The Art and Science of Sample Collection
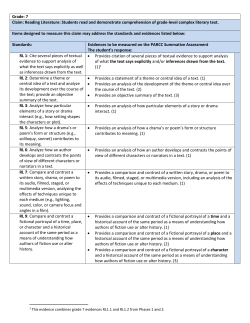
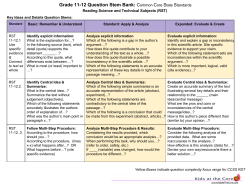
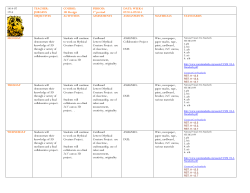
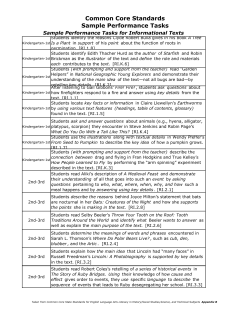
The Art and Science of Sample Collection Ana K. Stankovic, MD, PHD, MSPH WW VP, Medical Affairs BD Diagnostics – Preanalytical Systems Karen Scraba, MLT, BSc(MLS), MT(ASCP) Clinical Market Manager BD Diagnostics - Preanalytical Systems October 18, 2013 THE ART: History of Blood Collection It Started With Blood-Letting … Phlebotomy is the practice of opening a vein by incision or puncture to remove blood as therapeutic treatment or for diagnosis. The ancient art of phlebotomy dates back three thousand years as the practice began with the Egyptians in 1000 B.C. Egyptian history records blood-letting as a treatment for variety of ailments. Blood-letting was believed to drive out evil spirits; therefore, the procedure was performed by a priest, who was also a physician. In Greece, Hypocrites was responsible for early medical theory, which believed illness was caused by an “imbalance” in the body. The removal of this “excess” by plugging, starving, vomiting, or bloodletting was thought to restore this balance. Blood-letting continued as a practice in the middle ages where it began to fall into the duties of – strangely enough – barbers. The main process of blood-letting in 19th century medicine included the use of leeches to drain blood from a patient. During the 1830s, France imported approximately 40 million leeches for the purpose of blood-letting up to as late as the early 19th century as preventive medicine. It wasn't until the 19th century that members of the medical community seriously questioned the merits of this practice. In the 1830s, Pierre Charles Alexandre Louis convincingly argued against the perceived effectiveness of phlebotomy for the treatment of pneumonia and fever. … And Continued with Transfusion … The first historical attempt at blood transfusion was described by the 15th-century chronicler Stefano Infessura. Infessura relates that, in 1492, as Pope Innocent VIII sank into a coma, the blood of three 10-year-old boys was infused into the dying pontiff (through the mouth, as the concept of circulation and methods for intravenous access did not exist at that time) at the suggestion of a physician. However, not only did the pope die, but so did the three children. The first fully documented human blood transfusion was administered by Dr. Jean-Baptiste Denys, eminent physician to King Louis XIV of France, on June 15, 1667. He transfused the blood of a sheep into a 15-year old boy, who survived the transfusion. ... To Specimen Collection It is open to debate when blood first began to be examined for diagnostic purposes. It is known that other body fluids have been examined since medieval times. The invention of the microscope in the 17th century, coupled with advances in physiologic chemistry and cellular physiology in the 19th century, paved the way for the examination of blood as a diagnostic tool. In 1908, James C. Todd, professor of clinical pathology at the University of Colorado School of Medicine, published the first Manual of Clinical Diagnosis. The 1912 edition of the book has a chapter titled "The Blood." One passage reads: "For most clinical examinations only one drop of blood is required“. The Manual, in addition to describing general techniques and anatomical points for blood-letting, discusses the method of obtaining a blood culture from a skin puncture in the lobe of the ear "...by gently milking, 20 to 40 drops can usually be obtained." Between the two World Wars, specimens were collected with needles and glass syringes. In 1949, Joseph Kleiner patented the “Evacuator”, and the modern concept of evacuated blood collection was born. Blood Collection/Acquisition Devices: Timeline of Innovation Safety in Blood Collection for Laboratory Testing In recent years, major improvements have been made in the area of healthcare worker (HCW) safety. New and innovative safety devices, combined with effective HCW training, adoption of best practices, and elimination of sharps use, have ensured continued reduction of occupational exposure to pathogens and percutaneous injuries, thus successfully lowering rates of HCW acquired infections. Voluntary adoption of a culture of safety, as well as legislative mandates (US Needlestick Safety and Protection Act – NSPA) are external factors that will further facilitate safety adoption. Injury Rates From Conventional Devices vs. SEDs for Blood Collection Procedures 16 Italian hospitals, 1997-2009 [ total conventional devices = 9,860,855 , total safety-engineered devices (SEDs) = 13,288,640] Injuries per 100,000 devices used 12 conventional 10 safety year 1 safety year 2+ 8 6 -45% -60% 4 -74% -54% 2 -65% -69% -85% -94% -84% -98% 0 n la ce t s er ga t he d t ca oo bl IV sy g rin e e l ed y bl m ne se y as om ot ly rf tte b le bu ph J.Jaeger, personal communication Percutaneous Injuries Before and After NSPA The annual rates of percutaneous injuries per 100 full-time–equivalent hospital employees were calculated. There was a trend toward increasing rates of injuries before the legislation was enacted, which was followed by a drop of about 38% (95% confidence interval, 35 to 41) in 2001when the NSPA took effect. Subsequent injury rates, through 2005, remained well below pre-NSPA rates. Two factors directly linked to the legislation were: – shift from conventional to safetyengineered devices and – an increase in the number of OSHA citations for violation of the revised standard for handling bloodborne pathogens. Philips E.K. et al. NEJM 366:670-1, 2012 To see the on-line version http://www.canadianhe althcarenetwork.ca/heal thcaremanagers/ Click on “Management” then on “Patient Safety” Lastly, Click on: Second-generation collection set reduces needlestick injuries Open Collections are Still Common Developed markets: 6.3% Globally Emerging markets: 30% THE SCIENCE: Development of New Specimen Collection Devices IVD Product Life Cycle Management Laboratories are Faced with Constant Pressures to Improve Testing Turnaround Time This is particularly important in the Emergency Department (ED), where prolonged patient waiting time can result in ED “crowding”, which in turn can lead to: – Reduced patient satisfaction and diversion (to another facility) – Compromised patient care – Loss of revenue opportunity When trying to maximize the turnaround time (TAT) in the ED, plasma offers time savings as compared to serum; however, quality and stability issues, as well as potentially limited assay choices, are a concern. Serum, on the other hand, is often considered superior regarding specimen quality, but it can negatively impact the TAT. There is a need for a blood collection tube with an additive that will assure the speed of plasma and the quality of serum. General Flow Down Structure for Critical Parameter Management VOC: Needs… Flow down of the Voice of the Customer… Requirements to be fulfilled through the measurement of Critical Functional Responses (CFRs) & Critical to Function Specs (CTFs) … System Level: Requirements System Level: CFRs… Subsystem Level: Requirements Cp Cp = Subsystem Level: CFRs… VOC VOP Roll-up of the Voice of the Design & RollMfg. Critical Parameters…through the actual measurement of CFRs & CTFs Copyright PDSS Inc. 2003 Subassembly Subassembly: CFRs… Cp 6s >1.33 = standard ~ 2.00 = 6 s Subassembly Subassembly: Requirements Cp = USL--LSL USL Components: CTF Reqs. Components: CTF Specs… Cp Mfg. Process: Process Requirements Mfg. Process: Process CTF Specs… Effect of Manufacturing Variability on Additive to Blood Ratio Variability reduced by 50% Maximal Allowable variability Additive to Blood Ratio (mg/mL) Potential Advantages of BD Vacutainer® Rapid Serum Tubes (BD RST) 5 min Clotting Time Clean Serum ↓Fibrin ↓Hemolysis Less Instrument Downtime Fewer Redraws Faster Results BD RST Can Reduce Serum STAT Testing TAT BD RST: Ready to analyze in 8 min* TAT savings = 32 min** *Centrifuged at 4000 g for 3 minutes **Compared to standard serum separator control tubes, 30 min. clot time, 10 min centrifuge time Impact of BD RST on Preanalytical TAT 70 Tub e Ty p e 60 BD RS T Control Serum Separator Tube Minutes 50 40 30 Centrifugation: High Speed Centrifuge 20 10 0 Collection to clot Clot to centrifuge Centrifuge to Load 30.5 min gain 38.5 min gain Preanalytical intervals Prusa R, Douppvcova J, Stankovic AK, and Warunek D. Improving laboratory efficiencies through significant time reduction in preanalytical phase. Clin Chem Lab Med 2010; 48:293-6. BD RST - Clinical Evaluation Evaluations were conducted using multiple instrument testing platforms to compare the performance of the BD RST with the BD Vacutainer® SST™ Blood Collection Tube (BD SST™) for selected analytes in clinical chemistry, immunology and serology. For each analyte, between-tube comparisons at initial time were performed using a Deming Regression in order to obtain the BD RST vs. BD SST™ mean bias (with confidence intervals) at predetermined medical decision levels and at the average of the control tube. The tube comparisons were evaluated relative to the assigned clinical acceptance limit (CAL) for each analyte. Stability testing was performed for selected analytes by calculating the mean bias (with confidence intervals) for the 24 hrs vs. initial time comparison for each tube type. For Troponin I, the percentage of concordant and discordant results above or below medically important decision levels or lower limits of reportable ranges was determined. Overall, BD RST showed clinically equivalent or clinically acceptable performance for tested analytes when compared to the BD SST™. Instrument Platforms and Number of Tested Analytes: BD RST Comparison with BD SST™ Instruments Number of analytes/per instrument Beckman Coulter Access®/Access® 2 6 Beckman Coulter UniCel® DxC 800 17 Beckman Coulter UniCel® DxI 800 15 Biomerieux VIDAS® 2 Dynex DS2®/Wampole Laboratories 2 Ortho Clinical Diagnostics VITROS® 5,1 FS 10 Roche COBAS Integra® 800 27 Roche COBAS MODULAR ANALYTICS 25 Siemens Dimension® RxL 19 Siemens ADVIA Centaur®/Centaur® XP 15 Total number of analytes tested: 55 BD RST vs. BD SST™ Comparison of Clinical Chemistry, Immunology and Serology Analytes Albumin (ALB) Alkaline Phosphatase (ALKP) Alanine Aminotransferase (ALT) Amylase (Amy) Aspartate Aminotransferase (AST) Bilirubin, Direct (DBIL) Bilirubin, Total (TBIL) Blood Urea Nitrogen (BUN) Calcium (Ca) Carbon Dioxide (CO2) Chloride (Cl) Cholesterol (Chol) Complement C3 (C3) Complement C4 (C4) Cortisol (Cortisol) Creatine Kinase (CK) Creatine Kinase-MB fraction (CKMB) C-reactive Protein (CRP) Creatinine (Creat) Cytomegalovirus Antibodies, IgG (anti-CMV IgG) Cytomegalovirus Antibodies, IgM (anti-CMV IgM) Estradiol (E2) Ferritin (Ferritin) Folate (Folate) Follicle Stimulating Hormone (FSH) Free Triiodothyronine (FT3 Free Thyroxine (FT4) Gamma-glutamyl transferase (GGT) Glucose (Glu) Human Chorionic Gonadotropin (hCG) High Density Lipoprotein (HDL) Immunoglobulin G (IgG) Immunoglobulin M (IgM) Iron (Fe) Lactate Dehydrogenase (LDH) Lipase (Lip) Low Density Lipoprotein (LDL) Luteinizing Hormone (LH) Magnesium (Mg) Myoglobin (Myo) Phosphorus (Phos) Potassium (K) Progesterone (Prog) Rheumatoid Factor (RF) Sodium (Na) Testosterone (Testosterone) Thyroid Stimulating Hormone (TSH) Total Protein (TP) Total Triiodothyronine (TT3) Total Thyroxine (TT4) Transferrin (Transferrin) Triglycerides (Trig) Troponin I (TnI) Uric Acid (UA) Vitamin B12 (Vitamin B12) BD Rapid Serum Tube demonstrated clinically equivalent or clinically acceptable performance compared to the BD SSTTM for all analytes on each platform evaluated BD data on file Troponin I (TnI): Beckman Coulter Access® Bias and confidence limits for BD RST vs. BD SST™ CAL Medical decision level or average Type BD RST vs. BD SST™ Systematic bias (Two one-sided 95% confidence limits) TnI >0.04 ng/mL 20% 2.31 ng/mL AV 3.1% (-4.1, 10.9) TnI >0.06 ng/mL 20% 2.575 ng/mL AV 3.4% (-4.8, 12.3) 0.5 ng/mL CV 0.9% (-2.9, 4.9) Analyte Values listed are either the average of the analyte group or analyte-specific medical decision levels CV – Critical Value, AV – Derived Average From Control Group *White paper – VS8129 – data on file at BD. Concordance Table: Troponin I (Initial Time) (Beckman Coulter Access®) All BD RST BD SST™ Negative (<0.5 ng/mL) Positive (≥0.5 ng/mL) Negative (<0.5 ng/mL) 101 0 101 Positive (≥0.5 ng/mL) 0 4 4 101 4 105 All The observed percent concordance is 105/105 = 100% (with exact 95% lower confidence limit = 97.2%). There is no significant difference in the distribution of results per tube (McNemar's chi-square test with continuity correction, p-value = 1). *Whit e paper VS8129 – data on file at BD. The BD RST Demonstrated 59% Reduction in Hemolysis and Fibrin Strands Relative to a Comparator Serum Tube Hemolysis Rating Scale: 0-3 0=none, 1=trace, 2=moderate, 3=gross 0 1 2 3 Study Tube Type N % N % N % N % BD RST HG Comparator Serum Tube 1103 98.84 12 1.08 1 0.09 - - Total 724 97.18 16 2.15 3 0.40 2 0.27 59% relative decrease in hemolysis Fibrin Strand 0=none, 1=small, thin strand, 2=large, thick strand 0 1 2 Study Tube Type N % N % N % BD RST HG Comparator Serum Tube 1080 96.77 36 3.23 - - Total 687 92.21 54 7.25 4 0.54 *White paper VS8133 - Data on file 59% relative decrease in fibrin strands BD RST Improves Average Turnaround Time 90 80 70 60 Minutes 50 Creatinine Beta-hCG 40 30 20 10 0 June (Initial state) September (Analyzer change) November (Tube change) Improvements in Laboratory Turnaround Time Metrics. Poster Presented By Dr. J. Wesenberg at the AACC 2010. Breakdown of Average TAT Improvement Analyte TAT Improvement Total System New Analyzer BD RST Creatinine 24% 6% 18% b-hCG 43% 27% 16% * Improvements in Laboratory Turnaround Time Metrics. Poster Presented By Dr. J. Wesenberg at the AACC 2010. BD RST Decreases False-Positive Immunoassay Results BD RST tubes were investigated to reduce undetermined interferences contributing to false-positive immunoassay results in heparin plasma samples. Patients being evaluated for suspected myocardial infarction had specimens drawn into an RST in addition to a standard lithium-heparin plasma separator tube (PST). 28 separate analytes were measured in both specimens using immunoassay, electrochemical, and spectrophotometric methods. Higher results were observed in some PST specimens tested for troponin I, creatine kinase-MB isoenzyme, human chorionic gonadotropin, and thyroidstimulating hormone. These discrepancies were investigated by repeating analyses after recentrifugation of both specimens. Reanalysis showed results for the PST specimens that were lower and agreed well with initial results from RSTs, suggesting false-positive rates of 10.8% for troponin I and about 2% for each of the other 3 analytes. Overall, specimens collected in RSTs had fewer false-positive immunoassay results than specimens collected in plasma separator tubes. Strathman FG et al., AJCP, 136:325-9, 2011. Summary Development of new blood collection devices is a complex process. It requires thorough market needs assessment, good product requirement determination, optimal product design, determination of device safety and efficacy and successful product launch. ?... [email protected] [email protected]
© Copyright 2026