Vital Signs The ultimate tradition An EBP Journey of discovery
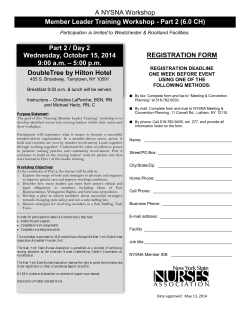
Vital Signs The ultimate tradition An EBP Journey of discovery Christine Malmgreen, RN-BC MS MA & Dr Lillie Shortridge-Baggett, EdD RN NP & Maggie Adler, RN-BC BSN Masters Candidate Literature synthesis to establish an evidencebased policy on routine vital sign frequency Have things really changed? Ways of Knowing = Sources of Knowledge Tradition Authority Experience (trial and error) Sources of knowledge for practice Tradition – Something is done in a specific way because it has always been done that way Authority – Something is done in a certain way because someone in authority has said to do it this way (Policy and procedure) Definitions of Ways of Knowing Experience – Trial and Error One method of doing something is tried Does it work? Yes - continue No – try something else (Definition of insanity) Begins with a question… Start here: What have you wondered about? Why do we do things this way? Is there a better way? Begin by asking a focused clinical question PICO P – (Patient, Population or Problem): For hospitalized patients I – (Intervention): what frequency of vital signs C – (Comparison with other treatments, if applicable): n/a O – (Outcomes): provides the most efficient model without sacrificing patient safety History of nurses taking vital signs No reference to any form of vital sign monitoring by nurses pre 1893 Concept of nurses taking vital signs evolved - 1893 to 1950 Codified into nursing text of the 1950s Zeitz & McCutcheon (2003) Traditional sources of practice guides Review Major nursing textbooks Policies for recommendations Frequency of recording postoperative vital signs Frequency of vital sign collection based on Traditions NONE supported by EVIDENCE Zeitz & McCutcheon (2003). A hierarchy of evidence Finding a systematic review We found three: Joanna Briggs Institute (1999). Vital Signs. Best Practice Bulletin 3 (3): ISSN 1329-187 Evans, D. Hodgkinson, B. & Berry, J. (2001). Vital signs in hospital patients: a systematic review. International Journal of Nursing Studies 3:6433-650 Lockwood, C., Conroy-Hiller, T., Page, T. (2004, December). Vital signs. Systematic Reviews Joanna Briggs Institute,1-38. Retrieved August 1, 2008, from ProQuest Nursing & Allied Health Source database. (Document ID: 1451791351). Also published in International Journal of Evidence-Based Healthcare, Vol 2(6), Jul 2004. pp. 207-230 as an update. Vital Signs, 1999 Best Practice Information Sheet summary of current best evidence on V/S Vital Signs versus Observations The measurement of temperature, pulse, heart rate and blood pressure is termed both Neither have been well defined Limitations A small number of studies: V/S are quite limited in terms of detecting important physiologic changes Level IV evidence ~expert opinion Frequency of Vital Signs Limited information based on Surveys of nurses* Clinical practice reports Expert opinion Surveys of nurses - many admit Carry out frequent V/S on patients they believed did not require them (ritual) Had become “routine”, unrelated to perceived individual patients needs There has been little evaluation of the optimal frequency of patient observations Systematic Review, 2001 Purpose: Establish an evidence base for V/S measurement in hospital patients Measurements that constitute V/S Optimal frequency Limitations of V/S Method: Explored systematic reviews, clinical trials and broader issues surrounding “routine” V/S within acute care setting Evans, Hodgkinson & Berry (2001) Conclusions: “Much of current practice of V/S measurement based more on tradition and expert opinion than on research” Recommendation: further research …into the broader issues of V/S measurement to ensure most useful parameters monitored at an appropriate frequency using accurate techniques Evans, Hodgkinson & Berry (2001) Systematic review - 2004 Objective To present the best available information related to the monitoring of patient V/S Purpose of V/S Limitations of V/S Optimal frequency of measurements What measures should constitute vital signs Lockwood, Conroy-Hiller, & Page (2004, December) The evidence A variety of measures may be useful additions to the traditional four V/S Monitoring these can change patient care and outcomes: pulse oximetry smoking status Evidence based: V/S monitoring frequency for patients returning from PACU after surgery Findings Considerable research on many aspects of V/S “wealth of research” on ensuring accuracy NOT reflected in practice Still need to know: WHAT parameters to measure Optimal frequency Role of technology (new) Conclusions A re-evaluation of the role of V/S : “ it appears that at times this practice is undertaken more through routine than any serious attempt to monitor patient status” The exact role of vital signs in healthcare institutions needs to be redefined to ensure optimal practice Vital Signs policy and procedure “Routine vital signs” - redefined Q shift = q 12 hr More frequent based on nursing judgment Specific guidelines for accurate measurement Unlicensed personnel assigned tasks Include as nursing observations - Pulse ox measurement, smoking and mental status enhances early detection of adverse events Improve outcomes Next steps: Incorporate the patient/family as collaborators in observation (consistent with EBP) Going further back in the medical literature… Cost-ineffective nursing care? 1978 Orders written by MEDICAL RESIDENTS … VS frequency did not correlate with subsequent critical events “Such orders …wasteful of nursing resources…other skilled observations may be neglected”! Resulted in a significant time-consuming & cost-ineffective nursing care Vautrain & Griner, 1978 The evidence mounts -2001 Premise: Frequent VS monitoring presumed to be required for safe management of transplant patients, even at night *Benefits did not outweigh detriments of sleep deprivation in frequent night monitoring time/expense for a nursing activity NEED: Prospective studies to accurately identify day time risk factors to predict need for night time monitoring Sharda, Carter, Wingard, & Mehta (2001) And mounts - 2003 Purpose: Evaluate benefit of routine V/S monitoring on clinical outcomes in DVT More frequent V/S evaluation did not result in statistically significant difference in: survival progression of disease predict of patient disposition Potti, Panwalkar, Hebert, Sholes, Lewis, & Hanley, 2003 And mounts - 2006 Purpose: Evaluate the benefit from frequent/routine monitoring of V/S on clinically relevant outcomes in hospitalized patients with CAP as a model *Urgent need for refinement of common clinical practice of ‘routine’ (Q6H) V/S in hospitalized patients Mariani, Saeed, Potti, Hebert, Sholes, Lewis, & Hanley (2006) Radical redefinition of what’s “vital” Vital signs = ‘vital’ for clinical decisions Monitoring is expensive and/or inaccurate Toms E. (1993) Nursing rituals: Vital observations. Nursing Times Present frequency not cost/time-effective Need: an individualized assessment of V/S measurement frequency More efficient allocation of resources Increased patient privacy and satisfaction …And about those frequencies..? One group of physician-researchers indicted what routine V/S frequency should NOT be more frequently than q 8 hrs None provided insight into How frequently V/S need to be done Who should determine this frequency On what basis? What about the impact of “routine” monitoring procedures on uncovering and/or warning of coming adverse events? Maybe there is no answer to these questions? What we do know We like to say our practice is evidence-based, however, “the reality is that this is merely rhetoric as we have done little to provide the rigorous evidence required to inform practice” Zeitz & McCutcheon, 2003 Presently “routine” V/S measurement is inaccurate Counterproductive ~ cost ineffective Mariani, Saeed, Potti, Hebert, Sholes, Lewis, & Hanley (2006) What we should do ACKNOWLEDGE: Collecting V/S is one nursing treatment supported more by tradition rather than empirical evidence Optimal frequency of V/S sign measurement has yet to be elucidated –nursing’s job! We need to individualize assessment of V/S measurement - for more efficient allocation of hospital resources Finding and using the evidence Critically appraise existing evidence that you find in your search Use “best evidence” to guide practice When there is a lack of evidence: Then what? Beyond routine V/S Becoming more cost-conscious Spiraling hospital costs = need for critical analyses of practices Significant attention to the rising cost of hospital care: Excessive (?) use of ancillary services Insufficient emphasis on appropriateness of nursing services effect on overall health-care costs ** What is role of Nursing skilled observation? Mariani, Saeed, Potti, Hebert, Sholes, Lewis, & Hanley (2006) Skilled observation Physicians! request nurses to use more efficient and appropriate methods of clinical observation (Vautrain & Griner, 1978) “Visual observation, more appropriate for monitoring patient status and progress” (Evans et al., 2001) The role of visual observation – When and if this could replace vital sign measures? (Lockwood, et Al., 2004) Nursing observations within 24 hours of surgical procedure (Zeitz, 2005) Redesigning the work environment Begins with nursing terminology External manifestation of professional thinking “the dress of our thoughts“ Meyer & Lavin ( 2005) Online Journal of Issues in Nursing "Vigilance: The Essence of Nursing" To encompass The Work of nurses requires redesigning, transforming reconceptualizing care concepts Nightingale’s wisdom Observation is “looking and listening to the subjective and objective information that the patient provides” Zeitz (2005) Our primary role: Surveillance Zeitz (2005); Meyer & Lavin ( 2005) What is the evidence? Present methods of frequency of V/S determination does not affect survival outcome Risk of clinical deterioration and relationship to increased frequency V/S measurement does not correlated with outcomes Appropriate utility of nursing services will: minimize expense of unnecessary tasks alleviate the burden to nurses Redirect resources ~ more imperative nursing treatments “Failure to rescue” Identifying patients at risk of an in-hospital adverse event The money question: How do we prevent adverse events, and what is the relationship to “routine” vital sign collection? Adverse event (AE) prevention LITERATURE REVIEW: Role of nurses in AE prevention from the perspective of “physiologic safety” Evidence: changes in LOC and altered respiratory rate/function = warning of AE NURSES -make decisions outside of usual boundaries in best interests of patient Considine & Botti (2004). International Journal of Nursing Practice Implications for practice With a growing emphasis preventing adverse events The vital role of nurses not just data collectors Interpreters of multiple and complex patient data gathered in context of the whole picture presented by the patient = enables capture of impending AE Surveillance ~ A STUDY * Earlier research identified: factors associated with hospital costs (one = nursing treatments) Purpose of this study: determine cost of one nursing treatment Independent variable: surveillance older hospitalized adults at risk for falls Shever, L., Titler, M*., Kerr, P. (2008). The effect of high nursing surveillance on hospital cost. Journal of Nursing Scholarship Patients who received high surveillance = 157 falls Patients who received low or no surveillance = 324 falls Cost avoidance for one fall = $17,483 Findings: High surveillance cost $191/ hospitalization The essence of surveillance = mundane, not dramatic Make sure nothing happens (at least, nothing bad) Amazing fact: Majority of protocols for Rapid Response teams look for alterations in V/S (B/P, pulse, rarely respirations) as reasons for initiating a rapid response! References Considine J, Botti M. (2004). Who, when and where? Identification of patients at risk of an in-hospital adverse event: Implications for nursing practice International Journal of Nursing Practice 2004; 10 : 21–31 Davis, M.J. (1990). Vital signs of Class I surgical patients. West J Nurs Res 12: 40-41 Evans, D. Hodgkinson, B. & Berry, J. (2001). Vital signs in hospital patients: a systematic review. International Journal of Nursing Studies 3 (2001) 6433-650 Hirter, J., & Van Nest, R.L. (1995). Vigilance: A concept and a reality. CRNA: The Clinical Forum for Nurse Anesthetists, 6(2), 96-98 Lockwood, C., Conroy-Hiller, T., Page, T. (2004, December). Vital signs. Systematic Reviews - Joanna Briggs Institute,138. Retrieved August 1, 2008, from ProQuest Nursing & Allied Health Source database. (Document ID: 1451791351). References (con’t) Mariani P, Saeed MU, Potti A, Hebert B, Sholes K, Lewis MJ, Hanley JF. (2006). Ineffectiveness of the measurement of ‘routine’ vital signs for adult inpatients with community-acquired pneumonia. International Journal of Nursing Practice 12 (105–109) Meyer, G., Lavin, M.A. (June 23, 2005). "Vigilance: The Essence of Nursing" Online Journal of Issues in Nursing. Available: http://nursingworld.org/ojin/topic22/tpc22_6.htm retrieved from the internet, 6/30/05 Potti, A., Panwalkar,A. Hebert, B., Sholes, K., Lewis, M.J., & Hanley, J. (2003). Ineffectiveness of Measuring Routine Vital Signs in Adult Inpatients With Deep Venous Thrombosis. Clin Appl Thrombosis/Hemostasis 9(2):163-166 Schumacher S.B (1995).. Monitoring vital signs to identify postoperative complications. Med Surg Nurs 4: 142-5 Sharda, S., Carter, J., Wingard, JR., & Mehta, P. (2001). Nursing observations Monitoring vital signs in a bone marrow transplant unit: are they needed in the middle of the night? Bone Marrow Transplantation 27 (1197–1200) References Shever, L., Titler, M., Kerr, P. (2008). The effect of high nursing surveillance on hospital cost. Journal of Nursing Scholarship 40 (2):161-69 Vautrain RL & Griner PF (1978). Physician's orders, use of nursing resources, and subsequent clinical events. Journal Of Medical Education [J Med Educ] 53 (2):125-8. Zeitz, K., & McCutcheon, H. (2003). Evidence-based practice: To be or not to be, this is the question. International Journal of Nursing Practice 9 (272–279) Zeitz, K. (2005). Nursing observations during the first 24 hours after a surgical procedure: what do we do? Journal of Clinical Nursing, 14, 334–343 Thanks to Magnet project listserv members for their responses to the query: General Medical Unit Frequency of Vital Signs
© Copyright 2026