7 Annual Centura Health EVIDENCE-BASED PRACTICE, RESEARCH and INNOVATION CONFERENCE
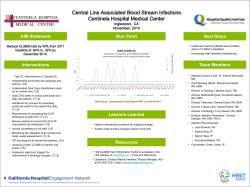
7th Annual Centura Health EVIDENCE-BASED PRACTICE, RESEARCH and INNOVATION CONFERENCE “Using Evidence to be Our Best” Friday, November 14, 2014 DU School of Hotel, Restaurant and Tourism Building # 204; Main Dining Room AGENDA 7:15 a.m. – 8:00 a.m. Registration 8:00 a.m. – 8:10 a.m. Welcome and Reflection Martha L. Grubaugh, RN, MS, NEA-BC 8:10 a.m. – 8:15 a.m. Opening Remarks Lavone Hastings, BSN, M.MGT., RN-BC 8:15 a.m. – 9:15 a.m. Translating Best Evidence into Daily Practice: A New Norm for Reliability Mary Beth Flynn Makic, RN, PhD, CNS, CCNS, FAAN 9:15 a.m. – 9:45 a.m. Break - Visit Poster Presentations and Exhibits 9:45 a.m. – 10:45 a.m. Learning Sessions (Choose 1, 2 or 3) Main Dining Room 1. Designing and Implementing a Nursing Peer Review Process in a Hospital Striving for Magnet Status (TL) Annie Stallings, RN, BSN, CCRN, Ronda Charboneau, RN, MS, CCRN Kate Knight, RN, CEN, CSTR, Eileen Havey, RN, MA, CNOR Sustaining the Culture of Safety: Strategies to Maintain the Gains (EP) Cynthia Oster, PhD, MBA, APRN, CNS-BC, ANP, Sherrie Deakins, MS, RN, CPPS Paradigm Shift: Infusing “Proactive” Lean and High Reliability Characteristics into Your Organization’s “Reactive” Safety Culture (TL) Jane Braaten, PhD, RN, CNS/ANP, Sheri Deakins, RN, MS, CPPS Room 231 2. Driving CLABSI Rate to Zero: Implementation of a Prevention Bundle (EP) Tiffany Curtice, RN, VA-BC, Erika Anderson, RN, BSN, CRNI Patient and Staff Satisfaction: Isolation Precautions (EP) Sarah Baumberger, RN, BSN Development of Evidence Based Guidelines for Ambulation after DVT(EP) Aspen Kunisch, PT, DPT, NCS, Susan Scherer, PT, PhD Room 229 3. We are not Machines: Post Code Pause in the Emergency Department (EP) Heather Liska, RN, BSN, MPA, CEN, Darcy Copeland, PhD, RN Treatment Efficacy of Dialectical Behavior Therapy Skills Training Group for Clients with Dependent Personality Disorder (EP) Stephanie Eells, MS, LPC, DBTC, Amanda Phillips, BA, Kathryn Wickman, BSW Cardiac Short Stay: Meeting Healthcare Challenges in the Current Healthcare Landscape (TL) Karen Kennedy, RN, BSN, CEN, Toni Standley, MSN, RN, ANP-BC 1 10:55 a.m. –11:55 a.m. Main Dining Room Learning Sessions (choose 4, 5 or 6) 4. Patient Outcomes Before and After the Adoption of the New Standardized Swallowing Assessment (SSA) Bedside Nursing Evaluations (EP) Toni Schoenleber, RN, BSN Improvement of Door to IV tPA in Acute Ischemic Stroke Using Quality Improvement Methods (EP) Alex Graves, MS, ANP, ANVP, Criss Potzer, RN, Christy Casper, MS, ANP, Rick Smith, MD The Rationale for Utilizing the “Flipped Classroom” Model for New Hire Orientation (SE) Penne McPherson, RN, BSN, MS Room 229 5. The Many Faces of Peer Review: Ten Strategies for Success (TL) Tiffany Meister, RN, BSN, CCRN Planned Paradigm Shifts – Empowering Nursing for Change (TL) Susan Barnett, RN, MSN, ONC Developing a Nursing Senate (TL) Karen Wilson, RN, MN, CGRN, Andi Rottman, BSN, RN-C, Renee Blattman, BSN, MBA Room 231 6. Pain Relief Starts in the Prehospital Setting: Is It Effective? (NKII) Mary Meyers, MS, EMT-P, Judy Jo Mackie, RN, MS, CEN, Brian Sobeck, MBA, EMT-P A Community Based Model for Concussion Management (NKII) Kelley Lau, RN, BSN, MBA Igniting Passion through an Educational Framework for Reaching Coloradans: The Stroke Experience (SE) Ellen Lane, RN, MSN, CCRN, Ashley Trujillo, RN 11:55 a.m. – 1:00 p.m. Lunch provided – Visit Poster Presentations and Exhibits 1:00 p.m. – 2:00 p.m. Learning Sessions (choose 7 or 8) Room 229 7. Energize with Exercise: Improving Functionality in Oncology Patients with Outpatient Rehabilitation (NKII) Lynette Olson, PTA, CES, Andi McDonough, MPT Improving Head and Neck Cancer Patient Outcomes with Multidisciplinary Team Management (EP) Helen Gercas, RN, OCN, Debra Flesher-Bratt, RDH, Teri Meno, RD Implementation of Evidence-Based Guidelines for Assessment of Adult Cancer Pain (NKII) Mary Murray, RN, BSN, CHPN Main Dining Room 8. Use of Therapeutic Hypothermia in Patients with Out-of-Hospital Cardiac Arrest and Resuscitation (EP) Amber Gates, RN, BSN c Early Progressive Mobility of the Artificially Ventilated Patient (NKII) Cortney Parsudi, RN, BSN, CCRN Addressing the Issue of Alarm Fatigue in the Cardiac ICU (NKII) Abbi-Lynn Washington, RN, MS, APRN, CCRN 2 2:00 p.m. – 2:30 p.m. Break - Visit Poster Presentations and Exhibits 2:30 p.m. – 3:30 p.m. Crew Resource Management - Captain Valerie V. Scott, ATP 3:30 p.m. – 3:45 p.m. Closing and Announcement of Poster Winners Magnet Model Components: TL=Transformational Leadership; EP=Exemplary Professional Practice; SE=Structural Empowerment; NKII=New Knowledge, Innovations and Improvements 3 7th Annual Centura Health EVIDENCE-BASED PRACTICE, RESEARCH and INNOVATION CONFERENCE “Using Evidence to be Our Best” Friday, November 14, 2014 DU School of Hotel, Restaurant, and Tourism Building #204 PURPOSE This conference will demonstrate how evidence-based practice and research provide a foundation for professional clinical practice. Podium Presentation Objectives Translating Best Evidence into Daily Practice: A New Norm for Reliability Mary Beth Flynn Makic, RN, PhD, CNS, CCNS, FAAN 1. Define evidence based practice. 2. List two mechanisms that can be implemented to move current best evidence into your daily practice. 3. Describe methods of finding national resources to apply best evidence in practice. Designing and Implementing a Nursing Peer Review Process in a Hospital Striving for Magnet Status (TL) Annie Stallings, RN, BSN, CCRN Ronda Charboneau, RN, MS, CCRN Kate Knight, RN, CEN, CSTR Eileen Havey, RN, MA, CNOR 1. Define the Magnet criteria required for nursing Peer Review Process. 2. List three events which are appropriate for referral to Nursing Practice Review. 3. State two elements required to maintain trust in a Peer Review Process. Sustaining the Culture of Safety: Strategies to Maintain the Gains (EP) Cynthia Oster, PhD, MBA, APRN, CNS-BC, ANP Sherrie Deakins, MS, RN, CPPS 1. Identify vulnerabilities, “perfect” performance and adherence to regulations and policies across the care continuum. 2. Discuss steps in developing culture change supporting individual professional accountability and healthcare system performance. Paradigm Shift: Infusing “Proactive” Lean and High Reliability Characteristics into Your Organization’s “Reactive” Safety Culture (TL) Jane Braaten, PhD, RN, CNS/ANP Sheri Deakins, RN, MS, CPPS 1. Describe the usefulness of HRO principles and Lean Techniques to patient safety in the hospital. 2. Describe HRO characteristics and Lean Techniques as applied to several patient safety initiatives. 4 Driving CLABSI Rate to Zero: Implementation of a Prevention Bundle (EP) Tiffany Curtice, RN, VA-BC Erika Anderson, RN, BSN, CRNI 1. Identify CLABSI prevention bundle guidelines. 2. Identify prevention bundle implementation strategies. 3. Identify strategies to drive prevention bundle adherence. 4. Analyze cost avoidance. Patient and Staff Satisfaction: Isolation Precautions (EP) Sarah Baumberger, RN, BSN 1. Improving staff satisfaction because we will be able to save time and resources by being able to check on our patients prior to donning PPE. 2. Improving patient satisfaction because they will feel less isolated if we have the freedom to step into their room without PPE. It will also increase safety, as staff members are able to check on their patients more frequently. 3. We will be maintaining infection prevention- Since we are not coming into physical contact with objects, and are maintaining a 6 foot distance from the patient while inside the safe zone, we still follow CDC protocol for preventing infection. 4. Patients and family members will know that we respect the need for precautions when we stay within the “Safe Zone.” 5. Patent and staff surveys will be handed out for two months prior to “Safe Zone” implementation to gather data based on the current methods used for Isolation Precautions. 6. The “Safe Zone” will then be implemented for two months, in which the same surveys will be given to patients and staff in order to assess satisfaction after the new protocol has been put into practice. 7. After data has been collected and assessed, further steps regarding the “Safe Zone” will be decided. Development of Evidence Based Guidelines for Ambulation after DVT (EP) Aspen Kunisch, PT, DPT, NCS Susan Scherer, PT, PhD 1. Describe the steps to develop and implement evidence-based protocol in the inpatient setting. 2. Apply evidence to determine when to ambulate patients after DVT. We are not Machines: Post Code Pause in the Emergency Department (EP) Heather Liska, RN, BSN, MPA, CEN Darcy Copeland, PhD, RN 1. Describe the process for developing and implementing a post code pause program in an emergency department. 2. Discuss the effect of a post code pause on staff perceptions of readiness to return to work and ability to pay homage to patients. Treatment Efficacy of Dialectical Behavior Therapy Skills Training Group for Clients with Dependent Personality Disorder (EP) Stephanie Eells, MS, LPC, DBTC Amanda Phillips, BA Kathryn Wickman, BSW 1. Distinguish similarities and differences between Dependent Personality Disorder and Borderline Personality Disorder. 2. Examine how Dialectical Behavior Therapy (DBT) addresses helplessness, attachment, and fear of abandonment for clients with Dependent Personality Disorder. 5 Cardiac Short Stay: Meeting Healthcare Challenges in the Current Healthcare Landscape (TL) Belinda Shaw, RN, MS, CEN, NE-BC Toni Standley, MSN, RN, ANP-BC Brande Andrews, RN, BSN, CEN 1. Explain the clinical and financial benefits of Cardiac Observation Units in our current healthcare system. 2. Define two distinct nursing roles used in a Cardiac Short Stay Unit. 3. Review the five year quality outcomes for the Cardiac Short Stay Unit. Patient Outcomes Before and After the Adoption of the New Standardized Swallowing Assessment (SSA) Bedside Nursing Evaluations (EP) Toni Schoenleber, RN, BSN 1. Discuss the evaluation of data including length of stay in the hospital and Intensive care units to see if there is a change in patient outcomes after the initiation of an evidence based practice nursing bedside swallow study. Improvement of Door to IV tPA in Acute Ischemic Stroke Using Quality Improvement Methods (EP) Alex Graves, MS, ANP, ANVP Criss Potzer, RN Christy Casper, MS, ANP Rick Smith, MD 1. Explain the importance of treating stroke quickly. 2. Discuss how to apply QI methodologies to other improvement projects. The Rationale for Utilizing the “Flipped Classroom” Model for New Hire Orientation (SE) Penne McPherson, RN, BSN, MS 1. Verbalize how the ‘Flipped Classroom’ model of learning differs from the traditional classroom model. 2. Identify how utilizing the ‘Flipped Classroom’ model for New Hire Orientation supports cost-savings. The Many Faces of Peer Review: Ten Strategies for Success (TL) Tiffany Meister, RN, BSN, CCRN 1. Name 5 different strategies for peer review. 2. Discuss how to disseminate peer review throughout an organization. Planned Paradigm Shifts – Empowering Nursing for Change (TL) Susan Barnett, RN, MSN, ONC 1. Verbalize the history and current state of health care practices related to resource allotment and burden of need. 2. Observe the impact of a change model for facilitating nursing paradigm shifts. Developing a Nursing Senate (TL) Karen Wilson, RN, MN, CGRN Andi Rottman, BSN, RN-C Renee Blattman, BSN, MBA 1. State the reasoning to change the shared governance structure. 2. State the difference between a nursing senate model and a practice council model of shared governance. 3. State the impact that the nursing senate has had on patient care. 6 Pain Relief Starts in the Prehospital Setting: Is It Effective? (NKII) Mary Meyers, MS, EMT-P Judy Jo Mackie, RN, MS, CEN Brian Sobeck, MBA, EMT-P 1. The student will summarize the differences found between reported pain levels prior to arrival at the emergency department and after arrival. 2. The student will discuss the data presented showing the changes in pain levels and association with age, chief complaint, admission as inpatient, and repeat doses of pain medication. A Community Based Model for Concussion Management (NKII) Kelley Lau, RN, BSN, MBA 1. Describe the value of having collaborative community based traumatic brain injury program. 2. Identify 3 best practices for the care of the TBI patient. Igniting Passion through an Educational Framework for Reaching Coloradans: The Stroke Experience (SE) Ellen Lane, RN, MSN, CCRN Ashley Trujillo, RN 1. Define the problem this project addressed. 2. Literature review and recommendations. 3. St. Mary Corwin’s implementation plan. 4. Future endeavors. 5. Framework and conclusions. 6. Energize with Exercise: Improving Functionality in Oncology Patients with Outpatient Rehabilitation (NKII) Lynette Olson, PTA, CES Andi McDonough, MPT 1. Identify two side effects of cancer or its treatment that can be improved with physical therapy. 2. Discuss the importance of screening and referring appropriate patients early in their treatment process to improve baseline mobility, safety and fall risk scores. Improving Head and Neck Cancer Patient Outcomes with Multidisciplinary Team Management (EP) Helen Gercas, RN, OCN Debra Flesher-Bratt, RDH Teri Meno, RD 1. Identify how a multidisciplinary approach can manage side effects for the head and neck cancer population through treatment. 2. Describe how team members develop unified goals for patients and the methods used to meet patients’ individualized needs. Implementation of Evidence-Based Guidelines for Assessment of Adult Cancer Pain (NKII) Mary Murray, RN, BSN, CHPN 1. Identify the importance of including pain interference in an assessment of cancer pain as per National Comprehensive Cancer Network guidelines. 2. Define pain interference. 3. Identify the correlation between “nurse engagement” and patient satisfaction with pain management. 7 Use of Therapeutic Hypothermia in Patients with Out-of-Hospital Cardiac Arrest and Resuscitation (EP) Amber Gates, RN, BSN 1. Review 2013 ACCF/AHA Guideline for the Management of ST-elevation Myocardial Infarction. 2. Review research supporting use of therapeutic hypothermia in patients with out-of-hospital cardiac arrest. 3. Discuss Nielsen, et al. study and new suggestions for treatment. Early Progressive Mobility of the Artificially Ventilated Patient (NKII) Cortney Parsudi, RN, BSN, CCRN 1. Articulate two examples of the benefits of early mobility in the artificially ventilated patients. 2. Describe three patient outcomes related to the implementation of an early progressive mobility protocol for artificially ventilated patients. Addressing the Issue of Alarm Fatigue in the Cardiac ICU (NKII) Abbi-Lynn Washington, RN, MS, APRN, CCRN 1. Define alarm fatigue and its causes in the ICU. 2. Identify the three best practice interventions to decrease alarm fatigue. Crew Resource Management Captain Valerie V. Scott, ATP 1. Define Crew Resource Management. 2. Provide education on various human factors which affect performance. 3. Explore ways CRM applies within the clinical environment to impact quality. 8 7th Annual Centura Health EVIDENCE-BASED PRACTICE, RESEARCH and INNOVATION CONFERENCE “Using Evidence to be Our Best” Friday, November 14, 2014 DU School of Hotel, Restaurant, and Tourism Building #204 Podium Presentation Abstracts Learning Session 1: “Designing and Implementing a Nursing Peer Review Process in a Hospital Striving for Magnet Status” Annie Stallings, RN, BSN, CCRN, Ronda Charboneau, RN, MS, CCRN, Kate Knight, RN, CEN, CSTR, Eileen Havey, RN, MA, CNOR Nursing Peer Review (NPR) is an essential part of being a Magnet Organization and affords bedside nurses the opportunity to bring bedside practice in line with current evidence and improve processes. The process St Anthony Hospital used to develop a NPR committee will be discussed. The NPR is a central place to bring nursingrelated concerns. Cases involving a near miss, error, process problem, or a success, are referred by any discipline to a multidisciplinary team primarily comprised of bedside nurses from all specialties in the hospital. The NPR meets monthly and has reviewed over 15 cases involving individual nurses’ practice as well as implemented process changes to improve patient care and nursing workflow in several high-profile cases. NPR is evaluated through the improvement in nursing workflow and processes, reduction in cases resulting in similar patient harm, and the empowerment of nurses to effect change as measured by PES scores. “Sustaining the Culture of Safety: Strategies to Maintain the Gains” Cynthia Oster, PhD, MBA, APRN, CNS-BC, ANP, Sherrie Deakins, MS, RN, CPPS Culture impacts performance. Three barriers to a culture of excellence are “failure to see,” “failure to move,” and “failure to finish.” The purpose of the initiative described was to create an organizational culture of personal and professional accountability by transforming and enculturating a no-fail exemplary practice environment. Methods used to overcome the above barriers are described. Since initiation of this cultural transformation initiative in 2009, patient harm adverse events have decreased from 29 to 12 in 2013. Estimated cost saving for avoidable harm approached $200,000 in 2013. “Paradigm Shift: Infusing “Proactive” Lean and High Reliability Characteristics into Your Organization’s “Reactive” Safety Culture” Jane Braaten, PhD, RN, CNS/ANP, Sheri Deakins, RN, MS, CPPS The five principles of High Reliability Organizations (HRO) as defined by Weick and Sutcliffe (2001) provide a framework in which to change the current focus of patient safety and improve outcomes. Lean principles further enhance the framework of current financial limitations by adding efficiency and value. The integration of quality, cost and value are imperative not only for hospitals to survive, but thrive. This presentation will contrast limitations and benefits of traditional models with new safety science models. Examples will be presented demonstrating the integration of HRO and Lean characteristics within an urban, Magnet designated hospital. 1 Learning Session 2: “Driving CLABSI Rate to Zero: Implementation of a Prevention Bundle” Tiffany Curtice, RN, VA-BC, Erika Anderson, RN, BSN, CRNI CLABSI is the most deadly HAI with a mortality rate between 12% and 25%. The excess cost per case for nosocomial CLABSI is approximately $17,000, costing the healthcare system nearly $700 million annually. In 2012, an evidence-based CLABSI prevention bundle was implemented. Adherence to prevention strategies and CLABSI rates were measured from FY12 to YTD FY14. Implementation strategies of the prevention bundle included standardized education for intravascular catheter care; focused staff education on central catheter maintenance; and an infection surveillance program. The CLABSI rate decreased 102% from 1.02 in FY12 to 0.00 in YTD FY14. There was a 100% reduction in the number of CLABSIs from FY12 (n = 10) to YTD FY14 (n =0) with 347 CLABSI free days. The Intensive Care Unit is 456 days CLABSI free. Adherence to the prevention bundle has improved to 86% house wide. “Patient and Staff Satisfaction: Isolation Precautions” Sarah Baumberger, RN, BSN This project involved implementing Safe Zones, or entryways in Contact and Droplet patient rooms, in which PPE is unnecessary, on the Post-Surgical/Trauma/Oncology unit at St. Anthony’s Hospital. Patients and staff were given surveys in order to assess satisfaction prior to and after implementation. “Development of Evidence Based Guidelines for Ambulation after DVT” Aspen Kunisch, PT, DPT, NCS, Susan Scherer, PT, PhD Historically, patients with the diagnosis of deep vein thrombosis (DVT) were managed conservatively with bed rest but recent literature supports early ambulation. Recent advances in managing patients with DVT include new regimens of prophylactic anticoagulation and earlier mobilization, however no detailed evidence based guidelines for physical therapists (PTs) regarding the timing of ambulation exist. A DVT committee consisting of 7 PTs and occupational therapists (OTs) was created to analyze current evidence and create an updated, evidence based guideline. This presentation will describe the interdisciplinary process used to develop and implement an evidence-based algorithm for patient ambulation after DVT in the inpatient setting. These clinical questions were posed: 1.Does ambulation of a patient with positive DVT increase the risk of further propagation of the clot, PE, or death? 2. What is the recommended time frame for starting ambulation with a patient under the following conditions? A.After a suspected DVT pending results of the noninvasive vascular assessment (NIVA)? B.After a diagnosed DVT limited to the calf? C.After a proximal DVT? 3. Should a patient with positive DVT ambulate with compression stockings? Learning Session 3: “We are not Machines: Post Code Pause in the Emergency Department” Heather Liska, RN, BSN, MPA, CEN, Darcy Copeland, PhD, RN Frontline staff members are frequently exposed to extreme events, predisposing them to the effects of vicarious trauma. The goal of the Post Code Pause (PCP) is to promote a healing work environment and reduce compassion fatigue by providing time for healthcare workers responding to codes to reflect on their own reactions and feelings, honor each other, and honor the lives of patients for whom they care. The development and implementation of the PCP in the emergency department will be described. Post implementation there was a 33% increase in the number of people reporting they have time to pay homage to patients at least half of the time (43% vs 76%) and a 31% increase in respondents feeling they are given adequate time to regroup before returning 2 to their assignments (40% vs 71%). The majority of respondents (53%) feel that attending a pause is helpful in reducing compassion fatigue. “Treatment Efficacy of Dialectical Behavior Therapy Skills Training Group for Clients with Dependent Personality Disorder” Stephanie Eells, MS, LPC, DBTC, Amanda Phillips, BA, Kathryn Wickman, BSW The self-sabotaging of progress made in the Dialectical Behavior Therapy (DBT) Skills Training Group by clients with Dependent Personality Disorder is of concern for group therapists. The purpose of this investigation is to show that building mastery with skills from the four DBT Modules: Mindfulness, Distress Tolerance, Emotion Regulation, and Interpersonal Effectiveness can reduce the negative reactions resulting in the fear of abandonment for clients with Dependent Personality Disorder. These clients will gain self-confidence, which impacts a sense of self-autonomy to diminish the need for reassurance and support from others before making everyday decisions. The results of the BASIS-24, a behavioral health assessment, at Intake, at the end of each 6-7 week Skill Module, and at graduation will be scored and compared with three groups: 1) those clients with a psychiatric diagnosis of an Affective Disorder, 2) clients with an Affective Disorder and Borderline Personality Disorder, and 3) clients with an Affective Disorder and Dependent Personality Disorder. Our hypothesis is that DBT Skills Training Group is effective for clients with Dependent Personality Disorder in reducing maladaptive behavior due to the fear of abandonment. “Cardiac Short Stay: Meeting Healthcare Challenges in the Current Healthcare Landscape” Belinda Shaw, RN, MS, CEN, NE-BC, Toni Standley, MSN, RN, ANP-BC, Brande Andrews, RN, BSN, CEN Cardiac Short Stay (CSS) is a process of care rather than a specific geographical area of the hospital. The primary function of the CSS unit is to provide extended diagnostic testing for patients with unspecified chest pain. This presentation will discuss the development, strategic plan, design and outcomes of a sustained nurse led CSS unit. Utilization of an advanced practice nurse in coordination with a designated cardiac short stay nurse, to meet the challenges of more than 350 patients (5%) presenting annually in the emergency department with low-risk cardiac chest pain will be described. Focused details will discuss the development of standard treatment algorithms, strengthened relationships with EMS, and measurement of patient and physician satisfaction scores. Outcomes include decreased cost per case by $1400 per patient, decreased door to ECG time to less than ten minutes, and decreased length of stay to less than 10 hours in the ED with 92% of patients discharged. Learning Session 4: “Patient Outcomes Before and After the Adoption of the New Standardized Swallowing Assessment (SSA) Bedside Nursing Evaluations” Toni Schoenleber, RN, BSN Assessments for dysphagia are part of policy to predict who would be at risk for aspiration or complication after a stroke. This study examined the outcomes before and after the adoption of the new Standardized Swallowing Assessment (SSA) bedside nursing evaluation at St Anthony Hospital. This study was to ensure the implementation of the SSA would correctly identify patients with dysphagia and the appropriate nutrition was provided to patients in a timely manner. Patients admitted with stroke three months prior to initiation of the SSA and three months after were examined via retrospective chart review. Data topics include ICU and hospital length of stay, time without nutrition and time to speech therapy consult. Preliminary results will be shared. 3 “Improvement of Door to IV tPA in Acute Ischemic Stroke Using Quality Improvement Methods” Alex Graves, MS, ANP, ANVP, Criss Potzer, RN, Christy Casper, MS, ANP, Rick Smith, MD During an ischemic stroke, one minute of brain ischemia kills 2 million nerves cells. Guidelines from the American Stroke Association indicate the less time between the onset of an ischemic stroke and a patient receiving intravenous thrombolytics is associated with improved outcomes. From 2003-2009, only 19-22% of patients had a door to tPA time of less than 60 minutes. A multidisciplinary team was created to improve door to tPA times for acute ischemic stroke patients. A total of 4 PDSA cycles were implemented. Each cycle brought new changes or removed processes that were not working well. Since the interventions were implemented for the Target Stroke project, the number of patients treated within 60 minutes has improved from 33% to 69%, with a median time of 58 minutes. “The Rationale for Utilizing the “Flipped Classroom” Model for New Hire Orientation” Penne McPherson, RN, BSN, MS Orientation as a part of new hire onboarding is often viewed as a painful necessity to meet the requirements of corporate, facility and regulatory mandates. Information is frequently given in lecture format with little student interaction and many times will repeat common knowledge. Development of creative approaches in which to enhance this information and bring personal value to the student occurred in response to post orientation evaluations. This presentation will focus on the integration of a teaching methodology common in the academic setting and its application to the acute care orientation setting. A description of the “Flipped Classroom” model and the process used to incorporate it into acute care while still maintaining regulatory agency mandates will be explained. Evaluations and financial savings have been tracked. As of June, 2014, all evaluation comments have been very positive. Cost savings to date has been over $5000. Learning Session 5 “The Many Faces of Peer Review: Ten Strategies for Success” Tiffany Meister, RN, BSN, CCRN Peer review promotes transparency, accountability, and professionalism within an organization. Nursing peer review influenced and role modeled the structure and process for integration of peer review to other disciplines. Ten distinct strategies of an innovative peer review model includes safety reviews; team assessment for hiring; shift handoff; 360° & Calibration Reviews of Leaders; annual evaluation; APN credentialing and peer review process through the Medical Staff office; routine performance practice assessments; review feedback of presentations; research proposal peer review; and staffing matrix compliance peer review. These distinct strategies of nursing peer review transformed a hospital culture to achieve improved patient safety outcomes, advanced staff quality and safety competencies and greater overall performance. “Planned Paradigm Shifts – Empowering Nursing for Change” Susan Barnett, RN, MSN, ONC Peri-operative care for joint replacement is undergoing rapid change across the industry. The move toward same day discharge greatly impacts care practices related to goals and timing. Guided by the PARiHS framework for change, a multidisciplinary team enabled Parker staff to incorporate same day discharge into care options for patients undergoing total hip and knee replacement procedures. Pre-operative discharge planning at an educational class, careful communication of care goals, and close teamwork between the physician and hospital departments have provided the context to successful facilitate this change in practice. Each of the outcomes assessed have added to the body of evidence that same day discharge for select total joint replacement patients is 4 a safe option of care. Through planned change by a dedicated resource person, the transition has been smooth and successful. “Developing a Nursing Senate” Karen Wilson, RN, MN, CGRN, Andi Rottman, BSN, RN-C, Renee Blattman, BSN, MBA Parker Adventist Hospital transitioned its shared governance structure from a Nurse Practice Council to an elected Nursing Senate. Some of the purposes of the Nursing Senate include: delineate the scope of nursing practice at Parker Adventist Hospital; facilitate the integration of nursing research findings into clinical practice and performance improvement through policies, procedures, protocols and/or professional development; consult on interdisciplinary issues that impact patient care; represent the nursing perspective in ethical/legal issues; serve as an implementation team for system-wide changes for advancing patient care; support the education and health of the communities served; promote strategies that enhance recruitment, retention and satisfaction of nursing staff; and facilitate the journey toward Magnet designation. This structure change began in 2012, and was fully adopted in June, 2013. While the Nursing Senate structure has been in place for only eight months Parker Adventist Hospital has seen a dramatic effect in patient care; including significant cost savings, increased HCAHPS scores and a decrease in specimen mislabeling. Learning Session 6 “Pain Relief Starts in the Prehospital Setting: Is It Effective?” Mary Meyers, MS, EMT-P, Judy Jo Mackie, RN, MS, CEN, Brian Sobeck, MBA, EMT-P Pre-hospital providers can have an impact providing pain relief for patients complaining of acute pain. Control of a patient’s pain with narcotic medication is a vital part of delivering comprehensive and expeditious patient care within the paramedic scope of practice in the pre-hospital setting. This research study sought to determine the measureable effects of prehospital pain relief. Patient complaint and condition data was abstracted for patients transported by Littleton Fire Rescue Paramedics between October 2013, and February 2014 to Littleton and Porter Adventist Hospital emergency departments. These patients had acute pain from injuries due to falls and other mechanisms, as well as acute pain from medical conditions. Our primary outcome variable was comparison of differences between reported pain levels using the Wong-Baker pain scale in EMS patients prior to arrival at the emergency department and after arrival. Findings demonstrate that prehospital providers affect the pain levels of patients arriving in the emergency department and are suggestive that this may have a positive impact on patient experience. Further research is necessary to quantify and determine the extent of this relationship. “A Community Based Model for Concussion Management” Kelley Lau, RN, BSN, MBA The purpose of this study was to establish an evidenced-based pathway for patients with very low risk of a clinically important traumatic brain injury (ciTBI) for medical and nursing staff at this facility. The hospital’s TBI committee designed a collaborative community-based concussion management program, implemented throughout 2010. The program involved our trauma centers, local schools, injury prevention groups, local physicians, and rehabilitation centers. As part of the quality initiative, the TBI committee developed and implemented many best practices for the care of the TBI patient, such as standardized after care instructions with symptom log, letters of education emphasizing brain rest and TBI resource lists. 5,567 trauma registry records were reviewed retrospectively. 1,625 (30% of the registry) was diagnosed with a concussion or a TBI. Through a large network of informed individuals and a community based concussion management program we decreased the use of head CT by 12%. There were no readmissions, missed injuries or complications observed due to reduced use of head CT. Implementing quality initiatives can be effective in helping establish best practices in management of mild traumatic brain injury in the ED. 5 “Igniting Passion through an Educational Framework for Reaching Coloradans: The Stroke Experience” Ellen Lane, RN, MSN, CCRN, Ashley Trujillo, RN Despite the fact that stroke is the fourth leading cause of death and the leading cause of disability, studies reveal that only 20% of stroke victims get to the hospital on time to receive acute treatment- which is proven to decrease disability by over 30%. In addition to the lack of public understanding of acute strokes, there was a wide variety of knowledge and skill level in both the prehospital and hospital areas across the nation and in Colorado. Therefore, a robust plan had to be devised to reach many different audiences. In March, 2011, five healthcare providers from the Centura Health Stroke Network learned the Advanced Stroke Life Support program and brought it to Colorado to spread knowledge across the state. In addition, several tools were utilized to educate the public on both primary and secondary prevention of stroke and the recognition of acute stroke symptoms. During this presentation, the MEGAbrain, Strike out Stroke and several other methodologies will also be reviewed and discussed. Ultimately, the purpose of this presentation will be to provide a practical framework to assist others in developing a comprehensive plan for other medical conditions/service lines for sharing best practices and health related education across Colorado. 6 Learning Session 7 “Energize with Exercise: Improving Funcionality in Oncology Patients with Outpatient Rehabilitation” Lynette Olson, PTA, CES, Andi McDonough, MPT Historically, patients undergoing active oncology treatment experience significant functional decline and severe fatigue that impairs their quality of life. Current research supports that early therapeutic intervention leads to better patient functional outcomes as well as significant reduction of fatigue. As part of a multidisciplinary cancer center team, the rehab department developed a screening tool to identify functional impairments in oncology patients who could benefit from outpatient rehab services. A focused rehabilitation program was aimed at quantifying the positive effect on fatigue and functionality for cancer patients receiving rehab services at any point during their cancer treatments. Preand post- physical therapy standardized functional and impairment tests were administered to all oncology patients who completed outpatient physical therapy. Overwhelmingly, patients demonstrated improved functionality with activities of daily living, and decreased levels of fatigue. In all of the test categories except pain scale, the average post-rehab scores placed patients back in the normal range for their age and gender, indicating increased safety with mobility and decreased fall risk. This translates to improved quality of emotional and physical life and increased control over daily activities, decisions, and responsibilities. “Improving Head and Neck Cancer Patient Outcomes with Multidisciplinary Team Management Helen Gercas, RN, OCN, Debra Flesher-Bratt, RDH, Teri Meno, RD Unplanned breaks and prolongation of radiation treatment time are associated with lower overall survival rates and higher recurrences in head and neck cancer. Ulcerative mucositis, significant weight loss, and unplanned hospitalizations are the major limitations to completing therapy as planned. In order to assist patients in completing their therapy as planned, head and neck patients have been collaboratively managed by a nurse navigator, registered dietician, and dental hygienist since 2010. The aim of this multidisciplinary team is minimize treatment and disease side effects, ensure treatment completion, decrease recovery time, and improve quality of life. At the completion of treatment, only 11% of patients progressed to a grade 3 or higher functional mucositis, with no grade 4 occurrences. Average weight loss from initiation to completion of treatment was 5% of starting body weight. Less than 7% of patients experienced an unplanned hospitalization during treatment. These outcomes support the multidisciplinary team approach to managing head and neck cancer patients before, during, and after treatment with comprehensive patient education, assessment, and intervention. “Implementation of Evidence-Based Guidelines for Assessment of Adult Cancer Pain” Mary Murray, RN, BSN, CHPN Pain is prevalent in the cancer population and has been found to be under-treated with lack of adequate assessment contributing to the problem. In the acute care setting measures of pain intensity alone are primarily used to assess pain and adequacy of treatment. Guided by the Colorado Patient-Centered Evidence-Based Practice Model and the Iowa Model, a project has begun on an inpatient oncology unit to implement the National Comprehensive Cancer Network Guidelines for assessment of adult cancer pain by incorporating measures of pain interference and patient satisfaction with pain management. It is anticipated that nurse engagement in pain management for oncology patients will increase (as measured by survey) and that patient satisfaction with pain management will increase (as measured by HCAHPS survey). A thorough assessment is the first step toward improved pain management and patient satisfaction. 7 Learning Session 8 “Use of Therapeutic Hypothermia in Patients with Out-of-Hospital Cardiac Arrest and Resuscitation” Amber Gates, RN, BSN This literature review examines the supporting research behind the 2013 ACCF/AHA Guideline for the Evaluation and Management of Patients with STEMI and Out-of Hospital Cardiac Arrest. The review was performed utilizing research collected between 2001 and 2013. The current guideline is based on data up to 2010, and was issued in January 2013. The 2013 Guideline recommends a target core temperature of between 32° and 34°C. In the course of research, new data was released. The most significant finding was new research shared in the New England Journal of Medicine in March 2013 regarding a change in goal temperature for therapeutic hypothermia in patients with Out-of Hospital Cardiac Arrest. In the first research of its kind, a large global study of nearly 1,000 patients determined no significant deviation in neurologic outcome or mortality rate in patients that were cooled to 36°C compared to 33°C. This research has the potential to change the care and management of patients with Out-of-Hospital Cardiac Arrest by reducing possible complications of cooling while offering the best long-term outcome. “Early Progressive Mobility of the Artificially Ventilated Patient” Cortney Parsudi, RN, BSN, CCRN In 2013 the Society of Critical Care Medicine released updated guidelines regarding the treatment of pain, agitation, and delirium and recommended early mobilization of adult ICU patients. In April 2014, a new protocol for early mobilization of ventilated patients was instituted to address the last piece of the updated guidelines. Independent pre and post studies were performed on adult patients in a twelve bed medical intensive care unit. An early mobility protocol was developed through an interdisciplinary approach and approved by all stakeholders. During the first month of implementation, five out of 16 artifically-ventilated patients were mobilized out of bed. By comparison, no patients who were artificially ventilated were mobilized out of bed during 2012. The implementation of the mobility protocol as well as outcomes attributed to it will be discussed. “Addressing the Issue of Alarm Fatigue in the Cardiac ICU” Abbi-Lynn Washington, RN, MS, APRN, CCRN Clinical alarms play an important role in patient safety practices. Unfortunately, continuous monitoring is inefficient in identifying these changes in patient condition because of the sheer number of false and nuisance alarms. Sensory overload from constant alarms desensitizes clinicians and can lead to delayed responses with serious consequences. This evidence-based project is carried out to identify if nurses monitoring patients in the CICU will experience a reduction in the number of nuisance/inactionable alarms by implementing monitoring best practices as compared to the current practices. By decreasing nuisance alarms, we conclude that sensory overload and desensitization will be decreased and prompt responses to actionable alarms, and thus patient safety, will be improved. 8 7th Annual Centura Health EVIDENCE-BASED PRACTICE, RESEARCH and INNOVATION CONFERENCE “Using Evidence to be Our Best” Friday, November 14, 2014 DU School of Hotel, Restaurant, and Tourism Building #204 Poster Presentations Room 229 1. Keeping it down LOW with LOW Air Loss Kim Collins, MSN, RN, Littleton Adventist Hospital Nora Allen, MS, RN, CCNS, CCRN, Littleton Adventist Hospital Janie Lastrapes, BSN, RN, CWON Littleton Adventist Hospital 2. I'm Coming Out! Nurse Driven Indwelling Urinary Catheter Removal Protocol Nora Allen, MS, RN, CCNS, CCRN, Littleton Adventist Hospital Kim Collins, MSN, RN, Littleton Adventist Hospital Megan Irons, BSN, RN, Littleton Adventist Hospital Connie Zachrich, MS, RN, Littleton Adventist Hospital 3. Changing the Perioperative Work Environment with Staff Nurse Involvement: Four Units Working as One Kristen Oster, MS, RN, APRN, ACNS-BC, CNOR, Porter Adventist Hospital Sandy Chamness, ADN, RN, Porter Adventist Hospital Karen Montgomery, ADN, RN, CAPA, Porter Adventist Hospital 4. Barriers to Asking Behavior Questions on Admission Rochelle Salmore, MSN, RN, NE-BC, Penrose-St. Francis Health Services 5. Standardized Dysglycemic Protocol for Hyperglycemic Emergencies in the Emergency Department Pamela A. Assid, BSN, MSN, RN, CNS, CEN, CPEN, NEA-BC, St. Francis Medical Center 6. Improving Pre-Operative Screening Turn - Around Times Beth Moxley, RN, BSN, BA, St. Anthony Hospital 7. Half Pipes, Terrain Parks and Hospital Air: Treatment options for Splenic Trauma in a Rural Environment Shelly Almroth, BSN, RN, CEN, St Anthony Summit 8. Dramatic decrease in traveler and agency usage via “train our own” nurses program Megan Yantiss, CCRN-CSC, Parker Adventist Hospital 9. Centura Libraries: A Hidden Research Treasure Loren Hackett, MLIS, Porter Adventist Health Services Kristina Slanc, MLIS, Penrose-St. Francis Health Services 9 Room 231 10. Sustainable Reduction in Blood Culture Contamination in the ED Diane Villavicencio, BSN, RN, St. Francis Medical Center Kim Dumont BSN, RN, CEN, St. Francis Medical Center 11. Pain Control Using a Multimodal Approach: Are We Controlling Pain in Our Post Operative Orthopedic Patients? Priscilla Bernard, MSN, BSN, RN-BC, St. Francis Medical Center 12. High Frequency Low Tidal Volume Ventilation: Improving Catheter Stability during Atrial Fibrillation Ablation Chad Stockinger, RT, Vascular Center of Colorado Jessica Cooke, RN, PSFHS, Vascular Center of Colorado 13. Comparison of Outcomes Related to Depression Scores in Phase II Cardiac Rehabilitation Tanis Quaid-Hurtt, RN-BC, EMB, Porter Adventist Hospital 14. Using Descriptive Statistics from a Registry to Evaluate the Effectiveness of a Cardiac Rehabilitation Program Helen Graham, PhD, CNS, RN-C, Penrose St. Francis Health Services Rochelle Salmore, MSN, RN, NE-BC, Penrose St. Francis Health Services 10
© Copyright 2026