How to begin treatment in chronic heart failure? * Ronnie Willenheimer
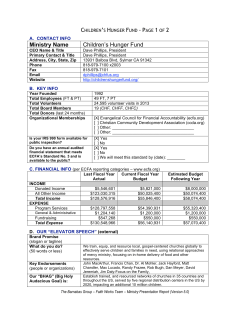
European Heart Journal Supplements (2006) 8 (Supplement C), C43–C50 doi:10.1093/eurheartj/sul013 How to begin treatment in chronic heart failure? Results of CIBIS III Ronnie Willenheimer* KEYWORDS Congestive heart failure; Therapy; Beta-blocker; Angiotensin-converting enzyme inhibitor; Sequence of drug initiation Aims To compare the effect of initial monotherapy with either bisoprolol or enalapril, followed by their combination, on mortality and hospitalization in patients with mild-to-moderate CHF. Methods and results One thousand and ten patients with mild-to-moderate CHF and left ventricular ejection fraction 35%, without ACE-inhibitor, beta-blocker, or angiotensin-receptor-blocker therapy were randomized to open-label monotherapy with either bisoprolol (target dose 10 mg od, n ¼ 505) or enalapril (target dose 10 mg bid, n ¼ 505) for 6 months, followed by their combination for 6–24 months. The combined primary endpoint was all-cause mortality or hospitalization; bisoprolol-first was considered non-inferior to enalapril-first if the upper limit of the 95% CI for the absolute between-group difference was below þ5%, corresponding to HR 1.17. In the intention-to-treat population, the primary endpoint occurred in 178 patients allocated bisoprolol-first vs. 186 allocated enalapril-first: absolute difference, 21.6%; 95% CI, 27.6 to þ4.4%; HR, 0.94; 95% CI, 0.77–1.16. Thus, non-inferiority was demonstrated in the intention-to-treat population. In the per-protocol population, the primary endpoint occurred in 163 patients in the bisoprolol-first group vs. 165 in the enalapril-first group: absolute difference, 20.7%; 95% CI, 26.6 to þ5.1%; HR, 0.97; 95% CI, 0.78–1.21. With bisoprolol-first, 65 patients died vs. 73 with enalapril-first (HR, 0.88; 95% CI, 0.63–1.22; between-group difference P ¼ 0.44), and 151 vs. 157 patients were hospitalized (HR, 0.95; 95% CI, 0.76–1.19; between-group difference P ¼ 0.66). Post hoc analysis of data from the first year indicated that a bisoprolol-first strategy reduced mortality by 31%, compared with an enalapril-first strategy (HR, 0.69; 95% CI, 0.46–1.02; between-group difference P ¼ 0.065). Conclusion Initiating treatment with bisoprolol is as effective and well-tolerated as initiating treatment with enalapril. Post hoc analysis suggests that starting treatment with bisoprolol may reduce the risk of death, especially in the first year of treatment. Introduction Current guidelines recommend initiating treatment for CHF with an ACE-inhibitor and then adding a beta-blocker,1,2 but this sequence is not evidence-based. Until, now, there has been no answer to the important clinical question of which agent to use first: ACE-inhibitor or beta-blocker? The Cardiac Insufficiency Bisoprolol Study-III (CIBIS-III) * Corresponding author. Tel: þ46 40 33 10 00; fax: þ46 40 33 62 09. E-mail address: [email protected] addressed this issue by comparing starting treatment with the beta1-selective beta-blocker bisoprolol or the ACE-inhibitor enalapril, followed by addition of the other agent (i.e. it compared bisoprolol-first with enalapril-first). The rationale, aims and design of CIBIS-III have been published previously in the European Journal of Heart Failure 3 and are reviewed by Ponikowski in this Proceedings. The results of CIBIS-III were published in September 2005,4 and are reviewed here with the kind permission of the Editor of Circulation. & The European Society of Cardiology 2006. All rights reserved. For Permissions, please e-mail: [email protected] Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 ¨, Sweden Department of Cardiology, Lund University, University Hospital, S-205 02 Malmo C44 R. Willenheimer Results and interpretation antiplatelet agents in 67%, and about 15% were receiving hypoglycaemic treatment. Baseline data Table 1 Baseline data in the CIBIS III trial Bisoprolol-first Enalapril-first (n ¼ 505) (n ¼ 505) Mean age (years) Males (%) NYHA class II (%) NYHA class III (%) Median duration of CHF (months) Mean LVEF (%) Mean serum creatinine (mmol/L) Mean heart rate (bpm) Mean systolic BP (mm Hg) Aetiologya Coronary artery disease (%) Hypertension (%) Valvular heart disease (%) Primary cardiomyopathy (%) Other (%) Baseline diuretic treatment (%) Thiazide diuretics (%) Loop diuretics (%) Potassium sparing diuretics (%) Aldosterone-receptor blockers (%) Baseline antiplatelet medication (%) Baseline cardiac glycoside treatment (%) Baseline hypoglycaemic medication (%) 72.4 65.9 48.5 51.5 20 72.5 70.5 49.5 50.5 18 28.8 99.6 28.8 101.9 78.8 134.5 79.5 133.7 61.2 39.0 2.2 9.7 13.5 63.6 34.1 3.0 10.1 9.9 85.1 83.4 19.2 71.5 10.3 22.8 66.9 10.5 14.3 12.3 68.3 66.1 32.9 30.7 14.3 17.0 The bisoprolol-first and enalapril-first groups were well-matched at baseline.4 a More than one aetiology may be given for each patient. Statistical analysis The primary endpoint was analysed by the log-rank test. Differences in time to event (in days from randomization) of mortality, the combined endpoint of mortality and hospital admission, and of relevant serious adverse events not covered by the primary endpoint were assessed by the log-rank test. Survival curves were calculated using Kaplan–Meier estimates. The proportion of patients with events was analysed by Fisher’s exact test. The intention-to-treat-population included all 1010 patients randomized at baseline. The per-protocolpopulation excluded nine patients entirely from the analysis: four who never took the study medication (one randomized to bisoprolol-first and three to enalapril-first), one with unstable CHF, three with inadmissible prior therapy, and one who did not meet the inclusion criteria. A further 152 had some data excluded from the per-protocol analysis at time points subsequent to other protocol violations (11 never started the second drug, five showed inadequate compliance, 54 had medically illegitimate introduction of the second drug, and 96 had medically illegitimate permanent treatment cessation). A P-value , 0.025 (unilateral test) denotes statistical significance for non-inferiority. For all other comparisons, P , 0.05 denotes statistical significance. Achievement of target treatment regimen During monotherapy, in the bisoprolol-first group, 65% of patients were uptitrated to the target dose (10 mg od) and 82% to at least 5 mg od. In the enalapril-first group, 84% were uptitrated to the target dose (10 mg bid) and 94% to at least 5 mg bid. There was no significant difference between the groups in the percentage started on the additional treatment at the beginning of the combined therapy phase: 89% of patients allocated to bisoprolol-first were started on additional enalapril, and 85% of enalapril-first patients were started on additional bisoprolol (P ¼ 0.13). However, in both study groups, the first-initiated therapy was significantly more likely to be given at higher doses (i.e. at 50% of the target dose) during the combined-therapy phase (Table 2). This observation underscores the findings of prior surveys that the first-initiated therapy stands a better chance of being uptitrated to the target dose.5–7 Primary endpoint (death or hospitalization due to any cause) Overall, the bisoprolol-first and enalapril-first groups were clinically comparable with regard to the primary endpoint (death or hospitalization owing to any cause). The Kaplan–Meier plots for the intention-to-treat and Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 CIBIS-III enrolled 1010 patients at 128 centres in 18 countries in Europe, and in Tunisia and Australia, who were followed up for a mean of 1.22 + 0.42 years (maximum 2.10 years). The two groups had similar clinical and demographic baseline characteristics (Table 1). The mean age was 72.4 years and 68.2% were male. The most common aetiology of CHF was ischaemic heart disease (62.4%); in 36.5% it was considered to be hypertension. Mean left ventricular ejection fraction (LVEF) was 28.8%, and patients were evenly distributed between NYHA classes II and III. About 50% of the patients had a history of acute myocardial infarction, 10% had a history of peripheral vascular disease, 10% a history of cerebrovascular disease, and 20% diabetes. Baseline cardiovascular medication was similar in the two groups, with 84.3% of the patients receiving diuretics (mostly loop diuretics). Fewer than 15% were receiving aldosterone antagonists. A cardiac glycoside was used in 31%, Results of CIBIS III C45 Table 2 Achievement of 50% of the target dose at the end of the CIBIS-III study End-of-study doses Bisoprolol-first (%) Enalapril-first (%) P-value Bisoprolol given at 50% of target Enalapril given at 50% of target 86 82 72 90 ,0.001 ,0.001 In both study groups, the first-initiated therapy was more likely to be last prescribed at 50% of the target dose during the combined-therapy phase. Figure 1 Kaplan–Meier plots of the combined primary endpoint (death or hospitalization) in the intention-to-treat protocol (A) and per-protocol (B) populations in CIBIS-III. Reproduced with permission from Willenheimer et al. Effect on survival and hospitalization of initiating treatment for chronic heart failure with bisoprolol followed by enalapril, as compared with the opposite sequence. Results of the Randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation 2005;112:2426–2435. Secondary endpoints and post hoc analyses All analyses of secondary endpoints were performed on the intention-to-treat population only. Overall, no significant differences were found between groups with regard to secondary endpoints at the end of the study period (e.g. total and cardiovascular mortality, hospitalizations, worsening of CHF requiring hospitalization or while in hospital). However, post hoc analysis of mortality revealed a trend towards fewer deaths in the bisoprolol group, especially during the early study phase (see below). Death or hospitalization due to any cause There was no significant difference between the groups in the secondary endpoint of death or hospitalization due Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 per-protocol populations were virtually superimposable (Figure 1). In the intention-to-treat population, the primary endpoint occurred in 178 patients (35.2%) allocated bisoprolol-first vs. 186 (36.8%) allocated enalapril-first: absolute difference, 21.6%; 95% CI 27.6 to þ4.4%; HR, 0.94; 95% CI, 0.77–1.16; non-inferiority for bisoprolol-first vs. enalapril-first, P ¼ 0.019. Thus, the intention-to-treat analysis met the pre-specified non-inferiority limits for the upper confidence interval of þ5% for absolute difference (¼relative risk of 1.125) and 1.17 for HR. In the per-protocol population (Figure 1), there were 163 events (32.4%) in the bisoprolol-first group vs. 165 (33.1%) in the enalapril-first group. However, despite the near-identical result compared with the intentionto-treat analysis, because of the smaller size of the perprotocol population, the non-inferiority analysis did not quite reach statistical significance. The absolute difference for the primary endpoint was 20.7%; 95% CI; 26.6 to þ5.1%; HR, 0.97; 95% CI, 0.78–1.21; non-inferiority P ¼ 0.046. Thus, the pre-specified non-inferiority criterion (upper limit of 95% CI for the absolute difference of less than þ5%, corresponding to a HR of 1.17) was not met. However, the upper limit of þ5.1% for the 95% CI of the absolute difference was very close to the target of less than þ5%. The field of non-inferiority in clinical trials has been constantly evolving during recent years. The per-protocol analysis is traditionally the preferred and most conservative approach with regard to non-inferiority, but was originally developed for use in short-term trials comparing the pharmacological effects of drugs (e.g. proprietary vs. generic formulations). However, the appropriate population for non-inferiority testing in mortality and morbidity trials is more controversial. In trials with relatively long follow-up periods, such as CIBIS-III, the per-protocol sample becomes difficult to define (despite a blinded definition of the per-protocol sample by the endpoint committee in CIBIS-III). Some experts believe that the intention-to-treat analysis may be considered equally relevant in terms of non-inferiority in long-term mortality and morbidity trials. As the number of patients in the perprotocol sample rapidly diminished with time in CIBIS-III (as in other long-term intervention trials) as a result of protocol violations and withdrawals, this analysis provided less statistical power than the intention-to-treat analysis. This lack of power is considered to be the cause for the lack of statistical significance for noninferiority in the per-protocol sample. Most importantly, the result in the per-protocol analysis was quite consistent with that of the intention-to-treat analysis. C46 R. Willenheimer to any cause at the end of the monotherapy phase (6 months), which occurred in 109 patients in the bisoprolol-first group vs. 108 in the enalapril-first group (HR, 1.02; 95% CI, 0.78–1.33; between-group difference P ¼ 0.90). In a post hoc analysis of the first year, the longest time period during which all patients were followed-up, 155 patients with bisoprolol-first vs. 165 with enalapril-first experienced death or hospitalization due to any cause (HR, 0.94; 95% CI, 0.76–1.17; between-group difference P ¼ 0.59). All-cause mortality Figure 2 Intention-to-treat analysis of all-cause mortality throughout the study (A) and up to 1 year (B). There was a trend towards reduced 1-year mortality in the bisoprolol-first group, which approached statistical significance. (A) Reproduced with permission from Willenheimer et al. Effect on survival and hospitalization of initiating treatment for chronic heart failure with bisoprolol followed by enalapril, as compared with the opposite sequence. Results of the Randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation 2005;112:2426–2435. All-cause hospitalization Over the entire study period, the number of patients hospitalized was similar in the two groups: 151 with bisoprolol-first vs. 157 with enalapril-first: HR, 0.95; 95% CI, 0.76–1.19; between-group difference P ¼ 0.66 (Figure 3). The total number of hospitalizations was also similar: 242 with bisoprolol-first vs. 249 with enalapril-first (between-group difference P ¼ 0.73). With regard to the secondary endpoint of hospitalizations at the end of the monotherapy phase (6 months), 99 bisoprolol-first vs. 92 enalapril-first patients had a hospitalization (HR, 1.08; 95% CI, 0.81–1.43; between-group difference P ¼ 0.59). This non-significant imbalance in favour of the enalapril group may be related to a slightly higher frequency in the bisoprolol-first group of worsening of CHF requiring hospitalization or occurring in hospital (see below). Cardiovascular mortality There was no significant difference in the number of patients dying of cardiovascular causes in the two groups: 55 with bisoprolol-first vs. 56 with enalapril-first: HR, 0.97; 95% CI, 0.67–1.40 (between-group difference P ¼ 0.86). Worsening of CHF requiring hospitalization or occurring in hospital Although there was no significant between-group difference with regard to the secondary endpoint of worsening Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 Over the whole study period, 65 patients died in the bisoprolol-first group vs. 73 in the enalapril-first group: HR, 0.88; 95% CI, 0.63–1.22; between-group difference P ¼ 0.44. The overall number of deaths in the two groups was not statistically different; nor was the difference in the number of patients dying of cardiovascular causes in the two groups: 55 with bisoprolol-first vs. 56 with enalapril-first. However, there was a trend towards fewer deaths in the bisoprolol group, especially early in treatment. At the end of the monotherapy phase, 23 patients had died in the bisoprolol-first group vs. 32 in the enalaprilfirst group (HR, 0.72; 95% CI, 0.42–1.24; between-group difference P ¼ 0.24) representing a 28% mortality reduction. Furthermore, post hoc analysis (Figure 2) showed that at the end of the first year, 42 patients had died in the bisoprolol-first group vs. 60 in the enalapril-first group (HR, 0.69; 95% CI, 0.46–1.02; between-group difference P ¼ 0.065). This amounts to a 31% reduction in mortality, which narrowly misses statistical significance. The trend towards reduced early mortality in the bisoprolol-first group might be explained by a reduction in sudden cardiac death, and these data will be analysed and published in due course. Sudden death is the commonest mode of death in early and mildly symptomatic CHF.8–10 Beta-blockers have a marked effect on sudden death in CHF,8,11,12 whereas ACE-inhibitors have not been convincingly shown to reduce sudden death.13,14 In newly diagnosed CHF, patients may have to remain on the first-initiated neurohormonal inhibitor therapy for several weeks, or even months, while the dose is slowly uptitrated and their condition stabilized. During this period, before the initiation of combination therapy, beta-blockade might be particularly valuable in improving survival through its action on the sympathetic nervous system. More patients might then survive to go on to combination treatment. Results of CIBIS III report heart failure worsening while in hospital as an endpoint. Importantly, as more patients survived the early phase of the study, more patients were at risk of worsening of CHF. This circumstance alone might explain the difference between the two study groups in the worsening of CHF events. A trend towards temporary worsening of heart failure leading to hospitalization might be partly due to physicians’ limited experience of uptitrating a beta-blocker in patients not on an ACE-inhibitor. With more experience, worsening of CHF during initial uptitration of the beta-blocker might be avoided. Other secondary endpoints There was no significant difference between groups in the need for early introduction of the second drug, or with regard to treatment discontinuation during the study overall or during the monotherapy phase (Table 3). Pre-specified subgroup analyses Figure 3 Intention-to-treat analysis of all-cause hospitalization throughout the study. There was no significant difference in hospitalizations between the two groups. In the pre-specified subgroup analyses, with regard to LVEF, there was a significant interaction regarding the primary endpoint (P ¼ 0.001) (Figure 5). Among patients with LVEF ,28%, those receiving bisoprolol-first were significantly less likely to die or be hospitalized than those receiving enalapril-first (HR, 0.61; 95% CI, 0.44–0.85; P ¼ 0.003), whereas there was an opposite trend among those with LVEF 28% (HR, 1.23; 95% CI, 0.94–1.61; P ¼ 0.13). The same pattern was seen if the median LVEF value of 30% was used as cut-off (interaction P ¼ 0.036). However, these findings may be explained by an imbalance between the groups in non-cardiovascular hospitalizations during the monotherapy phase, and are probably not of any clinical significance. Other pre-specified subgroup analyses showed no significant differences in the effect of treatment on different subgroups (in relation to sex, age, NYHA class, digitalis use, or heart rate, blood pressure, or serum creatinine at baseline). Table 3 Other secondary endpoints in the CIBIS-III study Early introduction of second drug (%) Permanent treatment cessation Monotherapy phase (%) Combination phase Bisoprolol (%) Enalapril (%) Figure 4 Intention-to-treat analysis of worsening heart failure requiring hospitalization or occurring in hospital. There was a non-significant trend in favour of enalapril. Reproduced with permission from Willenheimer et al. Effect on survival and hospitalization of initiating treatment for chronic heart failure with bisoprolol followed by enalapril, as compared with the opposite sequence. Results of the Randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation 2005;112:2426–2435. Total (%) Bisoprolol-first Enalapril-first 39 (7.7%) 37 (7.3%) 35 (6.9%) 47(9.7%) 19 (3.8%) 47 (9.3%) 24 (4.7%) 16 (3.2%) 101 (20.0%) 89 (17.6%) There was no significant difference between groups in the need for early introduction of the second drug because of poor control of CHF, or with regard to treatment discontinuation during the study overall or during the monotherapy phase. Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 of CHF requiring hospitalization or occurring in hospital, there was a non-significant trend in favour of enalaprilfirst (Figure 4). Heart failure worsening occurred in 63 patients in the bisoprolol-first group vs. 51 in the enalaprilfirst group: HR, 1.25; 95% CI, 0.87–1.81; between-group difference P ¼ 0.23. The total number of worsening events was 84 in the bisoprolol-first group vs. 66 in the enalapril-first (between-group difference P ¼ 0.27). In the long-term, beta-blockers decrease hospitalization in CHF.8,11,12 However, it is well-known that initiation and uptitration of a beta-blocker may cause minor and temporary worsening of heart failure symptoms (followed by improvement).1,2 It is conceivable that bisoprolol was uptitrated too aggressively for the predominantly elderly population included in CIBIS-III. However, this explanation is considered unlikely, as the uptitration schedule was slower than that used in CIBIS-II.11 It is possible that the early negative inotropic effect of beta-blockade might appear differently in patients not receiving background ACE-inhibition. Temporary worsening of symptoms is usually handled by an increase in the dose of diuretic, and this alone might have been enough reason for some physicians to C47 C48 R. Willenheimer Safety The two strategies were comparable in terms of serious and total adverse events (Table 4). During the entire trial, 119 patients were formally withdrawn from the Table 4 Serious adverse events and adverse events in the safety population in CIBIS-III (all patients who received at least one dose of randomised treatment)4 Number of patients (%) Monotherapy Serious adverse events Adverse events Entire study Serious adverse events Adverse events Bisoprolol-first (n ¼ 504) Enalapril-first (n ¼ 502) 113 (22.4) 316 (62.7) 111 (22.1) 319 (63.5) 184 (36.5) 396 (78.6) 187 (37.3) 395 (78.7) study, 60 from the bisoprolol-first group and 59 from the enalapril-first group. Discontinuations due to adverse events were similar in the two groups: 48 in the bisoprolol-first group vs. 51 in the enalapril-first group. Both regimens had similar effects on blood pressure, during both the monotherapy and combined therapy phases. Mean systolic blood pressure in the bisoprololfirst group was 134.5 mmHg at baseline and 124.8 mmHg at 1 year, compared with 133.7 mmHg at baseline and 124.8 mmHg at 1 year in the enalapril-first group. Mean diastolic blood pressure in the bisoprololfirst group was 80.4 mmHg at baseline and 74.5 mmHg at 1 year, compared with 80.7 mmHg at baseline and 75.0 mmHg at 1 year in the enalapril-first group. There was a more pronounced heart-rate-lowering effect during the monotherapy phase in the bisoprolol-first group, from a mean of 78.8–67.9 bpm, compared with 79.5–78.6 in the enalapril-first group. After 1 year (i.e. after half a year in the combined phase), heart rate was similar in both groups: 66.7 bpm in the bisoprololfirst group vs. 67.5 bpm in the enalapril-first group. Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 Figure 5 Pre-specified subgroup analyses with regard to the primary endpoint in the intention-to-treat population. Reproduced with permission from Willenheimer et al. Effect on survival and hospitalization of initiating treatment for chronic heart failure with bisoprolol followed by enalapril, as compared with the opposite sequence. Results of the Randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation 2005;112:2426–2435. Results of CIBIS III Conclusions There was an intriguing trend towards improved survival with bisoprolol-first, especially during the first year of treatment. With bisoprolol-first, fewer patients died and the deaths occurred later in the study. In the first year, bisoprolol-first reduced mortality by 31%, compared with enalapril-first (P ¼ 0.065). It may be speculated that this difference is related to the known protective effect of beta-blockade against sudden death, which is particularly common in early and mildly symptomatic CHF.8–10 As illustrated in Figure 6, the priority at this critical time is to inhibit the sympathetic system, which is achievable with beta-blockers, but not ACE-inhibitors. A beta-blocker-first strategy may therefore be particularly relevant in early CHF. Patients had to be at least 65 years of age to be included in the CIBIS-III study, and the mean age of the included patients was around 74 years at the end of the study, which is close to the mean age of around 75 years in the general population of CHF patients in clinical practice.5,16 In addition, many of the patients in CIBIS-III had co-morbidities such as hypertension and diabetes, again reflecting the real-life situation. Physicians can therefore be confident that a slow uptitration to the maximum tolerated dose within the target levels recommended by current guidelines is safe and well tolerated even in elderly patients and those with co-morbidities.1,2 The findings of CIBIS-III challenge the current recommendation that treatment of CHF should begin with an ACE-inhibitor followed by a beta-blocker, and imply that physicians should be free to initiate CHF treatment with either class of drug, according to their clinical judgement in individual patients.19,20 The daily practice of some physicians will probably change as a result of CIBIS-III. Although, European and US guidelines have only recently been revised, and are not due to be updated for some time, the evidence from CIBIS-III will probably be incorporated into national guidelines in the near future, contributing in a practical way to the rational and effective management of CHF. Conflict of interest: R.W. has served in the Steering Committee of CIBIS-III and has received lecture fees from Merck KGaA, Darmstadt, Germany. References Figure 6 Goals of treatment in CHF in relation to disease progression in CHF: the need for prevention of sudden cardiac death in the early stages of the disease. Reproduced with permission from Willenheimer and Silke. Possible clinical implications of the Cardiac Insufficiency Bisoprolol (CIBIS) III trial. Br J Cardiol 2005;12:448–454. 1. Swedberg K, Cleland J, Dargie H et al. Guidelines for the diagnosis and treatment of chronic heart failure: executive summary (update 2005): The Task Force for the Diagnosis and Treatment of Chronic Heart Failure of the European Society of Cardiology. Eur Heart J 2005;26:1115–1140. 2. Hunt SA, Abraham WT, Chin MH et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult–Summary Article: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). Circulation 2005;112:1825–1852. 3. Willenheimer R, Erdmann E, Follath F et al. Comparison of treatment initiation with bisoprolol vs. enalapril in chronic heart failure patients: rationale and design of CIBIS-III. Eur J Heart Fail 2004;6:493–500. 4. Willenheimer R, van Veldhuisen DJ, Silke B et al. Effect on survival and hospitalization of initiating treatment for chronic heart failure Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 ACE-inhibitors and beta-blockers are standard treatments for CHF, as recommended by international guidelines.1,2 CIBIS-III3,4 is the first large randomized controlled trial to examine whether the order of initiation of these two important treatments makes any difference to morbidity and mortality. This is important, as although combination treatment is highly desirable, many CHF patients do not receive this combination. Some patients may receive inadequate doses, or remain on the first-initiated drug for extended periods.5,15,16 CIBIS-III, therefore, provides a clear answer to a clinically relevant question. The bisoprolol-first and enalapril-first groups in CIBIS-III were clinically comparable with regard to the primary endpoint (all-cause mortality and hospitalization) and all secondary endpoints. Bisoprolol-first was demonstrated to be non-inferior to enalapril-first in the intention-to-treat analysis of the primary endpoint. Both strategies were equally safe and well tolerated. It is important to note that in CIBIS-III, the doses of both drugs were titrated up to maximum tolerated levels depending on the individual response to treatment. Uptitration was mandatory unless intolerance occurred, but could be carried out more slowly than planned if this was helpful in any individual patient. Individual dose adaptations of beta-blockers based on maximum tolerability do not seem to lead to an inferior effect on survival and morbidity.17,18 However, there is limited experience of uptitration of beta-blockers in the absence of ACE-inhibitors, and this may be relevant to the observed non-significant increase in the worsening of CHF requiring hospitalization or occurring in hospital. The bisoprololfirst strategy could be further improved with greater experience of uptitration of the beta-blocker-first, leading to less worsening of CHF. In this regard, it is important to consider the fact that more patients survived the early phase of the study in the bisoprolol-first group. Consequently, more patients were at risk of worsening of CHF in the bispoprolol-first group. C49 C50 5. 6. 7. 8. 9. 10. 12. with bisoprolol followed by enalapril, as compared with the opposite sequence. Results of the Randomized Cardiac Insufficiency Bisoprolol Study (CIBIS) III. Circulation 2005;112:2426–2435. Cleland JG, Cohen-Solal A, Aguilar JC et al. Management of heart failure in primary care (the IMPROVEMENT of Heart Failure Programme): an international survey. Lancet 2002;360: 1631–1639. Davies M, Hobbs F, Davis R et al. Prevalence of left-ventricular systolic dysfunction and heart failure in the Echocardiographic Heart of England Screening study: a population based study. Lancet 2001; 358:439–444. Komajda M, Lapuerta P, Hermans N et al. Adherence to guidelines is a predictor of outcome in chronic heart failure: the MAHLER survey. Eur Heart J 2005;26:1653–1659. MERIT-HF Study Group. Effect of metoprolol CR/XL in chronic heart failure: METOPROLOL CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF). Lancet 1999;353:2001–2009. Uretsky BF, Sheahan RG. Primary prevention of sudden cardiac death in heart failure: will the solution be shocking? J Am Coll Cardiol 1997;30:1589–1597. Aliot E, de Chillou C, Sadoul N. Ventricular instability and sudden death in patients with heart failure: lessons from clinical trials. Eur Heart J 2002;4(Suppl. D):D31–D42. CIBIS II Investigators and Committees. The Cardiac Insufficiency Bisoprolol Study II (CIBIS-II): a randomised trial. Lancet 1999; 353:9–13. Packer M, Coats AJ, Fowler MB et al. Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med 2001;344:1651–1658. 13. Cleland JG, Massie BM, Packer M. Sudden death in heart failure: vascular or electrical? Eur J Heart Fail 1999;1:41–45. 14. Garg R, Yusuf S. Overview of randomized trials of angiotensinconverting enzyme inhibitors on mortality and morbidity in patients with heart failure. Collaborative Group on ACE Inhibitor Trials. JAMA 1995;273:1450–1456. 15. Komajda M, Lapuerta P, Hermans N et al. Adherence to guidelines is a predictor of outcome in chronic heart failure: the MAHLER survey. Eur Heart J 2005;26:1653–1659. 16. Komajda M, Follath F, Swedberg K et al. The EuroHeart Failure Survey programme—a survey on the quality of care among patients with heart failure in Europe. Part 2: treatment. Eur Heart J 2003; 24:464–474. 17. Wikstrand J, Hjalmarson A, Waagstein F et al. Dose of metoprolol CR/XL and clinical outcomes in patients with heart failure: analysis of the experience in metoprolol CR/XL randomized intervention trial in chronic heart failure (MERIT-HF). J Am Coll Cardiol 2002;40:491–498. 18. Simon T, Mary-Krause M, Funck-Brentano C, Lechat P, Jaillon P. Bisoprolol dose-response relationship in patients with congestive heart failure: a subgroup analysis in the cardiac insufficiency bisoprolol study (CIBIS II). Eur Heart J 2003;24:552–559. 19. Willenheimer R, Silke B. Possible clinical implications of the Cardiac Insufficiency Bisoprolol (CIBIS) III trial. Br J Cardiol 2005;12:448–454. 20. Willenheimer R. Implications of CIBIS III: a commentary. JRAAS 2005;6:115–120. Downloaded from http://eurheartjsupp.oxfordjournals.org/ by guest on September 16, 2014 11. R. Willenheimer
© Copyright 2026