Consolidated CDA Creation Performance
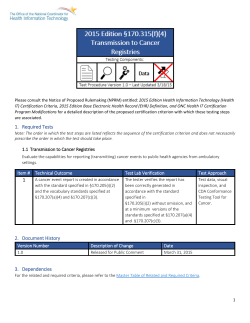
Please consult the Notice of Proposed Rulemaking (NPRM) entitled: 2015 Edition Health Information Technology (Health IT) Certification Criteria, 2015 Edition Base Electronic Health Record (EHR) Definition, and ONC Health IT Certification Program Modifications for a detailed description of the proposed certification criterion with which these testing steps are associated. 1. Description This certification criterion rigorously assesses a product’s ability to create Consolidated CDA (C-CDA) Documents for both the 2014 and 2015 NPRM Editions. This certification criterion is not stand-alone, and must be used in-conjunction with a criterion which expresses the capability of creating C-CDA documents (e.g. Transitions of care, Data Portability); however, if multiple C-CDA creation certifications are sought, this certification criterion only needs to be tested once. Additionally, the capabilities described can be demonstrated in tandem and do not need to be individually addressed in isolation or sequentially. Upon positive completion of the certification, the C-CDA files created under test must be retained and contributed to the ONC-maintained repository. 2. Required Tests Note: The order in which the test steps are listed reflects the sequence of the certification criterion and does not necessarily prescribe the order in which the test should take place. 2.1 Reference C-CDA Match Evaluate the capability of the Health IT Module to create both C-CDA Release 1.1 in accordance with the HL7 Implementation Guide for CDA® Release 1.1: Consolidated CDA Templates for Clinical Notes (US Realm), Draft Standard for Trial Use, Release 1.1 (C-CDA (Draft Standard for Trial Use, Release 1.1)), including the Common Clinical Data Set (CCDS) requirements AND C-CDA Release 2.0 documents in accordance with the HL7 Implementation Guide for CDA® Release 2: Consolidated CDA Templates for Clinical Notes (US Realm), Draft Standard for Trial Use, Release 2.0 (C-CDA (Draft Standard for Trial Use, Release 2.0)) including Common Clinical Data Set (CCDS) requirements, which match the ONC gold standard Reference C-CDA. 1 Item # Technical Outcome A C-CDA Release 1.1 document in 1a accordance with § 170.205(a)(3), which includes all of the Common Clinical Data Set (CCDS) data elements is created by a user. 1b A C-CDA Release 2.0 document in accordance with § 170.205(a)(4), which includes all of the CCDS data elements is created by a user. Test Lab Verification Test Approach The tester verifies that the created C-CDA document matches the gold standard Reference C-CDA which conforms to C-CDA (Draft Standard for Trial Use, Release 1.1) and includes the CCDS data element requirements. At a minimum, the Health IT Module must consume test data, create a C-CDA, and pass the CCDA through a test tool. The tester verifies that the created C-CDA document matches the gold standard Reference C-CDA which conforms to C-CDA (Draft Standard for Trial Use, Release 2.0) and includes the CCDS data element requirements. At a minimum, the Health IT Module must consume test data, create a C-CDA, and pass the CCDA through a test tool. 2.2 Document Template, Vocabulary, and Value Set Conformance Evaluate the capability of the Health IT Module to create both C-CDA Release 1.1 and Release 2.0 documents which conform to specified Templates, vocabularies, and value sets in the HL7 Implementation Guide for CDA® Release 1.1: Consolidated CDA Templates for Clinical Notes (US Realm), Draft Standard for Trial Use, Release 1.1 (C-CDA (Draft Standard for Trial Use, Release 1.1)) and HL7 Implementation Guide for CDA® Release 2: Consolidated CDA Templates for Clinical Notes (US Realm), Draft Standard for Trial Use, Release 2.0 (C-CDA (Draft Standard for Trial Use, Release 2.0)) respectively. Item # Technical Outcome The following C-CDA Release 1.1 1 documents are created: • Continuity of Care Document (CCD) • Consultation Note • History and Physical • Progress Note • Transfer Summary • Discharge Summary (for inpatient setting only) For CCDS data elements, the Health IT Module creates documents that comply with required vocabulary standards (and value sets). Test Lab Verification Test Approach The tester verifies that the C-CDA Release 1.1 documents can be created, and that each document type conforms to the C-CDA (Draft Standard for Trial Use, Release 1.1) standard templates which have been further constrained by the CCDS. Additionally the tester verifies the Vocabularies and values sets used in the xml file have been properly implemented for CCDS data elements. C-CDA Tool (document type conformance) and test data (health information). Visual inspection where necessary. 2 Item # Technical Outcome The following C-CDA Release 2.0 2 documents are created: • Continuity of Care Document (CCD) • Consultation Note • History and Physical • Progress Note • Care Plan • Transfer Summary • Referral Note • Discharge Summary (for inpatient setting only). For CCDS data elements, the Health IT Module creates documents that comply with required vocabulary standards (and value sets). Test Lab Verification Test Approach Tester verifies that the C-CDA Release 2.0 documents can be created, and that each document type conforms to the C-CDA (Draft Standard for Trial Use, Release 2.0) standard templates which have been further constrained by the CCDS. Additionally the tester verifies the Vocabularies and values sets used in the xml file have been properly implemented for CCDS data elements. C-CDA Tool (document type conformance) and test data (health information). Visual inspection where necessary. 3. Document History Version Number Description of Change Date 1.0 Released for Public Comment March 31, 2015 4. Dependencies For the related and required criteria, please refer to the Master Table of Related and Required Criteria. 3
© Copyright 2026