the elderly and fatigue. The sixth focused on the FACIT-T fatigue scale. Factors that impacted fatigue in elderly were sex, education, income, smoking and co-morbidity like hypertension. One of the research studies associated loss of teeth with onset of fatigue in older age. The studies indicated that elderly who had pre-existing conditions like sedentary lifestyle, were balance impaired or lived in long term care facilities encountered more fatigue than their counterparts. Different measurements scales were used in the studies - Berg Balance Scale, Vertical Analog Scales, the Timed up and Go test (TUG). The measuring scales were effective because they could successfully compare the fatigue level of healthy elderly and those who had hypertension, sedentary lifestyle or lived in long term care facility. Synthesis of Evidence: The literature review showed that fatigue is not normal part of aging. Most of the articles claimed that elderly who were balance impaired, sedentary and lived in long term care facilities experienced more fatigue as compared to their young adult counterparts. The result of almost all the studies found out that fatigue impacted independent functioning and quality of life of elderly. The research proved that fatigue is not expected or normal phenomenon in elderly population. Different factors like sedentary lifestyle, impaired balance, and residing in long term care facilities contribute towards increased fatigue in elderly as compared to their younger counterparts. Conclusions: Each population experienced more fatigue than healthy elders in the community and younger adults. They are at higher risk of poor functional mobility and balance performance than others and a lack of exercise leads to decreased functional fitness. Also, increased psychological stress led some elderly to having more fatigue than the others. Implications for Nursing Practice: As a nurse, it is important to address complaints about fatigue and educate the elderly population that fatigue is not part of normal aging process It is necessary for nurses and other healthcare providers to learn to use the Berg Balance Scale, vertical analog scales, the Timed up and Go test (TUG) appropriately and often to assist the elderly. 102 Abstract #077 Title: Prevention of Rehospitalizations in Older Adults Authors & Affiliations: Samantha LaBorde, Pam DeGravelles, RN, PhD; Southern Arkansas University Significance: Hospital discharge criteria on high risk older adults can be very useful in the prevention of rehospitalizations. More than half of older adults who are initially discharged from acute medical units (whether it is from the same problem they initially had or maybe another health problem that was looked over) are readmitted within a couple of weeks from discharge date. The ages of these older adults range from 65 years and older. Currently, there are studies that address this problem from different approaches by gathering evidence based practice data. The importance of discharge criteria will prevent rehospitalizations; however, health care professionals must recognize the relationship between older adults and the care that is provided. Purpose: The purpose of this literature review is to examine whether or not the use of standardized discharge criteria on older adults prevents rehospitalizations after initial discharge. PICO Question: Do the three themes: comprehensive assessment, communication and multidisciplinary team coordination help to prevent the rehospitalizations of older adults? Search Strategy & Screening: A literature review was undertaken by searching CINAHL and EBSCOHost. Articles gathered ranged in date from 2009-2013. Search terms used to locate appropriate literature were older adult readmission's, geriatric hospitalizations, and prevent geriatric readmission's. Evidence: The literature searched included 5 articles that were selected; 1 qualitative and 4 quantitative. The literature review examined whether or not the use of standardized discharge criteria on older adults prevents rehospitalizations after initial discharge. The studies described when a rapid assessment is performed and then treatment is provided by acute medical units will often cause other chronic health issues to be over looked. It also showed that proper communication between the health care providers and patient help to create a time for questions and clarification on any pertinent information the patient may have. It also showed multidisciplinary teams have better outcomes for patients and can reduce the number of readmission's tremendously with dedication and palliative care. Three main themes emerged from the literature; comprehensive assessment, communication, and multidisciplinary team coordination. Preventing rehospitalizations can be achieved by accomplishing the three main themes. Synthesis of Evidence: The articles and guidelines in the literature search together with the clinical evidence delivered by the authors demonstrate that by performing a full geriatric assessment on admission, employing proper and clear communication between patient and health care team members and coordinating care by using a multidisciplinary care team, rehospitalizations of older adults will be prevented Conclusions: The combined evidence from the literature demonstrates that it is vital to our older adult population that these three themes be used in an orderly manner to prevent readmission's and further complications. Implications for Nursing Practice: The implications for nursing practice can be achieved by performing a thorough full geriatric assessment on admission, utilizing proper and clear communication between patient and health care team members and coordinating care using a multidisciplinary care team. 103 Abstract #078 Title: Visitor effects on intracranial pressure of traumatic brain activity of traumatic brain injury patients Authors & Affiliations: Sadie Decker, Dr. Barbara Landrum, Ph.d Victoria Vickers, Shelby Hintson; Henderson State University Significance: Traumatic brain injury is a major medical and social-economic problem and is the leading cause of death and disability in young adults. Therefore, there is a high number of these patients present in ICU and hospital settings. Purpose: Nurses are concerned about the effects of visitor presence on spikes in intracranial pressure in traumatic brain injury patients. There is a perceived need for evidence-based practice guidelines that address whether or not visitors should be allowed for traumatic brain injury patients. PICO Question: In patients with traumatic brain injury, does allowing visitors to be present cause spikes in their intracranial pressure, and how does this affect the patient? Search Strategy & Screening: The literature search process used CINAHL, MedLine, ProQuest. Search terms used to locate appropriate literature were intracranial pressure, and traumatic brain injury, trauma, intracranial pressure monitoring, visitors, familiar voice intervention, using the Boolean operator AND. Search years were not limited due to limited resources. The article types were limited to full text, peer reviewed. Evidence: The search produced an initial total of 23,721 studies, but that number became smaller by eliminating all studies except full texts. Further limiting the results to peer review revealed 159 studies for appraisal. We concluded our search by choosing the following studies: “Relationships between intracranial pressure monitoring and outcomes in severe traumatic brain injury patients”, “Intracranial Pressure Changes and Family Presence”, and “The effects of familiar voice interventions on comatose head-injured patients”. Synthesis of Evidence: “Relationships between intracranial pressure monitoring and outcomes in severe traumatic brain injury patients” examines the relationship between ICP monitoring and outcomes in patients with severe traumatic brain injury. The study showed that ICP monitoring was not associated with reduced hospital mortality; however, there was a significant increase in mechanical ventilation duration, and ICU length of stay. “Intracranial Pressure Changes and Family Presence” monitored intracranial pressure levels during family visiting hours and compared it to the baseline levels. The results showed that there was a positive relationship between the two, and that ICP levels actually decreased in a majority of the cases when the families of the patients were present. “The effects of familiar voice interventions on comatose headinjured patients” investigates the effects of taped messages by a family member on key measures of physiological functioning in comatose head-injured patients in intensive care units. The results showed that there were no changes in the patients’ ICP levels while listening to the taped messages from a familiar voice/family member. Conclusions: ICP monitoring is not associated with a significant difference in ICU mortality or hospital length of stay. However, ICP monitoring is associated with an increase in mechanical ventilation duration, the need for tracheostomy, and ICU length of stay. There was a variance between the results from the two studies that compared family presence and familiar voices with ICP levels in traumatic brain injury patients. Implications for Nursing Practice: Since there is a need for further studies on this topic, the evidence is not yet relevant to apply in practice. The usual care at this time is the preferred practice due to the lack of evidence and current clinical practice guidelines. 104 Abstract #079 Title: Exercise in the Elderly Authors & Affiliations: Berenice Alfaro, Pam de Gravelles, PhD, RN; Southern Arkansas University Significance: In our society, the older population is expected to increase because of the “Baby Boomers.” It is important to find helpful interventions for this older population because they are prone to sarcopenia, bone loss, slower metabolism, chronic diseases, functional decline, hormonal decline, and decrease in sleep quality. Exercise is still as important in the elderly as when they were younger therefore it is essential for the medical staff to teach about the benefits of exercise to this age group. Purpose: The purpose of this literature review is to understand the older adults’ perception of exercise and discover safe, beneficial exercises for this particular age group. PICO Question: How do the elderly view exercise and how it affects their lives? Search Strategy & Screening: EBSCOhost and Science Direct Database were used to search for literature review content. Keywords included elderly, geriatrics, older people, exercise, health promotion, physical activity, nursing care, and benefits. The articles that were chosen ranged from 2011 to 2014. Of the six articles chosen, four were quantitative studies, one was a mixed study, and one was a qualitative study Evidence: Two themes were identified in the literature reviewed: older people’s views about exercise and the outcomes of physical activity programs. Wallace et al. (2014) older adult participants believe good health is when they still have energy to perform ADLs. Some believe that physical activity is necessary for achieving good health while others believe it is too tiring. So and Pierluissi (2012) discovered that many older adults perform exercise to avoid the negative effects of bed rest. Instead of their physical status declining and pain becoming present, they want to maintain a good health status by exercising. A “12-week; gym-based exercise program delivered by a qualified instructor twice each week” (Wallace et al., 2014, p.22) was performed by their older adult participants. The results demonstrated muscle gain (strength) and power with significant increase in bone mineral density. Furthermore, Jacobson et al. (2012) used six powered exercise machines and Fahlman et al. (2011) used resistance training on functional limited older adults unlike Wallace at al. (2014). Jacobson’s study demonstrated that powered exercise machines were effective in increasing muscle endurance. Fahlman et al. (2011) resistance exercise study demonstrated an increase in upper strength and lower body strength similar to the other studies, and an increase of functional ability just like in Jacobson’s study. Synthesis of Evidence: The articles in the literature search demonstrate that exercise is beneficial in the elderly population. The older adults’ perception of exercise should be acknowledged for healthcare personnel to cultivate the motivational and teaching techniques he/she will provide. Acknowledging the older adults physical abilities is important too when choosing an exercise program to prevent harm. Periodical evaluation should occur to view the effectiveness of the exercise program. Conclusions: Exercise plays an important factor in the lives of older adults. It is recommended because it improves balance, muscle strength, stability, mobility, power, physical function, sleep quality, bone density, health, wellbeing, insulin levels, and adiponectin levels. Implications for Nursing Practice: The assessment of older adults to suggest the proper exercise program is essential. Nurses should communicate with the older adult patients thoroughly to understand their perception of exercise and become aware of recent evidence- based studies to support their teaching and motivating techniques. Nurses should get more involved in their communities to help the older adults they do not encounter in their job settings. 105 Abstract #080 Title: Using the Beers Criteria for Potentially Inappropriate Medication use in the elderly Authors & Affiliations: Rebecca Moore, Pam deGravelles; Southern Arkansas University Significance: Includes knowing how to evaluate and educate not only patients but those who work for medical facilities including doctors and nurses. It is important to understand the effects of medication in the elderly and how to effectively assess the use of mediation they have been prescribed. Purpose: The purpose of this work was to explore evidence from literature, practice guidelines, and clinical setting experience to evaluate inappropriate medication use in the elderly. PICO Question: Does the Beers Criteria effectively monitor inappropriate medication use in the elderly? Search Strategy & Screening: This literature review was performed by searching the databases Science direct and Jstor. Articles gathered range in date from 2008-2013. The search terms used were “beers criteria”, “the beers list criteria”, “inappropriate prescribing”. Six quantitative articles were selected for this review. Evidence: The 4 main challenges to prescribing medications to the elderly include the age of the population, the lack of expertise by the prescribing clinicians, the gender of the population and risks associated with the multiple medications being prescribed. Synthesis of Evidence: All of the articles had their own views on the Beers Criteria. While some thought it was the most effective tool to use others felt as if it lacked information and needed to be replaced with a more up to date tool. Some did not say whether or not they agreed or disagreed. The criteria have met with critism for being too simplistic, failing to account for clinical judgment and lacking translation into measurable quality improvements (Skaar & O’Connor, 2012). All of the articles agreed in that, ineffective medication use in the elderly was increasing dramatically in those over the age of 65. Conclusions: Beers Criteria is useful for identifying inappropriate medications in the elderly population. We have discovered that while it is useful not everyone seems to agree on it. Both Doctors and Dentists have used the tool. Implications for Nursing Practice: We know that we have a problem with medication and how it is being prescribed but we fail to realize that we can make a change for the better. I am not sure if this is because we do not want to change due to setting our ways that might be more convenient rather than making a step in the right direction or just simply failure to make a change because we do not approve of the certain tools that are available. 106 Abstract #081 Title: Controversial Aging Theories Authors & Affiliations: Ashley Price, Pamela Degravelles; Southern Arkansas University Significance: The future increase in the gerontological population calls for a better understating of which aging theories the nursing profession can use as a foundation for knowledge. Building a strong foundation of understanding how we age can create great evidence based practice for prevention, intervention, and education. Purpose: Lack of consensus PICO Question: How does the controversy of aging theories affect the nursing care in the elderly population? Search Strategy & Screening: EBSCOhost was used to search using key terms such and programmed, nonprogrammed, aging theories, controversy. All five articles discussed comprised of four qualitative articles and one quantitative article. Evidence: The topics discussed in the review included modern biological theories of aging, programmed and nonprogrammed aging theories, testing predictions of the programmed and stochastic theories, and the value of nursing theory in context of evidence based practice and multidisciplinary health care. “Overall, while multiple theories of aging have been proposed, currently there is no consensus on this issue. Many of the proposed theories interact with each other in a complex way... [And] neither of them appears to be fully satisfactory” (Jin, 2010). The different articles express the controversy and portray the need of consensus on the issue. Synthesis of Evidence: All of the articles expressed this same controversy between the aging theories resulting in no absolute foundational knowledge for how we age. Conclusions: The fact that there is no consensus between the aging theories resembles the lack of a definitive of knowledge we can use to base the gerontological practice Implications for Nursing Practice: Since nursing is driven by evidence based practice it is important for our profession to obtain more research on this issue and come to a consensus. 107 Abstract #082 Title: Older Adult Suicide Prevention Authors & Affiliations: Laura Driggers, Pam de Gravelles, PhD, RN; Southern Arkansas University Significance: As our baby boomers age, suicide is becoming more prevalent in this particular population. Nurses lack proper risk-assessment training and/or risk-assessment tools on how to assess, implement, and possibly prevent suicide in this population. Purpose: The purpose of this literature review is to explore evidence from literature, practice guidelines, and clinical settings to evaluate the risk-assessment training and the use of risk- assessment tools provided to the healthcare professionals to assess depression and suicide in our older adult population. PICO Question: Are nurses participating in suicide prevention among our older adult population by assessing them for depression and suicidal tendencies during clinical office visits? Search Strategy & Screening: A literature review was conducted by searching the EBSCO host database using the search terms: older adult, elderly, suicide, prevention, nursing, nursing interventions, primary care, and assessment tools. Six articles were selected to be included in the literature review ranging in date from 2007 to 2012, while also utilizing the National Institute of Mental Health website. Evidence: There is a gap in assessing depression, properly diagnosing, and suicidal thoughts because of the complex health conditions that often mask depression in the older adult. Based on the surveys and interviews conducted, it was found that health care professionals have limited or no training in dealing with older adults experiencing depression and suicidal tendencies. Synthesis of Evidence: Statistically, it is shown that older adults experience increased risk of depression and suicide due to many circumstances that are uniquely specific to the older adult. Health care professionals are not being trained to assess our older adult population for depression early enough to provide appropriate treatment. Conclusions: Depression and suicide among our older adult population is a serious and alarming issue particularly as our baby boomers age. It is essential for all health care professionals to obtain adequate risk-assessment training and/or tools to assess for depression and potential suicidal behaviors in the older adult population. Implications for Nursing Practice: As the largest group of health care professionals, nurses interface with patients more than any other group. Nursing should conduct further research, educating and training themselves and other healthcare professionals to assess our older adult population for depression and suicide tendencies. Through continuing research, risk- assessment tools could be developed, modified, and provided to the nurses on the forefront of an older adult assessment within their primary care provider’s office thereby reducing the risk of suicide within our older adult population. 108 Abstract #083 Title: Receipt of Immunizations in the Older Adult Authors & Affiliations: Lauren Terry, Pam DeGravelles; Southern Arkansas University- Magnolia Significance: Immunizations are a crucial part of healthcare because they can prevent life threatening illness in the older adult population. Among older adults, vaccination rates vary across race and gender. It is important to investigate interventions targeted at increasing vaccination rates among the older adult population in order to raise the number of individuals receiving immunizations. Purpose: The purpose of this literature review was to search for evidence from literature to determine strategies that have been used effectively to increase immunization rates among older adults. PICO Question: In the older adult population, which interventions, compared with non- intervention, are effective in increasing influenza and pneumococcal vaccination rates? Search Strategy & Screening: A search of CINAHL, EBSCOHost, Gale Databases, and Medline Plus was performed using the search terms immunizations, older adult, elderly, vaccines, vaccinations, and aging population. Evidence: Non-Hispanic white individuals are more likely to be vaccinated than other populations, therefore it is imperative to target interventions at other racial populations. One study implemented calls to patients as reminders about vaccinations. While having the conversation, the nurses explained the risks and benefits of the vaccine, and more individuals received the vaccine if they received a phone call. Synthesis of Evidence: Upon compiling the data yielded from the literature search, it has been demonstrated that utilizing the interventions aimed at increasing the number of older adults receiving vaccinations has proven effective. It has been found that race, gender, educational background, socioeconomic status, and age are all variables linked to vaccination rates. Non- Hispanic, white individuals, females, those with higher educational background, those of higher socioeconomic status, and individuals in the younger years of the older adult category are all more likely to be vaccinated than their counterparts. Interventions including educating providers, immunization posters, mailed reminders, vaccination clinics, and personal phone calls by nurses have all lead to increased likelihood of people receiving immunizations. Therefore, high-risk groups and effective interventions were identified. Conclusions: After combining the research from the literature review, it has been determined that populations at a high risk of not getting vaccinated should be the primary targets of interventions used to increase the rate of vaccinations. Utilizing the interventions has been proven to increase vaccination rates. Implications for Nursing Practice: By increasing the vaccination rates, the health care system can prevent lifethreatening illnesses. The cost of vaccinations is substantially less than the cost of hospitalization older adults frequently encounter when influenza and pneumonia must be treated in an acute care facility. Therefore, increased vaccination rates will also save money for both older adults and health care organizations. 109 Abstract #084 Title: Importance of Assessing and Managing Delirium Patients Authors & Affiliations: Lacey Andrews, Pamela V. deGravelles, PhD, RN; Southern Arkansas University Significance: The prevalence of delirium superimposed on dementia ranges between 22-89% in individuals 65 and older (Flanagan and Fick, 2010). Many patients with delirium go undiagnosed because healthcare professionals fail to recognize delirium at the bedside. There are tools that healthcare professionals can be trained to use for diagnosis of delirium. A study by Fick, Kolanowski, and Waller found a high number of drug related problems (DRPs), such as delirium while receiving CNS-active medication. This warrants the need for further assessment by the nurse to keep the patient safe from harm and/or injury. Purpose: to discover ways nurses can recognize, assess, and manage patients with delirium. PICO Question: Do patients with delirium benefit from proper assessment and management by the nurse? Search Strategy & Screening: A literature review was undertaken by searching the database EBSCOHOST. The search terms “assessment”, “delirium”, “managing”, “cognitive impairment”, and “dementia” were utilized to gather relevant research articles. Articles gathered range in date from 2007-2012. Five articles were selected to be a part of the literature review. Evidence: Huang, Inouye, Jones, Fong, Rudolph (2012) acknowledge how difficult it is to evaluate delirium effectively at the bedside. A variety of manifestations of delirium require different assessment tools for correct diagnosis. Fick, Kolanowski, and Waller (2007) acknowledge that the time and training required to properly diagnose delirium are not being used and CNS- active drugs are being prescribed inappropriately resulting delirium. These medications put patients at risk for falls, fractures, and injury. Dementia patients inappropriately prescribed the CNS-active drug sustained more DRPs than those without. Flanagan and Fick (2010) found in their study is that clinicians avoid diagnosis using the correct tools due to lack of training, knowledge, and time. Travers, Byrne, Pachana, Klein and Gray (2012) find that 8.7% of patients without evidence of dementia had delirium at admission or developed delirium during the hospital stay. Keenan and Atkins (2011) mention that reassessing the patients with the CAM and MMSE is important because the time of day and level of the patient education can affect the results. Synthesis of Evidence: All of these authors found that there are misdiagnosis of delirium due to inappropriate prescribed medications, and lack of appropriate diagnosis due to lack of training and time. Conclusions: Patients with delirium require clinicians to recognize, manage medication use, and use appropriate assessment tools to provide better quality of care. As nurses, we should hold in-services to teach the interdisciplinary team the correct use of the assessment tools. Nurses also need to reconcile medications in the elder adult and question the purpose of the medication to the HCP. Nurses play a vital role in providing care for the patients with delirium to promote improved health outcomes. Implications for Nursing Practice: 110 Abstract #085 Title: The Effect of Baby Boomers on the Healthcare System Authors & Affiliations: Courtney Geesing, Pam de Gravelles, PhD, RN; Souther Arkansas University Significance: As the Baby Boomer generation ages and reaches retirement, there will be dramatic changes in healthcare and the healthcare system. There have been concerns regarding Medicare and health policies and these issues will be magnified as the Baby Boomer population requires more medical attention as they age. As the Baby Boomers near retirement, hospitals will lose the experienced workers at a more rapid rate leaving a gap in the knowledge and experience in the medical field. It is vital to address these issues and plan for the inevitable. Purpose: The purpose of this work was to recognize the issues that will become concerning to the Healthcare System as the Baby Boomer generation ages. By examining supporting literature and studies, we are better able to predict possible areas of concern and bring attention to the need for intervention. PICO Question: How will the Baby Boomer generation positively or negatively affect Healthcare compared to the general population’s affect on Healthcare, and how can we properly prepare for these changes? Search Strategy & Screening: This Review of Literature was performed by using CINAHL, EBSCOhost, and BioMed Central. The search terms used were “Baby Boom,” “Baby Boomers,” “Effect of Baby Boomers on Healthcare,” and “Boomers and Healthcare.” The articles used were published between the years 2007-2014. Evidence: The literature review was done by using four qualitative studies and one quantitative (cross-sectional) study article. These studies covered different aspects of the topic, but they all agreed that there will be three major effects that the Baby Boomers will have on Healthcare. The first concerning effect is that as the Baby Boomers retire, the Healthcare system will lose the values and experience of the Nurses of that generation. The next is that there will be an increased need to solve medical challenges as the number of retirees and Medicare eligible people increases. The final concerning effect is that there is an increase in patients diagnosed with obesity and diabetes in this age group, so the need for prevention and knowledge about this particular group and the diagnosis is much needed. “As the host organization, Children’s was identified as a system with the need and desire to improve retention of older nurses since nearly 60% of its nursing workforce is in the Baby Boomer age range (currently age 45 and older). My study included a system-wide look at the factors involved in older nurse retention, with the purpose of investigating the concerns of Boomer nurses to understand how hospital workforce strategy can effectively retain older nurses.” (Klug, 2009) Synthesis of Evidence: The literature search that was conducted, along with the clinical trials done agree that the Baby Boomer generation will have a great impact on the Healthcare system. It is apparent that solutions need to be made to prevent a severe negative effect as the Baby Boomer generation continues to age. One possible solution is the retention of older nurses past the traditional retirement age. Conclusions: In conclusion, all research that was reviewed points to the fact that the Baby Boomer generation will affect Healthcare in more ways than one. It is difficult to pinpoint an actual problem currently since the baby boomer generation is just now reaching the age where health concerns are more prevalent. Implications for Nursing Practice: At this point, it is more of a potential problem that we need to be prepared for as workers in the healthcare system. Policies need to be reviewed and possibly changed to prevent such a drastic impact. A possible change may be that older nurses may continue to work for shorter hours so hospitals still have the experience on the floor. Hospitals need to be prepared to hire enough workers to care for the increase in patients that are certainly going to need care. 111 Abstract #086 Title: Functional Decline in Older Adults: Assessment tools Authors & Affiliations: Morgan Saulsbury, Pam DeGravelles, PhD, RN; Southern Arkansas University Significance: Functional decline has shown an increase in mortality rates of older adults. In the elder population functional decline not only depends on the patients and their prognosis, but also on the quality of care given by nurses. The researchers in this review of literature point out various assessment tools that can be beneficial to the patient. Early detection can improve care and proper discharge planning can be essential in decreasing the functional decline rate and increasing quality of life. Purpose: The purpose of this review of literature is to investigate effective assessment tools nurses can implement to decrease the risk of functional decline in older adults. PICO Question: In geriatric patients suffering from functional decline, does implementing effective assessment tools benefit the patient after discharge? Search Strategy & Screening: This review of literature was created by searching EBSCOHOST. Five quantitative articles were obtained. Articles range from publication dates of 2006-2013. Evidence: It is suggested that “30-60% of older patients experience a decline in functioning, resulting in a decreased quality of life and autonomy” (Hoogerduijn, 2010). Identifying the risk for functional decline is a first priority in planning interventions for these patients so they do not suffer further deterioration. In this particular study the HARP shows the lowest sensitivity and the highest specificity, leading to possible underestimation of the patients who are at risk and overestimation of those who are not at risk (Hoogerduijn, 2010). The use of the Lawton scale to determine to risk for functional decline, although many aspects play a role in this some things can lead to dependency faster than others. Because the ultimate goal is prevention of functional decline, measurement of the instrumental activities of daily living (IADL) could be of interest too, not only because IADL’s are important for the patients well-being, but also because they could act as an earlier marker of ADL decline (Hoogerduijm, 2010). Handgrip strength is a physical performance test that requires little training and only requires a few minutes, with results comparable between populations (Garcia-Pena, 2013). The results were highly favorable to men. It is suggested that only males with low handgrip strength had an increased risk of functional decline at discharge with a specificity of 91.3% (Garcia-Pena, 2013) Synthesis of Evidence: This research focused on the efficacy of assessment tools such as HARP, Lawton IADLS, and Hand-Grip strength. The HARP tool showed to have “the poorest results” (Hoogerduijn, 2010) The Lawton IADL tool show that “depressed older persons with disabling hospitalizations resulting from an array of conditions were less likely to recover mobility function than those without depression. (Barry, 2011) Handgrip strength is an easily accessible tool to utilize in determining the risk of functional decline. HS is widely used in the elderly for different purposes and has been shown to be predictive of adverse outcomes in other settings. (Garcia-Pena, 2013) Information was also revealed on ways for families to be able to prepare if and when functional decline occurred in hospice patients. Conclusions: Assessment tools that take an extended amount of time are typically over looked. The assessments used should be cost efficient and only require a short amount of time because these tools are put to use upon admission. It is key that the nurse implements these tools in order to detect early functional decline after discharge. Although these tools may be effective, multiple comorbidities may result in functional decline. Implications for Nursing Practice: With proper use of these tools, the nurse can provide appropriate care to decrease functional decline, improve quality of life and extend the patient’s quality of life. 112 Abstract #087 Title: Muscle wasting in elderly women Authors & Affiliations: Shelley Coleman, Pamela V. de Gravelles, PhD, RN; Southern Arkansas University Significance: Sarcopenia is loss of muscle mass and muscle quality that has been linked to progressive destruction in autonomy and functional capabilities in the older adult. Purpose: The purpose of this literature review is to explore the relationship between decreased muscle mass and quality of life in the aging woman by synthesizing articles addressing the effects of aging on muscular strength and functional ability PICO Question: In elderly and aging women, does exercise and muscle training compared to sedentary lifestyle improve functional ability and quality of life? Search Strategy & Screening: A literature review was undertaken by searching the EBSCOhost database using the search terms: aging, women, muscles, sarcopenia, fatigue, post-menopausal, elderly, strength, exercise. Seven articles were selected to be included in the literature review and range in date from 2009 to 2012. Evidence: Twelve weeks of resistance training on physical and functional fitness in elderly women produced a training group that demonstrated moderate increase in the number of repetitions, while the control group performed a standardized stretching program. Manual skills in the training group showed a moderate reduction in time to complete the tasks. Subjective fatigue is influenced by number of comorbidities, depressive state, and levels of physical activity, functional capacity, peak torque, and perceived health. Grip, hip, and knee strength was also assessed, showing a general decline trend in mean grip, knee, and hip strength over time. Synthesis of Evidence: The aging process has been proven to cause a significant deterioration of muscle, and quality of life has also been proven to be affected by this loss of muscular strength. Levels of physical activity and perceived health are factors shown to most influence self-perceived fatigue, and exercise therapy may prevent balance disorders and falling among the elder population. Conclusions: Regular exercise is consistently associated with increased muscular strength, improvement in mobility, and may be used as a prevention method for falls, frailty, depression, obesity, and mobility limitations. Implications for Nursing Practice: Interventions that minimize sarcopenia related problems should be implemented in clinical practice. 113 Abstract #088 Title: Effects of Advanced Directives on Patient Care Authors & Affiliations: Jessica Curtis, Dr. Pam DeGravellels; Southern Arkansas University Significance: All hospitals and medical facilities in the United States are required by law to provide patients and families with information about advanced directives and they must document that they performed these actions. Therefore it is important to understand the effects ACP has on patient care. Purpose: The purpose of this work was to explore evidence from literature, practice guidelines, and clinical setting experience to evaluate wound care. PICO Question: Do advanced directives affect the quality of life for terminal patients? Search Strategy & Screening: This literature review was performed by searching the databases EBSCOhost, CINHAL, Education Research Complete, and PsychINFO. Articles gathered range in date from 2009-2013. The search terms used were “advanced directives”, “advanced care planning”, “end of life care”, and “older adults”. Evidence: The data supports that ACP is effective in improving the quality of life in terminal patients. The patients prefer an in-hospice death over an in-hospital death. It can also be conclude that a majority of patients want to receive comfort care at the end of life. As a result of this review of the literature, it can be determined that nurses and other health care officials can effectively improve the quality of life in terminal patients through the use of ACP Synthesis of Evidence: The researcher can conclude that ACP is associated with improved quality of life before death with an increased use of hospice and less in-hospital death (Bischoff, 2013). The theme of patient preferences revealed that patients prefer hospice during end of life and that comfort care the most optimized approach (Lawerence, 2009). The theme completion of the ACP process revealed that there is a disconnection between patients and health care officials during the process of completion an ACP. Conclusions: Hospice use is preferred over an in- hospital death. Knowing that patients would rather die in hospice than in a hospital can help the nurse when making decisions about ACP and patient care. More patients prefer hospice use and prefer comfort care compared to end of life care. Implications for Nursing Practice: This evidence can be used in nursing practice to help patients identify types of care they wish to receive. Even though patients are presented with opportunities several times, they are not completing AD or making ACP decisions. 114 Abstract #089 Title: Effects of Education and Attitudes Parents have Regarding Immunizing their Children Authors & Affiliations: Gary Grubbs, Patricia Loy, Ed.D., RN Megan Stone, Kenda Syler; Henderson State University Significance: Immunizations are a primary prevention treatment for diseases that can infect and seriously harm schoolaged children. The vaccines for these diseases have been proven to reduce the rate of infection significantly. A negative trend has emerged among the parents of school age children regarding immunization statuses. Education is the key to changing parents’ negative attitudes and refusal of vaccines. Purpose: In today’s world, it is simple for parents to go online and find information about their children’s required vaccinations. The problem is that most parents do not know how to find valid, reliable sources for the information they need. It is imperative that pediatricians and nurses stress the importance of asking questions when parents are curious about these vaccines; health care providers can provide correct information regarding immunization and potential complications. It is the nurses’ duty to provide information about immunizations to parents regardless of whether or not they ask for it; these parents could still have doubts or questions they may not feel comfortable expressing. PICO Question: How have attitudes and education influenced parents’ decisions regarding immunization of their children. Search Strategy & Screening: We utilized the data base CINAHL, using the search terms vaccination education. The results were limited based on several factors. The study had to have a link to the full article. The search years were limited to 2008-2014. The studies were then screened based on their relevance to our study question. Evidence: The search produced a total of 129 studies. That number dropped to 84 studies by eliminating those without a link to a full article. Further limiting results to studies that met the age requirements and pertained to our PICO question yielded 3 studies. Synthesis of Evidence: The examined articles indicate that the primary reason parents do not immunize their children is a lack of teaching and that parents respond positively to tailored educational materials. Some socio-demographic factors also play a role in immunization decisions. The articles revealed the main concerns that parents have regarding immunizations were a lack of necessity, a risk for autism, and an overloading of the immune system; these are the primary topics needed for educational materials. The reviewed materials led to an increase in governmental trust and in positive responses. Conclusions: Providing educational materials to under-educated parents can increase compliance with the ideal injection schedule for school aged children; therefore, we recommend an increase in the quality and amount of educational materials available to parents. Implications for Nursing Practice: An educational intervention would not be expensive to implement; most of the information could be given verbally or on paper and include the consequences of not vaccinating, the possible adverse effects of the vaccination, and the general information about the disease they are made to prevent. Improving education methods would be the best strategy to increase the number of children being immunized. 115 Abstract #090 Title: Loneliness and the Older Adult-Effective Strategies of Intervention Authors & Affiliations: Antonia Martin, Pamela DeGravelles, PhD, RN; Southern Arkansas University Significance: To evaluate the interventions (nursing and non-nursing) preformed across various healthcare settings and its effectiveness in the older adult population as nurses constitute one of the largest providers of care and therefore are at the forefront of this loneliness phenomenon. Purpose: The intention of this literature review is to explore successful strategies of intervention to decrease loneliness in the older adult. PICO Question: Are the current loneliness scales reliable and valid tools to utilize in the planning of successful interventions for the older adult? Search Strategy & Screening: To conduct this literature review a search was performed using CINAHL, Health Source Consumer Edition, Google Scholar, PsychInfo and Medline databases. Collectively the articles garnered range from 2004-2011. Evidence: A total of nine articles are used to provide support to the literature review. Three of the experimental articles utilized and reported the reliability and validity of the UCLA Loneliness Scale, and a few others, while the remaining articles used for this literature review assessed intervention tools with a test-retest method for their effectiveness of use in the older adult. Synthesis of Evidence: The three studies utilized information from older adults, male and female, living in the nursing home, institutions, and the home. Researchers were interested in the participants’ demographics, degree of social support, and level of emotional performance. Each article utilized a different approach regarding assessment tools. Conclusions: The study resulted in establishing reliability and validity in scales utilized as a standard tool for loneliness measures in the older adult. Although specific loneliness instrumentation did not provide significant differences in the studies the results were representative of statistically significant results in the intervention populations on the basis of socialization and other variables. Implications for Nursing Practice: Loneliness has a debilitating effect on the health of the older adult and interventions should be directed toward prevention as to avoid any decline in mental, emotional, or physiological functioning. The gerontological nurse must learn to recognize loneliness and be skilled in interventions to treat. 116 Abstract #091 Title: Housing the Elderly Authors & Affiliations: Morgan Sinclair, Pamela DeGravelles PhD; Southern Arkansas University Significance: The health care system must be aware of the older adult needs, whether it be mentally or physically. Simply taking the time to interact with them appears to make a huge difference in their sense of well-being. Making adjustments to living facilities is also a major concern. Showing the older adults that they matter will improve their sense of well-being. Providing the older adult with adequate information about their living arrangement options is very significant. The older adult should be involved in the choice of their living arrangements. A continuation of interviews would highly benefit the older adult due to the fact of changing emotions and feelings. It is of the utmost importance that the health care providers know how the elderly feel and their sense of well-being. Purpose: The purpose of this literature review is to explore the types of care offered to the older adult that can no longer function safely in the home environment alone. Also, another purpose is to examine the emotions the elders experience when being care for in these particular health care settings. PICO Question: Do various housing options affect the elderly’s quality of life? Search Strategy & Screening: The literature review was conducted searching various databases such as: EBSCOhost, and JSTOR. The data filled articles ranged from year 20082013. The review consisted of five total articles selected: 3 qualitative and 2 quantitative. Evidence: Individuals living in the sheltered housing evaluated their quality of life more positively than the older adults living independently. (Van Bilsen et al., 2008) The older adults learned that they must wait whenever they have a need for assistance from the health care providers working in the facility (Hellberg et al., 2011). The physical and mental condition of the patients affects the care they receive from the staff; therefore altering their views of the care they are receiving (Darton et al., 2011). Having living quarters that are adequate for the older adults will most likely improve the elder’s views on life and therefore; improve their quality of life (Paiva & Bruere, 2012). The data shows the elderly feel special and have a better sense of well- being when someone takes their own time to spend with them. The elders will benefit greatly from extra time taken out to care for them and to simply show that they are cared for (Lundin et al, 2013). Synthesis of Evidence: Depending upon the location and the care the older adult receives, their view may differ and their emotions may be alters about their experience in the living facilities. The living environments must be made according to the elders needs. The facility has to be engaged with the elderly patients for the patients to have a sense of well-being. Conclusions: Overall, healthcare professionals caring for the older individual must be aware of their feelings and emotions. The older adult will benefit from the extra time spent with them and they will have a better sense of well-being. Time is the most important when it comes to caring for the older adult. The older adult’s experience should always be taken into consideration when care for them. This will allow for the best care to be given both, mentally and physically. Implications for Nursing Practice: The nurses can set aside time to show the elder adults care and compassion. The elderly need to feel as if the nurses truly care for them. 117 Abstract #092 Title: Telemedicine and the Older Adult Authors & Affiliations: Brandy Litton, Pamela DeGravelles, PhD, RN; Southern Arkansas University Significance: There is a growing population of aging adults. Telemedicine could provide an enhanced method of providing healthcare to these individuals. Understanding the attitudes and limitations of the older adults in using the telemedicine is of great importance. Although research had been done to understand the attitudes and limitations of telemedicine in the older adult, more in-depth research is needed to bridge the gap between the proposed use of telemedicine and the actual functionality of telemedicine Purpose: The purpose of this literature review is to explore the various attitudes of the older adult towards telemedicine. PICO Question: In the older adult population, does the attitude of the older adult towards telemedicine impact the effectiveness of the technology? Search Strategy & Screening: The literature search process used CINAHL and Medline. Search terms used to locate the appropriate literature were telemedicine, geriatrics, and older adult. Evidence: Five articles were selected for this review of the literature: two quantitative and three qualitative. Three main themes emerged from the literature: maintaining independence, user friendly technology, and skill of those delivering telemedicine care. Training of staff to learn equipment, ease of use, and availability of telemedicine equipment had a direct impact on receptiveness of the older adult in utilizing telemedicine. Synthesis of Evidence: With the growing population of older adults, one aim of healthcare is to provide quality care while allowing them to live at home. In this case, telemedicine is a viable option. Home telecare systems are generally easy to use. With proper training, older adults are receptive to the use of telemedicine in their homes. Authors stated that nursing staff should also be educated in the proper use of the telemedicine equipment to better utilize and educate the elderly in the use of technology. Proper training for staff facilitates acceptance in the older adult population. All authors agreed that telemedicine can be a viable option to allow older adults to remain in their homes while receiving quality healthcare. It requires understanding by both staff and the older adults utilizing the technology. The articles and clinical experience demonstrate that the use of telemedicine to enhance healthcare delivery to the older adult population is a viable option. Conclusions: Older adults are open to telemedicine if it allows them to stay in their homes and communities. Older adults are open to utilizing the skills necessary to use telemedicine. Education of the nursing staff in the use of telemedicine can greatly impact the receptiveness of the older adult. Implications for Nursing Practice: Utilization of telemedicine can help the nurse provide better care of patients in their homes by providing access to doctors that can “see” the patients. 118 Abstract #093 Title: Identifying Intensive Care Unit Patients at Risk for Chronic Post-traumatic Stress Disorder Authors & Affiliations: Briana Hines, Tamisha Henderson, MSN, RN, CCN Jennifer Orahood, Linise Phillips, Caleb Stark, Whitney White; University of Arkansas for Medical Sciences College of Nursing Significance: Post-traumatic Stress Disorder (PTSD) is defined as a psychological disorder resulting from a stressful or traumatic event. Events directly involve or are witnessed by individuals. Those suffering from PTSD may relive or reexperience events through flashbacks, hallucinations, and illusions. Clients with symptoms of PTSD may also experience nightmares, behavior changes, be emotionally numb, abuse substances, and have increased arousal such as sleep disturbances. Clients diagnosed with this disorder are at an increased risk for self- harm. Manifestations of PTSD last at least a month and can persist for years. For this literature review, chronic PTSD is defined as lasting more than three months. Purpose: The purpose of this literature review was to gather evidence about the predictors of patients from intensive care units (ICU) at risk for chronic post-traumatic stress disorder (PTSD). PICO Question: For the ICU patient, what predictors identify risks for chronic PTSD? Search Strategy & Screening: The literature search process involved a PubMed search using the following search terms: post-traumatic stress disorder and intensive care unit patients. Search limitations included free full text articles, publication within the last 5 years, human species, and English journals. Evidence: The initial search using the search terms resulted in 239 articles. After limiting the search to free full text, published within the last 5 years, human species, and English journals, the search narrowed to 24 articles for appraisal. Out of the 24 articles returned, we reviewed six articles. The 4 articles selected for this project were based on inclusion of PTSD, post-ICU follow-up, availability, and most recent year of publication. Synthesis of Evidence: One study, using the Impact of Event Scale (IES), showed that at twelve months post-ICU admission, 27% of clients reported scores identifying PTSD. The major factors identified were high education, personality trait of optimism, factual recall, and memory of pain, each with a 95% Confidence Interval (CI). A second study, using the PTSD Checklist Civilian Version, showed that at twelve months post-ICU admission, 15% of clients reported PTSD symptoms. The major factor identified was inhospital substantial acute stress symptoms associated with PTSD at 95% CI. A third study, using the Davidson Trauma Scale, IES, and Post-traumatic Symptom Scale, showed that at nine months post-ICU admission, 38% of clients reported PTSD symptoms using the Davidson Trauma Scale; 29% based on the Post-traumatic Symptom Scale; and 8% based on IES intrusion and 22% based on IES avoidance, all at 95% CI. The major factors identified were younger age and use of prescription psychoactive medication at the time of ICU admission. A fourth study compared saliva samples to results of PTSD Checklist Civilian Version. At twelve months post-ICU admission, 14% reported PTSD symptoms. A genetic factor identified clients homozygous for the corticotropin-releasing hormone binding protein was linked to fewer PTSD symptoms with 95% CI. Conclusions: Clients who are post-ICU admissions are at risk for chronic PTSD symptoms. While there are many factors that may predict this, the underlying factor in this survey is surviving ICU admission. Understanding that chronic PTSD symptoms is a risk of post-ICU admission should encourage more studies to be performed in an effort to determine how to provide preventative and follow-up care for clients during and post-ICU admission. Implications for Nursing Practice: Nurses working in the ICU should be aware of the risk for PTSD post-ICU admission, understand what PTSD is, and how to assess for PTSD symptoms. Nurses can encourage patients and families to keep a journal of the ICU experience as well as provide assistance in communicating with clients, families, and medical staff in an effort to promote the clients’ well being. 119 Abstract #094 Title: Pay for Performance Policy Effect on Primary Care Hypertension Management Authors & Affiliations: Stephanie Kitch, BSN, RN, Jean McSweeney, PhD, RN Claudia Beverly, PhD; Donna Gullette, PhD;University of Arkansas for Medical Sciences Significance: Nearly one-third of American adults have hypertension. In many cases, hypertension can be prevented or maintained through healthy lifestyles, including medication adherence, proper diet and alcohol moderation, physical activity, and smoking cessation. Yet, more than half of those with hypertension do not have adequate blood pressure control. This presents a financial and societal burden that must be addressed effectively and efficiently. One policy-based approach is that of pay for performance, or financial incentives provided to health care providers upon achievement of standardized blood pressure management outcomes. This policy is designed to improve hypertension management in primary care. However, the effect of this policy on hypertension management outcomes has not been systematically reviewed. Purpose: The purpose of this systematic review was to examine and synthesize evidence regarding effectiveness of pay for performance policy on hypertension management quality outcomes in primary care. PICO Question: In primary care of adults with hypertension, does the pay for performance incentive policy for achieving management goals lead to improved hypertension management outcomes, as compared with non-incentivized usual care? Search Strategy & Screening: The literature search process used Pubmed, CINAHL, PsychInfo, EBSCO, and GoogleScholar. Search terms included: hypertension, management, chronic illness, pay for performance, financial/provider/physician incentive, reimbursement, performance based financing, healthcare economics, compensation, quality improvement, quality outcome, performance quality, quality measures, primary care, outpatient, managed care organization, and extrinsic/intrinsic motivation. Evidence: The initial search produced 198 articles focused on 1) financial based performance and 2) quality indicators, 3) direct relationship between financial incentive and hypertension outcomes, 4) based in primary care, and 5) published between 1990-2014, which encompassed pre, during, and after pay for performance implementation. Sixteen articles were selected for final inclusion. Based on the evidence, there is limited or contradictory evidence of the effectiveness of pay for performance on hypertension quality outcomes. Seven reported statistically significant hypertension quality outcomes; yet another 7 reported insignificant results. Four reported initial positive results that would plateau or taper over time. Other studies reported hypertension outcomes already near goal levels before policy implementation. These findings indicate pay for performance may be effective in a limited capacity, or in the short term. Synthesis of Evidence: The literature search yielded a number of patterns related to the implementation and effectiveness of pay for performance. These included a lack of long-term effectiveness, varying outcome measurements reported, varying approaches to and amounts of incentives, and varying results for different chronic illnesses, even when an identical pay for performance approach was used. These patterns of variability highlight the limitations of using a widespread policy approach to hypertension management. There is also lack of agreement about the best policy or incentive approaches, among policy makers and care providers alike. Notably, this policy approach does not account for individual behaviors necessary for adequate hypertension management. Conclusions: The literature reveals moderate and mixed short-term improvements related to pay for performance hypertension outcomes. However, alternative solutions are still needed to achieve adequate hypertension outcomes. Implications for Nursing Practice: Optimal hypertension management and outcomes depend on a partnership between care provider and patient. Nursing, as part of this partnership, must continue to labor toward an environment or support system that encourages crucial patient engagement and self-management. Likewise, future research should focus on identification of evidence that will guide effective policy development and implementation. 120 Abstract #095 Title: Effective Interventions to Decrease Childhood Obesity: Parental Role Authors & Affiliations: Jennifer Bailey, Dr. Laura Evans Leigh Ashley Gamble, Paesha Kindells, Shaynna Tanner; University of Arkansas at Monticello Significance: Obesity in children and adolescents is a large and growing problem in today’s society. Approximately one third of all children and adolescents are overweight in the United States. Obesity can affect the child’s emotional, social, and general well-being. Purpose: The purpose of this project was to review relevant literature related to the parental role in preventing obesity in children and to report best nursing practices to decrease childhood obesity. PICO Question: What interventions to encourage parental involvement are effective to decrease obesity in persons eighteen and under? Search Strategy & Screening: The literature search process used CINAHL Database and Academic Search Complete. Search terms used to locate appropriate literature were childhood obesity, school aged, parent’s role, interventions, and parental involvement. Search years were limited to 2010 through 2015, and article types were limited to research reports. Quality screenings included ensuring the researchers were qualified to conduct the study and the Johns Hopkins Nursing Evidence Based Practice (JHNEBP) Research Evidence Appraisal. Evidence: The search produced a total of 73 studies from CINAHL and 129 studies from Academic Search Complete. A review of titles decreased the sample to 12 relevant studies. Quality critiques using the JHNEBP Research Evidence Appraisal decreased reports to 11 research studies comprising the sample. Synthesis of Evidence: Six studies indicated that educational classes, camps, and activity assignments sent home as homework were beneficial to parents and children. All of the parents and children that received educational material had either weight loss or a positive dietary change. Parenting style, level of involvement, and views of the parent also had an impact on the success of the child’s weight loss and how the parent managed the child, but authors stated further research is needed to support this. One study stated that a child with two obese parents was six times more likely to have unsuccessful weight loss than a child whose parents did not have weight problems. Two articles identified that restricting all unhealthy food had a negative impact on the child’s weight loss but increasing parental monitoring of the diet is beneficial. One article found that the obese children were aware they needed to lose weight but felt they needed more involvement from their parents to be successful. Several studies identified that the behavior, attitude, and willingness to change had a major role in the success of weight loss. Conclusions: Educating parents to be non-judgmental and supportive and to stay involved in their children's diets are important to decrease childhood obesity. Implications for Nursing Practice: The most beneficial intervention noted was education. Teaching both parents and children about diet, exercise, and coping strategies is key in helping to prevent and treat childhood obesity. Parents should give positive reinforcement to the child, not use food as a reward, restrict all unhealthy foods, or fight with the child about their weight. 121 Abstract #096 Title: Evidence-Based Nursing Interventions for the Prevention of Ventilator-Associated Pneumonia for Patients in the ICU Authors & Affiliations: Marcos Romero, Dr. L. K. Evans Ph.D, RN Christina Patton, Andres Villeda, Valerie Johnson; University of Arkansas at Monticello Significance: Ventilator-associated pneumonia (VAP) is a preventable outcome and is the second most common healthcare-associated infection (HAI) in U.S. ICUs. Nurse-led interventions for care of critically ill intubated patients can help decrease the incidence of VAP. Purpose: Statement of Problem: The purpose of this project was to provide evidence-based nursing interventions that can decrease VAP incidence in mechanically ventilated ICU patients. PICO Question: What interventions are effective in decreasing VAP incidence in mechanically- ventilated patients in the ICU? Search Strategy & Screening: Search terms ventilator-associated pneumonia and interventions for VAP were used in CINHAL, yielding 54 articles. In PubMed database, 180 articles resulted with the search terms ventilator-associated pneumonia and nursing (using the Boolean operator AND). Inclusion criteria included research articles recommending nursing care interventions to reduce VAP in ICU settings. Exclusion criteria included studies published before 2010, studies not including nurses, and studies conducted in under-developed countries. Study reports were appraised for relevance and quality using John Hopkins Nursing Evidence-Based Practice Research Evidence Appraisal (JHNEBP) criteria. Evidence: The search produced a total of 234 articles of which 12 were selected as relevant for the project. Synthesis of Evidence: Seven out of twelve articles discussed the importance of oral care, including use of toothettes, 1% chlorhexidine, and teeth brushing to decrease oral bacterial counts. Six studies discussed suctioning on a regular basis following frequent assessment and for ten seconds prior to position change, four mentioned a head-of-bed elevation of 30-45 degrees to prevent aspiration, three discussed sedation interruptions and daily assessment of extubation readiness, and three educated nursing staff on protocols for ventilator care. Two articles discussed use of hand washing and using gloves, and one implemented an abdominal massage twice daily 30 minutes prior to enteral nutrition feedings to decrease abdominal distension and gastric residue. Finally, two studies included ZAP VAP posters posted by the bedside wall to ensure proper care. Conclusions: VAP is a nosocomial, life-threatening infection that can be prevented by appropriate nursing interventions in intubated, critically ill patients in the ICU. Implications for Nursing Practice: While all of these interventions are vital to the prevention of VAP, studies have shown that bundle care using multiple interventions prove to significantly reduce the incidence of VAP. Educating other health-care workers on how to prevent VAP rates is important as well, such as creating classes promoting knowledge of an effective care protocol for these particular patients. 122 Abstract #097 Title: Evidence of the Effectiveness of Assessment tools for Palliative Care in Dementia Patients Authors & Affiliations: Laura Gill, Dr. Laura Evans PhD Rachel Goodwin, Richard Rabb, Destiny Randolph; University of Arkansas at Monticello Significance: There is a high incidence of under-assessed pain and distress in persons with late stage dementia. Their inability to effectively communicate or express emotions leads to individuals with improperly treated pain. These people are entitled to the same standards of pain assessment and treatment as any other patient. Purpose: The purpose of this paper is to gain knowledge about different tools to better assess pain and distress in patients with late stage dementia. PICO Question: What screening tools can improve palliative care in late stage dementia patients? Search Strategy & Screening: The literature search process used the CINAHL database and MEDLINE database. Search terms included: pain tools, dementia, palliative care, dementia pain, dementia and palliative care, assessment dementia pain. We limited the search to Full Text. We limited the search years between 2009 through 2015 and limited to research reports. Quality was critiqued using the Johns Hopkins Nurse Evidence Based Practice (JHNEBP) tool. Evidence: The search produced 132 articles in MEDLINE and 11 to 21 articles in CINAHL complete. Review of titles and abstract, along with quality critique using the JHNEBP tool resulted in a final sample of 12 research reports. Synthesis of Evidence: Nine of the 12 articles used various toolkits to assess pain and distress/behavioral symptoms. Eighteen toolkits were used in these nine articles. PAINAD, DisDAT, MOBID, and PACSLAC were reviewed in two different research articles. The PAINAD and MOBID was found to be useful in screening for pain. DisDAT was deemed useful for distress. PACSLAC was useful for ongoing pain assessment. PAINAD and PACSLAC were also deemed useful for nonverbal clients. One of the nine articles used an observational scale, and was found to not improve pain interventions. Two articles assessed the barriers to pain relief and assessment in late stage dementia patients from the medical nursing staffs’ point of view. Communication was the biggest barrier to pain assessment in both nurse to patient interaction and nurse to physician interaction. The final article assessed the usefulness of touch in decreasing pain and distress while increasing calmness among patients with dementia and their care givers. Touch significantly decreased agitation and increased happiness among the dementia subjects and their care givers. A majority of the studies stressed the importance of advanced assessment of pain and distress in patients with advanced dementia. Conclusions: Pain and distress is frequently not assessed and/or treated in Alzheimer patients with advanced disease. Using the appropriate tool is important to both assess and ensure adequate treatment in this patient population. Implications for Nursing Practice: With the proper tools to assess pain and distress in late stage dementia patients, nurses can more adequately recognize and treat their physical and emotional needs. Better treatment of this allows for a happier patient and care giver and more comfortable times for the patient in their end of life care. 123 Abstract #098 Title: Establishing a Motivational Interviewing (MI) Learning Community Authors & Affiliations: Sandra R. Brown, Carrie E. Plummer, PhD, ANP-BC Terri A. Donaldson, DNP, ACNPBC, Treasa Leming-Lee, DNP, CPHQ, Joseph A. Banken, PhD; Vanderbilt University School of Nursing Problem & Purpose: Traditional advice giving, a mainstay in healthcare settings, is rarely effective in evoking sustainable behavior change. As an evidence-based alternative, MI is a collaborative conversation used to evoke intrinsic motivation and commitment to change. Motivational Interviewing training is typically offered as a one-time immersion workshop, where participants learn about MI but do not learn application skills or have the opportunity to practice outside of the immersion training. The purpose of this project is to establish an MI Learning Community to increase provider competence and confidence to integrate MI into daily practice. PICO Question: Will providers who participate in a MI Learning Community increase competence and confidence to integrate MI into daily practice as measured by the VASE-R, self-report, and peer observation? Evidence-based practice models & process: The Model for Improvement (MFI) which has two parts, guided the project. Part One has three fundamental questions: what are we trying to accomplish; how will we know that a change is an improvement; and what changes can we make that will result in an improvement. Part Two is the Plan-Do-Study-Act (PDSA) cycle. Relevant Literature: Patients receiving MI interventions have better health outcomes (Carey et al., 2006; Lundahl et al., 2013; Robbins et al., 2012). Qualitative studies examining MI training reveal one-time workshops are insufficient to build provider skill (Abramowitz et al., 2010; Baer et al., 2004; Duff & Latchford, 2013; Miller & Mount, 2001). Learning communities and peer coaching are effective mechanisms for achieving competency (Joyce & Showers, 1996; Schwellnus & Carnahan, 2014; Thorn, McLeod & Goldsmith, 2007). Competency and fidelity in performing MI skills, like other skills performed by healthcare providers, require continued practice with occasional peer-review. Miller and Rollnick (2012) present an MI Learning Community as a method to build upon an initial training in order to enhance retention of and improve utilization of MI skills. Methods: Five providers participated in six, 60-minute learning sessions over six consecutive weeks, engaging each other in collaborative conservations about behavior change. Baseline and post assessments were conducted using the Video Assessment of Simulated Encounters- Revised (VASE-R). The VASE-R is a proctored, evidence-based MI proficiency assessment tool, which was scored by MI trainers. Following baseline assessment, members of the community were given individual feedback about their proficiency from components of the VASE-R. Each session includes opportunities for practice, peer coaching, and observation from MI trainers. A postVASE-R will be administered at the final MI Learning Community session. Outcomes: VASE-R scores will measure differences from baseline to post-learning community proficiency. Participant pre and post self-rating scores will also be compared. Anticipated outcomes are increased proficiency and confidence in applying and sustaining MI skills. Conclusions: Participation in the MI Learning Community will demonstrate an increase in VASE-R proficiency scores. Participants will exhibit, during the Learning Community and by self-report, increased confidence in applying MI skills. Implications for Nursing Practice: Nurses have an indispensable role in assisting patients with behavior change to improve health status and health outcomes. Ongoing practice, coaching, and feedback are essential to acquire MI knowledge and skills. Establishing MI Learning Communities can have a positive influence in how nurses integrate MI into daily practice. Nurses can be change agents in initiating, sustaining, and spreading the concept and application of an MI Learning Community. 124 Abstract #099 Title: Perinatal Mortality Rates Compared in Home and Hospital Births Authors & Affiliations: Anna Davis HSU Nursing Student, Dr. Patricia Loy, Ed.D., RN Tess Langley, Clayton Sorrells, Olivia Rogers; Henderson State Henderson Problem & Purpose: The potential complications for home births related to limited resources, inadequately trained personnel, and availability of emergency services were thought to lead to higher mortality rates in home births. PICO Question: The research question the study attempts to answer is, “In perinates, is the mortality rate higher in home births compared to hospital births?" Evidence-based practice models & process: Relevant Literature: The three studies and meta-analysis that were reviewed, showed similar statistics for perinatal mortality rates in home and hospital births. However, we had a disconfirming article that showed slightly higher mortality rates in home births. The studies looked at low risk women that gave birth either in the hospital or at home, with the assistance of a midwife or physician. Methods: A search of CINAHL Complete, Consumer Health Complete-EBSCOhost, Health Source-Consumer Edition, HealthSource: Nursing/Academic Edition, MEDLINE, using the search term home births vs home births AND United States AND mortality rates produced 30,906 research reports. After the limits of full text, scholarly (peer reviewed), and published from 2009 to 2014, only 1,737 were yielded. Only low-risk women were chosen for our review. Outcomes: The three studies and meta-analysis that were reviewed, showed similar statistics for perinatal mortality rates in home and hospital births. However, we had a disconfirming article that showed slightly higher mortality rates in home births. The studies looked at low risk women that gave birth either in the hospital or at home, with the assistance of a midwife or physician. Conclusions: Evidence revealed there were no difference between mortality rates in home and hospital births; therefore, we do not suggest one place of birth over the other. Although there were no significant differences in the mortality rates related to birth settings, a decrease in interventions may make home births more appealing to expecting mothers. Implications for Nursing Practice: When helping low-risk women choose a place of birth, it would be helpful to share the findings of our study with future mothers. Some women may wish to avoid interventions and reduce complications that are often seen in the hospital setting. By offering this information to a future mother, it can reduce the anxiety of choosing a birth setting and help her decide which setting is best for her. 125 Abstract #100 Title: Is the Mini Nutritional Assessment (MNA) Essential for Geriatric Patients as a Preventive Tool? Authors & Affiliations: Sonya L. Gulley, Dr. Pamela DeGravelles; Southern Arkansas University Significance: Older adults, due to the normal aging process, poly drug use, and comorbidity are at an increased risk for malnutrition; early detection is imperative. Purpose: To establish if the Mini Nutritional Assessment is essential as a preventive tool to aid in the health and outcome of older adults. PICO Question: Can older adults benefit by nurses using the MNA? Is there evidence that the use of the MNA leads less hospitalization, decreased hospital readmits, less infections, and decubitus ulcers? Search Strategy & Screening: The research tools and process used were CINAHL via EBSCOhost, Medline, PubMed, PubMed plus, and one educational text book. The predominant search terms used were mini nutritional assessment, MNA, elderly, prevention, malnutrition, and nutrition. Other terms used were geriatric, aging, United States, and North America. Evidence: The research yielded seven articles, two of which were too dated to use. The five final articles used by the reviewer were found on EBSCOhost. Four subjects of discourse were revealed: the broad use of the Mini Nutritional Assessment (MNA); the prevalence of malnutrition is older adults; the comparison of the MNA to other assessment tools; and the fact tool has not been tested in the context of preventing disease. It has been found that the MNA is mainly used after patients presenting with known illnesses. Synthesis of Evidence: The literature review was done by using five quantitative studies, one of which was retrospective. The articles were found to parallel practices seen in clinical settings. MNA tool is often used in clinical settings, and it can identify when clients are at risk for malnutrition, but has not been seen used as a preventive tool. The review of the literature indicates that the Mini Nutritional Assessment (MNA) is essential; it can be used routinely in most settings, but there is no evidence that says it is essential as a preventive tool; not enough research done on patients prior to evidence of illness. Conclusions: The Mini Nutritional Assessment has been tested in many settings, with results indicating that malnutrition is prevalent; there is a need for routine nutrition assessment before the process of disease has exacerbated. The review of the literature indicates that the Mini Nutritional Assessment (MNA) is essential; however, there is no evidence that says it is essential as a preventive tool. There’s not enough research done on patients prior to evidence of illness. Implications for Nursing Practice: One of the main goals of nursing is health promotion and disease prevention. The MNA has not proven to be valuable in that aspect; however, it has great potential in being an aid to nurses. 126 Abstract #102 Title: Effective Rehabilitations for Patients with Brain Disorders Authors & Affiliations: Shelby Sanders, Pamela DeGravelles, PhD, RN; Southern Arkansas University Significance: Most brain disorders are not curable; only treatable. The researchers in this review of the literature have revealed effective rehabilitation therapies for patients with brain disorders. Although the rehabilitation therapies alone cannot treat the disorder, their effectiveness in conjunction with medications should be taken into consideration. Because each disorder has a different etiology, the therapy and rehab is focused on the disability of the individual. Purpose: The purpose of this literature review is to discover how rehabilitation therapies are effective in promoting the quality of life of an older patient with brain disorders such as Parkinson’s disease, stroke, dementia and brain injuries. PICO Question: In the geriatric population with Parkinson’s disease, stroke, dementia and brain injuries, do rehabilitation therapies for each individual disease promote the quality of life and functional ability in conjunction with pharmacological treatment? Search Strategy & Screening: The literature research was completed by searching the database EBSCOHOST. The literature was found by searching the terms: “Parkinson’s disease”, “stroke”, “dementia”, “brain injuries”, “older adults” and “rehabilitation therapies.” Evidence: Five articles were chosen ranging from years 2005-2013. The rehabilitation therapies found in the literature search include: EXPLICIT-strokemCIMT program, Neurodevelopmental Treatment, Motor Relearning Program, CARE program, PASS model for neurorehabilitation and typical physical exercise. The mCIMT focuses on upper limb recovery for patients with 2 week stroke onset. It involves improvement of wrist and finger extension as a key factor for regaining skill. Neurodevelopmental treatment is to reduce spasticity post stroke by promoting neutral posture, normal positioning, and normal movement. Motor Rehabilitation Program consists of motor tasks, training of controlled muscle action, and control over the components of movement for the tasks. The priority is to set goals that acknowledge skills that were important prior to stroke. The CARE program was developed to compare functional outcomes between two groups: older adults with cognitive impairment and those with intact cognition. It screened for cognitive impairment, depression and the level of functional dependence. Throughout 11 days of service, there was a 3.9-point functional gain and the cognitive impaired achieved a greater improvement in functional gain. Regular exercise for Parkinson’s disease patients starts with an initial assessment: disease severity, independently mobile indoors with or without walking aid, and absence of neurological problems or severe comorbidities. It focuses on cardiovascular fitness, strength and flexibility, balance, posture, and gait posture. The PASS model believes three principal functional units of the brain that should be assessed during rehabilitation therapy: arousal attention, simultaneous and successive and planning. The neurorehabilitation focuses on that criteria to reestablish functional ability and reengagement of vital life activities. Synthesis of Evidence: Each therapy represents a rehabilitation therapy that is appropriate for each individual regarding their disability. Although each is different from one another, completion of the programs showed an increase the patient’s quality of life. Conclusions: It is easy for non-pharmacological treatments to be overlooked for an older adult with brain disorders for reasons such as physical limitations or advanced age. Implications for Nursing Practice: Assessment of strength and coordination by the nurse can be implemented by simply getting a patient to squeeze hands or hold up certain fingers. It should never be assumed that a patient cannot overcome a disorder, therefore these therapies should be considered to help patients regain function rather than treat symptoms. 127 Abstract #103 Title: Restraint Use: The ability to do without Authors & Affiliations: Angela Walker, NS, BSN, Pamela Degravelles, PhD, RN; Southern Arkansas University Significance: The use of restraints has been an issue for many years because the use of restraints on the Elderly population is dangerous yet HCP continue to use them for the sake of convenience. Several researchers have delved into this topic, and have come to several different conclusions concerning what restraints are and what interventions work. In addition, the definition of restraints and safe use is unclear. Purpose: The purpose of this literature review was to find evidence of safe use of restraints in the elderly population and their effect on the healthcare environment. PICO Question: In the patient population of elderly clients, does the use of restraints create a safer and more positive healthcare environment? Search Strategy & Screening: The data collected for this review was gathered through CINHL, EBSCO Host, and an open search on Bing, an online search engine. The articles are dated from 2008-2012. Five articles were included in this literature review. Three articles are quantitative, one article is a literature review. Evidence: Articles were global set in the U.S., Great Britain, and Germany. The Barton group was the first research study team had positive use of restraints but staff had safety concerns. More research is needed, and more positive results within the interventions. “A restrained-free nursing environment is demanded as the standard of care while anything less is regarded as substandard” (Haastert, Kopke, Meyer, & Muhlhauser, 2008). Since the article is based on research in finding and creating guidelines that all facilities should use. The researchers came to the conclusion that, “it might not be sufficient to educate nurses not to use restraints or to suggest alternatives. A paradigm shift is necessary.” (Haastert, Kopke, Meyer, & Muhlhauser, 2008, p. 989) The most comprehensive definition of Physical restraints is “any device, material or equipment attached to or near a person’s body and which cannot be controlled or easily removed by the person and which deliberately prevents or is deliberately intended to prevent a person’s free body movement to a position of choice and /or a person’s normal access to their body” (Kopke, Meyer, Mohler, & Richter, 2012, p. 3071). All authors had some part of this definition in theirs. Synthesis of Evidence: There is a need for a universal definition of what restraints are and when they can be used. There are some issues due to human error or bias. Both the physician and the registered nurse or physician assistant should complete evaluations concerning placing, keeping, and removing restraints to provide a safe environment for our elders. Conclusions: The healthcare field is in need of a change regarding restraints and continues to put patients at risk. Research must continue so that there are universal rules and regulations that protect the client when concerning physical restraints. Implications for Nursing Practice: The implications for nursing practice were discussed within the article. A carefully prepared guideline may help with differences between centers. Researchers are developing a multidisciplinary practice guideline that will be going into random controlled trials before being implemented in the healthcare field. 128 Abstract #104 Title: Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Based Communities In the Rural Arkansas Delta Authors & Affiliations: Caroline Loyd, Dr. Keneisha Bryant Karen Hye-cheon Kim Yeary, PhD, Tiffany Haynes, PhD, Dennis Z. Kuo, MD, MHS, Johnny Smith, BS, Jerome Turner, MDiv, Stephanie Williams, MPH, M. Kathryn Stewart, MD, MPH, Kimberly Harris, PhD, Nakita Lovelady, MPH, Songthip T. Ounpraseuth, PhD; University of Arkansas for Medical Sciences Problem & Purpose: Clinically significant symptoms of depression have been documented in more than 20 percent of African Americans who responded in community based surveys. In addition, they are more likely to have chronic depression and experience a lower health related quality of life. Therefore, the purpose of this Community Based Participatory Research study was to formulate a culturally appropriate intervention to address depression in rural African American faith communities in the Arkansas Delta. African American churches were the avenues to the development and implementation of the intervention, because of their powerful influence and historical connections. PICO Question: Rural African American communities who participate in REJOICE will experience decreased depression symptoms compared to those who do not receive the intervention. Evidence-based practice models & process: A culturally enhanced behavioral activation (CEBA) method provided the framework for this depression intervention. CEBA aims to integrate culturally adapted psycho-education and skills training with accepted behavioral activation (BA) treatments for depression. Relevant Literature: The research team completed a literature review and found evidence that showed the success of lay health leaders’ influence in carrying out interventions. Evidence supported the impact of lay health leaders, as well as collaboration with African American churches an avenue for reaching these communities. Pastors of African American churches have also shown to have great influences on their church congregation and leading their congregation through specific interventions. As stated above, the Evidence-Based Practice model, CEBA, was used to develop guidelines for creating Renewed and Empowered for the Journey to Overcome in Christ Everyday (REJOICE). Based on BA and CEBA, we tailored the evidence-based interventions so that it was faith-based and also incorporated lay health leaders. REJOICE is a program to improve emotional health by applying Biblical principles. It is a lay leader led intervention – 8 week sessions for a group of approximately 10 participants (core activities) and two church activities (one mental health awareness and one social activity). Methods: Two counties in Arkansas collaborated to implement the REJOICE intervention. From these two counties, 3 churches from each county were selected (total: 6). Both counties will recruit church intervention sites, lay health leaders (REJOICE leaders), and participants at the same time. One county will receive the intervention, while we will delay the intervention in the other. Participant eligibility criteria include: Ages 26-50, African American, with moderate depressive symptoms with at least one risk factor, not currently being treated by a physician or health practitioner for mental illness, no cognitive deficits, and no substance abuse. Outcomes: This study is in process, but the assessment of the data will be taken at 3 points for each arm. The treatment arm (Phillips County) will be measured at baseline, two weeks post program, and then three months post program. The control arm (Jefferson County) will be measured at baseline, at two months, and two weeks after the program completion Conclusions: This study is in process, so we have not reached any definite conclusions thus far. Recommendations to establish cultural adaptation and community buy-in include: continuous communication, using our various expertise, encouraging critical discussion on conflicting cultural elements, and planning on frequent feedback during the pilot intervention. Implications for Nursing Practice: Information yielded from this study will enlighten nurses on providing evidence-based frameworks for helping patients/clients they interact with on ways to improve mental health. 129 Index (Presenters) Name Abstract No. Title of Abstract Alfaro, Berenice 079 Exercise in the Elderly Allard, Julie 062 Effects of Interventions on Depression in Caregivers Who Take Care of Alzheimer’s or Dementia Patients Allen, Amy 008 Preventing Needle Stick Injuries with new generation safety device technology: Can your device be safer? Andrews, Lacey 084 Archer, J. Presentation Place 2nd floor: Poster Area 1 Presentation Time 12:30PM-1:00PM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW105 11:00AM-11:30AM Importance of Assessing and Managing Delirium Patients 2nd floor: Poster Area 1 12:30PM-1:00PM 068 Bloodstream Infection Reduction: Utilizing Alcohol-Impregnated Caps in Patients with Central-Lines 2nd floor: 11:00AM-11:30AM Poster Area 1 Archer, Jeffrey 056 Fibromyalgia Syndrome and Hydrotherapy 2nd floor: 11:00AM-11:30AM Poster Area 1 Asfour S. 061 Effects of E-Ciggarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Bailey, Jennifer 095 Effective Interventions to Decrease Childhood Obesity: Parental Role 2nd floor: Poster Area 2 Ball, Susan 064 Electronic Cigarettes- Awareness, Perception, and Education 2nd floor: 11:00AM-11:30AM Poster Area 1 Banken, Joseph A. 098 Establishing a Motivational Interviewing (MI) Learning Community 2nd floor: Poster Area 2 Barone, Claudia P. 067 The Use of Dexmedetomidine in PostOperative Heart Surgery Patients for Decreasing Length of Stay and PostOperative Complications 2nd floor: 11:00AM-11:30AM Poster Area 1 Barron, Sharon 042 World Peace and the Standardization of Arterial Lines in a Pediatric Hospital in Arkansas Bean, Sarah 053 Psychological Differences in Adolescents Who Sexually Offend with a History of Childhood Sexual Abuse Betts, Kelly 027 Nursing Students’ Knowledge and Training During the Medication Administration Process 130 IDW106 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW226 9:45AM-11:00AM Name Abstract No. Title of Abstract Presentation Place Presentation Time IDW114 9:45AM-11:00AM 026 Adherence to Prostate Cancer Screening Recommendations after a Community/Internet-based Educational Program 045 Improving Infection Control Practices in a Long Term Care Facility through a Quality Improvement Project 2nd floor: 11:00AM-11:30AM Poster Area 1 094 Pay for Performance Policy Effect on Primary Care Hypertension Management 2nd floor: Poster Area 2 12:30PM-1:00PM Booth, Brenda M. 036 Perceived Need for HIV Testing among Rural and Urban African American Cocaine Users IDW104 2:30PM-3:45PM Borders, Tyrone F. 036 Perceived Need for HIV Testing among Rural and Urban African American Cocaine Users IDW104 2:30PM-3:45PM Brackett, C. 061 Effects of E-Ciggarettes in Smoking Cessation Brown, Lana 031 Tobacco Cessation in Older Adults: The Patient Perspective IDW104 9:45AM-11:00AM Brown, Sandra R. 098 Establishing a Motivational Interviewing (MI) Learning Community 2nd floor: Poster Area 2 12:30PM-1:00PM 018 Tracing Zeroes for Our Heroes IDW106 11:00AM-11:30AM 021 Delirium in Acutely Ill Elders: The Role of Nurses IDW106 11:00AM-11:30AM 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African 2nd floor: American Faith Based Based Communities Poster Area 2 In the Rural Arkansas Delta 12:30PM-1:00PM Burnett, Stephanie 043 Utilization of an interdisciplinary (ID) team to expand programming within an inpatient dual diagnosis program- quality improvement project. IDW106 12:30PM-1:00PM Buron, Bill 002 A Decade of Change: Nurse Practitioners in the Southern United States IDW226 2:30PM-3:45PM Burton, H. 061 Effects of E-Ciggarettes in Smoking Cessation Beverly, Claudia Bryant, Jody Bryant, Keneisha K. 131 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 Name Abstract No. Title of Abstract Presentation Place Presentation Time Burton, Haley 060 Effects of Chlorhexidine Gluconate Bathing 2nd floor: on MRSA Colonization and Infection Rates 11:00AM-11:30AM Poster Area 1 in Inpatient Populations Camp, Carol A. 039 Safe Flow Rate Nipple Selection for NICU Infants, Post Discharge Use PHASE II IDW106 12:30PM-1:00PM Capps, Natalie 011 Secondhand Smoke and Allelic Variances on Codon 98 as Risk Factors for Cervical Cancer IDW115 2:30PM-3:45PM 001 Systematic Review of the Impact of Glucose Control on Infections Following Cardiac Surgery IDW226 2:30PM-3:45PM 005 The Effects of Shared Medical Appointments on Managing Hypertension in the Veteran Population IDW126 2:30PM-3:45PM 019 Application of Diffusion of Innovation Theory to Increase APRN Adoption of Arkansas’ Prescription Monitoring Program IDW115 9:45AM-11:00AM IDW114 2:30PM-3:45PM IDW114 9:45AM-11:00AM 020 Carithers, Cathrin 026 The Impact of School Based Health Centers on Absenteeism in Rural Middle School Students Adherence to Prostate Cancer Screening Recommendations after a Community/Internet-based Educational Program 030 Increasing Hepatitis C Screening Rates by Screening CDC Recommended Birth Cohorts Prior to Endoscopy IDW114 9:45AM-11:00AM 032 Improving Adherence to ADA/APA Guideline Recommendations for Metabolic Monitoring: An Outpatient Quality Improvement Initiative IDW126 2:30PM-3:45PM 063 It’s a Small World: Providing Culturally Competent Care 2nd floor: 11:00AM-11:30AM Poster Area 1 Childs, Casey 069 Assistive devices and rehabilitation in the older adult with visual impairment: Literature review 2nd floor: 11:00AM-11:30AM Poster Area 1 Cleves, Mario A. 014 The Association of Sleep Disturbance, Depression, and Prodromal Symptoms of Coronary Heart Disease in Women Clinton, Laura 073 The Causes and Challenges Associated with Elderly Homelessness 132 IDW126 9:45AM-11:00AM 2nd floor: 11:00AM-11:30AM Poster Area 1 Name Cockerham, Jennifer Cockmon, Amber Abstract No. Title of Abstract Presentation Place Presentation Time IDW106 11:00AM-11:30AM 022 A Sweet Lesson in Research 056 Fibromyalgia Syndrome and Hydrotherapy Colclasure, M. 061 Effects of E-Ciggarettes in Smoking Cessation Coleman, Shelley 087 Muscle wasting in elderly women 2nd floor: 12:30PM-1:00PM Poster Area 1 Compas, Carol 045 Improving Infection Control Practices in a Long Term Care Facility through a Quality Improvement Project 2nd floor: 11:00AM-11:30AM Poster Area 1 Connors, A. 061 Effects of E-Ciggarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Cuningkin, Veneine P. 003 Relationship between nurse demographics, employee separation and unit assignment in an acute psychiatric hospital. Curry, Trenton 054 Benzodiazepines as an effective first-line treatment for insomnia in older adults 2nd floor: 11:00AM-11:30AM Poster Area 1 Curtis, Jessica 088 Effects of Advanced Directives on Patient Care 2nd floor: 12:30PM-1:00PM Poster Area 1 Davidson, Elizabeth Sloan 046 A Qualitative Pilot Study: Nursing Workplace Environment and Nurses’ Perspectives on Patient Outcomes 2nd floor: 11:00AM-11:30AM Poster Area 1 Davis, Anna 099 Perinatal Mortality Rates Compared in Home and Hospital Births 2nd floor: 12:30PM-1:00PM Poster Area 2 Davis, Dana 072 Elder Mistreatment Assessment 2nd floor: 11:00AM-11:30AM Poster Area 1 Davis, Jackie 039 Davis, Karen 015 Davis, Rodney 026 Decker, Sadie 078 DeGravelles, Pam Safe Flow Rate Nipple Selection for NICU Infants, Post Discharge Use PHASE II Predictors of Substance Use Recidivism in Arkansas Nurses Adherence to Prostate Cancer Screening Recommendations after a Community/Internetbased Educational Program Visitor effects on intracranial pressure of traumatic brain activity of traumatic brain injury patients 069 Assistive devices and rehabilitation in the older adult with visual impairment: Literature review 070 Falls in the Older Adult 071 Caring for the Caregiver 072 Elder Mistreatment Assessment 133 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW105 11:00AM-11:30AM IDW106 12:30PM-1:00PM IDW106 11:00AM-11:30AM IDW114 9:45AM-11:00AM 2nd floor: 12:30PM-1:00PM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 Name Abstract No. Title of Abstract Presentation Place Presentation Time 073 The Causes and Challenges Associated with Elderly Homelessness 2nd floor: 11:00AM-11:30AM Poster Area 1 074 Elderly and the Use of Telemedicine 2nd floor: Poster Area 1 12:30PM-1:00PM 075 Sleep Quality of the Older Adult using the Pittsburg Sleep Quality Index and Epworth 2nd floor: Poster Area 1 12:30PM-1:00PM 076 Fatigue and the Elderly: Expected versus Unexpected 2nd floor: Poster Area 1 12:30PM-1:00PM 077 Prevention of Rehospitalizations in Older Adults 2nd floor: Poster Area 1 12:30PM-1:00PM 079 Exercise in the Elderly 2nd floor: Poster Area 1 12:30PM-1:00PM 080 Using the Beers Criteria for Potentially Inappropriate Medication use in the elderly. 2nd floor: Poster Area 1 12:30PM-1:00PM 081 Controversial Aging Theories 082 Older Adult Suicide Prevention 083 Receipt of Immunizations in the Older Adult 2nd floor: Poster Area 1 12:30PM-1:00PM 084 Importance of Assessing and Managing Delirium Patients 2nd floor: Poster Area 1 12:30PM-1:00PM 085 The Effect of Baby Boomers on the Healthcare System 2nd floor: Poster Area 1 12:30PM-1:00PM 086 Functional Decline in Older Adults: Assessment tools 087 Muscle wasting in elderly women 2nd floor: Poster Area 1 2nd floor: Poster Area 1 088 Effects of Advanced Directives on Patient Care 2nd floor: Poster Area 1 090 Loneliness and the Older Adult-Effective Strategies of Intervention 091 Housing the Elderly 092 Telemedicine and the Older Adult 2nd floor: Poster Area 2 2nd floor: Poster Area 2 2nd floor: Poster Area 2 100 Is the Mini Nutritional Assessment (MNA) Essential for Geriatric Patients as a Preventive Tool? DeGravelles, Pam 134 2nd floor: Poster Area 1 2nd floor: Poster Area 1 2nd floor: Poster Area 2 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM Name Abstract No. Title of Abstract 102 Effective Rehabilitations for Patients with Brain Disorders 103 Restraint Use: The ability to do without Devine, Allison Shaw 006 Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study Donaldson, Terri A. 098 Establishing a Motivational Interviewing (MI) Learning Community Driggers, Laura 082 Older Adult Suicide Prevention DeGravelles, Pam 035 Dumont, Natalie 048 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions Content Validity Methods Applied to New Psychosocial Scale for Social Burden in Rare Genetic Conditions 12:30PM-1:00PM IDW126 9:45AM-11:00AM 2nd floor: Poster Area 2 2nd floor: Poster Area 1 IDW104 Presentation Time 12:30PM-1:00PM 12:30PM-1:00PM 12:30PM-1:00PM 2:30PM-3:45PM 2nd floor: 11:00AM-11:30AM Poster Area 1 Easley, Paul 022 Effrein, Rebecca 037 Enderlin, Carol 056 Fibromyalgia Syndrome and Hydrotherapy 010 Eye Drops and Adverse Events after Eye Examinations for Retinopathy of Prematurity 050 Adverse Events and Retinopathy of Prematurity Eye Exams 2nd floor: 11:00AM-11:30AM Poster Area 1 Ervin, Misty 056 Fibromyalgia Syndrome and Hydrotherapy 2nd floor: 11:00AM-11:30AM Poster Area 1 Estes, Cassidy 001 Systematic Review of the Impact of Glucose Control on Infections Following Cardiac Surgery Evans, Aubrey 058 Strategies to Prevent Medication Errors Erickson, Stephen A Sweet Lesson in Research Decreasing Length of Stay in Veterans undergoing a Primary Total Joint Procedure with the Total Joint Academy Pre-Operative Educational Class Presentation Place 2nd floor: Poster Area 2 2nd floor: Poster Area 2 135 IDW106 11:00AM-11:30AM IDW105 12:30PM-1:00PM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW115 IDW226 2:30PM-3:45PM 2:30PM-3:45PM 2nd floor: 11:00AM-11:30AM Poster Area 1 Name Abstract No. Title of Abstract Presentation Place Presentation Time 057 Factors Related to Early Breastfeeding Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 058 Strategies to Prevent Medication Errors 2nd floor: 11:00AM-11:30AM Poster Area 1 059 How Various Sexual Education Programs Influence Adolescents’ Risky Sexual Behavior 2nd floor: 11:00AM-11:30AM Poster Area 1 095 Effective Interventions to Decrease Childhood Obesity: Parental Role 2nd floor: Poster Area 2 12:30PM-1:00PM 096 Evidence-Based Nursing Interventions for the Prevention of Ventilator-Associated Pneumonia for Patients in the ICU 2nd floor: Poster Area 2 12:30PM-1:00PM 097 Evidence of the Effectiveness of Assessment 2nd floor: tools for Palliative Care in Dementia Poster Area 2 12:30PM-1:00PM 006 Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study IDW126 9:45AM-11:00AM Flavin, Susan 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions IDW104 2:30PM-3:45PM France, Sarah 007 Registered nurse and unlicensed assistive personnel perceptions on barriers to communication and teamwork: A pilot study IDW105 11:00AM-11:30AM Frazier, Lynn 030 Increasing Hepatitis C Screening Rates by Screening CDC Recommended Birth Cohorts Prior to Endoscopy IDW114 9:45AM-11:00AM Funderburk, Amy 063 It’s a Small World: Providing Culturally Competent Care 2nd floor: 11:00AM-11:30AM Poster Area 1 Gamble, Leigh Ashley 095 Effective Interventions to Decrease Childhood Obesity: Parental Role 2nd floor: Poster Area 2 12:30PM-1:00PM Geesing, Courtney 085 The Effect of Baby Boomers on the Healthcare System 2nd floor: Poster Area 1 12:30PM-1:00PM Gill, Laura 097 Evidence of the Effectiveness of Assessment 2nd floor: tools for Palliative Care in Dementia Poster Area 2 12:30PM-1:00PM Goodwin, Rachel 097 Evidence of the Effectiveness of Assessment 2nd floor: tools for Palliative Care in Dementia Poster Area 2 12:30PM-1:00PM Grant, Gianna M. 020 The Impact of School Based Health Centers on Absenteeism in Rural Middle School Students 2:30PM-3:45PM Evans, Laura K Fier, Audrey 136 IDW114 Name Abstract No. Title of Abstract 052 Family Coping after a Child's Traumatic Brain Injury Green, Jerril 042 World Peace and the Standardization of Arterial Lines in a Pediatric Hospital in Arkansas Grubbs, Gary 089 Effects of Education and Attitudes Parents have Regarding Immunizing their Children Grundy, Joyce 022 A Sweet Lesson in Research Gullette, Donna 094 Gulley, Sonya L. Green, Angela Presentation Place Presentation Time 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW106 12:30PM-1:00PM 2nd floor: Poster Area 2 12:30PM-1:00PM IDW106 11:00AM-11:30AM Pay for Performance Policy Effect on Primary Care Hypertension Management 2nd floor: Poster Area 2 12:30PM-1:00PM 100 Is the Mini Nutritional Assessment (MNA) Essential for Geriatric Patients as a Preventive Tool? 2nd floor: Poster Area 2 12:30PM-1:00PM Hadden, Kristie 026 Adherence to Prostate Cancer Screening Recommendations after a Community/Internet-based Educational Program IDW114 9:45AM-11:00AM Haley, Brandy 013 Effects of a 12 Week Maternal CPR Practice Program on Nursing Student Performance Recall IDW106 11:00AM-11:30AM Hall, Channing 056 Fibromyalgia Syndrome and Hydrotherapy Hall, Richard Whit 010 Eye Drops and Adverse Events after Eye Examinations for Retinopathy of Prematurity IDW115 2:30PM-3:45PM 036 Perceived Need for HIV Testing among Rural and Urban African American Cocaine Users IDW104 2:30PM-3:45PM 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Communities In the Rural Arkansas Delta 2nd floor: Poster Area 2 12:30PM-1:00PM Haynes, Tiffany 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Based Communities In the Rural Arkansas Delta 2nd floor: Poster Area 2 12:30PM-1:00PM Hays, Laura 044 Perceived Health Status and Self-Efficacy of Adult Survivors of Pediatric Orthotopic Heart Transplant: Pilot Study 2nd floor: 11:00AM-11:30AM Poster Area 1 Heaggans, Danelle 056 Fibromyalgia Syndrome and Hydrotherapy 2nd floor: 11:00AM-11:30AM Poster Area 1 Henderson, Tamisha 068 Bloodstream Infection Reduction: Utilizing Alcohol-Impregnated Caps in Patients with Central-Lines 2nd floor: 11:00AM-11:30AM Poster Area 1 Han, Xiaotong Harris, Kimberly 137 2nd floor: 11:00AM-11:30AM Poster Area 1 Name Henderson, Tamisha Hendrickson, Howard Hensley, Adam Abstract No. Title of Abstract Presentation Place Presentation Time 093 Identifying Intensive Care Unit Patients at Risk for Chronic Post-traumatic Stress Disorder 2nd floor: Poster Area 2 12:30PM-1:00PM 010 Eye Drops and Adverse Events after Eye Examinations for Retinopathy of Prematurity IDW115 2:30PM-3:45PM 050 Adverse Events and Retinopathy of Prematurity Eye Exams 2nd floor: 11:00AM-11:30AM Poster Area 1 070 Falls in the Older Adult 2nd floor: 11:00AM-11:30AM Poster Area 1 006 Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study 060 Effects of Chlorhexidine Gluconate Bathing 2nd floor: on MRSA Colonization and Infection Rates 11:00AM-11:30AM Poster Area 1 in Inpatient Populations 062 Effects of Interventions on Depression in Caregivers Who Take Care of Alzheimer’s or Dementia Patients Heo, Seongkum IDW126 9:45AM-11:00AM 2nd floor: 11:00AM-11:30AM Poster Area 1 Hester, Amy 051 Hill, Edward Lee 018 Development of a Fall Injury Prediction on Model Tracing Zeroes for Our Heroes Hill, William 074 Elderly and the Use of Telemedicine Hines, B. 061 Hines, Briana 093 Hintson, Shelby 078 Hoey, Shannon 067 Howell, Amy 056 Fibromyalgia Syndrome and Hydrotherapy 2nd floor: 11:00AM-11:30AM Poster Area 1 Huett, Amy 052 Family Coping after a Child's Traumatic Brain Injury 2nd floor: 11:00AM-11:30AM Poster Area 1 Huff, Jennifer 023 Reducing Heart Failure Readmissions Jackson, Jameka 056 Fibromyalgia Syndrome and Hydrotherapy Effects of E-Ciggarettes in Smoking Cessation Identifying Intensive Care Unit Patients at Risk for Chronic Post-traumatic Stress Disorder Visitor effects on intracranial pressure of traumatic brain activity of traumatic brain injury patients The Use of Dexmedetomidine in PostOperative Heart Surgery Patients for Decreasing Length of Stay and PostOperative Complications 138 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW106 11:00AM-11:30AM 2nd floor: 12:30PM-1:00PM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: Poster Area 2 12:30PM-1:00PM 2nd floor: Poster Area 1 12:30PM-1:00PM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW105 12:30PM-1:00PM 2nd floor: 11:00AM-11:30AM Poster Area 1 Abstract No. Title of Abstract Presentation Place Presentation Time 024 One Stick Too Many: Reducing PIV Sticks and Infiltrates in Pediatric Patients IDW105 12:30PM-1:00PM Jarvis, Elizabeth 019 Application of Diffusion of Innovation Theory to Increase APRN Adoption of Arkansas’ Prescription Monitoring Program IDW115 9:45AM-11:00AM Jensen, Ashley D. 009 Perspectives About Cyclic Vomiting Syndrome: Adult Explanatory Models IDW105 11:00AM-11:30AM Johnson, Cajun 057 Factors Related to Early Breastfeeding Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Johnson, Valerie 096 Evidence-Based Nursing Interventions for the Prevention of Ventilator-Associated Pneumonia for Patients in the ICU 2nd floor: Poster Area 2 Jones, James 065 Washington County Arkansas’ progress toward accomplishing Healthy People 2020 objective MHMD-8 2nd floor: 11:00AM-11:30AM Poster Area 1 Jones, Katlin 066 The Effect of Oral Care on the Incidence of 2nd floor: 11:00AM-11:30AM Ventilator-Associated Pneumonia Poster Area 1 053 Psychological Differences in Adolescents Who Sexually Offend with a History of Childhood Sexual Abuse 2nd floor: 11:00AM-11:30AM Poster Area 1 065 Washington County Arkansas’ progress toward accomplishing Healthy People 2020 objective MHMD-8 2nd floor: 11:00AM-11:30AM Poster Area 1 Jordan, Connie 043 Utilization of an interdisciplinary (ID) team to expand programming within an inpatient dual diagnosis program- quality improvement project. Kennedy, Robert 015 Kindells, Paesha 095 Kippenbrock, Thomas 002 Kitch, Stephanie Name Janisko, Jennifer Jones, Sara 12:30PM-1:00PM IDW106 12:30PM-1:00PM IDW106 11:00AM-11:30AM 2nd floor: Poster Area 2 12:30PM-1:00PM A Decade of Change: Nurse Practitioners in the Southern United States IDW226 2:30PM-3:45PM 094 Pay for Performance Policy Effect on Primary Care Hypertension Management 2nd floor: Poster Area 2 12:30PM-1:00PM Kuo, Dennis K. 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Communities In the Rural Arkansas Delta 2nd floor: Poster Area 2 12:30PM-1:00PM LaBorde, Samantha 077 Prevention of Rehospitalizations in Older Adults 2nd floor: Poster Area 1 12:30PM-1:00PM Predictors of Substance Use Recidivism in Arkansas Nurses Effective Interventions to Decrease Childhood Obesity: Parental Role 139 Name Abstract No. 054 Landrum, Barbara 055 078 Title of Abstract Presentation Place Presentation Time Benzodiazepines as an effective first-line treatment for insomnia in older adults 2nd floor: 11:00AM-11:30AM Poster Area 1 How Nurse’s Instructions Affect Patient Understand of NPO Visitor effects on intracranial pressure of traumatic brain activity of traumatic brain injury patients 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: Poster Area 1 12:30PM-1:00PM 12:30PM-1:00PM Langley, Tess 099 Perinatal Mortality Rates Compared in Home and Hospital Births 2nd floor: Poster Area 2 Lawson, Allisa 058 Strategies to Prevent Medication Errors 2nd floor: 11:00AM-11:30AM Poster Area 1 Lee, Jeannette Y. 006 Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study Leming-Lee, Treasa 098 Lewis, D. IDW126 9:45AM-11:00AM Establishing a Motivational Interviewing (MI) Learning Community 2nd floor: Poster Area 2 12:30PM-1:00PM 068 Bloodstream Infection Reduction: Utilizing Alcohol-Impregnated Caps in Patients with Central-Lines 2nd floor: 11:00AM-11:30AM Poster Area 1 Lewis, Telischa 005 The Effects of Shared Medical Appointments on Managing Hypertension in the Veteran Population Lingo, Joshuah 045 Improving Infection Control Practices in a Long Term Care Facility through a Quality Improvement Project Littlefield, Vivian 016 Nurses Educating to Help Save Lives: A Red Cross Program to Increase Blood Donations Litton, Brandy 092 Telemedicine and the Older Adult Lo, Wne-Juo 002 Lovelady, Nakita IDW126 2:30PM-3:45PM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW114 2:30PM-3:45PM 2nd floor: Poster Area 2 12:30PM-1:00PM A Decade of Change: Nurse Practitioners in the Southern United States IDW226 2:30PM-3:45PM 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Communities In the Rural Arkansas Delta 2nd floor: Poster Area 2 12:30PM-1:00PM 089 Effects of Education and Attitudes Parents have Regarding Immunizing their Children 2nd floor: Poster Area 2 12:30PM-1:00PM 099 Perinatal Mortality Rates Compared in Home and Hospital Births 2nd floor: Poster Area 2 12:30PM-1:00PM Loy, Patricia 140 Abstract No. Title of Abstract Presentation Place Presentation Time 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Communities In the Rural Arkansas Delta 2nd floor: Poster Area 2 12:30PM-1:00PM 056 Fibromyalgia Syndrome and Hydrotherapy 2nd floor: 11:00AM-11:30AM Poster Area 1 066 The Effect of Oral Care on the Incidence of 2nd floor: 11:00AM-11:30AM Ventilator-Associated Pneumonia Poster Area 1 Lyle, Rebecca 038 Diversional Activities to Decrease Harmful Behavior in Patients with Dementia Lynch, Brynna 056 Fibromyalgia Syndrome and Hydrotherapy 018 Tracing Zeroes for Our Heroes IDW106 11:00AM-11:30AM 022 A Sweet Lesson in Research IDW106 11:00AM-11:30AM Martin, Antonia 090 Loneliness and the Older Adult-Effective Strategies of Intervention 2nd floor: Poster Area 2 12:30PM-1:00PM Mayhue, C. 061 Effects of E-Cigarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 McAlister, Sarah 060 Effects of Chlorhexidine Gluconate Bathing 2nd floor: on MRSA Colonization and Infection Rates 11:00AM-11:30AM Poster Area 1 in Inpatient Populations McDowell, Karen 068 Bloodstream Infection Reduction: Utilizing Alcohol-Impregnated Caps in Patients with Central-Lines McMillian, Terry 024 One Stick Too Many: Reducing PIV Sticks and Infiltrates in Pediatric Patients McNabb, Rachel 055 How Nurse’s Instructions Affect Patient Understand of NPO 2nd floor: 11:00AM-11:30AM Poster Area 1 McNeely, L. 061 Effects of E-Ciggarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Name Loyd, Caroline MacLaird, Perry D. Mallard, Ellen 141 IDW105 12:30PM-1:00PM 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW105 12:30PM-1:00PM Abstract No. Title of Abstract Presentation Place Presentation Time 006 Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study IDW126 9:45AM-11:00AM 014 The Association of Sleep Disturbance, Depression, and Prodromal Symptoms of Coronary Heart Disease in Women IDW126 9:45AM-11:00AM 094 Pay for Performance Policy Effect on Primary Care Hypertension Management 2nd floor: Poster Area 2 12:30PM-1:00PM 044 Perceived Health Status and Self-Efficacy of Adult Survivors of Pediatric Orthotropic Heart Transplant: Pilot Study 2nd floor: 11:00AM-11:30AM Poster Area 1 017 Symptom Onset to Arterial Reperfusion (SOAR) Research Study IDW106 11:00AM-11:30AM 010 Eye Drops and Adverse Events after Eye Examinations for Retinopathy of Prematurity IDW115 2:30PM-3:45PM 050 Adverse Events and Retinopathy of Prematurity Eye Exams 2nd floor: 11:00AM-11:30AM Poster Area 1 Moore, Rebecca 080 Using the Beers Criteria for Potentially Inappropriate Medication use in the elderly 2nd floor: Poster Area 1 Morgan, Searcy 057 Factors Related to Early Breastfeeding Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Morris, Leanna 059 How Various Sexual Education Programs Influence Adolescents’ Risky Sexual Behavior 2nd floor: 11:00AM-11:30AM Poster Area 1 Morrisey, Carolyn 025 Incorporating the Electronic Medical Record into Nursing Curriculum Morrow, Morgan 056 Fibromyalgia Syndrome and Hydrotherapy 006 Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study Name McSweeney, Jean Meiklejohn, Deborah Mitchell, Anita Moser, Debra K. 142 IDW226 12:30PM-1:00PM 9:45AM-11:00AM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW126 9:45AM-11:00AM Name Abstract No. Presentation Place Presentation Time Moss, Jacqueline 025 Incorporating the Electronic Medical Record into Nursing Curriculum IDW226 9:45AM-11:00AM Nelson, Mary Kathryn 022 A Sweet Lesson in Research IDW106 11:00AM-11:30AM Nix, Lauren 057 Factors Related to Early Breastfeeding Cessation Odell, Ellen 002 A Decade of Change: Nurse Practitioners in the Southern United States Odom, Brandon 059 How Various Sexual Education Programs Influence Adolescents’ Risky Sexual Behavior Oglesby-Brown, Keisha 022 A Sweet Lesson in Research Onecic, Mara 061 Effects of E-Ciggarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 050 Adverse Events and Retinopathy of Prematurity Eye Exams 2nd floor: 11:00AM-11:30AM Poster Area 1 056 Fibromyalgia Syndrome and Hydrotherapy 2nd floor: 11:00AM-11:30AM Poster Area 1 093 Identifying Intensive Care Unit Patients at Risk for Chronic Post-traumatic Stress Disorder 2nd floor: Poster Area 2 12:30PM-1:00PM Ounpraseuth, Songthip T. 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Communities In the Rural Arkansas Delta 2nd floor: Poster Area 2 12:30PM-1:00PM Owens, C. 061 Effects of E-Cigarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Pate, Barbara 026 Adherence to Prostate Cancer Screening Recommendations after a Community/Internet-based Educational Program IDW114 9:45AM-11:00AM Patton, Christina 096 Evidence-Based Nursing Interventions for the Prevention of Ventilator-Associated Pneumonia for Patients in the ICU 2nd floor: Poster Area 2 12:30PM-1:00PM 004 Preventing Central-Line Associated Bloodstream Infections in the NICU: Are We Up to Date? IDW105 11:00AM-11:30AM Orahood, Jennifer Pennington, Tina Title of Abstract 143 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW226 2:30PM-3:45PM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW106 11:00AM-11:30AM Name Abstract No. Title of Abstract Presentation Place Presentation Time 061 Effects of E-Cigarettes in Smoking Cessation 066 The Effect of Oral Care on the Incidence of 2nd floor: 11:00AM-11:30AM Ventilator-Associated Pneumonia Poster Area 1 001 Systematic Review of the Impact of Glucose Control on Infections Following Cardiac Surgery IDW226 2:30PM-3:45PM 014 The Association of Sleep Disturbance, Depression, and Prodromal Symptoms of Coronary Heart Disease in Women IDW126 9:45AM-11:00AM Phillips, Linise 093 Identifying Intensive Care Unit Patients at Risk for Chronic Post-traumatic Stress Disorder 2nd floor: Poster Area 2 12:30PM-1:00PM Plummer, Carrie E. 098 Establishing a Motivational Interviewing (MI) Learning Community 2nd floor: Poster Area 2 12:30PM-1:00PM Poirrier, Teri 059 How Various Sexual Education Programs Influence Adolescents’ Risky Sexual Behavior 2nd floor: 11:00AM-11:30AM Poster Area 1 Poole, L. 061 Effects of E-Cigarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Powers, Cynthia 015 Predictors of Substance Use Recidivism in Arkansas Nurses IDW106 11:00AM-11:30AM Powers, Rachael 038 Diversional Activities to Decrease Harmful Behavior in Patients with Dementia IDW105 12:30PM-1:00PM Prakriti, K. C. 076 Fatigue and the Elderly: Expected versus Unexpected 2nd floor: Poster Area 1 12:30PM-1:00PM Prewitt, Elaine T. 006 Feasibility and Acceptability of a Tailored Dietary Sodium Intervention Combined with Technology and Psychosocial Support in Patients with Heart Failure: A pilot study IDW126 9:45AM-11:00AM Price, Ashley 081 Controversial Aging Theories 2nd floor: Poster Area 1 12:30PM-1:00PM Pritchett, Karen 022 A Sweet Lesson in Research IDW106 11:00AM-11:30AM Proffitt, Beth 022 A Sweet Lesson in Research IDW106 11:00AM-11:30AM 026 Adherence to Prostate Cancer Screening Recommendations after a Community/Internet-based Educational Program IDW114 9:45AM-11:00AM Peters, Jon Pettey, Christina Purifoy, Jody A. 144 2nd floor: 11:00AM-11:30AM Poster Area 1 Abstract No. Title of Abstract 056 Fibromyalgia Syndrome and Hydrotherapy Quill, Jim 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions Rabb, Richard 097 Randolph, Destiny Name Qualls, Krystal Presentation Place Presentation Time 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW104 2:30PM-3:45PM Evidence of the Effectiveness of Assessment tools for Palliative Care in Dementia 2nd floor: Poster Area 2 12:30PM-1:00PM 097 Evidence of the Effectiveness of Assessment tools for Palliative Care in Dementia 2nd floor: Poster Area 2 12:30PM-1:00PM 075 Sleep Quality of the Older Adult using the Pittsburg Sleep Quality Index and Epworth 2nd floor: Poster Area 1 12:30PM-1:00PM Rao, Aravind N. 017 Symptom Onset to Arterial Reperfusion (SOAR) Research Study IDW106 11:00AM-11:30AM Reed, Pam 024 One Stick Too Many: Reducing PIV Sticks and Infiltrates in Pediatric Patients IDW105 12:30PM-1:00PM Reynolds, Michele 032 Improving Adherence to ADA/APA Guideline Recommendations for Metabolic Monitoring: An Outpatient Quality Improvement Initiative IDW126 2:30PM-3:45PM Richardson, Leah 047 Identifying Gaps between Resources and Parents with Children Diagnosed with Autism-A Pilot Study 2nd floor: 11:00AM-11:30AM Poster Area 1 Robinson, Sundra 054 Benzodiazepines as an effective first-line treatment for insomnia in older adults 2nd floor: 11:00AM-11:30AM Poster Area 1 056 Fibromyalgia Syndrome and Hydrotherapy 2nd floor: 11:00AM-11:30AM Poster Area 1 066 The Effect of Oral Care on the Incidence of 2nd floor: 11:00AM-11:30AM Ventilator-Associated Pneumonia Poster Area 1 Rogers, Olivia 099 Perinatal Mortality Rates Compared in Home and Hospital Births 2nd floor: Poster Area 2 12:30PM-1:00PM Romero, Marcos 096 Evidence-Based Nursing Interventions for the Prevention of Ventilator-Associated Pneumonia for Patients in the ICU 2nd floor: Poster Area 2 12:30PM-1:00PM Raney, Kari Rogers, Mauri 145 Name Abstract No. Title of Abstract Presentation Place Presentation Time 102 Effective Rehabilitations for Patients with Brain Disorders 2nd floor: Poster Area 2 12:30PM-1:00PM 039 Safe Flow Rate Nipple Selection for NICU Infants, Post Discharge Use PHASE II IDW106 12:30PM-1:00PM 041 Evaluation of Implementation of an Influenza Cocooning Practice in the NICU for Infant Household Caregivers IDW106 12:30PM-1:00PM Saulsbury, Morgan 086 Functional Decline in Older Adults: Assessment tools 2nd floor: Poster Area 1 12:30PM-1:00PM Schmid, Barbara 022 A Sweet Lesson in Research IDW106 11:00AM-11:30AM Schmidt, Cheryl K. 016 Nurses Educating to Help Save Lives: A Red Cross Program to Increase Blood Donations IDW114 2:30PM-3:45PM 061 Effects of E-Ciggarettes in Smoking Cessation Scott, Angela 024 One Stick Too Many: Reducing PIV Sticks and Infiltrates in Pediatric Patients IDW105 12:30PM-1:00PM Shelby, Race 040 Early Prone Positioning: Why Wait for ARDS? IDW106 12:30PM-1:00PM Shellabarger, C. 068 Bloodstream Infection Reduction: Utilizing Alcohol-Impregnated Caps in Patients with Central-Lines Shelton, Kristina 028 Don’t Leave It To Chance… give breast milk a second glance! IDW105 12:30PM-1:00PM Shore, Lucinda 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions IDW104 2:30PM-3:45PM Sinclair, Morgan 091 Housing the Elderly 2nd floor: Poster Area 2 12:30PM-1:00PM 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions IDW104 2:30PM-3:45PM Sanders, Shelby Sartini, Rebecca P. Sineath, Marvin 146 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: 11:00AM-11:30AM Poster Area 1 Abstract No. Title of Abstract Presentation Place Presentation Time 007 Registered nurse and unlicensed assistive personnel perceptions on barriers to communication and teamwork: A pilot study IDW105 11:00AM-11:30AM Smith, Johnny 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African 2nd floor: American Faith Based Based Communities Poster Area 2 In the Rural Arkansas Delta 12:30PM-1:00PM Smith, Rebecca K. 041 Evaluation of Implementation of an Influenza Cocooning Practice in the NICU for Infant Household Caregivers IDW106 12:30PM-1:00PM Sorrells, Clayton 099 Perinatal Mortality Rates Compared in Home and Hospital Births 2nd floor: Poster Area 2 12:30PM-1:00PM Stark, C. 061 Effects of E-Ciggarettes in Smoking Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Stark, Caleb 093 Identifying Intensive Care Unit Patients at Risk for Chronic Post-traumatic Stress Disorder 2nd floor: Poster Area 2 12:30PM-1:00PM Steelman, Susan 001 Systematic Review of the Impact of Glucose Control on Infections Following Cardiac Surgery IDW226 2:30PM-3:45PM Stewart, Kathryn 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African 2nd floor: American Faith Based Based Communities Poster Area 2 In the Rural Arkansas Delta 12:30PM-1:00PM Stone, Megan 089 Effects of Education and Attitudes Parents have Regarding Immunizing their Children 2nd floor: Poster Area 2 12:30PM-1:00PM Strange, Charlie 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions IDW104 2:30PM-3:45PM Stroman, Sheila 012 Aromathearpy for Stress Reduction: A Strategy for Self-Care IDW105 11:00AM-11:30AM Sullivan, Sheila Cox 021 Delirium in Acutely Ill Elders: The Role of Nurses IDW106 11:00AM-11:30AM Summitt, Alice 028 Don't Leave It To Chance… give breast milk a second glance! IDW105 12:30PM-1:00PM Name Sisoukrath, Kaylee 147 Abstract No. Title of Abstract Presentation Place Presentation Time Syler, Kenda 089 Effects of Education and Attitudes Parents have Regarding Immunizing their Children 2nd floor: Poster Area 2 12:30PM-1:00PM Tadlock, Hannah 058 Strategies to Prevent Medication Errors 2nd floor: 11:00AM-11:30AM Poster Area 1 Taggart, Taneya 055 How Nurse’s Instructions Affect Patient Understand of NPO 2nd floor: 11:00AM-11:30AM Poster Area 1 066 The Effect of Oral Care on the Incidence of 2nd floor: 11:00AM-11:30AM Ventilator-Associated Pneumonia Poster Area 1 033 Inclusion of APRNs as Part of an Interprofessional Rapid Response Team: A Business Case Analysis Tanner, Shaynna 095 Tate, Linda Name Tanner, Mark IDW115 9:45AM-11:00AM Effective Interventions to Decrease Childhood Obesity: Parental Role 2nd floor: Poster Area 2 12:30PM-1:00PM 049 Older Adults Who Exercise Display Lower Temporal Discounting Rates Than NonExercisers 2nd floor: 11:00AM-11:30AM Poster Area 1 Taylor, Shannon 057 Factors Related to Early Breastfeeding Cessation 2nd floor: 11:00AM-11:30AM Poster Area 1 Taylor, Tanya 021 Delirium in Acutely Ill Elders: The Role of Nurses Terry, Lauren 083 Receipt of Immunizations in the Older Adult Thomason, Ayasha 011 Thornton-Orr, Denise Tsai, Pao-feng Tunstall, Sharon IDW106 11:00AM-11:30AM 2nd floor: Poster Area 1 12:30PM-1:00PM Secondhand Smoke and Allelic Variances on Codon 98 as Risk Factors for Cervical Cancer IDW115 2:30PM-3:45PM 003 Relationship between nurse demographics, employee separation and unit assignment in an acute psychiatric hospital. IDW105 11:00AM-11:30AM 049 Older Adults Who Exercise Display Lower Temporal Discounting Rates Than NonExercisers 2nd floor: 11:00AM-11:30AM Poster Area 1 051 Development of A Fall Injury Prediction Model 2nd floor: 11:00AM-11:30AM Poster Area 1 024 One Stick Too Many: Reducing PIV Sticks and Infiltrates in Pediatric Patients 148 IDW105 12:30PM-1:00PM Name Abstract No. Title of Abstract Presentation Place Presentation Time Turner, Jerome 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African 2nd floor: American Faith Based Based Communities Poster Area 2 In the Rural Arkansas Delta Urban, Kelly 029 Fall Prevention: A Concept Analysis Vann, Abigail 071 Caring for the Caregiver Vickers, Victoria 078 Villeda, Andres 096 Vuk, Jasna 015 Predictors of Substance Use Recidivism in Arkansas Nurses Wagner, Austin 054 Benzodiazepines as an effective first-line treatment for insomnia in older adults 2nd floor: 11:00AM-11:30AM Poster Area 1 Walker, Angela 103 Restraint Use: The ability to do without 2nd floor: Poster Area 2 12:30PM-1:00PM Walker, Deirdre 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions IDW104 2:30PM-3:45PM Walker, Liz 022 A Sweet Lesson in Research IDW106 11:00AM-11:30AM Wallace, Shea 059 How Various Sexual Education Programs Influence Adolescents’ Risky Sexual Behavior Ward, Nicole 034 E-cigarettes and pregnancy IDW104 9:45AM-11:00AM Warner, Barbara 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions IDW104 2:30PM-3:45PM Webb, Tammy 008 Preventing Needle Stick Injuries with new generation safety device technology: Can your device be safer? IDW105 11:00AM-11:30AM Visitor effects on intracranial pressure of traumatic brain activity of traumatic brain injury patients Evidence-Based Nursing Interventions for the Prevention of Ventilator-Associated Pneumonia for Patients in the ICU 149 IDW105 12:30PM-1:00PM 12:30PM-1:00PM 2nd floor: 11:00AM-11:30AM Poster Area 1 2nd floor: Poster Area 1 12:30PM-1:00PM 2nd floor: Poster Area 2 12:30PM-1:00PM IDW106 11:00AM-11:30AM 2nd floor: 11:00AM-11:30AM Poster Area 1 Name Abstract No. Title of Abstract Presentation Place Presentation Time White, Whitney 093 Identifying Intensive Care Unit Patients at Risk for Chronic Post-traumatic Stress Disorder 2nd floor: Poster Area 2 12:30PM-1:00PM Whitmore, Roselyn 038 Diversional Activities to Decrease Harmful Behavior in Patients with Dementia IDW105 12:30PM-1:00PM Wienke, Sara 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions IDW104 2:30PM-3:45PM Wilhelm, Sharon V. 041 Evaluation of Implementation of an Influenza Cocooning Practice in the NICU for Infant Household Caregivers IDW106 12:30PM-1:00PM Willard, Mary J. 064 Electronic Cigarettes- Awareness, Perception, and Education 035 Alpha-1 Antitrypsin Deficiency Community Members Describe Social Burdens: Informing Clinical Practices, Conceptual Framework & Psychometric Development in Rare Genetic Conditions 048 Content Validity Methods Applied to New Psychosocial Scale for Social Burden in Rare Genetic Conditions 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African 2nd floor: American Faith Based Based Communities Poster Area 2 In the Rural Arkansas Delta Wilson, Katrena 067 The Use of Dexmedetomidine in PostOperative Heart Surgery Patients for Decreasing Length of Stay and PostOperative Complications 2nd floor: 11:00AM-11:30AM Poster Area 1 Worsham, Alexis 055 How Nurse’s Instructions Affect Patient Understand of NPO 2nd floor: 11:00AM-11:30AM Poster Area 1 036 Perceived Need for HIV Testing among Rural and Urban African American Cocaine Users 046 A Qualitative Pilot Study: Nursing Workplace Environment and Nurses’ Perspectives on Patient Outcomes 2nd floor: 11:00AM-11:30AM Poster Area 1 047 Identifying Gaps between Resources and Parents with Children Diagnosed with Autism-A Pilot Study 2nd floor: 11:00AM-11:30AM Poster Area 1 Williams, Pamela Holtzclaw Williams, Stephanie Wright, Trish 150 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW104 2:30PM-3:45PM 2nd floor: 11:00AM-11:30AM Poster Area 1 IDW104 12:30PM-1:00PM 2:30PM-3:45PM Name Abstract No. Title of Abstract Presentation Place Presentation Time Yancy, L. 061 Effects of E-Cigarettes in Smoking Cessation Yates, Charlotte 010 Eye Drops and Adverse Events after Eye Examinations for Retinopathy of Prematurity IDW115 2:30PM-3:45PM 104 Cultural Adaptation of an Evidence-Based Depression Intervention for the African American Faith Based Communities In the Rural Arkansas Delta 2nd floor: Poster Area 2 12:30PM-1:00PM Yeary, Hye-cheon Kim 151 2nd floor: 11:00AM-11:30AM Poster Area 1
© Copyright 2026