Clinical Approach to Altered Serum Sodium levels
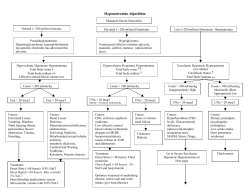
SPECIAL ARTICLE JIACM 2006; 7(2): 91-103 Clinical Approach to Altered Serum Sodium levels Ashish K Duggal*, Pushpa Yadav**, AK Agarwal***, BB Rewari**** Disorders of sodium and water balance are very common and are seen in the emergency department almost every day worldwide. Sodium is the principal solute in the extra cellular compartment and hence the plasma osmolality largely depends on the serum sodium concentration. Plasma osmolality in turn is regulated tightly within a narrow range of 275 - 290 mosm/kg by various mechanisms. A decrease or increase in the serum sodium level will have an effect on the plasma osmolality and this can have deleterious effects on the whole body – in particular, the central nervous system. Severe hypo- and hypernatraemia are associated with significantly high mortality and morbidity. Moreover, inappropriate treatment may result in treatment related complications such as osmotic demyelination syndrome. This article discusses the pathophysiology and management of both hyponatraemia and hypernatraemia with special emphasis on preventing treatment related complications. Hyponatraemia Hyponatraemia is defined as a decrease in the serum sodium concentration to a level below 136 mmol/l. Although plasma osmolality is closely related to serum sodium concentration, hyponatraemia can be associated with low, normal, or high osmolality1. Osmolality or tonicity refers to the contribution to osmolality of solutes such as sodium, glucose, and urea that cannot freely move across the cell membrane thereby reducing transcellular shifts in water2. Plasma osmolality can be measured by osmometry, or can be calculated by the following formula3: in the otherwise relatively impermeable section of the nephron5. Thirst is another crucial but less sensitive mechanism for maintaining plasma osmolality. Furthermore, because the cell membranes are freely permeable to water, all body fluids are in osmotic equilibrium. As a result, plasma sodium concentration not only reflects the plasma osmolality but also the intracellular osmolality. Any change in the serum sodium concentration not only changes the tonicity of the extracellular fluid, but also causes water to shift into or out of cells as the tonicity of the two compartments equilibrates. This shift has important implications because the CNS manifestations of hypo- and hypernatraemia are the result of these water fluxes3. Hyponatraemia is the most common electrolyte abnormality found in hospitalised patients3. It has an incidence of around 1% and the frequency increases with increasing age6. In acute (< 48 hrs) and symptomatic hyponatraemia, the mortality rates may be as high as 17.9%7-9. Hyponatraemia is more commonly caused by an excess free water rather than sodium depletion. There is convincing evidence that hyponatraemia is not only a marker of serious underlying disease, but when severe, can itself be the cause of major neurologic damage and death7, 10. Classification of hyponatraemia Hyponatraemia can be classified according to the plasma osmolality into hyperosmolar, iso-osmolar and hypoosmolar states. Table I lists the various causes of hyponatraemia according to the classification3, 11. Posm = 2 [Na](meq/l)+ [glucose] (mg/dl) + BUN (mg/dl) 18 2.8 Table I: Causes of Hyponatraemia Plasma osmolality is preserved within the normal range by the hormone arginine vasopressin, also known as the antidiuretic hormone (ADH). Osmoreceptors near the hypothalamus sense plasma osmolality and modulate vasopressin release4. Vasopressin functions at the distal collecting duct of the kidney to increase water reabsorption Hyperosmolar Hyponatraemia Hyperglycemia Hypertonic mannitol Iso-osmolar Hyponatraemia Pseudohyponatraemia Post-TURP Hypo-osmolar Hyponatraemia * Medical Officer, ** Senior Physician and Associate Professor, *** Consultant, Professor and Head, **** Senior Physician and Assistant Professor, Department of Medicine, Dr RML Hospital, New Delhi - 110 001. Hypovolaemic Hyponatraemia Renal sodium loss Diuretic agents Osmotic diuresis (glucose, urea, mannitol) Adrenal insufficiency Salt-wasting nephropathy Bicarbonaturia (renal tubular acidosis, disequilibrium stage of vomiting) Ketonuria Extra-renal sodium loss Diarrhoea Vomiting Blood loss Excessive sweating (e.g., in marathon runners) Fluid sequestration in “third space”, i.e., – Bowel obstruction – Peritonitis – Pancreatitis – Muscle trauma – Burns Hypervolaemic Hyponatraemia Congestive heart failure Cirrhosis Nephrotic syndrome Renal failure (acute or chronic) Pregnancy Euvolaemic Hyponatraemia Thiazide diuretics Hypothyroidism Adrenal insufficiency Syndrome of inappropriate secretion of antidiuretic hormone Cancer Pulmonary tumors Mediastinal tumors Extrathoracic tumors Central nervous system disorders Acute psychosis Mass lesions Inflammatory and demyelinating diseases Stroke Haemorrhage Trauma Drugs Desmopressin, oxytocin, prostaglandin-synthesis inhibitors, nicotine, phenothiazines, tricyclics, serotonin-reuptake inhibitors, opiate derivatives, chlorpropamide, clofibrate, carbamazepine, cyclophosphamide, vincristine Pulmonary conditions Infections 92 Acute respiratory failure Positive-pressure ventilation Miscellaneous Post-operative state Pain Severe nausea Infection with the human immunodeficiency virus Decreased intake of solutes Beer potomania Tea-and-toast diet Excessive water intake Primary polydipsia Dilute infant formula Hyperosmolar hyponatraemia Hyponatraemia can occur with increased plasma osmolality (> 290 mosm/kg) as a result of increased concentration of an effective solute in the extra-cellular fluid compartment. This creates an osmotic gradient that drives water from the cells into the extra cellular space leading to a lower, diluted sodium concentration. This can be seen in severe hyperglycaemia during uncontrolled diabetes. Quantitatively, the measured sodium decreases approximately 1.5 meq/l for every 100 mg/dl rise in serum glucose concentration12. This formula is based on the presumption that the volume of distribution of glucose is 45% of the total body water. But in many patients admitted in the hospital, the body composition may be altered and this formula cannot be used. The following formula is a more generalised formula to predict changes in serum sodium12: Change in sodium = 5.5 (1 - V)/2 C change in glucose where V is the volume of distribution of glucose as a fraction of total body water. Less common causes of hyperosmolar hyponatraemia include hypertonic mannitol, sorbitol, maltose and radiocontrast administration13, 14. This is also known as translocational hyponatraemia. Iso-osmolar hyponatraemia Hyponatraemia can occur with a normal plasma osmolality (275 - 290 mosm/kg). This occurs as a result of either pseudohyponatraemia, by massive absorption of irrigant solutions that do not contain sodium, as during transurethral resection of the prostate, and by accumulation of cations in the extracellular space other than sodium. Journal, Indian Academy of Clinical Medicine Vol. 7, No. 2 April-June, 2006 Pseudohyponatraemia is a laboratory artefact and occurs with severe hypertriglyceridaemia and paraproteinaemia. It occurs because the large non-aqueous molecules such as lipids or proteins occupy a greater proportion of the serum and there is a corresponding decrease in total sodium content per unit volume of serum. This is a laboratory artefact, which is now fairly obsolete with the use of modern instruments that use sodium ion specific electrodes15. Irrigating fluids used during TURP and endoscopic hysterectomies are hypotonic or isotonic glycine, mannitol, or sorbitol16, 17. Hyponatraemia is caused primarily by retention of near-isotonic fluid in the extracellular space. The plasma osmolality may be normal in case of isotonic solutions such as 5% mannitol, or hypo-osmolar if the solution used is hypotonic such as 1.5 percent glycine or 3.3% sorbitol11. Whether the symptoms derive from the presence of retained solutes, the metabolic products of such solutes, hypotonicity, or the low serum sodium concentration remains unclear17. Hypo-osmolar hyponatraemia Most cases of hyponatraemia are associated with a low plasma osmolality (< 275 mosm/kg) reflecting a net gain of free water3. Patients can be classified according to the total body volume state of the patient. Hypovolaemic hyponatraemia occurs when there is loss of both water and sodium, but sodium loss exceeds that of water. As a result of hypovolaemia, vasopressin release and the thirst mechanism are activated leading to increased water retention, thus further aggravating the hypo-osmolar state. Causes of water and sodium loss could be: with diuretic use, but does not require a change in therapy. Few patients, particularly elderly females who are volume depleted are at greater risk of developing severe hyponatraemia20, 21. It typically develops within three days to three weeks of initiation of therapy22. Multiple mechanisms are involved in the pathogenesis of diuretic-induced hyponatraemia. Diuretic-induced volume depletion impairs renal diluting capacity and diuretics block reabsorption in the thick ascending limb in the loop of Henle21. Diuretic-induced hypokalaemia and hypomagnesaemia may also contribute to hyponatraemia23. 2. Extra-renal causes include: loss of sodium and water from the gut as in diarrhoea and vomiting, or third space collection as in severe burns, pancreatitis, and peritonitis. In this case, sodium and water loss causes both water and sodium reabsorption by the kidneys, but the amount of water reabsorbed is more than the amount of sodium reabsorbed because of the baroreceptormediated ADH release and decreased GFR, and increased proximal tubular reabsorption because of hypovolaemia. So there is a relative deficiency of sodium24. Euvolaemic hyponatraemia occurs when there is free water gain and negligible sodium loss. These individuals make up the largest single group of hospitalised hyponatraemic patients7. In these cases, there is either decreased water excretion or increased water intake. Causes include: b. Hypoaldosteronism. 1. Adrenal insufficiency. Hyponatraemia in primary adrenal deficiency is related both to hypocortism and hypoaldosteronism. The water retention is primarily ADH dependent which is related to reduction in blood pressure and cardiac output. ADH secretion may also be directly increased by CRH secretion, which is also increased in primary adrenal insufficiency25, 26. c. 2. Hypothyroidism27. 1. Renal causes, which include: a. Salt wasting nephropathies such as polycystic kidney disease and chronic pyelonephritis in which there is loss of sodium in excess of water. Use of thiazide diuretics. Although thiazide diuretics are not the most common cause of hyponatraemia7, 18, 19, they are the most common causes of severe symptomatic hyponatraemia causing neurological sequelae 20, 21. Mild asymptomatic hyponatraemia frequently occurs Journal, Indian Academy of Clinical Medicine 3. Syndrome of inappropriate ADH secretion (SIADH), the most common cause of hyponatraemia in hospitalised patients7. Vasopressin is released from the posterior pituitary or an ectopic site inappropriately resulting in decreased free water excretion. In SIADH, there is no Vol. 7, No. 2 April-June, 2006 93 overt hypervolaemia inspite of water retention because only one-third of the water is distributed in the extracellular space. However, there is a modest expansion of the intravascular volume, which results in an increased RPF and GFR. It also results in reduced proximal tubular absorption of sodium, which further contributes to hyponatraemia. Once a steady state is reached, urinary sodium excretion becomes equal to dietary sodium intake28. Diagnostic criteria of SIADH are3: a. Hypo-osmolar hyponatraemia b. Clinical euvolaemia c. Inappropriately concentrated urine > 100 mosm/kg d. Normal adrenal, cardiac, thyroid, hepatic and renal functions. Causes of SIADH can be categorised into four major groups: malignancy, pulmonary disease, CNS disease and pharmacological use (Table I) 3,11. 4. Psychogenic polydipsia or compulsive water drinking is found predominantly in the psychiatric population, particularly in individuals with schizophrenia. These patients often drink over 15 lit of water a day, overwhelming their kidneys’ maximum capacity to excrete free water. This leads to dilutional hyponatraemia with urine osmolality less than 100 mosm/l29. 5. Reset osmostat is a chronic condition where vasopressin osmoreceptors have a lower threshold to trigger vasopressin release. This has been associated with quadriplegia, psychosis, tuberculosis, and chronic malnutrition30. 6. Beer potomania is seen in chronic alcoholism. Chronic alcoholics, who already have low dietary sodium and nutritional stores, ingest large quantities (4 - 5 l) of low sodium beer with minimal food intake, can have hyponatraemia. Although the kidneys produce maximally dilute urine, the amount of daily dietary solute intake is so low that the kidneys are unable to maintain isoosmolality leading to water retention and hyponatraemia31. Hypervolaemic hyponatraemia: Here free water gain exceeds sodium gain, resulting in hyponatraemia. This is 94 seen mainly in the setting of increased total body water as occurs in oedematous states such as CHF, hepatic cirrhosis, nephrotic syndrome, and renal failure. In these conditions, although the total body water is increased, the effective arterial volume is decreased. Intravascular volume depletion triggers secretion of ADH, renin-angiotensin, norepinephrine, and thirst. So the intake and retention of water exceeds the intake of sodium leading to dilutional hyponatraemia3. Clinical features The signs and symptoms of hyponatraemia depend not only on the absolute serum sodium levels but also on the rate of serum sodium decline 32. While chronic hyponatraemia defined as hyponatraemia for more than 48 hrs may be asymptomatic, acute hyponatraemia of duration < 48 hrs, may result in severe neurological dysfunction28. Those at extremes of age are less tolerant to hyponatraemia. Symptoms of hyponatraemia are listed in Table II32, 33. Table II: Clinical features of hyponatraemia. Serum sodium > 125 mmol/l: Usually asymptomatic Serum sodium 120 - 125 mmol/l: Gastrointestinal: Anorexia Nausea Vomiting Serum sodium < 120 mmol/l: Neuromuscular: Muscle cramps Generalised weakness Seizures Neurologic: Confusion Disorientation Agitation Delirium Lethargy Stupor Serum sodium < 110 mmol/l: Seizures Coma The neurological manifestations are most likely related to Journal, Indian Academy of Clinical Medicine Vol. 7, No. 2 April-June, 2006 diffuse cerebral oedema, which results from movement of water from extracellular fluid into brain cells. In severe cases, death can result from tentorial herniation and brain stem compression32. Brain adaptation to hyponatraemia During hyponatraemia, the brain cells exposed to hypotonic plasma swell because fluid shifts into the brain cells resulting in cellular swelling. The swelling occurs within the confines of the rigid skull leading to reduction in cerebral blood flow. The early adaptation of the brain cells to hyponatraemia is by loss of water into the CSF. This is followed by extrusion of sodium and potassium from the brain cells. This constitutes the early adaptive response34, 35. The late adaptive response occurs with the extrusion of organic osmolytes such as myoinositol, glycerophosphatylcholine, glutamate, glutamine, creatinine, and taurine35, 36. Organic osmolytes account for approximately one-third of the solute loss in chronic hyponatraemia36. If adaptation of the brain is incomplete, raised intracranial tension develops which may eventually lead to death. Risk factors for developing acute cerebral oedema during hyponatraemia are mentioned in Table III28. result, water is drawn from the brain cells and brain volume shrinks. Since there is a delay in the reaccumulation of organic osmolytes, there is a higher concentration of inorganic ions as compared to the organic osmolytes. This probably has a role in the pathogenesis of myelinolysis35. Table III enlists the various risk factors for development of ODS28, 41. The clinical manifestations of ODS may be delayed for 2 - 6 days after the elevation of serum sodium and include dysarthria, dysphagia, paraparesis or quadriparesis, and rarely even seizures or coma37, 42, 43. Demyelinating lesions can be detected by MRI and appear as areas of increased signal activity on T2-weighted images and as areas of decreased signal intensity on T1-weighted MRI scans28. ODS is associated with a very poor prognosis and there is no effective therapy, although plasmapheresis and IV immunoglobulins have been tried with variable success44. Management of hyponatraemia The treatement of hyponatraemia requires a proper assessment of the patient so as to determine the cause of hyponatraemia. The two primary goals of therapy are to initiate the treatment of the underlying condition and to restore the normal serum osmolality without causing an iatrogenic complication. Mild asymptomatic hyponatraemia Table III: Risk factors for developing acute cerebral oedema during hyponatraemia. Acute cerebral oedema Osmotic demyelination syndrome Young menstruating women Alcoholics Elderly women on thiazides Malnourished patients Children Hypokalaemic patients Psychiatric polydipsic patients Burn victims Hypoxaemic patients Elderly women on thiazide diuretics Liver transplant patients Osmotic demyelination syndrome (ODS) is associated with rapid correction of hyponatraemia37-39. The adaptive response of the brain creates a potential problem for therapy. A rapid increase in the plasma sodium concentration can lead to osmotic demyelination syndrome, previously known as central pontine myelinolysis. This rapid cellular dehydration originally was identified in the pons, but now has been identified in other areas of the brain40. Because of the organic solute loss that occurs during adaptation, the brain cells become hypotonic to the extracellular fluid during correction of hyponatraemia. As a Journal, Indian Academy of Clinical Medicine does not require specific therapy. The management of severe symptomatic hyponatraemia is controversial. Although a number of questions remain unanswered, the current evidence is in favour of the following points: a. Early recognition and correction of severe hyponatraemia is beneficial because, it itself is associated with significant morbidity and mortality32, 45, 46. b. ODS occurs because of rapid correction of hyponatraemia, and is not due to hyponatraemia itself38. c. Vol. 7, No. 2 If correction of severe hyponatraemia is carried out April-June, 2006 95 slowly these patients fare better32. d. Chronic hyponatraemia alongwith associated risk factors is associated with permanent neurologic sequelae than acute hyponatraemia32, 45,46. e. Patients with chronic hyponatraemia are more likely to develop ODS as compared to those with acute hyponatraemia28. Based on these evidences, certain guidelines can be made for treatment of severe hyponatraemia. Hypertonic saline is clearly indicated in patients who are both severely symptomatic and their serum sodium concentration is less than 120 meq/l. Patients with milder symptoms and serum sodium < 105 meq/l may also be given hypertonic saline22. Figure 1 shows a suggested algorithm for the diagnosis and management of hyponatraemia. Hyperosmolar and iso-osmolar hyponatraemia patients do not require immediate correction of hyponatraemia; instead, reversal of the underlying disorder, such as hyperglycaemia is sufficient3. Hypo-osmolar hyponatraemia: Treatment of hypoosmolar hyponatraemia depends on the volume status of the patient, severity of hyponatraemia, and the duration of hyponatraemia. In patients with severe symptomatic hyponatraemia, urgent treatment is necessary to prevent the complication of cerebral oedema46. Hyponatraemia < 135 meq/l Plasma osmolality Normal = 275 - 290 Isoosmolar Isoosmolar Hypoosmolar (most common) Pseudohyponatraemia Lipid Protein Bladder irrigation Glucose Hypervolaemic Volume status assessment Rx accordingly Euvolaemic Hypovolaemic Uosm Cirrhosis CHF Nephrotic syndrome Renal failure < 100 mosm/l Fluid restriction + Diuretics 1° polydipsia Reset osmostat Beer potomania Urinary Na+ > 100 mosm/l < 20 meq/l SIADH Hyothyroidism Adrenal insufficiency Diuretic use Extrarenal Na+ loss > 20 meq/l Renal Na+ loss Isotonic IVF Fluid restriction Isotonic IVF for Beer potomania Treat underlying disease Fluid restriction Hypertonic IVF for severe cases Fig. 1: Algorithm for management of Hyponatraemia. 96 Journal, Indian Academy of Clinical Medicine Vol. 7, No. 2 April-June, 2006 In hypervolaemic patients, water and sodium restriction are usually enough but in some very severe cases (presence of seizures or coma) hypertonic (3%) saline alongwith a loop diuretic may be used47. This helps in removing the excess of free water. These patients are however usually chronically hyponatraemic and care should be taken so as to avoid rapid or over-correction48. Euvolaemic patients can be subdivided into 2 groups: those with concentrated urine (Uosm > 100 mosm/kg), and those with a dilute urine (Uosm < 100 mosm/kg). The first group includes mainly patients with SIADH. These patients need to be treated according to the severity and duration of their symptoms. In severely symptomatic patients, particularly those with Na+ < 120 meq/l, hypertonic saline should be used3. The second group includes psychogenic polydipsia and reset osmostat where simple water restriction is enough3. In beer potomania, patients should be treated with isotonic saline to replenish low sodium stores3. Hypovolaemic patients with hyponatraemia initially require isotonic saline for concurrent salt and water repletion. Once the patient has reached a clinically euvolaemic state, there is no longer a stimulus for vasopressin release allowing self-correction of hyponatraemia. Therefore, once euvolaemia is achieved, hypotonic saline should be used instead of isotonic saline3. This will prevent a rapid correction of the sodium levels. hyponatraemia is the cessation of life-threatening manifestations, moderation of other symptoms, or the achievement of a serum sodium concentration of 125 to 130 mmol/l49, 50. In asymptomatic patients, the rate of correction should be not more than 0.5 to 1.0 mmol/l and less than 8 - 10 mmol/l in 24 hours38, 43. It is important to note that these asymptomatic patients are more likely to develop ODS with higher infusion rates as the brain in such patients has undergone adaptation. The rate of infusion of the selected solution can be determined by the following formula3, 11: Serum Na+ change with 1 l of IVF = Na+ content in IVF- Measured Serum Na+ [Correction factor * weight (kg)] +1 The correction factor is actually the total body water as a fraction of the total body weight. The correction factor varies according to age and sex as shown in Table IV. The amount of fluid to be infused in l/hr can be calculated as follows: Amount of fluid (l/hr) = (total body water +1)* rate of correction (meq/l/hr) Infusate Na+ – measured Na+ Table IV: Correction factor for calculation of amount of sodium to be infused. Patient Fluid resuscitation rate There is no consensus about the optimal treatment of symptomatic hyponatraemia. Nevertheless, correction should be made of a sufficient pace and magnitude to reverse the manifestations of hypotonicity, but not be so rapid and large as to pose a risk of ODS. Most reported cases of ODS have occurred when the rate of correction exceeded 12 mmol/l/day, but isolated cases have been reported with corrections of 9 - 10 mmol/l/ day37, 38, 41, 49. So the current consensus is that the rate of correction should not be more than 8 mmol on any day3, 11. Initially, the rate of correction may be rapid, but this also should not be more than 1 - 2 mmol/per hour for 3 - 4 hours, or even briefly if the symptoms improve11. Recommended indications for stopping the rapid correction of symptomatic Journal, Indian Academy of Clinical Medicine Paediatric Male, non-elderly Female, non-elderly Male, elderly Female, elderly Correction factor 0.6 0.6 0.5 0.5 0.45 For example, in a 60 kg elderly woman who presents with a significant altered mental status and a sodium concentration of 110 meq/l, hypertonic saline should be instituted immediately. The rate of correction in this case should initially be 2 meq/l/hr for the first two to three hours. The amount of fluid required is [(0.45*60 = 27) +1]*2/513110 = 0.139 l or 139 ml in the first hour. The sodium concentration of various commonly used solutions is shown in Table V. Vol. 7, No. 2 April-June, 2006 97 Table V: Various IV fluids used in the treatment of hyponatraemia and hypernatraemia and the amount of sodium in the fluid. Infusate Infusate Na+ (mmol per litre) Extracellular fluid distribution (%) 855 513 154 130 77 100 100 100 97 73 34 0 55 40 5% Sodium chloride in water 3% Sodium chloride in water 0.9% Sodium chloride in water Ringer’s lactate solution 0.45% Sodium chloride in water 0.2% Sodium chloride in 5% dextrose in water 5% Dextrose in water Other therapeutic options include: Classification of Hypernatraemia 1. Urea: it induces water loss by providing an osmotic load. Moreover, urea diffuses into the brain and its accumulation prevents excessive brain dehydration. It could also trigger the accumulation of organic osmolytes in brain51. Hypernatraemia is always associated with hypertonicity of the plasma. It can therefore be classified according to the volume status of the patient into the following categories: 2. Demeclocycline and lithium: these act on the collecting tubule, reducing its responsiveness to ADH. They can be considered for patients with persistent hyponatraemia unresponsive to water restriction, high salt intake, and a loop diuretic52. 3. Vasopressin receptor antagonists selective for the V2 receptor may be beneficial in patients with SIADH and in hyponatraemic patients with CHF and cirrhosis53. Hypernatraemia Hypernatraemia is defined as serum or plasma sodium concentration > 145 meq/l. Hypernatraemia represents a deficit of water in relation to the body’s sodium stores. It can result from net water loss or hypertonic sodium gain. Sustained hypernatraemia can occur only when thirst or access to water is impaired1. Those at highest risk are patients with altered mental status, intubated patients, infants, and elderly patients 1, 3. The incidence of hypernatraemia ranges from 0.3% to 1%54. In adults, acute hypernatraemia has been associated with a mortality rate as high as 75% and chronic hypernatraemia is associated with a mortality rate of around 60%55. Even in survivors, severe morbidity in the form of permanent neurological sequelae is quite common. 98 1. Hypovolaemic hypernatraemia: Here the fluid lost is hypotonic, so free water loss exceeds sodium loss, resulting in hypernatraemia. Water loss can be extrarenal or renal, and these patients display signs of hypovolaemia such as tachycardia, poor skin turgor, orthostatic hypotension, and dry mucous membranes. a. Extra-renal loss can occur through the skin, as with profuse sweating. Sweat is hypotonic and patients who have fever, or who are exposed to very high temperatures and have limited access to water or decreased thirst, can become hypernatraemic. Similarly, patients with burns or skin diseases such as pemphigus vulgaris can also have hypernatraemia. Alternatively, extra-renal loss can occur through the GIT as in diarrhoea (especially if hypertonic fluid is used for volume replacement, or there is inadequate volume replacement), nasogastric suctioning, vomiting, and third space collection (pancreatitis or bowel obstruction). In all these cases, the urinary sodium concentration is low (< 10 meq/l) and the urine osmolality is high (> 700 mosm/kg)3, 22. b. Renal loss can occur with diuretic use and severe osmotic diuresis resulting from hypertonic mannitol administration, severe glycosuria in diabetics, or elevated urea in the setting of post- Journal, Indian Academy of Clinical Medicine Vol. 7, No. 2 April-June, 2006 obstructive diuresis. In these cases, urinary Na+ is elevated (> 20 meq/l) and urine is isotonic or hypotonic (< 700 mosm/kg)3. 2. Euvolaemic hypernatraemia: In this case, there is pure water loss without the signs of hypovolaemia. Patients appear euvolaemic despite free water loss because most of the water is lost from intracellular space. The water loss can result from extra-renal or renal causes. a. Extra-renal causes: Extra-renal loss of water can occur through skin or respiratory tract. Healthy adults average 500 ml/day insensible loss of water through the skin – even in the absence of discernible sweating22. The normal insensible respiratory loss is also 500 ml/day22. This can increase greatly in the presence of fever, respiratory infection, high altitude, or hyperventilation during mechanical ventilation. Skin and respiratory losses may reach upto several litres/day, but this is easily replaced by most people. Hypernatraemia results when people do not have access to water or fail to drink. Relative hypodipsia is common in elderly patients with normal mental functions and neurological status. Primary hypodipsia is another cause of extra-renal loss of free water, which results from destruction of thirst centres in the hypothalamus, caused by multiple disorders such as hypothalamic tumours, granulomatous diseases, vascular abnormalities, and trauma56. Essential hypernatraemia is a variant of primary hypodipsia in which there is an upward resetting of the osmotic thresholds for thirst and vasopressin release, but their response to haemodynamic stimuli remains normal57. b. Renal causes: Renal loss of free water is due to diabetes insipidus (DI). DI is a disorder characterised by either an absence of ADH secretion (central or neurogenic DI) or a failure of the kidney to respond to ADH (nephrogenic DI)58. In diabetes insipidus, lack of ADH or its effect results in loss of large volumes of dilute urine and a consequent rise in plasma osmolality and serum Na+ concentration. Thirst is stimulated and alert patients are able to maintain their plasma osmolality within the normal Journal, Indian Academy of Clinical Medicine range. Hypernatraemia does not occur unless there is a concomitant defect in the thirst mechanism or restricted access to water. These patients are euvolaemic because water is lost both from the extracellular as well as intracellular space. Causes of DI are enlisted in Table VI3, 58, 59. 2. Hypervolaemic hypernatraemia: It results from pure Na+ overload. It is rare and frequently iatrogenic. This is seen in excessive sodium bicarbonate administration during cardio-pulmonary resuscitation, over-correction of hyponatraemia, hypertonic dialysate in peritoneal and haemodialysis, and hypertonic enteral and parenteral hyperalimentation. Non-iatrogenic causes include mineralocorticoid deficiency and near drowning in salty water. Causes of hypernatraemia are enlisted in Table VI3, 59. Table VI: Causes of hypernatraemia. Hypernatraemia due to net water loss Pure water (euvolaemic) Unreplaced insensible losses (dermal and respiratory) Hypodipsia Neurogenic (central) diabetes insipidus Post-traumatic Tumours, cysts, histiocytosis, tuberculosis, sarcoidosis Idiopathic Aneurysms, meningitis, encephalitis, Guillain–Barré syndrome Ethanol ingestion (transient) Nephrogenic diabetes insipidus Congenital nephrogenic diabetes insipidus Acquired nephrogenic diabetes insipidus Renal disease (e.g., medullary cystic disease) Hypercalcaemia or Hypokalaemia Drugs (lithium, demeclocycline, foscarnet, methoxyflurane, amphotericin B, vasopressin V2–receptor antagonists) Hypotonic fluid (hypovolaemic) Renal causes Loop diuretics Osmotic diuresis (glucose, urea, mannitol) Post-obstructive diuresis Polyuric phase of acute tubular necrosis Intrinsic renal disease Gastrointestinal causes Vomiting Nasogastric drainage Vol. 7, No. 2 April-June, 2006 99 Enterocutaneous fistula Diarrhoea Use of osmotic cathartic agents (e.g., lactulose) Cutaneous causes Burns Excessive sweating Pemphigus vulgaris Hypernatraemia due to hypertonic sodium gain (hypervolaemic) Hypertonic sodium bicarbonate infusion Hypertonic feeding preparation Ingestion of sodium chloride Ingestion of sea water Sodium chloride-rich emetics Hypertonic saline enemas Intrauterine injection of hypertonic saline Hypertonic sodium chloride infusion Hypertonic dialysis Primary hyperaldosteronism Cushing’s syndrome Clinical features: The principal manifestations of hypernatraemia largely reflect CNS dysfunction and are prominent when the increase in serum Na+ is large or occurs rapidly32. Neurological symptoms occur as a consequence of cellular dehydration in the brain32, 59. Loss of brain volume results in traction on the cerebral vessels, which may then tear. It is also associated with cerebral bleeding, subarachnoid haemorrhage, and venous sinus thrombosis33, 62. So the threshold for getting a CT scan in a patient with hypernatraemia and altered mental status should be low. Convulsions are usually absent and are more commonly seen in cases of inadvertent sodium loading or aggressive rehydration63, 64. Signs and symptoms of hypernatraemia are listed in Table VII32. Table VII: Clinical features of hypernatraemia. Anorexia, nausea, and vomiting Altered mental status, agitation, irritability Stupor, lethargy, and coma Signs of neuromuscular hyperactivity: hyperreflexia, spasticity, tremor, asterixis, chorea, and ataxia. Focal neurological deficits: hemiparesis and extensor plantars. Management of hypernatraemia Hypernatraemia (Na+ > 145 meq/l) Plasma osmolality > 290 mosm/kg Hypovolaemic Euvolaemic Hypervolaemic Urine osm. Urine osmolatity Na overload usually iatrogenic > 700 mosm/kg + < 700 mosm/kg Urinary Na + < 10 > 10 Extra-renal loss Renal loss Hypotonic IVF isotonic IVG if BP¯ > 700 < 700 Extra-renal loss – Skin loss – Resp tract loss – 1° Hypodipsia – GIT loss DI Renal loss Hypotonic IVF Hypotonic IVF ± vasopressin Urinary Na+ > 1,000 mmol/lit Diuretic and water replacement Fig. 2: Algorithm for management of Hypernatraemia. 100 Journal, Indian Academy of Clinical Medicine Vol. 7, No. 2 April-June, 2006 Management Proper management of hypernatraemia requires a twopronged approach: addressing the underlying cause and correcting the prevailing hypertonicity. Figure 2 shows an algorithm for diagnosis and treatment of hypernatraemia. The treatment of hypernatraemia depends on the volume status of the patient. Patients with hypovolaemic hypernatraemia should be treated with isotonic saline particularly if there is evidence of circulatory collapse3. Otherwise, if the volume depletion is mild without evidence of circulatory failure, hypotonic fluids such as one-quarter saline (0.2% saline), half isotonic saline (0.45%), pure water, or 5% dextrose should be used59. Even in cases of circulatory failure, once haemodynamic stability is achieved, hypotonic fluids should be used3. Euvolaemic patients also require pure water replacement with hypotonic saline or free water. When administering dextrose containing solutions, blood glucose should be closely monitored, because hyperglycaemia will worsen the hypertonic state and may lead to osmotic diuresis66. Patients with central DI can be given 5 - 10 units of aqueous vasopressin subcutaneously every 3 - 4 hours67. Serum sodium concentration and urinary specific gravity should be monitored every 2 - 4 hours to prevent overcorrection. Vasopressin is preferred over desmopressin because vasopressin has a shorter duration of action3. This will however be ineffective in nephrogenic DI. Hypervolaemic patients have sodium overload, and they require natriuresis with a loop diuretic and free water replacement. Dialysis may be required in patients with severe renal failure to achieve natriuresis3. Rate of correction of hypernatraemia The rate of correction of hypernatraemia depends on the rate of development of hypernatraemia. In cases of acute hypernatraemia (< 48 hrs), rapid correction improves the prognosis without increasing the risk of cerebral oedema, because accumulated electrolytes are rapidly extruded from the brain cells. In such patients, the serum sodium can be reduced by 1 meq/l/hour 65 . In chronic hypernatraemia, a slower pace is required, as full dissipation of accumulated brain solutes during adaptation occurs over a few days. In these patients the appropriate rate of correction is 0.5 meq/l per hour66, 67. The target should be to decrease the serum sodium by 10 meq/l in one day, Journal, Indian Academy of Clinical Medicine except in those in whom the disorder has developed over a matter of hours. The goal of treatment is to achieve a sodium concentration of 145 meq/l59. Lowering the plasma osmolality with hypotonic fluids too rapidly can lead to iatrogenic cerebral oedema because of osmotic shift of water into the brain cells68. Allowances must be made for ongoing hypotonic fluid loss (obligatory or incidental) while calculating the fluid requirement. The amount of fluid required can be calculated using the following formula: Serum Na+ change with 1 l of IVF = Na+ content in IVF – measured serum Na+ [Correction factor * weight (kg)] +1 This formula gives the amount of change in serum sodium with one litre of the given fluid. The amount of hypotonic fluid required can be calculated by the formula: Amount of fluid (l/hr) = (total body water +1)* rate of correction (meq/l/hr) Infusate Na+ – measured Na+ For example, in an elderly 80 kg male with a serum sodium concentration of 160 meq/l, the rate of decrease should be 0.5 meq/l/hr. The amount of 0.45% saline required will be [(0.5*80)+1]*0.5/77-160 = .246 l or 246 ml/hr. Table V lists the characteristics of various solutions used in management of hypernatraemia. Both hypernatraemia and hyponatraemia initially present with non-specific signs and symptoms and can only be diagnosed if a high index of suspicion is maintained for these conditions. The treatment of both these conditions is tricky, as over-treatment can lead to potentially dangerous complications and under-treatment is associated with significant mortality and morbidity. It is therefore essential to monitor the serum sodium concentration every 2 - 4 hours to prevent treatment related complications. Frequent neurological examination should also be performed during treatment as it can help in early detection of ODS and cerebral oedema. References 1. Vol. 7, No. 2 Genanri FJ. Hypo-hypernatraemia: disorders of water April-June, 2006 101 balance. In: Davison AM, Cameron JS, Grunfeld J-P, Kerr DNS, Ritz E, Winearls CG, eds. Oxford textbook of clinical nephrology. 2nd ed. Vol 1. Oxford, England: Oxford University Press, 1998; 175-200. 2. Genanri FJ. Serum osmolality: uses and limitations. N Engl J Med 1984; 310: 102-5. 3. Lin M, Liu SJ, Lim IT. Disorders of water imbalance. Emerg Med Clin North Am 2005; 23 (3): 749-70. 4. McKinley MJ, Mathai ML, McAllen RM et al. Vasopressin secretion: osmotic and hormonal regulation by the lamina terminalis. J Neuroendocrinol 2004 ; 16 (4): 340-7. Nephrol Necker Hosp 1984; 13: 1-28. 21. Ashraf N, Locksley R, Arieff AI. Thiazide-induced hyponatremia associated with death or neurologic damage in outpatients. Am J Med 1981; 70 (6): 1163-8. 22. Votey SR, Peters AL, Hoffman JR. Disorders of water metabolism: hyponatremia and hypernatremia. Emerg Med Clin North Am 1989; 7 (4): 749-69. 23. Fichman MP, Vorherr H, Kleeman CR, Telfer N. Diureticinduced hyponatremia. Ann Intern Med 1971; 75 (6): 853-63. 24. Lee CT, Guo HR, Chen JB. Hyponatremia in the emergency department. Am J Emerg Med 2000; 18 (3): 264-8. 5. Berliner RW, Levinsky NG, Davidson DG, Eden M. Dilution and concentration of the urine and the action of antidiuretic hormone. Am J Med 1958; 24 (5): 730-44. 25. Linas SL, Berl T, Robertson GL et al. Role of vasopressin in the impaired water excretion of glucocorticoid deficiency. Kidney Int 1980; 18 (1): 58-67. 6. Al-Salman J, Kemp D, Randall D. Hyponatremia. West J Med 2002; 176 (3): 173-6. 7. Anderson RJ, Chung HM, Kluge R, Schrier RW. Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med 1985; 102 (2): 164-8. 26. Schrier RW, Linas SL. Mechanisms of defect in water excretion in adrenal insufficiency. Miner Electrolyte Metab 1980; 4: 1-18. 27. Derubertis FR Jr, Michelis MF, Bloom ME et al. Impaired water excretion in myxedema. Am J Med 1971; 51 (1): 41-53. 28. Abraham A, Jacob CK. Severe hyponatraemia: current concepts on pathogenesis and treatment. Natl Med J India 2001; 14 (5): 277-83. 8. Tierney WM, Martin DK, Greenlee MC et al. The prognosis of hyponatremia at hospital admission. J Gen Intern Med 1986; 1 (6): 380-5. 9. Lee CT, Guo HR, Chen JB.Hyponatremia in the emergency department. Am J Emerg Med 2000; 18 (3): 264-8. 29. Riggs AT, Dysken MW, Kim SW, Opsahl JA. A review of disorders of water homeostasis in psychiatric patients. Psychosomatics 1991; 32 (2): 133-48. 10. Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain damage after elective surgery in healthy women. N Engl J Med 1986; 314 (24): 1529-35. 30. Robertson GL, Aycinena P, Zerbe RL. Neurogenic disorders of osmoregulation. Am J Med 1982; 72 (2): 339-53. 11. Adrogue HJ, Madias NE. Hyponatremia. N Engl J Med 2000; 342 (21): 1581-9. 12. Oh MS. Pathogenesis and diagnosis of hyponatremia. Nephron 2002; 92 (Suppl 1): 2-8. 13. Aviram A, Pfau A, Czaczkes JW, Ullmann TD. Hyperosmolality with hyponatremia, caused by inappropriate administration of mannitol. Am J Med 1967; 42 (4): 648-50. 14. Palevsky PM, Rendulic D, Diven WF. Maltose-induced hyponatremia. Ann Intern Med 1993; 118 (7): 526-8. 15. Maas AH, Siggaard-Andersen O, Weisberg HF, Zijlstra WG. Ion-selective electrodes for sodium and potassium: a new problem of what is measured and what should be reported. Clin Chem 1985; 31 (3): 482-5. 16. Gonzales R, Brensilver JM, Rovinsky JJ. Post-hysteroscopic hyponatremia. Am J Kidney Dis 1994; 23:735-8. 31. Fenves AZ, Thomas S, Knochel JP. Beer potomania: two cases and review of the literature. Clin Nephrol 1996; 45 (1): 61-4. 32. Arieff AI. Central nervous system manifestations of disordered sodium metabolism. Clin Endocrinol Metab 1984; 13 (2): 269-94. 33. Schrier RW, Berl T. Disorders of water metabolism. In: Schrier RW ed: Renal and Electrolyte Disorders. Ed 2. Boston, Little Brown and Co, 1986; 1. 34. Melton JE, Nattie EE. Brain and CSF water and ions during dilutional and isosmotic hyponatremia in the rat. Am J Physiol 1983; 244 (5): R724-32. 35. Verbalis JG, Gullans SR. Hyponatraemia causes large sustained reductions in brain content of multiple organic osmolytes in rats. Brain Res 1991; 20; 567 (2): 274-82. 17. Agarwal R, Emmett M. The post-transurethral resection of prostate Syndrome: therapeutic proposals. Am J Kidney Dis 1994; 24:108-11. 36. Paredes A, McManus M, Kwon HM, Strange K. Osmoregulation of Na(+)-inositol co-transporter activity and mRNA levels in brain glial cells. Am J Physiol 1992; 263 (6 Pt 1): C1282-8. 18. Chung HM, Kluge R, Schrier RW, Anderson RJ. Clinical assessment of extracellular fluid volume in hyponatremia. Am J Med 1987; 83 (5): 905-8. 37. Karp BI, Laureno R. Pontine and extrapontine myelinolysis: a neurologic disorder following rapid correction of hyponatremia. Medicine (Baltimore) 1993; 72: 359-73. 19. Kennedy PG, Mitchell DM, Hoffbrand BI. Severe hyponatraemia in hospital inpatients. Br Med J 1978; 2 (6147): 1251-3. 38. Sterns RH, Riggs JE, Schochet SS Jr. Osmotic demyelination syndrome following correction of hyponatremia. N Engl J Med 1986; 314: 1535-42. 20. Abramow M, Cogan E. Clinical aspects and pathophysiology of diuretic-induced hyponatremia. Adv 39. Tanneau RS, Henry A, Rouhart F et al. High incidence of neurologic complications following rapid correction of 102 Journal, Indian Academy of Clinical Medicine Vol. 7, No. 2 April-June, 2006 severe hyponatremia in polydipsic patients. J Clin Psychiatry 1994; 55: 349-54. 53. Gross P, Palm C. The treatment of hyponatraemia using vasopressin antagonists. Exp Physiol 2000; 85: S253-257. 40. Gocht A, Colmant HJ. Central pontine and extrapontine myelinolysis: a report of 58 cases. Clin Neuropathol 1987; 6 (6): 262-70. 54. Long CA, Marin P, Bayer AJ et al. Hypernatraemia in an adult in-patient population. Postgrad Med J 1991; 67 (789): 643-5. 41. Sterns RH, Cappuccio JD, Silver SM, Cohen EP. Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective. J Am Soc Nephrol 1994; 4 (8): 1522-30. 55. Janz T. Sodium. Emerg Med Clin North America 1986; 4 (1): 115-30. 42. Laureno R. Central pontine myelinolysis following rapid correction of hyponatremia. Ann Neurol 1983; 13 (3): 232-42. 43. Srivastava T, Singh P, Sharma B. Pontine and extrapontine myelinolysis following rapid correction of hyponatremia. Neurol India 2000; 48 (1): 97. 44. Finsterer J, Engelmayer E, Trnka E, Stiskal M. Immunoglobulins are effective in pontine myelinolysis. Clin Neuropharmacol 2000; 23 (2): 110-3. 56. Robertson GL. Antidiuretic hormone. Normal and disordered function. Endocrinol Metab Clin North Am 2001; 30 (3): 671-94. 57. DeRubertis FR, Michelis MF, Davis BB. Essential hypernatremia. Report of three cases and review of the literature. Arch Intern Med 1974; 134 (5): 889-95. 58. Robertson GL. Posterior Pituatry. In: Felig P, Baxter JD, Broadus AE et al (eds): Endocrinology and Metabolism. Ed 2. New York. McGraw Hill.1987; 338. 59. Adrogue HJ, Madias NE. Hypernatremia. N Engl J Med 2000; 342 (20): 1493-9. 45. Arieff AI. Hyponatremia, convulsions, respiratory arrest, and permanent brain damage after elective surgery in healthy women. N Engl J Med 1986; 314 (24): 1529-35. 60. Mattar JA, Weil MH, Shubin H, Stein L. Cardiac arrest in the critically ill. II. Hyperosmolal states following cardiac arrest. Am J Med 1974; 56 (2): 162-8. 46. Ayus JC, Krothapalli RK, Arieff AI. Changing concepts in treatment of severe symptomatic hyponatremia. Rapid correction and possible relation to central pontine myelinolysis. Am J Med 1985; 78 (6 Pt 1): 897-902. 61. Snyder NA, Feigal DW, Arieff AI. Hypernatremia in elderly patients. A heterogeneous, morbid, and iatrogenic entity. Ann Intern Med 1987; 107 (3): 309-19. 47. Schrier RW. Pathogenesis of sodium and water retention in high-output and low-output cardiac failure, nephrotic syndrome, cirrhosis, and pregnancy. N Engl J Med 1988; 319 (16): 1065-72. 48. Paterna S, Di Pasquale P, Parrinello G et al. Effects of highdose furosemide and small-volume hypertonic saline solution infusion in comparison with a high dose of furosemide as a bolus, in refractory congestive heart failure. Eur J Heart Fail 2000; 2 (3): 305-13. 49. Oh MS, Kim HJ, Carroll HJ. Recommendations for treatment of symptomatic hyponatremia. Nephron 1995; 70:143-50. 50. Berl T. Treating hyponatremia: damned if we do and damned if we don’t. Kidney Int 1990; 37: 1006-18. 51. Van Reeth O, Decaux G. Rapid correction of hyponatraemia with urea may protect against brain damage in rats. Clin Sci (Lond) 1989; 77: 351-5. 52. Forrest JN Jr, Cox M, Hong C et al. Superiority of demeclocycline over lithium in the treatment of chronic syndrome of inappropriate secretion of antidiuretic hormone. N Engl J Med 1978; 298 (4): 173-7. Journal, Indian Academy of Clinical Medicine 62. Macaulay D, Watson M. Hypernatraemia in infants as a cause of brain damage. Arch Dis Child 1967; 42 (225): 485-91. 63. Morris-Jones PH, Houston IB, Evans RC. Prognosis of the neurological complications of acute hypernatraemia. Lancet 1967; 2: 1385-9. 64. Hogan GR, Dodge PR, Gill SR et al. Pathogenesis of seizures occurring during restoration of plasma tonicity to normal in animals previously chronically hypernatremic. Pediatrics 1969; 43: 54-64. 65. Palevsky PM. Hypernatremia. In: Greenberg A, ed. Primer on kidney diseases. 2nd ed. San Diego, Calif.: Academic Press, 1998; 64-71. 66. Kahn A, Brachet E, Blum D. Controlled fall in natremia and risk of seizures in hypertonic dehydration. Intensive Care Med 1979; 5: 27-31. 67. Blum D, Brasseur D, Kahn A, Brachet E. Safe oral rehydration of hypertonic dehydration. J Pediatr Gastroenterol Nutr 1986; 5: 232-5. 68. Arieff AI, Guisado R. Effects on the central nervous system of hypernatremic and hyponatremic states. Kidney Int 1976; 10 (1): 104-16. Vol. 7, No. 2 April-June, 2006 103
© Copyright 2026