Annual Work Plan 2015
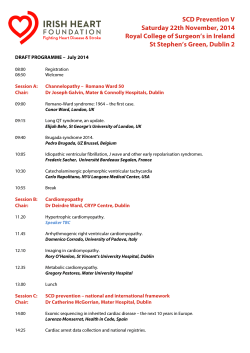
SHIKURI PROJECT ANNUAL WORKPLAN 2015 Vision: The Shikuri Project envisions the establishment of sustained, Sickle-Cell diagnostic and treatment Centres serving communities with high -prevalence and lack of access to national programmes in East Africa. Mission: The Shikuri Project exists to introduce and implement sustainable, Chronic Health Care Management (CHCM) programmes to reduce the number of deaths and painful crises suffered by young children with Sickle Cell Disease, in underserved communities in Kenya, and eventually East Africa. Overall Objective: Establish Pilot Programme, integrating and implementing 4 elements of WHO’s Strategy for Sickle Cell Disease in Africa and Advocacy deliverable in underserved communities of Western Kenya and Coast Province regions Responsible Activities Timeframe Indicators Shikuri Project employees and volunteers. County Community Health Workers and healthcare providers in community health centres and hospitals Means of Verification Resources Objective 1: To advocate for routine early Identification and screening of newborns and improved care of cases of Sickle Cell Disease/Sickle Cell Anaemia Conduct an assessment of the magnitude of CSD/SCA in Nov 2014 – March 2015 Nyanza and Western Shikuri Team CHMT Study Team Study report available Shikuri $10,000 provinces This study is intended to provide a rational and evidence based information for initial population estimates to inform recommendations on the provision of care continuum defined by level from community to all referral levels. 1.1.1 Identify study team 1.1.2 Finalise the study TOR 1.1.3 Conduct the study 1.1.4 Present study findings and recommendations 1.2 Develop Project Budget based on inception report October 2014 October 2014 Nov. 2014 – Feb 2015 End Feb 2015 X X X X X Comment [GS1]: 1.1 Deliverables 1. A comprehensive literature review of SCD/SCA in Kenya with focus on Western Kenya 2. Estimation of children with SCD in Western Kenya extrapolating the numbers for Homabay and Kakamega Counties 3. Recommend appropriate systems to enable early recognition, diagnosis and treatment continuum of sickle cell disease and as to close to communities as possible with reference to findings on health facilities at tiers 1?2-5 in Goal 2 above. 4. Outline current best care practices for SCD in communities, schools and health facilities 5. Generate a data base on: i.No of centres by comparative capacities and capabilities in diagnosis and treatment of SCD ii.Estimated no of patients with SCD iii.Estimates of typical syndromic presentations (crises) and comorbidities with: a.Malaria and/or b.Pneumonia and/or c.Malnutrition and/or Other 1.3 Prepare advocacy materials/messages 1.4 Sensitise/orient County Health Management Teams and Leadership March 2015 1.5 Conduct community awareness in targeted counties. March – June 2015 Onsite Project team March 2015 MOU or joint workplan signed with County /sub county public health officials and Shikuri Project 1.6 Advocate for inclusion of SCD interventions in in County and Sub County District workplans for 20162017 planning cycle ? Project Coordinator /team District workplan which incorporates SCD for 2016 Objective 2: Improve care of existing cases of SCD/SCA at County Level 2.1 In two counties of Homa March – June Bay and Kakamega, train 2015 health providers and update their knowledge and skills on SCD/SCA (initial X focus on two sub-counties in each county) 2.2 As part of 2.1, prepare and distribute learning and caregiver/parental education materials to health workers on SCD/SCA 2.3 Provide free and/or affordable medicines and essential supplies to targeted health facilities including: Penicillin prophylactics; Folic Acid; Pain medication; Hydration (ORS/ORT); Hydroxy Urea (to limit mortality and risk of strokes from low HGB); Antibiotics; Anti-Malarials; Thermometers Feb – June 2015 Xxx X JuneDecember 2015 X 2.4 Improve supportive supervision to targeted subcounties and health facilities 2.5 Monitor stock-outs of supplies and commodities in targeted sub-counties and health facilities March – December 2015 X March – December 2015 X 2.6 Introduce/pilot screening test for SCD and point of care test for June – Dec 2015 X This may include collaboration anaemia. This may include with collaboration with USA/NIH USA/NIHObjective 3: Improve community level awareness, syndromic diagnosis or screening of SCD and care/referral of cases. 3.1 Prepare learning materials for community health workers on SCD/SCA. 3.2 Print and distribute SCD/SCA CHW learning materials. 3.3 Identify/develop appropriate screening package for use at level 1 (community), 2 and 3 3.4 Identify target Communities (est 1,000 under 18 patients) for piloting community level sickle cell disease activities in 4 sub counties ( 2 each in Kakamega, 2 Homa Bay) Identifying partner clinics/hospitals March – June 2015 X June 2015 X March 2015 June – Dec 2015 3.5 Develop and March – Dec disseminate communication 2015 messages for public education and awareness X X X X X 3.6 Training/orient CHWs in X the care (home care, early referral) of SCD/SCA. Objective 4: Support counties to undertake newborn screening as part of district health package at community (1), dispensary (2), and Health Centre levels (3) 4.1 Share experiences from Feb – March ? other countries 2015 4.2 Develop policy June – Dec Shikuri Project guidelines on newborn 2015 collaboratively with CHWs screening within maternalnewborn care package 4.3 Adapt/develop newborn June Dec 2015 X screening protocols 4.4. Develop operational 2016 Shikuri Project collaboratively plan for screening newborn with CHWs screening in two sub counties, with target of 1000 OR 500 (anyone with family history, ) New Objective 6 : Infant diagnosis campaign conducted with Measles Vaccination Programme 2016 CHWs 4.6 Disbursement of family X stipends Objective 5: Surveillance: (i) Establish Cohort to capture data on Reduced Mortality/ mortality rates to highlight efficacy of interventions; capture the burden of disease due to Sickle Cell Anaemia (SCA). (ii) capture estimates on typical syndromic presentations (crises) and comorbidities with: Malaria and/or Pneumonia and/or Malnutrition and/or Other critical health variables 5.1 Elaborate computerized X data collection system in all facilities we operate in 5.2 Train data entry and analysis staff X 5.3 Objective 6: Improved coordination of partners involved in care of SCD/SCA patients 6.1. Map out all partners involved SCD/SCA in Kenya and other East African countries 6.2 Establish/strengthen coordination of partners – forming a stakeholders’ forum orassociation 6.3 Produce SCD newsletter 6.4 Hold Annual SCD meetings Nov-February 2015 X June 2015 X June 2015 Annually X X SAMPLE MULTI-PARTNER PROJECT FRAMEWORK (to be added to Workplan) Reducing Infant Mortality from Sickle Cell Disease in Homa Bay, Western Kenya Programme Deliverable Lead Partner 1. Systems established to provide sustainable, routine Early Identification and Screening Of newborns for SCD. (i) Syndromic Diagnosis and referrals at community level to district level Shikuri Project (Per our workplan we are to (ii) Neonatal screening of Shikuri project cohort at hospital level (IEF) at MOI Univ/Teaching Hospital; Homa Bay District Hospital, Webuye County Hospital and 1. Develop operational plan for screening newborn screening in two sub counties, with target of 1000 (anyone with family history 2. Conduct Infant diagnosis campaign in tandem with Measles Vaccination Programme AMPATH 2. SSA Surveillance System Initiated. MOI Univ/Teaching Hospital Study on SCA and prophylatic treatment in Homa Bay - Comment [m3]: Why append to measles campaigns and not just stick to above proposal for simplicity and sustainability? Shikuri Project Other (i) Comment [m2]: Retain this for children attending antenatal clinics and health facilities as a screening process for high risk. Suspect cases have blood taken for IEF electrophoresis at Moi Teaching.. Neonatal screening subsequently instituted longitudinally in families with identified cases Comment [m4]: Yes. Establish firm partnership since Ampath done as a research project rather than long term service that Shikuri wishes to undertake. Ampath would be a great joint researching/health worker training partner. The infrastructure would then be ideal for trying out of new innovations. Including larger cohort on hydroxyurea with outcome documentation besides TCD work and long term side-effects/safety in children. (ii) Surveillance: (i) an estimate of mortality rates to highlight the burden of disease due to Sickle Cell Anaemia (SCA). (ii) Findings and estimates on Shikuri Project Comment [m5]: Correct. We will need elaborate computerized data collection system in all facilities we operate in with trained data entry and analysis staff. Ampath may be willing to train the staff on entry and analysis. We will also need good social worker follow-up system to help monitor treatment compliance and referral support. We could consider registering needy clients on National Social health insurance fund which is pretty inexpensive and allows free hospital treatment. We could explore how cost-sharing and sustainability for annual premiums would happen. Process documentation on the processes evolving as we grow would form excellent scientific publications in Health Services Research journals to share experiences with others. Duke University/ AMPATH Comment [m6]: There is a global program on Access to Free drugs for developing countries needy that we could research more on. All free is not good hence need to devise way of getting them to pay minimal to value the service..free is taken for granted, not valued and could be abused! . Paper attached suggests blood counts alone would be justifiable in service for all but maybe study sample for more detailed tests on side-effects to inform service as part of applied research. typical syndromic presentations (crises) and comorbidities with: Malaria and/or Pneumonia and/or Malnutrition and/or Other critical health variables. (iii) additional research on the impact of ongoing initiatives which have resulted in reductions in infant mortality, including national malarial control programmes, Haemophilus influenzae type b; free access to insecticide-treated bed nets for children and pregnant women (to which major declines in malaria incidence have been attributed54) 10-valent conjugate vaccine against Streptococcus pneumonia 3. Free and/or affordable or free medicines provided to beneficiary group to prevent death, complications, reduce morbidity and suffering. (i) Hydroxy Urea: (ii) Other meds/supplies: See Shikuri Proj workplan Govt of Kenya 4. Chronic SCD health care management provided and integrated into local and community health- care system . MOI Univ/Teaching Hospital (i) Health worker training: Shikuri Project See Shikuri Proj workplan Comment [m7]: Role of paludrine, and folate in malaria prophylaxis not well studied and we could get important information. Papers on possible benefit of relative iron deficiency also interesting and could be studied. Comment [m8]: delete Comment [m9]: This section in my view should be devoted to Health Worker Training. Shikuri Project (II) Other elements: to build and/or enhance the See Shikuri Proj workplan capacity of community practitioners, comprehensive treatment (mobile?) centers accessible to the target populations, and interventions adaptable to the local needs of communities. The comprehensive treatment centers will provide: comprehensive (including emergency care); provision of medications, including anti-malarials, hydration; administration of specific vaccines; continuous medical follow-up; early detection and management of complications including fevers; patient referral to highercare centres when necessary; and - of paramount importance - parent/ care giver and patient education and counselling in the foregoing. This output will also create or enhance the capacity of a cadre of community Health practitioners with training in SCD control including prevention, diagnosis and management of cases. (ii) 5. Increased awareness and knowledge of SCD as well as Shikuri Project visibility on the public health agenda by community and KSCF national stakeholders (e.g., Community Health Committees in Others target counties) Comment [m10]: Work with Media and County governments as primary partners – religious leaders etc to educate and promote referals.
© Copyright 2026