The feasibility and usefulness of contrast
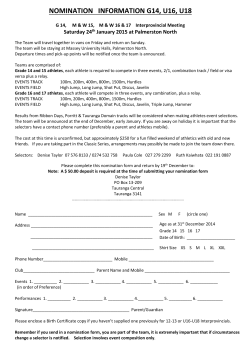
Eur J Echocardiography (2005) 6, 24e30 The feasibility and usefulness of contrast exercise echocardiography for the assessment of left ventricular function in master athletes Marta Rizzo, Maria Concetta Robertina Vono, Loira Toncelli, Patricia Pec xagna, Paolo Manetti, Laura Stefani, Giorgio Galanti) Department of Medical and Surgical Critical Care, Laboratory of Non-Invasive Cardiology, Sports Medicine Centre, University of Florence, Viale Gian Battista Morgagni, 85, 50134, Florence, Italy KEYWORDS Master athletes; Exercise echocardiography; Endocardial border Abstract Background The number of competitive master athletes (MA, over 40 years) has been rising. Since the incidence of coronary artery disease (CAD) is increasing in this population, cardiovascular pre-participation screening, including a maximum exercise test, is recommended. In this context the addition of contrast to echo could be useful because wall thickening and motion are better markers of myocardial function when the whole endocardial border (EB) is visible. Objective To evaluate the feasibility and usefulness of rest and exercise contrast echo for the assessment of LV wall motion in competitive master athletes with suboptimal acoustic windows. Methods Forty consecutive MA underwent echo and contrast echo both at rest and during exercise. Contrast-enhanced images were achieved at rest and at peak exercise after administration of SonoVue (BR1), using apical 4 and 2-chamber views divided into 6 myocardial segments (MS). The EB resolution for each segment was graded as: 0 Z not visible, 1 Z barely visible, 2 Z well-delineated. Results In the baseline at-rest echo 17/40 (45%) patients were graded as score 0, 22/40 (55%) were graded as score 1 and only 1 athlete has reached score 2. In atrest echo contrast 28/40 (70%) athletes have reached score 1 and 12/40 (30%) score 2. Nobody was graded as score 0. At the same time in the baseline peak-exercise echo 12/40 (30%) athletes were graded as score 0, 24/40 (60%) athletes reached score 1 and 4/40 (10%) score 2, while using contrast at peak-exercise echo 28/40 (70%) were grated as score 1 and 12/40 (30%) reached score 2. The differences about the grading of the score between the two groups with and without contrasts, at rest and at peak exercise, are statistically significant (p ! 0.001). Considering the whole of the MS analyzed in the majority of the athletic population studied, we can see that at-rest echo, 64/480 MS (13.3%) were graded as 0, 156/480 MS (32.5%) as 1 and 260/480 MS (54.2%) were graded 2, while ) Corresponding author. Tel.: C39-3294204277; fax: C39-0554279375. E-mail address: [email protected] (G. Galanti). 1525-2167/$30 ª 2004 The European Society of Cardiology. Published by Elsevier Ltd. All rights reserved. doi:10.1016/j.euje.2004.05.001 Downloaded from by guest on November 14, 2014 Received 26 September 2003; received in revised form 10 May 2004; accepted 19 May 2004 Contrast exercise echocardiography in sports cardiology 25 in the peak-exercise 96/480 MS (20%) were graded as 0, 235/480 MS (48.9%) as 1 and 209/480 MS (43.5%) were graded 2. On the other hand, using contrast, in atrest echo, 480/480 MS (100%) were graded as 2 while in the peak-exercise echo 460/480 MS (95.9%) were graded as 2 and 20/480 MS (4.1%) as 1. The percentage of the MS graded as 2 reach almost the whole number of the analyzed MS with a percentage increment in the at-rest and peak-exercise echo of 85% and 120%, respectively. Conclusions Our results show that the use of contrast echo improves the visibility of the EB in a way that the two groups of competitive athletes show at rest and after exercise a significant increment of the score 2 compatible with a better visibility of the EB. These results suggest that contrast echo, both at rest and during exercise, is a better method for EB analysis to understand the behaviour of the wall motion in subjects with suboptimal acoustic windows, and could be suitable for cardiovascular screening in master athletes. ª 2004 The European Society of Cardiology. Published by Elsevier Ltd. All rights reserved. Background Methods Study population The study group consisted of 40 consecutive male master athletes (age range: 51e72 years, mean age: 59 G 8.5) who were referred to our secondlevel Sports Cardiology Center of the University of Florence for an exercise echocardiogram to obtain eligibility for athletic competitions. At the moment of the evaluation, all the athletes were undergoing intensive aerobic training (at least 3 training sessions per week, each one lasting 90e120 min). They were engaged in different sports: marathon running (21 athletes), cycling (13 athletes), tennis (4 athletes) and swimming (2 athletes). The athletes evaluated had been referred to our laboratory after a previous evaluation in a firstlevel center for various problems: - all presented ECG abnormalities - 10 had borderline hypertension (mean values 150/85) Downloaded from by guest on November 14, 2014 Over the past few years the practice of competitive sports and vigorous physical conditioning programs has been widely spreading among middle-aged and elderly subjects. Physical inactivity and a sedentary lifestyle as well as age are recognized as major risk factors for the development of CAD.1e3 Conversely, it has been demonstrated that exercise can help to reduce cardiovascular risk factors and decrease the overall incidence of heart disease.4,5 Unfortunately, acute vigorous physical exertion in elderly people does not protect against exercise-related death in the presence of underlying cardiovascular disease. Sudden death often occurs as ‘a bolt from the blue’ during physical effort in asymptomatic and apparently healthy elderly subjects, and more than 80% of these events are due to CAD.6,7 For these reasons, the possibility of screening CAD in elderly people engaged in highly intensive training programs is a very important challenge for sports cardiologists. Thanks to its satisfactory specificity and sensibility, exercise echocardiography might be a more suitable test than standard exercise ECG for cardiovascular screening in active people over 40 years of age.8,9 However, LV regional wall motion evaluation both at rest and during exercise relies on clear visualization of the entire endocardial border (EB) in each cross-sectional image. Unfortunately to date, even after the introduction of tissue harmonic imaging, up to 10% of baseline echo and up to 30% of exercise echo are suboptimal, due to inadequate visualization of EB, which occurs more frequently in the anterior and lateral walls,10 especially in elderly people. A number of studies have demonstrated the usefulness of administering a contrast agent to enhance EB and optimize wall motion analysis in patients with coronary artery disease, both at-rest echo and during exercise or pharmacological stress echo.11e16 The feasibility and usefulness of contrast opacification of the left ventricle at rest and during exercise in the context of sports cardiology still has to be evaluated. This study was performed to evaluate the feasibility and usefulness of exercise contrast echo for the assessment of left ventricular wall motion in MA with poor acoustic windows. 26 - 8 had a trivial aortic regurgitation (evaluated as 1C at-rest echo) - 6 had a trivial mitral regurgitation - 7 had a combined mild aortic and mitral regurgitation All of them were selected for contrast echo and also harmonic imaging was used during baseline rest and stress echo because of poor acoustic windows. No particular exclusion criteria were considered. At baseline at-rest echo, no analysis about wall motion abnormalities were performed since the aim of the study was an assessment of the utility of the echo contrast to identify the EB at rest and after exercise even if this may improve the interpretation of wall motion. Informed consent for the protocol was obtained from all subjects before their participation. M. Rizzo et al. Contrast echo The contrast agent used in this study was SonoVue (also referred to as BR1), Bracco, Italy, a secondgeneration ultrasound contrast agent commercially available in Europe, which has outstanding stability, resistance to pressure and biological safety.18,19 A 20-gauge intravenous catheter was inserted into a peripheral vein in the antecubital fossa, and the contrast agent (SonoVue, 25 mg/ 5 ml 0.9 Na Cl) was injected at rest, 1.5 ml in bolus and 1.5 ml/min with an infusion pump (VueJECTBracco Switzerland) for 3 min; the same method was used at peak. Each subject received 12 ml of SonoVue. All subjects completed the examination without presenting any early or late side effects linked to the administration of the contrast agent. Study design Image analysis Stress testing All the exercise tests were performed on a specifically designed bicycle with a stiff, 45( sloped back, pliable on the left side, which allowed reduction of the artifacts due to chest movement and facilitated imaging acquisition during effort. The stress testing protocol used consisted of progressive increments of 25 W loading every 2 min, starting from a load of 25 W, up to physical exhaustion. All the subjects performed a maximum stress test, reaching 85% or more of the maximal heart rate estimated for age. Image acquisition Both baseline and contrast images were obtained using a commercially available echo machine (Megas, ESAOTE Biomedica) equipped with a harmonic scanner. Studies were performed from an apical window, using the apical 4 and 2-chamber views, each divided into 6 segments. The mechanical index, during contrast echo image acquisition, was lowered to 0.7e0.8. The gain was adjusted for each subject at the beginning of the rest study and kept constant thereafter. The focus was set at the upper third of the left ventricle to decrease bubble destruction in the near field. The left ventricle was divided into 6 segments in both the apical 4-chamber view (basal, mid and apical interventricular septum and lateral wall) and the 2-chamber view (basal, mid and apical anterior and inferior wall), for a total of 12 segments for each subject. Apical 4 and 2-chamber views were used, according to Standardized Myocardial Segmentation and Nomenclature for Tomographic Imaging of the Heart.17 Endocardial border visualization was scored for each segment using a 3-level-scale: 0 Z border invisible 1 Z barely visible (border visualized only partially throughout a heart cycle and/or incomplete segment length) 2 Z complete visualization of the endocardial border The scores were used to calculate the endocardial border delineation index (EBDI). This was defined as the sum of endocardial scores divided by 12 and was calculated for both the baseline and the contrast echo imaging. The images, collected in quad screen format, were reviewed by 2 experienced blinded readers who examined the baseline and contrast echo images at different times. If a discrepancy appeared, a third observer assessed the image and complete agreement was reached. Statistical analysis Statistical analysis was performed using a statistical computer software package for Social Sciences Downloaded from by guest on November 14, 2014 All the athletes were submitted to a standard examination followed by myocardial contrast opacification (MCO) both at rest and during exercise test. Standard and contrast exercise echo were performed with an interval of at least 2 days. Contrast exercise echocardiography in sports cardiology for Windows, (released 11.01, SPSS Inc, Chicago, IL-USA). Data were analyzed using t-Student test ( p ! 0.001) application. Results Baseline echocardiography Out of a total of 480 segments from 40 subjects, the regional LV endocardial border was not seen Table 2 Score for each master athlete investigated Baseline Baseline Contrast Contrast Score echo rest echo rest echo peak 0-1-2 exercise exercise for patient 1) 2) 3) 4) 5) 6) 7) 8) 9) 10) 11) 12) 13) 14) 15) 16) 17) 18) 19) 20) 21) 22) 23) 24) 25) 26) 27) 28) 29) 30) 31) 32) 33) 34) 35) 36) 37) 38) 39) 40) 0 1 0 1 0 0 1 0 1 0 1 1 1 0 1 0 1 0 1 1 0 1 2 1 1 0 0 0 1 1 0 1 0 1 1 1 1 0 1 0 0 0 1 1 1 1 0 0 1 0 1 0 0 1 1 1 1 0 0 1 1 0 1 1 2 0 1 1 2 1 2 1 1 1 1 2 1 1 2 1 1 2 2 1 1 1 1 1 1 1 1 2 2 1 1 1 2 1 2 1 2 1 2 1 1 1 1 1 2 1 1 1 1 1 2 2 1 1 2 1 1 1 2 2 2 2 2 2 2 1 2 2 1 1 1 2 2 1 2 2 2 2 1 2 2 2 1 1 2 2 2 1 2 1 2 2 1 2 2 2 (score Z 0) in 64/480 (13.3%) segments at rest examination. 156/480 (32.5%) segments, an average of 3.58 of 12 segments per subject (32.5%), were not correctly interpretable due to partial Rest and peak exercise EBD at standard and MC echo Score Echo rest Echo peak ex MCE rest MCE peak ex 0 1 2 TOT segments 64 (13.3%) 156 (32.5%) 260 (54.2%) 480 96 (20%) 235 (48.9%) 209 (43.5%) 480 0 0 480 (100%) 480 0 20 (4.1%) 460 (95.9%) 480 Downloaded from by guest on November 14, 2014 In the baseline at-rest echo 19/40 (47%) MA were graded as score 0, 22/40 (55%) were graded as score 1 and only 1 athlete had reached score 2. In at-rest echo contrast 28/40 (70%) athletes have reached score 1 and 10/40 (25%) score 2. Nobody was graded as score 0. At the same time in the baseline peakexercise echo 11/40 (27.5%) athletes were graded as score 0, 24/40 (60%) athletes reached score 1 and 12/40 (30%) score 2, while using contrast at peak-exercise echo 28/40 (70%) were grated as score 1 and 12/40 (30%) reached score 2. The differences about the grading of the score between the two groups with and without contrast, at rest and at peak exercise, are statistically significant ( p ! 0.001). Considering the whole of the MS analyzed in the majority of the athletic population studied, we can see that at the atrest echo, 64/480 MS (13.3%) were graded as 0, 156/480 MS (32.5%) as 1 and 260/480 MS (54.2%) were graded 2, while in the peak-exercise 96/480 MS (20%) were graded as 0, 235/480 MS (48.9%) as 1 and 209/480 MS (43.5%) were graded 2. On the other hand, using contrast, in at-rest echo, 480/ 480 MS (100%) were graded as 2 while in the peakexercise echo 460/480 MS (95.9%) were graded as 2 and 20/480 MS (4.1%) as 1 (Table 1). Table 2 shows the behaviour of the score in each group of the MA analyzed at rest and at peak exercise with and without contrast. Table 3 shows the percentage increment of the identification of the EB in the at-rest and peakexercise echo particularly for score 2 of 85% and 120%, respectively. The general and echocardiographic data of athletes are presented as mean G SD (Tables 4 and 5). Table 1 27 28 Table 3 the EB Score M. Rizzo et al. Percentage increment of the visibility of 0 Baseline 13.3 echo rest MS % Contrast 0 echo rest MS % Baseline echo 20 peak exercise MS % Contrast echo 0 peak exercise MS % 1 2 Percentage increment 32.5 54.2 0 100 85% 48.9 43.5 4.1 95.9 120% visualization of the border and/or incomplete segment length (score Z 1); these segments were generally observed in the anterior or lateral wall. After the administration of SonoVue, 100% of segments were completely visualized at-rest echo. At the peak of exercise 96/480 (20%) segments were not visible and 235/480 (48.9%), an average of 5.87 of 12 segments per subject, were not correctly interpretable (score Z 1) at standard exercise echo. After the administration of SonoVue at peak exercise, 460 segments could be perfectly visualized (score = 2) and only 20 segments belonging to the lateral wall (4.1%) (p ! 0.001 baseline vs. contrast) were scored 1 at peak exercise after administration of the contrast agent (Table 1). After the administration of SonoVue we failed to identify any abnormality in wall motion in any of the evaluated subjects. The interobserver agreement was 96% using the 3-point scoring system. Table 4 General data of the athletes Age ( years) Heart rate (bpm) BMI (kg/mq) BSA (mq) BPs (mmHg) BPd (mmHg) Total cholesterol (mg/dl) Training per week (h) 59 61 26.7 1.8 140 85 175 6 G G G G G G G G 8.5 7 2 2 15 5 10 3.8 Legend: BMI, body mass index; BSA, body surface area; Bps, systolic blood pressure; Bpd, diastolic blood pressure. Echocardiographic data of athletes LVIDd (mm) LVIDs (mm) LVPWTd (mm) IVSTd (mm) LVM ( g) LVMI ( g/mq) Parietal stress (dyn/cm2) EF% E/A 48 28 9.5 10.1 215 125 65 63 1.1 G G G G G G G G G 4.5 2.5 1.3 1.2 23.7 6.9 7 7 0.5 Legend: LVIDd Z left ventricular end diastolic internal dimension; LVIDs Z left ventricular end systolic internal dimension; LVPWTd Z end diastolic left ventricular posterior wall thickness; IVSTd Z end diastolic interventricular septum thickness; LVM Z left ventricular mass, LVMI Z left ventricular mass index; EF% Z ejection fraction; E/A Z EA ratio. Discussion and conclusions The importance of this study lies in two aspects: 1) First, it confirms that i.v. administration of SonoVue can enhance EB in subjects with poor acoustic windows, thus optimizing the evaluation of LV wall motion and systolic function, both at rest and during exercise testing. 2) Secondly, this is the first study evaluating the feasibility and usefulness of contrast exercise echocardiography in the setting of Master Athletes Sports Medicine, and to date, data regarding the feasibility of exercise contrast echo have been very limited.20 The results of this study are particularly significant because the number of master athletes is on the constant, continuous increase throughout the western world. The American Heart Association terms master athletes: ‘conditioned, experienced competitive athletes who continue to compete after their formal careers end but also [include] ‘‘walk-up’’ competitors, sometimes referred to as ‘‘weekend warriors’’ with only sporadic training regimens, as well as those who resume competition after long periods of physical inactivity’.21 In fact, as asymptomatic, sedentary individuals over 40 years old begin (or begin again) an exercise program, there is a period of increased risk during which exertion can provoke a cardiac event, whereas such risk associated with habitual exercise in active individuals is relatively low. Also, it is generally assumed that particularly strenuous exertion or sports competition may predispose athletes to greater cardiac risk than non-strenuous physical activity. An increasing number of sudden deaths while exercising are reported in master Downloaded from by guest on November 14, 2014 Exercise echocardiography Table 5 Contrast exercise echocardiography in sports cardiology - possibility of performing the test in an outpatient clinic - relatively low cost (vs. perfusion scintigraphy) - shorter time of performance and interpretation of the test (vs. perfusion scintigraphy) - absence of radiation The addition of the contrast agent makes the method specifically indicated for evaluation of global and segmental LV kinesis and systolic and diastolic function in competitive master athletes with poor acoustic windows. Limitations and future application This feasibility study used a fairly low number of subjects. The contrast echo must be compared both with a gold standard id e scintigraphy or coronarography, both of which have a higher cost. There is no doubt that the MA population is bound to increase considerably in the future and therefore, due to the particular nature of this population, a specific cardiovascular evaluation will become necessary. Only apical projections were used in this study; the basal segments may be difficult to evaluate, since they are parallel to the ultrasound beam. The addition of the infusion method permits image stabilisation. There is another equally, no less important, reason why the contrast echo method can be show itself to be very useful, i.e., the possibility of using a contrast agent coupled with new echo image software, to obtain information on perfusion and hence on the coronary reserve both at rest and during stress, and hence the possibility of assessing, with a non-invasive method, the true effects that the practice of sport has on the population of elderly athletes. References 1. Paffembarger RS, Hyde RT, Wing AL. The association of changes in physical activity level and other lifestyle characteristics with mortality among men. N Engl J Med 1999;328:538e45. 2. Lee IM, Hsieeh CC, Paffembarger Jr RS. Exercise intensity and longevity in men: the Harvard Alumni Health Study. JAMA 1995;273:1179e84. 3. Blair SN, Kohl III HW, Barlow CE, et al. Changes in physical fitness and all-cause mortality: a prospective study of healthy and unhealthy men. JAMA 1995;273:1093e8. 4. Berlin JA, Colditz A. A meta analysis of physical activity in the prevention of coronary heart disease. Am J Epidemiol 1990;132(4):612e27. 5. Blair SN, Kampert JB, Kohl III HW, Barlow CE, Macera CA, Paffembarger RS, et al. Physical fitness and incidence of Downloaded from by guest on November 14, 2014 athletes (1:15,000) as compared to young ones (1:200,000), and the most common cause of these tragic events is a latent and asymptomatic coronary artery disease.7 The American Heart Association recommends selective screening (including history, physical examination and symptom-limited maximal ECG exercise testing with treadmill or cycle ergometer) for athletes having a moderate-to-high cardiovascular risk profile for CAD, i.e. men over 40 years old or women over 50 years old (or postmenopausal) with 1 or more independent coronary risk factors.21 On the other hand, the Italian Society of Sports Cardiology (SIC Sport) recommends a periodical cardiovascular evaluation, including a maximum exercise test, for all subjects over 40 years of age before their participation in competitive sport activities, and this is compulsory by law in Italy.22 Although, unlike ECG, perfusion scintigraphy is a highly sensitive and moderately specific noninvasive method for the diagnosis of CAD, it has a limited feasibility in the setting of sports medicine, which traditionally deals with asymptomatic and apparently healthy people. Exercise echocardiography allows the diagnosis of coronary artery disease from exercise-induced alteration of regional wall motion. In unselected subjects this method has almost the same sensitivity (78% vs. 83%) and higher specificity (91% vs. 83%) as myocardial perfusion scintigraphy for the diagnosis of CAD.8,9 However, the prerequisite for accurate and reliable assessment of LV function both at rest and during exercise is clear visibility of the entire endocardial border in each crosssectional image. Unfortunately, at rest (5e10%) and during pharmacological stress (30%), even with the harmonic imaging, EB was not clearly delineated, and this problem is greater with exercise echo.6,10 Over the past decade, the introduction of second-generation contrast echocardiography has significantly improved LV opacification and enhanced endocardial border definition at rest. Similar improvements have been described for pharmacological stress echo (in particular the dobutamine type) performed in cardiac patients. However, experiences of contrast exercise echo are still limited, as are experiences of contrast echo in sports cardiology. This is the first experience of contrast echocardiography in the setting of sports medicine. Exercise echocardiography is in fact widely used in sports cardiology due to a number of advantages, which include: 29 30 14. Lang RL, Mor-Avi V, Zoghbi WA, Senior R, Klein AL, Pearlman AS. The role of contrast enhancement in echocardiographic assessment of left ventricular function. Am J Cardiol 2002; 90(Suppl):28Je34J. 15. Mulvagh SL, Demaria AN, Feinstein SB, Burns PN, Kaul S, Miller JG, et al. Contrast echocardiography: current and future applications. J Am Soc Echocardiogr 2000;13: 331e42. 16. Rainbird AJ, Mulvagh SL, Oh JK, McCully RB, Klarich KW, Shub C, et al. Contrast dobutamine stress echocardiography: clinical practice assessment in 300 consecutive patients. J Am Soc Echocardiogr 2001;14:378e85. 17. Yoshitani H, Takeuchi M, Hirose M, Miyazaki M, Otani S, Sakamoto K, et al. Head-to-head comparison of fundamental, tissue harmonic and contrast harmonic imaging with or without an air filled contrast agent, Levovist, for endocardial border delineation in patients with poor quality images. Circ J 2002;66:494e8. 18. Grayburn PA, Mulvagh S, Crouse L. Left ventricular opacification at rest and during stress. Am J Cardiol 2002; 90(Suppl):21Je7J. 19. Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professional from the cardiac imaging committee of the council on clinical cardiology of the American Heart Association. Circulation 2002;105: 539e42. 20. Bokor D. Diagnostic efficacy of Sono Vue. Am J Cardiol 2000 Aug 17;86(4A):19Ge24G. 21. Senior R, Andersson O, Caidahl K, Carlens P, Herregods MC, Jenni R, et al. Enhanced left ventricular endocardial border delineation with an intravenous injection of Sono Vue, a new echocardiographic contrast agent: a European multicenter study. Echocardiography 2000 Nov;17(8):705e11. 22. Shimoni S, Zoghbi WA, Xie F, Kricsfeld D, Iskander S, Gobar L, et al. Real-time assessment of myocardial perfusion and wall motion during bicycle and treadmill exercise echocardiography: comparison with single photon emission computer tomography. J Am Coll Cardiol 2001;37:741e7. Downloaded from by guest on November 14, 2014 hypertension in healthy normotensive men and women. JAMA 1996;276(3):205e10. 6. Maron BJ, Epstein SE, Roberts WC. Causes of sudden death in competitive athletes. J Am Coll Cardiol 1986;7: 204e14. 7. Maron BJ, Araujo CGS, Thompson PD, Fletcher GF, Bayes De Luna A, Fleg JL, et al. Recommendations for preparticipation screening and the assessment of cardiovascular disease in master athletes. An advisory for healthcare professionals from the working groups of the World Heart Federation, the International Federation of Sports Medicine, and the American Heart Association Committee on Exercise, Cardiac Rehabilitation, and Prevention. Circulation 2001;103: 327e34. 8. Galanti G, Sciagra ` R, Comeglio M. Diagnostic accuracy of peak exercise echocardiography in coronary artery disease: comparison with tallium-201 myocardial scintigraphy. Am Heart J 1991;122:1609e16. 9. Geleijnse ML, Elhendy A. Can stress echocardiography complete with perfusion scintigraphy in the detection of coronary artery disease and cardiac risk assessment? Eur J Echocardiogr 2000;12e21. 10. Geleijnse ML, Elhendy A, Firetti PM, Roeland JR. Dobutamine stress myocardial perfusion imaging. J Am Coll Cardiol 2000 Dec;36(7):2017e27. 11. Elhendy A, Sozzi FB, van Domburg RT, Bax JJ, Gelenijse ML, Valkema R, et al. Accuracy of exercise stress technetium 99m sestamibi SPECT imaging in the evaluation of extend and location of coronary artery disease in patients with an earlier myocardial infarction. J Nucl Cardiol 2000 SepteOct; 7(5):432e8. 12. Marwick TH, Nemec JJ, Pashkow FJ, Stewart WJ, Salcedo EE. Accuracy and limitations of exercise echocardiography in a routine clinical setting. J Am Coll Cardiol 1992;19: 74e81. 13. Kasprzak JD, Paelinck B, Ten Cate FJ, Vletter WB, De Jong N, Poldermans D, et al. Comparison of native and contrast-enhanced harmonic echocardiography for visualization of left ventricular endocardial border. Am J Cardiol 1999;83:211e7. M. Rizzo et al.
© Copyright 2026