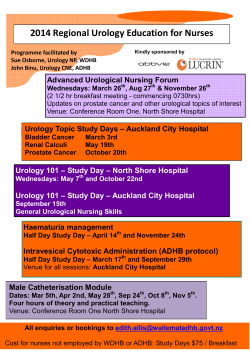
PDF - European Association of Urology
European Urology Today Official newsletter of the European Association of Urology 3 Vol. 26 No.5 - October/December 2014 How to serve as a peer reviewer Record attendance for 6th EMUC Infectious complication in prostate biopsies A rewarding, fulfilling experience More than 1,400 participants gather in Lisbon Alarming rate of ESBL positive E. coli Dr. Stephen Boorjian 5 7 Prof. Mete Çek EMUC 2014 underscores challenges in onco-urology Photography: Jack Tillmanns Multidisciplinary Lisbon meeting aims to align key treatment practices The EAU-ICUD Consensus Meeting takes a comprehensive look at current treatment options in onco-urology with the aim to provide recommendations. By Joel Vega Prospects and challenges are diverse in the management of urological cancers prompting onco-urology experts to identify key areas in the diagnostics of these diseases and help boost current efforts in aligning core treatment strategies. This was one of the aims of the EAU-International Consultation on Urological Diseases (ICUD) Consensus Meeting held on November 13 in Lisbon, Portugal, which preceded by a day the 6th European Multidisciplinary Meeting on Urological Cancers (EMUC) (See full EMUC report on page 5) and coincided with the 3rd Meeting of the EAU Section of Urological Imaging (ESUI) (Full report on page 11). “Our aim was to provide an overview and assessment of state-of-the-art systemic or medical treatment of urological cancers and we were grateful for the work of many experts from Europe and North America. They have identified major areas, where lies the challenges, which issues we can improve on and draw more attention,” said Prof. Christian Stief (DE), who co-organised the meeting in Lisbon together with Christopher Evans (USA) and Karim Fizazi (FR). To come up with an inclusive and in-depth assessment, 12 committees were created to examine a wide range of diagnostic and treatment issues in testicular, kidney, bladder and prostate cancers. Prostate cancer has the most extensive coverage with four committees investigating six areas such as androgen dependence and castration resistance, immuno- and gene-based therapies to cytotoxic chemotherapy and targeted agents. The meeting in Lisbon served as a preview to the collaborative effort, which has the goal to eventually publish in print and digital formats the collated views and expert opinions on first-line and follow-up treatments. Barring logistical and publication requirements, and awaiting the final text refinements of some committees, the plan is to release the consensus report by March in time for the 30th EAU Anniversary Congress in Madrid. Renewed interest Not only first-line but also follow-up targeted therapies were taken up in renal cell carcinoma (RCC) management. “There is renewed interest from researchers in recent years in immunotherapy. There is a doubling of abstracts at major conferences from 2009 and 2012. Approximately 800 clinical trials in various phases are on-going in breast, colon, head and neck, kidney cancer, etc.” said Allan Pantuck (USA), a member of the committee on alternative approaches in RCC. "The meeting in Lisbon served as a preview to the collaborative effort, which has the goal to eventually publish in print and digital formats the collated views and expert opinions on first-line and follow-up treatments." The discovery of a new class of drugs and checkpoint inhibitors have given rise to this renewed interest, and Cora Sternberg (IT) further described the committee’s recommendations on medical alternatives such as interleukin-2, interferon, cytokines plus targeted therapies, immune checkpoint inhibitors and therapeutic cancer vaccines. “Regarding interleukin-2, high dose intravenous IL-2 is currently the only approved treatment for mRCC that offers the possibility of long-term remission, but should be used as first-line treatment only in carefully selected patients,” said Sternberg. On cytokines combined with targeted agents, the committee said IFN with bevacizumab has yielded encouraging results and remains a first-line treatment option for kidney cancer patients. Prostate cancer was thoroughly discussed with the experts looking into the challenges and unresolved issues in castration resistance, cytotoxic chemotherapy, October/December 2014 immune-and gene-based therapies and androgen pathway targeted agents, to name a few. gemcitabine and MVAC, have an established role both in metastatic and perioperative settings. “Dendritic cell-based vaccines are promising but challenging strategies,” said Charles Drake (USA) who spoke on immunotherapy and other alternative treatments. He said more work needs to be done in the area of guidelines. Regarding DNA-based vaccines, he noted the flexibility of this treatment as a key attribute. Anders Bjartell (SE) gave an in-depth overview of the various issues in the chemotherapy of prostate cancer. “Chemotherapy with docetaxel has been the first treatment that provided an overall survival (OS) benefit in metastatic castration resistant prostate cancer,” said Bjartell. He added that taxanes exert an AR-axis mediated anti-prostate cancer effect which may be the background for future combinations with other AR-directed agents. On testicular cancer, Sophie Fosså discussed the long-term adverse effects in testis cancer survivors and said future research should examine how to reduce late complications and the mechanisms behind these adverse effects. Recommendations on urothelial carcinoma of the bladder, meanwhile, stated that cisplatin-based combinations, mainly ...there were also a lot of enthusiastic discussions... “The meeting was not only well-attended, there were also a lot of enthusiastic discussions. The committee members presented concise reports and data. What we have tried to achieve here in Lisbon is not only to show the methodology but also to provide practical recommendations and guidelines for daily practice,” said Fizazi at the end of the day-long meeting. #EAU15 30th Anniversary EAU Congress MADRID 20-24 March 2015 Sharing knowledge - Raising the level of urological care Register now for the early bird fee Deadline: 12 January 2015 European Urology Today 1 Update from the EAU Guidelines Office Dissemination: NGC, European Urology and Social Media EAU Guidelines on NGC Updated versions of three of the EAU Guidelines; Paediatric Urology, Male LUTS and Trauma, have recently been published on the National Guideline Clearinghouse™ (NGC). These can be viewed here: Paediatric Urology: http://www.guideline.gov/content.aspx?id=47872 Male LUTS: http://www.guideline.gov/content.aspx?id=48031 Trauma: http://www.guideline.gov/content.aspx?id=48030 EAU Guidelines on Social Media The Social Media Group are currently preparing to post Guidelines communications using the EAU Facebook: Like here: https://www.facebook.com/ EAUpage and Twitter accounts: Tweet @Uroweb: https://twitter.com/Uroweb Each panel chair has been contacted and asked to nominate a panel member who will act as a liaison with the Social Media Group, providing content from their panel that deserves special attention and dissemination to the urology community, such as interviews and information from panel meetings. This will be a highly engaging project and collaboration and comments are gratefully appreciated. Publications A systematic review by the EAU Muscle-invasive Bladder Cancer (MIBC) Panel on the impact of lymphadenectomy (LND) on oncological and perioperative outcomes in patients undergoing radical cystectomy (RC) for MIBC has recently been published in European Urology. The panel reviewed 23 studies reporting on >19,000 patients and found that any kind of LND was advantageous over none in terms of prolonged survival. However, it was evident that quality of data was poor and there is a need for higher quality studies. European Urology Today Read more on this interesting work here: http://www.ncbi.nlm.nih.gov/pubmed/25074764 Editor-in-Chief Prof. M. Wirth, Dresden (DE) Guidelines Office Workshops Following the recent changes to the Guidelines (meaning that all of the Guidelines are based on detailed and evidenced literature searchers), the Section Editors Prof. T.E. Bjerklund Johansen, Oslo (NO) Mr. Ph. Cornford, Liverpool (GB) Prof. O. Hakenberg, Rostock (DE) Prof. P. Meria, Paris (FR) Dr. G. Patruno, Rome (IT) Dr. G. Ploussard, Paris (FR) Prof. J. Rassweiler, Heilbronn (DE) Prof. O. Reich, Munich (DE) Dr. F. Sanguedolce, London (GB) Special Guest Editor Mr. J. Catto, Sheffield (GB) Founding Editor Prof. F. Debruyne, Nijmegen (NL) Guidelines Office European Official newsle tter Notification: Adolescen 9 of the Europe an Urology To day Association of Urolog y Active surveillanc EUT Editorial Office PO Box 30016 6803 AA Arnhem The Netherlands T +31 (0)26 389 0680 F +31 (0)26 389 0674 [email protected] Disclaimer No part of European Urology Today (EUT) may be reproduced without written permission from the Communication Office of the European Association of Urology (EAU). The comments of the reviewers are their own and not necessarily endorsed by the EAU or the Editorial Board. The EAU does not accept liability for the consequences of inaccurate statements or data. Despite of utmost care the EAU and their Communication Office cannot accept responsibility for errors or omissions. 2 European Urology Today Vol. 24 No.2 e for low-risk A word of warning: patients Active surveillance cancer and the risk of overdiagnosis on prostate Prof. Chris By Joel Vega Promoting your meetings t Special needs urology of adolescents creation of require the a stronger adolescent urology Wyndaele Prof. Jean-Jacques 31 27th Annual EAU Congres Sustained research s: work and multi-disciplin ary Bangma - March/May 9th ESOU Meeting 35 Collaborativ links are essential, 2012 800 participants gather in Hamburg on latest developments for update in urological cancers e work is crucial Further investments colleagues and specialists in innovative and urology’s said Prof. Hidehiro from other research studies stronger ties disciplines,” disciplines with other Japanese UrologicalKakizaki who co-chaired remain medical the Association that was reiteratedone of the key, overarching Chris Chapple. session with by opinion This year the themes returned Prof. five-day 27th leaders throughout Japanese delegation Annual EAU the nearly in full force with more February 24 Congress held than 150 a year after to 28 in Paris, from France. prevented many the Fukushima calamityparticipants, from attending which Experts who Vienna. the 2011 congress lectured and strategies during spoke in the congress on optimal treatment significant were one in The reporting gains made saying that sessions in medical management ICUD-EAU International of the Committees and surgical in recent years of the healthcare Consultation can only lead (5th ICI) held if innovative on Incontinence to better in the first two studies and closely working the need for days also demonstrated the crucial with other a balanced role of pursued. specialists are approach consistently fields such the rising incidence in other urological related Lower of incontinence Urinary Tract “This annual and the most highly Symptoms congress provides (LUTS). One together and of session collated attended meetings, the evidence that pursuing the reporting working research for goals of groundbreaki expert groups the consensus findings insights that of various on a range ng will help us treatment for of imaging, issues identify patients is only fistulas, pharmacology from epidemiology the strong links possible if we effective syndrome, , to bladder we now have,” among other maintain pain General Per-Anders incontinence said topics. Abrahamsson EAU Secretary ceremony. Focus on uro-oncology during the opening With eight Profs. Radziszewski EAU and Chapple plus the first Section Meetings held (3rd and 4th on plenary from left) chair cancer, participants session which tackledFebruary 25 the second plenary session variety of specialisedhad a full-day agenda bladder on functional Atala as he urology and a wide listed various topics to choose transmissions obstacles such complex work from. Live of involved in as rooms located surgeries conducted scaffolds, avoiding creating biologicalthe all-cause and in six operating in tumour formation prostate cancer were presented Paris, Aalst (BE) and construction added: “Surgery Mannheim mortality,” and the of stable blood (DE) (ESUT), a feat by the EAU Section of said Wilt. He did not reduce vessels. observation Uro-Technolo that exceeded mortality in men previous congresses. ESUT’s programmes gy The last-day cancer. A potential with low PSA or low more than plenary session The day-long in risk prostate in cooperation mortality benefi examined the session, conducted developments in exist in men with the ERUS, t from prostate cancer latest with higher presented complex EULIS and ESIU, Prof. Freddie PSA and possiblysurgery may disease.” (PCa) research. Hamdy giving surgical procedures bladder and high risk With personalised the keynote kidney surgeries. in prostate, treatment for remarks PCa, Professors low and intermediate on The concluding At the plenary risk late-breaking part of the last provided updatesTimothy Wilt and Lars session on Holmberg developments session focused on Professors managing bladder PCa, respectively. on the PIVOT and SPCG4 Mason and Manfred cancer Fritz Schröder with Professors Malcolm studies on in-depth discussions,Wirth and James neoadjuvant updating the highlighting Catto led hormone therapy audience on either medical the screening suitability data, respectively. and prostate cancer of the extent and or surgical approaches (depending aggressivenes on patient’s response s of the Key messages to the selected disease) and from Mason have seen an treatment. • Degarelix and improvement “We is ‘non-inferior’ Schröder were: quality of life,” in technique, goserelin to said capacity the combination Prof. Arnulf plus bicalutamide and on the benefi Stenzl in of volume in patients ts at reducing standard despiteof cystectomy, considered his lecture prostate with advanced dependent as the gold the emergence hormonePCa (Mason). therapies. of newer medical • The Phase 111b Catto noted the offered better CS30 trial revealed that issues, a fact critique on radical surgery degarelix control of lower symptoms (LUTS) underscored due to QoL urinary Live transmissions that chemo-radiat by Nicholas such as frequency, tract of prostate, James who hesitancy in ion offers benefi conducted in bladder and urgency and said Session urination. (Mason). of patients, kidney surgeries 6 operating ts to certain and pointed participants rooms organised by view the ESUT out that bladder-prese types deserves a 3D glasses ESUT in cooperationin 3 different countries, live surgeries • The two-year re-evaluation were rvation with with EULIS, in the light update on the ERUS and ESIU of recent data. 21% reduction ESRPC study The need for showed a of 1% comparedon PCa mortality rate, sustained research Right on the or an increase theme in the with the interim “In men with efforts was first day, the (Schröder); second plenary a recurring localised prostate study of 2009 joint the EAU with and urology with session on during the 11 other regional meetings organised cancer detected functional early PSA era, by underlining Profs. Chapple and associations radical prostatectomy compared to Piotr Radziszewski for the Urology and international • Early PCa the crucial role observation programme diagnosis has identifying did not signifi demonstrated Beyond Europe defi the most effectiveresearchers can play the known cantly reduce consultation the in disadvantage nite benefits, alongside treatment. Prof. medical or among various need for closer s, such as a overdiagnosis surgical Karl-Dietrich Particularly urology high emerging prospects, (Schröder). rate of Sievert examined groups. in uro-oncology and medical saying that newer options treatment for where new diagnostic in pharmacother current trends point cancers are prostate and current use to emerging, kidney of antimuscarini apy aside from the practitioners countries such On biomarker cs from research, Sievert and PDE-5 inhibitors. Latin-America as Japan, Iran, India, the diverse outcomes in expects more n Arab and the coming concrete vital to maintaincountries, to name a years as new data come in. effective collaborativefew, said it is and outside Technologica urology. work within l advances New technology “Our participation were discussed and the attendant myriad here reflects in the fourth-day challenges learning from topics such the important plenary session each other. as the optimal role of if we expand We can only with nephrolithoto use of percutaneous move forward our views to my, consider those ureterendosco new optical systems of our in py, benefits and the use of of simulation shock wave lithotripsy AUA lecture in surgical training. The on Anthony Atala, regenerative medicine given Regenerative director of the Wake Forest by Prof. Medicine, Institute for in tissue engineering, showcased the current efforts particularly cells to create biological substitutesthe use of stem kidney, heart, for the bladder, liver and many other organs. “There are still resolve several challenges ahead…we March/May still need issues in tissue 2012 engineering,” to said say opinio n leaders 28th Annu al EAU Cong ress www.eaumilan2 Editorial Team H. Lurvink, Arnhem (NL) J. Vega, Arnhem (NL) L. Keizer, Arnhem (NL) Guidelines Office Board are offering workshops to all panels. The workshops will cover systematic review methods as the backbone of guidelines production and will discuss the upcoming projects of the panel. The workshops will cover two days and are 013.org European Urology Today The EAU executive is pleased to help promote any scientific meetings. However, due to the large number of requests we are receiving, we have been forced to set up some rules and regulations related to the circulation of promotional material. All EAU related meetings (Section Offices either full members or partners) and national societies meetings with which we have a special alliance, may be promoted by e-mail (e-mail newsletter or separate e-mail communication), in addition to the other available channels. All other urological meetings may be included in our Uroweb and Urosource congress calendar as well as in the European Urology Today congress calendar. Please feel free to contact us ([email protected]) in case there are any queries or remarks related to this notice. 1 coordinated by Prof. James N’Dow’s team from Aberdeen University and Prof. Richard Sylvester. The Bladder Cancer Panels recently had a successful workshop and the aim is to complete these workshops for all panels by mid-2015. EAU Pocket Guidelines App FREE for EAU members available now in your Appstore search for “EAU Pocket Guidelines” in your appstore European Urological Scholarship Programme (EUSP) Do not forget to submit your online applications for Short Visit, Clinical Visit, Clinical and Lab Scholarship, and Visiting Professor Programme, before the next deadline of 1 January 2015! For more information and application, please contact the EUSP Office – [email protected] or check our website http://www.uroweb.org/education/scholarship/ October/December 2014 How (and why) to serve as a Peer Reviewer Table of Serving as a reviewer can be a rewarding, fulfilling experience Stephen Boorjian, MD Professor of Urology, Mayo Clinic Associate Editor, European Urology boorjian.stephen@ mayo.edu The currency of academics is peer-reviewed publication. Publications form the basis for communication of novel ideas and of research findings, while facilitating practice improvement and the expansion of knowledge. tables and figures, which should add to the data presentation rather than merely re-presenting information provided in the text. Introduction and Discussion sections While not as critical as the Methods or Results Sections, nevertheless, the text of the Introduction and Discussion serve as an important backdrop for the focus of the study. That is, the Introduction Section of a manuscript should appropriately define topic of study, should state the existing gap in knowledge which makes the present study relevant, and should clearly outline the hypothesis/question being investigated. Meanwhile, the Discussion should (a) summarise the critical findings of the manuscript, (b) contextualise these findings in light of the existing literature on the topic, (c) acknowledge the present study’s limitations, and (d) offer next steps for research in the field. Accordingly, an essential component of the publication process is peer review, without which journal publication would not be possible. Nevertheless, little attention has been given to provide training on how to perform a thorough and appropriate manuscript review. Largely, a perfunctory literature review at conferences/journal clubs comprises the extent to which our trainees are exposed to the process of critically evaluating a manuscript. The importance of references The References Section represents an absolutely critical element of a manuscript, and should be assessed in detail during a manuscript review. Why? Appropriate referencing of the relevant literature on the topic being presented reflects the authors familiarity (and as such expertise) with the subject. Are the most salient references on the topic included? At the same time, given numerous competing clinical, research, and teaching commitments, as well as the challenge of maintaining work-life balance, the relative value of serving as a journal peer reviewer has been questioned. Are the references timely? Look as well at the journal source for the references. In addition, while some degree of self-citation may be a result of the authors’ previous extensive work in the field, over self-citation may be a problem. Herein, an approach to performing effective manuscript review is offered, as well as reflections on the potential personal/professional benefits an individual might enjoy by participating in this time-honored and essential service. Is the “devil in the details” – do the listed author requirements for submission matter? As with clinical practice, careful attention to detail typically reflects quality work when it comes to manuscript submissions. Thus, when reviewing a manuscript, be knowledgeable about the journal’s Tips for Effective Manuscript Review guidelines (instructions for authors), and look to see Assessing the manuscript title/abstract whether the authors followed these. Was the abstract Frequently, the casual reader will go no further than structured according to journal specifications? Is the the manuscript title and abstract. As such, these must word count in compliance? Were the references provide an appropriate representation of the work. formatted correctly? Do the numbers provided in the One should determine whether the title accurately text of the manuscript match with those provided in represents the topic/findings being reported. the accompanying tables/figures? While none of these Moreover, the abstract should represent a “stand features alone should form the basis for a decision alone” element that contains the most important regarding a manuscript’s disposition to accept/reject, methodologic information and data from the such factors do in fact reflect the authors’ level of manuscript. In addition, the conclusions put forth in vigilance, and thus should be considered and the abstract should be supported by the data provided commented upon by the reviewer. in the Results Section of the abstract, rather than reflective of findings reported in the manuscript only, How to get better as a reviewer which the abstract-only reader will not be privy to. As with any new endeavor: practice, practice, practice. Early on, accept review invitations whenever your Methods and Results sections schedule allows. By going through the process These sections represent the most important repeatedly, you will become more efficient and will components of the manuscript, and should be the sharpen your skills. In addition, follow-up on the focus of the bulk of the reviewer’s time during disposition of the manuscripts you are invited to assessment of the manuscript. In the Methods review – did the editor agree with your Section, the reviewer should particularly evaluate recommendations? What were the other reviewers’ whether the appropriate level of detail regarding the comments? A great deal can be learned by seeing the study population is provided (i.e. are inclusion/ manuscript through another reviewer’s commentary. exclusion criteria clearly defined). Moreover, the Don’t be concerned if your comments and/or appropriateness of the methodology utilized to recommendation disagree – more important is to gain address the question of interest should be what each of the other reviewers and editors took as determined. That is, for example, if a study evaluated the “50,000 foot view” of the manuscript’s strengths quality of life, the reviewer should particularly note and weaknesses. what instruments are being used, and whether these represent validated measures. Likewise, for statistical analyses, the appropriate use of Cox proportional hazards regression models versus logistic regression models should be noted. Whenever feasible, standardised reporting guidelines should be utilised. The Results Section of a manuscript, meanwhile, represents central focus of the study, and should be the section to which the reviewer is most careful in evaluating. Herein, specific points for consideration include the robustness of the dataset (i.e. number of patients, number of events, duration of follow-up) and completeness of reporting (i.e. do the authors provide data on disease progression, cancer, cancer-specific mortality, and all-cause mortality). These measures should be contextualised within the disease state being studied. That is, a three year median follow-up would not be appropriate to assess mortality following surgery for localised prostate cancer, while three years would represent a reasonable duration to report mortality following cytoreductive nephrectomy for metastatic renal cell carcinoma. Attention should be given as well to the European Urology October/December 2014 Benefits of Serving as a Manuscript Reviewer Personal benefits The critical elements discussed above to evaluate when you are reviewing a manuscript are in turn the critical elements to include when writing a manuscript. As such, the practice of peer review will sharpen your writing for subsequent independent manuscript submissions. Through seeing what “works” (as well as what doesn’t) in papers, investigators can significantly enhance the quality of their own work. Moreover, appropriately contextualising the data from a manuscript under review, and being able to thereby determine the novelty of the topic and findings being reported, necessitates an understanding of the relevant literature on the topic in question. In this process, one gains an increased knowledge base that not only further improves research activities but also enriches one’s approach to clinical practice. Furthermore, by serving as a manuscript reviewer, you are the “front line” for what is often new data, and the opportunity to get a first glance at such findings can be quite exciting. Professional gain Young academic urologists often feel as if they toil in obscurity, with the myriad of senior, established colleagues making individual recognition difficult early in one’s career. Providing high-quality reviews in a timely fashion is one way to gain rapid visibility. Editors quickly identify “go to” reviewers who, based on their track record, can be counted on. These individuals are often recognized by journals with awards for their work, and/or are invited to contribute review articles, and to join editorial boards. Thus, quite rapidly junior faculty may be provided with numerous opportunities as a direct result of their work in the manuscript review process. A rewarding service In summary, the reviewer should consider four central concepts when considering a manuscript: (1) the originality of the topic, (2) the robustness of the dataset, (3) the appropriateness of the methodology, and (4) the importance of the findings. From these four issues, the reviewer can provide to the editor an assessment of whether the manuscript in question adds in a meaningful and significant way to the existing literature on a topic. Manuscript reviewing is a voluntary service, which may be time-consuming and, when starting out, even overwhelming. However, with time and practice, one can rather quickly become quite adept at performing a thorough critical assessment of a manuscript. Offered here are various insights to performing a manuscript review, although it should be noted that with experience one will undoubtedly develop an individualized approach and many styles can be equally effective. The service though demanding can be quite rewarding – through the process, you are contributing to the very essence of academics, and have the opportunity to view new data first and to improve contributions to the literature. Young academics may derive both personal and professional career development. Most importantly, this should represent an enjoyable and fulfilling compliment to one’s clinical and research practice. Contents EMUC Meeting underscores challenges in onco-urology. . . . . . . . . . . . . . . . . . . . . . . 1 Update from the EAU Guidelines office. . . . . . 2 How (and why) to serve as a Peer Reviewer. . 3 Clinical challenge. . . . . . . . . . . . . . . . . . . . . . 3 Record attendance for 6th EMUC edition. . . . . 5 EUREP section: Enthusiasm and opportunities at the 12th EUREP. . . . . . . . . . . . . . . . . . . . . . . . . . . 8 Honing surgical, medical skills in a friendly environment. . . . . . . . . . . . . . . . . . . . . . . . . . 8 EUREP 2014: An investment in the future of urology. . . . . . . . . . . . . . . . . . . . . . . . . . . . 9 Bringing resident training to another level. . . 9 An “Aussie” perspective on EUREP. . . . . . . . . 9 EBU section: EBU Certified Residency Training Programme in Urology. . . . . . . . . . . . . . . . . 10 Vall d’Hebrón University Hospital. . . . . . . . . 10 3rd ESUI Meeting: Insights and prospects on urological imaging . . . . . . . . . . . . . . . . . . 11 Supple prescription rules in oncology drugs in Italy . . . . . . . . . . . . . . . . . . . . . . . . 12 Infectious complication in prostate biopsies. 12 Key articles from international medical journals. . . . . . . . . . . . . . . . . . . . . . . . . . . . 14 Obituary Aldo Vittorio Bono. . . . . . . . . . . . . 17 CEM Symposium report: BPH. . . . . . . . . . . . 18 14th CEM: Closing the gap between East and West. . . . . . . . . . . . . . . . . . . . . . . . 19 10th SEEM reflects region’s growing role in urology. . . . . . . . . . . . . . . . . . . . . . . . . . . 20 ESU section: Comprehensive ESU course on male LUTS. . . 21 ESU-Weill Cornell Masterclass in historic Salzburg. . . . . . . . . . . . . . . . . . . . . . . . . . . . 22 ESU-Weill Cornell Masterclass in General Urology. . . . . . . . . . . . . . . . . . . . . . . . . . . . 22 ESU offers comprehensive course to Armenian urologists. . . . . . . . . . . . . . . . . . . 23 Simulation fellowship: growth of a new research field. . . . . . . . . . . . . . . . . . . . . . . . 23 ESUT section: Masterclass in advanced 3D video-assisted urological surgery . . . . . . . . . . . . . . . . . . . . 24 State-of-the-art urological surgery in Heidelberg. . . . . . . . . . . . . . . . . . . . . . . . . . 25 4th International Course on Advanced Laparoscopic Urology. . . . . . . . . . . . . . . . . . 25 Ten questions: Michael Jewett . . . . . . . . . . . 24 Global Action Plan on Active Surveillance for low risk PCa . . . . . . . . . . . . . . . . . . . . . . 26 Book reviews. . . . . . . . . . . . . . . . . . . . . . . . 27 EULIS section: Preventing stone migration during intracorporeal lithotripsy . . . . . . . . . . . . . . . 28 EULIS launches new postgraduate workshops on urolithiasis. . . . . . . . . . . . . . . 29 YUO section: ESRU’s objectives in practice . . . . . . . . . . . . 30 The New Portuguese Residents Society. . . . . 30 An excellent training experience in Belgium. 31 ESUR Meeting examines research prospects, challenges. . . . . . . . . . . . . . . . . . 31 Make fewer passes, use fewer products, and reduce costs. Prostate stem cell research continues hunt for genetic clues. . . . . . . . . . . . . . . . . . 32 EUSP Clinical Visit in Braga. . . . . . . . . . . . . . 32 EAU-RF: NIMBUS trial re-opens in Germany, starts in The Netherlands . . . . . . . 33 EAU and partners: synergies. . . . . . . . . . . . . 34 Don’t forget to renew your EAU Membership!. 35 Congress calendar 2014/2015 . . . . . . . . . 36-37 Flexor Parallel ® ERUS2014: Robotic Urology draws big crowd to Amsterdam . . . . . . . . . . . . . . . . . . 37 ™ R A P I D R E L E A S E ™ U R E T E R A L A C C E S S S H E AT H MEDICAL www.cookmedical.com © COOK 2012 URO-BEMEAADV-FLPEUT1-EN-201212 EAUN section: Nurses’ Programme at EAU Robotics Section Meeting. . . . . . . . . . . . . . . . . . . . . . . . . . . . 38 EAUN joins Chinese Urology Association meeting. . . . . . . . . . . . . . . . . . . . . . . . . . . . 39 15th Asia-Pacific Prostate Cancer Conference. 39 What to expect at the EAUN 2015 Annual Meeting. . . . . . . . . . . . . . . . . . . . . . . . . . . . 40 European Urology Today 3 Clinical challenge Prof. Oliver Hakenberg Section editor Rostock (DE) The Clinical challenge section presents interesting or difficult clinical problems which in a subsequent issue of EUT will be discussed by experts from different European countries as to how they would manage the problem. Readers are encouraged to provide interesting and challenging cases for discussion at [email protected] Oliver.Hakenberg@ med.uni-rostock.de Case study No. 40 This 74-year-old man, a retired general practitioner, was referred by a nephrologist with intermittent left lumbar pain and hydronephrosis of the left kidney for three months. A degree of renal failure had been known for several years, current serume creatinine was 180 mg/dl. The patient had been on antihypertensive treatment for several years; current blood pressure was well controlled. A renal scintigraphy showed reduced overall renal function, with a distribution of 80% to 20% for the right and left kidneys, respectively. A left retrograde ureterogram showed marked medialisation of the left ureter and a double-J stent was inserted on the left side. A CT scan of the abdomen was performed (Fig. 1 and 2). Discussion points: 1. What differential diagnoses should be considered? 2.Are further investigations needed? 3.What is the likely diagnosis? 4.Which treatment is appropriate? Fig. 1 and 2: Abdominal CT scan Case provided by Oliver Hakenberg, Department of Urology, Rostock University Hospital, Germany. ([email protected]) A case of inflammatory aortic aneurysm Comments by David Castro-Diaz, Santa Cruz de Tenerife (ES) The CT scan shows three main findings: 1. A non-dissecting aneurysm of the abdominal aorta, with displacement of the abdominal aorta to the left side; 2.A dilated left kidney with preserved parenchymal thickness, suggesting an acute or sub-acute rather than chronic cause such as a renal artery aneurysm (stenosis or dissection); and 3.A left ureter displaced medially with a ureteral stent inside. The presence of left hydronephrosis and medial displacement of the ureter associated with aortic aneurysm and urologic symptoms is typical of inflammatory aortic aneurysm (IAA). This entity represents 3-10% of abdominal aortic aneurysms and in contrast to degenerative aortic aneurysm (DAA), which remains asymptomatic until rupture, the IAA usually presents with abdominal or urological symptoms. Abdominal pain is present in 85% and back pain in 55% of cases and it is associated with hydronephrosis in 20-30% of patients. The latter usually leads to deterioration of renal function, eventually with elevation of serum creatinine. In addition, 90% of patients have an elevated erythrocyte sedimentation rate (ESR) indicating a systemic inflammatory state. There are several characteristic findings of this condition to be seen on the CT scan such as medialisation of the left ureter and four distinct layers of the aneurysm: lumen, mural thrombus, thickened aortic wall and associated fibrosis. Furthermore, contrast injection shows increasing density of the uniform periaortic inflammatory layer. An MRI scan might provide further useful information for the differential diagnosis, which mainly is retroperitoneal fibrosis. Medical treatment with corticosteroids is controversial, and may be indicated in symptomatic patients with an aneurysm size that does not require surgery. The surgical treatment of choice is challenging and would be the retroperitoneal resection of the aneurysm instead of a classical transperitoneal approach. Immunosuppressive treatment for periaortitis Comments by Joachim Thüroff, Mainz (DE) This 74-year-old man has hydronephrotic atrophy of the left kidney with a remaining split function of 20% on radionuclide testing. Despite left-sided renal deterioration that has obviously been ongoing for a longer period of time, clinical symptoms of left flank pain are reported only for the past three months. The left retrograde ureteropyelogram (not provided) reportedly shows medialisation of the left ureter. The two presented coronar CT images after placement of a double-j stent on the left side do not allow formal exclusion of all possible differential diagnoses of hydronephrotic atrophy of the left kidney, such as decompensated UPJ stenosis or an impacted ureteral stone. This is firstly, because not all parts of the left collecting system and ureter are visible on the two images, and secondly, because the described hydronephrosis of the left kidney is, at least, partially relieved by the indwelling double-j stent. However, these differential diagnoses are unlikely since other pictures, e.g. of the retrograde study or the CT scan, would have been provided in such cases. Hence, the most likely diagnosis is retroperitoneal fibrosis (Ormond’s disease), which characteristically is associated with medialisation of the ureter. Since retroperitoneal fibrosis has primary and secondary forms, the pathology of the aorta, which is depicted in Fig. 2, has to be discussed. Concerning the etiology, the tissue augmentation of the abdominal aorta is clearly located outside the genuine aortic wall, which can be identified by several small calcifications. In the literature, these changes are described as “chronic periaortitis”, “giant cell aortitis”, “coated aorta”, “Takayasu arteritis” and “Horton arteritis” (1 – 5). The etiology of the aortitis might be infective (mycotic, syphilitic) or – in the abdominal location – predominantly non-infective, non-syndromic of autoimmune nature or syndromic such as associated with Erdheim-Chester disease or histiocytosis X. Treatment of the most common autoimmune type is anti-inflammatory with cortisone and immunosuppressive medication such as Azathioprin. If ureteral obstruction does not respond to this medication, surgical ureterolysis and entrapment of the freed ureter into greater omentum or peritoneum may be considered for a wellfunctioning kidney. However, a poorly functioning kidney in a 74-year-old man, as in this case, might be subjected to nephrectomy. References 1. Svensson LG, Arafat A, Roselli EE, et al. Inflammatory disease of the aorta: Patterns and classification of giant cell aortitis, Takayasu arteritis, and nonsyndromic aortitis. J Thorac Cardiovasc Surg. 2014 Aug 8. [Epub ahead of print] 2. Vaglio A, Pipitone N, Salvarani C. Chronic periaortitis: a large-vessel vasculitis? Curr Opin Rheumatol. 2011 Jan;23(1):1-6. 3. Tölle PA, Kesten F, Daikeler T. Giant cell arteritis followed by idiopathic retroperitoneal fibrosis in the same patient - an unexpected positron emission tomography finding. Rheumatology (Oxford). 2012 Sep; 51(9):1549. 4. Chiba K, Kamisawa T, Tabata T, et al. Clinical features of 10 patients with IgG4-related retroperitoneal fibrosis. Intern Med. 2013; 52(14):1545-51. 5. Dion E, Graef C, Haroche J, et al. Imaging of thoracoabdominal involvement in Erdheim-Chester disease. AJR Am J Roentgenol. 2004 Nov;183(5):1253-60. Case Study No. 40 continued The most likely diagnosis seemed inflammatory aortic aneurysm with left renal hydronephrosis. The patient was treated medically with anti-inflammatory drugs including corticosteroids and continued left double-J ureteric drainage. This led to improvement in symptoms and renal function remained stable. Improvement of the para-aortic inflammation was also noted on follow-up CT scans. However, the patient complained of continuing, and subjectively, very bothersome symptoms related to the double-J stent which had been changed at regular intervals. He was offered reconstructive surgery for the left ureteric obstruction but instead he insisted on left nephrectomy which was ultimately performed. Case study No. 41 Discussion points: 1. What type of injury is present? 2. Are further investigations needed? 3. What treatment should be done? This 35-year-old man suffered a motorcycle accident. There was a fracture of the right hand and otherwise no bony injuries at all. He was seen at Accident & Emergency where right flank pain and some abdominal distension was noted. A urinary catheter was inserted and marked microscopic hematuria noted. The abdominal CT scan is shown in Figures 1 and 2. There were no other associated injuries except the hand fracture and the patient was hemodynamically stable at all times. Case provided by Oliver Hakenberg, Department of Urology, Rostock University Hospital, Germany. Figures 1 and 2: Abdominal CT scan 4 European Urology Today Readers are encouraged to provide interesting and challenging cases for discussion. October/December 2014 Record attendance for 6th EMUC edition Focus on chemo-resistance, evolving drug landscape By Joel Vega With 1,456 participants from 66 countries, the 6th European Multidisciplinary Meeting on Urological Cancers (EMUC) held in Lisbon, Portugal from November 14 to 16, marked the highest number of attendance for the annual meeting which aims to bridge the various treatment strategies by urologists, medical oncologists and radio-oncologists. “After seven years of holding this congress, we have always focused on the central aim to foster education and knowledge in urological cancer and improve diagnosis and treatment through a multi-disciplinary approach. Optimal treatment for cancer patients can only be achieved if we continue with collaborative activities such as the EMUC,” said EAU Secretary General Per-Anders Abrahamsson (SE) in his opening remarks. Together with Joaquim Bellmunt (USA) of the European Society for Medical Oncology (ESMO), Philip Poortmans (NL) of the European Society for Therapeutic Radiology and Oncology (ESTRO), Gertraud Heinz-Peer (AT) of the European Society of Urogenital Radiology (ESUR), and Antonio LopezBeltran (PT) of the European Society of Pathology (ESP), Abrahamsson said the surge in attendance testifies to the shared goal of onco-urology experts to benefit from the synergies of collaborative work. During the voting in the first plenary session around 46% in the audience were urologists, 21% radiooncologists, 15.6% medical oncologists and 0.6% radiologists. Based on the initial survey voting, a typical EMUC participant was academe-based (535), either a staff member or consultant physician (93.6%), based in Europe and a member of the EAU (42%). The two-and-half day scientific programme examined prostate, testis, penile, kidney and bladder cancers in lectures, roundtable discussions, debates and abstracts presentations. Hands-on training on radiotherapy delineation contouring workshops were also offered. For the first time, the EMUC was preceded on November 13 by two simultaneous, complementary meetings-- the EAU- International Consultation on Urological Diseases (ICUD) Consensus Meeting and the 3rd Annual Meeting of the EAU Section of Urological Imaging (ESUI). Progressing prostate disease Prostate cancer (PCa) was the first topic in the plenary session of the first day with a case presentation, followed by lectures on imaging, treatment for progressing PCa and a point-counterpoint presentation on intermittent androgen deprivation (IAD) versus continuous androgen deprivation (CAD) in the treatment of castration-resistant prostate cancer (CRPC). Maha Hussain (USA) argued for CAD while Abrahamsson gave the opposing views in favour of intermittent therapy. Downplaying the benefits of IAD, Hussain examined the strengths and weaknesses of major trials, survival outcomes and quality of life (QoL) data, and said no trial to date has demonstrated overall survival (OS) superiority or equivalence of IAD over CAD. In her concluding remarks, she compared CAD with IAD in various disease settings. Hussain said CAD has a role for the adjuvant setting where survival can be prolonged with androgen deprivation therapy (ADT) and local therapy. Regarding non-metastatic PSA-only relapse, neither approaches yield added benefit based on current data, but for IAD, she noted: “There is possibly (a role) but a balanced discussion is needed considering the lack of data to support significant outcome impact of either approaches.” Abrahamsson, arguing for IAD, underscored the discussion basically centres on the question whether “to give more drugs or giving less drugs” while noting that in maximal androgen blockade (MAB), majority of trials are sponsored by industry compared to a few trials for IAD. “There is no clear evidence for inferiority or superiority of intermittent androgen suppression (IAS) in terms of time to CRPC,” said Abrahamsson as he insisted that IAD is equivalent to CAD in selected patients. IAD is effective as continuous ADT but with better tolerability, according to Abrahamsson. “There is insufficient data to determine whether IAD is able to prevent the long-term complications of ADT,” he said. ”And more comparative analysis focused on QoL issues is warranted.” "Malignant and normal stem cells possess multiple mechanisms of resistance to radiotherapy." - Norman Maitland In the same session, Jelle Barentsz (NL) discussed optimising imaging for biochemical recurrence, Martin Gleave (CA) examined the natural history of progressing PCa and whether treatment is always needed, Marco Van Vulpen (NL) spoke on curative radiotherapy for local recurrence, Steven Joniau (BE) on curative surgery and salvage lymph node dissection, and Gerhardt Attard (GB) on optimal treatment for metastatic CRPC. A few of their concluding remarks are: • Van Vulpen on focal therapy: “Focal therapy seems the best approach, but there are no large series or long-term follow-up. In my opinion what technique to use is not relevant, but quality assurance is more essential.” • Joniau on salvage lymph node dissection (LND): “If salvage LND is considered, extended LND templates are necessary, and for majority of patients salvage LND will postpone hormonal therapy and has limited toxicity.” Chemoresistance in kidney cancer The second half of the first day was largely focused on renal cell carcinoma (RCC), testis and bladder cancer with topics ranging from the role of LND in renal surgery, new drugs in the pipline for RCC, checkpoint inhibitors in onco-urology, the role of minimally invasive radical cystectomy and management of bladder cancer. “Understanding and overcoming resistance is a major challenge and drugs to overcome resistance are needed,” he stressed. Escudier enumerated several drugs being eyed as the next generation in the fight against kidney cancer, the 13th most deadly cancer worldwide, and which accounts for only 4% of all adult malignancies in industrialised countries. However, kidney cancer kills many since 3 in 10 patients present with metastasis at the time of diagnosis. With a 25% mortality rate, it is the most malignant of urological tumours. October/December 2014 Drugs in development include AZD-8055, Buparlisib, MK-2206, GDC-0980/BEZ-235 and perifosine, which are either in phase 1 or 2 studies. Regarding immunotherapy Escudier said PD-1 blockade is a strategy for immunotherapy, which experts consider a promising option in the coming years. “New targets The 6th EMUC gathered the biggest attendance with more than 1,400 participants are arising, cMET being the most advanced one; targeted immunotherapy is very promising, but need to carefully select patients who can benefit from ‘when and how’ are the questions,” Escudier said. radiotherapy,” said Huddart as he noted patients with single, small tumours are suitable candidates. Bladder cancer management Heinz-Peer discussed imaging procedures in bladder cancer and new approaches in the evaluation of “There is a feeling that surgery is the only way to go. haematuria, the strengths of new imaging techniques But if you have a proper discussion with patients, radiotherapy can be an acceptable option to many, “ such as PET-CT and multi-detector computed tomography urography (MDCTU), which provides high said Huddart during the Q&A and in response to a query on why radiotherapy is not widely considered quality multi-planar reformations (MPRs) and 3D as an option in bladder cancer management. reconstructions including virtual cystoscopic views. Although MDCTU has excellent detection rates including lesions less than 5 mm, it has low sensitivity Torben Orntoft (DK) discussed the translational approach in bladder cancer. Among the core for Tis/Ta lesions and does not provide biopsy, challenges, Orntoft said are: identifying which tumour will recur, how physicians can simplify the follow-up In her concluding remarks, she noted the clear advantage in using MDCTU and flexible cystoscopy as process, which tumour will progress, and in case of muscle invasive cancers, which bladder tumours will a triage test for rigid cystoscopy and follow-up. Furthermore, the sensitivity of voided urine cytology is benefit from cystectomy and radiation therapy. He discussed the work being done on surveillance inferior to CT-ultrasound and flexible cystoscopy. markers and expressed optimism current research Carl Magnus Annerstedt (SE) discussed minimally will eventually yield a considerable amount of insightful data. “Genomic-wise, bladder cancer is a invasive radical cystectomy such as robot-assisted radical cystectomy (RARC), a safe procedure which very complex disease. But we hope big data will be coming,” he added. yields similar results as open radical cystectomy. He said intracorporeal diversion in RARC procedure is truly minimal but stressed standardisation is Best presentations EMUC highlighted innovative research work, selecting important in RARC. the best unmoderated posters and the best oral presentation. F. Al-Ubaidi (SE) won the first prize for Regarding bladder preserving strategies, Robert Huddart (GB) said radiotherapy has now wider appeal his study “Castration promotes radiosensitivity by direct to patients who want to preserve their bladder and regulation of DNA repair in prostate cancer.” sexual functions. Moreover, elderly patients and those Per-Anders Abrahamsson and his team (SE) took the with co-morbidities have more benefits with second prize for their work on “Disease characteristics radiotherapy compared to surgery. “But there is a influencing the duration of the off-treatment period during intermittent androgen deprivation therapy with degarelix in prostate cancer.” Third prize went to W. Ong (AU) for the study, “Comparison of short term oncological and functional outcomes between open and robotic-assisted radical prostatectomy for localized postate cancer in the Victorian prostate cancer registry.” The best unmoderated poster prizes on Sunday went to K. Izumi (JP) “The impact of androgen deprivation therapy on bladder cancer recurrence: Retrospective analysis,” (First Prize); V. Neiman (IL) won the second prize for his study “Clinicopathologic factors associated with the development of sunitinib induced hypertension (HTN) in patients (pts) with metastatic Renal Cell Carcinoma (mRCC),” and T. Yap’s (GB) study “Does pelvic lymph node dissection have a role in the treatment of penile cancer?” bagged the Third prize. Michael Blute (USA) spoke on LND in renal surgery, Bernard Escudier (FR) on new drugs for RCC, Joaquim Bellmunt discussed checkpoint inhibitors, while Heinz-Peer examined the various imaging approaches in bladder cancer. On RCC, Escudier gave an overview of new drugs and highlighted concerns about chemoresistance. “Although VEGF and mTOR inhibitors are still the backbone of renal cell carcinoma (RCC) treatment, new treatments are coming,” said Escudier. He, however, cautioned that patients are developing drug resistance. Audience votes on treatment strategies mentioned so-called inhibitor drugs such as nintedanib, linifanib and cediranib, which are currently in phase 3 studies but with efficacies that are still unclear. “There are several categories with regards to new drugs which target the VEGR/mTOR pathway, those aimed to overcome resistance, and drugs for new targets and immunotherapy,” said Escudier. He Plenary session on castration-resistant prostate cancer Bogdan Geavlete (RO) beat four other candidates to win the first prize in the best oral presentations with his study “The long term outcome of combined NBI-plasma vaporization approach in large NMIBT cases – a prospective, randomized controlled comparison to the standard management.” Selected key messages • On Prostate Cancer: “Active surveillance (AS) should be regarded as a temporary but indispensable solution for PSA screening related over-diagnosis and overtreatment. ” -Monique Roobol (NL) • On Cancer Stem Cells: “Every human prostate cancer contains a therapy resistant, quiescent population of stem-like cells…Malignant and normal stem cells possess multiple mechanisms of resistance to radiotherapy. The stem cells are stimulated to amplify by our current therapies.” -Norman Maitland (GB) • On Immunotherapy: “Immunotherapy (Sipuleucel-T) has demonstrated effect on overall survival in prostate cancer.” -Karim Fizazi (FR) • On Small Renal Masses: “Percutaneous biopsy is safe and adequate cores have good diagnostic yield and accuracy for diagnosis of malignancy.” -Alessandro Volpe (IT) European Urology Today 5 ESOU15 12th Meeting of the EAU Section of Oncological Urology 16-18 January 2015, Munich, Germany PRIME- approach to improve the outcome of cancer treatment in uro-oncology Known for its comprehensive and provocative discussion of uro-oncological issues, the ESOU will present key updates and insights from Europe’s leading opinion leaders. Presentations will not only include state-of-the-art lectures but they will also focus on pro and- contra debates, panel discussions including multidisciplinary tumour boards and videos demonstrating various surgical techniques in uro-oncology. Due to the broad spectrum of the scientifi c programme, the ESOU meeting is the number one place to go for young urologists in training, mid-career and veteran uro-oncologists to update their knowledge on the management of patients with urogenital malignancies as well as in ongoing clinical and basic research concerning urological cancers. In addition we also have the STEPS programme (Sessions To Evalute ProgresS in the management of urological cancers) which is now already in its fifth year. This innovative programme allows a limited number of young academic urologists to meet established experts in the fi eld of prostate, bladder and renal cancer. Application information will be distributed through European academic centres. We would strongly encourage those that meet the selection criteria to apply for this unique opportunity. Complementing the scientific programme we will also have handson training sessions for robotic assisted surgery. These sessions are always very popular but remember places are limited. Aside from its goal to provide closer professional links among Europe’s urological cancer experts, the ESOU also aims to help sustain the gains in urological research, education and training. Join us in Munich for yet another exciting ESOU event! Open radical prostatectomy: H. Lepor, New York (US) Laparoscopic radical prostatectomy: M. Colombel, Lyon (FR) Robotic radical prostatectomy: B. Rocco, Milan (IT) 08.30 - 08.40 Welcome A. Heidenreich, Aachen (DE) M. Brausi, Modena (IT) 08.40 - 09.00 Opening address Personalised medicine to treat cancer – already fact or still fiction? R. Büttner, Cologne (DE) 12.40 – 12.55 Discussion Prostate cancer I: Low Risk PCA and active surveillance Chairs: M. Brausi, Modena (IT) A. Heidenreich, Aachen (DE) 14.00 – 16.00 Renal cancer: Localised and locally advanced Chairs: D. Jacqmin, Strasbourg (FR) H. Özen, Ankara (TR) Prostate Biopsy 2014: TRUS, MRI, TRUS-MRI fusion via a transrectal or transperineal route? B. Djavan, Vienna (AT) 14.00 – 14.20 Management of the small renal mass – reliability of renal biopsy A. Volpe, Novara (IT) 09.00 - 12.55 09.00 - 09.20 12.55 – 14.00 Lunch 14.20 – 14.40 Discussion 09.20 – 09.30 Discussion 09.30 – 09.45 Molecular markers in the decisionmaking process of active surveillance versus active treatment in low risk PCA – are they ready to be used? J. W. Moul, Durham (USA) 09.45 – 09.55 Discussion 09.55 – 10.10 Can multiparametric MRI alone identify low risk PCA? M. Emberton, London (GB) 10.10 – 10.20 Discussion 10.20 – 10.35 Follow-up of patients under active surveillance: rebiopsy versus mpMRI J. Hugosson, Gothenburg (SE) 10.35 – 10.45 Discussion 10.45 – 11.00 Coffee break 11.00 – 11.40 DEBATE: Phase to phase comparison of PIVOT and SPCG-4 PIVOT trial: G. Andriole, St. Louis (US) SPCG-4 trial: J. Hugosson, Gothenburg (SE) 15 minutes each, 5 minutes rebuttal = 40 minutes 11.40 – 12.40 Radical prostatectomy in low/ intermediate risk prostate cancer – how to achieve maximum cancer control and best functional outcome Moderators: M. Emberton, London (GB) Y. Fradet, Quebec (CA) 6 European Urology Today Ileal conduit H. Abol-Enein, Mansora (EG) 17.00 – 18.00 Urothelial and bladder cancer II Chairs: W. Artibani, Verona (IT) Y. Fradet, Quebec (CA) 17.00 – 17.15 Long-term follow-up of orthotopic neobladder in men: Oncological and functional outcome G. Thalmann, Berne (CH) 17.15 – 17.30 Pathology and management of non urothelial bladder cancer Y. Fradet, Quebec (CA) 17.30 – 18.05 Challenging cases of upper urothelial cancer: Panel discussion Moderator: YAU representative Panel: H. Abol-Enein, Mansoura (EG) Y. Fradet, Quebec (CA) A. Stenzl, Tubingen (DE) G. Thalmann, Berne (CH) Saturday, 17 January 08.30 – 10.20 Prostate cancer II: Localised, high risk Chairs: W. Artibani, Verona (IT) M. Colombel, Lyon (FR) 08.30 – 09.10 Debate: Radical prostatectomy leads to lower mortality rates than radiotherapy D. P. Dearnaley, London (GB) P. Sooriakumaran, Oxford (GB) Scientific Programme Friday, 16 January 16.30 – 17.00 Coffee break 14.40 – 15.10 Organ sparing surgery in central tumours – is it feasible? (videos) Open partial nephrectomy: H. Van Poppel, Leuven (BE) Laparoscopic partial nephrectomy: J. Rassweiler, Heilbronn (DE) Robotic-assisted partial nephrectomy: M. Roupret, Paris (FR) 15.10 – 15.20 Discussion 15.20 – 15.35 Management of local recurrences following radical/partial nephrectomy D. Jacqmin, Strasbourg (FR) 15.35 – 15.45 Discussion 15.45 – 16.00 Achievements from the Corona database S. Brookmann-May, Regensburg (DE) 16.00 – 16.30 Urothelial cancer I: Multimodality approach of bladder cancer Chairs: A. Govorov, Moscow (RU) A. Heidenreich, Aachen (DE) Interdisciplinary Tumour Board – multimodality approach in reality Urology: D. Pfister, Aachen (DE) Radiation oncology: M. Pinkawa, Aachen (DE) Oncology: S. Wilop, Aachen (DE) Radiology: C. Kuhl, Aachen (DE) Pathology: R. Knüchel-Clarke, Aachen (DE) 09.10 – 09.40 Debate: Adjuvant radiation therapy following radical prostatectomy – do we still need it? Pro: M. Bolla, Grenoble (FR) Contra: W. Artibani, Verona (IT) 09.40 – 10.10 Debate: the role of choline/PSMA – PET/ CT in relapsing prostate cancer following local treatment Pro: A. Briganti, Milan (IT) Contra: J. W. Moul, Duke (US) 10.10 – 10.20 Discussion 10.20 – 11.20 Testicular cancer Chairs: H. Ozen, Ankara (TR) YAU Member 10.20 – 10.35 Active surveillance in clinical stage I testis cancer: the new standard? T. Tandstad, Trondheim (NO) 10.35 – 10.50 Long-term toxicity following systemic treatment: what to expect, how to monitor patients? S. Gillessen, St. Gallen (CH) 10.50 – 11.05 Postchemotherapy RPLND – tricks of the trade (video and presentation) A. Heidenreich, Aachen (DE) Orthotopic neobladder, open surgery A. Stenzl, Tübingen (DE) Robotic assisted orthotopic neobladder C.M. Annerstedt , Copenhagen (DK) 14.00 – 16.00 STEPS (Session To Evaluate Progress) programme (closed programme: participation by invitation only) Led by Prof. M. Brausi, Modena (IT) Sunday, 18 January 09.00 – 10.10 Management of postoperative functional complications following radical surgery in the small pelvis Chairs: J. Hugosson, Gothenburg (SE) F. Montorsi, Milan (IT) 09.00 – 09.20 Management of intraoperative complications H. Abol-Enein, Mansoura (EG) 09.20 – 09.40 Evaluation and management of erectile dysfunction (including videos) F. Montorsi, Milan (IT) 09.40 – 10.00 Evaluation and management of urinary incontinence (including videos) R. Bauer, Munich (DE) 10.00 - 10.10 Discussion 10.10 – 11.25 The Best of Uro-Oncology in 2014 – ESOU Journal Club Chairs: B. Rocco, Milan (IT) A. Stenzl, Tübingen (DE) 10.10 - 10.25 Kidney cancer TBC 10.25 - 10.40 Bladder Cancer TBC 10.40 - 10.55 Testis Cancer TBC 10.55 - 11.10 Prostate Cancer, localised and locally advanced TBC 11.10 - 11.25 Discussion 11.25 – 11.55 Coffee break 11.55 – 12.15 Award Ceremony 12.15 – 13.00 Prostate Cancer III: Metastatic and castration resistant Chairs: G. Thalmann, Berne (CH) S. Gillessen, St. Gallen (CH) 12.15 – 12.30 Are there new concepts in first-line treatment of metastatic prostate cancer? TBC 11.05 – 11.20 Discussion 11.20 – 11.50 Coffee break 11.50 – 13.50 Urothelial cancer III: Muscle invasive and advanced disease Chairs: Y. Fradet, Quebec (CA) A. Stenzl, Tübingen (DE) 11.50 – 12.20 Debate: Radical cystectomy and extended pelvic lymphadenectomy: roboticassisted versus open surgery Pro Open: M. Brausi, Modena (IT) Pro Robotic: P. Wiklund, Stockholm (SE) 12.20 – 13.50 How to avoid significant complications of urinary diversion (video and discussion) 12.30 - 12.45 Sequencing of medical therapy in CRPC – algorithm for clinical routine S. Gillessen, St. Gallen (CH) 12.45 – 13.00 Options of palliative surgery in symptomatic CRPC D. Pfister, Aachen (DE) 13.00 – 13.15 Discussion 13.15 Close of the ESOU meeting A. Heidenreich, Aachen (GER) M. Brausi, Modena (IT) Join the conversation at #ESOU15 Register now at http://esou.uroweb.org Deadline: 13 January 2015 October/December 2014 MADRID 20-24 March 2015 30th Anniversary Congress Sharing knowledge - Raising the level of urological care Controversies and key issues in Madrid congress Optimising your participation in EAU15 Prof. Morgan Rouprêt (FR) Controversies in urology, trends and new prospects in treatment will be highlighted in the plenary and thematic sessions, live surgeries, abstract presentations, Joint and Section Meetings that will be presented during the five-day 30th Anniversary EAU Congress in Madrid. Sessions, 10 Section Meetings and 11 joint EAU meetings with national and regional societies, not to mention the long list of poster and video presentations plus courses organised by the European School of Urology (ESU), among other activities, will require congress participants to select and prioritise their own interests. “The Scientific Congress Office (SCO) decided to introduce a bit more of controversies during the plenary sessions especially regarding hot topics such as the debate around robotics becoming a new standard or the current limits of partial nephrectomy, said Prof. Morgan Roupret (FR), member of the committee which is responsible for preparing the Scientific Programme. Roupret provided some tips: “From a personal perspective, it would be interesting to follow the discussions on BPH and surgical laser therapy, chemotherapy in treating urothelial carcinomas, robotics in prostate surgery and its potential use for lymphadenectomy, key findings from basic research in polymorphism from kidney and prostate cancer, and insights from molecular mechanisms in bladder disability in neurogenic patients.” With the 30th anniversary and expectations of a bigger attendance in Madrid, the SCO has carefully selected prime topics and salient issues that address the core of urological practice, research challenges and the impact of emerging technologies on medical treatment strategies. A line-up of four Plenary Sessions, 19 Thematic New findings from Magnetic Resonance Imaging and its usefulness in the diagnosis (and staging) of prostate cancer and ability to provide very targeted, accurate and a limited number of biopsies is another topic that will draw audience interest. For participants tracking research breakthroughs, Roupret mentioned findings on PDL1 for bladder cancer, new androgen deprivation and sequential treatment for prostate cancer, chemosensitivity of urothelial carcinomas based on histological variants and new insights regarding male sexuality/QoL particularly in diabetic patients. Responding to congress participants’ feedback, the SCO has also made adjustments in the programme such as extending the Thematic Sessions to 90 minutes to have more debate and input regarding specific urological topics. Abstract sessions will also be complemented with succinct summaries from the session chairmen. Regarding social media. Roupret encouraged participants to use platforms such as Twitter. “With Twitter one has the unique opportunity to be in a room, while having the capability to monitor what is going on elsewhere, and maybe change rooms during simultaneous sessions. Twitter is one of the best options if one wants to be fully involved and reactive,” he said. Tips on how to optimise your Scientific Programme coverage #EAU15 • Prepare for the congress in advance by looking carefully at the programme • Attend the highlight session early in the morning to have an overview of the best scientific data that will be presented • Stay until Tuesday and attend the souvenir session with all highlights of the EAU15 congress • Download the EAU15 Congress App a few weeks before the congress on your smartphone or tablet and build your own personal agenda or meeting planner • Use social media such as Twitter to monitor topics that are generating extra interest Morning sessions usually have intense discussions and debates that can prompt insights and fresh ideas Important dates Check out the new ew at programme overvi Congress participants are recommended to avail of the advantages in completing their registration ahead of the closing dates. Please mark the following important dates into your agenda! rg 015.o www.eaumadrid2 Early fee registration deadline: 12 January 2015 Late fee registration deadline: 9 February 2015 Live Surgery: prospects in minimal invasive techniques Reviewers to screen 4,272 submitted abstracts for Madrid Monday programme for live surgical procedures Many studies explore uro-oncology Unlike in previous annual congresses when live surgical procedures are held on a Saturday, the Live Surgery programme in Madrid will be presented on Monday, 23 March. A total of 4,272 abstracts (including 297 video abstracts) were submitted to the 30th Anniversary EAU Congress to be held in Madrid, Spain, or 253 more than the total abstracts submitted to the 2014 congress in Stockholm. To be organised by the EAU Section of UroTechnology (ESUT), in cooperation with the EAU Robotic Urology Section (ERUS) and the EAU Section of Urolithiasis (EULIS), the programme will start right after Plenary Session 3, from 11.15 until 17.30. Details of the programme are still under wraps with the three section offices still finalising the list of participants and procedures to be shown during the day-long meeting. All procedures comply with the strict regulations set forth in the EAU Policy on Live Surgery. The policy has been approved by the EAU Live Surgery Committee (ELSC) to ensure patient safety, and is considered a pioneering guideline of ethical requirements for live surgeries. ESUT has led the live surgery programme with the aim to demonstrate an actual overview of the prospects, challenges, best practices and technical requirements in new minimally invasive techniques in urology. In previous congresses the surgical techniques ranged from robot-assisted procedures, laparoscopy, robotic flexible ureteroscopy, or a combination of novel techniques that have not yet been adopted on a wide scale. During the 2014 congress in Stockholm, among the procedures that were shown were the use of 3D-HD-videotechnology for laparoscopy, miniaturised instruments for laparoscopic and endourologic procedures and image-guided endoscopic procedures. Commentary and questions from the audience also complemented the sessions. The ESUT surgeons and their collaborators from the ERUS and ESUI are internationally renowned experts who will serve as lead surgeons or moderators during the live sessions. From the participating hospital or expert centre, the live surgery will be transmitted in real time via high-definition and 3D quality video to a splitscreen that will allow the audience in the auditorium to closely follow all surgical steps. This year 278 reviewers will screen the 3,975 poster abstracts submitted, a record number for the annual congress. The reviewers will select at least 1,000 abstracts for presentation in Madrid, highlighting the most innovative and thought provoking. again actively participated this year with an even higher number of abstracts. Reviewers, however, will screen all submissions in a “blind review” process focusing mainly on the significance of the insights, the practical impact of the study and the innovations introduced or being pursued by researchers, among other considerations. Prostate cancer treatment garnered the most interest from researchers with 273 abstracts investigating a range of treatment and diagnostic issues. Surgical management of renal tumours was the topic in 195 abstracts, while 172 submissions focused on the surgical treatment of urothelial tumours. The abstract submissions came from 81 countries from all over the world, with mainland Europe, the Americas, Asia and the Middle East among the most active regions. Abstracts actually presented during the congress are eligible for the prizes that will be granted to the best in two main categories such as oncology, non-oncology, and abstracts by residents and for the three best video abstracts. Similar to previous years, researchers in Europe accounted for many of the submissions, with Italy and Germany the most active in terms of submitting their studies for critical review. Asian countries such as Japan and South Korea have also increasingly expanded their participation in recent years, and The review will take place the whole month of December 2014 and the accepted abstracts will be made available on-line for EAU members one month before the congress opens in Madrid. General users will have access as of 20 March via the EAU Resource Center. EAU congresses and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations www.eaumadrid2015.org October/December 2014 European Association European Urology Today 7 of Urology EUREP2014 12th European Urology Residents Education Programme 5-10 September 2014, Prague, Czech Republic Enthusiasm and opportunities at the 12th EUREP Participants and faculty commend comprehensive programme With more than a decade in the frontline of educating and training young urologists, the 12th European Urology Residents Education Programme (EUREP) this year received commendations from participants and faculty members for its comprehensive programme and achievement to link veteran urologists with their junior colleagues. Held from 5 to 10 September this year in Prague, Czech Republic, this year’s edition gathered 360 participants from 44 countries. Twenty faculty members from across Europe led the five teaching modules, together with experienced mentors for the 10 hands-on training (HoT) sessions that is part of EUREP’s core programme. The modules cover the breadth of urology including uro-oncology, prostate cancer and BPH, andrology, stones and upper tract endourology, functional urology, and paediatric urology, trauma and infection. “The EUREP is known among young residents for its inclusive approach, not only in the education programme that emphasises practical insights with sound theory, but also in its aim to foster professional links among young urologists,” according to the organisers. With Profs. Hein Van Poppel (BE) and Joan Palou (ES) as course directors, the annual programme is on its second decade of providing both practical and theoretical orientation to the scope of urology and the challenges young doctors may encounter in actual practice. “The success of the EUREP programme really depends on the interaction between the faculty and the residents,” said Mr. Jay Khastgir (UK) who joined the EUREP faculty for the first time this year. Khastgir noted the friendly atmosphere the programme is known for and said that this obviously prompted young urologists to freely discuss with and inquire from the faculty and experienced tutors. In the HoT sessions, where 15 laparoscopy stations, 4 TUR and 3 URS were available, the one-on-one mentored guidance was much appreciated by all participants. “At the hands-on training sessions, it was remarkable not only to have the time to improve your skills but also to learn tips from experienced This year’s ‘PERUE’ residents, part of the 360 residents from 44 countries mentors,” said Dr. Katherine Henriquez from Panama (See her full article on these pages). “HoT is a winning and solid format, thanks to the hard work by Ben (Van Cleynenbreugel) and the support of Olympus. Everything went smoothly this year just like in previous years. Our aim is now to bring the EUREP hands-on training to the next level and this goal will certainly require a lot of work from all those involved,” said Dr. Domenico Veneziano (US), who succeeds Ben as coordinator of the HOT programme. E-BLUS exams were also offered this year, allowing EUREP participants to further hone their laparoscopy skills and take it to the next level. And following EUREP’s social tradition, this year’s batch has to formulate a name for their group, which often reflects the casual if not bawdy humour of the residents. Submitted by Dr. M. Sochaj, “PERUE” won the selection, the acronym for ‘Powerful Experience of Rapid Urological Education” and actually ‘EUREP’ spelled backwards. Honing surgical, medical skills in a friendly environment Dynamic faculty-residents discussions spur faster learning process Mr. Jay Khastgir Morriston Hospital Dept. of Urology Swansea (UK) [email protected] The EUREP is an excellent opportunity for urology residents to update themselves in all the key areas of urology in a six-day course, a programme annually held in Prague, the Czech Republic, which is its permanent venue. The delegates rotate through five modules which are designed as a series of interactive lectures and discussions that address a specific area of urology each day. This provides a comprehensive update of all the key areas of urological practice. However, the talks are not mere lectures or updates one would listen to hear at scientific sessions of meetings. Instead, as an active teaching programme, the discussions are focussed on being interactive, which fosters learning by direct involvement of the audience. In addition there are excellent hands-on training (HOT) sessions. The teaching is delivered by a carefully selected faculty from several centres of excellence, which effectively brings together a large resource of experience and knowledge that urology trainees can tap into. There is a social element to the EUREP as well which enables professional 8 European Urology Today networking. Although the obvious benefits of this social interaction may not be immediately evident to a resident, this will certainly become apparent in the long-term. I am not aware of the existence of a comparable course for urology residents elsewhere, and it’s a testament to the EUREP’s success and reputation that the programme is now being emulated in some countries outside Europe. Preparing for EUREP Held since 2003, the EUREP is now in its second decade. Although an ever increasing number of residents apply each year, I would like to see it become a course that all residents can attend. I sincerely believe that those who did not attend during their training have missed a valuable opportunity to interact with, and learn from other residents and an excellent faculty of experts. Consequently if you haven’t attended the EUREP as yet, apply for it now! To get the most out of the EUREP, residents should review as many of the scheduled topics as possible in advance, as this will lead to more insightful discussions, reinforcing the participants’ current knowledge and help clarify areas of uncertainty by engaging in one-to-one discussions. The slides from the previous year’s presentations are available online and these provide a framework for the areas to be covered. The success of the EUREP programme derives from the interaction between the faculty and the residents, and although this is already superb it is an area which we should continually try to improve. There are several means of achieving this and one way is to encourage residents to bring examples of difficult clinical cases from their own practice for discussion with the faculty, both at the formal sessions as well as over lunch or coffee. The ability to apply the taught information to their own real-life practice will foster deep and long-term learning. It was clear to me that the friendly and informal approach of the faculty clearly helped many residents realise that no question was too basic to bring up for discussion, and this helped them overcome any reservations they might have had, enabling them to freely discuss difficult issues. Functional urology Regarding functional urology which I enjoyed being a part of the faculty for, I found residents enthusiastic and eager to learn as much as possible within the time allocated to the module, and I was posed interesting questions over coffee and lunch every day. It is common for some residents to lack confidence when dealing with various aspects of functional urology. This is because often the diagnosis of various functional conditions poses challenges which require a logical approach not too different to that required for solving a puzzle. From the discussions I had with several residents, topics such as the role and interpretation of urodynamics, the rationale for the choice of management options for stress incontinence and prolapse and the management of chronic pelvic pain are common grey areas of uncertaintyconsequently trainees were grateful for the opportunity to discuss such topics on a one-to-one basis. This probably reflects the inspiring teaching by my colleagues as well as a realisation that the subject requires analytical minds and a very different approach than other aspects of urology. Elevator pitch Residents attending the EUREP have already chosen their career path and consequently I don’t see them in need of persuasion or so-called ‘elevator pitch’. All of us who practise urology are aware that this very interesting surgical speciality involves the diagnosis and management of a vast range of pathology ranging from various common and uncommon cancers, functional and neurological disorders, and so much more. The rapid expansion in evidence base that underpins our knowledge have now made it impossible for any individual to know all the various aspects of urology in great depth, which gives trainees the freedom to choose from a wide range of subjects to subspecialise in or to remain proficient in, which includes core aspects of urology. The use of ever-advancing developments in technology keeps this speciality quite literally at the cutting edge of medicine and makes it both exciting and interesting. In many countries the expanding ageing population will guarantee that urologists will be kept busy. Urology is well recognised as a ‘family friendly’ surgical speciality which allows improved work-life balance, and this has attracted more female residents to the profession in recent years. Most importantly, the almost universal sense of humour that urologists I certainly do think there was an increased interest in seem to possess guarantees a good working functional urology among residents during the EUREP. environment in which to pursue a surgical career. October/December 2014 EUREP 2014: An investment in the future of urology Efficient organisation impresses young urologist from Panama Dr. Katherine Henriquez Urology resident Metropolitan Hospital Dr. Arnulfo Arias Madrid Panama City (PA) [email protected] I first heard about EUREP a year ago from fellow urology residents during my clinical visit at Fundació Puigvert in Barcelona. Although they recommended it as a useful tool for a review of urology with an excellent faculty, I consider its value as a programme that provides opportunities particularly for residents who are training outside Europe. I submitted my application eight months prior to the programme, paying close attention to the requirements for non-European residents and taking into account that applications are screened for the limited slots. Thus, when the acceptance letter came, I was thrilled for having the privilege to participate as a resident representative of Latin America. The organisers were efficient, quickly responding to my queries about the registration and details of the event. Study materials were accessible two months before the course, and a schedule for the hands-on training and European Basic Laparoscopic Urological Skills were provided. With the efficient logistical information, participants can prepare well ahead of time such as reviewing the guidelines, studying the content of the lectures, watching videos of endourological techniques and training for the laparoscopic exercises using simulators. Certainly, careful preparation is important when joining this programme. "...the extraordinary team of dedicated professors.." At the hands-on training sessions, it was remarkable not only to have the time to improve your skills but I traveled from Panama to Prague with the best also to learn tips from experienced mentors. The disposition, and has resolved to continue learning and course has certainly succeeded in its aim to enable training. participants to consolidate and expand the knowledge we have acquired during our resident Intensive review training. In Prague, the participants went through six days of intensive review of theory and updates on current We also had the opportunity to exchange views and urology. I have enjoyed the interactive clinical cases, share experiences during the coffee breaks and make the practical application of guidelines, and the new friends at the social programme (BBQ/Karaoke) opportunity to ask questions from expert lecturers. where everyone had a great time singing and dancing. Although the residents came from different countries, we share the same dreams and concerns regarding our future urological practice which, in some ways, united us. I’m thankful to the European Association of Urology, the European School of Urology and the extraordinary team of dedicated professors who have shown outstanding work to make this programme a success. Undoubtedly, the EUREP as a continuing medical education programme is a worthwhile investment with lasting gains that transcend cultural barriers. Bringing resident training to another level Training by experts mentors and unique social camaraderie Dr. Anthony KallasChémaly Department of Urology Hôtel-Dieu de France Hospital Beirut (LB} anthony_chemaly@ yahoo.com I first heard about EUREP from a colleague who participated in the programme and I was encouraged to apply for this year. I continually invest in my learning and education by reading articles in scientific journals such as the European Urology, or by assessing my knowledge in competition inspired me to improve my skills, enabling me to win the first prize. the MCQs and getting EU-ACME credits. I consider the EUREP as another criteria which would offer me some benefits, and I was therefore delighted when I received an e-mail confirming my admission to the EUREP. The EUREP courses we attended were led by well-known doctors and they were all very well organized and structured in such a way that held our interest and enthusiastic participation. It was a pleasure to discuss clinical issues with the faculty due to their insights and helpful tips. Practising laparoscopy at a HoT session EUREP is certainly a great opportunity to meet urology residents from all over the world. It was interesting to discover the differences and challenges we encounter in both medical and surgical managements. For my improvement and training, I welcome and can see the benefits of new ideas. In the social programme, the karaoke night was certainly unique and special, a fitting occasion to even get to know each other better. Another beneficial feature of the course discussions was the opportunity to debate or discuss in detail about the cases during the coffee breaks, since the participants are in a more informal and relaxed setting, making the learning process less intimidating. Regarding the hands-on training (HoT) sessions, I learned new tips and tricks in laparoscopy and ureterorenoscopy. These sessions helped me a lot to prepare for the E-BLUS exam which was also held during the EUREP. Moreover, the Olympus endoscopic For those who are interested, I can also give the same recommendation and encouragement to urology residents to participate in the EUREP, which to me is one of the best opportunities for young residents to improve their skills and bring their training to another level. An “Aussie” perspective on EUREP Well-structured programme impresses USANZ representative Deborah Klein Education and Training Manager Urological Society of Australia and New Zealand (USANZ) education@ usanz.org.au I recently attended the 12th EUREP as a representative of the Urological Society of Australia and New Zealand (USANZ). The governing training body (the Board of Urology) for urology residents in Australia and New Zealand was interested in gaining a detailed understanding of EUREP given its status in the European education and training arena. In particular, the Board of Urology was keen to October/December 2014 improve the learning experiences for USANZ trainees by benchmarking the USANZ Trainee Week Program (an intensive five-day educational programme for urology residents) with EUREP. Another aim was to establish an open exchange of ideas and practices for the benefit of both USANZ and the EAU. number of delegates, it is clear that EUREP provides an extremely worthwhile educational and social experience for those who are fortunate to attend. Their diligent attendance and participation at each session (even after the late night karaoke party) is to be commended. I would like to express my sincere gratitude to Prof. Joan Palou (Chair, ESU), Jacobijn Sedelaar-Maaskant (Manager, ESU), Jacqui McGrath (Congress Consultants) and the EUREP faculty for the wonderful hospitality afforded to me during my stay in Prague. It was an invaluable experience to observe all facets of the programme, including the logistics, methods of content delivery and methods for facilitating participant interaction. I was also particularly impressed with the dedication (and stamina!) of the expert faculty. Their ability to repeat presentations in their allocated module five times over the week in a dynamic and engaging manner was admirable. There was clearly a focus on ensuring an optimal educational experience for all participants and at times, modifications were made to PowerPoint presentations or style of delivery based on preliminary feedback from the daily evaluations. New faculty members were also provided with guidance and support from existing faculty members on delivery techniques, sophistication of content, methods of gaining delegate interaction and presentation of clear and concise slides. In my opinion, the programme is well structured and truly provides a comprehensive update and overview of current urological practice with particular reference to the relevant EAU Guidelines. From speaking to a Deborah Klein (R) with EUREP faculty member Vijay Ramani I commend the EAU and, in particular, the European School of Urology for their efforts in establishing EUREP. It is an extremely valuable educational initiative for urology residents and will continue to be a rewarding experience for all involved. European Urology Today 9 EBU Certified Residency Training Programme in Urology Institute Austria Medical University of Graz Landeskrankenhaus Leoben University Hospital Salzburg SMZ Ost - Donauspital Vienna Krankenhaus der Barmhezigen Brüder Vienna Krankenhaus Hietzing Wilhelminenspital der Stadt Wien Belgium Ghent University Hospital Algemeen Ziekenhuis Groeninge in Kortrijk University Hospitals Leuven Croatia University Hospital “Sestre milosrdnice” Zagreb Czech Republic Charles University Hospital Plzen Charles University Hospital Motol General University Hospital and Charles University 1st Faculty of Medicine Prague Estonia North Estonian Medical Centre Tallinn Finland Oulu University Hospital Germany Universitätsklinikum der RWTH Aachen Klinik für Urologie und Kinderurologie Klinikum Bamberg University of Bonn Klinikum Braunschweig Heinrich Heine University Düsseldorf Universitätsklinikum Essen Ev.-Luth. Diakonissenanstalt zu Flensburg University Hospital Frankfurt Klinikum Garmisch-Partenkirchen Justus Liebig-University Giessen Universitätsklinikum Halle (Saale) Asklepios Klinik Barmbek Hamburg Hannover Medical School University Heidelberg SLK Kliniken Heilbronn Urologische Klinik und Poliklinik des Universitätsklinikums Jena Klinikum Kassel GmbH Universitätsklinikum Schleswig-Holstein, Campus Kiel Malteser Krankenhaus St. Josefshospital Krefeld Klinik für Urologie, Klinikum Ludwigsburg Urologische Klinik, Klinikum der Stadt Ludwigshafen gGmbH Klinik für Urologie, Universitätsmedizin Mannheim Technische Universität München Klinikum rechts der Isar University of Regensburg - Caritas St. Josef Medical Centre Julius-Maximilians University Medical Center Würzburg Programme Director City Prof. Dr. K. Pummer Prof. Dr. T. Colombo Prof. Dr. G. Janetschek Dr. M. Rauchenwald Dr. P. Schramek Prof. Dr. H. Pflüger Dr. N. Szabo Graz Leoben Salzburg Vienna Vienna Vienna Vienna Prof. Dr. P. Hoebeke Dr. I. Billiet Prof. H. Van Poppel Ghent Kortrijk Leuven Prof. Dr. Davor Trnski Zagreb Assoc. Prof. M. Hora Prof. M. Babjuk Plzen Prague Prof. T. Hanuš Prague Dr. L. Kukk Tallinn Dr. P. Hellström Oulu Prof. Dr. A. Heidenreich Dr. K. Weingärtner Prof. Dr. S.C. Müller Prof. P. Hammerer Prof. Dr. P. Albers Prof. H. Rübben Prof. Dr. T. Loch Prof. A. Haferkamp Prof. Dr. H. Leyh Prof. W. Weidner Prof. P. Fornara Prof. Dr. A. Gross Prof. Dr. M.A. Kuczyk Prof. Dr. M. Hohenfellner Prof. Dr. J. Rassweiler Prof. Dr. M.-O. Grimm Prof. Dr. B.G. Volkmer Prof. K.P. Jünemann Dr. J. Westphal Dr. Med. A. Jurczok Prof. Dr. M. Müller Prof. Dr. M.S. Michel Prof. Dr. J.E. Gschwend Prof. Dr. W. F. Wieland Prof. Dr. H. Riedmiller Aachen Bamberg Bonn Braunschweig Düsseldorf Essen Flensburg Frankfurt am Main Garmisch-Partenkirchen Giessen Halle Hamburg Hannover Heidelberg Heilbronn Jena Kassel Kiel Krefeld Ludwigsburg Ludwigshafen Mannheim München Regensburg Würzburg Institute Greece Sismanoglio Hospital Athens University of Crete Hungary Semmelweis University Budapest Italy General Hospital of Bolzano Malta Mater Dei Hospital The Netherlands Academisch Medisch Centrum Amsterdam VU University Medical Centre Amsterdam Norway Sørlandet Sykehus HF Kristiansand/Arendal Poland Collegium Medicum Bydgoszcz Holy Cross Cancer Centre Kielce University Hospital in Kraków European Health Centre Otwock Pomeranian Medical University Szczecin Specjalistyczny Szpital Miejski im. M. Kopernika Torun Interdisciplinary Hospital Miedzylesie Warsaw Medical University of Warsaw Portugal Coimbra University Hospital Spain Vall D'Hebron University Hospital Barcelona Hospital del Mar (Parc de Salut Mar) Barcelona Fundació Puigvert Barcelona La Paz University Hospital Madrid Cliníca Universidad de Navarra in Pamplona Sweden Urologiska Kliniken Universitetssjukhuset Örebro Switzerland University of Berne Kantonsspital St. Gallen Kantonsspital Winterthur University Hospital Zürich Turkey Ankara University Medical Faculty Hacettepe University, School of Medicine Ankara Akdeniz University School of Medicine Uludag University in Bursa Istanbul University Faculty of Medicine Programme Director City Prof. C. Deliveliotis Prof. F. Sofras Athens Heraklion Crete Prof. I. Romics Budapest Prof. Dr. A. Pycha Bolzano Dr. K. German Msida Prof. Dr. T. De Reijke Prof. Dr. E. Meuleman Amsterdam Amsterdam Dr. A. Andersen Kristiansand/Arendal Prof. Z. Wolski Prof. P. L. Chłosta Prof. P. L. Chłosta Prof. A. Borówka Prof. A. Sikorski Prof. T. Drewa Dr. A. Antoniewicz Prof. P. Radziszewski Bydgoszcz Kielce Kraków Otwock Szczecin Torun Warsaw Warsaw Prof. A. Mota Coimbra Dr. J. Planas Morin Barcelona Dr. A. Francés Barcelona Prof. H. Villavicencio Mavrich Barcelona Dr. F.R. de Bethencourt Madrid Dr. J.I.P. Piédrola Pamplona Dr. O. Andrén Örebro Prof. Dr. G. N. Thalmann Prof. Dr. H.-P. Schmid Prof. Dr. H. John Prof. T. Sulser Berne St. Gallen Winterthur Zürich Prof. M.Y. Bedük Prof. H. Özen Prof. Dr. S.E. Guntekin Dr. Y. Kordan Prof. Dr. N. Aras Ankara Ankara Antalya Bursa Istanbul EBU Certified Sub-Speciality Centres Programme Director Prof. H. Van Poppel Prof. D. De Ridder Mr. J. Reynard Prof. J. De La Rosette Dr. C. Wagner Institute University Hospital Leuven (Belgium) University Hospital Leuven (Belgium) Oxford University (United Kingdom) Academisch Medisch Centrum Amsterdam (The Netherlands) St. Antonius Hospital Gronau (Germany) Sub-Specialty Oncology (Prostate, Kidney, Bladder) Female & Reconstructive Urology Stones Treatment Stones Treatment & BPH Prostate Cancer Vall d’Hebrón University Hospital Leading healthcare centre gains EBU certification Dr. Jacques Planas Morin Vall d'Hebrón University Hospital Dept. of Urology Barcelona (ES) One of the main goals of the urology residency is to educate residents for them to independently provide, at the end of their training, comprehensive and expert care to patients suffering from adult and paediatric urological diseases. In addition, the programme provides the opportunity for residents to engage in research and teaching activities giving them a foundation in these areas should they wish to pursue a career in academic urology. [email protected] Vall d’Hebrón University Hospital, located at the foot of the Collserola Hills in Barcelona’s northern district, was founded in 1955. Today, it is the largest healthcare, teaching and research complex in Catalunya and one of the most important in Spain. To achieve these aims, the full and part-time faculty are committed to developing an organised programme of diverse clinical activities, a rigorous and comprehensive conference schedule, guidance and support in clinical and laboratory research activities, and supervision commensurate with the resident’s level of ability in clinical patient care. With over 1,100 beds, it is a multispecialty academic medical centre that integrates clinical and hospital care with research and education, working together with the Universitat Autònoma de Barcelona, which makes it one of the leading academic institutions in Spain. All residents may keep a logbook of surgical and scientific activities. The logbook is presented to the National Board of Specialities every year. Evaluations (in which theoretical and technical aspects are included) are fulfilled by the residency programme co-directors after each resident rotation. The Hospital Vall d’Hebrón Urology Department has between 30 and 40 beds with a professional staff of 14 physicians representing all subspecialties of urology. Over 2,000 surgical procedures, 100 kidney transplants and 29,500 visits in the outpatient department are performed annually. The Urology Department covers the entire spectrum of the speciality with an emphasis on uro-oncology and kidney transplantation. Sub-speciality areas such as BPH (laser surgery), Urodynamics and Female Urology, Urethra and Reconstructive Surgery, Urolithiasis, Andrology, Laparoscopy and Robotic Surgery are led by experienced staff members. The Urology Department chairman, the Hospital Vall d’Hebrón Teaching Programme Director and the Residency Programme co-directors meet once a year to review the evaluations and individually assess the progress of each resident. If the recommendation is unanimous, a positive decision is taken and the resident may continue his residency programme. Resident Training Programme in Urology The Urology Department is nationally accredited for five years of clinical training. Two residents are appointed each year, and eight residents are currently in the programme. EBU Certified Centres 10 European Urology Today Residents may attend different weekly conferences that are held in the Urology Department. The following are the various types of conferences: • Case conference: Cases refer to patients that are scheduled to undergo surgery in the following week. This conference is designed to prepare residents for the oral board examination, provide them the experience in presenting cases in an organised manner, and enable them to use an efficient approach in managing clinical problems; • Renal transplantation conference: In cooperation with Nephrology Department, this conference is organized for a review of the medical history of Full staff of the Urology department of the Vall d'Hebrón University Hospital patients who are waitlisted for renal transplantation; • Journal club: Key articles from urologic literature are reviewed by the faculty and residents; • Urologic oncology conference: Attended by urology faculty and residents, with members of the Oncology, Radiotherapy, Radiology and Pathology Departments. All problematic urologic oncology cases are reviewed and recommendations are made regarding patient management; • Morbidity and mortality conference: Organized by the chief residents who present all complications recorded in the preceding month. Cases are presented and organised by the residents. Research The Urology Department believes strongly in the importance of research in advancing its goals. Located near the Hospital Vall d’Hebrón are the Vall d’Hebrón Institut de Recerca (VHIR) laboratories. The VHIR laboratories are fully equipped for molecular biology, biochemistry, genetics, and cellular biology research and include facilities for tissue culture, animal research, and immunohistochemical and in-situ hybridization facilities. Residents are encouraged to collaborate with investigators, provided they receive adequate mentorship and support and perform quality, hypothesis-based research related to a urologic topic. Residents are also encouraged to take an active part in regional, national and international educational courses and meetings, and the EBU In-Service assessment. Although the EBU exam is not mandatory to certify a Spanish urologist, we believe the assessment is the best way to validate the residents’ knowledge and practical skills based on high European standards. Our fifth-year residents attend the EUREP course in Prague and participate in the written part of the EBU exam. We believe that the EBU certification we recently gained is a mark of excellence and reflects our commitment to maintain high residency training standards. Furthermore, the application itself presents a valuable opportunity to gain external feedback, which is always helpful when continuous improvement is required. October/December 2014 3rd ESUI Meeting: Insights and prospects on urological imaging ESUI holds well-attended meeting in Lisbon, Portugal Dr. Jochen Walz Chairman EAU Section of Urological Imaging (ESUI) Marseille (FR) walzj@ ipc.unicancer.fr Leading European experts active in imaging and image-guided treatment in urology gathered in Lisbon, Portugal on November 13 for the 3rd Meeting of the EAU Section of Urological Imaging (ESUI) which was held in conjunction with the 6th European Multidisciplinary Meeting on Urological Cancers (EMUC). With the aim to provide insights into the latest developments for imaging especially in oncology, the ESUI meeting organised a comprehensive programme. The high attendance was beyond our expectations, proving that combining an imaging and multidisciplinary oncology meeting responds to the needs of physicians active in urological oncology. The programme also complemented the EMUC programme, adding details about the value of imaging in the management of urological malignancies. individualised treatment and better disease classification are among the major aims to address in the future. Outstanding presentations examined thematic blocs that prompted a lively interaction. Participants went home with actionable take-home messages, some of which are mentioned below: Real-time tissue characterisation One of the main observations regarding imaging in urological surgery was the increasing possibility to improve surgery by adding information gained from imaging and by creating what is called augmented reality. Several drugs and optical processing techniques allow real- time information on tissue function and tissue quality improving the safety and outcome of surgery. Moreover, new navigational computer systems and new imaging techniques such as the DYNA-CT allow real-time 3D navigation during surgery of renal masses or prostate cancer, providing major potential for improvements of surgery in the future especially when done by minimal invasive surgical techniques. Image-guided therapy of SRMs This session provided valuable information on how a focal therapy programme could be implemented in a urological department. The European leaders in this field gave tricks and hints to establish such Representatives from the European Society of Urogenital Radiology (ESUR) and the European Association of Nuclear Medicine (EANM) also participated. The overarching theme is that key improvements in future cancer management will be driven by better imaging. Providing better detection, staging, and better follow-up and salvage treatments will lead to improved and individualised treatment strategies. During the EMUC it was also apparent that EAU Section of Urological Imaging (ESUI) Best Poster winner Tobias Maurer (Munich, DE), with Jochen Walz, Manuel Ferreira Coelho and Dragos Georgescu programmes and stressed that these programmes require a multidisciplinary effort between urology and radiology, as well as pathology. This concern reflects the need for multidisciplinary meetings such as the EMUC and ESUI meeting. Joint ESUI and EANM One of the meeting’s highlights was the joint meeting between the European Association of Nuclear Medicine (EANM) and the ESUI. The role of PET/CT in the different urological malignancies was critically assessed and clarified the value and limits of PET/CT in managing individual pathology. There was a clear consensus that such information is essential when using this imaging tool in daily practice. Moreover, a point-counterpoint discussion concluded that the selection of the right patient with the right pathology in the right clinical situation plays a crucial role to improve the value of PET/CT as a diagnostic tool. Best poster award ESUI granted the prize for the best poster to Dr. T. Maurer (Munich, DE) for his study entitled “Preoperative lymph node staging of intermediate and high-risk prostate cancer using whole body integrated PET/MR with 68Gallium.lebelled ligand of prostatespecific membrane antigen.” The number of abstracts submitted increased substantially and the quality can be commended. We are confident that future meetings will attract even more talented urologists to submit their research on urological imaging. Jochen Walz speaking at the Opening Session There was unanimous agreement that standardisation, training and quality control are mandatory and essential before MRI or its alternatives (based on ultrasound) could reliably be used on a large-scale in daily practice outside specialised research centres. Well-designed trials are also necessary to clarify the real role of these tools and their potential in clinical practice. Future developments such as dispersion analysis for contrast enhanced ultrasound and multiparametric ultrasound were presented. The ESUI organised a very informative round-table discussion with the industry to improve communication and interaction between clinicians and engineers. Such meetings are important since the needs of urologists and radiologists can be conveyed Advanced imaging in PCa treatment Another highlight session was the imaging of prostate and joint efforts implemented to improve the quality of care. With the value of round-table discussions, the cancer (PCa), clearly the hottest topic in urological ESUI will organise them as regular feature in future imaging. The session opened with an excellent meetings. point-counterpoint discussion between Hashim Ahmed (UK) and Alberto Briganti (IT) who took With the success and the very positive feedback from pro-con positions regarding focal therapy in PCa. the participants, the 4th ESUI meeting is planned for Currently available imaging tools for PCa such as multiparametric MRI, elastography, contrast enhanced November 12, 2015 again in conjunction with the 7th EMUC in Barcelona. Save the date and we hope to see ultrasound ANNA/C-TRUS and HistoScanning were you in Barcelona! also critically assessed during the same session. In 2015, join us Down Under www.erus15.org ERUS15 12th Meeting of the EAU Robotic Urology Section 15-17 September 2015, Bilbao, Spain Robotic Live Surgery EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations Abstract Submission Deadline: April 3, 2015 Featuring the SIU-ICUD Joint Consultation on Image-Guided Therapy in Urology www.siucongress.org European Association A powerful resource for urologists At your fingertips, anywhere, any time. of Urology October/December 2014 www.siu-academy.org 4133_SIU2015_EUT_Nov_Ad_v02.indd 1 Client: SIU 2014 Description: GLASGOW SIU ACADEMY Docket number: 24-4133 14-10-01 3:25 PM European Urology Today File Size: Trim Size: 100 % 133,4 mm X 194,3 mm 11 Supple prescription rules in oncology drugs in Italy Italian urologists can now prescribe abiraterone Prof. Vincenzo Mirone Secretary General of the Italian Society of Urology University Federico II of Naples Naples (IT) that late-stage prostate cancer was not ‘hormone refractory’ but ‘castration resistant,’ and in fact the tumour was still dependent on testosterone but was able to progress since it could get androgens from elsewhere (perhaps even from the prostate cancer itself). He also reasoned that adrenal insufficiency would not be an issue with abiraterone, since children born with inherited deficiency of CYP17 do not suffer from it. [email protected] Abiraterone acetate represents a new therapeutic weapon in managing men with advanced prostate cancer who became castration-resistant. In 2012 it was made available on the National Health Service and transformed the options available for the 10,000 men each year who are diagnosed with aggressive forms of prostate cancer. Abiraterone was first patented in 1992 by the Institute of Cancer Research of London. Early-stage clinical trials in prostate cancer led by Professor Ian Judson, with pharmacodynamic studies carried out by Dr. Florence Raynaud, showed that abiraterone did hit the correct target and lowered the levels of male hormones. However, early in the drug’s development, concerns were raised about the possible side-effects of blocking CYP17 – in particular about the risk of adrenal insufficiency. The developmental progress was further hampered by a lack of interest in hormone treatments for prostate cancer. Part of the problem lay in the name of late-stage prostate cancer, often referred to as ‘refractory’ disease, and scientists and clinicians would argue that blocking androgen production at a late stage would be ineffective. But the skepticism surrounding the drug was challenged when Professor Johann de Bono joined the ICR in San Antonio, Texas, in 2003. Prof. De Bono recognised the potential of abiraterone as a treatment for men with advanced prostate cancer, and reasoned In 2004 the first phase I study of abiraterone in patients with advanced prostate cancer was run by the ICR and The Royal Marsden. The small study involved 21 men and found that the drug appeared safe in humans and that majority of patients who took it experienced both significant tumour shrinkage and dramatic falls in PSA levels. Significant benefits Less than a year later, the results of a larger phase I/II study were reported. This study of 54 patients confirmed the phase I results, and showed that up to 70% of men responded to abiraterone. These men experienced significant benefits for an average of eight months, with scans showing their tumours decreased in size and their PSA levels dropped substantially. "The ESOU Board updated the current situation ... regarding the prescription of oncological drugs by urologists.." Following these very positive results, the giant US pharmaceutical company Johnson & Johnson agreed to buy Cougar (the society which has the license to abiraterone and owned worldwide exclusive rights to develop and commercialise abiraterone) the royalties for just under £600 million, gaining access to the drug as it progressed through phase III evaluation. In 2010, a pivotal phase III trial showed that patients given abiraterone lived on average 15.8 months longer, compared with 11.2 months for men taking a placebo. This part of abiraterone’s story exemplified how basic molecular studies, followed by collaborations between researchers, doctors and industry, can lead to the successful development of effective drugs that can transform lives. Thanks to this strong clinical trial evidence for the effectiveness of abiraterone, the ICR submitted a new drug application to the US Food and Drug Administration, leading to the approval of abiraterone in the US. Later in 2011, the European Medicines Authority also licensed abiraterone. That opened the door to the drug being made available in the UK, but accessing it on the NHS continued to rely on local decisions by primary care trusts, or access via the government’s new NHS Cancer Drugs Fund. Abiraterone became one of the most requested drugs on the Cancer Drugs Fund, as anticipation grew that it would shortly be accepted by NICE. UK have the same rules wherein urologists cannot prescribe pharmaceutical drugs. In Germany, Holland and Belgium, urologists can prescribe all pharmaceuticals. In Switzerland, new pharmaceuticals for the kidneys and prostate can be prescribed; however, chemotherapy drugs cannot be prescribed. In Turkey, for kidney patients, urologists cannot prescribe pharmaceuticals, while for prostate cases, abi, enzalutamide and cabazitaxel can be prescribed only by oncologists. Taxotere, on the other, can be prescribed by urologists. In Spain and France, urologists can prescribe pharmaceuticals (affirmation from the staff of Sanofi). Urology specialists, having their own walk-in clinics, have a frontline role in diagnosis and are therefore the first to be in contact with uro-oncological patients. At the same time, they have been denied the possibility of establishing a perfectly synergetic route with the oncological specialist due to their inability to prescribe oncological pharmaceuticals by oral means. However, in February 2012, NICE announced its rejection of abiraterone based on the high costs of the drug unless more data are forthcoming or a better price is offered. In May 2012, NICE and Janssen finally reached an agreement over cost, and the drug was made available on the NHS in England, Wales and Northern Ireland. Since then, abiraterone has gained a further licence for the treatment of prostate cancer before chemotherapy, opening up the prospect that it will be made available for even more men. Considering the multidisciplinary rapport that is strictly followed, administrative shortcomings, in some cases, delay the therapeutic course of a management strategy that is surely a disadvantage to the patient who has paid the price for a breakdown in communication. Representatives of the Italian Association of Urology (SIU) and the national regulatory organ AIFA met, and following in-depth discussions, both institutions gathered and examined the requests of urologists. Their goal was to guarantee an improvement in managing patients with prostate tumours. Updating the guidelines The ESOU Board updated the current situation (via the country representations in the board) regarding the prescription of oncological drugs by urologists. The nations represented are Italy, France, the UK, Germany, Russia, Turkey, Switzerland and Sweden. Italy and the Starting last September 2014, when new prescription guidelines were subsequently approved, urologists can now administer oral oncological drugs. Today, with the ability to prescribe abiraterone on the part of urologist specialists, the gap in managing prostate cancer patients has somewhat been filled. Infectious complication in prostate biopsies Alarming rate of Extended Spectrum Beta-Lactamase producing Escherichia coli in TRUS-guided biopsy Prof. Mete Çek Member EAU Working Group on Urological Infections Edirne(TR) [email protected] Co-authors: Zafer Tandogdu, Tommaso Cai, Robert Pickard and Truls Erik Bjerklund Johansen of the EAU Working Group on Urological Infections. Transrectal ultrasound-guided biopsy (TRUS-Bx) of the prostate is a frequently used procedure for the detection of prostate cancer. The main risk of the trans-rectal biopsy technique is infective complications including urinary tract infection (UTI) and bloodstream infection. The rate of these infections after was reported at 5% in the Global Prevalence of Infections in Urology (GPIU) Study1. A number of studies have shown that fluoroquinolone-resistant microorganisms, particularly Escherichia coli (E. coli), are frequently the cause of these infections. More recently the emergence of firstly extended spectrum betalactamase (ESBL) producing microorganisms and, secondly, carbapenem-resistant organisms worldwide is a major concern in this regard. A multi-institutional study from Istanbul, Turkey reported the prevalence of faecal carriage of ESBL positive Escherichia coli in 400 patients undergoing TRUS-Bx2. The investigators also searched for risk factors for intestinal carriage of ESBL in this group of patients, as well as reporting the prevalence of UTI and infective complications following TRUS-Bx of the prostate. EAU Section of Infections in Urology (ESIU) 12 European Urology Today A rectal swab culture performed in all men undergoing biopsy showed that 19% were carriers of ESBL E. coli in the faecal reservoir. The authors noted that this high prevalence is one of the most important problems together with resistance to fluoroquinolones. They found that quinolone/ antibiotic use within the last two months, and DM are risk factors for ESBL-producing Enterobacteriaceae carriage before biopsy. In particular 20% of men had received a treatment course of fluoroquinolones in the previous two months. Despite the isolation of E. coli in the urine of 13% of patients on the third-day after biopsy, only 9% suffered symptomatic UTI and repeat urine culture on the 14th post-biopsy day showed no growth (Table 1). Interestingly, ESBL E. coli carriage was not associated with development of symptomatic UTI in the study group. Still, of the patients with UTI symptoms on the post-biopsy third day, 68% were ESBL-PE carriers. The authors suggested that the findings from their study deserves attention by all those involved in TRUS-Bx and further studies are needed concerning prophylaxis protocols as well as management of patients and TRUS-BX of the prostate. Investigation of the high rate of usage of fluoroquinolones in the community is also required. However, given the limited range of antibiotics that provide bacteriocidal concentrations within the prostate (is) sufficient, there is limited scope to use alternatives to fluoroquinolones for TRUS-Bx prophylaxis. EAU Guidelines on prophylaxis before TRUS-Bx suggest the use of fluoroquinolones, TMP ± SMX, and possibly Metronidazole, leaving targeted prophylaxis as an alternative. Single dose of one of these antibiotics is considered to be effective in low-risk patients. Prolonged course could be considered in high-risk patients3. Individualised prophylaxis approaches may prove to be more efficient and also would be helpful in avoiding unnecessary antibiotic consumption. References 1) Florian M.E. Wagenlehner , Edgar van Oostrum, Peter Tenke et al.: Infective Complications After Prostate Biopsy: Outcome of the Global Prevalence Study of Infections in Urology (GPIU) 2010 and 2011, A Prospective Multinational Multicentre Prostate Biopsy Study Eur Urol 63(2013)521–527. 2) Tigen ET, Tandogdu Z, Ergonul O et al: Outcomes of Fecal Carriage of Extended-spectrum β-Lactamase After Transrectal Ultrasound-guided Biopsy of the Prostate. Urology. 2014 Sep 17. pii: S0090-4295(14)00686-4. doi: 10.1016/j.urology.2014.04.060. [Epub ahead of print] PMID: 25239255). 3) Grabe M, Bartoletti R, Bjerklund-Johansen TE et al: European Association of Urology Guidelines on Urological Infections, 2014. allison@stevepeedenracing. com Take control. Table 1: Results of clinical follow-up of patients undergoing TRUS-Bx of the prostate (modified from Ref. 2) Pre-biopsy fecal cultures 400 patients ESBL producing bacteria 75 patients (19%) Post-biopsy 3rd day follow-up 289 patients Post-biopsy 3rd day urine culture positivity 39 patients (13%) Post-biopsy 3rd day symptomatic UTI 27 patients (9%) Post-biopsy 14th day follow-up 147 patients with no symptomatic UTI or positive urine culture LithAssist ™ SUCTION CONTROL FOR LASER LITHOTRIPSY For more information, contact a representative or [email protected]. MEDICAL www.cookmedical.com © COOK 2014 URO-BEMEAADV-LITHEUT-EN-201401 October/December 2014 EUREP15 13th European Urology Residents Education Programme 4-9 September 2015, Prague, Czech Republic www.eurep15.org Unique and exclusive training opportunity General information Participation and contribution This teaching programme has been developed and created exclusively for all European urological residents. The EUREP provides an almost complete update and overview of modern urological practice presented by a distinguished European faculty. The EUREP is an initiative of the European School of Urology in collaboration with the European Board of Urology. The written part of the FEBU exam (Fellow of the European Board of Urology) will take place at a later date in different cities throughout Europe. Further information will be available on www.ebu.org. Format The format is a full six-day course comprising five modules. Each day is made up of two sessions that last around seven hours. Morning sessions feature state-of-the-art lectures, while afternoon sessions offer interactive case discussions, video, and test-your-knowledge sessions. The hands-on-training sessions will take place around the modules. The training which is sponsored by Olympus helps the participants sharpen their skills and offers hands-on interaction with state-of-the-art equipment. Venue of the EUREP Meeting The EUREP will be organised in Prague, Czech Republic. The venue at the Clarion Congress Hotel provides excellent facilities and the four-star hotel has all the necessary facilities needed for both the scientific programme and social activities. Travel Arrival date: Thursday, 3 September 2015 Departure date: Wednesday, 9 September 2015 after the modules end. EUREP 2015 - Important information for applicants! From 2015 European participants in EUREP will no longer have their travel costs reimbursed. This means that all selected participants must pay for their travel to and from Prague. The EAU/ESU will continue to cover the cost of accommodation for European residents in a shared room as well as the cost of the course (incl. lunches, coffee breaks). Registration information Important dates Online registration opens on 6 January 2015. The selection process will be made after the close of registration on 1 May 2015. A total of 360 participants will be selected. Participants will be notified by email if they have been selected. If selected, the deadline for cancellation is 1 August 2015 after this time a cancellation fee of €500 will be charged. Selection criteria Registrations can only be submitted through the online registration system. The registration will only be considered complete if the registration is accompanied by: • A letter from the head of department indicating the date that the participants training will end • A copy of your passport Additional criteria 1. EAU membership. Priority is given to those who are or become a member before the registration deadline 2. Year of training. Priority is given to residents in their final year of training (i.e. training should be finished before September of the following year based on the information received from the proof of status) 3. It is required to obtain CME credits by completing European Urology multiple choice questions (MCQ’s). For further information please check http://eurep.uroweb.org 4. First come – first served 5. English skills 6. Target per country 7. It is only allowed to attend the EUREP course once For further detailed information regarding the registration rules for the 13th EUREP course we strongly recommend that you visit http://eurep.uroweb.org Registration non-European residents If you are a non-European resident that is interested in taking part in the 13th EUREP course please go to http://eurep.uroweb.org for the rules and regulations regarding participation. Preliminary programme 2015 Module 1 Urological cancer Testis Diagnosis & treatment of stage 1 disease Management of metastatic disease Penile cancer Treatment of primary lesion Management of inguinal lymph nodes Urothelial cancer Non-muscle invasive bladder cancer Diagnosis, staging and risk stratification Management of low, intermediate and high risk disease Muscle invasive bladder cancer Surgical and non-surgical treatment options Neo and adjuvant chemotherapy and the management of metastatic disease Upper urinary tract cancer Renal cancer Diagnosis and management of T1-2 disease Management of locally advanced and metastatic disease Module 2 Prostate cancer and BPH Prostate cancer Screening, early detection and staging Treatment for localised disease Active surveillance, surgical treatment, radiation, focal therapy Locally advanced and metastatic prostate cancer Treatment of castration resistant prostate cancer and new agents BPH Medical treatment BPH BPH: surgical treatment Module 3 Andrology, stones and upper tract endourology Andrology Physiopathology diagnosis and treatment of erectile dysfunction Penile curvature Priapism and metabolic syndrome Male infertility diagnosis and treatment Surgery for male infertility and vasectomy Male hypogonadism Stones Aetiology, management and prophylaxis of urolithiasis ESWL treatment of urolithiasis Percutaneous and open surgery Upper tract endourology Stents in the urinary tract Ureteroscopic stone manipulation Endourology in UPJ obstruction Module 4 Functional urology Essential terminology Initial assessment Fundaments of urodynamics Stress urinary incontinence and pelvic organ prolapse Overactive bladder Reconstruction and diversion Assessing the neuropathic patient General management of the neuropathic patient Post-prostatectomy incontinence Complex issues; pain, fistula and mesh exposure Module 5 Paediatric urology, trauma and infection Additional selection criteria! Please be aware of the additional selection criteria that was introduced in 2014 (see registration information number 3) Paediatric urology Essentials of obstructive uropathy Congenital malformations of the external genitalia Infections Urinary tract infections Trauma Diagnosis and management of kidney, bladder and urethral trauma “If you meet the criteria we would encourage you to register for this opportunity, “ Prof. Palou, course director Hands-on-training workshops Participants can only participate in 1 session Lap plus a TUR or URS. Places for URS and TUR are limited. Sharpening Your Skills: TUR, URS, and Laparoscopy As an essential part of the European Urology Residents Education Programme (EUREP) in Prague, intensive hands-on training will be delivered. This year's programme consists of hands-on interaction with state-of-the-art equipment in laparoscopy, ureteroscopy (URS) and transurethral resection (TUR) -all of which sponsored by Olympus. laparoscopic suturing. Tutors will, of course, gladly adapt tasks for more experienced individuals. Basic techniques will be trained in a dedicated step-by-step programme including intracorporeal suturing depending on individual skill level. The workshop provides the participants with a unique opportunity to train basic techniques with complex training models and under expert supervision. Thanks to the intense tutoring scheme -with a personal tutor The training curriculum for the ureteroscopy per training station- a fast learning effect can be workshop is designed by Prof. Olivier Traxer of Tenon expected. Hospital, Paris. Residents will learn about the proper use of flexible ureteroscopes using a variety of stone The courses in laparoscopy are specifically designed disposables in order to remove kidney stones. for individuals with minimal or no prior experience in The course in transurethral resection of the prostate gives residents the great opportunity to learn more about the basics of high-frequency surgery, the instruments needed, as well as tips and tricks for daily surgery. More information about the different training modules can be found at http://eurep.uroweb.org The hands-on-training workshops are sponsored by an unrestricted educational grant from: Scientific secretariat ESU Office PO Box 30016 6803 AA Arnhem, The Netherlands T +31 (0)26 389 0680 F +31 (0)26 389 0674 [email protected] October/December 2014 European Urology Today 13 Key articles from international medical journals Prof. Oliver Hakenberg Section Editor Rostock (DE) Oliver.Hakenberg@ med.uni-rostock.de Results of a randomised trial in prostate cancer Uncertainties about population screening, the risk of over treatments and concerns about what is the most effective management strategy led in 2001 to the ProtecT trial. This aims to investigate the clinical- and cost-effectiveness of active monitoring, external beam conformal radiotherapy with neoadjuvant androgen suppression and radical prostatectomy for men with PSA-detected clinically localised prostate cancer. The analysis of the primary outcome measure diseasespecific mortality at 10 years will not be available until 2016 but this paper presents the trial design and the initial results of the PSA testing and diagnostic phase. Designed in the late 1990s and opening in October 2001, this phase III trial invited 228,966 men between the age of 50-69 years, to attend for screening. 100,444 (44%) attended their initial appointment and 82,429 had a PSA test. Previous PSA testing results were checked in the medical record but were not an exclusion criterion. Participants with a PSA of at least 3.0 μg/l were invited for digital rectal examination and standardised ten-core transrectal ultrasound guided prostate biopsy. Participants with a PSA of 20 μg/l or more were offered biopsy but excluded from the study because of the high likelihood that they had more advanced cancer. Of the 8566 men with a PSA of 3.0-19.9 μg/l, 7414 underwent biopsies. 2896 men were diagnoses with prostate cancer, 4% of the tested men and 39% of those who had a biopsy. Of these 2417 had clinically localised disease based upon assessment by DRE, and isotope bone scan if the PSA was greater or equal to 10 μg/l or the Gleason score greater or equal to 7. MRI for staging was used at the discretion of the investigator. With the addition of 247 pilot study participants recruited between 1999 and 2001, 2664 men were eligible for the treatment trial and 1643 agreed to be randomly assigned (545 to active monitoring, 545 to radiotherapy and 533 to radical prostatectomy). Median age 62 years with a median PSA of 4.6 μg/l. Gleason score 6 in 1266 (77%) men, 7 in 339 (21%) men and 8-10 in 37 (2%) men. Clinically, T1c in 76% and T2 in 24% of participants. In men assigned active monitoring PSA was measured every 3 months in the first year and twice yearly thereafter. A rise of 50% or more over the previous 12 months triggered repeat PSA within 6-9 weeks and if that remained elevated a repeat biopsy was organised. …ProtecT will provide data for the comparative effectiveness of active monitoring, radical prostatectomy and radiotherapy… In men receiving external beam 3D conformal radiotherapy, neoadjuvant androgen suppression was given for 3-6 months before and concomitant with 74 Gy in 37 fractions. PSA was measured every 6 months for the first years and then annually. Biochemical failure had occurred when PSA was 2 μg/l above the nadir. The majority of men receiving surgery underwent open retropubic radical prostatectomy with bilateral lymphadenectomy if the PSA was 10 μg/l or more or the Gleason score at least 7. PSA was measure every 3 months for the first year, every 6 months for 2 years and then annually. Adjuvant radiotherapy was offered to those men with a positive surgical margin or extracapsular disease. Biochemical recurrence occurred when the PSA reached 0.2 μg/l. As with many studies looking at localised prostate cancer the treatments studied have evolved before the Key articles 14 results are available and although 10-year data might be available fairly shortly we may need longer follow-up still to separate outcomes in this relatively low risk group. Nevertheless, ProtecT will provide data for the comparative effectiveness of active monitoring, radical prostatectomy and radiotherapy, which will be especially significant as other similar trials did not complete randomisation Vira MA, Turkbey B, Fakhoury M, Yaskiv O, Villani R, Ben-Levi E, Rastinehad AR. Source: Active monitoring, radical prostatectomy or radiotherapy for localised prostate cancer: study design and diagnostic and baseline results of the ProtecT randomised phase 3 trial. Lane, JA, Donovan JL, Davis M, Walsh E, Dedman D, Down E, Turner EL, Mason MD, Metcalfe C, Peters TJ, Martin RM, Neal DE, Hamdy FC for the Protec study group. In Europe it is estimated that 92,200 men a year die of prostate cancer despite castrate levels of serum testosterone. Disease progression remains dependent upon androgen receptor (AR) signalling possibly as a consequence of adrenal or intratumoural androgen synthesis, increased AR expression and or constitutive AR activation due to splice variants or activating mutations. Cancer 2014; 120: 2876-82. More antiandrogens on the way in prostate cancer Lancet Oncol 2014; 15: 1109-18. MRI versus risk calculator in predicting significant prostate cancer Following the introduction of PSA testing there has been a steady rise in the detection of clinically insignificant prostate cancer (CaP) and subsequent overtreatment. The Prostate Cancer Prevention Trial risk calculator for high grade disease is a multivariable mathematical model attempting to predict the presence of clinically significant CaP. Recent data suggest multiparametric magnetic resonance imaging (mpMRI) has a high level of sensitivity and a high positive predictive value for identifying CaP. This paper compares the performance of PCPTHG and mpMRI in identifying men at risk of high grade or clinically significant CaP. The analysis used data collected on men enrolled into a phase III trial evaluating MRI/TRUS Fusion-guided prostate biopsy (NCT01566045). Men with an abnormal DRE of PSA level (> 4 ng/ml) underwent mpMRI using a 3-Tesla MRI and an endorectal coil. The images were reviewed by three radiologists who graded all lesions that were suspicious for CaP on a five-point Likert scale. Biopsy of suspicious lesion(s) was performed using a proprietary MRI/transrectal ultrasound fusion-guided prostate biopsy system, after which 12-core biopsy was performed. A genitourinary pathologist reviewed all pathology slides. Because this was a comparison with results from the PCPT, high-grade CaP was defined as a Gleason score > 7, which was used in the development of the PCPTHG. However, exploratory analyses were performed using the Epstein criteria for clinically significant CaP. …mpMRI out performed PCPTHG in predicting clinically significant prostate cancer 175 men met the inclusion criteria and consented to participate in the study. The overall cancer detection rate was 64.6% (113/175) and 47.4% (83/175) had high grade disease. Using the Epstein criteria, 82% (93/113) of men diagnosed with CaP had clinically significant disease. Age, abnormal DRE, PSA, PSA density, prostate size, extraprostatic extension on MRI, apparent diffusion coefficient value, and MRI lesion size were identified as significant predictors of high-grade CaP (all p < 0.05). The individual risk of high-grade CaP was calculated using the PCPTHG which suggested that the incidence should be 20.2% compared with the observed 47.4%. However, the AUC of PCPTHG and mpMRI were similar (0.676 vs. 0.769 p = 0.09). Nevertheless when clinically significant prostate cancer was defined using the Epstein criteria the AUC for mpMRI was 0.812 vs. 0.676 for the PCPTHG (p = 0.008). Prof. Oliver Reich Section editor Munich (DE) ODM-201 is a novel AR inhibitor which along with its major metabolite ORM-15341 has a higher AR-binding affinity than do bicalutamide, enzalutamide and ARN-509. ODM-201 inhibits nuclear translocation of AR in AR-overexpressing cells and significantly inhibits tumour growth in the murine VCaP CRPC xenograft model. Non-clinical data have also shown negligible penetrance of ODM-201 through the blood–brain barrier, thus suggesting a low risk of seizure. ARADES was an open-label, multicenter trial in men with progressive mCRPC. PSA progression was defined as a rising PSA above 2 ng/ml in soft tissue using the modified RECIST criteria or on bone scan by the occurrence of 2 or more new bone lesions. In the nonrandomized phase 1 dose escalation portion 24 men were treated with a daily doses of ODM-201 100 mg b.d. which was increased to 200 mg, 300 mg, 500 mg, 700 mg and 900 mg. Dose escalation was discontinued because a maximum plasma concentration was reached. …ODM-201 had a favourable safety profile and no seizures were noted The phase 2 randomised dose expansion study evaluated cohorts of approximately 35 patients at doses of 100 mg b.d. 200 mg bd and 700 mg b.d. It assessed the proportion of patients with a 50% or greater decrease in serum PSA at 12 weeks. In the phase 2 study patients were stratified by previous exposure to both CYP17 inhibitor and chemotherapy. oliver.reich@med. uni-muenchen.de Previous studies of donor or recipient origin of PTLDs following solid organ transplantation have either been small or with selected patient groups. In this study, tumour origin in a population-based cohort of 93 patients with PTLD following organ transplantation was studied. The tumour origin of PTLD tissue was analyzed by fluorescence in situ hybridization of the sex chromosomes in cases of sex mismatch between donor and recipient (n = 41) or HLA genotyping in cases of identical sex but different HLA type (n = 52). The authors concluded that the vast majority, if not all PTLDs, after solid organ transplantation are of recipient origin With these methods, tumour origin of PTLD could be determined in 67 of the 93 cases. All these 67 PTLDs were of recipient origin. They were found in recipients of kidney (n = 38), liver (n = 12), heart (n = 10) and lung (n = 7). The most common recipient-derived lymphomas were monomorphic B-cell PTLDs (n = 45), monomorphic T cell PTLDs (n = 9), indolent lymphomas (n = 6), and polymorphic PTLD (n = 4). Half of the recipient-derived PTLDs were Epstein-Barr viruspositive. Twelve of the recipient-derived PTLDs were located in the grafts: in four cases exclusively and in eight cases in combination with disseminated disease outside the graft. Tumour origin was indeterminable in 26 cases, probably due to low DNA quality. The authors concluded that the vast majority, if not all PTLDs, after solid organ transplantation are of recipient origin. Source: Donor or recipient origin of posttransplant lymphoproliferative disorders following solid organ transplantation. Kinch A, Cavelier L, Bengtsson M, Baecklund E, Enblad G, Backlin C, Thunberg U, Sundström C, Pauksens K. During the study the most common treatmentemergent adverse events were fatigue or asthenia (15 of 124 (12%) men), hot flushes (6) and decreased appetite (5). At 12 weeks 11(29%) of the patients in the Am J Transplant. 2014 Oct 10 [Epub ahead of print] 100 mg bd group showed a PSA response along with 13 (33%) in the 200 mg b.d. group and 11 (33%) in the 700 mg b.d group. Response was more marked in Chronic allograft nephropathy CYP-17 inhibitor-naïve patients. Findings from this phase 1–2 analysis show that ODM-201 has encouraging antitumour activity in both chemotherapy-naive patients and chemotherapytreated men with metastatic castration-resistant prostate cancer. ODM-201 had a favourable safety profile and no seizures were noted despite the fact that patients with a medical history of seizures were allowed to enter the trial. These results support further investigation of ODM-201 in a larger phase 3 trial in men with castration-resistant prostate cancer. Source: Activity and safety of ODM-201 in patients with progressive castration-resistant prostate cancer (ARADES): an open label phase 1 dose escalation and randomised phase 2 dose expansion trial. Fizazi K, Massard C, Bono P, Jones R, Kataja V, James N, Garcia JA, Protheroe A, Tammela TL, Eliott T, Mattila L, Aspegren J, Vuorela A, Langmuir P, Mustonen, for the ARADES study group. Lancet Oncol 2014; 15: 975-85. PCPTHG calculator has been limited by poor specificity at high sensitivity. In this study, mpMRI out performed PCPTHG in predicting clinically significant prostate Post-transplant cancer. Interestingly, only patients with a suspicious lymphoproliferative disorder is lesion on mpMRI were included and therefore it was not possible to compare the detection of prostate of recipient origin cancer or the grade of cancer between those with and Post-transplant lymphoproliferative disorder (PTLD) is without a suspicious lesion on MRI. a malignancy of lymphocytic origin typically occurring only in recipients of solid organ transplantation. Its Source: Multiparametric magnetic resonance etiology is related to immmunosuppression but imaging outperforms the prostate cancer other than that little is known about the condition and prevention trial risk calculator in predicting clinically significant prostate cancer. Salami SS, its origin. has a specific cause in many cases Chronic allograft nephropathy leads to late loss of graft function. It is clinically common and accepted as almost inevitable. This paper examined the pathology of chronic allograft failure, i.e. the relative impact of specific versus nonspecific chronic histological damage. All 1,197 renal allograft recipients who were transplanted at a single center between 1991 and 2001 were included. All post-transplant renal allograft indication biopsies performed in this cohort during follow-up (mean, 14.5 ± 2.80 years after transplantation) were rescored according to the current histological criteria and associated with death-censored graft outcome. This study conclusively shows that late graft loss is multifactorial In the cohort, 1,365 allograft indication biopsies were performed. Specific diagnoses were present in 69.4% of graft biopsies before graft loss, but 30.6% of grafts did not have specific diagnoses in the last biopsy before graft loss. Only 14.6% of the patients did never have any specific disease diagnosed before graft loss. Extensive interstitial fibrosis and tubular atrophy without a clear cause was identified as the single EAU EU-ACME Office European Urology Today October/December 2014 Prof. Truls Erik Bjerklund Johansen Section editor Oslo (NO) [email protected] cause of graft loss in only 6.9% of the cases. Acute T-cell-mediated rejection and changes suggestive of acute antibody-mediated rejection, diagnosed after the first year post-transplant, were associated independently with graft survival. Transplant glomerulopathy increased over time after transplantation and represented a major risk for graft loss, as well as de novo or recurrent glomerular pathologies and polyomavirus nephropathy. Chronic histological injury was associated with graft outcome, independent of specific diagnoses. This study conclusively shows that late graft loss is multifactorial. However, specific histopathologies are common suggesting that specific treatment is more often indicated. The conclusion must be that repeat biopsies and treatment of concomitant specific nephropathy might prolong graft survival. Source: The histology of kidney transplant failure: A long-term follow-up study. Naesens M, Kuypers DR, De Vusser K, Evenepoel P, Claes K, Bammens B, Meijers B, Sprangers B, Pirenne J, Monbaliu D, Jochmans I, Lerut E. Transplantation, 98(4):427-35, 2014 Is there an evidence-based need for vaginal spheres during pelvic floor muscle training for urinary incontinence? Pelvic floor rehabilitation is the most common first-line treatment for urinary incontinence in females, before corrective surgery indication. This training might be done alone or in combination with other exercises, including electrical stimulation, biofeedback techniques and/or use of vaginal spheres. Vaginal spheres may improve the pelvic floor musculature proprioception and may help the patient to control his voluntary musculature. However, strong level of evidence is not available regarding the real benefit/risks from intravaginal medical devices. This well-designed prospective study shows that performing pelvic floor exercises at home and without supervision is improved by the use of concomitant vaginal spheres In the present randomized controlled trial, authors compared twice daily Kegel exercises, five days a week, over six months, alone (control group) or in combination with vaginal spheres (treatment group). Three Spanish institutions were involved and 70 women enrolled. Inclusion criteria were women of 35-60 years with mainly mild or moderate stress or mixed urinary incontinence, who had delivered vaginally at least once and had not previously performed pelvic floor exercises. No medication interfering with incontinence was allowed. The primary and secondary endpoints were the ICIQ-UI-SF score at the one hand, and the one-hour pad-test, subjective efficacy and tolerance at the other hand. Evaluation visits were planned on Days 7, 30, 90, 180. Analysis between groups showed a statistically significant improvement in amount of urine leakage after three months. Within groups analysis revealed an improvement in frequency and urine leakage since one-month visit in treatment group versus six-month visit in control group. Interestingly, women in the control group did not improve their pad-test over six months whereas a significant improvement was seen in the treatment starting at one month and lasted during the remaining follow-up. Subjective efficacy assessed by investigators and by patients was slightly improved in the treatment group without statistical significance. Tolerance (approximately 90%) and compliance (approximately 37% at the last visit) were comparable in both groups. Key articles October/December 2014 Tolerance improved throughout the study in both groups whereas adherence decreased continuously. delayed impact of solifenacin on continence return. Several limitations can be highlighted. Some important factors such as surgeon or surgical team This well-designed prospective study shows that experience, nerve-sparing surgery, pre-existing performing pelvic floor exercises at home and without incontinence or detrusor instability that are strong supervision for six months is improved by the use of predictors of continence recovery, were not taken into concomitant vaginal spheres. Beneficial results are account. Moreover, concomitant use of pelvic floor faster and better objective evolution was achieved rehabilitation was not reported. Initial stratification by regarding pad-test results over the treatment period. storage symptom intensity or urodynamic The lack of long-term follow-up may preclude strong investigations could be relevant to identify patients clinically relevant conclusions as adherence to muscle who would benefit the most from solifenacin use. rehabilitation decreases over time. Moreover, such rehabilitation may not fit all because about one-third of women are unable to contract pelvic floor muscles. Another limitation of that study was that both patients and therapists were not blinded leading to potential interpretation biases. Source: Effect of vaginal spheres and pelvic floor muscle training in women with urinary incontinence: A randomized, controlled trial. Porta-Roda O, Vara-Paniagua J, Díaz-López MA, Sobrado-Lozano P, Simó-González M, DíazBellido P, Reula-Blasco MC, Muñoz-Garrido F. Neurourol Urodyn 2014 doi:10.1002/nau.22640. Continence recovery after radical prostatectomy: No clear benefit favouring solifenacin versus placebo Even if the viability of external sphincter is the most common factor of incontinence after radical prostatectomy, bladder dysfunction after prostate surgery may also influence urinary continence recovery. Thus, control of detrusor instability by antimuscarinics might improve return of continence. Nevertheless, due to the lack of well-designed trials, the EAU guidelines rank the evidence as C regarding the use of antimuscarinics in patients suffering from urgency or mixed urinary incontinence after radical prostatectomy. The present study was a phase 4, multi-center, randomized, double-blind, placebo-controlled trial assessing the impact of post-operative solifenacin in the recovery of urinary incontinence after radical prostatectomy. Enrolled men were those who were still incontinent (defined by at least two pads per day for seven consecutive days) seven to 21 days after catheter removal. The primary objective was the time to continence over a three-month study period. Continence was defined by 0 or one pad for security which remains completely dry. The secondary endpoints were the proportion of men who gained continence and the amount of daily pad use. Overall, 623 patients were randomized receiving 5 mg of solifenacin or placebo. Solifenacin dose could be doubled at week 4. Regarding the primary endpoint, there was no significant difference in the time to return to continence between both arms, whatever the final solifenacin dose (5 or 10 mg) used. Thus, the study was globally negative. However, a slight but significant improvement favouring solifenacin over placebo was reported in the proportion of patients continent at the end of the study (29% versus 21%, p=0.04). … no significant difference in the time to return to continence between both arms… however, a slight but significant improvement favoring solifenacin over placebo was reported in the proportion of patients continent at the end of the study The number of pads per day was slightly improved from week 12 in the solifenacin arm as compared with placebo (p=0.01). In contrast, analysis of quality of life outcomes and symptom scores did not show differences between groups. Dry mouth was reported in 6% of men receiving solifenacin (versus 0.6% of placebo patients) without any difference in terms of constipation rate between arms. To recap, the use of solifenacin over a three-month period does not globally improve time to continence in men undergoing radical prostatectomy. Nevertheless, analysis of survival curves that started separating after 50 days, suggested a trend for a Source: A Randomized, Double-Blind, Solifenacin Succinate vs Placebo-Control Phase 4, Multi-Center Study Evaluating Urinary Continence after Robotic Assisted Radical Prostatectomy. Bianco FJ, Albala DM, Belkoff LH, Miles BJ, Peabody JO, He W, Bradt JS, Haas GP, Ahlering TE. J Urol 2014 doi: 10.1016/j.juro.2014.09.106 Dr. Guillaume Ploussard Section editor Paris (FR) g.ploussard@ gmail.com be informed about a possible time-dependent alteration in functional results at the time of surgery. Nevertheless, only few patients required surgical re-treatment during the first five years after initial surgery. Source: 5-Year Longitudinal Follow-up after Retropubic and Transobturator Midurethral Slings. Kenton K, Stoddard AM, Zyczynski H, Albo M, Rickey L, Norton P, Wai C, Kraus SR, Sirls LT, Kusek JW, Litman HJ, Chang RP, Richter HE; Urinary Incontinence Treatment Network. Higher long-term success rate but greater negative impact J Urol 2014 doi: 10.1016/j.juro.2014.08.089 on QOL after retropubic-sling compared to transobturator- Factors affecting sling for stress urinary spermatogenesis upon incontinence gonadotropin-replacement therapy Failure rates increase over time after surgery for stress urinary incontinence. Whereas outcome equivalence has been demonstrated when comparing retropubic and transobturator slings, few long-term well-designed studies have characterized five-year equivalence between the two devices. Whereas authors … reported higher success rates after retropubic-sling, subjective assessment revealed that women felt better after transobturator-sling surgery Kenton et al. reported in this article the five-year outcomes of a randomized equivalence clinical trial of retropubic and transobturator midurethral slings. Treatment success was defined by the absence of re-treatment for stress urinary incontinence and no self-reported stress urinary incontinence symptoms on questionnaire. Satisfaction, urinary symptoms, quality of life and adverse events were also reported. The two previous publications from this trial concluded that objective success rates met the criteria for equivalence at 12 months but no longer met these criteria at 24 months. Overall, approximately two-thirds of women initially enrolled were followed at least five years and included in this observational study. Regarding the primary endpoint, treatment success was 8% greater after retropubic compared to transobturator sling (51.3% versus 43.4%). As difference did not reach statistical significance, success rates could not be considered different from one another. However, rates did not meet prespecified criteria for equivalence. Reasons for failure were incontinence symptoms in 85% of cases, and surgical re-treatment in 14% of cases. Interestingly, urgency incontinence symptoms and incontinence negative impact on QOL were greater in the retropubic-sling arm (p=0.001 and p=0.02) compared to transobturator-sling. Moreover, mean sexual function scores were lower in the retropubic group (p=0.001). In line with these significant differences regarding the secondary endpoints, women receiving transobturator-sling felt more frequently “very much better” or “much better” than women receiving retropubic-sling (p<0.0001). Overall satisfaction rate did not differ between both groups. No significant difference in terms of serious and non-serious adverse events was reported. This study is highly interesting and reveals that objective success rate should not be regarded as the only gold standard endpoint in incontinence treatment trial. Whereas authors were unable to attest to the long-term equivalence of both devices and reported higher success rates after retropubicsling, subjective assessment revealed that women felt better after transobturator-sling surgery thanks to lower urgency rates and improved sexual function. In line with two-year outcomes, failure rates increased over time highlighting that patients should The authors performed a meta-analysis to systematically analyse the results of gonadotropin and GnRH therapy in inducing spermatogenesis in subjects with hypogonadotropic hypogonadism (HHG) and azoospermia. An extensive Medline and Embase search was performed including the following words: 'gonadotropins' or 'GnRH', 'infertility', 'hypogonadotropic', 'hypogonadism' and limited to studies in male humans. Overall, 44 and 16 studies were retrieved for gonadotropin and GnRH therapy, respectively. Of those, 43 and 16 considered the appearance of at least one spermatozoa in semen, whereas 26 and 10 considered sperm concentration upon gonadotropin and GnRH, respectively. The combination of the study results showed an overall success rate of 75% (69-81) and 75% (60-85) in achieving spermatogenesis, with a mean sperm concentration obtained of 5.92 (4.72-7.13) and 4.27 (1.80-6.74) million/mL for gonadotropin and GnRH therapy, respectively. The results upon gonadotropin were significantly worse in studies involving only subjects with a pre-pubertal onset HHG, as compared with studies involving a mixed population of pre- and post-pubertal onset [68% (58-77) vs. 84% (76-89), p = 0.011 and 3.37 (2.25-4.49) vs. 12.94 (8.00-17.88) million/mL, p < 0.0001; for dichotomous and continuous data, respectively]. …gonadotropin therapy, even with urinary derivatives, is a suitable option in inducing/restoring fertility in azoospermic HHG subjects A similar effect was observed also upon GnRH. No difference in terms of successful achievement of spermatogenesis and sperm concentration was found for different FSH preparations. Previous use of testosterone replacement therapy (TRT) did not affect the results obtained with gonadotropins. Finally, a higher success rate was found for subjects with lower levels of gonadotropins at the baseline and for those using both human chorionic gonadotropin and FSH. The authors concluded that gonadotropin therapy, even with urinary derivatives, is a suitable option in inducing/restoring fertility in azoospermic HHG subjects. Gonadotropins appear to be more efficacious in subjects with a pure secondary nature (low gonadotropins) and a post-pubertal onset of the disorder, whereas previous TRT does not affect outcome. Source: Factors affecting spermatogenesis upon gonadotropin-replacement therapy: A meta-analytic study. Rastrelli G, Corona G, Mannucci E, Maggi M. Andrology. 2014 Nov;2(6):794-808. doi: 10.1111/ andr.262. Epub 2014 Oct 1. EAU EU-ACME Office European Urology Today 15 Dr. Francesco Sanguedolce Section editor London (UK) fsangue@ hotmail.com Link between lifestyle and health factors and severe Lower Urinary Tract Symptoms (LUTS) Despite growing interest in prevention of lower urinary tract symptoms (LUTS) through better understanding of modifiable risk factors, large-scale population-based evidence is limited. The authors intended to describe risk factors associated with severe LUTS in the 45 and Up Study, a large cohort study. A cross-sectional analysis of questionnaire data from 106,435 men ≥ 45 years, living in New South Wales, Australia was performed. culture. There were 7,728 consecutive patients included in the analysis, whose data were prospectively recorded. On the other hand, the data were pooled and analysed retrospectively to answer the study question. The authors reported as main findings that administration of antibiotic prophylaxis differed from 13% to 100%… There was a substantial disproportion between patients who received an antibiotic prophylaxis prior a URS (group 1 = 82.8%) and those who did not (group 2 = 17.2%); most of the patients of the latter group where recruited in centres from Iran, Tunisia and Germany. Data from the 1,141 patients who did not receive antibiotic prophylaxis and had complete parameters were compared with a similar number of patients who received an antibiotic prophylaxis matched on the basis of similar demographic variables (i.e. gender, ASA and pre-operative stent). LUTS were measured by a modified version of the International Prostate Symptom Score (m-IPSS). The strength of association between severe LUTS and socio-demographic, lifestyle and health-related factors was estimated, using logistic regression to calculate odds ratios, adjusted for a range of confounding factors. Several controversial results have been reported: patients receiving antibiotic prophylaxis were more likely to suffer from diabetes and to be under anticoagulant therapy; they have a significant lower stone burden, higher rates for complications (bleeding and perforation) and a lower stone-free rate; finally, they have a higher proportion of stone impaction and readmission rate within three months. …LUTS was associated with a number of factors, including modifiable risk factors, suggesting potential targets for prevention More interestingly, the prevalence of fever or UTI after a URS was low overall (< 2.2%), without difference between the two groups. On a multivariate analysis, pooling all the cases together, risk factors to develop a postoperative UTI were female gender, Crohn’s or cardiovascular disease and patient with ASA III or IV. Overall, 18.3% reported moderate, and 3.6% severe, LUTS. Severe LUTS were more common among men reporting previous prostate cancer (7.6%), total prostatectomy (4.9%) or having part of the prostate removed (8.2%). After excluding men with prostate cancer or prostate surgery, the prevalence of moderate-severe LUTS in the cohort (n = 95,089) ranged from 10.6% to 35.4% for ages 45-49 to ≥ 80; the age-related increase was steeper for storage than voiding symptoms. The authors reported as main findings that administration of antibiotic prophylaxis differed from 13% to 100%; however, it is not clear if these proportions reflect the clinical protocols applied throughout the relevant countries other than from the centres which participated in the study. They also emphasised that female and patients with high ASA were more likely to develop postoperative fever or UTI and this is a finding easily to understand. They finally highlighted that the prevalence of post-op UTI/fever is not affected by the antibiotic prophylaxis. The adjusted odds of severe LUTS decreased with increasing education (tertiary qualification versus no school certificate, odds ratio (OR = 0.78 (0.68-0.89))) and increasing physical activity (high versus low, OR = 0.83 (0.76-0.91)). Odds were elevated among current smokers versus never-smokers (OR = 1.64 (1.43-1.88)), obese versus healthy-weight men (OR = 1.27 (1.14-1.41)) and for comorbid conditions (e.g., heart disease versus no heart disease, OR = 1.36 (1.24-1.49)), and particularly for severe versus no physical functional limitation (OR = 5.17 (4.51-5.93)). It is also interesting to note that the authors cited the EAU guidelines in recommending the use of antibiotic prophylaxis only for those patients treated by URS for proximal or impacted stones. This recommendation is reported in the EAU Guidelines for Urological Infections, which is not entirely consistent with what is recommended in the EAU Guidelines for Urolithiasis, where it is stated that a short-term antibiotic prophylaxis should be administered prior to a URS anyway (LE 4; GR A). The authors concluded that LUTS was associated with a number of factors, including modifiable risk factors, suggesting potential targets for prevention. The authors also correctly reported results from two randomised controlled trials where the results tended to support the use of antibiotic prophylaxis. TRIAL REGISTRATION: clinicaltrials.gov Identifier: NCT00931528. Unfortunately, no recommendation can be given on the basis of the findings of this paper because of the study limitations. More extensive and robust data are needed to eventually identify patients who cannot necessarily receive an antibiotic prophylaxis prior to a URS for ureteric stones. Source: Relationship between lifestyle and health factors and severe Lower Urinary Tract Symptoms (LUTS) in 106,435 middle-aged and older Australian men: Population-based study. Smith DP, Weber MF, Soga K, Korda RJ, Tikellis G, Patel MI, Clements MS, Dwyer T, Latz IK, Banks E. PLoS One. 2014 Oct 15;9(10):e109278. doi: 10.1371 Antibiotic prophylaxis prior ureteroscopy for ureteric stones: Myth or need? The Clinical Research Office of the Endourological Society (CROES) is a well-known large international database with different branches investigating the clinical and surgical practice for the treatment of urolithiasis worldwide. One of the latest publications of CROES was focused on the role of the antibiotic prophylaxis in preventing the onset of urinary infection after ureteroscopic stone removal, in patients with negative baseline urine Key articles 16 Source: Postoperative infection rates in patients with a negative baseline urine culture undergoing ureteroscopic stone removal: a matched case-control analysis on antibiotic prophylaxis from the CROES URS Global Study. Martov A, Gravas S, Etemadian M, Unsal A, Barusso G, D'Addessi A, Krambeck A, de la Rosette J. J Endourol. 2014 Sep 5. [Epub ahead of print] The lower pole stones: A historical dilemma to an end? The dilemma on how to treat the lower pole stones has excited endourologists in the last 10 to 20 years. In the mid ‘90s, Lingeman et al showed that the Shock Wave Lithotripsy (SWL) poorly performed in this setting of stone patients. In the early 2000s, flexible ureteroscopy (fURS) was supposed to combine the high stone-free rates obtained by a percutaneous lithotripsy (PCNL) and the low complication rates of SWL; unfortunately, Pearle et al in a randomised controlled trial showed no significant difference between the SWL and fURS in terms of stone-free rates (SFR) and a higher complication rates for fURS. However, this study was focused on lower pole stones < 1 cm. On the other hand, several papers have been published in the last years supporting the use of fURS, mainly in the case of lower pole stones > 1 cm, even though in most of the cases the quality of the studies was suboptimal. The latest and more robust evidence comes from an Indian group which compared safety and efficacy, SWL and fURS in a prospective randomised comparison for lower pole stones ≤ 2 cm. Patients were randomised by using a computer randomisation table. A total of 90 +90 patients were included in the final analysis. Stone-free rates were comparable in both groups; surprisingly, SWL performed much better in this study than how it was historically described, with a SFR at a three-month follow-up of 84.9% for lower pole stones < 1 cm and 78.4% for lower pole stones of 1-2 cm, with respect to the < 50% in average reported in literature. Complications rates were also comparable; conversely, as expected, SWL accounted for a higher retreatment rate, but no difference was found in terms of auxiliary procedures needed (fURS or PCNL for SWL group; PCNL for fURS group). The conclusion of the authors is in line with previous evidences and the recommendation from the guidelines: for lower pole stones < 1 cm, SWL is safer, less invasive and with comparable efficacy to fURS Mr. Philip Cornford Section editor Liverpool (GB) philip.cornford@ rlbuht.nhs.uk Fifty and 53 patients were included in the HoLEP and PVEP groups, respectively. Operating time, hospital stay and time to catheter removal were comparable between both groups. There was significant, comparable improvement of IPSS and PVR at 1, 4 and 12 months. After four months, prostate size reduction was significantly higher in the HoLEP group (74.3% vs. 43.1%, p = 0.001). At 12-months, Qmax was significantly higher in the HoLEP group (26.4 ±11.5 vs. 18.4 ±7.5 mL/sec, p = 0.03). Re-intervention was needed in two and three cases in HoLEP and PVEP groups, respectively (p = 1.0). The mean estimated cost per HoLEP procedure was significantly lower than per PVEP procedure. The investigators stated, that compared to HoLEP, Greenlight laser PVEP-XPS is safe, non-inferior and effective in treatment of BPH The investigators stated, that compared to HoLEP, Greenlight laser PVEP-XPS is safe, non-inferior and effective in treatment of BPH. Trial Registration: ClinicalTrials.gov ID: NCT01494337. Source: Green light laser (XPS) photoselective vapo-enucleation of the prostate versus Holmium laser enucleation of the prostate for treatment of symptomatic benign prostate hyperplasia: A randomized controlled study. Elshal AM, Elkoushy MA, El-Nahas AR, Shoma AM, Nabeeh A, Carrier S, Elhilali MM. J Urol. 2014 Sep 24. pii: S0022-5347(14)04551-0. doi: 10.1016/j.juro.2014.09.097. The only advantage for fURS was showed when comparing the Efficiency Quotient (EQ) - which is the rate between the patients rendered stone-free by the primary intervention and those who became stone-free SUSPEND: The trial on Medical after an auxiliary procedure – in the subgroups of Expulsive Therapy for ureteric patient with lower pole stone of 1 to 2 cm. The conclusion of the authors is in line with previous evidences and the recommendation from the guidelines: for lower pole stones < 1 cm, SWL is safer, less invasive and with comparable efficacy to fURS. For lower pole stones 1 to 2 cm, fURS is more effective with a lower retreatment rate then SWL. Source: A prospective randomized comparison between shock wave lithotripsy and flexible ureterorenoscopy for lower calyceal stones ≤ 2 cm: A single center experience. Kumar A, Vasudeva P, Nanda B, Kumar N, Das MK, Jha SK. J Endourol. 2014 Sep 9. [Epub ahead of print] Green light laser (XPS) photoselective vapoenucleation of the prostate versus Holmium laser enucleation in treating BPH After the advent of the XPS (180W) 532nm-laser, Photoselective Vapo-Enucleation of the Prostate (PVEP) could compete with Holmium Laser Enucleation of the prostate (HoLEP) as a size independent procedure. The authors assessed whether PVEP-XPS is not less effective than HoLEP for improvement of lower urinary tract symptoms secondary to benign prostatic hyperplasia (BPH). A randomized controlled non-inferiority trial comparing HoLEP to PVEP- XPS 180W was conducted. International prostate symptoms score (IPSS), flow rate (Qmax), residual urine (PVR), prostate specific antigen (PSA) and prostate volume changes as well as perioperative and late adverse events were compared. Non-inferiority of IPSS at one year was evaluated using one-sided test at 5% level of significance. The statistical significance of other comparators was assessed at (two-sided) 5% level. stones we were waiting for? SUSPEND is a large UK-based, double blinded, placebo-controlled randomised trial which has been designed to confirm/reject the hypothesis that the Medical Expulsive Therapy (MET) with Tamsulosin 4 mg or Nifedipine 30 mg significantly increases the spontaneous passage of ureteric stones ≤ 10 mm. Even though several trials and systematic reviews have showed a quicker expulsion of ureteric stones and an improved pain relief significantly provided by MET, there are still consistent concerns on the real effectiveness of the treatment because of several and diverse limitations of the above mentioned studies: the trials have been reported to be usually small in size, patients mainly affected by lower ureteric stones, significant bias variably limiting the conclusions and frequent lack of a cost-effectiveness evaluation. Consequently, the results of the systematic reviews have been affected by the poor quality of the pooled data for the meta-analysis; hence the need of a large, multicentre, randomised clinical trial as claimed by most of them. This trial is expected to provide more robust and definitive information with respect to whether and which MET is effective in the management of ureteric stones The first patient of SUSPEND was recruited in January 2011, but the study design and the methodology have been published only at the end of June 2014. The trial involves two intervention arms (Tamsulosin 4 mg or Nifedipine 30mg, for 28 days) versus placebo, and randomisation is based on 1:1:1 proportion. Primary outcomes are 1) spontaneous passage of ureteric stones at four weeks and 2) reduction in EAU EU-ACME Office European Urology Today October/December 2014 incremental cost per quality-adjusted life years. With respect to the latter, interestingly the trial will not evaluate just the costs based on the National Health reported data: as the study has been designed to be societal, total costs will include expenses sustained also by the participants (travel, time, medications). It is noteworthy that clinical outcome is defined as no “further intervention required” which encompass subjective clinical conditions (symptoms and stone passage reported by the patient) and healthcare delivery; no imaging studies have been included to objectively report the stone status at the follow-up appointments (at 4 and 12 week). Based on previous data, the null hypothesis will be rejected if the increased stone passage rate will be at least > 25% in the MET arms compared to placebo (> 75% vs. 50%, respectively); moreover, the authors will investigate a supposed increase of 10% of stone passage in the treatments arms from 75% (Nifedipine group) to 85% (Tamsulosin group). To test these hypotheses, the sample size has been calculated to be 400 patients per arm at a 90% of power and 5% of error. This trial is expected to provide more robust and definitive information with respect to whether and which MET is effective in the management of ureteric stones; this is an important goal considering that the use of the MET is largely diffused worldwide from many years, even though the prescription of these drugs is still off-label. Source: Use of drug therapy in the management of symptomatic ureteric stones in hospitalized adults (SUSPEND), a multicentre, placebocontrolled, randomized trial of a calciumchannel blocker (nifedipine) and an α-blocker (tamsulosin): study protocol for a randomized controlled trial. McClinton S, Starr K, Thomas R, McLennan G, McPherson G, McDonald A, Lam T, N'Dow J, Kilonzo M, Pickard R, Anson K, Burr J; SUSPEND Study Group. Trials. 2014 Jun 20;15:238. doi: 10.1186/1745-6215-15-238. Higher hospitalisation rates and infections following prostate biopsy The authors conducted a population-based study of 75,190 men who underwent a transrectal ultrasound guided biopsy in Ontario, Canada, between 1996 and 2005. Hospital and cancer registry administrative databases were used to estimate the rates of hospital admission and mortality due to urological complications associated with the procedure. Of the 75,190 men who underwent transrectal ultrasound biopsy 33,508 (44.6%) were diagnosed with prostate cancer and 41,682 (55.4%) did not have prostate cancer. The hospital admission rate for urological complications within 30 days of the procedure for men without cancer was 1.9% (781/41,482). The 30-day hospital admission rate increased from 1.0% in 1996 to 4.1% in 2005 (p for trend = 0.0001). ...the hospital admission rates for complications following transrectal ultrasound guided prostate biopsy have increased dramatically during the last 10 years… The majority of hospital admissions (72%) were for infection related reasons. The probability of being admitted to hospital within 30 days of having the procedure increased four-fold between 1996 and 2005 (OR 3.7, 95% CI2.0 –7.0, p = 0.0001). The overall 30-day mortality rate was 0.09% but did not change during the study period. The authors concluded that the hospital admission rates for complications following transrectal ultrasound guided prostate biopsy have increased dramatically during the last 10 years primarily due to an increasing rate of infection related complications. to biopsy, the background incidence of urinary tract infection was approximately 2%. Within 30 days after biopsy, 6% had a dispensed prescription for urinary tract antibiotics and 1% were hospitalised with an infection. The strongest risk factors for an antibiotic prescription were prior infection (OR 1.59, 95% CI,1.45−1.73), high Charlson comorbidity index (OR 1.25, 95% CI 1.11−1.41) and diabetes (OR 1.32, 95% CI 1.17−1.49). Risk of an antibiotic prescription after biopsy decreased from 2006 to 2011 (OR 0.79, 95% CI 0.70-0.90), whereas risk of hospital admission increased (OR 2.14, 95% CI 1.58-2.94). No significant increase in 90-day mortality was observed. The absolute 90-day mortality rates for patients with dispensed prescriptions and those hospitalised were 1% and 1.5% respectively compared to a 90-day mortality rate of 1% for patients without infection diagnosis. ...severe infections with hospitalisation after prostate biopsy are increasing in Sweden and the risk of post-biopsy infection is highest among men with a history of UTI… In total, 516 (1%) patients died within 90 days of biopsy and 34 (6.6%) of these were registered as having died due to a urinary tract infection or sepsis. Of the patients hospitalised for infection the odds of dying of infection related cause was high (OR 12.6, 95%CI, 2.4-61.8)) compared to if they were not admitted, but the absolute numbers were low. Source: Increasing Hospital Admission Rates for Urological Complications After Transrectal Ultrasound Guided Prostate Biopsy. Robert K. Nam, Refik Saskin, Yuna Lee, Ying Liu, Calvin Law, Laurence H. Klotz, D. Andrew Loblaw John Trachtenberg, Aleksandra Stanimirovic, Andrew E. Simor, Arun Seth, David R. Urbach and Steven The authors concluded that severe infections with A. Narod. hospitalisation after prostate biopsy are increasing in J Urol 2013;189: S12-S18. DOI: http://dx.doi.org/10.1016/j. juro.2012.11.015 Sweden. The risk of post-biopsy infection is highest among men with a history of UTI and those with significant co-morbidities. Population-based study of infections after transrectal ultrasound guided prostate biopsy Source: Nationwide population-based study of infections after transrectal ultrasound guided prostate biopsy. Lundström KJ, Drevin L, Carlsson S, Garmo H, Loeb S, Stattin P, BillAxelson A. The authors estimated incidence and risk factors for infection after prostate biopsy as well as 90-day mortality using a nationwide Swedish sample. A population-based study was performed on data assembled between 2006 and 2011 of 51,321 men from the Prostate Cancer data Base (PCBaSe) Sweden. The primary outcome measures were dispensed prescriptions of antibiotics for urinary tract infection (UTI) and hospitalisations with a discharge diagnosis of a urinary tract infection. During the 6 months prior The Journal of Urology® (2014), doi: 10.1016/j. juro.2014.04.098. Freehand ultrasound-guided transperineal prostate biopsy In this video, the authors demonstrated a technique that avoids the infectious risks associated with passing the biopsy needle through the rectal wall using a transperineal freehand technique under ultrasound monitoring. Patients requiring prostate biopsy were offered the option of sedation and/or local anaesthesia. Intravenous access was obtained for a weight-based dose of cefazolin and propofol-induced procedural anaesthesia. No bowel preparation, prior rectal swab, or pre-/postoperative antibiotics were used. Patients were draped in a dorsal lithotomy position, using tape to secure the penis and testicles. A povidone– iodine swab, 10%, was used to prepare the perineum. Transrectal ultrasound of the prostate was performed for measurement and identification of potentially pathological regions. None of the patients suffered any postoperative physician or hospital intervention nor experienced any complication ≥ Clavien Grade I A 14-gauge needle was placed into the perineum at the midprostate on each side. Approximately 10 mL of 2% lidocaine was infiltrated into the skin, subcutaneous tissue, and pelvic floor. Under ultrasound supervision, the Bard 18-gauge biopsy gun (Bard Max-Core22 mm; Bard Medical) was placed and reintroduced through the 14-gauge needle into the prostate, with ultrasound-confirmed tip location. Three separate regions of the prostate (far lateral, middle, and apical) were sampled. Based on the size of the prostate gland, two to four tissue samples were obtained from each region. Pressure was applied to the perineum and a small amount of bacitracin was applied to the puncture sites. Patients were discharged following recovery from propofol anaesthesia and were instructed to avoid lifting for 24 hours. Two hundred and thirteen patients underwent freehand transperineal prostate biopsy from January 2012 to October 2013. All patients opted for sedation. Biopsy was performed within 10 minutes, and total room time within 15 minutes. None of the patients suffered any postoperative physician or hospital intervention nor experienced any complication ≥ Clavien Grade I. All episodes of haematuria were self-limiting. The technique described uses the same equipment as the traditional transrectal technique except for a 14-gauge needle and may feasibly be performed under local anaesthesia within the time frame usually allotted for a transrectal technique with an incidence of infection and hospitalisation of zero. Source: Freehand Ultrasound-Guided Transperineal Prostate Biopsy: Technique and Early Results. DiBianco JM, Allaway M. Jounal of Endourology, January 2014. doi: 10.1089/ vid.2014.0046 Key articles Aldo Vittorio Bono Dedicated doctor and true friend 1934 - 2014 Family and colleagues mourn the passing of Aldo Vittorio Bono who died in Varese, Italy on 25 August 1914. involving pathologists and basic scientists. Aldo authored (or co-authored) more than 300 scientific publications. But aside from his scientific pursuits he also had a very deep interest in art and music. He played the guitar and took courses in painting. Aldo graduated at the Milan University in 1959 with specialisation in urology, general surgery and paediatric urology. He became a professor of surgical pathology in 1971 and three years later was appointed chairman of the Department of Urology in Varese where he remained until he retired in 2006. He was also teaching professor of uro-oncology at the University of Pavia and Brescia. Despite his illness in 2006 he never allowed it to dampen his enthusiasm for his work, and even made plans for and joined voluntary service. In 2008 Aldo was nominated vice-president of Alzheimer Association of Varese and became president in 2012 until 2014. In 1979 he organised the “Varese International Meeting of Pediatric Urology” which mainly featured live surgery, at that time considered a unique event which gathered some of the most renowned European and American specialists. Aldo had a brilliant mind and was a very good organiser. He became a member of the EORTC-GU Group in the 1980s and was later appointed as chairman. From 2005 to 2008 he was president of the Italian Society of Urology. October/December 2014 He strongly believed in multi-disciplinary approaches in medicine and organised a special committee within the EORTC-GU that involved pathologists. He also prioritised translational research and collaborated with basic researchers, statisticians and other specialists. Aldo was a dedicated scientist and even when he was close to retirement he never tired of envisioning the future of urology and medicine. I remember that just before his retirement he discussed with me the future of uro-oncology strategies and its prospects, and showed his enthusiasm for multi-centre studies I am privileged to have had the opportunity to know Aldo personally and professionally since my involvement with the EORTC. We have travelled and shared ideas and projects, and he was not only a good teacher but also a true friend. His friendship was a source of joy to me. We lost a great scientist and a good friend. Ciao Aldo, rest in peace. -By Prof. Maurizio Brausi European Urology Today 17 CEM2014 SYMPOSIUM REPORT Benign Prostatic Hyperplasia (BPH) Report on Berlin-Chemie/Menarini - sponsored satellite symposium 2014 Chair: Prof. Bob Djavan, Professor of Urology, University of Vienna (AT) Prostatic T-Cell Products IL-2, -4, -5, -10, -13, -17 IFN-γ, TGF-β, FGF-2 It is always interesting and challenging to moderate a scientific symposium on the occasion of the CEM Congress. This year’s Berlin-Chemie/Menarini sponsored scientific event dealt extensively and appropriately with the role of phytotherapy and more in particular Serenoa repens extract for the treatment of voiding difficulties associated with benign prostatic hyperplasia (BPH). The scientific session which took place at the Holiday Inn Hotel in Cracow on Saturday, 11 October 2014, was attended by approximately 150 urologists mostly coming from Central and Eastern Europe. In these regions phytotherapy is a largely accepted treatment option for voiding difficulties due to BPH. Hence the large interest of these congress delegates in the symposium, which aimed at presenting an overview of current evidence focusing on the reasons for BPH, the risks of BPH, current treatment options for BPH rostatic T-Cell Products and how aggravation of BPH may be prevented. The 5, -10, -13,speakers, -17 IFN-γ,all TGF-β, FGF-2 experts in urology, well-known presented up-to date information on novel aspects of Typeof0 voiding symptoms due to Type 2treatment options BPH, IL -4, -5, -13 pos IL -4, -5, -13 pos BPH and preliminary IL -2, clinical IFN-γ pos results of IL -2, IFN-γ neg phytotherapeutic treatment. Type 1 IL -2, IFN-γ pos IL -4, -5, -13 neg Leukocytic Growth Factors of Non-Lymphoid Prostatic Cells IL-1α, & β, IL-6, -8, -13, -15, GM-CSF, TNF-α, TGF-β, FGF-2, VEGF, SCF Macrophages & Mast Cells IL -1, -6, -8, -13, GM-CSF, TNF-α Epithelial Cells IL -1, -4, -6, -8, -13 TGF-β FGF-2, GM-CSF, TNF-α Stromal Cells IL -1, -6, -8, -13 TGF-β FGF-2, GM-CSF, TNF-α Figure 2: Intraprostatic lymphokine network, IL = interleukin; IFN = Interferon; TGF = Transforming growth factor; FGF = Fibroblast growth factor; GM-CSF = Granulocyte macrophage colony stimulating growth factor; TNF = Tumor necrosis factor; ml/sec VEGF = Vascular endothelial growth factor; maxSCF = Stem cell 20 factor (Image adapted from Steiner GE, Djavan B, et al. 200218) 18 Q Prostate enlargement 20 12 0 10 -20 8 Initial 2 yrs 4 yrs 6 yrs 8 yrs BPH Symptoms Inflammation Stromal Cells IL -1, -6, -8, -13 TGF-β FGF-2, GM-CSF, TNF-α Overactive bladder Figure 3: Factors related to BPH Photo: A. Horstmann Q max 10 40 14 , & β, IL-6, -8, -13, -15, GM-CSF, F-α, TGF-β, FGF-2, VEGF, SCF RUV ml 60 16 kocytic Growth Factors of -Lymphoid Prostatic Cells Epithelial Cells IL -1, -4, -6, -8, -13 TGF-β FGF-2, GM-CSF, TNF-α Type 0 IL -4, -5, -13 pos IL -2, IFN-γ pos Type 2 IL -4, -5, -13 pos IL -2, IFN-γ neg of the product further contributes to these uncertainties. Prof. Debruyne stated that the underlying extraction method used to produce Prostate compound of Prostamol® uno, the Serenoa repens enlargement Berlin Chemie/Menarini is based on an ethanol extraction which ensures a more stable content of active products in its formulation. Based on a comprehensive review of the literature it can be concluded that Serenoa repens, already BPH known for centuries as a management option of BPH symptoms Symptoms has anti-inflammatory, anti-proliferative, proapoptopic and anti-androgenic properties which could result in positive clinical effect of BPH Inflammation Overactive bladder symptoms such as nocturia, for which Serenoa repens extract is significantly better than placebo. Prof. Debruyne said that it remains questionable and scientifically undefined which distinct substance is the most important and the most clinically valid and that these issues eventually could be clarified by further basic research in association with the evaluation of possible clinical findings related with the mode of action, such as prostate volume and prostate-specific antigen (PSA) evolution under Serenoa repens extract treatment. The take home message of Prof. Debruyne was “Longer treatment – better treatment!” and that combination therapy is a promising approach in the treatment of BPH. 10 yrs Initial 2 yrs 4 yrs 6 yrs 8 yrs 10 yrs How can further aggravation of BPH be prevented (Prof. A. Z. Vinarov, Moscow (RU)) The last presenter was Prof. Andrey Vinarov, from Moscow (RU) who published several articles about Serenoa repens21,22 and gave a detailed update of the long-term Russian clinical study in which patients with mild to moderate BPH were treated with 320 mg of Prostamol® uno once daily for ten years2. The results underlined the long-term benefits of Serenoa repens, namely, the reduction in IPSS score and the improved QoL2. In addition, the treatment displayed the high tolerability of Serenoa repens extract with no serious adverse events2 and confirmed earlier results3. This aspect may be the main advantage of treatment when compared to other pharmacological treatment. Treatment options of BPH symptoms (Prof. F. M. J. Debruyne, Arnhem (NL)) After the first introduction into the multifactorial reasons and the risk factors of BPH, Prof. Debruyne from Arnhem (NL) summarized current treatment options. He highlighted that the main aim of therapy has to be the improvement of bothering symptoms and quality of life (QoL) and the prevention of BPH-related complications such as urinary retention 9 . or upper urinary tract dilatation Initial 2 yrs 4 yrs 6 yrs 8 yrs 10 yrs RUV Prof. Bob Djavan Symposium Chair References 1. IuG Aliaev, et al., "[Efficacy and safety of prostamol-UNO in the treatment of patients with initial symptoms of prostatic adenoma and risk of progression: 2 years of investigations]," Urologiia (4), 36 (2009). 2. IuG Aliaev, et al., "[The results of the 10-year study of efficacy and safety of Serenoa repens extract in patients at risk of progression of benign prostatic hyperplasia]," Urologiia (4), 32 (2013). 3. A. L. Avins, et al., "Safety and toxicity of saw palmetto in the CAMUS trial," J Urol. 189(4), 1415 (2013). 4. Y. Bostanci, B. Djavan et al., "Correlation between benign prostatic hyperplasia and inflammation," Curr. Opin. Urol. 23(1), 5 (2013). 5. J. Breza, et al., "Prostamol uno (alcohol extract of the fruits of Serenoa repens) in the treatment of symptomatic benign prostatic hyperplasia," 54(4), 139 (2005). 6. F. Debruyne, et al., "[Evaluation of the clinical benefit of Permixon and tamsulosin in severe BPH patients--PERMAL study subset analysis]," Prog. Urol. 14(3), 326 (2004). 7. F. Debruyne, et al., "Comparison of a phytotherapeutic agent (Permixon) with an alpha-blocker (Tamsulosin) in the treatment of benign prostatic hyperplasia: a 1-year randomized international study," Eur Urol. 41(5), 497 (2002). 8. S. Fujikawa, et al., "Natural history of human prostate gland: Morphometric and histopathological analysis of Japanese men," Prostate 65(4), 355 (2005). 9. S Gravas, et al., 2014. S Gravas, et al., “Extended Guidelines 2014 Edition, Guidelines on the Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS), incl. Benign Prostatic Obstruction (BPO)” 2014. 10. M. M. Issa, et al., "An assessment of the diagnosed prevalence of diseases in men 50 years of age or older," Am J Manag. Care 12(4 Suppl), S83-S89 (2006). 11. S. J. Jacobsen, et al., "Treatment for benign prostatic hyperplasia among community dwelling men: the Olmsted County study of urinary symptoms and health status," J Urol. 162(4), 1301 (1999). 12. G. Kramer and M. Marberger, "Could inflammation be a key component in the progression of benign prostatic hyperplasia?," Curr. Opin. Urol. 16(1), 25 (2006). 13. G. Kramer, D. Mitteregger, and M. Marberger, "Is benign prostatic hyperplasia (BPH) an immune inflammatory disease?," Eur Urol. 51(5), 1202 (2007). 14. J. C. Nickel, "Inflammation and benign prostatic hyperplasia," Urol. Clin North Am 35(1), 109 (2008). 15. R. Rosen, et al., "Lower urinary tract symptoms and male sexual dysfunction: the multinational survey of the aging male (MSAM-7)," Eur Urol. 44(6), 637 (2003). 16. A. Sciarra, et al., "Prostate growth and inflammation," J Steroid Biochem. Mol. Biol. 108(3-5), 254 (2008). 17. I. Sinescu, et al., "Long-Term Efficacy of Serenoa repens Treatment in Patients with Mild and Moderate Symptomatic Benign Prostatic Hyperplasia," 86(3), 284 (2011). 18. G. E. Steiner, B. Djavan et al., "The picture of the prostatic Prostate lymphokine network is becoming increasingly complex," enlargement Rev. Urol. 4(4), 171 (2002). 19. G. E. Steiner, et al., "Expression and function of pro-inflammatory interleukin IL-17 and IL-17 receptor in normal, benign hyperplastic, and malignant prostate," Prostate 56(3), 171 (2003). 20.G. E. Steiner, et al., "Cytokine expression BPHpattern in benign prostatic hyperplasia infiltrating T cells and impact of Symptoms lymphocytic infiltration on cytokine mRNA profile in prostatic tissue," Lab Invest 83(8), 1131 (2003). 21. A. Z. Vinarov, et al., "[Results of three-year clinical study of prostamol uno efficacy and safety in patients with initial Inflammation Overactive symptoms of prostatic adenoma and risk of its bladder progression]," Urologiia (6), 3 (2010). 22. A. Z. Vinarov, IuG Aliaev, and K. L. Lokshin, "[Safety of continuous (more than 1 year) intake of Serenoa repens extract by patients with prostatic adenoma]," Urologiia (1), 84, 86, 87 (2009). Furthermore, Prof. Vinarov displayed that the treatment with Serenoa repens decelerated further prostate enlargement and that the prostate volume 10 18 was slightly reduced when compared to the control 60 16 group after ten years2. These results suggest that this 40 14 Figure 1: The speakers of the BPH Symposium at CEM 2014, treatment and the assumed anti-inflammatory 20 12 Cracow in order of the presentations: Prof. Djavan (AT), Prof. properties of Serenoa repens extract may contribute to 0 10 Debruyne (NL) and Prof. Vinarov the prevention of the further prostate enlargement. -20 8 After the presentation of Prof. Vinarov, Prof. Breza sr, Initial 2 yrs 4 yrs 6 yrs 8 yrs 10 yrs also a well-known expert on phytotherapy from What are the reasons for BPH, its progression and At the moment, several pharmacological treatment Bratislava (Slovakia) and the author of a Slovakian risks for the patient? (Prof. B. Djavan, Vienna (AT)) options (monotherapy or combination therapy), study which included more than 600 patients, who surgical, minimal invasive therapy and watchful had a follow up of 12 months, explained that the The opening of the session underlined the extent to T-Cell Products anti-inflammatory properties of Serenoa repens which the management of voiding symptoms due to waiting are available for urologists. Mainly used Prostatic extract are mainly due toFGF-2 inhibition of the BPH impacts the day-to-day work of urologists, since pharmacological therapies include the prescription of IL-2, -4, -5, -10, -13, -17 IFN-γ, TGF-β, inflammatory enzymes cyclo-oxygenase and this condition is the fourth most important health care α1-blockers (e.g. Tamsulosin) or 5-α-reductase issue of men ≥50 years in the US physicians are faced inhibitors (e.g. Finasteride) or a combination of both lipo-oxygenase5. Type 0 Type 2 Type 1 no with10. These symptoms have a major influence on in men with moderate symptoms (IPSS 8-19) with IL -4, -5, -13 pos IL -4, -5, -13 pos IL -2, IFN-γ pos 15 IL -2, pos IL -2,end IFN-γofneg erectile function and will aggravate when not indication for surgery. But since these IL -4, -5, -13 neg At the this interestingIFN-γ symposium all speakers treated10. pharmacological approaches do not target the agreed that there is still a need to institute early processes of inflammation associated with BPH, and treatment for these conditions before they progress 10 In recent years there is a change in perception of BPH. show side effects like orthostatic hypotension, erectile and require more extensive Leukocytic Growth Factors of and costly intervention It is clear that BPH is a progressive, age-related dysfunction, retrograde ejaculation, anejaculationNon-Lymphoid and and that patients suffering from voiding difficulties Prostatic Cells gastro-intestinal problems, alternative approaches are due to BPH the treatment outcome is more important disorder. However, new studies assume that IL-6,the -8,scientifically -13, -15, GM-CSF, inflammation seems to additionally have a serious mandatory, since these adverse effects may be IL-1α, & β, than based clinical evidence. Like in TNF-α, TGF-β, FGF-2, VEGF, SCF 4,12-14,16 impact on bothersome symptoms related to BPH . embarrassing for the patients who mostly need many diseases evidence based therapeutic results do It seems that there are three major components continuous treatment for their BPH symptoms. not always equal the clinical (partly subjective) Macrophages contributing to clinically relevant voiding symptoms, improvement seen in non-prospectively randomized Epithelial Cells Stromal Cells & Mast Cells IL -1,but -4, -6,as -8,stated -13 IL -1, -6, -8, -13 further research, As presented, one of the main aspects should be the namely, the prostate, inflammation and the bladder. trials, by the speakers IL -1, -6, -8, -13, TGF-β FGF-2, GM-CSF, TGF-β FGF-2, GM-CSF, GM-CSF, TNF-α by namelyTNF-α Several recently published studies demonstrated, inhibition of inflammation, which may be achieved well designed clinical studies are needed to TNF-α inflammation, evidenced as inflammatory cell additionally applying herbal products. Several herbal identify the mode of action and the long-term impact infiltration and up-regulation of several inflammatory products for the treatment of BPH exist, and the most of Serenoa repens extract in the treatment of voiding prominent and most studied is the extract of Serenoa difficulties in mild to moderate BPH. markers are often present in patients with BPH8,19,20. repens1,2,6,7,17,21,22. As explained by Prof. Debruyne, Main risk factors for the progression of BPH and associated voiding difficulties are age, symptoms, phytotherapy, although well recognized as a clinically flowrate (Qmax), prostate volume and prostate-specific valid therapeutic option, is usually considered as insufficiently scientifically evidence based and this is antigen (PSA) concentration11. In addition, the loss of elastic fibers in the bladder tissue, which is a normal one of the reasons why it is not (yet) recommended in ml ml/sec max 20 part of the aging process, contributes to clinically the EAU Guidelines for the treatment of BPH. In its 10 18 relevant symptoms in men as well as in women. 2014 edition the EAU Guidelines committee concluded Therefore, voiding symptoms cannot be monocausally that it was not yet able to formulate specific 60 16 explained by only prostate alterations. recommendations on phytotherapy of BPH because of 40 14 the heterogeneity of products and the methodological 20 12 The take home message for the audience was that all problems associated with meta-analyses, but Prof. 0 10 aspects contributing to bothersome symptoms have to Debruyne explained that this is mainly related to the -20 8 be kept in mind, that inflammation may be a potential different extraction methods of the Serenoa repens Initial 2 yrs 4 yrs 6 yrs 8 yrs 10 yrs Initial 2 yrs 4 yrs 6 yrs 8 yrs 10 yrs therapeutic target and that the assessment of extract. The heterogeneity of the substances included patient´s history is important to find the best in the compound and the different extraction methods Figure 4: Changes in Flowrate (Qmax, left) and Residual urinary volume (RUV, right) observed with daily treatment with Serenoa treatment option. for Serenoa repens resulting in different compositions repens (Image adapted from Aliaev et al. 20132) ml/sec 20 ml Q 18 European Urology Today RUV October/December 2014 14th CEM: Closing the gap between East and West Meeting demonstrates the high level of urological research in Central Europe By Monique Van Hout incidentalomas in elderly patients who often suffer from comorbidities which make them unfit for surgery. Sedelaar showed that the mortality rate in this particular patient group is low because small masses in the kidney tend to grow slowly and there is a very low risk that they progress to metastatic disease. The 14th EAU Central European Meeting (CEM) held in Cracow, Poland from 10-12 October, was an illustration of the high level of urological clinical care and scientific research in the region. Prof. Bob Djavan (Vienna, AT), Chairman of the EAU Regional Office, praised the high number of submitted abstracts, as well as their quality, Sedelaar stressed that not all small lesions are and proclaimed that urology in Central Europe is “at harmless and partial nephrectomy remains the gold Western European standards.” standard in young and otherwise healthy patients. Furthermore, the lack of biomarkers for kidney cancer Djavan mentioned in his opening address that the value makes it difficult to predict whether or not a tumour is of this meeting lies in the opportunity it provides to aggressive. identify key opinion leaders from Central Europe, to offer young urologists in the region a bridge to the Because of this, the role of renal tumour biopsy is also Annual EAU Congress, and, most importantly, to changing. Now that it has been established as a safe strengthen the urological network. and accurate diagnostic tool, biopsy can be important in determining histology. Only for patients who are Prof. Piotr Chlosta (Cracow, PL), Chairman of the 14th unfit for any type of active treatment is renal biopsy CEM, agreed with Djavan and said he is satisfied with unnecessary. Alternatively, patients who are unfit for the quality of the scientific programme and proud of surgery can be treated with various ablative treatment. the support he has gotten to organise this meeting. He These techniques are still experimental and require a stressed that it is the satisfaction of the participants that pre-treatment biopsy. determines the success of any meeting. Dr. Dejan Bratus (Maribor, SL) discussed treatment Attendees of the meeting were offered a full options for patients with metastatic kidney cancer. Even programme with state-of-the-art lectures on for though more randomised data is needed, surgery is instance prostate, kidney, and bladder cancer; as well indicated as a palliative approach, in combination with as hands-on training sessions, poster sessions, a systemic therapy. Studies show that immunotherapy is newly-introduced video session on various laparoscopic more effective after nephrectomy. Surgery can even be techniques of partial nephrectomy, and a Young curative if all metastases can be removed and should Urologists Competition. be offered to all patients who are fit enough for surgery. Personalised cancer treatment As of next year, Polish law mandates that cancer patients have to be treated by a multidisciplinary team. This is why the lecture of the Polish Association of Urology focused on personalised medicine in a multidisciplinary approach. Prof. Krzysztof Krzemieniecki (Cracow, PL) said that the simplest definition of personalised medicine is still the best: customised medical care for every patients’ unique condition. It is now clear that there are many different characteristics for cancers originating in the same organ. The heterogeneity of cancer is becoming more apparent. Krzemieniecki described the history of cancer treatment from blockbuster medicine via stratified medicine towards personalised medicine and predicted that the latter will become the standard approach in a few years. “We are all different,” Krzemieniecki said. “This is very obvious but it is a revolutionary realisation in cancer treatment. To take the many disease and patient characteristics into consideration, a multidisciplinary and holistic approach is necessary. The challenge is to provide equal availability of such an approach,” he continued. Kidney cancer Kidney cancer is an important topic for Central Europe because of the high prevalence of the disease in the region. This is primarily because the Czech Republic, for reasons which are still unknown, has the highest incidence of renal cancer in the world. Various aspects of this heterogeneous malignancy were discussed during a dedicated session. Dr. Michiel Sedelaar (Nijmegen, NL) talked about the indication for active surveillance (AS) in kidney cancer. He explained that, while partial nephrectomy is still the gold standard treatment, and an excellent curative option, there are reasons to investigate the possibilities of AS in specific patient groups. The need for this treatment modality has increased over the years, due to the growing numbers of low-grade One way to reduce overtreatment is by offering patients active surveillance (AS). Dr. Tomasz Borkowski (Warsaw, PL) clearly explained that AS is active treatment with curative intent. The aim of delayed treatment is to minimize treatment-related toxicity. This approach is only recommended in low or very low-risk cancers. AS is particularly suitable for patients over the age of 65. In younger patients, From left: speaker Dr. Michiel Sedelaar, with Prof. Bob Djavan and Prof. Piotr Chlosta chairing AS can be an option but radical prostatectomy has present their work to a group of judges made up of shown the best outcomes in this patient group. Even world-renowned urologists. Most competitors with very low-risk prostate cancer, younger patients benefit from surgery. The personal preference should presented research on kidney or prostate cancer but the awards went to those who covered non-oncological nonetheless always be taken into account, in any topics. patient group. In patients with high-risk prostate cancer, radical prostatectomy is the best treatment option. Prof. Günter Janetschek (Salzburg, AT) showed that surgery is better for cancer-specific survival as well as overall survival, compared to radiation therapy. Only for the treatment of distant metastases is radiation better, data shows. Dr. Béla Köves, delivering his winning presentation on Urinary Tract Infections Prof. Oliver Hakenberg (Rostock, DE) gave an overview of the latest developments in medical treatment of kidney cancer with tyrosine kinase inhibitors (TKI). A lot has been invested in research on TKI, but overall survival is not improved by these drugs. With the exception of soranifenib, axitinib and temsirolimus, which show some improvement in overall survival in patients with clear cell carcinoma, Hakenberg demonstrated that the new drugs mainly promote progression-free survival. Combination treatment of TKIs is not useful, Hakenberg continued. Additionally, it is also very expensive and appears to have no benefit on quality of life. Hakenberg concluded that it is necessary to acknowledge the palliative nature of medical treatment in renal cancer and urologists need to take the high costs of the treatment into consideration. Prostate cancer Another major topic at CEM14 was prostate cancer, because of its high prevalence and incidence. Diagnosis, active surveillance, and radical prostatectomy were the most notable topics. The greatest challenges in diagnosis of prostate cancer are to distinguish between clinically significant and insignificant tumours, to reduce the number of unnecessary biopsies, and to prevent overtreatment. “There is a need for a new biomarker,” said Dr. Peter Nyirády (Budapest, HU). This is not easy because none of the new biomarkers meet all requirements. MRI will get a more prominent role in the diagnosis of prostate cancers and can even be helpful for classification. If radical prostatectomy is the gold standard, what is then the role of robotassisted radical prostatectomy (RARP)? Djavan closed the prostate cancer session with a lecture on this topic. The latest data shows that the advantage lies in the short-term: patients treated with RARP show a quicker return to potency and continence, compared to open radical prostatectomy. Because of the favourable functional outcomes of RARP, young patients will benefit most from the treatment. High costs of the procedure are the biggest downside. Another problem mentioned by both Djavan and Janetschek is the pelvic lymph node dissection (PLND), which is essential in high-risk cases. Data shows that PLND is less often performed in patients treated with RARP compared to open radical prostatectomy. Dr. Dinko Hauptman (Zagreb, HR) won third prize with his presentation on the kidney transplantation programme in Croatia. He described the country’s donor and transplantation programme. The latter consists of 4 transplantation centres in which multidisciplinary teams operate. The donor programme is based on presumed consent and has become very successful after Croatia joined Eurotransplant: the number of donors has increased and waiting time decreased. Second prize went to Dr. Bogdan Geavlete (Bucharest, RO) for his comparative study on treatment options for enlarged prostates with a large volume. He compared bipolar resection, vaporisation, and enucleation and concluded that enucleation is most feasible in high volume prostates, whereas vaporisation is inferior in these high-volume cases. Dr. Béla Köves (Budapest, HU) won first prize in the competition for his presentation on treatment of urinary tract infections (UTI). According to Djavan the presentation was “a good example of a good presentation that is not about oncology.” Although not often thought about, UTI is common and rates of resistance are rising globally. Köves demonstrated that, in contrast to what is commonly believed and practised, asymptomatic bacteriuria (ABU) can help in the prevention of UTI. According to Köves, non-antibiotic prevention of UTI is the future. Nonetheless, he did advise to continue to treat ABU in pregnant women and before surgery in the urinary tract. “There is no doubt that the robot will come, ”Djavan concluded. It is therefore important to remember that it is a tool, and the role and skill of the surgeon remain crucial. Djavan: “A fool with a tool is still a fool.” Young Urologists Competition The Young Urologists Competition is a recently-introduced feature of the Regional Meetings, designed to give young talents the opportunity to represent their country and to Dr. Ignacy Korzelik (Cracow, PL) receiving the first prize for their paper on laparoscopic adrenalectomy CEM14 Poster Award Winners Karl Storz Awards for Best Clinical Study 1. C138 – I. Korzelik, et al. (Cracow, PL) Laparoscopic adrenalectomy. 10-year experience of a single institution 2.C50 – Z. Balory and L. Pajor (Szeged, HU) Aesthetic reconstruction of the penis after tumor resection 3.C131 – A. Minich et al. (Minsk, BY) Predictors of postoperative mortality after radical cystectomy Berlin Chemie Awards for Best Basic Research 1. C78 – A.S.C. Rascu et al. (Bucharest, RO) Genetic studies on Romanian prostate cancer patients confirm genetic risk variants for prostate cancer 2.C144 – R. Sobotka et al. (Prague, CZ) New potential tumor markers for primary diagnosis of kidney tumors 3.C33 – O. Banya et al. (Lviv, Kyiv, UA) Does cell phone radiation have a bad effect on semen quality? A laparoscopic hands-on training session at the CEM2014 October/December 2014 European Urology Today 19 10th SEEM reflects region’s growing role in urology Participants from 44 countries gather in Belgrade By Joel Vega With a nod to the region’s growing stature in international urology, Regional Office Chairman Prof. Bob Djavan (AT) acknowledged the contributions and innovative work from South Eastern Europe during his opening remarks at the 10th South Eastern European Meeting (SEEM) in Belgrade, Serbia. Around 500 participants gather in Belgrade from October 24 to 26 this year for the annual meeting, the third time the Serbian capital is hosting one of the Regional Office’s frontline events. With Professors Sava Micic (RS) as meeting chairman and Aleksandar Vuksanovic (RS) co-chairing the event, Djavan underscored the influence of urologists from the region. “In the last couple of years I am happy to see that the SEEM has evolved to a more inclusive and dynamic event, not only gathering more participants, but also providing the necessary platform to both young and veteran urologists in the region. Your work and active contributions have made this meeting a success,” Djavan said. (TR) spoke on the benefits of AS particularly for elderly patients and those with co-morbidities for which aggressive therapies only increase lifethreatening risks. “AS remains an option but age, disease stage and co-morbidities are key aspects that need to be carefully examined by doctors. Most of these SRMs have a lower malignant potential and are defined as predominantly solid enhancing tumours less than 4 cm in maximal diameter(cT1a),” said Huri. New trends First-day roundtable discussions and debates tackled topics such as ischemia in partial nephrectomy, AS in young men with localised PCa, diagnostic markers in PCa, new imaging techniques and current trends and prospects in biopsy. Among the key messages from the lectures focused on prostate cancer. Dr. Theodore Anagnostou (GR) spoke on new developments in PCa biopsy, and said that despite the emergence of new techniques such as MR-US (ultrasound) fusion-targeted prostate biopsy, the caution from guidelines and high equipment costs have reigned in the wider use of these techniques. Noting the rapid changes in imaging techniques, Anagnostou discussed multi-parametric ultra sound (US), or enhanced US in combination with elastography, which in some cases unfortunately carries a significant number of false negatives. “Elastography is a promising tool with the potential to assist detection. However, the results are still inconsistent. Besides, elastography is not recommended for initial biopsies in the EAU Guidelines,” he said. Prof. Vuksanovic, co-chairing the SEEM meeting The two-and-a-half day meeting took up a range of topics including uro-oncology, andrology, female urology, stone disease and paediatric urology, to name a few, in a scientific programme that features debates, panel discussions, a Country Competition, poster and video sessions and a hands-on training in laparoscopy co-organised by the EAU Section on Uro-Technology (ESUT). The European School of Urology also presented a course in andrology and incontinence with overview lectures on erectile dysfunction, stress incontinence and male infertility. Djavan gave the EAU Lecture on salvage lymph node dissection in prostate cancer during the opening session, and hammered on the message that although a viable option, salvage LND requires careful patient selection and the use of suitable imaging techniques. “The rationale for salvage LND might reside in the nodal metastasising spread of PCa which still needs to be investigated, and the requirement for any non-systemic salvage approach is the availability of accurate and sensitive imaging modality for detecting nodal recurrence,” he said. A debate on the management of small renal masses (SRMs) followed, and complemented by lectures on partial nephrectomy, active surveillance (AS) and minimal invasive treatments of SRMs. Prof. Emre Huri Participants from 44 countries gathered in Belgrade 20 European Urology Today Prof. Raja Khauli (LB) discusssed new PCa biomarkers and strategies while Prof. Axel Heidenreich gave succint overview lectures on AS in young PCa patients and hormone therapy for PCa. “Active surveillance is an option but there are still a lot of questions,” said Heindenreich as he noted that molecular characterisation of biopsy specimens is necessary to identify aggressive cancers. Following the poster and video sessions, a panel discussion focused on robotic and laparoscopic surgery, with the panellists and audience examining issues on robotic surgery in high-risk disease and whether laparoscopy is losing ground to robotic procedures. Country Competition A well-attended and new feature in the regional meetings, the Country Competition took centre stage on the second day with 10 young urologists discussing innovative approaches and findings during 10-minute presentations before a 12-man jury. The contest line-up was composed of 10 presenters from nine countries with Turkey fielding two candidates. The challengers were: Uros Bumbasirevic (Serbia), Denis Godaj (Albania), Ahmet Güdeloglu (Turkey), Evangelos Fragkiadis (Greece), Osman Hadžiosmanovic (Bosnia & Herzegovina), Ilija Kelepurovski (Macedonia), N. Narimanikali (Iran), Tayfun Oktar (Turkey) and Prodromos Philippou (Cyprus). Topics included testis, penis, prostate and kidney cancers, female urology, incontinence and stone disease. Dr. Bumbasirevic of Serbia won the top prize for his discussion on quality of life (QoL) of testis cancer survivors, a seldom-made study in which he recommended that doctor’s close follow-up and assessment of the patient’s QoL issues can make a difference in their therapy. V. Kojovic (middle) receives the Karl Storz First Prize for Best Poster from Profs. Djavan (L) and Sava Micic K. Mytilekas (middle) receives the Berlin Chemie First Prize for Best Poster from Profs. Djavan (L) and Micic O. Ivanovski (R) receives the first prize for Best Video from Prof. B. Djavan Uros Bumbasirevic (middle) receives the Country Competition First Prize from Profs. Djavan (L) and Sava Micic Bladder cancer was highlighted in the second day with lectures on new imaging tools in superficial bladder cancer and controversies in high-risk non-muscle invasive bladder cancer (NMIBC), given by Profs. Gunter Janetschek (AT) and Levant Turkeri (TR), respectively. sessions. From the accepted abstracts, 171 or more than half were submitted by participants from Turkey. Accepted abstracts came from at least 30 countries, with some of the submissions coming from as far as Taiwan, South Korea and Egypt. Researchers from the host country and Greece also topped the list of high submissions. Top winners for the best poster presentations were from Serbia, Greece and Macedonia (See list of winners). In his take-home messages, Janetschek said PDD remains the standard tool by far, and new tools such as SPIES, although easily available and with enhanced vision, still has missing data, with its value still unclear. Confocal laser endomicroscopy, on the other hand, remains experimental but has potentials in combination with PDD/NBI/SPIES. Turkey also topped this year’s abstract submission, with around 324 abstracts accepted for presentations in 14 poster Profs. Bob Djavan (L) and Sava Micic during the first plenary session Serbia, Greece and Macedonia win first prizes Serbia topped the Country Competition and also reaffirmed its dominant performance in the best posters and video prizes which went to Serbia, Greece and Macedonia. Mid-East countries such as Kuwait, Iran and the United Arab Emirates also did well, bringing home four of the runner-up prizes. Below is the complete list of winners: Berlin-Chemie Best Poster Awards 1st Prize: K. Mytilekas, et al., “Evaluation of two novel urodynamic parameters in the diagnosis of female obstructive voiding" (Thessaloniki, Greece) Country Competition 1st Prize: Uros Bumbasirevic (Serbia) 2nd Prize:Tayfun Oktar (Turkey) 3rd Prize: Prodromos Philippou (Cyprus) 3rd Prize- Co-winner: M. Ortac, et al., “Effects of low-energy shockwave therapy on angiogenesis factors at the penile tissue of diabetic rat,” (Istanbul, Turkey) 3rd Prize- Co-winner: S. Bajramovic, et al., “Surgery for incidental adrenal mass,” (Sarajevo, Bosnia and Herzegovina) Karl Storz Best Poster Awards 1st Prize: V. Kojovic, et al, “Reversal surgery in regretful male to female transsexuals after sex reassignment surgery," (Belgrade, Serbia) 2nd Prize: M. Al-Kandari, et al, “Loupe - assisted varicocelectomy with testicular delivery and proximal spermatic cord occlusion with a tourniquet for primary infertility” 3rd Prize-Co-winner: S. Shamrayev, et al. “The prostate tissue changes in patients with BPO after medical treatment (Donetsk, Ukraine) 3rd Prize- Co-winner: H. Aboutaleb, “Role of the urethral plate characters in the success of tubularized incised plate urethroplasty” (Al Ain, United Arab Emirates) 2nd Prize: S. Saidi, et al., “Microsatellite instability in urinary bladder cancer,” (Skopje, Macedonia) Best Video Awards 1st Prize: O. Ivanovski and B. Shabani, “Reconstruction of complicated urethral stricture in two stages with buccal mucosal graft” (Skopje, Macedonia) 2nd Prize: O. Alhunaidi, “Filarial epididymitis diagnosed by Filarial dance sign,” (Farwaniya, Kuwait) 3rd Prize: K. Tavakkoli Tabassi, “Fold back perineo-scrotal flap plus penile inversion vaginoplasty,” (Tehran, Iran) October/December 2014 Comprehensive ESU course on male LUTS Hungarian Society of Urology offers ESU course in 19th Annual Congress Dr. Károly Nagy Jahn Ferenc Dél-pesti Kórház Dept. of Urology Budapest (HU) dr.nkaroly@ gmail.com The European School of Urology (ESU) organised a course on complex therapy (conservative and surgical) of the non-neurogenic male LUTS at the 19th Congress of the Hungarian Society of Urology, and elicited enthusiastic response for its comprehensive programme from both participants and congress delegates. Knowledge of this topic is essential to the daily practice of urologists since Lower Urinary Tract Syndrome (LUTS) represents one of the most common clinical complaints in adult men. Course participants included the registered congress attendees and Hungarian residents in urology. The high-quality, well-structured thematic discussions included lectures by Prof. F. Van Der Aa (BE) and Prof. G. R. Kasyan (RU) whose presentations examined the topic clearly and concisely. and detrusor underactivity. In addition, many other conditions may also contribute to LUTS,” he said. Prof. Van Der Aa examined clinical assessment. “The first focus is to determine the specific nature of the LUTS of the patient (storage, voiding and postmicturition). The correct assessment helps the clinician to diagnoses and follow-up the patients,” he said. In his second lecture, Prof. Kasyan gave an overview of urodynamics studies in men. “The major aims of these studies are to explore the functional mechanism of LUTS and to identify potential risk factors for adverse outcomes. Most terms and disease condition are defined by urodynamics,” he said. In the second half of the course the medical and surgical treatment and their complications were highlighted. Prof. Van Der Aa spoke on conservative and medical treatments. “To give the best treatment to patients, it is necessary to perform a good history and clinical assessment in order to stratify the patients to the possible therapies. Depending on the spectrum of complaints, the risk of progression, the presence of complications and the potential side effects and cost of certain treatment, patients will be offered different possibilities,” he noted. The first half of the course examined pathophysiology and the investigation and evaluation of symptoms. Kasyan discussed pathophysiology and explained how the medical practice and patient management have evolved in the last decade. He underscored that urologists should treat the patient based on individual management and not only on diagnosis. ”LUTS are not necessarily related to prostatic pathologies. Various types of bladder dysfunctions may also be involved in the pathogenesis of LUTS, such as detrusor over-activity, impaired contractility Prof. Kasyan discussed surgical and minimally invasive therapies for male LUTS. Kasyan: “The choice of treatment depends on the assessed findings of patient evaluation, ability of the treatment to change the findings, treatment preferences of the individual patient, and the expectations to be met in terms of speed of onset, efficacy, side effects, QoL and disease progression. Transurethral resection of the prostate remains a golden standard treatment of patients with enlarged prostates.” In the last presentation Prof. Van Der Aa discussed complications from therapies. “Even when no treatment for male LUTS is offered, complications can occur. All treatment decisions can have a complication. With a good follow-up of the patient the vast majority of these complications can be dealt with accordingly,” he said. quirky cases, which led to in-depth discussions and debates. After each part of the course, a one-one case discussion was presented by Dr. Á. Tordé and the author. Both presentations described interesting and We are grateful to the ESU for organising this quality course which improved our knowledge and help us offer quality management to our patients. Prof. Kasyan thanked by Prof. Tenke Win a free registration to Madrid in 2015! EU-ACME members, join the MCQ quiz published in European Urology ESU faculty Prof. Frank Van Der AA and Prof. George Kasyan For details, visit: www.eu-acme.org/europeanurology European School of Urology www.baltic15.org Teaching activities 2015 BALTIC15 February 2nd EAU Baltic Meeting 1-6 7-10 Hands-on training skills programme on Laparoscopy and Endourology, Caceres (ES) European Urology Forum 2015 – Challenge the experts, Davos (CH) March 29-30 May 2015, Riga, Latvia 20-24 EAU meetings and courses are accredited by the EBU in compliance with the UEMS/EACCME regulations ESU Courses, HOT, Education and Innovation at the time of the 30th Anniversary EAU Congress, Madrid (ES) May 30 ESU course at the time of the EAU Baltic Meeting, Riga (LV) July 5-11 ESU – Weill Cornell Masterclass in General urology, Salzburg (AT) September 3-9 13th European Urology Residents Education Programme (EUREP), Prague (CZ) ESU Organised courses at National Urological Society meetings December 2014 14 ESU organised course on LUTS and incontinence: Where is the truth? at the time of the national congress of the Georgian Association of Urology, Tbilisi (GE) June 11 19 Call for Abstracts ESU organised course at the time of the national congress of the Slovak Urological Association, Presov (SK) ESU organised course on Prostate cancer at the time of the national congress of the Ukrainian Urological Association, Kiev (UA) October 23 Deadline 1 April 2015 ESU organised course at the time of the national congress of the Moldavian Urological Society, Chisinau (MD) November European Association of Urology October/December 2014 2 ESU organised course at the time of the national congress of the Scientific Society of Urologists of Uzbekistan, Tashkent (UZ) Contact: [email protected] ESU courses are accredited within the programme by the EBU with 1 credit per hour European Urology Today 21 ESU-Weill Cornell Masterclass in historic Salzburg Collegial atmosphere in an intensive, quality masterclass Dr. Kees Hendricksen NKI - Antoni van Leeuwenhoek Hospital Dept. of Urology Amsterdam (NL) k.hendricksen@ nki.nl It is Sunday, July 6, 2014 and I am travelling from Amsterdam, The Netherlands to Salzburg, Austria to attend the 10th European School of Urology (ESU)Weill Cornell Masterclass in General Urology. The week-long Masterclass is a collaborative programme of the ESU and the Weill Medical College of Cornell University which aims to provide a high-level post-graduate medical education programme on general urology for highly-qualified, English-speaking physicians from Central- and Eastern Europe, Russia, Central Asia and other countries in transition. Under the auspices of the Open Medical Institute (OMI) – Salzburg Medical Seminars International (SMSI), a programme of the American Austrian Foundation (AAF), the master class is annually held in Schloss Arenberg in Salzburg, Austria. This year, 156 candidates applied via the AAF, and 47 candidates applied via the ESU (which I did), of which 36 young lucky urologists were selected. The participants originated from Albania (2), Armenia, Belarus, Belgium, Bulgaria, Croatia (2), Czech Republic, Estonia, Germany, Greece, Hungary, Italy, Kosovo (2), Mexico, Republic of Moldova, the Netherlands, Romania (2), Russian Federation (2), Serbia, Spain (2), Switzerland, Tajikistan, United Republic of Tanzania, Turkey (3), Ukraine (2) and Uzbekistan (2). Due to the international heterogeneity of the group, the programme inevitably sharpens the English language skills of the participants as they learn from each other’s urological practices. On Sunday evening, W.K. Aulitzky (Vienna), AAF medical director, warmly welcomed all participants and faculty members, and hinted that it will be a week of extensive scientific information, interaction, network-building opportunities and the start of new friendships. A toast to that! disease: diagnosis, medical treatment and prevention of stone disease, and ureterorenoscopy, percutaneous surgery and laparoscopic surgery to treat stones. J.C. At the start of the week we took a pre-seminar Coleman (New York) discussed the management of multiple-choice test (and at the end of the week a localised and advanced kidney cancer. The medical post-seminar test was also taken) to examine our management and surgical treatment of BPH were knowledge-gap and prompt all participants to actively covered by C.R. Chapple (Sheffield) and B. Van contribute to the course. During the week, major Cleynenbreugel (Leuven). State-of-the-art in urethral topics were clustered in the morning and presented stricture surgery was covered by C.R. Chapple. Finally, by the American–European faculty. D.S. Scherr (New W.K. Aulitzky lectured on mentoring in medical York), T.W. Jarrett (Washington) and S.F. Shariat education and metabolic syndrome in urology. (Vienna) covered prostate cancer, and discussed topics such as screening in prostate cancer, imaging in and Case presentations treatment of localised prostate cancer, and treatment For the afternoon sessions, each participant prepared of high risk and castrate resistant prostate cancer. J.S. a case presentation, of which the five best cases were Sandhu (New York) covered management of urinary selected for the online library of the OMI. These were incontinence and impotence after radical subdivided into the topics that were lectured in the prostatectomy. morning. Since the group is mixed one can imagine that the case selection varied from astonishing to F.M.E. Wagenlehner (Gießen) and J. Angulo (Madrid) extraordinary, sometimes almost hilarious to deadly took up urological infections, including antibiotic serious, and from basic care in general urology to the prophylaxis in urological surgery, the increase in most exquisite treatment opportunities in highly antibiotic resistance, acute and chronic cystitis, and specialised urology. For example, there was a case the diagnosis and management of venereal diseases. where a shepherd got urethral trauma after he was T.W. Jarrett (Washington), B. van Cleynenbreugel attacked by a buffalo, or another case of traumatic (Leuven) and G. Janetschek (Salzburg) covered stone partial penectomy and penile reconstruction case ESU-Weill Cornell Masterclass in General Urology Excellent programme impresses Turkish urologist Dr. Ege Can Serefoglu Bagcilar Training & Research Hospital Department of Urology Istanbul (TR) Drs. B. Van Cleynenbreugel and G. Janetschek provided updates on stone diseases. Prof. Chris Chapple gave an overview on the management of benign prostatic hyperplasia and urethral stricture disease. Aside from the lectures, the participants took part in hands-on training in laparoscopy and endourology courses sponsored by Olympus Europe. egecanserefoglu@ hotmail.com Educational activities were not limited to the lectures already mentioned. Cases, which were presented by the participants, led to intense debates and increased our awareness regarding the urology practice in other parts of the world, from USA, Uzbekistan, and Mexico to Tanzania. We even discussed various topics with the lecturers during the meals and after the sessions in the evenings. The diverse nationalities of the participants also provided an excellent opportunity for cultural exchanges. FIFA World Cup matches clearly increased our excitement during the event. Salzburg, the inspiring city and birthplace of Wolfgang Amadeus Mozart, hosted 36 young academic urologists from all over the world for the ESU-Weill Cornell Masterclass in General Urology in July 2014. This one-week high-level programme is designed for young academic urologists and included state-of-theart lectures, case discussions and laparoscopic hands-on training sessions. The participants obtained full scholarship and enjoyed the beauties of the city while benefiting from the scientific programme with world renowned urology experts as faculty members. The breathtaking masterclass venue, Schloss Arenberg, was a recently renovated 19th century palace within walking distance to downtown Salzburg. Attending the lectures in such a historical atmosphere was absolutely a pleasant experience. The masterclass started with the welcome message from Prof. Wolfgang Aulitzky and followed by lectures from Drs. Douglas Scherr, Thomas Jarrett, Shahrokh Shariat and Jaspreet Sandhu. They presented various topics related to recent advancements in prostate cancer treatment. During the rest of the course, Dr. F Wagenlehner gave a summary of infectious diseases in urology while 22 European Urology Today after “circumcision at home by master.” Having such a case mix, it did not matter from which country participants were originating since there were ample opportunities to learn from each other, with enough room to ask questions. All participants were very respectful, open and willing to share ideas and opinions. In two other afternoon sessions, the group was split to experience hands-on laparoscopy and endourology training on various excellent training models, coached by B. van Cleynenbreugel and T. Kalogeropoulos. Participants who had the afternoon off visited the Salzburg’s beautiful historic city centre. We also enjoyed the wonderful Schloss Arenberg, which we had for ourselves the whole week. An evening chamber concert of classical music was also held in the castle’s premises. After such a delightful week I can only recommend young urologists to apply for this free ESU course. It gave me a warm feeling that after an educative week, our diverse group had become more homogenous due to the collegial spirit and true friendships we have formed. www.esusalzburg15.org ESU - Weill Cornell Masterclass in General urology 5-11 July 2015, Salzburg, Austria EAU Events are accredited by the EBU in compliance with the UEMS/EACCME regulations The ESU-Weill Cornell Masterclass provided an excellent overview of the latest updates and knowledge in general urology while enabling participants to connect with their colleagues and develop new friendships. I strongly recommend all young academic urologists to apply for this exceptional programme and take advantage of a unique opportunity. European Association of Urology October/December 2014 ESU offers comprehensive course to Armenian urologists Participants appreciate key updates on functional urology Dr. Ruben Hovhannisyan Head, International Relations Office, Armenian Association of Urology Yerevan (AM) ruben_hovhannisyan@ yahoo.com On September 26, 2014 the Armenian Association of Urology’s 2014 Annual Meeting opened with a course organised by the European School of Urology (ESU), a much anticipated and well attended course that has become a mainstay in the programme of the Armenian national meeting. To Armenian urologists the ESU Course is a highlight and we always look forward to these courses since it serve both educational and cultural aims. By cultural, we mean professional cultural development of the audience. Events like the ESU course have also taught several generations of urologists to adhere to unified standards of professional approaches. Moreover, these courses can serve as a “bridge” between generations, since gaps in training and knowledge are not only addressed but also skills and expertise are shared or disseminated among the country’s urologists. Holding these courses also demonstrates the aim to maintain high quality professional standards, and provide the necessary support to the goal of making our specialty a stronger medical discipline. Certainly, the ESU Courses also provide the opportunity for us to train our younger colleagues and thus contribute to the general objective of boosting the influence, scope of practice and expertise of urology. To us these are the multi-faceted goals and accomplishments of organising the ESU courses, making this event an ideal platform upon which urologists in Armenia can acquire new skills. By keeping us updated with the latest information, procedures and research findings we can find our place in the bigger and professional medical world. The ESU course last September, headed by Prof. Aulitzky, has definitely left an indelible mark in Armenian urologists, having enriched us with new skills and advanced knowledge. Among the course topics are the functional aspects of urinary and sexual (both male and female) disorders. The topics were not only carefully selected, but the lectures also examined core issues and salient aspects. Course participants expressed their satisfaction over the very interactive and enthusiastic discussions, with the session moderators and presenters doing their best to stimulate the audience and address their queries. Organisers of the Armenian Association of Urology and faculty of the ESU course gathered on the opening day of the meeting Prof. Aulitzky, Ms. Anna Maria Nics, Karina Van Lenthe (EAU) en Dr. John Heesakkers at the 9th century Island Monastery of Sevanavank The session on functional urology also tackled normal functionality, how disorders arise and various issues in dysfunction, which is a hugely heterogeneous topic. The organisers also achieved their aim to present a course where the emphasis is more on the quality of content and that the key messages, both practical and theoretical, are clearly conveyed to and learned by the participants. Undoubtedly, the team of Prof. Aulitzky has done a great job. On behalf of the Armenian Urological Association, we are grateful to our guests and lecturers, Prof. Aulitzky, Drs. John Heesakkers and George Kasyan. Our special thanks to Ms. Karina van Lenthe for her dedication and to the EAU leadership for their support and commitment to urology in Armenia, and to all those who participated, contributed and made the event a big success. Simulation fellowship: growth of a new research field Understanding the technical aspects of surgical skills Dr. Domenico Veneziano Ospedali Riuniti BMM Dept. of Urology and Kidney Transplantation Reggio Calabria (IT) info@ domenicoveneziano.it I left my daily surgical practice in October 2013 to start a one-year research fellowship at the University of Minnesota, Minneapolis, USA. Making the decision to put my surgical practice on hold is difficult, as the fear of having your surgical skills atrophy is high when you plan to dedicate all your working time to something else, even for just one year. medical school lectures, train-the-trainer sessions, practical skills building and simulation centre management. After the first few weeks I began to understand that “training” was not just performing basic tasks or sessions on pig/cadaver. Simulation in urology can be considered as a whole new field of research that finds its roots in a deep understanding of our everyday procedures. To understand these even better, it is often useful to perform a “cognitive task analysis” (CTA), a procedure that facilitates the deconstruction of the surgical procedure in steps. Once the CTA is completed, there is a multidisciplinary collaboration, which leads to the design and ultimately creation of one or multiple dedicated simulators. The possibilities offered by SimPORTAL from this point of view are endless. The aim was to follow my passions and to focus on something I’ve always loved: education and simulation technologies. SimPORTAL (Simulation PeriOperative Resource for Training And Learning) offered me every tool I could dream of to deepen my knowledge about surgical training. The centre is directed by Dr. Robert Sweet, a urologist renowned in the United States as a pioneer in training and simulation. Thanks to his dedicated work, SimPORTAL is today the only place in United States where a multi-disciplinary group of uniquely talented experts works everyday to find novel solutions in the field of medical education. The team includes surgeons, clinician educators, educational psychologists and psychometricians, electrical/mechanical/biomedical engineers, graphic artists, make-up artists, manufacturing and sales/ marketing experts, all paired with military collaborative research efforts and funding. The fellowship provided is the first simulation programme accredited by the American College of Surgeons (ACS) and incorporates several activities: simulator development, curriculum development, October/December 2014 Anaplastology lab The anaplastology lab, directed by Troy Reihsen, attracted my curiosity from the very beginning. Synthetic body parts, airway models, ureteral models for endoscopy were just a part of the number of prosthetics one could find in this dedicated laboratory. The process to follow in order to create a synthetic organ, has been one of the most valuable things I have learned at the University of Minnesota, where the starting point is always the patient. After acquiring the anatomy with 3D imaging, the graphic artist needs to “digitally clean” organs that are then 3D printed to create a solid model. When more detail is needed, the make up artists add additional effects manually with clay, starting from surgical pictures or actual ex vivo models. The consistency of silicones to be used, as well as their colours, are then chosen starting from the internal “tissue property database.” This dataset holds different information acquired by several ex vivo tissue samples. This process allows the synthetic tissues to behave as close as possible to the real ones, giving more value to the training sessions. Working part of my time in close collaboration with the team, I quickly learned how to sculpt clay, build a mould and choose the right silicon, in order to create the models I wanted to. In this phase the help of my wife, who left her job in Italy to follow me in this adventure, has been critical, as she decided to volunteer at the University and learn with me the art of creating a training model from scratch. Her collaboration is very important when I decide to replicate this knowledge base elsewhere. With Dr. Robert Sweet, director of SimPORTAL of assessment and validation. In this field, the presence of several engineering companies around Minneapolis has been beneficial: to assess a practical exercise advanced technologies are often useful. “It’s not the tool, it’s the tissue,” Dr. Sweet often reminds me, and this is why the use of sensors is fundamental to assess our respect for tissues during a simulated procedure and, finally, to assess its correct accomplishment. In case a physical simulation model does not fit the specific needs of a training session, a team of engineers inside SimPORTAL can be involved in the creation of a virtual simulator, which previously occurred for the AMS Greenlight simulator in 2011. My wife Cristina modelling clay in the anaplastology lab After almost one year of research in the vast field of medical training, I can say that not only do I know more about education, but I also understand more now the technical aspects of my surgical skills. This has left me without any doubt as to the Another fundamental part of my simulation path I have chosen in coming to the University of fellowship was the improvement in my understanding Minnesota. European Urology Today 23 • What do you think is the biggest challenge in urology? It’s adapting to the very rapid changes in our work environment, most of which are totally fascinating such as image-guided therapy. The definition of a surgeon is changing very quickly and not everyone is prepared to make the change. • If you were not a urologist, what would you be? My answer would change every five years. Recently, I have been interested in permaculture which is using building materials and other things in a sustainable way such as agriculture. I have some experience in innovative business. But I have no regrets about urology. • What is your most important piece of advice for doctors just starting out today? I don’t like to preach but I feel it is important for young people to identify role models to learn from. It is also important to realise your life will have many different phases and that your values may change. • What is the most rewarding aspect of being a doctor? The freedom to do what I wanted to do, not to work for anybody and to interact with a lot of very smart people. • What is your advice to other physicians on how to avoid burnout? I always have had trouble with this concept of work-life balance, because to me they’re the same thing. I never really thought of burnout. • If you could change something in the healthcare system, what would it be? There’s a great deal of inertia in the healthcare system. The information systems we use are grossly inadequate. The medical profession should be more conscious of where the financial resources are coming from and how they’re used. • What’s the last wonderful book you have read? I am interested in the impact of architecture on people’s lives. Christopher Alexander wrote “A Pattern Language: Towns, Buildings, Construction,” which is about architecture, urban design and liveability. • What’s the last thing that surprised you? The reaction of voters in national elections sometimes amazes me. As a North American I don’t understand the European concern about immigration. I live in a city where over 50% of the citizens were born overseas. • What’s your favourite hour in a day and why? I have two favourite times— when I wake up early in the morning and have my cup of coffee, and at the end of the day just reflecting or having a quiet time. • What do you most often wish you could say to patients, but didn’t? TEN QUESTIONS Interview by Joel Vega Photography by Jack Tillmanns Specialty: Uro-oncology City: Toronto, Canada Recent Awards: CUA Award, Queen’s Diamond Jubilee Medal from the Canadian Medical Association, AUA Honorary Member & Distinguished Contribution Award, SUO Medal Obviously, the biggest problem is when you know somebody is going to die and you can’t really tell them the whole story. Michael Jewett Masterclass in advanced 3D video-assisted urological surgery ESUT event in Braga, Portugal draws enthusiastic trainees Prof. Riccardo Autorino University Hospitals Case Medical Center Dept. of Urology Cleveland (USA) [email protected] Prof. Estevão Lima Hospital of Braga Dept. of Urology Braga (PT) estevaolima@ ecsaude.uminho.pt As part of its goals to promote minimally invasive surgeries, the EAU Section of Uro-Technology (ESUT) co-organised the Masterclass in Advanced 3D-Video-Assisted Urological Surgery, a two-day Faculty members Kris Maes and Burak Turna were tutors in the hands-on session EAU Section of Uro-Technology (ESUT) 24 European Urology Today educational course held from July 11 to 12, 2014 in Braga, Portugal. to ask questions regarding the procedures. The hands-on training sessions, which were a highlight of the course, were held at the Karl Storz Training Center, permanently hosted at the Minho University laboratories. The laboratories are equipped with unique cutting-edge training facilities for a variety of hands-on courses in various surgical specialties. Braga, one of Portugal’s biggest cities and called during the Roman Empire as “Bracara Augusta,” is renowned for its history and rich cultural legacy. Braga is also home to the School of Health Sciences of University of Minho, an internationally known academic centre. The centre’s faculty is involved in many initiatives and projects both in basic and clinical research, as well as educational events for students, residents and healthcare providers. This year the 5th edition of the course was directed by Prof. Estevao Lima, chairman of the Urology Department at Braga Hospital, Riccardo Autorino (Urology Institute, University Hospitals, Cleveland, OH, USA) and Jens Rassweiler (chairman of the ESUT and chairman of the Urology Department, SLK-Kliniken, Heilbronn, Germany). The course was part of the 2014 International Postgraduate Program of the University of Minho Surgical Sciences Research Domain, coordinated by Prof. Jorge Correia-Pinto. Each year well-known experts in minimally invasive urologic surgery join the faculty. This year’s international guests were Professors Burak Turna (Turkey), Pilar Laguna (Netherlands), Rafael Sanchez Salas (France), Salvatore Micali (Italy), Marco De Sio (Italy) and Rocco Damiano (Italy). A team of national faculty members from across Portugal have also actively contributed to the success of the course. Faculty members: Estevao Lima, Rocco Damiano, Maria Pilar Laguna, Burak Turna, Salvatore Micali, Riccardo Autorino, Marco De Sio interactive discussions. The live surgery session was held at the recently opened 700-bed Braga Hospital. Three procedures were performed: a 3D laparoscopic nephrectomy (B. Turna), a 3D Millin simple prostatectomy (E. Lima) and a laparoscopic partial nephrectomy (De Sio and Autorino). The participants followed the surgeries in small groups directly in the operating rooms, enabling them Under expert guidance, the participants performed laparoscopic kidney procedures in living animal models for a total of eight hours of hands-on training experience. The most recent tools and instruments supplied by the two main sponsors of the course, Karl-Storz Endoskope and Ethicon, were available for testing during the hands-on sessions. Once again, the Braga ESUT-sponsored course fulfilled its promise of providing a full and comprehensive update on the latest advances in laparoscopic urologic surgery. We look forward to more participants for the 2015 course, which will be held concurrently with the national meeting of the Portuguese Association of Urology. The masterclass offered practical surgical exercises with standard laparoscopic techniques as well more recent technology and instrumentation, including mini and 3D laparoscopy. Lectures, live surgeries and hands-on training were also offered. The lectures provided not only practical insights but also a rich video content which highlighted, in a step-by-step manner, the most commonly performed laparoscopic procedures in urology. In addition, tips and tricks were provided by all faculty members with the trainees participating in Participants and faculty members in the hall of the School of Health Sciences of University of Minho October/December 2014 State-of-the-art urological surgery in Heidelberg ‘Semi-Live 2015’- an innovative congress format From January 29 to 31, 2015, Heidelberg, Germany will host an innovative congress. “Semi-Live 2015” will gather internationally-renowned surgeons, including prominent EAU Section of Uro-Technology (ESUT) members, who will present videos of complex procedures with live commentary. Complemented by hands-on workshops, a faculty of surgeons will present the state-of-the-art videos of procedures in urologic oncology, reconstruction and stones. In collaboration with ESUT, the experts will take up anatomical landmarks, access strategies, important steps, elegant tricks, pitfalls and complication management, all in dynamic and interactive discussions. The video recordings are carefully selected and edited so that the resulting 15 minutes of high-definition videos, per speaker, will prompt enthusiastic response techniques. Workshop sessions will be held on Thursday, 29 January. Participation is limited and slots will be offered on a ‘first-come, first-served’ basis. The congress venue from January 30th to 31st, 2015 will be at the Communication Center of the German Cancer Research Center (DKFZ), Im Neunheimer Feld 280, 69120 Heidelberg, Germany. All presentations will be in English. from the audience. Each presentation will be followed by sufficient time for discussion. The faculty will also be available for specific questions in the "Speaker’s Corner," providing the participants to carefully discuss and examine the smallest details. Additional in-depth knowledge can be gained in the workshops which will feature hands-on training in the most widely used laparoscopic urological EAU Section of Uro-Technology (ESUT) ‘Surgery is at the heart of urology,’ said Prof. Markus Hohenfellner. ‘And urology has been one of the most innovative surgical specialties in modern medicine for the last 100 years.' Today, urologists manage indications in oncology, reconstruction, kidney stones, BPH, and andrology by open, laparoscopic, robotic, endourological, shock wave or microscopic procedures. This has led to a wide range of indications and procedures that creates a big number of treatment options. focuses on contemporary state-of-the-art procedures, providing urology professionals an effective navigation tool in an ever-changing, complex surgical landscape. Additionally, the topics of intestinal anastomosis and intra-abdominal vascular repair techniques will also be highlighted as important urological tools. ESUT Chairman Prof. Jens Rassweiler, who will participate as speaker and moderator, said: “ESUT is very happy to support this outstanding event and I look forward to welcome many EAU members to Heidelberg in January 2015.” Congress fee is €350. The programme has been submitted to the LÄK Baden-Württemberg and also to the EUACCME for CME points. For additional information and details on the programme and online registration, visit the event website at www.semi-live2015.com. With these challenges, the programme of Semi-Live 4th International Course on Advanced Laparoscopic Urology Cluj, Romania, hosts advanced laparoscopy course petrutbogo@ yahoo.com From 25 to 27 September 2014, Cluj hosted for the fourth year in a row the International Course on Advanced Laparoscopic Urology. In this beautiful university city, located in the heart of Transylvania, a group of friends and former fellows in Heilbronn decided to share their knowledge on minimally invasive surgeons by organising the course under the auspices of the EAU Section of Uro-Technology (ESUT). The course was held concurrently with the 28th International Applied Advanced Laparoscopy Course of the Turkurolap Society coordinated by Professors Yassar Ozgok and Lutfi Tunc from Ankara, Turkey. The course in Cluj gathered together an international team of trainers from six countries: Romania, Turkey, Norway, Germany, France and UK, and supervised by our honorary presidents Profs. I. Coman and Y. Ozgok. surgical techniques presentation and 3D live surgery performed this year by our special guests, namely: Prof. Antonio Alcaraz (ES), Prof Evangelos Liatsikos (GR), Prof. Lutfi Tunc (TR), and by the host, Dr Bogdan Petrut (RO). At the end of the course, the organizers invited the European School of Urology (ESU) to offer an EBLUS exam where trainees can measure objectively their level of training in laparoscopic manoeuvers. All 30 trainees worked in groups of two with an animal model, guided by a trainer, and were tasked to perform two sessions (of two hours) of live animal training (radical nephrectomy and tissue suture and/ or ureteral / bladder anastomosis). The live surgery day presented four live operations. The event was credited by the EAU with the EAU live surgery event endorsement. The first operation was a pro peritoneal laparoscopic radical prostatectomy performed by Dr. Petrut and his team followed by Prof. Evangelos Liatsikos who led a single port adrenalectomy. Prof. Lutfi Tunc performed his own technique of a 15- minute radical nephrectomy followed by Prof. Antonio Alcaraz who demonstrated Using the training facilities of the University of Medicine and Pharmacy from Cluj we organised a programme with four sections: dry lab (EBLUS exercises), wet lab (alive animal training), theoretical EAU Section of Uro-Technology (ESUT) Aspect from the live surgery transmission 3D Make fewer passes, use fewer products, and reduce costs. ™ a 3D kidney tumour enucleoresection. The operations took place in the Oncological Institute from Cluj Napoca in two operating theatres and were transmitted live 3D into the amphitheatre with the group of trainees. Given that laparoscopic surgery is a team work, we organised this year a section for scrub and intensive care nurses, with their participation free of charge. During the live surgery an experienced nurse provided expert commentary in the amphitheatre regarding the specific manoeuvers and technical tricks. During the Special guests from right: Assoc. Prof. Ali Gozen, Prof. Evangelos Liatsikos, Prof. Antonio Alcaraz, Assoc. Prof. Bogdan Petrut Apply for your EAU membership online! Go to www.uroweb.org and click EAU membership to apply online. It will only take you a couple of minutes to submit your application, the rest - is for you to enjoy! www.cookmedical.com © COOK 2012 October/December 2014 Animal training facilities Becoming a member is now fast and easy! R A P I D R E L E A S E ™ U R E T E R A L A C C E S S S H E AT H MEDICAL We hope that we have met the educational needs of the trainees for an intensive applied course, and conducted in a friendly environment. We intend to maintain the standards of this course and we invite you to join us next autumn in Cluj Napoca! Would you like to receive all the benefits of EAU membership, but have no time for tedious paperwork? Flexor Parallel ® dry and wet lab they also learned the maintenance and functionality of all laparoscopic instruments and video systems. Theoretical sessions and presentation for intensive care nurses were also held. www.uroweb.org Ass. Prof. Dr. Bogdan Petrut Institutul Oncologic 'Prof. Dr. I. Chiricuta' Dept. of Urology Cluj-Napoca (RO) URO-BEMEAADV-FLPEUT1-EN-201212 European Association of Urology European Urology Today 25 Global Action Plan on Active Surveillance for low risk PCa Movember Foundation launches integrated project on active surveillance Sophie Bruinsma Postdoctoral researcher Erasmus MC Dept. of Urology Rotterdam (NL) data. One of the aims of the project is to reduce the number of men switching to active therapy within a year of being on Active Surveillance with the view of greatly improving their quality of life. s.m.bruinsma@ erasmusmc.nl In August this year, the Movember Global Action Plan Active Surveillance project was launched. This is an integrated project lasting 30 months and is being implemented across 19 institutions in 14 countries and across five Movember regions (Australasia, Europe, UK, Canada, USA). The initiative is also open to other eligible centres (‘candidate centres’). Milestones of the project include a global Active Surveillance (AS) database for clinical, biospecimen, imaging and biomarker data (including a virtual biobank), as well as worldwide tailor-made guidelines on AS and a web-based platform on AS. Systematic PSA-based screening for prostate cancer can reduce deaths by 21% as compared to no or little screening, according to the latest 13-year follow-up results of the European Randomized Study of Screening for Prostate Cancer (ERSPC)1. However, prostate cancer screening remains controversial, since it is associated with the significant risks of overdiagnosis and overtreatment. Many prostate cancer tumours do not require immediate treatment because they're small, confined and slow growing. Prof. Chris Bangma Dr. Monique Roobol The initiative is coordinated by Prof. Chris Bangma and Dr. Monique Roobol from Erasmus Medical Centre, the Netherlands and governed by a Research Advisory Committee. Philips Research is responsible for the design of the database. The Movember Foundation has united 19 institutions, hospitals and research centres from Australia, Canada, France, Finland, Italy, Japan, Netherlands, UK and USA. The initiative is open for other eligible centres to join as well (‘candidate centres’). The Active Surveillance for low risk Prostate Cancer Project will take two and a half years to complete and is currently in its initial implementation phase. Philips Research is currently working on the integration of biospecimen, imaging About the Movember Foundation The Movember Foundation is the leading global organisation committed to changing the face of men’s health. The Movember community has raised over $580 million to date, funding over 800 programs in 21 countries. This work is saving and improving the lives of men affected by prostate cancer, testicular cancer and mental health problems. The Movember Foundation challenges men to grow moustaches during Movember (formerly known as November), to spark conversation and raise vital funds for its men’s health programs. Join Movember by signing up as Mo Bro or Mo Sista at http://www.movember.com/ to help change the face of men’s health. About the Movember Foundation’s Global Action Plan (GAP) “Our vision is to have an everlasting impact on the face of men’s health and it’s to this end that we've established our Global Action Plan or GAP. We believe that getting the best researchers from around the world to work together on key challenges will accelerate breakthroughs that will ultimately benefit men with prostate or testicular cancer.” - Paul Villanti, Executive Director, Programs, The Movember Foundation. By bringing together over 350 international researchers, the Movember Foundation’s Global Action Plan (GAP) facilitates a new and unprecedented level of global research collaboration, Accordingly, a selective approach to treatment is required, with AS suggested as an alternative strategy to minimise overtreatment. AS focuses on the prevention of overtreatment by selecting patients with low-risk disease features and strictly monitoring them over time to recognise any potential risk reclassification that would justify deferred radical treatment, still with curative intent2. In recent years, the concept of AS has become a more viable option for men with low-risk prostate cancer who decide not to undergo active treatment right away and the prevalence of active surveillance is growing3. Several AS studies have been initiated worldwide that show favourable outcomes: the prostate cancer mortality rate is very low, treatment is avoided in the majority of patients, and there are quality-of-life benefits compared with initial treatment4-8. In 2006, the Prostate Cancer Research International: Active Surveillance (PRIAS) study was initiated at Erasmus MC Rotterdam to counteract overtreatment and contribute to prospective data collection (https:// www.prias-project.org/). The PRIAS study comprises the world's largest patient cohort followed in an AS protocol. In this worldwide initiative, about 2500 patients with very low-risk disease from 17 countries and three continents are presently being followed in a mutual protocol. The aim of the study is to reflect daily practice by collecting data from affiliated centres worldwide using an internet-based decision tool and the PRIAS protocol2. Preliminary data from PRIAS support AS as a feasible strategy to reduce overtreatment2. Although acceptance of AS as a treatment option for prostate cancer has been increasing, robust data from the long-term follow-up of men with favourable or intermediate-risk prostate cancer on AS protocols is still limited. Many uncertainties remain, including the long-term safety of AS9, and a reliable method for identifying tumours which are “clinically insignificant” is still lacking. Triggers for implementation of curative measures, such as radical prostatectomy and radiation treatments, remain variable and un-validated9. Movember project With this in mind the Movember Global Action Plan Active Surveillance project for low risk prostate cancer was initiated. The Movember Foundation has utilised its global networks and unique position as the world’s largest non-government funder of prostate cancer research to unite clinicians and researches from around the globe. The Movember Foundation has invested EUR €1,664,950 into the Active Surveillance for low-risk Prostate Cancer Project to create the largest centralised prostate cancer AS database to date, comprising the majority of the world’s Active Surveillance patient Movember Foundation and biomarker data, into the central database. The second phase, commencing in 2015, will involve developing a consensus guideline on AS based on a review of the current guidelines available around the world. This consensus-based guideline will be adapted based on the outcomes of the statistical analysis of the database and tailor-made guidelines on AS will be generated. These analyses will include the development of individualised dynamic risk based strategies. Nomograms that use the clinical characteristics of patients at diagnosis have been developed to predict the presence of pathologically indolent tumours. Kattan et al10 created the first nomogram in 2003 based on PSA, biopsy Gleason grade, clinical stage, TRUS-based prostate volume, and percentage and total length of positive cores. Steyerberg et al11 developed an updated model more suitable for a situation in which screening is more prevalent. The Steyerberg nomogram is part of the so-called Rotterdam prostate cancer risk calculator website where besides information on PC several RC’s can be found (www.prostatecancer-riskcalculator.com). The nomograms predicting indolent disease can be incorporated and further developed in the analyses of the project. As a next step, an online platform will be created leveraging the Movember Foundation global collaboration portal to allow free access to the AS guidelines and related information. Clinicians will be able to use these guidelines to more confidently identify men suitable for Active Surveillance and to also decide whose prostate cancer has progressed and will therefore require treatment. This will provide reassurance to men that they have made the best treatment choice for their type of disease. not previously seen within the prostate and testicular cancer community. GAP was launched in 2011. There are five GAP projects focusing on the following areas: Global Prostate Cancer Biomarker Initiative; Imaging in Advanced Prostate Cancer; Active Surveillance for low risk prostate cancer; Prostate Cancer Exercise and Metabolic Health; and Testicular Cancer Translational Research Project. The outcomes of the Active Surveillance for low risk prostate cancer project will be linked to the other on-going GAP initiatives. In summary, over the years there has been increasing acceptance of Active Surveillance as an alternative to radical treatment for men with low risk prostate cancer. Unless the over-diagnosis of indolent prostate cancer is reduced by alternative diagnostic strategies, active surveillance will continue to play an important role. At this stage, active surveillance "is a treatment approach in evolution." This initiative will make a significance contribution to this field of research by offering standard, universally agreed-upon guidelines. We would like to thank Patricio Sepulveda and Mark Buzza from the Movember Foundation for critically reviewing the article. References 1. Schroder FH, Hugosson J, Roobol MJ, Tammela TL, Zappa M, Nelen V, et al. Screening and prostate cancer mortality: results of the European Randomised Study of Screening for Prostate Cancer (ERSPC) at 13 years of follow-up. Lancet. 2014 doi:10.1016/S0140-6736(14)60525-0. 2. Bul M, Zhu X, Valdagni R, Pickles T, Kakehi Y, Rannikko A, et al. Active surveillance for low-risk prostate cancer worldwide: the PRIAS study. EUR UROL. 2013 Apr;63(4):597-603. 3. Lund L, Svolgaard N, Poulsen MH. Prostate cancer: a review of active surveillance. Res Rep Urol. 2014;6:107-12. 4. Bul M, van den Bergh RC, Zhu X, Rannikko A, Vasarainen H, Bangma CH, et al. Outcomes of initially expectantly managed patients with low or intermediate risk screen-detected localized prostate cancer. BJU Int. 2012 Dec;110(11):1672-7. 5. Welty CJ, Cowan JE, Nguyen H, Shinohara K, Perez N, Greene KL, et al. Extended Follow-Up and Risk Factors for Disease Reclassification from a Large Active Surveillance Cohort for Localized Prostate Cancer. J UROL. 2014 doi:10.1016/j.juro.2014.09.094. 6. Klotz L, Zhang L, Lam A, Nam R, Mamedov A, Loblaw A. Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. J Clin Oncol. 2010;28(1):126-31. 7. Tosoian JJ, Trock BJ, Landis P, Feng Z. Active surveillance program for prostate cancer: an update of the Johns Hopkins experience. Journal of Clinical …. 2011. 8. Hayes JH, Ollendorf DA, Pearson SD, Barry MJ, Kantoff PW, Stewart ST, et al. Active surveillance compared with initial treatment for men with low-risk prostate cancer: a decision analysis. JAMA. 2010 Dec 1;304(21):2373-80. 9. Thomsen FB, Brasso K, Klotz LH, Roder MA, Berg KD, Iversen P. Active surveillance for clinically localized prostate cancer--a systematic review. J Surg Oncol. 2014 Jun;109(8):830-5. 10. Kattan MW, Eastham JA, Wheeler TM, Maru N, Scardino PT, Erbersdobler A, et al. Counseling men with prostate cancer: a nomogram for predicting the presence of small, moderately differentiated, confined tumors. J UROL. 2003 Nov;170(5):1792-7. 11. Steyerberg EW, Roobol MJ, Kattan MW, van der Kwast TH, de Koning HJ, Schroder FH. Prediction of indolent prostate cancer: validation and updating of a prognostic nomogram. J UROL. 2007 Jan;177(1):107-12; discussion 12. Patients first. At the end of the day, it’s all about our patients. We publish practicechanging research so that clinicians throughout our community can improve patient care. To involve patients in their treatment, we now publish summaries of each paper in language they can understand. europeanurology.com european urology Forward faster. Together. european urology Forward faster. Together. 26 European Urology Today October/December 2014 european urology Book reviews Prof. Paul Meria Section Editor Paris (FR) paul.meria@ sls.aphp.fr Cancer and Inflammation Mechanisms Publisher Publication Edition Binding Price Pages Website : Wiley : Aug. 2014 : 1st : Hardcover : 108.60€ : 400 : www.wiley.com Urinary and Fecal Incontinence: A training program for children and adolescents Inflammation remains a physiological response from the human body to various phenomena and environmental factors. Inflammation is also considered as responsible for almost 25% of cancers since epidemiological and experimental studies have demonstrated such correlation. Urinary and fecal incontinence are common in children and their incidence decreases as the age increases. Nevertheless, children and adolescents can be afflicted with various conditions such as enuresis, daytime urinary or fecal incontinence and in a few cases such problems can continue in adulthood. These problems are stressful and can be responsible Editors Y. Hiraku, S. Kawanishi, and H. Ohshima wrote for quality of life impairment. In many cases standard this book as an update on the correlation between treatments can be applied successfully but complex chronic inflammation and cancer development. More cases require special management. than 60 worldwide experts contributed to review various mechanisms involved in carcinogenesis related to inflammation and their possible prevention. The first section of the book was dedicated to an overview of inflammation-related cancer. The authors focused on various aspects of inflammation and cancer development mechanisms. They addressed the role of stem cells and that of epithelial-mesenchymal transition (EMT), which seems particularly involved in tumour cell dissemination. In this manual, editors M. Equit, H. Sambach, J. Niemczinski and A. von Gontard, worldwide experts in paediatric incontinence, present a training programme intended for children and adolescents suffering from elimination disorders. The first part of the textbook focused on three clinical problems: nocturnal enuresis, daytime urinary incontinence and fecal incontinence. For each condition, the authors considered all aspects of classifications, various subtypes, prevalence, comorbid disorders, psychological problems and etiology. The assessment and treatment were addressed in the succeeding chapter, including complex cases. The last part of the manual focused on the evaluation of the treatment, addressing the results obtained. A CD-Rom was included, containing worksheets and materials developed for the treatments. Editors ISBN e-Book : Y. Hiraku, S. Kawanishi, H. Ohshima : 978-1-118-16030-5 : 978-1-118-82655-3 Book reviews Multimorbidity refers to several co-occurring long-lasting conditions affecting a given patient and represents an increasing problem in our practice. It makes our management strategies in some patients challenging, particularly the elderly who develop a range of medical problems, such as diabetes mellitus, coronary disease, arterial hypertension, arthritis or mental disorders. Currently, all physicians, including urologists, have become more and more specialized and can have the tendency to narrowly view a patient, considering only the disease that is related to their sub-specialty. In this textbook, editors S.W. Mercer, C. Salisbury and M. Fortin, focused on a very important “topic,” which many of us may overlook. With the help of more than 20 worldwide experts they wrote a practical book that addressed various clinical problems related to multimorbidity in clinical practice. This ABC series book is a practical resource that is very useful to all physicians, regardless of their specialty and level of practice. Readers will find in this book information that will contribute to improving the quality of multimorbid patient’s management. Editors ISBN Publisher Publication Edition Binding Various other problems were also addressed, Price including the effects of multimorbidity on healthcare Pages resource use, the primary care management of Illustrations multimorbid patients, the role of healthcare electronic Website The second part was dedicated to therapy and presented as a manual which covered both bladder and bowel training, including group therapy techniques. The authors have chosen ‘training programme’ as the term, although such a programme represents more than a simple training. Various exercises were included in a special course of treatment, following the failure of standard therapy. Individual training sessions and group sessions were described. Seven sessions were addressed for bladder training and two sessions were considered for bowel training. The content of each session was exhaustively described. Undoubtedly, this outstanding textbook will be of interest to all oncology researchers and to those who want to update their knowledge. Although this textbook was not intended for urologists, many will find useful information related to urology. Trainees and young researchers would also be attracted by the book’s high quality. ABC of Multimorbidity Following a chapter that presented various definitions, the authors described the epidemiological aspects of multimorbidity, demonstrating its relationship with increasing age. The effects of multimorbidity were examined in the succeeding chapter, with emphasis on the consequences of high morbidity burden on functional status and quality of life. The succeeding section was dedicated to biochemistry. The authors focused on DNA damage during inflammation. The role of DNA damage in the development of cancer was discussed in various tumours, including urological and non-urological tumours. In the third section, the authors addressed the main aspects of molecular biology in inflammation related cancer. Various molecules such as Toll-like receptors, inflammasome and micro-RNAs were described and their role was discussed. Specific causes of inflammation related cancers were considered in the fourth part of the book, in which the authors focused on some peculiar cancers and their demonstrated or presumed cause. Most of them were infections due to human papilloma, hepatitis and Epstein Barr viruses and their role in cervical cancer, hepatocellular cancer and nasopharyngeal cancer were discussed. Other specific diseases were addressed such as asbestosis and radiation-induced injuries. The last section dealt with the prevention of carcinogenesis in patients with chronic inflammatory diseases. The authors also focused on various aspects of colorectal cancer prevention. medical record and computer-based technologies. Mental health problems, whose prevalence is higher in multimorbid patients, were addressed in a special chapter. The authors also focused on healthcare policy in the era of multimorbid patient’s management and concluded their work with a chapter dedicated to optimising patient’s management. Price : € 34.95 Pages : 92 including CD-ROM Illustrations : 40 tables/fig. (109 colour worksheets on CD ROM) Original language : German Website : www.hogrefe.com This manual is a compilation of the long experience of the authors and provides the reader with an exhaustive overview of elimination disorders. Many pediatricians and pediatric urologists will find useful information in this manual. Authors ISBN E-book Publisher Publication Edition Binding : M. Equit, H. Sambach, J. Niemczyk, A. v. Gontard : 978-0-88937-460-7 : 978-1-61334-460-6 : Hogrefe Publishing : 2015 : 1st : Softcover - Astellas European Foundation Award 2015 The Société Internationale d’Urologie and the Astellas European Foundation (AEF) are pleased to sponsor a $20,000 USD award granted to a scientist of notable professional and ethical standing. In preparation for the 35th SIU Congress, to be held October 15-18, 2015 in Melbourne, Australia, the SIU and the AEF solicit nominations for this prestigious award. Nominations should include a detailed curriculum vitae and a letter with a full explanation of the candidate’s merit, and must be submitted to the Awards Committee, SIU-Astellas European Foundation Award 2015 c/o SIU Central Office at the coordinates below no later than March 1, 2015. The Awards Committee, appointed by the SIU’s Board of Chairmen, will review all applications and announce the SIU-Astellas European Foundation Award 2015 laureate at the 2015 SIU Congress in Melbourne. Previous laureates were Dr. Donald S. Coffey (1994), Dr. Nils Kock (1997), Dr. Emil Tanagho (2000), Dr. Alvaro Morales (2002), Dr. Michael Marberger (2004), Dr. Frans Debruyne (2006), Dr. Andrew Novick (2007), Dr. Peter Alken (2009), Dr. Fritz Schröder (2011), Dr. Peter Scardino (2012), Dr. Ralph Clayman (2013), and Dr. Urs Studer (2014). Research Fellowship The California Urology Foundation, in association with the Société Internationale d’Urologie, announces the availability of a Research Fellowship for a fully- trained Urologist from Africa to do research for one year in a medical laboratory of the University of California in San Francisco (UCSF). This award is intended to prepare the candidate for an academic career in his or her home country; a firm commitment to return will be a material consideration in the evaluation of candidates. This fellowship carries a stipend of $50,000 USD, of which $14,000 is used to cover medical insurance and administrative fees. Applications for this fellowship will be evaluated by a joint SIU/UCSF Committee and should include a proposed area of study, a detailed CV, and a minimum of 2 letters of professional references. An application missing any of the items listed above will be considered incomplete. The deadline for the January-December 2016 Fellowship will be February 28, 2015. Application forms are available on the SIU website www.siu-urology.org under the Training Scholarships tab. Applications can be submitted by mail, fax or e-mail to UCSF-SIU Research Fellowship c/o SIU Central Office at the coordinates below. SIU CENTRAL OFFICE 1155 University Street, Suite 1012, Montreal, Quebec, Canada H3B 3A7 Telephone: +1 514 875 5665 Fax: +1 514 875 0205 [email protected] 4134_SIU-AstellasUCSF_EUT_NovAd.indd 1 October/December 2014 : S.W. Mercer, C. Salisbury, M. Fortin : 978-1-118-38388-9 : Wiley Blackwell : July 2014 : 1st : Softcover : 26.30 € : 64 : 120 : www.abcbookseries.com Client: Description: SIU 2015 ASTELLAS - UCSF Docket number: 24-4134 14-10-02 9:36 AM File Size: Trim Size: European Urology Today 100 % 133,4 mm X 194,3 mm 27 Preventing stone migration during intracorporeal lithotripsy Two out of 10 kidney stone patients have ureteral calculi at time of diagnosis Dr. Nicola Macchione Clinica Urologica III, Università di Milano, A.O. San Paolo-Polo Universitario Milan (IT) nicola.macchione@ unimi.it Prof. Emanuele Montanari Clinica Urologica III, Università di Milano, A.O. San Paolo-Polo Universitario Milan (IT) emanuele. [email protected] The therapeutic options for ureteral stones, according to EAU guidelines, include a conservative watch-andwait approach or active intervention. Usually, the choice to follow one of these two options depends on several factors related to stone size, density, location, patient’s factors, surgeon capability, and equipment availability. The surgical approach includes extracorporeal shock wave lithotripsy (SWL), retrograde uroteroscopy (URS), percutaneous antegrade ureteroscopy and open/laparoscopic ureterolithotomy. Although the SWL approach is considered (in all cases where it is not contraindicated) a good treatment option-- or by many urologists as the gold-standard primary treatment-- the introduction of new ureteroscopic instruments, as well as the development of effective intracorporeal lithotripsy methods, has increased in the last years the use of the endoscopic approach as first-line treatment (even if the difference of the results between the two procedures in terms of success rate and complication rate is not clear). Anti-repulsion devices In recent years, many instruments, strategies and antirepulsion devices have been developed in the field of endoscopic treatment of ureteral stones in order to reduce the the retropulsion rate during the laser/pneumatic lithotripsy. Anti-repulsion devices that are currently available are divided as either mechanical or gel-based. In the first group, these include: Lithovac (Boston Scientific Corp., USA), Stone Cone (Boston Scientific Corp., USA), Passport Ballon (Boston Scientific Corp., USA), PercSys Accordion (Percutaneous System, USA), NTrap (Cook Urological, USA), and Xenx (Xenolith Medical, Israel). The second group includes: BackStop gel (Pluromed Inc., USA) and, in general, lubricating jellies. Many physicians have described experiences using a stone basket like anti-repulsion device. The technique consists in the use of a two-port adaptor attached to the ureteroscope and insertion through that adaptor of the laser fibre and the basket at the same time. In that way, they are able to catch the stone with the basket and then perform a laser lithotripsy while avoiding bursting the basket’s wire. That technique has many limitations linked to stone size and location, and also looks less effective compared with the use of a normal anti-repulsion device. Studies have been described with baskets such as Escape (Boston Scientific Corp., USA), Lithocatch (Boston Scientific Corp., USA) and Parachute (Boston Scientific Corp., USA). Lubricating jellies There are, at present, limited experiences in the literature to suggest the safe and effective use of lubricating jellies as anti-repulsion device, and the few studies performed do not show results that suggest its routine use. In many of them, the number of patients treated is not enough to show a statistically significant result and some studies lack data with regards to details of the procedure such as information on irrigant fluid. An example is the follow-up randomised clinical trial on the use of lidocaine jelly as an antirepulsion device during a pneumatic lithotripsy of Currently, in literature, prospective studies comparing ureteral stone performed by Zehri et al. In that study, the authors enrolled 50 patients and showed the two modalities are limited. In a recent study published in the Journal of Endourology by A. Kumar a significant difference in stone or stone fragment migration for lidocaine-treated patients compared et al., the authors performed a prospective with controls, but they did not give any information randomised trial comparing SWL and semi-rigid ureteroscopy for upper ureteral stones less than 2 cm. regarding the location of the stone treated (proximal or distal ureter) and the use of the They enrolled 90 patients in each group, similar for the stone characteristics, and they concluded that SWL irrigant fluid. and URS are both safe and highly efficacious in the More substantial is the literature on BackStop. It is a management of upper ureteral stones < 20 mm. For thermosensitive water-soluble polymer with reverse upper ureteral stones < 10 mm, SWL is safer, less invasive and of comparable efficacy as URS. For upper properties. It is liquid at temperatures below 16° C, soft and injectable at room temperature and it ureteral stones 10 to 20 mm, URS is more effective becomes a viscous gel at body temperature. With a and has a lower re-treatment rate than SWL. ureteral catheter (3 or 5 F), it is delivered beyond the stone(s) to form a temporary plug, preventing stone Retropulsion of stone fragments migration during the lithotripsy. At the end of the Often the low success rate of the endoscopic procedure, the plug is dissolved by cold saline procedures is linked to the retropulsion of stone irrigation. fragments. It has been reported that 3-15% of stones in the distal ureter and 28-60% of stones in the A recent randomized controlled trial on the use of proximal ureter undergo retrograde stone retropulsion. In these cases it has been recorded that BackStop was published in the Journal of Urology by there was an increase of operative time, the need for A. Rane et al. In that study, the authors enrolled 68 patients with a single stone in the proximal ureter further ancillary procedures, a decrease of stoneand they showed a retropulsion rate of 8.8% in the free rates and, as can be expected, an increase of group treated with BackStop, versus a retropulsion healthcare costs. rate of 52.9% in the control group. No complications have been reported in the BackStop group. In Furthermore, stone/stone fragments retropulsion conclusion, they said that BackStop appears to be a could be associated with an increase of the risk for novel, safe and effective means of preventing stone urinary tract infections ( UTI), recurrent stone formation and renal colic. The cause of the migration fragment retropulsion. of the stone fragments depends on several factors, There are various considerations with regards the and are linked to the stone and ureter characteristics Lithovac, which works the opposite way compared such as the size and location of the stone and with the former mechanical device. Lithovac is a dilatation of the ureter, or related to the modality of suction hollow probe combined with a pneumatic the endoscopic procedure such as the pressure probe, which is used during lithotripsy for fragments generated by the irrigant fluid, insertion of the aspiration, preventing stone migration. In literature, instruments and laser burst. there is only one study by F. Delvecchio et al. published in the Journal of Urology. The authors In addition, using pneumatic or electrohydraulic enrolled 21 patients with ureteral calculi. They lithotripters, the stone migration rate reported in reported a 95% stone-free rate and in just one case literature is much higher if compared with the laser did a stone migration occurred. They used a lithotripsy. These results suggest that the energy source used for lithotripsy of ureteral stones is also an semi-rigid ureteroscope with a diameter of 8.5 F to accommodate the Lithovac equipment, and in order to important factor to consider in the endoscopic reach the stone they performed a balloon dilatation of treatment of the urinary stones to decrease the the ureteral orifice to 15 F in 7 cases (33.3%). The retropulsion rate. advantage reported was that the use of a suction during the lithotripsy improved stone clearance and EAU Section of Urolithiasis (EULIS) also the vision. 28 European Urology Today Anti-repulsion devices One of the most extensively studied anti-repulsion devices is the Stone Cone. It is made of an inner wire that lies in an outer radio-opaque carrying sheath. The inner wire is divided into three parts: the floppy tip, the cone, and the proximal part. During the introduction into the ureter, the cone portion lies inside the carrying catheter and is straight. Handling the device from the distal part on the carrying catheter, it is easy to deploy the cone. The cone size is available in two different sizes of 7 or 10 mm, and the coil portion diameters can also be adjusted according to the ureteric diameter. Since 2001, many papers regarding the use of Stone Cone as anti-repulsion device have been written. In 2009, a study was published by B.H. Eisner et al. in Urologia Internationalis with the largest series of patients treated in a single centre using a Stone Cone during ureteroscopy. They performed a retrospective review of medical records of 133 consecutive ureteroscopic holmium: YAG laser lithotripsy procedures in which the Stone Cone was used. The stone location was proximal ureter for 53 calculi and distal ureter for 80 calculi. They reported no calculus retropulsion in 131 patients (98.5%) and no major complications. The investigators also performed a Medline search showing that, as reported by them, the Stone Cone is efficient at preventing stone migration during endoscopic treatment of ureteral calculi. Regarding the PercSys Accordion, there are many studies made in vitro that showed the safety and efficacy of this device, but just a single experience in vivo is reported in literature. This device consists of a sheath wire system with a diameter of 0.038 inches with a 6 cm hydrophilic soft tip. It is introduced as a guide wire and once its position has been confirmed (under fluoroscopic or endoscopic control), the device could be deployed forming a multifold polyurethane film backstop of 7 or 10 mm. Figure 2: Xenx with nitinol mesh fully deployed mesh lies between two radiopaque markers, one on the top of the other in the closed device. At the end of the procedure the device could be close and used like a normal guide wire. Safety and efficacy of Xenx was evaluated by C. Sarkissian in an ex-vivo porcine model reporting good results. The first in vivo evaluation was done by E. Montanari et al. The investigators evaluated the safety and efficacy of the Xenx in 18 patients (recruited across three European stone centres) who underwent ureteroscopy and laser fragmentation. No complications have been reported. Median operator’s evaluation for Xenx property was good. In addition, no case of retropulsion was recorded. The same concept is employed with Passport, a balloon anti-repulsion device. It is composed of a noncompliant balloon mounted on a stainless steel wire for one-step ureteroscopic placement. The diameter of the inflated device is 0.038 inches. As a normal guide wire it is inserted endoscopically and placed beyond the stone under fluoroscopic control. Once positioned the balloon is inflated in order to avoid the passage of stone fragments. In literature, there are few studies regarding Passport, with the first published by Dretler et al. in 2000 in the Journal of Endourology. The investigators enrolled 42 patients and showed a successful placement of the balloon above the stone in 69% of the cases and achieved a stone-free rate of 90%. According to the authors, the Passport device lacks efficacy in more dilated ureters (more than 12 F of diameter). Moreover, the balloon is liable to puncture, so it never should come in contact with laser or pneumatic lithotripter probes. A recent study was published in the Journal of Endourology by J. Pagnani et al. The authors prospectively evaluated and treated 21 patients with distal ureteral stones. The patients were divided in two groups, one treated with PercSys and the other treated as control. They showed that the Accordion device effectively occludes the ureter and prevents the retrograde migration of stone fragments. We should point out that all the patients treated in this study were affected by ureteral distal stones, and usually for Cost-effectiveness stones located in the distal part of the ureter the In conclusion, overall results of literature showed that retropulsion rate is really low. all the devices tested decreased stone migration compared to ureteroscopic lithotripsy without use of Another mechanical anti-repulsion device is NTrap. these devices. On the other hand, the use of devices This device is composed of an inner wire and outer could increase the cost of the surgical procedure, so sheath catheter. The inner wire has a 7 mm umbrella the choice of the best option, in terms of costmade from tightly woven nitinol wires spaced effectiveness, remains the goal of every urologist. approximately 1 mm apart in the centre and 2 mm apart at either end. Diameter is 2.8 F. In a recent At first glance, it may look expensive to use an meta-analysis study by H. Ding et al. and published in anti-repulsion device during the endoscopic treatment the Journal of Endourology, the investigators of the ureteral stone, but we should consider how evaluated the efficacy and safety of NTrap studied in much the stone-free rate would cost the healthcare two randomised controlled trials and one-case control system in terms of ancillary procedures, study including 456 patients. The meta-analysis hospitalisation days, and all the attendant risks (UTI, showed that patients who underwent ureteroscopic renal colic, recurrence rate). Only considering one of lithotripsy with the use of the NTrap demonstrated a the ancillary procedures needed to reach the significant advantage over those without the use of retropulsed stones, such as the use of the flexible the device in terms of stone-free rate, and that the instruments, the cost of the procedure became incidence of stone migration was significantly lower completely different and much more expensive when in NTrap treatment than without NTrap. compared to the cost of the standard procedure plus an anti-repulsion device. Figure 1: Xenx device Not yet widespread on the market but already evaluated in vitro and in vivo is Xenx. The closed device looks like a normal hydrophilic guide wire with a tip of 0.038 inches and a shaft of 0.04 inches, 150 cm long (Fig.1) The tip is floppy and hydrophilic. It has an inner wire and an outer sheath. Once its position has been confirmed (under fluoroscopic control) the device could be opened, shifting on the distal part the outer sheath on the inner wire. During these procedures in the distal part, a nitinol mesh with a maximum diameter of 12 mm is deployed (Fig.2). The Many authors demonstrated that flexible ureteroscopes must undergo repair every five to 18 uses and flexible urteroscope repair may cost up to $5,000. In a recent study published by M. Ursiny et al. in the Journal of Urolog, the authors evaluated the cost-effectiveness of anti-repulsion devices for ureteroscopic lithotripsy. They constructed a decision analysis model to compare the cost-effectiveness of ureteroscopic lithotripsy with versus without an anti-repulsion device. They evaluated the following devices: NTrap, Lidocaine jelly, Stone Cone and Back-stop and the average cost estimated for the device was $278. Otherwise, the estimated costs of secondary procedures needed to treat retropulsed stones were estimated at $5,290 for SWL and $6,390 for ureteroscopy. They concluded that the use of anti-repulsion devices are cost-effective for ureteroscopic lithotripsy at a retropulsion rate greater than 6.3%. In addition, they suggested that urologists who perform this procedure should assess retropulsion rates to determine whether these devices would be beneficial in practice. October/December 2014 EULIS launches new postgraduate workshops on urolithiasis In 2014 the EAU Section of Urolithiasis (EULIS) has launched its new postgraduate workshops on urolithiasis. The initiative, conceived and enthusiastically promoted by EULIS Chairman Kemal Sarica, had intended to fill the gap between the two EULIS Congresses of 2013 and 2015. EULIS Board K. Sarica, Istanbul (TR) Chairman In the future, including the years when the convention is not held, EULIS will organise workshops in different European locations. The workshops will have different formats and will feature lectures, live surgery and hands-on sessions. The workshops aim to serve the needs of both urologists and nephrologists interested in urolithiasis. First two-day EULIS postgraduate workshop on urolithiasis held in Vienna Prof. Christian Seitz Medical University of Vienna Vienna (AT) Dr. Christian Tuerk Hospital Rudolfstiftung Vienna (AT) [email protected] christian.tuerk@ wienkav.at The first two-day EULIS post-graduate workshop on urolithiasis was held in Vienna in June 2014 at the Medical University of Vienna, represented by Prof. Christian Seitz and the Hospital Rudolfstiftung represented by Dr. Chistian Tuerk. It gave a comprehensive overview of urinary stone disease, N.P. Buchholz, London (GB) J. A. Galan, Elche (ES) G. Gambaro, Rome (IT) T. Knoll, Sindelfingen (DE) D.J. Kok, Rotterdam (NL) J.M. Reis, SantosLisboa (PT) R. Siener, Bonn (DE) O. Traxer, Paris (FR) A. Trinchieri, Lecco (IT) R. Unwin, London (GB) and the scientific programme covered the entire range of urolithiasis management from epidemiology and diagnosis to various surgical and conservative treatment modalities, and a glimpse into future developments. A distinguished line-up of speakers presented lectures and video sessions. The workshop’s compact programme allowed participants Christian Seitz (AT), Roswitha Siener (DE), Christian to meet leading experts in urinary stone disease and Tuerk (AT) and Michael Töpker (AT). exchange ideas with them in lively debate sessions. The participants learned from unedited video surgery The workshop was conducted by internationally demonstrations of rigid and flexible URS, prone/ supine PCNL including mini, ultra mini and micro renowned faculty members led by EULIS, including Professors Noor Buchholz (UK), Petrisor Geavlete (RO), PCNL. With around 75 participants it was possible to Thomas Knoll (DE), Sven Lahme (DE), Palle Osther hold intensive dialogue between participants and the (DK), José Reis Santos (PT), Kemal Sarica (TR), faculty during debate sessions. Enthusiastic participants at second EULIS postgraduate workshop on stones in Milan Prof. Emanuele Montanari Urology Clinic III University of Milan A.O. San Paolo-Polo Universitario Milan (IT) held for the training of flexible ureteroscopy and percutaneous nephrolithotomy, live demonstrations of Doppler renal ultrasound for diagnosing renal calculi by the twinkling artifact, demonstrations of software for dietary evaluation of renal stone patients, and a critical appraisal of several scientific articles on dietary risk factors for kidney stones. emanuele. [email protected] The next day featured live surgery demonstration of flexible ureteroscopy by Olivier Traxer and perc, ultramini-perc and micro-perc by Emanuele Montanari. A parallel course was held on epidemiological, genetic and nephrological aspects of Dr. Alberto Trinchieri A. Manzoni Hospital Urology Unit Lecco (IT) renal stone disease. The workshop ended with a session of unedited videos of difficult renal stone cases presented by Giampaolo Zanetti and Ioannis Kartalas Goumas of the Vimercate Hospital and Nicola Macchione of S. Paolo Hospital in Milan. For the social programme, the course participants visited San Eustorgio, one of Milan’s oldest religious buildings that keep holy relics attributed to the Three Magi (The Three Wise Men) and with a fresco of beautiful paintings from the 15th century. The church is also known for its underground ruins of Mediolanum, an ancient city of the Roman Empire. EULIS Chairman Kemal Sarica, presenting his lecture www.eulis15.org a.trinchieri@ ospedale.lecco.it The second EULIS post-graduate workshop on urolithiasis was held in Milan from 15-16 September 2014 and led by the chairmen Emanuele Montanari of the University of Milan - San Paolo Hospital and Alberto Trinchieri of the Manzoni Hospital of Lecco. The two-day course gathered around 30 urologists and 10 nephrologists interested in the management of kidney stones. The first day featured a general session with lectures on various aspects of pathogenesis, diagnosis and treatment of urolithiasis, presented by EULIS board members, namely, Kemal Sarica, Giovanni Gambaro, Dirk Kok, Emanuele Montanari and Alberto Hands-on training Trinchieri. In the afternoon, hands-on sessions were EULIS15 3rd Meeting of the EAU Section of Urolithiasis 10-12 September 2015, Alicante, Spain EAU Events are accredited by the EBU in compliance with the UEMS/EACCME regulations European Participants of the 2nd EULIS Postgraduate Workshop Association of Urology EAU Section of Urolithiasis (EULIS) October/December 2014 European Urology Today 29 Young Urologists/Residents Corner ESRU’s objectives in practice The Belgian example Dr. Vincent De Coninck NCO Belgium President-elect ESRU Belgium Brussels (BE) vincent.deconinck@ uzbrussel.be Dr. Barbara Hermans NCO Belgium Membership, ESRU Belgium Leuven (BE) barbarahermans@ hotmail.com after financial statements, a secretary and another member maintaining our database. Our PR officer maintains not only our Facebook page but also promotes our group to new residents. For instance, the PR officer has introduced the Movember competition in our social media pages, in which every Belgian urology resident (male or female) can send their pictures wearing or sporting a mustache. The best picture wins a special poster during the poster session on our national conference in December. Each university in Belgium has a representative in the ESRU. We try to divide these assignments to at least one representative of a university for us to reach many residents across the country. topic and every year we choose various areas such as functional urology, paediatric urology, oncology and andrology. Professors and experts on each respective subject discussed the latest updates. We end the day with a reception and dinner, and invite the participating residents to a party. Activities Our motivated team composes every year an expanded offer of courses, seminars and other workshops to enhance the quality and knowledge of future urologists. In our meetings, we discuss the gaps in our training and incorporate these into courses and updates. Every representative of a Belgian university has to organise a course every two years in order to have at least three to four national courses a year. This is illustrated with the Imaging Course held in Brussels, which is described later in this article. The purpose of the course was to discuss the value of different imaging techniques for a certain disease. Prof. Braeckman, a urologist of UZ Brussel, discussed the indications of ultrasonography in diseases of the kidneys, bladder and prostate. He explained what urologists should be able to see and do with the grey scales images. Concerning ultrasound of bladder and kidneys, he described the steps on how to recognise masses, stones and explained how to place tubes in case of hydronephrosis or a full bladder. Imaging course On a Friday afternoon in September 2014, ESRU Belgium organised a four-hour imaging course in urology. All Belgian residents were invited to the University Hospital of Brussels (UZ Brussel), where around 33 or a third of residents attended the course. Turning theory into practice ESRU.be is the Belgian association of residents in urology. We have the same goals as the ESRU in Europe to help ensure optimal urological care in Belgium. To do this we organise courses and workshops to achieve a high standard of clinical care. Every year, we organise the Starters’ Package, a laparoscopy course held in close collaboration with Members of the ESRU.be team carry out their the Belgian Laparoscopic Urology Group (BLUG) for responsibilities which are assigned to them during the fourth-year residents. The course is spread in four our first meeting of the year in July. Our chairman is modules over the year. responsible for leading the meetings and organising the Starters’ Package, an annual course on Annually, we hold in December the ESRU session laparoscopy for fourth-year residents. He is assisted during the Belgian congress (BAU congress). During by the chairman-elect, who will become chairman the this “How To” session, experts provide following year. The latter is responsible for organising understandable explanations on how to do certain the ‘ESRU.be Day,’ a day-long scientific programme surgical procedures. The sessions end with the award focusing on a particular subject in urology, and which for best poster. Belgian residents can send abstracts provides young doctors to meet their experienced and posters of research or case studies. The prize colleagues. aims to stimulate scientific work by residents and publish their clinical cases. We have a webmaster for our website (ESRU.be), another officer responsible for guiding the We end our academic year by organising the ESRU.be organisation in the right direction, a member looking day. Led by the chairman-elect, we try not to repeat a For prostate diseases, the indications and applications of grey-scale ultrasound were explained. Transrectal grey scale ultrasound is useful for BPH to measure the extent of the intravesical obstruction, which aids treatment decisions (medical or surgical). In prostate cancer it is the first test following DRE and PSA, since it allows a quick and useful evaluation of any induration in the prostate, providing a guide for biopsies in cases when PSA seems to be high for no clinically obvious reason. Doppler, contrast, elastography and HistoScanning were also discussed during the sessions. Dr. De Visschere, a radiologist of UZ Gent, highlighted the value of MRI in common prostate and kidney diseases. He outlined the diagnostic accuracy of multiparametric MRI for prostate cancer detection, and described the usefulness of MRI in characterising renal masses. He ended by evaluating this imaging technique in assessing Peyronie’s disease or urogenital fistula. Over 20 kidney diseases that can be diagnosed by CT were depicted in detail by Dr. De Brucker, a radiologist of UZ Brussel. He summarised the causes and pathophysiology of diseases and described how to recognise them. By describing interesting cases, the audience learned about the value of CT in assessing patients with recurrent urinary tract infections, renal trauma, congenital anomalies and suspicious lesions of the kidney on MRI or ultrasonography. Finally, Dr. Puttemans, a radiologist of Saint Pierre University Hospital, Brussels, shared his expertise on scrotal ultrasonography, and discussed how to interpret small testicular masses by looking at the position (center versus periphery), the vascularisation, the size and the amount of lesions. After the theoretical part, all participants tested their skills in ultrasonography on urological patients (See photo). Diseases to be recognised were renal tumours, kidney stones, spermatocoeles and small hypoechoic testicular lesions. In one patient, a computer-aided ultrasonography was performed to detect a prostate cancer of about 0.75 mL. Interested in our activities or an inspiration for your own society? Visit our website for additional information at ESRU.be The New Portuguese Residents Society What should be the role of national societies? Dr. Ricardo Pereira e Silva ESRU Project Manager Chairman Portuguese Urology Residents Society Lisbon (PT) Ricardomanuelsilva7@ gmail.com one can’t reach people, then all the other objectives one may want to achieve will be out of your reach. Thereafter, we created our own internal regulations. Although it is a time-consuming process, it helps to carefully think about the real purpose of the society and to remind all members of the main objectives, including those who are members of the Executive Committee. All residents are aware of these internal rules and were invited to present a list of five candidate residents, including a chairman and a secretary, which we consider sufficient to have an adequate To raise the level of medical education in urology, nationwide representation of our Portuguese trainees residents must actively participate in discussing the main issues and in finding solutions for problems and (nowadays slightly over 60) while maintaining a good level of functionality. needs of residents in Europe. To do so and enable us to express our opinions, it is essential that we first organise ourselves through structured national societies that can help define the global position of residents in that country. With the increasing number of urology residents in Portugal and the wide distribution of centres, communication has become a challenge for residents, which affects the effective discussion of these issues. The Executive Committee mandate was for a two-year period. Elections were scheduled so every resident could vote and choose one of the lists during an annual resident’s dinner. By doing this we had a democratic selection of the committee in an informal way, while at the same time we had the opportunity to exchange ideas and improve social links among us. We started by gathering residents from various parts of our country which were motivated to contribute to the creation of the society. After a couple of meetings to discuss on how to proceed, our first step was to create an updated database of our residents so that we could make official announcements and bring more people into the project. Full support The full support that the Portuguese Urology Association is providing us is essential not only for the success of our society but also for its future activities. Creating the national resident’s society within the national association may be an advantage since we can learn from the obstacles they have faced and dealt with, enabling us to focus on essential processes. Moreover, being recognised as part of the National Urology Association allows an open and active debate that includes various viewpoints from consultants, young urologists and residents. Even if it seems easy to create this database, our experience in ESRU is that most of the countries, with or without a resident’s society, still don’t have a global and updated list of all residents. To reiterate, if 30 European Urology Today Our Resident’s Society aims to be a consultative group within the Portuguese Urology Association, with the main goal of raising awareness regarding specific national problems. Thus, we can help contribute in raising the standards of urological education in our country. We can also assign ESRU National Communication Officers who can participate in the discussions with other European residents. an amazing experience since they came in touch with residents from all over the country, allowing an exchange of essential information. We strongly encourage countries that still haven’t created their own national residents society to consider the benefits and take the first steps. ESRU members can certainly provide support by sharing lessons from their own experience. And for countries The Portuguese National Association of Urology has which already have urology resident’s societies, also given us a time slot for a plenary session during actively recruiting active members and involving their National Annual Congress. This year, we selected them in current and future projects should be a post-residency career options as the main theme and priority. invited young urologists to speak about academic and non-academic career moves, as well as private Even though it is a daunting task, it is worth the effort. Involvement and commitment are certainly practice and working overseas. These are priority issues for us due to the growing number of specialists important. Knowing who we are and what we think in Portugal. can inspire residents to have an active voice in the debate of how urological education can be further Those who are participating in our project to create a improved based on the needs and concerns of the new Portuguese Resident’s Society have found it to be residents themselves. EUREP 2015 - Important information for applicants! From 2015 European participants in EUREP will no longer have their travel costs reimbursed. This means that all selected participants must pay for their travel to and from Prague. The EAU/ESU will continue to cover the cost of accommodation for European residents in a shared room as well as the cost of the course (incl. lunches, coffee breaks). October/December 2014 Young Urologists/Residents Corner An excellent training experience in Belgium Two-month fellowship in robot-assisted surgery in Aalst Dr. Viliam Kubas Vice-president, Residency Section Slovak Urological Society ESRU Representative for Slovakia Banska Bystrica (SK) Prof. Mottrie is a wonderful mentor who explains every step and discusses the procedures in a clear and understandable manner. I assisted mostly in robot-assisted radical prostatectomies and partial nephrectomies. I especially appreciated taking part in robot-assisted cystectomy since the Slovakian hospital where I work has plans to start introducing the robotic option soon. [email protected] What made my fellowship even more valuable was the possibility to go to ORSI or the OLV Vattikuti Robotic Surgery Institute, which is an impressive training centre where I could practise what I've seen at the operating theatre. ORSI is fully equipped and there are two robot-assisted surgical simulators and two daVinci Si Robots with a dual console. It‘s like very modern operating room with the latest airseal flow system and two anesthesia machines. I should also mention the friendly environment with the very professional and helpful staff members who all contributed to the outstanding reputation of the centre. Paul, the manager of ORSI, was also kind to give me a lift to and from the institute. You can imagine how excited I was when I received a letter from the secretary of Prof. Mottrie confirming that I was accepted for a surgical training fellowship in January 2014. I was on my way to the mecca of robotic surgery in Europe! Aalst is a small town located halfway between Brussels and Gent and is known for the Onze Lieve Vrouwziekenhuis (OLV). The OLV has a long history of innovative research and is considered one of Belgium’s best-known medical facilities. The OLV Hospital and its staff have earned a remarkable reputation not only in Belgium but across the world, particularly in cardiology, cardiovascular surgery, neurological surgery and, of course, urology. am finally satisfied with the scores. I noticed the improvement in my technique every day. I also set the Da Vinci Si system with training instruments and performed many simulated situations such as anastomosis using plastic models, an exercise which is difficult to access or perform anywhere else. Robotic course I was lucky since I had the chance to attend the official basic robotic course in ORSI. The day-long course was led by Luc, a very skilled mentor from Intuitive. The training started with a discussion about the programme. I was asked general questions about docking and setting up a robot before an operation. I then performed certain exercises with the simulators. Luc evaluated my experience level so he could focus on my weaknesses during the course. Meanwhile, Kevin, another ORSI-staff member, provided a pre-medicated pig and gave the anesthesia. When everything was ready, we placed the trocars, discussing every possible difficulty in a real case. Based on protocol, I was asked to dissect tissue, use the third arm or use coagulation just like in a real A typical day at the ORSI started begins with a cup of case scenario. Even though I had some experience coffee and friendly chat. Afterwards I practise at the with a robot, I never realised how many tips and console, doing the exercises on the simulators. Those tricks I did not know. The protocol steps advanced who tried the simulator will surely know that although smoothly that, at the end, we still had time to do there are easy exercises, there are also very tricky some optional exercises. At the end of the day, I The first day I arrived in the hospital, I was warmly procedures. I focused on the complex procedures, and realised that I just performed my first robotic partial welcomed by Prof. Mottrie who showed me the because I had enough time I would only stop when I and radical nephrectomies, which gave me a very operating rooms. I also met with the team and other wonderful feeling of accomplishment. The day ended fellows who begun their training a few months before with a final simulator exercise to assess the level of me. The fellows came from various countriesimprovement after the course. For satsifactorily Giacomo from Italy, Zach from London (and originally completing the training, I recieved a certificate for from South Africa) and Morgan from Australia. They console surgeon. were all very friendly and the enviroment was certainly supportive. Surgeons from all over the world come to ORSI for the training as a console surgeon. As a fellow, I could The hospital‘s operating days were Tuesdays and observe these training courses and also interact with Thursdays. Operations started at 8 am and the daily the trainees which enabled me to build up on routine would normally end by 6 pm at the earliest. important theoretical knowledge. This also gave me Due to our busy schedule, time flew by very quickly. the opportunity to get to know many future console After I was oriented about the procedures I started robotic surgeons from many countries. bedside assistance and helped in many procedures which enabled me to better understand the anatomy Just like other surgical techniques, adequate skill and of the prostate, kidney and bladder. experience are required from the surgeon and his Me and the skilled ORSI staff members I had the chance to attend the official basic robotic course in ORSI team. The ORSI offers physicians and their teams the opportunity to build the necessary expertise, such as robotic surgery training on a daVinci robot, allowing surgeons to share these new surgical techniques back in their own hospitals. The basic idea is that a learning curve is no longer acceptable, and that a living human body should no longer be considered for training purposes. ORSI offers the alternative in the animal laboratory. Moreover, the robotic surgery trainings are accredited by the European Accreditation Council for Continuing Medical Education (EACCME), providing CME points for medical specialists in their home country. When I returned to Slovakia I've brought with me many new tips and practical insights. I shared with my colleagues step-by-step segments or procedures in doing robot-assisted radical prostatectomy, under the supervision of my chief Dr. Balaz. Two months after my fellowship in Belgium, I've performed two real cases and the goal is to perform in more cases. For young surgeons, Aalst is an extraordinary place where one can train extensively in robot-assisted surgery while experiencing Belgian culture and hospitality. I would like to thank everyone who made possible this rewarding experience, particularly Prof. Mottrie and his staff for their warm welcome and expertise. ESUR Meeting examines research prospects, challenges Experts and top researchers gather in Glasgow Prof. Zoran Culig Chairman EAU Section of Urological Research Innsbruck (AT) zoran.culig@ i-med.ac.at Glasgow hosted the 22nd meeting of the EAU Section of Urological Research (ESUR) from 9 to 11 October which gathered researchers from leading European laboratories and experts who lectured on and discussed the latest developments. Young researchers delivered short oral and poster presentations on topics such as eipthelial to mesenchymal transition, epigenetics in urological disease, circulating tumour cells and tumour metabolism. The role of stromal cells in promoting epithelial to mesenchymal transition was highlighted by Gabri Van Der Pluijm (Leiden, NL), who said that it is necessary to develop therapies that block tumour cell invasiveness and epithelial to mesenchymal transition. An example is a small compound OCD195 that inhibits metastatic progression. There is an increased interest in non-coding RNA (miRNA) in stem cells in prostate cancer. The lectures in the first session have shown that specific miRNA and transcription factors such as ETS have a relevant role in the regulation of cellular stemness. A large number of miRNA is involved in the regulation of stemness as shown in the lectures of G. Van Der Pluijm and G. Carbone (Bellinzona). October/December 2014 One of the meeting's highlights was the presentation of insights from the Cancer Genome Atlas project on muscle invasive bladder cancer by Seth Lerner (Houston, USA). 38 significantly mutated genes from 238 tumours were identified, four of which are involved in epigenetic regulation in urothelium cancer. (Glasgow). In the well-established Pten mutant mice model, Dr. Ahmad has identified genes as potential drivers in aggressive prostate cancer. The poster sessions were well-attended and prompted lively discussions, and have shown that young ESUR researchers appreciated the feedback coming from experienced colleagues and their fellows. Another attractive topic were studies on tumour biology and circulating tumour cells. Although the presence of circulating tumour cells was not associated with clinical and pathological features, determination of circulating tumour cells in bladder cancer diagnostic has a value in survival prediction. S. Riethdorf (Hamburg, DE) gave a very informative lecture on this topic. Current studies have focused on metabolism in urological cancers and highlighted the role of cMyc and cdk4 in the regulation of tumour metabolism (I. Mills, Oslo and L. Fajas Coll, Lausanne). The cell cycle regulators trigger the metabolic switch that is required by cancer cells to proliferate. The excellent social programme included a welcome reception at the Glasgow City Chambers followed by a Scottish-themed evening with dinner and Ceilidh in the Oran Mor. The ESUR is grateful to Prof. Hing Leung, Meeting President (Beatson Institute and University of Glasgow) for his organisational skills and great efforts to secure funding. From left: M. Knowles (ESUR Vice-Chair), E. Zwarthoff (Dominique Chopin award winner), Z. Culig (ESUR Chair), J. Ceraline (ARTP representative) From left: G. Carbone (ARTP jury member), I. Ahmad (ARTP award winner), J. Ceraline (ARTP representative), Z. Culig (ESUR Chair) We look forward to another exciting meeting to be held in Nijmegen, the Netherlands, in September 2015! Two highlights of the meeting were presentations of the research awards. Professor Ellen Zwarthoff (Rotterdam, NL) received the Dominique Chopin Research Award for her contributions to urological research, mentoring, successful acquisition of research funds and contribution to European urology research networks. Her award lecture examined the development and validation of biomarkers for bladder cancer. Her lecture also took up molecular alterations in the pathway of fibroblast growth factor receptors. The Association pour la Recherche sur les Tumeurs de Travel award winners during the ESUR Meeting in Glasgow, la Prostate (ARTP) award was given to Dr. I. Ahmad 10 October 2014 – supported by the Movember Foundation European Urology Today 31 Prostate stem cell research continues hunt for genetic clues EAU-RF Career Development Programme backs PCa research By Joel Vega However, so-called “slow-cycling” stem cells will retain the label, enabling their identification as label-retaining cells, and their screening for expression of different markers. Researchers not only identified a candidate slow-cycling label retaining SC population in the basal cell layer, but more importantly they identified a candidate slow-cycling SC population in the luminal cell layer. With the backing of the EAU-Research Foundation (EAU-RF), a Sweden-based researcher investigating the characteristics of prostate stem cells in mouse models has identified a stem cell population in the prostate’s luminal cell layer. Although there are many questions that have to be resolved, the researchers have widened their goals as Aside from the candidate prostate SCs, the researchers the study enters its second year, adding objectives such as performing in vivo cell lineage tracing of also identified cell surface receptors and nuclear androgen receptor (AR) expression in the candidate SC candidate murine SCs and functional assays of isolated human normal and malignant SCs, with the populations, a finding that opens up the possibility that AR expressing luminal SCs or stem-like cells could aim to better identify and characterise human CSCs and biomarkers. function as cancer-initiating cells in PCa. The study has implications in the search for genetic clues that could later help in targetting and in the development of new therapeutics for prostate cancer (PCa) particularly those tumours which are metastatic or highly resistant to drug treatment. “Recent research has suggested the existence of cancer stem-like cells in prostate cancer, and that such cells may be the culprit behind therapy resistance and progression of the disease,” said Dr. Jens Ceder, lead study investigator who is based in Lund University and Skåne University Hospital in Malmö, Sweden. Dr. Jens Ceder “It has also been suggested that tumour-initiating cells of prostate cancers originate from adult stem cells in the basal layer of the prostate, since rare cells with a basal phenotypes survive castration in prostate cancer patients,” he explained. marker expression in the developing and adult prostate identifies basal and luminal stem cell subpopulations,” described findings of separate basal and luminal stem cell populations in the mouse prostate. Ceder recently presented the second-year results during an abstract session at the 22nd Annual Meeting of the EAU Section of Urological Research (ESUR) recently held in Glasgow, UK. The ongoing study, with funding from the EAU-RF Career Development Programme, has completed its initial aim to identify and characterise normal murine candidate prostate stem cells. In Glasgow, Ceder’s presentation titled “Label retaining and stem cell EAU Research Foundation are up-regulated/activated in these cells in prostate cancer, and which may aid in prognosis, and perhaps also in stratifying patients for different treatment, and targets that could be druggable,” Ceder said. The study used a process called label-retention to identify the normal stem cells (SCs) in the mouse prostate gland by using a label called bromodeoxyuridine (BrdU), which is taken up by dividing cells when the prostate is formed. Later, the BrdU label is washed out in rapidly growing transit amplifying cells. Stem cells “We have used a very robust method for identifying tissue stem cells that takes advantage of the relatively quiescent nature of stem cells, in which cells are pulsed with the BrdU,” explained Ceder. That finding supports current scientific theory which suggests that tumour-initiating cells of prostate cancers originate from adult stem cells, but it has remained controversial whether luminal SC exists in addition to basal SCs. “Our goal is for the studies to open up for the development of new therapeutics. It is beyond the scope of this study for any kind of clinical investigation at this stage,” added Ceder when asked if he is optimistic of a breakthrough outcome. “But we have indications that some of the markers we have identified will aid in future prognostics of prostate cancer, and that the pathways found downstream of these markers can be targeted, and naturally we intend to investigate this during the coming year.” “But translating the results from mouse to human being is perhaps the biggest obstacle since there are differences that should not be ignored. Therefore, human samples are of utmost importance…Moreover, it is extremely important to validate the data in human material, especially so in advanced disease,” added Ceder. Development programme The EAU-RF Career Development Programme, which is funding innovative studies in basic science, exerts efforts to bridge basic and translational research, while aiming to provide a platform for talented researchers to pursue pioneering research. Aside from its direct support to novel studies, the programme also hopes that its pool of researchers are ably supported in developing their career goals. The With scarce SC markers and experimental assays for functional studies, researchers still faced obstacles in EAU-RF links up with both medical and academic institutions in identifying promising talents and investigating the cancer stem cells (CSC) theory. The research work that deserves support. Supporting preliminary data also suggest that one of their candidate SC markers is up-regulated in advanced Ceder’s study are their partners and collaborators at the Radboud University in the Netherlands and the disease. University of York’s YCR Cancer Research United in “We are working on identifying pathway-proteins that the UK. EUSP Clinical Visit A comprehensive and rewarding training in Braga, Portugal Dr. Antonio Cicione Magna Graecia University Catanzaro (IT) electromagnetic kidney puncture system1. Likewise, the Braga Hospital’s Urology Department routinely offers 3D laparoscopic surgery to perform advanced laparoscopic procedures, including radical cystectomy with intracorporeal urinary diversion. Its emphasis on technology is among the centre’s many activities that make this institution attractive to a young urologist. The hospital has the following features and facilities: [email protected] • A science laboratory where all the endourological/laparoscopic equipment and pelvic trainer boxes can be used. As Prof. Lima has said: “If you have an idea- any idea- you can immediately test it in our laboratory”; • Uro-oncological surgery is performed principally using laparoscopy. Furthermore, as a tertiary centre in northern Portugal, many procedures for stone disease are performed every year, including extracorporeal lithotripsy, flexible and semi-rigid ureteroscopy and percutaneous renal lithotripsy, procedures which are done almost on a daily basis. • A friendly and professional environment for trainees. Each surgical procedure was explained by Prof. Lima and his team in a step-by-step manner, allowing me to fully understand any aspects of the procedures we were performing. In a very short time I gained more experience and confidence with urological laparoscopic surgery and percutaneous renal surgery. I also often used laser lithotripsy with flexible or semi rigid ureteroscopy. From April 1 to July 14, 2014 I had a three-month clinical visit under the auspices of the European Urology Scholarship Programme (EUSP) at the Braga Hospital, Universidade Do Minho Life and Science Research Institute in Braga, Portugal. Braga, one of Portugal’s largest cities and located in the northern Minho region, is known as “Portuguese Rome” due to its history and the many Catholic churches built in the city. And just like other university cities in Europe, the city has a lively cosmopolitan atmosphere with English widely spoken by local residents. A leading and well-equipped centre, the Braga Hospital is a tertiary academic hospital with 12 operating theatres and a 705-bed capacity. The hospital was recently opened and built according to the newest standards of healthcare architecture. Prof. Estevao Lima, an active member of the EAU Section of Uro-Technology’s (ESUT) expert panel, chairs the hospital’s Urology Department. A joint venture was established between this new hospital and the Universidade Do Minho Life and Science Research Institute where every physician has the opportunity to participate in pre-clinical hands-on training and to actively participate in several research projects in a fully equipped animal laboratory with the latest technology available. For instance, before my visit, Prof. Lima and his team had successfully conducted a research on a new European Urological Scholarship Programme Office 32 European Urology Today A “friendly” picture with Prof. Lima (lower left) and his team in Braga A and B: views of Life and Science Research Institute at Universidade do Minho; C and D: Endourological laboratory hosted in the Institute • A multi-disciplinary collaboration that enhances the training. Once a week, an oncological meeting is scheduled to discuss the optimal treatment option for borderline patient cases. Radiotherapist, oncologist and a urologist take part and present their viewpoints. Furthermore, the whole urology team conducts a weekly discussion of a singular case and takes a common decision regarding treatment options. Finally, a monthly research meeting is organized at the department, together with engineers and biologists, to update the participants on current research and suggest a new topic. I certainly had the opportunity during this threemonth visit to improve my surgical curriculum by taking part as first or second surgeon in many surgical procedures and while expanding my overseas contacts. My gratitude to the EAU and the EUSP board for this wonderful opportunity and to Prof Estevão Lima and his team, including the nurses and administrative workers, for their hospitality, and for the experience that surely reflected the EUSP’s goal: enhancing skills and cooperation through European schooling. Reference 1. Rodrigues PL, Vilaça JL, Oliveira C, Cicione A, Rassweiler J, Fonseca J, Rodrigues NF, Correia-Pinto J, Lima E Collecting system percutaneous access using real-time tracking sensors: first pig model in vivo experience. J Urol. 2013 Nov; 190(5):1932-7. October/December 2014 NIMBUS trial re-opens in Germany, starts in The Netherlands A European multi-centre prospectively randomised Phase III clinical trial in high grade NMIBC patients Dr. Wim Witjes Scientific and Clinical Research Director EAU Research Foundation Arnhem (NL) w.witjes@ uroweb.org Dr. Raymond Schipper Clinical Project Manager EAU Research Foundation Arnhem (NL) r.schipper@ uroweb.org National Coordinators: Marc-Oliver Grimm, Antoine Van Der Heijden, Hugh Mostafid, Luis MartinezPiñeiro, Marko Babjuk, Levent Turkeri The NIMBUS trial assesses whether a reduced number of BCG instillations is not inferior to standard number and dose intravesical BCG treatment in patients with high grade non-muscle invasive bladder cancer (NMIBC). The target is to enrol 1000 patients with high grade Ta-T1 urothelial carcinoma of the bladder with or without CIS and who did not receive any BCG intravesical instillation therapy from urology departments in European hospitals participating in this study. The EAU Research Foundation (EAU-RF) has started this European study in patients who undergo intravesical BCG treatment for their non-muscle invasive bladder (NMIBC) cancer. The study is titled: Treatment of High Grade Non-Muscle Invasive Urothelial Carcinoma of the Bladder by Standard Number and Dose of Intravesical BCG Instillations versus Reduced Number of Intravesical Instillations with Standard Dose of BCG. A European Association of Urology Research Foundation Prospectively Randomised Phase III Clinical Trial. (NIMBUS) NIMBUS started in Germany in 32 centres with a grant from the German Cancer Fund. Randomisation was put on-hold temporarily due to the lack of availability of BCG Medac. This situation is expected to change in November/December 2014 whereafter randomisation efforts can be resumed. In the Netherlands, the first centres are now initiated and the first 2 patients were randomised. In the UK and Spain we have performed a feasibility that showed there is much interest to participate in this EAU-RF project. In the UK, grant applications are being prepared and the expectation is that it is likely that we can start the project next year in 20 to 25 UK centres. Also in Spain, preparations are ongoing to start next year in approximately 15 centres. Possibilities to cooperate and start up in other countries like Czech Republic, Turkey, France and Italy are currently being evaluated. The primary endpoint for inferiority analysis is time-to-first-recurrence. The secondary objectives are to identify if number and grade of recurrent tumours, rate of progression to a higher stage (T2 or higher) of the disease and safety, specifically the presence of treatment related toxicity > grade 2 differ between the two study arms. The objectives of a cytokines sub-study and a DNA sub-study- studies that will take place in selected centres only- are to evaluate the impact of therapy on cytokines and to evaluate the results of DNA analysis as a prognostic factor, respectively. Rationale Intravesical instillation of BCG is a widely accepted strategy to prevent recurrence of non-muscle invasive bladder cancer. The most accepted treatment schedule is induction of BCG: weeks 1 through 6 plus maintenance (weeks 1,2,3) at months 3,6 and 12, but it is unknown how many administrations are really necessary. Scientific evidence supports the hypothesis that after an initial sensitisation to BCG antigens has occurred, the number of instillations can be reduced for a proper anamnestic immune response resulting in similar clinical efficacy and potentially less side-effects and costs. EAU Research Foundation Study Design This is a multicentre prospective, randomised, parallel group, not blinded, trial to compare the efficacy and safety of two different adjuvant treatment schedules: 1) Induction cycle BCG-full dose; weeks 1 through 6 plus maintenance cycles at months 3, 6 and 12 (wks 1,2,3); total 15 full dose BCG instillations 2) Induction cycle BCG-full dose (reduced frequency); weeks 1,2, and 6 plus maintenance cycles at months 3, 6 and 12 (wks 1,3); total 9 full dose BCG instillations. 10. Presence of active tuberculosis, any form of immunodeficiency (e.g., HIV + serology, transplant recipients) and/or any other contraindication of BCG therapy 11. Patients with a WHO performance score of > 2 or ASA grade 4-5 12. Patients who have received any systemic cytostatic agents within the last 3 months 13. Patients older than 80 years of age 14. Patients with uncontrollable UTI 15. Patients with White Blood Count (WBC) below 3.0 x 109/l or platelet count below 100 x 109/l at baseline 16. Renal and hepatic function values BCG intravesical instillation therapy is registered as adjuvant treatment for the prevention of recurrence of NMIBC and can be considered as standard treatment for the type of patients requested in this trial. For each individual centre, one of the three locally available BCG strains in Europe will be used: BCG Tice, BCG Medac or BCG Connaught. • Levent Türkeri, Istanbul • Marc-Oliver Grimm, Jena • Wim Witjes, Arnhem Study status As of press time (cut-off date 28 October 2014), 30 centres are initiated in Germany of which 7 sites randomised, in total, 12 patients. The Clinical Studies Coordination Centre at the University Clinic in Jena is coordinating the activities to enable the German participants to include their patients. In the Netherlands (approval of the study by the central After the first transurethral resection (TUR), according to the EAU Guidelines, patient undergoes ethical committee was obtained in October 2014) 13 centres will be initiated before the end of 2014. a re-TUR 6 weeks (between 4-8 weeks) after the The EAU Central Research Office is currently active in complete resection. Patients with histological the initiation of Dutch centres. detection of high grade NMBIC in the re-TUR who undergo a second re-TUR are eligible for the study Study team if they fulfil all selection criteria, i.e., patients Protocol Writing Committee should be macroscopically tumour-free. If so, first • Marko Babjuk, Prague re-TUR is considered as TUR as defined by the protocol. Treatment with the randomised treatment • Luis Martinez-Pineiro, Madrid schedule will start 2 weeks after and no later than • Joan Palou Redorta, Barcelona • Anup Patel, London 6 weeks after the last resection (re-TUR). The first maintenance therapy should be given 3 months (12 weeks) after the last instillation of the induction BCG cycle (week 6) and hereafter at months 6 (24 weeks) and 12 (48 weeks) after the last instillation of the induction BCG cycle. Standard Dose Instillations will take place with 1 vial of BCG. The weekly BCG instillations during induction and maintenance cycles have to be conducted within 7 ± 2 days. Follow-up cystoscopy and cytology will be done every 3 months in the first 2 years and bi-annually until the fifth year. Study population Inclusion Criteria: 1. Presence of high grade (Ta-T1) urothelial carcinoma of the bladder with or without CIS 1.1. Tumours can be primary or recurrent 1.2.Tumours can be single or multiple 2. Re-TUR should be performed at weeks 4-8 after initial resection, which must include the deep resection or cold cup biopsy (deep enough to obtain muscle tissue) of the initial tumour site(s) 3. All visible tumours must be completely resected 4. Early postoperative (within 6 hours of resection) single-dose chemotherapy is allowed after the first resection. However, it should not be given after re-TUR if the patient is considered eligible for this study 5. Prior multi-instillation intravesical chemotherapy is allowed, provided that the last instillation was completed 3 months before randomisation in this study. 6. Signed and dated informed consent form. Exclusion Criteria: 1. Any previous intravesical BCG therapy 2. Presence of primary CIS only. 3. Presence of histopathologically proven muscle invasive urothelial carcinoma of the bladder at first or re-TUR surgical specimens 4. Patients with incomplete resection of visible tumours 5. Absence of muscle tissue in the re-TUR specimen(s) 6. Presence of any upper urinary tract tumours at any time 7. Presence of any other histological type of resected tumour other than urothelial carcinoma on the first or second resection 8. Presence of another malignancy other than the basal cell carcinoma of the skin 9. Presence of pregnancy or lactation Study Principal Investigators • Levent Türkeri Marmara University Medical School – Istanbul, Turkey • Marko Babjuk Charles University 2nd Faculty of Medicine – Prague, Czech Republic National Coordinators • Germany: Marc-Oliver Grimm, Jena • The Netherlands: Antoine Van Der Heijden • United Kingdom: Hugh Mostafid • Spain: Luis Martinez-Piñeiro • Czech Republic: Marko Babjuk • Turkey: Levent Türkeri • France: Marc Colombel • Italy: Andrea Tubaro EAU Research Foundation Wim Witjes, Scientific and Clinical Research Director Raymond Schipper, Clinical Project manager Christien Caris, Clinical Project manager Sheik Nurmohamed, Clinical Project/data manager Ria Janzing, Clinical Research Associate Joke Van Egmond, Data manager Arm 1 – N= 500 Inducon Cycle - Full Dose Total 15 full dose BCG Insllaons N = 1000 High Grade Non-Muscle In- Study Duraon: 2-year recruitment RANDOMIZATION vasive Bladder Cancer 3-year observaon Arm 2 – N= 500 Inducon Cycle - Full Dose (Reduced Frequency) Total 9 full dose BCG Ins llaons Lageübersicht Prüfstellen – NIMBUS - Studie NIMBUS Centres in Germany: Green - centres with randomised patients, Blue - centres initiated, Red - Jena centre Blauw zijn de sites die wel al geïnitieerd zijn maar nog geen patiënten gerandomiseerd hebben October/December 2014 Groen zijn de sites die al patiënten gerandomiseerd hebben European Urology Today 33 European Urology Forum 2015 Challenge the experts 7-10 February 2015, Davos, Switzerland Saturday, 7 February 2015 Sunday, 8 February 2015 16.10 – 16.15 Opening and welcome C.R. Chapple, Sheffield (GB) J. Palou, Barcelona (ES) 07.30 – 08.45 An update on medical urology for the urooncologist Chair: N. Clarke, Manchester (GB) Participants: P-A. Abrahamsson, Malmö (SE) C. Stief, Munich (DE) M. Wirth, Dresden (DE) 16.15 – 18.00 What is new in urology 1 Chairs: C.R. Chapple, Sheffield (GB) J. Palou, Barcelona (ES) 16.15 – 16.35 Functional urology P. Abrams, Bristol (GB) 16.35 – 16.55 What’s new in renal cancer H.G. Van Der Poel, Amsterdam (NL) 16.55 – 17.15 Recent developments in laparoscopy A. Breda, Barcelona (ES) 17.15 – 17.35 What is new in endourology E. Liatsikos, Patras (GR) 17.35 – 18.00 Prostate cancer A. Bjartell, Malmö (SE) 08.45 – 09.00 Coffee break 09.00 – 11.00 Urological challenge Chair: F.M.J. Debruyne, Arnhem (NL) Challengers: J. Dobruch, Warsaw (PL) H. Hashim, Bristol (GB) S. Hruby, Salzburg (AT) O. Rodriguez Faba, Barcelona (ES) S. Tyritzis, Athens (GR) 11.00 – 11.30 18.00 – 18.10 Coffee break 18.10 – 19.30 What is new in urology 2 Chair: J. Palou, Barcelona (ES) 18.10 – 18.30 Erectile dysfunction W. Aulitzky, Vienna (AT) 18.30 – 18.50 Bladder cancer N. Clarke, Manchester (GB) 18.50 – 19.10 Paediatric urology J.M. Nijman, Groningen (NL) 19.10 – 19.30 Screening and treating prostate cancer in the elderly J.C. Hu, LA (US) 11.30 – 15.30 “Minimally invasive percutaneous stone therapy: MIP 2.0 XS, S, M + L, Downsizing is not enough” U. Nagele, Hall inn (AT) Industry sponsored Video session 1 17.00 – 19.00 Hands-on training on URS Tutors: A. Breda, Barcelona (ES) J-T. Klein, Heilbronn (DE) T. Knoll, Sindelfingen (DE) P.J. Osther, Fredericia (DK) Industry sponsored 18.00 – 19.15 Urological challenge Chair: F.M.J. Debruyne, Arnhem (NL) Monday, 9 February 2015 08.15 – 08.45 Complications of mesh and how to manage them C.R. Chapple, Sheffield (GB) 08.45 – 09.00 Coffee break 09.00 – 11.00 Urological challenge Chair: F.M.J. Debruyne, Arnhem (NL) 11.00 – 15.30 Video Session 2 16.00 – 16.30 Critical evaluation of minimally invasive surgery for renal oncology J.C. Hu, LA (US) 16.30 – 17.15 16.00 – 16.45 Update on new interventional management of urolithiasis ESWL – J. Rassweiler, Heilbronn (DE) URS – K. Sarica, Istanbul (TR) PCNL – T. Bach, Hamburg (DE) 16.45 – 17.45 Functional urology cases Chair: P. Abrams, Bristol (GB) Participants: D.M. Castro Diaz, Santa Cruz de Tenerife (ES) C.R. Chapple, Sheffield (GB) 17.45 – 18.00 Coffee break How to avoid complications and deal with them with radical prostatectomy Moderator: W. Artibani, Verona (IT) Participants: A. Bjartell, Malmö (SE) J. Palou, Barcelona (ES) C. Stief, Munich (DE) 17.15 – 17.45 Testosterone replacement therapy – a contemporary update on its use in clinical urology W. Aulitzky, Vienna (AT) 17.00 - 19.00 Hands-on training on URS Tutors: A. Breda, Barcelona (ES) J-T. Klein, Heilbronn (DE) T. Knoll, Sindelfingen (DE) P.J. Osther, Fredericia (DK) Industry sponsored 17.45 – 18.00 Coffee break 18.00 – 19.15 Urological Challenge Chair: F.M.J. Debruyne, Arnhem (NL) Tuesday, 10 February 2015 07.30 – 08.15 Update on bladder cancer management Chair: C. Stief, Munich (DE) Participants: J. Palou, Barcelona (ES) N. Clarke, Manchester (GB) 08.15 – 08.45 Adjunct therapy for prostate cancer – has this come of age? P-A. Abrahamsson, Malmö (SE) 08.45 – 09.00 Coffee break 09.00 – 11.00 Urological challenge Chair: F.M.J. Debruyne, Arnhem (NL) 11.00 – 15.30 Video session 3 16.00 – 16.30 Personalised medicine – an important new direction for urology W. Artibani, Verona (IT) 16.30 – 17.00 Translational research in oncology Chair: N. Clarke, Manchester (GB) Participants: A. Bjartell, Malmö (SE) J.C. Hu, LA (US) H. Van Der Poel, Amsterdam (NL) 17.00 – 18.00 Paediatric cases J.M. Nijman, Groningen (NL) 18.00 – 18.15 Coffee Break 18.15 – 19.30 Urological challenge Chair: F.M.J. Debruyne, Arnhem (NL) EAU and partners: synergies Collaborative partnerships enable EAU to pursue goals Prof. Chris Chapple EAU Secretary General Elect Chairman, EAU International Relations Office C.R.Chapple@ sheffield.ac.uk The ethos of the European Association of Urology (EAU) is to work closely with all the European national associations to promote and advance urological practice. In this context, the EAU collaborates closely with a number of patient organisations to achieve this aim. It is also particularly important to work with the European Commission to fulfil this goal and to help represent the interests of our partner national associations within Europe. We have continued to further expand our ongoing educational and scientific activities within Europe. Following on from the enormous success of our annual meeting in Stockholm, preparations are well advanced for the forthcoming meeting in Madrid. In addition to the scientific congress activities, more about which you will be reading on our website in the next few months, we also organise the incredibly successful residents training meeting (EUREP) which has now been held for 13 consecutive years and at which 350 residents in the final stages of their training attend. This is just a sample of the wide range of activities which are ongoing including the activities related to the enormously successful Guidelines publications which are available to all members and can be The EAU has had a number of very successful downloaded and utilised not only in their long form meetings which have been held at a national and pan-national level within Europe and beyond over the but also in the abridged version with an last nine months. We recently had a very successful meeting with our colleagues in Russia at the Russian Society of Urology Congress in Saratov. The Société Internationale d'Urologie (SIU) meeting was recently held in Glasgow and the strong collaboration between EAU and SIU was exemplified by the EAU session at this meeting and the strong participation of EAU members. The EAU is continuing to strengthen its close interaction with fellow urologists across the globe as emphasised by the number of teaching activities which we have participated in, such as the EAU joining in with the Asian Society of Urology meeting held on Kish Island from 5 to 9 December. In addition, we recently held the 11th meeting of the European Robotic Urology Section (ERUS) in Amsterdam, under the auspices of the EAU, with over 700 attendees. Another major event is the European Multidisciplinary Meeting on Urological Cancers (EMUC) of which the sixth edition was held in Lisbon, Portugal in November, which attracted over 1400 attendees, and hosted an ICUD meeting on the preceding Friday and and the 3rd Meeting of the EAU Section of Urological Imaging. 34 European Urology Today Under the auspices of the EAU Section of Genitourinary Reconstructive Surgeons (ESGURS) and in close collaboration with the European Society for Paediatric Urology (ESPU), the first ESGURS-ESPU meeting was held, tackling issues in genito-urinary reconstruction particularly those affecting adolescent and paediatric patients. On the occasion of the Emirates Urology Society meeting, the EAU collaborated with the society to stage a comprehensive educational programme on 14-15 November and have further similar activities planned for next year. accompanying app which can be purchased for a nominal fee. The EAU Section Office organised successful projects and their activities cover the whole area of contemporary urology. The integration of all of our activities and offices, including the Scholarship Office, the Education Office (European School of Urology), and the Scientific Congress Office, and the participation of all EAU members with the strong support of their national societies, exemplify the wide and unified goals of our on-going educational programmes within European urology. Please make sure you have the date of the next annual meeting in your diaries - 20-24 March 2015, Madrid, Spain. We look forward to meeting you there! No one succeeds alone. We are proud to be a part of a hard-working, dedicated community. We know and understand the importance of collaboration, of sharing and building on the ideas of others. That’s why we’re expanding into social media platforms so that we can increase interaction with and within the community. europeanurology.com european urology Forward faster. Together. european urology October/December 2014 Forward faster. Together. Don’t forget to renew your EAU Membership! A message from the Membership Office Our members are the heart of the EAU. Their knowledge, experience, and talents help to make the EAU the vibrant community it is today. We would like to thank you for your membership and your contribution to our association. It helps us to continuously improve urological practice, research and education in order to raise the level of urological care in Europe and beyond. Please pay your fees on time in order to keep enjoying the benefits of EAU membership. Thanks to your support we were able to accomplish many successes in 2014. Our major achievements of last year are: •Scholarships: The European Urological Scholarship Programme (EUSP) supports young and upcoming urologists and researchers financially to stimulate clinical and experimental research across Europe and to share of expertise and knowledge exchange. This year we approved 5 scholarships, 3 visiting professor programmes, 1 short visit and 18 clinical visits. •Guidelines: This year, besides EAU Pocket Guidelines for iOS, we launched an Android version as well. Both apps are free for members and have been downloaded 4180 times in 2014. • European Urology: Our official journal, is currently read by more than 20,000 urologists across the globe, recently received an Impact Factor of 12.480, making it the leading scientific publication in the field of urology. The European Urology app, which was launched earlier this year, was downloaded 2860 times. What to Expect in 2015: In this rapidly changing field we aim to offer you a platform to keep you abreast with the latest developments in urology, to prepare you for new technology and to help you better serve your patients’ needs. For 2015 we are focussing on the following innovations: •Education: Easy access to quality education and scientific resources is a top priority of the EAU. That is why we are currently developing a comprehensive online resource centre, which will contain the best scientific content from our meetings, innovative e-courses, top-notch surgical videos and practical workshops to improve your surgical skills. To be expected in March 2015. •Policy: Political initiatives impact urology professionals and patients in various areas. For 2015 the EAU will focus on enlarging its influence in the European politics and law-making to raise the voice of the urological community. • Patient Information: Patients are the driving force and inspiration for all of our activities. This year we will launch four new topics in EAU Patient Information and we translated the existing Patient Information into 10 different languages. For 2015 we plan to add several new topics in major European languages. Renew your membership! We kindly remind all EAU members to pay their membership fees for 2015 on time. In early November we sent an e-mail invoice to all current members for the 2015 fees (1 January – 31 December 2015). This invoice has to be paid by 1 January 2015. Members can pay by bank transfer, online with credit card through MY-EAU or by direct debit. Please check your MY-EAU account to ensure that we have your correct e-mail address, as invoices and reminders will be sent by e-mail. In case the invoice is not paid on time, a reminder will be sent, followed by a second reminder which will include an additional €15 administrative fee. Should the fees still not be paid, a third reminder will be sent with another €15 administrative fee, for a total of €30. If payment has not been received after these reminders, membership will be cancelled. Should you wish to register for the 2015 Annual EAU Congress, and your membership is cancelled, you cannot make use of the membership discount. In order to reactivate your membership, you will have to pay the membership fee as well as the outstanding costs amounting to around €45 to €75 (depending on your membership type). The EAU offers its members the convenience of paying by direct debit. A SEPA form will be made available through MY-EAU which can be filled out, signed and sent to the EAU by email. The SEPA form can also be printed and sent by post. This way, membership fees will be transferred from your account automatically when due, and you have no risk of additional administrative fees due to delayed payment. This option is available to members in the Single Euro Payments Area (SEPA), which includes all EU Help urologists collect CME credits and register your activity today! countries as well as Iceland, Liechtenstein, Norway, Switzerland and Monaco. Don’t miss the opportunity to renew your membership! Have you moved? Changed name? New employer? (Inter)National Urological Associations and the CME providers (organisers of CME activities) are invited and encouraged to send in requests to register nationally accredited CME activities or requests for European accreditation. Alter your personal data on-line: fast and easy - www.eu-acme.org www.eu.acme.org UROLOGY WEEK 2014 Various events to increase awareness of urology and inform the public Journée d’information le 24 septembre 2014 de 9h à 18h à la Clinique Charcot – Sainte Foy-lès-Lyon RASTREIOS GRATUITOS NA REDE SAÚDE CUF organised Urology Week events for the first time “in itsWehistory. It was also the first time Urology Week took 2014 Vážení mediální zástupci, zveme Vás na tiskovou konferenci na téma: Onkologická onemocnění v urologii, prevence, jak je včas diagnostikovat a vyléčit, novinky v diagnostice i léčbě HIPERPLASIA BENIGNA DA PRÓSTATA INFORMEZ-VOUS ! Consultez un urologue kterou pořádáme v rámci projektu European Association of Urology – Urology Week. Občanské sdružení Europa UOMO CZ je českou odnoží Evropské koalice proti rakovině prostaty. 25. září 2014 od 10.00 hodin národní Banka vín, platnéřská 4, praha 1 (vchod z ulice křížovnická 1) program tiskové konference Karcinom prostaty prof. MUDr. Dalibor Pacík, CSc. přednosta urologické kliniky FN Brno, předseda Europa UOMO CZ, člen International Prostate Health Council Nádory ledvin as. MUDr. Vítězslav Vít vedoucí onkologické poradny urologické kliniky FN Brno LF MU Nádory varlat as. MUDr. Gabriel Varga, FEBU vedoucí lékař JIP a UD poradny urologické kliniky FN Brno LF MU Marque em qualquer receção ou através de telefone Nádory močového měchýře as. MUDr. Vítězslav Vít vedoucí onkologické poradny urologické kliniky FN Brno LF MU DIA 27 SETEMBRO APOSTE NA PREVENÇÃO O aumento do tamanho da próstata denomina-se hiperplasia ou hipertrofia benigna da próstata. É uma das patologia mais frequentes em homens a partir dos 50 anos e a sua prevalência aumenta com a idade. CUF Infante Santo 213 926 100 • CUF Descobertas 210 025 200 • CUF Porto Hospital 220 039 000 • CUF Porto Instituto 220 033 500 CUF Belém 213 612 300 • CUF Alvalade 210 019 500 • CUF Torres Vedras 261 008 000 • CUF Cascais 211 141 400 Na závěr tiskové konference Vás zveme na malé občerstvení. La Semaine de l’Urologie, du 22 au 26 Septembre, est une initiative de l’Association Européenne d’Urologie afin de sensibiliser le grand public aux différentes pathologies touchant les reins, la vessie, la prostate. Těšíme se na společné setkání! Pořadatel: V případě zájmu prosíme o potvrzení Vaší účasti. Eliška Kubátová – produkční Forinel Trading SE, Na hlídce 22, 130 00 Praha 3 Mobil. tel.: 733 710 382 E-mail: [email protected] Záštita: Organizátor: Pod záštitou MUDr. R. Krause, MBA, ředitele FN Brn France, Clinique Charcot An open day in Lyon with urologists ready to answer people’s questions The Urology Week events organised by AUSA were not only an initiative of urology professionals but patients groups and the general public were also involved. The initiative was widely promoted through posters and pamphlets distributed by AUSA. Pod záštitou prof. MUDr. J. Mayera, CSc., děkana LF MU www.saudecuf.pt Portugal, Saúde Cuf Free prostate screening in all clinics and hospitals in Portugal place in Albania. The main event was called “Urologist for a Day” – a fun, but highly educational initiative aimed to create awareness about kidney cancer, bladder cancer, and prostate cancer. The focus was on early detection of these diseases. Czech Republic, EUROPA UOMO CZ Organised a press conference for its Czech branch in Prague A Urology Week rally in the centre of Albania’s capital, Tirana, was a perfect way to attract the attention of both the media and the general public. AUSA carried out a street poll among bystanders, inquiring about their knowledge of PSA tests and offering them information about it when necessary. The opportunity for AUSA members to engage with the general public face-to-face painted a clear picture of the information level and helped to generate ideas for follow-up initiatives. In another event urologists provided free consultations on kidney, bladder, and prostate cancer. The President of AUSA, Prof. Kim, published several articles in local newspapers and was interviewed by two important national television channels. AUSA also helped to arrange free PSA examinations. More than 350 men received a free consultation. Albania, Albanian Society of Urology Organised Urological Week 2014, 11 symposia of Urology, 242 doctors participated Find out more: www.urologyweek.org October/December 2014 Finally, AUSA organised an informative walk against kidney cancer, bladder cancer and prostate cancer in Tirana which gathered over 700 people – mostly men with these conditions and their spouses. It was not aimed to address the seriousness of the situation in which cancer patients can find themselves, but this event was dedicated to the positive outlook on life. It stressed the fact that patients with these conditions can, and should, be able to have the respect of society and live a normal life. ” By Prof.Ass.Dr.Kim Drasa - President AUSA Albanian Urologists & Sexologists Association Czech ek activities of hospitals in the Check the other Urology We n, Poland, ista Pak rg, bou em Greece, Italy, Lux Republic, France, Germany, Kingdom at in, Switzerland and the United Portugal, Romania, Serbia, Spa www.urologyweek.org #urologyweek European Urology Today 35 Congress calendar 2014/2015 December 11-12: Hall in Tirol, Austria Minimally Invasive Percutaneous Stone Therapy Clinical Workshop (MIP) Contact: Dept of Urology and Andrology Phone: +43 50 504 36310 Fax: +43 50 504 67 36310 E-mail:[email protected] 11-15: Maastricht, The Netherlands Pelvic Floor Neuromodulation advanced training program Contact: European Continuing Medical Training ECMT Phone: +31 618099653 Fax: +31 847413849 E-mail:[email protected] Website:http://www.ecmt-training.com 12: Spa, Belgium BAU2014: 14th edition of the annual congress of the Belgian Association of Urology Contact: e-HIMS bvba Fax: +32 3 491 8271 E-mail:[email protected] Website:http://bau2014.be/ 12-13: Aurassi Algiers, Algeria 10th Congress of Urology Algerian Contact: Dr. Chawki Djeffal, General secretary Algerian Association of Urology AAU E-mail:[email protected] 14: Tbilisi, Georgia National congress of the Georgian Association of Urology Contact: Prof. L. Managadze Phone: +995 32 96 48 70 Fax: +995 32 96 48 70 Website:www.gua.org.ge 14: ESU organised course on LUTS and incontinence: Where is the truth? at the time of the national congress of the Georgian Association of Urology Contact:ESU 18-20: Cairo, Egypt 17th Copenhagen Symposium on Endoscopic Urological Surgery Contact: International Conference Services ICS Phone: +45 3946 0500 E-mail:[email protected] Website:www.seus2015.com Operative Skills in Urology: Modules 3 and 4 Contact: RCS Education Phone: +44 20 7869 6300 E-mail:[email protected] Website:https://www.rcseng.ac.uk/courses/ course-search/operative-skills-inurology-modules-3-4 February 2015 1-6: Caceres, Spain Hands-on training skills programme on Laparoscopy and Endourology Contact:ESU 5-7: Rome, Italy 3rd Edition Global Congress on Prostate Cancer 2015 E-mail:[email protected] Website:www.prosca.org 5-7: Copenhagen, Denmark 17th Congress of the European Society for Sexual Medicine Phone: +49 40 6708820 E-mail:[email protected] Website:http://www.essm-congress.org 5-8: Ranchi - Jharkhand, India 48th Annual Conference of Urological Society of India (USICON) Contact: USICON 2014 Secretariat Phone: +91 11 23404323 Fax: +91 11 23360067 E-mail:[email protected] Website:www.usicon2015.com 7-10: Davos, Switzerland European Urology Forum 2015 – Challenge the experts Contact:ESU Phone: +31 26 389 0680 Fax: +31 26 389 0674 E-mail:[email protected] Website:www.esudavos15.org 12-14: Doha, Qatar 19-20: Arezzo, Italy 19-20: Hall in Tirol, Austria 3rd Junior Users Meeting, To Begin and Progress Urologic Robotic Surgery - EAU Endorsed Location: San Donato Hospital Contact: Prof. Filippo Annino E-mail:[email protected] Minimally Invasive Percutaneous Stone Therapy – Clinical Workshop Contact: Ms. Sabine Weinberger and Ms. Miriam Faik Phone: +43 50 504 36310 Fax: +43 50 504 67 36310 E-mail:[email protected] 12th Meeting of the EAU Section of Oncological Urology (ESOU) Contact: Congress Consultants B.V. Phone: +31 26 389 1751 Fax: +31 26 389 1752 E-mail:[email protected] Website:www.esou15.org 23-26: Belgrade, Serbia 1st International course on uro-genital reconstructive surgery Contact: Center for Genito-Urethral Reconstructive Surgery Phone: +381 11 2474 918/ +381 66 600 9902 Fax: +381 11 2475 954 E-mail:[email protected] [email protected] Website:www.savaperovic.com www.savaperovicfoundation.com 27: Copenhagen, Denmark Pre-course in Robotic Surgery at the time of the 17th Copenhagen Symposium on Endoscopic Urological Surgery Contact: International Conference Services ICS Phone: +45 3946 0500 E-mail:[email protected] Website:www.seus2015.com 36 12-13: London, United Kindom The 6th International Workshop for Vaginal Fistula Repair and Female Urethral Reconstruction Contact: Pan Arab Continence Society Phone: +2010 5355353 Fax: +20 2 2455 3443 E-mail:[email protected] 16-18: Munich, Germany European Urology Today www.uroweb.org 28-30: Copenhagen, Denmark AUA Segura International Urolithiasis Course Contact: Depts of Urology and Medical Education at Hamad Medical Corporation Phone: +91 268 2520248 or +974 4439 1864 E-mail: [email protected] or [email protected] Website:auasegura.hamad.qa January 2015 Worldwide, continually updated urological meeting calendar at 20-27: Istanbul, Turkey 11th Pan Arab Continence Society Meeting in collaboration with International Continence Society Contact:PACS Fax: +2 24553443 E-mail:[email protected] Website:http://www.pacsoffice.com/PACS/ 26: London, United Kingdom Urological Anatomy for Surgery course Organiser:RCS Education E-mail:[email protected] Website:http://www.rcseng.ac.uk/courses March 2015 4-8: Vienna, Austria European Congress of Radiology (ECR2015) Contact: European Society of Radiology (ESR) Phone: +43 1 533 4064 0 Fax: +43 1 533 4064 448 E-mail:[email protected] Website:http://www.myesr.org/cms/website. php?id=/en/ecr_2015.htm 6-8: Sudan, Sudan The Third Academic Conference of SUA Contact: Sudanese Urological Association Website:www.sudaneseurology.net 20–24: Madrid, Spain 30th Anniversary EAU Congress Contact: Congress Consultants B.V. Phone: +31 26 389 1751 Fax: +31 26 389 1752 E-mail:[email protected] Website:www.eaumadrid2015.org 21-23: ESU Courses, HOTs, Education and Innovation at the time of the 30th Anniversary EAU Congress Contact:ESU 21-23: Madrid, Spain 16th International EAUN Meeting Contact: Congress Consultants B.V. Phone: +31 26 389 1751 Fax: +31 26 389 1752 E-mail:[email protected] Website:www.eaumadrid2015.org/eaun April 2015 11-14: Adelaide, Australia 68th Annual Scientific Meeting of the Urological Society of Australia and New Zealand (USANZ) Contact:USANZ Phone: +61 2 9362 8644 Fax: +61 2 9362 143 E-mail:[email protected] Website:www.usanz2015.com 18-21: Kanazawa, Japan 103rd Annual Meeting of the Japanese Urological Association Contact: Secretariat 102JUA Phone: +81 11 738 3503 Fax: +81 11 738 3504 E-mail:[email protected] Website:http://www.urol.or.jp/en/meeting.html 21-25: Acapulco, Mexico 39th Annual Meeting of CMU Contact:CMU Phone: +52 664 634 1138 E-mail:[email protected] 29-30: ESU organised course at the time of the EAU Baltic Meeting Contact:ESU 29 May–2 June: Chicago (IL), USA American Society of Clinical Oncology (ASCO) Annual meeting 2015 Contact:ASCO Phone: +1 571 483 1300 E-mail:[email protected] Website:www.asco.org/portal/site/ascov2 June 2015 10–11: Presov, Slovakia National congress of the Slovak Urological Association Contact: Assoc. Prof. Ivan Mincík (President of Slovak urological society) Phone: +421 51 7722756 Fax: +421 51 7722756 E-mail:[email protected] 11: ESU organised course at the time of the national congress of the Slovak Urological Association Contact:ESU 15–18: Manchester, United Kingdom Annual Meeting of The British Association of Urological Surgeons (BAUS) Contact:BAUS Phone: +44 20 7869 6950 E-mail:[email protected] Website:http://www.baus.org.uk 18–20: Kiev, Ukraine Congress of the Association of Urology of Ukraine Phone: +380 44 489 39 80 Fax: +380 44 254 00 40 or +380 44 486 65 69 E-mail:[email protected] 19: ESU organised course on Prostate cancer at the time of the national congress of the Ukrainian Urological Association Contact:ESU 24–26: Rome, Italy 2nd Edition Global Congress on Lower Urinary Tract Dysfunction Contact: Vita-Salute San Raffaele University Website:http://lutd.org/ 28-30: Paris, France 23–26: Antalya, Turkey 5th International Meeting “Challenges in Endourology & Functional Urology” (CIE 2015) Contact: Erasmus Conferences Tours & Travel S.A. Phone: +30 210 7414700 E-mail: [email protected] Website:www.challenges-endourology.com/ 11th National Turkish Endourology Congress Website:www.endouroloji2015.org 28–30: Ottawa, Canada 24–26: Beijing, China 4th International Forum on Frontiers in Urology (IFFU) Contact: Wu Jieping Medical Foundation E-mail:[email protected] May 2015 15–20: New Orleans (LA), USA Annual AUA Meeting 2015 Contact:AUA Phone: +1 410 689 3700 Fax: +1 410 689 3800 E-mail:[email protected] Website:www.auanet.org/eforms/planning/ index.cfm 20–22: Madrid, Spain 10th European Congress on Menopause and Andropause Contact: EMAS administrative office Phone: +49 30 24603-0 Fax: +49 30 24603 310 E-mail:[email protected] 29–30: Riga, Latvia 2nd EAU Baltic meeting Contact: EAU Regional Office Phone: +31 26 389 0680 Fax: +31 26 389 0674 E-mail:[email protected] 70th Annual meeting of the Canadian Urological Association Contact: Canadian Urological Association Phone: +1 514 392 7703 Fax: +1 514 227 5083 E-mail:[email protected] Website:www.cua.org/ 29 June–3 July: Lyon, France IUGA-ICS 2015 Contact: ICS Office Phone: +44 117 944 4881 Fax: +44 117 944 4882 E-mail:[email protected] Website:http://www.ics.org/2015 July 2015 5–11: Salzburg, Austria ESU – Weill Cornell Masterclass in General urology Contact:ESU Augustus 2015 19–23: Cartagena, Columbia Congreso Curso Internacional de Urologia Contact: Sociedad Colombiana de Urologia Phone: +571 218 67 00 / 57 310 322 12 10 Fax: +571 218 86 95 E-mail:[email protected] Website: www.scu-congreso.com/www.scu.org.co October/December 2014 Congress calendar 2014/2015 Worldwide, continually updated urological meeting calendar at www.uroweb.org 27–29: Zurich, Switzerland 11: Nijmegen, the Netherlands 5-9: Montreal, Canada 4th International Neuro-Urology Meeting Contact: Swiss Continence Foundation Phone: +41 44 386 3721 Fax: +41 44 386 3731 E-mail:[email protected] Website:www.swisscontinencefoundation.ch "Personalized Cure and Care in Urology - 50 Years Academic Urology in Nijmegen" Contact: Dept. of Urology, Radboud UMC Phone: +31 6 223 116 30 E-mail:[email protected] Annual Meeting of the International Continence Society (ICS) Contact: ICS Office Phone: +44 117 944 4881 Fax: +44 117 944 4882 E-mail:[email protected] Website:http://www.ics.org/2015 16-18: Bilbao, Spain September 2015 3-9: Prague, Czech Republic 13th European Urology Residents Education Programme (EUREP) Contact:ESU Phone: +31 26 389 0680 Fax: +31 26 389 0674 E-mail:[email protected] Website:www.eurep15.org 3-6: Shanghai, China Asian Urological Association meeting Contact: Angie See, Department of Urology Phone: +65 6 3214693 Fax: +65 6 2273787 E-mail:[email protected] [email protected] Website:http://uaanet.org/ 10-12: Alicante, Spain 3rd Meeting of the EAU Section of Urolithiasis (EULIS) Contact: Congress Consultants B.V. Phone: +31 26 389 1751 Fax: +31 26 389 1752 E-mail:[email protected] 12th Meeting of the EAU Robotic Urology Section (ERUS) Contact: Congress Consultants B.V. Phone: +31 26 389 1751 Fax: +31 26 389 1752 E-mail:[email protected] Website:www.erus15.org 23-26: Hamburg, Germany 67th Congress of the German Society of Urology (DGU) Contact:DGU Phone: +49 211 516 0960 Fax: +49 211 516 0960 E-mail:[email protected] Website:www.dgu.de/ October 2015 2-4: Budapest, Hungary EAU 15th Central European Meeting (CEM) Contact: Congress Consultants B.V. Phone: +31 26 389 1751 Fax: +31 26 389 1752 E-mail:[email protected] Website:www.cem15.org 15-18: Melbourne, Australia 23: ESU organised course at the time of the national congress of the Moldavian Urological Society Contact:ESU November 2015 2: Tashkent, Uzbekistan National Congress of the Scientific Society of Urologists of Uzbekistan E-mail:[email protected] 35th Congress of the Société Internationale d'Urologie (SIU) Contact: SIU Central Office Phone: +1 514 875 5665 Fax: +1 514 875 5665 E-mail:[email protected] Website:www.siu-urology.org/ 2: ESU organised course at the time of the national congress of the Scientific Society of Urologists of Uzbekistan Contact:ESU november 2015: 22-23: Chisinau, Moldavia 12-15: Barcelona, Spain National congress of the Moldavian Urological Society Contact: Prof. V. Ghicavîi Phone: +373 79469515 Fax: +373 22 733805 E-mail:[email protected] 7th European Multidisciplinary Meeting on Urological Cancers (EMUC) Contact: EAU, ESMO and ESTRO Phone: +31 26 389 0680 Fax: +31 26 389 0674 E-mail:[email protected] Website:www.emuc15.org For more elaborate information on all EAU meetings please contact Congress Consultants or consult the EAU website: Phone: +31 (0)26 389 1751 Fax: +31 (0)26 389 1752 E-mail:[email protected] Website:www.uroweb.org For more elaborate information on all ESU courses please contact the European School of Urology or consult the EAU website: Phone: +31 (0)26 389 0680 Fax: +31 (0)26 389 0684 E-mail:[email protected] Website:www.uroweb.org ERUS2014: Robotic Urology draws big crowd to Amsterdam Three-day meeting included programme for nurses, young robotic urologists By Loek Keizer The YAU - Junior ERUS Programme All-day, state-of-the-art live surgery might have been an important attraction, but it’s certainly not the only important development that drew over 700 delegates to central Amsterdam for three days. Educational courses, expert lectures, hands-on training and new developments in certification of the field were important topics for the urologists, nurses and residents that attended the 11th EAU Robotic Urology Section Meeting on 17-19 September. ERUS14 featured a special programme for young urologists and others interested in getting involved in robotic surgery. Important topics include the economics of robotic surgery, a look at the literature, and the importance of a viable certification programme. Dr. Carl Wijburg (Arnhem, NL), Session co-chairman: We spoke to Dr. Henk Van Der Poel (Amsterdam, NL), Chairman of the local organising committee, about the scope of the meeting, choices behind the scientific programme and the specifics of robotic urology. “This marks the first year that the ERUS meeting is completely organised by the EAU. We’ve seen around 700 registrations, which is extremely encouraging. In terms of what we have to offer, my personal interest is training.” ERUS14 offered several daily sessions of hands-on training for novice surgeons and those who wanted to familiarise themselves with the basics of robotic surgery. In addition, there was an extensive “YAU-Jr. ERUS” programme for the beginning robotic urologist. Dr. Van Der Poel demonstrating the wide range of optical technologies available for robotic surgeons Nationwide live surgery Instead of being confined to Amsterdam, Dr. Van Der Poel was pleased to highlight the national level of cooperation that made the live surgery aspect of the Robotic training congress possible. While all delegates were gathered “We’re making strides towards certification for in the Beurs van Berlage in the Dutch capital, the robotic surgery. In the Netherlands, people drove cars actual surgery took place in the Maasstad Hospital in for thirty years before the concept of a “driver’s Rotterdam. The distance of 70 km between the two license” based on testing was introduced in the 1920s. locations was a new distance record for live Of course we don’t want a repeat of that in robotic transmission at an ERUS meeting. “This is truly a surgery. We’re developing a certification process and nationwide effort, involving patients from all across the results of the second, six-month pilot were the country being referred to Rotterdam to make this presented at ERUS14. We’re also gaining a lot of data possible. It’s a testament to the efforts of Dr. Sjoerd and insights from the hands-on training and Klaver and his team that all national and EU-protocols simulation programmes that we have. Steps during a were followed to the letter, as well as the EAU’s own surgical procedure are now analysed individually, Policy on Live Surgery.” helping pinpoint where improvement of the individual surgeon is needed.” More and more urological events are following the EAU’s policy, which puts patient concerns first. “The “Rather than wait for laws to come into practice, we EAU can be commended for facing up to concerns are already gaining insights so that we can advise about live surgery. Session chairs are required to cut-off points for robotic competence. The EAU helps interrupt the two-way broadcast if he or she feels the by supporting this scientific side of the debate: surgeon is distracted. There is also an independent publications, gathering data and strengthening our doctor, a patient advocate closely monitoring case in that regard.” proceedings to ensure that the patient is getting the best possible care.” October/December 2014 While live surgery is an important draw, Dr. Van Der Poel emphasises that presentations based on pre-recorded footage are valuable as well. “It can be an advantage to pause the footage, and to know how the procedure ends. At the next ERUS meeting, we will present the follow-up for the patients operated in Rotterdam, but with pre-recorded cases, we of course already have this information.” Optics in robotic surgery Having performed a sentinel lymph node and extended radical prostatectomy the afternoon before, Dr. Van Der Poel explains the unusual colours that the audience was treated to during the procedure. “We used both Storz FI near-infrared and Intuitive Firefly to highlight different optical techniques that are available to surgeons. We use tracers that do not show up in natural white light, preserving the normal view for the surgeon. By using special wavelengths of light, we can reveal much more information than is available to the naked eye.” During the procedure, which involved fluorescent and radiological tracer injection into the prostate to reveal the nodes, the audience followed along, with different filters and views showing different parts of the “The programme was especially geared to young urologists who are interested in starting with robotic surgery, so we try to keep it approachable.” Dr. Wijburg also spoke at the session, looking at the total costs and benefits for institutions who are considering the purchase of a surgical robot. One big advantage of the robot is that patients spend less time recuperating and have a shorter hospital stay. The high purchase price of the robot can already be recouped within several years. “Besides costs, we are more interested in the quality of care, so we also had an excellent session that looked at the best articles about outcomes of robotic surgery. What can we say about complications and the learning curve? We need standardised reports of complications to compare outcomes. The learning curve is probably never ending, because robotic urology is a fast-evolving field.” anatomy. “There aren’t any standards yet, using different tracers will allow tissue labelling in the future. I would expect that in ten years’ time, everyone will have implemented imaging modalities that provide detailed information on tissue properties e.g. cancer location. What we demonstrated yesterday was truly cutting-edge but only the beginning of image guided surgery.” For more information about the Nurses’ Programme at ERUS14, please turn to page 38. For a complete impression of ERUS14, including photo albums, interviews and abstracts, please visit erus2014. uroweb.org European Urology Today 37 Nurses’ Programme at EAU Robotics Section Meeting Shifting roles for nurses and the importance of certification By Loek Keizer the nurses did take the initiative as well. When ERUS was founded, there was a simultaneous desire to Uniquely for a Section Meeting, the ERUS Meeting in involve nurses in the emerging field of robotic Amsterdam featured a full-day programme for nurses urology. The whole team, from surgeons to nurses, involved or interested in robotic surgery. With ERUS should be certified and trained for robotic urology.” coming under the wings of the EAU, the EAUN is now cooperating with the ERUS nurses' group. Special De Blok on the roles of nurses in the OR: “There are topics were covered, with opportunities for some international differences, which become knowledge exchange and hands-on training. apparent at meetings like this. In some countries, the nurse is a surgeon’s first assistant whereas in others Mr. Willem De Blok, clinical nurse specialist in one urologist is required to assist another. Amsterdam and local organiser for the EAUN Programme in Amsterdam on September 17th spoke “In some countries nurses or OR assistants have a to us looking back on the successful day. The EAU larger role to play, taking care of routine procedures Robotic Urology Section Meeting is the only so that the surgeon can focus on patients that do specialised meeting with its own nurses programme: require specialist care. In the UK, there is a similar “I think ERUS can be commended for this, although division of labour although it’s not formally arranged this way like in the United States or Canada, which pioneered the concept of the nurse practitioner.” European Association of Urology Nurses The day’s programme ended with a frank discussion with a patient who suffered some complications after Apply for your EAUN membership online! Would you like to receive all the benefits of EAUN membership, but have no time for tedious paperwork? Becoming a member is now fast and easy! www.eaun.uroweb.org Nurses Söderkvist and Rundin from Stockholm speak on their hospital’s experiences with performing five prostatectomies in a single day The day’s programme attracted 76 nurses (including faculty) and offered lectures and workshops on a variety of topics including cost-efficiency throughout robotic procedures, a case of five prostatectomies in one day, and state-of-the-art overview lectures from urologists. Break-out sessions allowed ward and OR nurses to attend a special scientific programme, as well as an opportunity for hands-on training. “The hands-on training was popular and well-received. We would have dearly liked to have given more nurses the opportunity to take part in hands-on training, but we were limited by the number of machines available.” Go to www.eaun.uroweb.org and click EAUN membership to apply online. It will only take you a couple of minutes to submit your application, the rest - is for you to enjoy! relationship as a result of the procedure. As nurses, we of course deal with the patient on a different level from the surgeons. It’s important that we keep this human element in mind at meetings like these.” EAUN Board The nurses' day at ERUS attracted nurses from 10 European countries, South Korea and the USA a robotic prostatectomy. Involving a patient gave the attending nurses a good indication of how a patient experiences the whole procedure, and also allowed them to ask questions that one would not necessarily ask one’s own patients as they are treated. De Blok: “The patient was very open to talk about issues like incontinence and impotence, including the end of his Chair Chair Elect Past Chair Board member Board member Board member Board member Board member Board member Lawrence DrudgeCoates (UK) Stefano Terzoni (IT) Kate Fitzpatrick (IE) Paula Allchorne (UK) Simon Borg (MT) Willem De Blok (NL) Erica Grainger (DK) Susanne Vahr (DK) Giulia Villa (IT) www.eaun.uroweb.org Urinary Tract Infections 1st Course of the European School of Urology Nursing (ESUN) 8-9 May 2015, Amsterdam, the Netherlands Includes risk factors for UTI, treatment and prevention, health care worker and patient education and development of a prevention plan for your own clinic 9 modules – expert faculty – concluded with test Full programme and application form can be requested at [email protected] Registration fee 100€ (flight and 1 hotel night are covered by EAUN) Application deadline: 20 December 2014 Supported with an educational grant from Wellspect Fellowship Programme European Association of Urology Nurses European Association of Urology European Nurses Association of Urology Nurses Call for Papers The International Journal of Urological Nursing - The Official Journal of the BAUN The International Journal of Urological Nursing is clinically focused and evidence-based and welcomes contributions in the following clinical and nonclinical areas: • General urology • Clinical audit • Continence care • Clinical governance • Oncology • Nurse-led services • Andrology • Reflective analysis • Stoma care • Education • Paediatric urology • Management • Men’s health • Research There are many benefits to publishing in IJUN, including: • Broad readership of papers—all published papers will be available in print and online to institutional subscribers and all members of the British Association of Urological Nurses • Fast and convenient online submission— articles can be submitted online at http://mc.manuscriptcentral.com/ijun 38 European Urology Today Visit a hospital abroad! 1 or 2 weeks - expenses paid • Fast turnaround—papers will be reviewed and published quickly and efficiently by the editorial team • Quality feedback from Reviewers and Editors—double-blind peer review process with detailed feedback • Citation tracking—authors can request an alert whenever their article is cited • Listed by the Science Citation Index Expanded™ (Thomson ISI) For further information and a free sample copy go to: www.wileyonlinelibrary.com/journal/ijun Application deadline: 31 January 2015 • Only EAUN members can apply, limited places available • Host hospitals in Belgium, Denmark, the Netherlands, Sweden, Switzerland and the United Kingdom • A great way of widening your horizon For Fellowship application forms, rules and regulations and information on which specialities the hosting hospitals can offer please visit the EAUN website. T +31 (0)26 389 0680 F +31 (0)26 389 0674 [email protected] www.eaun.uroweb.org European Association of Urology Nurses October/December 2014 EAUN joins Chinese Urology Association meeting Education strengthens collaborative work on urological nursing care Lawrence DrudgeCoates Clinical Nurse Specialist, Urooncology EAUN Chair London (UK) l.drudge-coates@ eaun.org My visit to China on invitation by the Chinese Urology Association's Nursing Committee, started in Wuhan, capital of Hubei province and the most populous city (population at 10 million) in Central China. Wuhan lies in the eastern Jianghan Plain where the Yangtze and Han Rivers meet. Accompanied by Mr. Larry Tsang and Gilbert Lui, Nursing committee members of the Chinese Urology Association, who were instrumental in organising this visit, I met with Ms. HE Wei, chair of the Nursing Committee and Prof. YE Zhang Qun, immediate past president of the Chinese Urological Association (CUA). Their department, at the Hospital of Tongji Medical College of Huazhong University of Science and Technology, is an extremely busy unit where around 10,000 urology outpatients are attended to every week. urology nursing care, areas for educational collaboration and EAUN membership. Such discussions proved to be both highly informative and productive. CUA meeting It was truly an honour to be the first foreign urology nurse to attend the CUA Annual Meeting, and my visit was met with both intrigue and delight as I was introduced to CUA members I also renewed old acquaintances from Hong Kong and again met Prof G. Zhou, urology professor of the Beijing Hospital of Ministry of Health, who had completed his PhD work at my institution some 12 years ago. As head of international relations for the CUA, he interviewed me regarding my visit, which provided an opportunity to highlight the work of the EAUN and the benefit of collaboration with CUA nurses. presentations focusing on the growing role of rehabilitation, its impact on traditional postoperative care, improvements being made in the patient's postoperative recovery rate and shortened hospital stay. This was something all too familiar in my own clinical practice, but nevertheless not with the same population base. The visit to China very much highlighted the need and benefit for collaboration across different urology nursing organisations and the ensuing challenges. The EAUN’s mission is not only to support and encourage the development of urology nursing within Europe, but also to collaborate with national societies across the globe in support of the development and application of high-quality urology nursing practices. This particular issue was evident in discussions regarding EAUN clinical guidelines-- with translation and modification to fit local practices- which will Ms Xiong Wenting presenting a paper on Clean intermittent catheterisation and bladder puncture gastrostomy in females with neurogenic bladder prove to be a very successful initiative. I therefore look forward to our continued collaboration. My thanks to the CUA committee for its hospitality and very warm welcome. 21st CUA conference, Jinan The nursing component of the meeting was held in the Shandong Hall. After a few words of Mandarin (which I practised many times!), I presented an overview of the EAUN, including its key clinical guideline developments, e-learning education and membership benefits, all of which were positively received. With translators, language did not prove to be of any hindrance as we discussed common issues we faced in Colleagues from Hong Kong inc Chinese Urology Nursing Committee members. From left: Ms Lo Yi Mei, Ms Yang Jiahui, Mr Larry Tsang, Mr Gilbert Lui , Ms Sophie Come European Association of Urology Nurses Being all too familiar with the EAUN abstract presentations, it was a real insight for me to hear some of the work being carried out by urology nurses in China, which was not different from our own. The meeting received 738 nursing papers for consideration which covered key aspects of urological clinical care, nursing education, scientific management and innovative research. Only 29 of the 738 were presented at the meeting due to practical considerations of hosting this event. There were Members of the CUA nursing committee – Ms HE Wei- Nursing Chair (in blue) 15th Asia-Pacific Prostate Cancer Conference Meeting presents salient nursing issues in prostate cancer Tanja Rogers, RN Counties Manukau Health Urology Dept. Auckland (NZ) Tanja.Rogers@ cmdhb.org.nz I attended the 15th Asia-Pacific Prostate Cancer Conference 2014 held in Melbourne, Australia from 31 August to 2 September together with around 600 other delegates from around the globe. The conference is renowned for a comprehensive and stimulating programme that covers clinical urology, translational science and nursing and other allied areas. The nursing and allied health section included many presentations with topics such as: continence, active surveillance, hormone therapy, advanced prostate cancer and current nursing and allied health research trends. The following is a summary of key points from three of the sessions I attended. leakage post-operatively and return earlier to normal life. She added that one of the main benefits of teaching PFE pre-operatively is that it is easier to teach motor control to men who don’t have pain. The pre-operative PFE education session also provides an opportunity for health professionals to cover information that helps establish realistic postoperative goals and expectations. Assessment during this phase also allows for identification of any pre-existing voiding patterns that may require investigation prior to surgery such as detrusor overactivity. Neumann also said that teaching PFE needs to be personalised to suit each individual since not everyone learns the same way. She believes that the best way to deliver PFE education is to use a combination of written and verbal information, as well as pelvic anatomy models and pictures. Transperineal ultrasound and digital rectal Dr. Trish Neumann, specialist continence and pelvic floor physiotherapist, presented a session entitled ‘Teaching pelvic floor exercises (PFE) to men before prostate surgery- what is best practice?' According to Neumann, post-operative PFE training isn’t effective and that men who are taught PFE prior to prostate surgery have an earlier return of bladder control, less European Association of Urology Nurses October/December 2014 Melbourne was hosting the 15th Asia-Pacific Prostate Cancer Conference examination can also be used to assess how well men are contracting their pelvic floor muscles. Mr. Jeremy Grummet, a urological surgeon specialised in urological cancers, gave an overview of transperineal (TP) and transrectal ultrasound (TRUS) guided prostate biopsy techniques focussing on the implications for the patients undergoing the procedures. Grummet said approximately 50% of TRUS biopsies are negative for cancer since either the cancer has been missed by the biopsy sampling process or because there was no cancer present in the opined that TP biopsy should be offered as an option prostate gland. He reported that the TRUS biopsy to all patients in whom a prostate biopsy is indicated. procedure causes pain and carries a significant risk of post-procedure infection. Prof. Daniel Galvao presented a session entitled ‘Active surveillance for prostate cancer- potential application of exercise medicine’. Galvao has been "...participants undergoing involved with numerous trials of the potential benefit of exercise in men with prostate cancer. He said that supervised exercise had a more participants undergoing supervised exercise had a positive outlook and a stronger more positive outlook and a stronger sense of social belonging. They also had fewer symptoms of sense of social belonging." depression and fatigue and an improvement in their quality of life measures. He also underscored the According to Grummet, one way to address the risks importance of the role of nurses in educating patients on how to increase their quality of life. He added that of TRUS biopsy is to be smarter in the way we use PSA testing, ensuring it is used in men most likely to there is a wealth of evidence showing that exercise is benefit from an early diagnosis of prostate cancer. He safe and well tolerated by prostate cancer patients on also recommended that men should have an MRI scan active surveillance. prior to TRUS biopsy to enable a targeted biopsy, thus decreasing the detection of insignificant low-risk Overall, I found the conference very interesting with content that motivates me to pursue ideas that can cancers. Grummet advocated TP biopsy as a method of decreasing infection risk and avoiding the use of lead to improved care of prostate cancer patients. The broad spectrum prophylactic antibiotics. TP biopsy next conference in the series is the Prostate Cancer also enables targeted biopsies and reduces the World Congress in Cairns, Australia from August 18 to discomfort associated with prostate biopsy since it is 21, 2015. I hope you can join us for another dynamic meeting! performed under general anaesthetic. Grummet European Urology Today 39 What to expect at the EAUN 2015 Annual Meeting Madrid programme will feature new topics, current issues and trends Stefano Terzoni Chair EAUN Scientific Congress Office Milan (IT) Other items in the programme aim to provide practical and useful information which can be useful in our everyday clinical practice, including topics such as practical management of urological emergencies, urological care for people with learning disabilities, ongoing challenges in male sexuality, intravesical instillation and BCG treatments, 3Tesla magnetic resonance, and many others. [email protected] Workshops and panel discussions Several workshops will be offered, including a session on perioperative care in prostate disease, updates on pelvic floor rehabilitation, an ESU course on female sexual assessment and rehabilitation (in collaboration with the European School of Urology), success factors in self-dilatation, UTI in clean intermittent catheterisation, troubleshooting in patients with indwelling catheters, psychological aspects of living with cancer, and care pathways in bladder cancer treatment. More than 300 delegates from 27 countries attended the 15th EAUN Meeting held in Stockholm last April, which attracted this year outstanding contributions by lecturers from all over Europe. The meeting in 2015, to be held in Madrid from March 20 to 24, promises to be even more interesting: the EAUN scientific committee and the board took into consideration the suggestions provided by the delegates in Stockholm. The most appreciated sessions will also be in next year’s programme plus new topics and current issues. The programme, available on the website www. eaunmadrid2015.uroweb.org, begins with a plenary session regarding the future of urological nursing and the need for a common framework. Currently, there is an important European debate regarding the definition (and therefore the future) of urological nursing. In two years, the European Union is expected to make a stand on this issue, and this will have an impact on education, mobility, and working possibilities for urological nurses across Europe. Thus, the opening session of the EAUN meeting will focus on this important topic, with lectures on the various aspects followed by a panel discussion. We invite you to join the discussion, as this will have repercussions on our daily practice. European Association of Urology Nurses A new EAUN guideline on intravesical instillation, developed by the EAUN guidelines panel, will be presented. The Marketplace Session, already a well-known and appreciated session in past meetings, will allow participants to discuss adapted physical activity, sexual and urological rehabilitation, and ERAS (Enhanced Recovery After Surgery) with internationally renowned experts. As in the previous editions, two poster sessions have been included in the programme. The number of abstracts submitted over the years has been increasing, and many important topics have been addressed by high quality posters. Everyone eligible for EAUN membership has the opportunity to submit their abstract before December 1st via the congress website. A video session called “Surgery in Motion,” first introduced in Milan and greatly appreciated by the delegates, will be included in the Madrid programme. Original videos, produced in the operating theatre, will show and comment on unusual surgical Panel discussion on the European perspective of urology nursing at the EAUN Meeting in Stockholm last April situations. Additional expert commentary on these procedures will be shared with the audience to provide practical information. Deadline for submitting, by email, your research proposal is December 1 (further details on the website). The classic Nursing Difficult Case Solution session entitles free registration for authors of the most interesting nursing cases. These selected authors will also present their work during the meeting. We encourage submissions of original cases by e-mail (details on the website) before December 1. Those who submit a case and are not yet EAUN members will be granted free membership for 12 months. The 16th EAUN Meeting in Madrid will serve as an excellent opportunity to share expertise and for both EAUN members and non-members to be directly involved in improving urological nursing and play an active role in discussing current issues. Nursing cases, posters and research projects are welcome, and would contribute greatly in an active exchange of knowledge and information. Finally, if you have a planned research project, the EAUN Research Competition is open with a €2,500 prize to be awarded to the most significant research project, enabling authors to receive support and funding. The author’s proposed research will be presented in summary form on the EAUN website. We look forward to receiving your ideas and suggestions for discussion topics. For additional information, visit our website or contact eaun@ uroweb.org in case of queries. 16th International Register now for the early bird fee! EAUN Meeting Deadline 12 January 2015 21-23 March 2015, Madrid, Spain Preliminary Programme Saturday, 21 March 2015 Sunday, 22 March 2015 Monday, 23 March 2015 09.00 – 10.00 Workshop Intravesical instillation in NMIBC 09.00 – 10.00 Workshop Difficult case session 09.00 – 10.00 Workshop Pelvic floor rehabilitation for LUTS: What’s new? 10.15 – 10.45 State-of-the-art lecture PSA, is it a Patient Stress Amplifier? 09.00 – 10.15 Opening Plenary Session The future of urological nursing The need for a common framework: time is running out Inside the body - surgery in motion (videos) 10.15 – 10.45 State-of-the-art lecture BCG treatments for superficial bladder cancer 10.30 – 11.15 Workshop Nursing challenges in urodynamics 10.15 – 11.15 10.45 – 11.15 10.30 – 11.15 Workshop Contemporary issues in patient pathways and cancer treatment Workshop Troubleshooting and quality of live in indwelling catheterisation State-of-the-art lecture 3Tesla Magnetic Resonance Imaging for PCa 10.45 – 11.15 10.15 – 12.45 Workshop Ongoing challenges in health and sexuality in male patients State-of-the-art lecture Not only instillation: BCG perfusion for kidney and urethra EAUN-ESU Course - 2 Female sexual assessment and rehabilitation 11.30 – 12.15 Workshop Care pathway and rehabilitation in bladder cancer surgery 13.15 – 13.45 EAUN General Assembly 09.00 – 10.15 11.30 – 12.30 11.30 – 12.30 Nursing Research Competition 12.45 – 13.45 EAUN-EORNA Workshop Diagnosis and peri-operative care in prostate disease 14.00 – 14.30 State-of-the-art lecture Best practice principles in the urological care for people who have a learning disability 14.00 – 15.15 Poster Abstract Session 14.45 – 17.00 EAUN-ESU Course - 1 Practical management of urological emergencies 11.30 – 13.15 Poster Abstract Session 12.15 – 13.15 Workshop Living with prostate cancer: Daily issues and quality of life 14.45 – 16.45 Market Place Session Rehabilitation in urology cancer care 14.45 – 15.45 Workshop UTI in clean intermittent catheterisation: What’s new? 16.00 – 17.00 Workshop Clean intermittent catheterisation and self dilatation: quality of life and success factors 13.45 – 14.00 EAUN Award Session Supported with an educational grant from AMGEN Scientific Committee: Stefano Terzoni (IT), Chair Bente Thoft Jensen (DK) Jerome Marley (GB) Lisette Van De Bilt (NL) Rita Willener (CH) For more information: [email protected] #EAUN15 www.eaumadrid2015.org/eaun 40 European Urology Today See you in Madrid! in conjunction with October/December 2014
© Copyright 2026