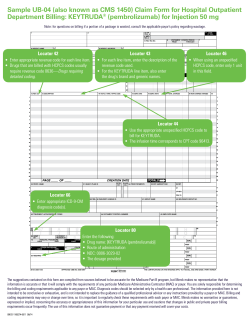
Sample CMS1450 (UB-04) Claim Form
Sample CMS1450 (UB-04) Claim Form For Use with a Drug that does have a HCPCS/Pass-Through Code Assigned Under Medicare’s APC System for Hospital Outpatient Services MM/DD/YY Smith, Jane, D. MM/DD/YY F Column 47 — Total Charges • Indicate the facility’s actual charges for products and procedures. Column 43 — Description • Description of services/products provided • Drug Name, Strength, NDC# 0510 0636 Clinic Drug Name 11111-2222-33 Column 42 — Revenue Code(s) Enter appropriate revenue codes for services provider. List all revenue codes in ascending numerical order. Product Revenue Codes: • Revenue Code 0636 (“Drugs that require detail coding”) should be used. Please note: revenue code requirements may vary by payor. Check with payor to determine the appropriate revenue code for billing. MM/DD/YY 123 Main Street, Anytown, Anystate 12345 96409 CXXXX MM/DD/YY MM/DD/YY Column 44 —Product/Procedure Code(s): Product Code: • Indicate the appropriate HCPCS/ pass-through code for the drug administered. X $$$ $$ X $$$ $$ Column 46 — Service Units • Enter the number of units of each product/service administered. Procedure Code: • Enter the CPT code that represents the administration procedure performed. Procedure Revenue Codes: • CMS requires a revenue code for each line item on the UB-04 form. CMS instructs billers to use the most appropriate revenue code for the setting where the service is performed (i.e. 0360 - operating room; or 0510, clinic) National Provider Identifier (Box 56) • Enter appropriate NPI as assigned by CMS (Note: see also Boxes 76, 77, 78, 79) XXX.XX Diagnosis Codes (Box 67) • Enter appropriate ICD-9-CM diagnosis code corresponding to a particular patient’s diagnosis. This Billing Instruction Sheet is intended as a reference for potential coding, billing and associated services. It is not intended to be a directive, nor is it a suggestion about the likelihood of obtaining reimbursement. Physicians and staff may deem other codes or policies more appropriate. Providers should select the coding options that most accurately reflect a patient’s condition, their internal system guidelines, payer requirements, practice patterns, and the services rendered.
© Copyright 2026