Bleeding and /or pain in early pregnancy Gynaecology service Information for patients
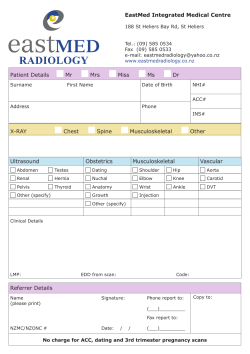
Gynaecology service Bleeding and /or pain in early pregnancy Information for patients May 2014 Great Staff – Great Care – Great Future INTRODUCTION This leaflet has been produced to give you general information about your condition. Most of your questions should be answered by this leaflet. It is not intended to replace the discussion between you and your nurse/doctor, but may act as a starting point for discussion. If after reading it you have any concerns or require further explanation, please discuss this with a member of the healthcare team who has been caring for you. WHAT IS VAGINAL BLEEDING IN EALRY PREGNANCY? Vaginal bleeding is common in early pregnancy and does not always mean there is a problem. However, bleeding can be a warning sign of a miscarriage. What are the causes of early bleeding? There are a number of causes of bleeding in early pregnancy which include: Spotting or bleeding may occur shortly after conception, this is known as an implantation bleed. It is caused by the fertilised egg embedding itself in the lining of the womb. This bleeding is often mistaken for a period, and it may occur around the time your period is due. Hormonal bleeding is when some women experience a light bleed at around four to eight weeks of pregnancy, or around the time their period would have been due. This can be very confusing for women who are pregnant and is the reason many women do not realise they are pregnant for a while. Again, it is totally normal. This usually settles around the 13th week of pregnancy as by this time the placenta is sufficiently developed to produce all of the hormones needed to sustain the pregnancy. After the egg is fertilised, the fertilised egg then goes on to implant itself into the lining of the womb (uterus). Sometimes this results in a little bleeding that shows up on an early scan as a haematoma(collection of blood). This isn't anything to Leaflet reg: ……..Title: Early pregnancy pain and bleeding Author E Morris Review date May 2017 worry about. When it happens the woman may notice a small amount of vaginal bleeding, but this is not necessarily the case. The haematoma will gradually disappear and in most cases, the pregnancy remains safe. Cervical Erosion (alternatively known as cervical ectropion) may be a source of spotting or bleeding. The blood supply to the womb and cervix is increased during pregnancy and the cervix may bleed harmlessly and painlessly. An erosion may cause bleeding following sexual intercourse; therefore this type of bleeding must always be reported to your doctor. CAN BLEEDING INDICATE A MISCARRIAGE? Not all bleeding in pregnancy is harmless, and it can be the first sign of a miscarriage. As many as 1 in 5 pregnancies are thought to end in miscarriage. The cause of miscarriage is not always known, but researchers have shown that in some cases there is a problem with the developing pregnancy, which means it is unable to develop normally. For most women, miscarriage is a very sad and upsetting experience. Experiences of miscarriage vary. In some cases there may be only very slight spotting, in other cases bleeding may stop and start or heavier bleeding with clots and cramping period type pains can occur. Sometimes there may be no bleeding at all. For further information relating to miscarriage, please ask your nurse for further details. WHAT SHOULD I DO IF I EXPEIENCE BLEEDING DURING PREGNANCY? If you experience bleeding, it is wise to have this checked out. If you have been seen on Early Pregnancy Assessment Unit (EPAU) during your pregnancy, you may contact us directly, up to 15 weeks of pregnancy. Your GP or midwife can also help you. If you have been seen in the EPAU and you then experience more bleeding contact the EPAU. Depending on how much bleeding and for how long the nursing staff will decide if you need to be seen again. Leaflet reg: ……..Title: Early pregnancy pain and bleeding Author E Morris Review date May 2017 WHAT IF I EXPERIENCE PAIN IN EARLY PREGNANCY? If you experience pain that does not go away, or which you feel is becoming more sever, you should seek advice from your doctor, nurse or midwife. It is important that any serious causes of pain are excluded. For example there is a need to rule out an ectopic pregnancy (this is where the pregnancy develops outside the womb). What kind of pain may I feel? Some women experience abdominal (tummy) pain in early pregnancy. This may be low cramping pain, similar to that felt during a period, or a stitch like or stabbing pain on one or both sides of the tummy. Aches and pains may come and go or be present continuously. What are the causes of abdominal and back pain? Some of the aches and pains experienced during pregnancy are thought to be due to hormonal changes. Large amounts of the hormone progesterone are produced, which are needed to sustain pregnancy. In addition to this, progesterone acts on the muscles, ligaments and joints causing them to become slacker and more flexible. This hormonal effect is thought to be responsible for some of the stitch like pains that some women experience in the lower part of the tummy and in some cases this can be quite severe. The same hormones can be responsible for constipation during pregnancy; this can also cause abdominal pain. The enlarging womb is made up of layers of muscles and is held in place in the pelvis by supporting ligaments. As the womb expands to accommodate the developing baby, it can pull on the ligaments and muscles, to cause these “growing pains”. The backache that some women get in early pregnancy is also thought to be due to a hormonal effect, and the supporting muscles are softer. Abdominal and/or backache can also be a sign of a urine infection. This may also cause burning or stinging when passing urine and the need to pass urine more frequently. You must inform your doctor of these symptoms, so that a urine test can be obtained and treatment given if needed. Pain on its own does not mean that a miscarriage will occur. However if you experience bleeding as well as pain this could indicate a threatened miscarriage and you should always seek advice from your doctor, nurse or midwife. Leaflet reg: ……..Title: Early pregnancy pain and bleeding Author E Morris Review date May 2017 Can I take pain killers during pregnancy? If you find that you need to take painkillers to relieve any pain, it is safest to use something simple such as paracetamol. Drugs such as aspirin and ibuprofen should be avoided. If you find that you need a stronger painkiller, you must always check with your doctor, nurse or midwife first. SCANNING IN EARLY PREGNANCY An ultrasound scan is used during pregnancy for a number of reasons. In the first three months of pregnancy it can be used to check the presence of the baby’s heartbeat, which can be reassuring if you have experienced a problem, such as vaginal bleeding or pain. A scan will also be used to check to see if the pregnancy is in the correct place and to accurately predict the estimated date of delivery (the date the baby is due) by measuring the end points (size) of the embryo or fetus. Will I have an ultrasound scan? Yes, if the nurse/doctor thinks it is appropriate for you to have a scan. What is an ultrasound scan? Ultrasound uses high frequency sound waves that are sent out from a transducer or probe. These sound waves are received back and converted into an image on a screen. Below is an ultrasound image of a nine-week-old fetus: Leaflet reg: ……..Title: Early pregnancy pain and bleeding Author E Morris Review date May 2017 Is it safe to have a scan in early pregnancy? Yes it is safe, there is so far no evidence to suggest that an ultrasound scan is unsafe. What type of scan will I have? A vaginal scan is the best method in early pregnancy (under 8 weeks) as it gives us a more accurate result at an earlier stage in pregnancy than an abdominal scan. It may be a little uncomfortable but it is safe to be done, you do not need a full bladder when having a vaginal scan. If you have concerns about a vaginal scan, please let the nurse, midwife doctor know. What will the scan tell us? A scan can only tell us how your pregnancy is at that particular time. Unfortunately it is no guarantee that your pregnancy will continue successfully. If your symptoms persist or become worse, you must contact EPAU, midwife or your GP. In later pregnancy ultrasound scanning is used to look more closely at the anatomy and organs of the developing baby. This is usually done between 18 – 21 weeks. WHAT IF THE SCAN CONFIRMS A MISCARRIAGE? If the scan confirms that you have miscarried, the choices of how we can manage this will be discussed with you. Occasionally, the scan may pick up an unexpected finding such as a cyst on the ovary. If this is the case, the staff will explain the findings and any necessary follow up. Common abbreviations use on scans LMP -Last menstrual period FH - Fetal heart-rate EDD- Estimated date of delivery FM - Fetal movement USS -Ultrasound scan YS - Yolk sac CRL - Crown to rump length (a measurement of the embryo/fetus used in early pregnancy) BPD - Bi-Parietal Diameter Leaflet reg: ……..Title: Early pregnancy pain and bleeding Author E Morris Review date May 2017 HC Head circumference - both of these measurements of the fetus are used in later pregnancy - after 12-14 weeks. Should you require further advice on the issues contained in this leaflet, please do not hesitate to contact the: Early Pregnancy Assessment Unit/ Emergency Gynaecology Unit Women and Children’s Hospital 01482 608767 Gynaecology Ward Women and Children’s Hospital 01482 604387 Useful information Information on Gynaecology Services at Hull and East Yorkshire Hospitals NHS Trust can be found at: www.hey.nhs.uk/content/services/gynaecology Information on Maternity Services at Hull and East Yorkshire Hospitals NHS Trust can be found at: http://www.hey.nhs.uk/maternity www.womens-health.co.uk http://www.nhs.uk www.earlypregnancy.org.uk www.patient.org.uk http://www.screening.nhs.uk/annbpublications Leaflet reg: ……..Title: Early pregnancy pain and bleeding Author E Morris Review date May 2017 GENERAL ADVICE AND CONSENT Most of your questions should have been answered by this leaflet/booklet, but remember that this is only a starting point for discussion with your doctor. You will be asked to sign a consent form and you should be satisfied that you have received enough information before going ahead. Consent to treatment Before any doctor, nurse or therapist examines or treats you, they must seek your consent or permission. In order to make a decision, you need to have information from health professionals about the treatment or investigation which is being offered to you. You should always ask them more questions if you do not understand or if you want more information. INFORMATION ABOUT YOU As part of your care, when you come to the hospital, information about you is shared between members of a healthcare team, some of whom you may not meet. It may be used to help train any staff involved in your care. Information we collect may also be used after you have been treated to help us to maintain and improve the quality of our care, to plan services, or to research into new developments. We may pass on information to other health organisations to help improve the quality of care provided by the NHS generally. All information is treated as strictly confidential, and is not given to anyone who does not need it. If you have any concerns please ask your doctor, or the person caring for you. Under the Data Protection Act (1998), Hull and East Yorkshire Hospitals NHS Trust is responsible for maintaining the confidentiality of any information we hold on you. This leaflet was produced by the Gynaecology Service, Hull and East Yorkshire Hospitals NHS Trust and will be reviewed in May 2017. Ref: HEY13/2014 Leaflet reg: ……..Title: Early pregnancy pain and bleeding Author E Morris Review date May 2017
© Copyright 2026