27 Gastrointestinal drugs
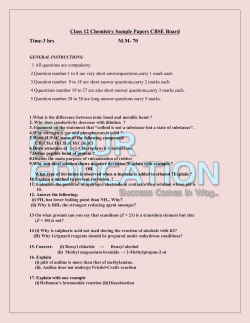
27 Gastrointestinal drugs Interactions of H2-receptor antagonists Table 27.1 Gastrointestinal drugs Group Drugs 5-Aminosalicylates Balsalazide, Mesalazine, Olsalazine, Sulfasalazine m pl Cimetidine is a non-specific weak inhibitor of a number of the cytochrome P450 isoenzymes, including CYP1A2, CYP2C19, CYP2D6 and CYP3A4, and therefore inhibits the metabolism of many drugs, increasing their plasma levels and/or bioavailability. These interactions are most likely to be clinically significant for drugs with a narrow therapeutic index. Famotidine, nizatidine and ranitidine do not inhibit cytochrome P450 to a clinically relevant extent and are therefore less likely than cimetidine to be involved in interactions that occur by this mechanism. However, it should be noted that the absorption of some drugs may be affected by the changes in gastric pH, which can be produced by any of the H2-receptor antagonists. Furthermore, drug interactions may also occur because of inhibition of renal tubular secretion: cimetidine, famotidine and ranitidine have all been implicated in this type of interaction, which occurs via renal organic cation transporters. with poor metabolisers e.g. in the eradication of H. pylori, as they tend to have lower therapeutic levels of proton pump inhibitors.2-4 Poor metabolisers, who lack CYP2C19 metabolising capacity, use alternative pathways to metabolise proton pump inhibitors, and this is mainly CYP3A4. Because poor metabolisers are more dependent on CYP3A4 for e The various gastrointestinal drug groups covered in this section are listed in ‘Table 27.1’ (below). Some of the interactions of these drugs occur by causing alterations in the absorption of other drugs, and these are covered under the affected drug. The section ‘Drug absorption interactions’, p.3, discusses how these interactions occur and contains more detailed information on some of the mechanisms. Antacids Aluminium hydroxide, Aluminium-magnesium complexes, Bismuth salicylate, Bismuth subnitrate, Magnesium carbonate, Magnesium hydroxide, Magesium trisilicate Antidiarrhoeals Loperamide Antiemetics Antihistamines Cinnarizine, Cyclizine, Promethazine Dronabinol, Nabilone Interactions of 5-HT3 receptor antagonists Dopamine antagonists Domperidone, Metoclopramide Many 5-HT3 receptor antagonists (dolasetron, ondansetron, palonosetron and tropisetron) are metabolised in part by CYP2D6.1 This isoenzyme is subject to genetic polymorphism (see ‘Genetic factors in drug metabolism’, p.4, for a further explanation of polymorphism). Granisetron is not metabolised by CYP2D6, and is principally metabolised by CYP3A; and alosetron is primarily metabolised by CYP1A2. The available 5-HT3 receptor antagonists appear to have little effect on the metabolism of other drugs by cytochrome P450. 5-HT3-receptor antagonists Alosetron, Dolasetron, Granisetron, Ondansetron, Palonosetron, Ramosetron, Tropisetron Neurokinin-1 receptor antagonists Aprepitant, Fosaprepitant Phenothiazines Prochorperazine Sa Cannabinoids Antisecretory drugs H2-receptor antagonists Interactions of neurokinin receptor antagonists Aprepitant and its prodrug fosaprepitant are currently the only available drugs in this class. Aprepitant is metabolised by CYP3A4, and may interact with drugs that inhibit or induce this isoenzyme. Aprepitant is unusual in that in the short term it acts as a dose-dependent, weak to moderate inhibitor of CYP3A4, but this is followed by a period of induction of CYP3A4, CYP2C9 and glucuronidation after treatment is stopped. It can therefore both increase and/or decrease the levels of drugs that are metabolised by these isoenzymes, such as midazolam (see ‘Benzodiazepines + Aprepitant’, p.749), warfarin (see ‘Coumarins + Aprepitant’, p.378), and the combined hormonal contraceptives (see ‘Combined hormonal contraceptives + Aprepitant’, p.1075). Prostaglandin analogues Misoprostol Proton pump inhibitors Esomeprazole, Dexlansoprazole, Lansoprazole, Omeprazole, Pantoprazole, Rabeprazole Antispasmodics Antimuscarinics Other antispasmodics Laxatives Bulk-forming Dicycloverine, Hyoscine, Propantheline Alverine, Mebeverine Ispaghula, Methycellulose, Sterculia Osmotic Lactulose, Macrogols, Magnesium hydroxide, Phosphates, Sodium citrate Peripheral opioid antagonists Alvimopan, Methylnaltrexone Stimulants Bisacodyl, Dantron, Docusate sodium, Glycerol, Senna, Sodium picosulfate Interactions of proton pump inhibitors The cytochrome P450 isoenzyme CYP2C19 is the main route of metabolism of esomeprazole, lansoprazole, omeprazole, pantoprazole, and is also involved in the metabolism of rabeprazole. This isoenzyme is subject to genetic polymorphism1 (see ‘Genetic factors in drug metabolism’, p.4, for a further explanation of polymorphism). The poor metaboliser phenotype for CYP2C19 (that is, those lacking or deficient in this isoenzyme) is found in approximately 1 to 6% of Caucasians, 1 to 7.5% of Blacks and 12 to 23% of Oriental and Indian Asians.2 Most patients are extensive CYP2C19 metabolisers (that is, they have normal levels of this isoenzyme), and their major route for the metabolism of these proton pump inhibitors will be through this isoenzyme. As a consequence,2 the levels of the proton pump inhibitors in these patients are likely to be affected by drugs that inhibit or induce CYP2C19, such as fluvoxamine (see ‘Proton pump inhibitors + SSRIs’, p.1062). Patients of the extensive metaboliser phenotype have also been shown in some studies to have a poorer clinical outcome, when compared Cimetidine, Famotidine, Nizatidine, Ranitidine, Roxatidine Mucosal protectants Bismuth compounds Other mucosal protectants Prokinetic drugs (motility stimulants) Chloride-channel activator Bismuth subcitrate potassium, Tripotassium dicitratobismuthate Carbenoxolone, Liquorice, Sucralfate Lubiprostone Dopamine antagonists Domperidone, Metoclopramide 5-HT4-receptor agonists Cisapride, Mosapride, Prucalopride 1044 Sample from Stockley's Drug Interactions, 10th Edition Gastrointestinal drugs tions. A possible example of this is the increase in levels of these proton pump inhibitors caused by the P-glycoprotein inhibitor clarithromycin, see ‘Proton pump inhibitors + Macrolides’, p.1061. 1. Robinson M, Horn J. Clinical pharmacology of proton pump inhibitors. What the practising physician needs to know. Drugs (2003) 63, 2739–54. 2. Desta Z, Zhao X, Shin JG, Flockhart DA. Clinical significance of the cytochrome P450 2C19 genetic polymorphism. Clin Pharmacokinet (2002) 41, 913–58. 3. Furuta T, Shirai N, Sugimoto M, Nakamura A, Hishida A, Ishizaki T. Influence of CYP2C19 pharmacogenetic polymorphism on proton pump inhibitor-based therapies. Drug Metab Pharmacokinet (2005) 20, 153–67. 4. Klotz U. Pharmacokinetic considerations in the eradication of Helicobacter pylori. Clin Pharmacokinet (2000) 38, 243–70. 5. Pauli-Magnus C, Rekersbrink S, Klotz U, Fromm MF. Interaction of omeprazole, lansoprazole and pantoprazole with P-glycoprotein. Naunyn Schmiedebergs Arch Pharmacol (2001) 364, 551–7. Sa m pl e metabolism of the proton pump inhibitors the levels of proton pump inhibitors may be more significantly raised in these patients, when compared with extensive metabolisers, when they are given CYP3A4 inhibitors, such as ketoconazole, see ‘Azoles + Proton pump inhibitors’, p.223. Omeprazole and esomeprazole are potent inhibitors of CYP2C19, and therefore they may increase the levels of drugs that are metabolised by this isoenzyme, such as diazepam.1,2 Omeprazole is a very weak inducer of CYP1A2, but this is probably not clinically relevant. In vitro study suggests that some proton pump inhibitors, including omeprazole, lansoprazole and pantoprazole, may possibly be P-glycoprotein substrates and inhibitors, and this may be a factor in some of their interac- 1045 5 Sample from Stockley's Drug Interactions, 10th Edition Chapter 27 Aluminium hydroxide + Ascorbic acid (Vitamin C) or Citrates Patients with renal failure given aluminium compounds and oral citrates can develop a potentially fatal encephalopathy due to a very marked rise in blood-aluminium levels. There is also some evidence that aluminium compounds and ascorbic acid (vitamin C) may interact similarly. Clinical evidence Alvimopan + Miscellaneous (a) Ascorbic acid A study in 13 healthy subjects given aluminium hydroxide 900 mg three times daily found that ascorbic acid 2 g daily increased the urinary excretion of aluminium threefold.1 (b) Citrates The gastrointestinal adverse effects of alvimopan are expected to be greater in those who have recently taken opioids. Alvimopan does not appear to alter the pharmacokinetics of intravenous morphine. Antibacterials that affect gut flora and drugs that inhibit gastric acid secretion appear to reduce the formation of the metabolite of alvimopan. Theoretically, potent P-glycoprotein inhibitors may interact with alvimopan. Clinical evidence, mechanism, importance and management (a) Antibacterials In a drug interaction study, 42 healthy subjects were given alvimopan 6 mg twice daily for 30 days, with ciprofloxacin 500 mg twice daily on days 11 to 20. Ciprofloxacin almost totally abolished the plasma levels of the metabolite of alvimopan, and this effect partially persisted in some subjects 10 days after ciprofloxacin was stopped. The AUC of alvimopan was unchanged by ciprofloxacin.1 In a population pharmacokinetic analysis, the pharmacokinetics of alvimopan were not affected by the preoperative use of oral antibacterials (not specified), but the plasma concentration of its metabolite was reduced by 81%.2 Alvimopan is metabolised by intestinal flora to a metabolite that is slightly less active than the parent molecule. Any antibacterial that reduces intestinal flora may therefore reduce the formation of this metabolite. However, the manufacturer notes that as this metabolite is not required for efficacy, no alvimopan dose adjustment is needed if antibacterials are also given.2 m pl Four patients with advanced chronic renal impairment taking aluminium hydroxide and citrate (Shohl’s) solution died due to hyperaluminaemia.2 When these cases were compared with another 34 renal patients, it was found that the fatalities had occurred in patients who had taken more aluminium hydroxide, more citrate, and who were older. When both groups were considered together, increased serum aluminium levels were found to be correlated with increased citrate intake.3 In a study in 5 healthy subjects given aluminium hydroxide with or without citrate solution, aluminium levels were found to be 11 micrograms/L at baseline, 44 micrograms/L when aluminium hydroxide was given, and 98 micrograms/L when citrate was given with the aluminium hydroxide. Aluminium clearance also dramatically increased in the presence of citrate.3 Another report describes this interaction in 2 patients with renal impairment, and in a possible further 6 patients with renal failure, all of whom died.4 In a further single-dose study in 6 patients with end-stage renal disease, sodium citrate with citric acid 30 mL markedly increased the AUC of aluminium (from a 30-mL dose of aluminium hydroxide gel) 4.6-fold.5 A haemodialysis patient given effervescent co-codamol had a tenfold increase in serum aluminium levels. This was attributed to sodium citrate in the formulation, which is used to produce the effervescence.6 A number of other studies, mainly in healthy subjects, have confirmed that citrate markedly increases aluminium absorption, see Mechanism, below. Mechanism 10. Slanina P, Frech W, Ekström L-G, Lööf L, Slorach S, Cedergren A. Dietary citric acid enhances absorption of aluminum in antacids. Clin Chem (1986) 32, 539–41. 11. Weberg R, Berstad A. Gastrointestinal absorption of aluminium from single doses of aluminium containing antacids in man. Eur J Clin Invest (1986) 16, 428–32. 12. Fairweather-Tait S, Hickson K, McGaw B, Reid M. Orange juice enhances aluminium absorption from antacid preparation. Eur J Clin Nutr (1994) 48, 71–3. 13. Dorhout Mees EJ, Basçi A. Citric acid in calcium effervescent tablets may favour aluminium intoxication. Nephron (1991) 59, 322. 14. Mauro LS, Kuhl DA, Kirchhoff JR, Mauro VF, Hamilton RW. Impact of oral bases on aluminium absorption. Am J Ther (2001) 8, 21–5. e 1046 Studies in healthy subjects clearly demonstrate that citrate markedly increases the absorption of aluminium from the gut,3,7,8 and one study in 20 adults with end-stage renal failure receiving chronic haemodialysis found that the administration of calcium citrate gave rise to enhanced aluminium absorption.9 The absorption of aluminium is increased threefold if it is taken with lemon juice,10 eight- to tenfold if it is taken with orange juice,11,12 and five- to 50-fold if it is taken with citrate,3,7,8,11 but the reason for this is not understood. It could be that a highly soluble aluminium citrate complex is formed.4,7 Importance and management Sa The interaction between aluminium compounds and citrates in patients with renal impairment is established and clinically important as it is potentially fatal. Concurrent use should be strictly avoided. Remember that some effervescent and dispersible tablets (including many proprietary non-prescription analgesics, indigestion and hangover remedies such as Alka-Seltzer) contain citric acid or citrates,6,13 and they may also occur in soft drinks.13 Haemodialysis patients should be strongly warned about these products as aluminium is not dialysed and will accumulate in this patient group. The interaction between aluminium compounds and ascorbic acid is not yet well established, but the information available so far suggests that this combination should also be avoided by patients with renal impairment. It is not clear whether orange juice is also unsafe but the available evidence suggests that concurrent administration is probably best avoided. The importance of the interaction between aluminium and citrates in subjects with normal renal function is by no means clear because it is still not known whether increased aluminium absorption results in aluminium accumulation over the long-term in those with normal renal function.12 Some authors have recommended that food or drinks containing citric acid (citrus fruits and fruit juices) should not be taken at the same time as aluminium-containing medicines, and that their ingestion should be separated by 2 to 3 hours.12 However, one study in healthy subjects reported significantly raised aluminium levels when a citric acid solution and an aluminium hydroxide antacid were taken 2 hours apart.14 1. Domingo JL, Gomez M, Llobet JM, Richart C. Effect of ascorbic acid on gastrointestinal aluminium absorption. Lancet (1991) 338, 1467. 2. Bakir AA, Hryhorczuk DO, Berman E, Dunea G. Acute fatal hyperaluminemic encephalopathy in undialyzed and recently dialyzed uremic patients. Trans Am Soc Artif Intern Organs (1986) 32, 171–6. 3. Bakir AA, Hryhorczuk DO, Ahmed S, Hessl SM, Levy PS, Spengler R, Dunea G. Hyperaluminemia in renal failure: the influence of age and citrate intake. Clin Nephrol (1989) 31, 40–4. 4. Kirschbaum HB, Schoolwerth AC. Acute aluminum toxicity associated with oral citrate and aluminumcontaining antacids. Am J Med Sci (1989) 297, 9–11. 5. Rudy D, Sica DA, Comstock T, Davis J, Savory J, Schoolwerth AC. Aluminum-citrate interaction in endstage renal disease. Int J Artif Organs (1991) 14, 625–9. 6. Main J, Ward MK. Potentiation of aluminium absorption by effervescent analgesic tablets in a haemodialysis patient. BMJ (1992) 304, 1686. 7. Coburn JW, Mischel MG, Goodman WG, Salusky IB. Calcium citrate markedly enhances aluminum absorption from aluminium hydroxide. Am J Kidney Dis (1991) 17, 708–11. 8. Walker JA, Sherman RA, Cody RP. The effect of oral bases on enteral aluminum absorption. Arch Intern Med (1990) 150, 2037–9. 9. Lindberg JS, Copley JB, Koenig KG, Cushner HM. Effect of citrate on serum aluminum concentrations in hemodialysis patients: a prospective study. South Med J (1993) 86, 1385–8. (b) Cytochrome P450 isoenzyme inhibitors, inducers and substrates Alvimopan is not a substrate of the cytochrome P450 isoenzyme system, and therefore drugs that are inhibitors or inducers of these isoenzymes are not expected to alter the pharmacokinetics of alvimopan by this mechanism.2 Alvimopan is not an inhibitor or inducer of any of the key cytochrome P450 isoenzymes, and would therefore not be expected to alter the pharmacokinetics of drugs that are substrates of these isoenzymes by this mechanism.2 (c) Drugs that inhibit gastric acid secretion The manufacturer of alvimopan notes that, in a population pharmacokinetic analysis, the pharmacokinetics of alvimopan were not affected by ‘acid blockers’ (not specified), but the pharmacokinetics of its metabolite were reduced by 49%.2 However, the manufacturer notes that as the metabolite is not required for efficacy, no alvimopan dose adjustment is needed if these drugs are also given.2 (d) Opioids The manufacturer of alvimopan briefly states that alvimopan had no clinically relevant effect on the pharmacokinetics of intravenous morphine or its 6-glucuronide metabolite. Therefore, no dose adjustment of intravenous morphine is likely to be needed on concurrent use.2 However, as alvimopan is a peripheral μ-opioid receptor antagonist, it may antagonise the peripheral effects of opioids, such as morphine, on gastrointestinal motility without reversing their central analgesic effects.2 Patients who have been taking opioids in the week before starting alvimopan are expected to be more sensitive to alvimopan, and may experience more gastrointestinal adverse effects (abdominal pain, nausea and vomiting, diarrhoea).2 Alvimopan should therefore be used with caution in these patients.2 (e) P-glycoprotein inhibitors and substrates Alvimopan and its metabolite are both substrates for P-glycoprotein in vitro.2 However, the manufacturer briefly states that, in a population pharmacokinetic analysis, there was no evidence that the pharmacokinetics of alvimopan and its metabolite were altered by mild to moderate P-glycoprotein inhibitors (not specified).2 Nevertheless, they state that no clinical studies have been conducted on the effect of potent Pglycoprotein inhibitors on alvimopan2 and until more is known, some caution might be prudent with these drugs (they name amiodarone, ciclosporin (cyclosporine), diltiazem, itraconazole, quinidine, quinine, spironolactone, and verapamil). Alvimopan does not inhibit P-glycoprotein, and would therefore not be expected to alter the pharmacokinetics of drugs that are P-glycoprotein substrates.2 1. Schmith VD, Johnson BM, Vasist LS, Kelleher DL, Hewens DA, Young MA, Ameen V, Dukes GE. The effects of short courses of antibiotics on alvimopan metabolite pharmacokinetics. J Clin Pharmacol (2010) 50, 338–349. 2. Entereg (Alvimopan). GlaxoSmithKline. US Prescribing information, November 2009. Antacids + Calcium compounds Hypercalcaemia, alkalosis and renal impairment (milk-alkali syndrome) can develop in patients taking antacids with calcium-containing sub- Sample from Stockley's Drug Interactions, 10th Edition Gastrointestinal drugs stances, including dairy products. Note that excess calcium carbonate alone can cause this syndrome. Clinical evidence Milk-alkali syndrome was a common cause of hypercalcaemia when milk plus antacids was the standard therapy for peptic ulcer disease, and reports for this are not cited here. Nevertheless, occasionally, cases of milk-alkali syndrome are still reported in patients taking antacids and milk to excess. For example, a man presented with nausea, vomiting, constipation, polyuria and polydipsia, which was diagnosed as milk-alkali syndrome, due to daily treatment with 6 tablets of Caved-S and about 2 litres (3.5 pints) of milk, for dyspepsia related to a peptic ulcer.1 This dose of Caved-S meant he was taking 600 mg of aluminium hydroxide, 1.2 g of magnesium carbonate, 600 mg of sodium bicarbonate and 2.28 g of deglycyrrhizinised liquorice daily.1 The most common cause of milk-alkali syndrome is now the use of calcium carbonate alone for osteoporosis or as an antacid. Note that calcium carbonate is both a source of calcium and of alkali. These cases tend to occur when the doses used are excessive, or when there are other risk factors for hypercalcaemia such as renal impairment. The many reports for this are not cited here as they are not an interaction. Two cases are cited in patients taking large amounts of Rennies antacid (calcium/ magnesium carbonate) for which milk consumption may have contributed.2,3 High intake and absorption of calcium can suppress the parathyroid hormone, which leads to bicarbonate retention by the kidneys, leading to metabolic and respiratory alkalosis. The alkalosis also causes reduced excretion of calcium by the kidneys. Hypermagnesaemia may also have a part to play. Importance and management For recommendations regarding antineoplastics that are CYP3A4 substrates, see ‘Antineoplastics + Aprepitant’, p.604. 1. EMEND (Aprepitant). Merck Sharp & Dohme Ltd. UK Summary of product characteristics, January 2010. 2. EMEND Capsules (Aprepitant). Merck & Co., Inc. US Prescribing information, July 2012. 3. IVEMEND (Fosaprepitant dimeglumine). Merck Sharp & Dohme Ltd. UK Summary of product characteristics, December 2011. 4. EMEND for Injection (Fosaprepitant dimeglumine). Merck & Co., Inc. US Prescribing information, July 2012. Aprepitant + Ketoconazole and other CYP3A4 inhibitors Ketoconazole (a potent CYP3A4 inhibitor) markedly increases aprepitant concentrations, and would also be expected to increase the concentrations of aprepitant derived from fosaprepitant. Other potent inhibitors of CYP3A4 are predicted to interact in a similar way to ketoconazole. Clinical evidence, mechanism, importance and management The manufacturers note that when a single 125-mg dose of aprepitant was given on day 5 of a 10-day course of ketoconazole 400 mg daily, the AUC of aprepitant was increased by about 5-fold, and the half-life by about 3-fold.1,2 Ketoconazole is an inhibitor of the cytochrome P450 isoenzyme CYP3A4, by which aprepitant is metabolised, and concurrent use therefore raises aprepitant concentrations. Although the clinical outcome of these increases has not been assessed, such marked increases in concentrations could increase the risk of aprepitant adverse effects. The manufacturers recommend caution when aprepitant is given with ketoconazole or other drugs that are potent inhibitors of CYP3A4. They name the HIVprotease inhibitors (the US manufacturer specifically names nelfinavir and ritonavir2), clarithromycin, itraconazole, telithromycin, troleandomycin, nefazodone, posaconazole, and voriconazole.1,2 Until more is known it would seem prudent to consider using the lowest dose of aprepitant possible, and monitor for an increase in aprepitant adverse effects (such as hiccups, fatigue, constipation, headache) on the concurrent use of these drugs. Fosaprepitant is rapidly metabolised to aprepitant and would therefore be expected to be similarly affected. For the effect of diltiazem (a moderate CYP3A4 inhibitor), see ‘Calcium-channel blockers + Aprepitant’, p.942. Other inhibitors of CYP3A4 are listed in ‘Table 1.9’ (p.9). e Mechanism 1047 m pl While taking antacids, even well within the recommended dose range, as in the first case, it is still possible to develop a serious and potentially life-threatening reaction (known as milk-alkali syndrome) if the intake of calcium is high. The milk-alkali syndrome was a common adverse effect of antacid use when the concurrent use of milk and antacids was the primary treatment of peptic ulcer disease, and chronic milk-alkali syndrome can lead to the formation of calcification and kidney damage, which may be irreversible. The quantity of calcium ingested does not appear to be directly correlated to either the development or severity of milk-alkali syndrome, which has been reported with an intake of between 4 g to 60 g of calcium carbonate.3 However, milk-alkali syndrome as a result of an interaction has become very uncommon with the advent of H2-receptor antagonists and proton pump inhibitors and now the principal cause of the ‘milk-alkali’ syndrome would appear to be the use of calcium carbonate alone (for osteoporosis or as an antacid), as this is both a source of calcium and a source of alkali. Although the risk of this might also be higher in patients also taking calcium from milk, the milk is not necessary for the syndrome, so many of the cases are probably not actually interactions at all. Nevertheless, consider the possibility of an interaction in patients who take medications containing calcium, such as antacids or supplements for the prophylaxis of osteoporosis, and also consume large quantities of dairy products in their diet. Note that many calcium-containing antacids are freely available without prescription. Sa 1. Gibbs CJ, Lee HA. Milk-alkali syndrome due to Caved-S. J R Soc Med (1992) 85, 498–9. 2. Verburg FA, van Zanten RAA, Brouwer RML, Woittiez AJJ, Veneman TF. Een man met een ernstig klassiek melk-alkalisyndroom en een maagcarcinoom. Ned Tijdschr Geneeskd (2006) 150, 1624–7. 3. Gordon MV, Hamblin PS, McMahon LP. Life-threatening milk-alkali syndrome resulting from antacid ingestion during pregnancy. Med J Aust (2005) 182, 350–351 Aprepitant + CYP3A4 substrates Aprepitant can increase the levels of CYP3A4 substrates in the shortterm, then reduce them within 2 weeks. Any effect is likely to be important with drugs that have a narrow therapeutic range (e.g. ciclosporin) and be most important with drugs associated with significant toxicity with elevated levels (e.g. pimozide). Clinical evidence, mechanism, importance and management In the first few days of use, aprepitant 125 mg on day one followed by 80 mg daily for 4 days markedly increased levels of midazolam, a probe drug substrate for the cytochrome P450 isoenzyme CYP3A4. Then, within 2 weeks, a reduction in levels was seen, see ‘Benzodiazepines + Aprepitant’, p.749, for the full details. This effect was not seen with a dose regimen of 40 mg on day one followed by 25 mg daily for 4 days. Aprepitant is therefore both a dose-dependent inhibitor and an inducer of CYP3A4. Because of this, aprepitant is expected to increase the levels of other CYP3A4 substrates up to about 3-fold, and the manufacturers recommend caution if aprepitant is given with CYP3A4 substrates.1,2 The UK manufacturer specifically recommends caution with CYP3A4 substrates that have a narrow therapeutic range including some immunosuppressants (ciclosporin, tacrolimus, sirolimus, everolimus), ergot derivatives, alfentanil, fentanyl, and quinidine.1 For details of recommended everolimus dose reductions on concurrent use with CYP3A4 inhibitors such as aprepitant, see ‘Everolimus + Ketoconazole and other CYP3A4 inhibitors’, p.1162. Note that the manufacturers specifically contraindicate the concurrent use of aprepitant with some CYP3A4 substrates, including pimozide,1,2 because of the risk of life-threatening torsade de pointes with increased levels of these drugs. As fosaprepitant is rapidly converted to aprepitant, the manufacturers apply the same contraindication.3,4 For a list of CYP3A4 substrates, see ‘Table 1.10’ (p.10). Within 2 weeks of aprepitant use, a reduced level of CYP3A4 substrates might occur, and caution is also advised during this time. 1. EMEND (Aprepitant). Merck Sharp & Dohme Ltd. UK Summary of product characteristics, January 2010. 2. EMEND Capsules (Aprepitant). Merck & Co., Inc. US Prescribing information, July 2012. Aprepitant + Phenytoin and other CYP2C9 substrates Aprepitant is predicted to decrease the levels of phenytoin, a CYP2C9 substrate and phenytoin is predicted to decrease aprepitant levels and efficacy. Aprepitant is also predicted to reduce the levels of other CYP2C9 substrates. Both aprepitant and phenytoin are available as prodrugs: fosaprepitant would be expected to interact in the same way as aprepitant and fosphenytoin would be expected to interact in the same way as phenytoin. Clinical evidence, mechanism, importance and management Aprepitant is an inducer of the cytochrome P450 isoenzyme CYP2C9, and slightly reduces the plasma levels of substrates of this isoenzyme such as warfarin (see ‘Coumarins + Aprepitant’, p.378) and tolbutamide (see ‘Sulfonylureas; Tolbutamide + Aprepitant’, p.510). The manufacturers therefore recommend caution when aprepitant is given with other drugs that are known to be metabolised by CYP2C9, because of the possibility that their plasma levels may be reduced.1,2 They specifically name phenytoin. However, phenytoin is also an inducer of CYP3A4 and the manufacturers1,2 predict that it will decrease the levels of aprepitant, and might reduce its efficacy, see ‘Aprepitant + Rifampicin (Rifampin) and other CYP3A4 inducers’, p.1047. Consequently, the UK manufacturers advise avoiding the concurrent use of aprepitant and phenytoin.1 The manufacturers of aprepitant1,2 recommend caution when aprepitant is given with other drugs that are known to be metabolised by CYP2C9, because of the possibility that their levels may be reduced. See ‘Table 1.5’ (p.7), for a list of CYP2C9 substrates. Fosaprepitant, the prodrug of aprepitant, is expected to interact in the same way as aprepitant, and as fosphenytoin is a prodrug of phenytoin, it would be expected to interact in the same way as phenytoin. 1. EMEND (Aprepitant). Merck Sharp & Dohme Ltd. UK Summary of product characteristics, January 2010. 2. EMEND Capsules (Aprepitant). Merck & Co., Inc. US Prescribing information, July 2012. Aprepitant + Rifampicin (Rifampin) and other CYP3A4 inducers Rifampicin (an inducer of CYP3A4) markedly reduces the AUC of aprepitant, and other potent inducers of CYP3A4 may also interact Sample from Stockley's Drug Interactions, 10th Edition Chapter 27 with aprepitant in this way. Fosaprepitant would be expected to be affected in the same way as aprepitant. Clinical evidence, mechanism, importance and management The manufacturers of aprepitant note that when a single 375-mg dose of aprepitant was given on day 9 of a 14-day course of rifampicin 600 mg daily, the AUC of aprepitant was decreased by 91% and the half-life was decreased by 68%.1,2 Rifampicin is an inducer of the cytochrome P450 isoenzyme CYP3A4, by which aprepitant is metabolised. Concurrent use therefore decreases aprepitant levels. Fosaprepitant is rapidly metabolised to aprepitant and would therefore be expected to be similarly affected. Although not assessed, this marked reduction in aprepitant levels is likely to result in reduced efficacy. In the UK, the manufacturer states that the concurrent use of aprepitant or fosaprepitant with potent inducers of CYP3A4, such as rifampicin, should be avoided.1,3 They also name phenytoin (see also ‘Aprepitant + Phenytoin and other CYP2C9 substrates’, p.1047), carbamazepine, and phenobarbital, and also state that concurrent use of St John’s wort is not recommended.1,3 Note that primidone is metabolised to phenobarbital and is therefore likely to interact similarly. Other inducers of CYP3A4 are listed in ‘Table 1.9’ (p.9). 1. EMEND (Aprepitant). Merck Sharp & Dohme Ltd. UK Summary of product characteristics, January 2010. 2. EMEND Capsules (Aprepitant). Merck & Co., Inc. US Prescribing information, July 2012. 3. IVEMEND (Fosaprepitant dimeglumine). Merck Sharp & Dohme Ltd. UK Summary of product characteristics, December 2011. Bismuth compounds + Food Clinical evidence, mechanism, importance and management (a) Bismuth carbonate Ranitidine possibly causes an increase in the absorption of bismuth from tripotassium dicitratobismuthate, but not bismuth salicylate or bismuth subnitrate. Other H2-receptor antagonists would be expected to interact similarly. Clinical evidence, mechanism, importance and management In a study in 12 healthy subjects, the AUC of a single 240-mg dose of tripotassium dicitratobismuthate (De Noltab) was increased fourfold by two 300-mg doses of ranitidine (taken the night before and 2 hours before the bismuth compound). The maximum serum levels of bismuth were approximately doubled by ranitidine. In contrast, the same regimen of ranitidine had no significant effect on the absorption of bismuth from bismuth salicylate (Pepto-Bismol) or bismuth subnitrate (Roter tablets).1 The authors suggest that the reduction in gastric acidity maintains tripotassium dicitratobismuthate in its colloidal form, which is more likely to be absorbed, and that this may result in increased bismuth toxicity.1 Therefore other H2-receptor antagonists would be expected to interact similarly. However, the manufacturers of tripotassium dicitratobismuthate state that the toxic range of bismuth is arbitrary and a small increase in absorption is not clinically relevant, except perhaps in patients with renal failure, in whom this bismuth compound should be avoided in any case.2 No clinically relevant effect would be expected with recommended short courses for H. pylori eradication; however, some caution might be appropriate with longer term use of H2-receptor antagonists and bismuth compounds. 1. Nwokolo CU, Prewett EJ, Sawyerr AM, Hudson M, Pounder RE. The effect of histamine H2-receptor blockade on bismuth absorption from three ulcer-healing compounds. Gastroenterology (1991) 101, 889– 94. 2. Yamanouchi Pharma Ltd. Personal communication, November 1994. m pl Food may reduce the absorption of bismuth from some, but not all, bismuth compounds. Bismuth compounds + H2-receptor antagonists e 1048 Bismuth compounds + Proton pump inhibitors Omeprazole markedly increases the absorption and bioavailability of bismuth from bismuth subcitrate potassium and tripotassium dicitratobismuthate. Other proton pump inhibitors are expected to interact similarly. (b) Bismuth subcitrate potassium Clinical evidence In one study, food reduced the bioavailability of a single tablet containing a combination of bismuth subcitrate potassium, metronidazole and tetracycline. However, the efficacy of this combined preparation for eradication of Helicobacter pylori did not seem to be affected (eradication rates reported at nearly 90%) and the authors suggested that this prolonged local exposure in the stomach may be clinically beneficial.2 The manufacturer notes that the reduced absorption of bismuth in the presence of food is not considered clinically relevant and they recommend that bismuth subcitrate potassium (Pylera) should be given after meals and at bedtime.3 The manufacturer of ranitidine bismuth citrate (Pylorid) noted that food causes a decrease in bismuth absorption which is not of clinical relevance. However, because of limited data that suggest increased ulcer healing when ranitidine bismuth citrate is given with food, they noted that it should preferably be taken with food.4 In a randomised study, 34 healthy subjects were given a triple therapy capsule Helizide (containing bismuth subcitrate potassium 140 mg, metronidazole 125 mg, and tetracycline 125 mg) at a dose of three capsules four times daily, with or without omeprazole 20 mg twice daily for 6 days. Omeprazole increased the maximum plasma levels and AUC of bismuth about threefold. However, the maximum plasma level achieved was 25.5 micrograms/L, which was still well below 50 micrograms/L, a bismuth level reported to be highly unlikely to cause toxicity.1 The authors also state that in clinical studies in which Helizide was given with omeprazole for 10 days to several hundred patients,2 no patient showed signs of encephalopathy, a notable toxic adverse effect of bismuth.1 In an earlier single-dose study in 6 healthy subjects, a single 240-mg dose of tripotassium dicitratobismuthate was taken one hour after the last dose of a oneweek course of omeprazole 40 mg daily. Omeprazole increased the AUC of bismuth fourfold, and increased its maximum plasma levels from 36.7 micrograms/L to 86.7 micrograms/L, which the authors pointed out approaches the considered ‘toxic range’ for bismuth (100 micrograms/L and above).3 (d) Tripotassium dicitratobismuthate Mechanism In a study in healthy subjects given tripotassium dicitratobismuthate (containing about 216 mg of bismuth) 2 hours before a standard breakfast, peak plasma levels of bismuth were found to be on average 64 micrograms/L around 30 minutes later; one subject had a bismuth level of 232 micrograms/L and ten others had a level greater than 50 micrograms/L. However, when the same bismuth compound was taken immediately after a standard breakfast, the bismuth levels were found to be lower (an average of 10.9 micrograms/mL, one subject levels were 120 micrograms/mL).1 The authors note that levels achieved in the fasted state are within the range associated with bismuth toxicity.1 As bismuth is thought to have a local effect, there is no advantage in it being absorbed. Nevertheless, the manufacturers recommend that tripotassium dicitratobismuthate (De-Noltab, containing 120 mg of bismuth oxide per tablet, usual dose of up to 4 tablets daily) should be taken half an hour before each of the three main meals of the day and 2 hours after the last meal of the day or taken twice daily, half-an-hour before both breakfast and the evening meal.5 The solubility and absorption of some bismuth compounds are known to be increased by decreased acidity of the stomach, which increases the risk of bismuth toxicity.1 Sa In a single-dose study in healthy subjects, bismuth carbonate (equivalent to 160 mg of bismuth) produced very low systemic levels of bismuth (no subject had a level greater than 2.7 micrograms/L) and food did not significantly affect its absorption.1 It therefore appears that bismuth carbonate may be taken without regard to food. (c) Ranitidine bismuth citrate 1. Madaus S, Schulte-Frohlinde E, Scherer C, Kämmereit A, Schusdziarra V, Classen M. Comparison of plasma bismuth levels after oral dosing with basic bismuth carbonate or tripotassium dicitrato bismuthate. Aliment Pharmacol Ther (1992) 6, 241–9. 2. Spénard J, Aumais C, Massicotte J, Brunet J-S, Tremblay C, Grace M, Lefebvre M. Effects of food and formulation on the relative bioavailability of bismuth biskalcitrate, metronidazole, and tetracycline given for Helicobacter pylori eradication. Br J Clin Pharmacol (2005) 60, 374–7. 3. Pylera (Bismuth subcitrate potassium, metronidazole, and tetracycline hydrochloride). Axcan Pharma Inc. US Prescribing information, May 2007. 4. Pylorid Tablets (Ranitidine bismuth citrate). GlaxoSmithKline UK. UK Summary of product characteristics, December 2005. 5. De-Noltab (Tripotassium dictratobismuthate). Astellas Pharma Ltd. UK Summary of product characteristics, July 2008. Importance and management The authors of the single-dose study recommended that the dose of tripotassium dicitratobismuthate should be halved if it is given with omeprazole because of the possibility of systemic bismuth toxicity.3 However, the manufacturers of tripotassium dicitratobismuthate say that the toxic range of bismuth is arbitrary and the small increase in absorption is not clinically relevant, except perhaps in patients with renal failure, in whom this bismuth compound should be avoided in any case.4 No clinically relevant effect would be expected if the use of omeprazole and either of these two bismuth salts is limited to the recommended 2-week regimen for resistant Helicobacter pylori infection. However, some caution might be appropriate with the longer term use of omeprazole and bismuth compounds. There appear to be no studies with bismuth compounds and other proton pump inhibitors, but as this interaction is due to changes in gastric pH, all proton pump inhibitors would be expected to interact similarly. 1. Spénard J, Aumais C, Massicotte J, Tremblay C, Lefebvre M. Influence of omeprazole on bioavailability of bismuth following administration of a triple capsule of bismuth biskalcitrate, metronidazole, and tetracycline. J Clin Pharmacol (2004) 44, 640–5. 2. O’Morain C, Borody T, Farley A, De Boer WA, Dallaire C, Schuman R, Piotrowski J, Fallone CA, Tytgat G, Mégraud F, Spénard J. Efficacy and safety of single-triple capsules of bismuth biskalcitrate, metronidazole and tetracycline, given with omeprazole, for the eradication of Helicobacter pylori: an international multicentre study. Aliment Pharmacol Ther (2003) 17, 415–20. Sample from Stockley's Drug Interactions, 10th Edition Gastrointestinal drugs 3. Treiber G, Walker S, Klotz U. Omeprazole-induced increase in the absorption of bismuth from tripotassium dicitrato bismuthate. Clin Pharmacol Ther (1994) 55, 486–91. 4. Yamanouchi Pharma Ltd. Personal communication, November 1994. Clinical evidence In a study, healthy subjects were given domperidone 10 mg four times daily and erythromycin 500 mg three times daily, alone and in combination. The maximum plasma level and AUC of domperidone were increased about threefold by erythromycin. In this study, domperidone and erythromycin alone were found to increase the QTc interval by 2.5 milliseconds and 4.9 milliseconds, respectively, whereas the mean increase in the QTc interval on concurrent use was 9.9 milliseconds, which was greater than the additive effect of each drug alone.1 (b) Ketoconazole In a crossover study in 10 healthy subjects, omeprazole 20 mg twice daily was given for 5 doses, with a single 10-mg dose of domperidone (as the free base or the maleate) given 4 hours after the last dose of omeprazole. Omeprazole had no effect on the AUC of domperidone given as either the maleate or the free base, and slightly decreased the rate of absorption of the free base (maximum level decreased by 16%).1 A single case report describes the development of myopathy and rhabdomyolysis in a patient 2 days after rabeprazole 20 mg daily and domperidone 6 tablets daily (strength not specified) were started. The patient had a creatine kinase level of 12 700 units/L (range 15 to 100 units/L) and a myoglobin level of 650 micrograms/ L (level usually less than 90 micrograms/L). The patient had no significant medical history and the domperidone and rabeprazole were prescribed to treat epigastric pain post-hysterectomy.2 Mechanism Rhabdomyolysis has rarely been reported with proton pump inhibitors,3 and the authors considered that rabeprazole itself, rather than the concurrent use of domperidone, was the likely cause in this particular case.2 Importance and management Omeprazole does not appear to cause a clinically relevant change in the pharmacokinetics of domperidone, and so no dose adjustment of domperidone is needed on concurrent use. The case of rhabdomyolysis with rabeprazole and domperidone is likely to be due to the proton pump inhibitor alone, and is not therefore an interaction. m pl Ketoconazole and erythromycin increase domperidone levels about threefold and further increase the QT prolongation seen with domperidone alone. Other CYP3A4 inhibitors might be expected to interact similarly, but the increase in QTc interval is probably only of concern for CYP3A4 inhibitors that themselves also prolong the QT interval, such as ketoconazole and erythromycin. (a) Erythromycin Clinical evidence e In many countries cisapride has been withdrawn from the market, or is only available for restricted use because of its potential to cause torsade de pointes, especially when cisapride levels are elevated.1 This can lead to cardiac arrest and sudden death. Cisapride is known to be metabolised by CYP3A4, and the manufacturers of many drugs known to inhibit this isoenzyme, even weakly, often still include contraindications for the concurrent use of cisapride because of the possible risk of torsade de pointes. For a list of clinically relevant CYP3A4 inhibitors, see ‘Table 1.9’ (p.9), but note that this list may not include every drug contraindicated for use with cisapride. Also, see ‘Drugs that prolong the QT interval + Other drugs that prolong the QT interval’, p.260, for a further discussion on the concurrent use of drugs that prolong the QT interval. Studies and reports of interactions with cisapride and their importance and management are summarised in ‘Table 27.2’ (p.1050). Domperidone + CYP3A4 inhibitors Domperidone + Proton pump inhibitors Omeprazole does not alter the pharmacokinetics of domperidone. An isolated case describes myopathy and rhabdomyolysis in a patient taking rabeprazole and domperidone. Cisapride + Miscellaneous 1. Ahmad SR, Wolfe SM. Cisapride and torsades de pointes. Lancet (1995) 345, 508. 1049 Sa In a study, healthy subjects took domperidone 10 mg four times daily and ketoconazole 200 mg twice daily, alone and in combination. The maximum plasma level and AUC of domperidone were increased about threefold by ketoconazole. In this study, domperidone and ketoconazole alone were found to increase the QTc interval by 1.6 milliseconds and 3.8 milliseconds, respectively, whereas the mean increase in the QTc interval on concurrent use was 9.8 milliseconds, which was greater than the additive effect of each drug alone.1 Mechanism Domperidone is metabolised by the cytochrome P450 isoenzyme CYP3A4, which is inhibited by drugs such as erythromycin and ketoconazole. Concurrent use therefore increases domperidone levels, which increases its modest effects on the QT interval after oral administration. Giving erythromycin or ketoconazole with domperidone therefore has more than additive effects on the QT interval. Importance and management Evidence for an interaction between domperidone and erythromycin or ketoconazole is limited. The manufacturers advise that the concurrent use of domperidone with other drugs that are potent inhibitors of CYP3A4 and that also prolong the QT interval should be avoided. They specifically name erythromycin,1,2 ketoconazole1,2 and ritonavir.2 This seems to be a very cautious approach, but may be prudent because alternatives to these combinations would usually be available. The increase in the QT interval due to increased exposure to domperidone caused by CYP3A4 inhibition alone would probably not be clinically relevant, but when added to the increase seen with erythromycin or ketoconazole alone (which at less than 5 milliseconds would not normally be considered to be clinically important, see ‘Drugs that prolong the QT interval + Other drugs that prolong the QT interval’, p.260), the increase is possibly of some concern. 1. Motilium 10 Tablets (Domperidone maleate). McNeil Ltd. UK Summary of product characteristics, December 2009. 2. Domperidone (Domperidone maleate). Wockhardt UK Ltd. UK Summary of product characteristics, January 2008. 1. Zhang YF, Chen XY, Dai XJ, Zhang YN, Liu QZ, Yu HL, Zhong DF. Influence of omeprazole on pharmacokinetics of domperidone given as free base and maleate salt in healthy Chinese patients. Acta Pharmacol Sin (2007) 28, 1243–6. 2. Bourlon S, Veyrac G, Armand C, Lambert O, Bourin M, Jolliet P. Rhabdomyolyse lors d’un traitement par rabéprazole (Pariet®), un inhibiteur de la pompe à protons associé à la dompéridone (Peridys®). Therapie (2002) 57, 597–600. 3. Clark DWJ, Strandell J. Myopathy including polymyositis: a likely class adverse effect of proton pump inhibitors? Eur J Clin Pharmacol (2006) 62, 473–9. Enteral feeds + Aluminium compounds and/or Sucralfate Aluminium-containing antacids and sucralfate can interact with highprotein liquid enteral feeds to produce an obstructive plug. Clinical evidence (a) Aluminium-containing antacids Three patients, who were being fed with a liquid high-protein nutrient (Fresubin liquid) through an enteral tube, developed an obstructing protein-aluminium-complex oesophageal plug when intermittently given an aluminium/magnesium hydroxide antacid (Alucol-Gel).1 Another report also describes the blockage of a nasogastric tube in a patient given aluminium hydroxide (Aludrox) with an enteral feed (Nutrison).2 (b) Sucralfate alone or with aluminium-containing antacids A number of reports describe the development of hard putty-like or creamy precipitations and encrustations that have blocked the oesophagus or stomach of patients given sucralfate with enteral feeds (Ensure Plus,3 Fresubin plus F,4 Glucerna,5 Jevity,5 or Osmolite6). Another patient developed this precipitate when given an enteral feed (Isocal) and sucralfate with aluminium/magnesium hydroxide.7 Similarly, a patient receiving a nasogastric feed (Pulmocare), sucralfate and aluminium hydroxide gel also developed an oesophageal bezoar, which was analysed and found to contain components of both the drugs and the enteral feed.8 Data from the French Pharmacovigilance system database found 16 adults and 5 newborn babies who developed bezoars while taking sucralfate; nasogastric feeding was identified as a risk factor.9 Mechanism It seems that a bezoar (a relatively insoluble complex) forms between the protein in the enteral feeds, and the aluminium from the antacids or sucralfate (sucralfate is about 18% aluminium). It thickens when the pH falls.3 Importance and management An established and clinically important interaction that can result in the blockage of enteral or nasogastric tubes. The authors of one report state that high molecular protein solutions should not be mixed with antacids or followed by antacids: if an antacid is needed, it should be given some time after the nutrients and the tube should be vigorously flushed beforehand.1 The authors of another report state that they feed for 18 hours daily and then give the sucralfate overnight without problems.2 The manu- Sample from Stockley's Drug Interactions, 10th Edition
© Copyright 2026