Session New ESGENA Conference
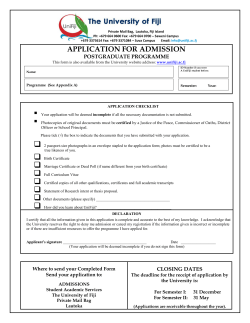
Weekend Edition October 18/19, 2014 Vienna, Austria 22nd United European Gastroenterology Week Session Session New ESGENA Conference Postgraduate Teaching Programme Advanced Endoscopic Techniques Sunday, 08.30 – 10.30 Hall A Postgraduate Teaching Programme Terminal GI Cancer Sunday, 11.00 –13.00 Hall B UEG launches the Young GI Network Let’s Meet! Event Sunday, 17.00 Welcome to the ESGENA conference delegates Welcome to the Postgraduate Teaching Programme in Vienna! Professor Guido Costamagna (Editor-in-Chief, UEG Week News) & Professor Magnus Simrén (Chair, UEG Scientific Committee and Editor, UEG Week News) Those delegates who attended the Postgraduate Teaching Programme in previous years will notice a change in the format of this year’s programme. The key theme this year is ‘interactive learning’. In 2014, the Postgraduate Teaching Programme will incorporate a greater than ever mix of teaching methods with increased opportunities for discussion and debate, including live demonstrations and case-based teaching sessions involving small groups of delegates. We are also pleased to include two live endoscopy sessions as part of the programme – take a look at the separate article in this edition of the UEG Week News. The 2-day programme comprises worldclass education for training and practicing gastroenterologists alike. The programme is expected to attract gastrointestinal (GI) physicians and general practitioners with an interest in GI and hepatology topics, alongside fellows in training and established physicians currently without expert- or specialist-level knowledge of the field. There is no age restriction for delegates attending the Postgraduate Teaching Programme. UEG is committed to promoting education and training and in this regard, the Postgraduate Teaching Programme has been incorporated into a 3-year, rolling curriculum. This is in response to feedback from delegates attending previous years’ meetings and the need to build on the success of these meetings. The curriculum consists of clinically important topics within the areas of GI, liver and pancreatic diseases. Delegates who attend the 2-day Postgraduate Teaching Programme over three consecutive years will receive information covering all major updates in these areas, which will hopefully boost their professional careers. Attending the Postgraduate Teaching Programme on a yearly basis is therefore a smart move to keep abreast of state-of-the-art updates and topics in clinically relevant topics. Professor Guido Costamagna Professor Magnus Simrén Editor-in-Chief, UEG Week News Università Cattolica del Sacro Cuore, Rome, Italy Chair, UEG Scientific Committee and Editor, UEG Week News Sahlgrenska University Hospital, Gothenburg, Sweden This year’s Postgraduate Teaching Programme also offers delegates the opportunity to personalise the programme by selecting sessions according to their educational needs. A Syllabus is available as a further educational tool consisting of additional information on the presentations in the Programme; be sure to pick up your USB-stick containing the Syllabus at the distribution counter in the entrance hall of the conference centre. New for 2014 is the ability to view all presentations (except for live endoscopy sessions) from the Postgraduate Teaching Programme via live streaming. So, if you’re held up at your hotel or arriving late from the airport, there’s no need to miss out on that important session. Visit www.ueg.eu and register for access to live-streamed videos. We hope that you find the Postgraduate Teaching Programme useful to expand your knowledge base, stimulate new ideas and create lasting educational collaborations with colleagues. We also hope that you stay in Vienna to attend UEG Week. Take a look at the UEG Week News for more news from all the events taking place in conjunction with UEG Week. Tweet us at #UEGWeek Each day, we’ll publish our favourite tweets throughout the newspaper. Tweet us at #WeekChat www.ueg.eu/week UEG Week News UEG Week Keep Connected UEG Booth Find out more about the work we do. Opening Hours Main Entrance Hall, Ground Floor Saturday October 18 08.00 – 17.00 Sunday October 19 08.00 – 17.00 Monday October 20 08.00 – 17.00 Tuesday October 21 08.00 – 17.00 Wednesday October 22 09.00 – 14.00 Wifi WiFi in the foyers and in the exhibition halls allow easy access to the Internet. Please select the WiFi network: UEG Week Connecting with colleagues at UEG Week Scientific Programme Hands-on @ UEG Week Practise and perfect your endoscopic techniques, interact with experienced medical colleagues and learn about the uses of ultrasound. offers delegates the ideal opportunity of learning in small groups. These Handson Sessions are organised in co-operation with ESGE. Head to the ESGE Learning Area to watch and learn as experts demonstrate endoscopic procedures with cutting-edge equipment. You will have the opportunity to interact, ask questions and practise the techniques yourself – all under the watchful eye of a personal tutor. Each Hands-on Session lasts 90 minutes. Hands-on Endoscopy @ UEG Week, ESGE Learning Area For those attending the ESGENA Conference, Hands-on training forms part of the core Scientific Programme and Register on-site at the ESGE desk to book your place on one of the Saturday, Sunday or Monday sessions, or walk straight into the Tuesday and Wednesday demonstrations Throughout UEG Week, the Ultrasound Learning Centre will offer all delegates the opportunity to have individual, Hands-on training on the use of ultrasonography for Stay in touch with your colleagues and easily create new connections at UEG Week via Facebook, Twitter and LinkedIn. E-learning: Meet the editors Gastroenterology trainees and young fellows can now join the Young GI Network Facebook group. At lunchtime on Monday, don’t miss the chance to meet the editors of UEG’s online learning platform (Monday, 13.00 – 13.30, Education Lounge). Connect, participate and be active on social media; discover more on the UEG website: www.ueg.eu! Get social Use the official hashtag #UEGWeek or post on the UEG Facebook group to share your thoughts, snaps and ‘selfies’. Conversations will appear on the Social Wall – see what’s trending via the UEG Week App, or have a look online and on big screens around the congress venue. Go on post your UEG Week photos and selfies now! Find out whether you are today’s winner of Tweet of the day, Facebook quote of the day or the selfie contest. Tweet us on @my_ueg #uegweek Since 2009, UEG E-learning has established itself as one of the richest educational resources in gastroenterology, and we continue to work hard to make it even better. Project Manager within the UEG Secretariat - Ben Smith and Web Editor Dr Tomer Adar will discuss their plans for 2015. They have ideas for new online courses, including ones aligned to the Gastro Blue Book. This is a great opportunity to find out how to get involved. The team is particularly keen to hear from you if you wish to contribute to, or even author new courses, so come along and share your ideas. Courses Discover a world of learning at www.ueg.eu/education www.ueg.eu/week Library diagnosis and intervention. This gives you the opportunity to see for yourself the practical applications of ultrasonography under the guidance of experts. Experienced medical colleagues will be there to teach beginner and experienced gastroenterologists alike about the technique. Hands-on Ultrasonography @ UEG Week, Ultrasound Learning Centre Check your programme for times and courses. Whether you’re a beginner or experienced, training is tailored to all levels and will run from Saturday to Wednesday Tweet of the day The Education Lounge Drop by to learn more about UEG’s educational initiatives and discover our full range of accredited courses. @my_UEG Some people really do like to make an effort when attending a congress #uegweek Spencer Gore @SJGore More at https://www.ueg.eu/education Learn online Register for a free myUEG account. Current online courses include: •Acute gastroenteritis (in association with ESPHGAN) •Dyspepsia (worth 4 European CME credits) • Feeding difficulties (in association with ESPHGAN) The universal source of knowledge in gastroenterology Latest News For those, who prefer to read the newspaper online, please visit the UEG Week website (www.ueg.eu/week) and download an online issue. ESGENA welcomes you to Vienna! Welcome to Vienna for the 18th European Society of Gastroenterology and Endoscopy Nurses and Associates (ESGENA) Conference in conjunction with the 22nd UEG Week. At a glance Free paper session encompassing a diverse range of subjects pertinent to clinical practice (Session 3) Sunday October 19 11.00 – 12.30 Hall G/H Michael Ortmann President of ESGENA & Ulrike Beilenhoff ESGENA Scientific Secretariat This year, the three-day ESGENA Conference will be hosted by ESGENA and the Austrian Society of Endoscopy and Gastroenterology Nurses and Associates (IVEPA) and will run from Saturday to Monday (October 18 – 20). The theme for the ESGENA Conference is to maximise learning by using interactive formats. The Conference includes state-of-the-art lectures, free papers and posters, hands-on training and a platform from which nurses can network with their international colleagues. The ESGENA Scientific Programme incorporates hands-on training sessions during which delegates will use biosimulators for learning new procedures or fine-tune their existing endoscopic techniques. We anticipate that these sessions will be extremely popular and because this particular training works best in small groups, entrance to the sessions will be limited to ticket holders. Tickets for these handson training sessions are available at the entrance of the European Society of Gastrointestinal Endoscopy (ESGE) Learning Area, so get your ticket early to avoid disappointment. The ESGE Learning Area is equipped to provide an expert practical teaching arena. It has accomplished physicians and nurses available to promote good endoscopy techniques, demonstrate the latest developments in endoscopy and support training in small groups. There will be parallel workshops during the ESGENA Conference, which will be conducted primarily in English, but with some in German. Workshop sessions will cover a range of topics pertinent to today’s nurses and associates, including an update on the management of patients with inflammatory bowel disease, how to structure audit or research investigations and the application of electrosurgery in the gastrointestinal setting. There are also parallel lecture sessions covering a variety of themes, such as the care of patients undergoing endoscopy, endoscopic techniques, in addition to free paper and poster round sessions. Session 3 on Sunday (11.00 – 12.30, Hall G/H) is a free paper session encompassing a diverse range of subjects pertinent to clinical practice, including endoscopic mucosa resection of large benign colonic polyps, improving the experience and satisfaction of children and patients undergoing endoscopic procedures and the oral health status of patients with liver cirrhosis. The poster rounds will also take place on Sunday (12.30 – 14.30 and 16.30 – 17.00, Lobby of Hall G/H) and include posters under general themes, such as patient preparation, sedation and endoscopic procedures. Awards for the best free paper and best poster will be presented on Monday (Session 9, 09.00 – 10.30, Hall F1). We hope that you find the ESGENA Conference useful to expand your knowledge base, stimulate new ideas and create lasting educational collaborations with colleagues. Poster rounds Sunday October 19 12.30 – 14.30 and 16.30 – 17.00 Lobby of Hall G/H Awards for the best free paper and best poster (Session 9) Monday October 20 09.00 – 10.30 Hall F1 Michael Ortmann President of ESGENA University Hospital, Basel, Switzerland UEG Week News Postgraduate Teaching Programme CRC screening and the detection of early-stage cancer Postgraduate Teaching Programme Clinical case scenarios: Managing patients with terminal GI cancer Cancers of the gastrointestinal (GI) tract are among the most common worldwide, causing a high proportion of cancerrelated deaths.1 Much of the difficulty with treating these cancers arises from their late diagnosis, with many patients seeking medical attention only when they have symptoms and the disease is already in the advanced stage.2,3 So, the care of patients with advanced and terminal GI cancers will continue to be an important element for medical staff. Interested in learning more about CRC care? Don’t miss Monday’s Symposium, ‘European guidelines on treatment of colorectal cancer’ Monday October 20 14.00 – 15.30 Hall E A clinical case-based session on Sunday (11.00 – 13.00, Hall B) will explore how best to care for patients with terminal GI cancers. Chaired by Professor Marco Bruno (Erasmus Medical Center, Rotterdam, The Netherlands) the session will specifically focus on common symptoms experienced by these patients: anorexia; nausea; and pain. Using a clinical case as an example, evidence-based approaches to the management of these symptoms will be presented. The session will also give special attention to the important aspect of palliative care beyond that provided by medical intervention. Palliative care usually encompasses the needs of the individual patient, ranging from the medical management of symptoms to supporting the psychological and spiritual needs of patients and their carers. Quality of life is a central aspect in this setting. With the example of a clinical case, this session will provide evidence for how best to support patients using palliative means. 1.Ferlay J, et al. Available from: http://globocan. iarc.fr. 2.Van Cutsem E, et al. Ann Oncol 2014;pii:mdu260 [Epub ahead of print]. 3.Cabebe EC, et al. Available from: http:// emedicine.medscape.com/article/278744overview. Colorectal cancer has a relatively long lead time and lends itself well to screening in an effort to reduce mortality. But, is colonoscopy the best method for screening? Colonoscopy for all is not only associated with risks and decreased compliance, but also carries a high economic burden. Do non-invasive screening tests perform better? Once suspected, what is the optimal diagnostic method for early CRC? Identifying CRC can be a conundrum, which is why the Postgraduate Teaching Programme has incorporated Sunday’s Session, Colorectal cancer (CRC): Cure by early detection and local treatment, in which experts provide the latest updates on effective screening and guidance on treatment of screen-detected cancers Sunday October 19 08.30 – 10.30 Hall L/M Dr Michal Kaminski from the Medical Centre for Postgraduate Education and Maria Sklodowska-Curie Memorial Let’s tweet! Tweet us on @my_ueg Participate in our moderated Twitter discussions at #WeekChat live Don’t forget the Round Table Discussion ‘Treating IBD in patients with cancer’ Monday October 20 12.45 – 13.45 Hall G/H UEG Week Live Clip UEG launches new interactive platform: “UEG Week Live” enhances your congress experience. Watch our UEG Week Live Video. Follow the link: www. ueg.eu/uegweek2014.live.video/ Cancer Centre and Institute of Oncology, Warsaw, Poland, will give an overview of different screening strategies and their impact on patients and healthcare providers. He will put forward the case for colonoscopy as the optimal screening test. In contrast, Dr Antoni Castells from Hospital Clinic, Barcelona, Spain, will propose non-invasive screening tests as being optimal. Research has provided information on the molecular basis of CRC development and Dr Castells will introduce potential biomarkers and tests from this information, and how these can help in the future prevention of CRC and/ or early detection of the disease. Professor Colin Rees from South Tyneside NHS Trust, UK, and Dr Monique van Leerdam from the Netherlands Cancer Institute, Amstelveen, The Netherlands, will present conflicting views of decision-making for suspicious lesions in the colon. Is endoscopy superior to histopathology for the diagnosis of early cancer? Screening for CRC has paved the way for the detection of early-stage cancer and the presentations by Professor Rees and Dr van Leerdam will provide an insight into the information available on potentially curative treatments in this setting and the optimal management of such patients. “It is vitally important that patients are accurately diagnosed and the correct treatment modalities carried out to provide a cure with minimal incidence of recurrence,” says Dr Roger Leicester from St George’s Hospital, London, who Co-Chairs the Session. Endoscopic submucosal dissection has emerged as an innovative technique for resection of early lesions, but is this technically challenging procedure superior to transanal endoscopic microsurgery for early rectal tumours? Professor Alessandro Repici from Humanitas Medical School, Milan, Italy, will present the case for and against both techniques in early CRC. Look out for three Live Endoscopy sessions transmitted from Vienna General Hospital (Medical University) Your direct access to congress recordings, E-posters & abstracts www.ueg.eu/week/24-7 www.ueg.eu/week Tuesday October 21 Hall A Vienna Info-Counter Vienna Info-Counter is located in the registration area. Helpful Information Saturday 18 - Tuesday October 21 08.00 – 18.00 Wednesday October 22 08.00 – 16.00 Vienna Skyline Coffee Breaks & Lunch Coffee breaks and lunch for the Postgraduate Teaching Programme and the ESGENA Conference on Saturday October 18 and Sunday October 19 are provided in the foyers A, B, C, E and F as well as in the Crystal Lounge of the ACV. Visit the UEG Association Village on the 1st floor Meet representatives of UEG’s Member Societies St. Charles’s Church Imperial Court Theatre Postgraduate Teaching Programme Diagnosing IBD: What’s significant? Patients with inflammatory bowel disease (IBD) can present with a variety of symptoms, the most common of which include abdominal pain, rectal bleeding, diarrhoea, weight loss and extreme tiredness. However, some patients suffer only a few symptoms at intermittent intervals, making accurate diagnosis a challenge. In today’s Plenary I Session, What is important when diagnosing IBD? Dr Maria Abreu from the University of Miami, FL, USA, will discuss what information clinicians need to make a confident IBD diagnosis Saturday October 18 09.00 – 10.30 Let’s tweet! Tweet us on @my_ueg Ask the experts or express your point of view by using the hashtag #WeekChat Hall A She will consider the essential role of endoscopy and biopsies, then discuss the evidence that underpins the use of diagnostic tools including genetic testing, radiology and serology. Dr Abreu works at the forefront of IBD research and has recently described a novel hypothesis to explain the link between bacteria, inflammation and colon cancer in IBD patients. Syllabus Registered participants for the Postgraduate Teaching Programme receive their syllabus USB stick of UEG Week 2014 at the distribution counter in the Entrance Hall. Live Streaming of Sessions live Become part of UEG Week and view There are many possible complications over 100 sessions of Europe’s largest in IBD. Dr Ben-Horin Shomron from Tel GI meeting from wherever you want! Aviv University, Ramat Aviv, Israel, will discuss whether disease complications UEG will connect everyone to its and outcomes can be predicted at initial annual meeting via live stream on the diagnosis. There are many predictive UEG Week live website. markers of IBD but integrating the Lean back and get updated on relevant impact of each is not easy. Dr Shomrom st will discuss computer models that have GI and liver topics free of charge, and connect with the community via the been developed toVisit help clinicians create the ESGE Learning AreaSocial Wall. UEG Week individual patient profiles to inform (training in cooperation with ESGENA) optimal management strategies and Simply sign in to myUEG. For more & the Ultrasound Learning Centre. please visit www.live. treatment selection. information, ueg.eu/week Find more information on pages XY-XY For treatments to be effective, clinicians need to differentiate between IBD subtypes, ulcerative colitis and Crohn’s disease. During today’s session Professor Geert d’Haens from Academic Medical Centre, Amsterdam, The Netherlands, will discuss There is a room set apart for prayer. It how clinicians can differentiate between the is a quiet place, where delegates may two conditions and if such differentiation is withdraw to seek divine strength and guidance. The prayer room is located in as important as first thought. Room OE F140 on the ground floor. Improve your skills in the Hands On @ UEG Week Area on the 1 floor Prayer Room UEG Association Village Improve your skills in the Hands On @ UEG Week Area on the 1st floor Visit the ESGE Learning Area (training in cooperation with ESGENA) & the Ultrasound Learning Centre. Location: The Gallery, 1st Floor Opening Hours Saturday October 18 09.00 – 17.00 Sunday October 19 09.00 – 17.00 Monday October 20 09.00 – 17.00 Tuesday October 21 09.00 – 17.00 Wednesday October 22 09.00 – 14.00 UEG Week News Scientific Programme Gastroenterology: A political priority for Europe’s future Gastrointestinal (GI) and liver diseases are a burden to healthcare in Europe. Almost 1 in every 3 European citizen will suffer from a GI disease at least once in their lifetime, while the prevalence of hepatocellular carcinoma – the most common type of liver cancer – is increasing throughout Europe.1,2 Despite this, the European health agenda does not prioritise research or clinical care in these areas. But before any politician is ready to sanction more strategic investment in digestive and liver health, they always ask one thing: what difference will my support make in the future? Monday’s Session, Gastroenterology and hepatology in Europe: Past, present and future, gives you a chance to speculate on the future. What could European healthcare look like in 10, 20 or even 30 years from now? Monday October 20 14.00 – 15.30 Hall C Speakers will discuss three stark scenarios: an economic crash and the collapse of public healthcare; an age of silicon advances and automated diagnoses; and a golden age of unified healthcare across the continent. But these bright visions of optimal care for all are more than pure speculation; these scenarios could possibly become reality as soon as 2040, the speakers insist. What the gastroenterology community does today will affect what we can achieve tomorrow. So how can we usher in that techno-golden age? UEG is already working towards a brighter future. It promotes awareness of GI diseases in the European Parliament in Brussels and political spheres across Europe. Following the European Parliament’s landmark adoption of the Written Declaration on Fighting Colorectal Cancer in 2010, UEG has continued to work tirelessly to support this initiative. Colorectal cancer (CRC) is the second highest cause of cancer mortality in Europe, but screening can reduce mortality by 30%.3 UEG wants to see more research and the EU-wide introduction of screening; it has kept this topic high on the European Union’s health agenda through campaigns, conferences and active promotion. Invitation hear results from two major new reports UEG Week Symposium Gastroenterology and Hepatology in Europe: Past, present and future Date: Monday October 20, 2014 Time: 14.00-15.30 Hosted by United European Gastroenterology Room: Hall C Scientific Programme CRC is just one of many GI diseases that together account for significant mortality, according to findings just published in the UEG White Book. This publication contains results of a comprehensive survey into the impact of digestive disorders and liver disease on patient mortality, morbidity and quality of life. Do not miss Monday’s session to hear all about the importance of the White Book’s analysis of the economic burden of GI and liver diseases in Europe, and their implications for the future of healthcare in Europe. What the gastroenterology community does today will affect what we can achieve tomorrow 1. https://www.ueg.eu/eu-affairs/activities/ 2. Venook AP, et al. Oncologist 2010;15:5–13 3. https://www.ueg.eu/press/crceurope/ UEG Week: Facts and figures 14,000 PARTICIPANTS 406 1721 ABSTRACTS PRESENTED AS ORAL PRESENTATIONS ABSTRACTS PRESENTED AS POSTERS ROUND TABLE DISCUSSION SESSIONS www.ueg.eu/week 6 POSTERS IN THE SPOTLIGHT SESSIONS Live endoscopy: Watch world-class experts at work Have you ever wished you could be taught endoscopy procedures by an expert? The UEG Postgraduate Training Programme and UEG Week conference now offer you the chance. As part of the event, the panel of experts on stage will also discuss how the latest endoscopy innovations, including novel materials and concepts, are being integrated into clinical practice.1 Take front row seats as we bring you procedures performed live at the Vienna General Hospital (Medical University)! Live sessions offer you a unique ‘fly on the wall’ opportunity to take your learning to the next level. As part of the Postgraduate Teaching Programme, Saturday’s live transmissions (11.00 – 13.00 and 14.00 – 16.30, Hall A) will reveal tips and techniques from two endoscopy sessions. The hospital team, accompanied by speakers on stage, will guide you through each step of the procedure with a full commentary. You can learn about their choice of instruments, observe teamwork dynamics and see how experts make difficult decisions. Short talks will accompany each live broadcast. But don’t worry if you miss out: Live Endoscopy hits the big screen again on Tuesday during UEG Week with three live transmissions Tuesday October 21 08.30 – 10.30, 11.00 – 12.30 and 14.00 – 15.30 Hall A 1. Vanbiervliet G, et al. Endoscopy 2014;46:791–4 New treatments help to stem upper GI bleeding Acute upper gastrointestinal (GI) tract bleeding is the most common emergency for clinical gastroenterologists and it has significant morbidity. Despite advances in therapeutic endoscopy, mortality has not improved significantly in the past 50 years. Elderly patients and those with chronic medical conditions are at higher risk for death, particularly from rebleeding after endoscopic therapy. At Sunday’s Upper gastrointestinal bleeding (UGIB): Management and outcomes Session, speakers will discuss how the latest research is helping to improve clinical outcomes for patients with such bleeding (Sunday, 14.00 – 16.00, Hall A).1 Professor Ian Gralnek from the Technion-Israel Institute of Technology, Haifa, Israel, will describe his recent work with video capsules. Delivering good visibility of the GI tract without the risk of additional trauma, these tiny cameras are helping to improve haemorrhage interventions.2 Professor Gralnek’s research is also looking at how gastroenterologists can use the latest endoscopy strategies to stem bleeds.3 Upper GI bleeding may be a serious side effect in patients on nonsteroidal anti-inflammatory drugs (NSAIDs), which are known to trigger perforations in the gut and sometimes cause acute obstructions. According to Chair of Sunday’s Session, Professor Chris Hawkey (University of Nottingham, UK), all types of NSAIDs significantly increase upper GI complications.4 He suggests that gastroenterologists should adapt their clinical approach based on a patient’s specific NSAID regime.4 Although clinicians now have a much clearer picture of the adverse effects from NSAIDs and anticoagulants such as clopidogrel, novel oral anticoagulants are emerging as exciting treatment options for a variety of conditions. Speakers at Sunday’s session will discuss how these new treatments and pharmacological strategies will affect gastroenterology case loads. “This session will provide an important update on the optimal management of upper GI bleeding and how we deal with patients who are taking preparations that increase the risk of bleeding,” says Dr Roger Leicester from St George’s Hospital, London, who Co-Chairs the Session. Attention will turn to acute GI bleeding again on Wednesday during the day’s Poster Session (Wednesday, 09.00 – 17.00, Hall XL). A poster presented by Dr Pardeep Maheshwari from Galway University Hospitals, Ireland, offers the latest evidence that patients with a score of 2 on the Glasgow Blatchford Scoring (GBS) system can be treated safely as outpatients (Abstract P1262). The GBS system helps gastroenterologists select appropriate treatment options. It was previously thought that scores of 0 to 1 pointed to outpatient endoscopy, while higher scores indicated the need for inpatient treatment. Other results presented in Wednesday’s Poster Session also support use of the GBS system. A retrospective study has assessed how inpatient referral rates are affected when GBS is introduced as a mandatory part of the endoscopy referral pathway (Abstract P1586). Completion of the GBS assessment rose from 10% to 34% in the study, according to Dr Radu-Ionut Rusu from St George’s Hospital, London, UK, who will present the findings. This led to a drop of 8.5% in referrals for inpatient treatment among patients with scores of 0 to 1. Also on Wednesday, Dr Vera Hoffman-Kloss from the University Hospital of Cologne, Germany, will present a poster on an alternative to GBS: Cologne-Watch Risk Prediction (C-WATCH, Abstract P1588). This system focuses on variceal bleeding in a preendoscopic assessment. Dr Hoffman-Kloss will show that C-WATCH easily stratifies patients requiring in- and outpatient treatment and the next step is its validation in a variety of patient populations. Scoring systems help identify patients who require hospital admission, but can clinicians predict which lesions warrant endoscopic treatment? A recent study shows that patients with haematemesis, systolic hypotension or leukocytosis are more likely to be diagnosed with lesions that pose a high risk of haemorrhage. Dr Pedro Boal Carvalho from the University of Minho, Guimarães, Portugal found that one-third of patients with non-variceal upper GI bleeds had lesions that presented a high risk for haemorrhage during esophagogastroduodenoscopy (Abstract P1585). He will present the full results of his study in a poster on Wednesday, showing that patients who undergo esophagogastroduodenoscopy (EGD) within 12 hours of haemorrhage are more likely to be diagnosed with high risk lesions. These advances in haemorrhage prevention and treatment are set to make a significant clinical impact. But what is the economic burden of acute upper GI bleeding today? Wednesday’s Poster Session will include estimates of the economic and quality of life burden of acute upper GI bleeds. According to Dr Vipul Jairath (University of Oxford, UK), the mean cost of 1-month’s treatment for acute upper GI bleeding is £2822 (Abstract P1589). Dr Jairath found that patients had a quality of life much lower than that of the population average. His findings are expected to inform analyses of the cost-effectiveness of different treatments for acute bleeds and support the future development of interventions and clinical guidelines. How do you manage upper GI bleeds? Have your say via the UEG Week App to vote at the interactive panel discussion in Sunday’s Session, Upper gastrointestinal bleeding (UGIB): Management and outcomes Sunday October 19 14.00 – 16.00 Hall A 1. 2. 3. 4. Granlek IM. Endoscopy 2014;46:772–4 Meltzer AC, et al. Am J Emerg Med 2014;32:823–32 Khamaysi I, et al. Best Pract Res Clin Gastroenterol 2013;27:633–8 Bhala N, et al. Lancet 2013;382:769–79 UEG Week News Let’s tweet! Tweet us on @my_ueg Participate in our moderated Twitter discussions at #UEGWeek live UEG Week Live What’s new at UEG Week in 2014? UEG Week Live offers livestreams including Q&A options to ask questions live to the podium, a social media feed to share your congress experience, daily up-todate news on GI, and UEG Week 24/7 presenting recordings of the latest livestreams including plenary lectures. Discover the full live experience, visit www.live. ueg.eu/week There will be multiple opportunities to discuss burning questions, case studies and more with leading international researchers and clinicians. At the end of some symposia, a moderated Panel Discussion will involve invited speakers, while other sessions offer delegates the chance to chat with speakers in small groups. Interact: Look for Panel Discussion and Chat with the Speakers Sessions in your programme UEG has also boosted the number of daily lunchtime Round Table Discussions from one to four. These sessions were a resounding success when introduced in 2013, but no tickets are issued, so arrive early to avoid disappointment! New for 2014 are Therapy Updates on state-of-the-art treatment options in key disorders, such as biologics in inflammatory bowel disease. There will also be more Translational/Basic Science Sessions covering potentially practicechanging research. Posters continue to offer a great format for sharing Free Paper findings with peers and this year, the UEG Week Programme includes Poster Champ and Posters in the Spotlight Sessions. These Sessions promote hot topic research and give poster presenters additional exposure, while offering an opportunity for delegates to exchange ideas with the presenters. Recent advances in the diagnostics and therapeutics of digestive oncology warrant the focus of the one-day symposium, Advances in Clinical Gastroenterology and Hepatology. The National Societies Symposia will expand this year and focus on Helicobacter pylori and liver transplantation – key topics in clinical practice. More than ever before, UEG Week 2014 sees an even greater number of sessions live streamed online – indicated by the ‘live’ icon in your programme. Be sure to register at myUEG (www.ueg. eu/myueg), then log in or use the UEG Week App to view live streamed sessions Whichever sessions you attend, you will be able to interact, participate and engage with colleagues from around the world more than ever before at UEG Week. Young GI Network Pick up you certificate of attendance Foyer B on 2nd Floor www.ueg.eu/week UEG prides itself on providing high quality educational initiatives for gastroenterologists, hepatologists and other medical specialists working in the field. Once again this year, UEG Week has been accredited by the European Accreditation Council for Continuing Medical Education (EACCME). A maximum of 28 hours of European external continuing medical education (CME) credits are available for UEG Week 2014. To claim your CME credits, simply go along to the CME Terminals next to the registration counter in the entrance lobby, fill out the evaluation form and print out your CME certificate straight away or you can get it online at the UEG Week website. Visit the AMA website to find out how you can convert EACCME credits. Posters in the Spotlight Sessions are an excellent platform for in-depth scientific exchange with Faculty and peers in a relaxed atmosphere Don’t forget! A certificate of attendance at UEG Week 2014 can be issued at the CME Terminals located next to the registration counter in the entrance lobby. You can also obtain your certificate on the UEG Week website (www.ueg.eu/week). CME credits Are you a North American delegate attending UEG Week 2014 and want to claim CME credits? What to expect from Monday onwards Each year, UEG Week strives to be even better than before. This year, we are more interactive than ever, with greater opportunities to network with experts and participate in sessions. Pick up your... Our new initiative offers young delegates the opportunity to network and exchange scientific ideas with peers and senior experts and get recommendations and guidance on the scientific programme. In 2014 we proudly present Experience UEG Week live: Follow the livestream on the UEG website and get updated on the latest GI and liver topics! Connect to the UEG Week Social Wall and become part of the GI community. Visit www.live.ueg.eu/week Livestreams including Q&A options Social Media feed to share your congress experience Daily up-to-date News UEG Week 24/7 presenting recordings of the latest livestreams Make ueg.eu your mobile landing page for the complete congress experience Inserate2_FinalProg_130x210.indd 3 15.09.14 14:40 Young GI Network Wondering what ‘YGN’ stands for on your UEG Week 2014 conference badge? Welcome to a world of tailored benefits and extra support to make this year’s congress an event to remember! As a registered UEG Week delegate younger than 40 years of age, you are automatically a member of the Young GI Network, with access to the Young GI Lounge. If you are below the age of 40, but do not have ‘YGN’ on your conference badge, stop by at the Young GI Lounge to join the Network. Access to the Lounge is also granted to dedicated Young GI Network mentors. The Young GI Network was set up to give young trainees the best chance to share ideas, gain advice and network with other early career delegates and senior colleagues. This new initiative offers you all this, as well as the opportunity to exchange scientific ideas with top speakers and senior experts and be guided through the scientific programme by mentors. As a young gastroenterologist, this week is about much more than just listening to presentations of the latest research advances. We anticipate that you will also want to forge friendships, build up contacts and develop your professional network with peers from across Europe and around the world. The Young GI Lounge, located in Foyer B, is open every day for you to drop in and network. Grab a coffee and charge your tablet as you meet contemporaries. This is a great place for impromptu debates as you explore scientific ideas and tease apart what you have learned. You can also contribute to UEG Week social media activities, connecting delegates and bringing highlights to a global audience. Senior academics, clinicians and mentors – including members of UEG’s Young Talent Group – will also be around to guide you through the scientific programme, help you to pick the most relevant presentations and provide you with whatever advice they can. Remember to follow the Young GI Track in your conference programme, designed especially for gastroenterology trainees and young fellows to get the most out of UEG Week 2014. The UEG Young Talent Group members will be on hand in the Young GI Lounge to answer your questions about ongoing activities and help you become involved with these. The Young Talent Group has eight international members whose responsibility is to make UEG and UEG Week initiatives more accessible and appealing for young gastroenterologists. As a registered UEG Week delegate younger than 40 years of age, you will have received your invite to Sunday’s Let’s Meet! event. New for 2014, this drinks reception offers a unique opportunity for you to network with peers, mentors and senior GI experts while admiring the picturesque views over Vienna and the Danube. At a glance Flash your YGN conference badge to access the Young GI Lounge at the following times: Saturday October 18 10.30 – 17.00 Sunday October 19 10.30 – 16.30 Monday October 20 10.30 – 18.00 Tuesday October 21 08.00 – 18.00 Wednesday October 22 08.00 – 14.00 Please note that ‘Let’s Meet!’ is a pre-registered event with limited space, but there is still room if you are eligible to attend and you have not yet received your invite; check back at the Young GI Lounge on Saturday and Sunday. UEG Week News Your questions answered! There’s so much choice! How do I create a customised congress itinerary? Keep forgetting which sessions you flagged for the day? You can create your own personalised schedule of scientific sessions online or by using the UEG Week App. To make a personalised programme, create an account and log into UEG Week online (www.live.ueg.eu/week/) to browse the congress programme. If you want to attend an event or talk, just click the check box. When you’re done, press the ‘Add’ button in the green feature box of the Personalised Programme. You can even add these events to your personal calendar via the UEG Week App (download via Apple’s AppStore or Google Play). Just click on the star icon next to events you want to attend in the app’s programme section. You can browse and manage your bookmarked events in the My Congress section located in the Main Menu. What does the Young Talent Group do? UEG Week 2014 welcomes a record number of trainee gastroenterologists and young fellows. The eight international members of the UEG Young Talent Group have pulled out all the stops to make this congress a memorable event for all our budding investigators and clinicians. The Young GI Track, for example, highlights the most relevant scientific sessions for early career delegates, while the Let’s Meet! event (Sunday, 17.00) provides the perfect ambiance for international networking. Want to know what else the Young Talent Group has to offer? If you haven’t yet hit 40, find out more by visiting the Young GI Lounge (Foyer B). Got fresh ideas on how to support trainees? If you are below the age of 35, why not apply to join the Young Talent Group? Watch out for more details on the UEG website later this year! How can I ask a question to the speaker? Questions to speakers may be addressed via the hall microphones or the congress mobile app. The Q & A tool is available in the following session halls: Hall A, Hall B, Hall C, Hall D, Hall E, Hall F1, Hall F2, Hall G/H, Hall I/K. www.ueg.eu/week Postgraduate Teaching Scientific Programme Programme Bad bugs – the fight against Clostridium difficile New innovations Saturday afternoon’s session is a difficult to treat. Dr Eero Mattila from the Why is UEG so excited about the Postgraduate Teaching Programme in 2014? A key innovation this year is the introduction of the 3-year, rolling curriculum. The curriculum content was hand-picked by the course directors on the basis of its clinical importance within gastrointestinal, liver and pancreatic diseases. The idea was to give all of you the possibility to educate yourselves not only on the mainstream topics, but also with the option of choosing from a variety of topics according to your individual clinical needs. We felt strongly that symptom-based sessions rather than organ- or disease-based sessions would reflect your daily practice and we focused on this in the break-out sessions. By establishing a 3-year curriculum, we offer you participation in a comprehensive course for every European gastroenterologist. In addition this year, we have revamped the Programme’s format; the result of many discussions and input from key educators. Feedback from previous years of the 2-day Postgraduate Teaching Programme and from the UEG Summer School has told us that increasing the interactivity of the sessions enhances the learning experience for participants. To this end, one of the key innovations of the 2014 Postgraduate Teaching Programme is the inclusion of clinical case sessions that offer the opportunity for discussion with the Faculty and peers. These sessions are designed to include what is seen in everyday clinical practice and should enhance your ability to deal with these scenarios from an evidencebased background. We strongly rely on your participation to make these sessions a success but we are sure that your involvement will be rewarded in many ways. reminder that common conditions like gastroenteritis should never be taken lightly. Infections caused by Clostridium difficile are increasing, with surprisingly high rates of mortality.1 Hospital patients with C. difficile infection (CDI) are up to three times more likely to die in hospital, or within a month of infection, than those without CDI.2,3 According to the European Centre for Disease Prevention and Control, CDI may cost the EU as much as €3 billion per annum, a figure expected to double over the next 40 years.4 Misdiagnosis is partly to blame. In 2013 the European EUCLID study found that CDI is misdiagnosed in nearly a quarter of hospital patients.5 The study found that over half of European hospitals still do not follow the most accurate two-stage testing procedure.5 Professor Mark Wilcox from the University of Leeds, UK, co-ordinated the EUCLID study. He stresses the importance of optimised diagnostics and universal testing for all hospital in-patients. Even with better diagnosis, CDI remains University of Helsinki, Finland, outlines treatment options for severe cases and recurrent infections that arise in almost half of treated patients. He has found that C. difficile immune whey is well tolerated and as effective as metronidazole in the prevention of CDI recurrences. Faecal microbiota transplantation using colonoscopy also appears to be effective against infections from the virulent 027 strain. Also in this session: • Prevention of CDI transmission: Immunisation, probiotics, reduced transmission? • Management of acute infectious diarrhoea in infants and young children • Management of food poisoning and traveller’s diarrhoea in adults 1.Mitchell BG, Gardner A. Antimicrob Resist Infect Control 2010;1:20 2. Oake N, et al. Arch Intern Med 2010;170:1804–10 3. Hensgens MP, et al. Clin Infect Dis 2013;56:1108–16 4.http://www.ecdc.europa.eu/en/healthtopics/ Healthcare-associated_infections/clostridium_ difficile_infection/Pages/basic_facts.aspx. 5.Davies K, et al. ECCMID, Berlin, Germany, 27–30 April 2013. Poster LB-2968 The Postgraduate Teaching Programme offers world-class Continuing Medical Education delivered by the best presenters. Worldleading experts have been selected on the basis of their excellent teaching ability, their competence in providing an overview of the topic and their ability to interact with the audience. Please feel free to challenge them so that you maximise your knowledge! We would especially like to draw your attention to sessions, such as What is important when diagnosing IBD? (Saturday, 09.00 – 10.30, Hall A) and Refractory IBD: A clinical challenge (Saturday, 11.00 – 13.00, Hall E). We all agree that 2014 will be known as the year in which hepatitis C has been cured and Professors Joost P.H. Drenth and Heiner Wedemeyer have put together an extremely enlightening programme on this topic (Viral hepatitis: Cure by modern regimens? Saturday, 11.00 – 13.00, Hall C). Pancreatic adenocarcinoma is predicted to be the second leading cause of cancer death in 2030 and we hope that you will learn in the Postgraduate Teaching Programme how to prevent this dismal forecast (Pancreatic adenocarcinoma (PDAC): Still without hope? Saturday, 11.00 – 13.00, Hall B). Also, we are all faced with ‘abdominal emergencies’ and it may be time to refresh our knowledge in this area (An update on the management of abdominal emergencies, Saturday, 14.00 – 16.30, Hall E). Please have a look at the programme and enjoy the course in 2014. We are confident that 2014’s Postgraduate Teaching Programme will be the best yet! Need an energy boost? Recharge yourself and your electronic devices in the Young GI Lounge in Foyer B on the 2nd floor. Join the Young GI Network today! Access is granted to UEG Week delegates below the age of 40 and dedicated Young GI Network mentors. Find out more on www.ueg.eu/week or on the UEG Week App Ins_YoungGILoung_FP_130x210_RZ.indd 1 15.09.14 14:56 UEG Colorectal Cancer Media Campaign UEG Week Live: ColoReCtal CanCeR (CRC) in euRope second biggest cancer killer CRC is the seCond biggest CanCeR killeR in euRope 3rd men aRe less likely than women to get sCReened thiRd most Common CanCeR in euRopean men 215,000 crc deatHs UP to 30% redUction the fob sCReening test is Commonly available in euRope and ReduCes the Risk of dying fRom CRC by 20-30% 215,000 estimated numbeR of CRC deaths in euRope in a yeaR one deatH eVerY tHree minUtes 1 euRopean dies eveRy 3 minutes fRom CRC Colorectal cancer is the second biggest cancer killer in Europe yet the percentage of eligible adults taking part in CRC screening throughout the EU is lower than the uptake of other cancer screening programmes. To address this issue and continue UEG‘s commitment to the European Parliament’s Written Declaration on Fighting Colorectal Cancer, UEG delivered a call to action media campaign from March to June 2014. The campaign was timed to coincide with European Cancer Awareness Month (March) and the UEG meeting at the Brno conference on CRC screening (April 25-26). The campaign highlighted the growing incidence of colorectal cancer and urged 13% of all cancer if you aRe maRRied you aRe moRe likely to take paRt in sCReening CRC aCCounts foR 13% of all Cases of adult CanCeR in euRope annually 2nd studies highlight that embaRRassment is a key Reason foR people not getting sCReened embarrassment seCond most Common CanCeR in euRopean women the European population to participate in colorectal cancer screening to help reduce incidence and meet the EU target of a 2030% reduction in colorectal cancer deaths. been identified as a major challenge to screening uptake and UEG called for an increase in nurse endoscopy training across Europe to highlight these issues. In addition to a patient campaign, healthcare professionals were targeted via key European medical media to broach the subject of colorectal cancer screening and encourage their patients to overcome the ‘embarrassment barrier’ and mobilise them to participate in life-saving national programmes. The campaign was supported with a European incidence map, data infographic and a #ScreeningSavesLives social media campaign. Pan-European media coverage was achieved across 79 media channels and the social media campaign received strong support from a range of patient organisations, medical professionals and consumers throughout Europe, with a potential audience engagement of 100,000+. Disparity in training provision and healthcare professional resources across European countries has also Instant access to live streaming Stuck at the hotel or leaving for the airport early? Don’t worry, there’s no need to miss a session! Around half of this year’s UEG Week sessions will be streamed live online. To tune in, first register at myUEG (www.ueg.eu/myueg), then log in or use the UEG Week App. You can even pose questions to the speakers during our interactive Q&A slots. You can also catch up on UEG Week when you get home. All delegates have free, continuous access to our session webcasts, so you can listen again to key sessions, watch some of the presentations you missed and view E-posters and abstracts again and again. Log into www.ueg.eu/week/24-7 and relive UEG Week at your own pace, 24/7! Download the App! •Conference programme – pathways, presenters and more! • Favourite sessions •Ask a question – interactive Q&A with speakers • Audience voting •UEG Week Live – live streaming of top sessions •Exhibitors •Maps •Social Wall – post your messages and feedback •FAQs – all you need to know about UEG Week Postgraduate Teaching Programme Recent research offers hope in pancreatic adenocarcinoma Pancreatic adenocarcinoma (PDAC) is among the most lethal solid tumours.1 Patients initially have few symptoms and 80% are diagnosed with metastasis, while median overall survival is less than 6 months.1 3 Early resection offers a chance of cure provided PDAC is detected at an early stage; however, more effective screening is needed to improve risk stratification and early detection of disease.4 Speakers in Saturday’s Session, Pancreatic adenocarcinoma (PDAC): Still without hope? will discuss how the latest research brings new hope to patients and clinicians working in this field (11.00 – 13.00, Hall B). Professor Marco Bruno from Erasmus Medical Center, Rotterdam, The Netherlands, will discuss new advances in the use of endoscopic ultrasound (EUS) for detecting PDAC. Screening with EUS provides detailed images of the pancreas, helping in the early detection of disease. Used in combination with magnetic resonance imaging, EUS is effective for detecting small, cystic lesions and is useful for staging PDAC.2,4 Dr Andrea Laghi from Sapienza University of Rome, Italy and Dr Johanna Munding from Ruhr-University Bochum, Germany, will present the radiologist’s and the pathologist’s perspectives on the differential diagnosis of pancreatic lesions. Possible differential diagnoses are benign and malignant pancreatic tumours, intrapancreatic metastasis, pancreatic malformations and abnormalities of the pancreas presenting as solid masses.5 Professor John Neoptolemos from the University of Liverpool, UK, will give his perspectives on resectable PDAC and how this affects outcomes. As a member of the International Study Group of Pancreatic Surgery, who recently published a consensus statement defining borderline resectability and treatment of these patients,6 Professor Neoptolemos is ideally placed to discuss this topic. Professor Jean-Luc Van Laethem from Erasme University Hospital, Brussels, Belgium, will present on systemic therapies. Gemcitabine has been the mainstay of systemic treatment for PDAC over the past 15 years, but patient outcomes remain poor. Professor Van Laethem will stress the need to provide personalised, rather than standard therapy. To help achieve this, however, he says, “We need to enrol patients and tissue in co-operative trials in which we gain a better understanding of PDAC at the molecular level and which incorporate the development of biomarkers.” 1. He XY, Yuan YZ. World J Gastroenterol 2014;20:11241–8 2. Tamburrino D, et al. World J Gastroenterol 2014 28;20:11210–5 3. Gayral M, et al. World J Gastroenterol 2014;20:11199–209 4. Becker AE, et al. World J Gastroenterol 2014;20:11182–98 5. Kersting S, et al. JOP 2012;13:268–77 6. Bockhorn M, et al. Surgery 2014;155:977–88 Audience voting Look out for our interactive Audience Voting Sessions with audience participation – answer audience polls and vote on motions. Pick up a keypad device at the hall entrance or use the voting feature available on the free UEG Week App. Download the UEG Week App from Apple’s AppStore or Google Play. Now iN PubMed CeNtral aNd searChable iN PubMed Now online and available to download! Visit us on Stand D02 for more information. ueg.sagepub.com NDM 18242_1 UEG Syllabus A4 ad_1.indd 1 08/09/2014 17:20
© Copyright 2026