PDF hosted at the Radboud Repository of the Radboud University Nijmegen
PDF hosted at the Radboud Repository of the Radboud University
Nijmegen
This full text is a publisher's version.
For additional information about this publication click this link.
http://hdl.handle.net/2066/77574
Please be advised that this information was generated on 2014-11-17 and may be subject to
change.
Enteroviruses, Pancreatic ß-cells
and Dendritic Cells: a Dangerous
Triangle in Type 1 Diabetes
Etiology?
The research presented in this thesis was performed at the Department of
Medical Microbiology of the Nijmegen Centre for Molecular Life Sciences,
Radboud University Nijmegen Medical Centre, The Netherlands.
Printing of this thesis was financially supported by the Radboud University
Nijmegen, Dutch Diabetes Research Foundation, J.E. Jurriaanse Stichting, and
Corning Nederland B.V.
© 2010 B. M. Schulte
All rights reserved. No part of this book may be reproduced or transmitted in
any form or by any means without written permission of the author and the
publisher holding the copyright of the published articles.
Cover and page design: Barbara Schulte
Printed by: Ipskamp Drukkers B.V Enschede, The Netherlands
Enteroviruses, Pancreatic ß-cells
and Dendritic Cells: a Dangerous
Triangle in Type 1 Diabetes
Etiology?
Een wetenschappelijke proeve op het gebied van de
Medische Wetenschappen
Proefschrift
ter verkrijging van de graad van doctor
aan de Radboud Universiteit Nijmegen
op gezag van de rector magnificus prof. mr. S.C.J.J. Kortmann,
volgens besluit van het college van decanen
in het openbaar te verdedigen op woensdag 23 juni 2010
om 15.30 uur precies
door
Barbara Maria Schulte
geboren op 12 juli 1982
te Almelo
Promotores:
Prof. dr. J.M.D. Galama
Prof. dr. G.J. Adema
Copromotor:
Dr. F.J.M. van Kuppeveld
Manuscriptcommissie:
Prof. dr. M.G. Netea (Voorzitter)
Prof. dr. C.J.J. Tack
Prof. dr. E.J.H.J. Wiertz (Universiteit Utrecht)
Voor pap en mam
Contents
Contents
Chapter 1
General Introduction
Chapter 2
Cross-talk between human dendritic cell subsets
influences expression of RNA sensors and inhibits
picornavirus infection
Jou rn al o f Innate Immunity. 2010 in press.
29
Chapter 3
Echovirus infection causes rapid loss-of-function and
cell death in human dendritic cells
Cell M icrobiol. 2007 9(6):1507-18.
45
Chapter 4
Phagocytosis of picornavirus-infected cells induces
an RNA-dependent antiviral state in human dendritic
cells
J Virol. 2008 82(6):2930-7.
61
Chapter 5
Phagocytosis of enterovirus-infected pancreatic
beta-cells triggers innate immune responses
in human dendritic cells
Diabetes. 2010 in press.
75
Chapter 6
Cytokine and chemokine production by human
pancreatic islets upon enterovirus infection
M anuscript in preparation.
93
Chapter 7
Detection of enterovirus RNA in peripheral blood
mononuclear cells of type 1 diabetic patients:
beyond the stage of acute infection
Viral Immunol. 2010 23(1):99-104
109
Chapter 8
Summary and General Discussion
119
9
Nederlandse Samenvatting
137
Dankwoord
143
Curriculum Vitae & List of Publications
147
Chapter 1
General Introduction
"W e don't know a millionth of one
percent about anything"
Thomas A. Edison
Chapter 1
Introduction
he greatest part of the world's biomass is composed of invisible microbes
(bacteria, fungi, viruses). This microbial environment partly serves to
benefit higher order species, i.e. the visible world. The microbial world is
responsible for the recycling of inorganic sources (carbon, phosphates etc.) from
dead biomass, for symbiotic interaction with higher order species, for maintaining
balance in complex ecosystems, and is a thriving force in evolution1-4. For higher
order species, actually thriving in a microbial environment, it means, however, that
these crucial benefits have some kind of trade-off in the sense of disease. Viruses,
for example, are obligatory invaders and the host has to evolve counter-measures
for maintaining its integrity; the innate and adaptive immune systems. Historically
the focus is on the threats and frequently it is said that microbes and their host
maintain a "race of arms" for survival5. The other side of the coin is, however,
that most microbes are innocuous, beneficial, and even shape the host's immune
system. Deprivation of infections (hygiene) is recently noted as a possible element in
occurrence of immune mediated diseases like asthma and type 1 diabetes (T1D)6-8. A
major task of the immune system, whether innate or cognate, is to discriminate self
from non-self and dangerous from innocent invaders. The immune system itself can
be subject of derailments in the sense of inflammatory and autoimmune diseases,
conditions where the host immune system takes part in the disease process. This
thesis deals with T1D, which is considered to be an autoimmune disease, with
the immune system and with enteroviruses which are proposed to play a role in
T1D. In this chapter, a general overview of the immune system will be provided.
Furthermore, the enteroviruses and their pathogenesis will be introduced. Finally,
T1D and the putative role of enteroviruses in T1D etiology will be introduced.
T
The immune system
The immune system can be divided in an innate and adaptive arm; the innate arm is
responsible for a quick first line of defense against many different pathogens and does
not require prior exposure to a certain pathogen. Among the cells involved in innate
immunity are phagocytes, or "eating cells", such as macrophages and neutrophils. These
cells phagocytose pathogens and subsequently degrade them intracellularly. Natural
killer cells (NK-cells) do not phagocytose pathogens, but recognize pathogen-infected
host-cells and release cytotoxic granules that will destroy the pathogen-infected cell.
The adaptive immune response, also known as acquired immune response,
targets one specific pathogen, and takes some time to develop (4 to 7 days). Once
this pathogen has been encountered and cleared from the body, memory cells have
been generated that enable more rapid responses upon future confrontations with this
particular pathogen. Key players in adaptive immunity are B cells, that produce pathogenspecific antibodies, and T cells, that aid in antibody production and kill infected cells. B
cells become activated upon recognition of a particular antigen (Ag) by its unique B cell
receptor. The activated B cell can mature to an antibody-producing plasma cell once
appropriate help by T cells is provided (see below). The produced antibodies (Abs) can
bind the corresponding pathogen, which is then more easily recognized by phagocytes,
or triggers the complement system. Furthermore, Abs can neutralize bacterial toxins. For
10
Introduction
T cell-mediated immunity, Ag has to be presented to naïve T cells as a processed peptide
in the context of a major histocompatibility complex (MHC) molecule by specialized
antigen-presenting cells (APCs). The most important APC is the dendritic cell (DC, see
below), but also B cells and macrophages can function as APCs. Naïve CD8+ T cells will
become activated upon binding of their T cell receptor (TCR) to a matching peptide
presented in a MHC class I molecule by an APC. For optimal T cell activation, besides
TCR-stimulation, also adequate co-stimulation and activating cytokines are required9.
Activated CD8+ T cells will expand and develop into cytotoxic T lymphocytes (CTLs), that
recognize and kill infected cells (Fig. 1).
Naïve CD4+ T cells are activated upon binding of their TCR to peptides presented
in MHC II molecules and, with appropriate co-stimulation and cytokine stimulation, will
subsequently develop into helper T cells (Th) (Fig. 1). Activated Th cells can differentiate
into different subsets depending on the microenvironment and cytokines, such as
interleukins (ILs), that are present10, 11. Th1 cells which mainly produce interferon-y (IFNY), drive cell-mediated CTL responses and activate macrophages. Th2 cells which produce
IL-4, IL-5 and other cytokines stimulate antibody-mediated responses via stimulation of
B cells11-13. Recently, Th17 cells, which produce the cytokine IL-17, have been described14,
15. This subset is thought to be involved in protection from viral, bacterial and fungal
infections16-20, but may also mediate auto-immune diseases10, 21-23. A special subset of T
cells is the regulatory T cell (Treg) which can suppress functions of the above-mentioned
CD4+ and CD8+ effector T cells via cell-cell contact dependent mechanisms. TGF-ß and
IL-10 contribute to the inhibition of effector T cells24. Tregs are crucial for prevention of
excessive immune responses that may result in auto-immunity25-28.
Dendritic cells
Dendritic cells (DCs) are APCs with the unique ability to activate naïve T cells, and
thereby induce adaptive immune responses. They are required to regulate T cell activity
to boost immune responses when necessary, but also prevent autoimmunity. On the
other hand, DCs exert influence on innate immunity: for example, NK cell activity can
be regulated via DCs29-32. Thus DCs are an essential link that bridges innate and adaptive
immune responses33-35.
DCs can be roughly divided into two distinct populations; the myeloid DCs (mDCs,
also referred to as conventional DCs) and the plasmacytoid DCs (pDCs) (Fig. 2). Within
this subdivision, further populations can be discriminated on the basis of expression
of distinct markers either on the cell surface or intracellularly. These two DC subsets
can also be functionally separated; mDCs are thought to be the major cells involved in
activation and differentiation of naïve T cell populations36-38, whereas pDCs can produce
vast amounts of IFN-a/ß (IFNs) suggesting a major role in viral infections39-41. Cross-talk
between different DC subsets is thought to be critical for good immune regulation. Due
to the low frequency in which mDCs and pDCs are detected in human blood, research on
the function of mDC biology frequently makes use of monocyte-derived DCs (moDCs).
These can be generated via in vitro differentiation from more common monocytes, using
IL-4 and granulocyte-macrophage colony-stimulating factor (GM-CSF). moDCs share
many of the phenotypic and functional characteristics of naturally occurring mDCs, and
thus function as a good model42.
DCs reside in virtually all tissues of the human body as phagocytic immature
DCs. Immature DCs (iDCs) capture Ag and subsequently migrate to the lymph nodes
11
Chapter 1
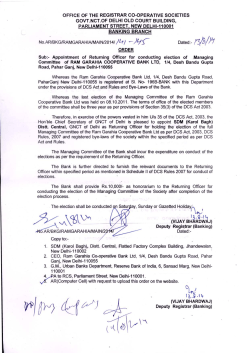
DCs are present in nearly all tissues of the body and continuously phagocytose antigens from their environ
ment (1). Depending on the stimuli associated with the antigen encountered, such as PAMPs or DAMPs (2),
DCs will start maturation and migrate towards the draining lymphoid tissues (3). Here, DCs interact with naïve
T lymphocytes (Th0) and, depending on the costimulatory signals and cytokines provided by the DC (4), will
steer proliferation and differentiation of cytotoxic T cells (CTL) and helper T cells (5). Activated effector T cells
and regulatory T cells (Treg) will subsequently migrate back to the periphery and eliminate the antigen (ef
fector T cells), or induce tolerance (Treg) (6). Alternatively, Th cells can provide help for B cells, transforming
them into antibody (Ab)-producing plasma cells (7). The produced Abs can aid in immune responses.
where matching T cells will get instructions. iDCs are very efficient in Ag-capture and use
several uptake mechanisms such as macropinocytosis, receptor-mediated phagocytosis
via scavenger receptors (e.g. C-type lectins), or Fcy-receptor-mediated endocytosis of
antibody-complexes. Pathogen-associated molecules are engulfed, but also apoptotic
or necrotic cells are phagocytosed42-46. When DCs encounter pathogen-associated
molecules such as bacterial LPS or double-stranded RNA they start a process called
maturation, a process that is associated with decreased phagocytic activity, upregulation
of costimulatory molecules such as CD40, CD80 and CD86, production of proinflammatory
cytokines, and major changes in morphology and intracellular pathways involved in Agpresentation. Once matured, matDCs are optimally equipped to activate and instruct
naïve T cells37, 38. Depending on the microenvironment and maturation stimulus, the DCs
will produce particular cytokines, such as IL-12, IL-4 or TGF-ß, that will control T cell
differentiation47 (Fig. 1).
Endogenous Ags are processed by the proteasome and subsequently loaded
onto MHC class I molecules48. In general, exogenous Ags are targeted to MHC class II
compartments where they are processed into peptides and loaded onto MHC class II
molecules. The MHC class II-peptide complexes can be recognized by matching CD4+ T
cells that will develop into distinct types of helper T cells. DCs are rather unique in that
they can also efficiently present exogenous Ags in the context of MHC class I molecules
12
Introduction
to CD8+ T cells, a process called cross-presentation. Cross-presentation enables DCs to
induce efficient CTL-responses directed against for example tumors or viruses that do
not infect DCs48.
In addition to the major role that DCs play in induction of immune responses,
they also play a very important role in maintaining tolerance. DCs play a major role
in negative selection of autoreactive T and B cells in the thymus49, 50, but it has been
reported that peripheral DCs may also have the capability to suppress T cell activity51'
55. These so-called tolerogenic DCs present Ags through specific MHC-TCR complexes,
but fail to deliver adequate co-stimulatory signals and cytokines required for effective
T cells stimulation. Such an encounter will result in either T cell apoptosis or anergy,
or might give rise to immunosuppressive Tregs53, 55-57. Such tolerizing responses occur
for example upon encountering apoptotic cells in steady-state conditions58. In mouse
models, tolerogenic DCs have been shown to suppress experimental autoimmune
diseases59, 60. Moreover, defects in the cross-tolerance via DCs results in accumulation of
autoreactive T cells and renders mice more prone to autoimmunity61. This implies that
these tolerogenic responses might play an important role in immune homeostasis and
autoimmune disease, also in humans.
Pattern recognition receptors
As described above, DCs are crucial initiators of immunity, but are also critical mediators
of self-tolerance. This raises an intriguing question: How can DCs distinguish between
pathogens, nonpathogenic microbes and self Ags? Detection of microorganisms is
mediated by pattern recognition receptors (PRRs) that recognize pathogen-associated
molecular patterns (PAMPs)62. PAMPs are structures which are unique to pathogens and,
in general, are not present in healthy tissue (self). Most PAMPs are either ubiquitously
present on pathogens, such as beta-glucans or flagellins, or are required and produced
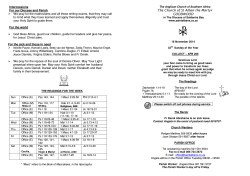
Figure 2. Schematic representation of the two major subclasses of DCs.
DCs can be roughly divided into two subpopulations: myeloid DC (mDC, also referred to as conventional DCs)
and plasmacytoid DC (pDC). Immature mDCs are generally considered to best phagocytose antigens. Mature
mDCs play a key role in activation and differentiation of T cells. Immature pDCs appear as round cells, that
transform into cells with a more dendritic cell-like morphology upon maturation. Cross-talk between the vari
ous DC-subsets is thought to be key for adequate immune regulation.
13
Chapter 1
during infection, such as dsRNA63-65. Next, it was proposed that DCs, in addition to
sensing pathogen products, sense danger in the form of altered self, for example factors
released from damaged cells66, 67. According to this model, immune responses are not
generated upon microbial invasion itself, but when detectable harm is done to the
body. The ligands involved in danger-associated PRR-stimulation, the so-called dangerassociated molecular patterns (DAMPs), are generated or released upon tissue or cell
damage. DAMPs are proteins/products that are usually sequestered within cells, but are
released upon damage, such as heat-shock proteins, high-mobility group box 1 (HMGB1)
or adenosine triphosphate (ATP)68-71. Furthermore DAMPs can be generated or altered
during cell stress or damage, possibly altering their immunogenic potential72. Upon
detection of pathogens or damage to the host by PRRs, subsequent signaling cascades
are initiated by the PRR family members resulting in induction of immune responses.
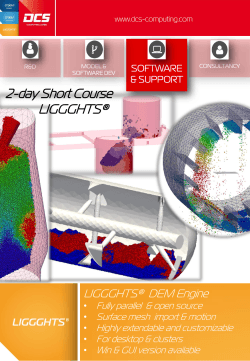
Several classes of PRRs exist (Fig. 3), of which the best characterized are
the Toll-like receptors (TLRs). This family of trans-membrane receptors consists of 10
members that are present on the plasma membrane (TLR1, 2, 4, 5, 6 and 10) or within
the endosomal compartment (TLR3, 7, 8, 9). Each TLR binds to distinct ligands. Formation
of hetero-dimers with other TLRs causes further specificity and diversity in the ligands
that are recognized. TLRs bind to a variety of different ligands, originating from bacteria,
viruses, and other pathogens. Importantly, PAMPs from virtually all pathogens can be
recognized, but also DAMPs can bind to these receptors68, 73, 74. Complex signaling occurs
following binding of a ligand to a PRR, which eventually results in transcription of genes
encoding for pro-inflammatory cytokines and other inflammatory mediators.
Another important family of PRRs, that is involved in recognition of viruses, is
the cytoplasmic RIG-I-like helicase (RLH) family. The RLHs retinoic acid-inducible gene I
To ll-like receptors
R IG -lik e h elicases
Liga n d s: various PAMPs & DAMPs
Liga n d s: viral RNA
Location: plasma membrane and
Location: cytoplasm
endosomal membrane
Effects:
Effects:
- Type I IFN production
- DC maturation
- Antiviral state induction
- Cytokine production
- T cell activation
NOD-like receptors
Liga n d s: various PAMPs & DAMPs
Location: cytoplasm
Effects:
-Cytokine production
- IL-1ß and IL-18 processing
P a t tern
R e ce Dtors
C-tvpe lectin receptors
Liga n d s: carbohydrate structures
Location: plasma membrane &
endosomes
Effects:
- Ag internalization
- Cytokine production
Figure 3. Schematic overview of the four main pattern recognition receptor (PRR) families and their main
characteristics.
The ligands and location of PRRs are depicted. Furthermore, the most important effects initiated upon trig
gering of the receptor-families is specified.
14
Introduction
(RIG-I) and melanoma differentiation-associated gene 5 (Mda5) respond to virus infection
by recognition of distinct RNA structures. Via the adaptor molecule mitochondrial
antiviral signaling protein (MAVS), they start a signaling cascade that results in activation
of interferon regulatory factors (IRFs), such as IRF-3 and IRF-7 that initiate type I IFN
production75, 76. The third family member, laboratory of genetics and physiology 2 (LGP2)
lacks a signaling domain and is thought to be a negative regulator, although this was
recently challenged when it was shown that LGP2 can also stimulate Mda5 function75-78.
Two other PRR-families are the C-type lectin receptors (CLRs) and Nod-like
receptors (NLRs). CLRs are membrane-bound receptors that recognize carbohydrate
structures, such as mannose, glycoproteins and ß-glucans, and can interact with a variety
of pathogens. The NLRs are a cytoplasmic family that recognize diverse bacteriumrelated products such as peptidoglycans79. Recent studies have suggested that some
NLR-family members, such as NALP3, are critical for inflammasome activation by virusassociated PAMPs like dsRNA80, 81. New PRRs are still being discovered. These include
sensors for cytoplasmic DNA, that were proposed to exist for quite some time, but have
only recently been discovered82, 83.
As mentioned above, DCs play a critical role in maintaining tolerance to self-Ags.
Immune tolerance results from phagocytosis under conditions where no PRR triggering
by either PAMPs or DAMPS occurs. Autoimmunity may thus be induced when self-Ags are
phagocytosed and presented by DCs under conditions of simultaneous PRR triggering47.
For example, phagocytosis of DNA-containing immune complexes in the presence of
HMGB1 has been suggested to play a role in systemic lupus erythematosus (SLE)84. Also
in rheumatoid arthritis (RA), exposure to self-Ags and simultaneous triggering of TLRs is
thought to be involved in disease development85.
Inhibition of PRRs and immune responses by viruses
RNA viruses are mainly recognized by TLR3, 7 and 8 and the RLHs RIG-I and Mda5. Upon
encountering a virus, type I IFNs will be produced; a process that can be initiated in
nearly all nucleated cell types. DCs, and pDCs in particular, can produce exceptionally
large amounts of IFNs39. These IFNs will stimulate cells to adopt an antiviral state, which
restricts virus replication. Furthermore, IFNs will also stimulate innate immunity e.g. via
NK cell stimulation, and adaptive immunity e.g. via influencing DC maturation86-90. To
establish a productive infection, viruses have evolved to counteract these host defense
mechanisms. Multiple strategies have been devised and virtually all steps in antiviral
immunity have been targeted.
Interference with IFN production and IFN function itself is a widely used
strategy: IFN-transcription can be inhibited by viruses91, 92, or they can produce IFN
decoy receptors93. In addition, the JAK-STAT signaling cascade, which is activated upon
triggering of the IFN-a/ß receptor (IFNAR), is targeted by several viruses94. Furthermore,
the effector molecules (e.g. RNA-dependent protein kinase, PKR; 2'-5'oligoadenylate
synthetase, OAS; RNaseL), which are induced via JAK-STAT signaling, can be targeted
once these cells become infected95, 96. In addition, also initiation of IFN-responses via
PRRs can be inhibited by interfering with the PRR-signaling pathway or prevention of
binding of viral RNA to PRRs97-99.
15
Chapter 1
Other strategies that are employed to inhibit immune responses include
targeting of DC maturation and function100-102. Furthermore, the genetic content of some
viruses has evolved to encode for their own anti-inflammatory cytokines103, 104.
Enteroviruses
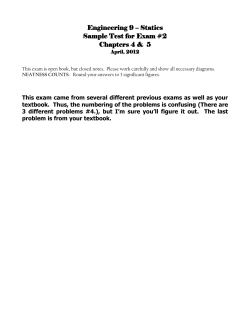
Enteroviruses belong to the family of the Picornaviridae (Fig. 4). Picornaviruses are the
cause of a number of serious human and animal diseases and major economical damage.
This large family of small RNA viruses consists of eight genera that include enteroviruses
(described below), parechoviruses, hepatoviruses, cardioviruses, kobuviruses and
genera that solely contain animal pathogens, such as the aphthoviruses (including
foot-and-mouth-disease virus). The enterovirus genus is divided into several species,
namely human enterovirus-A (HEV-A), HEV-B, HEV-C and HEV-D, rhinoviruses (that cause
common cold) and bovine and porcine species (Fig. 4). The best-known and mostly
studied enterovirus is the poliovirus, causative agent of poliomyelitis, which belongs to
the HEV-C species105. HEV-A species include EV71 which is a major health threat causing
hand-foot and mouth disease and central nervous system infections in Asia nowadays105,
106. The enteroviruses most often associated with type 1 diabetes belong to the HEV-B
—
Human enterovirus A
■
Human enterovirus B
—
—
Human enterovirus D
—
Simian enterovirus A
—
Bovine enterovirus A
—
Porcine enterovirus A
—
Porcine enterovirus B
—
“
“
Enterovirus
“
Cardiovirus
__ I1
__
1
“
1
Aphthovirus
—
Hepatovirus
—
Parechovirus
Human enterovirus C
p
Coxsackie B viruses
I
Echoviruses
Polioviruses
Human rhinovirus A
Human rhinovirus B
Encephalomyocarditis virus
Theilovirus
i
Foot-and-mouth disease virus
'
Equine rhinitis Avirus
—
Enterovirus 71
Hepatitis A virus
Picornaviridae —
—
Erbovirus
—
Kobovirus
I
Human parechovirus
1
Ljungan virus
—
Equine rhinitis Bvirus
■
—
Teschovirus
1
1
-
Aichi virus
Bovine kobuvirus
Porcine teschovirus
Figure 4. Schematic representation of the picornavirus family.
The eight different genera are depicted and their subdivision into species is specified. Some examples of
important human pathogens are given within the enterovirus species.
16
Introduction
species, e.g. coxsackie B viruses (CVB) and echoviruses (EV)105. A more detailed overview
of their life cycle and pathogenesis will be described below (Fig. 5).
The first requirement for viral infection is entry into cells which is mediated
by virus-specific receptors. All known serotypes of CVB make use of the coxsackie-andadenovirus receptor (CAR), and for CVB1, -3 and -5 decay accelerating factor (DAF, or
CD55) can be used as a co-receptor. Different EV serotypes use different receptors,
including DAF and very late antigen-2 (VLA2). Other cellular molecules that are used
as enteroviral receptors include integrins and other adhesion molecules107. Upon cell
entry, the virus releases a single-stranded positive RNA genome in the cytoplasm, that
is translated via an internal ribosomal entry site (IRES) into one large polyprotein. Virusencoded proteases subsequently cleave this polyprotein to yield the capsid proteins
and the non-structural replication proteins. The non-structural proteins form replication
RNA
release
VPg
translation
COOH
proteolytic
processing
*
K/PÏ1
cell
lysis
|2BC|I 2C
capsids
VPg
VPg
VPg
VPg
VPg
VPg
AAA(+)
— — AAA(+)
AAA(+)
VPg
AAA(+)
AAA(+)
(+) RNA
AAA(+
synthesis
i
Æ
“
!
W
|3D||3CD|
3A||3AB||3C|
replication proteins
I
(-) RNA
I synthesis
AAA(+)
UUU(
Figure 5. Schematic representation of the picornavirus life cycle.
The virus gains entry into the cell via a virus-specific entry receptor. After this, viral RNA is released into the
cytoplasm of the cell, where it is translated into a large polyprotein. Processing of the polyprotein by virally
encoded proteases yields the structural capsid proteins and the non-structural replication proteins. The ge
nomic RNA is used as a template for the production of complementary negative strand molecules, which, in
turn can be used for the generation of large numbers of positive stranded RNA molecules. Newly generated
positive stranded RNA molecules can be encapsidated to produce progeny virus. Alternatively, they can be
used for additional translation, or they may enter a new round of replication. Progeny viruses are released
via cell lysis.
complexes and, using the positive RNA strand as a template, will initiate production of
complementary negative-stranded RNAs. These will subsequently be used to synthesize
new positive-stranded RNAs. Positive-stranded RNAs can be translated to generate more
viral proteins, used for amplified replication, or encapsidated to produce new infectious
virus particles. The newly formed particles accumulate in the cytoplasm and are released
via cell lysis when the host cell loses its integrity108.
Enterovirus infection leads to massive rearrangement of intracellular
membranes, resulting in the accumulation of small ER/golgi-derived replication vesicles
17
Chapter 1
in the cytoplasm. Other modifications caused by the non-structural proteins are
rearrangement of the cytoskeleton, inhibition of transcription and translation of host
mRNA, and inhibition of ER to golgi transport108, 109. These alterations in the host cell
serve to shape the best possible environment for viral replication and to suppress the
host immune response. The virus-induced morphological changes in the infected cells
are known as cytopathic effects (CPE). Upon infection, apoptotic pathways are switched
on by the infected host cell, yet the virus suppresses the apoptotic program, at least in
vitro. Consequently, the cell-death that results after virus infection has hallmarks of both
apoptosis and necrosis110, 111.
Pathogenesis of Human Enterovirus B
Enterovirus transmission occurs primarily via the fecal-oral route, facilitated by the
acid-stability of the virus. However, also respiratory transmission may play a role105.
The majority (up to 80%) of enterovirus infections remains asymptomatic, and most
of the symptomatic infections are characterized by minor illness with fever, diarrhea,
vomiting and possibly rashes105, 112. Mild viremia can occur, but virus levels are low and
transient. Infection with different serotypes is common105. More severe enterovirus
infections can be accompanied by major viremia and spreading of the virus to secondary
organs. This can result in myocarditis, pancreatitis, meningitis, encephalitis and other
complications105. Severe disease is most often observed in neonates, but can also occur
later in life105, 113. Besides acute forms of disease, HEV-Bs have also been implicated in
chronic conditions, such as chronic myocarditis, dilated cardiomyopathy105, 114, 115 and
type 1 diabetes (see below)105.
The efficacy of the immune system is key to the outcome of enteroviral
infections. Both innate immune responses (e.g. IFN-production and NK cell activation105,
116) and adaptive immune responses (e.g. antibody production105, 114, 116, 117) are crucial to
fight enterovirus infections. Prolonged infections might develop in case of a defect in
one of the above-mentioned antiviral mechanisms. In particular, individuals suffering
from X-linked agammaglobulinemia may develop severe chronic infections possibly
with fatal outcome105, 116, 117. Besides host factors, also the virulence of the virus strain
concerned may play a role105, 118-120. As mentioned above, persistent infections have
been associated with certain chronic diseases, yet this issue remains controversial105,
114, 121, 122. when, on the other hand, part of the immune system reacts too aggressive,
uninfected cells and tissues may also be targeted. The subsequent damage might result
in chronic inflammation and could result in autoimmune responses. Autoimmunity has
been suggested to play a role in CVB-induced inflammation, starting with the report
that uninfected myocytes were also targeted in CVB-induced murine myocarditis105,
116. Furthermore antibodies reactive to heart tissue have been described in human
cardiomyopathy105, 116, although this was not confirmed in other studies123. Also in type 1
diabetes (T1D), a role for enterovirus infections has been proposed (see below).
Type 1 diabetes
Type 1 diabetes (T1D, also known as insulin-dependent diabetes mellitus, IDDM) is a
chronic, progressive disease that results from the failure of the insulin-producing ßcells in the islets of Langerhans to produce enough insulin. Islets of Langerhans consists
of insulin-producing ß-cells (~60%), glucagon-producing a-cells (~30%), somatostatin-
18
Introduction
producing 5-cells (~10%) and polypeptide-producing PP-cells (>5%)124, 125. T1D treatment
includes lifelong insulin-injections accompanied by careful monitoring of blood glucose
levels. T1D can have a long sub-clinical course during which ß-cell damage occurs;
however, clinical symptoms only arise when over 80% of the total ß-cells mass is impaired
in insulin production126, 127. Type 1 diabetes is commonly diagnosed in childhood and
adolescence - hence its former name "juvenile diabetes" -, but it can occur at any age,
even in the 8th and 9th decades of life128.
T1D can be further classified as immune-mediated (type 1A diabetes) or
idiopathic (type 1B diabetes). The majority of type 1 diabetes cases (~85-90%) is immunemediated129, 130. In immune-mediated T1D, antibodies against islets constituents such as
glutamic acid decarboxylase (GAD) 65, insulin, tyrosine phosphatase-like protein (IA-2)
appear before clinical onset of disease. When Abs against multiple ß-cell associated
proteins are found, the risk to develop T1D is increased131-134. Infiltration of immune cells
is frequently observed during immune mediated diabetes, as determined after biopsy
or at autopsy126, 135, 136. It has been postulated that autoimmune CTL responses may be
responsible for final ß-cell destruction137, 138.
In idiopathic, or fulminant diabetes, there is no evidence for an autoimmune
process, and diabetes-associated islets cell antibodies (ICA) are not found128, 139. Patients
often present with abrupt onset of symptoms. No evidence of insulitis was found in
the islets after biopsy or at autopsy in Japanese patients140; however, whether this
finding is universal for patients with idiopathic diabetes is unknown141. Furthermore,
recent studies reported autoreactive T cell populations and autoantibodies in patients
with fulminant T1D, thereby questioning whether immune-processes are not involved in
this type of T1D after all142-144. Due to the controversy between immune-mediated and
idiopathic diabetes143, the term T1D will be used in the remainder of this thesis to refer
to both types of diabetes.
Susceptibility to T1D is inherited, and many studies have been performed to
identify the genetic factors that predispose to T1D. The strongest genetic predisposition
to T1D is found in the HLA-locus. Especially individuals with HLA-DR3 or DR4 are prone to
develop T1D145-147. Other susceptibility loci that have been identified include the insulin
locus, the CTLA4 gene and the PTPN22 gene148-153. New associations are still being found,
and recently single nucleotide polymorphisms (SNPs) were identified in genes which are
involved in antiviral immunity154-157.
Studies in monozygotic twins revealed that the concordance rate for the
development of T1D is only 25-50%, suggesting that T1D development is environmentally
determined153, 158-160. Further evidence that environmental factors play a role in T1D
etiology is derived from migration studies; children that migrated from South-Asia where T1D incidence is lowest - to the United Kingdom at young age have similar chance
to develop T1D as indigenous British. Additional evidence arises from the geographical
variations in T1D. The lowest incidence (0.6 per 100,000) is found in South-Asia and
Oceania, whereas Europe has higher T1D incidence, with the highest incidence (40.9 per
100,000 in 1999) found in Finland134, 160, 161 (Fig. 6). Finally, a substantial rise in incidence
has been reported over the last decades, which must be due to factors in the environment
and lifestyle134, 161, 162. Taken together, the epidemiologic and genetic studies indicate that
environmental factor(s) can initiate disease in a susceptible individual134, 160.
Many different environmental factors have been mentioned as possible causes
or triggers of T1D. Among these are dietary factors such as cow milk, toxins, and virus
19
Chapter 1
Figure 6. Incidence of type 1 diabetes in children under age 14 years in Europe, 1990-1999.
Shown is a map reflecting the incidence of T1D in different countries in Europe. This map was generated using
data from the Diamond project group, Incidence and trends of childhood Type 1 diabetes worldwide 1990
1999, Diabet Med. 2006 Aug;23(8):857-66.
infections134, 163. Virus infections have been associated with T1D for over a century. The
most extensive evidence for an association with diabetes is found for enteroviruses,
mainly HEV-B such as CVB and EV. The first associations of HEV-B infections with T1D
originate from over 4 decades ago (Reference164 and references therein), and were
strengthened when Yoon and colleagues isolated a CVB4 strain from the pancreas of
a child with diabetic ketoacidosis165. This virus was capable to induce a diabetes-like
disease in mice. More cases where enterovirus was isolated from T1D patients have
been described since166-168, and these strains have been shown to induce diabetes in
mice166 or productively infect human pancreatic islets in vitro169, 170. Further evidence
that enteroviruses are involved in T1D arises from serological studies. More diabetes
patients were found to have anti-enterovirus Abs than a control population and the titers
of Abs against enteroviruses are higher in T1D patients (reviewed in171). Yet, controversy
as to whether HEV-B may cause T1D still remains172, 173. The development of reversetranscriptase polymerase chain reaction (RT-PCR) techniques, which are more sensitive
for detection than serological techniques, further supported the T1D-enterovirus
association. Analysis of blood or serum from T1D patients and control individuals showed
that enterovirus RNA is found at onset of disease in 20 to 75% of T1D patients, but not, or
with much lower frequency, in controls174-181. Enteroviruses have furthermore been found
in auto-antibody positive (pre-diabetic) persons179, 182, 183and in patients with established
T1D174, 175, but importantly, not, or with a much lower frequency, in matched healthy
controls without predisposition for T1D or in T2D patients174. These studies reinforced
20
Introduction
the conclusions of earlier serological studies suggesting that enterovirus infection is
associated with the development of type 1 diabetes. However, it should be noted that
the available data is circumstantial and no direct evidence for a causal relation of HEV-B
with T1D exists. Although much studies were initially focused on CVB4 and other CVBs,
also other HEV-B and, albeit rarely, HEV-A species have been have been associated with
T1D167, 169, 184. Furthermore, Roivainen and colleagues reported that a wide range of HEVB serotypes can infect human pancreatic islets in vitro185, indicating that the capacity of
HEV-B species is not restricted to CVB4, but that many, if not all, HEV-B species might
trigger or accelerate T1D development.
Putative mechanisms of HEV-B induced T1D
There are several, not mutually exclusive mechanisms by which enteroviruses may play
a role in T1D development. (i) These viruses may directly infect and kill ß-cells due to
lytic activity of the virus. Several independent groups have reported that enterovirus
RNA and proteins can be detected in the islets of T1D patients136, 186, 187. As mentioned
above, different serotypes can infect ß-cells in vitro and could thus be involved via
this mechanism. (ii) Virus-induced inflammation in the pancreas might result in the
production of cytokines such as TNF-a, IL-1ß and IFN-y, that are toxic to ß-cells either
alone or in combination188-191. The production of nitric oxide (NO), that occurs during
inflammation has been mentioned as a cause of ß-cell dysfunction and cell death191-195.
Not only cells of pancreatic origin may contribute to this bystander effect, also cells of the
innate immune system such as NK cells and macrophages might be activated and cause
ß-cell damage195, 196. (iii) Another mechanism that might contribute to the development
of T1D is activation of the adaptive immune system. Due to both the pro-inflammatory
microenvironment and the ß-cell damage that have developed upon infection, APCs such
as DCs encounter self-Ags in an environment where PAMPs and DAMPs are excessively
present, which could result in DC maturation and priming of (naive) autoreactive T cells.
It has been reported that development of T1D depends on the balance of autoreactive
Th1 and Tregcells56, 197 and this balance is greatly influenced by microenvironment and
maturation status of APCs34, 37, 38. (iv) Autoimmunity might be provoked due to molecular
mimicry: immune responses directed against the virus may also cross-react with selfAgs, such as suggested for the viral protein 2C and GAD65198-200. Although cross-reactivity
between these proteins has been reported201, 202, its importance in the pathogenesis of
T1D remains unproven203, 204.
The above-mentioned mechanisms by which HEV-B might contribute to
the pathogenesis of T1D are not mutually exclusive and could even contribute to the
development of this autoimmune disease in a synergistic manner. However, more
research is required to pinpoint the putative mechanisms leading to ß-cell damage and
establish a potential causal relationship between HEV-B infections and T1D.
21
Chapter 1
Aim & outline of this thesis
The aim of this thesis was to gain more insight in the possible pathogenic mechanisms
of HEV-B induced disease. Research focused on DCs, HEV-B and pancreatic cells and the
interplay between them.
Chapter 2 provides a brief overview of the expression of different PRRs in DC subsets
under pro-inflammatory and steady-state conditions. Additionally, cross-talk between
different DC subsets was investigated and a mechanism how pDCs may protect mDCs
in an environment with high viral burden is postulated. In Chapter 3 we investigated
the susceptibility of DCs for infection with HEV-B species. This study revealed that CVBs
are unable to infect DCs or influence their function, whereas EVs productively infect
DCs resulting in loss-of-function, aberrant response upon subsequent TLR-triggering and
ultimately, cell death. Chapter 4 reveals that poly I:C matured DCs are protected from
infection via an IFN-dependent mechanism, whereas DCs matured with other TLR-ligands
are not protected from infection. Furthermore, we provide evidence that CVB-infected
cells are efficiently phagocytosed by DCs leading to upregulation of IFNs and ISGs resulting
in an antiviral state, that also protects DCs from subsequent infection. Chapter 5 focuses
on the interaction between primary human pancreatic islets and DCs. We showed that
CVB-infected human islets are phagocytosed by DCs resulting in an upregulation of ISGs.
Using porcine islets and murine Min6 insuloma cells, we confirmed the importance of
IFNs for ISG-induction in DCs. We revealed that DC-responses depended on IFNs produced
by the DCs themselves, but not by the infected cells. Furthermore, RNA within infected,
phagocytosed pancreatic cells was shown to be of great importance for DC-responses.
These findings provide important new insights in the possible role of DCs during human
type 1 diabetes development. Chapter 6 describes the response of primary human islets
upon infection with HEV-B. We report that antiviral immunity is activated, indicated by
the induction of ISGs. Furthermore, expression of several cytokines and chemokines was
induced, and importantly, these could also be detected in the supernatant from infected
islets. These data suggest that islets, upon infection with HEV-B species, start antiviral
immune responses and produce a variety of cytokines and chemokines that can attract
and/or activate cells of both the innate and adaptive immune system that may maintain/
aggravate inflammation and might even trigger development of autoimmune processes
against ß-cells. In Chapter 7 we investigate the presence of enteroviruses in PBMC of
T1D patients and show that enterovirus RNA can be detected in 4 out of 10 patients,
but not in any of the controls. Merely complete absence of viral RNA in throat and stool
samples suggests that it might concern prolonged enterovirus infection. What the role
of prolonged infection in T1D is remains to be determined, yet one can envisage that
it results in continuous arousal of the immune system. Finally, Chapter 8 discusses the
results and significance of the findings described in this thesis.
22
Introduction
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
W. B. Whitman, D. C. Coleman, W. J. W iebe (1998). Prokaryotes: the unseen majority. Proc Natl Acad Sci U S A , 95, 6578-6583.
N. Bannert, R. Kurth (2004). Retroelements and the human genome: new perspectives on an old relation. Proc Natl Acad Sci U S A,
101 Suppl 2, 14572-14579.
D. Lindell, M. B. Sullivan, Z. I. Johnson, A. C. Tolonen, F. Rohwer, S. W . Chisholm (2004). Transfer of photosynthesis genes to and
from Prochlorococcus viruses. Proc Natl Acad Sci U S A, 101, 11013-11018.
L. P. Villarreal, V. R. DeFilippis (2000). A hypothesis for DNA viruses as the origin of eukaryotic replication proteins. J Virol, 74, 7079
7084.
G. J. Vermeij (1987). Evolution and Escalation: An Ecological History of Life
H. Feillet, J. F. Bach (2004). On the mechanisms of the protective effect of infections on type 1 diabetes. Clin Dev Immunol, 11, 191
194.
J. F. Bach (2005). Six questions about the hygiene hypothesis. Cell Immunol, 233, 158-161.
C. King, A. Ilic, K. Koelsch, N. Sarvetnick (2004). Homeostatic expansion of T cells during immune insufficiency generates
autoimmunity. Cell, 117, 265-277.
J. A. Gonzalo, T. Delaney, J. Corcoran, A. Goodearl, J. C. Gutierrez-Ramos, A. J. Coyle (2001). Cutting edge: the related molecules
CD28 and inducible costimulator deliver both unique and complementary signals required for optimal T cell activation. J Immunol,
166, 1-5.
L. Steinman (2007). A brief history of T(H)17, the first major revision in the T(H)1/T(H)2 hypothesis of T cell-mediated tissue damage.
Nat Med , 13, 139-145.
A. K. Abbas, K. M. Murphy, A. Sher (1996). Functional diversity of helper T lymphocytes. Nature, 383, 787-793.
T. R. Mosmann, H. Cherwinski, M. W. Bond, M. A. Giedlin, R. L. Coffman (1986). Two types of murine helper T cell clone. I. Definition
according to profiles of lymphokine activities and secreted proteins. J Immunol, 136, 2348-2357.
K. M. Murphy, S. L. Reiner (2002). The lineage decisions of helper T cells. Nat Rev Immunol, 2, 933-944.
L. E. Harrington, R. D. Hatton, P. R. Mangan, H. Turner, T. L. Murphy, K. M. Murphy, C. T. W eaver (2005). Interleukin 17-producing
CD4+ effector T cells develop via a lineage distinct from the T helper type 1 and 2 lineages. Nat Immunol, 6, 1123-1132.
H. Park, Z. Li, X. O. Yang, S. H. Chang, R. Nurieva, Y. H. Wang, Y. Wang, L. Hood, Z. Zhu, Q. Tian, C. Dong (2005). A distinct lineage of
CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat Immunol, 6, 1133-1141.
K. I. Happel, P. J. Dubin, M. Zheng, N. Ghilardi, C. Lockhart, L. J. Quinton, A. R. Odden, J. E. Shellito, G. J. Bagby, S. Nelson, J. K. Kolls
(2005). Divergent roles of IL-23 and IL-12 in host defense against Klebsiella pneumoniae. J Exp Med, 202, 761-769.
W. Hou, H. S. Kang, B. S. Kim (2009). Th17 cells enhance viral persistence and inhibit T cell cytotoxicity in a model of chronic virus
infection. J Exp Med, 206, 313-328.
F. L. van de Veerdonk, R. J. Marijnissen, B. J. Kullberg, H. J. Koenen, S. C. Cheng, I. Joosten, W. B. van den Berg, D. L. Williams, J. W.
van der Meer, L. A. Joosten, M. G. Netea (2009). The macrophage mannose receptor induces IL-17 in response to Candida albicans.
Cell Host Microbe , 5, 329-340.
W. Huang, L. Na, P. L. Fidel, P. Schwarzenberger (2004). Requirement of interleukin-17A for systemic anti-Candida albicans host
defense in mice. J Infect Dis , 190, 624-631.
T. Zelante, A. De Luca, C. D'Angelo, S. Moretti, L. Romani (2009). IL-17/Th17 in anti-fungal immunity: what's new? Eur J Immunol,
39, 645-648.
M. Chabaud, J. M. Durand, N. Buchs, F. Fossiez, G. Page, L. Frappart, P. Miossec (1999). Human interleukin-17: A T cell-derived
proinflammatory cytokine produced by the rheumatoid synovium. Arthritis Rheum, 42, 963-970.
G. X. Zhang, B. Gran, S. Yu, J. Li, I. Siglienti, X. Chen, M. Kamoun, A. Rostami (2003). Induction of experimental autoimmune
encephalomyelitis in IL-12 receptor-beta 2-deficient mice: IL-12 responsiveness is not required in the pathogenesis of inflammatory
demyelination in the central nervous system. J Immunol, 170, 2153-2160.
C. L. Langrish, Y. Chen, W. M. Blumenschein, J. Mattson, B. Basham, J. D. Sedgwick, T. McClanahan, R. A. Kastelein, D. J. Cua (2005).
IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J Exp Med, 201, 233-240.
R. P. Sutmuller, M. E. Morgan, M. G. Netea, O. Grauer, G. J. Adema (2006). Toll-like receptors on regulatory T cells: expanding
immune regulation. Trends Immunol, 27, 387-393.
M. Feuerer, J. A. Hill, D. Mathis, C. Benoist (2009). Foxp3+ regulatory T cells: differentiation, specification, subphenotypes. Nat
Immunol, 10, 689-695.
S. Sakaguchi, M. Ono, R. Setoguchi, H. Yagi, S. Hori, Z. Fehervari, J. Shimizu, T. Takahashi, T. Nomura (2006). Foxp3+ CD25+ CD4+
natural regulatory T cells in dominant self-tolerance and autoimmune disease. Immunol Rev, 212, 8-27.
S. Sakaguchi, T. Yamaguchi, T. Nomura, M. Ono (2008). Regulatory T cells and immune tolerance. Cell, 133, 775-787.
Y. Belkaid, K. Tarbell (2009). Regulatory T cells in the control of host-microorganism interactions (*). Annu Rev Immunol, 27, 551
589.
G. Ferlazzo, M. L. Tsang, L. Moretta, G. Melioli, R. M. Steinman, C. Munz (2002). Human dendritic cells activate resting natural killer
(NK) cells and are recognized via the NKp30 receptor by activated NK cells. J Exp Med, 195, 343-351.
D. Piccioli, S. Sbrana, E. Melandri, N. M. Valiante (2002). Contact-dependent stimulation and inhibition of dendritic cells by natural
killer cells. J Exp Med, 195, 335-341.
A. B. Geldhof, M. Moser, L. Lespagnard, K. Thielemans, P. De Baetselier (1998). Interleukin-12-activated natural killer cells recognize
B7 costimulatory molecules on tumor cells and autologous dendritic cells. Blood, 91, 196-206.
P. D. Shah (1987). Dendritic cells but not macrophages are targets for immune regulation by natural killer cells. Cell Immunol, 104,
440-445.
K. Palucka, J. Banchereau (1999). Dendritic cells: a link between innate and adaptive immunity. J Clin Immunol, 19, 12-25.
C. Reis e Sousa (2004). Activation of dendritic cells: translating innate into adaptive immunity. Curr Opin Immunol, 16, 21-25.
N. Kadowaki, S. Antonenko, J. Y. Lau, Y. J. Liu (2000). Natural interferon alpha/beta-producing cells link innate and adaptive
immunity. J Exp Med, 192, 219-226.
J. A. Villadangos, P. Schnorrer (2007). Intrinsic and cooperative antigen-presenting functions of dendritic-cell subsets in vivo. Nat Rev
Immunol, 7, 543-555.
J. Banchereau, F. Briere, C. Caux, J. Davoust, S. Lebecque, Y. J. Liu, B. Pulendran, K. Palucka (2000). Immunobiology of dendritic
cells. Annu Rev Immunol, 18, 767-811.
J. Banchereau, R. M. Steinman (1998). Dendritic cells and the control of immunity. Nature, 392, 245-252.
M. Colonna, G. Trinchieri, Y. J. Liu (2004). Plasmacytoid dendritic cells in immunity. Nat Immunol, 5, 1219-1226.
T. Ito, H. Kanzler, O. Duramad, W. Cao, Y. J. Liu (2006). Specialization, kinetics, and repertoire of type 1 interferon responses by
human plasmacytoid predendritic cells. Blood, 107, 2423-2431.
Y. J. Liu (2005). IPC: professional type 1 interferon-producing cells and plasmacytoid dendritic cell precursors. Annu Rev Immunol, 23,
275-306.
23
Chapter 1
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
81.
82.
83.
84.
24
F. Sallusto, A. Lanzavecchia (1994). Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by
granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J Exp Med,
179, 1109-1118.
M. L. Albert, S. F. Pearce, L. M. Francisco, B. Sauter, P. Roy, R. L. Silverstein, N. Bhardwaj (1998). Immature dendritic cells phagocytose
apoptotic cells via alphavbeta5 and CD36, and cross-present antigens to cytotoxic T lymphocytes. J Exp Med, 188, 1359-1368.
K. Inaba, M. Inaba, M. Naito, R. M. Steinman (1993). Dendritic cell progenitors phagocytose particulates, including bacillus
Calmette-Guerin organisms, and sensitize mice to mycobacterial antigens in vivo. J Exp Med, 178, 479-488.
C. Reis e Sousa, P. D. Stahl, J. M. Austyn (1993). Phagocytosis of antigens by Langerhans cells in vitro. J Exp Med, 178, 509-519.
F. Sallusto, M. Cella, C. Danieli, A. Lanzavecchia (1995). Dendritic cells use macropinocytosis and the mannose receptor to
concentrate macromolecules in the major histocompatibility complex class II compartment: downregulation by cytokines and
bacterial products. J Exp Med , 182, 389-400.
D. R. Green, T. Ferguson, L. Zitvogel, G. Kroemer (2009). Immunogenic and tolerogenic cell death. Nat Rev Immunol, 9, 353-363.
W. R. Heath, G. T. Belz, G. M. Behrens, C. M. Smith, S. P. Forehan, I. A. Parish, G. M. Davey, N. S. Wilson, F. R. Carbone, J. A.
Villadangos (2004). Cross-presentation, dendritic cell subsets, and the generation of immunity to cellular antigens. Immunol Rev,
199, 9-26.
T. Brocker, M. Riedinger, K. Karjalainen (1997). Targeted expression of major histocompatibility complex (MHC) class II molecules
demonstrates that dendritic cells can induce negative but not positive selection of thymocytes in vivo. J Exp Med, 185, 541-550.
L. W u, K. Shortman (2005). Heterogeneity of thymic dendritic cells. Semin Immunol, 17, 304-312.
V. Kronin, K. Winkel, G. Suss, A. Kelso, W. Heath, J. Kirberg, H. von Boehmer, K. Shortman (1996). A subclass of dendritic cells
regulates the response of naive CD8 T cells by limiting their IL-2 production. J Immunol, 157, 3819-3827.
G. Suss, K. Shortman (1996). A subclass of dendritic cells kills CD4 T cells via Fas/Fas-ligand-induced apoptosis. J Exp Med, 183, 1789
1796.
D. Hawiger, K. Inaba, Y. Dorsett, M. Guo, K. Mahnke, M. Rivera, J. V. Ravetch, R. M. Steinman, M. C. Nussenzweig (2001). Dendritic
cells induce peripheral T cell unresponsiveness under steady state conditions in vivo. J Exp Med, 194, 769-779.
K. Liu, T. Iyoda, M. Saternus, Y. Kimura, K. Inaba, R. M. Steinman (2002). Immune tolerance after delivery of dying cells to dendritic
cells in situ. J Exp Med, 196, 1091-1097.
R. M. Steinman, D. Hawiger, M. C. Nussenzweig (2003). Tolerogenic dendritic cells. Annu Rev Immunol, 21, 685-711.
N. Cools, P. Ponsaerts, V. F. Van Tendeloo, Z. N. Berneman (2007). Balancing between immunity and tolerance: an interplay between
dendritic cells, regulatory T cells, and effector T cells. J Leukoc Biol, 82, 1365-1374.
K. Steinbrink, K. Mahnke, S. Grabbe, A. H. Enk, H. Jonuleit (2009). Myeloid dendritic cell: From sentinel of immunity to key player
of peripheral tolerance? Hum Immunol, 70, 289-293.
R. M. Steinman, S. Turley, I. Mellman, K. Inaba (2000). The induction of tolerance by dendritic cells that have captured apoptotic
cells. J Exp Med, 191, 411-416.
P. Verginis, H. S. Li, G. Carayanniotis (2005). Tolerogenic semimature dendritic cells suppress experimental autoimmune thyroiditis
by activation of thyroglobulin-specific CD4+CD25+ T cells. J Immunol, 174, 7433-7439.
M. Menges, S. Rossner, C. Voigtlander, H. Schindler, N. A. Kukutsch, C. Bogdan, K. Erb, G. Schuler, M. B. Lutz (2002). Repetitive
injections of dendritic cells matured with tumor necrosis factor alpha induce antigen-specific protection of mice from autoimmunity.
J Exp Med, 195, 15-21.
N. Luckashenak, S. Schroeder, K. Endt, D. Schmidt, K. Mahnke, M. F. Bachmann, P. Marconi, C. A. Deeg, T. Brocker (2008).
Constitutive crosspresentation of tissue antigens by dendritic cells controls CD8+ T cell tolerance in vivo. Immunity, 28, 521-532.
C. A. Janeway, Jr. (1992). The immune system evolved to discriminate infectious nonself from noninfectious self. Immunol Today, 13,
11-16.
A. Roeder, C. J. Kirschning, R. A. Rupec, M. Schaller, G. Weindl, H. C. Korting (2004). Toll-like receptors as key mediators in innate
antifungal immunity. Med Mycol, 42, 485-498.
F. Hayashi, K. D. Smith, A. Ozinsky, T. R. Hawn, E. C. Yi, D. R. Goodlett, J. K. Eng, S. Akira, D. M. Underhill, A. Aderem (2001). The
innate immune response to bacterial flagellin is mediated by Toll-like receptor 5. Nature, 410, 1099-1103.
F. Weber, V. Wagner, S. B. Rasmussen, R. Hartmann, S. R. Paludan (2006). Double-stranded RNA is produced by positive-strand RNA
viruses and DNA viruses but not in detectable amounts by negative-strand RNA viruses. J Virol, 80, 5059-5064.
P. Matzinger (1994). Tolerance, danger, and the extended family. Annu Rev Immunol, 12, 991-1045.
P. Matzinger (2002). The danger model: a renewed sense of self. Science, 296, 301-305.
M. A. Willart, B. N. Lambrecht (2009). The danger within: endogenous danger signals, atopy and asthma. Clin Exp Allergy, 39, 12
19.
M. E. Bianchi (2007). DAMPs, PAMPs and alarmins: all we need to know about danger. J Leukoc Biol, 81, 1-5.
P. Scaffidi, T. Misteli, M. E. Bianchi (2002). Release of chromatin protein HMGB1 by necrotic cells triggers inflammation. Nature, 418,
191-195.
S. Gallucci, P. Matzinger (2001). Danger signals: SOS to the immune system. Curr Opin Immunol, 13, 114-119.
H. Kazama, J. E. Ricci, J. M. Herndon, G. Hoppe, D. R. Green, T. A. Ferguson (2008). Induction of immunological tolerance by
apoptotic cells requires caspase-dependent oxidation of high-mobility group box-1 protein. Immunity, 29, 21-32.
K. Takeda, T. Kaisho, S. Akira (2003). Toll-like receptors. Annu Rev Immunol, 21, 335-376.
J. S. Park, D. Svetkauskaite, Q. He, J. Y. Kim, D. Strassheim, A. Ishizaka, E. Abraham (2004). Involvement of toll-like receptors 2 and
4 in cellular activation by high mobility group box 1 protein. J Biol Chem, 279, 7370-7377.
A. Pichlmair, C. Reis e Sousa (2007). Innate recognition of viruses. Immunity, 27, 370-383.
T. Kawai, S. Akira (2006). Innate immune recognition of viral infection. Nat Immunol, 7, 131-137.
T. Venkataraman, M. Valdes, R. Elsby, S. Kakuta, G. Caceres, S. Saijo, Y. Iwakura, G. N. Barber (2007). Loss of DExD/H box RNA
helicase LGP2 manifests disparate antiviral responses. J Immunol, 178, 6444-6455.
D. A. Pippig, J. C. Hellmuth, S. Cui, A. Kirchhofer, K. Lammens, A. Lammens, A. Schmidt, S. Rothenfusser, K. P. Hopfner (2009). The
regulatory domain of the RIG-I family ATPase LGP2 senses double-stranded RNA. Nucleic Acids Res, 37, 2014-2025.
E. Meylan, J. Tschopp, M. Karin (2006). Intracellular pattern recognition receptors in the host response. Nature, 442, 39-44.
I. C. Allen, M. A. Scull, C. B. Moore, E. K. Holl, E. McElvania-TeKippe, D. J. Taxman, E. H. Guthrie, R. J. Pickles, J. P. Ting (2009). The
NLRP3 inflammasome mediates in vivo innate immunity to influenza A virus through recognition of viral RNA. Immunity, 30, 556
565.
P. G. Thomas, P. Dash, J. R. Aldridge, Jr., A. H. Ellebedy, C. Reynolds, A. J. Funk, W. J. Martin, M. Lamkanfi, R. J. Webby, K. L. Boyd,
P. C. Doherty, T. D. Kanneganti (2009). The intracellular sensor NLRP3 mediates key innate and healing responses to influenza A virus
via the regulation of caspase-1. Immunity, 30, 566-575.
T. Fernandes-Alnemri, J. W. Yu, P. Datta, J. W u, E. S. Alnemri (2009). AIM2 activates the inflammasome and cell death in response
to cytoplasmic DNA. Nature , 458, 509-513.
A. Takaoka, Z. Wang, M. K. Choi, H. Yanai, H. Negishi, T. Ban, Y. Lu, M. Miyagishi, T. Kodama, K. Honda, Y. Ohba, T. Taniguchi (2007).
DAI (DLM-1/ZBP1) is a cytosolic DNA sensor and an activator of innate immune response. Nature, 448, 501-505.
J. Tian, A. M. Avalos, S. Y. Mao, B. Chen, K. Senthil, H. W u, P. Parroche, S. Drabic, D. Golenbock, C. Sirois, J. Hua, L. L. An, L. Audoly,
Introduction
85.
86.
87.
88.
89.
90.
91.
92.
93.
94.
95.
96.
97.
98.
99.
100.
101.
102.
103.
104.
105.
106.
107.
108.
109.
110.
111.
112.
113.
114.
115.
116.
117.
118.
119.
120.
121.
122.
123.
124.
125.
G. La Rosa, A. Bierhaus, P. Naworth, A. Marshak-Rothstein, M. K. Crow, K. A. Fitzgerald, E. Latz, P. A. Kiener, A. J. Coyle (2007).
Toll-like receptor 9-dependent activation by DNA-containing immune complexes is mediated by HMGB1 and RAGE. Nat Immunol, 8,
487-496.
M. F. Roelofs, S. Abdollahi-Roodsaz, L. A. Joosten, W. B. van den Berg, T. R. Radstake (2008). The orchestra of Toll-like receptors and
their potential role in frequently occurring rheumatic conditions. Arthritis Rheum, 58, 338-348.
C. A. Biron, K. B. Nguyen, G. C. Pien, L. P. Cousens, T. P. Salazar-Mather (1999). Natural killer cells in antiviral defense: function and
regulation by innate cytokines. Annu Rev Immunol, 17, 189-220.
C. A. Biron, G. Sonnenfeld, R. M. Welsh (1984). Interferon induces natural killer cell blastogenesis in vivo. J Leukoc Biol, 35, 31-37.
T. Luft, K. C. Pang, E. Thomas, P. Hertzog, D. N. Hart, J. Trapani, J. Cebon (1998). Type I IFNs enhance the terminal differentiation of
dendritic cells. J Immunol, 161, 1947-1953.
J. Walker, D. F. Tough (2006). Modification of TLR-induced activation of human dendritic cells by type I IFN: synergistic interaction
with TLR4 but not TLR3 agonists. Eur J Immunol, 36, 1827-1836.
T. Nagai, O. Devergne, T. F. Mueller, D. L. Perkins, J. M. van Seventer, G. A. van Seventer (2003). Timing of IFN-beta exposure during
human dendritic cell maturation and naive Th cell stimulation has contrasting effects on Th1 subset generation: a role for IFN-betamediated regulation of IL-12 family cytokines and IL-18 in naive Th cell differentiation. J Immunol, 171, 5233-5243.
J. Jaworska, A. Gravel, K. Fink, N. Grandvaux, L. Flamand (2007). Inhibition of transcription of the beta interferon gene by the human
herpesvirus 6 immediate-early 1 protein. J Virol, 81, 5737-5748.
A. Billecocq, M. Spiegel, P. Vialat, A. Kohl, F. Weber, M. Bouloy, O. Haller (2004). NSs protein of Rift Valley fever virus blocks
interferon production by inhibiting host gene transcription. J Virol, 78, 9798-9806.
Z. Waibler, M. Anzaghe, T. Frenz, A. Schwantes, C. Pohlmann, H. Ludwig, M. Palomo-Otero, A. Alcami, G. Sutter, U. Kalinke (2009).
Vaccinia virus-mediated inhibition of type I interferon responses is a multifactorial process involving the soluble type I interferon
receptor B18 and intracellular components. J Virol, 83, 1563-1571.
R. E. Randall, S. Goodbourn (2008). Interferons and viruses: an interplay between induction, signalling, antiviral responses and virus
countermeasures. J Gen Virol, 89, 1-47.
R. Sanchez, I. Mohr (2007). Inhibition of cellular 2'-5' oligoadenylate synthetase by the herpes simplex virus type 1 Us11 protein. J
Virol, 81, 3455-3464.
J. O. Langland, J. M. Cameron, M. C. Heck, J. K. Jancovich, B. L. Jacobs (2006). Inhibition of PKR by RNA and DNA viruses. Virus Res,
119, 100-110.
P. M. Barral, J. M. Morrison, J. Drahos, P. Gupta, D. Sarkar, P. B. Fisher, V. R. Racaniello (2007). MDA-5 is cleaved in poliovirusinfected cells. J Virol, 81, 3677-3684.
F. Weber, G. Kochs, O. Haller (2004). Inverse interference: how viruses fight the interferon system. Viral Immunol, 17, 498-515.
E. Meylan, J. Curran, K. Hofmann, D. Moradpour, M. Binder, R. Bartenschlager, J. Tschopp (2005). Cardif is an adaptor protein in the
RIG-I antiviral pathway and is targeted by hepatitis C virus. Nature, 437, 1167-1172.
J. Engelmayer, M. Larsson, M. Subklewe, A. Chahroudi, W. I. Cox, R. M. Steinman, N. Bhardwaj (1999). Vaccinia virus inhibits the
maturation of human dendritic cells: a novel mechanism of immune evasion. J Immunol, 163, 6762-6768.
M. J. Raftery, M. Schwab, S. M. Eibert, Y. Samstag, H. Walczak, G. Schonrich (2001). Targeting the function of mature dendritic cells
by human cytomegalovirus: a multilayered viral defense strategy. Immunity, 15, 997-1009.
I. Fugier-Vivier, C. Servet-Delprat, P. Rivailler, M. C. Rissoan, Y. J. Liu, C. Rabourdin-Combe (1997). Measles virus suppresses cellmediated immunity by interfering with the survival and functions of dendritic and T cells. J Exp Med, 186, 813-823.
S. V. Kotenko, S. Saccani, L. S. Izotova, O. V. Mirochnitchenko, S. Pestka (2000). Human cytomegalovirus harbors its own unique
IL-10 homolog (cmvIL-10). Proc Natl Acad Sci U S A, 97, 1695-1700.
W. L. Chang, N. Baumgarth, D. Yu, P. A. Barry (2004). Human cytomegalovirus-encoded interleukin-10 homolog inhibits maturation
of dendritic cells and alters their functionality. J Virol, 78, 8720-8731.
M. A. Pallansch, R. P. Roos (2007). Enteroviruses: Polioviruses, Coxsackieviruses, Echoviruses, and Newer Enteroviruses. In Virology.
Fields Virology .
(2009). Watch your back. Nature, 459, 751-752.
J. M. Bergelson (2002). Receptors for Coxsackieviruses and Echoviruses. Molecular biology o f Picornaviruses.
V. R. Racaniello (2007). Picornaviridae: The Viruses and Their Replication. In Virology. Fields Virology.
L. Carrasco, R. Guinea, A. Irurzun, A. Barco (2002). Effects of Viral Replication on Cellular Membrane metabolism and Function.
Molecular biology o f Picornaviruses .
G. A. Belov, L. I. Romanova, E. A. Tolskaya, M. S. Kolesnikova, Y. A. Lazebnik, V. I. Agol (2003). The major apoptotic pathway
activated and suppressed by poliovirus. J Virol, 77, 45-56.
V. I. Agol, G. A. Belov, K. Bienz, D. Egger, M. S. Kolesnikova, L. I. Romanova, L. V. Sladkova, E. A. Tolskaya (2000). Competing death
programs in poliovirus-infected cells: commitment switch in the middle of the infectious cycle. J Virol, 74, 5534-5541.
J. A. Jenista, K. R. Powell, M. A. Menegus (1984). Epidemiology of neonatal enterovirus infection. J Pediatr, 104, 685-690.
H. A. Rotbart (2002). Clinical Significance, Diagnosis, and Treatment of Picornavirus Infections. Molecular biology o f Picornaviruses.
F. Colbère-Garapin, I. Pelletier, L. Ouzilou (2002). Persistent Infections by Picornaviruses. M olecular biology o f Picornaviruses.
N. M. Chapman, K. S. Kim (2008). Persistent coxsackievirus infection: enterovirus persistence in chronic myocarditis and dilated
cardiomyopathy. Curr Top Microbiol Immunol, 323, 275-292.
N. M. Chapman, C. J. Gauntt, S. Tracy (2002). Immunology of Coxsackieviruses. Molecular biology of Picornaviruses.
J. M. D. Galama (1997). Enteroviral infections in the immunocompromised host. REVIEWS IN MEDICAL MICROBIOLOGY 8, 33-40
J. J. Dunn, S. S. Bradrick, N. M. Chapman, S. M. Tracy, J. R. Romero (2003). The stem loop II within the 5' nontranslated region of
clinical coxsackievirus B3 genomes determines cardiovirulence phenotype in a murine model. J Infect Dis, 187, 1552-1561.
K. S. Kim, S. Tracy, W. Tapprich, J. Bailey, C. K. Lee, K. Kim, W. H. Barry, N. M. Chapman (2005). 5'-Terminal deletions occur in
coxsackievirus B3 during replication in murine hearts and cardiac myocyte cultures and correlate with encapsidation of negative
strand viral RNA. J Virol, 79, 7024-7041.
H. Yin, A. K. Berg, J. Westman, C. Hellerstrom, G. Frisk (2002). Complete nucleotide sequence of a Coxsackievirus B-4 strain
capable of establishing persistent infection in human pancreatic islet cells: effects on insulin release, proinsulin synthesis, and cell
morphology. J Med Virol, 68, 544-557.
W. J. Melchers, J. Zoll, F. J. van Kuppeveld, C. M. Swanink, J. M. D. Galama (1994). There is no evidence for persistent enterovirus
infections in chronic medical conditions in humans. Reviews in Medical Virology, 4, 235-243.
P. Muir, L. C. Archard (1994). There is evidence for persistent enterovirus infections in chronic medical conditions in humans. Reviews
in Medical Virology , 4, 245-250.
N. de Leeuw, W. J. Melchers, D. J. Ruiter, A. L. Caforio, A. H. Balk, N. de Jonge, J. M. Galama (1999). Autoimmune markers are
undetectable in end stage idiopathic dilated cardiomyopathy. J Clin Pathol, 52, 739-743.
M. Brissova, M. J. Fowler, W. E. Nicholson, A. Chu, B. Hirshberg, D. M. Harlan, A. C. Powers (2005). Assessment of human pancreatic
islet architecture and composition by laser scanning confocal microscopy. J Histochem Cytochem, 53, 1087-1097.
O. Cabrera, D. M. Berman, N. S. Kenyon, C. Ricordi, P. O. Berggren, A. Caicedo (2006). The unique cytoarchitecture of human
pancreatic islets has implications for islet cell function. Proc Natl Acad Sci U S A, 103, 2334-2339.
25
Chapter 1
126.
127.
128.
129.
130.
131.
132.
133.
134.
135.
136.
137.
138.
139.
140.
141.
142.
143.
144.
145.
146.
147.
148.
149.
150.
151.
152.
153.
154.
155.
156.
157.
158.
26
A. K. Foulis, C. N. Liddle, M. A. Farquharson, J. A. Richmond, R. S. W eir (1986). The histopathology of the pancreas in type 1 (insulin
dependent) diabetes mellitus: a 25-year review of deaths in patients under 20 years of age in the United Kingdom. Diabetologia, 29,
267-274.
M. A. Atkinson, N. K. Maclaren (1994). The pathogenesis of insulin-dependent diabetes mellitus. N Engl J Med, 331, 1428-1436.
(2003). Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care, 26 Suppl 1, S5-20.
C. Pihoker (2006). What type of diabetes do young people have? Curr Diab Rep, 6, 108-112.
R. D. White, G. D. Harris (2006). Case Study: "Birds of a Feather Flock Together": Type 1A Diabetes and Other Autoimmune Disease
States. Clinical Diabetes , 24, 40-43.
N. Maclaren, M. Lan, R. Coutant, D. Schatz, J. Silverstein, A. Muir, M. Clare-Salzer, J. X. She, J. Malone, S. Crockett, S. Schwartz, T.
Quattrin, M. DeSilva, P. Vander Vegt, A. Notkins, J. Krischer (1999). Only multiple autoantibodies to islet cells (ICA), insulin, GAD65,
IA-2 and IA-2beta predict immune-mediated (Type 1) diabetes in relatives. J Autoimmun, 12, 279-287.
M. Kukko, T. Kimpimaki, S. Korhonen, A. Kupila, S. Simell, R. Veijola, T. Simell, J. Ilonen, O. Simell, M. Knip (2005). Dynamics of
diabetes-associated autoantibodies in young children with human leukocyte antigen-conferred risk of type 1 diabetes recruited from
the general population. J Clin Endocrinol Metab, 90, 2712-2717.
T. Kimpimaki, P. Kulmala, K. Savola, P. Vahasalo, H. Reijonen, J. Ilonen, H. K. Akerblom, M. Knip (2000). Disease-associated
autoantibodies as surrogate markers of type 1 diabetes in young children at increased genetic risk. Childhood Diabetes in Finland
Study Group. J Clin Endocrinol Metab , 85, 1126-1132.
M. Knip, R. Veijola, S. M. Virtanen, H. Hyoty, O. Vaarala, H. K. Akerblom (2005). Environmental triggers and determinants of type 1
diabetes. Diabetes, 54 Suppl 2, S125-136.
A. K. Foulis (2008). Pancreatic pathology in type 1 diabetes in human. Novartis Found Symp, 292, 2-13; discussion 13-18, 122-129,
202-123.
F. Dotta, S. Censini, A. G. van Halteren, L. Marselli, M. Masini, S. Dionisi, F. Mosca, U. Boggi, A. O. Muda, S. D. Prato, J. F. Elliott,
A. Covacci, R. Rappuoli, B. O. Roep, P. Marchetti (2007). Coxsackie B4 virus infection of beta cells and natural killer cell insulitis in
recent-onset type 1 diabetic patients. Proc Natl Acad Sci U S A, 104, 5115-5120.
M. Roivainen (2006). Enteroviruses: new findings on the role of enteroviruses in type 1 diabetes. Int J Biochem Cell Biol, 38, 721
725.
S. Martin, D. Wolf-Eichbaum, G. Duinkerken, W. A. Scherbaum, H. Kolb, J. G. Noordzij, B. O. Roep (2001). Development of type 1
diabetes despite severe hereditary B-lymphocyte deficiency. N Engl J Med, 345, 1036-1040.
E. Kawasaki, N. Matsuura, K. Eguchi (2006). Type 1 diabetes in Japan. Diabetologia, 49, 828-836.
A. Imagawa, T. Hanafusa, J. Miyagawa, Y. Matsuzawa (2000). A novel subtype of type 1 diabetes mellitus characterized by a rapid
onset and an absence of diabetes-related antibodies. Osaka IDDM Study Group. N Engl J Med, 342, 301-307.
A. Pinero-Pilona, P. Raskin (2001). Idiopathic Type 1 diabetes. J Diabetes Complications, 15, 328-335.
R. Kotani, M. Nagata, A. Imagawa, H. Moriyama, H. Yasuda, J. Miyagawa, T. Hanafusa, K. Yokono (2004). T lymphocyte response
against pancreatic beta cell antigens in fulminant Type 1 diabetes. Diabetologia, 47, 1285-1291.
A. Shimada, J. Morimoto, K. Kodama, Y. Oikawa, J. Irie, Y. Nakagawa, S. Narumi, T. Saruta (2002). T-cell-mediated autoimmunity
may be involved in fulminant type 1 diabetes. Diabetes Care, 25, 635-636.
A. Shimada, Y. Oikawa, T. Shigihara, T. Senda, K. Kodama (2002). A case of fulminant type 1 diabetes with strong evidence of
autoimmunity. Diabetes Care , 25, 1482-1483.
J. A. Todd (1995). Genetic analysis of type 1 diabetes using whole genome approaches. Proc Natl Acad Sci U S A, 92, 8560-8565.
F. Cucca, R. Lampis, M. Congia, E. Angius, S. Nutland, S. C. Bain, A. H. Barnett, J. A. Todd (2001). A correlation between the relative
predisposition of MHC class II alleles to type 1 diabetes and the structure of their proteins. Hum Mol Genet, 10, 2025-2037.
M. A. Atkinson, G. S. Eisenbarth (2001). Type 1 diabetes: new perspectives on disease pathogenesis and treatment. Lancet, 358,
221-229.
G. I. Bell, S. Horita, J. H. Karam (1984). A polymorphic locus near the human insulin gene is associated with insulin-dependent
diabetes mellitus. Diabetes , 33, 176-183.
L. Nistico, R. Buzzetti, L. E. Pritchard, B. Van der Auwera, C. Giovannini, E. Bosi, M. T. Larrad, M. S. Rios, C. C. Chow, C. S. Cockram,
K. Jacobs, C. Mijovic, S. C. Bain, A. H. Barnett, C. L. Vandewalle, F. Schuit, F. K. Gorus, R. Tosi, P. Pozzilli, J. A. Todd (1996). The CTLA-4
gene region of chromosome 2q33 is linked to, and associated with, type 1 diabetes. Belgian Diabetes Registry. Hum M ol Genet, 5,
1075-1080.
H. Ueda, J. M. Howson, L. Esposito, J. Heward, H. Snook, G. Chamberlain, D. B. Rainbow, K. M. Hunter, A. N. Smith, G. Di Genova,
M. H. Herr, I. Dahlman, F. Payne, D. Smyth, C. Lowe, R. C. Twells, S. Howlett, B. Healy, S. Nutland, H. E. Rance, V. Everett, L. J. Smink,
A. C. Lam, H. J. Cordell, N. M. Walker, C. Bordin, J. Hulme, C. Motzo, F. Cucca, J. F. Hess, M. L. Metzker, J. Rogers, S. Gregory, A.
Allahabadia, R. Nithiyananthan, E. Tuomilehto-Wolf, J. Tuomilehto, P. Bingley, K. M. Gillespie, D. E. Undlien, K. S. Ronningen, C.
Guja, C. Ionescu-Tirgoviste, D. A. Savage, A. P. Maxwell, D. J. Carson, C. C. Patterson, J. A. Franklyn, D. G. Clayton, L. B. Peterson, L.
S. Wicker, J. A. Todd, S. C. Gough (2003). Association of the T-cell regulatory gene CTLA4 with susceptibility to autoimmune disease.
Nature , 423, 506-511.
N. Bottini, L. Musumeci, A. Alonso, S. Rahmouni, K. Nika, M. Rostamkhani, J. MacMurray, G. F. Meloni, P. Lucarelli, M. Pellecchia,
G. S. Eisenbarth, D. Comings, T. Mustelin (2004). A functional variant of lymphoid tyrosine phosphatase is associated with type I
diabetes. Nat Genet , 36, 337-338.
D. Smyth, J. D. Cooper, J. E. Collins, J. M. Heward, J. A. Franklyn, J. M. Howson, A. Vella, S. Nutland, H. E. Rance, L. Maier, B. J.
Barratt, C. Guja, C. Ionescu-Tirgoviste, D. A. Savage, D. B. Dunger, B. Widmer, D. P. Strachan, S. M. Ring, N. Walker, D. G. Clayton,
R. C. Twells, S. C. Gough, J. A. Todd (2004). Replication of an association between the lymphoid tyrosine phosphatase locus (LYP/
PTPN22) with type 1 diabetes, and evidence for its role as a general autoimmunity locus. Diabetes, 53, 3020-3023.
J. Kaprio, J. Tuomilehto, M. Koskenvuo, K. Romanov, A. Reunanen, J. Eriksson, J. Stengard, Y. A. Kesaniemi (1992). Concordance for
type 1 (insulin-dependent) and type 2 (non-insulin-dependent) diabetes mellitus in a population-based cohort of twins in Finland.
Diabetologia , 35, 1060-1067.
L. L. Field, V. Bonnevie-Nielsen, F. Pociot, S. Lu, T. B. Nielsen, H. Beck-Nielsen (2005). OAS1 splice site polymorphism controlling
antiviral enzyme activity influences susceptibility to type 1 diabetes. Diabetes, 54, 1588-1591.
D. J. Smyth, J. D. Cooper, R. Bailey, S. Field, O. Burren, L. J. Smink, C. Guja, C. Ionescu-Tirgoviste, B. Widmer, D. B. Dunger, D. A.
Savage, N. M. Walker, D. G. Clayton, J. A. Todd (2006). A genome-wide association study of nonsynonymous SNPs identifies a type
1 diabetes locus in the interferon-induced helicase (IFIH1) region. Nat Genet, 38, 617-619.
M. C. Tessier, H. Q. Qu, R. Frechette, F. Bacot, R. Grabs, S. P. Taback, M. L. Lawson, S. E. Kirsch, T. J. Hudson, C. Polychronakos
(2006). Type 1 diabetes and the OAS gene cluster: association with splicing polymorphism or haplotype? J Med Genet, 43, 129-132.
J. A. Todd, N. M. Walker, J. D. Cooper, D. J. Smyth, K. Downes, V. Plagnol, R. Bailey, S. Nejentsev, S. F. Field, F. Payne, C. E. Lowe,
J. S. Szeszko, J. P. Hafler, L. Zeitels, J. H. Yang, A. Vella, S. Nutland, H. E. Stevens, H. Schuilenburg, G. Coleman, M. Maisuria, W.
Meadows, L. J. Smink, B. Healy, O. S. Burren, A. A. Lam, N. R. Ovington, J. Allen, E. Adlem, H. T. Leung, C. Wallace, J. M. Howson,
C. Guja, C. Ionescu-Tirgoviste, M. J. Simmonds, J. M. Heward, S. C. Gough, D. B. Dunger, L. S. Wicker, D. G. Clayton (2007). Robust
associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet, 39, 857-864.
D. Kumar, N. S. Gemayel, D. Deapen, D. Kapadia, P. H. Yamashita, M. Lee, J. H. Dwyer, P. Roy-Burman, G. A. Bray, T. M. Mack (1993).
Introduction
159.
160.
161.
162.
163.
164.
165.
166.
167.
168.
169.
170.
171.
172.
173.
174.
175.
176.
177.
178.
179.
180.
181.
182.
183.
184.
185.
186.
187.
188.
189.
190.
191.
192.
193.
194.
195.
196.
197.
198.
199.
North-American twins with IDDM. Genetic, etiological, and clinical significance of disease concordance according to age, zygosity,
and the interval after diagnosis in first twin. Diabetes, 42, 1351-1363.
M. J. Redondo, L. Yu, M. Hawa, T. Mackenzie, D. A. Pyke, G. S. Eisenbarth, R. D. Leslie (2001). Heterogeneity of type I diabetes:
analysis of monozygotic twins in Great Britain and the United States. Diabetologia, 44, 354-362.
R. Varela-Calvino, M. Peakman (2003). Enteroviruses and type 1 diabetes. Diabetes Metab Res Rev, 19, 431-441.
(2006). Incidence and trends of childhood Type 1 diabetes worldwide 1990-1999. Diabet Med, 23, 857-866.
C. C. Patterson, G. G. Dahlquist, E. Gyurus, A. Green, G. Soltesz (2009). Incidence trends for childhood type 1 diabetes in Europe
during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet, 373, 2027-2033.
H. K. Akerblom, M. Knip (1998). Putative environmental factors in Type 1 diabetes. Diabetes Metab Rev, 14, 31-67.
(1971). Coxsackie viruses and diabetes. Lancet, 2, 804.
J. W. Yoon, M. Austin, T. Onodera, A. L. Notkins (1979). Isolation of a virus from the pancreas of a child with diabetic ketoacidosis.
N Engl J Med , 300, 1173-1179.
H. F. Champsaur, G. F. Bottazzo, J. Bertrams, R. Assan, C. Bach (1982). Virologic, immunologic, and genetic factors in insulin
dependent diabetes mellitus. J Pediatr , 100, 15-20.
G. R. Vreugdenhil, N. C. Schloot, A. Hoorens, C. Rongen, D. G. Pipeleers, W. J. Melchers, B. O. Roep, J. M. Galama (2000). Acute
onset of type I diabetes mellitus after severe echovirus 9 infection: putative pathogenic pathways. Clin Infect Dis, 31, 1025-1031.
M. Hindersson, A. Elshebani, A. Orn, T. Tuvemo, G. Frisk (2005). Simultaneous type 1 diabetes onset in mother and son coincident
with an enteroviral infection. J Clin Virol, 33, 158-167.
A. Elshebani, A. Olsson, J. Westman, T. Tuvemo, O. Korsgren, G. Frisk (2007). Effects on isolated human pancreatic islet cells after
infection with strains of enterovirus isolated at clinical presentation of type 1 diabetes. Virus Res, 124, 193-203.
A. Paananen, P. Ylipaasto, E. Rieder, T. Hovi, J. Galama, M. Roivainen (2003). Molecular and biological analysis of echovirus 9 strain
isolated from a diabetic child. J Med Virol, 69, 529-537.
H. Hyoty, K. W. Taylor (2002). The role of viruses in human diabetes. Diabetologia, 45, 1353-1361.
E. A. Gale, M. Atkinson (2004). A piece of nucleic acid surrounded by controversy: coxsackievirus and the causes of Type 1 diabetes.
Diabet Med , 21, 503-506.
K. W. Taylor (2005). Viruses and diabetes. Diabet Med, 22, 957-958; author reply 958.
L. Andreoletti, D. Hober, C. Hober-Vandenberghe, S. Belaich, M. C. Vantyghem, J. Lefebvre, P. W attre (1997). Detection of coxsackie
B virus RNA sequences in whole blood samples from adult patients at the onset of type I diabetes mellitus. J Med Virol, 52, 121
127.
W. Chehadeh, J. Weill, M. C. Vantyghem, G. Alm, J. Lefebvre, P. Wattre, D. Hober (2000). Increased level of interferon-alpha in blood
of patients with insulin-dependent diabetes mellitus: relationship with coxsackievirus B infection. J Infect Dis, 181, 1929-1939.
G. B. Clements, D. N. Galbraith, K. W. Taylor (1995). Coxsackie B virus infection and onset of childhood diabetes. Lancet, 346, 221
223.
M. E. Craig, N. J. Howard, M. Silink, W. D. Rawlinson (2003). Reduced frequency of HLA DRB1*03-DQB1*02 in children with type 1
diabetes associated with enterovirus RNA. J Infect Dis , 187, 1562-1570.
G. G. Dahlquist, J. Forsberg, L. Hagenfeldt, J. Boman, P. Juto (2004). Increased prevalence of enteroviral RNA in blood spots from
newborn children who later developed type 1 diabetes: a population-based case-control study. Diabetes Care, 27, 285-286.
V. Moya-Suri, M. Schlosser, K. Zimmermann, I. Rjasanowski, L. Gurtler, R. Mentel (2005). Enterovirus RNA sequences in sera of
schoolchildren in the general population and their association with type 1-diabetes-associated autoantibodies. J Med Microbiol, 54,
879-883.
C. Nairn, D. N. Galbraith, K. W. Taylor, G. B. Clements (1999). Enterovirus variants in the serum of children at the onset of Type 1
diabetes mellitus. Diabet Med , 16, 509-513.
H. Yin, A. K. Berg, T. Tuvemo, G. Frisk (2002). Enterovirus RNA is found in peripheral blood mononuclear cells in a majority of type 1
diabetic children at onset. Diabetes, 51, 1964-1971.
M. Lonnrot, K. Korpela, M. Knip, J. Ilonen, O. Simell, S. Korhonen, K. Savola, P. Muona, T. Simell, P. Koskela, H. Hyoty (2000).
Enterovirus infection as a risk factor for beta-cell autoimmunity in a prospectively observed birth cohort: the Finnish Diabetes
Prediction and Prevention Study. Diabetes, 49, 1314-1318.
M. Lonnrot, K. Salminen, M. Knip, K. Savola, P. Kulmala, P. Leinikki, T. Hyypia, H. K. Akerblom, H. Hyoty (2000). Enterovirus RNA
in serum is a risk factor for beta-cell autoimmunity and clinical type 1 diabetes: a prospective study. Childhood Diabetes in Finland
(DiMe) Study Group. J Med Virol, 61, 214-220.
G. Frisk, E. Nilsson, T. Tuvemo, G. Friman, H. Diderholm (1992). The possible role of Coxsackie A and echo viruses in the pathogenesis
of type I diabetes mellitus studied by IgM analysis. J Infect, 24, 13-22.
M. Roivainen, P. Ylipaasto, C. Savolainen, J. Galama, T. Hovi, T. Otonkoski (2002). Functional impairment and killing of human beta
cells by enteroviruses: the capacity is shared by a wide range of serotypes, but the extent is a characteristic of individual virus strains.
Diabetologia , 45, 693-702.
S. J. Richardson, A. Willcox, A. J. Bone, A. K. Foulis, N. G. Morgan (2009). The prevalence of enteroviral capsid protein vp1
immunostaining in pancreatic islets in human type 1 diabetes. Diabetologia.
P. Ylipaasto, K. Klingel, A. M. Lindberg, T. Otonkoski, R. Kandolf, T. Hovi, M. Roivainen (2004). Enterovirus infection in human
pancreatic islet cells, islet tropism in vivo and receptor involvement in cultured islet beta cells. Diabetologia, 47, 225-239.
C. A. Delaney, D. Pavlovic, A. Hoorens, D. G. Pipeleers, D. L. Eizirik (1997). Cytokines induce deoxyribonucleic acid strand breaks and
apoptosis in human pancreatic islet cells. Endocrinology, 138, 2610-2614.
T. Mandrup-Poulsen (2003). Apoptotic signal transduction pathways in diabetes. Biochem Pharmacol, 66, 1433-1440.
T. Mandrup-Poulsen (1996). The role of interleukin-1 in the pathogenesis of IDDM. Diabetologia, 39, 1005-1029.
D. Mauricio, T. Mandrup-Poulsen (1998). Apoptosis and the pathogenesis of IDDM: a question of life and death. Diabetes, 47, 1537
1543.
M. Ankarcrona, J. M. Dypbukt, B. Brune, P. Nicotera (1994). Interleukin-1 beta-induced nitric oxide production activates apoptosis
in pancreatic RINm5F cells. Exp Cell Res, 213, 172-177.
J. A. Corbett, J. L. Wang, J. H. Hughes, B. A. Wolf, M. A. Sweetland, J. R. Lancaster, Jr., M. L. McDaniel (1992). Nitric oxide and cyclic
GMP formation induced by interleukin 1 beta in islets of Langerhans. Evidence for an effector role of nitric oxide in islet dysfunction.
Biochem J, 287 ( Pt 1), 229-235.
E. Kawasaki, N. Abiru, K. Eguchi (2004). Prevention of type 1 diabetes: from the view point of beta cell damage. Diabetes Res Clin
Pract, 66 Suppl 1, S27-32.
S. A. Steer, A. L. Scarim, K. T. Chambers, J. A. Corbett (2006). Interleukin-1 stimulates beta-cell necrosis and release of the
immunological adjuvant HMGB1. PLoS Med, 3, e17.
H. Rothe, H. Kolb (1999). Strategies of protection from nitric oxide toxicity in islet inflammation. J Mol Med, 77, 40-44.
S. Arif, T. I. Tree, T. P. Astill, J. M. Tremble, A. J. Bishop, C. M. Dayan, B. O. Roep, M. Peakman (2004). Autoreactive T cell responses
show proinflammatory polarization in diabetes but a regulatory phenotype in health. J Clin Invest, 113, 451-463.
M. Solimena, P. De Camilli (1995). Coxsackieviruses and diabetes. Nat Med, 1, 25-26.
G. R. Vreugdenhil, A. Geluk, T. H. Ottenhoff, W. J. Melchers, B. O. Roep, J. M. Galama (1998). Molecular mimicry in diabetes
27
Chapter 1
200.
201.
202.
203.
204.
28
mellitus: the homologous domain in coxsackie B virus protein 2C and islet autoantigen GAD65 is highly conserved in the coxsackie
B-like enteroviruses and binds to the diabetes associated HLA-DR3 molecule. Diabetologia, 41, 40-46.
R. J. Ellis, R. Varela-Calvino, T. I. Tree, M. Peakman (2005). HLA Class II molecules on haplotypes associated with type 1 diabetes
exhibit similar patterns of binding affinities for coxsackievirus P2C peptides. Immunology, 116, 337-346.
J. Tian, P. V. Lehmann, D. L. Kaufman (1994). T cell cross-reactivity between coxsackievirus and glutamate decarboxylase is associated
with a murine diabetes susceptibility allele. J Exp Med, 180, 1979-1984.
M. A. Atkinson, M. A. Bowman, L. Campbell, B. L. Darrow, D. L. Kaufman, N. K. Maclaren (1994). Cellular immunity to a determinant
common to glutamate decarboxylase and coxsackie virus in insulin-dependent diabetes. J Clin Invest, 94, 2125-2129.
N. C. Schloot, S. J. Willemen, G. Duinkerken, J. W. Drijfhout, R. R. de Vries, B. O. Roep (2001). Molecular mimicry in type 1 diabetes
mellitus revisited: T-cell clones to GAD65 peptides with sequence homology to Coxsackie or proinsulin peptides do not crossreact
with homologous counterpart. Hum Immunol, 62, 299-309.
M. S. Horwitz, L. M. Bradley, J. Harbertson, T. Krahl, J. Lee, N. Sarvetnick (1998). Diabetes induced by Coxsackie virus: initiation by
bystander damage and not molecular mimicry. Nat Med, 4, 781-785.
Chapter 2
Cross-talk between human
dendritic cell subsets influences
expression of RNA sensors and
inhibits picornavirus infection
Barbara M. Schulte*, Matthijs Kramer*, Dagmar EleveldTrancikova, Maaike van Hout-Kuijer, Liza W.J. Toonen,
Jurjen Tel, I. Jolanda M. de Vries, Frank J. M. van Kuppeveld,
Bastiaan J.H. Jansen, Gosse J. Adema
* These authors contributed equally
Journal of Innate Immunity, in press
Chapter 2
Abstract
endritic cells (DCs) are professional antigen presenting cells that provide a link
between innate and adaptive immunity. Multiple DC subsets exist and their
activation by microorganisms occurs through binding of conserved pathogenderived structures to so-called pattern recognition receptors (PRRs). In this study we
analyzed the expression of PRRs responding to viral RNA in human monocyte-derived
DCs (moDCs) under steady-state or pro-inflammatory conditions. We found that mRNA
and protein levels for most PRRs were increased under pro-inflammatory conditions,
with the most pronounced increases in the RIG-like helicase (RLH)-family. Additionally,
freshly isolated human plasmacytoid DCs (pDCs) displayed significantly higher levels
of TLR7, RIG-I, MDA5 and PKR as compared to myeloid DCs and moDCs. Finally, we
demonstrate for the first time that cross-talk between TLR-matured or virus-stimulated
pDCs and moDC leads to a type I interferon-dependent antiviral state in moDCs. This
antiviral state was characterized by enhanced RLH expression and protection against
picornavirus infection. These findings might represent a novel mechanism by which
pDCs can preserve the function and viability of myeloid DCs that are attracted to a site
with ongoing infection, thereby optimizing the antiviral immune response.
D
30
Human DC cross-talk influences antiviral immunity
Introduction
Dendritic cells (DCs) are specialized antigen-presenting cells that are crucial players
in the decision process between tolerance and immunity. They participate in the
innate immune response, but also orchestrate adaptive immunity via regulation of T
cell activation and differentiation1, 2. Different DC subsets exist that are specialized in
regulation of distinct facets of the immune response. For instance, plasmacytoid DCs
(pDCs) are well equipped to recognize viral structures, resulting in potent type I interferon
(IFN) production3. Myeloid DCs (mDCs) can recognize structures derived from several
classes of microorganisms and are key to the induction of Th1 responses via release of IL123-5. For in vitro studies monocyte-derived DCs (moDCs) are often used in stead of mDC.
Responses of moDCs are similar to mDCs in many aspects3, 6, yet differences exist7, 8.
Recognition of microorganisms occurs via binding of pathogen-associated
molecular patterns, PAMPs, to so-called pattern-recognition receptors (PRRs), such as
the cytoplasmic NOD-like receptors and RIG-I-like helicases and the membrane-bound
C-type lectins and Toll-like receptors9. Triggering of TLRs on DCs by PAMPs, such as
double-stranded RNA (dsRNA) or lipopolysaccharide (LPS), results in production of proand anti-inflammatory cytokines and upregulation of MHC and costimulatory molecules
that collectively determine T cell activation and differentiation10. Despite their crucial
role in antiviral immunity, TLRs that recognize viral RNA are unable to detect viruses
in the cytoplasm, due to their endosomal localization. However, the recently identified
PRR-family called the RIG-I-like helicases (RLHs) appears to be involved in responses to
cytoplasmic viral RNA. The RLHs retinoic acid-inducible gene I (RIG-I) and melanoma
differentiation-associated gene 5 (MDA5) respond to different RNA viruses through
recognition of distinct RNA structures11-14. Activation of RIG-I or MDA5 is of crucial
importance for the induction of innate antiviral immune responses upon virus infection15.
The third member of the RLH family, LGP2, lacks a signaling domain and is thought to
serve as a negative regulator16. Another RNA-sensor that does not belong to the RLH
family is protein kinase R (PKR), which inhibits translation upon detection of dsRNA in
the cytoplasm17.
Unlike TLRs, much less is known regarding the function and expression of RLHs.
The vast majority of studies concerning RLHs have been done in mice or cell lines, with
little data on expression of these molecules in primary human cells. In this study we
investigated the expression levels of TLRs and RLHs in human moDCs under steady-state
or pro-inflammatory conditions. In addition, we determined the expression profiles
of RNA sensors in different primary human DC subsets which revealed remarkably
high expression of RLHs in plasmacytoid DCs compared to their myeloid counterpart.
Differential expression of PRRs likely tailors the response to specific pathogens executed
by various DC subsets. Cross-talk between DCs subsets might further aid in induction
of optimal immune responses. We therefore determined the influence of cross-talk
between pDCs and moDCs, which showed that TLR- or virus-activated pDCs increased
expression of RLHs in moDCs and induced protection against picornavirus infection.
31
Chapter 2
Materials & Methods
Culture and stimulation of cells
Monocyte-derived DCs (moDCs) were generated from different donors as described previously18. Immature
moDCs were harvested on day 6 using cold PBS and incubated with medium (RPMI-1640) alone or stimulated
with purified LPS (100 ng/ml) + IFNy (400 U/ml) at 37°C for a period of 4, 8 or 24 h. Alternatively, moDCs
were stimulated using 100 U/ml IFNa2 (Roferon-A®, Roche) or a 1:100 dilution of cell-free supernatant of
CpG-C or R848 activated-plasmacytoid DCs (pDCs) (collected 24 h after stimulation) or virus-simulated pDC
(see below). Myeloid and plasmacytoid DCs were isolated using anti-BDCA-1 and anti-BDCA-4-conjugated
magnetic microbeads, respectively, according to the manufacturer's instructions (Miltenyi Biotec).
RNA isolation
Total RNA was isolated from DC cultures using TRIZOL reagent (Invitrogen Life Technologies) according to
manufacturer's instructions. RNA integrity was determined by analyzing the ribosomal 28S and 18S bands on
a 1% agarose gel. The reverse transcription reaction was performed using Moloney murine leukemia virus (M
MLV) reverse transcriptase (Invitrogen) according to the manufacturers' instructions. To exclude genomic DNA
contamination we included a '-RT' control for each sample in which the reverse transcriptase was replaced by
DEPC treated milli-Q after which qPCR on a single-exon gene (SOCS-1) was performed. The cDNA was stored
at -20°C until further use.
Quantitative PCR
Quantitative PCR (qPCR) analysis of gene expression in DCs was performed using TaqMan® Custom Arrays
(Applied Biosystems) based on microfluidic card technology. Arrays were run on the ABI PRISM 7900HT
Sequence Detection System and data were analyzed using SDS 2.2.2 software (Applied Biosystems).
Alternatively, qPCR data were obtained using SYBR Green (Applied Biosystems) based qPCR according to the
manufacturers' instructions. Primer sequences are available upon request and were from the Primer Bank
database19. Reactions were performed on an ABI PRISM 7900 Sequence Detection System (Applied Biosystems).
Data were analyzed using 7000 System SDS software (Applied Biosystems). Genes with a Ct-value higher than
37 were considered not expressed. ACt values were calculated for all individual genes in all donors, with that
of porphobilinogen deaminase (PBGD, also known as hydroxymethylbilane synthase (HMBS)) as a reference.
An Excel macro was used to generate a heatmap, where 1 grayscale encompasses 2 ACt units. White indicates
highest expression, whereas black corresponds to undetectable expression.
Confocal microscopy
Monocyte-derived DCs (moDC) or plasmacytoid DCs (pDCs) were harvested, washed and allowed to adhere to
poly-L-lysine coated coverslips in serum free medium for 1 h at 37oC. Cells were fixed with 1% paraformaldehyde
(PFA) and blocked in PBS with 3% BSA, 10 mM glycine and 2% human serum (blocking buffer, BB). For cell
surface stainings, moDCs and pDCs were incubated using mouse-anti-human DC-SIGN (Beckman Coulter) or
mouse-anti human BDCA4 (Miltenyi Biotec GmbH), respectively, or the appropriate isotype control in BB.
Following incubation and washes, cells were incubated with isotype specific Alexa labeled goat-anti-mouse IgGs
(Molecular Probes). For intracellular staining, cells were fixed using 1% PFA, permeabilized using 0.1% TritonX100 in PBS and incubated with rabbit polyclonal anti-MDA520followed by incubation with goat-anti-rabbit IgG
Alexa 488 (Pharmingen) in BB. Cells were sealed using Mowiol (Merck) and analyzed by confocal laser scanning
microscopy on a MRC1024 confocal microscope (BioRad, Hercules, CA). Signals were collected sequentially to
avoid bleed through and were processed with Photoshop 7.0 software (Adobe Systems incorporated).
Western blot
Equal amounts of protein were separated by 7.5 % SDS-PAGE, electroblotted onto nitro-cellulose membranes
(Bio-Rad), followed by probing with the indicated antibodies. Anti-RIG-I and anti-PKR antibodies were purchased
from ProSci Incorporated and Becton Dickinson Transduction Laboratories, respectively. RIG-I, PKR and MDA5
antibodies were used in 1:1,000; 1:500 and 1:10,000 dilutions, respectively. After washes, membranes were
32
Human DC cross-talk influences antiviral immunity
incubated with IRDye anti-mouse or anti-rabbit IgG (1:15,000) (Li-Cor Biosciences). Imaging was done using
the Odyssey System.
Virus stimulation of pDC and infection of moDC
Echovirus 9 Hill (EV9) and Coxsackievirus B3 Nancy (CVB3) were propagated as described before18. pDCs,
isolated as described above, were stimulated with CVB3 at a multiplicity of infection (MOI) of 100 in the
presence or absence of 10% human serum. After 24h supernatants are harvested and used in a 1:10 dilution
to stimulate moDC cultures. Unstimulated and stimulated moDCs were harvested using cold PBS, washed and
infected with Echovirus 9 (Hill) at an MOI of 1 in serum free RPMI. After a 60 min incubation at 37oC, cells
were washed 3 times in an excess volume of PBS after which viral titers were determined at different time
points post infection (p.i.) as described before18. To exclude CVB3 interference during EV9 replication analysis
titrations were done in the presence of neutralizing anti-CVB3 antibodies.
Statistical analysis
Differential expression was assessed by means of one-factor ANOVA, and non-parametric pairwise comparison
of the DC subsets was done using the Tukey's post-hoc test in the R statistics package21. A P value of < 0.05 was
considered a significant difference.
Results
TLR and RLH profiles in human immature and mature monocyte-derived DCs
Messenger RNA (mRNA) levels of TLRs, RLHs and other PRRs in human moDCs from
three different donors were determined using custom-designed low density arrays based
on microfluidic card technology (see materials and methods) and qPCR. In line with
their function as 'sentinels' of the body, human immature DCs were found to express
a broad variety of PRRs. Regarding TLRs responding to RNA, i.e. TLR3, TLR7 and TLR8,
moderate steady-state levels were observed (Fig 1A). In contrast to their RNA-sensing
TLR-counterparts, significant transcript levels of the RLHs RIG-I, MDA5 and LGP2 were
detected in all donors, along with high levels of the dsRNA activated anti-viral effector
molecule PKR. The levels of RIG-I and MDA5 were as much as 25- to 100-fold higher
compared to expression of TLR3 or TLR7, implying an important role for RLHs in moDC
biology (Fig 1A). Furthermore, transcripts for essentially all TLRs were detected, as well
as a broad panel of C-type lectin receptors (CLRs) (Supplementary Figure 1) that can
bind many pathogens, among which different viruses, and potentially function as entry
receptors22,23.
To study potential changes in PRR mRNA levels under pro-inflammatory
conditions, we stimulated DCs with LPS (100 ng/ml) + IFNy (400 U/ml) for 24 h. Some
members of the TLR family showed a modest up- or downregulation following exposure
to LPS/IFNy, and significant donor differences were observed. Also the expression of
CLRs showed moderate changes (Supplementary Fig. 1). Among the TLRs, the largest
increases were found in the RNA-sensing TLRs (Fig 1A and Supplementary Fig. 1). TLRs
involved in the detection of bacteria, such as TLR1, 2 and 4, which expression levels
were already substantial, showed only a modest increase. Interestingly, differences
in expression levels were more apparent within the family of cytoplasmic viral RNA
sensors. Expression of RLHs RIG-I and MDA5 as well as effector molecules like PKR were
significantly upregulated following stimulation with LPS/IFNy, suggesting that exposure to
these pro-inflammatory stimuli can affect the responsiveness of DCs to viral pathogens.
33
Chapter 2
A
Gene
TLR3
TLR7
TLR8
RIG I
PKR
MDA-5
LGP-2
Donor 1
Medium
LPS/IFNy
Donor 2
Medium
LPS/IFNy
Donor 3
Medium
LPS/IFNy
B
7 to 5
5 to 3
3 to 1
1 to -1
-1 to -3
-3 to -5
-5 to -7
-7 to -9
-9 t o -11
C
»I
0
time (h)
Figure 1. Expression of RNA sensors in human moDCs in steady-state and under pro-inflammatory condi
tions.
(A) Human moDCs were obtained by culturing freshly isolated blood monocytes from three different donors
with IL-4 and GM-CSF. Unstimulated moDCs or DCs stimulated with LPS (100 ng/ml) + IFNy (400 U/ml) for
24h were used. Total RNA of unstimulated, or stimulated cells was isolated and quantitative mRNA expres
sion levels of the indicated genes were analyzed using low density arrays and conventional qPCR. DCt values
were calculated with the Ct value for PBGD as a reference. One gray scale color encompasses a 2 DCt range.
Black corresponds to undetectable mRNAs. (B) Immature moDCs of three different donors were stimulated as
described for figure 1 and total RNA was isolated 4, 8 or 24 h after stimulation. Quantitative mRNA expression
levels of the indicated genes were analyzed using conventional qPCR and is displayed relative to unstimulated
cells (put to 1). PBGD was used as reference gene. One representative example of three independent experi
ments using different donors is shown. (C) DCs were stimulated as described for (A) and protein levels of RIG
I, MDA5, PKR and actin were analyzed using western blot 24 h after stimulation. Shown is a representative
example from two independent experiment using different donors.
Dynamics of PRR expression upon DC stimulation
Next, we analyzed kinetics of PRR expression following stimulation of DCs, focusing on
PRRs involved in recognition of viral RNA, i.e. TLR3, TLR7, TLR8, and the cytoplasmic viral
RNA sensors. Upregulation of TLRs and RLHs peaked approximately 8 h after exposure
to pro-inflammatory stimuli, and expression of most genes had returned to baseline
levels after 24 h (Fig. 1B). TLR3 expression showed surprisingly little modulation in time
compared to the other TLRs and RLHs studied (Fig. 1B, right panel), whereas RIG-I and
MDA5 mRNA expression increased more than 50-fold (Fig. 1B, left panel). Western blot
analysis corroborated our PCR results on protein level by showing enhanced expression
of RIG-I, MDA5 and PKR following 24 h treatment with LPS/IFNy (Fig. 1C). Thus, upon
exposure to PAMPs and pro-inflammatory stimuli, moDCs rapidly upregulate expression
of PRRs responding to viral RNA at the mRNA and protein level, which might result in an
increased capacity to respond to microorganisms.
Expression of RNA sensors in blood myeloid DCs and plasmacytoid DCs, and moDCs
To further study the RLH-family of RNA sensors in human DC subsets, we determined
their expression profile in moDC, freshly isolated mDCs and plasmacytoid (p)DCs, which
play a crucial role in antiviral immunity. The expression of TLR3, TLR7 and TLR8 that
34
Human DC cross-talk influences antiviral immunity
are also involved in viral RNA recognition was analyzed in parallel. Quantitative analysis
showed that TLR8 levels were approximately 10-fold higher than levels of TLR3 or TLR7
in moDCs, while differences in expression of these TLRs in freshly isolated mDCs were
less pronounced (Fig. 2A). In contrast, pDCs were found to express approximately 100
fold higher levels of TLR7 as compared to TLR8 and as much as 500 times more TLR7
than TLR3. In addition, highly divergent TLR expression profiles were detected between
the different DC subsets analyzed. The most pronounced TLR3 expression was found in
mDCs that showed over 20-fold higher expression compared to moDCs or pDCs. The
observed differences in expression of TLR7 were even more dramatic: pDCs showed 40and over 200-fold higher TLR7 levels as compared to mDC and moDC (Fig. 2A). Thus far,
no data is available regarding the expression or function of cytoplasmic RNA sensors in
human mDCs or pDCs. We found that all DC subsets expressed mRNA of RIG-I, MDA5,
PKR and LGP2 (Fig. 2B). Of these genes, LGP2 expression was the lowest in all DC-types
analyzed, which might be related to its proposed function as negative regulator of MDA5
and RIG-I responses16. For both myeloid DC subsets only a relatively modest difference
was observed in expression levels of RIG-I and MDA5. In contrast, pDCs expressed
considerably higher levels of MDA5 compared to RIG-I (Fig. 2B). Furthermore, pDCs
expressed both RIG-I and PKR at higher levels than moDCs and/or mDCs. The most striking
difference was observed for expression of MDA5 mRNA, which was expressed in pDCs
at 10-fold and 20-fold higher levels than in moDCs or mDCs, respectively (Fig. 2B). The
abundance of MDA5 in pDCs was confirmed at the protein level by confocal microscopy
(Fig. 2C). The high expression of not only TLR7, but also cytoplasmic RNA sensors and
antiviral effector molecules in pDCs provides additional evidence for specialization of DC
subsets and the essential contribution of pDCs to antiviral immunity. This was further
substantiated by the high constitutive mRNA level of interferon regulatory factor 7 (IRF7), a key transcription factor in the innate immune response against viruses, which was
significantly higher than in moDCs or mDCs (Fig. 2D)24-26.
Plasmacytoid DC mediated anti-viral immunity in moDCs
Taking into account the crucial role of pDC in antiviral immunity, we next investigated
whether pDCs could influence antiviral responses in other DC subsets. Therefore, we
set out to determine whether activation of pDCs could influence RNA-sensor expression
in DCs of the myeloid lineage by analyzing RLH levels in moDCs that were exposed to
supernatant of pDCs activated with CpG DNA. No significant direct effect of CpG DNA
on moDC was observed (data not shown). Strikingly, pDC supernatant diluted as much
as 100 times triggered a 150- to 300-fold increase in RIG-I, MDA5 and PKR transcript
levels in moDC. Similar ISG induction in moDCs was found when using recombinant
human IFNa2 and supernatant from R848-stimulated pDC (Fig. 3A and data not shown),
suggesting an important role for type I IFNs in this process. Addition of CpG or R848 to
moDC did not induce ISG-expression (data not shown and Kramer et al.27), excluding
the possibility that the observed effects are due to direct PRR-stimulation of moDC. The
importance of type I IFNs was confirmed by the use of blocking anti-IFN-a/ß antibodies,
which completely prevented the induction of these RNA-sensors following stimulation
with either pDC supernatant or rIFNa2 (Fig. 3A). The increased mRNA levels of MDA5 in
moDCs were confirmed at the protein level by confocal analysis (Fig. 3B). Furthermore,
western blot analysis confirmed increased protein levels of not only MDA5, but also
RIG-I and PKR upon IFN-stimulation (Fig 3C). Interestingly, MDA5 has been reported
35
Chapter 2
A
^^m oD C
I lm DC
■
B
■2m
§
t0oû-
55000
**
44000
<
z rc
o
0
□
**
n.s.
__ __
ñ
*
,— ,
la
■
moDC
mDC
**
■
*
22000
11000
T
■
*
33000
cu cu
**
pDC
pDC
n.s.
r=, r=l ■
RIG-I
C
IRF7
D 0Q
to CÛ
<
VQ.
sí o
50000
10000
«¡Ü cu
1*
H
*
0
¿ L
mDC
pDC
Figure 2. Human DC subsets express different profiles of viral nucleic acid receptors.
(A) Mean expression (+SD) of TLR3, TLR7 and TLR8 in human moDCs, freshly isolated mDCs and freshly iso
lated pDCs. RNA was isolated from unstimulated cells and TLR mRNA transcript levels determined using con
ventional qPCR. Expression levels relative to PBGD. * P<0.05; ** P<0.01. (B) Expression levels of RIG-I, MDA5,
PKR and LGP2 in resting human DC subsets were determined as described for (A). Shown is mean expression
+ SD. * P<0.05; ** P<0.01. (C) Confocal laser scanning microscopy analysis of MDA5 expression in human
moDCs and pDCs. Unstimulated cells were stained using antibodies against DC-SIGN and MDA5 (for moDCs)
or BDCA2 and MDA5 (for pDCs) followed by incubation with Alexa labeled secondary antibodies. Green indi
cates MDA5 expression, red indicates DC-SIGN or BDCA2 in moDCs and pDCs, respectively. A representative
example of three independent experiments using different donors is shown. (D) IRF-7 expression in human
DC subsets was determined using qPCR as described for (A). Shown is mean expression + SD. * p <0.05; ** p
<0.01. Mean quantitative gene expression + SD from 6 moDCs, 3 pDCs and 3 mDCs is displayed (for figures
A, B and D).
to play a crucial role in the responses to the picornavirus encephalomyocarditisvirus
(EMCV) in mouse DCs12 and we recently showed that echoviruses, single-stranded RNA
viruses also belonging to the picornavirus family, can efficiently infect human moDCs18.
To study whether upregulation of viral sensors, including MDA5, was associated with
decreased susceptibility for infection, moDCs were exposed to pDC supernatant and
subsequently infected with the echovirus EV9. EV9 titers rapidly increased in untreated
moDCs or moDCs exposed to supernatant of unstimulated pDCs, indicating efficient virus
replication. In contrast, treatment with supernatant of CpG-stimulated pDCs completely
blocked EV9 replication in human moDCs (Fig. 3D).
To study DC cross-talk under more physiological conditions, pDC were stimulated
with coxsackievirus B3 (CVB3) in the presence or absence of 10% human serum (HS). As
we have shown before, CVB3 is not capable of infecting moDC, and has no effect on
moDC function18. However, pDC activation by CVB3 has been reported in the presence
of specific antiviral antibodies found in HS28. Stimulation of moDC with supernatant
36
Human DC cross-talk influences antiviral immunity
of unstimulated pDCs, or CVB3-stimulated pDC without HS had little or no effect on
expression of RIG-I, MDA5 and PKR mRNA. However, supernatant of pDC exposed to
CVB3 in the presence of 10% HS caused a profound increase in RNA-sensors in moDC
(Fig. 4A). The observed effects were highly IFN-a/ß dependent, since mRNA induction in
the presence of blocking anti-IFN-a/ß antibodies was completely absent (Fig. 4A). pDCs
produced up to 40 ng/ml IFN-a upon stimulation with CVB3 and human serum (data not
shown). This is a substantial increase that even exceeds the induction of IFN-a by CpG
(approx 17 ng/ml, data not shown). To determine if stimulation with virus-activated pDC
supernatant provided functional protection from infection, moDCs were subsequently
exposed to EV9. Efficient EV9 replication was observed in moDC that had been treated
with pDC supernatant from mock-stimulated pDC, as indicated by the increase in virus
titer. In contrast, moDCs stimulated with supernatant from pDC that were exposed to
CVB3 in the presence of HS were completely protected from EV9 infection, as shown by
the dramatic effect on EV9 replication (Fig. 4B). Thus, pDC activation can increase the
resistance against viral infection in DCs from the myeloid lineage.
Figure 3 TLR-stimulated human pDC induce a state of antiviral resistance in moDCs that inhibits infection
with EV9.
(A) Human moDCs were exposed to cell free supernatants of pDCs (in a 1:100 dilution in RPMI 1640) that
had been stimulated with CpG DNA (5^g/ml) for a period of 24 h. Alternatively, moDCs were stimulated using
100 U/ml IFNa2 (Roferon- A®, Roche). Total RNA was isolated at the indicated time points following stimula
tion and mRNA transcript levels determined using qPCR with expression of PBGD as a reference. Expression
is given relative to unstimulated cells (medium). (B) Confocal laser scanning microscopy analysis of MDA5
expression in human moDCs that were left untreated or exposed to supernatant of pDC activated with CpG
DNA as described for (A). Cells were stained using antibodies against DC-SIGN and MDA5 followed by incuba
tion with Alexa labeled secondary antibodies. Green indicates MDA5 expression; red indicates expression of
DC-SIGN. (C) Human moDCs were stimulated with 200 U/ml IFNa2, or were left untreated. After 24h cells
were harvested and protein levels of RIG-I, MDA5, PKR and actin were analyzed using western blot. Shown
is a representative example from two independent experiments using different donors. (D) Human moDCs
were exposed to cell free supernatants of differently stimulated pDCs for a period of 24 h and subsequently
harvested, washed and exposed to EV9 at an MOI of 1 in serum free medium for 1 h at 37°C. After washes
to remove unbound virus, cells were plated out and viral titers were determined at several time points after
infection. Shown is a representative example of two independent experiments using different donors.
37
Chapter 2
A
MDA5
RIG-I
6lh
OO
»8
tUoQ.D
Û
36
ÌL
O
x
+
o o* 24'
z I 12'
U
„
1__ 1medium
48- H a n ti- IFN
B
n
60'
24-
40'
20'
|“ |
■
0-
i/ O0^ x'*5’
aj
' /
<?
1__ 1medium
80' H a n ti- IFN
36-
12-
n
<P°
PKR
100-
61h
1__ 1medium
48 ■ anti-IFN
/
„O
v<?
0' f t a
n™
jd ^ O .
J “
/ / '
/
- ^ s u p pDC MOCK
-▼- sup pDC MOCK + HS
- ^ s u p pDC C V B
-©- sup pDC C V B + HS
« I
E a
>9
.£ O
Sì m
r«e o
12
24
36
hours p.i.
Figure 4. CVB-stimulated pDC induce a type I IFN-dependent induction of viral RNA sensors in moDC and
protection from subsequent EV9 infection.
(A) Human moDCs were exposed to cell free supernatants of pDCs (1:10 dilution in RPMI 1640) that were
either mock or CVB-stimulated in the presence of absence of 10% human serum as indicated. Total RNA was
isolated following stimulation and mRNA transcript levels were determined using qPCR with expression of
PBGD as a reference. Expression is given relative to unstimulated cells (medium). (B) moDC were stimulated
with pDC supernatant as described in (A) for 24h and subsequently harvested, infected with EV9 at an MOI of
1. EV9 replication was analysed as for Fig 3D. Shown is a representative example of two independent experi
ments using different donors.
In conclusion, we show that endosomal and cytoplasmic viral RNA sensors
are widely expressed in moDCs, and this expression is increased upon inflammation.
Furthermore, under steady-state conditions, these RNA sensors display a differential
expression pattern in various human DC subsets, with the most substantial expression
found in pDCs. Finally, cross-talk between virus-activated pDCs and moDCs offers
protection against viral infection, which underscores the importance of cross-talk between
DC subsets in optimal induction of immune responses against invading pathogens.
Discussion
DCs act as sentinels of the body and are present in virtually all tissues, where they
constantly monitor their surroundings for signs of infection. To recognize microorganisms,
DCs express a vast array of PRRs. Although a large body of information is available
regarding the expression and function of TLRs in DCs, data on expression and function
of the different RLH family members in human DCs is virtually absent. We set out
to determine the quantitative expression levels of TLRs and RLHs in human DCs at
different experimental conditions, focusing on PRRs involved in recognition of viral RNA.
Furthermore we compared steady-state expression levels of these sensors in different
DC subsets, and investigated cross-talk between virus-stimulated pDCs and moDCs.
38
Human DC cross-talk influences antiviral immunity
Human moDCs were found to express transcripts for all TLR family members,
and most of the C-type lectins analyzed. The mean expression levels of TLRs responding
to nucleic acids were considerably lower than those responding to bacterial or fungal
pathogens. This could represent a mechanism to prevent unwanted responses to host
nucleic acids that have been associated with autoimmune diseases like systemic lupus
erythematosus29, 30. On the other hand, expression of PRRs in different cell types can
be altered under pro- or anti-inflammatory conditions (this study and Homma et al.,
Rosenstiel et al., and Fitzner et al 31-33). Under pro-inflammatory conditions (i.e. LPS/IFNy)
the expression of TLRs -especially TLR7 and TLR8 -was increased, providing a mechanism
to efficiently fight infection upon encounter with pathogens. The upregulation of these
molecules was most pronounced at early time points following stimulation, and had
declined again after 24h. The rather swift PRR downregulation most likely functions to
prevent unnecessary high PRR expression levels once infection has been cleared, thereby
avoiding uncontrolled inflammatory responses.
Myeloid DCs and pDCs have been shown to display distinct TLR profiles that
enable them to respond to different microbial structures4, 34. We here confirmed these
data on a quantitative level and showed that expression of TLR7 in pDCs vastly exceeded
that of TLR3 and TLR8. This is in accordance with the findings that pDCs respond
strongly to synthetic TLR7, but not TLR8-specific ligands35 and are unresponsive to the
synthetic dsRNA mimic poly(I:C)4. In contrast, moDCs expressed much higher levels of
TLR8 compared to TLR3 and TLR7. The highly divergent expression profile of TLR7 and
TLR8 in human pDCs and myeloid DC subsets likely reflects their ability to induce specific
responses following recognition of different virus structures.
Virtually no data is currently available regarding RIG-I and MDA5 in human
DC subsets. A recent mouse study has suggested that RIG-I is crucial for the antiviral
response of myeloid DCs following exposure to the RNA virus Newcastle disease virus
(NDV). In contrast, in pDCs RIG-I was shown to be dispensable and the antiviral responses
against NDV in mice were dependent on the TLR signaling pathway16. Interestingly, our
finding that RIG-I mRNA levels in human pDCs were significantly higher than the levels
found in moDCs suggests that in the human setting RIG-I could play a pivotal role in the
response of pDCs to RNA viruses. Even more pronounced were the expression levels
of MDA5 in human pDCs that were remarkably higher than those found in moDCs
or mDCs. MDA5 has recently been shown to mediate type I IFN responses following
exposure of mouse myeloid DCs to poly(I:C) and the picornavirus EMCV12. Whether the
prominent expression of MDA5 signifies involvement of this molecule in the response of
pDCs to picornaviruses remains to be determined. It could be envisioned that the high
constitutive levels of TLR7, RLHs and PKR in pDCs might not only mediate the robust type
I IFN production of pDCs in response to viral pathogens but could also protect these cells
from becoming infected themselves.
The cytoplasmic localization of RIG-I and MDA5 suggests that they play a
dominant role in case of infection of DCs themselves. However, it could be envisioned
that viral replication intermediates can come into contact with these molecules upon
phagocytosis of infected cells, as it has been shown that antigen delivery from the
endosomal compartment to the cytosol takes places in DCs, for instance to facilitate
cross-presentation 36-38. However, whether these pathways can efficiently contribute to
the RIG-I or MDA5 mediated antiviral responses remains to be determined.
39
Chapter 2
Finally, we revealed a novel effect of cross-talk between pDCs and DCs of
myeloid origin. It has been described that cross-talk between pDCs and mDCs can
influence cytokine production, DC maturation and antigen presentation3, 39-41. In this
study we showed that cross-talk can induce rapid upregulation of RNA sensors in moDCs
and protection against infection with picornaviruses. This protection depended on type
I IFNs, cytokines with well-known anti-viral activity that signal through the ubiquitously
expressed type I IFN receptor. Myeloid DCs are known to respond to IFNa40, 42, 43, but
pDC derived type I IFNs are known to affect many other cell types when present in their
vicinity. For example, it has been shown that type I IFNs can influence expression of RLHs
in keratinocytes and macrophages44-46. Importantly, our study revealed that protection of
mDC by pDC-derived type I IFNs not only occured upon pDC stimulation using synthetic
TLR ligands, but also following a more physiological exposure to CVB. The finding that
pDC mediated protection largely depended on the presence of human serum during virus
exposure is in line with earlier result by Wang et al. Most likely, virus particles coated with
anti-viral antibodies are being taken up via an FcR-mediated process, which ultimately
leads to activation of the pDC through TLRs and possibly other PRRs28. This antibodymediated process depends on the presence of specific anti-viral antibodies induced
following activation of B-cells. Hence, it is likely to be more efficient upon secondary
encounter with the same virus, when antibodies are already present and production is
enhanced. Thus, pDCs could preserve the function and viability of myeloid DCs in case of
infection with DC-tropic viruses. This will ensure antigen-presentation to both CTL and
Th-cells, thereby enhancing the antiviral immune response. On the other hand, pDCs
might mediate unbalanced responses by myeloid DCs or T-cells47, possibly contributing
to immune-mediated diseases associated with CVB infections, such as cardiomyopathy
and type 1 diabetes48,49.
In conclusion, we demonstrate for the first time that human moDCs express
high mRNA and protein levels of RLHs and PKR, which show a transient increase
following exposure to pro-inflammatory stimuli. Expression profiling of PRRs involved in
the antiviral response in different human DC subsets demonstrated that pDCs express
significantly higher levels of RLHs, PKR and IRF-7 compared to myeloid DCs. The profound
expression of these antiviral genes in human pDCs is in line with their important function
in antiviral immunity, and might also explain how these cells survive and function in an
environment with high virus burden. Finally, cross-talk between virus-stimulated pDCs
and moDCs enhanced the expression of RIG-I, MDA5 and PKR in moDCs and created
a state of antiviral resistance that protected these cells against viral infection. Further
investigation into the novel findings presented here regarding the effect of human DC
cross-talk on RLH expression and antiviral resistance will contribute significantly to our
understanding of DC-pathogen interaction.
Acknowledgments
The authors would like to thank Daniel Benitez-Ribas (department of Tumor Immunology,
Nijmegen Centre for Molecular Life Sciences, Radboud University Medical Centre,
Nijmegen, The Netherlands) for help with pDC experiments, Paul Fisher (Departments
of Pathology, Neurosurgery and Urology, Columbia University, College of Physicians and
Surgeons, New York, USA) for providing us with anti-MDA5 antibody, and Harrie van der
Avoort (National Institute for Public Health and the Environment, RIVM, Bilthoven, The
40
Human DC cross-talk influences antiviral immunity
Netherlands) for providing neutralizing anti-CVB3 antibody. This work was supported
by grants from the Netherlands Diabetes Foundation (DFN 2001.00.047) to G.J.A., the
Netherlands Organization for Scientific Research (NW0-VIDI-917.46.305) to F.J.M.v.K.
and (NWO-912-02-034) to G.J.A. and the Juvenile Diabetes Research Foundation (Grant
Number: 24-2008-949) to G.J.A. and F.J.M.v.K.
Authorship contributions
M.K., B.M.S., F.J.M.v.K and G.J.A. designed the research, analyzed data and wrote the
paper. M.K., B.M.S., M.v.H.K., L.W.J.T., J.T., B.J.H.J. and D.E.T. performed research. B.J.H.J.
analyzed data. F.J.M.K. and G.J.A. supervised the study.
The authors declare there is no conflict of interest.
41
Chapter 2
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
42
J. Banchereau, R. M. Steinman (1998). Dendritic cells and the control of immunity. Nature, 392, 245-252.
S. Agrawal, A. Agrawal, B. Doughty, A. Gerwitz, J. Blenis, T. Van Dyke, B. Pulendran (2003). Cutting edge: different Toll-like receptor
agonists instruct dendritic cells to induce distinct Th responses via differential modulation of extracellular signal-regulated kinasemitogen-activated protein kinase and c-Fos. J Immunol, 171, 4984-4989.
T. Ito, H. Kanzler, O. Duramad, W. Cao, Y. J. Liu (2006). Specialization, kinetics, and repertoire of type 1 interferon responses by
human plasmacytoid predendritic cells. Blood, 107, 2423-2431.
N. Kadowaki, S. Ho, S. Antonenko, R. W. Malefyt, R. A. Kastelein, F. Bazan, Y. J. Liu (2001). Subsets of human dendritic cell precursors
express different toll-like receptors and respond to different microbial antigens. J Exp Med, 194, 863-869.
T. Ito, R. Amakawa, T. Kaisho, H. Hemmi, K. Tajima, K. Uehira, Y. Ozaki, H. Tomizawa, S. Akira, S. Fukuhara (2002). Interferon-alpha
and interleukin-12 are induced differentially by Toll-like receptor 7 ligands in human blood dendritic cell subsets. J Exp Med, 195,
1507-1512.
F. Sallusto, A. Lanzavecchia (1994). Efficient presentation of soluble antigen by cultured human dendritic cells is maintained by
granulocyte/macrophage colony-stimulating factor plus interleukin 4 and downregulated by tumor necrosis factor alpha. J Exp Med,
179, 1109-1118.
Y. Osugi, S. Vuckovic, D. N. Hart (2002). Myeloid blood CD11c(+) dendritic cells and monocyte-derived dendritic cells differ in their
ability to stimulate T lymphocytes. Blood, 100, 2858-2866.
A. Karlsson, E. Nygren, J. Karlsson, I. Nordstrom, C. Dahlgren, K. Eriksson (2007). Ability of monocyte-derived dendritic cells to
secrete oxygen radicals in response to formyl peptide receptor family agonists compared to that of myeloid and plasmacytoid
dendritic cells. Clin Vaccine Immunol, 14, 328-330.
R. Medzhitov (2007). Recognition of microorganisms and activation of the immune response. Nature, 449, 819-826.
A. Macagno, G. Napolitani, A. Lanzavecchia, F. Sallusto (2007). Duration, combination and timing: the signal integration model of
dendritic cell activation. Trends Immunol, 28, 227-233.
H. Kato, O. Takeuchi, S. Sato, M. Yoneyama, M. Yamamoto, K. Matsui, S. Uematsu, A. Jung, T. Kawai, K. J. Ishii, O. Yamaguchi, K.
Otsu, T. Tsujimura, C. S. Koh, C. Reis e Sousa, Y. Matsuura, T. Fujita, S. Akira (2006). Differential roles of MDA5 and RIG-I helicases in
the recognition of RNA viruses. Nature, 441, 101-105.
L. Gitlin, W. Barchet, S. Gilfillan, M. Cella, B. Beutler, R. A. Flavell, M. S. Diamond, M. Colonna (2006). Essential role of mda-5 in
type I IFN responses to polyriboinosinic:polyribocytidylic acid and encephalomyocarditis picornavirus. Proc Natl Acad Sci U S A, 103,
8459-8464.
K. Takahasi, M. Yoneyama, T. Nishihori, R. Hirai, H. Kumeta, R. Narita, M. Gale, Jr., F. Inagaki, T. Fujita (2008). Nonself RNA-sensing
mechanism of RIG-I helicase and activation of antiviral immune responses. M ol Cell, 29, 428-440.
M. Schlee, A. Roth, V. Hornung, C. A. Hagmann, V. Wimmenauer, W. Barchet, C. Coch, M. Janke, A. Mihailovic, G. Wardle, S.
Juranek, H. Kato, T. Kawai, H. Poeck, K. A. Fitzgerald, O. Takeuchi, S. Akira, T. Tuschl, E. Latz, J. Ludwig, G. Hartmann (2009).
Recognition of 5' Triphosphate by RIG-I Helicase Requires Short Blunt Double-Stranded RNA as Contained in Panhandle of Negative
Strand Virus. Immunity.
O. Takeuchi, S. Akira (2008). MDA5/RIG-I and virus recognition. Curr Opin Immunol, 20, 17-22.
M. Yoneyama, M. Kikuchi, K. Matsumoto, T. Imaizumi, M. Miyagishi, K. Taira, E. Foy, Y. M. Loo, M. Gale, Jr., S. Akira, S. Yonehara, A.
Kato, T. Fujita (2005). Shared and unique functions of the DExD/H-box helicases RIG-I, MDA5, and LGP2 in antiviral innate immunity.
J Immunol, 175, 2851-2858.
M. J. Clemens, A. Elia (1997). The double-stranded RNA-dependent protein kinase PKR: structure and function. J Interferon Cytokine
Res , 17, 503-524.
M. Kramer, B. M. Schulte, L. W. Toonen, M. A. de Bruijni, J. M. Galama, G. J. Adema, F. J. van Kuppeveld (2007). Echovirus infection
causes rapid loss-of-function and cell death in human dendritic cells. Cell Microbiol, 9, 1507-1518.
X. Wang, B. Seed (2003). A PCR primer bank for quantitative gene expression analysis. Nucleic Acids Res, 31, e154.
L. Lin, Z. Su, I. V. Lebedeva, P. Gupta, H. Boukerche, T. Rai, G. N. Barber, P. Dent, D. Sarkar, P. B. Fisher (2006). Activation of Ras/Raf
protects cells from melanoma differentiation-associated gene-5-induced apoptosis. Cell Death Differ, 13, 1982-1993.
R Development Core Team (2005). R: A language and environment for statistical computing.
T. B. Geijtenbeek, D. S. Kwon, R. Torensma, S. J. van Vliet, G. C. van Duijnhoven, J. Middel, I. L. Cornelissen, H. S. Nottet, V. N.
KewalRamani, D. R. Littman, C. G. Figdor, Y. van Kooyk (2000). DC-SIGN, a dendritic cell-specific HIV-1-binding protein that enhances
trans-infection of T cells. Cell, 100, 587-597.
A. Cambi, F. de Lange, N. M. van Maarseveen, M. Nijhuis, B. Joosten, E. M. van Dijk, B. I. de Bakker, J. A. Fransen, P. H. BoveeGeurts, F. N. van Leeuwen, N. F. Van Hulst, C. G. Figdor (2004). Microdomains of the C-type lectin DC-SIGN are portals for virus entry
into dendritic cells. J Cell Biol, 164, 145-155.
E. M. Coccia, M. Severa, E. Giacomini, D. Monneron, M. E. Remoli, I. Julkunen, M. Cella, R. Lande, G. Uze (2004). Viral infection and
Toll-like receptor agonists induce a differential expression of type I and lambda interferons in human plasmacytoid and monocytederived dendritic cells. Eur J Immunol, 34, 796-805.
A. Izaguirre, B. J. Barnes, S. Amrute, W. S. Yeow, N. Megjugorac, J. Dai, D. Feng, E. Chung, P. M. Pitha, P. Fitzgerald-Bocarsly (2003).
Comparative analysis of IRF and IFN-alpha expression in human plasmacytoid and monocyte-derived dendritic cells. J Leukoc Biol,
74, 1125-1138.
M. Kerkmann, S. Rothenfusser, V. Hornung, A. Towarowski, M. Wagner, A. Sarris, T. Giese, S. Endres, G. Hartmann (2003). Activation
with CpG-A and CpG-B oligonucleotides reveals two distinct regulatory pathways of type I IFN synthesis in human plasmacytoid
dendritic cells. J Immunol, 170, 4465-4474.
M. Kramer, B. M. Schulte, L. W. Toonen, P. M. Barral, P. B. Fisher, K. H. Lanke, J. M. Galama, F. J. van Kuppeveld, G. J. Adema (2008).
Phagocytosis of picornavirus-infected cells induces an RNA-dependent antiviral state in human dendritic cells. J Virol, 82, 2930
2937.
J. P. Wang, D. R. Asher, M. Chan, E. A. Kurt-Jones, R. W. Finberg (2007). Cutting Edge: Antibody-mediated TLR7-dependent
recognition of viral RNA. J Immunol, 178, 3363-3367.
T. K. Means, A. D. Luster (2005). Toll-like receptor activation in the pathogenesis of systemic lupus erythematosus. Ann N Y Acad Sci,
1062, 242-251.
J. A. Deane, P. Pisitkun, R. S. Barrett, L. Feigenbaum, T. Town, J. M. Ward, R. A. Flavell, S. Bolland (2007). Control of toll-like receptor
7 expression is essential to restrict autoimmunity and dendritic cell proliferation. Immunity, 27, 801-810.
T. Homma, A. Kato, N. Hashimoto, J. Batchelor, M. Yoshikawa, S. Imai, H. Wakiguchi, H. Saito, K. Matsumoto (2004). Corticosteroid
and cytokines synergistically enhance toll-like receptor 2 expression in respiratory epithelial cells. Am J Respir Cell Mol Biol, 31, 463
469.
P. Rosenstiel, M. Fantini, K. Brautigam, T. Kuhbacher, G. H. Waetzig, D. Seegert, S. Schreiber (2003). TNF-alpha and IFN-gamma
regulate the expression of the NOD2 (CARD15) gene in human intestinal epithelial cells. Gastroenterology, 124, 1001-1009.
N. Fitzner, S. Clauberg, F. Essmann, J. Liebmann, V. Kolb-Bachofen (2008). Human skin endothelial cells can express all 10 TLR genes
Human DC cross-talk influences antiviral immunity
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
and respond to respective ligands. Clin Vaccine Immunol, 15, 138-146.
D. Jarrossay, G. Napolitani, M. Colonna, F. Sallusto, A. Lanzavecchia (2001). Specialization and complementarity in microbial
molecule recognition by human myeloid and plasmacytoid dendritic cells. Eur J Immunol, 31, 3388-3393.
K. B. Gorden, K. S. Gorski, S. J. Gibson, R. M. Kedl, W. C. Kieper, X. Qiu, M. A. Tomai, S. S. Alkan, J. P. Vasilakos (2005). Synthetic TLR
agonists reveal functional differences between human TLR7 and TLR8. J Immunol, 174, 1259-1268.
A. Rodriguez, A. Regnault, M. Kleijmeer, P. Ricciardi-Castagnoli, S. Amigorena (1999). Selective transport of internalized antigens to
the cytosol for MHC class I presentation in dendritic cells. Nat Cell Biol, 1, 362-368.
C. Hotta, H. Fujimaki, M. Yoshinari, M. Nakazawa, M. Minami (2006). The delivery of an antigen from the endocytic compartment
into the cytosol for cross-presentation is restricted to early immature dendritic cells. Immunology, 117, 97-107.
M. C. Ramirez, L. J. Sigal (2002). Macrophages and dendritic cells use the cytosolic pathway to rapidly cross-present antigen from
live, vaccinia-infected cells. J Immunol, 169, 6733-6742.
S. Kuwajima, T. Sato, K. Ishida, H. Tada, H. Tezuka, T. Ohteki (2006). Interleukin 15-dependent crosstalk between conventional and
plasmacytoid dendritic cells is essential for CpG-induced immune activation. Nat Immunol, 7, 740-746.
D. Piccioli, C. Sammicheli, S. Tavarini, S. Nuti, E. Frigimelica, A. G. Manetti, A. Nuccitelli, S. Aprea, S. Valentini, E. Borgogni, A. Wack,
N. M. Valiante (2009). Human plasmacytoid dendritic cells are unresponsive to bacterial stimulation and require a novel type of
cooperation with myeloid dendritic cells for maturation. Blood.
Y. Lou, C. Liu, G. J. Kim, Y. J. Liu, P. Hwu, G. W ang (2007). Plasmacytoid dendritic cells synergize with myeloid dendritic cells in the
induction of antigen-specific antitumor immune responses. J Immunol, 178, 1534-1541.
T. Kanto, N. Hayashi (2007). Innate immunity in hepatitis C virus infection: Interplay among dendritic cells, natural killer cells and
natural killer T cells. Hepatol Res, 37 Suppl 3, S319-326.
T. Kanto (2008). Virus associated innate immunity in liver. Front Biosci, 13, 6183-6192.
D. C. Kang, R. V. Gopalkrishnan, Q. Wu, E. Jankowsky, A. M. Pyle, P. B. Fisher (2002). mda-5: An interferon-inducible putative RNA
helicase with double-stranded RNA-dependent ATPase activity and melanoma growth-suppressive properties. Proc Natl Acad Sci U
S A , 99, 637-642.
E. P. Prens, M. Kant, G. van Dijk, L. I. van der Wel, S. Mourits, L. van der Fits (2008). IFN-alpha enhances poly-IC responses in human
keratinocytes by inducing expression of cytosolic innate RNA receptors: relevance for psoriasis. J Invest Dermatol, 128, 932-938.
J. Siren, J. Pirhonen, I. Julkunen, S. Matikainen (2005). IFN-alpha regulates TLR-dependent gene expression of IFN-alpha, IFN-beta,
IL-28, and IL-29. J Immunol, 174, 1932-1937.
D. Benitez-Ribas, G. J. Adema, G. Winkels, I. S. Klasen, C. J. Punt, C. G. Figdor, I. J. de Vries (2006). Plasmacytoid dendritic cells of
melanoma patients present exogenous proteins to CD4+ T cells after Fc gamma RII-mediated uptake. J Exp Med, 203, 1629-1635.
H. Hyoty, K. W. Taylor (2002). The role of viruses in human diabetes. Diabetologia, 45, 1353-1361.
P. L. Schwimmbeck, B. Bigalke, K. Schulze, M. Pauschinger, U. Kuhl, H. P. Schultheiss (2004). The humoral immune response in viral
heart disease: characterization and pathophysiological significance of antibodies. Med Microbiol Immunol, 193, 115-119.
43
Chapter 2
TLRs
Donor 1
M edium
LPS/IFNy
Donor 2
Medium
LPS/IFNy
Donor 3
M edium
LPS/IFNy
9 to 7
7 to 5
5 to 3
TLR1
TLR2
3 to 1
TLR3
1 t o -1
TLR4
-1 t o -3
TLR5
-3 t o -5
TLR6
-5 t o -7
TLR7
-7 t o -9
TLR8
-9 t o -11
TLR9
-1 1 t o -12
> -1 2
TLR10
CLRs
M edium
LPS/IFNy
Medium
LPS/IFNy
M edium
LPS/IFNy
M edium
LPS/IFNy
Medium
LPS/IFNV
M edium
LPS/IFNV
DC-SIGN
DCIR
DEC205
M RC1
DECTIN1
CLEC10A
CLEC1
M D L1
DCAL1
LANGERIN
CLEC2
BDCA2
RNA sensors
RIG I
PKR
M D A -5
LGP-2
S upplem entary Figure 1.
Expression o f PRRs in hum an moDCs in steady-state o r under p ro -in fla m m a to ry conditions.
Human moDCs w ere obtained by c ultu ring freshly isolated blood monocytes fro m three diffe ren t donors w ith
IL-4 and GM-CSF. Unstim ulated moDCs or DCs stim ulated w ith LPS (100 ng/m l) + IFNy (400 U /m l) fo r 24h
w ere used. Total RNA o f unstim ulated, or stim ulated cells was isolated and quantitative mRNA expression
levels o f the indicated genes were analyzed using low density arrays and conventional qPCR. DCt values were
calculated w ith the Ct value fo r PBGD as a reference. One gray scale color encompasses a 2 DCt range. Black
corresponds to undetectable mRNAs.
44
Chapter 3
Echovirus infection causes rapid
loss-of-function and cell death in
human dendritic cells
Matthijs Kramer, Barbara M. Schulte, Liza W.J. Toonen,
Mike A.M. de Bruijni, Jochem M.D. Galama,
Gosse J. Adema, Frank J.M. van Kuppeveld
Cellular M icrob io lo g y 2007 9(6):1507-18.
Chapter 3
Abstract
oxsackie B viruses (CVB) and Echoviruses (EV) form a single species; Human
enterovirus B (HeV-B), within the genus Enterovirus. Although HeV-B infections
are usually mild or asymptomatic, they can cause serious acute illnesses. In
addition, HeV-B infections have been associated with chronic immune disorders, such
as type 1 diabetes mellitus and chronic myocarditis/dilated cardiomyopathy. It has
therefore been suggested that these viruses may trigger an autoimmune process.
Here, we demonstrate that human dendritic cells (DCs), which play an essential role
in orchestration of the immune response, are productively infected by EV, but not CVB
strains, in vitro. Infection does not result in DC activation or the induction of anti-viral
immune responses. Instead, EV infection rapidly impedes Toll-like receptor mediated
production of cytokines and upregulation of maturation markers, and ultimately causes
loss of DC viability. These results describe for the first time the effect of EV on the
function and viability of human DCs and suggest that infection of DCs in vivo can impede
regulation of immune responses.
C
46
EV9 causes loss-of-function and cell death in human DCs
Introduction
Dendritic cells (DCs) are the most efficient antigen-presenting cells. They are present in
virtually all organs and tissues throughout the body and are potent initiators of immunity
via activation of (naïve) T- and B-cells, but also regulate tolerance to self-antigens in
order to prevent auto-immunity1. Via expression of a broad array of pattern recognition
receptors, for instance Toll-like Receptors (TLRs) and C-type lectins, DCs can sense the
presence of a large variety of pathogens, such as bacteria and fungi2, 3. Triggering of
TLRs results in DC maturation and cytokine production, enabling them to regulate T cell
activation and differentiation4.
Also in the event of viral infection, DCs play a crucial role in the induction of
anti-viral immune responses. Besides responding to virus-associated structures, such as
ssRNA and dsRNA5, 6, DCs can take up virus particles or (apoptotic) virus-infected cells.
This enables presentation of viral peptides in the context of MHC-II or MHC-I7, 8 and
the induction of potent anti-viral T cell responses. However, viruses have co-evolved
with their host to evade the immune system by several mechanisms. Considering the
central role of DCs in the immune system, it is not surprising that these cells are often
targeted by viruses. For instance, infection of DCs with cytomegalovirus results in
defective maturation, hampering the activation of naïve T cells9, 10. In addition, measles
virus impedes DC derived IL-12 production, while increasing the production of the anti
inflammatory cytokine IL-1011. This mechanism could possibly explain the observed
immune suppression as a result of measles virus infection. Thus, although DCs are
important contributors to anti-viral immunity, virus infection can impair DC function and
immune responses, potentially leading to persistent infections.
Coxsackie B viruses (CVB) and Echoviruses (EV) are small (20-30 nm), non
enveloped enteroviruses that are closely related and classified as a single species,
Human enterovirus B (HeV-B), within the Enterovirus genus of the Picornaviridae family.
They mainly differ in their capsid-coding region and thus in receptor usage. They are
acid stable and primarily cause infection of the gastrointestinal tract. Infection usually
remains limited to the intestine and causes mild disease or remains asymptomatic.
Incidentally, however, infection spreads via the blood stream to affect specific target
organs as the brains, pancreas and heart where it can give rise to severe and potentially
fatal illnesses such as (meningo)encephalitis, pancreatitis and myocarditis12. In addition,
it has been suggested that CVB and EV play a role in the pathogenesis of chronic immune
disorders like type 1 diabetes mellitus (T1D)13-15, primary Sjögren's syndrome16 and
chronic myocarditis/dilated cardiomyopathy17-19. Hence, it has been proposed that HeVB infections may trigger autoimmunity20-22.
To date, no information is available concerning the direct effect of HeV-B
infections on DCs. We investigated the capacity of several CVB and EV strains to infect
human DCs and analyzed the potential effects on DC function. We show here that
the ability of these viruses to infect and replicate in human monocyte-derived DCs is
restricted to EV strains only. EV infection does not lead to DC activation, but instead
results in a rapid loss of responsiveness to TLR ligands and induction of cell death.
47
Chapter 3
Materials & Methods
Virus stocks and purification
Reference strains Echovirus 1 Farouk (EV1 Farouk), EV7 Wallace, EV8 Bryson, EV9 Hill and Coxsackievirus B4
strain Tilo (CVB4 Tilo) were obtained from th e National Institute fo r Public Health and th e Environment (RIVM,
Bilthoven, The Netherlands). CVB3 Nancy and CVB4 Edwards2 were kindly provided by R. Kandolf (University o f
Tübingen, Germany) and J.W. Yoon (University o f Calgary, Canada), respectively. Production o f virus stocks and
virus titra tions were perform ed on buffalo green monkey cells. Cells were grown in m inim al essential medium
(M EM ) (Gibco) supplem ented w ith 10% fetal bovine serum, 100 U /m l penicillin, and 100 m g /m l streptom ycin
at 37°C in a 5% CO2-incubator. A fter infection, cells were incubated until com plete cytopathic effect was
observed. Virus was released by 3 successive cycles o f freezing and thaw ing and cell debris was removed by
centrifugation fo r 5 min at 3000 rpm. For purification, viral particles w ere pelleted by centrifugation through a
30% sucrose cushion in a Beckman SW28 ro tor fo r 6 h at 25,000 rpm. Virus was resuspended in PBS and virus
titers were determ ined by endpoint titra tio n . Serial 10-fold dilutions were tested in 96-well m icro titer plates
and fifty percent Tissue Culture Infective Doses (TCID50) were calculated as described before23.
Plasmids
The CVB3 infectious cDNA clone used in this study, p53CB3/T7, has been described previously23. The EV9 Hill
infectious cDNA clone 24 was generously provided by B. Nelsen-Salz (Virology Institute, University o f Cologne,
Germany).
Isolation of mononuclear cells and generation of monocyte-derived DC
Buffy coats (Sanquin bloodbank Nijmegen) were diluted using PBS containing 0.45% sodium citrate (dilution
solution). M ononuclear cells were isolated by density gradient centrifugation using Lymphoprep (1.077 g /
ml; Axis Shield PoC AS) according to m anufacturer's instructions. Cells w ere washed once in dilution solution
to remove Lymphoprep remains and fu rth e r washed using ice cold dilutio n solution containing 0.1% BSA
until clear supernatant was obtained. A fter counting, cells were resuspended in RPMI 1640 (Invitrogen Life
Technologies) containing 2% human serum at a density o f 12.5 to15 X 10 6 cells/m l and plated o u t in T75 culture
flasks (Costar) at 37°C fo r a period o f 1 h. N on-adherent cells were removed by washing thoroughly w ith PBS
and th e adherent cell fraction was cultured in RPMI 1640 supplem ented w ith 100 U /m l antibiotic-antim ycotic
(Invitrogen), 10 m M L-glutamine and 10% FCS. To generate m onocyte-derived DC, 300 U /m l IL-4 and 400 U/ml
GM-CSF (Strahtman) was added to the culture medium. M edium was refreshed and com plete cytokines added
at day 3. On day 6 , im m ature DCs were harvested using cold PBS and directly used as described below. To
obtain m ature DCs, cells were stim ulated w ith LPS (100 ng /m l) or R848 (4 ^ g /m l) fo r a period o f 24 h.
Infection of monocytes and DCs
M onocytes w ere obtained by incubation o f PBMC in RPMI w ith 2% HS in 96-wells plates fo r 1 h at 37 °C.
N onadherent cells were removed by washing tho rou ghly w ith PBS and the adherent cells w ere infected w ith
virus at th e indicated MOI in SF medium . A fter incubation fo r 60 min at 37oC, cells were washed 3 tim es w ith
PBS and 150 ^ l fu ll medium was added to th e wells. For replication analysis, viruses w ere released at specific
tim es post infection by 3 successive freeze-thaw cycles. Im m ature and m ature DCs were harvested using cold
PBS, washed and infected at an MOI o f 10 in SF RPMI, unless indicated otherw ise. A fter a 60 min incubation at
37oC, cells were washed 3 tim es in an excess volum e o f PBS and plated o u t in 96-wells plates in fu ll medium.
Titrations were done as described above.
Western blot analysis
At 4 and 8 h post infection, cells were lysed and lysates stored at -20°C. Equal am ounts o f protein were
separated by 12.5% SDS-PAGE, electroblotted onto nitro-cellulose membranes (Bio-Rad), follow ed by probing
w ith rabbit polyclonal antiserum raised against th e firs t 60 aa o f CVB3 3A (anti-3A [1-60])25 in a 1:300 dilution.
Because th e 3A proteins o f CVB3 and EV9 are nearly identical (98% identity, 100% sim ilarity), this antibody
recognizes th e 3A protein o f both viruses. A fter 3 washes, membranes were incubated w ith a 1:1000 dilution
48
EV9 causes loss-of-function and cell death in human DCs
o f peroxidase-conjugated goat a n ti-rab bit im m unoglobulins (Dako Diagnostika). Analysis was perform ed using
th e Lumi-Lightplus W estern blotting substrate (Roche M olecular Biochemicals) according to the manufacturer's
instructions.
Immune fluorescence
Im m ature DC (day 6 ) were harvested using cold PBS and infected w ith CVB3 or EV9 at an MOI o f 10 in SF
medium . A fter a 7 h infection period cells were washed 2 tim es in PBS, resuspended in SF medium and 50 X
10 3 cells w ere allowed to adhere to poly-L-lysine coated coverslips fo r 1 h at 37oC. Cells were washed, fixed
w ith 1% paraform aldehyde (PFA) at room tem perature (RT) fo r 20 min and blocked in PBS w ith 3% BSA, 10
m M glycine and 2% human serum (blocking buffer, BB) fo r 60 min at RT. All antibody incubation steps were
perform ed in BB. Cells w ere incubated at RT fo r 45 min using monoclonal anti-DC-SIGN (PN A07406, Beckman
Coulter), washed 2 tim es w ith PBS, follow ed by incubation w ith goat-anti-m ouse IgG Alexa 488 (M olecular
Probes). After fixation w ith 1% PFA and perm eabilization using 0.1% Triton-X100 in PBS fo r 5 min at RT, cells
w ere incubated fo r 45 min w ith rabbit polyclonal anti-3A(1-60), washed 2 tim es in PBS, follow ed by incubation
w ith goat a n ti-rab bit IgG Alexa 594 (M olecular Probes). A fter final washes, cells were sealed using M owiol
(M erck) and visualized w ith a fluorescence microscope.
Blocking studies
Before addition o f virus, cells w ere preincubated at RT fo r 30 min w ith isotype control (mouse IgG1), antiVLA-2 (BD Pharmingen) or a m ixture o f anti-DC-SIGN mAbs AZN-D1 and AZN-D326, 27 (15 ^g /m l). Cells were
washed w ith PBS, resuspended in SF RPMI and infected as described above.
Transfection of viral RNA
p53CB3/T7 and pEV9Hill were linearized by digestion w ith SalI and NotI, respectively, and transcribed in vitro
w ith T7 RNA polymerase. DCs were harvested, washed w ith PBS and resuspended in phenol-red free Optimem
(Invitrogen Life Technologies). RNA (20 ^g) was transferred to a 4-m m cuvette to w hich 200 ^ l cell suspension
containing 3 to 5 X 10 6 cells was added. Cells and RNA were incubated fo r 3 min prio r to being pulsed using
a BioRad GenePulser Xcell (pulse conditions: exponential-wave pulse, 300 V, 150 ^F). A fter transfection, DCs
w ere transferred to full medium and incubated at 37°C. Virus yields were determ ined at various tim e points
after transfection as described above.
Flow cytometry
After harvest, cells were washed in ice-cold PBA (PBS containing BSA and azide) and added to a v-bottom 96wells plate. A fter incubation fo r 30 m in w ith PBA containing 2% HS, cells were stained using m ouse-anti-human
monoclonal antibodies against CD40 (mab 89, kind gift o f Dr R. de W aal-M alefyt, DNAX Research Institute,
Palo Alto, CA), CD80, CD8 6 (both BD Pharmingen) and CD83 (Im m unotech) or th e appropriate isotype controls
(Pharmingen) on ice fo r a period o f 30 min. Cells w ere washed tw ice in PBA and incubated w ith phycoerythin
(PE) labeled goat-anti-m ouse IgG (Pharmingen) on ice fo r a period o f 30 min. A fter washes, cells were fixed in
2% paraform aldehyde and analyzed by flo w cytom etry on a FACSCalibur apparatus (BD Biosciences). Analysis
was done using W inM D I 2.8 software.
ELISA
Dendritic cells were stim ulated w ith TLR ligands as described above and 75 X 10 3 cells/w ell were plated out
in trip lica te in round-bottom 96-wells plates in full m edium . A fter 6 h or 24 h, plates were centrifuged and
supernatants harvested and stored at -80°C until cytokine analysis was done. Cytokine concentrations in
supernatants w ere determ ined using a TNFa or IL-12p70 specific ELISA (both Pierce-Endogen), respectively
DAPI staining
Im m ature DC (day 6 ) w ere harvested using cold PBS and exposed to CVB3 o r EV9 at an MOI o f 10 in SF medium.
After a 24 h infection period cells w ere harvested using trypsin-EDTA, resuspended in SF medium and 50 X 10 3
cells were allowed to adhere to poly-L-lysine coated coverslips fo r 1 h at 37oC. Cells were washed once w ith
PBS and fixed w ith 1% PFA fo r 20 min at RT. Following fixation, cells w ere washed using PBS and incubated at
RT using DAPI (5 m g /m l) at a 1:15,000 dilution in PBS fo r 15 min. After final washes, cells were sealed using
49
Chapter 3
M ow iol (M erck) and visualized using a fluorescence microscope.
Caspase-3/7 activity assay
Caspase a ctivity was measured using th e Apo-one® homogeneous caspase-3/7 assay kit (Promega) according
to m anufacturer's instructions. Briefly, caspase-3/7 reagent was prepared by diluting th e caspase-3/7 substrate
(1:100) w ith caspase-3/7 buffer. Reagent and cell lysates w ere added to w h ite 96-well plates (Porvair Sciences),
m aintaining a 1:1 ratio o f reagent to lysate. Enhanced lysis o f DCs was achieved by fre eze/thaw ing cells prior
to use in assay. Contents were mixed by shaking at 300 rpm on a plate shaker fo r 2 h at RT. Fluorescence was
measured at an excitation wavelength o f 485 nm and an emission o f 540 nm.
Statistical analysis
The differences in th e mean values o f cytokine production o f infected cells compared to controls were
determ ined by tw o-tailed Student's t test. A P value o f <0.05 was considered a significant difference.
A
B
_
TOÜ
<U
O<
f/
È
.Y
■
1 1 -------6
12
EVI(Farouk)
-A- EV7(Walace)
EV8(Bryson)
EV9(Hill)
-e- CVB3(Nancy)
-B-CVB4(Tilo)
-A-CVB4(E2)
18
hours p.i.
C
DC-SIGN
merge
D
CVB3
EV9
hours p.i.
EV9
Figure 1. P roductive infe ction o f hum an m onocyte-derived DCs by several EV strains.
(A) DCs w ere infected w ith various CVB- or EV-strains at an MOI o f 10 and viral titers determ ined at several
tim e points p.i. Representative example o f at least 3 independent experiments using diffe ren t donors. (B) DCs
were exposed to CVB3 or EV9 and lysates made 4 or 8 h p.i. Presence o f virus was shown by W estern blot
using a polyclonal antibody against th e non-structural viral protein 3A. Notice th e double bands, representing
3A and its precursor 3AB. Results shown are fro m one o f 3 independent experim ents w ith sim ilar results. (C)
DCs exposed to CVB3 or EV9 were co-stained using antibodies against th e DC marker DC-SIGN and the viral
protein 3A at 7 h p.i. Presence o f 3A protein in DCs was analyzed using confocal microscopy. M iddle panel
shows individual EV9-infected cell, low er panel shows 3 EV9-infected cells. Representative example o f 2 inde
pendent experiments. (D) DCs were exposed to CVB3 or EV9 at different MOIs and the increase in viral tite r
was determ ined at indicated tim e points.
Results
EV, but not CVB, can productively infect human monocyte-derived DCs
To date, little is known concerning the direct effect of infection with CVB or EV on cells
of the immune system. We aimed to investigate the capacity of these viruses to infect
50
EV9 causes loss-of-function and cell death in human DCs
human DCs and the potential consequences of infection for DC function. Therefore, we
selected a number of representatives from the CVB (CVB3 Nancy, CVB4 Tilo and CVB4
Edwards 2) and EV group (EV1 Farouk, EV7 Wallace, EV8 Bryson and EV9 Hill) that are
reported to use several different receptors for cell entry. As shown in figure 1A, all EV
strains used were capable of infecting DCs, as indicated by a rapid increase in virus titers
with maximal virus titers already observed after 8 h. Interestingly, DCs did not support
replication of closely related CVB strains, as no increase in the amount of infectious virus
was found, even at 48 h post infection (p.i.) (Fig. 1A and data not shown). Thus, a clear
difference exists in susceptibility of DCs for infection with different HeV-B serotypes.
CVB3 Nancy and EV9 Hill (further indicated as CVB3 and EV9) were used during the
remainder of our experiments, unless indicated otherwise. Analysis of viral protein
synthesis by Western blot using a polyclonal antibody that recognizes the CVB3 and EV9
3A proteins showed the presence of significant amounts of viral protein in DC cultures
exposed to EV9, but not CVB3 (Fig. 1B). To exclude that viral replication in cells other
than DCs accounted for the observed effects, infected cultures were co-stained using
antibodies against the viral 3A protein and the DC marker DC-SIGN (dendritic cell-specific
ICAM-3-grabbing nonintegrin)26 at 7 h p.i. Immune fluorescence analysis showed that
>90% of the EV9-infected cells were positive for both 3A and DC-SIGN. No 3A positive
cells could be detected in CVB3-exposed cultures (Fig. 1C). This finding confirmed that
viral replication takes place in DCs.
To investigate whether infection of DCs at a lower multiplicity of infection (MOI)
would also result in efficient replication, the increase in virus titer after exposure of DCs
to CVB3 or EV9 at an MOI of 10, 0.1 or 0.001 was determined. Infecting DCs with EV9 at
an MOI 10,000 X lower than initially used led to a similar increase in virus titer 24 h p.i.,
while no replication was observed for CVB3 at any of the MOIs tested (Fig. 1D). These
results indicate that EV9 is capable of multiple rounds of infection in DC cultures.
Mature DCs, but not monocytes, are permissive for EV infection
Because we used monocyte-derived DCs throughout our experiments and taking into
account that monocytes can function as DC precursors both in vitro and in vivo28-30, we
set out to determine whether these cells are also susceptible to infection. Therefore,
A
B
- © - CVB3, medium
- H - CVB3, LPS
- A - CVB3, R848
EV9, medium
EV9, LPS
- A - EV9, R848
> 9
= o
rs O
H<
6
12
18
hours p.i.
24
hours p.i.
Figure 2. M a tu re DCs, b u t n o t monocytes, are perm issive fo r EV infection.
(A) Monocytes were infected as described fo r DCs in figure 1 and virus titers determ ined at several tim e points
p.i. (B) Im m ature DCs were stim ulated w ith TLR ligands LPS (100 ng /m l) or R848 (4 ^ g /m l) fo r 24 h or left
untreated (m edium ) and subsequently exposed to CVB3 or EV9 at an MOI o f 10, after which viral titers were
determ ined at several tim e points p.i. Data shown are representative o f at least 3 independent experiments.
51
Chapter 3
A
- © —EV1 (IgG1)
gs
& i=
-B -E V 9 (IgG1)
.= IO
- ■ - EV9 (anti DC-SIGN)
EV1 (anti DC-SIGN)
>Q
EO
6
12
18
hours p.i.
B
C
~Q
'A P
6
12
hours p.i.
18
24
hours p.i.
Figure 3. EV infe ction is n o t m ediated via DC-SIGN, b u t requires in te raction w ith a specific cell surface
receptor.
(A) DCs were preincubated w ith a com bination o f DC-SIGN blocking antibodies (AZN-D1, AZN-D3, 15 ^ g /m l)
or the relevant isotype controls fo r a period o f 30 min at RT and subsequently infected w ith EV9 or EV1 at
an MOI o f 10. Increase in virus tite r was determ ined at several tim e points p.i. Representative example o f 3
independent experiments. (B) DCs were preincubated w ith a VLA-2 blocking antibody or isotype control for
a period o f 30 min at RT and subsequently infected w ith EV1 at an MOI o f 10. Increase in virus tite r was de
term ined at several tim e points p.i. Data shown are from one o f tw o representative experiments w ith similar
results. (C) Im m ature DCs were resuspended in 200 ^l phenol-red free Optim em and electroporated w ith 20
^g in v itro transcribed RNA encoding th e viral genome o f CVB3 or EV9. Viral titers were determ ined at several
tim e points after transfection. Data shown are representative o f 3 independent experiments.
monocytes were isolated from peripheral blood mononuclear cells (PBMCs) of healthy
controls and exposed to CVB3 or EV9. No detectable increase in the amount of infectious
virus was observed, indicating that monocytes are not permissive for infection with
either of these viruses (Fig. 2A). In concordance with these data, no 3A protein could
be detected after staining of virus-exposed monocyte cultures with anti-3A antibodies
(data not shown).
Because of the apparent difference in susceptibility between (immature) DCs
and monocytes, we investigated whether mature DCs would support viral replication.
DCs were activated prior to infection by triggering TLR4 or TLR8, involved in recognition
of bacteria- or virus-associated structures, respectively. Full DC maturation was achieved,
as determined by flowcytometric analysis of the expression levels of maturation markers
CD40, CD80, CD83 (data not shown). Infection of both immature and mature DCs with
EV9 resulted in an approximate 3-log increase in viral titers over a 24-h infection period,
whereas no titer increase could be observed for CVB3 (Fig. 2B). Thus, DCs are highly
susceptible to EV infection, irrespective of the DC maturation state.
EV infection of DCs is not mediated via DC-SIGN
DC-SIGN is a C-type lectin specifically expressed by DCs, but not monocytes, and
functions as a pattern recognition receptor for many pathogens. In addition, DC-SIGN
has been reported to facilitate infection of DCs with several viruses31, 32. Considering the
52
EV9 causes loss-of-function and cell death in human DCs
difference in susceptibility between monocytes and DCs, we tested whether EV infection
of DCs could be mediated through DC-SIGN. Therefore, DCs were pre-incubated with
a combination of DC-SIGN blocking antibodies, which have been previously shown to
block interaction between DC-SIGN and measles virus31 as well other pathogens33, 34.
Blocking DC-SIGN did not affect susceptibility of DCs for either EV9 or EV1 (Fig. 3A). Also
pretreatment of DCs with EGTA, a calcium chelator that inhibits C-type lectin function, did
not affect infection efficiency (data not shown). These data make it unlikely that DC-SIGN
is involved in EV entry into DCs. To date, a number of receptors have been identified for
different HeV-B viruses. However, the receptor for EV9(Hill) is yet unknown. The integrin
very late antigen-2 (VLA-2) has been recognized as the receptor for EV1 in HeLa cells35. To
investigate whether infection of DCs is mediated via a specific virus receptor, we tested
the effect of VLA-2 blockage on EV1 infection. Blocking of VLA-2 completely abrogated
EV1 infection of DCs, whereas an isotype control antibody had no effect (Fig. 3B). These
data suggest that EV infection of DCs is mediated via a specific virus receptor.
The difference in susceptibility of DCs for CVB and EV could possibly be due to
lack of expression of the coxsackievirus and adenovirus receptor (CAR) on DCs. Indeed,
no CAR (or decay accelerating factor (DAF)) was detected on the cell surface by flow
cytometry (data not shown), in concordance with earlier findings36. To study whether
CVB3 is capable of replicating in DCs upon bypassing its receptor, cells were transfected
with RNA transcribed in vitro from full-length cDNA clones of CVB3 and EV9. Transfection
resulted in rapid virus production and both CVB3 and EV9 reached similar titers at 8 to
CD40
CD80
CD83
CD86
CVB3
EV9
B
~
£
g
10000
Jö
100
J= 1000
1000
nd
nd
MOCK CVB3
nd
EV9
nd
LPS
R848
nd
MOCK CVB3
nd
EV9
LPS
R848
Figure 4. EV infection does n o t lead to DC m a tura tion o r cytokin e productio n.
(A) DCs were exposed to CVB3 or EV9 at an MOI o f 10 and th e expression o f m aturation markers CD40, CD80,
CD83 and CD8 6 was determ ined by flo w cytom etry 24 h after infection. Thin black lines indicate isotype con
tro l. Grey filled histogram represents expression on mock-infected DCs, thick black lines indicate expression
levels on CVB- or EV9- exposed DCs. (B) DCs w ere infected w ith CVB3 o r EV9 and levels o f TNFa and IL-12p70
in supernatants o f infected DC were determ ined by ELISA after a 24 h infection period. To determ ine the
capacity o f DCs fo r cytokine production, cells were stim ulated in parallel w ith TLR ligands LPS (100 ng/m l)
or R848 (4 |ig /m l). Graphs show mean + SD o f trip lica te measurements. Results shown are representative
example o f 3 independent experiments.
53
Chapter 3
CD 80
CD 83
CD86
A
M OCK
CVB3
EV9
ár» à
k k
I K.
'
'
B
C
C
CLT
O
h
CL
medium
LPS
Figure 5. EV infe ction im pairs responsiveness o f DCs to TLR ligands.
(A) DCs were exposed to CVB3 or EV9 and im m ediately stim ulated w ith TLR ligands LPS (100 ng/m l, data not
shown) or R848 (4 ^ g /m l) a fter last washing step to remove unbound virus. Expression levels o f costim ulatory
molecules CD80, CD83 and CD8 6 w ere determ ined using flo w cytom etry. Thin black lines represent isotype
controls. Grey filled histogram indicate expression on m edium stim ulated DCs and thick black lines represent
expression levels on R848-stimulated DCs. (B and C) DCs w ere exposed to CVB3 or EV9 and im m ediately
stim ulated w ith LPS or R848. TNFa or IL-12p70 levels in DC supernatants were determ ined using ELISA after
a 6 h or 24 h incubation period, respectively. Graphs show mean + SD o f trip lica te wells. Representative ex
amples o f 3 independent experiments. * * , P<0.01 (cytokine production by EV9-infected DCs vs m ock-infected
or CVB3-exposed DCs; tw o-tailed Students t test).
10 h after electroporation of viral RNA (Fig. 3C). After this time, only the titer of EV9
continued to rise because this virus, but not CVB3, is capable of infecting cells that were
not initially transfected. These results support the idea that the incapability of CVB to
replicate in DCs is due to the absence of the appropriate receptor.
Human enteroviruses B do not induce DC activation
Next, it was studied whether infection leads to DC activation, as determined by analyzing
the expression of costimulatory molecules and cytokine production. No upregulation of
54
EV9 causes loss-of-function and cell death in human DCs
the maturation-associated molecules CD40, CD80, CD83 and CD86 could be observed
after a 24-h infection period (Fig. 4A). Instead, EV9 infection led to a small decrease in the
expression of some maturation markers, but this effect was not observed consistently.
To investigate whether infection of DCs results in the production of pro-inflammatory
cytokines, the levels of TNFa and IL-12p70 in DC supernatants were determined at 24 h
p.i. No significant levels (<10 pg/ml) of these cytokines were detected after infection, in
contrast to the high production observed upon stimulation of DCs with LPS or R848 (Fig.
4B). Similar results were found for the production of IL1ß, IL-6 and the anti-inflammatory
cytokine IL-10 (data not shown).
Viral infection is a potent inducer of type I IFNs in many cell types. However, no
IFNa or IFNß was detected using ELISA and quantitative PCR (qPCR) following infection
of DCs with CVB3 or EV9, even at early time points after infection (2, 4, or 6 h p.i.) (data
not shown). Preliminary experiments using a new micro fluidic based qPCR technique,
to study the expression of a broad array of chemokines and cytokines, revealed that
infection did not induce significant changes in any of the target genes analyzed (e.g. IL-6,
IL-8, RANTES (regulated on activation normal T cell expressed and secreted), CCL4, CCL5
etc) at 7 h p.i. (data not shown). Together, these data indicate that DCs do not become
activated upon infection with either EV9 or CVB3.
EV infection impairs TLR responses in DCs
To analyze whether infection affects the response of DCs to TLR ligands, cells were
stimulated with LPS or R848 immediately following infection. Both uninfected and CVB3exposed DCs stimulated with LPS or R848 for 24 h showed an increased expression of
A
B
-A -M O C K
■- 0 - CVB3
—
$
EV9
50
0
0
6
hours p.i.
D
C
MOCK
CVB3
EV9
<
-A -M O C K
- © - CVB3
—
EV9
:rr_ g = — 0
5
6
12
18
24
Figure 6 . EV9 infe ction results in rapid cell death in DC cultures.
(A) DCs were exposed to CVB3 or EV9 at an MOI o f 10 and the percentage o f dead cells in DC cultures was
determ ined at several tim e points p.i. using a Trypan Blue exclusion assay. Graphs show mean +/- SD o f 5
independent experiments. (B) DC m orphology 24 h after exposure to CVB3 or EV9, as analyzed using light
microscopy. (C) DCs were exposed to CVB3 or EV9 at an MOI o f 10 and nuclear staining was perform ed using
DAPI 24 h post exposure. (D) DCs were exposed to CVB3 or EV9 and lysates made at several tim e points p.i.
Caspase-3/7 activity was measured in DC lysates. Graphs show mean +/- SD o f triplicate measurements. One
representative example o f 3 independent experim ents is shown.
55
Chapter 3
CD80, CD83 and CD86 (Fig. 5A). In contrast, infection with EV9 prior to TLR stimulation
consistently resulted in a profound reduction of DC maturation. In addition to phenotypic
maturation of DCs, TLR ligation leads to the release of cytokines like TNFa and IL-12p70.
High levels of these pro-inflammatory cytokines were detected following stimulation
with LPS or R848 in supernatants of uninfected and CVB3-exposed DCs. In contrast,
EV9-infected DCs produced significantly lower levels of TNFa and this deficiency
became apparent as soon as 6 h after stimulation (Fig. 5B). The modest decrease in
TNFa production after activation of CVB3-exposed DCs was not observed consistently.
IL-12p70 levels were undetectable during these early time points, since it is secreted
at a later phase after activation. However, analysis of supernatants at 24 h p.i. showed
that the production of this cytokine is also dramatically impaired (Fig. 5C). Analysis of
cytokine mRNA levels in TLR-activated infected cells revealed that EV9 infection hinders
transcription of TNFa and IL-12p70 at very early time points after infection (data not
shown). These findings indicate that infection can rapidly shut-down TLR responses in
DCs.
Effect of HeV-B on DC viability
HeV-B virus release from infected cells is generally thought to be mediated via cell lysis.
The kinetics of lytic activity was studied in relation to the observed functional impairment
of DCs after infection. Therefore, DCs were exposed to CVB3 or EV9 and the percentage
of dead cells determined by a Trypan Blue (TB) exclusion assay at different time points
p.i. While at 8 h p.i. no significant difference could be observed in cell viability in the
different cultures, hardly any viable cells could be detected 24 h after EV9 infection.
Survival in mock-infected or CVB3-exposed cultures was comparable (Fig. 6A). These
findings were confirmed by light microscopic analysis, revealing obvious signs of cell
death in EV9-infected DC cultures (Fig. 6B).
Enteroviruses are known to trigger a complex type of cell death that shows
characteristics of both necrosis and apoptosis. Staining of the nuclei of EV9-infected DCs
at 24 h p.i. with DAPI revealed predominantly crescent-shaped nuclei with condensed
chromatin (Fig. 6C), a feature that is typical for enterovirus-infected cells37. Only few
cells with fragmented nuclei were typically observed. No changes in nuclear phenotype
were observed in CVB3-exposed cells. Analysis of the activity of effector caspases-3 and
-7 in infected DCs showed little caspase activity up to 8 h p.i., but a steep increase was
observed at later time points in EV9-infected, but not CVB3- exposed cells (Fig. 6D).
Thus, EV9 infection of DCs triggers rapid cell death that shows signs of both necrosis and
apoptosis.
Discussion
In this study, we showed that EV, but not CVB strains, are highly efficient in productively
infecting both immature and mature DCs in vitro. Remarkably, the infection did not
result in activation of DCs. Instead, EV impaired the response of DCs to TLR ligands,
since both maturation and cytokine secretion following stimulation with LPS or R848
were significantly decreased in EV-infected DCs. The clear difference between CVB and
EV regarding outcome of infection is most likely related to absence of the appropriate
receptor for CVB on the DC surface, since bypassing the receptor by electroporation of
56
EV9 causes loss-of-function and cell death in human DCs
CVB RNA resulted in highly efficient replication in DCs. Finally, infection with EV led to
rapid killing of DCs within 24 h after infection.
HeV-B belong to the most common viral causes of intestinal infections in life.
Although infection usually remains limited to the intestinal tract, the virus can cause
serious illnesses by spreading to target organs12. In addition, HeV-B infections have
been associated with chronic immune disorders14, 17-19, but direct proof is lacking and a
pathogenic mechanism has not yet been elucidated. Explanations are sought either in
viral persistence in target organs19, 38, 39, blood40-42 or in viral triggering of an autoimmune
process21, 43, theories that are not mutually exclusive. So far, particularly CVB are thought
to be involved. However, evidence is growing that other serotypes, like EV, can also play
a role15, 44, 45. Our study shows that DCs, which are critically involved in orchestration of
the immune response, can become directly affected by EV in vitro, raising the possibility
that EV may modulate immune responses in vivo.
In contrast to monocyte-derived DCs and macrophages, monocytes themselves
are refractory to HeV-B infection in vitro 46, 47. In line with this, poliovirus, another
member of the genus Enterovirus, has recently been shown to replicate in monocytederived macrophages but not in monocytes48. Thus, within the myeloid lineage, there
is a profound difference in susceptibility for infection. Interestingly, it has been shown
that also the maturation stage of DCs can determine susceptibility for and outcome of
infection with for instance cytomegalovirus49, 50. However, we found that both immature
and mature DCs were equally supportive of EV replication, whereas neither of them could
be productively infected by CVB. Also the type of TLR triggered to induce maturation
(e.g. TLRs involved in recognition of bacterial vs viral structures) could possibly affect
outcome of infection. Therefore, we determined susceptibility of DCs which had been
activated with LPS (TLR4) or R848 (TLR7/8). Both ways of DC activation allowed for
similar replication efficiency of EV in DCs. These findings indicate that DCs are highly
permissive for infection with EV, independent of DC maturation stage or nature of the
maturation stimulus. Also poliovirus has recently been shown to productively infect both
immature and mature DCs, although it should be noted that in their study the DCs were
not activated using TLR ligands48.
The difference in susceptibility between monocytes and DCs, led us to
investigate whether infection was mediated by DC-SIGN, a DC-specific C-type lectin
that was discovered in our lab and is crucially involved in recognition and uptake of
many different pathogens51. It has recently been described that DC-SIGN can serve as a
receptor for measles virus52 and human herpesvirus 832, thereby facilitating infection of
DCs. Blocking of DC-SIGN did not alter the susceptibility of DCs for EV infection. However,
infection with EV1 could be prevented by blocking VLA-2, the EV1 receptor. These data
suggest that EV infection most likely takes place through interaction with a specific cell
surface receptor rather than DC-SIGN. In concordance with this idea, no CAR or DAF
expression was found on DCs, which explains the incapability of the CVB strains tested to
infect DCs. CVB3 was capable of efficient replication upon transfection of viral RNA. The
latter finding suggests that DCs, when infected via alternative routes, may also become
functionally affected by CVB. Such alternative routes can be antibody-mediated uptake
via Fc-receptors, or phagocytosis of infected, dying cells. Indeed, it has recently been
described that the susceptibility of PBMC and monocytes to CVB4 can be enhanced
via an antibody-dependent mechanism46, 53. This mechanism might provide a possible
explanation for the observed presence of CVB in PBMCs of some T1D patients at onset of
57
Chapter 3
the disease54. Whether such alternative routes mediate infection of DCs by CVB requires
further investigation.
Although several viruses induce DC activation upon infection55, 56 and exposure
of monocytes or PBMC to HeV-B results in the production of cytokines57-59, infection of
DCs with CVB or EV did not result in DC activation. This unresponsiveness is striking
since DCs play a central role in the defense against viruses and other microorganisms.
However, enteroviruses are known to deploy several strategies to curtail anti-viral host
cell responses. This is achieved by for instance the action of viral proteases that cleave
transcription factors and translation initiation factors, thereby shutting off cellular
gene expression60, 61. In addition, the 3A protein has been shown to inhibit ER-to-Golgi
transport23, 62 thereby interfering with cytokine secretion and antigen presentation63, 64.
These mechanisms might underlie the absent upregulation of co-stimulatory molecules
and lack of synthesis of cytokines like type I IFNs, TNFa and IL-12 in infected DCs. In
addition, the virus affected the response of DCs to TLR ligands. This might be mediated
via above mentioned effects of infection on gene expression or protein transport or
altered TLR expression levels or localization. Furthermore, decreased cell viability
following infection might also contribute to inhibited TLR responses. However, we found
that also early responses, such as TNFa production, were dramatically impaired, already
before signs of cell death became apparent. This finding demonstrates that the EV not
only suppresses DC activation as a direct result of infection but also limits TLR-mediated
immune responses. Previous studies have yielded similar results upon infection of DCs
with other viruses9, 65. Our findings add EV to the growing list of pathogens that can
interfere with DC function.
In summary, our data demonstrate for the first time that DCs can become
productively infected with EV, but not with CVB strains. Infection does not result in
DC activation or the induction of anti-viral immune responses, but instead impairs
the response to TLR ligands and induces cell death. This might represent an important
evasion strategy, as targeting DCs would interfere with stimulation of T cells specific for
EV or other pathogens. Consequently, failure in clearing virus-infected cells could result
in persistent infection and possibly contribute to HeV-B associated diseases, such as T1D
and chronic myocarditis.
Acknowledgments
This work was supported by grants from the Netherlands Diabetes Foundation (DFN
2001.00.047) to M.K. and The Netherlands Organization for Scientific Research (NWOVIDI-917.46.305) to F.J.M.v.K. and (NWO-912-02-034) to G.J.A.
58
EV9 causes loss-of-function and cell death in human DCs
References
1.
J. B a n c h e re a u , R. M . S te in m a n (1998). D e n d ritic cells and th e c o n tro l o f im m u n ity . N a tu re , 392, 245-252.
2.
T. K aw ai, S. A k ira (2005). Pathogen re co g n itio n w ith T oll-like re ce p to rs. C urr O pin Im m u n o l, 17, 338-344.
3.
C. G. F igdor, Y. va n Kooyk, G. J. A d e m a (2002). C -type le ctin re ce p to rs on d e n d ritic cells and Langerhans cells. N a t Rev Im m u n o l, 2,
7 7-8 4.
4.
R. S p o rri, C. Reis e Sousa (2005). In fla m m a to ry m e d ia to rs are in su ffic ie n t fo r fu ll d e n d ritic cell a c tiv a tio n and p ro m o te e xpansion of
CD4+ T cell p o p u la tio n s lacking h e lp e r fu n c tio n . N a t Im m u n o l, 6, 163-170.
5.
L. A le x o p o u lo u , A . C. H o lt, R. M e d z h ito v , R. A . Flavell (2001). R ecognition o f d o u b le -s tra n d e d RNA and a c tiv a tio n o f N F-kappaB by
T o ll-lik e re c e p to r 3. N a tu re , 4 1 3 , 732-7 3 8 .
6.
F. H e il, H. H e m m i, H. H o c h re in , F. A m p e n b e rg e r, C. K irsch n in g , S. A k ira , G. L ip fo rd , H. W a g n e r, S. B a u e r (2004). Species-specific
re c o g n itio n o f s in g le -stra n d e d RNA via to ll-lik e re c e p to r 7 and 8. Science, 303, 1526-1529.
7.
8.
G. A rro d e , C. D a v rin c h e (2003). D e n d ritic cells and H CM V cro ss-p re se n ta tio n . C u rr Top M ic ro b io l Im m u n o l, 276, 277-294.
C. R u ed l, T. S to rn i, F. Lechner, T. B achi, M . F. B ach m a n n (2002). C ross-p re se n ta tio n o f v iru s-like p a rticle s by s k in -d e rive d CD8(-)
d e n d ritic cells: a d ispensable role fo r TAP. E u r J Im m u n o l, 32, 8 1 8-825.
9.
M . M o u ta fts i, A . M . M e h l, L. K. B o rysie w icz, Z. Tabi (2002). H um an c y to m e g a lo v iru s in h ib its m a tu ra tio n and im p a irs fu n c tio n of
m o n o c y te -d e riv e d d e n d ritic cells. B lood, 99, 2913 -2 9 2 1 .
10.
M . Kruse, O. R osorius, F. Kratzer, G. Stelz, C. K u h n t, G. S chuler, J. H auber, A . S te in k a s s e re r (2000). M a tu re d e n d ritic cells infected
w ith h e rpes s im p le x v iru s ty p e 1 e x h ib it in h ib ite d T-cell s tim u la to ry capacity. J V iro l, 74, 7127-7136.
11.
C. S e rv e t-D e lp ra t, P. O. V id a la in , H. Bausinger, S. M a n ie , F. Le D e ist, O. A zocar, D. H anau, A . Fischer, C. R a b o u rd in -C o m b e (2000).
M ea sle s v iru s induces a b n o rm a l d iffe re n tia tio n o f CD40 lig a n d -a ctiva te d h um an d e n d ritic cells. J Im m u n o l, 164, 1753-1760.
12.
R. R. P. Pallansch M .A . (2001). E nteroviruses: P olioviruses, coxsackieviruses, e ch o viru se s and n e w e r en te ro v iru s e s ., in V iro lo g y, 4 ed.
13.
J. W . Y oon, M . A u s tin , T. O n o d e ra , A . L. N o tk in s (1979). Iso la tio n o f a v iru s fro m th e pancreas o f a ch ild w ith d ia b e tic ketoacidosis.
(Ed.: K. Fields B.N., D .M ., H ow ley, P.M .), Lippincot-R aven, P h ila d e lp h ia , pp. 723-7 7 5 .
N E n g l J M e d , 300, 1 173-1179.
14.
H. H y o ty , K. W . T a ylo r (2002). The role o f viruses in h u m a n d ia b e te s. D ia b e to lo g ia , 4 5 , 1353-1361.
15.
G. R. V re u g d e n h il, N. C. S c h lo o t, A . H o o re n s, C. Rongen, D. G. P ipeleers, W . J. M e lc h e rs , B. O. Roep, J. M . G a la m a (2000). A cute
o n s e t o f ty p e I d ia b e te s m e llitu s a fte r severe e ch o viru s 9 in fe c tio n : p u ta tiv e p a th o g e n ic p athw ays. Clin In fe c t Dis, 31 , 1025-1031.
16.
A . T r ia n ta fy llo p o u lo u , N. T apinos, H. M . M o u ts o p o u lo s (2004). Evidence fo r coxsackievirus in fe c tio n in p rim a ry S jogren's syndrom e.
A r th r itis R heum , 50, 2897 -2 9 0 2 .
17.
B. M a is c h , A . D. R istic, I. P o rtig , S. P a n k u w e it (2003). H um an vira l ca rd io m y o p a th y . F ro n t Biosci, 8, s39-67.
18.
S. F u jio k a , Y. K ita u ra , H. D eg u ch i, A . S h im izu , T. Is o m u ra , H. S um a, H. N. S abbah (2004). Evidence o f vira l in fe c tio n in th e m yoca rd iu m
o f A m e rica n and Japanese p a tie n ts w ith id io p a th ic d ila te d ca rd io m y o p a th y . A m J C ardiol, 94 , 602-605.
19.
R. K a n d o lf, M . Sauter, C. A e p in u s , J. J. Schnorr, H. C. S elinka, K. K lin g e l (1999). M e ch a n ism s and co nsequences o f e n te ro v iru s
20 .
M . L o n n ro t, K. K o rp e la , M . K nip, J. Ilo n e n , O. S im e ll, S. K o rh o n e n , K. Savola, P. M u o n a , T. S im e ll, P. Koskela, H. H y o ty (2000).
21 .
N. R. Rose (2000). V ira l dam age o r 'm o le c u la r m im ic ry '-p la c in g th e bla m e in m y o ca rd itis. N a t M e d , 6, 631-632.
p ersistence in cardiac m yocytes and cells o f th e im m u n e system . Virus Res, 62, 149-158.
E n te ro v iru s in fe c tio n as a risk fa c to r fo r b e ta -ce ll a u to im m u n ity in a p ro s p e c tiv e ly obse rve d b irth c o h o rt: th e Finnish D iabetes
P re d ic tio n and P re ve n tio n Study. D iabetes, 4 9 , 1314-1 3 1 8 .
22.
D. F a irw e a th e r, S. F risancho-K iss, N. R. Rose (2005). V iruses as a d ju va n ts fo r a u to im m u n ity : e vidence fro m C oxsackievirus-induced
m y o c a rd itis. Rev M e d V iro l, 15, 17-27.
23.
E. W essels, D. D u ijsin g s, R. A . N o te b a a rt, W . J. M e lc h e rs , F. J. va n K u p p e ve ld (2005). A p ro lin e -ric h region in th e coxsackievirus 3A
24 .
H. Z im m e rm a n n , H. J. Eggers, A . Z im m e rm a n n , W . Kraus, B. N elsen-S alz (1995). C o m p le te n u c le o tid e sequence and biological
25 .
E. W essels, D. D uijsin g s, T. K. N iu , S. N e u m a n n , V. M . O o rs c h o t, F. d e Lange, K. H. Lanke, J. K lu m p e rm a n , A . H enke, C. L. Jackson,
p ro te in is re q u ire d fo r th e p ro te in to in h ib it e n d o p la s m ic re tic u lu m -to -g o lg i tra n s p o rt. J V iro l, 79, 5163-5173.
p ro p e rtie s o f an in fe c tio u s clone o f p ro to ty p e e ch o viru s 9. Virus Res, 39 , 311-319.
W . J. M e lc h e rs , F. J. va n K u p p e ve ld (2006). A viral p ro te in th a t blocks A rf1 -m e d ia te d COP-I a ssem bly by in h ib itin g th e guanine
n u c le o tid e exchange fa c to r GBF1. D ev Cell, 11, 191-201.
26 .
T. B. G e ijte n b e e k , R. T orensm a, S. J. va n V lie t, G. C. va n D u ijn h o v e n , G. J. A d e m a , Y. va n K ooyk, C. G. F ig d o r (2000). Id e n tific a tio n
o f DC-SIGN, a n ovel d e n d ritic c e ll-sp e cific IC AM -3 re c e p to r th a t s u p p o rts p rim a ry im m u n e responses. Cell, 100, 575-585.
27 .
A . A . B ashirova, T. B. G e ijte n b e e k , G. C. va n D u ijn h o v e n , S. J. va n V lie t, J. B. E ile rin g , M . P. M a rtin , L. W u , T. D. M a rtin , N. V ie b ig ,
P. A . K n o lle , V. N. K e w a lR a m a n i, Y. va n K ooyk, M . C a rrin g to n (2001). A d e n d ritic c e ll-sp e cific in te rc e llu la r a dhesion m o le c u le 3g ra b b in g n o n in te g rin (D C -SIG N )-related p ro te in is h ig h ly expressed on h u m an liv e r sinusoidal e n d o th e lia l cells and p ro m o te s HIV-1
in fe c tio n . J Exp M e d , 193, 6 7 1-678.
28 .
F. C h ap uis, M . R osenzw ajg, M . Y agello, M . E km an, P. B ib e rfe ld , J. C. G lu ckm a n (1997). D iffe re n tia tio n o f h u m an d e n d ritic cells fro m
29 .
N. R o m ani, S. G ru n e r, D. B rang, E. K am pgen, A . Lenz, B. Trocke n b a ch e r, G. K o n w a lin k a , P. O. F ritsch, R. M . S te in m a n , G. S ch u le r
30 .
S. M . K iertsch e r, M . D. R oth (1996). H um an CD14+ le u ko cyte s a cq u ire th e p h e n o ty p e and fu n c tio n o f a n tig e n -p re s e n tin g d e n d ritic
m o n o c y te s in v itro . E ur J Im m u n o l, 27, 431-441.
(1 99 4). P ro life ra tin g d e n d ritic cell p ro g e n ito rs in h u m a n b lo o d . J Exp M e d , 180, 83-93.
cells w h e n c u ltu re d in GM-CSF and IL-4. J Leukoc Biol, 59 , 208-218.
31 .
L. d e W itte , M . A b t, S. S chneide r-S ch a u lie s, Y. va n K ooyk, T. B. G e ijte n b e e k (2006). M easles v iru s ta rg e ts DC-SIGN to enhance
d e n d ritic cell in fe c tio n . J V iro l, 80 , 3477 -3 4 8 6 .
32 .
G. R a p p o ccio lo , F. J. Jen kin s, H. R. H ensler, P. Piazza, M . Jais, L. B o ro w s k i, S. C. W a tk in s , C. R. R in a ld o , Jr. (2006). DC-SIGN is a
33 .
A . C a m b i, K. G ijzen, J. M . d e Vrie s, R. T orensm a, B. Jo o ste n , G. J. A d e m a , M . G. N e te a , B. J. K u llb e rg , L. R o m a n i, C. G. F ig d o r (2003).
re c e p to r fo r h u m a n h e rp e sviru s 8 o n d e n d ritic cells and m a crophages. J Im m u n o l, 176, 1741-1749.
T h e C -type le ctin DC-SIGN (CD209) is an a n tig e n -u p ta k e re c e p to r fo r C andida albicans o n d e n d ritic cells. E ur J Im m u n o l, 33, 5 32
538.
34 .
T. B. G e ijte n b e e k , S. J. V an V lie t, E. A . K o p p e l, M . S a n chez-H ernande z, C. M . V a n d e n b ro u c k e -G ra u ls , B. A p p e lm e lk , Y. V an K oo yk
35 .
J. M . B ergelson, M . P. S hepley, B. M . C han, M . E. H e m le r, R. W . F inberg (1992). Id e n tific a tio n o f th e in te g rin VLA-2 as a re c e p to r fo r
(2 00 3). M y c o b a c te ria ta rg e t DC-SIGN to suppress d e n d ritic cell fu n c tio n . J Exp M e d , 197, 7-17.
e c h o v iru s 1. Science, 255, 1718-1720.
36 .
D. Rea, F. H. Schagen, R. C. H o e b e n , M . M e h ta li, M . J. H avenga, R. E. Toes, C. J. M e lie f, R. O ffrin g a (1999). A d e n o v iru s e s activate
37 .
E. A . Tolskaya, L. I. R o m a n o va , M . S. K o le sn iko va , T. A . Iv a n n ik o v a , E. A . S m irn o v a , N. T. R a ik h lin , V. I. A g o l (1995). A p o p to sis-
38 .
P. Y lip a a s to , K. K lin g e l, A . M . L in d b e rg , T. O to n k o s k i, R. K a n d o lf, T. H o vi, M . R o iva in e n (2004). E n te ro viru s in fe c tio n in hum an
39 .
S. B o pe gam age, J. K ovacova, A . V argova, J. M o tu s o v a , A . P e tro v ic o v a , M . B e n ko vico va , P. G o m o lc a k , J. Bakkers, F. va n K u p p e ve ld ,
h um a n d e n d ritic cells w ith o u t p o la riz a tio n to w a rd a T -h e lp e r ty p e 1 -in d u c in g subset. J V iro l, 73, 10245-10253 .
in d u c in g and a p o p to s is -p re v e n tin g fu n c tio n s o f p o lio v iru s . J V iro l, 69, 1181-1189.
p a n c re a tic islet cells, islet tro p is m in vivo and re c e p to r in v o lv e m e n t in c u ltu re d isle t beta cells. D ia b e to lo g ia , 47 , 225-239.
59
Chapter 3
W . J. M e lc h e rs , J. M . G alam a (2005). Coxsackie B v iru s in fe c tio n o f m ice: in o c u la tio n by th e o ra l ro u te p ro te c ts th e pancreas fro m
d am ag e , b u t n o t fro m in fe c tio n . J Gen V iro l, 86 , 3 271-3280.
4 0.
G. B. C le m e n ts, D. N. G a lb ra ith , K. W . T a y lo r (1995). Coxsackie B v iru s in fe c tio n and o n se t o f c h ild h o o d dia b e te s. Lancet, 346, 2 2 1
223.
4 1.
L. A n d r e o le tti, D. H ober, C. H o b e r-V a n d e n b e rg h e , S. B elaïch, M . C. V a n ty g h e m , J. Lefe b vre , P. W a ttre (1997). D e te ctio n o f coxsackie
B v iru s RNA sequences in w h o le b lo o d sam ples fr o m a d u lt p a tie n ts at th e o n se t o f ty p e I d ia b e te s m e llitu s . J M e d V iro l, 52 , 1 21
127.
4 2.
W . C h e h a d e h , J. W e ill, M . C. V a n ty g h e m , G. A lm , J. L efebvre, P. W a ttre , D. H o b e r (2000). Increased level o f in te rfe ro n -a lp h a in blood
o f p a tie n ts w ith in s u lin -d e p e n d e n t d ia b e te s m e llitu s : re la tio n s h ip w ith coxsackievirus B in fe c tio n . J In fe c t Dis, 181, 1929-1939.
4 3.
4 4.
D. F a irw e a th e r, N. R. Rose (2002). Type 1 d ia b e te s: v iru s in fe c tio n o r a u to im m u n e disease? N a t Im m u n o l, 3, 338-340.
M . R o iv a in e n , P. Y lip a a sto , C. S a vo la in e n , J. G alam a, T. H o vi, T. O to n k o s k i (2002). Functio n a l im p a irm e n t and k illin g o f h um an beta
cells by e n te ro v iru s e s : th e c a p a city is shared by a w id e range o f se ro typ e s, b u t th e e x te n t is a c h a ra c te ris tic o f in d iv id u a l v iru s strains.
D ia b e to lo g ia , 4 5 , 6 9 3-702.
4 5.
T. O to n k o s k i, M . R o iva in e n , O. V aarala, B. D in e se n , J. A . Leipala, T. H o vi, M . K n ip (2000). N e o n a ta l Type I d ia b e te s associated w ith
m a te rn a l e c h o viru s 6 in fe c tio n : a case re p o rt. D ia b e to lo g ia , 4 3 , 1235-1238.
4 6.
D. H o be r, W . C h e h a d e h , A . B o u zid i, P. W a ttre (2001). A n tib o d y -d e p e n d e n t e n h a n c e m e n t o f coxsackievirus B4 in fe c tiv ity o f hum an
p e rip h e ra l b lo o d m o n o n u c le a r cells re su lts in increased in te rfe ro n -a lp h a synthesis. J In fe c t Dis, 184, 1098-1108.
4 7.
P. H o fm a n n , M . S c h m id tk e , A . S telzner, D. G em sa (2001). S uppression o f p ro in fla m m a to ry cy to k in e s and in d u c tio n o f IL-10 in
h u m a n m o n o c y te s a fte r coxsackievirus B3 in fe c tio n . J M e d V iro l, 64, 487-498.
4 8.
R. W a h id , M . J. C a n n o n , M . C h o w (2005). D e n d ritic cells and m acrophages are p ro d u c tiv e ly in fe cte d by p o lio v iru s . J V iro l, 79 , 4 0 1
409.
4 9.
L. H e rte l, V. G. Lacaille, H. S tro b l, E. D. M e llin s , E. S. M o c a rs k i (2003). S u s c e p tib ility o f im m a tu re and m a tu re Langerhans c e ll-typ e
d e n d ritic cells to in fe c tio n and im m u n o m o d u la tio n by h u m an c y to m e g a lo v iru s . J V iro l, 77, 7563-7574.
50.
B. S e ne cha l, A . M . B o ru ch o v, J. L. Reagan, D. N. H a rt, J. W . Y oung (2004). In fe c tio n o f m a tu re m o n o c y te -d e riv e d d e n d ritic cells w ith
51.
A . C am b i, C. G. F ig d o r (2003). Dual fu n c tio n o f C -type le c tin -lik e re ce p to rs in th e im m u n e system . C u rr O pin C ell Biol, 15, 539-546.
h u m a n c y to m e g a lo v iru s in h ib its s tim u la tio n o f T-cell p ro life ra tio n via th e release o f so lu b le CD83. B lood, 103, 4207-4215.
52.
L. c de W itte , M . A b t, S. S chn e id e r-S ch a u lie s, Y. van K ooyk, T. B. G e ijte n b e e k (2006). M easles v iru s ta rg e ts DC-SIGN to enhance
d e n d ritic cell in fe c tio n . J V iro l, 80, 3477-3 4 8 6 .
53.
D. H ob e r, W . C h e h a d e h , J. W e ill, C. H ober, M . C. V a n ty g h e m , P. G ro n n ie r, P. W a ttre (2002). C ircu la tin g and c e ll-b o u n d a n tib o d ie s
increase coxsackievirus B 4-induced p ro d u c tio n o f IFN -alpha by p e rip h e ra l blood m o n o n u c le a r cells fro m p a tie n ts w ith ty p e 1
d ia b e te s . J G en V iro l, 83, 2169-2 1 7 6 .
54.
H. Y in, A . K. B erg, T. T uve m o , G. Frisk (2002). E n te ro viru s RNA is fo u n d in p e rip h e ra l b lo o d m o n o n u c le a r cells in a m a jo rity o f ty p e 1
55.
C. B. Lopez, B. M o lte d o , L. A le x o p o u lo u , L. B o n ifa z, R. A . Flavell, T. M . M o ra n (2004). T LR -in d e p e n d e n t in d u c tio n o f d e n d ritic cell
d ia b e tic c h ild re n at o n s e t. D iabetes, 51 , 1 964-1971.
m a tu ra tio n and a d a p tiv e im m u n ity by n e g a tive -stra n d RNA viruses. J Im m u n o l, 173, 6 882-6889.
56.
P. M . d e G ra aff, E. C. d e Jong, T. M . van Capel, M . E. va n D ijk, P. J. R o h o ll, J. Boes, W . L u y tje s, J. L. K im p e n , G. M . van B le e k (2005).
R e s p ira to ry syncytial v iru s in fe c tio n o f m o n o c y te -d e riv e d d e n d ritic cells decreases th e ir c a p a city to a c tiva te CD4 T cells. J Im m u n o l,
175, 5 9 04 -59 1 1.
57.
G. R. V re u g d e n h il, P. G. W ijn a n d s , M . G. N e te a , J. W . van d e r M e e r, W . J. M e lc h e rs , J. M . G alam a (2000). E ntero viru s-in d u ce d
58.
A . H enke, M . N a in , A . S telzner, D. G em sa (1991). In d u c tio n o f c y to k in e release fro m h um an m o n o c y te s by co xsackievirus in fe c tio n .
59.
A . H en ke, C. M o h r, H. S prenger, C. G ra e b n e r, A . S telzner, M . N a in , D. G em sa (1992). C oxsackievirus B3-induced p ro d u c tio n o f tu m o r
6 0.
S. J. K u e c h le r E., Liebig H.D., S o m m e rg ru b e r W . (2002). P icorn a viru s p ro te in a s e -m e d ia te d s h u to ff o f host cell tra n s la tio n : d ire ct
6 1.
Y. P. D a sgu pta A ., C la rk M ., K lie w e rS ., F radkin L., R u b in s te in S., Das S., Shen Y., W e id m a n M .K ., B a n e rje e R., D a tta U., Igo M ., Kundu
p ro d u c tio n o f p ro -in fla m m a to ry and T -h e lp e r cy to k in e s by h um an leu ko cyte s. C yto kin e , 12, 1 793-1796.
E u r H e a rt J, 12 S u p p l D, 134-136.
n ecrosis fa c to r-a lp h a , IL-1 b e ta , a nd IL-6 in h u m an m o n o cyte s. J Im m u n o l, 148, 2270 -2 2 7 7 .
cleavage o f a c e llu la r in itia tio n fa cto r. , in The m o le c u la r b io lo g y o f picorna viru se s. (Ed.: W. E. S e m le r B.L.), ASM Press, W ashin g to n ,
pp. 3 0 1 -31 1.
P., B a ra t B., B e rk A.J. (2002). Effects o f p ic o rn a v iru s pro te in a se s on h ost cell tra n s c rip tio n , in The m o le c u la r b io lo g y o f p ico rn a viru se s
(Ed.: W. E. S e m ler B.L.), ASM Press, W a sh in g to n , pp. 3 2 1-335.
6 2.
J. R. D o ed en s, K. K irke g a a rd (1995). In h ib itio n o f c e llu la r p ro te in secre tio n by p o lio v iru s p ro te in s 2B and 3A . Em bo J, 14, 894-907.
6 3.
S. B. D e itz , D. A . D o d d , S. C ooper, P. P arham , K. K irke g a a rd (2000). MHC I-d e p e n d e n t a n tig e n p re s e n ta tio n is in h ib ite d by p o lio v iru s
p ro te in 3A. P roc N a tl A c a d Sci U S A , 97 , 1 3790-13795 .
6 4.
D. A . D o d d , T. H. G id d in g s , Jr., K. K irke g a a rd (2001). P olio viru s 3A p ro te in lim its in te rle u k in -6 (IL-6), IL-8, and beta in te rfe ro n
s e c re tio n d u rin g vira l in fe c tio n . J V iro l, 75, 8158-8 1 6 5 .
6 5.
G. P olla ra , K. S pe id e l, L. S am ady, M . R a jp o p a t, Y. M c G ra th , J. L e d e rm a n n , R. S. C o ffin , D. R. Katz, B. C hain (2003). H erpes sim plex
v iru s in fe c tio n o f d e n d ritic cells: balance a m o n g a ctiv a tio n , in h ib itio n , and im m u n ity . J In fe c t Dis, 187, 165-178.
60
Chapter 4
Phagocytosis of picornavirusinfected cells induces an RNAdependent antiviral state in human
dendritic cells
Barbara M. Schulte*, Matthijs Kramer*, Liza W.J. Toonen, Paola
M. Barral, Paul B. Fisher, Kjerstin H.W. Lanke, Jochem M.D.
Galama, Frank J.M. van Kuppeveld, Gosse J. Adema
* These authors contributed equally
Journal o f V irology 2008 82(6):2930-7
Chapter 4
Abstract
D
endritic cells (DCs) play a central role in instructing antiviral immune responses.
DCs, however, can become targeted by different viruses themselves. We recently
demonstrated that human DCs can be productively infected with echoviruses
(EV), but not coxsackieviruses (CVB), both of which are RNA viruses belonging to the
Enterovirus genus of the Picornavirus family. We now show that phagocytosis of CVBinfected, type I IFN deficient cells induces an antiviral state in human DCs. Uptake of
infected cells increased the expression of the cytoplasmic RNA helicases RIG-I and MDA5
as well as other interferon stimulated genes and protected DCs against subsequent
infection with EV9. These effects depended on recognition of viral RNA and could be
mimicked by exposure to the synthetic dsRNA analogue poly(I:C), but not other TLRligands. Blocking endosomal acidification abrogated protection, suggesting a role for
TLRs in the acquisition of an antiviral state in DCs. In conclusion, recognition of viral
RNA rapidly induces an antiviral state in human DCs. This might provide a mechanism by
which DCs protect themselves against viruses when attracted to an environment with
ongoing infection.
62
Recognition o f viral RNA inhibits infection o f DCs
Introduction
Dendritic cells (DCs) are crucial for the induction of antiviral immunity via instruction of
both the innate and adaptive immune system1-3. The hallmark of antiviral responses is
production of type I IFNs. Although classically plasmacytoid DCs were thought to be the
major producers of type I IFNs4, 5, it has been shown that conventional DCs can produce
similarly high type I IFN levels upon viral infection6. In fact, all nucleated cells are capable
of type I IFN production, resulting in the establishment of an antiviral state in neighboring
cells via upregulation of so-called interferon stimulated genes (ISGs).
DCs express a vast array of pattern recognition receptors (PRRs), such as Toll
like receptors (TLRs) that enable them to recognize viral pathogen-associated molecular
patterns (PAMPs) like dsRNA7 and ssRNA8-10. TLRs responding to viral nucleic acids are
localized within the endosomal compartment11, 12 and are triggered upon endocytosis
of viral particles or virus-infected cells, but presumably do not sense cytoplasmic virus
replication upon infection of the DC itself. Instead, recent studies have identified two
structurally related RNA helicases, retinoic acid inducible gene I (RIG-I)13 and melanoma
differentiation associated gene 5 (MDA5)14, both ISGs, as critical mediators in the
response to infection with different RNA viruses in mice15-17. Triggering of MDA5 or RIG-I
causes recruitment of the shared adaptor protein IFN-ß promoter stimulator 1 (IPS-1),
also known as mitochondrial antiviral signaling protein (MAVS), virus-induced signaling
adaptor (VISA), and CARD adaptor inducing IFN-ß (Cardif)18-21, leading to induction of
type I IFNs. RIG-I deficient cells display greatly diminished type I IFN responses to various
RNA viruses and in vitro transcribed dsRNA17, 22. Interestingly, MDA5 deficient cells are
selectively unresponsive to certain picornaviruses, such as encephalomyocarditis virus
(EMCV) and Theiler's encephalomyelitis virus as well as the synthetic dsRNA analogue
poly(I:C)15, 17. This specificity might be related to the presence or absence of 5' triphosphate
groups, which was recently reported to be a critical structure for RIG-I activation23, 24. The
essential contribution of these RNA helicases to antiviral immunity becomes evident in
RIG-I or MDA5 KO mice that readily succumb upon infection with Japanese encephalitus
virus or EMCV, respectively15, 17.
To date, most data regarding RIG-I and MDA5 are derived from mouse studies,
while still little is known regarding the role of these viral sensors in human cells. We
recently showed that infection of human monocyte-derived DCs with EV, but not CVB,
results in rapid inhibition of TLR-mediated responses and massive cell death25. As it is
difficult to reconcile these in vitro effects with the generally mild clinical outcome of
EV infections, we set out to investigate the conditions that could potentially alter DC
susceptibility. In the present work, we demonstrate that phagocytosis of virus-infected
cells results in enhanced expression of RIG-I, MDA5 and other ISGs and protects DCs
against EV infection. These effects require intact endosomal acification and depend on
the presence of RNA in infected cells. Thus, DCs engage a state of antiviral resistance
following recognition of viral RNA.
63
Chapter 4
Materials & Methods
Virus stocks and purification
Reference strains Echovirus 1 Farouk (EV1 Farouk), EV7 Wallace, EV8 Bryson, EV9 Hill and EV11 Gregory were
obtained fro m th e National Institute fo r Public Health and th e Environment (RIVM, Bilthoven, The Netherlands),
CVB3 Nancy was kindly provided by R. Kandolf (University o f Tübingen, Germany). Production o f virus stocks
and virus titra tions were perform ed on buffalo green monkey cells as described previously 25. Serial 10-fold
dilutions w ere tested in 96-well m icro titer plates and fifty percent Tissue Culture Infective Doses ( T C ^ J were
calculated as described before26.
Plasmids
The EV9 Hill infectious cDNA clone 27 was generously provided by B. Nelsen-Salz (Virology Institute, University
o f Cologne, Germany).
Stimulation of monocyte-derived DCs
M onocyte-derived DCs w ere generated as described previously25. M ature DCs w ere obtained by stim ulating
cells w ith poly(I:C) (20 ^ g /m l), LPS (100 ng /m l), R848 (4 ^ g /m l), PAM 3Cys-SKKKK (PAM, 2 ^ g /m l) fo r a period
o f 24 h, unless indicated otherw ise. To block th e actions o f type I IFN, cells were stim ulated in presence or
absence o f neutralizing anti-hum an type I IFN antibodies (1:100, Iivari, Kaaleppi or bovine serum, courtesy of
I. Julkunen, National Public Health Institute, Helsinki, Finland)28. To block endosomal acidification, DCs were
cultured w ith chloroquine (CQ, 10 ^ M ) starting 1 h prior to poly(I:C) stim ulation. For infection, im m ature or
m ature DCs were harvested using cold PBS, washed and infected at an MOI o f 1 w ith indicated viruses in SF
RPMI. A fter 60 m in incubation at 37oC, cells were washed 3 times in an excess volum e o f PBS after w hich viral
titers were determ ined at different tim e points post infection (p.i.) as described above.
Western blot
Equal am ounts o f protein w ere separated by 12.5% SDS-PAGE, electroblotted onto nitro-cellulose membranes
(Bio-Rad), follow ed by probing w ith the indicated antibodies. Anti-RIG-I and anti-PKR antibodies were purchased
fro m ProSci Incorporated and Becton Dickinson Transduction Laboratories, respectively. Production o f rabbit
polyclonal anti-M DA5 was described previously29. RIG-I, PKR and MDA5 antibodies were used in 1:1,000; 1:500
and 1:10,000 dilutions, respectively. A fter washes, membranes were incubated w ith IRDye anti-m ouse o r anti
rabbit IgG (1:15,000) (Li-Cor Biosciences). Imaging was done using th e Odyssey System. W estern blo t analysis
o f viral protein 3A was done as described before25.
Transfection of viral RNA
pEV9Hill was linearized by digestion w ith NotI and transcribed in vitro w ith T7 RNA polymerase (Promega). DCs
w ere harvested, washed w ith PBS and resuspended in phenol-red free Optim em (Invitrogen Life Technologies).
RNA electroporation was perform ed as described before 25.
RNA isolation
Total RNA was isolated fro m DC cultures using TRIZOL reagent (Invitrogen Life Technologies) according to
m anufacturer's instructions, w ith m inor m odifications. RNA inte grity was determ ined by analyzing the
ribosomal 28S and 18S bands on a 1% agarose gel. The reverse transcription reaction was perform ed using
M oloney m urine leukemia virus (MMLV) reverse transcriptase (Invitrogen) according to th e m anufacturer's
instructions. For each sample a "-RT" control was included in which th e reverse transcriptase was replaced by
DEPC treated milli-Q. The cDNA was stored at -20°C until fu rth e r use.
Quantitative PCR
Q uantitative analysis o f gene expression in DCs was done using SYBR Green based qPCR. The qPCR reactions
w ere perform ed in a 25 ^ l volum e containing: 12.5 ^ l SYBR Green mix (Applied Biosystems), 1.5 ^l fo rw a rd /
reverse prim er (300 nM endconcentration), 4.5 ^l m illi-Q and 5 ^l cDNA dilution. Reactions were perform ed on
an ABI 7900HT Sequence Detection System (Applied Biosystems). Analysis was done using sequence detection
system software (SDS, version 2.0, Applied Biosystems). Primer sequences are available upon request and were
64
Recognition o f viral RNA inhibits infection o f DCs
designed using the freely accessible Primer Bank program 30.
Uptake of Vero cells
Vero cells were labeled using PKH26 (Sigma-Aldrich) according to m anufacturers instructions and infected
w ith CVB3 at an MOI o f 10. Cells were harvested and washed 6 -8 h p.i. and resuspended in fresh m edium at a
density o f 5 X 10 6 cells/m L prior to placing them at -20°C until fu rth e r use. Vero cell preparations were added
to DC cultures at a ratio o f 1:1 (in some experiments DCs had been pretreated w ith CQ as described above).
Alternatively, Vero cell preparations w ere exposed to a m ixture o f RNAse A (Roche) and RNAse V-I (Ambion) or
an equal volum e o f PBS fo r a period o f 15 min at 37°C prior to addition to DCs. Uptake o f Vero cells by DCs was
analyzed using flo w cyto m e try and confocal microscopy.
Confocal microscopy
DCs w ere harvested, washed and allowed to adhere to poly-L-lysine coated coverslips in serum free medium
fo r 1 h at 37oC. Cells w ere fixed w ith 1% paraform aldehyde (PFA) and blocked in PBS w ith 3% BSA, 10 mM
glycine and 2% human serum (blocking buffer, BB).
For cell surface stainings, cells were incubated using
m ouse-anti-hum an DC-SIGN (Beckman Coulter) or mouse-anti human HLA-DR/DP (ascites) in BB, washed
and incubated w ith isotype specific Alexa labeled goat-anti-mouse IgGs (Alexa 568/Alexa 647, Molecular
Probes). For intracellular staining, cells w ere fixed using 1% PFA, permeabilized using 0.1% Triton-X100 in
PBS and incubated w ith rabbit polyclonal anti-M DA5 follow ed by incubation w ith goat an ti-rabbit IgG Alexa
488 (M olecular Probes) in BB. A fter final washes, cells w ere sealed using M ow iol (Merck) and analyzed using
confocal microscopy (Biorad MRC 1024).
Statistical analysis
Statistical analysis was perform ed using Student's t test (2-tailed distribution). A P-value < 0.05 was
considered a significant difference.
Results
Poly(I:C) induces resistance against viral infection in human DCs
We previously reported that human DCs display a striking difference in susceptibility to
infection with distinct enteroviruses, a genus of the picornavirus family. While DCs are
productively infected with EV, they are resistant to infection with the closely related CVB25.
Here, we investigated the effect of stimulation with different TLR ligands on susceptibility
for EV infection. Untreated DCs and DCs stimulated with LPS (TLR4), PAM3Cys (TLR1/2)
or R848 (TLR7 or TLR8) were all highly susceptible to EV9 infection, leading to significant
increases in virus titers and viral proteins (Fig. 1A). In contrast, stimulation with the
synthetic viral dsRNA analogue poly(I:C) dramatically reduced EV9 replication (Fig. 1A),
in a concentration dependent manner (data not shown). Time course analysis showed
that resistance to EV9 infection was accrued within 6 h after poly(I:C) exposure (Fig. 1B).
Additionally, infection of DCs with EV1, EV7, EV8 and EV11 could also be inhibited by
poly(I:C) treatment, showing that the protective effect applied to a broad range of EV
strains (Fig. 1C). Poly(I:C) stimulated DCs also displayed reduced virus replication upon
delivery of in vitro transcribed EV9 RNA directly into the DC cytoplasm, suggesting the
induction of an active antiviral state, rather than simple downregulation of the (as yet
unidentified) EV9 receptor on the cell surface (Fig. 1D).
To evaluate the effects of TLR triggering on expression of genes that are crucially
involved in the innate antiviral response, we determined mRNA levels of the viral sensors
RIG-I and MDA5 and the effector molecule PKR. Stimulation with PAM, R848 or lipoteichoic
acid (LTA) did not affect ISG expression and only a modest increase was observed in
some experiments using LPS. However, stimulation with poly(I:C) consistently induced a
65
Chapter 4
A
B
4.0
C
--
-©-• medium
-érpoly(I:C)
/
0.5
3AB
3A
12
18
-0
24
-14
-10
- 6 - 2
..J
4.0
* f
3.0
8 S
2.0
ï |
c j»
i i
1.0
~
2
EV11
0.0
-1.0
medium
poly(I:C)
timepoint of poly(I:C) exposure
prior to infection (h)
E
D
--- ---$
I f 30'
Í
m
£
« *
IE
g.
«
a
\
15
0
6
3
5
8
hours after electroporation
F
I
s
12
18
time (h)
24
G
s
6
12
18
time (h)
DC-SIGN
6
24
MDA-5
12
18
time (h)
24
merge
ë
medium
RIG-I
Sp/
A y
.
MDA5
PKR
po]y(l:C)
0 »
0
actin
H
H medium
Kpoly(I:C)
-L P S
45
H
RIG-I
I .
- IFN ab
+ IFN ab
u rn
- IFN ab
+ IFN ab
- IFN ab
+ IFN ab
-B- medium
poly(I:C)
-©■ poly(I:C) + IFN ab
1.5
Eß
0.5
£ §
/
1.0
/X “
K
--
0.0« £
0.5
6
hours p.i
Figure 1. Poly(I:C) s tim u la tio n protects hum an DCs against EV infe ction and increases expression o f RIG-I,
MDA5 and PKR.
(A) DCs w ere left untreated or stim ulated w ith poly(I:C) (20 ^ g /m l), LPS (100 ng/m l), R848 (4 ^ g /m l) or PAM3Cys-SKKKK (PAM, 2 ^ g /m l) fo r 24 h and infected w ith EV9 at an MOI o f 1, after w hich viral titers were de
term ined at several tim e points p.i. Insert shows th e expression o f viral protein 3A and its precursor 3AB in
unstim ulated DCs (left lane) or poly(I:C) stim ulated DCs (right lane) (B) DC were stim ulated w ith poly(I:C) (20
^ g /m l) at different tim e points p rio r to infection w ith EV9 at an MOI o f 1. Increase in viral titers was deter
mined 24 h p.i. (C) DCs were left untreated or stim ulated w ith poly(I:C) (20 ^ g /m l) fo r a period o f 24 h and
subsequently infected w ith EV1, EV7, EV8 , EV9 or EV11 at an MOI o f 1. Shown is the increase in viral titers 24
h p.i. (D) DCs were stim ulated w ith poly(I:C) (20 ^ g /m l) fo r 24 h and subsequently electroporated using 20
^g in v itro transcribed RNA fro m th e full-length cDNA clone o f EV9. Increase in viral titers was determ ined at
several tim e points after electroporation. (E) DCs w ere stim ulated using LPS, R848, PAM or poly(I:C) as de
scribed fo r (A) and mRNA levels o f RIG-I, MDA5 and PKR were determ ined using qPCR at several tim e points
after stim ulation. (F) Protein expression o f RIG-I, MDA5 and PKR was analyzed by w estern b lo t 24 h after
stim ulation o f DCs as described in (A). (G) DCs were left untreated or stim ulated w ith poly(I:C) (20 ^g /m l)
fo r 24 h after which DCs were harvested, stained using DC-SIGN and MDA5-specific antibodies and analyzed
using confocal microscopy as described in materials and methods. (H) DCs were stim ulated w ith poly(I:C) (20
^ g /m l) in th e presence or absence o f type I IFN neutralizing antibodies (Iivari, Kaaleppi and bovine anti-IFNa,
see materials and methods). A fter 8 h, mRNA expression levels o f RIG-I, MDA5 and PKR w ere determ ined
using qPCR. Shown is mean expression + SD o f 3 independent experiments using diffe ren t donors (*, P<0.05;
* * , P<0.01). (I) DCs w ere stim ulated w ith poly(I:C) (20 ^ g /m l) in the presence or absence o f type I IFN neutral-
66
Recognition o f viral RNA in h ibits infection o f DCs
izing antibodies fo r 24 h, washed and subsequently infected w ith EV9 at an MOI o f 1 after which virus titers
w ere determ ined at several tim e points p.i. Data shown is representative o f >5 (A, E), 3 (C, D, F, G, H, I)) or 2
(B) independent experim ents
strong upregulation of RIG-I, MDA5 and PKR (Fig. 1E and data not shown). Western blot
(WB) analysis corroborated our findings by qPCR and demonstrated elevated protein
levels following exposure to poly(I:C) (Fig. 1F). Confocal analysis showed an increased
expression of endogenous MDA5 in the cytoplasm of poly(I:C) stimulated human DCs
(Fig. 1G). Furthermore, neutralizing antibodies against type I IFN inhibited the effect of
poly(I:C) on both expression of ISGs (Fig. 1H) and viral infection (Fig. 1I) implying that
poly(I:C) exerts its effect at least in part via autocrine type I IFN stimulation.
A
B
no Vero
Vero(M )
Vero(CVB)
Vero(MOCK)
Vero(CVB)
PKH26
C
IRF7
PKR
- medium
- © - Vero(M)
Vero(CVB)
X <C.
<
z
D£C
2
3
-A-m edium
- © - Vero(M)
Vero(CVB)
4
5
6
tim e o f c o c u ltu re (h)
E
MHC-II
MDA5
2
3
4
5
6
tim e o f c o c u ltu re (h)
Vero(PKH)
merge
Figure 2. Phagocytosis o f virus-infected cells increases th e expression o f RIG-I, MDA5 and PKR.
(A) PKH26 labeled Vero cell preparations (m ock-or CVB3-infected) w ere added to CFSE labeled DC cultures in
a ratio o f 1:1. A fter 24 h, the num ber o f CFSE+PKH26+ DCs was analyzed using flow cytom etry. (B) Presence of
PKH26+ Vero cell m aterial w ith in DCs after a 24 h coculture as analyzed using confocal microscopy. DCs were
stained using anti-MHCII (C) DCs w ere cocultured w ith mock- or CVB3-infected Vero cell preparations and the
mRNA expression o f PKR and IRF7 was determ ined using qPCR at different tim e points after start o f cocul
ture. (D) DCs w ere cocultured w ith Vero cell preparations as described in (A) and protein expression o f RIG-I,
MDA5 and PKR was determ ined using w estern blot 24 h after start o f coculture. (E) DCs w ere cocultured w ith
Vero cell preparations as described in (A) and 24 h later cells w ere stained w ith MHC-II and MDA5-specific
antibodies and analyzed using confocal microscopy. Data shown are representative o f > 6 (A), 4 (B) or 3 (C-E)
independent experim ents using diffe ren t donors.
67
Chapter 4
Collectively, these data indicate that exposure to synthetic dsRNA causes
upregulation of both viral sensors and effector molecules and protects DCs against EV
infection.
Phagocytosis of infected cells by DCs leads to upregulation of ISGs
To study the DC-virus interaction in a more physiological model, we explored whether
phagocytosis of CVB3-infected cells by DCs would induce similar effects as stimulation
with poly(I:C). CVB3 was used because this virus, if released from infected (dying) cells,
does not cause infection of DCs 25 nor upregulation of RIG-I, MDA5 or PKR (data not
shown). Since secretion of type I IFNs by infected cells could influence susceptibility
for infection and ISG expression in DCs, all experiments were performed with Vero
cells, which carry a genetic defect in type I IFNs synthesis 31 32. CVB3-infected, but not
uninfected Vero cells, were efficiently taken up by DCs (data not shown), likely reflecting
the effect of infection on Vero cell viability. For the remainder of our experiments we used
freeze-thawed cell preparations that were taken up with equal efficiency, irrespective
of the infection status of the cells (Fig. 2A). This enabled us to analyze the effect of
uptake of uninfected or virus-infected cells on ISG expression and susceptibility in DCs.
Confocal analysis confirmed the flowcytometry data by showing the presence of PKH26+
compartments within DCs (Fig. 2B). As the primers for human RIG-I and MDA5 crossreact with their Vero cell (Cercopithecus aethiops, African green monkey) homologues,
we focused on mRNA expression of the ISGs IRF7 and PKR. Although uptake of mockinfected Vero cells had no effect, phagocytosis of CVB3-infected cells caused a rapid and
profound upregulation of IRF7 and PKR in DCs (Fig. 2C). Western blot analysis showed
that uptake of CVB-infected, but not of mock-infected Vero cells, resulted in increased
protein levels of RIG-I, MDA5 and PKR (Fig. 2D). No ISG protein expression was detected
in CVB3-infected Vero cell preparations as such (data not shown). Confocal analysis
further confirmed increased MDA5 levels in DCs that had taken up CVB3-infected Vero
cells as compared to mock-infected cells (Fig. 2E). Thus, phagocytosis of CVB3-infected
cells by DCs leads to rapid upregulation of molecules involved in the innate antiviral
response and can occur independently of type I IFN released by infected cells.
Phagocytosis of CVB-infected cells protects DCs against EV infection
To determine whether upregulation of ISGs following uptake of infected cell preparations
by DCs resulted in functional protection, DCs were subsequently infected with EV9.
Vero cell preparations themselves did not support replication of EV9 (data not shown).
Phagocytosis of infected preparations resulted in a markedly decreased EV replication in
DC cultures, while uptake of uninfected cells had no effect (Fig. 3A). Western blot analysis
showed notably lower levels of the viral protein 3A and its precursor 3AB in DCs that had
taken up CVB-infected Vero cells, which confirmed inhibited EV growth (Fig. 3A).
We next assessed whether phagocytosis of these preparations could protect
DCs against EV9-induced cell death. As shown in figure 3B, EV9 caused massive cell
death in both untreated DCs and DCs that had taken up uninfected cell preparations. In
contrast, uptake of CVB3-infected cell preparations strongly enhanced cell survival. Also
exposure to poly(I:C) decreased cell death following EV infection. Taken together, these
data indicate that phagocytosis of virus-infected cells can effectively protect human DCs
against the lethal effects of EV infection.
68
Recognition o f viral RNA inhibits infection o f DCs
A
B
100
3 MOCK
I EV9
75
50
25
0
hours p.i.
Figure 3. Phagocytosis o f infected cells protects DCs against EV infe ction.
(A) DCs were left untreated or cultured w ith mock o r CVB-infected Vero cell preparations fo r a period o f 24 h
after which DCs w ere harvested, washed and subsequently infected w ith EV9 at an MOI o f 1. Viral titers were
determ ined at different tim e points p.i. Insert shows the expression o f viral protein 3A and its precursor 3AB
follow in g uptake o f mock-infected (left lane) o r CVB3-infected (right lane) Vero cells, 8 h after infection o f DCs
w ith EV9. (B) DCs were treated as described in (A) and the percentage o f dead cells was determ ined using
a trypan blue exclusion assay 48 h p.i. Graph shows mean + SD o f 4 quadruplicates per condition ( * * * , P <
0.001). Data shown are representative o f at least 3 independent experim ents using diffe ren t donors.
ISG upregulation in DCs following phagocytosis of infected cells requires intact
endosomal acidification and is mediated via recognition of viral RNA
Infected, dying cells taken up by DCs are localized to so-called phagosomes, which
subsequently "mature" via fusion with the endosomal/lysosomal compartments,
resulting in a progressive decrease in pH33. Interestingly, intracellular TLRs are also
recruited to these compartments, enabling interaction with potentially released PAMPs,
like dsRNA, which occurs in a pH dependent fashion34. To determine if endosomal
acidification is required for the induction of viral resistance following uptake of infected
cell preparations, we pretreated DCs with chloroquine (CQ), a chemical that blocks
acidification of these compartments. Pretreatment of DCs with CQ markedly decreased
mRNA expression of IRF7 and PKR (Fig. 4A) as well as RIG-I, MDA5 and PKR protein
levels (Fig. 4B). Importantly, the CQ mediated reduction in ISG levels was accompanied
by reduced protection against EV infection (Fig. 4C). These effects were not related to
impaired phagocytosis, since CQ had no effect on uptake of Vero cell preparations (data
not shown). CQ also reduced the poly(I:C) mediated increase in ISG expression (Fig. 4D)
and completely abrogated the inhibitory effect of poly(I:C) on infection (Fig. 4E).
We next investigated the potential contribution of viral RNA present in the
infected Vero cell preparations to both upregulation of ISGs and the induction of
a resistant state. To this aim, CVB3-infected and uninfected cell preparations were
incubated with a mixture of RNAses prior to addition to DCs. RNAse treatment did not
affect uptake of preparations by DCs (data not shown). Degradation of RNA resulted in
a strongly reduced upregulation of IRF7 and PKR mRNA levels (Fig. 4F) and RIG-I, MDA5
and PKR protein expression in DCs (Fig. 4G). Furthermore, RNAse treatment abrogated
the protective effect on EV infection of DCs (Fig. 4H), demonstrating the essential role of
recognition of viral RNA in the induction of an antiviral state.
69
Chapter 4
A
B
R IG -I
MDA5
PKR
a ctin
D
C
medium
- © - Vero(M)
- • - Vero(M)+CQ
-B-V ero(C V B )
■*V e ro (C V B )+ C Q
>Q
co
äs ?
§â
_
< ^
“
j= |
> (A
S2
CQ
6
12
+ CQ
CQ
+ CQ
CQ
+ CQ
18
hours p.i.
E
F
3.0
-© - med
-•-m ed+CQ(10^M)
-B-po!y(!:C)
-B-poly(I:C)+CQ(10^M)
2.0
1.0
0.01
12
18
hours p.i.
H
G
medium
-e-V ero(M )
Vero(M)+RNAse
-B-Vero(CVB)
Vero(CVB)+RNAse
R IG -I
MDA5
PKR
6
12
18
24
hours p.i.
a ctin
Figure 4. Ind uction o f an an tivira l state requires inta ct endosom al acidifica tion and is m ediated via recogni
tio n o f vira l RNA.
(A) DC w ere left untreated or preincubated w ith CQ (10 ^M ) fo r 1 h prio r to addition o f Vero cell preparations.
A fter an 8 h coculture, cells were harvested and mRNA expression o f IRF7 and PKR was analyzed using qPCR.
(B) DCs w ere stim ulated as in (A) and protein expression o f RIG-I, MDA5 and PKR was determ ined using WB 16
h after coculture (C) DCs were stim ulated as in (A) and infected w ith EV9 at an MOI o f 1 16 h after coculture.
Viral titers were determ ined at several tim e points p.i. (D) DC were left untreated or preincubated w ith CQ
(10 ^ M ) prior to addition o f poly(I:C) (20 ^ g /m l). After 8 h stim ulation, the expression o f RIG-I, MDA5 and
PKR and IRF 7 was analyzed using qPCR. Shown is mean expression + SD o f 3 independent experiments using
different donors (* * , P<0.01). (E) DCs were treated as described in (A) and after 8 h stim ulation, cells were
harvested, washed extensively and infected w ith EV9 at an MOI o f 1, after w hich viral titers were determ ined
at several tim epoints p.i. (F) Vero cell preparations were left untreated or exposed to a m ixture o f RNAseA
70
Recognition o f viral RNA inhibits infection o f DCs
and RNAseV-I prior to addition to DC cultures as described in materials and methods. Expression o f PKR and
IRF7 in DCs was analyzed using qPCR 8 h after addition o f Vero cell preparations. (G) DCs w ere cocultured
w ith Vero cell preparations as described in (D) and protein expression o f RIG-I, MDA5 and PKR was analyzed
by WB 16 h after start o f coculture. (H) DCs w ere treated as described in (D) and 16 h after start o f coculture,
cells were harvested, washed and infected w ith EV9 at an MOI o f 1. Data are representative o f 3 independent
experim ents using diffe ren t donors.
Discussion
Phagocytosis of infected cells represents one of the defense mechanisms against viral
infection and is executed by different immune cells. Here we report that uptake of CVB3infected cells by human DCs resulted in rapid increase in both mRNA and protein levels
of viral sensors including the RNA helicases RIG-I and MDA5 and effector molecules like
PKR. Upregulation of these ISGs required intact endosomal acidification, was dependent
on the presence of viral RNA and could be mimicked by exposure to the synthetic dsRNA
analogue poly(I:C). Moreover, DCs that had taken up CVB-infected cells were protected
against lethal infection with EV.
Recent mouse studies have highlighted the role of various RIG-like helicases in
recognition of viral RNA15' 17, 22. These findings have challenged our view of the relative
importance of TLRs and non-TLRs in anti-viral immunity. For instance, recognition of
the synthetic dsRNA mimetic poly(I:C) was classically thought to be mediated via TLR3
7, while more recent data implicate MDA5 to be a crucial component for type I IFN
production upon poly(I:C) stimulation or viral infection in mice15, 17. Very limited data
is available regarding these novel RNA sensors in the human setting, but one study
shows that poly(I:C) responses in human cell lines are RIG-I dependent35, suggesting the
existence of species-specific or cell-type specific differences, analogues to the speciesspecific difference in recognition of ssRNAs by TLR7 and TLR89.
We previously demonstrated the dramatic consequences of EV infection on the
function and viability of human DCs25. We presently document that distinct TLR ligands
displayed a remarkably different effect on the induction of viral resistance in DCs. While
poly(I:C) rapidly increased the level of different ISGs, including RIG-I and MDA5, and
protected DCs against infection, other ligands such as PAM, LTA and R848 did not. LPS
caused a modest increase in ISG expression. This might imply that ISG upregulation is
mediated in a TRIF dependent fashion, as both poly(I:C) and LPS have been reported to
signal via this adaptor protein36.
To study the effects of viral RNA recognition under conditions that more closely
resemble the physiological situation, we used a model system in which DCs acquired
virus-infected cells via phagocytosis. Uptake of CVB3-infected cells resulted in ISG
upregulation and protection against EV, both of which could be blocked by CQ. As CQ is
known to increase endosomal pH and it has been shown that the interaction between
poly(I:C)/TLR334 and CpG/TLR937 is pH dependent, this would suggest a role for TLR3
in our experiments. Alternatively, CQ could hamper transport of viral structures, such
as dsRNA, to the cytoplasm where recognition by other PPRs like RIG-I or MDA5 could
take place. However, a recent study has shown that CQ treatment of human DCs rather
increases export of soluble antigen from early endosomes into the cytosol thereby
promoting antigen cross-presentation38. Identification of the exact routing of viral PAMPs
following uptake by DCs can possibly aid in dissecting the relative contribution of TLRs
and RNA helicases to different facets of the antiviral immune response.
71
Chapter 4
It has been shown that, besides viral nucleic acids, viral proteins can also alter the
activation status of DCs39, 40, which could affect DC susceptibility following phagocytosis
of infected cells. Our experiments identified RNA within infected Vero cell preparations
to be the crucial component for both ISG upregulation and resistance against infection.
Since uptake of non-infected cells had no effect, we favor a role for viral RNA in these
processes. However, we can not exclude that infection leads to modification of host RNA
structures that could be subsequently recognized by different RNA sensors. The use of
Vero cells in our experiments showed that phagocytosis of infected cells by DCs can
induce protection independently of type I IFN released by infected cells. Thus, recognition
of RNA could preserve the ability of DCs to engage an antiviral state, even when type I
IFN responses in the infected cells are blocked as a consequence of viral immune evasion
strategies.
In conclusion, recognition of viral RNA rapidly induces an antiviral state in
human DCs. This might reveal a mechanism by which DCs protect themselves against
viruses when attracted to an environment with ongoing infection, thereby facilitating
adequate instruction of virus-specific T cells to clear viral infection.
Acknowledgments
The authors would like to thank Bianca Blom (Amsterdam Medical Center/University
of Amsterdam, Amsterdam, The Netherlands) for help with the type I IFN blocking
experiments. This work was supported by grants from the Netherlands Diabetes
Foundation (DFN 2001.00.047) to M.K. and The Netherlands Organization for Scientific
Research (NWO-VIDI-917.46.305) to F.J.M.v.K. and (NWO-912-02-034) to G.J.A. P.M.B
and P.B.F. were supported by a National Institutes of Health, General Medical Sciences
grant (1R01 GM068448).
72
Recognition o f viral RNA inhibits infection o f DCs
References
1.
H. B a rth , A . U ls e n h e im e r, G. R. Pape, H. M . D ie p o ld e r, M . H o ffm a n n , C. N e u m a n n -H a e fe lin , R. T h im m e , P. H e n n e ke , R. K le in , G.
P ara nh os-B accala, E. D epla, T. J. Liang, H. E. B lu m , T. F. B a u m e rt (2005). U ptake and p re s e n ta tio n o f h e p a titis C viru s -lik e p articles
by h um a n d e n d ritic cells. B lood, 105, 3605-3 6 1 4 .
2.
C. E. A n d o n io u , S. L. van D o m m e le n , V. V o ig t, D. M . A n d re w s , G. B riza rd , C. A s s e lin -P a tu re l, T. D elale, K. J. Stacey, G. T rin c h ie ri,
M . A . D egli-E sposti (2005). In te ra c tio n b e tw e e n c o n v e n tio n a l d e n d ritic cells and n a tu ra l k ille r cells is in te g ra l to th e a c tiv a tio n of
e ffe c tiv e a n tiv ira l im m u n ity . N a t Im m u n o l, 6, 1011-1019.
3.
N. C. F ernandez, A . Lozier, C. F la m e n t, P. R iccia rd i-C a sta g n o li, D. B e lle t, M . S uter, M . P e rric a u d e t, T. Tursz, E. M ara sko vsky, L.
Z itv o g e l (1999). D e n d ritic cells d ire c tly trig g e r NK cell fu n c tio n s : cro ss-ta lk re le v a n t in in n a te a n ti-tu m o r im m u n e responses in vivo.
N a t M e d , 5, 4 0 5-411.
4.
M . C ella, F. Facchetti, A . Lanzavecchia, M . C o lo n n a (2000). P lasm acytoid d e n d r itic cells a c tiv a te d by influenza v iru s and CD40L drive
a p o te n t TH1 p o la riz a tio n . N a t Im m u n o l, 1, 3 0 5-310.
5.
D. Jarrossay, G. N a p o lita n i, M . C o lo n n a , F. S allu sto , A . Lanzavecchia (2001). S pecialization and c o m p le m e n ta rity in m icro b ia l
6.
S. S. D ie b o ld , M . M o n to y a , H. U nger, L. A le x o p o u lo u , P. Roy, L. E. H a sw e ll, A . A l-S h a m k h a n i, R. Flavell, P. B o rro w , C. Reis e Sousa
m o le c u le re c o g n itio n by h um an m y e lo id and p la sm a cyto id d e n d ritic cells. E ur J Im m u n o l, 31, 3 388-3393.
(2 00 3). V ira l in fe c tio n sw itc h e s n o n -p la s m a c y to id d e n d ritic cells in to high in te rfe ro n pro d u ce rs. N a tu re , 4 2 4 , 324-328.
7.
L. A le x o p o u lo u , A . C. H o lt, R. M e d z h ito v , R. A . Flavell (2001). R ecognition o f d o u b le -s tra n d e d RNA and a c tiv a tio n o f N F-kappaB by
T o ll-lik e re c e p to r 3. N a tu re , 4 1 3 , 732-7 3 8 .
8.
S. S. D ie b o ld , T. Kaisho, H. H e m m i, S. A k ira , C. Reis e Sousa (2004). In n a te a n tiv ira l responses by m eans o f TLR 7-m ediated re co g n itio n
o f s in g le -stra n d e d RNA. Science, 303, 1 529-1531.
9.
F. H e il, H. H e m m i, H. H o c h re in , F. A m p e n b e rg e r, C. K irsch n in g , S. A k ira , G. L ip fo rd , H. W a g n e r, S. B a u e r (2004). Species-specific
10.
J. M . Lund, L. A le x o p o u lo u , A . S ato, M . K arow , N. C. A d a m s , N. W . G ale, A . Iw a sa ki, R. A . Flavell (2004). R ecognition o f s in g le
re c o g n itio n o f s in g le -stra n d e d RNA via to ll-lik e re c e p to r 7 and 8. Science, 303, 1526-1529.
s tra n d e d RNA viruses by T oll-like re c e p to r 7. P roc N a tl A c a d Sci U S A , 101, 5598-5603.
11.
M . M a ts u m o to , K. F u n a m i, M . T anabe, H. O s h iu m i, M . S hingai, Y. S eto, A . Y a m a m o to , T. Seya (2003). S u b ce llu la r lo ca liza tio n of
T o ll-lik e re c e p to r 3 in h um an d e n d ritic cells. J Im m u n o l, 171, 3 154-3162.
12.
T. N is h iy a , E. K a jita , S. M iw a , A . L. D e fra n co (2005). TLR3 and TLR7 are ta rg e te d to th e sam e in tra c e llu la r c o m p a rtm e n ts by d is tin c t
13.
M . Yone yam a, M . K iku ch i, T. N a ts u k a w a , N. S h in o b u , T. Im a iz u m i, M . M iy a g is h i, K. Taira, S. A k ira , T. F u jita (2004). The RNA helicase
re g u la to ry e le m e n ts . J B io l Chem , 280, 3 7 1 0 7 -3 7 1 1 7 .
RIG-I has an essential fu n c tio n in d o u b le -s tra n d e d R N A -induced in n a te a n tiv ira l responses. N a t Im m u n o l, 5, 730-737.
14.
D. C. Kang, R. V. G o p a lk ris h n a n , Q. W u , E. Ja n kow sky, A . M . Pyle, P. B. F ish e r (2002). m da-5: An in te rfe ro n -in d u c ib le p u ta tiv e RNA
helicase w ith d o u b le -s tra n d e d R N A -d e p e n d e n t ATPase a c tiv ity and m e la n o m a g ro w th -s u p p re s s iv e p ro p e rtie s . P roc N a tl A c a d Sci U
S A , 99, 6 3 7-642.
15.
L. G itlin , W . B a rch e t, S. G ilfilla n , M . C ella, B. B e u tle r, R. A . Flavell, M . S. D ia m o n d , M . C o lo n n a (2006). Essential ro le o f m da-5 in
ty p e I IFN responses to p o ly rib o in o s in ic :p o ly rib o c y tid y lic acid and e n c e p h a lo m y o c a rd itis p ico rn a viru s. P roc N a tl A c a d Sci U S A , 103,
8 45 9-8 4 6 4 .
16.
M . Yone yam a, M . K iku ch i, K. M a ts u m o to , T. Im a iz u m i, M . M iy a g is h i, K. Taira, E. Foy, Y. M . Loo, M . G ale, Jr., S. A k ira , S. Y onehara, A.
K ato, T. F u jita (2005). Shared and u n iq u e fu n c tio n s o f th e D E xD /H -box helicases RIG-I, M D A 5, and LGP2 in a n tiv ira l in n a te im m u n ity.
J Im m u n o l, 175, 2851-2 8 5 8 .
17.
H. K ato, O. T akeuchi, S. Sato, M . Yoneyam a, M . Y a m a m o to , K. M a ts u i, S. U e m a ts u , A . Jung, T. K aw ai, K. J. Ish ii, O. Yam aguchi, K.
O ts u , T. T s u jim u ra , C. S. Koh, C. Reis e Sousa, Y. M a ts u u ra , T. F u jita , S. A k ira (2006). D iffe re n tia l roles o f M D A 5 and RIG-I helicases in
th e re c o g n itio n o f RNA viruses. N a tu re , 4 4 1 , 101-105.
18.
T. K aw a i, K. T akahashi, S. Sato, C. C oban, H. K um ar, H. K ato, K. J. Ish ii, O. T akeuchi, S. A k ira (2005). IPS-1, an a d a p to r trig g e rin g RIG
I- and M d a 5 -m e d ia te d ty p e I in te rfe ro n in d u c tio n . N a t Im m u n o l, 6, 981-988.
19.
R. B. S e th , L. Sun, C. K. Ea, Z. J. Chen (2005). Id e n tific a tio n and ch a ra c te riz a tio n o f MAVS, a m ito c h o n d ria l a n tiv ira l sign a lin g protein
t h a t a ctiva te s N F-kappaB and IRF 3. Cell, 122, 669-6 8 2 .
20 .
L. G. X u , Y. Y. W a n g , K. J. H an, L. Y. Li, Z. Zhai, H. B. Shu (2005). VISA is an a d a p te r p ro te in re q u ire d fo r v iru s -trig g e re d IFN-beta
sign aling. M o l Cell, 19, 727-7 4 0 .
21 .
E. M e y la n , J. C u rra n , K. H o fm a n n , D. M o ra d p o u r, M . B in d e r, R. B arte n sch la g e r, J. T schopp (2005). C ardif is an a d a p to r p ro te in in th e
RIG-I a n tiv ira l p a th w a y and is ta rg e te d by h e p a titis C virus. N a tu re , 4 3 7 , 1 167-1172.
22.
H. Kato, S. Sato, M . Y oneyam a, M . Y a m a m o to , S. U e m a tsu , K. M a ts u i, T. T s u jim u ra , K. Takeda, T. F u jita , O. T akeuchi, S. A k ira (2005).
23 .
V. H o rn u n g , J. Ellegast, S. K im , K. Brzozka, A . Jung, H. K ato, H. Poeck, S. A k ira , K. K. C o n ze lm a n n , M . Schlee, S. Endres, G. H a rtm a n n
24 .
A . P ic h lm a ir, O. Schulz, C. P. Tan, T. I. N a slu n d , P. L ilje s tro m , F. W e b e r, C. Reis e Sousa (2006). R IG -I-m ediated a n tiv ira l responses to
Cell ty p e -s p e c ific in v o lv e m e n t o f RIG-I in a n tiv ira l response. Im m u n ity , 23, 19-28.
(2 00 6). 5 '-T rip h o s p h a te RNA is th e ligand fo r RIG-I. Science, 314, 994-9 9 7 .
s in g le -s tra n d e d RNA b e a rin g 5 '-p h o s p h a te s . Science, 314, 9 97-1001.
25 .
M . K ram er, B. M . S ch u lte , L. W . T oonen, M . A . d e B ru ijn i, J. M . G a la m a , G. J. A d e m a , F. J. van K u p p e ve ld (2007). E chovirus in fe ctio n
causes rapid lo s s -o f-fu n c tio n and cell d e a th in h um an d e n d ritic cells. C ell M ic ro b io l, 9, 1507-1518.
26 .
E. W essels, D. D u ijsin g s, R. A . N o te b a a rt, W . J. M e lc h e rs , F. J. va n K u p p e ve ld (2005). A p ro lin e -ric h region in th e coxsackievirus 3A
27 .
H. Z im m e rm a n n , H. J. Eggers, A . Z im m e rm a n n , W . Kraus, B. N elsen-S alz (1995). C o m p le te n u c le o tid e sequence and biological
p ro te in is re q u ire d fo r th e p ro te in to in h ib it e n d o p la s m ic re tic u lu m -to -g o lg i tra n s p o rt. J V iro l, 79, 5163-5173.
p ro p e rtie s o f an in fe c tio u s clone o f p ro to ty p e e ch o viru s 9. Virus Res, 39 , 311-319.
28 .
K. E. M o g e n s e n , L. P yhala, K. C a n te ll (1975). Raising a n tib o d ie s to h u m an le u ko cyte in te rfe ro n . A c ta P a th o l M ic ro b io l S cand [B ], 83,
4 4 3 -45 0.
29 .
L. Lin, Z. Su, I. V. Lebedeva, P. G u p ta , H. B ouke rch e , T. Rai, G. N. B arber, P. D e n t, D. Sarkar, P. B. F isher (2006). A c tiv a tio n o f Ras/Raf
30 .
X. W a n g , B. Seed (2003). A PCR p rim e r b a n k fo r q u a n tita tiv e gene expression analysis. N u cle ic A cids Res, 31, e154.
31 .
J. M . Em eny, M . J. M o rg a n (1979). R egulation o f th e in te rfe ro n system : e vidence th a t V ero cells have a g e n e tic d e fe c t in in te rfe ro n
32 .
J. D es m yte r, J. L. M e ln ic k , W . E. R aw ls (1968). D efectiveness o f in te rfe ro n p ro d u c tio n and o f ru b e lla v iru s in te rfe re n c e in a lin e of
33 .
J. M . B la n d e r, R. M e d z h ito v (2006). On re g u la tio n o f p hagosom e m a tu ra tio n and a n tig e n p re s e n ta tio n . N a t Im m u n o l, 7, 1 0 2 9
34 .
O. d e B o u te ille r, E. M e rc k , U. A . H asan, S. H ubac, B. B e n g u ig u i, G. T rin c h ie ri, E. E. Bates, C. C aux (2005). R ecognition o f d o u b le
p ro te c ts cells fro m m e la n o m a d iffe re n tia tio n -a s s o c ia te d g e n e -5 -in d u ce d a p o p to sis. Cell D eath D iffe r, 13, 1982-1993.
p ro d u c tio n . J Gen V iro l, 4 3 , 2 4 7-252.
A fric a n green m o n ke y kid n e y cells (V ero). J V iro l, 2, 955-961.
1035.
s tra n d e d RNA by h u m an to ll-lik e re c e p to r 3 and d o w n s tre a m re c e p to r sign a lin g re q u ire s m u ltim e riz a tio n and an a cidic pH. J Biol
C hem , 2 80, 38133-3 8 1 4 5 .
35 .
G. C heng, J. Z h o n g , J. C hung, F. V. C h isa ri (2007). D o u b le -stra n d e d DNA and d o u b le -s tra n d e d RNA induce a c o m m o n a n tivira l
73
Chapter 4
s ign aling p a th w a y in h u m a n cells. P roc N a tl A c a d Sci U S A , 104, 9 035-9040.
3 6.
M . Y a m a m o to , S. Sato, H. H e m m i, K. H o s h in o , T. K aisho, H. S anjo, O. T akeuchi, M . S ugiyam a, M . O ka b e , K. Takeda, S. A k ira (2003).
Role o f a d a p to r TRIF in th e M y D 8 8 -in d e p e n d e n t to ll-lik e re c e p to r sign a lin g p athw ay. Science, 301, 640-643.
3 7.
M . R utz, J. M e tzg e r, T. G e lle rt, P. L uppa, G. B. L ip fo rd , H. W a g n e r, S. B a u e r (2004). T oll-like re c e p to r 9 binds s in g le -stra n d e d CpGD N A in a s e q u ence- and p H -d e p e n d e n t m anner. E ur J Im m u n o l, 34, 2 541-2550.
3 8.
D. A ccap ezza to, V. V isco, V. F ra n ca villa , C. M o le tte , T. D o n a to , M . P aroli, M . U. M o n d e lli, M . D o ria , M . R. T o rrisi, V. B a rn a b a (2005).
3 9.
A . R o lla n d , E. J o u v in -M a rc h e , C. V ir e t, M . Faure, H. P e rro n , P. N. M a rc h e (2006). T he en ve lo p e p ro te in o f a h um an endo g e n o u s
C h lo ro q u in e e nhances h um an CD8+ T cell responses against so lu b le a n tig e n s in vivo . J Exp M e d , 202, 817-828.
re tro v iru s -W fa m ily a ctiva te s in n a te im m u n ity th ro u g h CD14/TLR4 and p ro m o te s T h 1 -like responses. J Im m u n o l, 176, 7636-7 6 4 4 .
4 0.
E. M a r tin e lli, C. Cicala, D. V an Ryk, D. J. G o o d e , K. M a c le o d , J. A rth o s , A . S. Fauci (2007). HIV-1 g p 120 in h ib its T LR 9-m ediated
a c tiv a tio n and IF N -{alpha} se cre tio n in p la sm a cyto id d e n d ritic cells. P roc N a tl A c a d Sci U S A , 104, 3 396-3401.
74
Chapter 5
Phagocytosis of enterovirusinfected pancreatic beta-cells
triggers innate immune
responses in human dendritic cells
Barbara M. Schulte, Matthijs Kramer, Marleen Ansems,
Kjerstin H.W. Lanke, Neeltje van Doremalen, Jon D. Piganelli,
Rita Bottino, Massimo Trucco, Jochem M.D. Galama,
Gosse J. Adema, Frank J.M. van Kuppeveld
D iabetes, in press
Chapter 5
Abstract
ype 1 diabetes is a chronic endocrine disorder, in which enteroviruses, such as
coxsackie B viruses and echoviruses, are possible environmental factors that
can trigger or accelerate disease. The development or acceleration of type 1
diabetes depends on the balance between autoreactive effector T cells and regulatory T
cells. This balance is particularly influenced by dendritic cells (DCs).
Objective. To investigate the interaction between enterovirus-infected human pancreatic
islets and human DCs.
Research Design and Methods. In vitro phagocytosis of human or porcine primary islets
or Min6 mouse insuloma cells by DCs was investigated by flow cytometry and confocal
analysis. Subsequent innate DC responses were monitored by qPCR and western blotting
of interferon-stimulated genes (ISGs).
Results. We show that both mock- and coxsackievirus B3 (CVB3)-infected human and
porcine pancreatic islets were efficiently phagocytosed by human monocyte-derived DCs.
Phagocytosis of CVB3-infected, but not mock-infected human and porcine islets resulted
in induction of ISGs in DCs, including the RIG-I-like helicases (RLHs) RIG-I and Mda5.
Studies with murine Min6 insuloma cells, which were also efficiently phagocytosed,
revealed that increased ISG-expression in DCs upon encountering CVB-infected cells
resulted in an antiviral state that protected DCs from subsequent enterovirus infection.
The observed innate antiviral responses depended on RNA within the phagocytosed
cells, required endosomal acidification and were type I interferon (IFN)-dependent.
Conclusions. Human DCs can phagocytose enterovirus-infected pancreatic cells and
subsequently induce innate antiviral responses, such as induction of RLHs. These
responses may have important consequences for immune homeostasis in vivo and may
play a role in the etiology of type 1 diabetes.
T
76
Uptake of ß-cells results in human DC activation
Introduction
Type 1 diabetes mellitus, or insulin-dependent diabetes, is a chronic endocrine disorder
characterized by the progressive loss of insulin-producing ß-cells. In the majority of cases,
type 1 diabetes is associated with an autoimmune reaction against ß-cell constituents.
Genetic predisposition is a major risk factor for the acquisition of type 1 diabetes but the
pair-wise concordance between monozygotic twins is limited (< 40%), which indicates
that other, environmental, factors are involved1. Also other observations (a gradual rise
of the incidence and a 10-fold difference in occurrence of type 1 diabetes in different
parts of Europe) point to a significant contribution of the environment1.
Enteroviruses of the Human Enterovirus B (HEV-B) species of the Picornaviridae,
such as coxsackievirus B (CVB) and echovirus (EV), have since long been associated
with type 1 diabetes2-4. These small, non-enveloped single-stranded RNA viruses are
widespread. Infection usually remains limited to the gastrointestinal tract and causes
mild disease or even remains asymptomatic. However, during severe infections it can
spread to secondary target organs such as the pancreas, brain and heart5. CVB has been
implicated in type 1 diabetes on the basis of (i) isolation of virus from patients with acute
diabetes, (ii) detection of viral RNA in blood at onset (iii) epidemiological surveys, and
(iv) prospective studies (reviewed in6, 7).
Importantly, several recent studies reported detection of HEV-B in the pancreatic
islets of type 1 diabetes patients at autopsy, providing evidence that these viruses are
able to infect beta cells in vivo8-10. Inflammation in pancreatic islets is common in type
1 diabetes patients, and several immune cells can be detected in the islets of type 1
diabetes patients. Among these are phagocytes, as well as different subsets of T cells,
such as effector CD4+ and CD8+ T cells and in some cases regulatory T cells (Treg)8, 11 12. The
development or acceleration of type 1 diabetes might depend on the balance between
autoreactive effector T cells and Treg13; a balance which is predominantly decided by
dendritic cells (DCs).
The importance of antigen-presenting cells (APCs, such as macrophages and
DCs) in type 1 diabetes development has been shown in vivo in mouse studies, where
phagocytosis of CVB-infected islet cells was crucial for development of auto-immune type
1 diabetes. Resident APCs were shown to engulf CVB-infected ß-cells, and subsequently
stimulated antigen-specific T cell proliferation and induced diabetes upon adoptive
transfer14. Furthermore, mouse studies have revealed that influx of macrophages and
DCs precedes that of effector T cells in the islets and aberrantly express pro-inflammatory
cytokines15. In human pancreatic islets DCs are present in low numbers under steadystate conditions; however, as ß-cell destruction ensues leading to diabetes there is an
increase in DC-infiltrate16, 17, strengthening the hypothesis that these cells likely play an
important role in the progression of human type 1 diabetes. To our knowledge, no studies
have been performed that examine the interaction between CVB-infected human islets
and human DCs.
DCs are the professional APCs of the immune system and play a decisive role in
initiating immune responses and maintaining self tolerance. They do not only participate
in innate immunity, but also initiate and control adaptive immunity18. DCs continuously
sample their microenvironment; they phagocytose pathogens or pathogen-associated
products such as immune complexes, yet also apoptotic cells are taken up19. This results
in the induction of immunity against invading pathogens and tolerance to self-antigens,
77
Chapter 5
respectively20. Induction of an immune response occurs when DCs detect pathogenassociated "danger signals" or pathogen-associated molecular patterns (PAMPs),
through specialized receptors, known as pattern recognition receptors (PRRs). These
PRRs include several receptors that sense the presence of viral RNA, such as Toll-like
receptors (TLR) 3, 7 and 8 and the RIG-I-like helicases (RLHs), retinoic acid-inducible gene
I (RIG-I) and melanoma differentiation-associated gene 5 (Mda5)21, 22. Polymorphisms
and mutations in PRR family members have been associated with disease, including
autoimmune diseases such as type 1 diabetes23-25. The interaction between PRRs and
PAMPs facilitates DC maturation, after which the DCs migrate to draining lymph nodes
where they present antigen to T lymphocytes18. During viral infection, triggering of these
receptors induces type I interferons (IFNs). The IFNs are crucial for a first innate line of
defense against invading viruses, yet they also influence adaptive immunity by affecting
DC cytokine production and maturation26 and autoimmunity27.
In this study, we set out to investigate the interaction between human DCs
and CVB-infected islets and the immunological consequences that follow. For this, we
used monocyte-derived DCs from healthy blood donors and CVB-infected pancreatic
islet preparations or CVB-infected Min6 cells, a murine insuloma cell line. We show that
both human islets and Min6 cells are phagocytosed by human DCs. CVB-infected cells,
but not mock-infected cells, induced DC activation as indicated by the expression of
interferon-stimulated genes (ISGs) resulting in protection of the DCs from subsequent
enteroviral infection. These innate DC responses depended on the recognition of RNA
in the CVB-infected cells and additionally required IFNs produced by the DC itself, but
did not depend on soluble factors secreted by the infected cells. These virus-induced
alterations in DCs may have important consequences for immune homeostasis in vivo
and may play a role in the etiology of type 1 diabetes.
78
Uptake of ß-cells results in human DC activation
Research Design and Methods
Virus stocks and purification
Reference strain Echovirus 9 Hill (EV9) was obtained fro m th e National Institute fo r Public Health and the
Environment (RIVM, Bilthoven, The Netherlands). CVB3 Nancy (CVB3) was kindly provided by R. Kandolf
(University o f Tübingen, Germany). Production o f virus stocks and virus titra tions w ere perform ed on buffalo
green monkey cells as described previously. Serial 10-fold dilutions were tested in 96-well m icro titer plates and
50% Tissue Culture Infective Doses (TCID50) were calculated as described before28.
Islet and Min6 cell culture
Human and porcine pancreatic islets w ere isolated in Pittsburgh as described before29. Human islets were
obtained fro m deceased anonymous donors procured by CORE (Center fo r Organ recovery and Education,
Pittsburgh), and islets were isolated using a m odification o f th e sem i-autom ated m ethod described by Ricordi29
Islets batches used in this study w ere obtained fro m 4 adult human pancreas and 3 porcine donors, cultured
fo r a m inim um o f 3 to 6 days in CMRL-1066 m edium containing 10% fetal calf serum, 2 m M L-glutamine, 100U/
ml penicilin, 0.1m g/m l streptom ycin (Complete CMRL), at 37°C in an atm osphere o f 5% CO2. Islet viability was
estim ated by dual fluorescence viability dyes (Calcein-AM and Propidium Iodide, Invitrogen, Eugene, OR) and
was higher than 80% in all batches. Glucose stim ulated insulin release was carried o u t by dynamic perifusion31.
A fter culture fo r 3 to 6 days th e islets were sent to Nijmegen as fre e-flo ating islets and cultured in Complete
CMRL in ultra low attachm ent culture plates (Corning) at 37°C in 5% CO2. Islets were cultured in Nijmegen for
m axim um 2 days before start o f the experiments,
M in 6 cells 32 were a kind gift fro m Dr. Merja Roivainen and Dr. Per Bendix Jeppesen, and were cultured in
DMEM (Gibco) supplem ented w ith 15% FCS, ciproxin, 50 ^M ß-m ercaptoethanol at 37°C in 5% CO2. Medium
was refreshed every oth er day.
Infection of islets and Min6 cells
Islets and M in 6 cells were infected in a small volum e o f CMRL-1066 or DMEM, respectively, at indicated
m u ltip licity o f infection (MOI) fo r 1 h at 37°C. Subsequently, cells w ere washed and viral titers w ere determ ined
at different tim e points as described above. In some experiments supernatant from infected cultures was
harvested at indicated tim e post infection (p.i.) and cleared fro m cell debris by centrifugation before stim ulation
o f other cells.
Stimulation of monocyte-derived DCs
M onocyte-derived DCs were generated as described previously28. M ature DCs were obtained by stim ulating
cells w ith poly(I:C) (20 ^ g /m l). Stim ulation o f DCs w ith supernatant fro m M in 6 cells or fro m D C /M in 6 co
cultures was perform ed using a 1:2 dilutio n o f supernatant. To block the actions o f type I interferons (IFNs),
cells were stim ulated in presence or absence o f neutralizing anti-hum an IFN antibodies (1:75, Iivari, Kaaleppi
or bovine serum, courtesy o f Dr Julkunen, National Public Health Institute, Helsinki, Finland)33. For infection,
stim ulated or unstim ulated DCs w ere harvested using cold PBS and infected in RPMI. A fter 60 min incubation
at 37oC, cells were washed and viral titers were determ ined as described above.
Uptake of human pancreatic islets and Min6 cells
Human and porcine pancreatic islets or M in 6 cells were labeled using PKH26 (Sigma-Aldrich) according to
m anufacturers instructions and infected w ith CVB3 at an MOI o f 10. DCs were labeled using CFSE (Invitrogen)
according to m anufacturer's instructions. PKH-labeled cells were added to CFSE-labeled DC cultures at a ratio
o f 1:1. Alternatively, labeled, infected M in 6 cells were incubated fo r 48h and subsequently harvested and
resuspended in fresh medium at a density o f 5^10 6 cells/m L prio r to placing them at -20°C until fu rth e r use.
Freeze-thawed cell preparations were subsequently used in DC co-cultures at a 1:1 ratio and resulted in similar
inductions o f ISGs and innate responses com pared to co-culture w ith viable cells (Supplementary figure 1
and34). These cell preparations w ere also used fo r RNase-treatment prior to DC stim ulation. For th a t purpose
79
Chapter 5
M in 6 cell preparations were exposed to a m ixture o f RNaseA, RNase VI and RNaseI (all Am bion) or an equal
volum e o f PBS fo r a period o f 30 min at 37°C prior to addition to DCs. Uptake o f islets or M in 6 cells by DCs was
analyzed using flo w cytom etry and confocal microscopy. In some experiments phagocytosis was inhibited using
cytochalasin D (CytD) (2 ,5^g/m l), or endosomal acidification was inhibited using chloroquine (CQ) (10^M ). DCs
w ere pretreated fo r 30 min w ith CytD or CQ, and subsequently stim uli were added. Both treatm ents had no
effect on cell viability as assessed by trypan blue exclusion 8 h after stim ulation.
Confocal microscopy
Staining and visualization o f DCs has been described before34. Human islets were adhered on to fibronectincoated coverslips fo r 2h at 37°C in islet medium and subsequently fixed in 2% PFA. Cells were blocked in PBS
containing 100 m M glycine and 2% goat serum, permeabilized using TX-100 and stained w ith mouse anti-VP1
(D akocytom ation) and rabbit anti-3A 35 follow ed by incubation w ith goat anti-m ouse IgG alexa 488 and goat
an ti-rab bit IgG alexa 594. Cells were analyzed using a Leica DMR microscope.
RNA isolation, quantitative PCR (qPCR), western blot and flow cytometry
These techniques have been described before 34
Statistical analysis
Statistical analysis was perform ed using Student's t te s t (2-tailed distribution). A P-value < 0.05 was considered
a significant difference.
80
Uptake of ß-cells results in human DC activation
Results
Human dendritic cells phagocytose human pancreatic islets and induce innate immune
responses.
Human pancreatic islets were found to be susceptible to infection by CVB3 as indicated
by the profound increase in virus titer, cytopathic effects and immunofluorescence
staining against viral proteins 3A and VP1 (Fig. 1A-C). The latter revealed that only a
small number of cells were infected. Infected cells mainly resided at the outer layers of
the islets, where cells might be more accessible for the virus (Fig. 1C). Previously it was
shown that such a productive infection results in impaired islet function36.
To investigate whether human DCs can phagocytose human pancreatic islets,
PKH-labeled human islets were mock- or CVB3-infected for 48 hours and subsequently co
cultured with CFSE-labeled DCs. CVB3 has no direct effect on human DCs and is incapable
of infecting DCs28. Mock- and CVB3-infected islets were taken up with equal efficiency,
as indicated by the number of DCs that became PKH-positive (Fig. 1D). Confocal analysis
confirmed uptake of human pancreatic islets material by DCs. The DC plasma membrane
was stained with CD86 specific antibodies (green), and PKH-positive islet cells (red) were
observed within the DCs (Fig. 1E).
To examine whether and how DCs respond to virus-infected human islets we
studied activation of innate immune response pathways by measuring levels of ISGs,
such as RIG-I, Mda5, PKR and IRF-7 following phagocytosis of infected cells. qPCR
revealed induction of ISGs after engulfment of CVB3-infected islets; moreover, increased
expression was observed for all ISGs tested (Fig. 1F). Importantly, stimulation of DCs with
mock-infected human islets alone did not induce any ISGs (Fig. 1F). Furthermore, also
stimulation with CVB3 alone did not induce ISGs28, suggesting that the induction depends
on the presence of virus or viral products within phagocytosed cells. CVB3 was not able
to replicate in DCs upon entry via phagocytosis, as determined by endpoint titration at
several times after start of co-cultures (data not shown). In some experiments, freezethawed mock- or CVB-infected cells were used. This had no effect on either phagocytosis
or ISG-induction (see below).
At this stage we were unable to discriminate whether the ISGs were upregulated
in DCs or in the islets themselves. Therefore, we performed experiments using porcine
islets, which have been shown a useful model for studies on the interaction of CVBs with
ß-cells37. To discriminate between ISGs in porcine islets and human DCs, primers were
used that specifically recognize human, but not porcine ISG sequences. Infection and
uptake of porcine islets by DC was similar as described above for the human islets (data
not shown). Phagocytosis of CVB-infected porcine islets resulted in a profound increase
in human ISGs (Fig. 1G). Thus, using porcine islets we confirmed induction of ISGs in
human DCs upon uptake of CVB3-infected human islets, and, additionally revealed that
ISG-expression is increased in the human DC-population.
Phagocytosis of CVB3-infected Min6 cells by human DCs results in an antiviral state
that protects DCs from subsequent enterovirus infection.
To further investigate the underlying mechanism of DC responses upon uptake of islets,
we selected the murine Min6 cell line as a model for pancreatic ß-cells. Min6 cells retain
the physiological characteristics of normal ß-cells, and respond to glucose within the
physiological range32. These islet-like cells grow in patches (Fig. 2B, left panel) and were
81
Chapter 5
hoechst
A
B
VP1
C
Mock
CVB3
D
E
DC + Islet/M
DC + Islet/CVB
DC + Islet/CVB
PKH
F
Mda5
RIG-I
f..
G
M Med
- # ■ Islet/M
- A - Islet/CVB
~
D
<
i0
0
8
16
PKR
0
8
16
2
RIG-I
40
Med
—# • porc Islet/M
A
porc Islet/CVB
30
20
§
10
8
2
0_
0
8
16
0
8
PKR
IRF-7
f -----------
Mda5
16
24
IRF-7
K
K
/
0
8
16
24
8
Time (h p.i.)
16
24
8
16
24
8
Time (h p.i.)
16
24
Figure 1. CVB replicates in hum an and porcine pancreatic islets, and DC can phagocytose islets, resulting
in in d u ctio n o f ISGs.
(A and B) Human islets cells w ere infected w ith CVB3 at an MOI o f 10 and (A) at indicated tim e points replica
tion was analysed and (B) at 48h p.i. images w ere taken. (C) Human islets w ere infected w ith CVB3 at an MOI
o f 10. A fte r 24 h incubation, islets were adhered onto fibronectin coated coverslips and stained using 3A (red)
and VP1 (green) specific antibodies. Hoechst stain is included to visualize cell nuclei (D) Human islets w ere
PKH-labeled and infected w ith CVB3 at an MOI o f 10 and cultured fo r 48h before addition to CFSE-labeled DC.
Uptake o f islets eith er mock-infected (M ) or CVB-infected (CVB) was analyzed by flo w cytom etry 24h after
co-culture. (E) Human islets w ere PKH-labeled and infected as in (D) and co-cultured w ith unlabeled DC for
24h. Subsequently, DCs w ere harvested, stained using CD8 6 -specific antibodies (green), and analyzed using
confocal microscopy. (F) Human islets w ere infected w ith CVB3 at an MOI of 10 fo r 48 h prio r to addition
to DCs. Expression o f RIG-I, Mda5 and PKR mRNA in DCs was analyzed using qPCR. (G) Porcine islets w ere
prepared and co-cultured as in (F) and at indicated tim es ISG-induction was analyzed. In some experiments
(F, G) freeze-thawed preparations of islets w ere used, but these yielded sim ilar results compared to using vi
able cells. Experiments are representative of 2, 3 or more than 3 independent experiments. Med = medium,
unstim ulated DCs; Islet/M = mock-infected human islets; Islet/CVB = CVB-infected human islets; porc Islet/M
= m ock-infected porcine islets; porc Islet/CVB = CVB-infected porcine islets.
82
Uptake of ß-cells results in human DC activation
A
Mock
D
C
.\
CVB3
V
'
-,
P'
f
„
DC
M in6
'V
*
^
W
\
DC + M6/CVB
DC + M6/M
/
s
Ir «
r
f 'C
DC + M6/M
DC + M6/CVB
PKH
E
F
IFN-p
RIG-I
Mda5
PKR
*
G
ÍV*
H
J * KV&
RIG-I
- Medium
- po ly I:C
-M 6/M
- M6/CVB
PKR
Mda5
Actin
Figure 2. M in 6 cells are a good m odel fo r prim a ry pancreatic cells, are phagocytosed by DCs and induce
innate a n tiviral im m une responses.
(A and B) M in 6 cells w ere infected w ith CVB3 at an MOI o f 10 and (A) at indicated tim e points replication was
analyzed and (B) at 48h p.i. images w ere taken. (C) M in 6 cells w ere PKH-labeled and infected w ith CVB3 at
an MOI of 10. A fter 24h incubation cells w ere harvested and added to CFSE-labeled DCs at a 1:1 ratio. 24h
after co-culture cells w ere harvested and uptake was determ ined using flo w cytom etry. (D) M in 6 cells were
prepared as in (C) and co-cultured w ith unlabeled DCs fo r 24h, after which DCs w ere harvested, stained as fo r
1E and analyzed using confocal microscopy. (E and F) M in 6 cells w ere prepared as in (C), and after 48h incuba
tion, cells w ere harvested and added to DCs at a 1:1 ratio, or DCs w ere stim ulated w ith 20|ag/ml poly I:C or left
untreated. At (E) 5h after addition, or (F) 5h and 8 h after addition, mRNA induction o f ISGs was determ ined
as described. (G) Protein expression o f RIG-I, Mda5, and PKR was analyzed by w estern blot 24h after stim ula
tion o f DCs as described fo r panel (E). (H) DCs w ere stim ulated as in (E) and after 24h co-culture cells were
harvested and infected w ith EV9 at an MOI of 1. At indicated tim es p.i. EV9 replication was analysed. Poly I:C
was used as a positive control (34). In some experim ents freeze-thawed cell populations w ere used but these
yielded sim ilar results compared to using viable cells (Supplementary figure 1). Data shown are representa
tive (A-D, G, H) or averages (E, F) o f at least 3 independent experiments. Med = m edium, unstim ulated cells;
M 6 /M = mock-infected M in 6 cells; M 6 /CVB = CVB-infected M in 6 cells. * = p < 0.05; n.s. = not significant.
83
Chapter 5
confirmed to express several ß-cell associated mRNAs (e.g. GAD65, IGRP, IA2, insulin,
data not shown). Analogous to human and porcine islets, Min6 cells were susceptible to
infection with CVB3 as shown by the increase in virus titer (Fig. 2A). Cytopathic effects
were observed in nearly 100% of the cells (Fig. 2B), suggesting that the majority of cells
were infected. Uptake of mock- and CVB3-infected Min6 cells by DCs was very efficient
(up to 75%) as shown by flow cytometry and confocal analysis (Fig. 2C and 2D).
Upon engulfment of CVB-infected Min6 cells, IFN-ß and ISGs were strongly
induced in DCs (Fig. 2 E and F), reaching a greater than 100-fold increase compared to
unstimulated DCs in the case of RIG-I, while Mda5 and PKR showed increases of up to
20- and 10-fold, respectively (Fig. 2F). The induction of ISGs following uptake of infected
Min6 cells was confirmed at the protein level by western blotting (Fig. 2G). No ISG signal
was observed in mock- or CVB3-infected Min6 cells alone (data not shown), excluding
that the observed protein induction in DC/Min6 co-cultures is due to detection of Min6
cell proteins. In some experiments, freeze-thawed mock- or CVB-infected cells were
used. This had no effect on either phagocytosis or ISG-induction (Supplementary Fig 1).
IFNs and ISGs induce an antiviral state that restricts virus replication38. To
determine whether upregulation of ISGs following uptake of CVB3-infected Min6 cells
protects DCs from subsequent infection, DCs that had taken up Min6 cells were infected
with EV9, an enterovirus strain that does replicate in DCs28, but not in Min6 cells (data
not shown). Uptake of mock-infected cells had no influence on replication of EV9 in DCs.
In contrast, phagocytosis of CVB-infected Min6 cells strongly protected the DCs from EV9
replication (Fig. 2H).
Innate responses in DC that phagocytosed CVB3-infected Min6 cells depend on
autocrine IFN-a/ß signaling.
ISGs can be upregulated through both IFN-dependent and IFN-independent pathways39,
40. To investigate whether secreted cytokines like IFN-a/ß were involved in ISG induction,
we stimulated fresh DCs with cell-free supernatant from DC/Min6 co-cultures. An
increase in ISGs was observed upon stimulation of DCs with supernatant from co-cultures
of DCs plus CVB-infected Min6 cells, but not of DCs plus mock-infected Min6 cells (Fig.
3A). Moreover, the induction of ISGs after uptake of CVB-infected cells was markedly
reduced in the presence of neutralizing IFN-a/ß antibodies, at both the mRNA level
(Fig. 3B) and protein level (Fig. 3C compare lanes 6 and 7), implying that ISG induction
strongly depends on IFNs.
To determine whether IFNs produced by DCs or the infected Min6 cells were
responsible for ISG upregulation, supernatants from infected Min6 cultures were added
to DCs, after which ISG-induction was monitored. Although recombinant murine IFNa
induced ISG expression in DCs, supernatant of either mock- or CVB-infected Min6 cells
did not (Fig. 3D). Thus cytokines potentially produced by infected Min6 cells are not
responsible for ISG expression in DCs.
Collectively, these data imply that DCs induce an innate immune response upon
uptake of CVB3-infected Min6 cells and that this induction depends on IFN-induction by
DCs themselves.
Induction of ISGs in DCs following uptake of CVB3-infected Min6 cells require endosomal
acidification and recognition of viral RNA.
Both PRRs located on the cell surface and those with intracellular localization may
84
Uptake of ß-cells results in human DC activation
Figure 3. Type I IFNs produced by DC them selves are required fo r ISG indu ction.
(A) DCs were stim ulated w ith cleared supernatants fro m stim ulated DC and D C /M in 6 co-cultures (harvested
24h after co-cultured started and used at a 1:2 dilution) and 8 h after stim ulation mRNA induction o f RIG-I,
Mda5, and PKR were determ ined using qPCR. (B) M in 6 cells were infected w ith CVB3 at an MOI o f 10 and
after 48h incubation cells w ere harvested and added to DCs at a 1:1 ratio. Stimulations were perform ed in
th e absence or presence o f neutralizing antibodies (Iivari, Kaaleppi, and bovine anti-IFN -a/ß; see M aterials
and M ethods). After 8 h, mRNA expression levels o f RIG-I, Mda5, and PKR w ere determ ined using qPCR. (C)
DC w ere treated as in (B) and after 24h protein expression o f RIG-I, Mda5, and PKR was analyzed by western
blotting. (D) DCs were stim ulated w ith 100U /m l mIFNaA o r cleared supernatants fro m M in 6 cells (harvested
48h p.i. and used at a 1:2 dilutio n) and after 8 h ISG mRNA induction was determ ined. Data shown are rep
resentative o f 2 (C), or average o f 3 (A, B, D) independent experiments. Sup = supernatant; Med = medium,
unstim ulated cells; IC = poly I:C; M 6 /M = mock-infected M in 6 cells; M 6 /CVB = CVB-infected M in 6 cells; w /o
Ab or w Ab = w ith o u t or w ith neutralizing anti IFN-a/ß antibodies, respectively; mIFNa = m urine recom binant
IFN-a. * = p < 0.05; n.s. = not significant.
85
Chapter 5
A
B
RIG-I
PKR
RIG-I
RIG-I
*
Mda5
n.s.
*
PKR
n.s.
w/o RNase
w RNase
D
x*
X*
Figure 4. Ind uction o f innate im m une responses in DC a fte r M in 6 /CVB uptake requires (viral) RNA w ith in
M in 6 cells.
(A) DCs were pretreated w ith Cytochalasin D fo r 30 minutes prio r to stim ulation w ith TLR ligands or M in 6
cells. After 8 h, mRNA expression levels o f RIG-I, Mda5, and PKR w ere determ ined using qPCR. (B) DCs were
pretreated w ith chloroquine fo r 30 m inutes, stim ulated as in (A) and mRNA expression was determ ined as in
(A). (C) M in 6 cell preparations were exposed to a m ixture o f RNase A, RNase VI and RNase I prior to addition
to DC cultures as described. Expression o f RIG-I, Mda5 and PKR in DCs was analyzed using qPCR 5h after ad
dition o f M in 6 cell preparations. (D) DCs were co-cultured w ith M in 6 cell preparations as described fo r panel
A, and protein expression o f RIG-I, Mda5, and PKR was analyzed by w estern blotting 24h after th e start o f
co-culture. Data are representative o f 2 (D) or average o f 2 (A, B, C) independent experiments. In these ex
perim ents freeze-thawed cell populations were used. Med = m edium , unstim ulated cells; IC = poly I:C; M 6 /M
= mock-infected M in 6 cells; M 6 /CVB = CVB-infected M in 6 cells; w /o RNase or w RNase = w ith o u t or w ith
RNase-treatment o f M in 6 cell preparations p rio r to co-culture. * = p < 0.05; n.s. = no t significant.
86
Uptake of ß-cells results in human DC activation
mediate the observed responses in DCs. To investigate whether phagocytosis of cells
is required for the induction of ISGs, or whether extracellular exposure to infected cells
might initiate ISG reponses in DCs (e.g. via TLRs on the plasma membrane), phagocytosis
was inhibited using Cytochalasin D (CytD). DCs pretreated with CytD and subsequently
stimulated with CVB3-infected Min6 cells did not show any induction of ISGs, indicating
that phagocytosis is required for ISG-induction. Similar decreases in ISG induction were
observed when using CVB-infected primary porcine islets (data not shown). Poly I:Cinduced ISGs were also reduced upon CytD-treatment, as has been reported before41.
Importantly, LPS induced responses were not abrogated in the presence of CytD, proving
that CytD has no adverse effects on DC viability or ISG-induction (Fig 4A)42.
Phagocytosed cells are localized to so-called phagosomes, which subsequently
"mature" via fusion with the endosomal/lysosomal compartments, followed by
progressive decrease in pH20, 43. Intracellular TLRs (TLR3, 7, 8, 9) are also recruited to
these compartments, enabling interaction with potentially released PAMPs, like dsRNA,
which occurs in a pH-dependent fashion44. Alternatively, phagocytosed material might be
translocated into the cytoplasm, where for example the RLHs (RIG-I, Mda5) can interact
with viral RNA. To determine if endosomal acidification is required for the induction of
ISGs following uptake of infected cell preparations, we pretreated DCs with chloroquine
(CQ), a chemical that blocks acidification of these compartments. Pretreatment of DCs
with CQ markedly decreased CVB-infected Min6-induced mRNA expression of RIG-I, Mda5
and PKR (Fig 4B), suggesting that endosomal acidification is critical for DC reponses upon
phagocytosis of infected cells. Similar decreases in ISG induction were observed when
using CVB-infected primary porcine islets (data not shown). FACS analysis showed that
phagocytosis of Min6 cells was not inhibited due to CQ treatment (data not shown). Poly
I:C induction, known to require endosomal acidification, was also decreased41, 44. LPSinduced responses do not require endosomal acidification41, 44. As expected, LPS-induced
ISG and IL-6 expression was not decreased, indicating that viability and intracellular
signaling to induce cytokines was unaltered upon CQ-treatment (Fig 4B and data not
shown).
Using RNases, we investigated the contribution of (viral) RNA in our CVB-infected
cells to DC responses. For this, freeze-thawed Min6 cell preparations were used, as
viable cells with an intact plasma membrane will make degradation of intracellular RNA
impossible. RNase-treatment of freeze-thawed Min6 cell preparations prior to addition
to DCs reduced upregulation of RIG-I, Mda5 and PKR at both mRNA and protein level
(Fig. 4C and Fig. 4D compare lane 4 and lane 6), demonstrating the important role of viral
RNA present in infected cells for the induction of innate immunity. Together, our data
show that phagocytosis of CVB-infected cells is required, and that subsequent signaling
requires endosomal acidification and depends on the presence of viral RNA.
Discussion
DCs play a critical role in inducing immunity and preventing auto-immunity. Although
diabetes pathogenesis and the possible role of APCs such as DCs therein has been
investigated in mice14, 15, to our knowledge, no studies have been performed that
examined the interaction between islets and DCs in humans. Here, we show for the
first time that CVB-infected human islets are efficiently phagocytosed by human DCs
resulting in a rapid RNA- and IFN-dependent innate antiviral response by the DCs.
87
Chapter 5
The response of DCs was further characterized with use of porcine islets and
murine Min6 cells. Mock-infected cells did not induce innate responses, even though,
surprisingly, their phagocytosis was as efficient. The reason for equal uptake of mockand CVB-infected cells is unknown; islets/ß-cells may display enhanced molecular signals
that mediate phagocytosis ("eat-me signals", such as phosphatidyl serines (PS))45, possibly
caused by ER-stress inherent to massive insulin production 46. Preliminary data revealed
that PS are higher expressed on the outer cell surface of steady-state insulin-producing
Min6 cells when compared to other steady-state cell lines that are not efficiently
phagocytosed (e.g. HeLa, L929, BGM, Vero) (data not shown). Whether PS or other "eatme signals" are present on isolated primary human pancreatic islets, and facilitate their
engulfment requires further investigation. Nevertheless, equal uptake of mock- and
CVB-infected cells enabled us to make a good comparison of DC-responses, because
only the infection status of islets or Min6 cells or islets differed. Phagocytosis of CVBinfected islets and Min6 cells invariably resulted in an increase in ISGs. Importantly, this
IFN-dependent ISG-increase was sufficient to completely protect DCs from subsequent
EV9 infection. This reveals a mechanism by which DCs may protect themselves when
attracted to an environment with ongoing infection, ensuring their functional integrity.
Viral RNA is known to be an important inducer of antiviral immunity by triggering
PRRs from the TLR and RLH family. Here we show that induction of innate responses
in DCs requires endosomal acidification and is largely dependent on the presence of
RNA within the infected cells. Some residual ISG induction is still observed after RNase
treatment. Possibly, part of the RNA might be shielded within intact virus particles, and
therefore be inaccessible for RNases. This residual viral RNA may have triggered ISG
induction, when recognized in endosomes and/or lysosomes following phagocytosis.
Although we favor the idea that viral RNA present in CVB-infected cells triggers antiviral
immunity, we can not exclude that viral proteins or modified host proteins contribute to
the observed antiviral responses.
Interestingly, engulfment of CVB-infected cells resulted in the development
of type 1 diabetes in a susceptible mouse model14. In that study, resident APCs in the
pancreas were shown to engulf CVB-infected ß-cells, and these APCs were capable
to subsequently stimulate antigen-specific T cell proliferation and trigger diabetes,
demonstrating that the (infectious) microenvironment may drive innate, as well as
adaptive and autoimmune responses in vivo. We studied human DC maturation in
vitro and our preliminary data on the induction of costimulatory molecules showed
no consistent upregulation, even though ISG-induction was consistently observed. In
some donors upregulation of CD80 and CD86 and production of TNF-a and IL-12 were
observed in DCs upon uptake of CVB3-infected Min6 cells; however, in the majority of
DC-donors no increases were observed. The reason for these inconsistent outcomes is
unknown and requires further investigation.
Obviously, during phagocytosis of infected cells by DCs in vivo, other cell
populations are present that can interact with DCs. These cells, including macrophages,
plasmacytoid DCs and NK cells, and the cytokines they produce, can greatly influence
the microenvironment and DC responses. For instance, IFNs can, besides their function
in innate immunity, also influence adaptive immunity. The amount of IFNs, timing
of encountering IFNs, but also possible synergy with other PRR-stimuli can greatly
influence DC maturation47, 48. Moreover, other pancreas-constituents, such as duct cells
may influence DC function. For example, duct cells produce TNF-a upon CVB3 infection
88
Uptake of ß-cells results in human DC activation
(G. Vreugdenhil, F. van Kuppeveld J. Galama and D. Pipeleers, unpublished observation),
and duct cell-derived TNF-a has been shown to influence DC maturation49. Further in
depth investigation of adaptive immune responses in DCs from healthy controls upon
encountering CVB-infected islets and the interplay with other cell types and cytokines
would be extremely valuable.
Most human infections with enteroviruses are efficiently controlled due to
adequate antiviral immune responses. Prolonged or successive enterovirus infections
have been suggested to play a role in the development of type 1 diabetes50, 51, raising the
possibility that individuals susceptible for type 1 diabetes may have impaired anti-viral
defense. The genetic background of susceptible individuals greatly influences disease
development. For example, polymorphisms in Mda5, the RNA sensor that recognizes
picornavirus RNA52, have been associated with type 1 diabetes development25,53.
Alterations in Mda5 function may affect adequate sensing of viral infections, and thus
hamper antiviral immunity. CVB-infection in a genetically susceptible individual might
therefore progress to chronic inflammation in the pancreas. In this pro-inflammatory
environment, where self-antigens and viral antigens are encountered by DCs,
autoimmunity might develop or accelerate, ultimately resulting in type 1 diabetes.
In conclusion, we show that CVB-infected human islets, porcine islets and
Min6 cells are phagocytosed by human DCs and that this results in an RNA- and IFNdependent antiviral state in DCs. These events may alter programming of DCs and thus
influence the development of Tregand/or effector T cell populations. These novel findings
provide important new insights in the possible role of DCs during human type 1 diabetes
development.
Acknowledgements
The authors are grateful to Dr Merja Roivainen and Dr Per Bendix Jeppesen for providing
Min6 cells. Furthermore, we thank Dr Paul Fisher and Dr Ilkka Julkunen for providing us
with anti-Mda5 and anti-type I IFN antibodies, respectively. This work was supported
by grants from the Netherlands Diabetes Foundation (DFN 2001.00.047) to J.M.D.G and
G.J.A.; The Netherlands Organization for Scientific Research (NWO-VIDI-917.46.305) to
F.J.M.v.K. and (NWO-912-02-034) to G.J.A; and the Radboud University Medical Centre
Nijmegen (grant number 2005-8) to F.J.M.v.K and J.M.D.G; and the Juvenile Diabetes
Research Foundation (Grant Number: 24-2008-949) to G.J.A and F.J.M.v.K.
89
Chapter 5
References
1.
M . K nip, R. V e ijo la , S. M . V irta n e n , H. Hyoty, O. V aarala, H. K. A k e rb lo m (2005). E n viro n m e n ta l trig g e rs and d e te rm in a n ts o f ty p e 1
d ia b e te s . D ia betes, 54 Suppl 2, S 125-136.
2.
D. R. G a m ble, M . L. Kinsley, M . G. FitzG erald, R. B o lto n , K. W. Taylor (1969). V ira l a n tib o d ie s in d ia b e te s m e llitu s . Br M e d J, 3, 6 2 7
630.
3.
D. R. G am b le , K. W. Taylor, H. C u m m in g (1973). Coxsackie viruses and d ia b e te s m e llitu s . Br M e d J, 4, 260-262.
4.
J. W. Y oon, M . A u s tin , T. O n odera, A . L. N o tkin s (1979). Iso la tio n o f a v iru s fr o m th e pancreas o f a ch ild w ith d ia b e tic ketoacidosis. N
Engl J M e d , 3 00, 1 173-1179.
5.
J. L. W h itto n (2002). Im m u n o p a th o lo g y d u rin g coxsackievirus in fe c tio n . S pringer S em in Im m u n o p a th o l, 24, 201-213.
6.
R. V arela-C alvino, M . Peakm an (2003). E n teroviruses and ty p e 1 d ia b e te s. D iabetes M e ta b Res Rev, 19, 431-441.
7.
H. H yoty, K. W. Taylor (2002). T he role o f viruses in h u m a n dia b e te s. D ia b e to lo g ia , 45, 1353-1361.
8.
F. D o tta , S. C ensini, A. G. van H a lte re n , L. M a rs e lli, M . M a s in i, S. D ionisi, F. M osca, U. Boggi, A . O. M u d a , S. D. Prato, J. F. E llio tt, A.
Covacci, R. R appuoli, B. O. Roep, P. M a rc h e tti (2007). Coxsackie B4 viru s in fe c tio n o f beta cells and n a tu ra l k ille r cell in s u litis in recento n s e t ty p e 1 d ia b e tic p a tie n ts . Proc N atl Acad Sci U S A, 104, 5115-5120.
9.
P. Y lipa asto , K. Klingel, A . M . Lindberg, T. O to n ko ski, R. K andolf, T. H ovi, M . R oivainen (2004). E n te ro viru s in fe c tio n in hum an
p a n c re a tic islet cells, isle t tro p is m in vivo and re c e p to r in v o lv e m e n t in c u ltu re d isle t beta cells. D ia b e to lo g ia , 47 , 225-239.
10.
S. J. R ichardson, A . W illco x, A . J. Bone, A. K. Foulis, N. G. M org a n (2009). T he prevalence o f e n te ro v ira l capsid p ro te in vp1
11.
A . W illc o x , S. J. R ichardson, A. J. Bone, A . K. Foulis, N. G. M o rg a n (2009). A nalysis o f isle t in fla m m a tio n in h u m an ty p e 1 dia b e te s. Clin
12.
J. H. V e lth u is , W. W. Unger, A. R. van d e r Slik, G. D uinkerken, M . Engelse, A . F. S chaapherder, J. Ringers, C. van K ooten, E. J. de Koning,
13.
S. A rif, T. I. Tree, T. P. A s till, J. M . T re m b le , A . J. B ishop, C. M . Dayan, B. O. Roep, M . Peakm an (2004). A u to re a c tiv e T cell responses
im m u n o s ta in in g in p a n cre a tic islets in h um an ty p e 1 dia b e te s. D iabetologia.
Exp Im m u n o l, 155, 173-181.
B. O. Roep (20 09). A c c u m u la tio n o f a u to re a c tiv e e ffe c to r T cells and a llo -s p e c ific re g u la to ry T cells in th e pancreas a llo g ra ft o f a ty p e
1 d ia b e tic re c ip ie n t. D ia b e to lo g ia , 52, 494-503.
s h o w p ro in fla m m a to ry p o la riz a tio n in d ia b e te s b u t a re g u la to ry p h e n o ty p e in h e a lth . J Clin Invest, 113, 451-463.
14.
M . S. H o rw itz , A. Ilic, C. Fine, B. Balasa, N. S a rve tn ick (2004). C oxsackie vira l-m e d ia te d d ia b e te s: in d u c tio n re q u ire s an tig e n -p re s e n tin g
cells and is a c co m p a n ie d by p h a g ocytosis o f beta cells. Clin Im m u n o l, 110, 134-144.
15.
E. D ah len , K. D awe, L. O hlsson, G. H e dlund (1998). D e n d ritic cells and m acrophages are th e firs t and m a jo r p ro d u c e rs o f TNF-alpha
16.
W. Lu, D. G. P ipeleers, G. K loppel, L. B ouw ens (1996). C o m p a ra tive im m u n o c y to c h e m ic a l s tu d y o f M HC class II e xpression in hum an
17.
S. U no, A. Im agaw a, K. O kita , K. Sayama, M . M o riw a k i, H. Iw ahashi, K. Y am agata, S. Tam ura, Y. M a tsu za w a , T. H anafusa, J. M iyagaw a,
18.
J. B a nch ere au , R. M . S teinm an (1998). D e n d ritic cells and th e c o n tro l o f im m u n ity . N a tu re , 392, 245-252.
19.
J. B a nch ere au , F. B riere, C. Caux, J. D avoust, S. Lebecque, Y. J. Liu, B. P ule n d ra n , K. Palucka (2000). Im m u n o b io lo g y o f d e n d ritic cells.
2 0.
J. M . B lander, R. M e d z h ito v (2006). On re g u la tio n o f p h agosom e m a tu ra tio n and a n tig e n p re s e n ta tio n . N at Im m u n o l, 7, 1029-1035.
2 1.
T. Kaw ai, S. A k ira (2006). In n a te im m u n e re c o g n itio n o f viral in fe c tio n . Nat Im m u n o l, 7, 131-137.
2 2.
A . P ichlm air, C. Reis e Sousa (2007). In n a te re c o g n itio n o f viruses. Im m u n ity , 27, 370-383.
in p a n c re a tic islets in th e n o n obese d ia b e tic m ouse. J Im m u n o l, 160, 3 585-3593.
d o n o r pancreas and isolated islets. V irch o w s A rch , 429, 205-211.
I. S h im o m u ra (2007). M a cro p h a g e s and d e n d ritic cells in filtra tin g islets w ith o r w ith o u t beta cells pro d u ce tu m o u r necrosis fa c to r
alp ha in p a tie n ts w ith re ce n t-o n se t ty p e 1 diabetes. D ia b e to lo g ia , 50, 596-601.
A n n u Rev Im m u n o l, 18, 767-811.
2 3.
S. Y. Zhang, E. Jouanguy, S. U g o lin i, A. Sm ahi, G. Elain, P. R om ero, D. Segal, V. S ancho-S him izu, L. Lorenzo, A . Puel, C. Picard, A.
C hapgier, S. P lanco u la in e , M . T ite u x , C. C ognet, H. vo n B e rn u th , C. L. Ku, A. C asrouge, X. X. Zhang, L. B a rre iro , J. Leonard, C. H a m ilto n ,
P. Lebon, B. H eron, L. Vallee, L. Q u in ta n a -M u rc i, A . H ovn a n ia n , F. R ozenberg, E. V ivier, F. G eissm ann, M . Tardieu, L. A b e l, J. L. Casanova
(2 00 7). TLR3 d e fic ie n c y in p a tie n ts w ith h erpes s im p le x e n c e p h a litis . Science, 317, 1522-1527.
2 4.
Y. O g ura , D. K. B onen, N. Ino h a ra , D. L. N icolae, F. F. C hen, R. Ram os, H. B ritto n , T. M o ra n , R. Karaliuskas, R. H. Duerr, J. P. Achkar,
S. R. B ran t, T. M . Bayless, B. S. Kirschner, S. B. Hanauer, G. N unez, J. H. Cho (2001). A fra m e s h ift m u ta tio n in NOD2 associated w ith
s u s c e p tib ility to C rohn's disease. N a tu re , 411, 603-6 0 6 .
2 5.
D. J. S m yth , J. D. Cooper, R. Bailey, S. Field, O. B u rre n , L. J. Sm ink, C. G uja, C. Ionescu -T irg o viste , B. W id m e r, D. B. Dunger, D. A. Savage,
N. M . W alker, D. G. C la yto n , J. A. Todd (2006). A g e n o m e -w id e a ssociation s tu d y o f n o n syn o n ym o u s SNPs id e n tifie s a ty p e 1 d iabetes
locus in th e in te rfe ro n -in d u c e d helicase (IFIH1) re g io n . N at G e n e t, 38, 617-619.
2 6.
P. F itzgerald-B ocarsly, D. Feng (2007). The role o f ty p e I in te rfe ro n p ro d u c tio n by d e n d ritic cells in host defense. B io ch im ie , 89 , 8 4 3
855.
2 7.
K. S. Lang, M . Recher, T. Junt, A . A . N ava rin i, N. L. H arris, S. Freigang, B. O d e rm a tt, C. C onrad, L. M . Ittn e r, S. Bauer, S. A. Luther, S.
U e m a ts u , S. A kira, H. H eng a rtn e r, R. M . Zinkernagel (2005). Toll-like re c e p to r e n g a g e m e n t co n v e rts T-cell a u to re a c tiv ity in to o ve rt
a u to im m u n e disease. N at M e d , 11, 138-145.
28.
M . Kram er, B. M . S chulte, L. W. Toonen, M . A. de B ru ijn i, J. M . G alam a, G. J. A d e m a , F. J. van K uppeveld (2007). E chovirus in fe c tio n
causes rapid lo s s -o f-fu n c tio n and cell d e a th in h um an d e n d ritic cells. Cell M ic ro b io l, 9, 1507-1518.
29.
R. B o ttin o , A. N. B ala m u ru g a n , H. Tse, C. T h iru n a vu kka ra su , X. Ge, J. P rofozich, M . M ilto n , A. Ziegenfuss, M . Trucco, J. D. Piganelli
30.
A. N. B ala m u ru g a n , Y. C hang, J. J. Fung, M . Trucco, R. B o ttin o (2003). F lexible m a n a g e m e n t o f e n z y m a tic d ig e s tio n im proves hum an
3 1.
A . N. B a la m urugan, Y. Chang, S. B e rte ra , A . Sands, V. Shankar, M . Trucco, R. B o ttin o (2006). S u ita b ility o f h u m a n ju v e n ile pancreatic
3 2.
J. M iy a z ak i, K. A ra ki, E. Yam ato, H. Ikegam i, T. A sano, Y. Shibasaki, Y. O ka, K. Yam am ura (1990). E stablishm ent o f a p a n cre a tic beta cell
(2004). R esponse o f h um an islets to is o la tio n stress and th e e ffe c t o f a n tio x id a n t tre a tm e n t. D iabetes, 53, 2 559-2568.
is le t is o la tio n o u tc o m e fro m su b -o p tim a l d o n o r pancreata. A m J T ra n sp la n t, 3, 1135-1142.
islets fo r clin ic a l use. D ia b e to lo g ia , 49 , 1845-1854.
lin e th a t re ta in s g lu c o s e -in d u cib le insulin se c re tio n : special re fe re n ce to expression o f glucose tra n s p o rte r iso fo rm s. E ndocrinology,
127, 126-132.
3 3.
K. E. M o g e n s e n , L. Pyhala, K. C antell (1975). Raising a n tib o d ie s to h um an le u k o c y te in te rfe ro n . A cta P athol M ic ro b io l Scand [B ], 83,
44 3 -4 5 0.
3 4.
M . Kram er, B. M . S chulte, L. W. T oonen, P. M . Barral, P. B. Fisher, K. H. Lanke, J. M . G alam a, F. J. van Kuppeveld, G. J. A d e m a (2008).
P hagocytosis o f p ic o rn a v iru s -in fe c te d cells induces an R N A -d e p e n d e n t a n tiv ira l sta te in h um an d e n d ritic cells. J V iro l, 82 , 2 9 3 0
2937.
3 5.
E. W essels, D. D uijsings, T. K. N iu, S. N e u m a n n , V. M . O o rsch o t, F. de Lange, K. H. Lanke, J. K lu m p e rm a n , A . H enke, C. L. Jackson, W. J.
M e lc h e rs , F. J. van Kuppeveld (2006). A viral p ro te in th a t blocks A rf1 -m e d ia te d COP-I a ssem bly by in h ib itin g th e g uanine n u cle o tid e
exchange fa c to r GBF1. Dev Cell, 11, 191-201.
36.
M . R oivainen, P. Y lipaasto, C. S avolainen, J. G alam a, T. Hovi, T. O to n ko ski (2002). F u n ctio n a l im p a irm e n t and k illin g o f h um an beta
cells by e n te ro v iru s e s : th e c a p a city is s hared by a w id e range o f se ro typ e s, b u t th e e x te n t is a c h a ra c te ris tic o f in d iv id u a l virus strains.
90
Uptake of ß-cells results in human DC activation
D ia b e to lo g ia , 45 , 693-702.
37.
M . R oivainen, P. Y lipaasto, J. U stinov, T. H ovi, T. O to n ko ski (2001). S creening e n te ro v iru s e s fo r beta-cell tro p is m using fo e ta l porcine
38.
C. E. S am uel (2001). A n tiv ira l a c tio n s o f in te rfe ro n s . Clin M ic ro b io l Rev, 14, 7 7 8 -8 0 9 , ta b le o f co n te n ts.
39.
J. S. Y o unt, T. M . M o ra n , C. B. Lopez (2007). C yto k in e -in d e p e n d e n t u p re g u la tio n o f M D A 5 in vira l in fe c tio n . J V iro l, 81, 7 316-7319.
40.
J. Di D om izio, A. B lum , M . G a lla g h e r-G a m b a re lli, J. P. M o le n s, L. C h a p e ro t, J. Plum as (2009). TLR7 s tim u la tio n in h u m a n p la sm acytoid
b eta -c e lls. J Gen V iro l, 82 , 1 909-1916.
d e n d ritic cells leads to th e in d u c tio n o f e a rly IF N -in d u cib le genes in th e absence o f ty p e I IFN. B lood.
41 .
K. Ito h , A . W a ta n a b e , K. Funam i, T. Seya, M . M a ts u m o to (2008). The c la th rin -m e d ia te d e n d o c y tic p a th w a y p a rtic ip a te s in dsRNAin d u ce d IFN -beta p ro d u c tio n . J Im m u n o l, 181, 5522-5529.
42.
D. P ie tre lla , C. C orbucci, S. P erito, G. B istoni, A. V e cch ia re lli (2005). M a n n o p ro te in s fro m C ryptococcus n e o fo rm a n s p ro m o te
d e n d ritic cell m a tu ra tio n and a ctiv a tio n . In fe c t Im m u n , 73, 8 2 0-827.
43 .
L. R am a chandra, D. S im m ons, C. V. H arding (2009). M HC m o le cu le s and m ic ro b ia l a n tig e n processing in phagosom es. C urr O pin
44.
O. de B o u te ille r, E. M e rc k , U. A. Hasan, S. H ubac, B. B enguigui, G. T rin c h ie ri, E. E. Bates, C. Caux (2005). R ecognition o f d o u b le
Im m u n o l, 21, 98-104.
s tra n d e d RNA by h u m an to ll-lik e re c e p to r 3 and d o w n s tre a m re c e p to r sign a lin g re q u ire s m u ltim e riz a tio n and an a cidic pH. J Biol
C hem , 280, 38133-3 8 1 4 5 .
45 .
K. S. R a vichandran, U. Lorenz (2007). E n g u lfm e n t o f a p o p to tic cells: signals fo r a good m eal. N at Rev Im m u n o l, 7, 964-974.
46 .
D. L. E izirik, A. K. C ardozo, M . C nop (2008). The role fo r e n d o p la s m ic re tic u lu m stress in d ia b e te s m e llitu s . E ndocr Rev, 29, 42-61.
47 .
T. N agai, O. D evergne, T. F. M u e lle r, D. L. Perkins, J. M . van Seventer, G. A. van S eventer (2003). T im in g o f IFN -beta e xposure d u rin g
h um a n d e n d ritic cell m a tu ra tio n and naive Th cell s tim u la tio n has co n tra s tin g effe cts on Th1 subset g e n e ra tio n : a ro le fo r IFN-betam e d ia te d re g u la tio n o f IL-12 fa m ily cy to k in e s and IL-18 in naive Th cell d iffe re n tia tio n . J Im m u n o l, 171, 5233-5243.
48.
J. W alker, D. F. Tough (2006). M o d ific a tio n o f TLR -induced a c tiv a tio n o f h u m a n d e n d ritic cells by ty p e I IFN: syn e rg istic in te ra c tio n
w ith TLR4 b u t n o t TLR3 agonists. Eur J Im m u n o l, 36, 1827-1836.
49 .
B. M o v a h e d i, M . Van d e C asteele, N. C aluw e, G. Stange, K. B re ckp o t, K. T h ie le m a n s, G. V re u g d e n h il, C. M a th ie u , D. P ipeleers (2004).
H u m an p a n cre a tic d u c t cells can pro d u ce tu m o u r necrosis fa c to r-a lp h a th a t dam ages n e ig h b o u rin g beta cells and a ctiva te s d e n d ritic
c e lls. D ia b e to lo g ia , 47, 9 98-1008.
50.
M . O ik a rin e n , S. T au ria in e n , T. H onkanen, S. O ika rin e n , K. V u o ri, K. K aukinen, I. R antala, M . M a ki, H. H y o ty (2008). D e te ctio n of
e n te ro v iru s e s in th e in te s tin e o f ty p e 1 d ia b e tic p a tie n ts . Clin Exp Im m u n o l, 151, 71-75.
51.
K. K. S a lm inen, T. V u o rin e n , S. O ika rin e n , M . H e lm in e n , S. S im ell, M . Knip, J. Ilo n e n , O. S im ell, H. H y o ty (2004). Iso la tio n o f e n te ro v iru s
stra in s fr o m c h ild re n w ith p re clin ica l Type 1 dia b e te s. D ia b e t M e d , 21, 156-164.
52.
L. G itlin , W. B archet, S. G ilfilla n , M . Cella, B. B eutler, R. A . Flavell, M . S. D ia m o n d , M . C olonna (2006). Essential role o f m d a -5 in ty p e I
IFN responses to p o ly rib o in o s in ic :p o ly rib o c y tid y lic acid and e n c e p h a lo m y o c a rd itis p ic o rn a viru s. Proc N a tl Acad Sci U S A , 103, 8 4 5 9
8 46 4.
53.
S. Liu, H. W ang, Y. Jin, R. Podolsky, M . V. Reddy, J. P edersen, B. B ode, J. Reed, D. S teed, S. A n d e rs o n , P. Yang, A . M u ir, L. Steed, D.
H o p kin s, Y. H uang, S. P u ro h it, C. Y. W ang, A . K. Steck, A . M o n te m a ri, G. E ise n b a rth , M . Rewers, J. X. She (2009). IFIH1 p o ly m o rp h is m s
a re s ig n ific a n tly associated w ith ty p e 1 d ia b e te s and IFIH1 gene expression in p e rip h e ra l b lo o d m o n o n u c le a r cells. H um M o l G enet,
18, 35 8-365.
91
Chapter 5
A
Live M in6
M in6 lysate
M in6 cells
10
LL
u
DC + M in 6 /M
DC + Min6/CVB
B
PKH
RIG-I
PKR
Mda5
15h
]8 h
L í .n
* V
/s
/
'/ / s
/
*
/' / s
/
S upplem entary Figure 1. Uptake o f and response to live M in 6 cells and freeze-thaw ed M in 6 cell lysate by
DCs is com parable.
(A) M in 6 cells were PKH-labeled and infected w ith CVB3 at an MOI o f 10 and cultured fo r 48h before addi
tion to CFSE-labeled DC in a 1:1 ratio. Alternatively, labeled, infected M in 6 cells were harvested 48h p.i. and
stored at -20°C. Subsequently, these freeze-thawed cell lysates were added to CFSE-labeled DCs in a 1:1
ratio. Uptake o f islets either mock-infected (M in 6 /M ) or CVB-infected (M in 6 /CVB) M in 6 was analyzed by flo w
cytom etry 24h after co-culture. (B) Live, infected M in 6 cells o r infected M in 6 cell lysates were added to DCs as
in (A). Expression o f RIG-I, Mda5 and PKR mRNA in DCs was analyzed using qPCR at 5 and 8 h after coculture.
92
Chapter 6
Cytokine and chemokine
production by human pancreatic
islets upon enterovirus infection
Barbara M. Schulte, Kjerstin H.W. Lanke, Jon D. Piganelli,
Rita Bottino, Massimo Trucco, Richard J. Huijbens,
Timothy R.D.J. Radstake, Gosse J. Adema, Jochem
M.D. Galama and Frank J.M. van Kuppeveld
M a n uscript in preparation
Chapter 6
Abstract
nteroviruses, such as coxsackie B viruses (CVB) and echoviruses (EV), have
been implicated as environmental factors that may trigger or accelerate type
1 diabetes, but the underlying mechanism remains elusive. The aim of this
study was to gain insight into the antiviral responses that are generated by primary
human pancreatic islets upon enterovirus infection. Upon CVB-infection, transcription
of interferons and interferon-stimulated genes was induced, and also mRNA of several
different cytokines and chemokines was upregulated. Analysis of secreted cytokines
and chemokines revealed that a variety of pro-inflammatory cytokines is produced,
such as interleukin (IL) 8, IL-6 and tumor necrosis factor-a (TNF-a). Also chemotactic
proteins such as interferon-inducible protein 10 (IP-10) were produced. UV-inactivated
CVB did not induce any responses, suggesting that replicating virus is a prerequisite for
antiviral responses. The double-stranded RNA (dsRNA) analog poly I:C induced a partially
overlapping cytokine response, implying that dsRNA generated during CVB infection may
be the trigger that initiates antiviral responses. These data provide insight in antiviral
responses of human islets, and may shed light on the underlying mechanisms of virusinduced type 1 diabetes.
E
94
Cytokine production in enterovirus-infected human islets
Introduction
Type 1 diabetes is an endocrine disorder in which the pancreatic beta cells in the islets
of Langerhans are gradually destroyed. The aetiology of the disease is not completely
understood; however, it is known that both genetic and environmental factors play a role1.
Inflammation is observed in the islets of type 1 diabetes patients and may mediate ß-cell
dysfunction and cell death, thereby contributing to diabetes development (reviewed by
Eizirik et al.2). In addition, autoimmune responses against ß-cell constituents are found
in the majority of type 1 diabetes cases, and this may further add to type 1 diabetes
development.
Enterovirus infections, especially with human enterovirus B species (HEV-B,
such as coxsackie B viruses (CVB) and echoviruses (EV)), are implicated as environmental
factors that may trigger or accelerate type 1 diabetes3, 4. Enteroviruses are small non
enveloped single-stranded RNA viruses with a lytic life cycle. Infections are common
and usually mild; however, during severe infections virus can spread to secondary target
organs such as the pancreas, brain and heart5, 6. Recently, we have shown that HEVBs interact with dendritic cells (DCs) and influence DC function7, 8. Several studies have
reported HEV-B detection in the pancreatic islets of type 1 diabetes patients at autopsy,
providing evidence that these viruses are able to infect beta cells in vivo9-11. Consistently,
human pancreatic islets can be infected with several different species of enteroviruses
in vitro12.
Upon infection, type I interferons (IFNs) are produced as a first line of antiviral
defense. They bind to the IFN receptors in a paracrine and autocrine fashion and thereby
induce a signaling cascade which results in the production of several IFN-stimulated
genes (ISGs). Among these are transcription factors such as interferon regulatory
factor 7 (IRF-7), which mediate induction of antiviral proteins. Furthermore, effector
proteins, such as 2'-5'oligoadenylate synthethase 1 (OAS1) and RNA-dependent protein
kinase (PKR), which are involved in degradation of viral RNA and translation inhibition,
respectively. In addition, also RNA sensors, such as melanoma differentiation-associated
gene 5 (Mda5) and retinoic acid-inducible gene I (RIG-I), that recognize viral RNA and
subsequently induce antiviral responses are induced. Besides IFNs, also other cytokines
may be induced.
Cytokines can have harmful effects on ß-cell viability13, 14, and furthermore
trigger and maintain inflammation and infiltration of immune cells into pancreatic islets.
Tumor necrosis factor a (TNF-a) and interleukin 1ß (IL-1ß) are pro-inflammatory cytokines
which are detected in the islets of type 1 diabetes patients at autopsy15. Furthermore,
also interferon-a (IFN-a) and interferon-inducible protein 10 (IP-10) can be found in
islets of type 1 diabetes patients, but not in islets from controls16, 17. These inflammatory
mediators may be involved in the etiology of type 1 diabetes.
Little is known about cytokine production and secretion upon enterovirus
infection in islets. In this study, we show that a broad array of cytokines is produced and
secreted upon CVB3 infection. We further showed that virus replication is required for
cytokine production and investigated what triggers may mediate cytokine production.
95
Chapter 6
Research Design and Methods
Virus stocks and purification
CVB3 Nancy (CVB) and CVB4 Edwards2 w ere kindly provided by R. Kandolf (University o f Tübingen, Germany)
and J.W. Yoon (University o f Calgary, Canada), respectively. Production o f virus stocks and virus titra tions were
perform ed on buffalo green monkey cells as described previously7. Serial 10-fold dilutions were tested in 96well m icro titer plates and fifty percent Tissue Culture Infective Doses (TCID50) were calculated as described
before18.
Human islet culture
Human pancreatic islets w ere isolated in Pittsburg as described before19. Human islets were obtained from
deceased anonymous donors procured by CORE (Center fo r Organ recovery and Education, Pittsburgh),
and islets were isolated using a m odification o f the sem iautom ated m ethod described by Ricordi19, 20. Islets
batches used in this study w ere obtained fro m 8 adult pancreas donors, cultured fo r a m inim um o f 3 to 6
days in CMRL-1066 m edium containing 10% fetal calf serum, 2 m M L-glutamine, 100U /m l penicilin, 0.1m g/m l
streptom ycin (Complete CMRL), at 37°C in an atm osphere o f 5% CO2. Islet viability was estim ated by dual
fluorescence viability dyes (Calcein-AM and Propidium Iodide, Invitrogen, Eugene, OR) and was higher than
80% in all batches.Glucose stim ulated insulin release was carried o u t by dynamic perifusion21. A fter culture for
3 to 6 days th e islets w ere sent to Nijmegen as fre e-flo ating islets and cultured in Complete CMRL in ultra low
attachm ent culture plates (Corning) at 37°C in 5% CO2. Islets w ere cultured in Nijmegen fo r maxim um 2 days
before start o f th e experiments,
Infection of human pancreatic islets
Human pancreatic islets were infected in a small volum e o f Complete CMRL, at indicated m u ltip licity of
infection (MOI) fo r 1 h at 37°C. Subsequently, cells were washed 3 tim es in PBS and cultured in Complete
CMRL. For replication analysis, viral titers w ere determ ined at different tim e points post infection (p.i.) as
described above. At indicated times p.i. cells and supernatant were harvested fo r RNA isolations and cytokine
detection, respectively.
RNA isolation
Total RNA was isolated fro m islets using TRIZOL reagent (Invitrogen Life Technologies) according to
m anufacturer's instructions, w ith m inor m odifications. The reverse transcription reaction was perform ed using
M oloney m urine leukemia virus (MMLV) reverse transcriptase (Invitrogen) according to th e m anufacturer's
instructions. For each sample a "-RT" control was included in which th e reverse transcriptase was replaced by
DEPC treated water. The cDNA was stored at -20°C until fu rth e r use.
Quantitative PCR
Q uantitative analysis o f gene expression in islets was done using SYBR Green based qPCR. The qPCR reactions
w ere perform ed in a 20 ^l volum e containing: 10 ^ l SYBR Green m ix (Roche), 1.5 ^l forw ard/reverse prim er
(300 nM endconcentration), 2 |il m illi-Q and 5 |il cDNA dilution. Reactions w ere perform ed on a LightCycler 480
(Roche). Analysis was done using LightCycler 480 Software (LC480 SW Version 1.5, Roche). Primer sequences
are available upon request and were designed using th e freely accessible Primer Bank program 22.
Cytokine detection
Supernatant o f islet cultures were harvested at indicated tim es p.i., and stored at -20°C. Prior to cytokinemeasurements, supernatants were filtered using M icrocon Centrifugal filte r devices w ith a cut-off value of
100 KDa (M illipore) according to m anufacturer's instructions, in order to remove infectious virus, but retain
th e cytokines and chemokines (which have a maxim um size o f approx 30 KDa). Microcons were washed w ith
200^l Complete CMRL once, before applying th e supernatants. Cytokine levels w ere measured and analysed
using th e Bio-Plex system and a 27-plex lum inex kit (Bio-Rad Laboratories) and data analysis was perform ed
w ith Bio-Plex Manager software (Bio-Rad Laboratories). Luminex 27-plex included the fo llow in g cytokines and
chemokines: IL-1ß, IL-1Ra, IL-2, IL-4, IL-5, IL-6 , IL-7, IL-8 , IL-9, IL-10, IL-12p70, IL-13, IL-15, IL-17, eotaxin, bFGF,
96
Cytokine production in enterovirus-infected human islets
G-CSF, GM-CSF, IFN-y, IP-10, MCP-1, MIP-1a, MIP-1ß, GG-BDGF, RANTES, TNFa and VEGF.
Statistical analysis
Statistical analysis was perform ed using a paired Student's t test (tw o-tailed distribution) on 10log transform ed
lum inex data sets. A p-value >0.05 was considered a significant difference.
A
B
— ■ — Mock
CVB3
UV CVB 3
■
IL-18
-A
Mock
CVB3
- UV CVB3
IL-15
0
12
24
36
48
0
12
24
36
48
Figure 1. mRNA indu ction o f various a n tivira l genes, cytokines and chem okines in hum an pancreatic islets
upon CVB3 infe ction.
(A) Human islets w ere infected w ith an MOI o f 10 and at indicated tim es p.i. virus titers were determ ined
by endpoint titra tio n . (B) Human islets were infected w ith CVB3 or UV-inactivated CVB3 at an MOI o f 10, or
were mock infected and at indicated tim es mRNA induction o f IFN-ß, RIG-I, MDA5, IRF7, OAS1 and PKR was
determ ined using qPCR. (C) mRNA induction o f IL-6 , IL-8 , IL-1ß, IFN-y, IL-18, IP-10, RANTES, MIP-1ß, MCP-1
and IL-15 was determ ined by qPCR in islets infected as in B.
Results
mRNA expression in human pancreatic islets upon enterovirus infection
To study the islet responses upon enterovirus infection, we infected islets with CVB3 and
determined expression of IFN-ß and ISGs. Replication of CVB3 in primary human islets
was very efficient, as indicated by the rapid increase of virus titer over time (Fig. 1A)
and the induction of cytopathic effects (CPE, data not shown). Quantitative PCR (qPCR)
revealed that IFN-ß was induced 24h p.i. and further increased over time. All ISGs tested
were induced, at varying levels. The highest induction was observed for OAS1; up to
100-fold increase at 48 h p.i., whereas other ISGs showed increases of 20- to 40-fold
at 48 h p.i. (Fig. 1B). Although ISGs were induced upon infection in all experiments, the
magnitude of the responses varied greatly between individual donors (e.g. range 8 - 99
times increase of OAS1 in 5 donors at 48 h p.i.).
97
Chapter 6
To further study innate immune responses, we examined expression of a
selection of cytokines and chemokines that might be induced upon infection. We found
that mRNA expression of several genes was induced. Interferon-inducible protein 10
(IP-10) induction was most pronounced in all donors, up to 1000-fold increases were
observed compared to mock-infected islets. Also RANTES (Regulated upon Activation
Normal T-cell Expressed and Secreted) expression was strongly induced, whereas other
genes were induced at lower levels (MIP-1ß, MCP-1, IL-1ß, IL-6, IL-8), or were hardly
induced at all (IFN-y, IL-15, IL-18) (Fig. 1C).
To study whether replicating virus is required for antiviral responses, UVinactivated CVB3 was used to infect islets in parallel. UV-inactivated virus did not replicate
and no CPE was induced (data not shown). None of the ISGs, cytokines or chemokines
tested showed any mRNA increase with inactivated virus; indicating that replication is a
requirement for antiviral gene induction (Fig. 1B &1C).
Several cytokines and chemokines are produced upon infection with CVB3.
The amount of gene transcription does not necessarily relate to the amount of
synthesized, or bioactive protein. Several cellular mechanisms are operating which
regulate translation of mRNAs. Additionally, for some cytokines, such as IL-1ß, a posttranslational modification/processing is required to yield bioactive protein. Moreover, in
the case of enterovirus infection, viral proteases are able to suppress cellular translation.
These proteases are known to cleave cellular factors and may thus also cleave the
produced cytokines and chemokines. Therefore, we set out to investigate the amount
of secreted cytokines and chemokines in supernatant of mock- or CVB3-infected islet
cultures. Because very limited information is available regarding cytokine and chemokine
production by enterovirus-infected islets, we chose to investigate a broad range of
cytokines and chemokines using a luminex 27-plex bead-assay (Biorad). We determined
cytokine expression in mock- or CVB-infected islets at 48 h p.i. in four different
experiments using islets from different donors. Various cytokines and chemokines were
detected in the supernatant of human islets. Mock-infected islets produced relatively
high basal levels (more than 1ng/ml) of IL-6, IL-8, MCP-1, VEGF and some IL-10 (Fig. 2 and
supplementary table 1). Upon CVB3-infection pro-inflammatory cytokines (e.g. IL-1ß, IL6, TNF-a) were induced. IL-6 production was most pronounced (>10 ng/ml in all donors)
and TNF-a production reached approximately 1 ng/ml for all donors. IL-1ß production
was increased, yet cytokine levels remained low (below 100 pg/ml for all donors). IFN-y,
a Th1 cytokine which also has antiviral properties, was induced, whereas production of
the Th1-inducer IL-12 was not increased upon infection. Of the Th2-associated cytokines,
IL-4 was increased upon infection, yet the concentration remained low (below 200 pg/
ml for all donors). IL-5 and IL-13 were not induced upon infection at all. Also the anti
inflammatory IL-10 was not induced. Several of the chemokines tested were increased
(IP-10, RANTES, IL-8, MIP-1a, eotaxin). IP-10 showed the most pronounced induction of
all cytokines and chemokines tested; 20 to 100-fold increases were observed, depending
on the donor. This confirmed our qPCR data, which also showed highest increases for
IP-10. IL-8 showed a substantial increase and was produced at highest levels (up to 200
ng/ml). Notably, MCP-1, that was already produced in mock-infected islets, did not show
obvious increases in all donors. Several growth factors were included in the analysis and
a striking increase was observed for G-CSF. Other growth factors such as PDGF and GMCSF were not significantly increased and VEGF even showed a minor decrease.
98
Cytokine production in enterovirus-infected human islets
IL-1ß
IL -6
*
TNF-a
*
Experim ent 1
100000:
Pro.
inflam matory
■Experim ent 2
-A -
10000:
Experim ent 4
1000:
IFN-y
*
10000 _ , A
A n tiv ira l/
Chemokine
10000
100
IP-10
RANTES
*
100000
1000
10000
100
1000
IL -8
eotaxin
MIP-1a
**
*
10000
IT
Experim ent 3
10000
1000
1000
100
100
Chemokine
IL-4
IL-5
*
-
Th2
V
100
Various
10000
''
10
1000
IL-9
ns
f
i • •A
T—----- —▼
10
10000
1000
IL-17
ns
É P -y ;^ ê
1000
100
G-CSF
10000
ns
ns
10000
100
VEGF
100000
100000
100
IL-7
1000
IL-10
ns
1000
IL-Ra
**
*
10000
Various
Mock
CVB3
Mock
CVB3
Mock
CVB3
Figure 2. Human islets produce various cytokines and chem okines upon CVB3 infe ction.
Human islets w ere mock or CVB3-infected w ith an MOI o f 10 and at 48h p.i. supernatant was harvested and
analyte-levels were determ ined as described. Data shown are fro m 4 different experim ents using different
donors. All values are in pg/m l. ns, no t significant; *, p-value >0.05; * * , p-value >0.01.
In short, many pro-inflammatory cytokines and chemokines were induced upon
CVB-infection of human pancreatic islets, as well as Thl-associated IFN-y, whereas no or
little Th2 and anti-inflammatory cytokines were induced.
Kinetics of cytokine induction follow replication kinetics.
To further study the kinetics of virus-induced cytokines and chemokines production,
a more detailed analysis of cytokines and chemokines produced at several times p.i.
was performed. This revealed that most CVB-induced cytokines were hardly induced
at 8h p.i., but were increased at 24h p.i. and further increased 48h and 72h p.i. (Fig.
3). This increased cytokine production follows the increases in virus titer, although
cytokine production further increases up to 72 h p.i., whereas virus replication reaches
a maximum at 48h p.i. Comparison of cytokine secretion with mRNA induction kinetics
99
Chapter 6
IL-6
1000
A"
IL-8
.#10000
100
1000
0 12 24 36 48 60 72
0 12 24 36 48 60 72
IP-10
RANTES
100
----A__
IL-15
100
10
Time (h p.i.)
■Mock
-
#
-C V B 3
- - A - - UV CVB3
CVB4 E2
Time (h p.i.)
Figure 3. C ytokine productio n in CVB3, CVB4 E2, and UV-inactivated CVB-infected islets.
Human islets were infected w ith CVB3, UV-inactivated CVB3 or CVB4 E2 w ith an MOI o f 10, or were mockinfected. At indicated tim es p.i. supernatant was harvested and analyte-levels were determ ined as described.
Shown are IL-6 , IL-8 , IP-10, RANTES, MCP-1 IL-15 and G-CSF. Values in pg/m l.
in the corresponding donor, revealed that the continuous increase in cytokines and
chemokines is found at both mRNA and protein level for most genes/proteins (data not
shown) with the exception of IP-10. mRNA levels of IP-10 were already at maximum
levels around 24h p.i. and showed a decrease afterwards (Fig. 1C).
CVB3 and CVB4 induce the same cytokine pattern upon infection of pancreatic islets.
HEV-Bs are the viruses which are most often associated with T1D and include six
different CVBs and several echoviruses. Among the CVBs is the CVB4 Edwards 2 (CVB4
E2) strain that was isolated from the pancreas of a type 1 diabetes patient and is
therefore considered to be more "diabetogenic" compared to other CVBs23. To asses
whether different responses were generated upon infection with a different serotype,
we compared CVB3-induced responses to CVB4 E2-induced responses.
Similar cytokine patterns were induced by both CVB3 and CVB4 E2, although
the magnitude of the induction and the kinetics were somewhat different between the
two. CVB4 E2-induced responses were a little reduced compared to CVB3, and induced
rather later for some cytokines (Fig. 3). The observed differences might be due to minor
variation in amount of virus or replication kinetics. UV-inactivated virus did not induce
100
Cytokine production in enterovirus-infected human islets
cytokines and chemokines at any of the time points tested (Fig. 3), corroborating our
qPCR data and providing further proof that viral replication is a prerequisite for induction
of antiviral responses in human pancreatic islets. When using UV-inactivated virus, it
is unknown whether virus entry and RNA release occur. Using the compound AG7404,
we further dissected whether virus entry or replication is a prerequisite for cytokine
induction. AG7404 was recently discovered to inhibit enterovirus replication, but does
not inhibit virus entry, RNA release, or translation. AG7404 completely abolished CVB3
replication in islets (data not shown). No CVB3-induced cytokine production was observed
in islets in the presence of AG7404 (data not shown). This further confirms that virus
replication is required for cytokine induction, and indicates that viral RNA release and
translation are not sufficient to induce cytokines and chemokines in pancreatic islets.
CVB-induced cytokines may be induced by dsRNA and IFNs
The enterovirus genome is a single-stranded RNA strand of positive polarity. During
replication, viral replication proteins are involved in the replication of viral RNA.
Replication starts with synthesis of a negative strand, giving rise to the double-stranded
(ds) RNA intermediate. Negative strands are subsequently used as a template for the
production of new positive strands, again giving rise to dsRNA intermediates. dsRNA is
Time (h p.i.)
Figure 4. C ytokine indu ction by p o ly I:C and recom bin ant hum an IFN-a2.
Human islets were stim ulated w ith poly I:C (100^g/m l), or recom binant human IFNa2 (150 U /m l) and at
indicated tim es cytokines were determ ined as fo r Fig 3. Shown are IL-6 , IL-8 , IP-10, RANTES, MCP-1 IL-15 and
G-CSF. Values in pg/m l.
101
Chapter 6
a known ligand for several pattern recognition receptors (e.g. Toll-like receptor 3, TLR3;
Mda5), and induces the production of type I IFNs. We set out to investigate the response
of islets to dsRNA and IFN-a. Therefore, we determined responses induced by poly I:C, a
dsRNA analog, or by recombinant human IFNa2.
Addition of poly I:C (100^g/ml) to the culture medium gave rise to increased
IL-6, IL-8, IP-10 and RANTES production in islets, similar to viral infection. In contrast, no
G-CSF was produced after poly I:C stimulation. IL-15 and MCP-1, that were only slightly
induced upon infection, were markedly increased after poly I:C stimulation (Fig. 4). This
suggests that the receptors and downstream signaling pathways involved in detection of
viral infection and poly I:C may largely overlap, yet some differences exist.
Stimulation of islets with recombinant IFN-a2 (150U/ml) caused increased IP10 production, yet had no effect on any of the other cytokines and chemokines tested
(Fig 4 and data not shown). The concentration used induced several ISGs, as assessed
by qPCR (data not shown), indicating that this concentration is sufficient to induce an
antiviral state. IP-10 induction is known to be IFN-dependent24. We examined whether
other pro-inflammatory cytokines and chemokines indeed did not rely on IFN-feedback
for their induction using neutralizing anti-IFN-a/ß antibodies (Abs). Cytokines and
chemokines such as IL-6, IL-8, G-CSF, IFN-y and others were still induced upon infection
in the presence of neutralizing anti-IFN Abs, suggesting that these did not depend on
IFNs for their induction (data not shown). These data indicate that IFN-a feedback may
mostly contribute to the major IP-10 increases that are observed upon CVB-infection.
Discussion
Enterovirus infections are considered to be environmental factors in type 1 diabetes
etiology, yet the underlying mechanisms that result in ß-cell destruction remain elusive.
Here we report that upon CVB-infection, a broad anti-viral response is generated in
primary human islets, which encompasses the production of a variety of IFNs, ISGs,
cytokines and chemokines. Our study shows that these cytokines and chemokines are
not only expressed at the mRNA level, but are also translated and secreted.
Human pancreatic islets produced several cytokines under steady-state culture
conditions. Among these were IL-6, IL-8 and MCP-1. Previous studies have shown that
these cytokines are produced by human pancreatic islets ex vivo, and this may be partially
due to stress generated during the isolation procedure19. Besides these three, IL-10 and
VEGF were also produced. The anti-inflammatory cytokine IL-10 might be produced in
order to reduce inflammation caused by isolation. During islet isolation endothelium may
be damaged and disrupted, possibly leading to VEGF induction in order to revascularize
the islets.
Upon CVB-infection, expression of a variety of cytokines and chemokines was
induced or increased. Highest production was found for IP-10, corroborating earlier
findings25. IP-10 is known for its chemotactic effects on lymphocytes, monocytes and
NK-cells26, 27, but has also been reported to inhibit angiogenesis and colony formation27'
29. Expression is reported to rely on IFN-y30, 31; however, we show that recombinant IFNa2
highly induces production of IP-10, in agreement with other reports24. Interestingly,
several independent groups have shown that IP-10 serum-levels are increased in type
1 diabetes patients and individuals at risk to develop the disease32-34, and recently, IP-10
was detected in islets of type 1 diabetes patients with fulminant diabetes16. This implies
102
Cytokine production in enterovirus-infected human islets
an important role for IP-10 in disease-development. Mouse studies corroborate this,
ß-cells secrete IP-10 in response to inflammation, and this subsequently mediates the
chemoattraction of T cells35. Furthermore, neutralization of IP-10 was shown to decrease
diabetes in mice36, 37.
Besides IP-10, several other pro-inflammatory cytokines and chemokines were
produced upon infection, such as IL-8, IL-6, TNF-a, RANTES, MIP-1ß and others. These
can have adverse effects on islet function, and may induce ER-stress and ß-cell death
(reviewed by Eizirik et al.2). Furthermore, T lymphocytes, monocytes, NK cells and other
immune cells may be attracted to the site of infection, and activation of these cells may
be triggered. The generated T cell responses will probably be Th1, as IFN-y is induced,
whereas secretion of Th2-associated cytokines (e.g. IL-4, IL-5, IL-13) is much lower, and
hardly increased upon CVB infection. IL-17-producing Th17 cells have been reported to
contribute to several autoimmune diseases38-40. Although some IL-17 was detected in
islet preparations, it was not increased upon infection.
Several growth factors were included, of which only G-CSF was increased upon
infection. G-CSF is a colony stimulating factor that particularly induces granulocyte
proliferation and differentiation in the bone marrow. It also stimulates survival,
proliferation and function of granulocytes, especially neutrophils, in the blood41. What
the role of G-CSF in type 1 diabetes etiology is remains to be determined.
The use of UV-inactivated CVB and AG7404 revealed that replicating virus
was a prerequisite for induction of antiviral responses and cytokine production. The
observation that the dsRNA analog poly I:C induced several cytokines and chemokines
that were also induced upon CVB-infection suggests that viral dsRNA may be a trigger
to induce antiviral responses. Recombinant IFN-a2 only induced production of IP-10,
but just one concentration was tested. Perhaps higher levels of IFN-a2 will induce
other cytokines and chemokines as well. Furthermore, other IFN-a subtypes may also
contribute to these inductions. However, preliminary experiments using neutralizing
anti-IFN Abs suggest that the majority of virus-induced cytokines and chemokines do
not rely on IFNs for their induction.
Islets consist of several types of endocrine cells, endothelium and resident
immune cells such as macrophages and DCs42. All these cell types could contribute to
the cytokines and chemokines that are induced. Duct cells, for example, can produce
TNF-a43, and pancreatic endothelium produces pro-inflammatory cytokines like IL-6 and
IL-8 upon CVB-infection44. To identify the cell type that is responsible for the production
of cytokines and chemokines, further investigation is required. However, that also the ßcells themselves may play a role is demonstrated by the study of Tanaka and colleagues16.
They detected IP-10 in all subtypes of islet cells, including a-cells and ß-cells, in the islets
of three deceased type 1 diabetes patients that were found positive for enterovirus
capsid protein. Furthermore, IFN-a can be found in human ß-cells of diabetes patients,
indicating that ß-cells themselves participate in cytokine production17.
Our findings suggest that a full-blown immune-response is ongoing in infected
islets. Feedback-mechanisms should restrict further inflammation when the infection
resolves. However, these feedback mechanisms may be differently regulated in different
individuals, and unrestrained inflammation may result in type 1 diabetes2. Perhaps
inflammation is not correctly cut down once infection is resolved in individuals at risk
for type 1 diabetes. In addition, in susceptible individuals aberrant adaptive immune
103
Chapter 6
responses against ß-cells may be generated, potentiated by inflammation in the islets.
These autoimmune responses may further contribute to type 1 diabetes.
As mentioned above, IP-10 serum levels are increased in type 1 diabetes
patients, and this has also been reported for IFN-a, MIP-1a, MIP-1ß and TNF-a45-47. Thus,
sustained production of inflammatory mediators seems to occur in individuals with type
1 diabetes. These inflammatory mediators may be produced by PBMC in the blood, but
also cytokines originating from elsewhere in the body, such as inflamed pancreatic islets,
may contribute to increased serum levels. The underlying mechanism for sustained
cytokine production is unknown, but could relate to delayed or ineffective clearance of
virus infection, or the genetic makeup of these individuals. Polymorphisms present in
the population can predispose for disease, and some single nucleotide polymorphisms
(SNPs) that are associated with type 1 diabetes are found in inflammatory mediators
such as RANTES, TNF-a and others48-50. Furthermore, SNPs in Mda5, which is the viral
sensor for enteroviruses, have been associated with type 1 diabetes51, 52. Additionally,
an association was found for SNPs in OAS1, an important effector protein in antiviral
defense, with type 1 diabetes53, 54. Thus individuals may be more prone to aberrant
antiviral responses depending on their genetic makeup.
In conclusion, we report that a broad antiviral response is generated by human
pancreatic islets upon CVB-infection. This response is characterized by the induction
of IFNs and ISGs and further encompasses the secretion of several pro-inflammatory
cytokines, chemokines and growth factors. Virus replication is a prerequisite for these
responses and the observation that the dsRNA analog poly I:C yields a largely similar
cytokine pattern implies that viral dsRNA may trigger these responses. These data
provide new insight in the antiviral responses of human pancreatic islets and provide
a mechanism by which enteroviruses may induce type 1 diabetes in susceptible
individuals.
Acknowledgements
The authors are grateful to Lonneke van der Linden for help with statistical analysis. This
work was supported by grants from The Netherlands Organization for Scientific Research
(NWO-VIDI-917.46.305) to F.J.M.v.K.; the Radboud University Medical Centre Nijmegen
(grant number 2005-8) to F.J.M.v.K and J.M.D.G; and the Juvenile Diabetes Research
Foundation (Grant Number: 24-2008-949) to G.J.A and F.J.M.v.K.
104
Cytokine production in enterovirus-infected human islets
References
1.
M . K nip, R. V e ijo la , S. M . V irta n e n , H. Hyoty, O. V aarala, H. K. A k e rb lo m (2005). E n viro n m e n ta l trig g e rs and d e te rm in a n ts o f ty p e 1
d ia b e te s . D iabetes, 54 Suppl 2, S125-136.
2.
D. L. E izirik, M . L. C olli, F. O rtis (2009). The role o f in fla m m a tio n in in s u litis and b e ta -ce ll loss in ty p e 1 d ia b e te s. N at Rev E ndocrinol,
5, 2 1 9 -226.
3.
H. H yoty, K. W. Taylor (2002). T he role o f viruses in h u m a n d ia b e te s. D ia b e to lo g ia , 45, 1353-1361.
4.
R. V a re la-C alvino, M . Peakm an (2003). E n teroviruses and ty p e 1 d ia b e te s. D iabetes M e ta b Res Rev, 19, 431-441.
5.
J. L. W h itto n (2002). Im m u n o p a th o lo g y d u rin g coxsackievirus in fe c tio n . S pringer S em in Im m u n o p a th o l, 24, 201-213.
6.
M . A . Pallansch, R. P. Roos (2007). E nteroviruses: P olioviruses, C oxsackieviruses, Echoviruses, and N e w e r E nteroviruses. In V irology.
Fields V irology.
7.
M . Kram er, B. M . S chulte, L. W. T oonen, M . A. de B ru ijn i, J. M . G alam a, G. J. A d e m a , F. J. van Kuppeveld (2007). Echovirus in fe ctio n
causes rapid lo s s -o f-fu n c tio n and cell d e a th in h um an d e n d ritic cells. Cell M ic ro b io l, 9, 1507-1518.
8.
M . Kram er, B. M . S chulte, L. W. T oonen, P. M . Barral, P. B. Fisher, K. H. Lanke, J. M . G alam a, F. J. van Kuppeveld, G. J. A d e m a (2008).
P ha g ocytosis o f p ic o rn a v iru s -in fe c te d cells induces an R N A -d e p e n d e n t a n tiv ira l s ta te in h u m an d e n d ritic cells. J V iro l, 82 , 2 9 3 0
2 93 7.
9.
F. D o tta , S. C ensini, A. G. van H a lte re n , L. M a rs e lli, M . M a sin i, S. D ionisi, F. M osca, U. Boggi, A . O. M u d a , S. D. Prato, J. F. E llio tt, A.
Covacci, R. R appuoli, B. O. Roep, P. M a rc h e tti (2007). Coxsackie B4 viru s in fe c tio n o f beta cells and n a tu ra l k ille r cell in s u litis in recento n s e t ty p e 1 d ia b e tic p a tie n ts . Proc N a tl Acad Sci U S A, 104, 5115-5120.
10.
P. Y lipa a sto, K. Klingel, A . M . Lindberg, T. O to n ko ski, R. K andolf, T. H ovi, M . R oivainen (2004). E n te ro viru s in fe c tio n in hum an
11.
S. J. R ichardson, A . W illco x, A . J. Bone, A . K. Foulis, N. G. M o rg a n (2009). The prevalence o f e n te ro v ira l capsid p ro te in vp1
p a n c re a tic islet cells, islet tro p is m in vivo and re c e p to r in v o lv e m e n t in c u ltu re d isle t beta cells. D ia b e to lo g ia , 47, 225-239.
im m u n o s ta in in g in p a n cre a tic islets in h um an ty p e 1 d ia b e te s. D iabetologia.
12.
M . R oivainen, P. Y lipaasto, C. S avolainen, J. G alam a, T. Hovi, T. O to n ko ski (2002). F unctio n a l im p a irm e n t and k illin g o f h um an beta
cells by e n te ro v iru s e s : th e c a p a city is shared by a w id e range o f se ro typ e s, b u t th e e x te n t is a c h a ra c te ris tic o f in d iv id u a l v iru s strains.
D ia b e to lo g ia , 45 , 693-702.
13.
G. S o ldevila, M . Buscem a, M . D oshi, R. F. Jam es, G. F. B ottazzo, R. P u jo l-B o rre ll (1991). C y to to x ic e ffe c t o f IFN -gam m a plus TNF-alpha
on h u m an isle t cells. J A u to im m u n , 4, 291-306.
14.
F. O rtis , P. P iro t, N. N aam ane, A . Y. Kreins, J. Rasschaert, F. M o o re , E. T h e a tre , C. V e rhaeghe, N. E. M agnusson, A . C h a rio t, T. F. O rn to ft,
D. L. E izirik (2008). In d u c tio n o f n u cle a r fa c to r-ka p p a B and its d o w n s tre a m genes by TN F-alpha and IL-1beta has a p ro -a p o p to tic role
in p a n c re a tic beta cells. D ia b e to lo g ia , 51, 1 213-1225.
15.
S. U no, A . Im agaw a, K. O kita , K. Sayama, M . M o riw a k i, H. Iw ahashi, K. Y am agata, S. Tam ura, Y. M a tsu za w a , T. H anafusa, J. M iyagaw a,
I. S h im o m u ra (2007). M a cro p h a g e s and d e n d ritic cells in filtra tin g islets w ith o r w ith o u t beta cells p ro d u c e tu m o u r necrosis fa c to r
a lp ha in p a tie n ts w ith re c e n t-o n s e t ty p e 1 dia b e te s. D ia b e to lo g ia , 50, 596-601.
16.
S. Tanaka, Y. N ishida, K. A id a , T. M a ru y a m a , A. S him ada, M . Suzuki, H. S him ura, S. Takizaw a, M . Takahashi, D. A kiya m a , S. A raiY am ashita, F. F uruya, A . Kaw aguchi, M . Kaneshige, R. K atoh, T. Endo, T. Kobayashi (2009). E n te ro viru s in fe c tio n , CXC ch e m o k in e ligand
10 (CXCL10) and CXCR3 c irc u it: a m echanism o f a ccelerated b e ta -ce ll fa ilu re in fu lm in a n t ty p e 1 d ia b e te s. D iabetes.
17.
A . K. Foulis, M . A. F arquharson, A. M e a g e r (1987). Im m u n o re a c tiv e a lp h a -in te rfe ro n in in su lin -se cre tin g beta cells in ty p e 1 d iabetes
18.
E. W essels, D. D uijsings, R. A . N o te b a a rt, W. J. M e lch e rs, F. J. van K uppeveld (2005). A p ro lin e -ric h region in th e coxsackievirus 3A
19.
R. B o ttin o , A . N. B ala m u ru g a n , H. Tse, C. T h iru n a vu kka ra su , X. Ge, J. P rofozich, M . M ilto n , A. Ziegenfuss, M . Trucco, J. D. Piganelli
20.
A . N. B ala m u ru g a n , Y. Chang, J. J. Fung, M . Trucco, R. B o ttin o (2003). F lexible m a n a g e m e n t o f e n z ym a tic d ig e s tio n im p ro ve s hum an
21.
A . N. B a lam urugan, Y. Chang, S. B e rte ra , A . Sands, V. Shankar, M . Trucco, R. B o ttin o (2006). S u ita b ility o f h um an ju v e n ile pancreatic
22.
X. W an g, B. Seed (2003). A PCR p rim e r bank fo r q u a n tita tiv e gene expression analysis. N ucleic Acids Res, 31, e154.
23.
J. W. Yoon, M . A u s tin , T. O n odera, A . L. N o tkin s (1979). Is o la tio n o f a v iru s fro m th e pancreas o f a ch ild w ith d ia b e tic ketoacidosis. N
m e llitu s . Lancet, 2, 1 423-1427.
p ro te in is re q u ire d fo r th e p ro te in to in h ib it e n d o p la s m ic re tic u lu m -to -g o lg i tra n s p o rt. J V iro l, 79, 5163-5173.
(2 00 4). Response o f h u m an islets to is o la tio n stress and th e e ffe c t o f a n tio x id a n t tre a tm e n t. D iabetes, 53, 2559-2568.
is le t is o la tio n o u tc o m e fro m s u b -o p tim a l d o n o r p ancreata. A m J T ran sp la n t, 3, 1135-1142.
isle ts fo r clin ic a l use. D ia b e to lo g ia , 49 , 1 845-1854.
Engl J M e d , 300, 1 173-1179.
24.
M . H u ltcra n tz, M . H. H uhn, M . W o lf, A . O lsson, S. Jacobson, B. R. W illia m s , O. K orsgren, M . F lo d s tro m -T u llb e rg (2007). In te rfe ro n s
ind u c e an a n tiv ira l sta te in h u m an p a n c re a tic islet cells. V iro lo g y, 367, 92-101.
25.
A . K. Berg, O. Korsgren, G. Frisk (2006). In d u c tio n o f th e c h e m o k in e in te rfe ro n -g a m m a -in d u c ib le p ro te in -1 0 in h u m an pancreatic
26.
J. M . Farber (1997). M ig and IP-10: CXC ch e m o kin e s th a t ta rg e t ly m p h o c y te s . J Leukoc Biol, 61, 246-257.
isle ts d u rin g e n te ro v iru s in fe c tio n . D ia b e to lo g ia , 49, 2 697-2703.
27.
M . B ag giolini, B. D ew ald, B. M o s e r (1997). H um an ch e m o kin e s: an u p d a te . A n n u Rev Im m u n o l, 15, 675-705.
28.
A . L. A n g io lillo , C. S gadari, D. D. Taub, F. Liao, J. M . Farber, S. M a h e s h w a ri, H. K. K le in m a n , G. H. Ream an, G. Tosato (1995). Hum an
in te rfe ro n -in d u c ib le p ro te in 10 is a p o te n t in h ib ito r o f angiogenesis in vivo. J Exp M e d , 182, 155-162.
29.
K. L. T aylor, D. W. Leam an, R. G rane, N. M e c h ti, E. C. B ord e n , D. J. L in d n e r (2008). Id e n tific a tio n o f in te rfe ro n -b e ta -s tim u la te d genes
t h a t in h ib it angiogenesis in v itro . J In te rfe ro n C yto kin e Res, 28, 733-740.
30.
A . D. Luster, J. V. Ravetch (1987). B iochem ical c h a ra c te riza tio n o f a gam m a in te rfe ro n -in d u c ib le c y to k in e (IP-10). J Exp M e d , 166,
31.
G. K aplan, A . D. Luster, G. H ancock, Z. A. C ohn (1987). The expression o f a gam m a in te rfe ro n -in d u c e d p ro te in (IP-10) in delayed
32.
A . S him ada, J. M o rim o to , K. K odam a, R. Suzuki, Y. O ikaw a, O. Funae, A. Kasuga, T. Saruta, S. N a ru m i (2001). Elevated se ru m IP-10
1 08 4-1 097.
im m u n e responses in h u m a n skin. J Exp M e d , 166, 1098-1108.
levels o bse rve d in ty p e 1 d ia b e te s. D iabetes Care, 24 , 510-515.
33.
F. N ic o le tti, I. C onget, M . Di M a u ro , R. Di M a rco , M . C. M a zzarino, K. Bendtzen, A . M essina, R. G om is (2002). Serum co n c e n tra tio n s of
th e in te rfe ro n -g a m m a -in d u c ib le c h e m o k in e IP-10/CXCL10 are a u g m e n te d in b o th n e w ly diagn o se d Type I d ia b e te s m e llitu s p a tie n ts
and s u b je cts a t risk o f d e v e lo p in g th e disease. D ia b e to lo g ia , 45, 1107-1110.
34.
A . A n to n e lli, P. Fallahi, S. M . F errari, C. P up illi, G. d'A n n u n zio , R. Lo rin i, M . V a n e lli, E. F e rra n n in i (2008). Serum Th1 (CXCL10) and Th2
35.
S. F rig erio, T. J u n t, B. Lu, C. G erard, U. Z um steg, G. A . H olla n d e r, L. Piali (2002). Beta cells are respo n sib le fo r CXCR3-m ediated T-cell
36.
J. M o rim o to , H. Y oneyam a, A. S him ada, T. S higihara, S. Yam ada, Y. O ikaw a, K. M a ts u s h im a , T. S aruta, S. N a ru m i (2004). CXC chem o kin e
(CCL2) c h e m o k in e levels in c h ild re n w ith n e w ly diagn o se d Type 1 d ia b e te s: a lo n g itu d in a l study. D ia b e t M e d , 25, 1349-1353.
in filtra tio n in in s u litis . N at M e d , 8, 1 414-1420.
ligand 10 n e u tra liz a tio n suppresses th e o c c u rre n ce o f d ia b e te s in nono b e se d ia b e tic m ice th ro u g h enhanced beta cell p ro life ra tio n
w ith o u t a ffe c tin g in s u litis . J Im m u n o l, 173, 7017-7 0 2 4 .
37 .
U. C hris ten, D. B. M cG avern, A . D. Luster, M . G. von H e rra th , M . B. O ld sto n e (2003). A m o n g CXCR3 c h e m o kin e s, IF N -gam m a-inducible
105
Chapter 6
38.
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
106
protein of 10 kDa (CXC chemokine ligand (CXCL) 10) but not monokine induced by IFN-gamma (CXCL9) imprints a pattern for the
subsequent development of autoim mune disease. J Immunol, 171, 6838-6845.
M . Chabaud, J. M. Durand, N. Buchs, F. Fossiez, G. Page, L. Frappart, P. Miossec (1999). Human interleukin-17: A T cell-derived
proinflamm atory cytokine produced by the rheumatoid synovium. A rthritis Rheum, 42, 963-970.
C. L. Langrish, Y. Chen, W. M . Blumenschein, J. M attson, B. Basham, J. D. Sedgwick, T. M cClanahan, R. A . Kastelein, D. J. Cua (2005).
IL-23 drives a pathogenic T cell population that induces autoimmune inflammation. J Exp Med, 201, 233-240.
L. Steinman (2007). A brief history of T(H)17, the first major revision in the T(H)1/T(H)2 hypothesis of T cell-mediated tissue damage.
Nat Med, 13, 139-145.
R. C. Furze, S. M. Rankin (2008). Neutrophil mobilization and clearance in the bone marrow. Immunology, 125, 281-288.
W. Lu, D. G. Pipeleers, G. Kloppel, L. Bouwens (1996). Comparative immunocytochemical study of MHC class II expression in human
donor pancreas and isolated islets. Virchows Arch, 429, 205-211.
B. Movahedi, M. Van de Casteele, N. Caluwe, G. Stange, K. Breckpot, K. Thielem ans, G. Vreugdenhil, C. M athieu, D. Pipeleers (2004).
Human pancreatic duct cells can produce tum our necrosis factor-alpha that damages neighbouring beta cells and activates dendritic
cells. Diabetologia, 47, 998-1008.
M . M. Zanone, E. Favaro, E. Ferioli, G. C. Huang, N. J. Klein, P. C. Perin, M. Peakman, P. G. Conaldi, G. Camussi (2007). Human
pancreatic islet endothelial cells express coxsackievirus and adenovirus receptor and are activated by coxsackie B virus infection.
Faseb J, 21, 3308-3317.
W. Chehadeh, J. W eill, M. C. Vantyghem, G. Alm, J. Lefebvre, P. W attre, D. Hober (2000). Increased level of interferon-alpha in blood
of patients with insulin-dependent diabetes mellitus: relationship with coxsackievirus B infection. J Infect Dis, 181, 1929-1939.
P. Hanifi-Moghaddam, S. Kappler, J. Seissler, S. Muller-Scholze, S. M artin, B. O. Roep, K. Strassburger, H. Kolb, N. C. Schloot (2006).
Altered chemokine levels in individuals at risk of Type 1 diabetes mellitus. Diabet Med, 23, 156-163.
A . B. Erbagci, M. Tarakcioglu, Y. Coskun, E. Sivasli, E. Sibel Namiduru (2001). M ediators of inflammation in children with type I
diabetes mellitus: cytokines in type I diabetic children. Clin Biochem, 34, 645-650.
A . Zhernakova, B. Z. Alizadeh, P. Eerligh, P. Hanifi-Moghaddam, N. C. Schloot, B. Diosdado, C. Wijmenga, B. O. Roep, B. P. Koeleman
(2006). Genetic variants of RANTES are associated with serum RANTES level and protection for type 1 diabetes. Genes Immun, 7,
544-549.
A . Settin, A. Ismail, M . A . El-Magd, R. El-Baz, A . Kazamel (2009). Gene polymorphisms of TNF-alpha-308 (G/A), IL-10(-1082) (G/A),
IL-6(-174) (G/C) and IL-1Ra (VNTR) in Egyptian cases with type 1 diabetes mellitus. Autoimmunity, 42, 50-55.
R. Kumar, R. Goswami, S. Agarwal, N. Israni, S. K. Singh, R. Rani (2007). Association and interaction of the TNF-alpha gene with other
pro- and anti-inflammatory cytokine genes and HLA genes in patients with type 1 diabetes from North India. Tissue Antigens, 69,
557-567.
D. J. Smyth, J. D. Cooper, R. Bailey, S. Field, O. Burren, L. J. Smink, C. Guja, C. Ionescu-Tirgoviste, B. W idmer, D. B. Dunger, D. A. Savage,
N. M. Walker, D. G. Clayton, J. A. Todd (2006). A genome-wide association study of nonsynonymous SNPs identifies a type 1 diabetes
locus in the interferon-induced helicase (IFIH1) region. Nat Genet, 38, 617-619.
S. Liu, H. Wang, Y. Jin, R. Podolsky, M. V. Reddy, J. Pedersen, B. Bode, J. Reed, D. Steed, S. Anderson, P. Yang, A . Muir, L. Steed, D.
Hopkins, Y. Huang, S. Purohit, C. Y. Wang, A . K. Steck, A . M ontemari, G. Eisenbarth, M . Rewers, J. X. She (2009). IFIH1 polymorphisms
are significantly associated with type 1 diabetes and IFIH1 gene expression in peripheral blood mononuclear cells. Hum Mol Genet,
18, 358-365.
M . C. Tessier, H. Q. Qu, R. Frechette, F. Bacot, R. Grabs, S. P. Taback, M . L. Lawson, S. E. Kirsch, T. J. Hudson, C. Polychronakos (2006).
Type 1 diabetes and the OAS gene cluster: association with splicing polymorphism or haplotype? J Med Genet, 43, 129-132.
L. L. Field, V. Bonnevie-Nielsen, F. Pociot, S. Lu, T. B. Nielsen, H. Beck-Nielsen (2005). OAS1 splice site polymorphism controlling
antiviral enzyme activity influences susceptibility to type 1 diabetes. Diabetes, 54, 1588-1591.
Cytokine production in enterovirus-infected human islets
Cytokine
Donor 1
Donor 2
Donor 3
Donor 4
Mock
CVB3
Mock
CVB3
Mock
CVB3
Mock
CVB3
IL-1ß
10
45
15
19
17
85
<7
51
p-value
0,039
I L-1Ra
226
1334
531
712
712
2820
187
1308
0,036
50
23
178
83
97
43
138
56
10 2
459
158
50
23
174
80
0,023
0,027
IL-2
IL-4
IL-5
20
29
49
20
59
46
20
20
0,521
IL-6
IL-7
2626
241
18036
233
5727
395
11855
184
6930
451
311861
457
3664
74
16547
103
0,056
0,658
IL-8
17465
74661
28338
75891
40453
237003
44953
151638
0,004
IL-9
370
420
486
346
582
689
245
409
0,552
IL-10
IL-12p70
2304
870
1866
665
3716
1285
1462
527
5007
1727
3869
1459
686
688
235
235
0,183
0,186
IL-13
190
164
377
142
320
322
78
78
0,320
IL-15
IL-17
547
335
759
550
381
335
2 11
398
596
378
894
1034
391
<90
1017
611
0,455
0,099
eotaxin
397
996
597
550
690
1207
279
657
0,091
bFGF
232
362
266
189
298
403
76
232
0,293
G-CSF
85
1433
116
614
177
4606
306
2314
0,007
GM-CSF
IFN-y
IP-10
172
703
662
535
3235
62792
357
1378
557
340
2131
11522
389
1851
779
959
6931
20004
104
625
2528
458
2929
118975
0,077
0,019
MCP-1
MIP-1a
19452
298
>21877
968
15181
381
110 2 2
25841
434
36617
1258
25241
260
48042
1072
0,403
0,045
MIP-1ß#
541
1605
479
775
621
1788
743
2613
0 ,0 10
PDGF
140
218
347
163
403
471
28
177
0,491
RANTES
TNF-a
2 10
1209
325
510
416
1214
2 10
995
0,025
262
9923
1126
6712
490
19247
698
5132
522
30399
2513
20461
198
2277
1107
1979
0,026
0,119
VEGF
429
51
0 ,0 0 2
Supplementary Table 1. Cytokine and chemokine production by human pancreatic islets upon CVB3
infection.
Human islets were mock or CVB3-infected with an MOI of 10 and at 48h p.i. supernatant was harvested and
analyte-levels were determined by 27-plex as described. Data shown are from 4 different experiments using
different donors.
107
Chapter 7
Detection of enterovirus RNA in
peripheral blood mononuclear cells
of type 1 diabetic patients beyond
the stage of acute infection
Barbara M. Schulte, Judith Bakkers, Kjerstin H.W. Lanke,
Willem J.G. Melchers, Ciska Westerlaken, Wil Allebes,
Henk-Jan Aanstoot, G. Jan Bruining Gosse J. Adema,
Frank J.M. van Kuppeveld, Jochem M.D. Galama
Viral Im m unology (2010) 23(1):99-104
Chapter 7
Abstract
revious studies have shown that enteroviral RNA can be detected in blood at
onset of type 1 diabetes (T1D). The infection may play a role in triggering of T1D
and genetic host factors might contribute to this process. We investigated (i)
whether enterovirus is present at onset of T1D in peripheral blood mononuclear cells
(PBMC), plasma, throat or stool and (ii) w hether enteroviral presence is linked with HLADR type and/or polymorphisms in melanoma differentiation-associated gene 5 (MDA5)
and 2'-5' oligoadenylate synthetase 1 (OAS1), factors of anti-viral immunity. For this,
PBMC, plasma, throat and stool samples from 10 T1D patients and 20 unrelated controls
were tested for presence of enteroviruses (RT-PCR), for HLA-DR type and polymorphisms
in MDA5 and OAS1. Enterovirus RNA was detected in PBMC of 4/10 T1D patients, but
none of 20 controls. Plasma was positive in 2/10 T1D patients and none of 20 controls,
suggesting that enteroviruses found at onset of T1D are mainly present in PBMC. All
throat samples from positive T1D patients were virus-negative and only 1 fecal sample
was positive. The negative results for all throat- and most stool samples argues against
acute infection. Enterovirus presence linked with HLA-DR4 but not with polymorphisms
in MDA5 or OAS1.
P
110
Enterovirus in PBMCs of type 1 diabetes patients
Background
Coxsackie B viruses (CVB) and echoviruses, both belonging to the human enterovirus
B (HEV-B) species, have for decades been indicated as environmental factors in type
1 diabetes (T1D) which is generally regarded an autoimmune disease (reviewed in1,
2). Support for their role in T1D is deduced from: (i) prospective cohort studies which
showed that enterovirus infections coincide with onset of autoimmunity and with clinical
onset of T1D1; (ii) detection of enterovirus RNA in blood of T1D patients (see below)
and (iii) detection of enterovirus in islets of individuals with established T1D3-5. Thus,
enteroviruses may be involved in T1D along various routes: indirectly, through triggering
of autoimmunity, or more directly, through infection of islets and destruction of ß cells.
It should be noted, however, that these two processes do not necessarily exclude each
other; they may even be interrelated.
Enterovirus RNA has been found in blood by RT-PCR at onset of disease in 20
to 75% of T1D patients6-13. Enterovirus has furthermore been found in auto-antibody
positive (pre-diabetic) persons11, 14, 15 and in patients with established T1D7, 13, but not,
or with a much lower frequency, in matched healthy controls without predisposition for
T1D or in T2D patients13. So far, none of the studies that detected viral RNA in blood of
T1D patients investigated the stage of infection: w hether a positive RT-PCR was due to
early infection with virus excreted in the throat, or convalescence with virus detectable
in stool only, which can last for up to 3 months16. Another possibility is that virus remains
detectable beyond convalescence (stool negative). Taken together, the difference with
unrelated healthy people suggests that T1D patients and those at risk for the disease are
more susceptible for enteroviruses or are unable to clear the infection, both conditions
which might be involved in T1D.
Besides environmental factors, a strong genetic predisposition is involved.
HLA-DR3 and DR4 are major risk factors, whereas DR2 is negatively associated with
the disease17-21. Also other genetic factors have been associated with T1D and new
associations are still being found, including two recently identified single nucleotide
polymorphisms (SNPs) that are involved in antiviral immunity22-25. These factors,
melanoma differentiation-associated gene 5 (MDA5) and 2'-5'oligoadenylate synthetase
1 (OAS1), play an important role in the innate defence against RNA viruses by sensing or
degrading (entero)viral RNA, respectively. These SNP's may thus provide a link between
(entero)viruses and T1D.
In this study we investigated (i) w hether blood mononuclear cells contain enteroviral
RNA, (ii) what is the stage of infection and (iii) whether infection is linked with particular
risk alleles for HLA-DR and/or with SNPs in MDA5 and OAS1.
111
Chapter 7
Patients and methods
Patients and control group
Patients and controls were included at the Paediatric Clinics of the Erasmus University Medical Centre
Rotterdam and the Canisius-Wilhelmina Hospital Nijmegen. Ten T1D patients (5 males, 5 females) were
included and samples were collected within a month of diagnosis. Mean age of the patient group was 9.7 years
(range 5-14 years). For comparison, a group of 20 hospitalized children (9 males, 10 females, 1 of whom the
gender is unknown) of the same age range, with non-endocrine disorders was included. Their mean age was
12.5 (range 6-17 years). Samples from T1D patients were obtained between November 2003 and November
2004, and from healthy controls in June 2004. Informed consent was given by the parents, based on a study
protocol which was approved by the local Ethical Committees of the respective hospitals.
Laboratory samples
The following samples were collected: (1) 5 ml of citrate blood for isolation of plasma and PBMC, (2) 5 ml
of clotted blood for serum, (3) throat swab in virus transport medium and (4) a fecal sample. PBMC were
isolated as instructed by the manufacturer (Becton and Dickinson, Erembodegem, Belgium). After processing,
all samples were quickly frozen and stored at -800 C until use.
Virus detection
RNA was isolated from 200 ^l plasma, an equivalent of 2 -105 PBMCs (isolated PBMCs dissolved in PBS), and
stool sample homogenate. For the in-house nested RT-PCR, RNA extraction was done using the MagNaPure
LC Isolation station (Roche Applied Science, Mannheim, Germany). Amplification was performed in a nested
PCR reaction as described previously26. Real-time PCR was performed as described previously27. Real-time
NASBA (NucliSens EasyQ) was performed according to manufacturer's instructions (BioMérieux, Boxtel, The
Netherlands). Amplification techniques were regularly tested by Quality Control for Molecular Diagnostics
(QCMD) standards. An enterovirus-specific internal homologous control RNA was included in each sample
during the extraction to monitor the NucliSens EasyQ and PCR procedures at the individual sample level. This
excludes false negatives due to possible inhibitory factors in input samples, which could be present especially in
stool samples. Sensitivity of the methods is at least 0.002 to 0.01 TCID50 for in-house nested RT-PCR and real
time PCR, depending on the enterovirus strain tested. NASBA is similar, or somewhat less sensitive compared
to the PCRs, depending on the enterovirus strain.
Interferon-a detection
The amount of Interferon-a (IFNa) in plasma samples was determined using a commercial ELISA kit, product
number RDI-PB41110, from Research Diagnostics Inc (Fitzgerald Industries International, North Acton, USA).
The test was performed according to instructions of the manufacturer
HLA typing
Total NA were isolated using MagNaPure as described above. HLA typing was performed on RNase-treated
DNA using the lifecodes HLA-SSO typing kit (Tepnel, Manchester, UK) according to manufacturer's instructions
and EFI/ASHI guidelines for histocompatibility testing.
MDA5 and OAS1 single nucleotide polymorphism (SNP) typing
The MDA5 SNP tested is the A946T polymorphism (rs1990760) that has been described by Smyth et al.24. The
OAS1 SNP tested is rs10774671, which is an A/G splice-site SNP22, 23, 28. SNPs in MDA5 and OAS1 were assessed
by amplification of the relevant region, followed by sequencing of the PCR product. From the sequence,
presence of the SNP and homo- or heterozygosity was determined. Primers are available upon request.
112
Enterovirus in PBMCs of type 1 diabetes patients
Results
Detection of enterovirus RNA in PBMC of T1D patients.
Ten recently diagnosed T1D patients were tested by RT-PCR26 and compared with 20
healthy children of the same age without known risk factors for T1D. PBMC and plasma
were tested separately. Four of the 10 T1D patients (40%) reacted positive for enterovirus
in their PBMC, two of them were also positive in plasma (Table 1). The outcome was
confirmed on separately isolated total NA by real-time PCR27 and by NASBA, an RNAbased amplification technique (data not shown). Amplification of part of the 5'UTR
Table 1. Background information and enterovirus RNA detection in T1D patients and controls.
P atien t Date o f B irth
Gender HLA DRB1
1
2
M
M
M
M
F
M
F
F
F
F
3
4
5
6
7
8
9
10
04-05-1998
11-05-1989
02-08-1992
30-05-1995
22-03-1996
29-11-1995
31-08-1993
03-03-1995
11-07-1995
04-02-1993
DRB1*04/DRB1*13
DRB1*0301/DRB1*04
DRB1*01/DRB1*13
DRB1*0301/DRB1*04
DRB1*04/DRB1*15
DRB1*01/DRB1*0301
DRB1*04/DRB1*10
DRB1*01/DRB1*04
DRB1*04/DRB1*08
DRB1*04/DRB1*04
C ontrol Date o f B irth
Gender HLA DRB1
1
2
F
M
F
M
F
M
M
M
M
M
?
3
4
5
6
7
8
9
10
11
12
13
14
15
16
17
18
19
20
03-07-1998
06-03-1997
20-05-1989
15-08-1988
25-05-1992
01-02-1989
23-05-1995
29-09-1989
07-02-1996
29-01-1993
17-02-1997
17-06-1991
27-03-1993
10-09-1989
30-08-1993
19-04-1989
08-01-1987
10-09-1988
04-10-1988
15-03-1988
F
F
M
F
F
F
F
M
F
Plasma
+
+
Plasma
DRB1*14/DRB1*15
DRB1*0301/DRB1*11
DRB1*04/DRB1*11
DRB1*13/DRB1*14
DRB1*04/DRB1*13
DRB1*07/DRB1*07
DRB1*01/DRB1*04
DRB1*14/DRB1*14
DRB1*04/DRB1*15
DRB1*01/DRB1*13
DRB1*01/DRB1*04
DRB1*04/DRB1*14
DRB1*07/DRB1*13
DRB1*04/DRB1*11
DRB1*01/DRB1*0301
DRB1*01/DRB1*04
DRB1*14/DRB1*15
DRB1*0302/DRB1*07
DRB1*04/DRB1*13
DRB1*01/DRB1*0301
-
PBMC
Feces
+
-
+
-
-
-
-
-
-
-
-
+
+
+
PBMC
-
-
-
Throat
-
n.t.
n.t.
-
-
-
-
Feces
Throat
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
n.t.
-
-
-
-
-
1
IFN-a
<
<
13
<
<
<
<
<
n.t.
n.t.
IFN-a
<
>500
<
<
<
<
<
<
<
<
<
<
<
75
<
<
<
<
<
<
Abbreviations: M, male; F, female;? gender unknown; + positive reaction; - negative reaction; n.t. = not tested;
Interferon- a (IFN-a) plasma levels in pg/ml; detection threshold 10 pg/ml; <, less than the detection limit.
113
Chapter 7
yielded a fragment which showed highest similarities with viruses from the HEV-B
species. Unfortunately, attempts to amplify the variable region (VP1-2A) using degenerate
primers failed, thereby making further typing of the enteroviruses impossible. None of
the 20 children in the control group were positive for enteroviral RNA in either PBMC
or plasma (Table 1). All controls were sampled in June 2004, whereas T1D patients were
sampled throughout the year. Although this could have led to a bias, there is no obvious
cluster of the four positive patients with a particular season, and only one of the four
was sampled in the "enterovirus season", late summer and early autumn. Virus-positive
T1D patients were sampled in August, November (2) and February.
1
2
3
4
5
Virus
+
-
+
-
6
-
7
+
8
-
9
-
10
+
Control
1
2
3
4
5
Virus
-
6
-
7
-
8
-
9
-
10
11
12
13
14
15
16
17
18
19
20
-
1
Patient
S
A
O
f
o
Table 2. SNP genotypes
polymorphisms.
MDA5 OAS1
GA
GA
GG
AA
AA
GA
GA
GA
AA
GA
AA
GA
GA
AA
GG
AA
GG
GA
AA
AA
MDA5 OAS1
GG
AA
GA
GA
AA
AA
GG
AA
GA
GA
GA
GA
GA
GA
GA
AA
GA
GA
GG
GA
Abbreviations: + enterovirus-positive;
- enterovirus-negative.
114
and MDA5
AA
GA
GA
GA
GG
GA
GA
AA
GA
AA
GA
AA
AA
GG
AA
GA
AA
AA
GG
AA
Prolonged enterovirus infection in T1D
patients.
Little is known about the stage of
enterovirus infection in T1D patients
that are enterovirus-positive at onset of
the disease. Therefore, we investigated
whether virus could be detected in throat
or stool, which gives some indication
of the duration of infection. Throat and
stool samples were collected at the same
day as blood samples were drawn. The
samples were tested by RT-PCR (throat) or
virus isolation and NASBA (fecal samples).
Throat samples were invariably negative
as was virus isolation, whereas enterovirus
was detected by NASBA in only 1 of the 4
virus positive patients, suggesting that
the infections were in a late stage or of
prolonged duration16 (Table 1).
Detection of IFNa
A previous study found that T1D patients
have elevated levels of IFNa in their blood,
which correlated with the presence of
enterovirus7. Using ELISA, we investigated
whether presence of viral RNA was linked
with increased IFNa levels in blood, but no
association was found (Table 1).
Enterovirus and genetic risk factors.
The (prolonged) presence of viral RNA
in PBMC of T1D patients suggests some
intrinsic susceptibility to enterovirus
infection or an inability to clear the
infection. Some of the genetic risk factors
that predispose for T1D, play a role in
antiviral defence and may thus be involved
Enterovirus in PBMCs of type 1 diabetes patients
in aberrant clearance of enteroviruses. Therefore, we tested whether the presence of
viral RNA linked with HLA-DR type and(or) with SNPs in either MDA5 or OAS1.
HLA-typing was performed on DNA isolated from PBMC. The T1D predisposing
HLA-DR4 and to a lesser extent DR3 were more abundant in the T1D population; 9 of
the 10 (90%) T1D patients had a DR3 and/or DR4 allele versus 13 out of 20 (65%) in the
control group (Table 1). The "high risk" DR3/DR4 or DR4/DR4 phenotype was found in 3
of 10 (30%) T1D patients: 2 of 4 (50%) virus-positive, versus 1 of 6 (17%) virus-negative
patients, but not in any of 20 controls. All virus-positive patients had a DR4 allele.
The MDA5 and OAS1 polymorphisms were assessed by amplification of the
region containing the SNPs, followed by sequencing of the PCR product. Smyth et al.
found a higher prevalence of AA and GA in MDA5 in T1D patients (AA + GA 87.4 % in T1D
patients, 85.5 % in controls)24. We found that the T1D-associated AA and GA genotypes
in MDA5 are present in 3 and 6 of 10 patients (90%) and in 5 and 12 of 20 controls
(85%), respectively. Heterozygosity was most prominent in virus-positive patients (3 of
4, 75%) (Table 2). The remaining virus-positive patient had an AA genotype. Three out
of 6 virus-negative patients (50%) had a GA genotype, 2 (33%) a GG genotype and 1
(17%) an AA genotype (Table 2). Thus no major differences were observed in the MDA5
polymorphism between virus-positive and virus-negative patients.
Field and colleagues reported increased prevalence of GG and GA in OAS1
in the T1D group (GG + GA 58.7 % in T1D patients, compared to 50.3% in controls)22.
However, Smyth et al. did not And increased prevalence for GG and GA genotypes in T1D
patients28. We found that T1D-associated GG and GA genotypes of OAS1 were present
in 2 and 3 of 10 T1D patients (50%) and in 3 and 8 out of 20 controls (55%), respectively
(Table 2). Thus, no obvious differences were observed between T1D patients and the
control group. Remarkably, only 1 of 4 (25%) virus-positive patients had a GG or GA
genotype compared to 4 out of 6 (67%) virus-negative T1D patients (Table 2). Due to the
small sample size, future studies in which more T1D patients are included are required
to shed more light on the association of MDA5 and OAS1 SNPs with T1D, and with the
presence of viral RNA in PBMCs of T1D patients.
Discussion
In this study we demonstrated the presence of enterovirus RNA in blood of 4 out of 10
T1D patients early after onset. Viral RNA was mainly detected in PBMC: Throat samples
were negative and only in 1 case the stool was also positive. An HLA-DR4 allele was
present in all enterovirus-positive patients, yet no obvious link with polymorphisms in
MDA5 or OAS1 was found.
Four out of 10 T1D patients were found positive for enterovirus RNA in PBMCs.
We have used very sensitive methods for virus detection; at least 0.002 to 0.01 TCID50
is detectable with the PCR and NASBA, depending on the enterovirus strain. All patient
samples were tested with 2 different PCRs and NASBA, to confirm the outcome. However,
we can not exclude that the 6 virus-negative T1D patients had RNA levels in their PBMCs
that were below the detection limit of the PCRs and NASBA.
The finding of viral RNA in blood of T1D patients corresponds with results of
previous studies6'9, n'13. Most studies have examined presence of enteroviral RNA in
blood using whole blood, plasma or serum samples. So far, only one study determined
the presence of enteroviral RNA specifically in PBMCs of T1D patients8. Our study shows
115
Chapter 7
that the viral RNA is mainly present in the fraction of PBMCs, as only 2 out of 4 PBMCpositive patients were also positive in plasma. This indicates that the PBMC-fraction may
be the most important fraction to consider when screening for enterovirus positivity in
blood. That viral RNA is mainly detected in PBMCs suggests either infection of cells of the
immune system or uptake of virus-infected cells or cell-debris, e.g. by dendritic cells as
we demonstrated in vitro29. Infection of immune cells versus uptake of virus-containing
material may have different consequences for immune functioning (impairment versus
immune activation). Whether, and how altered immune homeostasis in the blood may
affect immune homeostasis in the pancreas, thereby contributing to T1D development,
requires further investigation.
During the early phase of infection, enterovirus is excreted in throat and
gastrointestinal tract. In this phase, the virus can sometimes also be detected in blood,
but this is highly exceptional and occurs mainly during a severe infection30, 31. We found
no enterovirus RNA in blood of healthy controls, a finding that corresponds with other
reports, where no or very few controls were found enterovirus RNA-positive in blood6, 7
n '13. During convalescence, virus is only detected in stool and fecal excretion can last for
up to 3 months16. Throat- and 3 of 4 stool samples were negative in the 4 T1D patients
that were positive in PBMCs, arguing against acute infection. W hether this concerns late
stage of infection or even a prolonged duration remains to be determined.
Occurrence of prolonged enterovirus infection in T1D patients has also been
suggested by Hyöty and co-workers32 who provided evidence for ongoing enteroviral
infection in gut mucosa of T1D patients. Detection of enterovirus antigens and RNA in
pancreatic islets from T1D patients also suggests inadequate clearance3'5.
Assuming that T1D patients or individuals at risk for T1D have delayed clearance
of enteroviruses, the question raises whether, and which genetic factors predispose to
it. Thereto we selected genetic risk factors for T1D which play a role in antiviral defence
and investigated their linkage with viral presence. The most obvious risk factors are
HLA-DR and molecules of the IFN pathway. It was to be expected that an association
was found with the well known "high risk" alleles DR3/DR4 and DR4/DR4, but a linkage
with one of these phenotypes was not found. DR4 was present in all 4 virus-positive
patients. A previous study reported impaired cellular immune reactivity against CVB4 in
T1D patients, but this was not associated with either HLA-DR3 or HLA-DR433. Published
data is inconsistent regarding HLA and virus positivity: Andreoletti et al. found DR3/DR4
in 2 out of 6 virus-positive T1D patients and 3 carrying a DR3 allele13, whereas Craig et al.
reported that DR3 is significantly less prevalent in virus-positive T1D patients9. Clearly,
further studies are required to address the association, but it seems unlikely that a link
with viral presence will be found.
Among the other genetic risk factors, MDA5 and OAS1 are of ultimate interest,
because they are involved in the innate response against RNA viruses, e.g. enteroviruses.
No major differences were found between the T1D and control group, and between
virus-positive and virus-negative T1D patients in particular. Again, a linkage seems
unlikely, but the sample size is small.
In conclusion, our data indicate that T1D patients may have delayed enterovirus
clearance, with virus detected predominantly in PBMC. No obvious linkage was found
with polymorphisms in MDA5 or OAS1, yet HLA-DR4 was present in all enteroviruspositive patients. Further studies are required to elucidate the intriguing relationship
116
Enterovirus in PBMCs of type 1 diabetes patients
between enterovirus infection, genetic determinants of antiviral immunity and risk of
acquiring T1D.
Acknowledgements
The authors thank Kjeld van Houwelingen (Department of Bloodtransfusion and
Transplantation Immunology, Radboud University Nijmegen Medical Centre, Nijmegen)
for help with HLA-DR typing and Annemieke Boot (Sophia Children's Hospital, Erasmus
Medical Centre, Rotterdam) for contribution to sample collection.
Author Disclosure Statement
No competing financial interests exist.
Funding
This study was supported by the Dutch Diabetes Research Foundation (DFN, pilot grant
2002.11.003), the Juvenile Diabetes Research Foundation (JDRF grant number 24-2008
949) and a grant from the Radboud University Nijmegen Medical Centre (grant number
2005-8).
117
Chapter 7
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
118
H. Hyoty, K. W. Taylor (2002). The role of viruses in human diabetes. Diabetologia, 45, 1353-1361.
M . Roivainen (2006). Enteroviruses: new findings on the role of enteroviruses in type 1 diabetes. Int J Biochem Cell Biol, 38, 721
725.
P. Ylipaasto, K. Klingel, A . M. Lindberg, T. Otonkoski, R. Kandolf, T. Hovi, M. Roivainen (2004). Enterovirus infection in human
pancreatic islet cells, islet tropism in vivo and receptor involvement in cultured islet beta cells. Diabetologia, 47, 225-239.
F. Dotta, S. Censini, A. G. van Halteren, L. M arselli, M . Masini, S. Dionisi, F. Mosca, U. Boggi, A . O. M uda, S. D. Prato, J. F. Elliott, A.
Covacci, R. Rappuoli, B. O. Roep, P. M archetti (2007). Coxsackie B4 virus infection of beta cells and natural killer cell insulitis in recentonset type 1 diabetic patients. Proc Natl Acad Sci U S A, 104, 5115-5120.
S. J. Richardson, A . Willcox, A . J. Bone, A. K. Foulis, N. G. Morgan (2009). The prevalence of enteroviral capsid protein vp1
immunostaining in pancreatic islets in human type 1 diabetes. Diabetologia.
G. B. Clem ents, D. N. Galbraith, K. W. Taylor (1995). Coxsackie B virus infection and onset of childhood diabetes. Lancet, 346, 221
223.
W. Chehadeh, J. W eill, M. C. Vantyghem, G. Alm, J. Lefebvre, P. W attre, D. Hober (2000). Increased level of interferon-alpha in blood
of patients with insulin-dependent diabetes mellitus: relationship with coxsackievirus B infection. J Infect Dis, 181, 1929-1939.
H. Yin, A. K. Berg, T. Tuvemo, G. Frisk (2002). Enterovirus RNA is found in peripheral blood mononuclear cells in a majority of type 1
diabetic children at onset. Diabetes, 51, 1964-1971.
M . E. Craig, N. J. Howard, M. Silink, W. D. Rawlinson (2003). Reduced frequency of HLA DRB1*03-DQB1*02 in children with type 1
diabetes associated with enterovirus RNA. J Infect Dis, 187, 1562-1570.
G. G. Dahlquist, J. Forsberg, L. Hagenfeldt, J. Boman, P. Juto (2004). Increased prevalence of enteroviral RNA in blood spots from
newborn children who later developed type 1 diabetes: a population-based case-control study. Diabetes Care, 27, 285-286.
V. Moya-Suri, M. Schlosser, K. Zimm ermann, I. Rjasanowski, L. Gurtler, R. Mentel (2005). Enterovirus RNA sequences in sera of
schoolchildren in the general population and their association with type 1-diabetes-associated autoantibodies. J Med Microbiol, 54,
879-883.
C. Nairn, D. N. Galbraith, K. W. Taylor, G. B. Clements (1999). Enterovirus variants in the serum of children at the onset of Type 1
diabetes mellitus. Diabet Med, 16, 509-513.
L. Andreoletti, D. Hober, C. Hober-Vandenberghe, S. Belaich, M. C. Vantyghem, J. Lefebvre, P. Wattre (1997). Detection of coxsackie B
virus RNA sequences in whole blood samples from adult patients at the onset of type I diabetes mellitus. J Med Virol, 52, 121-127.
M . Lonnrot, K. Salminen, M. Knip, K. Savola, P. Kulmala, P. Leinikki, T. Hyypia, H. K. Akerblom, H. Hyoty (2000). Enterovirus RNA in
serum is a risk factor for beta-cell autoimmunity and clinical type 1 diabetes: a prospective study. Childhood Diabetes in Finland
(DiMe) Study Group. J Med Virol, 61, 214-220.
M . Lonnrot, K. Korpela, M. Knip, J. Ilonen, O. Sim ell, S. Korhonen, K. Savola, P. M uona, T. Simell, P. Koskela, H. Hyoty (2000). Enterovirus
infection as a risk factor for beta-cell autoimmunity in a prospectively observed birth cohort: the Finnish Diabetes Prediction and
Prevention Study. Diabetes, 49, 1314-1318.
P. W. Chung, Y. C. Huang, L. Y. Chang, T. Y. Lin, H. C. Ning (2001). Duration of enterovirus shedding in stool. J Microbiol Immunol Infect,
34, 167-170.
M . A. Atkinson, G. S. Eisenbarth (2001). Type 1 diabetes: new perspectives on disease pathogenesis and treatm ent. Lancet, 358,
221'229.
H. Ounissi-Benkalha, C. Polychronakos (2008). The molecular genetics of type 1 diabetes: new genes and emerging mechanisms.
Trends Mol Med, 14, 268-275.
F. Cucca, R. Lampis, M. Congia, E. Angius, S. Nutland, S. C. Bain, A . H. Barnett, J. A . Todd (2001). A correlation between the relative
predisposition of MHC class II alleles to type 1 diabetes and the structure of their proteins. Hum Mol Genet, 10, 2025-2037.
J. A . Noble, A . M . Valdes, M. Cook, W. Klitz, G. Thomson, H. A. Erlich (1996). The role of HLA class II genes in insulin-dependent
diabetes mellitus: molecular analysis of 180 Caucasian, multiplex fam ilies. Am J Hum Genet, 59, 1134-1148.
G. Thomson, W. P. Robinson, M . K. Kuhner, S. Joe, M. J. MacDonald, J. L. Gottschall, J. Barbosa, S. S. Rich, J. Bertram s, M . P. Baur, et
al. (1988). Genetic heterogeneity, modes of inheritance, and risk estimates for a joint study of Caucasians with insulin-dependent
diabetes mellitus. Am J Hum Genet, 43, 799-816.
L. L. Field, V. Bonnevie-Nielsen, F. Pociot, S. Lu, T. B. Nielsen, H. Beck-Nielsen (2005). OAS1 splice site polymorphism controlling
antiviral enzyme activity influences susceptibility to type 1 diabetes. Diabetes, 54, 1588-1591.
M . C. Tessier, H. Q. Qu, R. Frechette, F. Bacot, R. Grabs, S. P. Taback, M . L. Lawson, S. E. Kirsch, T. J. Hudson, C. Polychronakos (2006).
Type 1 diabetes and the OAS gene cluster: association with splicing polymorphism or haplotype? J Med Genet, 43, 129-132.
D. J. Smyth, J. D. Cooper, R. Bailey, S. Field, O. Burren, L. J. Smink, C. Guja, C. Ionescu-Tirgoviste, B. W idmer, D. B. Dunger, D. A. Savage,
N. M. Walker, D. G. Clayton, J. A. Todd (2006). A genome-wide association study of nonsynonymous SNPs identifies a type 1 diabetes
locus in the interferon-induced helicase (IFIH1) region. Nat Genet, 38, 617-619.
J. A . Todd, N. M. Walker, J. D. Cooper, D. J. Smyth, K. Downes, V. Plagnol, R. Bailey, S. Nejentsev, S. F. Field, F. Payne, C. E. Lowe, J. S.
Szeszko, J. P. Hafler, L. Zeitels, J. H. Yang, A . Vella, S. Nutland, H. E. Stevens, H. Schuilenburg, G. Coleman, M . Maisuria, W. Meadows,
L. J. Smink, B. Healy, O. S. Burren, A . A . Lam, N. R. Ovington, J. A llen, E. Adlem, H. T. Leung, C. W allace, J. M. Howson, C. Guja, C.
Ionescu-Tirgoviste, M. J. Simmonds, J. M . Heward, S. C. Gough, D. B. Dunger, L. S. Wicker, D. G. Clayton (2007). Robust associations
of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet, 39, 857-864.
N. de Leeuw, W. J. M elchers, A . H. Balk, N. de Jonge, J. M. Galama (1998). No evidence for persistent enterovirus infection in patients
with end-stage idiopathic dilated cardiomyopathy. J Infect Dis, 178, 256-259.
M . Nijhuis, N. van M aarseveen, R. Schuurman, S. Verkuijlen, M. de Vos, K. Hendriksen, A . M. van Loon (2002). Rapid and sensitive
routine detection of all members of the genus enterovirus in different clinical specimens by real-time PCR. J Clin M icrobiol, 40, 3666
3670.
D. J. Smyth, J. D. Cooper, C. E. Lowe, S. Nutland, N. M . Walker, D. G. Clayton, J. A . Todd (2006). No evidence for association of OAS1
with type 1 diabetes in unaffected siblings or type 1 diabetic cases. Diabetes, 55, 1525-1528.
M . Kramer, B. M . Schulte, L. W. Toonen, P. M. Barral, P. B. Fisher, K. H. Lanke, J. M. Galama, F. J. van Kuppeveld, G. J. Adema (2008).
Phagocytosis of picornavirus-infected cells induces an RNA-dependent antiviral state in human dendritic cells. J Virol, 82, 2930
2937.
J. M. D. Galama (1997). Enteroviral infections in the immunocompromised host. REVIEWS IN MEDICAL MICROBIOLOGY 8, 33-40
J. B. W elch, K. M cGowan, B. Searle, J. Gillon, L. M . Jarvis, P. Simmonds (2001). Detection of enterovirus viraemia in blood donors. Vox
Sang, 80, 211-215.
M . Oikarinen, S. Tauriainen, T. Honkanen, S. Oikarinen, K. Vuori, K. Kaukinen, I. Rantala, M. Maki, H. Hyoty (2008). Detection of
enteroviruses in the intestine of type 1 diabetic patients. Clin Exp Immunol, 151, 71-75.
S. Skarsvik, J. Puranen, J. Honkanen, M. Roivainen, J. Ilonen, H. Holmberg, J. Ludvigsson, O. Vaarala (2006). Decreased in vitro type 1
immune response against coxsackie virus B4 in children with type 1 diabetes. Diabetes, 55, 996-1003.
Chapter 8
Summary and Discussion
Chapter 8
Summary
ype 1 diabetes (T1D) is a chronic endocrine disorder in which the insulinproducing ß-cells in the pancreas are destroyed. It is often accompanied by
autoimmunity to ß-cell constituents and is therefore regarded as an autoimmune
disease. Both genetic factors and environmental factors play a role in T1D etiology1.
Enteroviruses, particularly those of the human enterovirus B (HEV-B) species such as
coxsackie B viruses (CVBs) and echoviruses (EVs), are considered to be an environmental
factor in the development of T1D2, 3.
HEV-Bs have been associated with T1D etiology by several findings, including (i)
prospective studies in T1D patients, non-affected siblings and unrelated controls, which
showed increased numbers of HEV-B infections in T1D patients, (ii) case-control studies
which showed the presence of HEV-B RNA in blood of T1D patients at onset of disease,
in the prediabetic stage and in established T1D and (iii) the presence of HEV-B in ßcells of T1D patients at autopsy and their ability to infect and damage pancreatic islets
in vitro 2 3. Several, not mutually exclusive mechanisms have been proposed via which
these viruses may initiate or accelerate T1D, (i) HEV-Bs can directly infect the pancreatic
ß-cells and destroy them by their lytic life cycle, (ii) HEV-B induced inflammation results
in bystander activation of innate immune components resulting in chronic inflammation
which is harmful for ß-cell function and viability, (iii) autoimmune responses develop in
the pro-inflammatory microenvironment of the infected pancreatic islets, (iv) molecular
mimicry, whereby immune responses directed against the virus also recognize self
antigens and therefore induce autoimmunity4.
Inflammation in pancreatic islets is common in type 1 diabetes patients, and
immune cells, such as T cells, macrophages and dendritic cells can be detected in the
islets of type 1 diabetes patients5. The development or acceleration of type 1 diabetes
might depend on the balance between autoreactive CD4+ and CD8+ effector T cells and
regulatory T cells (Treg); a balance which is predominantly decided by dendritic cells
(DCs). DCs are the professional antigen-presenting cells (APCs) of the immune system
and play a decisive role in initiating immune responses and maintaining self tolerance.
They do not only participate in innate immunity, but also initiate and control adaptive
immunity6.
In order to preserve tolerance to self, but fight invading pathogens, DCs need
to distinguish between Ags in dangerous or steady-state conditions. To this end, DCs
express a variety of pattern recognition receptors (PRRs), that sense pathogen-associated
molecular patterns (PAMPs), such as viral double-stranded RNA (dsRNA), or dangerassociated molecular patterns (DAMPs)7, 8. Upon triggering of these PRRs, the DC will
start a process called maturation, which includes phenotypical and functional changes.
Mature DCs are able to generate immune responses via the activation of T cells, whereas
immature DCs or DCs receiving anti-inflammatory signals in general induce tolerizing
responses when encountering T cells6, 9.
T
120
Sum m ary and Discussion
Summary of main findings
In this thesis, the interaction between pancreatic islets, enteroviruses and DCs has been
explored in order to shed light on the putative mechanism of HEV-B-induced T1D.
As stated above, sensing of pathogens or pathogen-associated danger through PRRs is
crucial for DCs to determine whether immune responses need to be initiated. In light
of this, chapter 2 gives a concise overview of the expression of different PRRs that are
involved in viral RNA sensing in DC subsets under pro-inflammatory and steady-state
conditions. We focussed on viral RNA sensors, such as Toll-like receptor (TLR) 3, 7 and
8, and RIG-I and Mda5. Furthermore, cross-talk between different DC subsets was
investigated and a mechanism by which plasmacytoid DCs (pDCs) protect myeloid DCs
(mDCs) from viral infection via the production of IFNs is described. Chapter 3 deals with
the susceptibility of DCs to infection with HEV-B species. CVBs were unable to infect
DCs or influence their function, probably due to lack of the viral entry receptor, CAR
(coxsackie and adenovirus receptor). EVs, on the contrary, could productively infect
DCs, resulting in loss-of-function, such as diminished responses upon subsequent TLRtriggering and ultimately loss of viability. Chapter 4 reveals that DCs can be protected
from infection when matured with the double-stranded RNA (dsRNA) analogue poly I:C.
However, DCs matured with other TLR-ligands were not protected from infection. dsRNA
is formed in HEV-B-infected cells during virus replication, and we provide evidence that
CVB-infected cells are efficiently phagocytosed by DCs leading to upregulation of type
I interferons (IFNs) and IFN-stimulated genes (ISGs) resulting in an antiviral state, that
also protects DCs from subsequent infection. In chapter 5 the interaction between CVBinfected cells and DCs is further explored, with a particular focus on the interaction
between primary human pancreatic islets and DCs. We report that human pancreatic
islets are efficiently phagocytosed by DCs, and this also holds true for porcine islets and
the murine insuloma cell line Min6. Uptake of CVB-, but not mock-infected cells resulted
in the induction of ISGs and offered DCs protection from subsequent EV-infection.
This required the presence of viral RNA within CVB-infected islets, and furthermore
depended on production of IFNs by the DCs. These findings show that antiviral immune
responses are generated by DCs upon encountering HEV-B-infected islets, and provide
important new insights in the possible role of DCs in T1D development. In chapter 6 we
examined the direct responses of pancreatic islets to HEV-B infection. Primary human
islets that were infected with HEV-B induced antiviral immune responses, as indicated
by the production of ISGs. Furthermore, mRNA expression of several cytokines and
chemokines was induced, and importantly, these were also detected in the supernatant
from infected islets. These data imply that islets, upon infection with HEV-B species,
start antiviral immune responses and produce a variety of cytokines and chemokines
that can attract and/or activate components of both the innate as well as the adaptive
immune system. Although generated in order to control viral infection, these responses
may under certain circumstances maintain or aggravate inflammation and might even
trigger development of autoimmune processes against ß-cells.
Imbalance in the immune system may play an important role T1D development,
and although the pancreatic cells are targeted during T1D, players outside the pancreas
can be involved as well. Chapter 7 focuses on the presence of enteroviruses in PBMCs
of T1D patients. We show that enterovirus RNA can be detected in 4 out of 10 T1D
121
Chapter 8
patients, but not in any of the controls. Merely complete absence of viral RNA in throat
and stool samples suggests that the presence of RNA in PBMCs may concern prolonged
enterovirus infection. What the role of prolonged infection in T1D is, remains to be
determined; however, the continuous immune stimulation that this prolonged infection
entails, could affect the balance in the immune system.
Putative mechanism of HEV-B-induced type 1 diabetes
Here, a putative model for HEV-B induced T1D is proposed and discussed in relation to
the data presented in this thesis and existing data. The model will be shortly introduced
and the separate steps in the putative disease process will be further addressed in a
step-wise manner. Although I will focus on the role of HEV-B in T1D, this does not exclude
the existence of other possible triggers in T1D etiology.
Increasing evidence suggests that HEV-B infection and subsequent ß-cell death
is involved in T1D etiology, and infection of the pancreatic islets may be the initiating
step in HEV-B induced T1D. Based on this assumption and the results from this thesis we
propose a putative model for HEV-B induced T1D that originates at infection of islets (Fig.
1). Infection of islets by HEV-B will result in rapid replication of the virus, and host-cell
modifications will be induced by the viral proteins leading to cell damage and ultimately
cell death (Fig 1., step 1). The resulting inflammation causes ß-cell damage, and will
attract various immune cells. Upon activation, these will also produce cytokines and
thereby mediate further ß-cell damage and inflammation (Fig 1., step 2, 3). Infection
and inflammation also facilitate development of autoimmune responses, as DCs will be
attracted to the islets. They will phagocytose HEV-B infected ß-cells and start maturation
after sensing PAMPs and DAMPs in the infected ß-cells and in the microenvironment.
Additional signals, such as pro-inflammatory cytokines from surrounding pancreatic cells
and immune cells may add to the maturation process (Fig 1., step 4, 5). Matured DCs will
migrate to the draining lymph nodes where they will activate (autoreactive) T cells in a
susceptible host. Activated, autoreactive T cells subsequently migrate to the islets where
they initiate autoimmune processes that facilitate destruction of ß-cells, ultimately
resulting in clinical T1D (Fig 1., step 6, 7). Below, the several steps of the proposed model
will be discussed with regard to the data described in this thesis and existing data in
literature.
Step 1: HEV-B infection of pancreatic ß-cells
The first step in our model is the infection of pancreatic islets with HEV-Bs. We and
other groups have shown that human pancreatic islets can be infected with CVBs and
other HEV-Bs in vitro (Chapter 5 and 6 and references10-12). In line with this, expression
of several HEV-B virus receptors, such as CAR and the integrin a vß3 in pancreatic islets
has been reported12, 13.
Importantly, evidence exists that HEV-B infections also occur in T1D patients in
vivo. Viral RNA and viral proteins can be detected in the islets of T1D patients, whereas
this is not the case for healthy controls13-16(Fig 2). This raises the question how HEV-B can
spread to the pancreatic islets. HEV-Bs spread via the fecal-oral route and their primary
replication occurs in the gut. From the gut, a direct connection with the pancreas exists:
the pancreatic duct, from where pancreatic enzymes are released into the digestive tract
122
Sum m ary and Discussion
Figure 1. Putative mechanisms of HEV-B-induced T1D.
Virus infection of pancreatic islets (1) results in the production of cytokines and chemokines that induce
an antiviral state but may also have damaging effects on ß-cells (2). Various immune cells, including macro
phages, NK cells and DCs are attracted and activated due to the infection and cytokines produced by these
cells can have adverse effects on ß-cell function and viability (3). Furthermore, NK cell-mediated killing of
infected ß-cells may occur (3). DCs phagocytose infected ß-cells and get activated by the signals provided by
the infected cells (e.g. viral RNA and other PAMPs and DAMPs)(4). Additional influence on DC maturation is
exerted via surrounding immune cells (macrophages, NK cells), duct cells, and the pro-inflammatory environ
ment that has arisen (5). Maturing DCs migrate to the draining lymph nodes, where they activate autoreactive
T cells ( 6 ). Activated, autoreactive T cells subsequently migrate to the islets where they initiate autoimmune
processes that facilitate destruction of ß-cells, ultimately resulting in clinical T1D (7).
and via which the virus may reach the pancreas. Interestingly, prolonged HEV-B infection
in the gut has been suggested to occur in T1D patients, and the gut may thus provide
a HEV-B reservoir17. Alternatively, virus can spread via the blood stream (viremia), and
thereby target secondary organs, including the pancreas. During severe infections in
neonates, virus is known to infect the pancreas, causing pancreatitis. Viremia is common
during severe infections, and blood may thus be the transport route of the virus.
Interestingly, in T1D patients, or prediabetic individuals (at risk to develop T1D), HEV-B
123
Chapter 8
can be detected in blood, and virus may spread to the pancreas via this route.
HEV-B infection of particularly ß-cells within the pancreatic islets, has been
shown by Dotta and colleagues (Fig. 2), and was also suggested by Richardson e t a/.14,
15. This suggests that ß-cells might be the primary target of HEV-B, and could explain
why ß-cells are destroyed in stead of a-cells, 5-cells or PP-cells for example. Infection
of ß-cells may furthermore stimulate autoimmune responses against ß-cells, as more
ß-cell associated Ags may be released and/or presented in the presence of danger
signals. Additionally, ß-cells are sensitive for cytokine-induced cell death (discussed in
the section "Toxic effects o f p ro -in flam m ato ry cytokines and chemokines on ß-cells"),
and this may also add to specific destruction of ß-cells, but not other islet cells. That ßcell damage and cell death may be the initial step in T1D etiology is further supported
by studies using the drug streptozotocin (STZ). This drug induces cell death, particularly
of ß-cells, and administration of multiple low doses of STZ induces immune aggression
against ß-cells and development of autoimmune T1D18, 19.
Step 2: Production of inflam m atory mediators in the pancreas
Interferons: a tw o-sided sword?
Infection of pancreatic islets will result in rapid virus replication and antiviral responses
will be induced in the islets, such as the production of type I IFNs. These IFNs are an
important first defense from the host against viruses. IFNs induce antiviral responses in
an autocrine and paracrine manner and thereby restrict virus replication in primed cells.
IFNs can be detected in the islets of T1D patients but not of controls, and this may reflect
a response to virus infection in T1D15, 20, 21. That the IFNs are critical for host defense
is shown by Flodström and colleagues who reported that mice with a dysfunctional
IFN-response in their ß-cells develop rapid and fullblown diabetes upon CVB infection,
due to complete destruction of ß-cells22, 23. This may represent the type 1B diabetes, in
which rapid decrease of ß-cell mass is observed, which could be the result of massive,
unrestricted virus replicaton in ß-cells. Clearly, massive virus replication is inhibited
Fig. 2. Enteroviral infection of pancreatic ß-cells.
Confocal microscopy images from islets of Langerhans from a type 1 diabetes patient demonstrate that ßcells (A-C), but not a-cells (D-F), are positive for VP-1. Cells stained in green are positive for insulin (A and C)
and glucagon (D and F), those stained in red are positive for VP-1 (B, E, and F), and those stained in yellow are
double-positive cells for insulin and VP-1 (C). (Scale bars: 18^m.) Reprinted from Dotta et al., PNAS 2007 with
permission from the authors, © 2007 by The National Academy of Sciences of the USA.
124
Sum m ary and Discussion
by IFNs. However, IFNs can work as a two-sided sword; excessive IFN-stimulation can
stimulate the induction of diabetes. Prolonged administration of IFNs, for example to
individuals with chronic hepatitis infection, may cause overt diabetes (reviewed by
Devendra & Eisenbarth24). How IFNs mediate T1D induction is unclear. One possibility
is direct negative effects of IFNs on ß-cell function by inhibition of insulin production
and secretion25, 26. In this situation the ß-cells will be continuously stimulated to produce
more insulin, and this results in cell stress such as ER-stress, which can lead to cell death.
Indirect effects of IFNs on islet function or viability are the induction of cytokines and
chemokines that can subsequently affect islets (discussed in the section "Toxic effects
o f p ro -in flam m ato ry cytokines and chemokines on ß-cells"). Furthermore, IFNs can also
mediate the chemotaxis of several leukocytes, and stimulate their activation, survival
and proliferation27-30. Another way how IFNs can promote disease development is
via stimulation of the adaptive immune system. IFNs differentially affect DC function
and maturation depending on the time, amount and duration of IFN-stimulation31-34.
Additionally, IFNs were shown to be crucial for autoimmune transition in mice with
autoreactive T cells35. Furthermore, IFNs play an important role in systemic lupus
erythematosus (SLE) development via their actions on DCs36-38. Thus IFNs could take
part in diabetes development via several ways, yet the exact mechanism remains to be
elucidated.
Although IFNs are produced in response to viral infection of pancreatic islets
in all individuals, it is currently unknown why some individuals develop T1D, whereas
others do not. One of the underlying reasons might be w hether prolonged, or chronic
IFN production occurs, and this may be directly related to the prolonged or chronic
presence of HEV-B. Both successive as well as prolonged or chronic HEV-B infections
have been suggested to occur more often in T1D patients than healthy controls (Chapter
7 and references17, 39). The production of IFNs in the islets prevents rapid virus-induced
cytolysis and will largely restrict virus replication. But in this situation, the virus may
persist and replicate at low levels, thereby maintaining continuous IFN production that
mediates T1D induction. Additionally, DCs that encounter HEV-B infected islets will also
produce IFNs (Chapter 5), thereby possibly contributing to IFN-mediated ß-cell damage.
Differences in genetic background of individuals also influence antiviral responses
(discussed in the section "Predisposition to T1D").
Toxic effects o f p ro -in flam m ato ry cytokines and chemokines on ß-cells
Virus infection of pancreatic islets results in the production of several pro-inflammatory
cytokines and chemokines (Chapter 6), and as already noted above, virus-induced IFNs
can further stimulate the production of several cytokines and chemokines (Chapter 6 and
references40-44). These cytokines and chemokines serve to start inflammatory processes
and attract immune cells in order to fight virus infection, yet they can have adverse
effects on ß-cell function and viability. TNF-a, IL-1ß and IFN-y, for example, are toxic to
ß-cells either alone or in combination45-48. Thus virus-induced cytokine production may
contribute to ß-cell death.
Step 3: Chemoattraction and activation of incoming immune cells and progression to
chronic inflammation
HEV-B induced cytokines which are produced upon infection of islets include several
chemokines, such as IP-10, RANTES, IL-8, eotaxin and others (Chapter 6). These
125
Chapter 8
chemokines will mediate the chemoattraction of migratory immune cells via binding of
the corresponding chemokine receptor. Several different immune cells will be attracted
by the above-mentioned chemokines, and these include monocytes, macrophages, T
lymphocytes, NK cells and DCs27, 49.
Immune cells that have migrated towards the inflamed, infected pancreas can
be activated by cytokines that are produced in the pancreas. For example, IFNs and IL15 are known to stimulate NK cell activity27, IL-8 activates neutrophils49, and IFN-y and
TNF stimulate macrophage activity and nitric oxide production. Activated immune cells
produce additional pro-inflammatory cytokines and other inflammatory mediators such
as nitric oxide, that are toxic to ß-cells, and this process may be aggravated due to the
pro-inflammatory microenvironment that has arisen. PAMPs, DAMPs and (modified)
Ags that are released from (infected) dying ß-cells can contribute to excessive activation
of immune cells leading to a vicious circle of enhanced inflammation, continued ß-cell
death, and release of more inflammatory mediators. When inflammation is not put to
a stop, ß-cell mass might further decrease until clinical T1D arises. When on the other
hand inflammation declines and ß-cell proliferation is stimulated, the homeostasis in the
islets may slowly return and ß-cell mass might be largely restored, without transition
to clinical T1D50. What determines whether inflammation is put to a halt is not exactly
known, but prolonged and/or successive infection may play a role (discussed in the
section "Interferons: a tw o-sided sw o rd ?'), and furthermore, the genetic background of
an individual is important, as will be discussed below.
Step 4: Phagocytosis o f infected ß-cells by DCs
DCs are critical players in both innate and adaptive immunity and are crucial to maintain
tolerance to self. In human pancreatic islets DCs are present in low numbers under
steady-state conditions; however, as ß-cell destruction ensues leading to T1D there is
an increase in DC-infiltrate5, 51. In chapter 4 and 5 it is shown that DCs can phagocytose
HEV-B infected cells, and importantly, also pancreatic islets are efficiently phagocytosed.
We showed that upon engulfment of infected cells, the DCs will start innate responses
such as IFN production. DCs may also produce other cytokines and chemokines upon
engulfment of infected islets, although this has not been studied. Induction of innate
responses depended on the presence of (ds)RNA in the HEV-B infected cells, suggesting
that dsRNA intermediates formed during virus replication may serve as a PAMP.
That phagocytosis of infected ß-cells may be an important event in T1D etiology is
further supported by a mouse study from Horwitz and colleagues. They showed that
phagocytosis of CVB-infected ß-cells by APCs is crucial for the induction of T1D. Although
caution should be taken when interpreting mouse data due to the differences that exist
between mice and humans (see "Future Challenges and Treatment of T1D"), these data
do support our model.
It is currently unknown what signals on islets/ß-cells facilitate their uptake by
DCs. Several "eat-me" signals have been described, such as phosphatidyl serines, which
are expressed on apoptotic and/or necrotic cells52, 53. It is known that under steady-state
conditions, antigens from ß-cells are phagocytosed by APCs that subsequently migrate
to the draining lymph nodes54, 55. Presentation of ß-cell peptides under steady-state
conditions results in deletion of autoreactive T cells and prevents the development of
T1D56-59.
126
Sum m ary and Discussion
Step 5: The difficult decision a DC has to make
W hether a DC will induce immune responses or tolerance depends on the maturation
status of the DC, which is influenced by PRR-stimulation and other signals from the
microenvironment. Viral RNA, viral proteins, modified host proteins and other virusassociated PAMPs and DAMPs may all contribute to maturation induction. Preliminary
data revealed that DC maturation does not necessarily occur upon in vitro phagocytosis
of HEV-B-infected cells (Chapter 5). A reason for the observed lack of maturation can be
the presence of conflicting signals within the infected cells. Although viral PAMPs and
DAMPs contribute to maturation induction, other signals may inhibit DC maturation.
For example, apoptotic cells are generally considered to inhibit DC maturation60, 61,
and apoptotic hallmarks are observed in enterovirus-infected cells62, 63. Additionally, in
the past years it has become evident that phenotypically mature DCs can also induce
tolerance and vice versa, thus the picture on DC maturation is not fully complete64, 65.
In order to understand the interaction between DCs and CVB-infected islets and the
subsequent (auto)immune responses, further dissection of the players that dictate
immunogenicity is required. These include viral PAMPs and DAMPs, but also signals
derived from damaged (infected) ß-cells. W hether a particular (self)Ag will be presented
by a mature DC may even be determined by how and where the Ag and these different
signals are sensed inside the DC66.
It should be taken into account that the encounter of infected ß-cells in the
pancreas occurs in an environment where DCs and HEV-B-infected ß-cells are not the
only cells present. Signals from the microenvironment greatly influence DC maturation.
For instance, DAMPs associated with damaged ß-cells, such as high-mobility group box
1 (HMGB1), can influence the DC. Maturation can furthermore be influenced by proinflammatory cytokines produced by surrounding immune cells, infected duct cells
or endothelial cells. Duct cells, for example, produce TNF-a upon CVB-infection (G.
Vreugdenhil, unpublished observation), and CVB-infected endothelial cells produce IL1ß, IL-6, IFNs and others67. These cytokines may add to the process of DC maturation.
Furthermore, also cell-cell contact-dependent signaling influences DCs68. Future
studies aimed at dissecting the requirement for DC maturation upon phagocytosis of
CVB-infected islets could provide insight in the mechanisms underlying T1D etiology.
Monitoring DC-responses upon addition of particular cytokines or (virus-stimulated)
leukocytes to co-cultures of DCs and CVB-infected islets are a good option to investigate
the human situation. This will provide important insight in the role of DCs in the disease
process, but may also yield new targets to interfere with autoimmune induction.
Virus infection not only affects ß-cell function and viability, but can also affect
DCs. EVs, but not CVBs, are able to infect and replicate in DC in vitro, thereby disabling DC
responses and resulting in cell death (Chapter 3). Further studies revealed that IFNs can
protect DCs from EV-infection, and also phagocytosis of HEV-B infected cells results in the
protection of DC from subsequent infection (Chapter 2, 4 and 5). W hether EV infection
of DCs occurs in the pancreas in vivo and how it could contribute to T1D development is
currently unknown. However, the production of IFNs by infected islet cells may provide
some means of protection of DCs that migrate into pancreatic islets. Therefore, it seems
unlikely that direct EV infection of DCs will play a major role in T1D etiology in humans.
Moreover, CVBs are unable to infect DCs and are associated with T1D as well.
127
Chapter 8
Step 6: The induction of autoim m unity
DCs that have phagocytosed damaged (HEV-B infected) ß-cells migrate to the draining
lymph nodes. Depending on the maturation status of the DC, it will either stimulate
corresponding T cells, or induce tolerance. Responses against viral Ags will be generated,
and because (modified) self-Ags are phagocytosed and presented by these DCs,
autoimmune responses may be provoked. This also depends on the T cell repertoire of
the host. W hether autoreactive T cells are activated by DCs that have phagocytosed HEVB infected, damaged ß-cells, has not been investigated so far. One of the future challenges
will be to determine w hether this occurs, what the requirements for activation are, and
if, and how this may be inhibited or prevented in individuals at risk to develop T1D.
Both activated autoreactive CD8+ effector T cells and Tregs can be found in
the pancreas of T1D patients69. The balance of different T cell subsets, such as CD4+
and CD8+ effector T cells and Tregs, in the pancreas is critical in the development of
autoimmunity70. Therefore, not only the induction of autoreactive T cells on itself, but
also the presence and number of Tregs determines w hether an individual will develop
autoimmune T1D or not.
Step 7: Full-blown autoim mune responses in the pancreas
Once autoreactive immune cells are activated, they will start proliferating and migrate
towards the pancreas. Upon arrival in the islets, autoreactive T cells will recognize
and kill ß-cells that express the particular self-Ag. This dramatically reduces ß-cell
mass, and will additionally result in the accumulation of apoptotic ß-cells. Self-Ags can
be modified during the process of apoptosis, and this provides new self-Ags that can
aggravate the autoimmune process. Furthermore, dying ß-cells may undergo secondary
necrosis, thereby releasing PAMPs and DAMPs that potentiate the (innate and adaptive)
inflammatory processes in the islets.
Controversy remains as to whether adaptive immune responses are required
for T1D development, or are merely an effect of the disease process71. If autoimmunity
is not required, the strong association of HLA, PTPN22 and CTLA4 with T1D will still have
to be explained. The involvement of autoimmune processes may speed up the process
of ß-cell damage and can strengthen the vicious circle of ß-cell death. Thus, adaptive
immune mediated responses may potentiate inflammation and disease progression.
Presence of enterovirus in blood: a role in T1D etiology?
Local imbalance in immune homeostasis in the pancreatic islets may be a critical factor
in the development of T1D, and this can be initiated by enterovirus infection of the islets.
This does not exclude that cells and signals from outside the pancreas can influence
homeostasis in the pancreas. This is fortified for example by the altered cytokine levels
of IP-10 and IFN-a in the serum of T1D patients72-74. It is unlikely that events outside
the pancreas, such as altered immune homeostasis in the blood, are the major events
in T1D initiation, because they cannot explain why specifically the ß-cells, and not cells
in the kidney, liver or other organs are destroyed. Thus, even though alterations in the
remainder of the body could largely contribute to T1D, events in the ß-cells probably
initiate T1D development. The increased cytokine production in blood of T1D patients
may prime immune cells that subsequently migrate into the pancreatic islets, which may
128
Sum m ary and Discussion
alter the responses of these immune cells once they encounter infected or damaged
ß-cells. The source of the enhanced serum-cytokines is not well-defined, and could
originate from tissues which secrete cytokines into the blood stream, but they may also
be produced by PBMCs in the blood. In this regard, it is interesting that HEV-B RNA can
be detected in PBMC and serum of T1D patients (discussed in chapter 7). This raises two
questions, i) whether and how these viruses can infect immune cells and ii) what the
responses of PBMCs are upon infection.
With regard to the first question, it is known that PBMCs can not be directly
infected with coxsackieviruses in vitro75'77. However, Fcy-receptor (FcyR)-mediated
uptake of coxsackievirus-antibody complexes by PBMCs, monocytes and pDCs has
been reported78, 79 and could be in place during viremia. Alternatively, (prolonged) local
enteroviral infection, such as described in the intestine of T1D patients17 might serve as
a virus reservoir, from which several PBMCs (e.g. monocytes, macrophages, DCs) might
phagocytose virus-containing material. The detection of enterovirus RNA in peripheral
blood may thus reflect antibody-dependent infection of immune cells or uptake of
particles/RNA in the absence of active virus replication within PBMCs.
With regard to the second question, FcyR-mediated Ab-dependent activation of
PBMCs, monocytes and pDCs, results in IFN-a production78, 79. This has been confirmed
in our laboratory using PBMCs and pooled human serum containing anti-CVB Abs. We
observed production not only of IFN-a, but many other pro-inflammatory cytokines and
chemokines, such as IL-6, IL-8, IP-10, MIP-1ß and others upon stimulation of PBMCs with
CVB in the presence of human serum (unpublished observations). Thus presence of virus
in the blood provokes inflammatory responses which can influence homeostasis of the
immune system. Upon phagocytosis of infected cells by blood cells, pro-inflammatory
cytokines and inflammatory mediators may also be produced. We have described the
induction of IFNs and ISGs in DCs upon phagocytosis of infected cells (Chapter 4 and 5),
and also macrophages and monocytes can respond to infected cells with the production
of cytokines such as IL-1ß, IL6 and TNF-a and inflammatory mediators such as nitric
oxide. To recap, interactions between enteroviruses and PBMCs may result in immune
activation in which cytokines such as IFNs are produced. Thus although the local events
in the islets may be critical in T1D development, inflammatory processes outside the
pancreas may also influence the disease process.
P re d is p o s itio n to T 1D
One of the major unanswered questions that remains is: Who develops T1D? In our
proposed model, T1D will arise/persevere due to flaws in restraining inflammation.
Some important questions in this context are i) Why is inflammation not restrained? ii)
Why does autoimmunity develop, in other words, how is peripheral tolerance broken?
It will be a major challenge to answer these questions, because the answers probably
depend on both the complex genetic background of people at risk for diabetes and a
combination of environmental factors such as when and how many encounters with
HEV-Bs an individual will face. Below some of the genetic factors that are involved in T1D
etiology will be discussed.
Altered virus clearance could well play a role in T1D development, since prolonged
or successive HEV-B infections are associated with T1D (chapter 7 and references17, 39).
129
Chapter 8
As discussed above, this may potentiate prolonged or chronic IFN stimulation, which
can add to T1D development (section "Interferons: a tw o-sided sw o rd ?'). With regard
to the putative role of HEV-B in T1D development, it is interesting that single nucleotide
polymorphisms (SNPs) have been identified in genes which are involved in the innate
antiviral response. Several SNPs that alter the risk to develop T1D have been found in
the Mda5 gene80-82. The Mda5 protein is a RIG-I-like helicase (RLH) that is involved in the
recognition of enterovirus RNA and induces downstream signaling and IFN production
(S. Hato, unpublished data). Because it is crucial for enterovirus sensing, it may be an
important gene in HEV-B-induced T1D. Alterations in Mda5 expression levels or function
may have massive consequences for timing and amount of IFNs that are produced,
and may therefore influence the antiviral response. A study by Liu et a/. suggests that
people with increased risk for T1D have higher expression levels of Mda5, and this may
result in increased IFN production81, 83. This can add to T1D etiology via several ways, as
described above. On the other hand, diminished Mda5 function can result in suboptimal
antiviral responses, and may induce prolonged or chronic infections, which can also be
detrimental. Several polymorphisms in Mda5 have been described, and it is still largely
unknown if and how they affect the antiviral responses and which SNP (or combination
of SNPs) may be most critical for T1D predisposition84. New directions for future studies
include investigating whether the identified SNPs confer increased risk for prolonged or
successive virus infections, and whether altered IFN responses are found in individuals
that carry these SNPs upon encountering HEV-Bs.
Another antiviral gene that has been associated with T1D is OAS1, the protein
that activates RNaseL upon binding of dsRNA and thereby initiates degradation of cellular
and viral RNAs, although this association was not found in all studies85-87. Particular SNPs
in OAS1 are known to alter OAS1 splicing and could thereby affect prevalence of OAS
isoforms, which may influence antiviral responses88. Additionally, OAS1 levels are elevated
in T1D patients, suggesting that OAS1 plays an important role in disease development89,
90. Increased OAS1 levels could be the result of (prolonged) HEV-B infection. Thus, SNPs in
genes that are involved in antiviral defense may affect viral clearance and could thereby
play a role T1D etiology.
In chapter 7 we studied the prevalence of two SNPs in the above-mentioned
genes in a small cohort of T1D patients and unrelated controls. We divided T1D patients
in two groups, those where enteroviral RNA was detected in their PBMCs, and those
that were negative for enteroviral RNA. We did not find any clear association of either
SNPs with virus positivity or T1D, but our cohort was small. Large-scale patient-control
studies in which positivity for viral RNA in PBMCs is determined, as well as an individuals'
response to HEV-B will shed more light on the role of Mda5 and OAS1 in T1D etiology.
Many other gene-associations have been proposed that confer risk to T1D91,
92. Among those are loci which are involved in adaptive immunity, such as those that
shape the T cell repertoire (HLA-locus), and that influence T cells activation (e.g. CTLA4,
PTPN22)93-96, implying that autoimmunity does play an important role in T1D etiology.
Furthermore, several SNPs have been identified in cytokines and chemokines, that may
contribute to enhanced inflammation. For instance, T1D-associated SNPs are found in
RANTES, where protective alleles correlate with lower levels of RANTES in serum97. This
implies that people which carry the predisposing alleles have higher RANTES levels, and
this may contribute to excessive inflammation. A likewise scenario may hold for other
inflammatory genes in which susceptibility loci are found, such as TNF-a and others98,
130
Sum m ary and Discussion
99. Additionally, these cytokines and chemokines are (indirectly) involved in clearance of
viral infection, and SNPs that alter protein function or expression could thus influence
viral clearance.
It is clear that multiple different genes and loci are involved in T1D development,
and that only part of the polymorphisms involved has been discovered. Since there is
not one specific diabetes gene, "wrong" combinations of several polymorphisms may
in the end be responsible in determining whether an individual develops T1D or not.
Besides genetic factors, also age and immune-status of the individual (e.g. lymphopenia)
may play a role100-102. Future studies that combine several SNPs in their analysis and that
will determine functional characteristics such as protein expression in parallel may shed
more light on which genes make up this "wrong" combination.
Future Challenges and Treatment of T1D
The biggest challenge obviously is to find a way to prevent clinical T1D, and in order to
do so, it will be important to identify the cause(s) of T1D, to know how initiation and
progression of disease are induced, and to know if and how autoimmunity is involved
in disease development. Much data is available on (CVB-induced) T1D pathogenesis in
mice, and this is extrapolated to the human situation. However, inter-species differences
exist103, 104and therefore, mouse data cannot blindly be extrapolated to humans. Therefore,
studies with human material, such as pancreas material from biopsies or autopsies of
patients with clinical T1D and from "pre-diabetic individuals" is extremely valuable.
Future studies that further investigate the presence of HEV-B in the pancreas, or the
composition of mononuclear cells greatly add to our view of human T1D pathogenesis
even though some contradictions on the observed cell types have been reported5, 15, 69, 105,
106. A complicating factor is the long pre-clinical phase, which makes it largely impossible
to investigate composition of infiltrates at the initiating events and early phases of the
disease. In this regard, another challenge will be to establish methods to identify T1D
patients, or individuals at risk in an early stage of disease development. (Case-) reports
of early and/or preclinical T1D may shed light on the events that occur in the pancreas
before clinical T1D, and on the immune cells that are involved.
Vaccination against HEV-Bs?
HEV-Bs are considered to be triggers that can initiate or accelerate T1D. In that regard,
some researchers are in search of the HEV-Bs that are "diabetogenic", i.e. those that
can trigger/accelerate T1D, whereas other HEV-B strains cannot83, 107, 108. Vaccination
against those diabetogenic viruses early in life may prevent initiation/acceleration of
T1D. However, several different HEV-Bs were isolated from T1D patients. Additionally,
various different HEV-Bs have been associated with T1D on the basis viral RNA sequences
yielded after RT-PCR11, 74, 107, 109, 110. Moreover, most HEV-B species are capable to replicate
in human islets in vitro, resulting in impaired function and ß-cell death10, 111. Furthermore,
HEV-Bs can be made more diabetogenic by undergoing several rounds of replication in
vivo in the pancreas, or in vitro in islets, suggesting that all HEV-Bs have diabetogenic
potential112. Thus, there may not be one - or a small group of - diabetogenic viruses.
If vaccination studies would be commenced, which viruses should be included? And is
it feasible to vaccinate against various HEV-Bs, in addition to the currently conducted
131
Chapter 8
vaccinations against mumps, measles, rubella, polio etc? Who has to be vaccinated? I
believe vaccination against HEV-Bs may not be the best solution, development of more
reliable screening methods, and earlier interference in individuals developing T1D may
be a better option.
How to intervene w ith T1D?
As already shortly mentioned above, an important unanswered question is whether
it is possible to stop and/or reverse the ß-cell mass decrease. Restoration of immune
balance might be realized via the inhibition of inflammatory processes within the islets.
An additional difficulty is that this should preferably be done in the islets only, without
systemic inhibition of inflammation in order to maintain immune homeostasis in the
rest of the body and to prevent opportunistic infections. Furthermore, if autoimmune
responses have developed, inflammation inhibition in the pancreas may not be sufficient
to restore homeostasis, because T cell mediated ß-cell killing will reinitiate inflammation
again. Thus besides restriction of inflammation, also restoration of tolerance to ß-cells
may be important. The latter might furthermore be important regarding the regeneration
of ß-cells or transplantation of islets, where continuous autoimmune-mediated attacks
on ß-cells may reduce ß-cell mass again and thus interfere with insulin production.
Several studies have already been inititated to halt autoimmunity. Among those are
studies trying to eliminate autoaggressive T cells113, 114, attempting to regain tolerance to
particular self-Ags115, 116, and studies that try to regain the balance in the immune system
via tolerization of DCs in vitro117. In my opinion the best option available so far would be
the attempt to generate Ag-specific tolerance-inducing DCs. This approach deals with the
autoimmunity problem at its basis and therefore may have the best chances of success.
Besides, tolerance to multiple antigens may be achieved, a benefit when compared to
the "tolerance-to-1-antigen approaches". Furthermore, immune homeostasis may be
regained due to possible induction of regulatory T cells, making this a preferred method,
compared to depletion of T cells. Future studies using human pancreatic islets and human
DCs may give important insights of their role and function in T1D and may provide more
means that can be used to steer the immune system towards control over inflammation
and autoimmunity.
132
Sum m ary and Discussion
References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
35.
36.
37.
38.
M . Knip, R. V eijola, S. M . V ïrtanen, H. Hyoty, O. Vaarala, H. K. A kerblom (2005). Environmental triggers and determinants of type 1
diabetes. Diabetes, 54 Suppl 2, S125-136.
H. Hyoty, K. W . Taylor (2002). The role of viruses in human diabetes. Diabetologia, 4 5 , 1353-1361.
R. Varela-Calvino, M . Peakman (2003). Enteroviruses and type 1 diabetes. Diabetes M etab Res Rev, 19, 431-441.
M . Roivainen (2006). Enteroviruses: new findings on the role of enteroviruses in type 1 diabetes. Int J Biochem Cell Biol, 38, 721
725.
S. Uno, A . Imagawa, K. Okita, K. Sayam a, M . M oriw aki, H. Iw ahashi, K. Yamagata, S. Tam ura, Y. M atsuzawa, T. Hanafusa, J.
M iyagawa, I. Shimomura (2007). Macrophages and dendritic cells infiltrating islets with or without beta cells produce tumour
necrosis factor-alpha in patients with recent-onset type 1 diabetes. Diabetologia, 50, 596-601.
J. Banchereau, R. M. Steinm an (1998). Dendritic cells and the control of immunity. Nature, 392, 245-252.
A . Pichlmair, C. Reis e Sousa (2007). Innate recognition of viruses. Imm unity, 27, 370-383.
S. G allucci, P. M atzinger (2001). Danger signals: SOS to the immune system. Curr Opin Imm unol, 13, 114-119.
R. M . Steinm an, D. Hawiger, M . C. Nussenzweig (2003). Tolerogenic dendritic cells. Annu Rev Immunol, 21, 685-711.
M . Roivainen, P. Ylipaasto, C. Savolainen, J. G alam a, T. Hovi, T. Otonkoski (2002). Functional impairment and killing of human beta
cells by enteroviruses: the capacity is shared by a wide range of serotypes, but the extent is a characteristic of individual virus strains.
D iabetologia, 45, 693-702.
A . Elshebani, A . Olsson, J. W estm an, T. Tuvemo, O. Korsgren, G. Frisk (2007). Effects on isolated human pancreatic islet cells after
infection with strains of enterovirus isolated at clinical presentation of type 1 diabetes. Virus Res, 124, 193-203.
W . Chehadeh, J. Kerr-Conte, F. Pattou, G. A lm , J. Lefebvre, P. W attre, D. Hober (2000). Persistent infection of human pancreatic islets
by coxsackievirus B is associated with alpha interferon synthesis in beta cells. J Virol, 74, 10153-10164.
P. Ylipaasto, K. Klingel, A . M . Lindberg, T. Otonkoski, R. Kandolf, T. Hovi, M. Roivainen (2004). Enterovirus infection in human
pancreatic islet cells, islet tropism in vivo and receptor involvement in cultured islet beta cells. Diabetologia, 47, 225-239.
S. J. Richardson, A . W illcox, A . J. Bone, A . K. Foulis, N. G. Morgan (2009). The prevalence of enteroviral capsid protein vp1
immunostaining in pancreatic islets in human type 1 diabetes. Diabetologia.
F. Dotta, S. Censini, A . G. van Halteren, L. M arselli, M . M asini, S. Dionisi, F. M osca, U. Boggi, A . O. M uda, S. D. Prato, J. F. Elliott,
A . Covacci, R. Rappuoli, B. O. Roep, P. M archetti (2007). Coxsackie B4 virus infection of beta cells and natural killer cell insulitis in
recent-onset type 1 diabetic patients. Proc Natl Acad Sci U S A , 104, 5115-5120.
S. Tanaka, Y. Nishida, K. A ida, T. M aruyam a, A . Shim ada, M . Suzuki, H. Shim ura, S. Takizaw a, M . Takahashi, D. A kiyam a, S. AraiYam ashita, F. Furuya, A . Kawaguchi, M . Kaneshige, R. Katoh, T. Endo, T. Kobayashi (2009). Enterovirus infection, CXC chemokine
ligand 10 (CXCL10) and CXCR3 circuit: a mechanism of accelerated beta-cell failure in fulminant type 1 diabetes. Diabetes.
M . O ikarinen, S. Tauriainen, T. Honkanen, S. O ikarinen, K. Vuori, K. Kaukinen, I. R antala, M . M aki, H. Hyoty (2008). Detection of
enteroviruses in the intestine of type 1 diabetic patients. Clin Exp Immunol, 151, 71-75.
L. M. Karabatas, C. Pastorale, L. F. de Bruno, F. M aschi, O. H. Pivetta, Y. B. Lombardo, H. Chemes, J. C. Basabe (2005). Early
manifestations in multiple-low-dose streptozotocin-induced diabetes in mice. Pancreas, 30, 318-324.
S. Lenzen (2008). The mechanisms of alloxan- and streptozotocin-induced diabetes. Diabetologia, 51, 216-226.
A . K. Foulis, M . A . Farquharson, A . Meager (1987). Immunoreactive alpha-interferon in insulin-secreting beta cells in type 1 diabetes
mellitus. Lancet, 2, 1423-1427.
X . Huang, J. Yuang, A . Goddard, A . Foulis, R. F. Jam es, A . Lernm ark, R. Pujol-Borrell, A . Rabinovitch, N. Somoza, T. A . Stewart
(1995). Interferon expression in the pancreases of patients with type I diabetes. Diabetes, 44, 658-664.
M . Flodstrom , A . M aday, D. Balakrishna, M . M . Cleary, A . Yoshim ura, N. Sarvetnick (2002). Target cell defense prevents the
development of diabetes after viral infection. Nat Immunol, 3, 373-382.
M . Flodstrom , D. Tsai, C. Fine, A . M aday, N. Sarvetnick (2003). Diabetogenic potential of human pathogens uncovered in
experim entally permissive beta-cells. Diabetes, 52, 2025-2034.
D. Devendra, G. S. Eisenbarth (2004). Interferon alpha--a potential link in the pathogenesis of viral-induced type 1 diabetes and
autoimmunity. Clin Imm unol, 111, 225-233.
F. Shim izu, M . Shimizu, K. Kamiyama (1985). Inhibitory effect of interferon on the production of insulin. Endocrinology, 117, 2081
2084.
C. J. Rhodes, K. W . Taylor (1984). Effect of human lymphoblastoid interferon on insulin synthesis and secretion in isolated human
pancreatic islets. Diabetologia, 27, 601-603.
C. A . Biron, K. B. Nguyen, G. C. Pien, L. P. Cousens, T. P. Salazar-M ather (1999). Natural killer cells in antiviral defense: function and
regulation by innate cytokines. Annu R ev Imm unol, 17, 189-220.
C. A . Biron (2001). Interferons alpha and beta as immune regulators--a new look. Immunity, 14, 661-664.
G. A vraam ides, C. Y. Ng, R. David, Y. Gu, H. Fazekasova, V. M irenda, G. R. Foster, L. Runkel, G. Lombardi, F. M. M arelli-Berg (2007).
I FN-alpha2 induces leukocyte integrin redistribution, increased adhesion, and migration. J Interferon Cytokine Res, 27, 291-303.
G. R. Foster, S. H. M asri, R. David, M . Jones, A . Datta, G. Lombardi, L. Runkell, C. de Dios, I. Sizing, M . J. Jam es, F. M . M arelli-Berg
(2004). IFN-alpha subtypes differentially affect human T cell motility. J Immunol, 173, 1663-1670.
J. W alker, D. F. Tough (2006). Modification of TLR-induced activation of human dendritic cells by type I IFN: synergistic interaction
with TLR4 but not TLR3 agonists. Eur J Immunol, 36, 1827-1836.
T. Nagai, O. Devergne, T. F. M ueller, D. L. Perkins, J. M . van Seventer, G. A . van Seventer (2003). Timing of IFN-beta exposure during
human dendritic cell maturation and naive Th cell stimulation has contrasting effects on Th1 subset generation: a role for IFN-betamediated regulation of IL-12 fam ily cytokines and IL-18 in naive Th cell differentiation. J Immunol, 171, 5233-5243.
K. Honda, S. Sakaguchi, C. N akajim a, A . W atanabe, H. Yanai, M . M atsum oto, T. Ohteki, T. Kaisho, A . Takaoka, S. A kira, T. Seya, T.
Taniguchi (2003). Selective contribution of IFN-alpha/beta signaling to the maturation of dendritic cells induced by double-stranded
RNA or viral infection. P roc Natl A cad Sci U S A , 100, 10872-10877.
T. Luft, K. C. Pang, E. Thom as, P. Hertzog, D. N. Hart, J. Trapani, J. Cebon (1998). Type I IFNs enhance the term inal differentiation of
dendritic cells. J Immunol, 161, 1947-1953.
K. S. Lang, M . Recher, T. Jun t, A . A . Navarini, N. L. Harris, S. Freigang, B. Oderm att, C. Conrad, L. M . Ittner, S. Bauer, S. A . Luther, S.
Uem atsu, S. A kira, H. Hengartner, R. M. Zinkernagel (2005). Toll-like receptor engagement converts T-cell autoreactivity into overt
autoimmune disease. Nat M ed , 11, 138-145.
P. Blanco, A . K. Palucka, M . G ill, V. Pascual, J. Banchereau (2001). Induction of dendritic cell differentiation by IFN-alpha in systemic
lupus erythem atosus. Science, 294, 1540-1543.
J. Banchereau, V. Pascual (2006). Type I interferon in systemic lupus erythem atosus and other autoimmune diseases. Immunity, 25,
383-392.
J. Banchereau, V. Pascual, A . K. Palucka (2004). Autoim m unity through cytokine-induced dendritic cell activation. Imm unity, 20,
539-550.
133
Chapter 8
39.
40.
41.
42.
43.
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
134
K. K. Salm inen, T. Vuorinen, S. O ikarinen, M . Helm inen, S. Sim ell, M. Knip, J. Ilonen, O. Sim ell, H. Hyoty (2004). Isolation of
enterovirus strains from children with preclinical Type 1 diabetes. Diabet M ed , 21, 156-164.
C. M. Hilkens, J. F. Schlaak, I. M . Kerr (2003). Differential responses to IFN-alpha subtypes in human T cells and dendritic cells. J
Immunol, 171, 5255-5263.
K. Yasuda, C. Richez, J. W . M aciaszek, N. A grawal, S. A kira, A . M arshak-Rothstein, I. R. Rifkin (2007). Murine dendritic cell type I IFN
production induced by human IgG-RNA immune complexes is IFN regulatory factor (IRF)5 and IRF7 dependent and is required for
IL-6 production. J Immunol, 178, 6876-6885.
B. W einstock-Guttm an, J. Hong, R. Santos, M . Tamano-Blanco, D. Badgett, K. Patrick, M . Baier, J. Feichter, E. Gallagher, N. Garg,
M . Ram anathan (2006). Interferon-beta modulates bone-associated cytokines and osteoclast precursor activity in multiple sclerosis
patients. M u lt Scler, 12, 541-550.
J. Satoh, Y. Nanri, H. Tabunoki, T. Yamamura (2006). M icroarray analysis identifies a set of CXCR3 and CCR2 ligand chemokines
as early IFNbeta-responsive genes in peripheral blood lymphocytes in vitro: an implication for IFNbeta-related adverse effects in
multiple sclerosis. BM C Neurol, 6, 18.
M . J. Crane, K. L. Hokeness-Antonelli, T. P. Salazar-M ather (2009). Regulation of Inflammatory Monocyte/Macrophage Recruitment
from the Bone M arrow during Murine Cytomegalovirus Infection: Role for Type I Interferons in Localized Induction of CCR2 Ligands.
J Imm unol.
C. A . Delaney, D. Pavlovic, A . Hoorens, D. G. Pipeleers, D. L. Eizirik (1997). Cytokines induce deoxyribonucleic acid strand breaks and
apoptosis in human pancreatic islet cells. Endocrinology, 138, 2610-2614.
T. M andrup-Poulsen (2003). Apoptotic signal transduction pathways in diabetes. Biochem Pharm acol, 66, 1433-1440.
T. M andrup-Poulsen (1996). The role of interleukin-1 in the pathogenesis of IDDM. Diabetologia, 39, 1005-1029.
D. M auricio, T. M andrup-Poulsen (1998). Apoptosis and the pathogenesis of IDDM: a question of life and death. Diabetes, 47, 1537
1543.
M . Baggiolini, B. Dewald, B. M oser (1997). Human chemokines: an update. Annu Rev Immunol, 15, 675-705.
D. L. Eizirik, M . L. Colli, F. Ortis (2009). The role of inflammation in insulitis and beta-cell loss in type 1 diabetes. Nat R ev Endocrinol,
5, 219-226.
W . Lu, D. G. Pipeleers, G. Kloppel, L. Bouwens (1996). Comparative immunocytochemical study of MHC class II expression in human
donor pancreas and isolated islets. Virchows Arch, 429, 205-211.
K. S. Ravichandran, U. Lorenz (2007). Engulfment of apoptotic cells: signals for a good meal. Nat R ev Immunol, 7, 964-974.
D. V. Krysko, K. D'Herde, P. Vandenabeele (2006). Clearance of apoptotic and necrotic cells and its immunological consequences.
A poptosis, 11, 1709-1726.
B. Calderon, A . Suri, M. J. M iller, E. R. Unanue (2008). Dendritic cells in islets of Langerhans constitutively present beta cell-derived
peptides bound to their class II MHC molecules. Proc Natl Acad Sci U S A , 105, 6121-6126.
C. Kurts, W . R. Heath, F. R. Carbone, J. Allison, J. F. M iller, H. Kosaka (1996). Constitutive class I-restricted exogenous presentation
of self antigens in vivo. J Exp M ed , 184, 923-930.
C. Kurts, H. Kosaka, F. R. Carbone, J. F. M iller, W. R. Heath (1997). Class I-restricted cross-presentation of exogenous self-antigens
leads to deletion of autoreactive CD8(+) T cells. J Exp M ed , 186, 239-245.
J. Hernandez, S. Aung, W. L. Redmond, L. A . Sherm an (2001). Phenotypic and functional analysis of CD8(+) T cells undergoing
peripheral deletion in response to cross-presentation of self-antigen. J Exp M ed , 194, 707-717.
S. Hugues, E. M ougneau, W . Ferlin, D. Jeske, P. Hofman, D. Homann, L. Beaudoin, C. Schrike, M . Von Herrath, A . Lehuen, N.
G laichenhaus (2002). Tolerance to islet antigens and prevention from diabetes induced by limited apoptosis of pancreatic beta cells.
Imm unity, 16, 169-181.
A . M ukhopadhaya, T. Hanafusa, I. Jarchum , Y. G. Chen, Y. Iw ai, D. V. Serreze, R. M . Steinm an, K. V. Tarbell, T. P. DiLorenzo (2008).
Selective delivery of beta cell antigen to dendritic cells in vivo leads to deletion and tolerance of autoreactive CD8+ T cells in NOD
mice. Proc Natl A cad Sci U S A , 105, 6374-6379.
L. M. Stuart, M . Lucas, C. Sim pson, J. Lamb, J. Savill, A . Lacy-Hulbert (2002). Inhibitory effects of apoptotic cell ingestion upon
endotoxin-driven myeloid dendritic cell maturation. J Immunol, 168, 1627-1635.
A . E. M orelli, A . T. Larregina, W. J. Shufesky, A . F. Zahorchak, A . J. Logar, G. D. Papworth, Z. W ang, S. C. W atkin s, L. D. Falo, Jr., A . W.
Thomson (2003). Internalization of circulating apoptotic cells by splenic marginal zone dendritic cells: dependence on complement
receptors and effect on cytokine production. Blood, 101, 611-620.
G. A . Belov, L. I. Rom anova, E. A . Tolskaya, M . S. Kolesnikova, Y. A . Lazebnik, V. I. Agol (2003). The major apoptotic pathway
activated and suppressed by poliovirus. J Virol, 77, 45-56.
V. I. Agol, G. A . Belov, K. Bienz, D. Egger, M . S. Kolesnikova, L. I. Rom anova, L. V. Sladkova, E. A . Tolskaya (2000). Competing death
programs in poliovirus-infected cells: commitment switch in the middle of the infectious cycle. J Virol, 74, 5534-5541.
C. Reis e Sousa (2006). Dendritic cells in a mature age. Nat R ev Immunol, 6, 476-483.
D. R. Green, T. Ferguson, L. Zitvogel, G. Kroem er (2009). Immunogenic and tolerogenic cell death. Nat R ev Immunol, 9, 353-363.
J. M . Blander, R. M edzhitov (2006). Toll-dependent selection of microbial antigens for presentation by dendritic cells. Nature, 440,
808-812.
M . M . Zanone, E. Favaro, E. Ferioli, G. C. Huang, N. J. Klein, P. C. Perin, M . Peakm an, P. G. Conaldi, G. Camussi (2007). Human
pancreatic islet endothelial cells express coxsackievirus and adenovirus receptor and are activated by coxsackie B virus infection.
Faseb J , 21, 3308-3317.
D. Piccioli, S. Sbrana, E. M elandri, N. M . Valiante (2002). Contact-dependent stimulation and inhibition of dendritic cells by natural
killer cells. J Exp M ed , 195, 335-341.
J. H. Velthuis, W. W . Unger, A . R. van d er Slik, G. Duinkerken, M . Engelse, A . F. Schaapherder, J. Ringers, C. van Kooten, E. J. de
Koning, B. O. Roep (2009). Accumulation of autoreactive effector T cells and allo-specific regulatory T cells in the pancreas allograft
of a type 1 diabetic recipient. Diabetologia, 52, 494-503.
S. A rif, T. I. Tree, T. P. A still, J . M . Trem ble, A . J. Bishop, C. M . Dayan, B. O. Roep, M . Peakman (2004). Autoreactive T cell responses
show proinflammatory polarization in diabetes but a regulatory phenotype in health. J Clin Invest, 113, 451-463.
A . L. Notkins, A . Lernm ark (2001). Autoimmune type 1 diabetes: resolved and unresolved issues. J Clin Invest, 108, 1247-1252.
A . Shim ada, J. M orim oto, K. Kodama, R. Suzuki, Y. O ikaw a, O. Funae, A . Kasuga, T. Saruta, S. Narumi (2001). Elevated serum IP-10
levels observed in type 1 diabetes. Diabetes Care, 24, 510-515.
F. Nicoletti, I. Conget, M . Di M auro, R. Di M arco, M . C. Mazzarino, K. Bendtzen, A . M essina, R. Gomis (2002). Serum concentrations
of the interferon-gamma-inducible chemokine IP-10/CXCL10 are augmented in both newly diagnosed Type I diabetes mellitus
patients and subjects at risk of developing the disease. Diabetologia, 45, 1107-1110.
W . Chehadeh, J. W e ill, M . C. Vantyghem, G. A lm , J. Lefebvre, P. W attre, D. Hober (2000). Increased level of interferon-alpha in blood
of patients with insulin-dependent diabetes mellitus: relationship with coxsackievirus B infection. J Infect Dis, 181, 1929-1939.
T. Vuorinen, R. V ainionpaa, J. Heino, T. Hyypia (1999). Enterovirus receptors and virus replication in human leukocytes. J Gen Virol,
80 ( Pt 4 ), 921-927.
T. Vuorinen, R. Vainionpaa, H. Kettinen, T. Hyypia (1994). Coxsackievirus B3 infection in human leukocytes and lymphoid cell lines.
Blood, 84, 823-829.
Sum m ary and Discussion
77.
78.
79.
80.
81.
82.
83.
84.
85.
86.
87.
88.
89.
90.
91.
92.
93.
94.
95.
96.
97.
98.
99.
100.
101.
102.
103.
104.
105.
106.
G. R. Vreugdenhil, P. G. W ijnands, M . G. Netea, J. W. van der Meer, W. J. M elchers, J. M . G alam a (2000). Enterovirus-induced
production of pro-inflammatory and T-helper cytokines by human leukocytes. Cytokine, 12, 1793-1796.
J. P. W ang, D. R. Asher, M . Chan, E. A . Kurt-Jones, R. W. Finberg (2007). Cutting Edge: Antibody-Mediated TLR7-Dependent
Recognition of Viral RNA. J Immunol, 178, 3363-3367.
D. Hober, W . Chehadeh, A . Bouzidi, P. W attre (2001). Antibody-dependent enhancem ent of coxsackievirus B4 infectivity of human
peripheral blood mononuclear cells results in increased interferon-alpha synthesis. J Infect Dis, 184, 1098-1108.
D. J. Smyth, J. D. Cooper, R. Bailey, S. Field, O. Burren, L. J. Smink, C. G uja, C. Ionescu-Tirgoviste, B. W idm er, D. B. Dunger, D. A.
Savage, N. M. W alker, D. G. Clayton, J. A . Todd (2006). A genome-wide association study of nonsynonymous SNPs identifies a type
1 diabetes locus in the interferon-induced helicase (IFIH1) region. Nat G enet, 38, 617-619.
S. Liu, H. W ang, Y. Jin , R. Podolsky, M . V. Reddy, J. Pedersen, B. Bode, J. Reed, D. Steed, S. Anderson, P. Yang, A . M uir, L. Steed,
D. Hopkins, Y. Huang, S. Purohit, C. Y. W ang, A . K. Steck, A . M ontem ari, G. Eisenbarth, M . Rewers, J. X. She (2009). IFIH1
polymorphisms are significantly associated with type 1 diabetes and IFIH1 gene expression in peripheral blood mononuclear cells.
Hum M ol G enet, 18, 358-365.
S. Nejentsev, N. W alker, D. Riches, M . Egholm, J. A . Todd (2009). Rare variants of IFIH1, a gene implicated in antiviral responses,
protect against type 1 diabetes. Science, 324, 387-389.
M . von Herrath (2009). Diabetes: A virus-gene collaboration. Nature, 459, 518-519.
T. Shigemoto, M . Kageyama, R. Hirai, J. Zheng, M . Yoneyama, T. Fujita (2009). Identification of loss of function mutations in human
genes encoding RIG-I and MDA5: implications for resistance to type I diabetes. J Biol Chem, 284, 13348-13354.
L. L. Field, V. Bonnevie-Nielsen, F. Pociot, S. Lu, T. B. Nielsen, H. Beck-Nielsen (2005). OAS1 splice site polymorphism controlling
antiviral enzyme activity influences susceptibility to type 1 diabetes. Diabetes, 54, 1588-1591.
M . C. Tessier, H. Q. Qu, R. Frechette, F. Bacot, R. G rabs, S. P. Taback, M . L. Lawson, S. E. Kirsch, T. J. Hudson, C. Polychronakos
(2006). Type 1 diabetes and the OAS gene cluster: association with splicing polymorphism or haplotype? J M ed G enet, 43, 129-132.
D. J. Sm yth, J. D. Cooper, C. E. Lowe, S. Nutland, N. M . W alker, D. G. Clayton, J. A . Todd (2006). No evidence for association of OAS1
with type 1 diabetes in unaffected siblings or type 1 diabetic cases. Diabetes, 55, 1525-1528.
V. Bonnevie-Nielsen, L. L. Field, S. Lu, D. J. Zheng, M . Li, P. M . M artensen, T. B. Nielsen, H. Beck-Nielsen, Y. L. Lau, F. Pociot (2005).
Variation in antiviral 2',5'-oligoadenylate synthetase (2'5'AS) enzyme activity is controlled by a single-nucleotide polymorphism at a
splice-acceptor site in the OAS1 gene. Am J Hum G enet, 76, 623-633.
N. Petrovsky, K. O. Kyvik, V. Bonnevie-Nielsen, H. Beck-Nielsen, A . Green, L. C. Harrison (2002). Evidence from tw ins for acquired
cellular immune hyperactivity in type 1 diabetes. Imm unology, 106, 584-589.
V. Bonnevie-N ielsen, P. M. M artensen, J. Justesen, K. O. Kyvik, B. Kristensen, K. Levin, H. Beck-Nielsen, A . W orsaa, T. Dyrberg
(2000). The antiviral 2',5'-oligoadenylate synthetase is persistently activated in type 1 diabetes. Clin Imm unol, 96, 11-18.
J. A . Todd, N. M . W alker, J. D. Cooper, D. J. Smyth, K. Downes, V. Plagnol, R. Bailey, S. Nejentsev, S. F. Field, F. Payne, C. E. Lowe,
J. S. Szeszko, J. P. Hafler, L. Zeitels, J. H. Yang, A . Vella, S. Nutland, H. E. Stevens, H. Schuilenburg, G. Colem an, M . M aisuria, W.
M eadow s, L. J. Smink, B. Healy, O. S. Burren, A . A . Lam, N. R. Ovington, J. A llen, E. A dlem , H. T. Leung, C. W allace, J. M . Howson,
C. G uja, C. Ionescu-Tirgoviste, M . J. Simm onds, J. M . Heward, S. C. Gough, D. B. Dunger, L. S. W icker, D. G. Clayton (2007). Robust
associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat G enet, 39, 857-864.
J. D. Cooper, D. J. Smyth, A . M . Sm iles, V. Plagnol, N. M . W alker, J. E. A llen, K. Downes, J. C. Barrett, B. C. Healy, J. C. M ychaleckyj,
J. H. W arram , J. A . Todd (2008). M eta-analysis of genome-wide association study data identifies additional type 1 diabetes risk loci.
Nat G enet, 40, 1399-1401.
F. Cucca, R. Lampis, M . Congia, E. Angius, S. Nutland, S. C. Bain, A . H. Barnett, J. A . Todd (2001). A correlation between the relative
predisposition of MHC class II alleles to type 1 diabetes and the structure of their proteins. Hum M ol G enet, 10, 2025-2037.
D. Sm yth, J. D. Cooper, J. E. Collins, J. M . Heward, J. A . Franklyn, J. M . Howson, A . Vella, S. Nutland, H. E. Rance, L. M aier, B. J.
Barratt, C. G uja, C. Ionescu-Tirgoviste, D. A . Savage, D. B. Dunger, B. W idm er, D. P. Strachan, S. M . Ring, N. W alker, D. G. Clayton,
R. C. Tw ells, S. C. Gough, J. A . Todd (2004). Replication of an association between the lymphoid tyrosine phosphatase locus (LYP/
PTPN22) with type 1 diabetes, and evidence for its role as a general autoimmunity locus. Diabetes, 53, 3020-3023.
L. Nistico, R. Buzzetti, L. E. Pritchard, B. Van der A uw era, C. G iovannini, E. Bosi, M. T. Larrad, M . S. Rios, C. C. Chow, C. S. Cockram,
K. Jacobs, C. M ijovic, S. C. Bain, A . H. Barnett, C. L. V andew alle, F. Schuit, F. K. Gorus, R. Tosi, P. Pozzilli, J. A . Todd (1996). The CTLA-4
gene region of chromosome 2q33 is linked to, and associated w ith, type 1 diabetes. Belgian Diabetes Registry. Hum M ol G enet, 5,
1075-1080.
H. Ueda, J. M. Howson, L. Esposito, J. Heward, H. Snook, G. Cham berlain, D. B. Rainbow, K. M . Hunter, A . N. Sm ith, G. Di Genova,
M . H. Herr, I. Dahlm an, F. Payne, D. Sm yth, C. Lowe, R. C. Tw ells, S. Howlett, B. Healy, S. Nutland, H. E. Rance, V. Everett, L. J. Smink,
A . C. Lam, H. J. Cordell, N. M . W alker, C. Bordin, J. Hulme, C. Motzo, F. Cucca, J. F. Hess, M . L. M etzker, J. Rogers, S. Gregory, A.
A llahab ad ia, R. N ithiyananthan, E. Tuomilehto-Wolf, J. Tuom ilehto, P. Bingley, K. M . Gillespie, D. E. Undlien, K. S. Ronningen, C.
G uja, C. Ionescu-Tirgoviste, D. A . Savage, A . P. M axw ell, D. J. Carson, C. C. Patterson, J. A . Franklyn, D. G. Clayton, L. B. Peterson, L.
S. W icker, J. A . Todd, S. C. Gough (2003). Association of the T-cell regulatory gene CTLA4 with susceptibility to autoim mune disease.
Nature, 423, 506-511.
A . Zhernakova, B. Z. A lizadeh, P. Eerligh, P. Hanifi-M oghaddam, N. C. Schloot, B. Diosdado, C. W ijm enga, B. O. Roep, B. P. Koeleman
(2006). Genetic variants of RANTES are associated with serum RANTES level and protection for type 1 diabetes. Genes Immun, 7,
544-549.
A . Settin, A . Ism ail, M . A . El-Magd, R. El-Baz, A . Kazamel (2009). Gene polymorphisms of TNF-alpha-308 (G/A), IL-10(-1082) (G/A),
IL-6(-174) (G/C) and IL-1Ra (VNTR) in Egyptian cases with type 1 diabetes mellitus. Autoim m unity, 42, 50-55.
R. Kumar, R. G osw am i, S. A garw al, N. Israni, S. K. Singh, R. Rani (2007). Association and interaction of the TNF-alpha gene with
other pro- and anti-inflammatory cytokine genes and HLA genes in patients with type 1 diabetes from North India. Tissue Antigens,
69, 557-567.
R. D. Leslie, M . Delli Castelli (2004). Age-dependent influences on the origins of autoim mune diabetes: evidence and implications.
D iabetes, 53, 3033-3040.
C. King, A . Ilic, K. Koelsch, N. Sarvetnick (2004). Homeostatic expansion of T cells during immune insufficiency generates
autoimmunity. Cell, 117, 265-277.
C. Le Saout, S. M ennechet, N. Taylor, J. Hernandez (2008). Memory-like CD8+ and CD4+ T cells cooperate to break peripheral
tolerance under lymphopenic conditions. Proc Natl Acad Sci U S A , 105, 19414-19419.
B. O. Roep, M . Atkinson, M . von Herrath (2004). Satisfaction (not) guaranteed: re-evaluating the use of animal models of type 1
diabetes. Nat Rev Immunol, 4, 989-997.
J. M estas, C. C. Hughes (2004). Of mice and not men: differences between mouse and human immunology. J Immunol, 172, 2731
2738.
A . W illco x, S. J . Richardson, A . J. Bone, A . K. Foulis, N. G. Morgan (2009). Analysis of islet inflammation in human type 1 diabetes.
Clin Exp Immunol, 155, 173-181.
N. Itoh, T. Hanafusa, A . M iyazaki, J. M iyagawa, K. Yamagata, K. Yamamoto, M . W aguri, A . Imagawa, S. Tam ura, M . Inada, et al.
(1993). M ononuclear cell infiltration and its relation to the expression of major histocompatibility complex antigens and adhesion
molecules in pancreas biopsy specim ens from newly diagnosed insulin-dependent diabetes mellitus patients. J Clin Invest, 92, 2313-
135
Chapter 8
107.
108.
109.
110.
111.
112.
113.
114.
115.
116.
117.
136
2322.
H. Yin, A . K. Berg, T. Tuvemo, G. Frisk (2002). Enterovirus RNA is found in peripheral blood mononuclear cells in a majority of type 1
diabetic children at onset. Diabetes, 51, 1964-1971.
G. Frisk, T. Tuvemo (2004). Enterovirus infections with beta-cell tropic strains are frequent in siblings of children diagnosed with type
1 diabetes children and in association with elevated levels of GAD65 antibodies. J M ed Virol, 73, 450-459.
L. A ndreoletti, D. Hober, C. Hober-Vandenberghe, S. Belaich, M . C. Vantyghem , J. Lefebvre, P. W attre (1997). Detection of coxsackie
B virus RNA sequences in whole blood samples from adult patients at the onset of type I diabetes mellitus. J M e d Virol, 52, 121
127.
G. R. Vreugdenhil, N. C. Schloot, A . Hoorens, C. Rongen, D. G. Pipeleers, W . J. M elchers, B. O. Roep, J. M . G alam a (2000). Acute
onset of type I diabetes mellitus after severe echovirus 9 infection: putative pathogenic pathways. Clin Infect Dis, 31, 1025-1031.
P. Klem ola, S. Kaijalainen, P. Ylipaasto, M. Roivainen (2008). Diabetogenic effects of the most prevalent enteroviruses in Finnish
sewage. Ann N Y A cad Sci, 1150, 210-212.
H. Al-Hello, B. Davydova, T. Sm ura, S. Kaialainen, P. Ylipaasto, E. Saario, T. Hovi, E. Rieder, M . Roivainen (2005). Phenotypic and
genetic changes in coxsackievirus B5 following repeated passage in mouse pancreas in vivo. J M e d Virol, 75, 566-574.
B. Keym eulen, E. Vandem eulebroucke, A . G. Ziegler, C. M athieu, L. Kaufm an, G. Hale, F. G orus, M . G oldm an, M . W alter, S. Candon,
L. Schandene, L. Crenier, C. De Block, J. M. Seigneurin, P. De Pauw, D. Pierard, I. W eets, P. Rebello, P. Bird, E. Berrie, M . Frew in, H.
W aldm ann, J . F. Bach, D. Pipeleers, L. Chatenoud (2005). Insulin needs after CD3-antibody therapy in new-onset type 1 diabetes. N
Engl J M ed, 352, 2598-2608.
K. C. Herold, S. G itelm an, C. G reenbaum , J. Puck, W . Hagopian, P. G ottlieb, P. Sayre, P. Bianchine, E. Wong, V. Seyfert-M argolis,
K. Bourcier, J. A . Bluestone (2009). Treatment of patients with new onset Type 1 diabetes with a single course of anti-CD3 mAb
Teplizumab preserves insulin production for up to 5 years. Clin Immunol, 132, 166-173.
J. Ludvigsson, M. Faresjo, M . Hjorth, S. Axelsson, M . Cheramy, M. Pihl, O. Vaarala, G. Forsander, S. Ivarsson, C. Johansson, A.
Lindh, N. O. Nilsson, J. A m an, E. O rtqvist, P. Zerhouni, R. Casas (2008). GAD treatm ent and insulin secretion in recent-onset type 1
diabetes. N Engl J M ed , 359, 1909-1920.
L. C. Harrison (2008). Vaccination against self to prevent autoim mune disease: the type 1 diabetes model. Imm unol Cell Biol, 86,
139-145.
A . G. van Halteren, O. M . Tysm a, E. van Etten, C. M athieu, B. O. Roep (2004). 1alpha,25-dihydroxyvitamin D3 or analogue treated
dendritic cells modulate human autoreactive T cells via the selective induction of apoptosis. JA utoim m un, 23, 233-239.
Samenvatting
Nederlandse Samenvatting
Introductie
ype 1 diabetes (T1D) is een chronische endocriene aandoening, waarbij
de insuline-producerende ß-cellen in de alvleesklier kapot gaan. Wanneer
de insuline-producerende cellen niet meer voldoende werken blijft de
bloedsuikerspiegel in het bloed niet goed op peil; mensen met type 1 diabetes
moeten insuline inspuiten. Vaak treden bij type 1 diabetes
Endocrien
auto-immuun reacties op die gericht zijn tegen de ß-cellen.
u itsch e id en d in h e t b lo ed. En do crien e
k lieren sch eid e n ho rm on en a f in het
Daarom wordt T1D gezien als een auto-immuun ziekte. Zowel
b lo ed. V oorbeeld en zijn d e eilandjes
genetische factoren als omgevingsfactoren spelen een rol bij
van L a ng erhan s (oa in sulin e p ro du ctie),
d e hy p o fy se (o a g ro eih o rm o o n ) en de
het ontstaan van T1D. Verschillende soorten virussen worden
b ijnieren (o a a dren alin e).
gezien als mogelijke omgevingsfactoren die betrokken zijn bij
het ontstaan van T1D. Onder hen ook de enterovirussen, specifiek degene uit de Humane
Enterovirus B familie (HEV-B). Hiertoe behoren onder andere coxsackie B virussen (CVB)
en echovirussen (EV). Deze virussen zijn "broertjes" van het meer bekende poliovirus,
dat kinderverlamming kan veroorzaken. In het algemeen zijn deze virussen vrij mild. De
meeste infecties verlopen zonder symptomen, of met een mild ziektebeeld (zomergriep).
Echter, ernstige infecties komen ook voor, vooral bij jonge kinderen. Verschillende
complicaties (zoals hersenvliesontsteking of alvleesklierontsteking) kunnen ontstaan en
dit kan een dodelijke afloop hebben.
De HEV-Bs worden geassocieerd met het ontstaan van T1D op basis van
Prospectieve studies
verschillende bevindingen, waaronder (i) prospectieve studies
stu d ie s w a a rb ij in e en b ep a a ld e g ro e p
waarin T1D patiënten worden vergeleken met broers en
m e n se n o n d e rzo ek w o rd t g ed a a n
d a t vo o ra fg a a t aan e en b ep aa ld e
zussen zonder T1D en ongerelateerde controle individuen
g eb eu rte n is (h e t krijgen van T1D in dit
(geen familie). In deze studies vond men dat T1D patiënten
g e v a l), m e t h e t d o e l inzicht te krijgen
in d e o n tsta a n sg e sch ie d e n is.
méér enterovirus infecties krijgen dan controle individuen.
"Case-control" studies
(ii) "Case-control" studies die RNA van enterovirussen (het
w a a rb ij e en g ro ep p erso n e n m et
erfelijk
materiaal van deze virussen) in het bloed van T1D
een b ep a a ld e zie k te (ca se ) en een
g ro ep p erso n e n z o n d e r d eze ziekte
patiënten hebben aangetoond vlak na de diagnose, vóór de
(co n tro l) w o rd en o n derzo ch t. M en
diagnose, of in bloed van patiënten die al langer T1D hebben.
ve rg e lijk t d e b lo o tste llin g aan een
m o g elijke risico fa cto r in b eide g ro ep en
In gezonde controles wordt dit RNA vrijwel nooit aangetroffen.
(retro sp ectie f).
(iii) De aanwezigheid van enterovirus RNA in de ß-cellen van
Enterovirus RNA
T1D patiënten ná overlijden. (iv) Het vermogen van deze
het
e rfe lijk
m a teria a l
van
en tero viru sse n
w a t co d e e rt
voor virussen om in vitro de ß-cellen in eilandjes van Langerhans te
virale eiw itten . N et als on s m enselijke
infecteren en kapot te maken.
DNA m o e t h e t e n teroviru s
RNA
ve rm enigvuld ig d w o rd en vo o r virus
Er zijn meerdere theorieën over de manier waarop
replicatie.
deze virussen T1D zouden kunnen initiëren, dan wel de
¡n vitro
ontwikkeling versnellen: (i) HEV-Bs kunnen de ß-cellen direct
stu d ie s die in een p e trisch a a ltje o f
k w e e k fle s in h e t la b o rato riu m w orden
infecteren en door hun lytische levenscyclus de ß-cellen kapot
uitg evoerd .
maken. (ii) Ontstekingsreacties (inflammatie) die geïnduceerd
Lvtisch
zijn
door de infectie kunnen tot zogenaamde "bystander
lytisch b eteke n t le tte rlijk : oplossen d.
De ce l kla p t uit e lka ar (en g a a t dus
activatie" van allerlei immuun cellen leiden en zo immuun
ka po t) w a a rd o o r n ie u w g evo rm de
reacties tot gevolg hebben. Deze activatie kan op zijn beurt
viru ssen vrijkom en.
leiden tot chronische ontstekingsreacties, en dit is schadelijk
Inflammatie
on tstekin g . P ro -in fla m m ato ir: fa c to re n
voor de functie en integriteit van de ß-cellen. (iii) auto-immuun
d ie d e o n tste k in g b evo rd ere n . Antireacties kunnen ontwikkelen in de pro-inflammatoire microin fla m m a to ir:
fa c to re n
d ie
de
o n tste k in g rem m en.
omgeving van de virus-geïnfecteerde ß-cellen. (iv) moleculaire
T
138
Nederlandse Samenvatting
mimicry, w aar responsen die gericht zijn tegen het virus per Bystander activatie
o n b e d o e ld e
a ctiva tie
van
cellen
ongeluk ook delen van het eigen lichaam herkennen en (b ijv o o rb e e ld d o o rd a t ze in e en p ro
aanvallen, en die daardoor leiden tot auto-immuniteit. De ene in fla m m ato ire om g evin g zijn).
theorie sluit de ander niet uit; het zou zelfs kunnen dat 2 of Moleculaire mimicry
o veree n k o m st
tu ssen
gastheermeer theorieën samen een goede weergave zijn van wat er m olecu len (van het e ig en lichaam ) en
p a th o g e n e a n tig en en (zie b en eden ).
tijdens de ontwikkeling van T1D gebeurt.
Een re sp o n s die o o rsp ro n k elijk g erich t
Ontstekingsreacties in de eilandjes van Langerhans is teg en h e t p a th o g e e n kan zich o o k
van T1D patiënten komt veel voor. Immuuncellen, zoals T keren teg en d elen van het eigen
lichaam . D it kan leiden tot autocellen, macrofagen en dendritische cellen zijn aangetoond in im m uniteit.
de eilandjes van Langerhans van patiënten. De ontwikkeling of Effector Tcellen
versnelling van het T1D ziekteproces hangt af van meerdere d e T cellen van het im m u un systeem
d ie b etro kken zijn b ij h e t aanvallen
factoren. De balans tussen auto-reactieve effector T cellen van p a th o g en en . H iertoe b eh o re n de
(die helpen met maken van antistoffen en het aanvallen van T cellen d ie h elp en b ij a a n m a a k van
a n tisto ffe n g e ric h t teg en p ath o g en en ,
geïnfecteerde cellen) en zogenaamde regulatoire T cellen (die m a a r o o k de T cellen d ie g eïn fecte erd e
de effector cellen remmen en zo een goede balans bewaren g a sth ee rcelle n aanvallen.
tussen immuun reacties en tolerantie) is daarbij erg belangrijk. Regulatoire Tcellen
d e g ro ep T cellen d ie e rv o o r z o rg t dat
Deze balans wordt voornamelijk bepaald door dendritische im m u un respo n sen g o e d g eco n tro lee rd
cellen (DCs). De DCs zijn de professionele antigeen- b lijven en n iet uit d e h a n d lopen. Ze
kunnen d e e ffe c to r T cellen rem m en.
presenterende cellen van ons immuun systeem. Ze spelen een
Antiaeen
zeer belangrijke rol bij het initiëren van immuun responsen en een m o lecu u l d a t een re a ctie van h e t
het bewaren van tolerantie tegen ons eigen lichaam. Zowel bij im m u u n systee m k a n o pw ekken. D it kan
e en m o lecu u l zijn van een p a th o g e e n ,
de aangeboren immuun responsen (ofwel "innate respons") als o f een lich a am seig en m olecu ul. Ons
de verkregen immuun responsen (ofwel "adaptieve respons") im m u un systeem b o u w t tolera n tie op
teg en d e lich a am seig en m o lecu len ,
zijn de DCs belangrijke spelers. DCs zijn onder andere bekend te rw ijl teg en
licha am svreem de
om hun vermogen om allerlei ziekteverwekkers op te eten en a ntig enen ju is t w e l een re a ctie w o rd t
g esta rt.
vervolgens het immuunsysteem aan te schakelen.
Om ervoor te zorgen dat de tolerantie tegen het lichaamseigen gehandhaafd
wordt, maar er tegelijkertijd wel immuun responsen worden opgewekt tegen invasieve
pathogenen is het belangrijk dat de DC onderscheid kan maken tussen "eigen" (of
ongevaarlijk) en vreemd (of gevaarlijk). Hiervoor brengt de DC een aantal specifieke
receptoren tot expressie die bepaalde patronen op oatroon-herkenninas receptoren
re cep to re n op cellen d ie b ep aa ld e
pathogenen kunnen herkennen, of die de schade aan het m o lecu la ire
p a tro n en
kunnen
lichaam herkennen die een infectie met zich meebrengt. Dit h erken n en. Deze m o lecu la ire p a tro n en
kom en v a ak voor op e en p ath o g een .
zijn de zogenaamde "patroon-herkennings receptoren". Ze D a a rna a st w o rd en o o k signalen
herkennen pathogeen-geassocieerde moleculaire patronen, h erken d d ie a an g eve n d a t e r sch ad e
is aan ons eig en licha am (b ijvo o rb e e ld
zoals bijvoorbeeld viraal RNA. Nadat een receptor op een DC a ls g evo lg van een infectie).
een indringer heeft herkend, begint de DC een proces dat
oathoaeen-aeassocieerde
maturatie heet. Dit gaat gepaard met veranderingen in het moleculaire patronen
fenotype en de functie van de DC. Gematureerde DCs zijn m o lecu la ire p a tro n en d ie voorkom en
op p a th o g en en en d ie h erken d w orden
in staat om immuun responsen te starten bijvoorbeeld via d o o r re cep to re n op onze im m uun
de activatie van T cellen. Niet-gematureerde DCs, of DCs die cellen. V oorbeeld en h ierva n z ijn : de
ce lw a n d van een b a c te rie , het RNA
anti-inflammatoire signalen krijgen, zullen daarentegen juist (g enetisch m a teriaa l) van een virus.
tolerantie induceren wanneer ze een T cel tegenkomen.
139
Nederlandse Samenvatting
Samenvatting van de belangrijkste resultaten
In dit proefschrift is de interactie onderzocht tussen eilandjes van Langerhans,
enterovirussen en dendritische cellen, met als doel meer inzicht te verkrijgen in de
mogelijke mechanismen die aan de basis staan van enterovirus-geïnduceerde type 1
diabetes.
Zoals al eerder genoemd is het herkennen van pathogenen
of pathogeen-geassocieerde schade aan het lichaam door
DCs belangrijk om te bepalen of er een immuun respons moet worden gestart of niet.
Hoofdstuk 2 geeft een beknopt overzicht van de expressie van verschillende "patroonherkennings receptoren" in DCs in zowel de "steady state" als onder pro-inflammatoire
omstandigheden (gestimuleerd met een "stukje pathogeen"). Hierbij zijn de receptoren
geselecteerd die betrokken zijn bij het herkennen van virussen. Verder is ook onderzocht
hoe verschillende "ondersoorten" van DCs elkaar beïnvloeden. Er is een mechanisme
gevonden waarvia de plasmacytoïde DCs (pDCs) de myeloïde DCs (mDCs) kunnen
beschermen tegen virus infecties door de productie van het stofje interferon. Hoofdstuk
3 houdt zich bezig met de gevoeligheid van DCs voor infectie met verschillende HEV-B
soorten. We laten zien dat coxsackie B virussen (CVBs) niet in staat zijn de DCs te infecteren,
waarschijnlijk omdat de receptor die ze nodig hebben om de DC binnen te komen niet
aanwezig is. Echovirussen daarentegen, zijn wel in staat om DCs te infecteren. Dit heeft
duhhei-strenas viraai RNA
tot gevolg dat de DC zijn functie niet meer goed kan uitoefenen
d e vorm van r n a d ie h e t virus m a a k t
(bijvoorbeeld geen respons meer wanneer de "patroon-
steady state
o n gestim uleerd, in balans.
om zijn g en o o m te verm enigvuldigen.
Tijdens d e verm enigvuldiging p la k t h e t
virus ee n te g en g este ld e s tr eng r n a
teg en h e t RNA aan en m a a k t op deze
m a n ie r kopieën van zijn gen o o m . D it
d u b bel-stren g s r n a ko m t n o rm a liter
n ie t in een cel vo o r en is d a a ro m een
sig n a a l vo o r d e g a sth e e rc e l d a t e r
g eva a r d re ig t.
interferon
sto fje s
g ep ro d u cee rd
door
het
im m u un systeem d ie in terfere re n m e t
herkennings receptoren" gestimuleerd worden) en uiteindelijk
dood gaat. In Hoofdstuk 4 laten we zien dat DCs beschermd
worden tegen echovirussen wanneer ze gestimuleerd worden
met het stofje poly I:C. Dit is een chemisch geproduceerd
molecuul dat erg sterk lijkt op dubbel-strengs viraal RNA.
Echter, wanneer DCs gestimuleerd werden met andere stofjes
die "patroon-herkennings receptoren" stimuleren (zoals
j.
i
■
i
_
i
stukjes van een bacterie) ontstond er geen bescherming van
(verh in d e ren van) virus replica tie.
de DC tegen infectie. Dubbel-strengs viraal RNA wordt door
V andaar d e n aam in terfero n .
enterovirussen gemaakt om zichzelf voort te planten (het
virus maakt kopieën van zijn eigen genoom). We laten zien dat CVB-geïnfecteerde cellen
worden opgegeten door DCs. Dit heeft tot gevolg dat de DCs het beschermende stofje
interferon gaan maken. Ook worden interferon-gestimuleerde genen aangezet. Dit alles
brengt de cellen in een zogenaamde "anti-virale" staat, waarbij ze beschermd worden
tegen infectie. In hoofdstuk 5 hebben we de interactie tussen CVB-geïnfecteerde cellen
en DCs verder onderzocht. Hierbij hebben we specifiek gekeken naar wat er gebeurt als
primaire ß-cellen worden geïnfecteerd en worden opgegeten door de DCs. We laten zien
dat eilandjes van Langerhans van een mens of een varken efficiënt worden opgegeten
door DCs. Ook een muizen ß-cel lijn, Min6 (cellen die lijken op ß-cellen uit de eilandjes
van Langerhans en makkelijk in het lab gekweekt kunnen worden), werd efficiënt door
de DC opgegeten. Opname van niet-geïnfecteerde eilandjes had geen effect op de DCs,
maar wanneer een DC virus-geïnfecteerde cellen opnam resulteerde dit in het maken
van interferon en de interferon-gestimuleerde genen. DCs die geïnfecteerde cellen
hadden opgenomen bleken ook beschermd tegen een opvolgende infectie. Voor al deze
140
Nederlandse Samenvatting
responsen was het virale RNA in de geïnfecteerde cellen nodig; dat is waarschijnlijk het
waarschuwingssignaal waar de DC op reageert. Ook het stofje interferon bleek onmisbaar
in de reactie van de DCs. Samenvattend laten we zien dat een antivirale immuunrespons
wordt gegenereerd door DCs nadat ze in aanraking komen met geïnfecteerde ß-cellen.
Dit leidt mogelijk tot belangrijke nieuwe inzichten in de rol die DCs spelen tijdens het
ontstaan van T1D. In hoofdstuk 6 hebben we de reactie van de eilandjes van Langerhans
op HEV-B-infectie onderzocht. Primaire humane eilandjes van mRNA
Langerhans die zijn geïnfecteerd met HEV-B startten een anti- m e sse n g e r RNA, o fw e l b oo d sch a p p e
,
,
«_
■
,
,
..
.
.
-
virale respons, gekenmerkt door de productie van interferon
en de interferon-gestimuleerde genen. Ook mRNA productie
,
. «■
i
i/ •
van andere cytokines en chemokines (signaal stoffen van
het immuun systeem) werd aangeschakeld. We konden niet
alleen het mRNA van cytokines en chemokines aantonen,
maar ook de eiwitten die door de cellen gemaakt werden
RNA. H et m RNA w o rd t a fg eschreven
van on s d n a
(onze g en etische
in fo rm a tie) en c o d e e rt vo o r
p ro d u ctie van e en b ep a a ld eiw it.
de
cytokinesenchemoknes
sto fje s d ie g em a a k t w o rd en d o o r het
im m u un systeem die w itte b loedcellen
a ctivere n (cy tokin e) o f m n u e ^ n
n a a r d e p la a ts van d e in fectie
(ch em okin e). D a a rn a a st kunnen ze
en uitgescheiden werden. Dus, wanneer infectie van de
eilandjes van Langerhans plaatsvindt starten deze een anti- o ° k d e o n tw ikkeling van n ieu w e witte
b lo e dce llen stim uleren .
virale respons en produceren ze cytokines en chemokines. Die
kunnen op hun beurt andere cellen van het immuunsysteem aantrekken naar de plaats
van de infectie. Hoewel deze stofjes geproduceerd worden ter bescherming van de ßcellen kunnen ze er ook voor zorgen dat langdurige inflammatie optreedt. Dit kan zelfs
bijdragen aan het ontstaan van auto-immuun reacties tegen de ß-cellen.
Onbalans in het immuunsysteem speelt waarschijnlijk een belangrijke rol tijdens
T1D ontwikkeling. Cellen in de alvleesklier worden kapot gemaakt tijdens T1D, maar
ook invloeden van buiten de pancreas kunnen belangrijk zijn. Hoofdstuk 7 onderzoekt
de aanwezigheid van enterovirus RNA in de witte bloedcellen van T1D patiënten en
gezonde controle individuen. In 4 van de 10 T1D patiënten is viraal RNA aangetroffen,
terwijl geen van de 20 controles positief was. Het nagenoeg afwezig zijn van viraal RNA
in keel samples en feces samples suggereert dat de aanwezigheid van viraal RNA in de
witte bloedcellen misschien een langdurige of chronische infectie betreft. Wat de rol van
deze langdurige infectie is in het ontstaan van T1D moet nog verder uitgezocht worden.
Echter, duidelijk is dat er hierdoor een continue stimulatie van het immuun systeem kan
plaatsvinden, die de balans van het hele immuun systeem kan beïnvloeden.
Toekomstperspectief
Bovenstaande bevindingen passen in een model voor het ontstaan van diabetes waarbij
enterovirussen aan de basis staan. Infectie van eilandjes van Langerhans leidt tot anti-virale
responsen en inflammatie, onder andere het produceren van cytokines en chemokines.
Dit leidt vervolgens tot het aantrekken en activeren van diverse witte bloedcellen. Die
kunnen schade veroorzaken aan de ß-cellen, waardoor deze niet goed meer functioneren.
Er wordt "gevaar" gesignaleerd door de witte bloedcellen, terwijl ook de eigen antigenen
aanwezig zijn. Dit kan tot gevolg hebben dat auto-immuun reacties tegen de ß-cellen
ontstaan. Dendritische cellen spelen hierbij waarschijnlijk een belangrijke rol; zij zijn
immers de witte bloedcellen die de balans tussen immuunresponsen en tolerantie in het
lichaam bewaren. De adaptieve responsen na opname van enterovirus-geïnfecteerde
cellen dienen nog verder onderzocht te worden.
141
Nederlandse Samenvatting
De grootste uitdaging is het vinden van een therapie tegen type 1 diabetes.
Wanneer een goed beeld is gecreëerd van de manier waarop T1D ontstaat kan ook
het best een passende therapie worden bedacht. Een belangrijk punt is het stoppen of
terugdraaien van de ß-cel schade. Om dit mogelijk te maken moet de homeostase in de
alvleesklier hersteld worden. Omdat de dendritische cellen zo'n belangrijke rol spelen
bij het in balans houden van het immuunsysteem zijn zij wellicht een goed doelwit om
op in te grijpen. Toekomstige therapieën die dendritische cellen gebruiken die tolerantie
induceren zijn in dat opzicht veelbelovend, aangezien ze zowel de auto-immuniteit
aanpakken en tegelijkertijd kunnen helpen om de homeostase te behouden/terug te
krijgen.
Het is belangrijk dat er verder onderzoek met patiënten gedaan wordt naar het
ontstaan van T1D. Daarnaast zijn toekomstige in vitro studies die gebruik maken van
humane eilandjes van Langerhans en humane DCs onmisbaar om goed inzicht te krijgen
in hun rol tijdens het ontstaan van type 1 diabetes. Bovendien kunnen ze belangrijke
nieuwe aanknopingspunten bieden om het immuunsysteem zó aan te sturen dat er
minder inflammatie en auto-immuniteit optreden.
142
Dankwoord
Curriculum Vitae
List of publications
Dankwoord
Dankwoord
AF! Nou ja, bijna dan... Er zijn veel mensen die een bijdrage hebben geleverd aan het tot
stand komen van mijn proefschrift.
Ten eerste wil ik Frank van Kuppeveld bedanken. Beste Frank, jij was degene die mij op
de stagemarkt jaren geleden enthousiast maakte voor een stage in de virologie. Toen je
me vroeg of ik een promotietraject binnen de virologie zag zitten heb ik nog wel even
getwijfeld tussen Utrecht en Nijmegen. Nu ben ik blij dat ik JA heb gezegd! We hebben
altijd een goed contact gehad en het was fijn dat ik altijd gewoon kon binnenlopen
naast ons wekelijkse overleguurtje. Ik heb enorm veel geleerd van jouw manier om
problemen aan te pakken. Je hebt me op allerlei vlakken dingen bijgebracht, van het
logisch indelen van een manuscript of presentatie tot aan het belang van de controles in
ieder experiment! Je oneindige enthousiasme is een voorbeeld voor me. Bedankt!
Vervolgens mijn promotor Joep Galama. Beste Joep, bedankt voor je input als klinisch
viroloog op het basaal wetenschappelijke onderzoek dat ik heb gedaan. Je hebt altijd een
iets andere kijk op het onderzoek en de manuscripten en daardoor juist commentaar op
punten waar anderen niet aan hebben gedacht! Fijn dat je iedere dinsdag een uurtje vrij
probeerde te plannen voor ons overleg.
Mijn tweede promotor Gosse Adema. Beste Gosse, jij gaf de onmisbare immunologieinput in ons onderzoek. Als immunoloog heb je altijd een net iets andere kijk gehad op
allerlei dingen dan virologen (en waren jij en Frank het niet altijd eens), maar dat was des
te leerzamer voor mij. Na mijn promotietraject ben ik bij jou begonnen als postdoc en ik
hoop veel van je te leren in de komende jaren!
Mijn twee paranimfen: Kjerstin en Matthijs. Jullie zijn degene die me tijdens de afgelopen
4% jaar het meest hebben geholpen met praktisch werk, maar waren zeker net zo
belangrijk voor de gezelligheid! Kjerstin, jij hebt me enorm geholpen met een groot
aantal experimenten. Daarnaast ben je onmisbaar op het virologie-lab en ben jij degene
die het lab goed draaiende houdt! Naast de werkzaamheden ben je een heel gezellige
collega; bedankt voor alle gezelligheid in de pauzes, op het lab en natuurlijk tijdens het
cellen uitvullen op maandag!
Matthijs, dankzij jou kon ik op een lopende trein springen aan het begin van
mijn aio-periode. Je hebt me wegwijs gemaakt in de wereld van de DCs! Je bent enorm
gedreven en ik heb er bewondering voor dat je ook nog geneeskunde (theorie) hebt
afgerond tijdens je promotie! Onze samenwerking was vanaf het begin af aan erg prettig
en het was gezellig om tijdens de buffy's lekker te kunnen kletsen! Samen hebben we
een aantal mooie papers, ik ben er trots op! Ondanks al die jaren trappen lopen heb ik
nog steeds geen goede co n d itie.
Alle collega's van de virologie wil ik bedanken voor de gezellige periode op het lab. Fabrizio,
het was leerzaam, maar vooral gezellig om met jou een Utje te delen. Ook al was GAAP
voor jou uiteindelijk niet zo'n succes, ik hoop dat je nu op je plek zit! Danny, voor alle
biochemische vragen kon ik bij jou terecht! Buiten dat was je gezellig en een aantal van
je uitspraken zijn nog altijd blijven hangen ("ik heb geen slechte dag, ik heb een slecht
144
Dankwoord
millennium"). Jan, jij hebt een enorme hoeveelheid virologie kennis waarvoor mensen
bij je aankloppen. Het zijn echter de droge, maar gevatte opmerkingen die ik niet snel zal
vergeten. Stanley en Kelly, als medeaio's weten jullie precies welke ups en downs er zijn
tijdens je promotie. Kelly, leuk om met jou op congres te gaan naar de kou (ook al was
het uiteindelijk toch geen -30°C) en daarna Helsinki. Stanley, leuk om jou van een andere
kant te leren kennen tijdens de salsa-lessen! Lonneke en Hilde, medecellenuitvullers!
Altijd gezellig op de maandagmiddag! Lonneke, succes met de antivirals en de rest van
je promotie-onderzoek! Qian, ik doe het gewoon in het Nederlands! Het was gezellig
samen op de Europic in Barcelona. Succes met de RLHs en veel geluk met Andy!
De RNAi-groep onder leiding van Ronald kwam het virologie-lab versterken.
Ronald jij bent een goede en kritische wetenschapper. Van jouw kijk op dingen heb ik
veel geleerd. Joël, Koen en Walter, succes met het ontrafelen van de RNAi pathways
tijdens virale infectie en het karakteriseren van RNAi-remmers in nieuwe virussen.
Els en Mike, jullie gingen vrij snel weg nadat ik begon als junior onderzoeker.
Bedankt voor alle leerzame en gezellige dingen, zowel tijdens mijn studenten tijd als mijn
aio-periode.
De studenten die me geholpen hebben tijdens mijn jaren bij de virologie
verdienen zeker ook een plekje. Marijke, Neeltje en Katharina: succes met jullie PhDs en
buitenlandse stages. Het begeleiden van een student is volgens mij net zo leerzaam als
het doen van een stage zelf!
Ook al zit het research-lab van de virologie een eindje weg van de diagnostiek, toch kon ik
altijd terecht voor advies. Judith, bedankt dat je tussen al je diagnostiek werkzaamheden
door tijd maakte om me te helpen met het T1D patiënten project. W illem, bedankt voor
je interesse en input. Marij, bedankt voor al je hulp bij de celkweek. Marian, jij was
degene die zorgde dat de afspraken met Joep goed liepen, bedankt daarvoor!
De buren van het parasitologie lab wil ik bedanken voor alle hulp en gezelligheid aan
de koffietafel. Matthew en Anne, bedankt voor de hulp met opzetten van PBMCexperimenten en FACS kleuringen. Ben, Krystelle, Karina, Ivo, Martijn, W ill, Rob, Adrian,
Robbert en alle anderen, bedankt! De gezamenlijke Wii-avonden en bowling competities
waren een groot succes! Dat er nog veel mogen volgen! Natuurlijk wil ik ook de buren
van de urologie bedanken!
Een deel van mijn aio-periode bestond uit trappen lopen naar de 5e, en alle mensen
van het TIL die me hebben geholpen verdienen ook een plekje in dit dankwoord. Liza,
bedankt voor al je praktische ondersteuning. Al je kleuringen en qPCRs hebben enorm
geholpen! Maaike L, Maaike vH-K, Dagmar, Bas, Jurjen en Marleen bedankt voor alle
hulp bij kloneren, qPCRs, statistiek, pDC proeven etc. En natuurlijk alle Tillers bedankt
voor de gezelligheid en behulpzaamheid.
Huib, bedankt voor je hulp met de confocal.
QM Diagnostics, in de personen van Marleen, Patrick en Ronald, bedankt voor alle hulp
met de LC480!
145
Dankwoord
Tijdens de afgelopen 4 jaar zijn er samenwerkingen gestart met verschillende afdelingen.
Henk-Jan Aanstoot, Mu Bruining, Ciska Westerlaken, Wil Allebes en Kjeld van Houwelingen
wil ik bedanken voor het patiënten werk en de HLA-typeringen. Mihai, Trees en Liesbeth,
bedankt voor jullie hulp bij de PBMC-experimenten met RSV en CVB. Dit deel van het
werk is ongoing, ik hoop dat het nog mooie resultaten oplevert! Richard, Tim en Mark,
bedankt voor de hulp met al het cytokine-werk! Paul and Paola, thank you for the antiMda5 antibody! We have used it a lot!
Dear Jon, I would like to thank you for the opportunity to work in your lab for 6 weeks.
You broadened my view and taught me the mouse-world of diabetes. I really enjoyed all
the discussions we had in the car on the way to work! Furthermore, I was a guest in your
family during my stay! Cheryl, Dominic and Jack, thank you for making me part of the
Piganelli family! Cheryl, you are still the Queen of Margarita's (thanks for sending them
by fedex!). Jack and Dominic, I really enjoyed having two little brothers for 6 weeks! You
taught me the guitar hero! Also the people in the Piganelli lab and islet-isolation lab
should not be forgotten: Jennifer, Hubert, Gina, Martha, Rita and Susan: thanks (for help
in the lab and for the nice time at the baseball games etc.)! Rita and Massimo, thank you
for all the help with the primary pancreatic islets. It is very important for my research!
Zonder ontspanning is een promotietraject niet vol te houden! Gelukkig waren een
aantal mensen om lekker mee te gaan eten, stappen of gewoon lekker bij te kletsen.
Anouk, Richard, Chris, Marianne, Joost, Sylvie, Karla, Roel, Femke, Kim, Louis, Wouter,
Janneke, Ralph, Wendela, bedankt voor alle gezelligheid en interesse!
De basis voor dit alles is natuurlijk Thuis! Lieve pap en mam, bedankt voor alles! Jullie
hebben me altijd in alles gesteund in al mijn keuzes en ik ben enorm blij met jullie!
Ook al is het denk ik moeilijk om 5 kinderen op te voeden; jullie hebben ons allemaal
vrij gelaten om te gaan doen wat we zelf kozen. Hester & Jelle, Jolien, Tijmen, Luuk en
M arriët, het is altijd enorm gezellig als we allemaal thuis zijn. Broeries, leuk dat jullie ook
in het lab komen te staan!
Hans, Alies, Thijs, Petra en Luuk, mijn tweede familie, bedankt voor al jullie
interesse en de gezelligheid bij de "Te Riet"familie!
Lieve Joost, bedankt dat je er altijd bent! Jij bent degene die mijn leven in balans houdt!
Ik hou van je!
146
Curriculum Vitae
Curriculum Vitae
Barbara Maria Schulte werd op 12 juli 1982 geboren te Almelo. In 2000 haalde zij haar
VWO diploma op het Pius X College te Almelo. Aansluitend volgde zij de studie Biologie
aan de Katholieke Universiteit Nijmegen (Thans Radboud Universiteit Nijmegen) met de
afstudeerrichting Medische Biologie. Tijdens deze studie liep ze 9 maanden stage op
de afdeling Medische Microbiologie onder begeleiding van Ing. Mike de Bruijni en Dr.
Frank van Kuppeveld. Dit onderzoek richtte zich op de functie van het Leader eiwit van
het mengovirus, dat antivirale interferon responsen in de gastheer kan onderdrukken.
Een tweede stage van 9 maanden werd gedaan aan de Universiteit Utrecht in het lab
Fysiologische Chemie onder leiding van Dr. Karen Lyle en Prof. Dr. Hans Bos. Tijdens deze
stage werd de kleine GTPase Rhes (Ras homolog enriched in striatum) gekarakteriseerd.
Gedurende de studie heeft zij vier opeenvolgende jaren geassisteerd bij het vak
"Functionele Histologie" onder leiding van Dr. Toine Lamers (en later ook Dr. Ineke van der
Zee). Als nevenactiviteit was ze actief bij de feestcommissie van de Nijmeegse Biologen
vereniging BeeVee en was ze meerdere malen als mentor betrokken bij de introductie
van eerstejaars biologie studenten.
Na het behalen van haar doctoraal (Cum Laude) begon ze als junior onderzoeker
op de afdeling Medische Microbiologie van het UMC St. Radboud. Onder begeleiding
van Dr. Frank van Kuppeveld en Prof. Dr. Joep Galama werd het promotieonderzoek
uitgevoerd wat in dit proefschrift beschreven is. Gedurende het promotie traject bracht
ze een 6 weken durend werkbezoek aan het lab van Dr. Jon Piganelli in het Rangos
Diabetes Centre van de University of Pittsburgh (Pittsburgh, Pennsylvania, Verenigde
Staten).
Thans is ze werkzaam als postdoc in het Tumor Immunologie laboratorium van
het UMC St. Radboud onder begeleiding van Prof. Dr. Gosse Adema. Hier doet zij in een
Juvenile Diabetes Research Foundation-gefundeerde studie onderzoek naar de interactie
tussen enterovirussen, primaire humane dendritische cellen en insuline-producerende
cellen.
147
List of publications
List of publications
Kramer M, Schulte BM, Toonen LW, de Bruijni MA, Galama JM, Adema GJ, van
Kuppeveld FJ.
Echovirus infection causes rapid loss-of-function and cell death in human dendritic
cells.
Cell Microbiol. 2007 Jun;9(6):1507-18. Epub 2007 Feb 9.
Hato SV, Ricour C, Schulte BM, Lanke KH, de Bruijni M, Zoll J, Melchers WJ, Michiels T,
van Kuppeveld FJ.
The mengovirus leader protein blocks interferon-alpha/beta gene transcription and
inhibits activation of interferon regulatory factor 3.
Cell Microbiol. 2007 Dec;9(12):2921-30.
Kramer M, Schulte BM, Toonen LW, Barral PM, Fisher PB, Lanke KH, Galama JM, van
Kuppeveld FJ, Adema GJ.
Phagocytosis of picornavirus-infected cells induces an RNA-dependent antiviral state
in human dendritic cells.
J Virol. 2008 M ar;82(6):2930-7. Epub 2008 Jan 9.
Schulte BM, Kramer M, Ansems M, Lanke KH, van Doremalen N, Piganelli JD, Bottino R,
Trucco M, Galama JM, Adema GJ, van Kuppeveld FJ.
Phagocytosis of enterovirus-infected pancreatic beta-cells triggers innate immune
responses in human dendritic cells.
Diabetes. 2010 Jan 13. [Epub ahead of print]
Schulte BM, Bakkers J, Lanke KH, Melchers WJ, Westerlaken C, Allebes W, Aanstoot HJ,
Bruining GJ, Adema GJ, Van Kuppeveld FJ, Galama JM.
Detection of enterovirus RNA in peripheral blood mononuclear cells of type 1 diabetic
patients beyond the stage of acute infection.
Viral Immunol. 2010 Feb;23(1):99-104.
Kramer M, Schulte BM, Eleveld-Trancikova D, van Hout-Kuijer M, Toonen LW, Tel J, de
Vries IJ, van Kuppeveld FJ, Jansen BJ, Adema GJ.
Cross-Talk between Human Dendritic Cell Subsets Influences Expression of RNA
Sensors and Inhibits Picornavirus Infection.
J Innate Immun. 2010 Mar 20. [Epub ahead of print]
148
© Copyright 2026