ACS NSQIP: Preventing complications Reducing costs Improving surgical care
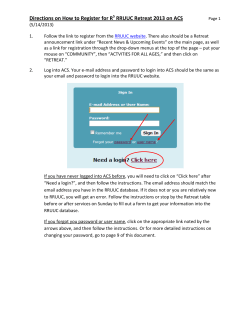
ACS NSQIP: Preventing complications Reducing costs Improving surgical care Wednesday, October 8, 2014 Presentation to: New South Wales Agency for Clinical Innovation Sydney, Australia ACS Mission Statement ACS Mission: Dedicated to improving the care of the surgical patient and to safeguarding standards of care in an optimal and ethical practice environment NSQIP: Improving Surgical Care and Outcomes High Quality Surgical Care Tools/ Guidelines/ Teamwork/ Set Standards/ Partnerships Data Collection/ Analysis/ Risk-adjusted outcomes Feedback; QI Planning Improving Care, Reduce Costs Current Participants ACS NSQIP: Proven to Reduce Complications, Save Lives 2009 Annals of Surgery study: • Prevent 250-500 complications annually • Save 12-36 lives annually • Leading to reduced costs What is ACS NSQIP? • • • • • • • • • Hospital based quality improvement program Risk and Case Mix-Adjusted 30 Day Clinical Outcomes Data collected by trained abstractors Allows benchmarking among participating sites Data entry via web-based Workstation Based solely in English Based upon CPT Codes Multi-specialty (GS, Vasc, Ortho, NS, Uro, Gyn…) Improvement/Educational “Tools”: Best Practices/Guidelines (e.g. SSI, UTI), case studies, collaboratives, Calculator, partnerships (Joint Commission, IHI, CMS, AHRQ, CUSP, ERAS, others) Data Integrity • • • • • • • • Trained Surgical Clinical Reviewers (SCRs) Annual SCR Certification Exam Data Validation in Workstation Inter Rater Reliability Audits Webinars/Conference calls Clinical & Technical Support ACS NSQIP National Conference Surgeon Champion/SCR/Administrator Toolkits CPT Codes • Procedure selection within the NSQIP workstation • -ICD-9 and CPT Code Look Up in the Outcome Database • -Ingenix Procedural Cross Coder book • -Ingenix ICD-9-CM for Hospitals – Volumes 1, 2, & 3 • -American Medical Association CPT 2012 • http://www.codapedia.com Clinical Data Better for Measuring Quality Following Patients After Discharge • Half or more of all complications occur after discharge • Quality programs based on admin data don’t track post-discharge • Complications after discharge can lead to readmissions Tracking quality can’t stop at the hospital’s door 30-Day Post-Op Follow Up Review Outcome /follow-up information can be obtained in a variety of ways: • Review of the patient’s medical record. • Screen for readmissions • Separate clinic or the private surgeon’s office outpatient follow-up visits • Additional methods would be either a phone call placed directly to the patient or a follow-up letter can be mailed for the patient to respond to in writing Program Staffing Surgeon Champion (SC) • Program Mentor/Advocate Surgical Clinical Reviewer (SCR) • Data Collector *Remember that the nature of this relationship will determine the success of your program Surgeon Champion Qualifications • • • • • • • Well Respected & Highly Regarded Chief of Surgery or Chief Medical Officer Program Mentor/Advocate Must be trusted by peers and administration Experience with Quality Improvement Lead Quality Improvement Initiatives Participate in Monthly SC Conference Calls Surgical Clinical Reviewer Qualifications Recommended … • 1 Year experience in surgery, medical records, clinical research • Nursing Background • Computer and Internet experience • Quality improvement or patient safety knowledge and experience SCR Training • • • • Registration available after invoice payment Online, Web-Based Training 4 Weeks Total Weekly webinars and Conference Calls – 1 to 2 every week • Recorded Sessions available due to time difference • Workstation Access – Week 2 • Data collection starts - Week 2 • Certification Exam - 6 months and every October Data Collection Case Selection Inpatient and Outpatient excluding … • Trauma • Transplant • Ophthalmology • C-Sections • Endoscopy • Colonoscopy Data Collection Sampling Methodology • A randomized sampling system called the 8-day cycle - Required to submit data on 42, 8-day cycles/year - ~40 cases every 8-day cycle = 1,680 cases annually Risk and Case-Mix Adjustment Matters To judge care fairly and understand where problems are occurring: • Health of the patient must be considered - Patient characteristics - Pre-op Risk Factors • Risk of the procedure must be considered - All variations in surgical outcomes - Surgical Complexity Risk Adjustment Odds Ratios An Odds Ratio of 1 is like “par on a golf course” – the score that is expected It is a metric showing the risk-adjusted performance at a specific site compared to the average hospital • An Odds ratio < 1 means that the site is performing better than expected, while a ratio > 1 indicates an excess of adverse events • The odds is defined as the #events / #non-events i.e. 5/95=.053, is the odds for a hospital if there are 5 deaths among 100 patients • Our Odds Ratio is the risk-adjusted odds for an event at a site divided by the odds for an event at the average site • Our Odds Ratios are also adjusted so they are useful even for hospitals that provide very small samples Audits Data Needs to be Believed: Validation with Audits 10% 2005 2006 2007 2008 3.15% 2.26% 1.99% 1.56% 0% Inter-Rater Reliability (% Disagreement) Audits Annual random 5% selection of all ACS NSQIP participating hospitals Hospital is given 4 to 6 weeks’ notice of a site visit 12 to 24 charts are selected and access to the OR Log Book ACS representatives are sent to review charts 1 to 2 day process Results are provided within a summary report o Disagreement(s) of variables/operative log book o Re-education requirements if needed o Pass/Fail/Incomplete score Available Data Real-Time/On Line Reports • Allows comparison to other ACS NSQIP hospitals using online reports Interim & Semiannual Benchmark Reports • Provides risk-adjusted comparisons of all ACS NSQIP hospitals regarding morbidity, mortality, and complications Participant Use File • Contains all cases reported from 2004 to date Reporting Real Time Reports • Workflow Reports • Site-Level Reports • Database Statistics • Data Analysis Reporting 30 Day Post-Op Summary Reporting Mortality Patient Report Reporting Post-Operative Occurrence Analysis Reporting Reporting Online Collaborative Report: Hospital Online Collaborative Report: Leadership & Administration Reporting Semiannual Report Risk adjusted for hospital-to-hospital patient mix differences. Reporting Over 195 Risk-Adjusted Models • • • • • • • • • • • • • 30-Day Mortality 30-Day Morbidity 30-Day Death and Serious Morbidity Cardiac Occurrences Pneumonia Unplanned Intubation Ventilator Dependence >48 hours DVT/PE Renal Failure Urinary Tract Infection/UTI Surgical Site Infection/Deep & Organ Space SSI Colorectal LOS Unplanned Return to the OR Reporting High Outliers 1st Decile 10th Decile Exemplary Needs Improvement 278,198 4,429 1.59 2 6 28 29 28 29 289 278,198 27,427 9.86 34 41 28 29 37 45 289 278,198 2,423 0.87 5 16 28 29 28 29 Pneumonia Unplanned Intubation 289 289 277,791 277,890 3,792 3,535 1.37 1.27 13 8 35 21 28 28 29 29 28 28 40 29 Ventilator > 48 Hours 289 276,643 4,505 1.63 9 21 28 29 28 33 289 289 278,198 277,979 2,591 2,096 0.93 0.75 0 1 14 9 28 28 29 29 28 28 29 29 289 277,724 3,881 1.40 15 38 28 29 28 40 289 275,905 11,002 3.99 32 46 28 29 35 54 Observed Rate Low Outliers Low Outliers Observed Rate 289 Morbidity 1 Total Cases Mortality Sites Included Observed Events SAR Model Summary Reports Overall (General / Vascular) Cardiac 3 DVT / PE 4 Renal Failure UTI 11 10th Decile Exemplary Needs Improvement 5,368 1.35 7 6 28 29 28 29 398,906 34,993 8.77 43 54 28 29 45 56 289 398,906 2,968 0.74 9 24 28 29 28 33 Pneumonia Unplanned Intubation 289 289 398,397 398,545 4,772 4,320 1.20 1.08 18 15 42 28 28 28 29 29 28 28 45 31 Ventilator > 48 Hours 289 397,033 5,362 1.35 17 31 28 29 28 35 289 289 398,906 398,656 3,728 2,540 0.93 0.64 2 1 23 11 28 28 29 29 28 28 30 30 289 398,137 5,847 1.47 28 48 28 29 34 50 289 396,257 12,961 3.27 31 59 28 29 32 60 Observed Events 398,906 289 Total Cases 289 Sites Included 1st Decile 6 High Outliers SSI 5 Overall (Multispecialty - All Cases) Mortality Morbidity Cardiac 1 3 DVT / PE 4 Renal Failure UTI 11 SSI 6 5 Site Summary Report (SAR & ISAR) Semi-Annual Report: Site Specific Bar Plot SAR Collaborative Report SAR Collaborative Report • Collaborative ranking by decile for the most recent SAR period • Collaborative “Minimum” and “Maximum” OR based on Hospital ORs Model Name GEN Mortality GEN Morbidity GEN Cardiac GEN Pneumonia GEN Unplanned Intubation GEN Ventilator > 48 Hours GEN DVT/PE GEN Renal Failure GEN UTI GEN SSI GEN ROR 1 7 6 9 6 8 6 7 6 7 7 8 2 7 6 9 6 8 6 7 6 7 7 8 Decile 3-8 7 6 9 6 8 6 7 6 7 7 8 9 7 6 9 6 8 6 7 6 7 7 8 10 7 6 9 6 8 6 7 6 7 7 8 OR Range Min Max 0.79 1.38 0.85 1.26 0.87 1.55 0.55 1.46 0.90 1.34 0.84 1.38 0.87 1.44 0.77 1.39 0.72 1.64 0.81 1.50 0.91 1.66 Rank of Collaborative Hospitals • Each collaborative hospital is represented by a yellow dot on the corresponding line (which represents all NSQIP hospitals) – All hospitals may not have cases fitting a specific model. Thus, fewer dots would appear on the corresponding line. • Rankings are based on Hospital ORs from the most recent SAR – Lower ranks indicate lower ORs, while higher ranks indicate higher ORs Collaborative GENERAL Dashboard • Collaborative ORs and Deciles from the current and past SAR • Percentage of “Exemplary”, “As Expected”, and “Needs Improvement” hospitals from the most recent SAR • Provided for 6 GENERAL NSQIP models: – Mortality, Morbidity, Pneumonia, Unplanned Intubation, DVT/PE, SSI Previous SAR values Collaborative Current SAR Summary • All of NSQIP • Collaborative Level – Full OR Range – Interquartile OR Range – Case Counts – ORs and Deciles – Hospital Percentages Collaborative NSQIP ORs Total Cases Observed Cases OR Decile Percent "Exemplary" Percent "As Expected" Percent "Needs Improvement" Minimum OR 25th Percentile 75th Percentile Maximum OR 13 GEN Mortality 9031 119 1.10 7 0 71 29 0.56 0.90 1.14 2.02 14 GEN Morbidity 9031 680 1.06 6 0 86 14 0.51 0.87 1.19 3.00 15 GEN Cardiac 9031 57 1.16 9 0 71 29 0.60 0.91 1.10 1.78 16 GEN Pneumonia 9001 90 1.01 6 14 86 0 0.32 0.76 1.34 5.09 17 GEN Unplanned Intubation 9022 98 1.16 8 0 100 0 0.55 0.87 1.17 2.02 18 GEN Ventilator > 48 Hours 8996 97 1.01 6 0 100 0 0.36 0.83 1.22 2.81 19 GEN DVT/PE 9031 74 1.10 7 0 86 14 0.49 0.87 1.16 2.46 20 GEN Renal Failure 9023 46 1.03 6 14 57 29 0.52 0.90 1.13 3.25 21 GEN UTI 9014 97 1.19 7 0 86 14 0.46 0.84 1.23 2.26 22 GEN SSI 8935 345 1.14 7 0 71 29 0.49 0.83 1.22 4.54 23 GEN ROR 9031 250 1.16 8 0 71 29 0.54 0.89 1.14 2.14 SAR Model Name General ACS NSQIP: Proven to Reduce Complications, Save Lives 2009 Annals of Surgery study: • Prevent 250-500 complications annually • Save 12-36 lives annually • Leading to reduced costs Surgical Complications Drive Readmissions 2012 Journal of the American College of Surgeons study: • Surgical complications key driver of 30-day readmissions • SSIs – 22% • Gastrointestinal – 28% • Pulmonary – 8% ACS NSQIP: Better Care, Lower Costs Not only will patients benefit, but hospitals see a significant return on their investment with ACS NSQIP. • Significant cost savings per year • Reduced readmissions and reduced lengths of stay translate to better patient outcomes, better satisfaction and even more cost reduction • Pays for itself by avoiding about a dozen surgical complications ACS NSQIP: Reducing Costs Surry Memorial Hospital in Vancouver, BC • $2.7 million savings over two years by reducing breast surgery SSI by 13.3% and general and vascular SSI by 5.7% • Averted ~$380,000 in costs over 4 months via initiatives to reduce UTI’s Henry Ford in Detroit • $2 million annual savings and 1.54 days reduced LOS Baptist Hospital of Miami • $4 million annual savings • Sustained efforts to reduce its rate of hospital-acquired infections have led to a savings of about $4 million a year since 2007 ACS NSQIP: Reducing Costs Winthrop University Hospital, Mineola, NY • Reduction in Pneumonia from 1.36% (July 2011) to 1.25% (July 2012) = $1,436,305.00 (65 averted cases) • Ventilator >48hours reduction from 1.9% (July 2011) to 1.04% (July 2012) = $2,903,655.00 (105 averted cases) Savings exceeding >$4,000,000.00 Beaumont Hospital in Royal Oak, MI • $2.2 million savings reduced average LOS by 6.5 days by reducing SSI. • Nearly 300 SSI’s prevented in 2009 Stanford in Stanford, CA • SSI reduced from 1.03 to 0.58 at a savings of $28,000 per SSI. Case Study: Improvement in CAUTI in Surgical Wards, (Sheikh Khalifa Medical City, Abu Dhabi, UAE) • High outlier status identified in SAR, (Jan, 2011) • Multidisciplinary Task Force • Education/QI Initiative • Expansion throughout entire hospital *Results: > 3 CAUTI/yr since Aug. 2012 Sheikh Khalifa Medical City (SKMC), Managed by the Cleveland Clinic, Abu Dhabi, United Arab Emirates; ACS NSQIP Best Practice Case Studies, Vol. 4, July 2013 ACS NSQIP System Participation • Discounts for systems enrolling multiple hospitals • Ability to work on QI together, as other hospitals enroll • Ability to collect custom variables to tailor to system’s needs • Possible to share resources across system hospitals • Greater impact on system’s bottom line Collaborative Case Study: BC UTI Improvement Project Notable Gains in UTI Rates across 10 Hospitals • A collective drop in UTI rates from 3% before Apr. 2012 to 2.25% in 2013 • A combined average of 39 events/month before Apr. 2012 to 31.5/month after Apr. 2013 2 Case Study: Vancouver General Hospital CLEAN Program Cost Avoidance of ~$100, 000.00 over 5 months • GOAL: Reduce Cardiac SSI’s from 6% to 2% by Jan. 2014 • SSI team collaboration with Infection Control • Best Practices identified & implemented • No SSI’s since July 2013 • ~$100,000 cost avoidance 2 Return on Investment Non-Monetary Benefits … • Valid benchmarking for surgical outcomes • Provides proactive, value-oriented performance measurement before it’s dictated by outside agents • Improves local market position through publicly visible improvement programs • Optimizes cross-departmental partnerships and collaboration through shared knowledge • Helps build high performance surgical teams and employee retention, (i.e. nurses) • Offers CME’s for Surgeon Champions and CEU’s for SCR’s NSQIP Provides Improvement Tools and Education • Robust Interactive Training for Abstractors (Surgical Clinical Reviewers) • Surgeon Champion/SCR/Administrative Toolkits • Best Practice Guidelines • Case Studies • Collaborative learning (Regional or Specialty) • ERAS: Enhanced Recovery After Surgery in NSQIP • NSQIP Annual Conference Best Practice Guidelines • Complete yet concise resource for health care providers and QI professionals • Evidence-based • Expert panel-rated • Framework to: • Prevent postsurgical complications • Prioritize/direct QI efforts aimed at reducing incidence/impact of postsurgical complications Best Practice Case Studies Surgeon Champion Toolkit Recent Publications • American University of Beirut Medical Center, Beirut, Lebanon Postoperative outcomes after laparoscopic splenectomy compared with open splenectomy. Musallam KM, Khalife M, Sfeir PM, Faraj W, Safadi B, Abi Saad GS, Abiad F, Hallal A, Alwan MB, Peyvandi F, Jamali FR.Ann Surg. 2013 Jun;257(6):1116-23. doi: 10.1097/SLA.0b013e318275496a. [PubMed - in process] • Vancouver General Hospital, Vancouver, British Columbia Surgical-site infections within 60 days of coronary artery by-pass graft surgery. Swenne CL, et al.; Society of Thoracic Surgeons. Adult Cardiac Surgery Database Executive Summary. Available at: http://www.sts.org/sites/default/files/documents/20112ndHarvestExecutiveSummary.pdf . Accessed July 27, 2014. • Sheikh Khalifa Medical City, Abu Dhabi, United American Emirates Are results of bariatric surgery different in the Middle East? Early experience of an international bariatric surgery program and an ACS NSQIP outcomes comparison. Nimeri A, Mohamed A, El Hassan E, McKenna K, Turrin NP, Al Hadad M, Dehni N. J Am Coll Surg. 2013 Apr 23. doi:pii: S1072-7515(13)00160-9. 10.1016/j.jamcollsurg.2013.01.063. [Epub ahead of print] Surgical Risk Calculator http://riskcalculator.facs.org/ 2 ACS NSQIP National Conference ACS NSQIP Options Four Adult ACS NSQIP options 1. 2. 3. 4. ACS NSQIP Essentials ACS NSQIP Small & Rural ACS NSQIP Procedure Targeted ACS NSQIP Measures ACS NSQIP Pediatric The Options Regardless of Which Option, All Hospitals Will Receive: • • • • • • Interim and Semi Annual Reports Real Time Online Reports (including new SPCs) Benchmarking ACS NSQIP Best Practices/Guidelines ACS NSQIP Improvement Case Studies Additional Items (e.g. Risk Calculator, Public Use File) The Options For All Options, the Rigor and Validity of ACS NSQIP is Unchanged • • • • • • Risk Adjustment 30 Day Follow Up Clinical Data Data Audits SCR Training SCR Certification ACS NSQIP Essentials • General/Vascular = 1,680 cases per year, 8-day sampling cycle • Multispecialty = 20% total case volume by specialty, 8-day sampling cycle • Collection of core variables for QI purposes – approximately 46 clinical variables • 1 FTE ACS NSQIP Small & Rural • • Small Hospital: < 1,680 cases per year 100% collection of cases across all specialties • Collection of core variables for QI purposes – approximately 46 clinical variables • 1 FTE (or less depending upon case volume) ACS NSQIP Procedure Targeted • Larger hospitals targeting high-risk/high volume procedures • Hospital selects procedures • Selection may be CPT code-driven • Minimum of 1,680 cases per year: - 15 “Core” cases per 8-day cycle - 25 “Procedure Targeted” cases per 8-day cycle • Minimum 1 FTE (or more depending on volume) ACS NSQIP Procedure Targeted Nine Subspecialties • • • • • • • • • General Surgery Vascular Gynecologic Urologic Plastic & Reconstructive Surgery Otolaryngology Orthopedic Surgery Neurosurgery Thoracic Surgery ACS NSQIP Procedure Targeted 30+ Procedures Pancreatectomy▪ Colectomy ▪ Ventral Hernia Repair ▪ Bariatric ▪ Proctectomy ▪ Hepatectomy ▪ Thyroidectomy ▪ Esophagectomy ▪ Appendectomy ▪ Cartoid Endarterectomy ▪ Cartoid Artery Stenting ▪ Open AAA Repair ▪ EVAR ▪ Open Aortoiliac Bypass ▪ Endo Aortoiliac Repair ▪ Lower Extremity Open Bypass ▪ Lower Extremity Repair Endovascular ▪ Hysterectomy ▪ Myomectomy ▪ Reconstructive Procedures ▪ TURP ▪ Bladder Suspension ▪ Radial Prostatectomy ▪ Radical Nephrectomy ▪ Radical Cystectomy ▪ Muscle/Myocutaneous Flap ▪ Reduction Mammoplasty ▪ Breast Reconstruction ▪ Abdominoplasty ▪ Thyroidectomy ▪ Total Hip Arthroplasty ▪ Total Knee Arthroplasty ▪ Spine Surgery ▪ Hip Fracture ▪ Brain Tumor Procedure ▪Spine Procedure ▪ Lung Resection ACS NSQIP Measures • 5 High Impact Outcome Measures: - UTI - Colorectal - SSI - Lower Extremity Bypass - Elderly • Minimal Data Collection = 840 cases annually • Collection of ~25 clinical variables • 1/2 FTE ACS NSQIP Peds • >100 Clinical Variables - Demographics - Surgical Profile - Pre-Operative Data (risk factors) - Intra-Operative Data - Post-Operative Data (outcomes) • Patients under 18 years of age • Additional data points for neonates for a minimum of 28 days old SCR Staffing Requirements Program Option Pricing Recognition Institute of Medicine named ACS NSQIP “the best in the nation” for measuring & reporting surgical quality and outcomes. Thank You: Questions & Discussion Gina M. Pope RN, CNOR Business Development Representative [email protected] 312-202-5607 Additional Program Details Surgery: 100 Years of Quality Improvement >80% hospitals improve, including top USN&WR Minimum Standard for Hospitals Joint Commission 2004 2011 2012 1951 1913 1922 1950 1998 TQIP COMMITTEE ON TRAUMA 80% of incident cancers; 1500+ hospitals Trauma center designations, ATLS, 400+ hospitals SSR Improved safety and survival; 800+ hospitals Individual surgeon registry: endorsed for MOC (ABS, ABCRS), PQRS (CMS), OPPE (JC); 5000+ surgeon users Clinical Variables Participation Options for All Hospitals Risk Adjustment Risk adjustment has a profound effect in determining the true performance of a medical center 01 01 04 04 08 Rank by unadjusted Mortality A B 08 12 12 16 16 20 20 24 24 28 28 32 32 36 B 40 44 Rank by risk-adjusted Mortality 36 A 40 44 Changes in Medical Center Rank After Risk Adjustment For 30-Day Mortality Customer Support • Outcome Sciences/Quintiles: vendor support • ACS NSQIP: Clinical support; administrative – Staff of 50+ in ACS NSQIP Reporting Pre-Operative Risk Factor Summary System Case Study: Kaiser Permanente Zero Pneumonia Project • Based on ACS NSQIP data, implemented post-op pneumonia bundle in Kaiser Northern California • Cross-functional team • Clinical, cultural and patient education issues identified • Achieved zero pneumonia and now among top performers for this measure in ACS NSQIP • Expect to save 200 lives/yr Fuchshuber, PR, et al. The Power of the National Surgical Quality Improvement Program—Achieving A Zero Pneumonia Rate in General Surgery Patients. The Permanente Journal/ Winter 2012/ Volume 16 No. 1. 2
© Copyright 2026