“Why help AWP” I’m willing to Julian Hendy on the
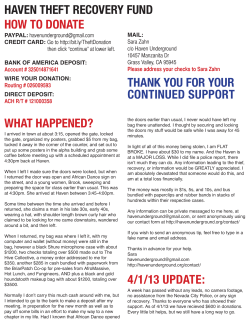
Issue 14 “Why I’m willing to help AWP” PLUS: A Haven of recovery The spiritual side of mental health Meet The Moustache of the Year 2012 And more! Julian Hendy on the death of his father and what we need to learn from it. December 2012 welcome welcome Recognised for improving lives Winter has arrived and you find the Ourvoice team huddled around a candle for warmth. Should it get particularly cold we may even light it. Many congratulations to all the winners, finalists and nominees in the Staff Awards 2012 – and to the fourteen staff and teams who were awarded NHS Heroes certificates at the celebration. Still, it’s not exactly a big change from the rest of 2012 which turned out to be damp and miserable. Makes you wonder how we manage to stay so positive! The secret to that seems to be keeping busy, and this issue is further proof of the packed working lives the AWP gang lead. All our winners, finalists and guests Another reason for keeping busy is that we have a new boss, as Iain Tulley has recently joined us as Chief Executive. While there wasn’t quite the fanfare and bunting of the US presidential elections, we’d like to extend our welcome and we look forward to hearing from Iain in future issues. We’re also very pleased to welcome Julian Hendy to Ourvoice (see pages 4-5). The tragedy that Julian’s family went through has led to him giving AWP a unique and challenging perspective on the way we manage service users who may be violent. We think you’ll find the interview thought-provoking. Our three lifetime achievers share a congratulatory group hug An ironically unforgettable performance: ‘Why, why, why, dementia? ’ sung by Forget-Me-Not Centre members and staff Above: Duncan, Nicolette and Rosie survey the wall of sound, while (opposite) preparing for the abseil. Ourvoice stalwart and roving reporter Lucy Robinson has been finding out about living a good life down at the Haven recovery project, plus we’ll discover what H.O.P.E. is all about and so much more besides. Before we see you next there’s the small matter of Christmas to look forward to. Whether you celebrate or not, have a happy, warm and safe festive season from everyone on the Ourvoice team. All the best Joyce Starkie, delighted winner of the ‘volunteers’ category, with runners up Gladys Medcroft and Emilia Love 2 Enabling people to reach their potential. Simon 4 Father and son Julian Hendy talks to Ourvoice 6The Mysterious World of AWP Meet Chris Wall, Moustache of the Year! 6 Stand by for action Dealing with problems is a real team effort 7 Driven and determined 8 A haven of recovery 9 Getting support and motivation from your peers Lucy Robinson discovers a secret garden in the heart of Bristol 30 Second interview Meet Dan Meron 10 In essence! How good practice is energising us all 11 All of me Faith, H.O.P.E. and spirituality Simon Gerard, Editor Empowering people to live fulfilling lives. 3 feature feature Ourvoice: Julian, prior to the tragic death of your father, what was your view of mental health issues? You’d made some films on the subject, hadn’t you? Julian Hendy: I’d made a number of films on the subject and I was – and actually still am – very supportive of good mental health. I was very aware of the blight that some serious mental illness can have on people’s lives and their families and communities. Following the killing of his father by an AWP service user, Julian Hendy had found himself at odds with the Trust. So what has led him to want to help us? Interview by Simon Gerard convictions for violence seemed not to have been part of a risk assessment and he was therefore “at liberty” in the community. Julian’s battle to get the answers he needed took place across emails, telephone calls, newspaper articles and a BBC2 documentary called Why Did You Kill My Dad? In April 2007, Philip Hendy was walking to pay his paper bill in Bristol when a chance encounter with an AWP service user ended in tragedy. Mr Hendy, a 75 year old father and grandfather was attacked and stabbed by Stephen Newton. There was no motive, no reason, no explanation. A week later, Philip Hendy died in intensive care… Above: Philip and Julian Hendy. Opposite page: Philip Hendy with grandson Alexander, Philip with children in 1962. Following his father’s death, Julian Hendy found it difficult to come to terms with how any of this could have happened. In his view, it was preventable; all the signs were there but nobody was paying attention to them. Stephen Newton’s previous 4 Enabling people to reach their potential. Fast forward to September 2012 and Julian Hendy is preparing to stand in front of an audience, primarily made up of AWP staff, for an event called Violence, Anxiety and Coping. It seems strange to see him here, shaking hands and talking with people that he had been desperately trying to get answers from for so long. It was at this event that he agreed to talk to Ourvoice just as soon as schedules would allow. November arrives and so does a space in his hectic diary… JH: I was surprised there was no contact from AWP to the family of the victim, even if just to say “We’re here” so I was very affected when I found out much later that, within days of the incident, the Trust had sent condolences to the perpetrator’s family but hadn’t bothered to contact me or my family. I since understand why that was the case and that unfortunately it isn’t all that unusual. I also understand that there are times when there’s no way that incidents like this can be prevented. But all too often it appears these are accidents waiting to happen. I was particularly affected by going to Brixton prison where we made a film about mentally disordered “When my father was offenders OV: Back when going through the justice we spoke at killed I had, in the most system and the event in how many of September, I fundamental way possible, them were said you’d be ending up forgiven for s to question those feeling there rather running a mile than hospital; from having and beliefs.” that didn’t do anything more their health to do with a very much trust that you good. I genuinely thought they were found yourself completely at odds some of the most tortured [through with. And yet, there you were, the their illness] people I’d ever met and keynote speaker... Why did you feel my heart went out to them. able to do that? OV: You certainly didn’t have any axe to grind then...? JH: Certainly not! I’ve had friends that have gone through their own mental health problems and I certainly didn’t feel it was anything that should be hidden or ashamed of. When my father was killed I had, in the most fundamental way possible, to question those feelings and beliefs. What I began to realise is that, particularly in mental health care, there seemed to be a real problem with learning from previous incidents. I appreciate the difficulties; we’re not making tins of beans, we’re dealing with people who are undergoing emotional crises. OV: Did you feel then, after your father was killed and you were starting to deal with AWP, that you and the Trust were on either side of a chasm of understanding? There was no common ground? OV: But if we accept this view of things, what is it that brought us to this point? Is it the rights of service users being put before anything else? Bureaucracy? What’s your view? JH: Patient confidentiality is obviously important but…we don’t need all the details of a patient as sometimes the bare bones is enough to inform or raise the point that there may be a particular risk to others. To also be mindful of the rights of the people who may be affected is not a bad thing. This is why I agreed to speak at the event, because I felt I had a point of view which wasn’t often heard. OV: Are you pleased you attended the Trust conference? Does it feel like the right thing to have done for you? JH: Yes, definitely. I know it was a one-off or pilot event but I’d be keen to come along to another one. If I can help to inform discussions amongst professionals, to try and stop this from ever happening again, then it’s worth it. Julian has created a web site which offers information and support on the issues surrounding serious mental illness and violence www.hundredfamilies.org JH: Part of it was that I felt I had no option but to be there! I follow the Press regarding mental health and it concerns me that there’s a message coming across about violence and people with a serious mental illness that’s exceptionally one-sided. There’s a fear that addressing that will lead to increased stigma against people with mental illness and I think that’s misguided. If someone with serious mental illness is left untreated then the consequences could be another horrible incident which, in my view, could create more stigma. I think if you treat the [causes of] violence you treat the stigma. I’ve seen all these anti-stigma campaigns – and I support them – but they do seem to concentrate on essentially “well” people, rather than those people I see on the street with serious problems, who appear to be off their medication and in a lot of distress. Empowering people to live fulfilling lives. 5 feature feature The Mysterious World of AWP Welcome once more to our mysterious world. This time we meet Chris Wall, Care Home and Community Hospital Liaison Nurse (BANES), and owner of an award-winning facial feature… Where are you right now? I am at my desk at Bath NHS house adopting the RiO position. Can you describe your job in twelve words? Care Home and Community Hospital Liaison Nurse in Banes busy but enjoyable. That’s some fine facial topiary you have there, Chris. How long has it taken to reach this point? I started flirting with facial hair a few years ago, around the same time the charity Movember started. I decided to keep the ‘tache after Glastonbury festival in 2011. It hit a few snags early on with wild trims and an incident with a flaming cocktail but I started to look after it properly in the last year. And you’re officially Moustache of the Year 2012…? Yes! The British Beard and Moustache championships is a bit like Crufts but for facial hair. You wouldn’t believe the different categories, they range from sideburns, full beards and moustache styles. The category I won was the ‘natural’ moustache which meant no styling aids such as glues or waxes. The competition was extremely high, some of the guys take it extremely seriously. The judging criteria is always a closely guarded secret so I was even more surprised that I had won. Stand by for actiON It may not exactly be International Rescue, but our staff are every bit as ready to cope with a crisis as the fictional Thunderbirds team. AWP’s Resilience Manager, Chris Williams picks up the story. It’s not unusual at the start of any incident, for a little bit of doubt to creep in, and you may ask yourself, ‘Am I over-reacting, should we do anything, should we wait to see what happens?’ Taking decisive action is often better than delaying a response otherwise you may find yourself playing catch-up. With the recent flooding of the Elmham Way site in Weston-superMare, service users had to be evacuated so local staff advised the service users’ next of kin that they were safe, were being relocated, where they were and how to contact them. Thanks to the calm professionalism of our staff, along with those of our maintenance contractors Rydon, and the emergency services, the problem at Elmham Way demonstrated that when the right procedures are followed, events can be rapidly and effectively resolved. 6 Enabling people to reach their potential. Do you have any hirsute heroes? Not really. I’m too young to have appreciated the likes of Jimmy Edwards or even Tom Selleck, for that matter… I’m going to give you £50,000 taxfree. What are you going to spend it on? I would spend it on helping my family, in particular my three-week old daughter Lily. Time’s up! Driven and determined Last year Bristol specialist drug and alcohol service (BSDAS) recruited 12 volunteer peer mentors to support and motivate fellow service users, using their own experiences to reduce fear and give hope. A year on, four from the original group (most have moved on to studies or employment) have worked with Gareth Sharman, BSDAS service user involvement worker, to train 17 new peer mentors. Lisa I did my rehab in prison. With different lengths of sentence not all women prisoners are psychologically ready to actually make changes and they keep going back in. Support from a peer mentor while they’re there could be really valuable. On graduation day the positivity and enthusiasm were almost tangible. The volunteer peer mentors are all BSDAS service users who have overcome huge challenges in their recovery journeys. Listening to their stories it is evident that many of them hadn’t believed it would be possible to get to where they are. Now they want to help others make similar achievements. Marcus I had a problem with authority but peer mentors would have helped get me in the right place. I didn’t realise there was a solution to the destructive situation I was in and for I while I thought ending my life would be the easiest thing. Now it is nice to be on the other side and to ‘be present’, and I think I can use my experience to help others. Helping brings me out of myself. I owe it to myself and to the people in BSDAS. I feel passionate about this. Ellie This has been absolutely brilliant and a great opportunity to talk to doctors and psychologists. I want to help other women in a similar situation. I want to give them hope about their children and the opportunities that are out there for them. Peer mentors fill the middle ground between service users and the authority figures of doctors, nurses and social workers. Sean As one of the original peer mentors, it was very useful to take part in the training. The role has evolved so it was slicker and more focused this time. Being a peer mentor has made me realise that, with the benefit of hindsight, I would have chosen a very different path in life. I can honestly say I get more out of being a peer mentor than I ever got out of my previous career. Wayne Facing rehab can be very scary so I’m hoping to meet people early in their contact with SDAS. I look forward to using what I’ve learned on the training – it was extremely interesting, useful for life as well as for being a peer mentor. Gareth Everyone on the training has been positive and passionate and they are providing a huge range of experience that we can match to the situations and needs of service users. The peer mentor programme is about two things: helping people progress through treatment, and our peer mentors continuing their own recovery. I’m looking forward to witnessing their achievements with service users but also their personal progress. Taffy I see the peer mentor role as about being there, supporting someone, using my experience to help someone else get well. People have a fear of the unknown, they don’t know what will happen during treatment. Talking to peer mentors could kill a lot of the fear. If I can stop one person from going where I went I will be happy. “I see the peer mentor role as about being there, supporting someone, using my experience to help someone else get well.” Empowering people to live fulfilling lives. 7 feature feature A chilly early morning in autumn. As per directions from 3 THE recovery support an inner city block of flats. worker Grace Weatherburn, I park outside high metal gate, our fingers Following Grace under a railway arch to a n. Then I catch my first glimpse are almost too numb to wrestle the lock ope : of the magical place I’ve been invited to see SECOND INTERVIEW to do anything like this before. I love that I can try things out, do a bit of digging, have a cup of tea, dig some more.” by Lucy Robinson Lisa agrees with Rob’s sentiments. “It is great to be involved in something that gives me a bit of structure, something to look after. I feel good after being here, buzzing from the fresh air. It’s really good to genuinely care about something and to watch it progress – and to sit by an open fire with a cup of tea and a biscuit. It would be great to maybe keep bees or a few chickens here in future.” This extraordinary 1.3 acre recovery project was established by drug and alcohol service users five years ago in a hidden river valley. Once the site of a market garden, the site was derelict when co-founders Paul and Terry secured it from Bristol City Council. The site has evolved into an enchanting series of sculpture-dotted gardens, ponds, seating areas, workshops and a hut complete with sofas and woodburner. Everything including the quirky composting toilet has been handmade on site from recycled materials. Reused signs are ironically amusing (‘please keep off the grass’) and useful (the ‘stop/go’ sign on the path to the toilet). Described by Paul as a missing link for people in recovery, the Haven provides something other than conventional group work and therapy. Penny adds, “The Blackberry Centre raised £37 with a ‘wear your wellies to work’ day and Viki is planning a sponsored bike ride. We are so grateful to everyone. But we need donations of seeds, plants and gardening equipment as well – not to mention tea, coffee and biscuits!” This year a group from SDAS’s Bristol and South Gloucestershire recovery drop-ins took on a plot within the Haven, supported by Grace, Penny Stanbury, Viki Bakehouse and Kim Hewlett. The SDAS group is creating a wildflower bed, pond and vegetable plots divided by a mosaic path. Eventually they hope to sell produce and chutneys at a farmers’ market. Haven participants, importantly, are not volunteers, but instead ‘owners’ of the project. There are some basic rules but the project is hierarchy-free albeit under the caring eye and gentle guidance of Paul and Terry. Open to all each Tuesday and Friday, people can wander or sit, but most garden or create. Thursdays, led by artist Julia, are for women only. Showing me progress on their plot, Grace explains, “The Haven manages with almost no money, relying on donations and Paul and Terry’s ingenuity. But we need funds to support the project and to develop our plot; we are really lucky to have contributions from Bristol and South Gloucestershire specialist drug and alcohol services.” 8 Enabling people to reach their potential. The benefits are many and varied. But as the gang sips tea and bounces ideas around, I realise they are all learning one very valuable lesson: it is okay to try things, make mistakes and learn from them. There is no right or wrong way of doing things at the Haven and that is one of the keys to its considerable success. By now my fingers are so cold that I can no longer write so Paul and BSDAS service users Rob, Lisa and Tim join us for a warming cuppa in front of the wood burner. “I love coming here,“ says Rob several times. “Paul was my befriender at Second Step so I’d heard of the Haven but I only came when Grace suggested it. I look forward to it every week, it’s something I can commit to. I’d never been offered the chance You can now follow Grace’s online ‘Haven diary’ via the links at www.awp.nhs.uk/ Who has time to talk these days? Consultant Psychiatrist at Beechlydene Dan Meron does but only for 30 seconds! Your time starts now… Q: Describe your most productive day so far this week. We take pride in our close working with the home treatment team to shorten hospital admissions which means we have a high turnover of patients on the ward. Each Monday I meet a whole new ward of people and new families. At the end of the day we are shattered but with a great feeling of having helped a lot of people. So Monday is always my most productive day – but closely followed by Tuesday. And Wednesday. Q: Who has made you laugh today? You! My children – they always make me laugh. And my dog. They are a massive part of my life. Q: If you weren’t working right now what would you be doing? Kite surfing badly in Poole harbour. Recovery drop-ins Colston Fort recovery drop-in: every other Thursday, 2pm-4pm. Contact Penny 0117 923 2077 or Grace 0117 919 2310. Blackberry Centre recovery drop-in: last Tuesday of the month, 3pm-4.30pm. Contact Viki 0117 378 4500. Q: If you could swap jobs with anyone in the world, who would it be? I don’t think there’s anyone I’d swap with… although I’d trade with Arden Tomison for a week to see what challenges a medical director faces. Q: What’s the best thing about your job? I’ve wanted to be a doctor since I was 12 years old. It’s never the same from moment to moment. I work with really interesting patients, I get to work with really great people – service users, their families and colleagues – in a lovely city. Life is good. Time’s up! Opposite: l-r: Lisa, Grace, Penny, Paul & Rob. Photo by Tim. Above: Tim, Penny & Lisa. Photo by Tim. Empowering people to live fulfilling lives. 9 feature feature In essence... All of me Pictured: Lou, Ben & Teagle How can “spiritual assessments” give us a fuller picture of the person under our care? And how will staff be supported to carry them out? AWP chaplain Rev. Michael Belfield discusses the need for H.O.P.E. With AWP ‘energising for excellence’, the Essence of Care team have been hearing about good practice from across the Trust. Ben Padfield reports… Essence of Care is an initiative which is for use by us all to get at the heart of what we do. It aims to value and improve communication, respect and dignity, our care environments and our standards of food and drink. It involves gathering service users’, carers’ and staff perspectives on care, (both giving and receiving), in order to set standards and recognise areas of best practice. So what better than to share some of that best practice with everyone reading Ourvoice? Working Together: Natalie Davenport in North Somerset, ran her Essence of Care project across Natalie Davenport inpatient and community settings to increase efficiency and to develop a culture of self-assessment and improvement for staff. Service users reported that the transition from home to hospital and back was smooth, and that the standard of care was consistently high at all times. Nikki Hobbs ‘diabetes-friendly’ Talking & Listening: and ‘no-hassle’ In Bristol, service user (for individuals representative Lou with limited Winstone worked with cooking skills or inpatient staff to develop facilities). guidance around one to one interactions. This Teams and service insight into service users’ users have used experiences continues Essence of Care to ‘think outside the to support staff to question their box’, bringing their creativity and practice and enhance their talking and imagination to the improvement listening skills. New staff members and process. In central Bristol Nikki Hobbs students have welcomed having direct used therapeutic activities to gather access to service users’ experiences in a service user opinions, including a busy acute ward. tombola of service-improvement ideas, where prizes were given for the Meaningful Activity: most inventive, the most comical and Lou Curtis and Pete Aston in Bath the most forward-thinking. started running nutrition and Improving care is something we all do wellbeing workshops for service users, as part of our day to day work, and involving cooking, physical exercise it is not limited to registered nursing and relaxation. Taking account staff. So if you are a student or an of feedback, nurses and OTs have HCA, why not use Essence of Care to teamed up to offer creative activities, celebrate the good stuff in what including ‘al fresco’ mindfulness we do? and meditation sessions with a Buddhist nun. Managing the Menu: Simon Hall’s early intervention team in Wiltshire used service user feedback to offer community food boxes matched up to individuals’ needs and preferences. Types of food box included ‘vegetarian’, 10 Enabling people to reach their potential. For more information, colleagues can search ‘Essence of Care’ on Ourspace. “It’s the great British reserve,“ Michael Belfield explains. “We never talk about sex, money, politics or religion!” That old line is about to be challenged as it’s become clear that finding out about the whole person can help us understand and support them during times of mental health crisis. AWP has recently launched H.O.P.E. – H= sources of Hope, O= Organised religion, P= Personal practice, E= Effects on care – a spiritual assessment tool aimed at understanding more about the service user. “We have moved on from asking service users simply what their religion is; ‘religious’ describes the organised worshipping faith, while ‘spiritual’ is the personal – it is about those things which give meaning and value and purpose to someone’s life,” says Michael. “H.O.P.E. assists in finding out what we can do to help identify those things that really matter to a person while they are in our care. It is about helping them to feel human rather than just ‘a patient’ or service user.” a prayer mat. Having these items helps him practise his faith but the strength comes from the faith itself and not from the mat or the book.” H.O.P.E. is intended to be a conversation between staff and service user, not a set of questions. Understanding if a person has any faith or spirituality and what that means to them will be an ongoing process and there’s no intention of bombarding service users with surveys the minute they arrive. Michael stresses that, while some training will be put in place for nursing staff, they won’t be expected to work as experts in a multitude of faiths and beliefs: “Nobody is expecting our colleagues to do anything more than understand a little more about an aspect of the person they will be talking with anyway. “How they then use that information to support a service user better is what will make a great difference.” You can find further information about using H.O.P.E. by visiting the RiO Clinical Manual (wiki) and finding Spirituality under Assessments. But what will we find out by using this tool, and what difference could it make to service users and staff? The first, crucial point is that this is not about ticking boxes; it’s about what makes people tick: “It should be about spiritual strengths as well as needs and those two things may be linked,” Michael says. “As an example, a Muslim patient’s spiritual strength is his faith in Allah, but his needs may be for a Qur’an and Empowering people to live fulfilling lives. 11 The achievers Congratulations to the following colleagues for passing their courses and exams. Tracy Smith, HCA, Fromeside. Achieved NVQ in health and Social Care level 3 Rebecca Parkhill, Administrator, North Bristol Recovery team. Achieved NVQ in Business and administration level 3 Joanna Humphries, PA, North Bristol Assertive Outreach team. Achieved NVQ in Business and administration level 3 Rachael Burfitt, PA, Prison drug service. Achieved NVQ in Business and administration level 3 Gillian Bailey, Administrator, CJIT Bristol. Achieved NVQ in Business and administration level 3 NVQ in health and social care achieved August 2012 Stacey Bennell, Administrator, LLLS Management team, BBH. Achieved NVQ in Business and administration level 3 Claire Hutton, Senior Administrator, L & D team, Woodland View, Brentry. Achieved NVQ in Business and administration level 4 James Adams, Administrator, L & D team, Woodland View, Brentry. Achieved NVQ in Business and administration level 3 Alison Weerawardena, Administrator, BBH. Achieved NVQ in Business and administration level 3 Shelley Smith, Medical Education Administrator, Woodland View, Brentry. Achieved NVQ in Business and administration level 3 Missed an issue? Don’t worry! We know how annoying it can be to miss an issue of your favourite magazine, especially one which features the people you know and work alongside. But don’t despair as we have a small stock of back issues of Ourvoice, including the very first published when it was called ‘Name Me’. It must be a collector’s edition by now… If you prefer to read them online you can now find them on our website. Search ‘Ourvoice’ on www.awp.nhs.uk and you can catch up on all your favourite features. Published: December 2012 Editor: Simon Gerard AWP communications team Email: [email protected] Trust Headquarters Jenner House, Langley Park Estate, Chippenham, Wiltshire SN15 1GG Telephone: 01249 468 000 www.awp.nhs.uk Printed on FSC approved paper using vegetable inks Story for the next issue? Email: [email protected] using subject header ‘story’. Designed by: Ice House Design – Bath
© Copyright 2026