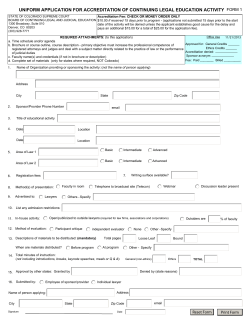
Corrected Claims / Reconsideration Request Form
Corrected Claims / Reconsideration Request Form Requests must be received within 180 days from the date of service (or per the terms of your contract). Please allow 30 days to process this reconsideration request. Please return this completed form and any supporting documentation to INTotal Health Plan. Please use a separate request form for each claim reconsideration request sent to: INTotal Health Attn: Provider Claims P.O. Box 5448 Richmond, VA 23220 – 0448 *Please note, this form should not be used for New Claims or Payment Appeals. Member Demographic Information Member ID: Member Last Name: Date Form Completed: ___/_____/____ Control/Original Claim#: Date of Service: Billed Amount: _____ /____/_____ $___________ First Name: MI: Paid Amount: $__________ Physician /Health Care Professional Information Provider’s Name: Contact Name: Tax ID Number: Mailing Address: Contact Ph#: NPI Number: If this is a Corrected Claim please choose from the following: ☐ Corrected Diagnosis ☐ Corrected Procedure Code (CPT/HCPCS) ☐ Corrected Date of Service ☐ Corrected Charges ☐ Corrected Place of Service ☐ Addition or Correction of Modifier ☐ Corrected Provider Information ☐ Other (Please Specify Below) If this is a Reconsideration please choose from the following: ☐ Previously denied / Timely Filing ☐ Previously denied/ duplicate ☐ Previously denied / Additional Information ☐ Previously denied / Not covered ☐ Resubmission: Underpayment ☐ Resubmission: Overpayment ☐Previously denied/ No Authorization ☐ Other (Please Specify Below) Additional Comments: Supporting Documentation Attached? ☐ YES ☐ NO
© Copyright 2026