R Periodontics perspective in identifi cation and age estimation eview Article
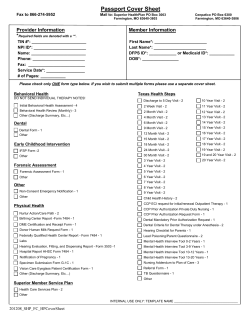
European Journal of Forensic Sciences Review Article www.ejfs.co.uk DOI: 10.5455/ejfs.163440 Periodontics perspective in identification and age estimation Thorakkal Shamim Department of Dentistry, Government Taluk Head Quarters Hospital, Malappuram, Kerala, India Address for correspondence: Thorakkal Shamim, Department of Dentistry, Government Taluk Head Quarters Hospital, Malappuram, Kerala, India. E-mail: shamu3duad@gmail. com Received: July 02, 2014 Accepted: July 16, 2014 Published: August 06, 2014 ABSTRACT Forensic odontology is a specialized field of dentistry that analyses dental evidence in the interest of justice. Periodontics is a clinical dental speciality dealing with diseases of the periodontium. This speciality is utilized for identification of individuals through morphology and pathology of periodontium and is also utilized for age estimation studies which include periodontosis, root transparency and root length. This paper aims to discuss the periodontics perspective in identification and age estimation. KEY WORDS: Forensic sciences, forensic odontology, age estimation, identification, periodontics, perspective, periodontium INTRODUCTION Forensic odontology is a specialized field of dentistry which analyses dental evidence in the interest of justice. Dental evidence has been used for the identification of victims and suspects in mass disasters, abuse and crimes [1]. Dental evidence is presented in the following sequence in the court of law i.e., proper handling, thorough examination, evaluation and presentation [1]. A working classification for forensic odontology was formulated based on the relationship of various dental specialities with forensic odontology [2]. A detailed review about the utility of these dental specialities with forensic odontology was ascertained to understand the forensic implications of each individual dental speciality and to do research in the parent dental speciality [3]. The new working classification proposed for forensic odontology based on its relationship with other dental specialties was evaluated in scientometric research [4]. The role of forensic odontology in the identification of the homicide cases has been extensively reported [5]. The resilience of the dental structures to postmortem assault and teeth as a source of DNA will contribute to making identification successful [6]. The late President of Pakistan, General Zia-ul-Haq who died in a plane crash and the late Indian Prime Minister, Mr. Rajiv Gandhi who was assassinated in a terrorist attack in 1991 were identified from their dentition [7]. 18 The introduction of universal coding will be of immense help in forensic dental identification. A simplified Indian coding was proposed for forensic dental identification based on the interrelationship of dental specialties with forensic odontology [8]. A simple and cost-effective technique, easily performed in dental clinic practice using discarded Lead foil of the intraoral periapical radiograph as an inclusion agent in the dentures of the individuals for the identification process was proposed recently [9]. Periodontics is a clinical dental speciality dealing with diseases of periodontium [3]. This speciality is utilized for identification of individuals through morphology and pathology of periodontium and is also utilized for age estimation studies which include (periodontal ligament attachment level) periodontosis, root transparency and root length [2]. This paper aims to discuss the periodontics perspective in identification and age estimation in terms of the following aspects. METHODS A review of the literature was done using PubMed to evaluate the periodontics perspective in identification and age estimation. The following keywords were searched in PubMed: Identification, gingival morphology and pathology, the contour of the gingiva, gingival recession, gingival enlargement, interproximal craters, the color of the gingiva, plaque and calculus deposits, periodontal ligament morphology and pathology, thickness of periodontal ligament, widening of periodontal ligament, lateral periodontal cysts, periodontal abscess, status of alveolar Eur J Forensic Sci ● Oct-Dec 2014 ● Vol 1 ● Issue 1 Shamim: Periodontics perspective in identification and age bone, height, contour and density of crestal bone, thickness of interradicular bone, pattern of lamina dura, trabecular bone pattern, bone islands, bone loss, periodontal cosmetic surgeries, crown lengthening procedure, root hemisection, regenerative surgery, periodontal microsurgery, age estimation, periodontosis. Root transparency and root length. DISCUSSION Identification Focal and Diffuse Enlargements of the Gingiva Gingival enlargements are quite common and can be classified as focal and diffuse enlargements. The etiology of the gingival enlargement may be inflammatory (abscess), idiopathic (hereditary gingival fibromatosis), drug induced (calcium channel blocker, phenytoin, cyclosporine), granulomatous disease (tuberculosis), neoplasms (leukemia) and any other systemic and local pathology [17-21]. Interproximal Craters Periodontics is the speciality of dentistry dealing with diseases of the gums and other structures around the teeth [3]. This speciality is utilized for identification of individuals through gingival morphology and pathology, periodontal ligament morphology and pathology, status of alveolar bone and periodontal cosmetic surgeries [Table 1]. Interproximal craters are usually presented in necrotising ulcerative gingivitis with interdental necrosis, punched out ulcerated papillae, gingival bleeding and pain [22]. Similar ulcerative changes of gingiva is also reported in Fanconi’s anaemia and HIV infection [23,24]. Gingival Morphology and Pathology The Color of the Gingiva The clinical parameters of the gingiva such as contour, recession, enlargements, interproximal craters, color (inflammatory changes, physiological [racial] or pathological pigmentations), dental plaque and calculus deposits were taken into consideration for establishing identity of the individuals [Table 1]. The usual color of the gingiva is coral pink and gingiva will exhibit physiologic pigmentation. The most common site of physiologic pigmentation is the labial part of the gingiva, and the attached gingiva is the most common pigmented anatomic division [25]. The highest rate of gingival pigmentation has been observed at the incisors [26]. The pathologic pigmentations in gingiva may be smoker’s melanosis, melanotic macule, oral melanoacanthoma, pigmentation by foreign bodies or induced by drugs, Peutz–Jeghers syndrome, Addison’s disease and oral melanoma [27]. The Contour of the Gingiva The contour or shape of the gingiva varies considerably among individuals and depends on the shape of the teeth and their alignment in the arch, the location and size of the area of proximal contact and the dimensions of the facial and lingual gingival embrasures [10]. The harmony of gingival contour is jeopardized by improperly constructed dental restorations and prosthetic abutments [11]. The anatomical form, marginal adaptation, marginal discoloration and surface roughness of the dental restorations and prosthetic abutments in relation with the contour of the gingiva should be assessed. Stillman’s cleft (apostrophe shaped identations extending from the gingival margin apically) and McCall’s festoons (life saver shaped enlargements of marginal gingiva in canine premolar region) associated with occlusal trauma will enhance the identification process [12,13]. Gingival Recession Gingival recession is an undesirable condition presenting as localized and generalized form resulting in root exposure [14]. The etiology of gingival recession was traced to bad oral hygiene practices, high level of dental plaque and calculus and tobacco consumption habit with more cases reported in older population [14]. Gingival recession was reported in young Israeli adults with history of past orthodontic treatment and oral piercing [15]. The presence and extent of gingival recession will increase with age and it is frequently seen on buccal surfaces than on other aspects of the teeth [14]. Gingival recession is also associated with clinical crown length, arch relationship and frenum involvement [16]. Eur J Forensic Sci ● Oct-Dec 2014 ● Vol 1 ● Issue 1 Plaque and Calculus Deposits The oral hygienes status can be assessed by recording plaque and calculus deposits and there is a definite correlation between bad oral hygiene status with higher plaque and calculus deposits [28]. Plaque and calculus deposits will be higher in certain pathologic conditions [29,30]. Periodontal Ligament Morphology and Pathology The clinical parameters of the periodontal ligament such as thickness of periodontal ligament, widening of periodontal ligament and pathologies of the periodontal ligament such as lateral periodontal cysts and periodontal abscess were taken into consideration for establishing identity of the individuals [Table 1]. Thickness of Periodontal Ligament The thickness of the periodontal ligament will be directly related to age and mesiocclusal drifting of teeth [31]. A more recent study on rats about the importance of periodontal ligament thickness, it was interfered that periodontal ligament thickness is directly proportional to root dimensions [32]. Widening of Periodontal Ligament The widening of the periodontal ligament space is seen related to 19 Shamim: Periodontics perspective in identification and age Table 1: Interrelationship of periodontics with forensic odontology Thickness of Interradicular Bone Identification Gingival morphology and pathology: a. Contour, recession, focal/diffuse enlargements, interproximal craters b. Colour-inflammatory changes, physiological (racial) or pathological pigmentations c. Plaque and calculus deposits Periodontal ligament morphology and pathology: a. Thickness b. Widening c. Lateral periodontal cysts and periodontal abscess Status of alveolar bone: a. Height, contour, density of crestal bone b. Thickness of interradicular bone c. Pattern of lamina dura d. Bone loss (horizontal/vertical) e. Trabecular bone pattern and bone islands Periodontal cosmetic surgeries: a. Crown lengthening procedure b. Root hemisection along with regenerative surgery c. Periodontal microsurgery Age estimation Periodontosis (gum recession) Root transparency and root length The buccal interradicular cortical bone thickness between canine and first premolar or between first premolar and second premolar is the greatest and between central incisor and lateral incisor is the least and buccal and palatal interradicular cortical bone thickness and alveolar process width will tend to increase from crest to base of alveolar process [43]. bisphosphonate-associated osteonecrosis of the jaws, progressive systemic sclerosis and primary hyperparathyroidism [33-35]. Lateral Periodontal Cysts and Periodontal Abscess The lateral periodontal cyst is a rare developmental odontogenic cyst seen in mandibular premolar region of adults [36]. Lateral periodontal cysts are non-keratinized cysts located adjacent or lateral to the root of a vital tooth [37]. Periodontal abscess is localized, purulent infection within the tissues adjacent to the periodontal pocket that may lead to the destruction of periodontal ligament and alveolar bone [38]. More recently, an unusual case of recurrent periodontal abscess in a 31-year-old male electrician due to his habit of using his teeth as a tool for stripping electrical wires was reported [39]. Status of Alveolar Bone The clinical parameters of the alveolar bone such as height, contour and density of crestal bone, thickness of interradicular bone, pattern of lamina dura, bone loss (horizontal or vertical), trabecular bone pattern and bone islands were taken into consideration for establishing identity of the individuals [Table 1]. Height, Contour and Density of Crestal Bone Bone mineral density is an important risk indicator for periodontitis in postmenopausal women [40]. Tobacco consumption induces alveolar crest height loss independently of mandibular bone mass and bone density [41]. Osteoporosis or low systemic bone mineral density is considered as a risk factor for periodontal disease progression [42]. 20 Pattern of Lamina Dura, Trabecular Bone Pattern and Bone Islands Partial or complete loss of lamina dura, delicate or absent trabecular patterns, and an overall granular or chalky white appearance associated with an increase in radiographic density are seen in patients with renal osteodystrophy [44]. Trabecular pattern can be assessed in mandible using periapical and panoramic radiographs [45,46]. Bone Loss (Horizontal or Vertical) Horizontal alveolar bone loss is seen more often than the vertical bone defects in periodontal patients [47]. Periodontal Cosmetic Surgeries The periodontal cosmetic surgeries such as crown lengthening procedure, root hemisection along with regenerative surgery and periodontal microsurgery were taken into consideration for establishing identity of the individuals [Table 1]. Crown Lengthening Procedure Open-flap and minimally-invasive flapless esthetic crown lengthening procedures are usually recommended for the treatment of excessive gingival display [48]. The effect of esthetic crown lengthening procedures play a major role in the perception of whether a person is attractive and whether or not they are perceived as friendly, trustworthy, intelligent, and self-confident [49]. Root Hemisection along with Regenerative Surgery Hemisection is a viable method of preserving periodontally or endodontically compromised teeth or roots (mainly mandibular first molars) [50]. Among regenerative surgical procedures in periodontics, guided tissue regeneration is still the favourable technique with significant clinical and histologic documentation of periodontal regeneration [51]. Periodontal Microsurgery Periodontal microsurgery is now grouped under minimally invasive periodontal therapy that preserves dentition and supporting structures and allows less extensive manipulation of surrounding tissues than conventional procedures and accomplishing the same treatment results [52]. Eur J Forensic Sci ● Oct-Dec 2014 ● Vol 1 ● Issue 1 Shamim: Periodontics perspective in identification and age Age Estimation One of the interesting applications of forensic odontology is age estimation by means of teeth [53]. Periodontics is also utilized for age estimation studies which include periodontosis (gum recession), root transparency and root length [Table 1] [2]. Periodontosis 16. 17. 18. 19. Periodontosis is one of the six dental changes that is used along with attrition, secondary dentin deposition, root translucency, cementum apposition and root resorption to estimate age by Gustafson’s method [1]. Root Transparency and Root Length The dental features such as root translucency and root length can be used along with the extent of periodontosis to estimate age in adults [54]. Lamendin et al. developed a general technique to estimate age of adults at death using two dental features (periodontosis and translucency of the tooth root) and Prince and Ubelaker modified this method, creating a formula for each sex and for different ancestries and obtained more precise age estimations [55]. 20. 21. 22. 23. 24. 25. 26. 27. CONCLUSION 28. To conclude, this article hopes to sensitize all dental fraternities and periodontics specialists around the globe to know the interrelationship of periodontics with forensic odontology. 29. 30. REFERENCES 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. Shamim T. Forensic odontology. J Coll Physicians Surg Pak 2010;20:1-2. Shamim T. A new working classification proposed for forensic odontology. J Coll Physicians Surg Pak 2011;21:59. Shamim T. Forensic odontology. J Coll Physicians Surg Pak 2012;22:240-5. Shamim T. Publication trends in the journal of forensic dental sciences 2009-2012. J Sci Res 2013;2:152-6. Shamim T, Ipe Varghese V, Shameena PM, Mahesh MR. Forensic odontology to the rescue: A case report. Med Legzal Update 2006;6:115-8. Shamim T. Deoxyribonucleic acid profiling in forensic dental identification. Indian J Hum Genet 2013;19:513. Shamim T, Sudha S, Shameena PM, Ipe Varghese V. An insight to forensic odontology. Kerala Dent J 2006;29:45-7. Shamim T. A simplified Indian coding proposed for forensic dental identification. J Coll Physicians Surg Pak 2014;24:609-10. Shamim T. Lead foil in the intraoral periapical radiograph as an inclusion agent: A simple method in denture identification. J Coll Physicians Surg Pak 2012;22:130-1. Fiorellini JP, Kim DM, Uzel NG. Anatomy of the periodontium. In: Newman MG, Takei H, Klokkevold PR, Carranza FA, editors. Carranza’s Clinical Periodontology. China: Saunders, Elsevier; 2012. p. 12-27. Simon Z, Rosenblatt A. Challenges in achieving gingival harmony. J Calif Dent Assoc 2010;38:583-90. Thom G. Stillman’s cleft caused by traumatic occlusion. The interesting case. Stomatol DDR 1979;29:374-7. Bhola M, Cabanilla L, Kolhatkar S. Dental occlusion and periodontal disease: What is the real relationship? J Calif Dent Assoc 2008;36:924-30. Kassab MM, Cohen RE. The etiology and prevalence of gingival recession. J Am Dent Assoc 2003;134:220-5. Slutzkey S, Levin L. Gingival recession in young adults: Occurrence, Eur J Forensic Sci ● Oct-Dec 2014 ● Vol 1 ● Issue 1 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. severity, and relationship to past orthodontic treatment and oral piercing. Am J Orthod Dentofacial Orthop 2008;134:652-6. Mathur A, Jain M, Jain K, Samar M, Goutham B, Swamy PD, et al. Gingival recession in school kids aged 10-15 years in Udaipur, India. J Indian Soc Periodontol 2009;13:16-20. Aghili H, Goldani Moghadam M. Hereditary gingival fibromatosis: A review and a report of a rare case. Case Rep Dent 2013;2013:930972. Livada R, Shiloah J. Calcium channel blocker-induced gingival enlargement. J Hum Hypertens 2014;28:10-4. Subramani T, Rathnavelu V, Alitheen NB. The possible potential therapeutic targets for drug induced gingival overgrowth. Mediators Inflamm 2013;2013:639468. Gill JS, Sandhu S, Gill S. Primary tuberculosis masquerading as gingival enlargement. Br Dent J 2010;208:343-5. Arul AS, Verma S, Ahmed S, Arul AS. A clinical and fine needle aspiration cytology study of gingiva in acute leukemia. Dent Res J (Isfahan) 2012;9:80-5. Atout RN, Todescan S. Managing patients with necrotizing ulcerative gingivitis. J Can Dent Assoc 2013;79:d46. Srirangarajan S, Shetty S, Prasanna D. Necrotic ulcerative changes in Fanconi’s anaemia: A case report. Oral Health Prev Dent 2011;9:91-7. Mataftsi M, Skoura L, Sakellari D. HIV infection and periodontal diseases: An overview of the post-HAART era. Oral Dis 2011;17:13-25. Gorsky M, Buchner A, Fundoianu-Dayan D, Aviv I. Physiologic pigmentation of the gingiva in Israeli Jews of different ethnic origin. Oral Surg Oral Med Oral Pathol 1984;58:506-9. Tamizi M, Taheri M. Treatment of severe physiologic gingival pigmentation with free gingival autograft. Quintessence Int 1996;27:555-8. Gondak RO, da Silva-Jorge R, Jorge J, Lopes MA, Vargas PA. Oral pigmented lesions: Clinicopathologic features and review of the literature. Med Oral Patol Oral Cir Bucal 2012;17:e919-24. Chandrashekar BR, Suma S, Kiran K, Manjunath BC. The use of school teachers to promote oral hygiene in some secondary school students at Hyderabad, Andhra Pradesh, India: A short term prospective pilot study. J Family Community Med 2012;19:184-9. Bayraktar G, Kurtulus I, Duraduryan A, Cintan S, Kazancioglu R, Yildiz A, et al. Dental and periodontal findings in hemodialysis patients. Oral Dis 2007;13:393-7. Machuca G, Segura-Egea JJ, Jiménez-Beato G, Lacalle JR, Bullón P. Clinical indicators of periodontal disease in patients with coronary heart disease: A 10 years longitudinal study. Med Oral Patol Oral Cir Bucal 2012;17:e569-74. Louridis O, Demetriou N, Bazopoulou-Kyrkanidou E. Periodontal ligament thickness as related to age and mesiocclusal drifting of teeth: A histometric study. J Periodontol 1974;45:862-5. Cuoghi OA, Tondelli PM, Aiello CA, Mendonça MR, Costa SC. Importance of periodontal ligament thickness. Braz Oral Res 2013;27:76-9. Phal PM, Myall RW, Assael LA, Weissman JL. Imaging findings of bisphosphonate-associated osteonecrosis of the jaws. AJNR Am J Neuroradiol 2007;28:1139-45. Mehra A, Kumar S. Periodontal manifestations in systemic sclerosis: A review. Dent Today 2008;27:50, 52, 54. Padbury AD Jr, Tözüm TF, Taba M Jr, Ealba EL, West BT, Burney RE, et al. The impact of primary hyperparathyroidism on the oral cavity. J Clin Endocrinol Metab 2006;91:3439-45. Ku m u d a A r v i n d Ra o H T, S h e t t y S R , B a b u S. U n u s u a l clinicoradiographic presentation of a lateral periodontal cyst. J Dent (Tehran) 2012;9:265-9. Formoso Senande MF, Figueiredo R, Berini Aytés L, Gay Escoda C. Lateral periodontal cysts: A retrospective study of 11 cases. Med Oral Patol Oral Cir Bucal 2008;13:E313-7. Marquez IC. How do I manage a patient with periodontal abscess? J Can Dent Assoc 2013;79:d8. Bhat GS, Singh V, Bhat KM. Recurrent periodontal abscess associated with “teeth as a tool”. J Indian Soc Periodontol 2012;16:113-4. Singh A, Sharma RK, Siwach RC, Tewari S, Narula SC. Association of bone mineral density with periodontal status in postmenopausal women. J Investig Clin Dent 2013. Mesa F, Souki N, Galindo-Moreno P, Velasco-Torres M, O’Valle F, Bravo M. Tobacco consumption induces alveolar crest height loss independently of mandibular bone mass and bone density. Clin Oral Implants Res 2014;25:1034-40. 21 Shamim: Periodontics perspective in identification and age 42. 43. 44. 45. 46. 47. 48. 49. 22 Esfahanian V, Shamami MS, Shamami MS. Relationship between osteoporosis and periodontal disease: Review of the literature. J Dent (Tehran) 2012;9:256-64. Sawada K, Nakahara K, Matsunaga S, Abe S, Ide Y. Evaluation of cortical bone thickness and root proximity at maxillary interradicular sites for mini-implant placement. Clin Oral Implants Res 2013;24 Suppl A100:1-7. Antonelli JR, Hottel TL. Oral manifestations of renal osteodystrophy: Case report and review of the literature. Spec Care Dentist 2003;23:28-34. Pham D, Jonasson G, Kiliaridis S. Assessment of trabecular pattern on periapical and panoramic radiographs: A pilot study. Acta Odontol Scand 2010;68:91-7. Aranha Watanabe PC, Moreira Lopes De Faria L, Mardegan Issa JP, Caldeira Monteiro SA, Tiossi R. Morphodigital evaluation of the trabecular bone pattern in the mandible using digitized panoramic and periapical radiographs. Minerva Stomatol 2009;58:73-80. Jayakumar A, Rohini S, Naveen A, Haritha A, Reddy K. Horizontal alveolar bone loss: A periodontal orphan. J Indian Soc Periodontol 2010;14:181-5. Ribeiro FV, Hirata DY, Reis AF, Santos VR, Miranda TS, Faveri M, et al. Open-flap versus flapless esthetic crown lengthening: 12-month clinical outcomes of a randomized controlled clinical trial. J Periodontol 2014;85:536-44. Malkinson S, Waldrop TC, Gunsolley JC, Lanning SK, Sabatini R. The effect of esthetic crown lengthening on perceptions of a patient’s attractiveness, friendliness, trustworthiness, intelligence, and selfconfidence. J Periodontol 2013;84:1126-33. 50. Ronay V, Sahrmann P, Ender A, Bindl A, Schmidlin PR. Cerec reconstruction of a hemisected mandibular molar: Method and case report. Int J Comput Dent 2012;15:55-66. 51. Wolff LF. Guided tissue regeneration in periodontal therapy. Northwest Dent 2000;79:23-8, 40. 52. Dannan A. Minimally invasive periodontal therapy. J Indian Soc Periodontol 2011;15:338-43. 53. Shamim T, Ipe Varghese V, Shameena PM, Sudha S. Age estimation: A dental approach. J Punjab Acad Forensic Med Toxicol 2006;6:14-6. 54. Ubelaker DH, Parra RC. Application of three dental methods of adult age estimation from intact single rooted teeth to a Peruvian sample. J Forensic Sci 2008;53:608-11. 55. González-Colmenares G, Botella-López MC, Moreno-Rueda G, Fernández-Cardenete JR. Age estimation by a dental method: A comparison of Lamendin’s and Prince & Ubelaker’s technique. J Forensic Sci 2007;52:1156-60. © GESDAV; licensee GESDAV. This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited. Source of Support: Nil, Conflict of Interest: None declared. Eur J Forensic Sci ● Oct-Dec 2014 ● Vol 1 ● Issue 1
© Copyright 2026