2014 OREGON’S HEALTH CO-OP PROVIDER MANUAL
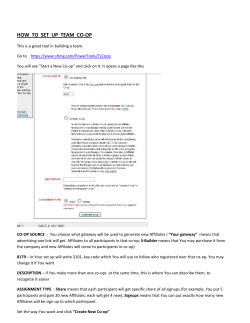
2014 OREGON’S HEALTH CO-OP PROVIDER MANUAL PROVIDER MANUAL | 2014 1. INTRODUCTION Contents 1. Introduction.............................................................. 1 2. Membership..........................................................3 3. Resources...............................................................8 4. Primary Care and Specialty Care..... 13 5. Prior Authorizations or Preauthorizations........................................... 15 6. Billing and Payment........................................ 18 7. Quality Improvement and Credentialing.........................................23 8. Pharmacy Program........................................ 31 Oregon’s Health CO-OP Oregon’s Health CO-OP is a new type of nonprofit health insurance company: a Consumer Operated and Oriented Plan enabled under the Affordable Care Act. We’re building a movement with providers, individuals, families and employers who believe the insurance industry can do better: where health insurance is driven by the members, in their communities; where everyday people have a voice, and health insurance companies listen. And where profits are returned to the members through lower premiums, more benefits and improved services. Our Envision Statement At Oregon’s Health CO-OP, we dare to stand for justice, for hope, for clean air, better schools and fresh water. Together, we dare to deliver on the promises of the Affordable Care Act. This is a dream that affords every Oregonian access to excellent health care. To do it, we will offer services and insurance products unlike anything you’ve seen in our industry. We are focused on positive change. Some have an agenda while we have friends who deserve better care. So to the naysayers we reply: Everyone is welcome at the CO-OP. Join us. 1 OREGON’S HEALTH CO-OP Oregon’s Health CO-OP Priorities • Prevention • Members’ access to the information and care they need, and in the way they want it • Patients and providers working together for better health • Cultural competence • Strategies to reduce providers’ administrative burden • Clear, predictable medical costs for members • Improved health for all Oregonians Oregon’s Health CO-OP Mission Guided by our members and our board of directors, Oregon’s Health CO-OP provides excellent health coverage that’s easy to use and understand. By reinvesting profits in our members, we improve service, reduce costs and ensure that members are protected for the long term. 2 Oregon’s Health CO-OP Care Philosophy Our role is to give a voice to our members and facilitate their engagement with you, their health professionals. Members, providers and the health plan will: • Take the best possible care of each other. • Keep costs down through low administrative, medical and pharmacy costs. All may choose to have a role in governing and operating this health plan. PROVIDER MANUAL | 2014 2. MEMBERSHIP Any Oregon resident or Oregon-based employer is eligible to enroll in our plans. We accept applications directly, through insurance brokers, and through Cover Oregon, the state’s online health insurance marketplace or exchange. Members’ Rights and Responsibilities Oregon’s Health CO-OP members are entitled to be treated in a manner that respects their rights, while also addressing their responsibilities. All rights and responsibilities may be extended to any person who may have legal responsibility to make decisions on their behalf regarding medical care. Member Rights • To refuse treatment, and in turn, be informed of the medical consequences of this action. • To refuse to sign a consent form if they do not clearly understand its purpose, or to cross out any part of the form they do not want applied to their care. • To change their mind about any treatment for which they have previously given consent. • To be informed of policies regarding Advanced Directives (living wills) as required by state and federal law. • To exercise these rights regardless of race, color, national origin, ethnicity, ancestry, religion, gender, marital status, sexual orientation, mental or physical disability, medical condition or history, age, source of payment for care, or any other category deemed protected under state and federal law. • To be treated with respect, dignity, compassion, and to be given the right to privacy. • To have timely access to their providers and to specialist referrals when medically necessary. • To have the expected consideration of privacy concerning their care and confidentiality in all communications and in their medical records. • To receive continuity of care and advance notice of the time and location of appointments, and of the providers providing care. • To be informed why various tests, treatments or procedures are ordered, to know who is providing them and any risks that may be associated with them. • To participate with providers in decisionmaking regarding their health care and treatment plans. 3 OREGON’S HEALTH CO-OP • To have an honest discussion of appropriate or medically necessary treatment options for their condition, regardless of cost or benefit coverage. • To participate, as much as possible, in understanding their health problems, including behavioral health, and developing agreed-upon treatment goals. • To have providers explain their diagnosis, the prognosis of their condition, and instructions required for care. • To inform Oregon’s Health CO-OP if they feel they are not receiving appropriate care. Member Responsibilities • To be on time for appointments or to contact the provider if they’re going to be late. • To contact the provider right away if there’s a need to cancel. If the provider has a policy for assessing charges regarding late cancellations or missed appointments, members will be responsible for such charges. • To identify themselves as Oregon’s Health CO-OP members and present their mostrecent identification card when requesting health care services. • To do their part to improve their own health condition by following instructions and care plans that they’ve agreed upon with the provider. • To provide, when possible, information about their health to providers so appropriate care may be provided. • To review their benefit booklet to ensure services are covered under the plan, and to contact Customer Service with any questions they may have about the plan. 4 • To follow Plan requirements to have services authorized before receiving medical care. • To accept financial responsibility for any copayments, coinsurance and deductible that may be associated with covered services. Member Benefits Oregon’s Health CO-OP member benefits include a comprehensive set of medical services, including but not limited to the Affordable Care Act’s 10 Essential Health Benefits. Summary of Covered Services: • Primary care and preventive services • Specialty services • Non face-to-face services • Inpatient services • Maternity and newborn care • Emergency and urgent care • Behavioral health (mental health and substance abuse treatment) • Rehabilitative services • Diagnostic testing • Imaging PROVIDER MANUAL | 2014 • Prescription drugs Member Appeal • Home health and hospice services “Appeal” includes any grievance, complaint, reconsideration or similar terms, and is either a written or verbal request from a member, the treating provider or identified personal representative. • Durable medical equipment and supplies • Orthotics and prosthetics • Ambulance transport • Acupuncture (with our SiMPLE plans) Member ID Cards • Access to health care benefits, including an adverse benefit determination made as a result of utilization review Plan: Name of Plan Primary Member: Martha Member ID Number: 12345647890DX Member Martha Member George Member Patsy Member Eleanor Member John Member ID Number 12345647890DX 12345647891DX 12345647892DX 12345647893DX 12345647894DX • Claims payment or handling for health care services Primary Specialist $XX / $XX Urgent/ER $XX / $XX Rx $X / $X / $X / $X Deductible $XX / $XX ohcoop.org front Customer Service: Local 503-488-2833, toll-free 1-855-722-8207 or TTY 1-800-73502900 Members: In an emergency, go to your nearest hospital or call 911. VSP: 1-800-877-7195 Provider: For Prior Authorization forms: ohcoop.org/providers Send claims to: Mail: Oregon’s Health CO-OP Electronic Payer ID: 21455 PO Box 40048 Portland, OR 97240 Pharmacists: For assistance, toll-free 1-855-577-6530 Catamaran - Bin: 610011 PCN: IRX Group: CORCOOP This card is for identification only and does not certify eligibility. back An appeal may apply to any of the following: • Matters pertaining to the contractual relationship between a member and Oregon’s Health CO-OP • Other matters as specifically required by law or regulation Guidelines Level One and Two Appeals and External Review Oregon’s Health CO-OP offers two levels of internal appeal. After internal levels are exhausted, the appeal may be eligible for external review by an independent review organization. Level One Internal Appeal The member or the member’s representative has the right to request an appeal within one hundred eighty (180) days of receiving written CO-OP Member ID Card-11.07.13 5 OREGON’S HEALTH CO-OP notification of an adverse benefit determination. If a member chooses to file an appeal, Customer Service will assist the member by accepting information over the phone about the appeal. Members may also submit their appeal in a written letter. If the appeal involves a pre-service authorization denial, it should be submitted in writing to: Oregon’s Health CO-OP Quality Improvement Appeal Coordinator PO Box 40048 Portland, OR 97240 Fax: 503-416-8118 If the appeal involves a post-service claim denial, it should be submitted in writing to: Oregon’s Health CO-OP Claims Reconsideration/Claims Appeals PO Box 40048 Portland, OR 97240 Attn: CO-OP Claims Appeals Coordinator Fax: 503-416-1301 We’ll acknowledge receipt of an appeal, in writing, within seven (7) calendar days. Internal appeals are reviewed by an employee or employees who were not involved in, or subordinate to anyone involved in, the initial decision. Upon completion of the review, the Appeal Coordinator will send a written response to the member. Appeals involving pre-service issues are responded to within fifteen (15) days. • Investigational post-service issues are responded to within twenty (20) working days. • Expedited reviews are responded to within seventy-two (72) hours of the receipt of the request. If the decision is not in the member’s favor, the member or member representative will be informed of the right to further appeal. Level Two Internal Appeal The member or the member’s representative may file a Level Two appeal. Requests for a Level Two appeal must be submitted within sixty (60) days of the receipt of an adverse determination at the first level. The member or member’s representative may submit written materials in support of the appeal. Documentation is compiled by the Appeal Coordinator then presented to an internal appeal panel. The panel’s voting members will not have been previously involved with the case. A written response is sent to the member in: • Fifteen (15) calendar days for pre-service issues. • Twenty (20) working days for post-service investigational procedures. • Thirty (30) days for all other appeals. 6 PROVIDER MANUAL | 2014 If the decision is not in the member’s favor, the member is informed of the right to file for review by an Independent Review Organization (IRO). External Review If the member has exhausted the internal appeal process (or has been deemed to have done so) and remains dissatisfied, and the issue is one of medical necessity, investigational supplies or services, continuity of care or whether a course or plan of treatment is delivered in an appropriate health care setting and with the appropriate level of care, the member or member representative may request external review within one hundred eighty (180) days of receipt of the previous level’s determination. An IRO is an independent organization employing physicians and other medically qualified individuals or experts. It acts as the decision maker for external appeals (regular or expedited), through assignment to the Plan via state regulatory requirements. The Independent Review Organization will provide to the member and/or appeal representative in writing: • Its decision • A full description of its rationale Oregon’s Health CO-OP agrees to be bound by the decision of the Independent Review Organization. The member or member representative may request external review by submitting the request to either Oregon’s Health CO-OP or to the state’s Director of the Department of Consumer and Business Services. The Appeal Coordinator/specialist will notify the Oregon Insurance Division of the receipt of a request for external review, and the Division will then assign the request to the next Independent Review Organization (IRO) on a rotating list. The appeal, including all documentation, will be delivered to the IRO within six (6) working days of assignment by the state. 7 OREGON’S HEALTH CO-OP 3. RESOURCES Care Management The Oregon’s Health CO-OP Care Management Group can help providers in caring for members with complex or co-morbid health care needs, including mental illness and chemical dependency. Care Management Program Referrals Potential candidates for Care Management service referral include: • Members with complex care needs and difficulty with self-management skills • Members transitioning home from a hospital or other inpatient facility • Members who need support in establishing and maintaining provider relationships The team of registered nurse case managers, behavioral health specialists and health care coordinators offers case management and care coordination services. • Members who have difficulty in accessing appropriate health care The team’s goal is to help members achieve the best possible outcomes from care, despite any physical and mental health challenges or economic obstacles that may exist. • Members who suffer from mental health and/or substance abuse issues • Members who have social support needs that interfere with their health care Referrals to Care Management can be made by: Care Management CO-OP Group • Providers In partnership with providers, Care Management helps members: • Members and their families • Navigate the health care system • Become actively engaged in their care • Improve self-management skills • Manage chronic conditions • Follow the treatment plan developed by their provider • Access community resources to address social support issues • Transition from one level of care to another • Access appropriate end-of-life care resources 8 • Members’ authorized representatives To make a referral: • Call the Care Management CO-OP Group at 503-416-1792. • Explain the reason for the call. • The Health Care Coordinator will either address the service need or forward the referral to a case manager. PROVIDER MANUAL | 2014 Network Relations Associates Oregon’s Health CO-OP Network Relations Associates (NRAs) are part of the Provider Services Department. They are assigned to physicians and hospitals based on geographic territories and health systems. The Network Relations Associates are dedicated to meeting the service needs of our contracted clinics, facilities and vendors. They are a link between our network providers and the Oregon’s Health CO-OP staff. The Network Relations staff maintains contractual agreements to develop a comprehensive network, ensuring member access. Contact a Network Relations Associate: • If you want to become a contracted clinic, facility or vendor with Oregon’s Health CO-OP. • You are already contracted and have questions about your agreement. Network Relations Associates provide certain information and trainings on site. Contact them to schedule: • Orientation to health plan operations, policies and procedures (upon contracting). • Refresher orientations for new clinic, billing or management staff as needed. eligibility, authorizations and claims/ payment detail) and the Oregon’s Health CO-OP website. IMPORTANT: Email or fax updates to the Network Relations teams about changes such as: • New or terminated providers or clinic staff • Locations • Phone and fax numbers • Email addresses. Timely updates facilitate accurate directory listings, mailings, correct claims payment and system access for your staff. Network Relations Associates collaborate with clinicians and other partners to address health care-related issues in the communities we all serve. We see their role as a partnership. Do not hesitate to contact your associate to discuss solutions/ideas or to schedule a meeting or training. Want to know the name of your Network Relations Associate or how to contact the associate? Click here: www.ohcoop.org/ providers/who-to-contact. If you can’t reach your Network Relations Associate, you’re welcome to contact Customer Service for assistance: Toll-free at 1-855-722-8207 or in the Portland area, 503-488-2833. • Targeted in-depth training on specific topics. • Training on using our online resources such as Provider Portal (verifies member 9 OREGON’S HEALTH CO-OP The Provider Portal Medical Record Review The Oregon’s Health CO-OP provider portal is a confidential online system that allows clinics and vendors to verify member eligibility and check the status of their authorizations and claims. Oregon’s Health CO-OP reviews medical records of contracted primary care providers on a regular schedule. Oregon’s Health CO-OP staff adheres to HIPAA-mandated confidentiality standards. The Provider Portal will be under construction through 2013. Prior to Jan. 1, 2014, we’ll include information on our website (www.ohcoop.org) that describes the process for registration and addresses what we believe will be frequently asked questions. We welcome your additional questions. To review the National Committee for Quality Assurance (NCQA) rules that direct the audit process, contact your Network Relations Associate. Clinical Best Practices and Health Promotion Guidelines Oregon’s Health CO-OP, through its Quality Improvement Committee (QIC), reviews and adopts evidence-based practice guidelines. These define standards of practice that pertain to improving the quality of health care for certain diseases, diagnoses and preventive services. A nationally recognized body of experts reviews these guidelines at least once every two years. After our Quality Improvement Committee approves them, we post the guidelines on our website. You can access this resource at (link coming soon). 10 Here’s a description of the process: 1.Oregon’s Health CO-OP’s Quality Improvement (QI) staff identifies a sample of contracted clinics to be reviewed. 2.QI mails a letter with patients’ names to each clinic. We ask clinic staff to send us a copy of those patients’ medical records. 3.QI Coordinators (registered nurses) review the medical records for legibility, content, organization and completeness. 4.The Quality Improvement department mails audit results to providers. A passing score is 90 percent or greater. A provider who does not receive a score of at least 90 percent is evaluated by an Oregon’s Health CO-OP Medical Director and/or by the internal Peer Review Committee. Oregon’s Health COOP may ask a provider to send us a written corrective action plan. Additional audits may occur. PROVIDER MANUAL | 2014 Reviewers verify that the medical records contain the following documentation: • Member information identified on each page by two (2) patient identifiers. • A problem list, with significant medical and/or psychological illnesses. • Presenting complaints, physical examinations, diagnoses, treatment plans and referrals or consultations as appropriate to each visit. • Lab results and diagnostic test reports. • Prescribed medications, including dosages and dates of initial/refill prescriptions. Allergies and adverse reactions, or documentation of no known allergies or history of adverse reactions. • Advance Directives: ›› Documentation of discussion with all members, if condition warrants, of advance medical planning. ›› Documentation of discussion must be noted in a prominent location in the medical record. • Health education, preventive screening and anticipatory guidance, as appropriate. • Provider identification or signature for each review visit note. Faxed, digital, electronic, scanned or photocopied signatures are acceptable. Signature stamps are not acceptable. Confidentiality Health care providers who transmit or receive health information in one of the Health Insurance Portability and Accountability Act’s (HIPAA) transactions must adhere to the HIPAA Privacy and Security regulations. Providers must provide privacy and security training to any staff members who have contact with individually identifiable health information. All individually identifiable health information contained in the medical record, billing records or any computer database is confidential, regardless of how and where it’s stored. Examples of stored information include clinical and financial data in paper, electronic, magnetic, film, slide, fiche, floppy disk, compact disk or optical media formats. You may disclose health information in medical or financial records only to the patient or legal guardian unless the patient or legal guardian authorizes the disclosure to another person or organization, or a court order has been sent to you. Health information may only be disclosed to those immediate family members with the verbal or written permission of the patient or the patient’s legal guardian. Health information may be disclosed to other providers involved in caring for the member without the member or member’s legal representative’s written or verbal permission. 11 OREGON’S HEALTH CO-OP Patients must have access to, and be able to obtain copies of, their medical and financial records from the provider. Information may be disclosed to insurance companies or their representatives for quality and utilization review, payment or medical management. Providers may release legally mandated health information to state and county health divisions and to disaster relief agencies. All health care personnel who generate, use, or otherwise deal with individually identifiable health information must uphold the patient’s right to privacy. Patient information (financial and clinical) must not be discussed with anyone who is not directly involved in the care of the patient or involved in payment or determination of the financial arrangements for care. Providers’ employees (including physicians) must not have unapproved access to their own records or records of anyone known to them who is not under their care. Oregon’s Health CO-OP staff adheres to the HIPAA-mandated confidentiality standards. 12 Release of Information Providers must obtain an authorization to release individually identifiable health information whenever information is released about the patient, unless the release is for payment, treatment of the patient, or the healthcare operations of another organization that is providing health care or payment for health care for the patient. • A general release of information form is not necessary for Oregon’s Health CO-OP and the providers to communicate regarding treatment or payment for treatment of Oregon’s Health CO-OP members, according to HIPAA privacy regulations. • The general authorization form is not valid for information regarding HIV, sexually transmitted diseases, genetic, mental health or alcohol and drug treatment information. Do not release this information unless the member signs an authorization specifying that these types of records may be released. PROVIDER MANUAL | 2014 4. PRIMARY CARE AND SPECIALTY CARE Responsibilities of Primary Care Providers Primary care providers will provide at least the following level of service to Oregon’s Health COOP members seeking care from them: • Maintain in the member’s record a comprehensive problem list which lists all medical, surgical and psycho-social problems for that patient. • Maintain a comprehensive medication list that includes all prescription medications that the member is taking and any medication allergies. This includes medications prescribed by specialists. • Provide accessible outpatient care within four weeks for any routine visit (e.g. preventive care). • Provide accessible outpatient care within 24 hours for any member with an urgent problem. • Provide access to telephone advice for member questions 24 hours per day. • Arrange specialty consultation with a network consultant within four weeks for any member with a non-urgent problem needing such consultation. • Arrange specialty consultation with a network consultant within 24 hours for any member with an urgent problem needing such consultation. • Have a policy and/or procedure that arranges for and provides access to an appropriate back-up physician or practitioner for any leave of absence you may have. Access to Care: Primary and Specialty Care It is the policy of Oregon’s Health CO-OP to ensure that our members have access to timely and appropriate preventive and curative health services that are delivered in a patientfriendly and culturally competent manner. Oregon’s Health CO-OP requires practitioners to have policies and procedures that prohibit discrimination in the delivery of health care services. Appointment Availability and Standard Scheduling Procedures • Provide preventive services as recommended by the U.S. Preventive Services Task Force (www.uspreventiveservicestaskforce.org). • Routine and follow-up appointments should be scheduled to occur as medically appropriate within four weeks. • Provide immunizations as recommended by the Centers for Disease Control and Prevention (www.cdc.gov). • Urgent care cases should be scheduled to be seen within 24 hours or as indicated in initial screening. 13 OREGON’S HEALTH CO-OP • Appointments for initial history and physical assessment should be scheduled in longer appointment slots to allow for preventive care and health education as needed. • Members should wait no longer than an average of 20 minutes for scheduled appointments. • Appointments for initial history and physical assessment should be scheduled in longer appointment slots to allow for preventive care and health education as needed. 24-Hour Telephone Access Oregon’s Health CO-OP has a commitment to its members to provide 24-hour phone access to health care. Our contracted primary care providers must have a telephone triage system. During Office Hours A primary care provider (physician, naturopath, osteopath, nurse practitioner or physician assistant) or registered nurse triages member calls to determine appropriate care and to assist the member with advice, an appointment or a referral. After Hours The Provider Services team conducts an annual after-hours survey to ensure that the following criteria are met. If you have questions, contact a Network Relations Associate at www.ohcoop.org/providers/who-to-contact 14 After-hours access includes: • Answering Service ›› Urgent situations: The person who answers the phone must offer to either page the provider on call (with the provider then calling the member) or to transfer the member’s call directly to the on-call provider. ›› Emergency situations: The person who answers the phone must tell the member to call 911 or go to the nearest emergency room if the member feels the situation is too emergent to wait for the provider’s call. • Answering Machine ›› Urgent situations: The outgoing message must instruct callers on how to page the provider in urgent situations. ›› Emergency situations: The outgoing message must provide information to callers about accessing emergency services, i.e., to call 911 or go to the nearest emergency room if the member feels the situation is emergent. PROVIDER MANUAL | 2014 5. PRIOR AUTHORIZATIONS OR PREAUTHORIZATIONS Definition Prior Authorization or Preauthorization is approval given by Oregon’s Health CO-OP in advance of a proposed hospitalization, treatment, supply purchase or other covered service, in accordance with Oregon’s Health COOP Policies and Procedures. Oregon’s Health CO-OP will provide authorizations for non-emergency covered services in the form of a Preauthorization and shall certify or recertify lengths of stay, if required, by telephone contact or other mutually agreeable form of communication between the Provider and Oregon’s Health CO-OP personnel, according to the Policies and Procedures. specialty or ancillary services if the specialist or ancillary provider has not previously seen the member. Specialists or ancillary providers are responsible for obtaining any required authorizations once they have seen the member, and the service that will be provided requires an authorization. • For elective ambulatory surgery and facility admissions, the admitting or performing provider is responsible for obtaining the authorization. The facility is responsible for verifying that an authorization was issued. • For urgent/emergent facility admissions, the facility is responsible for notifying Oregon’s Health CO-OP of the admission and for obtaining an authorization. • For inpatient stays, the facility is responsible for providing Oregon’s Health CO-OP with ongoing clinical review information daily or as requested in order to authorize the length of stay. For a current listing of services requiring preauthorization and printable authorization request forms, please see ohcoop.org/ providers/medical-management. • For obstetrical admissions, the facility must notify Oregon’s Health CO-OP of all admissions within one business day of the member’s admission Failure to obtain an authorization for any service that requires one, including a facility length of stay, will result in claim payment denial. • For deliveries, the facility must notify Oregon’s Health CO-OP of the date of delivery, type of delivery and discharge date. Hospital stays beyond federal guidelines (two days for vaginal delivery, four days for caesarean section) require authorization. Preauthorization Responsibilities Who’s responsible for preauthorizations? Primary care providers are responsible for obtaining any required authorizations for 15 OREGON’S HEALTH CO-OP Retroactive Authorization Requests Oregon’s Health CO-OP accepts retroactive authorization requests. When requests are submitted, an authorization decision is based on the member’s coverage, benefit rules and medical appropriateness criteria in effect at the time of the service. Because the service has already been provided, it may take Oregon’s Health CO-OP up to fortyfive (45) days from the date of the request to make a decision. Providers will receive written notification when the request is denied or approved. If a denial determination is issued, the provider cannot bill the member. Therefore, we recommend that providers submit authorization requests prior to the service being provided, whenever possible. Regardless of whether a retroactive authorization was issued, claims must be submitted to Oregon’s Health CO-OP within one year of the date of service. Authorization Determinations Prior authorization requests that are submitted with complete information, including correct coding, with relevant chart notes attached, allow Oregon’s Health CO-OP to make timely authorization determinations. Oregon’s Health CO-OP may take up to fourteen (14) calendar days to make prior authorization determinations. Additional time, up to fourteen (14) more days, is allowed if Oregon’s Health 16 CO-OP does not immediately receive all the information needed to make a benefit determination. Prior authorization decisions are based on benefit rules, guidelines and limits, Oregon’s Health CO-OP policies and, as appropriate, evidence-based practice guidelines. Concurrent review determinations are made within twenty-four (24) hours of notification. Oregon’s Health CO-OP may deny days if requested information is not provided in a timely manner. Review determinations are based on Interqual criteria for both the level of care and length of stay. In all cases, authorization determinations are based solely on plan benefits, medical appropriateness and the least costly alternative for the service requested. Oregon’s Health CO-OP does not reward staff for denying prior authorizations or facility admission or length-ofstay authorizations. Feel welcome to call the Oregon’s Health CO-OP Customer Service Department to request the criteria we use for authorization decisions. Authorization Time Frames and Number of Visits Authorization time frames and number of visits approved differ based on the type of service being authorized and any benefit limits that may exist. The authorization details for faxed requests will be included in the authorization response that you receive back via fax, or, for online authorization submittals, in the response you receive. A new authorization will be required if the previous authorization has expired or the number of visits has been exhausted. PROVIDER MANUAL | 2014 Denials and Appeals of Authorizations Denial Determinations • Benefit exclusion denials (benefit specifically excluded) are made by Oregon’s Health CO-OP staff. • Benefit limit denials (benefit specifically limited to number of visits or dollar amounts) are made by Oregon’s Health CO-OP staff. • All other denials, including facility admissions and lengths of stay, are made by a Medical Director. Appeals A Medical Director will review all appeals within thirty (30) days. Oregon’s Health CO-OP will communicate a written decision on an Appeal within forty-five (45) days of our receipt of all documentation reasonably needed to make the determination. The decision to uphold the denial or approve the requested service is sent in writing to the member, primary care physician or requesting provider, and specialist (when applicable) within one week of the decision. Decision making, which includes medical/ surgical services and equipment, pharmacy and chemical dependency, is based only on plan benefits and limitations, appropriate care, coverage guidelines and rules. Oregon’s Health CO-OP does not reward staff for denying authorization requests, and we do not use financial incentives to reward underutilization. Oregon’s Health CO-OP physician reviewers are available to discuss denial decisions. Contact Customer Service, 7 a.m. to 6 p.m. Monday through Friday, to schedule a time to speak with a physician reviewer: 503-488-2833 in the Portland metro area or toll-free 1-855-722-8207. 17 OREGON’S HEALTH CO-OP 6. BILLING AND PAYMENT Billing Address Provider Claims Oregon’s Health CO-OP PO Box 40048 Portland, OR 97240 Submit Claims To submit claims electronically, use EDI Payer ID 21455. For information on billing claims electronically, contact Emdeon toll-free at 1-877-363-3666 for EDI medical claims, and 1-888-255-7293 for EDI dental claims. Or visit www.emdeon.com/ProviderSolutions/ provider_billingmanagement.php to submit claims using the standard CMS (formerly HCFA) 1500 or UB04 claim forms. For more information, see instructions for completing the CMS 1500 or UB04 forms at www.cms.hhs.gov/manuals/downloads/ clm104c26.pdf and www.cms.hhs.gov/ manuals/downloads/clm104c25.pdf. Incomplete claims are denied for resubmission with the missing information. Claims must include the member’s ICD9 code to the highest level of specificity and the appropriate procedure codes(s). See OARs 410-130-0160 and 410-120-1280. 18 Oregon’s Health CO-OP will deny claims in the following circumstances with instructions to resubmit the claim with a valid diagnosis code: • Claims that use non-primary diagnosis codes for the primary or sole diagnosis. • Claims for services billed with an E-code as primary or sole diagnosis. • Claims with an invalid diagnosis or invalid procedure or revenue code. CMS has mandated that the ICD-9 diagnostic coding system be replaced by the more flexible ICD-10 CM and PCS system. The deadline for nationwide conversion is October 2014; Oregon’s Health CO-OP is preparing for the change. For more ICD-10 information, including key dates, please visit: www.cms.hhs.gov/ICD10/01_ Overview.asp#TopOfPage. Timely Filing Claims for covered services must be received within one year of the date of service to be considered eligible for payment. Timely Payment Oregon’s Health CO-OP agrees to pay a clean claim within the time required by applicable Oregon law. ORS 743.911 ORS 743.913 PROVIDER MANUAL | 2014 A clean claim is a bill for services, line item of service or all services for one Member on a claim form acceptable to Oregon’s Health CO-OP that can be processed without obtaining additional information from the provider of services or from a third party. A clean claim does not include a claim from a provider under investigation for fraud or abuse, or a claim under review for Medical Necessity. Claims Appeals Contact Oregon’s Health CO-OP Customer Service to appeal an action. An action includes but is not limited to the denial, in whole or in part, of payment for service. Reconsideration for Payment • Denied for missing information/ documentation not including authorization related denials • Duplicate claims • Timely filing denials Submit provider reconsideration/appeal requests, in writing, by completing the Provider Post Service Claim Reconsideration/ Appeal Form. Include the reason for the dispute and any relevant information and/or documentation related to the dispute. If the claim was denied because of authorization issues, please send current medical documentation with the appeal. Mail or fax written claim appeals to: Oregon’s Health CO-OP Claims Department Reconsiderations/Claims Appeals PO Box 40048 Portland, OR 97240 Attn: CO-OP Claims Appeals Coordinator Or fax written claims appeals to Provider Appeals Coordinator: 503-416-1301. Oregon’s Health CO-OP resolves the appeal and sends a notice of determination to the provider no later than 45 calendar days after the day the appeal is received. Post Service Provider Claim Appeal • Previously upheld reconsiderations for payment • Authorization related denials • Contract rate • Excluded benefits IMPORTANT: Oregon’s Health CO-OP must receive appeals no more than one year from the original processing date of the claim. Coordination of Benefits If a member has health care coverage under more than one health insurance plan, we will coordinate benefits with the health insurance plan to ensure the member receives the maximum coverage allowable under Oregon law. A set of rules governs coordination of benefits (COB) in Oregon. The plan that pays first is called the “primary plan.” The primary plan must pay 19 OREGON’S HEALTH CO-OP benefits in accordance with its policy terms without regard to the possibility that another plan may cover some expenses. The plan that pays after the primary plan is the “secondary plan.” The secondary plan may reduce the benefits it pays so that payments from all plans do not exceed one hundred percent (100%) of the total allowable expense. Clinical Editing Oregon’s Health Co-OP uses the OptumTM Claims Edit System® (iCES) to ensure the efficiency and accuracy of our claims payments. Clinical edits are based on OptumInsights’ Approved Sources for Edit Development, such as American Medical Association (AMA) Current Procedural Terminology (CPT) guidelines, Centers for Medicare & Medicaid (CMS) policies, National Correct Coding Initiative (NCCI) coding edits and specialty society recommendations, as well as policies developed by Oregon’s Health CO-OP. Actions of the clinical editing system include, but are not limited to: • Rebundling lab, X-ray, medicine, anesthesia and surgical procedure codes. • Denial warning message when surgery is inconsistent with the diagnosis. • Denial warning message on claims when a patient’s age does not fall into the normal age range for the procedure or diagnosis. 20 • Denial of a procedure considered integral to another billed procedure. • Denial of procedures not customarily billed on the same day as a surgical procedure. • Denial of services normally included as follow-up care associated with a surgical procedure. Because valid exceptions to clinical editing exist, Oregon’s Health CO-OP reviews records for unusual or extraordinary circumstances that may influence the benefit. Hold Harmless Network providers have agreed to accept our allowable fee as payment in full for covered services and supplies, whether paid by Oregon’s Health CO-OP, the member or another payer. As a network provider, this means you may charge our members only for deductible, coinsurance, copayments and non-covered services. Providers must hold the member harmless for any amounts identified below, which will be considered contractual adjustments. Please refer to your provider agreement for further clarification. • Charges above the maximum allowable fee You must not bill a member for any amount of your charge that is greater than the maximum allowable fee per your provider agreement. PROVIDER MANUAL | 2014 • Charges denied due to Oregon’s Health CO-OP You must not bill a member for any amount deemed a provider write-off based on Oregon’s Health CO-OP policies, including any services and supplies determined to be not medically necessary. • Charges related to associated claims Claims for associated services rendered to support any non-covered or not medically necessary service will be denied and may not be billed to a member. Services may include, but are not limited to, anesthesia, radiology, laboratory and hospital services. Associated claim denials may occur at any time: during pre- or post-payment reviews and/or on appeal. Overpayment Recovery Oregon’s Health CO-OP will conduct retrospective reviews of claims and reimbursements to Providers. Except in the case of fraud or abuse billing, any request for refund of a payment previously made to Providers shall be made in writing within 18 months — or, if for reasons relating to coordination of benefits, within 30 months — after payment was made, and shall specify why Oregon’s Health CO-OP believes the refund is owed. payment of the claim. If a request for a refund is not disputed in writing within 30 days after the request is received, the request will be deemed accepted, and Providers must pay the refund within 30 days after the request is deemed accepted. Overpayments identified by Providers shall be refunded within 60 days of identification of the overpayment by Providers. Notwithstanding the foregoing, Oregon’s Health CO-OP may at any time request a refund of a claim it has previously paid if liability is imposed by law on a third party and we are unable to recover from the third party because the third party has paid or will pay Providers for the services covered by the claim. If Providers fail to refund an uncontested overpayment within the time periods set forth in this section, Oregon’s Health CO-OP may withhold any overpayment amount from future payments for services rendered by Providers. If a refund is not timely received and we are unable to withhold overpayments from future payments, Oregon’s Health CO-OP may initiate a collection or legal proceeding to recover overpayment amounts; in a collection or legal proceeding to recover overpayment, Oregon’s Health CO-OP shall be entitled to recover its reasonable attorneys’ fees and costs incurred in such proceeding. If the refund is requested for reasons relating to coordination of benefits, Oregon’s Health CO-OP will include in the written request the name and mailing address of the other insurer or entity that has primary responsibility for 21 OREGON’S HEALTH CO-OP Locum Tenens Claims and Payments Oregon’s Health CO-OP allows licensed providers acting in a Locum Tenens capacity to temporarily submit claims under another licensed provider’s NPI number when that provider is on leave from his/her practice. The Locum Tenens provider must have the same billing type or specialty as the provider on leave, e.g., a physician must substitute for another physician. Oregon’s Health CO-OP is not responsible for compensation arrangements between the provider on leave and the Locum Tenens provider. Oregon’s Health CO-OP sends a payment to the billing office of the provider on leave. Per CMS guidelines, Oregon’s Health CO-OP allows Locum Tenens to substitute for another provider for 60 days. Providers serving in a Locum Tenens capacity should bill with Modifier Q6 to indicate the Locum Tenens arrangement. Interim Billing Oregon’s Health CO-OP reimburses for the first and subsequent interim billings for facilities not reimbursed at Diagnosis Related Group (DRG) rates. Interim claims must be submitted in sequential order and in 30-day increments or on a monthly basis. Each claim must include all applicable diagnoses and procedures. Facilities reimbursed based on DRG methodology are paid when the patient is discharged and the final billing is received. All authorization guidelines apply. Readmissions to Diagnosis Related Group (DRG) Hospitals The following readmissions within 15 days of discharge are considered part of the initial admission and are included in payment for the initial admission: • Additional surgery or follow-up care that was planned at the time of discharge. • Readmission for treatment of the same condition. 22 PROVIDER MANUAL | 2014 7. QUALITY IMPROVEMENT AND CREDENTIALING Program Goals Our Quality Improvement Program focuses on improvements that make health care: • Safer • More effective • More patient-centered • More timely • More efficient • More equitable Program Objectives Our Quality Improvement (QI) process is driven by the Oregon’s Health CO-OP mission and vision. Our objectives are to: • Ensure that members receive maximal health benefits from the resources available to Oregon’s Health CO-OP. • Monitor the health status of our members to identify areas that most significantly impact health status and/or quality of life. • Ensure the optimal use of health strategies known to be effective, including prevention, risk reduction and evidence-based practices. • Develop population-based health improvement initiatives that can best be implemented at a health plan level. • Ensure quality and accountability through measurement of performance and utilization. • Provide enhanced support for those with special health care needs through: ›› Proactive identification of those at risk. ›› Case management and coordination of fragmented services. ›› Promotion of improved chronic care practices. • Coordinate fragmented services by supporting integrated models of mental and physical health care services. • Participate in efforts that improve health care for all Oregonians by: ›› Supporting community, state and national health initiatives. ›› Building partnerships with other health care organizations. ›› Pursuing research on new models of health care design and delivery. ›› Seeking collaboration within the community to identify and eliminate health care disparities. To meet these objectives, we have a process for prioritizing QI projects that is consistent with our mission, vision, care philosophy and values. The process is based on the following parameters: 23 OREGON’S HEALTH CO-OP • Improve our members’ satisfaction. • Focus on high-volume, high-risk areas that have a significant impact on members’ health. • Have measurable outcomes in terms of quality of life and/or health resource utilization. • Involve programs or interventions that are confirmed to improve outcomes, or that can be evaluated to find out if outcomes will improve. • Align with efforts by provider groups, community groups and other health plans focused on improving the health of Oregonians. • Promote or improve models of care that can be broadly generalized in the health care system, such as the chronic care model or the Patient Centered Primary Care Home initiatives. • Focus on areas that have a significant impact on a population with exceptional needs and those individuals with potential for risk. QI Program Committees • Pharmacy and Therapeutics Accountable for oversight of the Oregon’s Health CO-OP pharmacy program, the development and maintenance of the Oregon’s Health CO-OP formulary and programs that impact utilization. 24 • Medical Benefits Assurance Accountable for oversight of the Oregon’s Health CO-OP Medical Benefits Assurance Unit and approval of medical policies and new technology assessments. • Quality Improvement Advisory committee that provides oversight and direction for Oregon’s Health CO-OP initiatives that impact the quality of care for our members. • Peer Review Accountable for monitoring and ensuring the quality of care and service provided by individual contracted providers. • Service Quality Accountable for identification of issues impacting the satisfaction of our members through the analysis and integration of information from multiple sources. •Credentialing Accountable to ensure that Oregon’s Health CO-OP offers a high quality panel of providers to our members. It is also accountable for delegation oversight. PROVIDER MANUAL | 2014 Scope of Service and Issues Reviewed Our Quality Improvement Program defines the processes that we measure and monitor. Major plan components include processes involved with quality outcomes, patient safety and service as they pertain to access, availability and satisfaction. The scope of service also includes any and all regulatory requirements. Oregon’s Health CO-OP has determined that areas in which our members receive care and service should be monitored and evaluated for opportunities for improvement. These areas include: • Hospitals • Urgent care centers • Primary care clinics • Community health centers • Consultation services • Vision clinics • Dialysis centers • Hospices • Skilled nursing facilities • Drug and alcohol dependency facilities • Health departments The areas listed above encompass the care and services delivered by our network providers. Network providers of care to our members are all primary care providers and specialists. Behavioral health providers are included in the Quality Improvement process. These providers offer chemical dependency treatment, smoking cessation and mental health services. Issues reviewed by the Quality Improvement Committee include, but may not be limited to: • Selected Health Employer Data Information Set (HEDIS) indicators • Access to care • Patient satisfaction • Outcomes of care • Patient safety • Compliance with government regulations Data sources may include claims data, medical record data, patient complaints (grievances), case management reports, pharmacy data, satisfaction surveys and Quality Improvement projects. Research analysts, quality program staff and Information System (IS) staff may use data elements to develop a reporting format that is reviewed and evaluated by the Quality Improvement Committee. The QI Committee uses data to recommend interventions aimed towards improvement. Any member-specific or provider-specific data are considered confidential and treated according to Oregon’s Health CO-OP policy. This policy is fully congruent with HIPAA regulations. The appropriate sources receive feedback with findings, conclusions and recommendations. The Quality Improvement Program staff prepares a yearly evaluation of the program and presents it to the QI Committee for review. The following year’s program is built from this evaluation. 25 OREGON’S HEALTH CO-OP Credentialing Initial credentialing: The application for provider status of a provider who is new to the Oregon’s Health CO-OP panel, or a provider who has terminated more than thirty (30) days prior to applying and is requesting reinstatement. Recredentialing: The process of periodically re-evaluating current panel providers for continuing competency to provide high quality services to Oregon’s Health CO-OP members. General Guidelines Most providers must complete a credentialing application when contracting with Oregon’s Health CO-OP. Providers who are subject to the credentialing process include: • Certified Nurse Midwife • Doctor of Medicine • Doctor of Naturopathy • Doctor of Osteopathy • Doctor of Podiatric Medicine • Nurse Practitioner • Physician Assistant • Occupational Therapist • Speech Therapist • Physical Therapist On an ongoing basis, we review providers’ practice utilization data, member complaints, quality of care assessments and any changes in application status. Oregon’s Health CO-OP credentialing process maintains a “professional misconduct” policy to ensure the safety of our members. This policy guides the Credentialing Committee in the decision-making process when incidents of inappropriate sexual behavior are identified. During the credentialing process, our Credentialing Committee may deny, suspend or terminate a provider’s participation with the plan. The revised Fair Hearing Policy outlines the process for providers to appeal and/or challenge an adverse action. Fair hearing is offered to both initial and recredentialed providers. If you have questions, please contact your Network Relations Associate. Initial Credentialing Providers interested in joining the network serving Oregon’s Health CO-OP members must submit a signed and dated Oregon Practitioner Credentialing Application, along with the following information: • Audiologist • Signed and dated attestation questions. • Behavioral Health/Chemical Dependency Specialist • Attachment A, referring to the attestation questions answered “yes.” • Licensed Acupuncturist • Signed and dated Authorization and Release of Information form. 26 PROVIDER MANUAL | 2014 • Evidence of current licensure by State of Oregon (copy of wallet-sized license is sufficient). • Evidence of current DEA certification or prescriptive privileges, if applicable. • Evidence of current professional liability insurance coverage in the amount of no less than $1 million per incident and $3 million aggregate, or equivalent protection. • Copies of specialty board certificate(s), if applicable. • Copy of current curriculum vitae. Recredentialing All credentialed providers are recredentialed at least once every three years. Ninety days before the provider’s recredentialing date, Oregon’s Health CO-OP sends a recredentialing packet to the provider. The following information is needed to complete the recredentialing process: • Copy of state license. • Current DEA registration and proof of prescriptive privileges, if applicable. IMPORTANT: The applicant must inform Oregon’s Health CO-OP within 30 days if changes occur to any statements on the application. • Current professional liability insurance coverage in the amount of $1 million per incident and $3 million in aggregate, or equivalent protection. Oregon’s Health CO-OP’s Credentialing Committee reviews the initial application documents, including the provider’s application, attached documents, verification of state licensure, National Practitioner Data Bank report, closed claim reports, license action report, Medicare Opt-Out Report, any patient complaints about the provider and site visit reviews (for primary care providers only). • The Oregon Practitioner Recredentialing Application, including: Education, work history and call coverage are also elements of the review process. The Credentialing Committee may request additional informationif necessary. The Credentialing Committee recommends acceptance or rejection of the application. The Oregon’s Health CO-OP Network and Quality Committee (a subcommittee of the board) grants final approval. ›› Signed and dated attestation questions ›› Attachment A, referring to attestation questions answered “yes” ›› Signed and dated Authorization and Release of Information form Our Credentialing Committee considers this information along with the National Practitioner Data Bank inquiry results, closed claim reports, license action report, Medicare Opt-Out Report and member complaints. Failure to provide recredentialing information in a timely manner may be brought to the attention of the Oregon’s Health CO-OP Credentialing Committee. Noncompliance may result in a recommendation to send the provider a notice of termination. 27 OREGON’S HEALTH CO-OP Providers’ Rights: Policy and Procedures Background Oregon’s Health CO-OP considers it essential to maintain a provider panel that has the legal authority, relevant training and experience to provide care for our members. Provider rights ensure that all participants in the credentialing process are aware of their rights during the credentialing process. We advocate for provider rights to be readily accessible and understandable to all providers. Policy The Oregon’s Health CO-OP Credentialing Unit adheres to the following provider rights and notifies each provider of these rights during initial credentialing and at the beginning of each recredentialing cycle. This policy applies to all records maintained on behalf of the Oregon’s Health CO-OP provider panel and is limited to the credentials and performance improvement files of individual practitioners. NOTE: References from peers and other recommendations are protected information that is excluded from this list of rights. Oregon’s Health CO-OP has adopted the following statement of provider rights that applies to all contracted medical professional providers. Providers are notified of these rights in two ways: 28 • The Provider Rights document is included with the Initial /Recredentialing applications. • Provider rights are documented in the Provider Manual. Providers in the credentialing/recredentialing process have the following rights: • To be free from discrimination in terms of participation or indemnification solely on the basis of licensure, as long as providers are acting within the lawful scope of licensure/certification. • To be notified in writing of any decision that denies participation on the Oregon’s Health CO-OP panel. • To be aware of applicable credentialing/ recredentialing policies and procedures. • To review information submitted by the applicant to support the credentialing application. • To correct erroneous information submitted by third parties that does not fall under the Oregon Peer Review Statute protections (Section 41.675). • To be informed of the status of their credentialing or recredentialing application on request, and to have that request granted within a reasonable period of time. • To be notified of these rights. Source: NCQA Standard CR 1, Element B; 42 CFR 422.202(a) and (c) PROVIDER MANUAL | 2014 Procedures Responsibility Actions Provider A provider has the right to examine his or her credentialing folder. Request to review your credentialing file by asking (written, electronic or telephone) the Oregon’s Health CO-OP Quality Improvement Manager/Chief Medical Officer to schedule a review time. Make this request at least 24 hours in advance of your preferred review time. You must present a driver’s license or other photo identification before reviewing the file. Staff from the Quality Management Department/ Credentialing Unit must supervise a provider during the examination/review. Sufficient time must be allowed for providers to review their credentialing file. Review time must be mutually agreed upon by the provider and credentialing specialist. Records may not be removed or copied unless expressly permitted by the chief medical officer or a designated representative. You have the right to receive a copy of any document (s) in your credentialing folder that you submitted or that were addressed or copied to you. If you file an appeal, you are entitled to full access to your credentialing/ recredentialing and Quality Improvement (QI) folder(s). After you review your file according to this policy and procedure, you may submit a written request to the chief medical officer that asks for corrections or deletions of information in the file. The request must include a statement of the basis for the action requested. Chief Medical Officer Review a provider’s requests for correction or deletion of information within thirty (30) days and recommend to the Credentialing Committee whether or not to honor the request(s). 29 OREGON’S HEALTH CO-OP Responsibility Actions Credentialing Committee Notify the provider in writing within two (2) weeks of the committee’s decision. The decision of the Credentialing Committee is final. Provider You may clarify discrepancies by providing documentation such as a license, malpractice claims history or board certification decisions. You must submit this information in writing (electronic or hard copy) within two weeks of receiving the request. Information obtained from you becomes part of the credentialing application. Credentialing Specialists Send a copy of the document to the provider if he or she does not have it. Review new information with the provider by phone. Write a summary memo based on the provider’s own words. Note the review date on the memo and initial the date. If the provider does not provide information that clarifies discrepancies within the two-week time frame, process the application. Assess extensions on a case-by-case basis. Inform the Quality Improvement (QI) manager of any delinquencies related to providers and information discrepancies. Organizational Credentialing Oregon’s Health CO-OP credentials institutional providers or suppliers such as hospitals, skilled nursing facilities, home care agencies, behavioral health services, clinical laboratories, outpatient speech and physical therapists, ambulatory surgery centers, end-stage renal 30 disease services, outpatient diabetes selfmanagement training, portable X-ray providers, rural health centers and Federally Qualified Health Centers. A standardized application is used for this process. PROVIDER MANUAL | 2014 8. PHARMACY PROGRAM • Drugs used for non-medically accepted indications. Oregon’s Health CO-OP Formularies • Drugs used to promote fertility or to treat sexual dysfunction or disorder in either men or women. The Oregon’s Health CO-OP Formulary is a list of covered drugs selected by a pharmacy and therapeutics committee to treat medical conditions that are covered by Oregon’s Health CO-OP. General Formulary Information Formulary decisions are based on critical review of the available scientific evidence for efficacy, safety, outcomes, cost-effectiveness and value. In general, the following are not covered: • Brand name drugs for which FDA approved and equivalent generic drugs are available, except select “narrow therapeutic index” drugs. • Experimental or investigational drugs, or drugs used in a research study or in another similar investigational environment. • Over-the-counter (OTC) drugs or medications or vitamins that may be purchased without a prescription, or prescribed drugs that are available in an OTC therapeutically similar form. • Drugs not listed in the formulary. • Drugs removed from the formulary throughout the year by the pharmacy and therapeutics committee. The drug names are then posted on our website at (link coming soon). • Drugs used for cosmetic purposes or hair growth. • Drugs used for treatment of obesity or weight loss. • Drugs used as a preventive measure against the hazards of travel. • Growth hormone except to treat documented growth hormone deficiencies. • Other drugs specifically excluded from coverage, such as drugs not approved by the FDA, including compound drugs from bulk powder, and DESI drugs. The formularies apply only to drugs provided by a pharmacy and do not apply to drugs used in an inpatient setting or furnished by a provider. The drugs listed in the CO-OP formulary might have copays or coinsurance that may change from year to year. For more information, visit the Provider Portal or contact Customer Service at 503-488-2833 or toll-free, 1-855-722-8207. Drugs that require prior authorization or step therapy, or that carry age restrictions or quantity limits, are designated as PA, ST, AR and Qty Limit, respectively. Drugs labeled PA or PA required require prior authorization before a member can fill the prescription at a network pharmacy. 31 OREGON’S HEALTH CO-OP Drugs labeled ST or Step Therapy are limited to coverage only when certain conditions have been met—for example, the member has an approved claim for a formulary alternative in his or her prescription profile. The member or provider must submit a Formulary Exception form if ST criteria are not met and the member does not have claims history of the prerequisite drug. Drugs labeled AR or Age Restriction require the member to be younger than or older than a specific age. For example, a drug may be restricted to those under age 6 or over age 16. The member or provider must submit a Formulary Exception form if member does not meet age criteria. Drugs labeled QTY, QL or QTY Limit are restricted to specific quantities. If a provider or member wants to exceed the limit, a Formulary Exception form must be submitted. To obtain prior authorization or request a formulary exception, fax a completed Prior Authorization or Formulary Exception form, available at (link coming soon). Providers will receive a faxed response which may include an approval, denial or request for additional information in support of medical necessity no later than 72 hours of receipt. The formula and formulary updates are on our website at (link coming soon). Note: We’ll post formulary updates by the 15th of each month. 32 Please contact Oregon’s Health CO-OP Customer Service at 503-488-2833 or toll-free at 1-855-722-8207 if: • You would like a paper copy or additional copies of the formulary book. • You want formulary updates. • You have questions or concerns about the pharmacy benefit or formulary. • You have suggestions for formulary changes or have questions related to pharmacy claims. Office Administered Injectables Requiring Prior Authorization Some drugs require prior authorization when furnished by and administered incident-to a physician’s service in a clinic or facility. For more information, please refer to the Injectables/Medications Administered Under the Medical Benefit Authorization Policy web link here. To request prior authorization, please complete the appropriate Injectables Billed to the Medical Benefit Form available here add web link here, attach medical record information in support of medical necessity (including diagnosis, co-morbidities and treatment history), and fax all documents to Oregon’s Health CO-OP at 503-416-1308. PROVIDER MANUAL | 2014 Drug Denials, Appeals and Retro Authorizations Oregon’s Health CO-OP pharmacist and Medical Director are available to discuss drug denial decisions. The benefit provisions, guidelines or criteria on which the denial decision was based are available upon request by contacting Customer Service at 503-488-2833 or toll-free at 1-855-722-8207. Oregon’s Health CO-OP will request medical records for a thorough review of the appeal. Retro authorizations are accepted. For more information, please refer to Section 5 of this Manual, Prior Authorizations or Preauthorizations. Oregon’s Health CO-OP looks forward to being partners in improving the health and well being of Oregonians. 12.09.13 33 OREGON’S HEALTH CO-OP www.ohcoop.org facebook.com/oregonshealthcoop twitter.com/orhealthco_op OHC-PR-Provider Manual-103-11.13 12.10.13 38
© Copyright 2026