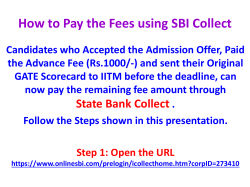
SESLHD MHS PROCEDURE COVER SHEET
SESLHD MHS PROCEDURE COVER SHEET NAME OF DOCUMENT Patient Flow Operational Framework for Mental Health Service TYPE OF DOCUMENT Procedure DOCUMENT NUMBER SESLHDPR/245 DATE OF PUBLICATION March 2013 RISK RATING Medium LEVEL OF EVIDENCE N/A REVIEW DATE March 2016 FORMER REFERENCE(S) SESIMHS Patient Flow Operational Framework 015_10 EXECUTIVE SPONSOR or Dr Murray Wright, Director, SESLHD Mental Health Service EXECUTIVE CLINICAL SPONSOR AUTHOR Gayle Jones, A/ SESLHD MHS Access & Service Integration Manager POSITION RESPONSIBLE FOR THE DOCUMENT Gayle Jones, A/ SESLHD MHS Access & Service Integration Manager KEY TERMS Patient flow; access management; demand management; mental health access SUMMARY This document provides a framework for standardised patient flow operations in SESLHDMHS. Standardised operations aim to enhance mental health patients‟ experience and outcomes and as such this document should be used a s a reference tool by mental health staff. Feedback about this document can be sent to [email protected] SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Table of Contents Introduction and Background…………………….………………………………… 2 SESLHD MHS Geography……………………………………………………………. 3 SESLHD MHS Inpatient Facilities……………………………………………………. 4 Patient Flow Coordination The Role of the Patient Flow Coordinator………………………………………….. 6 PFC Communications Schedule……………………………………………………. 7 Capacity/Demand Profile Reports……………………………………………………. 8 LLOS Meetings, Second Opinion Policy, Demand Planning………..…………… 9 Weekend Demand Planning………………………………………………………….. 10 Collaborative Patient Flow Operations The three R‟s of Patient Flow………………………………………………………. 11 Over Census / Over Numbers……………………………………………………… 12 Collaborative Patient Flow, After Hours Patient Flow …………………………… 13 Accepting Referrals of Patients for Mental Health Admission……………………. 13 Transfer of Care …………………………………………………………………….... 15 Repatriation of Out of District Patients – Establishing Catchment Area………….. 16 Repatriation Negotiation / Requesting Transfer to Alternate Facility..………..….. 17 Repatriation within SES LHD MHS, within NSW, Interstate and International……. 17,18 Inter-hospital Transfer Algorithm…………………………………………………… 19 Transport………………………………………………………………………………. 20 SESLHD MHS Priority Transport Options……………………………………………. 21 Referral to/from Private Hospitals…………………………………………………….. 22 Referral to Rehabilitation Services…………………………………………………. 23 Referral to Bloomfield Rehabilitation Services, Drug and Alcohol Services…… 24 Special Needs Referrals……………………..…………..………………………..….. 25 Appendix 1 - Useful Numbers……………………………………………………….. 26 Appendix 2 – Escalation Algorithm………….…………..………………………….. 27 Appendix 3 – Referral to IPCU/ MHICU Facilities Algorithm……………………..... 28 References and version control ……………………………………………………… 29 Revision 0 Trim No. T13/5626 Date: March 2013 page 1 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Introduction and Background This document provides a framework for standardised, district-wide, patient flow operations in South Eastern Sydney Local Health District Mental Health Services (SESLHD MHS). The framework applies to the management of operational patient flow for patients in SESLHD MHS and for patients who are being transferred to or from SESLHD MHS. Aims Standardised patient flow operations aim to enhance mental health patients‟ experience and outcomes and as such this document should be used a reference tool by all mental health staff. Patient flow is a dynamic process not limited to business hours and this framework provides consistency of patient flow operations within and outside of business hours. This framework complements the processes outlined in the NSW Health Mental Health for Emergency Departments – A Reference Guide 2009. Target Audience The framework is aimed at Sector Service Directors (SD), Clinical Operations Managers (COM), Inpatient Service Managers (ISM), Nursing Unit Managers (NUM), Patient Flow Coordinators (PFC), Nurses in Charge (NIC), Registrars and Consultant Psychiatrists and all other mental health staff involved in the patient flow process. Patient Flow Philosophy The Garling Report (2008) identified the link between efficient use of inpatient beds and improvement in the quality of care provided to patients.* Persons requiring mental health inpatient care should receive timely and efficient access to the best possible care available. The core principle of patient flow is to provide sustainable access to inpatient beds and is identified as a State-wide standard. Consideration must be given at all times to ensure that people with a mental illness or mental health disorder “receive the best possible care and treatment in the least restrictive environment enabling the care and treatment to be effectively given", NSW Mental Health Act 2007. What is Patient Flow? „Patient Flow‟ refers to the patient journey through a health service, in this instance the SESLHD MHS and predictable. SESLHD MHS operates at or near 100% bed occupancy most of the time therefore daily transfers of care out of mental health inpatient services must be planned to accommodate predicted daily admissions. Most admissions occur via the Emergency Department (ED). To achieve this KPI all patients requiring mental health admission should be transferred to an appropriate facility as soon as assessment and/or treatment processes are completed. It should be noted that some venues such as Prince of Wales (POW) Mental Health Service have points of admission that may bypass ED. For example Police / Community Mental Health Team (CMHT) presentations and patients sent directly from courts or prison for assessment can be transported directly to the Kiloh Centre. Multiple points of admission make patient flow coordination more complex and heighten the need for predictive and collaborative transfer of care planning around the clock. * Final Report of the Special Commission of Inquiry Acute Care Services in NSW Public Hospitals Overview Peter Garling SC 27 November 2008, Pg. 30, (1.193) Revision 0 Trim No. T13/5626 Date: March 2013 page 2 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 SESLHD Geography hern Network Central Network SESLHD Hospital and Health Service Sectors (*Mental Health Inpatient unit/s on site) (+Mental Health assessment service in ED) Northern Sector Prince of Wales Hospital*+ Royal Hospital for Women Sydney Hospital Sydney Eye Hospital Southern Sector St George Hospital*+ The Sutherland Hospital*+ The Garrawarra Centre Southern Network Revision 0 Trim No. T13/5626 Date: March 2013 page 3 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 SESLHD MHS Inpatient Facilities Site Prince of Wales Hospital St George Hospital Sutherland Hospital Acute Mental Health Inpatient Units (MHU) Name Total beds Bed Configuration Kiloh Centre 50 20 x observation, 30 x general acute MHU 28 Mental Health Inpatient Unit 28 9 x observation, 19 x general acute including 6 SMHSOP beds 10 x observation, 18 x general acute Most MHU‟s provide both high-level acute (observation) and general acute care when community treatment is not possible due the patient‟s clinical condition. MHU‟s are declared under the NSW Mental Health Act 2007 (MHA) to accommodate people who are acutely unwell and require involuntarily treatment and care. Psychiatric Emergency Care Centres (PECC’s) St George 6 PECC beds Prince of Wales 4 PECC beds PECCs provide rapid access to mental health assessment and short stay admissions up to 72 hours. Patients referred to PECC must have a clearly defined admission / transfer of care pathway documented including the plan and expected date of discharge from hospital (EDD). Patients must have a manageable level of risk in all domains including suicide, self harm, aggression, sexual safety and absent without leave. Admissions are direct from the ED following mental health assessment and authorisation by the Medical Superintendent or delegate. Appropriate patients may be transferred from an acute mental health inpatient facility to PECC and on occasion at some facilities may be admitted direct from the community to PECC. Site Prince of Wales Sutherland Mental Health Rehabilitation Units (MHRUs) Name Beds + Configuration MHRU 14 non acute beds - non-declared MHRU 20 non acute beds - declared Several Mental Health Rehabilitation Units (MHRUs) are also available in SESLHD. These non-acute facilities provide a range of programs to support patients to develop or regain skills for living independently or in supported accommodation. Where capacity exists during times of peak bed demand a MHRU bed may be considered as a temporary venue for limited number of „transition‟ patients from an acute facility. Careful consideration should be given to the use of MHRU beds for this purpose due to the disruption to patients involved. Wherever possible, patients who have already been referred to and/or are awaiting a MHRU bed and who have minimal risk factors should be considered. MHRUs may also provide venue for completion of Clozapine titration for suitable patients. Revision 0 Trim No. Date: February 2013 page 4 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework Site Prince of Wales St George Sutherland SESLHDPR/245 Specialist Mental Health Service for Older People (SMHSOP) – acute Configuration Name Total beds Euroa 6 (declared)beds + 2 Neuro-Psychiatry beds (non declared) MHU 6 allocated within the MHU (declared) MHU 6 allocated within the MHU (declared) SMHSOP provides specialist mental health assessment and treatment for older people with acute mental illness. Patients with a primary organic or physical health condition leading to disturbed behaviour are generally outside the referral criteria for SMHSOP. Where capacity exists SMSHOP beds may be considered during periods of peak bed demand as temporary venue for limited number of „transition‟ patients from an adult acute facility. This strategy should only be used at times of peak demand and after all other strategies to increase acute bed capacity have been exhausted. In general only patients who are close to the admission age and with minimal risk factors should be considered for transition placement. Tertiary Intensive Psychiatric Care Units (IPCU or MHICU) Hornsby MHICU Northern Sydney Central Coast Area Health Service Cumberland IPCU Sydney West Area Health Service Concord IPCU Sydney South West Area Health Service SESLHD MHS does not currently have an IPCU/MHICU planning has commenced for a 12 bed facility to be commissioned January 2013. SES shares access to tertiary IPCU / MHICU beds in the facilities above with all other Local Health Districts in NSW. See Appendix 3 for Referral Algorithm. Tertiary Child & Adolescent MHS Inpatient Units (CAMHS) – acute Shellharbour Acute Shellharbour Hospital beds Gna Ka Lun Acute Campbelltown Hospital Redbank House Acute, incl Child & Family Westmead Hospital Nexus Unit Acute John Hunter Hospital Sydney Children’s Acute - non declared Randwick Hospital Campus The 8 beds available at Sydney Children‟s Hospital are not declared under the Mental Health Act 2007(MHA) so are unable to accommodate patients detained involuntarily. SESLHD MHS can make referrals to the declared tertiary CAMHS beds listed above. Revision 0 Trim No. Date: February 2013 page 5 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Patient Flow Coordination The Role of the Patient Flow Coordinator (PFC) The PFC is the central point of contact for information and access to Site/Sector mental health beds in SESLHD during business hours Mondays to Fridays. After hours and on weekends, the role is delegated at each site for continuity of patient flow coordination. More details about after hours coverage is provided on page 13. Northern Sector Southern Sector PFC Contact Numbers Prince of Wales St George / Sutherland Ph: 0411 653 463 Ph: 0411 658 967 The core responsibility of the PFC is to be aware of current capacity and demand within their sector at all times. Capacity refers to the number of mental health inpatient beds physically available to accommodate patients requiring admission. Demand refers to the number of patients from all sources (including ED, Police, Community Mental Health, other inpatient services and other MHS) that require admission at any given point in time. To remain abreast the PFC must review relevant databases, attend clinical meetings and liaise continuously with NUMs, ED clinicians, inpatient clinicians, Community Mental Health Teams (CMHT) and peer PFCs (general and MH) to collect information such as: Number of patients physically present on the unit(s) Number of patients on leave and for how long Patients absent without leave (AWOL) and whether they are expected to return and if not, when the bed will be confirmed as available Patients in ED awaiting assessment and/or likely to require admission CMHT patients being assessed and likely to require admission The PFC records capacity/demand details in twice-daily Profile Reports (see page 8). Updates are sent to clinical teams, District MH Access & Service Integration Team, Site/Sector MH Executives and other relevant stakeholders as required. PFC’s should be especially alert for: Avoidable admissions – ensuring admissions are consistent with the principle of least restrictive care as outlined in the MHA, 2007. Out of District patients requiring repatriation to their local MHS. Patients with private health insurance who may be transferred to a private facility. Barriers to transfer of care or leave for a patient who is otherwise clinically ready. Patients suitable for referral to Acute CMHT, MHRU, inpatient drug and alcohol services, NGO supported accommodation (such as NEAMI) or general aged care services. Revision 0 Trim No. Date: February 2013 page 6 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Patients awaiting CTO hearings that could be placed on leave pending the hearing. Planning for discharge and transfer of care is initiated as soon as possible after admission, including the allocation of an estimated date of discharge (EDD). The PFC has a key role in tracking the patient journey. By attending daily ward and multidisciplinary team (MDT) clinical meetings, the PFC maintains awareness of all patients‟ progress and can facilitate the removal of any non clinical barriers to transfer of care such as accommodation, transport, or social issues in collaboration with the NUM, MDT and others. Patient Flow Coordinator Communication Schedule The aim of this PFC communication schedule is to ensure timely and regular exchange of information between the Sector PFC and the District Access & Service Integration Team. Ad hoc communications includes challenges to patient flow as they occur, e.g. access blocked patients in the ED, other issues enquiring escalation. Time 0830 0930 1100 1200 1400 Monday Tuesday Wednesday Thursday Friday Sat/Sun Email AM Profile Report to District Access & Service Integration Manager Verbal, email or SMS update of ED Demand and placement plans 1100 MH Site Manager on-call Telco with District Executive on-call Verbal, email or SMS update - pt flow challenges Email Weekend Demand Plan 1500 1530 1550 1630 District MH Access & Service Integration Manager provides briefing & service overview to District Risk Manager and District Director SES LHD MHS on request Email PM Profile Report to District Access Team Manager Verbal, email or SMS update of any significant variance from 1530 report Close of Business 0830 0930 Verbal, email or SMS update from morning meetings District MH Access Manager Telco with District Patient Access team: Provide specific overview of Site Self Sufficiency / Placement Plans for ED Admissions Time 1200 1400 1500 1500 1530 1550 1630 Revision 0 Trim No. Date: February 2013 page 7 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Site/Network Capacity/Demand (Profile) Reports Sector profile reports are collated by PFCs and published at 0830hrs and 1530hrs daily via email to: Site Registrars, Consultant Psychiatrists, Team Leaders, MH Executives, NUM‟s, Allied Health, General Hospital Executives, District Risk Manager, District Access & Service Integration Team. The reports are a summary of current Site/Sector capacity and demand. In line with NSW Ministry of Health protocols the profile reports also indicate predictive patient flow for the next 24 and 48 hours. See sample profile report below. Revision 0 Trim No. Date: February 2013 page 8 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Long Length of Stay (LLOS) meetings Long Length of Stay (LLOS) meetings are held weekly or fortnightly to discuss patients with length of stay in the MHU of greater than 28 days and in MHRU for patients reaching length of stay thresholds of 100, 150 and 180 days. Meetings should be attended by the Chief Psychiatrist, Social Workers, CMHT Team Leaders, NUM, ISM, Clinical Operations Manager, PFC and District Access and Service Integration Manager. Representatives from the District MH Rehabilitation Team attend the MHRU LLOS meetings. Patients are discussed from a MDT and holistic perspective, aiming to remove any barriers to transfer of care or leave. Second Opinion Policy The SESLHD MHS Policy Obtaining a Second Opinion from a Consultant Psychiatrist 2007/06 v5, outlines the length of stay thresholds for obtaining a second opinion: LOS >28 Days LOS >49 Days LOS >75 Days Thresholds for Obtaining a Second Opinion Flexible format, may seek opinion from another Consultant Psychiatrist within the unit or within the service Second opinion and face to face review to be sought from the Chief Psychiatrist / Medical Superintendent. Review may be conducted by the Chief Psychiatrist / Medical Superintendent of the treating facility or another facility Automatic referral to Complex Care Committee The thresholds should be routinely reviewed during LLOS meetings and action to obtain a second opinion initiated if required. Demand Planning The aim of demand planning is to maximise the use of mental health inpatient beds using a non-reactive, predictive approach to patient flow. The District MHS Access & Service Integration Manager is using historical data to generate Demand Prediction figures. Data is based on previous three month discharges and EDD as entered into the NSW Health Patient Flow Portal. The figures should guide Site/Sector planning to enable mental health beds to be available as required. Proactive and predictive planning ensures site self sufficiency and reduces waiting time for patients in ED. Revision 0 Trim No. Date: February 2013 page 9 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Weekend Demand Planning As with patient flow and demand planning in general, weekend demand planning strengthens site capacity, maintains self-sufficiency and minimises reliance on neighbouring services over the weekends. Local site sufficiency plans are documented on the Weekend Demand Plan (WDP) template below to ensure sufficient capacity in line with predicted weekend demand. Venue PECC Planned D/C JB Saturday/SundayMonday Planned Possibility for D/C or Leave & Leave Return Date Planned D/C Planned Leave & Return Date Possibility for D/C or Leave Total Obs Unit Issues Possible Suitable for Sub Acute, PECC, MHRU, OPU transfer? M S – to PECC OOA's / Outliers for repatriation FM 6/7 4 JB awaiting crisis accommodation ME to OPU JC 2 Issues Endorsement Endorsed by: Site Executive or delegate and Medical Superintendent or delegate. Additional Resources to be accessed in cases of surge demand Distribution List Distributed to: Weekend CNCs, On call Execs, On call Registrars and Consultants Deployment of additional ward staff Consultant on notice to attend facility in person to assist in reviewing patients on ward and/or in ED ACT/CMHT on notice to attend facility to assist in identifying ward patients for potential leave/DC with intensive community support The WDP flags those patients confirmed for leave or transfer of care over the weekend and identifies their expected day/time of departure. The WDP records the patient‟s full name, whether their care is being transferred or they are going on leave. If going on leave the WDP identifies when they are due to return. Any issues that may impede leave or transfer of care such as accommodation or transport issues are also highlighted. Site self sufficiency is essential for efficient patient flow on weekends. The WDP identifies patients who can be temporarily and safely transferred at times of peak demand to venues such as MHRU, PECC or SMHSOP Units should capacity be available. The WDP also identifies patients who may be considered for transfer to alternate SES MHUs, MHRU‟s, PECC‟s or SMHSOP Units should local capacity be unavailable. The PFC prepares the WDP in collaboration with the NUM and MDT and has it signed off by a representative of the site mental health executive. The WDP provides a reference tool and enhances communication for weekend staff including after hours clinical teams. The WDP is displayed in each MHU and is emailed to the weekend site on call MH executive, on call registrar and Consultant Psychiatrist and the District MHS Weekend Access & Service Integration Team Manager. Revision 0 Trim No. Date: February 2013 page 10 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Collaborative Patient Flow Operations Patient flow is a collaborative process incorporating both operational and clinical bed management. Effective patient flow entails collaboration and co-operation between the PFC and MDT. The role of PFC is to „coordinate‟ patient flow in partnership with the MDT. The Three R’s of Patient Flow Remember the Three R‟s before recommending placement of a patient: Right Patient Consider the patient‟s presenting issues, age, risk factors, illness, physical health, gender, history and social supports – do they need admission, what is the purpose of admission, is the admission planned, what is the expected date of discharge from the inpatient facility (EDD)? Right Bed Consider the environment you are recommending placement into, ward acuity/patient mix, sexual safety risks, staffing resource issues, clinical skill mix, specialist medical and multidisciplinary services, relationships or history with other patients or staff, physical security of the environment (e.g. risk of absconding, falls risk). Right Time Consider whether the patient has any physical complaint which requires investigation and resolution prior to transfer, how does the patient feel about going to a particular ward, are there staff available to admit the patient, is transport available or additional escort staff available, has the bed become physically vacant (even if the bed is not yet physically available, the patient may, in an emergency, be moved to the unit while the bed is being prepared). It is important to note that admission or transfer should not be delayed for the sake of staff convenience e.g. meal breaks, clinical hand over for example. Mitigation strategies should be implemented to ensure patient‟s transfer is not delayed other than for safety reasons. Revision 0 Trim No. Date: February 2013 page 11 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Over Census / Over Numbers Over Census refers to the census report taken at midnight every night. There may be at times more patients listed as admitted to the unit than there are formal beds. As such the report seeks to capture the actual head count of patients at midnight and excludes patients on overnight or extended leave. In extreme and rare circumstances where SESLHD MHUs surge to over census capacity, the situation must be approved by the Service Director or delegate or the on call MH Executive after hours and additional staffing resources must be sourced. Over Numbers refers to circumstances where there are physically more patients than beds on a unit at a particular point in time. This can include: Patients returning from leave whose beds have been used. Day patients awaiting or recovering from ECT. Patients commencing Clozapine who are undergoing initial dose monitoring. Patients on the unit awaiting CTO hearing. Patients brought directly to the unit (eg Kiloh) by Police or CMHT awaiting assessment. Over numbers or over census admission can compromise patient care and place undue pressure on staff. The aim of efficient patient flow is to avoid over numbers and over census by anticipating demand and ensuring there is sufficient capacity to accommodate actual or predicted admissions. In the event that a MHU goes over numbers or over census the following actions should occur without delay: Inform the Duty Consultant Psychiatrist/ Registrar as soon as it is known that the unit will be over numbers or over census. Inform the site Executive or on call MH Executive after hours and District MH Access & Service Integration Team (within office hours). Discuss with the site Nurse In Charge (NIC) any patients who may be suitable for review for leave, transfer or discharge. Identify any patients who may be suitable for temporary transition placement in MHRU, PECC, SMHSOP Unit. Identify patients who may be supported by CMHT whilst on leave from the unit. Contact peer PFCs during business hours to establish alternate site bed capacity and seek assistance with alternate placement for suitable patient. After hours this may require direct contact with each facility. Over numbers/over census situations can be stressful and place teams under significant pressure. It is imperative for all parties to remain open and supportive and communicate transparently to preserve goodwill. Operational patient flow management is the administrative tasks associated with accessing a mental health inpatient bed and includes: Bed finding and/ or negotiations within and between services regarding bed availability. Revision 0 Trim No. Date: February 2013 page 12 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Repatriation and identifying suitable patients for clinical review, leave, transfer or admission to a private facility. Clinical patient flow and bed management involves the clinical review and decision making process to determine whether any additional acute beds can be made available including: Review of out of district patients / out of sector patients for repatriation. Review of patients who may be considered for transfer and admission to a private mental health facility. Review of patients on leave for extension of leave. Review of appropriate patients for early transfer of care with additional supports or overnight leave with acute CMHT follow-up. This includes reviewing bed allocations and transfer of care status of patients, status of patients on leave, voluntary patients requesting to have care transferred or patients who have supportive family and/ or community networks. After Hours Patient Flow Each site has a role designated to co-ordinate patient flow after hours (evenings and overnight including weekends). At times of peak demand t h e On-call Consultant Psychiatrists can support the patient flow process by advocating for access to alternate venues if needed e.g. by discussing assessment and management of an individual patient with the Consultant Psychiatrists on call at another hospital. Where site bed capacity is nil and Consultant Psychiatrist to Consultant Psychiatrist negotiation for alternate site placement has been unsuccessful, negotiations may be escalated to the on call MH Executive for peer discussion and resolution. The hospital After Hours Nurse Manager is another valuable resource for advocating and facilitating strategies to generate additional bed capacity after hours.The SESLHD MHS After Hours patient flow coordination contact list is below: Accepting Patients for Mental Health Admission Revision 0 Trim No. Date: February 2013 page 13 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 From ED Acceptance of patients for admission is a collaborative process between the Mental Health clinician assessing the patient in the ED, duty Consultant Psychiatrist / ED Consultant Psychiatrist or Registrar and the PFC or after hours delegate. Important factors to consider include: Is there a less restrictive alternative to admission? Can the patient go to a private hospital or drug and alcohol rehabilitation centre, be transferred to CMHT follow up, are they suitable for a brief PECC admission? Is there a documented admission plan? Has the patient had a physical health assessment clearing them for a MH admission? Has the medical assessment and treatment in ED been completed? To minimise the risk of medically compromised patients being transferred to a MH bed, the ED medical staff are required to document in the medical record that there are no further investigations or treatments pending subsequent to a thorough physical examination. Prior to patients being transferred from ED the patient must be de-cannulated, ECG leads removed (ligature risk) and extubated at least 24 hours previously. Is the medical record complete? MH-OAT Assessment module (A1), treatment plan for admission, medication chart including PRN‟s and depots, MHA original papers, blood pathology forms for example. Acceptance of patients for admission is also a collaborative process between the PFC and the MHU or PECC NUM or NIC. A patient may have been assessed as suitable for a sub acute unit for example but following clinical handover it may be apparent the patient requires placement on an acute unit. Negotiation must take place with the NIC to establish the time for transfer into the MH bed. There may be times when it is necessary for the NUM or NIC to defer transfer at a particular time due to acuity. Other factors include staffing resources. It is therefore essential for the PFC to maintain regular contact with the NUM or NIC to communicate information about Police / Ambulance / CMHT presentations, unit acuity and staffing, AWOL‟s, transfers of care and leaves. Direct Presentations When patients present directly to the unit with Police, Ambulance or CMHT it is imperative to assess whether they are intoxicated. An Alcolmeter is available on each acute unit to measure alcohol intoxication. Patients should be observed for evidence of other intoxication such as illicit or prescribed substances e.g. pinpoint or dilated pupils, high pulse / respirations. If a patient is found to be intoxicated they must be transferred to the ED immediately for monitoring and medical assessment. From General Hospital The Consultation Liaison (CL) Teams will inform the PFC of any patients in a general hospital bed awaiting Mental Health admission. The same criteria as per ED apply. It is imperative all medical investigations and treatments have been completed and the patient has been reviewed Revision 0 Trim No. Date: February 2013 page 14 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 by CL team for the least restrictive care option prior to transfer to MHU. Prioritisation for Admission When there are patients in the ED and General Hospital awaiting mental health placement at the same time, especially when bed capacity is limited, priority for placement should be negotiated with the hospital Patient Flow Manager in consultation with the Mental Health Clinical Operations Manager and Duty Consultant (or delegate) Transfer of Care Discharge from an acute care facility is not the end point in the continuum of care for most people accessing acute care services, hence, “transfer of care” is a term adopted by NSW Ministry of Health to demonstrate that care continues beyond the hospita l setting. In the context of Mental Health, transfer of care ensures the safe, effective and efficient movement of people with mental health problems between inpatient settings to the community or alternative care settings. T he decision to transfer c a r e o f a patient should be made by the MDT in consultation with the patient and carers wherever possible. Planning for transfer of care optimises the patient journey and ensures timely service. The section below is consistent with PD2011_015 Care Co-ordination: Planning from Admission to Transfer of Care in NSW Public Hospitals. On Arrival to the Inpatient Unit On arrival to the unit (or as soon as practicable) each patient should receive information on the Expected Date of Discharge (EDD) outlining expected date and time of departure from the unit / clinical area and the expectations around transportation. The Registrar under whom the patient is admitted should allocate and verify the EDD within 48 hours of admission, wherever possible. Within 48hrs of admission the EDD should be communicated to the MDT. The EDD should be based on the patient‟s presenting clinical signs and symptoms, historical length of stay, psychosocial and non-clinical factors that may influence length of stay where known. A transfer of care risk assessment should be conducted and the admission / transfer of care checklist commenced within 48hrs of admission. The EDD should be verified by the Consultant Psychiatrist at the patient‟s first MDT clinical review and the date relayed to the patient and family / carer as soon as is practicable. Each patient should be actively involved in their own transfer of care planning wherever possible. Prior to Transfer of care On the EDD the departure time from the ward should be no later than 1000hrs. Transfer of care medications should be ordered and stored in the clinical area at least 12hrs prior to 1000hrs on the EDD. Transportation bookings and arrangements should be confirmed within 24-48hrs prior to transfer of care. It is usually the patient‟s / carer‟s responsibility to arrange their transportation home, however exceptions can be made in consultation with the NUM / MH Executive, particularly if EDD will be unduly compromised. Revision 0 Trim No. Date: February 2013 page 15 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 All items on the transfer of care checklist should be completed prior to transfer of care, including notification of NGO‟s, case managers, GP‟s etc. Repatriation of Out of District Patients Establishing Catchment Area Establishing catchment area usually comes down to confirmed residential address. However, this can be unclear for a variety of reasons including: The patient has just been released from prison. The patient has been admitted directly from the airport. The patient is homeless. The patient has an AVO preventing them returning to their accommodation. The patient has a breakdown of relationship preventing them returning to their accommodation. When the address is unclear other factors may be taken into consideration to determine which catchment area the patient is best serviced by such as: Has the patient had any previous psychiatric treatment, if so where and how recently? Does the patient have relatives or support networks? If so where? Where does the patient want to live? Does the patient have an identified care provider or a case manager? Does the patient have a complex medical condition requiring local specialist care? Repatriation Negotiation Repatriation negotiation occurs between Site/Sector PFCs in the first instance. This can be escalated to Site/Sector Registrars, Consultant Psychiatrists and/or Service Dirceors if there is uncertainty about suitability of a patient for repatriation. If the issue remains unresolved and is impacting on patient flow, escalation to the District Access & Service Integration Manager may be required. It is useful to confirm all negotiations via email with relevant parties to avoid misunderstandings. When negotiating repatriation the requesting service must fax copies of the following to the receiving venue: MH-OAT Assessment module (A1) or A4 plus another recent A1 if available (usually in medical record). Confirmation of address of relatives / carers, or most recent residential address. Mental Health Act papers / recent clinical nursing notes / current risk assessment / Plan for admission/medication chart. Details of case manager if available, and whether the patient is known to the Acute Care Team. Revision 0 Trim No. Date: February 2013 page 16 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Requesting Transfer to Alternate Facility When requesting temporary transition placement (e.g. to PECC or SMHSOP Unit) to enable capacity for acute patient flow or when repatriating a patient the following process is required: Telephone contact PFC to PFC (weekdays 0800-1630hrs), or between afterhours Site/Sector patient flow delegate roles and/or on call Registrars to discuss request for placement. Faxing of MH-OAT assessment, risk assessment and additional modules where necessary, medication charts, MHA papers, progress notes and any transfer of care summaries from previous admissions. Once paperwork has been received and thoroughly reviewed the referring Duty Registrar is required to discuss the referral with the accepting Duty Registrar. Should the patient provisionally be accepted for transfer this should be discussed with the Consultant Psychiatrist or on call MH Executive to ensure that the transfer is appropriate. The referring venue is responsible for ensuring all required information is forwarded (see page 20). The receiving venue is responsible for reviewing the paperwork prior to accepting the patient, ensuring the patient is clinically appropriate and if appropriate satisfying themselves that the patient is a resident of their catchment area. Where transfer request cannot be resolved at local level, escalation to Service Director or On-call Executive may be required (see Appendix 2). Repatriating within SESLHD MHS Where a patient is from within SESLHD catchment area negotiations for inter-Site/Sector transfers are undertaken by the relevant PFCs. District Access & Service Integration Team is kept informed of progress. Repatriating within NSW Negotiations for repatriation of patients who are from outside of SESLHD MHS are between local PFC and other receiving MHS PFC, NUM, NIC or on call Registrar / Consultant Psychiatrist dependent on local practices. NSW Metro PFC Contact Numbers South Western Sydney LHD Ph: 0425 237 499 Central Coast & Northern Sydney LHDs Ph: 0404 830 169 Sydney West LHD Ph: 9840 3864 Illawarra Shoalhaven LHD Ph: 0403 571 299 St Vincent‟s Hospital Ph: 0416 141 026 Nepean Blue Mountains LHD Ph: 0434 396 111 Repatriating Interstate There are various factors to be considered when transferring a patient interstate. Is the patient suitable for transfer in terms of risk and clinical presentation for example? Logistically how will the patient be transferred e.g. air, train, relative/carer assistance, hospital vehicle and escort. Mental Revision 0 Trim No. Date: February 2013 page 17 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Health Act status – each jurisdiction has its own MHA and patient‟s status may become altered once over the border. The issue is complex and requires direct involvement of the site Chief Psychiatrist, sector Director of Operations and/or SESLHD MHS Director. International Repatriation A patient may require transfer to their residence overseas. Where relevant the patient‟s travel insurance may cover the cost of repatriation. Alternatively the family/ carers may be able to escort the patient. Where unclear it is useful to contact the relevant Embassy/ Consulate to advise what repatriation options can be provided. For example Switzerland has an excellent retrieval process where a team will be sent to escort the patient back to Switzerland. Retrieval agencies generally quote tens of thousands of dollars to assist in the repatriation of a patient to their place of origin. Such an agency is SOS International, Ph: 9372 2400. International repatriation requires a MDT approach to consider risk factors and clinical presentation. Airlines require an assessment form confirming suitability of the patient to fly, usually obtainable via their websites. Revision 0 Trim No. Date: February 2013 page 18 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Inter-hospital Transfer Algorithm Team identifies the need to transfer a patient to another venue following comprehensive clinical assessment, medical review & detailed risk assessment. Business Hours After Hours Referring team contacts Patient Flow Coordinator (PFC) via routine process to communicate requirement for transfer of patient & provides all paperwork. Requesting site PFC alerts Duty Registrar / Consultant, site Executive & District Access Team of transfer requirement, faxes all relevant documentation to receiving venue & checks receiving venue has received the fax. Duty Registrar at receiving venue reviews relevant paperwork in consultation with PFC / NUM / site Mental Health Executive. Current documentation to be compiled at this stage: Complete MH-OAT assessment Risk assessment & additional modules Care plans Management plans etc Historical information Medication / PRN charts 7 days progress notes Original legal papers plus S78, 80 & 81 where required. On-Call Registrar / CNC alerts NIC, On-Call Consultant, On-Call Executive of transfer requirement. NIC/ CNC faxes paperwork and phones to confirm receipt of fax. Registrar at receiving venue reviews relevant paperwork. Clinical discussion occurs between referring venue & receiving venue Registrars & On- Call Consultant Psychiatrist where necessary. Clinical discussion occurs between referring venue & receiving venue Registrars & Duty Consultant Psychiatrist where necessary. After clinical discussion the decision to transfer a patient to another venue is made in consultation with the Medical Officers, Nurse in Charge / CNC, On-Call Executive and after hours Nurse Manager. After clinical discussion the decision to transfer a patient to another venue is made in consultation with Medical Officers, NUM‟s, PFC & Executive. A clinical handover must precede or coincide with the patient‟s arrival at the receiving venue. Once the decision to transfer has been made, appropriate transport can be booked and it is imperative the original Mental Health Act paperwork accompanies patient and nursing clinical handover takes place. A clinical handover must precede or coincide with the patient‟s arrival at the receiving venue Ref: Inter-hospital Transfer of Mental Health Inpatients including ED, PECC, MHRU, OPU and MHU facilities Document No: 002_10 Revision 0 Trim No. Date: February 2013 page 19 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Transport When transferring a patient to another unit the following should be collated prior to transfer: Original MHA papers must accompany the patient. Photocopies should be kept in the patient medical record. A current Section 78 form for transfer should be completed and original to accompany patient. Copies of the recent clinical notes from the medical record, MH-OAT assessment, risk assessments and additional modules where necessary, medication chart, investigations, and other relevant assessments or correspondence. Any medications or belongings such as money, cards cigarettes and lighters. Scheduled patients must be risk assessed by the attending medical officer and a collaborative transport and escort plan formulated. Clinical handover must be given at the receiving destination. SESLHD MHS Priority Transport Options The patient‟s risk status will determine the most suitable means of transport. Risk status should include risk of AWOL, self harm, harm to others, sexual safety, patient‟s current mental state, willingness to be transported and historical risk factors. The following is a repertoire of transport options in escalating order for consideration and collaborative discussion in line with risk assessment: 1. 2. 3. 4. 5. 6. 7. 8. Hospital Transport with nurse escort Hospital transport driver (overtime) and hospital car with nurse escort Hospital car with Health and Safety Assistant (HASA) as the driver with nurse escort Hospital car with two nurse escorts (one driving) Networked hospital transport service with nurse escort Networked hospital transport driver and hospital car with nurse escort If the transfer is a repatriation arrange to use the donor site transport service Consider admitting a high risk patient to the local MHU and transferring a low risk patient via hospital car with ward staff or taxi and ward staff to another sector hospital 9. Consider delaying transport until acuity settles in 24 hrs 10. Consider temporarily placing a stable low risk patient in a transitional PECC bed to facilitate high risk MHU admission 11. Consider assertive CMHT engagement to expedite low risk MHU patient transfer of care to community to facilitate capacity to accept high risk admission 12. Contact Consultant Psychiatrists to review Mental Health inpatients to create capacity 13. Consider occupying medical / surgical bed for low risk voluntary patient to facilitate high risk patient admission to MHU 14. Consider buying a private hospital bed for low risk admission to facilitate capacity 15. NSW Ambulance / Hospital Security Officer with nurse escort 16. NSW Ambulance / Overtime Hospital Security Officer with nurse escort 17. NSW Ambulance / Casual Pool Hospital Security Officer with nurse escort 18. NSW Ambulance / Sector Security Officer with nurse escort 19. NSW Ambulance / NSW Police where a public safety issue is identified in consultation with Site/ District Mental Health Executives, Security Manager and / or Corporate Service Manager Revision 0 Trim No. Date: February 2013 page 20 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Hospital Vehicle/ Taxi Based on risk and following discussions with Consultant Psychiatrist and Clinical Operations Manager voluntary patients may be transferred in the ward car driven by nursing staff. Taxi vouchers can also be obtained from the NUM to transfer a patient to another hospital or home if nurse escort not required. If the patient requires an escort in the taxi a return taxi voucher for the nursing staff will be required. The destination of the taxi voucher must be completed in advance to prevent misuse of the vouchers. Ambulance St Vincent‟s Hospital Transport NSW Ambulance Bookings NSW Ambulance Liaison Officer NSW Ambulance Senior Operations Manager Medical Retrieval Unit Ph: 8382 2141 Ph: 131 233 Ph: 0407 296 254 Ph: 8396 5150 Ph: 9553 2222 *St Vincent‟s Transport can transfer patients within New South Wales and interstate. To organise transfer contact ph:8382 2238. Aero-medical Transport of Patients Where distance prohibits the use of a motor vehicle, aero-medical transport may be considered. Medical Retrieval Unit (ph: 9553 2222) is the central booking point for medical retrieval or long distance patient transport (for patients requiring air transport). However if Air Ambulance declines the transport, St Vincent‟s Transport (above) will organise transport with Wing-away. Patients who are Involuntary under the MHA can be transported but must be adequately settled. Wing-away have nurses who conduct a transport risk assessment prior to accompanying the patient on the flight. The accepting hospital will usually arrange to collect the patient from the destination airport. In exceptional circumstances Wing-away will also transfer from the airport to the destination hospital. In appropriate circumstances, provision may be made for a relative to accompany the patient on the flight. Authorisation must be obtained from the Sector Service Director and Chief Psychiatrist prior to organising the transfer. Revision 0 Trim No. Date: February 2013 page 21 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Referral to Private Hospitals Private psychiatric hospitals‟ admission criteria may vary slightly. In general these hospitals do not accept patients who are Involuntary under the MHA or have high levels of risk. Therefore patients must be voluntary prior to transfer and have current risk assessment demonstrating low-moderate levels of risk. Consideration must be given to risks such as suicidality, deliberate self harm, aggression, AWOL, sexual safety and self neglect. Private psychiatric hospitals also vary in their referral requirements. Essentially the same information is required as when negotiating repatriation: MH-OAT assessment and risk modules (A1& A4). Private Health Fund provider and number. Evidence of address and phone number of patient. Recent clinical notes from medical record / Current risk assessment / Psychiatric / Physical history / Plan for admission. GP / Private Psychiatrist / Psychologist contact details / Next of kin / carer contact details. Patients may not know their health fund reference numbers and it may be necessary to contact the health fund with the patient‟s name, date of birth, address so they can supply the health fund reference number. Patients who have health insurance may be required to pay an excess before they can be transferred to a private psychiatric hospital. This must be established before transfer takes place to ensure the patient is not put in financial difficulty. Private Hospitals Wandene (Kogarah) Wesley Private (Ashfield) St John of God (Richmond) St John of God (Burwood) Sydney Clinic (Bronte) Northside Clinic (Greenwich) Northside West Clinic (Wentworthville) The Park Central Clinic (Campbelltown) Southwest Clinic (Liverpool) Ph: 8197 5800 Ph: 9716 1400 Ph: 024570 6100 Ph: 9715 9200 Ph: 9389 8888 Ph: 9433 3555 Ph: 8833 2222 Ph: 024621 9111 Ph: 9600 4000 Accepting Referrals from Private Hospitals Patients who experience a significant deterioration in their clinical condition while in a private psychiatric hospital may be Scheduled under the MHA, 2007 and require transfer to a public hospital. When this occurs the private hospital will contact the nearest declared MHU and notify them of the patient‟s pending transfer. Most often the patient is taken to ED for assessment prior to transfer to MHU. The same principle applies as for accepting patients from ED or the general hospital (see page 14). Revision 0 Trim No. Date: February 2013 page 22 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Referral to Rehabilitation Services SESLHD MHS MHRU Clinical Access Pathway 1. Consumer identified by treating team for MHRU Referral from acute inpatient setting (priority) or community. Informal visit to MHRU may occur at this point. *Referral to Bloomfield or other SESLHD MHS MHRU may occur at this point* 2. Referral completed by referring clinician and sent to MHRU NUM Referral incomplete or consumer needs do not match Rehabilitation service. Referral complete and contains sufficient information for assessment of urgency, risk, relevance and processing of referral in a timely manner. Referrer contacted by MHRU to provide additional information and /or discuss possible alternative options. *Bloomfield most suitable for consumer Contact Bloomfield PFC MHRU assesses person within 2 weeks *Other SESLHD MHS MHRU more suitable for consumer Referral negotiated directly between Sectors Place available MHRU NUM facilitates admission processes in consultation with referrer/treating team, priority list adjusted accordingly. Local MHRU suitable for consumer Place not available Consumer prioritised on waiting list: bed list + waiting list circulated weekly by Sectors MHRU NUM commences engagement process in consultation with referrer/treating team – includes consumer visit(s) to MHRU POW SESIMHS MHRU’s Ph: 9382 3798 Fax: 9382 4237 TSH Ph: 9540 8200 Fax: 9540 8237 Revision 0 Trim No. Date: February 2013 page 23 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Referral to Bloomfield Rehabilitation Services Bloomfield is a specialist psychiatric facility based in Orange, NSW and includes several locked and declared rehabilitation units. The rehabilitation units at Bloomfield offer single gender accommodation for men and women and a limited number of long stay beds for patients deemed unsuitable for rehabilitation but for who all other placement options have been exhausted. The model at Bloomfield targets patients with higher acuity and more complex presentations than standard rehabilitation services. Beds are also available for patients undergoing Clozapine titration. Once a patient has been assessed as suitable for referral to Bloomfield a referral form must be completed. This is a collaborative process between the MDT and PFC. The following documents are required for referral to Bloomfield: Completed referral form, MH-OAT documentation, OT assessment / 7 days progress notes, medication chart. Transfer of care summaries from previous non-acute admissions, clinical handover / referral letter and site ownership letter. Bloomfield‟s allocation meetings take place on a Wednesday and the referral is processed within approximately a week. Once a patient has been accepted it may take a few more weeks before a bed comes available. However the date for transfer is generally indicated in advance to enable the patient and MHU to prepare. Following acceptance by Bloomfield, if transport is required, St Vincent‟s Transport should be contacted at least 48 hours in advance. It is approximately a 10 hour round trip to Orange so the patient and escort are usually collected by Transport at 0700hrs. The NUM must be informed so that extra staff can be arranged if needed to cover the escort. All original MHA paperwork must accompany patient, along with a completed Section 78. Due to the remote location of Bloomfield Hospital it is essential patients have a supply of personal money, personal items and clothing upon transfer. The patient‟s family/carers should be given the contact details and address for Bloomfield. Drug and Alcohol Services There are drug and alcohol teams based at every hospital and at various community services throughout SESLHD to provide support and education to patients with addiction issues. Clinical Nurse Consultants specialising in Alcohol and Other Drugs can attend ED‟s and MHUs to assess and support patients with co-morbid mental health and drug and alcohol issues. There are various facilities for Drug and Alcohol rehabilitation in NSW. Alcohol and Other Drugs rehabilitation facilities in SES LHD include: Sydney Hospital offers two inpatient rehabilitation beds for patients at risk of seizure during alcohol withdrawal: 9382 7111. The Langton Centre is a community based Drug and Alcohol service: 9332 8777. Revision 0 Trim No. Date: February 2013 Page 24 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Special Needs Referrals „Special Needs‟ refers to patients who may be unable to be treated in their local catchment due to actual or potential risk or conflict of interest. This can include patients who are employed within the hospital, a member of the local Police, Security or Ambulance Officers or relatives of patients or staff employed within the hospital. It can also relate to patients who have a clinical presentation that precludes admission to the local hospital, such as delusional thoughts regarding a member of staff or past threats of harm toward a staff member. When this situation occurs, the issue should be escalated to the Site / Sector Service Director to confirm whether transfer to another venue is required and to negotiate with another venue where appropriate. Should the matter not be resolved locally, the Area Access & Service Integration Team should be advised of the situation and the following information provided via email: Name / MRN / Date of Birth / Address. Special needs requirement, eg. Patient is RN working in the local hospital or patient a Police Officer working in local Area Command. Patients‟ current mental state/ diagnosis / prognosis / history. Patients MHA status. Revision 0 Trim No. Date: February 2013 Page 25 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Appendix 1 Useful Numbers Services and Contacts Numbers District Access & Service Integration 9113 2468 / 0404 033596 0404 ED 033 596 SHH Eloura East 4295 2546 SHH SHH Eloura West 4249 2549 Shoalhaven ED SHH Mirrabook 4295 2310 Milton ED TWH MHU 4253 4304 TWH ED TSH MHU 9540 7506 / 7485 TSH ED STG MHU 9113 2559 STG ED STG PECC 9113 1419 STG PECC Fax POW General 9382 4319 / 4357 POW ED POW Obs 9382 4333 / 4356 Kiloh Reception Fax POW PECC 9382 7772 / 7770 POW Euroa (SMHSOP) SVH Caritas 8382 1590 SVH ED SVH PECC 8382 4090 SVH PECC fax POW MHRU 9382 3798 NUM TSH MHRU 9540 8200 NUM SHH MHRU 4295 2357 NUM Sydney Children‟s Child and Adolescent Ward (CAMHs) TWH SMSOP Unit 4296 6666/switch 4421 3111/switch 4454 9133/switch 4222 5000/switch 9540 7115 9113 1516 9113 1499 9382 8400 9382 4399 9382 3796 8382 2473 8382 4091 9382 3495 9540 8231 4295 2352 9382 8283 4253 4465 Revision 0 Trim No. Date: February 2013 Page 26 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Appendix 2: SESLHD MHS Patient Flow Escalation Algorithm Revision 0 Trim No. Date: February 2013 Page 27 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES SESLHD MHS PROCEDURE Patient Flow Operational Framework SESLHDPR/245 Appendix 3: Referral to IPCU / MHICU Facilities Algorithm Patient presents with associated loss of capacity for self-control, with a corresponding increase in risk, which does not enable their safe, therapeutic management and treatment in an acute ward. Treating team notifies PFC of need to refer patient for mental health intensive care. PFC notifies site Executive and MHS Access & Service Integration Manager PFC faxes all documentation to receiving venue. Documentation to be compiled at this stage: Comprehensive Consultant psychiatrist assessment Risk assessment Care plans Details of containment strategies trialled: management plans etc Historical information Medication / PRN charts 7 days progress notes Appropriate legal papers SES LHD MHS PFC contacts corresponding PFC to establish IPCU / MHICU bed availability and makes referral. PFC informs referring team of outcome. Referring Consultant Psychiatrist contacts Chief Consultant of receiving venue to support request for higher level care and clinical / therapeutic / pharmaceutical discussion. Bed available PFC to arrange appropriate transport and escort, ensure original MHA paper work and copies of notes etc accompany patient and escort is able to provide full clinical hand over. Bed unavailable If no bed available, referring site Service Director to contact site Service Director of Intensive Care Venue to ascertain if bed can be made available. Bed available Bed unavailable The referring venue has an obligation to ensure repatriation of the patient within 24hrs of notification by IPCU / MHICU of criteria for admission no longer applying Where no bed available, site Service Director to prepare brief of action so far for SES LHD MHS Director IPCU/MHICU Venues & Contacts Sydney/ Sydney West (Concord) Sydney West (Cumberland) North Shore Central Coast (Hornsby) PFC 0425 237 499 PFC 984 0386 PFC 0404 830 169 Revision 0 Trim No. Date: February 2013 Page 28 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES References Garling, P. Final Report of the Special Commission of Inquiry. Acute Care Services in NSW Public Hospitals Overview 27 November 2008, pp. 30, (1.193) NSW Health Mental Health for Emergency Departments – A Reference Guide 2009 NSW Health Sustainable Access Plan 2004 Referral to Intensive Psychiatric Care Unit (IPCU) or Mental Health Intensive Care Unit (MHICU) Business Rule Document No: 004_10. April 2010 SESLHD Acute Patient Flow and Sustainable Access Management for Mental Health January 2013 Discharge/Transfer Planning For Adults & Children in Acute Facilities, SESLHD PD 107 August 2009 Inter-hospital Transfer of Mental Health Inpatients including ED, PECC, MHRU, OPU and MHU facilities SESLHD Document No: 002_10 Obtaining a Second Opinion from a Consultant Psychiatrist SESLHD PD 2007/07 v5 Revised April 2012 8. Revision and Approval History Date 22/11/2012 Revision no: 0 Author and approval Updated and changed from previous SESIAHS Procedure. Gayle Jones, A/Access & Service Integration Manager, SESLHD MHS. Approved by SESLHDMHS Clinical Council. Revision 0 Trim No. Date: March 2013 Page 29 of 29 THIS DISTRICT DOCUMENT BECOMES UNCONTROLLED WHEN PRINTED OR DOWNLOADED UNLESS REGISTERED BY LOCAL DOCUMENT CONTROL PROCEDURES
© Copyright 2026