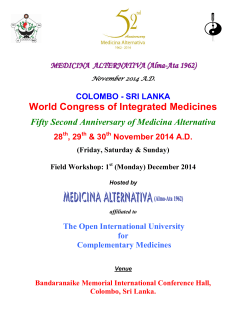
Medico Legal Journal of Sri Lanka
Original article Prevalence and features of triticea cartilage in an autopsy sample of tertiary care hospital in Sri Lanka Senanayake S.M.H.M.K. Teaching hospital Anuradhapura *Corresponding author: Tel: 0094-71-8195569 E-mail address:[email protected] MLJSL. Vol 2. No 2. Dec. pp 1-4 Abstract Introduction Triticea cartilage is a grain like cartilage situated just above the tips of the superior thyroid horns. Inexperienced medical officers could mistake this incidental finding for a fracture and thereby an evidence of pressure on the neck. Objective This study was designed to find the prevalence of the Triticea cartilage in an autopsy sample in the Kurunegala District of Sri Lanka and if present to ascertain its size and shape. Methodology All autopsies performed by the author during the last four months of the year 2011 were included in to this research. Results The sample studied included 182 males and 67 females (n=249). In males triticea cartilage was present in 101 (55.5 %) cases, of which cartilages were present bilaterally in 76 (41.2%).Unilateral cartilage on the left side was found in 12 (6.5%) of the males and on the right side in13(7.1%) cases. Site was just above the tip of the thyroid cartilage in 94 (93%) cases. Spherical shape of the cartilage was observed in 80(79.3%) and elongated shape in 21(20.7%) cases. Triticea cartilage was present in 24(35.8%) of females of which cartilages were present bilaterally in14(20.8%). Unilateral cartilage on the left side was found in 7(10.5%) of the females and on the right side in3(4.5%). Commonest site was just above the tip of thyroid cartilage in 23 (95.8%) cases. Spherical shape in 21(87.5%) cases and 3 (12.5%) cases cartilage was elongated. Conclusion This study showed that 50.2% (half) of the autopsy population has the triticea cartilage. 36.1% (One third) of population has it on both sides. More than three quarter (80.8%) of triticea cartilages are spherical in shape. 92.8% of triticea cartilages were found just above the tip of superior thyroid horn. Key words: Triticea cartilage, autopsy sample, presence, prevalence, above the tip of thyroid cartilage, 1 Introduction Triticea cartilage[1](triticea cartilago),tritiate cartilage[2] or triticious cartilage [3] is a grain like cartilage situated just above the tips of the superior horns of thyroid cartilage [1]. “Tritiate” is a Latin word the meaning of which is grain. Inexperienced medical officers could mistake this incidental finding for a fracture of the thyroid cartilage and conclude that there was evidence of pressure on the neck [4]. Another importance of this cartilage is that fracture of a thyroid horn could be misrecognized as a triticea cartilage. One common postmortem artifact which gained worldwide attention was laryngeal fracture occurring due to handling during the autopsy [5,6]. It is possible that much attention was not drawn to the triticea cartilage due to its scarcity in developed countries. Literature survey showed only a few publications about this cartilage and a few more articles just mentioned this name when dealing with the thyroid cartilage. Even though anatomy text books devote a few sentences to this cartilage, many forensic text books [7, 8] do not even mention it. Anatomically it was considered unimportant earlier but now it is accepted as being relevant for strengthening of the thyrohyoid ligament. In the practice of radiology it is important to separate calcified triticea cartilage from a calcified carotid atheroma and soft tissue calcifications [3]. This cartilage has been a frequent finding for the author in the autopsies done in Sri Lanka and was the reason that prompted this research. Objective This study was designed to find the prevalence of the triticea cartilage in autopsies performed in the Kurunegala Teaching Hospital and if present to ascertain its site and shape. Methodology during the last four months of the year 2011 were included in to this research. Upper margin of thyroid cartilage is connected by the thyrohyoid membrane to the lower border of the hyoid bone. The thyrohyoid membrane is limited posteriorly by the thyrohyoid ligament. When this ligament is palpated, a grain like nodule is felt somewhere between the tip of the superior thyroid horn and hyoid bone. When soft tissues are dissected away, triticea cartilage is found in the ligament. Rounded and smooth ends help to separate it from a fracture of the thyroid horn because fracture surfaces are flat and irregular [9]. Shape of the cartilage was studied, length was measured and distance between the tip of thyroid horn and triticea cartilage was measured. Results Prevalence Out of the 182 males Triticea cartilage was present in 101 (55.5 %) cases. (Table no. 01). Out of these 101 cases, cartilages were present bilaterally in 76 (41.2%) cases (Table no.02). Unilateral cartilage on the left side was found in 12(6.5%) cases and on the right side in 13(7.1%) cases. In females Triticea cartilage was absent in 43 (64.2%) cases. Cartilages were present bilaterally in 14(20.8%) cases. Unilateral cartilage on left side was found in 7 (10.5%) cases and on the right side in 3(4.5%) cases. Table no. 01. Prevalence of cartilage Presence of the cartilage Male Female Total P value Present Absent Total 101 81 182 24 43 67 125 124 249 0.005 All 249 postmortem examinations (182 males and 67 females) performed by the author 2 Table no. 02.Presence of bilateral and unilateral cartilages-in males and females Presence of Male Female P bilateral cartilage value Bilateral cartilage 76 present 14 Unilateral cartilage 10 25 0.103 Site In males, the commonest site was just above the tip of the superior horn of the thyroid cartilage(thyroid horn) in 93(92%) cases. In 4 cases it was found 0.25cm above, in 2 cases 0.5cmabove and in 2 cases 1cmabove the tip of the thyroid horn. In females, commonest site was just above the tip of thyroid horn in 23 (95.8%) cases. In the remaining case cartilage was found 0.5cm above the tip of thyroid cartilage. Shape Spherical shape was seen in 80 (79.3%) males and elongated in 21 (20.7%)males. Spherical shape was found in21 (87.5%) females and elongated in 3 (12.5%) females. Size Length of the cartilage was variable and measured between 0.25 to one centimeter. Width was equal to the width of its thyroid horn. Discussion This study indicates that 50.2 % of the study population has the triticea cartilage. 36.1% (slightly more than one third) of the study population has it on both sides. Presence of this cartilage in males is statistically significantly higher than in females. (P value = 0.005). Presence of bilateral cartilage is statistically significantly higher in males than females. (P value = 0.103). In more than three quarter of the subjects(80.8%), the cartilage was spherical in shape. In 92.8% cases it was found just above the tip of the thyroid horn. The size was variable. The length was between 0.25 cm to one centimeter and the width was equal to the width of the thyroid horn. Since half the population possess this cartilage, careful neck dissection will reveal it. It is therefore medico legally important to recognize this cartilage and separate it from a fracture of thyroid horn. More than 90% of the cases it was found just above the tip of the thyroid horn and can be easily mistaken for a fracture of tip of the thyroid horn. In the remaining cases due to the larger gap it is unlikely to be mistaken for a fracture. One third of the population has it only on one side. When there is a suspicion about neck trauma and if fracture of thyroid horn is found on one side, triticea cartilage on other side may give the misleading impression of bilateral thyroid fractures. A spherically shaped triticea cartilage can give a false impression of a fracture of the tip of the thyroid horn. An elongated cartilage can give the impression of a fracture of the middle of the thyroid horn. Because of the rounded shape of its lower end, the cartilage can be easily distinguished from a fracture. X ray examination of the larynx will be useful to separate the cartilage from a thyroid fracture, but practically it is not required. A study done on laryngeal cartilages for age changes has not shown any value of calcification of triticea cartilage [10] for assessment of age. On calcification, the triticea cartilage might fuse with the tip of the thyroid horn and give a false impression of an old thyroid fracture [11]. This cartilage is known as a variable cartilage because of embryological developmental variations [12]. This study determined the prevalence, sites, size and 3 shape of Triticea cartilage indicating its importance as one common postmortem artifact found during neck dissections in Sri Lanka. 4. 5. Conclusions This study showed that 50.2% (half) of the autopsy population has the triticea cartilage and in 92.8% the cartilage was found just above the tip of superior thyroid horn. More than one third of the population has it on both sides and more than a three quarter (80.8%) of the Triticea cartilage were spherical in shape. Because half of the population possess this Triticea cartilage just above the tip of superior thyroid horn, it is a very important, common artifact of neck dissection in Sri Lanka. Awareness of the presence of Triticea cartilage as well as its smooth and rounded upper and lower ends will prevent medical officers from misrecognizing it as a fracture of the tip of the superior horn of the thyroid cartilage. 6. 7. 8. 9. 10. 11. References 1. Anderson JE. Grant’s Atlas of Anatomy. Williams & Wilkins 1978; 7th edition.pp-965 2. StandringS.Gray’s Anatomy. Elsevier th Churchill Livingston; 39 edi.2005 pp-63435 3. Mansur Ahmad et al. Triticeous cartilage: prevalence on panoramic radiographs and 12. diagnostic criteria. Oral Surg Oral Med pathol Oral radiol Endod. 2005;99:225-30. Vanezis P. Pathology of neck injuries. Butterworth. First edition. 1989 p-7 Dunsby AM, Davison AM. Causes of laryngeal cartilage and hyoid bone fractures at postmortem. Med Sci Law. 2011 Apr;51(2):109-13 Draven KP, Reay DT, Harruff RC. Artifactual injuries of the larynx produced by resuscitative intubation. Am J Forensic Med Pathol. 1999 Mar ;20(1) 31-6 Knight B. Forensic pathology. Edward Arnold 1991. 1st edition. pp340-345 Mason JK, Purdue BN. The pathology of trauma. Arnold London.3rd edition.pp241247 Charoonnate N, Narongchai P, Vongvaivet S. Fractures of hyoid and thyroid cartilages in suicidal hanging. J Med Assoc Thai. 2010 Oct:93 (10)1211-6 Munir Turk L, Hogg DA. Age changes in human laryngeal cartilage. Clinical Anatomy. 1993: 6(3) 154-162 Maxeiner H. Healed fractures of the larynx and lingual bone in forensic autopsy. Arch Kriminol. 1999 May-June:203 (5-6): 175-83 Grossman JW. Triticeous cartilage. The American Journal of Roentgenology & Radiotheraphy. Vol L111 no 2 Feb1945. pp 166–170 4 Original article Trends of suicides in Galle-Sri Lanka Rathnaweera RHAI1 Department of Forensic Medicine, Faculty of Medicine, Karapitiya, Galle, Sri Lanka *Corresponding author: Tel: 0094-772969060. E-mail address:[email protected] MLJSL.Vol 2. No 2. Dec. pp 5-10 Abstract Introduction Suicide is considered as a complex event that has biological, psychological and social implications. For many years now Sri Lanka has been among the countries where suicide and attempted suicide have been frequent. Objective To document epidemiological and socio-economic data on suicides reported to the Teaching hospital, Karapitiya in the year 2011 and to compare with the findings of previous studies done in other parts of the country. Materials and Methods All suicidal deaths reported to Teaching hospital, Karapitiya from 1st of January 2011 to 31st of December 2011 were studied retrospectively. Results During the study period, 110 deaths due to suicide were documented and analyzed - 86 males (78%) and 24 females (22%). A significant proportion (22%) was in the 21-30 and (22%) in the 41-50 year age groups. Sixty males (70%) were alcohol addicts. A suicidal note was found at the scene in 17% of cases. The majority (85%) of the families had a monthly income of less than $100US. Commonest method used by males was hanging (60%), and by female was plant poisoning (30%).The commonest reason for suicide was debt (35%) and dispute with the spouse/marital disharmony (31%). Of the 12 adolescent deaths 9 had been due to scolding by parents. Conclusions Majority were young married males belonging to lower socio-economic group. A significant number of teenagers were found to commit suicide following minor disappointments. The method of choice for suicide was hanging among males and plant poisoning among females. Among males, alcohol addiction remains a major contributory factor for committing suicide. Key words: Suicide methods, Hanging, plant poisoning, debt 5 Introduction Suicide is considered as a complex event that has biological, psychological and social implications [1]. Historically, suicide has been approached as a personal pathology or a sinful act rather than as a social, structural or genderized phenomenon [2]. The first sociologist who systematically studied suicide as a social occurrence was Durkheim (1951) who claimed that suicide was a social problem rather than an individual illness [3]. Durkheim’s exclusive interest was why men killed themselves. Ironically, women have the “highest suicidal behavior” even though more men die as a result of a suicidal act [4]. Since Durkheim, although sociological research on suicide has declined, most research continue to focus on the behaviour of men. The World Health organization (WHO) estimates that every year, nearly one million people kill themselves [5]. Suicide has become one of the top 20 causes of death in the world over for all ages [5]. For many years now Sri Lanka has been among the countries where suicide and attempted suicide have been frequent frequent. According to Sri Lanka Sumithrayo organization, an organization set up to help prevent suicide in Sri Lanka, the rate of suicide has reduced from 47/100,000 of the population in 1995 (highest suicidal death rate in the world) to 20/100,000 in 2008 [6]. According to the literature, reasons offered to explain the higher rate of suicide in Sri Lanka include spouse/marital disharmony, financial matters, psychiatric disorders, alcohol dependence, unemployment, broken love affairs, and problems at work [1,2]. Objective hospital, Karapitiya in the year 2011 and to compare with the findings of previous studies done in other parts of the country. Materials and Methods All deaths where a verdict of ‘suicide’ was issued at the inquest following a post-mortem examination at the Teaching hospital Karapitiya, were retrospectively studied during the oneyear period from 1st of January 2011 to 31st of December 2011. A pre-coded data collection form was developed and ages, sex, marital and occupational status, level of education, living circumstances, and method and reasons for the suicide were studied. Results During the study period, 110 deaths from suicide were found. They were documented and analyzed. The study included 86 men (78%) and 24 women (22%). A significant percentage (22%) of those who committed suicide were in the age groups of 21-30 and another 22% in the 41-50 year group. Collectively 59% was in the 21–50 year age group, indicating that most of the deaths from suicide occurred among the young and middleaged population (Table 1). Table 1: Age group of suicide victims Age group (years) 00 – 10 11 – 20 21 – 30 31 – 40 41 – 50 51 – 60 61 – 70 71 – 80 No 00 12 24 17 24 16 11 06 % 00% 11% 22% 15% 22% 14% 10% 5% The objective of this retrospective study was to document epidemiological and socio-economic data on suicides reported to the Teaching 6 As shown in Table 2, out of the eighty six males, twenty two (28%) were single, and out of twenty four females, thirteen (55%) were single. Table 2: Marital status of suicide victims Marital status Married Single Widowed Living together Unknown Separated Divorced Total Males No. 58 22 00 00 00 00 6 86 % 67 28 00 00 00 00 5 Females No. 10 13 00 00 00 00 1 24 % 40 55 00 00 00 00 5 Sixty males (70%) were alcohol addicts. A suicidal note was found at the scene in 17% of cases. Occupational status of victims showed that not a single professional had committed suicide in this population (Table 3). Table 3: Occupational status of victims Occupation Unemployed Unskilled Semiskilled Skilled Professional Clerical and related work Managerial and administration No 39 30 20 18 00 03 00 % 35% 27% 18% 16% 00% 02% 00% Of the study population, approximately 38% were illiterate or barely literate, without any formal training. The proportion of those who had gone beyond high school was less than 20%. (Table 4). Table 4: Level of education Level of education None Year 01 – 05 Year 06 – 11 Year 12 – 13 Degree or higher Not known No. 09 33 22 22 13 11 % 08% 30% 20% 20% 12% 10% The majority (85%) of the families had a monthly income of less than $100US Living circumstances showed that the majority, (80 subjects - 73%), were living with the family at the time of committing suicide (Table 5). Table 5: Living circumstances of the victim Living circumstances on day of suicide With family (including partner) With others (e.g. friends) Alone Not known Lodging/hostel Other institution No. % 80 09 10 4 4 3 73% 8.5% 9.5% 3.5% 3.5% 2% Eighty percent committed suicide at their dwelling place. Sixteen percent of deaths due to suicide were reported during the month of April. About42% had been in contact with medical personnel in the month before their death. Analysis of the method of suicide (Table 6) showed that hanging was the commonest method (n = 56; 51%). Agrochemical substances accounted for 37 (33%) of deaths. Paraquat was the commonest pesticide used (11%). Other common causes of death includes plant poisoning (6%), “Prinso poisoning”( a detergent comprising of potassium 7 permanganate and oxalic acid) (4%) and corrosive poisoning (3%). Commonest method used was hanging in males (60%), and plant poisoning in females (30%). Table 6: Method of suicide Hanging Agrochemical Corrosives Plant poisoning Prinso Medicinal drugs Total Male No 51 32 03 00 00 00 86 Female % 60% 37% 3% 0% 0% 0% 05 05 00 07 05 02 24 21% 21% 0% 30% 21% 7% According to the evidence given at the inquest, the commonest reason for suicide was debts (35%) followed by dispute with the spouse (31%) (Table 7). Of the 12 adolescent deaths 9 had been due to scolding by parents. Past history of psychiatric illness was present in 10% and previous attempts of suicide was reported in 7%. Table 7: Reason given at the inquest for committing suicide Reason given Financial matters Dispute with spouse Dispute with parents Disputes in love affairs Problems at work Dispute with children Alcohol dependence Psychiatric disorders No 39 33 16 09 4 4 3 2 % 35% 31% 15% 8% 3% 3% 3% 2% Discussion Suicidal behavior and, in particular, the preferred suicide method varies between countries [7]. Some patterns are well known, such as the high percentage of firearm suicides in the United States of America [8]. In addition, the role of pesticide suicide in Asian countries became apparent in the 1990s [7]. While numerous factors contribute to the choice of a suicide method, societal patterns of suicide can be understood from basic concepts such as the social acceptability of the method (i.e. culture and tradition) and its availability (i.e. opportunity). International or intercultural comparisons of suicide methods help increase the understanding of the interplay between these two factors and provide a basis for preventive strategies. In 2008, 3260 men (79%) and 860 women (21%), (total 4120) committed suicide in Sri Lanka and in 2009, 1609 men (77%) and 465 women (23%), (total 2074) committed suicide [6]. The male-to-female ratio was around 5:1. In the present study the male to female ratio was around 3.5: 1 (male 78% and female 22%). In our study the victims of suicide were mostly young, married men who had interpersonal problems with their families which they could not handle. Similar observations were made in previous studies done within Colombo city limits in 2006[1] and in the Department of Forensic Medicine, Galle in 2009[9]. However, the male-to-female ratio shows that a significant number of women too had committed suicide. A significant number of deaths were reported (11%) from the age group of 11-20 years. Similar findings were observed in other studies as well [1,9]. Measures need to be taken to address these teenage suicidal trends. Most of the victims were of a low socioeconomic status; 35% were unemployed and 45% had been working as semiskilled or unskilled workers. Not a single professional committed suicide in this study. This indicates 8 that the pressures were commoner among the lower socioeconomic class. Highest number of suicides was reported during the month of April (16%). This also could be due to the increased expenditures during the festival season causing more stress. Similar findings were observed during the 2009 study at the Department of Forensic Medicine, Galle [9]. Of the study population, approximately 38% were illiterate or barely literate, without any formal training. Two fifths had completed primary school (20%) or high school education (20%). The proportion of those who had studied beyond high school was less than 20%. Similar findings were observed during the 2009 study at the Department of Forensic Medicine, Galle [9]. In previous studies done at Colombo city limits in 2006 [1] and in the Department of Forensic Medicine, Galle in 2009[9], pesticide ingestion was the commonest method of suicide among both the males and females (42%). But in this study, commonest method of suicide used by males was found to be hanging (60%) and the commonest method used by females was found to be plant poisoning (30%). From the time the first case of pesticide poisoning was reported in Sri Lanka in 1962, pesticide poisoning reached epidemic proportions in the 1990s[1]. Acute pesticide poisoning is a major health problem and in several agricultural districts it is the principal cause of death in hospitals [10]. Reduction in the number of suicidal deaths due to pesticide ingestion is a very significant finding in this study. In all the studies conducted in this regard in the past in Sri Lanka, the commonest method of suicide was found to be the pesticide ingestion. This is the first time; a change has been reported in this country. The reason for this change needed to be studied further. The possible reasons are improved management of pesticide poisoning patients in the hospitals, and the measures taken by the authorities to ban some of the very toxic pesticides in Sri Lanka. Not a single case of self immolation had been reported during this period. Newer methods like “Prinso” poisoning was found to be popular (20%) among the female victims. Debt and marital disharmony was the main reason for committing suicide (66%). Psychiatric illnesses were responsible for only 2% of suicides. Studies done in the past have shown that only 20% had a psychiatric illness and the rest were considered to have ‘impulsive personalities’[11]. The finding in our study also suggests that the majority of suicide attempts were due to sudden impulse. Sixty males (70%) were alcohol consumers and this remains a major contributory factor for committing suicide. Conclusions Majority were young married males belonging to lower socio-economic group. A significant number of teenagers were found to commit suicide following minor disappointments. Method of choice was hanging among males and plant poisoning among females. A significant reduction in suicides by pesticide poisoning can be seen. It should be noted that a new washing powder called ‘Prinso’ is being used as a method of suicide popularly among females. It was evident that both social and personal causes had contributed. Majority had been first timers. Among males, alcohol addiction remains a major contributory factor for committing suicide. 9 References 1. 2. 3. 4. 5. 6. Fernando R, Hewagama M, Priyangika W, Range SS, Karunaratne S. Study of suicides reported to the Coroner in Colombo, Sri Lanka. Med Sci Law 2010;50(1):25–28. Isaacs S, Keogh S, Menard C, Hockin J. Suicide in the Northwest Territories: a descriptive review. Chronic Dis Can 1998;19(4):152-6. A. Sev’er & R. Erkan. The dark faces of poverty, patriarchal oppression, and social change: Female suicides in Batman, Turkey. Women and International Development Journal. 2004. 282: 1-24. Garro LC. Suicides by status Indians in Manitoba. Arctic Med Res 1988;47 (Suppl 1):590-2. Lesage AD, Boyer R, Grunberg F, Vanier C, Morissette R, Ménard-Buteau C, et al. Suicide and mental disorders: a case– control study of young men. Am J Psychiatry 1994;151:1063-8. Sri Lanka Sumithrayo:Statistics and data: availableat 7. 8. 9. 10. 11. http://srilankasumithrayo.org/statistics-adata; viewed on 21/01/2012. Eddleston M, Sheriff MH, Hawton K. Deliberate self harm in Sri Lanka: an overlooked tragedy in the developing world. British Medical Journal 1998; 317: 133-5. Chan KP, Yip PS, Au J, Lee DT. Charcoalburning suicide in post-transition Hong Kong. British Journal of Psychiatry 2005; 186: 67-73. Vidanapathirana M,Rathnaweera R.H.A.I. A study on deaths due to suicides, based on cases reported to Teaching Hospital Karapitiya from 2007 to 2009. The College of Forensic pathologists of Sri Lanka – annual academic sessions 2009. Hettiarachchi J, Kodituwakku GCS, Chandras iri N. Suicide in Southern Sri Lanka. Med Sci Law 1988;28:248–51. Senanayake N, Peiris H. Mortality due to poisoning in a developing agricultural country: trends over 20 years. Hum ExpToxicol 1995;14:808–11. 10 Original article Probability of death – a guesstimate or an estimate? Recommendation for a more accurate prediction Perera Jean1*, SenanayakeSMHMK2, Appuhamy P1, Hulathduwa S3 1 Department of Forensic Medicine, Faculty of Medicine, Colombo, 2 Institute of Legal Medicine and Toxicology, Colombo, 3 Department of Forensic Medicine, Faculty of Medical Sciences, Sri Jayawardenapura. *Corresponding author: Tel – 0094-77-676-5983, e mail: [email protected] MLJSL.Vol 2. No 2. Dec. pp 11-14 Abstract Introduction The estimation of the probability of death in an injured victim is a crucial duty of the judicial medical officer in Sri Lanka. Several instruments can be used to approximately predict the probability of death/or survival. To the authors’ knowledge, so far no instrument has been used or proposed to predict the probability of death for medico-legal purposes in Sri Lanka. As such there is low inter - rater reliability with possible confusion in a criminal trial. We propose that it is the need of the hour to use such instruments in view of the current controversies around the concept “endangering life”. These instruments can also be used to categorize injuries as “fatal in the ordinary course of nature” , which are terminology used in criminal trials to categorise the severity of injuries following trauma in Sri Lanka. Description The simplest instrument, Abbreviated injury scale (AIS), an anatomical scoring system ranks each injury individually from 01 to 06. Using the AIS, Injury severity score (ISS)which takes multiple injuries into consideration is calculated which predicts the probability of death. The Revised trauma scale (RTS)is a physiologic scoring system which has a high inter - rater reliability and demonstrated accuracy. The Trauma score – Injury Severity Score (TRISS) determines the probability of survival of a patient with a formula using both ISS and RTS. Conclusion and recommendation Four injury scales/scores would be described with outlines of their usefulness and limitations. The predictive value of each code can be identified by performing multi centre studies to identify which code was more accurate in predicting the probability of death for trauma victims. This would ensure uniform expression of opinions regarding the percentage probability of death; an opinion crucial to express whether an injury is endangering life or fatal in the ordinary course of nature. Key words: endangering life, probability of death, injury severity score, estimate 11 Introduction The estimation of the probability of death in an injured victim is a crucial duty of the Judicial Medical Officer (JMO) in Sri Lanka. After examination of survivors of violence the JMO is expected to categorise each injury for legal purposes, depending on their severity and other factors. The nature of the offence and the severity of punishment for the accused in cases of assault may depend on this categorisation. If there is an existent threat to the life of the patient, an injury is categorized as “endangering life”. An injury is designated as “fatal in the ordinary course of nature”, if it causes death in the absence of prompt and proper medical attention. According to section 294 of the Sri Lanka Penal code “culpable homicide is murder if it is done with the intention of causing bodily injury to any person, and the bodily injury intended to be inflicted is sufficient in the ordinary course of nature to cause death”. Thus the JMO has to give an opinion whether an injury is “fatal in the ordinary course of nature” or “endangering life” in the columns provided in the medico – legal examination form. These two opinions are expressed taking into consideration the JMO’s knowledge, clinical and medico – legal experience. It has been noted that certain injuries categorized as ‘endangering life’ by one JMO, may not be designated as endangering life by another. As such there is low inter - rater reliability with possible confusion in a criminal trial where two experts disagree on these technical issues. To the authors’ knowledge as of now, no validated instruments are being used nor proposed in Sri Lanka to cateogorise these injuries, nor consensus arrived regarding them. At times these opinions could be a blend of guesswork and an estimate - a guesstimate. We propose that it is the need of the hour to develop an instrument in view of the current controversies especially around the concept “endangering life”. These instruments can also be used to categorise injuries as “fatal in the ordinary course of nature” , “likely to cause death”, and “unsurvivable” or “necessarily fatal” – all legal expertise. In this scores that can instrument will examples. concepts needing medical paper the injury scales and be used to develop an be elaborated quoting Description In clinical practice the probability of death and probability of survival are assessed in triage especially in disaster situations using several scores and scales. Triage is the process of classifying patients according to injury severity and determining the priority for further treatment [1].These same scores and scales can be used to quantitatively determine the probability of death for medico legal purposes. The purpose of this paper is to create awareness regarding the scales and scores available to objectively conclude the probability of death. Several instruments can be used to approximately predict the probability of death and/or survival. More than 50 experts all over the world have got together to calculate the probability of death in a given injury/injuries and devised these instruments. These are termed injury scales/scores. The simplest instrument designed in 1969 by over 75 experts all over the world and revised six times after research using trauma victims is the Abbreviated injury scale (AIS). This is an anatomical scoring system and ranks each injury individually from 01 to 06, 01 being minor, 02 moderate, 03 serious, 04 severe, 05 being critical and 06 unsurvivable (Table 01). Unsurvivable is a more appropriate medical term for what is termed as ‘necessarily fatal’ in legal parlance in Sri Lanka. AIS comprises of a dictionary with a section for each anatomical area such as the head. AIS is useful in predicting the severity of each independent injury and remains one of the most commonly used injury coding systems [2]. 12 Table 01. 01 02 03 04 05 06 patient and predicts the probability of death, is calculated using the AIS using 06 main body regions; head and neck, face, chest, abdomen, extremities (including pelvis), external. The ISS is the sum of the squares of the highest AIS code in each of the three most severely injured body regions. An example is given below. Minor Moderate Serious Severe being critical Unsurvivable Abbreviated injury score – AIS Body region Abbreviated injury score Examples of AIS and their corresponding probability of death is given below. Head and neck 4 Face 2 Thorax 5 Abdomen 1 Lower limb(extremities) Skin(external) 3 AIS(severity score) 1 2 3 4 5 6 Example superficial laceration fractured sternum open fracture humerus perforated trachea ruptured liver with tissue loss total severance of aorta %probability of death(POD) 0 1-2 8 - 10 1 50 50 100 The disadvantage of AIS when applied to medico – legal practice is that at a given time only a single injury is graded. In routine practice, often injured victims have multiple injuries and the injuries taken together will determine whether or not death will supervene. Therefore, a scale taking multiple injuries in to consideration should be available. However, in court trials into homicide and attempted homicide, sometimes it is crucial to determine whether a single injury has contributed to death; especially when there are multiple assailants and there is the need to determine the probability of death of a single specific injury. In such cases the AIS alone would be of use. Injury severity score Injury severity score(ISS) [3] which considers the overall injury burden sustained by the The bold numerals represent the three most severe injuries in a patient. The square of the AIS of these three injuries are taken to calculate the ISS. ISS = (5x5)+(4x4)+(3x3) = 50 The ISS range is 0 – 75 where a score of 75 is unsurvivable. An AIS of 6 = ISS score of 75 or unsurvivable. An ISS more than 15 has been designated as a major trauma [4]. An ISS less than 9 is a minor injury, between9 – 16 moderate, 16 – 25 serious, and over 25 severe. The Revised trauma score (RTS)is a physiologic scoring system based on the blood pressure(BP), Glasgow coma scale(GCS) and the respiratory rate(RR), and has a high inter - rater reliability and demonstrated accuracy in predicting death. Furthermore current revisions accommodate correction for low income countries, thereby it can be applied to Sri Lanka if studies are conducted to check its validity to predict death. Although calculating the score seems complex, simple computer programs are available to help. The revised trauma score ranges from 0 (dead) to 7.84 (normal). The formula for RTS = 0.9368 GCS + 13 0.7326 SBP + 0.2908 RR, thus it is heavily weighted towards the Glasgow Coma Scale to compensate for major head injury without multisystem injury or major physiological changes. The RTS (Table 02)is said to correlate well with the probability of survival [5]. In fact it has been suggested as a reliable indicator for distinguishing life threatening injuries [6]. usage can be recommended through the college. This will lead to uniformity in the expression of opinions regarding the percentage probability of death; an opinion crucial to express whether an injury is endangering life or fatal in the ordinary course of nature. References 1. ACS-COT: Resources for optimal care of the injured patient: Chicago: American College of Surgeons; 2006.available at www.ncbi.nlm.nih.gov/pubmed/22237112 (Table 02) The TRISS Calculator - Trauma - Injury Severity Score The Trauma score – Injury Severity Score (TRISS) determines the probability of survival of a patient with a formula using ISS and RTS and patient's age [7]. Conclusion and recommendation Four injury scales/scores which can be used in order to ascertain the probability of death or survival have been defined with outlines of their usefulness and limitations. The authors recommend a multi centre research through the College of Forensic Pathologists of Sri Lanka to ascertain the most appropriate score or scale for Sri Lanka. If the available scores are not valid for the above purpose then an instrument could be developed based on the above scores and a consensus should be reached. Thereafter its 2. William C Wilson, Christophe M Grandy, David B Hoyt,Trauma and critical care, First edition 2007 Informa Healthcare USA p. 432. 3. Baker SP et al, The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care, J Trauma, Vol.14,1974:187-196. 4. Lossius HM, Rehn M, Tjosevik KE, Eken T, Calculating trauma triage precision: effects of different definitions of major trauma. Journal of Trauma Management & Outcomes, 6:9 5. WWW.TRAUMA.ORG//archive/scores/rts.ht ml 6. Boyd CR, Tolson MA, Copes WS, Evaluating Trauma Care: The TRISS Method. J Trauma Vol. 27, 1987:370-378. 7. Bilgin N.G., Mert E., ÇamdevirenH., The usefulness of trauma scores in determining the life threatening condition of trauma victims for writing medical-legal reports, Emerg Med J 2005; Vol.22 issue 11:783-787. Contribution of authors Design to the study – JP Analysis of the data– JP, KS Interpretation of the results- JP, KS Writing the manuscript –JP, KS Revising the manuscript- JP, KS, PA, SH 14 Original article Sudden unexpected deaths of young adults in a tertiary care hospital for a period of four years Kitulwatte IDG*, Edirisinghe PAS, 1 Department of Forensic Medicine, Faculty of Medicine, Ragama, *Corresponding author: Tel: 0094-71-961237. E-mail address: [email protected] MLJSL. Vol 2. No 2. Dec. pp 15-21 Abstract Introduction Sudden unexpected natural death of a young adult is rare, but has a disproportionate impact on the community. This always requires a systematic forensic autopsy. At the completion of the autopsy it is expected to have the answers for all unanswered questions. However it is a challenge to the forensic pathologist since there are many sudden deaths without significant morphological anomalies. Objective: The aim of the study was to identify the causes and characteristics of sudden death among the young adults (less than 40 years of age) Study Design: Retrospective descriptive study was done based on the reports of post mortems performed on young adults who had died suddenly and unexpectedly due to natural reasons during past 4 years. The information was gathered on a pro-forma to fulfill the objectives. The data was analyzed using SPSS statistical package version 18. Results: Out of 54 autopsies analyzed, 78 % were males. 39% of the victims were of the age group of 36 to 40 years. 33% of the victims were brought to hospital before death. In 76% of the cases, a cause of death could be identified after macroscopic autopsy examination and the percentage increased to 89% after microscopy. Microscopy revealed or confirmed the cause of death in 52% of the cases. 44% were victims of sudden cardiac death. Cause of death was unascertained at the end of all the investigations in 11% of the cases. Conclusion: Cause of death has a cardiac origin in majority of sudden unexpected deaths in young adults in the sample examined. Macroscopic autopsy examination could identify a cause of death in majority while abnormalities identified at microscopic examination accounted for death in nearly half of the sudden unnatural deaths in young adults. Key words: sudden natural death, young, autopsy, microscopy, cardiac, unascertained 15 Introduction From a forensic point of view, a sudden death is defined as a rapid, natural and unexpected death [1]. Sudden unexpected natural death of a young is rare, but has a disproportionate impact on the community. The incidence of sudden natural deaths among the 1-40 year age group, is reported as 1.3 to 8.5 per 100 000 person years [2,3] while the incidence of sudden death in the general population is reported as 1 in 1000 individuals[4]. Sudden death of a young adult is a tragedy to the family and always requires systematic forensic autopsy performed by a pathologist. It is expected to have the answers for all unanswered questions at the completion of the autopsy. Historical evidence obtained from the witnesses and the family members of the deceased is crucial for this investigation. Recent symptoms prior to death and past medical history and the family history must be probed. Notes of resuscitation and the hospital records are also useful. Recent autopsy studies have revealed coronary artery disease as the major cause of death in people aged more than 35 years while cardiomyopathies are commonly seen in younger age groups (less than 35 years of age). Arrhythmogenic right ventricular cardiomyopathy is an increasingly recognized type of cardiomyopathy causing sudden deaths in young adults [5]. Diagnosis of these cardiomyopathies at the autopsy plays an important role to counsel and screen the first degree relatives. However, since all sudden deaths are not thoroughly autopsied, extracardiac causes are not well estimated [5].There are many cases of sudden deaths without significant morphological anomalies. Thus, a significant number of sudden deaths remain as autopsy negative sudden unexplained deaths even after a through autopsy. Presently due to the advancement of molecular biology, many such autopsy negative sudden unexplained deaths have ended up with a pathogenic basis worldwide [6]. An accurate diagnosis through a molecular autopsy, directs initiation of preventive strategies among the relatives. However, the molecular studies are still new and not available to the forensic community of Sri Lanka due to its high cost. Objective: The aim of the study was to identify the presentation, causes, and characteristics of sudden death among the young (less than 40 years of age) with a view to have an insight into the causation in our community and to make suggestions to improve the standards in our investigation process. Method: Retrospective descriptive study was performed based on the recorded historical evidence and the reports of the post mortems done on young adults who had died suddenly and unexpectedly due to natural reasons during past 4 years. The information was gathered on a pro-forma to fulfill the objectives. The data was analyzed using SPSS statistical package. Results: Out of the 54 autopsy cases studied, 42 (78%) were males and 12 (22%) were females. 21 (39%) were of the age group of 36 to 40 while there were 11 (20%) each for the age groups of 21-25 and 31-35. (Table:1) Table 1: Age distribution of the group Age group Frequency <20 yrs 20-25 yrs 26-30 yrs 31-35 yrs 36-40 yrs Total 5 11 6 11 21 54 Percentage (%) 9 20 11 20 39 100% Most deaths (43%; n=9 out of 21) in the age group of 36 to 40 were due to ischaemic heart disease and majority of deaths (50%; 9 out of 18) due to ischaemic heart disease are also 16 coming under this age group.18 (33%) of the group were hard working manual labourers while there were 12 (22%) office workers. (Table: 2) to death. 14 (26%) had a witnessed collapse while 12 (22%) died at sleep.(Table: 4) Table 2: Occupation of the victims Death occurred Died at sleep Witnessed collapse Brought to hospital Died on the way to hospital Died at work Other Total Occupation Manual labourer Office worker Student Other Total Frequency 18 12 5 19 54 Percent (%) 34 22 9. 35 100 29(54%) were smokers. Ethanol abuse was observed among 29 (54%). 40 (74%) had some form of ill health prior to death. Out of these 40, 15 (28%) were suffering from some illness for less than 1 day. 13 (24%) had some form of ill health for 2 days to 1 week. There were 14 (26%) with no complaints of any ill health. However 13 (24%) out of them had a diagnosed chronic condition for years.(Table: 3) Table 3: Duration of ill health Duration of ill health <1day 1day 2days-1wk 1 wk-2wk >2wk Diagnosed for years but no recent ill health None Total Frequency Percent (%) 15 2 13 5 5 13 28 4 24 9 9 24 1 54 2 100 Chest pain was observed by the next of kin in 8 (15%) of the victims while14 (26%) had shortness of breath. Symptoms were nonspecific in 15 (28%). 24 (44%) had consulted a doctor for the ill health.18 (33%) were brought to hospital prior Table 4: Presentation Frequency 12 14 18 2 Percent 22 26 33 4 1 7 54 2 13 100.0 At the end of the gross examination a cause of death was found in 41 (76%) of the cases while at completion of the microscopic examination the cause of death could be identified in 48 (89%). Macroscopic or gross autopsy examination revealed cardiac findings in 27 (50%) while 9 (17%) had nonspecific findings and 8 (15%) had none. (Table: 5) Table 5: Autopsy findings –macroscopy Macroscopic findings at autopsy Cardiac Other Nonspecific None Frequency 27 10 9 8 Percent (%) 50 18 17 15 Microscopy had been done in 34 (63%) of the cases and 6 (11%) had no significant microscopic findings. The cause of death was revealed or confirmed by microscopy in 28 (52%) cases. Microscopic examination revealed 3 cases of myocarditis and 4 cases of recent myocardial infarction where gross examination revealed nonspecific or negative findings. Thus, following microscopy, positive cardiac findings further increased and a total of 34 (63%) were observed to have cardiac findings at the end. Cardiac findings observed either macroscopically and microscopically were coronary artery disease in 17(31%) cases with associated thrombosis in 6 of them. A recent 17 myocardial infarction was observed in 5 cases (9%). Myocardial fibrosis with no recent infarction was noted in 6(11%) cases and 3(6%) had isolated myocardial hypertrophy while there were 8 others with myocardial hypertrophy associated with other cardiac findings. Cardiac causes accounted for deaths in 22 (41%) cases while 6(11%) had negative autopsy after toxicological and microscopic studies.(Table:6) Table 6: Cause of death Cause of death Frequency Sudden cardiac death Non cardiac Unascertained Total 22 26 6 54 Percent (%) 41 48 11 100 Discussion: The etiologies of sudden death of young vary among studies [7-10]. Unexplained case of sudden natural death of a young individual has a great impact on the living relatives. With the advancement of science, new methods to screen for risk factors of sudden adult deaths are available [11]. However, without a proper understanding into the etiologies in our own community, population screening methods cannot be planned. Inadequate or inconsistent investigation of young sudden deaths, results in failure to identify potentially fatal, yet treatable familial disease. A detailed investigation of sudden death in the young can reveal hereditary cardiac disease in more than 40% of the cases [12, 13]. Systematic forensic autopsy and autopsy based studies are extremely important for this purpose. Study revealed that 78% of the victims of sudden natural death are males. The mortality rate for sudden cardiac death per 100,000 person-years was observed as 6.7 for males and 1.4 for females in an autopsy-based series of a population undergoing active surveillance [14].Most of the sudden deaths due to ischaemic heart disease belonged to the age group of 36 to 40. A similar picture was observed in a study done in India where majority were towards the upper limit of the age group [15]. Majority of deaths due to ischaemic heart disease are coming under this age group. Puranik R. et al found in their study, more than two thirds of deaths caused by acute myocardial infarction occurred in the age group from 30-35 years [16]. 33% of the group were hard working manual labourers. Exertion acts as a trigger for lethal ventricular tachyarrhythmias, especially when there is underlying cardiac disease [17-19]. Literature reveals that the reported cases of sudden deaths among the young athletes are on the rise [20]. More than half of the victims were reported smokers and also there were more than half with a history of ethanol abuse. Cigarette smoking is a known risk factor for sudden cardiac death. Similarly, heavy alcohol consumption is associated with an increased risk of sudden cardiac death [21, 22]. 74% of the group reported to have some form of ill health prior to death. Mostly the symptoms were nonspecific and of a short duration. However in a study on prodromal symptoms only 18% had symptoms prior to death [23]. The recorded prodromal symptoms in this group are based on statements made by the relatives who at this desperate moment, try to relate their loved one’s death to some form of illness. However chest pain and shortness of breath were observed in 41%. Further, 44% had consulted a physician for their ill health prior to death which has to be considered important. 33% was brought to hospital prior to death while 26% had a witnessed collapse.22% of the deaths had occurred while at sleep. DeVreede Swagemakers JJM had reported that 40% of sudden deaths can be un-witnessed[24]. Macroscopic examination revealed positive findings in 85% with 50% cardiac findings. Positive cardiac findings further increased up to 63%at the end of the microscopic examination, where 3 cases of myocarditis and 4 cases of recent myocardial infarctions were added to the group. Furthermore, microscopy revealed or confirmed the cause of death in 52% of the 18 cases. The cause of death was revealed only after microscopy in 13%. At the end of the external and internal examination a cause of death was found in 76% while it increased to 89% at the end of the microscopy. Coronary artery disease was observed in 31% cases and a recent myocardial infarction was observed in 9%. Myocardial fibrosis with no recent infarction was noted in 11%. Myocarditis was diagnosed 6%. Atherosclerotic coronary artery disease accounts for the large majority of cases of sudden natural deaths in older people (over 40 years of age)[1]. The most frequent structural cardiac diseases in the young population reported are premature coronary artery disease, myocarditis, left ventricular hypertrophy and hypertrophic cardiomyopathy respectively[25,26]. Although, there were 63% cardiac findings there were only 41% cases of sudden cardiac death while there were 48% deaths due to non cardiac causes. This is due to presence of other morphological abnormality accounting for death in a person with a cardiac pathology. However, the main cause responsible for the sudden natural deaths was cardiac pathology. This highlights the importance of methodical autopsy with microscopy in all sudden natural deaths of young. However, this study revealed that microscopy had been done only in 63% of the cases in this group which needs further attention. This can prevent detection of cardiac causes of death which is extremely important in planning the screening process of the family members. 11% had no morphological cause of death. Autopsy of sudden unexpected death is sometimes inconclusive even after microscopy and molecular biology may have played a crucial role in coming to a conclusion [27]. Thus, it is high time for us to pay attention to molecular autopsy. This will reduce the number of cases ending up as “cause of death unascertained”. Conclusions: Predominantly male victims of 36-40 years are the risk group for sudden natural deaths. Cardiac causes account for majority of sudden natural deaths of young adults with coronary artery disease placed first. Systematic forensic autopsy with proper ancillary testing is essential in sudden natural deaths of young. There is a significant proportion of cases with an unascertained cause of death highlighting the importance of further studies. References 1. Grandmaison GL: Is there progress in the autopsy diagnosis of sudden unexpected death in adults? Forensic Sci Int. 2006, 156:138-144 2. Shen WK, Edwards WD, Hammill SC, Bailey KR, Ballard DJ, Gersh BJ. Sudden unexpected nontraumatic death in 54 young adults: a 30-year population-based study. Am J Cardiol. 1995;76:148 –152. 3. Liberthson RR. Sudden death from cardiac causes in children and young adults. N Engl J Med. 1996; 334:1039 –1044. 4. De Vreede-Swagemakers JJ, Gorgels AP, Dubois-Arbouw WI, van Ree JW, Daemen MJ, Houben LG, Wellens HJ. Out-of-hospital cardiac arrest in the 1990’s: a populationbased study in the Maastricht area on incidence, characteristics and survival. J Am Coll Cardiol. 1997;30:1500–1505 5. G.L. de la Grandmaison, M. Durigon, Sudden adult death: a medico-legal series of 77 cases between 1995 and 2000, Med. Sci. Law 42 (2002) 225–232 6. Tester DJ, Ackerman MJ. The role of molecular autopsy in unexplained sudden cardiac death. Curr Opin Cardiol. 2006 May;21(3):166-72 19 7. Maron BJ, Epstein SE, Roberts WC. Causes of sudden death in competitive athletes. J Am Coll Cardiol 1986;7:204 –14. 8. Maron BJ, Doerer JJ, Haas TS, Tierney DM, Mueller FO. Sudden deaths in young competitive athletes: analysis of 1866 deaths in the United States, 1980-2006. Circulation 2009;119:1085–92. . 9. Puranik R, Chow CK, Duflou JA, Kilborn MJ, McGuire MA. Sudden death in the young. Heart Rhythm 2005;2:1277– 82. 10. Wisten A, Forsberg H, Krantz P, Messner T. Sudden cardiac death in 15-35-year olds in Sweden during 1992–99. J Intern Med 2002;252: 529–36. 11. Ackerman MJ, Tester DJ, Driscoll DJ. Molecular autopsy of sudden unexplained death in the young. Am J Forensic Med Pathol 2001;22:105–11. 12. Behr E, Wood DA, Wright M, Syrris P, Sheppard MN, Casey A, Davies MJ, McKenna W. Cardiological assessment of first-degree relatives in sudden arrhythmic death syndrome. Lancet. 2003;362:1457-9. 13. Tan HL, HofmanN , van Langen IM, van der Wal AC, Wilde AA. Sudden unexplained death: heritability and diagnostic yield of cardiological and genetic examination in surviving relatives. Circulation. 2005;112:207-13. 14. Eckart RE, Shry EA, Burke AP, McNear JA, Appel DA, Castillo-Rojas LM, Avedissian L, Pearse LA, Potter RN, Tremaine L, Gentlesk PJ, Huffer L, Reich SS, Sudden death in young adults: an autopsy-based series of a population undergoing active surveillance. J Am Coll Cardiol. 2011 Sep 13;58(12):125461. 15. Chaturvedi M, Satoskar M, Khare MS, Kalgutkar AD. Sudden, unexpected and natural death in young adults of age between 18 and 35 years: A 16. 17. 18. 19. 20. 21. 22. 23. 24. clinicopathological study. Indian J Pathol Microbiol 2011;54:47-50 Puranik R, Chow CK, Duflou JA, Kilborn MJ, McGuire MA. Heart Rhythm. Sudden death in the young. 2005 Dec;2(12):1277-82. Heart Rhythm. 2005 Dec;2(12):1277-82 Maron BJ, Shirani J, Poliac LC, Mathenge R, Roberts WC, Mueller FO. Sudden death in young competitive athletes: clinical, demographic and pathologic profiles. JAMA. 1996;276:199 –204., Maron BJ, Gohman TE, Aeppli D. Prevalence of sudden cardiac death during competitive sports activities in Minnesota high school athletes. J Am Coll Cardiol. 1998;32:1881– 1884. Corrado D, Basso C, Rizzoli G, Thiene G. Does sport activity enhance the risk of sudden death in adolescents and young adults? J Am Coll Cardiol. 2003;42:1964 – 1966 Barry J. Maron and Antonio Pell. The Heart of Trained Athletes : Cardiac Remodelling and the Risks of Sports, Including Sudden Death. Circulation. 2006;114:1633-1644] Wannamethee G, Shaper AG. Alcohol and sudden cardiac death. Br Heart J. 1992;68:443– 448. , Dyer AR, Stamler J, Paul O, Berkson DM, Lepper MH, McKean H, Shekelle RB, Lindberg HA, Garside D. Alcohol consumption, cardiovascular risk factors, and mortality in two Chicago epidemiologic studies. Circulation. 1977;56:1067–1074 TIAN Zhao-xing, LÜ Yan-yu, YAN Wei, ZHAO Wen-kui and LI Xuan. Analysis of the prodromal symptoms of unexplained sudden death in patients with or without underlying diseases. Chinese Medical Journal 2012;125(20):3619-3623 de VreedeSwagemakers JJM, Gorgels APM, Dubois-Arbouw WI, van Ree JW, Daemen 20 MJAP, Houben LGE, Wellens HJJ. Out-ofhospital cardiac arrest in the 1990’s: a population-based study in the Maastricht area on incidence, characteristics and survival. J Am CollCardiol. 1997; 30:1500 – 1505 25. Wren C, O’Sullivan JJ, Wright C. Sudden death in children and adolescents. Heart. 2000;83:410–413. 26. Morris VB, Keelan T, Leen E, Keating J, Magee H, O’Neill JO, Galvin J. Sudden cardiac death in the young: a 1-year postmortem analysis in the Republic of Ireland. Ir J Med Sci. 2009;178:257–261 27. De Salvia A, De Leo D, Carturan E, Basso C. Sudden cardiac death, borderline myocarditis and molecular diagnosis: evidence or assumption? Med Sci Law. 2011;51Suppl 1:S27-9. doi: 10.1258/msl.2010.010056. Contribution of authors Design to the study - IDGK, PASE, Analysis of the data- IDGK Interpretation of the results- IDGK Writing the manuscript -IDGK Revising the manuscript-IDGK, PASE 21 Original article Practices and attitudes of specialists in Forensic Medicine in the management of general health care needs of victims of sexual violence Perera J1*, Arambepola C2, Wijeratne P1 1 Department of Forensic Medicine and Toxicology, 2Department of Community Medicine, Faculty of Medicine, University of Colombo, Sri Lanka *Corresponding author: Tel – 0094-77-676-5983, e mail: [email protected] MLJSL.Vol 2. No 2. Dec. pp 22-29 Abstract Introduction The emphasis of sexual assault forensic management (SAFM) in Sri Lanka has been mainly pertaining to collection of forensic evidence and as a referral point to other specialist services. Objectives To describe the practice and attitudes of Specialists in Forensic Medicine (SpFM) regarding the management of general health care needs in victims of sexual violence as part of sexual assault forensic management (SAFM) with a view to providing a victim friendly management. Methods A cross-sectional study was conducted to include all practicing (SpFM) in Sri Lanka. Victim centred practices as well as attitudes underlying their practice were assessed using a self-administered questionnaire. Results The response rate was 52.08% (n=25). 92% of the SpFM were males and had a mean age of 45.48years (SD=5.561). Many (48%) felt that only those who appeared to be psychologically disturbed need to be referred to a counselor. The majority (72%) never provided and 32% never prescribed emergency contraceptive pills (ECP) to victims. Most of them strongly disagreed that giving emergency contraception or reviewing the victim introduced victim bias. Conclusions Despite positive attitudes towards victim-friendly management, health care needs like pregnancy prevention and relieving psychological distress were not addressed adequately. Fear of being accused of victim bias was not a significant factor for not taking adequate steps. It could be due to inadequate awareness regarding new developments in victim friendly management and hesitancy to change existing practice during SAFM. Key words: Sexual assault forensic examination, victim-friendly management, emergency contraception, attitudes, victim bias, health care needs 22 Introduction Sexual assault is an aggressive act motivated by power and control [1]. It has both long term and short term physical and psychological effects on the health and wellbeing of a victim. Thus, during sexual assault medical forensic management (SAFM), the health and welfare of patients become the foremost priority [1] that goes well beyond proving the case in a court of law [2]. As such, in addition to providing evidence for legal proceedings, forensic medical practitioners have a crucial responsibility to ensure that the health care needs of victims of sexual violence are addressed adequately in their clinical practice. The “victim-friendly approach or management” advocated in many SAFM protocols recognizes that “every sexually assaulted victim deserves timely, compassionate, respectful and appropriate care”[3]. In many centres in the developed countries appropriate care in SAFM includes the treatment of injuries, prevention of unwanted pregnancies, prevention and treatment of sexually transmitted infections (STI), and the provision of psycho-social support and adequate rehabilitation programs [3,4] in addition to the collection of forensic evidence. In these countries, victims are often referred to emergency medical units where all these services are available under one roof. However at times, lapses on addressing health care needs of these victims are reported from these countries as well. A survey done on emergency departments in Pennsylvania, USA revealed that 16% of the hospitals do not offer any emergency contraception nor counseling [5] while in USA on the whole, 42% of non-Catholic and 55% Catholic hospitals neither dispense ECP nor provide a valid referral for ECP [6], thus causing lost therapeutic opportunities. In Sri Lanka, the legal procedure when a victim lodges a police complaint regarding sexual violence is to subject her to medico–legal examination. Quite commonly, the first contact health care personnel for such examinations would be the Specialist in Forensic Medicine (SpFM). In the absence of guidelines on providing victim-friendly SAFM, the SpFM are in the practice of engaging exclusively in the medicolegal aspect of care and referring the victims to relevant specialists for management of their general health care needs. However, there is no systematic approach to verify whether in fact all referred victims would access these clinical services. Clinical guidelines ensure the provision of minimum care with acceptable standards and are proven to be effective universally [1,3,7,8]. However, when developing guidelines for providing victim-friendly SAFM, they should be pragmatic, based on the challenges faced by SpFM in addressing the general healthcare needs of victims as well as their own attitudes that may influence their practice. Authors particularly intended to find out whether fear of being accused of victim bias had affected the decision to look after the general health care needs. Therefore, in the absence of such evidence in Sri Lanka, we conducted a study that aimed at describing the practices and attitudes of SpFM in the management of general health care needs of victims of sexual violence. Methodology A descriptive cross-sectional study was conducted among all clinicians who were Board certified by the Postgraduate Institute of Medicine (PGIM) as Specialists in Forensic 23 Medicine in Sri Lanka. Those who did not have more than six months experience as specialists and those who were not in active practice were excluded from the sample. Data on the attitudes and practices of SpFM with regards to psychological counseling, pregnancy and STI prevention, and review of victims was collected using a self-administered questionnaire prepared in English language. Guidelines for medico – legal care of victims of sexual violence by the World Health Organisation (WHO)1 were perused for developing the questionnaire. A five-point Likert scale (‘strongly agree’, ‘agree’, ‘neutral’, ‘agree’, ‘strongly disagree’) was used as responses to the questions on attitudes. They were requested to return the questionnaire within six weeks. Those who did not return the questionnaire at the end of six weeks were taken as not consenting to the study and thus taken as non-respondents. Ethics clearance for the study was obtained from the Ethics review committee of the Faculty of Medicine, University of Colombo. SPSS statistical software was used for data analysis. Categorical data were described in proportions and quantitative data in mean and standard deviation (SD). Results Out of 48 SpFM Board certified by the PGIM, University of Colombo as at September 2012, 25 returned the completed questionnaires (response rate =52.08%).92% of the participants were males and of the average age of45.48years (SD=5.561). All except one (96%) had examined more than 80 victims of sexual assault during their entire practice while the majority (57%) had performed the last SAFM within the last week. The level of victim friendly management during communication with the victim was assessed. The key phrases used were “speaking to victims in a nonjudgmental manner” , “encouraging the victim during history taking by appropriate body language”, and using appropriate words like” hmm”, “go on” with a scale ranging from ‘always to never done’. The questionnaire with an enclosed selfaddressed envelope and an information sheet about the objectives of this study were posted to all SpFM in the specialist register maintained at the PGIM. Most of the SpFM practiced speaking to a victim in a non-judgmental manner always or most of the time (84%). (See Table 1.) Table 1: Results concerning, following the formal routine in Communicating with victims (n = 25) (%- Number of respondents as a percentage) Form of routine Speaking to a victim in a nonjudgmental manner Using appropriate gestures or non verbal communication skills Using appropriate words Number of respondents Always Most of the Time figure % Figure % Sometimes Never figure % figure % 13 52% 08 32% 01 4% 01 4% 10 40% 07 28% 03 12% 05 20% 10 40% 08 32% 02 8% 05 20% 24 Only 10 (40%) always used appropriate gestures. Two (8%) used appropriate words only sometimes and 20% never did so. Out of the five who never used appropriate gestures or words reasons were given by three. One comment was “not aware of the importance of it’, another, “gestures are not always reliable” and the other one “it is an inappropriate practice in medico-legal setting”. A statement was included in the questionnaire “Giving emergency contraception denotes partiality towards victims”. Most of the participants (80%) strongly disagreed with this statement. Furthermore, taking action to prevent pregnancy was considered as being ‘extremely important’ by 96% of responders. During SAFM, 80% explained the risk of getting pregnant to victims ‘always’ or ‘most of the time’. However, a significant number (72%) never provided emergency contraception to the victims and 32% never prescribed emergency contraceptive pills (ECP)(Table 02) One reason for not prescribing ECP was due to the referral made to a Gynecologist ‘sometimes’ (60%) or ‘most of the time’ (20%). Reviewing the victim for late psychological complications was not a regular event, with 32% never reviewing and 16% rarely doing so (Table 02). Likewise, review for assessment of healing was not common, with 16(64%) reviewing rarely or never. 72% considered that ‘review of the victim was not extremely important. However, 68% ‘disagreed’ or ‘strongly disagreed’ that reviewing the victim indicates victim bias. Table 2: Prevention of pregnancy, referral for counseling and Post-examination reviews (n = 25) (%- Number of respondents as a percentage) Number of respondents Always Figure % Most of the Time figure % 09 (36%) 06 (24%) 04 (16%) 01 (4%) 05 20% 02 (08%) 04 (16%) 09 (36%) 02 (8%) 08 32% 01 4% 04 16% 08 32% 04 16% 08 32% 01 04% 03 12% 05 20% 07 28% 09 36% Form of routine Referral psychological counseling Prescribing ECP Review for psychological complications Review assessment healing Sometimes Rarely Never figure % figure % figure % for late for of 25 Only 60% referred the victim ‘most of the time’ or ‘always’ to a counselor. 48% either agreed or strongly agreed with the statement “only those who appear to have psychological disturbances should be counseled” (Chart 01). Information regarding risk of getting STI was given always or most of the time by 76% of respondents. STI prophylaxis (Table 03) was never prescribed by 23(92%); lack of knowledge regarding STI prophylaxis being the reason given by 01 SpFM for not prescribing. Others gave the reason as referral to STI clinic. STI prophylaxis was provided sometimes by 01(4%), most of the time by 01(4%) and never provided by the remaining 23(92%). stronly disagreed disagreed 6, 24% 7, 28% agreed 5, 20% Unavailability of drugs for STI prophylaxis was given as the reason for not prescribing by 04 (16%). Obtaining necessary samples for STI testing was never done by 21(84%), sometimes by 02(08%) and most of the time by 02(08%). However, all 25(100%) referred them to the STI clinic always or most of the time. 20(80%) strongly agreed that it is their duty to prevent STI in sexual assault victims while 03(12%) agreed with the view, but 02(8%) strongly disagreed. neutral 5, 20% stronly agreed 2, 8% Chart 01.Response to the statement “Only those who appear to have psychological disturbances should be counseled” Table 03: Action taken to prevent STI (n = 25)(%- Number of respondents as a percentage) Number of respondents Form of routine Giving Information regarding risk of getting STI Prescribing STI prophylaxis Referral to STI clinic Always Figure % Most of the Time figure % Sometimes figure % Rarely figure 08 (32%) 11 (44%) 01 (04%) - - 01 04% 01 13 52% 12 48% - Discussion The SpFM is in many instances the first contact health care professional for the sexual violence victim in Sri Lanka. Therefore, it is in the interest of the victim if SpFM addresses the % Never figure % 04 (16%) 01 04% 04% - - 23 92% - - - - - general health care needs of the victim whenever possible or devise a mechanism to ensure they are addressed. According to our study, SpFM seemed to have positive attitudes regarding prevention of 26 pregnancy (96%), with only one participant (4%) dissenting, which indicates that they are much concerned about the welfare of the victim. Despite these positive attitudes, they preferred to entrust this responsibility to a Gynaecologist routinely even though there was no way of verifying whether they in fact obtained emergency contraception when indicated. Such dependence on the gynaecologist to prescribe or administer ECP can lead to secondary victimization due to long waits; consequent failure to comply can cause an unwanted pregnancy. This practice is unlikely to be due to the attitude that providing ECP indicates victim bias or partiality as 80% strongly disagreed with that view. The role of therapy or psychological counseling for recovery from sexual violence is well established [1,7,8]. However, only 60% referred victims to a mental health professional or counselor most of the time or always. This may be in connection with the decision of 48% of the participants to refer only those victims who appear to be psychologically disturbed for counseling. This attitude appears risky as psychological effects of trauma may be more difficult to recognize [7] than physical effects especially to the doctor who has only a basic knowledge in psychiatry. When severely traumatized, victims can appear to be calm, indifferent, submissive, jocular, etc. [3], thus masking the real emotional disturbance. Furthermore, the late occurrence of mental health effects of sexual violence are well documented [7]. Reviewing the victim regularly is recommended in the WHO guidelines [1] and in many other protocols [7,8]. This is necessary for follow-up action for pregnancy and STI, to ascertain evidence of healing of injuries that could have medico–legal significance, to assess the emotional or mental status [1] and also for further relevant referral. However, according to our study, 32% never reviewed the victim for psychological complications and 36% never reviewed for evidence of healing (Table 02). This practice reflects the attitude of the majority (72%) that review is not extremely important. However, it can be concluded from this study that reluctance to review the victim was not directly connected with their fear of being accused of victimbiasas68% of SpFM either disagreed or strongly disagreed with that view. It could probably be due to lack of awareness regarding the benefits and the global stand regarding review. However, 20% have deviated from the traditional practice and have been conducting a review for psychological effects most of the time or always. The role of a SpFM is to conduct the SAFM in a manner that initiates fast healing of the victim physically as well as mentally9. The fact that 84% treated the victims in a nonjudgmental manner, with 68 % routinely using appropriate gestures - nonverbal communication and a significant percentage(72%) often using appropriate words indicate that SpFM have endeavoured to create a victim friendly environment in SAFM. Using words like “please go on” and appropriate gestures such as nodding the head make victims comfortable and encourage them to reveal the complete story. However, 32% of the SpFM stated that they did not routinely use such gestures and 05(20%) stated that they never used them. Judging from the comments, one reason for not using effective communication skills could be the traditional stand that medico-legal professionals have to appear impassive and without expression in order to appear impartial. On the contrary, an ideal SpFM should be 27 sensitive to the victim’s physical and psychological trauma while avoiding partisanship [4] and being impartial [1]. Another reason is the inadequate training in nonverbal communication skills as commented by one or even lack of awareness for its necessity in SAFM [9]. Conforming with standard traditional practice for SpFM in Sri Lanka 92% never prescribed or provided STI prophylaxis but all took necessary action by referring them to the STI clinic either always or most of the time which is satisfactory. But it is interesting to note that 02 have broken away from the traditional practice and have been either prescribing or providing STI prophylaxis as advocated in many protocols. Limitations of the study The response rate was only 52.08%, which was relatively satisfactory for a postal questionnaire. Conclusions In keeping with the current global thinking, the majority of SpFM possessed the attitude that attending to general health care needs such as prevention of pregnancy and STI, provision of counseling and victim friendly communication was important. However, many did not take adequate steps to apply it to practice except in the case of victim friendly communication. Fear of being accused of victim bias was not a significant factor for not taking adequate steps. One possibility is inadequate awareness of new global developments in SAFM. Another possibility is their attitude of not taking a different view from traditional practices, thereby being hesitant to change while confining themselves exclusively to taking care of only forensic management during SAFM. Recommendations Specialization courses in Forensic Medicine should include a mental health module and input in effective communication skills. Attitudes of SpFM described above should be taken into consideration when developing guidelines for the management of general health care needs of victims. Awareness programmes should be conducted for SpFM on the global changes regarding SAFM. Such programmes could contribute towards an attitudinal change towards victim-friendly SAFM. References: 1. Guidelines for medico – legal care of victims of sexual violence. Geneva, World Health Organization, 2003. 2. Nadesan K (2001)Rape: An Asian perspective. Journal of clinical forensic medicine, 8: 93 – 98. 3. U. S. Department of Justice. A national protocol for sexual assault medical forensic examinations (adults/adolescents), U.S. Department of Justice, Office of Violence Against Women; 2004. 4. Cunningham N (2012) Sexual assault consultations: From high risk to high reliability. Journal of Forensic and Legal Medicine.19:pg 53 – 59 5. Harrison T. (2005) Availability of emergency contraception: a survey of hospital emergency department staff. Annals of Emergency Medicine, 46(2):105-110 6. Patel A, Simons R, Piotrowski ZH, Shulman L, Petraitis C. (2004)Under-use of emergency contraception for victims of sexual assault. International Journal of Fertility and Women's Medicine, 49(6):269-273. 7. Harris L, Freccero J, Sexual violence: medical and psychosocial support, Sexual violence and accountability project, Human Rights centre University of California, May 2011. 28 8. Clinical management of rape survivors: Developing protocols for use with refugees and internally displaced persons, InterAgency Lessons Learned Conference: Prevention and Response to Sexual and Gender-Based Violence in Refugee Situations, 2001, World Health Organisation, Geneva, Switzerland pg 25 28. 9. Perera JM, De Zoysa P. The need for effective communication skills in the medico-legal management of child sexual assault victims: observations from the Sri Lankan context. Sri Lanka Journal of forensic medicine science and law 2012;3(1) 16 – 19. Acknowledgements All specialists in Forensic Medicine who participated in the study, Dr. Subhani Poornima for assisting in data analysis, and formatting the paper. CONTRIBUTION OF AUTHORS Design and Supervision of the study - JP, CA Data collection – JP, PW Analysis of data – CA, JP, PW Interpretation of results – JP, CA Writing the manuscript – JP, CA, PW Revising the manuscript –CA, JP 29 Case report An unusual case of mediastinal malignant melanoma with a cardiac metastasis Lakmali MGN, Mudduwa L, Fernando LBM, Mahinda HA Institute of Legal Medicine and Toxicology, Colombo *Corresponding author: Tel: 0094-718208938. E-mail address: [email protected] MLJSL. Vol2. No2. Dec. pp30- 34 Abstract: Introduction Mediastinal tumours are often seen in patients aged 30–50 years. Most of them are neurogenic tumours and thymomas. Others include lymphomas, phaeochromocytomas, melanomas, germ cell tumours and thyroid and parathyroid lesions. Although primary cardiac tumours are rare, metastasis in the heart is commoner than primary cardiac tumours. Case report A 41 year old woman was admitted to the Teaching Hospital, Karapitiya with a recent onset progressive dyspnoea. She was found to have a rapidly filling pericardial effusion. She died on the third day of admission. A whitish mass infiltrating the full thickness of the right atrial myocardium was found at the autopsy. A similar tumour was present in the anterior mediastinum measuring 7x3cm. There was no direct connection between the two tumours. H&E stained sections revealed a similar microscopic appearance in both mediastinal and cardiac masses. The differential diagnosis included lymphoma, melanoma, carcinoma and germ cell tumors. Immunohistochemical staining for LCA, pan cytokeratin, S100 and PLAP were done and only S100 was positive. Conclusion Negative staining for LCA, pan cytokeratin and PLAP excluded the possibility of lymphoma, carcinoma and germ cell tumours. Positive staining for S100 confirmed the diagnosis of melanoma. This was diagnosed as a rare case of primary mediastinal malignant melanoma with a right atrial metastasis causing pericardial effusion. Key words: mediastinal tumours, melanoma, metastasis, heart 30 Introduction: Malignancies are found rarely in the mediastinum. Only 3% of mediastinal tumours are primary tumours [1]. Out of them 25-49% are malignant. Primary mediastinal malignancies comprise 55% lymphomas, 16% germ cell tumours, 14% thymomas, 5% sarcomas, 3% neurogenic tumours and 7% other rare tumours [2]. Malignant melanoma belongs to this rare category. Patients with mediastinal tumours often present with cough, dyspnoea, chest pain and fever. Investigations helpful in diagnosis are chest X-ray, computed tomography, MRI chest and mediastinoscopy with biopsy. Treatment for these tumours include radiation, chemotherapy and surgical excision [1]. The prognosis of primary mediastinal malignant melanoma has not being described probably due to the rare occurrence of the disease [3]. The five year survival of malignant melanoma of the skin is extremely poor; one will therefore not expect that of the mediastinum to be any better [4]. At autopsy the pericardium contained 100cc of straw coloured fluid. Heart was enlarged and measured 370g. There was a mass involving the full thickness of the anterior wall of the right atrium and measured 7×7×1.5cm in size (Figure 01). The cut surface appeared whitish with necrotic areas. Bleeding into the myocardium was found. Coronary arteries and the large blood vessels appeared normal. Figure 01: Cardiac tumour Case report: A 41 years old mother of 3 children presented to a medical ward complaining of loss of appetite for 2 months, dyspnoea on mild exertion and chest pain for 2 weeks and on and off fever for 1 week. She was found to be having anaemia and features of pericardial and bilateral pleural effusions. Urgent echocardiogram revealed an early cardiac tamponade. Straw coloured pericardial fluid measuring 850ml was aspirated. It was rapidly filling and 500cc of fluid was removed during a second pericardiocentesis done on the next day. Microscopic examination of the pericardial fluid was negative for acid fast bacilli but contained malignant cells. Ultrasound scan of the abdomen revealed mild hepatomegaly with a small amount of free fluid in the peritoneum. The patient expired away on the third day of admission while waiting for further investigations. Another whitish mass measuring 7×3×2cm in size was found in the middle mediastinum. The tumour was lying anterior to the trachea, above the bifurcation and it encircled the left carotid vessels (Figure 02). The cut surface had a similar appearance with the cardiac tumour. Mediastinal lymph nodes were not enlarged. Mild pulmonary oedema was present. Peritoneum contained 300cc of ascetic fluid. Liver was congested with no macroscopic metastatic deposits. Other organs were normal except for the kidneys which showed surface scarring. Sections were obtained from both tumours and each organ for histological examination. Haematoxylin and Eosin stained sections were evaluated (Figure 03). 31 Figure 2: Mediastinal tumour The differential diagnosis included lymphoma, melanoma, epithelial cell tumours and germ cell tumours. Immunohistochemical staining for LCA, pancytokeratin, S100 and PLAP were done and only S100 was positive which was confirmatory of melanoma. Figure 3: Tumour cells myocardium (H&E x10) infiltrating I. II. III. IV. the Discussion: Skin is the most common site for primary malignant melanoma; the most fatal cutaneous neoplasm [5]. Malignant melanomas are developed by neoplastic transformation of melanocytes in the epidermis invading the dermis secondarily. Patients with cutaneous melanomas often develop metastasis at other sites of the skin, lymph nodes and lungs. More than 90% of malignant melanomas are cutaneous in origin [5]. In addition, melanoma can arise from mucous membranes of nasal cavity, sinuses, lips, buccal mucosa, palate, base of the tongue and tonsils [4]. They can arise in the oesophagus, larynx, gallbladder and leptomeninges rarely. Primary malignant melanoma in the mediastinum is extremely rare, with only a few cases reported to date [6]. A primary malignant melanoma of the mediastinum could be confirmed on the following grounds [4, 5, 7]. No history suggestive of previous melanoma on skin. No demonstrable melanoma was found in the skin or other organs during the autopsy. Tumour morphology compatible with that of a melanoma. Confirmation by immunohistochemical staining for S100. There are several explanations as to how these primary melanomas developed in the mediastinum. The most likely explanation is that these tumours arise from melanocytes which have migrated along with the down growth of the primordial respiratory tract during the intrauterine life from the primitive foregut [7]. Ectopic naevus cells in the mediastinal lymph nodes or thymus may undergo malignant change and produce primary melanoma of the anterior mediastinum [7]. Alternatively tumours may arise from areas of squamous metaplasia in which some of the epithelial cells have undergone differentiation into melanocytes [7]. Almost half of mediastinal tumours cause no symptoms and are found on a chest x-ray done for some other reason. Symptoms that do occur are due to compression of local structures and may include: chest pain, chills, cough, haemoptysis, fever, hoarseness, night sweats and shortness of breath In this case tumour metastasis was found in the heart. Although primary cardiac 32 tumours are rare, metastasis in the heart is common. Due to its resemblance of the morphology and histology to the mediastinal tumour and the absence of possible explanation for a primary malignant melanoma of the heart, we suggest that the cardiac tumour is a secondary from a primary mediastinal tumour. Myocardial involvement by neoplasm arising elsewhere in the body is no longer considered rare [8]. Secondary or metastatic heart tumours occur comparatively more frequently, with at least a 100 times higher incidence than primary tumours [9]. Effects of metastases to the heart include a rapid increase in heart size by pericardial effusion, new signs of heart failure or valve disease, conduction defects, and atrial or ventricular heart rhythm disturbances [9]. Pericardial involvement of tumour cells causes pericarditis and serosanguinous or haemorrhagic pericardial effusion. Rapid filling of pericardial fluid leads to cardiac tamponade due to the low compliance of the pericardium to accommodate such an acute increase of pericardial fluid [9]. It causes severe haemodynamic compromise and death. It is treated with expansion of intravascular volume (small amounts of crystalloids or colloids may lead to improvement, especially in hypovolaemic patients) and urgent pericardial drainage [10]. Replacement of the myocardium by tumour cells and obliteration of the heart chambers by intra cavitatory growth of the tumour end up in cardiac failure. Invasion of the conducting tissues of the heart leads to atrial and ventricular rhythm abnormalities. Complete AV block causes syncope and sudden death. Tumour embolism to a coronary artery and invasion or compression of coronaries by tumour result in myocardial infarctions [9]. In this case the pericardial fluid at the time of death was 100cc and as little as 100ml of pericardial fluid can be fatal depending on the rapidity of its accumulation although 400- 500ml of fluid is thought to be sufficient to cause fatal cardiac tamponade [11]. So the mechanism of death can be cardiac tamponade, arrhythmia, heart failure, myocardial infarction or sudden cardiac death. Conclusion We report this case as a primary malignant melanoma of the mediastinum with a right atrial metastasis causing pericardial effusion, as there was no evidence of a primary pigmented lesion on the skin or at any other site in spite of thorough pathological evaluation. 1. References 1. Strollo DC, Christenson RD, Jett JR. Primary mediastinal tumours. Part 1. Tumours of the anterior mediastinum. Chest 1997 Aug; 112(2): 511-522 2. Temes R, Chavez T, Mapel D, Ketal L, Crowell R, Key C, Follis F, Pett S, Warnly J. Primary mediastinal malignancies; Findings in 219 patients. West J med 1999 march; 170(3): 161-166 3. Kalra A, Kalra A, Palaniswami C, Gajendra E, Rajput V. Primary malignant melanoma presenting as superior mediastinal mass. Int J Surg Case Rep 2011; 2(8): 239-240 4. Adebonojo SA, Grillo IA, Durodola JI. Primary malignant melanoma of the bronchus. Journal of the national medical association 1979; 71(6): 579-581 5. Neri S, Komatsu T, Kitamura J, Otsuka K, Katakami N, Tkahashi Y. Malignant melanoma of the lung. Report of two cases. Ann Thoracic Cardiovascsurg 2011; 17(2): 170-171 6. Park SY, Kim MY, Chae EJ. Primary malignant melanoma of the mediastinum. KJR 2012; 13(6) : 823-826. 7. Farrel DJ, Kashyap AP, Ashcroft T, Morrit GN. Primary malignant melanoma of the bronchus. Thorax 1996; 51: 223-224 33 8. Young JM, Goldman JR. Tumour metastasis to heart. J of the American heart Association 1954; 9: 220-227. 9. Reynen K, Kockeritz U, Strasser RH. Metastasis to the heart. Annals of Oncology 2004; 15: 375-381. 10. Hoit BD. Pericardial disease and pericardial tamponade. Crit Care Med. Aug 2007;35(8 Suppl):S355-64 11. Ebert LC, Ampanozi G, Ruder TD, Hatch G, Thali MJ, Germerott T. CT based volume measurement and estimation in case of pericardial effusion. J of forensic and Legal Medicine 2012; 19: 126-131. Contribution of authors Performing the autopsy-LMGN, MHM Opinion- LMGN, ML Writing the manuscript –LMGN Revising the manuscript- FLBM, ML 34 Stories given by children, when to take it with a pinch of salt? Case report Warushahennadi J1. Hewage Chandanie G.2 1. Department of Forensic Medicine, Faculty of Medicine, University of Ruhuna, Galle. 2. Department of Psychiatry, Faculty of Medicine, University of Ruhuna, Galle. *Corresponding author: Tel: 0094-773909525. E-mail address: [email protected] MLJSL. Vol 2. No 2. Dec. pp 35 –38 Abstract The history given by a child is very important in child abuse investigations. This is especially relevant in cases of child sexual abuse as in some forms of sexual abuse injuries may be absent. The only evidence to prove the case sometimes is the evidence given by the child. The law presumes that the statements given by the child are true. To what extent can a doctor believe a child’s history? This case report describes a situation where a child gave a history of being kidnapped and in the child’s own words, “cared for” twice, by an unknown person. There was a suspicion that the child may have been sexually abused. The child gave a similar detailed history to the Judicial medical officer (JMO), police, and the psychiatrist. Based on the information received from the child, various investigatory procedures were initiated by the police. But the detailed examination of this “victim” by the child psychiatrist revealed that the child was having a significant and very prominent fantasy life of a romantic/sexual nature. It was also detected that the child was not very bright intellectually. It appeared that a big proportion of the story given by the child was coloured by her experiences and fantasies. This case reveals the importance of suspecting the possibility of fantasy, when an unusual story without supporting evidence is given by a child. Key words: child abuse, fantasy, admissibility, evidence Introduction The investigation of a case of child abuse is initiated with the history obtained from the child in many instances. The history given by the child is taken as a guide for medico legal investigation by the doctor and for criminal investigation by the police and it helps the clinician to judge whether the child’s history fits the given situation [1].The child’s history plays a very important role especially in cases where there is no medical evidence or laboratory evidence to support sexual abuse. 35 This is a case where a child gave a story of being taken away by an unknown male which aroused the suspicion of possible abuse, and was later found to be a fantasy. the girl. The examination of genitalia revealed no evidence of penetration. She was referred to the child psychiatrist as part of the routine assessment. Case report The police had started investigations in to the case and done a scene visit of the house where she lived. The house was a partially broken mud hut which was an illegal construction. Police had taken the child along several roads to see if she could identify the house she was taken to. An 11 year old girl disclosed to her mother that a teacher of her school promised to give her a new house to live in and took her to visit this new house during school time. She claimed that she was shown a beautiful house and there she was given food and drinks. Her illiterate mother who is not legally married and has no income or a proper place to live, believed this story because school teachers have been helping them throughout in various ways. But her partner did not believe this story and insisted that the mother go and meet the teacher. The mother went to see the teacher to thank her for trying to help them. The teacher was surprised to hear the story and started to probe in to it. Then the girl revealed that on the way to school she met a man and a woman in a van, who promised to gift her a house to live, and had taken her by van to a house where there were several naked foreign women. She claimed that she was given a meal of fried rice and a drink of lemon juice after which she felt sleepy and they helped her by giving a comfortable bed to sleep. When she woke up she was brought back and dropped near the school by the time the school was over. She claimed that the man and woman asked her to tell the mother that it was a teacher who took her to show the house. According to her the incident happened twice. She gave a detailed description of the house, people who were there and the meals she was given. Then the school authorities contacted the police due to a suspicion of child abuse. Similar detailed description of the incident was given to the JMO and the police repeatedly by The girl attended psychiatric assessment with her mother. Mother agreed that they were desperately looking for a better place to live. She also revealed that the food and drink the child claimed to have been served by those who took her away were her favorites. The school attendance was checked and she was found to have 100% attendance during that particular school term. At the end of the assessment, the mother produced an exercise book with the child’s handwriting. As there were “hearts” drawn everywhere in the book, the mother thought it was not a school book. The psychiatrist found seven romantic letters which were addressed to the girl, and sent by seven different males judging from the names of the sender. All were of the girl’s handwriting and on confrontation she agreed that she wrote them as if boys were writing to her. There were drawings of a sexual nature in some of her school books as well. At the end of the psychiatric assessment it was concluded that the child’s story was a fantasy. Discussion The law presumes that a history given by a child is true. Therefore it is important to evaluate the credibility of the history given by a child. A false history given by a child may lead to unnecessary investigations by the doctors, police and law 36 enforcement personnel and may lead to the conviction of an innocent person and also destroy the family especially when the accused is a parent [6]. Children usually have fantasies; preschoolers have more fantasies [2]. With age their fantasy may reduce, but school going children also have a rich fantasy life. During early adolescence fantasies of romantic and erotic nature appear. Frequency of the occurrence is not clearly known. Most children’s fantasies are selflimited. Few reveal them in various ways. Some children colour their stories with their fantasies and experiences. Those who are craving for love and attention are more likely to tell stories coloured by fantasies [3]. Fantasy prone personality (FPP) is a disposition or personality trait in which a person experiences a lifelong extensive and deep involvement in fantasy [3]. An individual with this trait (termed a fantasizer) may have difficulty differentiating between fantasy and reality. A fantasy prone person is reported to spend a large portion of his or her time fantasizing, have vividly intense fantasies, have paranormal experiences, and have intense religious experiences [4]. The fantasies may include dissociation and sexual fantasies. Fantasizers have had a large exposure to fantasy during early childhood [3,5]. This overexposure to childhood fantasy has at least three important causes: Parents or caregivers who provided a very structured and imaginative mental and/or play environment, exposure to physical and/or sexual abuse, such that fantasizing provides a coping or escape mechanism from the abuse and exposure to severe loneliness and isolation, such that fantasizing provides a coping or escape mechanism from the boredom. Regarding psychoanalytic interpretations, Sigmund Freud has stated that "unsatisfied wishes are the driving power behind fantasies, every separate fantasy contains the fulfillment of a wish, and unproves an unsatisfactory reality." This shows loneliness and dissatisfaction in life and can result in people creating a fantasy world of happiness in order to fill the void. Young children who once were treated for abuse and had a parent leave created a world of fantasies to escape from reality [1]. It is not a psychiatric illness and there is no treatment or therapy required. This case report reveals the importance of suspecting the possibility of fantasy when an unusual story without supporting evidence is given by a child. The introduction of psychiatric testimony intended to impeach the child`s credibility will be helpful in this type of case where substantial corroboration supporting the charge is lacking. In order to justify the admissibility of mental health evidence, courts should identify specific and legitimate relevance to the complainant`s credibility [6]. This should be balanced against the potentially misleading and confusing effect that the information will have on the fact finding procedure. In some states of America a psychiatric evidence of credibility of sexual assault complainants are adopted but no state has adopted a coherent approach that considers mental health as a category [6]. References 1. Roy Meadow, Jacqualine Mak, Donna Rosenberg, ABC of child’s protection. 4th Edition Blackwell publishing 2007 P - 6. 2. Taylor M, Carlson SM, Maring BL, Gerow L, Charley CM. Department of Psychology, University of Oregon, Eugene, OR, USA. [email protected]. Pub Med – indexed for Medicine. 37 3. Lynn, Steven J., and Judith W. Rhue (1988). Fantasy Proneness: Hypnosis, developmental antecedents, and psychopathology. American Psychologist, vol. 43, pages 35 - 44. 4. Merckelbach, H. et al. (2001). The Creative Experiences Questionnaire (CEQ): a brief self-report measure of fantasy proneness. Personality and Individual Differences, vol. 31, 987-995. 5. Rhue, Judith W., and Steven Jay Lynn (1987). "Fantasy Proneness: Developmental Antecedents." Journal of Personality, vol. 55, 121 – 137. 6. Cossins, A. (1999) 'Recovered Memories of Child Sexual Abuse: The Science and the Ideology' in J. Breckenridge and L. Laing (eds) in Australian Perspectives on Violence against Women, Allen & Unwin: Sydney. Contribution of authors Examination of the patient-JW Opinion- JW,CH Writing the manuscript –JW, CH Revising the manuscript- CH 38 Ravindra Fernando Department of Forensic Medicine and Toxicology, Faculty of Medicine, Colombo Appreciation m Professor H. V. J. Fernando – A tribute MLJSL. Vol 2. No 2. Dec. pp 39 – 42 Dr. Fernando could not enter the MD programme in the UK without a primary British medical degree. Therefore, to obtain MBBS of the University of London, he was attached for two years to the School of Medicine, University of Leeds, as an External Student. During this period he also worked part time with Professor Matthew Stewart, Professor of Pathology of the University. On 1st April 1919 a child was born to wealthy parents, Henry Domingo Fernando and Vivienne Muriel Fernando (nee de Mel), who was destined to become an intelligent doctor, a great academic, a teacher par excellence, a true friend, a faithful colleague and a great humanist. He was named Hubert Vernon Jerrold. He was a brilliant student at Royal College, Colombo and entered the University College, Colombo, in 1937 and the Medical College of the University of Ceylon in 1938. In 1943, he passed MBBS (Ceylon) with Second Class Honours. From 1943 to 1947 he worked as a medical officer in the Department of Health Services serving as a House Officer to the Professor of Medicine and in the Department of Pathology. He then worked at the Medical Research Institute, Colombo and as a pathologist in the Civil Hospital, Kandy. He resigned from this post in July 1947 to proceed to the United Kingdom to pursue higher studies. He passed M.B.B.S. (London) with ease in 1949 and was appointed as Demonstrator in the Department of Pathology of the King’s College Hospital Medical School, London. He took part in the routine work of the Department and the teaching. In June 1952, he obtained MD (London) in Pathology with Morbid Anatomy as his special subject. After his MD, he worked with Dr. Keith Simpson, then a Home Office Pathologist and a Reader in Forensic Medicine, at Guy’s Hospital Medical School, University of London. He also spent some time in the Biological Laboratories of Scotland Yard learning their crime investigating techniques. After returning to Ceylon in October 1952, he joined as a Pathologist of the Colombo Group of Hospitals. On 13th February 1953 after Dr. Fernando’s selection to the University of Colombo, Professor G.S.W. de Saram, the first Professor of Forensic Medicine, wrote to the University 39 stating that “Dr. Fernando be appointed on the maximum salary of a Grade 2 Lecturer and be stepped up to Grade 1 a year later, because he has obtained the highest degree in his specialty and has also acquired practical knowledge of medico-legal work under Dr. Keith Simpson who is one of the leading consultants to Scotland Yard. Dr. Simpson’s high opinion of Dr. Fernando has already been submitted to the Selection Committee”. On 4th March 1953 Sir Ivor Jennings, the Vice- Chancellor appointed him to the lecturer post in the Department. After the retirement of Professor de Saram in May 1958, he had been the acting Head of the Department of Forensic Medicine, and he was responsible for the administrative work of the Department. Dr. H. V. J. Fernando was appointed the second Professor of Forensic Medicine on 10th July 1959. In 1961, Professor Fernando took one year sabbatical leave and proceeded to London and was successful in the Barrister’s examination of the Lincoln’s Inn of the Inns Court, London. However, he was not called to the bar due to inability to “keep dining terms” – a traditional requirement before a student is called to the bar at the Inns of Court. During his sabbatical leave, he visited medicolegal institutions at London, Sheffield, Leeds, Edinburgh, Glasgow, Cambridge, Cardiff, and Copenhagen. In January 1962, the Asia Foundation awarded a grant to Professor H. V. J. Fernando to visit the medico-legal institutions at New York, Connecticut, Washington, Chicago, Los Angeles and San Francisco in the USA. Later he visited the All India Institute of Medical Sciences to attend a WHO conference on “Evaluation Methods in Medical Teaching”. He has also visited Turkey and the Federal Republic of Germany to attend conferences. Participating in professional activities with dedication, Professor Fernando served as the President of the Medico-Legal Society of Sri Lanka in late seventies. He was the President of the Sri Lanka Cancer Society and served the Society with dedication. His professional colleagues included Drs. W.D.L. Fernando, Chandra Amarasekera, Dr. Haris Ranasinghe, Dr. C. H. S. Jayawardene, Dr. N. Saravanapavananthan and Dr. S. Sivaloganathan. Professor Fernando always wrote very favourable reference letters to his juniors and also kept in touch with them when they went on study leave. He had many friends in the international forensic scene. Some of them were Professor Donald Teare, Professor of Forensic Medicine at St. George’s Hospital, London, Dr. H. P. Terfloth, Institute of Forensic Medicine, University of Munchen, West Germany, Dr. J. M. Cameron, the Professor of Forensic Medicine at the London Hospital, Dr. Tom Noguchi, Chief Medical Examiner and Coroner for the County of Los Angeles, who was known as the "coroner to the stars", as he determined the causes of death in many high profile cases such as Marilyn Monroe, Robert F. Kennedy, Sharon Tate and Natalie Wood, Dr. W. G. Eckert and Dr Milton Helpern of the USA. A keen and dedicated teacher in the Faculty of Medicine, Colombo, he held the post of Chairman of the Centenary Celebration Association of the Faculty in 1970. He was the Founder Chairman of the Statistical Unit of the University of Ceylon. In 1982, he became the Registrar of the Ceylon Medical Council when Professor Milroy Paul retired, and served in this position till 1994. During this period he compiled “An Index of Important Decisions of the Medical Council from 1948 to March 1996”, and “Legislation relating to the Sri Lanka Medical Council formerly Ceylon Medical Council”, which 40 included a “Summary of Legislative Enactments from 1905”. He was the first Chairman of the Board of Study in Forensic Medicine in the Post Graduate Institute of Medicine, which commenced the postgraduate training in Forensic Medicine in Sri Lanka. He was responsible for the initial spade work of the Board to prepare the training programme and conducting the first couple of post graduate examinations. Professor Fernando was consulted by the Attorney General’s Department and the private bar for expert opinion in difficult cases and many eminent legal professionals visited him at his residence for expert opinion. He performed the post mortem examinations of Mrs. Padmini Kularatna of Galle, who died of arsenic poisoning. In the well known Getangama murder case in Ratnapura, where a man murdered and hanged his wife with the help of his mistresses, Professor Fernando was requested by the Attorney-General’s Department to advice on the post mortem findings of Dr. D.J. Bandara and Dr. Saravanapavananthan, who did the first and the second postmortems respectively. In 1960s excavations at the site of Dakkina Thupa, Anuradhapura, were recommenced by Professor Senarath Paranavithana and when the ashes were recovered from the basement of Dakkina Thupa, which was believed to be of king Dutugemunu, they were sent to Professors H V J Fernando for expert opinion by the archaeologists. When he was in King’s College he contributed an article on “Pulmonary Aspergillosis Following Post-influenzal Bronchopneumonia Treated with Antibiotics” with J. D. Abbott, K. Gurling, and B. W. Meade to the prestigious British Medical Journal in 1952. Only very few Sri Lankans are fortunate enough to get an article published in the prestigious British Medical Journal. Professor Fernando’s other publications include “Forensic aspects of post-maturity” in the Ceylon Medical Journal in 1957, “Distribution of A-B-O and M-N blood groups among the Ceylonese, their Significance in Forensic Work” in the Ceylon Journal of Medical Sciences in 1958, and “Survival after penetrating injury of the heart” with Dr. C. Mylvaganam, in the Journal of Forensic Medicine in 1959. He presented several scientific papers with other colleagues. For example with Chandra Amarasekera, N. Saravanapavananthan and others he read papers on “Socio-medical aspects of road traffic accidents in Colombo” and “An epidemiological study of intentional violence in Colombo” at the Annual Scientific Sessions of the Sri Lanka Medical Association in 1979. A very useful publication of Professor Fernando was “Injuries and their legal definition” with Consultant Surgeon Dr. A. Thavendran, Chief Justice H.N.G. Fernando, and eminent lawyer Eardley Perera in the Journal of the Colombo General Hospital in 1973. Another joint publication with Chief Justice H.N.G. Fernando, Dr. Chandra Amarasekera and Dr. N. Saravanapavananthan and others was on “Hurt in relation to the Ceylon Penal Code” in the Sri Lanka Police Journal in 1974. In 1984 Professor Fernando and I submitted a paper on "Examination and reporting of victims of assault to Police and Courts in Sri Lanka” for the Tenth Meeting of the International Association of Forensic Sciences, held in Oxford, England. The abstract of this article was published in the Journal of Forensic Science Society. In September 1984, Professor Stanley Wijesundera, the then Vice Chancellor of the University wrote to Professor Fernando about his impending retirement stating that he would like to make special mention of the invaluable counsel and support given to him during his tenure of office as Vice Chancellor. 41 I wish to quote a sentence from Professor Fernando’s reply. “I have always felt that loyalty is an important part of any service and I have tried to live up to it”. A profound statement to be made note of! In 1944 young Dr. Fernando married Marie Constance Gwendoline Philip, a daughter of Dr. B.D.H. Philip from Kaluthara. Their son Nirmal and daughter Marina became accountants but one of his grand daughters, Sahani, is now a Consultant Anaesthetist in the USA. He retired on 31st December 1984 and the Senate of the University elected him Emeritus Professor on 12th September 1985. After a fruitful academic and social life Professor Fernando passed away peacefully on 2nd May 1998. 42
© Copyright 2026