How to make the Affordable Care Act more affordable: The employer’s perspective
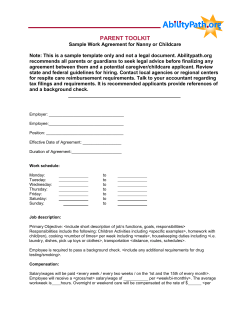
How to make the Affordable Care Act more affordable: The employer’s perspective Karen Kirkpatrick In the sixteen years Karen Kirkpatrick has worked at Infinisource, she has gained a national reputation for being one of the foremost experts on HR, Payroll, COBRA, HIPAA, FMLA, Consumer Driven Health Plan Options and Health Care Reform. She has conducted more than 1,000 seminars, webinars and executive briefings on numerous federal insurance laws. Karen brings Infinisource the valuable expertise of many years of marketing and professional development experience. “The only thing that is constant is change.” ― Heraclitus Agenda • • • • Employer mandate Employer requirements Employer disclosures and reporting Plan design options Employer Mandate 5 What is the Affordable Care Act (ACA)? Part of it expands health insurance coverage by: Individual mandate Requiring individuals to obtain minimal essential coverage (MEC) for themselves Play-or-pay and Requiring employers to offer minimum essential coverage for substantially all employees (70% in 2015 and 95% in 2016) Employer Mandate • Applicable Large Employers (ALE) must offer to all full time employees, Minimum Essential Coverage (MEC) that is both Affordable and meets the Minimum Value (MV) definitions • Or - be subject to potential penalties. • As seen below: the $2,000 penalty is referred to as the No Coverage Penalty. This means no MEC. • The $3,000 penalty is referred to as the Inadequate Coverage Penalty. This means the MEC is not meeting both the Affordable and MV requirements. • The lesser of: • $2,000 x total FT employee count – 80 (if at least one FT employee gains coverage and a subsidy in the HIX) or, • $3,000 for each FT employee who gains coverage and a subsidy in the HIX Who Does the Act Apply to? Employer mandate: What is an ALE? Do you have 100+ employees in 2014 for 2015 and 5099 in 2015 for 2016? # full-time employees (FT) # hours worked by part-time employees per month 120 Full-time Employee Status Is not always clear, is it? Hours of Service Each hour of work for which the employee is paid Each hour of non-work for which employee is paid or entitled to payment (e.g., vacation, PTO, holidays, various leaves, etc.) Ongoing Employee Employed for at least one complete standard measurement period Employer permitted to use defined measurement and stability periods of up to 12 months Employers may need time between the those periods to determine which ongoing employees are eligible for coverage, and to notify and enroll employees Employer may make time for these administrative steps by having its standard measurement period end before the associated stability period begins Defined as an “administrative period” not to exceed 90 days New Employee-Safe Harbor Employer maintains a GHP that would offer coverage only if the employee were determined to be a full-time employee The employer may use both a 3-12 month measurement period and an administrative period of up to 90 days for variable hour and seasonal employees (now defined as <6 months) The initial measurement and administrative period, combined, can’t extend beyond 13 months, plus a fraction of a month New Employee-Safe Harbor • Employer using facts and circumstances on the employee’s start date cannot reasonably ascertain that the employee will work an average of 30 hours a week • After January 2015 these employees will be considered employed for the entire measurement period Controlled Groups Look at entire group to determine 100 FTE count Each corporation is looked at individually to determine penalty Each corporate gets a ratio % of less 80 FT count Rehired or Resuming Employees On/off employees, unpaid for some legitimate reason or even unpaid leave of absence affected employees – Break of at least 26 weeks - treat as new employee – Break is not 26 weeks - employer determines average hours of service per week during the measurement period (excluding special unpaid leave period) and uses that average for the entire measurement period Dependent IRC Section 4980H requires large employers to offer minimum essential coverage to all full-time (30 hours) employees and their dependents Dependent is defined as the employee’s child under age 26 (2015 is another year of transition for this requirement) No penalty for not offering coverage to spouses Substantially all Full-time Employees The penalties under IRC Section 4980H(a) should not apply to employers who offer minimum essential coverage to substantially all full-time employees – Defined as 70% of their full time employees (so, coverage can be offered to all but 30%-think those working 30-39 hours?) Ongoing Employee Example Measurement period (MP): October 15-October 14 Administrative period (AP): October 15-December 31 Stability period (SP): January 1-December 31 John & Amy are ongoing employees. John works 31 hours per week during the MP, Amy works 29 hours. John is a full-time employee during 2014, even if his hours drop below 30 in 2014; Amy is not a full-time employee during 2014, even if her hours increase above 30 in 2014 Non-standard Measurement Periods Subcategories of employees Employers can use different measurement, administrative and stability periods for: – – – – Both collectively and noncollectively bargained employees Groups of employees within different unions Salaried and hourly employees Employees working in different states Graphic that Marketing is working on Administrative Periods • Employers have an option to use specified administrative periods of up to 90 days from measurement period - stability period to determine which ongoing employees are eligible for coverage and to notify and enroll employees • The employer can use an administration period of up to 90 days for new variable-hour and seasonal employees, which may not extend beyond the last day of the first calendar month beginning on or after the one-year anniversary of their start date (13 months and some change) Affordable Coverage Employee’s portion for self only coverage does not exceed 9.5% (Box 1) of W-2 income Safe harbors for affordability include – Rate of pay – Federal poverty line Cost Sharing Tiers • Effective in 2014 with the HIM • ACA established four standard tiers of insurance coverage − Bronze (60%) - minimum amount of coverage to meet the individual mandate − Silver (70%)and Gold (80%) - must be offered by any health insurer participating in the HIM − Platinum - provides for 90% • Tiers vary by level of cost sharing required, also defined as actuarial value − Represents amount of health expenses a health insurer will pay for a standard population − The individual is responsible for the remaining percent, paying through some combination of deductibles, co-pays and coinsurance Waiting Period 24 Waiting Period • A group health plan (GHP) or individual health insurance coverage shall not apply any waiting period (as defined in section 2704(b)(4)) that exceeds 90 days • Effective for plan years starting on or after January 1, 2014 • Non-compliance would violate ERISA making employer subject to ERISA Penalties 25 General Rules • Applies to group health plans, fully insured and self-insured and individual insurance • Not applicable to HIPAA excepted benefits • Time spent as a part-time employee would not count if eligibility were based on full-time status Future Reporting Responsibilities 27 Employer Disclosures and Reporting 28 Model Exchange Notice • Applies to all employers that are subject to the Fair Labor Standards Act • Model Exchange Notice must be sent to all current employees • Model Notice should have been sent no later than October 1, 2013; thereafter, it must be provided within 14 days to all new hires Summary of Benefits & Coverage (SBC) • All applicants and enrollees for all GHPs, except HIPAA-excepted benefits (e.g., stand-alone dental, vision, most Health FSAs) • The ACA requires employers to provide an SBC, a four-page, double-sided summary that allows health care consumers to compare coverage options • Annual requirement Grandfathered Plan Notices • ACA requires this notice be provided to all participants if the plan is to maintain its grandfathered status • Explains that the plan or coverage is a grandfathered health plan with the ACA definition • Annual requirement while GHP maintains grandfathered status • Grandfathered plans do not have to comply with some of the rules related to the ACA. However, they must comply with other rules, like annual and lifetime limits, dependent coverage up to age 26, rescission and limits on preexisting condition exclusions (PCEs) Patient Protection Disclosures • Employers must notify participants of their right to designate any primary care provider who participates in the network • Annual notice must be provided whenever the plan provides a SBC • This notice provides individuals enrolled in the health plan information regarding rights to choose a primary care provider or a pediatrician when a plan or issuer requires designation of a primary care physician or obtain obstetrical or gynecological care without prior authorization COBRA Qualifying Event Communications • During the release of the Marketplace Notice, an updated Qualifying Event Notice was posted on the DOL/EBSA website • Employer’s notices should have been updated immediately • New language in notice regarding rights within the marketplace • Language for TAA and HIPAA deleted Form 8928 and Form 720 • http://www.irs.gov/pub/irs-pdf/f720.pdf • http://www.irs.gov/pub/irs-pdf/f8928.pdf PCOR Matrix 35 Marketplace Notice 38 • May 8, 2013, the DOL issued Technical Release 2013-02 • All employers subject to the FLSA must provide: – Model Notice to Employees of Coverage Options related to Health Insurance Marketplace • Current employees no later than October 1 regardless of eligibility for health insurance and employee class • Post October, to all new hires within 14 days (through 2014) Existence of the Marketplace Description of the services provided by the Marketplace How employees may contact the Marketplace for assistance If the employer’s share of total costs of provided benefits is less than 60 percent (i.e., whether it offers minimum value) • The possibility of being eligible for a premium tax credit under the Marketplace • The loss of their employer’s contribution (if any) for health benefits and • All or a portion of the contribution may be excludable from income for federal tax purposes • • • • Plan Design Options 41 Account based plans •FSAs •HRAs •HSAs •CDH combo •Pitfalls Prohibited arrangements HRAs, Health FSAs and Employer Payment Plans must either be a HIPAAexcepted benefit or integrated with a medical plan Prohibited arrangements HIPAA-excepted Health FSAs must meet two conditions: 1 The employer makes available GHP coverage that is not HIPAA-excepted 2 The maximum benefit cannot exceed two times the salary reduction or, if greater, cannot exceed $500 plus the salary reduction Permitted arrangements Two categories of arrangements remain permissible: HIPAA-excepted HRAs Integrated HRAs Permitted arrangements HIPAA-excepted benefits retiree-only plans, limited scope dental/vision plans, and plans that cover cancer, hospital indemnity, accident and disability Permitted arrangements Permissible: An HRA that covers only HIPAA-excepted benefits Retiree-only HRAs More and more large employers are moving to a retiree-only HRA model to control retiree medical costs. Permitted arrangements An HRA must pass one of two integration tests to be considered integrated with another non-HRA group health plan (GHP) (i.e., a major medical plan) Permitted arrangements Five criteria for each test When it’s effective A stand-alone HRA that was in effect before September 13, 2013, can continue until the end of the current plan year New HRAs created on or after September 13, 2013, will be out of compliance Penalties What are the penalties for a prohibited arrangement? Reimbursements made to highly compensated employees are considered taxable. Violations of the ACA rules on annual limits and preventive services: payment of a daily excise tax equal to $100 per participant. New: IRS Allows FSA Carryover • An employer must amend its 125 cafeteria plan document no later than the last day of the plan year from which it wants to carry over the amount • Cannot have a carry over feature and a grace period • Eliminate current grace period by the same deadline that applies to the carryover • Employer may limit carryover amount to less than $500 or not allow at all New: IRS Allows FSA Carryover • Carry over amount is available for the entirety of the next plan year • Carry over amount is available, even if a participant does not make an election for the next plan year • In theory, a balance could be carried over for several years even though the participant does not elect Health FSA coverage New: IRS Allows FSA Carryover • The carry over amount does not affect the 125(i) limit on salary reduction contributions • Carryover is a plan option and applies to all participants, including COBRA Qualified Beneficiaries • This Notice does not change the COBRA rule that applicable HIPAA-excepted Health FSAs may be terminated at the end of the plan year in which the qualifying event occurs New: IRS Allows FSA Carryover • Any unused amounts above the employerestablished carry over limit are subject to forfeiture • Cash-out of unused amounts or a transfer of unused amounts to other taxable or nontaxable benefits is not allowed • Health FSAs can still use run-out periods Elections • The IRS also expanded application of an election change exception • Under the guidance, noncalendar (fiscal) year plans can permit participants to make election changes in 2013 to enroll in or drop coverage outside of open enrollment • This rule applies to employers of all sizes • Employers must amend their plan documents before December 31, 2014 Wellness Initiatives 57 Wellness Incentives A program of health promotion or disease prevention 58 Wellness Incentive Types 1. Participatory 2. Health-contingent 59 Wellness Requirements • • • • • Frequency Amount Availability Reasonableness Notice Examples Annual medical plan premium: $6,000 Employer pays: $4,500 Employee pays $1,500 Employer offers $600 health-contingent reward and imposes $2,000 tobacco premium surcharge Good incentive. The total of all rewards is $2,600, which is less than 50% of premium and $600 reward does not exceed 30%. Total cost is $6,000, not $1,500. 61 Examples Annual medical plan premium: $5,000 Employer provides: $250 reward for completing health risk assessment, $1,500 for meeting health-contingent standard Good incentive. Even though $1,750 is more than 30% of premium cost, the $250 reward is not counted because it is participation based. 62 Examples • Employer rewards cholesterol test under 200. Employer provides a different, reasonable means of qualifying for reward. June’s count is above 200. Employer’s nurse recommends diet and exercise routine that is not unreasonably difficult. After program, June’s count is still above 200. Program requires doctor visit and to follow additional recommendations. Doctor prescribes medication and requires periodic evaluations. Good incentive. June qualifies for reward, but only if she actually follows doctor’s advice. 63 Gray Areas • Financial reward apportionment • How to define tobacco use • Applying percentage limits to a financial reward • Design requirement – use evidence- or practice-based standards? Join over 29,000 of your peers and receive our Newsroom blog. Visit us at www.infinisource.com 800.300.3838
© Copyright 2026