time, effort and catheters why bother ? C Egeler, Swansea
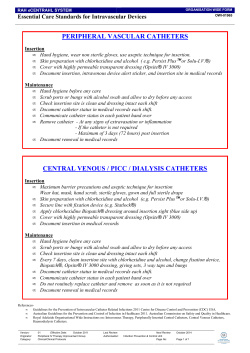
time, effort and catheters why bother ? Contiplex C Catheter Set in clinical practice C Egeler, Swansea Alec Snell Photography why use nerve blocks ? • • • • post op pain relief no GA side effects no opioids recovery / discharge time • day surgical stay • cost savings • reduce risk of chronic pain (?) problems of single shot block • weak dose = short duration • strong dose = longer duration – motor block • how painful after block resolution ? • what analgesic, how much and when? femoral nerve block double dose = double duration ? pilot study • lateral cut. nerve forearm • superficial radial nerve • median nerve • ulnar nerve lateral brachio radialis medial CV LCN superf RN deep RN biceps tendon BA MN elbow joint methods • US identification of nerve at elbow / forearm • 0.25 % chirocaine – – – – 1.25 ml 2.5 ml 5 ml 5 ml 0.5 % chirocaine onset of block min 10 9 8 7 6 5 4 3 2 1 0 1.25 ml 2.5 5 5 of 0.5 % LCNF Sup rad median uln ar block duration of 0.25 % chirocaine 16 14 12 10 1.25 8 2.5 6 5 4 5 of 0.5 % 2 0 LCNF Sup rad median ulnar doc, I was great until 3 am …. • waking up in pain • no analgesia • catch up on oral analgesia – opioids • loss of confidence in blocks – patient, nurses, surgeons catheters allow • continuing analgesia • less initial bolus • less motor block Catheter use in Swansea: • trauma patients • shoulder / elbow surgery • hip / knee replacements • abdominal / urological procedures • amputations / chronic pain • 5 ml /hr Chirocaine 0.15 % infusion Catheters – options so far • Stimulating needle – non stimulating catheter – end position ? • Stimulating needle – stimulating catheter – time consuming – good positioning – expensive • Morin, Astrid M. et al: The Effect of Stimulating Versus Nonstimulating Catheter Techniques for Continuous Regional Anesthesia: A Semiquantitative Systematic Review RAPM 2010 - Volume 35/2 - pp 194-199 • Antonakakis, John G. MD: Ultrasound-Guided Posterior Approach for the Placement of a Continuous Interscalene Catheter. RAPM 2009, 34 /1 - pp 64-68 16 patients insertion time 17 min infusion 10 ml/hr I don’t do catheters because : • • • • • • • it’s a fiddle takes too long don’t work in the way of surgeon they fall out / migrate need for follow up risk of nerve damage The Ideal Catheter • painless to insert • easy to direct • good US visibility 20 + G needle • no fiddle • no leakage / migration • no kinking / falling out catheter over needle • versatile – distal and proximal blocks – parallel or transverse to nerve Wang, Ai-Zhong MD* et al: Ultrasound-Guided Continuous Femoral Nerve Block for Analgesia After Total Knee Arthroplasty: Catheter Perpendicular to the Nerve Versus Catheter Parallel to the Nerve. RAPM 2010 – 35/2 - pp 127-131 12 vs 22 min insertion time Catheters should allow • bolus = infusion level – catheter over needle catheters used in Swansea • stimulating catheter • Supraclavicular • lumbar plexus • Fascia Iliaca Compartment • 18 G epidural set • Femoral – TAP / QLC – paravertebral – sciatic popliteal Fascia Iliaca Compartment Supraclavicular catheter Contiplex A Supraclavicular catheter Contiplex A catheter • • • • easy, quick insertion good feel for tissues excellent US visibility bolus = infusion position • 18 G = req. LA • too big for distal blocks ? • too short for deeper blocks • can kink and obstruct R.I.P. Contiplex C • 25 G 190 mm 30 ° bevel • 19 G catheter over needle • non kinkable • stimulator attachment • bolus = infusion Contiplex C • • • • • distal block proximal block deep block in line / out of line in plane / out of plane Peripheral block – deep radial nerve • • • • 65 year old intolerant of analgesics trapezectomy elbow + tourniquet blocks • awake surgery • postop deep radial nerve catheter deep radial nerve catheter • • • • • procedure time = 18 min ambulatory infusion 2 ml/hr 0.25 % Chirocaine 48 hour review rescan + removal deep radial catheter review • not 100 % sufficient after 16 hours • bolus via catheter: • Conclusion: don’t put across joints axillary catheter • • • • • • • • 17 year old wedge osteotomy wrist GA + axillary block postop axillary catheter median + ulnar nerve ambulatory infusion 4 ml 0.25 % Chirocaine removal 48 hours by patient axillary catheter • • • • insertion time 17 min out of plane approach several attempts tip between median and ulnar nerve in axilla • good catheter visibility X Paravertebral Catheter • • • • 72 year old partial nephrectomy GA + Paravertebral T5/6 20 ml 0.5 % Chirocaine bolus • 8 ml/hr 0.15 % Chirocaine infusion • 3 days postop removal Paravertebral Catheter • in plane approach • sagittal plane • angle of 50 ° – US visibility poor • good LA spread • effective analgesia Quadratus Lumborum Compartment Catheter • • • • 25 year old ORIF hemipelvis GA + QLC catheter 40 ml 0.375 % Chirocaine • 8 ml/hr 0.15 % Chirocaine 3 days • effective analgesia QLC catheter • • • • in plane approach 30 ° angle reasonable visibility good LA spread • 17 min Femoral Catheter in plane • • • • 68 year old femoral # post TKR ORIF GA + femoral catheter – obturator single shot • 8 ml 0.375 % Chirocaine • 5 ml/hr 0.15 % Chirocaine infusion • insertion time 5 min • good visibility • shallow angle sciatic popliteal catheter • 15 year old CRPS • sural nerve biopsy • GA, sciatic catheter – saphenous single shot • 20 ml 0.5 % Chirocaine • 8 ml/hr 0.25 % Chirocaine 2 days • out of plane approach • parallel to nerve • end position at bifurcation • insertion time 10 min Sciatic Catheter in plane • 68 year old • ankle fusion • GA + sciatic catheter – saphenous single shot • 10 ml 0.375 % Chirocaine bolus • 5 ml/hr 0.15 % Chirocaine infusion 2 days Sciatic catheter in plane • parallel to probe • good visibility • tip between tibial and CFN • good spread • effective analgesia • 5 min insertion time Conclusion • Contiplex C is versatile – – – – distal blocks proximal blocks superficial blocks (deep blocks ) • in plane approach transverse to nerve – easier = faster • US visibility wish list: • 20 – 21 G needle – better handling for deep blocks – US visibility – tissue feel (Contiplex A tip) • 100 mm for in plane catheters
© Copyright 2026